FULL PRESCRIBING INFORMATION
WARNING: ADDICTION, ABUSE, AND MISUSE; RISK EVALUATION AND MITIGATION STRATEGY (REMS); LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS; ULTRA-RAPID METABOLISM OF CODEINE AND OTHER RISK FACTORS FOR LIFE-THREATENING RESPIRATORY DEPRESSION IN CHILDREN; NEONATAL OPIOID WITHDRAWL SYNDROME; and INTERACTIONS WITH DRUGS AFFECTING CYTOCHROME P450 ISOENZYMES
- •
- Addiction, Abuse, and Misuse ASCOMP with CODEINE exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient’s risk prior to prescribing ASCOMP with CODEINE, and monitor all patients regularly for the development of these behaviors and conditions [see Warnings and Precautions (5.1)].
- •
- Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
- To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse and misuse, the Food and Drug Administration (FDA) has required a REMS for these products [see Warnings and Precautions (5.2)]. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant educations programs available to healthcare providers. Healthcare providers are strongly encouraged to do all of the following:
- •
- complete a REMS-compliant education program,
- •
- counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products,
- •
- emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist, and
- •
- consider other tools to improve patient, household, and community safety.
- •
- Life-Threatening Respiratory Depression Serious, life-threatening, or fatal respiratory depression may occur with use of ASCOMP with CODEINE. Monitor for respiratory depression, especially during initiation of ASCOMP with CODEINE or following a dose increase [see Warnings and Precautions (5.3)].
- •
- Accidental Ingestion Accidental ingestion of even one dose of ASCOMP with CODEINE, especially by children, can result in a fatal overdose of ASCOMP with CODEINE [see Warnings and Precautions (5.3)].
- •
- Risks From Concomitant Use With Benzodiazepines Or Other CNS Depressants Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death [see Warnings and Precautions (5.4, 5.8), Drug Interactions (7)].
- •
- Reserve concomitant prescribing of ASCOMP with CODEINE and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate.
- •
- Limit dosages and durations to the minimum required.
- •
- Follow patients for signs and symptoms of respiratory depression and sedation.
- •
- Ultra-Rapid Metabolism of Codeine and Other Risk Factors for Life-Threatening Respiratory Depression in Children Life-threatening respiratory depression and death have occurred in children who received codeine. Most of the reported cases occurred following tonsillectomy and/or adenoidectomy, and many of the children had evidence of being an ultra-rapid metabolizer of codeine due to a CYP2D6 polymorphism. [see Warnings and Precautions (5.5)]. ASCOMP with CODEINE is contraindicated in children younger than 12 years of age and in children younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Contraindications (4)]. Avoid the use of ASCOMP with CODEINE in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of codeine.
- •
- Neonatal Opioid Withdrawal Syndrome Prolonged use of ASCOMP with CODEINE during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Warnings and Precautions (5.6)].
- •
- Interactions with Drugs Affecting Cytochrome P450 Isoenzymes The effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with codeine are complex. Use of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with ASCOMP with CODEINE requires careful consideration of the effects on codeine, and the active metabolite, morphine [see Warnings and Precautions (5.7, 5.8), Drug Interactions (7)].
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosage and Administration Instructions
Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
Initiate the dosing regimen for each patