FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Riluzole tablets is indicated for the treatment of amyotrophic lateral sclerosis (ALS).
2 DOSAGE AND ADMINISTRATION
The recommended dosage for riluzole tablets is 50 mg taken orally twice daily. Riluzole tablets should be taken at least 1 hour before or 2 hours after a meal [see Clinical Pharmacology ( 12.3)] .
Measure serum aminotransferases before and during treatment with riluzole tablets [see Warnings and Precautions ( 5.1)].
3 DOSAGE FORMS AND STRENGTHS
Tablets: 50mg white to off-white, film-coated, capsule-shaped and engraved with “795” on one side, plain on the other.
4 CONTRAINDICATIONS
Riluzole tablets is contraindicated in patients with a history of severe hypersensitivity reactions to riluzole or to any of its components (anaphylaxis has occurred) [see Adverse Reactions ( 6.1)] .
5 WARNINGS AND PRECAUTIONS
5.1 Hepatic Injury
Cases of drug-induced liver injury, some of which were fatal, have been reported in patients taking riluzole tablets. Asymptomatic elevations of hepatic transaminases have also been reported, and in some patients have recurred upon rechallenge with riluzole tablets.
In clinical studies, the incidence of elevations in hepatic transaminases was greater in riluzole-treated patients than placebo-treated patients. The incidence of elevations of ALT above 5 times the upper limit of normal (ULN) was 2% in riluzole -treated patients. Maximum increases in ALT occurred within 3 months after starting riluzole tablets. About 50% and 8% of riluzole-treated patients in pooled Studies 1 and 2, had at least one elevated ALT level above ULN and above 3 times ULN, respectively [see Clinical Studies ( 14)].
Monitor patients for signs and symptoms of hepatic injury, every month for the first 3 months of treatment, and periodically thereafter. The use of riluzole tablets is not recommended if patients develop hepatic transaminases levels greater than 5 times the ULN. Discontinue riluzole tablets if there is evidence of liver dysfunction (e.g., elevated bilirubin).
6 ADVERSE REACTIONS
The following adverse reactions are described below and elsewhere in the labeling:
- Hepatic Injury [see Warnings and Precautions ( 5.1)]
- Neutropenia [see Warnings and Precautions ( 5.2)]
- Interstitial lung disease [see Warnings and Precautions ( 5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adverse Reactions in Controlled Clinical Trials
In the placebo-controlled clinical trials in patients with ALS (Study 1 and 2), a total of 313 patients received riluzole tablets 50 mg twice daily [see Clinical Studies ( 14)] . The most common adverse reactions in the riluzole group (in at least 5% of patients and more frequently than in the placebo group) were asthenia, nausea, dizziness, decreased lung function, and abdominal pain. The most common adverse reactions leading to discontinuation in the riluzole group were nausea, abdominal pain, constipation, and elevated ALT.
There was no difference in rates of adverse reactions leading to discontinuation in females and males. However, the incidence of dizziness was higher in females (11%) than in males (4%). The adverse reaction profile was similar in older and younger patients. There were insufficient data to determine if there were differences in the adverse reaction profile in different races.
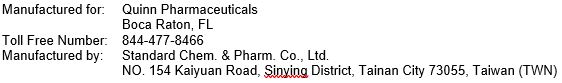
Table 1 lists adverse reactions that occurred in at least 2% of riluzole-treated patients (50 mg twice daily) in pooled Study 1 and 2, and at a higher rate than placebo.
Table 1. Adverse Reactions in Pooled Placebo-Controlled Trials (Studies 1 and 2) in Patients with ALS
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of riluzole tablets. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Acute hepatitis and icteric toxic hepatitis [see Warnings and Precautions ( 5.1)]
- Renal tubular impairment
- Pancreatitis
7 DRUG INTERACTIONS
7.1 Agents that may Increase Riluzole Blood Concentrations
CYP1A2 inhibitors
Co-administration of riluzole (a CYP1A substrate) with CYP1A2 inhibitors was not evaluated in a clinical trial; however, in vitro findings suggest an increase in riluzole exposure is likely. The concomitant use of strong or moderate CYP1A2 inhibitors (e.g., ciprofloxacin, enoxacin, fluvoxamine, methoxsalen, mexiletine, oral contraceptives, thiabendazole, vemurafenib, zileuton) with riluzole may increase the risk of riluzole-associated adverse reactions [see Clinical Pharmacology ( 12.3)] .
7.2 Agents that may Decrease Riluzole Plasma Concentrations
CYP1A2 inducers
Co-administration of riluzole (a CYP1A substrate) with CYP1A2 inducers was not evaluated in a clinical trial; however, in vitro findings suggest a decrease in riluzole exposure is likely. Lower exposures may result in decreased efficacy [see Clinical Pharmacology ( 12.3)] .
7.3 Hepatotoxic Drugs
Clinical trials in ALS patients excluded patients on concomitant medications which were potentially hepatotoxic (e.g., allopurinol, methyldopa, sulfasalazine). Riluzole-treated patients who take other hepatotoxic drugs may be at an increased risk for hepatotoxicity [see Warnings and Precautions ( 5.1)] .
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no studies of riluzole in pregnant women, and case reports have been inadequate to inform the drug-associated risk. The background risk for major birth defects and miscarriage in patients with amyotrophic lateral sclerosis is unknown. In the U.S. general population, the background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
In studies in which riluzole was administered orally to pregnant animals, developmental toxicity (decreased embryofetal/offspring viability, growth, and functional development) was observed at clinically relevant doses [see Data]. Based on these results, women should be advised of a possible risk to the fetus associated with use of riluzole during pregnancy.
Data
Animal Data
Oral administration of riluzole (3, 9, or 27 mg/kg/day) to pregnant rats during the period of organogenesis resulted in decreases in fetal growth (body weight and length) at the high dose. The mid dose, a no-effect dose for embryofetal developmental toxicity, is approximately equal to the recommended human daily dose (RHDD, 100 mg) on a mg/m 2 basis. When riluzole was administered orally (3, 10, or 60 mg/kg/day) to pregnant rabbits during the period of organogenesis, embryofetal mortality was increased at the high dose and fetal body weight was decreased and morphological variations increased at all but the lowest dose tested. The no-effect dose (3 mg/kg/day) for embryofetal developmental toxicity is less than the RHDD on a mg/m 2 basis. Maternal toxicity was observed at the highest dose tested in rat and rabbit.
When riluzole was orally administered (3, 8, or 15 mg/kg/day) to male and female rats prior to and during mating and to female rats throughout gestation and lactation, increased embryofetal mortality and decreased postnatal offspring viability, growth, and functional development were observed at the high dose. The mid dose, a no-effect dose for pre-and postnatal developmental toxicity, is approximately equal to the RHDD on a mg/m 2 basis.
8.2 Lactation
Risk Summary
It is not known if riluzole is excreted in human milk. Riluzole or its metabolites have been detected in milk of lactating rat. Women should be advised that many drugs are excreted in human milk and that the potential for serious adverse reactions in nursing infants from riluzole is unknown.
8.3 Females and Males of Reproductive Potential
In rats, oral administration of riluzole resulted in decreased fertility indices and increases in embryolethality [see Nonclinical Toxicology ( 13.1)] .
8.4 Pediatric Use
Safety and effectiveness of riluzole tablets in pediatric patients have not been established.
8.5 Geriatric Use
In clinical studies of riluzole tablets, 30% of patients were 65 years and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
Patients with mild [Child-Pugh's (CP) score A] or moderate (CP score B) hepatic impairment had increases in AUC compared to patients with normal hepatic function. Thus, patients with mild or moderate hepatic impairment may be at increased of adverse reactions. The impact of severe hepatic impairment on riluzole exposure is unknown.
Use of riluzole tablets is not recommended in patients with baseline elevation of elevations of serum aminotransferases greater than 5 times upper limit of normal or evidence of liver dysfunction (e.g., elevated bilirubin) [Clinical Pharmacology ( 12.3)] .
8.7 Japanese Patients
Japanese patients are more likely to have higher riluzole concentrations. Consequently, the risk of adverse reactions may be greater in Japanese patients [see Clinical Pharmacology ( 12.3)] .
10 OVERDOSAGE
Reported symptoms of overdose following ingestion of riluzole ranging from 1.5 to 3 grams (30 to 60 times the recommended dose) included acute toxic encephalopathy, coma, drowsiness, memory loss, and methemoglobinemia.
No specific antidote for the treatment of riluzole overdose is available. For current information on the management of poisoning or overdosage, contact the National Poison Control Center at 1-800-222-1222 or www.poison.org.
11 DESCRIPTION
Riluzole is a member of the benzothiazole class. The chemical designation for riluzole is 2-amino-6-(trifluoromethoxy)benzothiazole. Its molecular formula is C 8H 5F 3N 2OS, and its molecular weight is 234.2. The chemical structure is:
Riluzole is a white to slightly yellow powder that is very soluble in dimethylformamide, dimethylsulfoxide, and methanol; freely soluble in dichloromethane; sparingly soluble in 0.1 N HCl; and very slightly soluble in water and in 0.1 N NaOH.
Each film-coated tablet for oral use contains 50 mg of riluzole and the following inactive ingredients: dibasic calcium phosphate anhydrous, microcrystalline cellulose, colloidal silicon dioxide, magnesium stearate, croscarmellose sodium, hypromellose, lactose monohydrate, titanium dioxide, triacetin, citric acid monohydrate.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism by which riluzole exerts its therapeutic effects in patients with ALS is unknown.
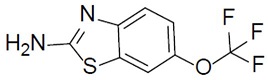
12.3 Pharmacokinetics
Table 2 displays the pharmacokinetic parameters of riluzole.
Specific Populations
Hepatic Impairment
Compared with healthy volunteers, the AUC of riluzole was approximately 1.7-fold greater in patients with mild chronic hepatic impairment (CP score A) and approximately 3-fold greater in patients with moderate chronic hepatic impairment (CP score B). The pharmacokinetics of riluzole have not been studied in patients with severe hepatic impairment (CP score C) [see Use in Specific Populations ( 8.6)] .
Race
The clearance of riluzole was 50% lower in male Japanese subjects than in Caucasian subjects, after normalizing for body weight [see Use in Specific Populations ( 8.7)] .
Gender
The mean AUC of riluzole was approximately 45% higher in female patients than male patients.
Smokers
The clearance of riluzole in tobacco smokers was 20% greater than in nonsmokers.
Geriatric Patients and Patients with Moderate to Severe Renal Impairment
Age 65 years or older, and moderate to severe renal impairment do not have a meaningful
effect on the pharmacokinetics of riluzole. The pharmacokinetics of riluzole in patients
undergoing hemodialysis are unknown.
Drug Interaction Studies
Drugs Highly Bound To Plasma Proteins
Riluzole and warfarin are highly bound to plasma proteins. In vitro, riluzole did not show
any displacement of warfarin from plasma proteins. Riluzole binding to plasma proteins was
unaffected by warfarin, digoxin, imipramine and quinine at high therapeutic concentrations
in vitro.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Riluzole was not carcinogenic in mice or rats when administered for 2 years at daily oral doses up to 20 and 10 mg/kg/day, respectively, which are approximately equal to the recommended human daily dose (RHDD, 100 mg) on a mg/ m 2 basis.
Mutagenesis
Riluzole was negative in in vitro (bacterial reverse mutation (Ames), mouse lymphoma tk, chromosomal aberration assay in human lymphocytes), and in vivo (rat cytogenetic and mouse micronucleus) assays.
N-hydroxyriluzole, the major active metabolite of riluzole, was positive for clastogenicity in the in vitro mouse lymphoma tk assay and in the in vitro micronucleus assay using the same mouse lymphoma cell line. N-hydroxyriluzole was negative in the HPRT gene mutation assay, the Ames assay (with and without rat or hamster S9), the in vitro chromosomal aberration assay in human lymphocytes, and the in vivo mouse micronucleus assay.
Impairment of Fertility
When riluzole (3, 8, or 15 mg/kg) was administered orally to male and female rats prior to and during mating and continuing in females throughout gestation and lactation, fertility indices were decreased and embryolethality was increased at the high dose. This dose was also associated with maternal toxicity. The mid dose, a no-effect dose for effects on fertility and early embryonic development, is approximately equal to the RHDD on a mg/m 2 basis.
14 CLINICAL STUDIES
The efficacy of riluzole tablets was demonstrated in two studies (Study 1 and 2) that evaluated riluzole tablets 50 mg twice daily in patients with amyotrophic lateral sclerosis (ALS). Both studies included patients with either familial or sporadic ALS, a disease duration of less than 5 years, and a baseline forced vital capacity greater than or equal to 60% of normal.
Study 1 was a randomized, double-blind, placebo-controlled clinical study that enrolled 155 patients with ALS. Patients were randomized to receive riluzole 50 mg twice daily (n=77) or placebo (n=78) and were followed for at least 13 months (up to a maximum duration of 18 months). The clinical outcome measure was time to tracheostomy or death.
The time to tracheostomy or death was longer for patients receiving riluzole compared to placebo. There was an early increase in survival in patients receiving riluzole compared to placebo. Figure 1 displays the survival curves for time to death or tracheostomy. The vertical axis represents the proportion of individuals alive without tracheostomy at various times following treatment initiation (horizontal axis). Although these survival curves were not statistically significantly different when evaluated by the analysis specified in the study protocol (Logrank test p=0.12), the difference was found to be significant by another appropriate analysis (Wilcoxon test p=0.05). As seen in Figure 1, the study showed an early increase in survival in patients given riluzole. Among the patients in whom the endpoint of tracheostomy or death was reached during the study, the difference in median survival between the riluzole 50 mg twice daily and placebo groups was approximately 90 days.
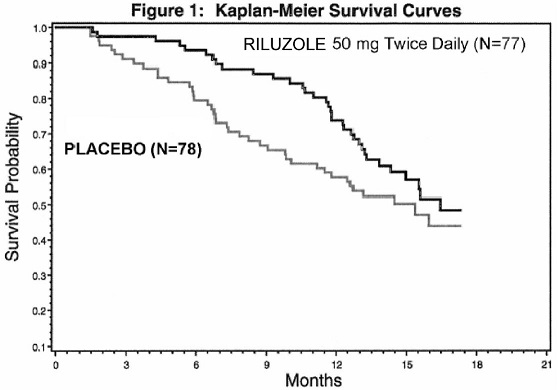
Figure 1. Time to Tracheostomy or Death in ALS Patients in Study 1 (Kaplan-Meir Curves)
Study 2 was a randomized, double-blind, placebo-controlled clinical study that enrolled 959 patients with ALS. Patients were randomized to riluzole 50 mg twice daily (n=236) or placebo (n=242) and were followed for at least 12 months (up to a maximum duration of 18 months). The clinical outcome measure was time to tracheostomy or death.
The time to tracheostomy or death was longer for patients receiving riluzole compared to placebo. Figure 2 displays the survival curves for time to death or tracheostomy for patients randomized to either riluzole 100 mg per day or placebo. Although these survival curves were not statistically significantly different when evaluated by the analysis specified in the study protocol (Logrank test p=0.076), the difference was found to be significant by another appropriate analysis (Wilcoxon test p=0.05). Not displayed in Figure 2 are the results of riluzole 50 mg per day (one-half of the recommended daily dose), which could not be statistically distinguished from placebo, or the results of riluzole 200 mg per day (two times the recommended daily dose), which were not distinguishable from the 100 mg per day results. Among the patients in whom the endpoint of tracheostomy or death was reached during the study, the difference in median survival between riluzole and placebo was approximately 60 days.
Although riluzole improved survival in both studies, measures of muscle strength and neurological function did not show a benefit.
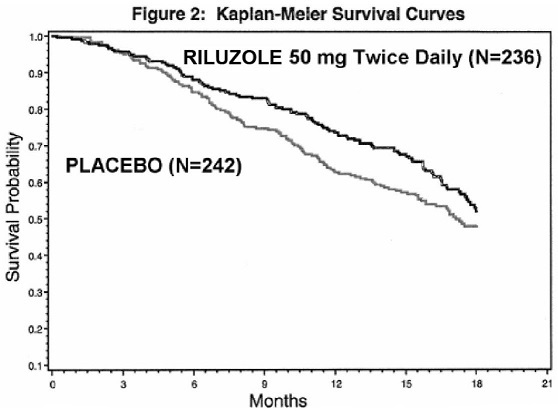
Figure 2. Time to Tracheostomy or Death in ALS Patients in Study 2 (Kaplan-Meir Curves)”
16 HOW SUPPLIED/STORAGE AND HANDLING
Riluzole Tablets, USP 50 mg are white to off-white, film-coated, capsule-shaped and engraved with “795” on one side, plain on the other. Riluzole is supplied in bottles of 60 tablets, NDC 69076-200-60.
Store at 20º to 25ºC (68º to 77ºF) [See USP Controlled Room Temperature]. Protect from bright light.
17 PATIENT COUNSELING INFORMATION
Advise patients to inform their healthcare provider if they experience:
- Yellowing of the whites of the eyes [see Warnings and Precautions ( 5.1)]
- Fever [see Warnings and Precautions ( 5.2)]
- Respiratory symptomsfor example, dry cough and difficult or labored breathing [see Warnings and Precautions ( 5.3)]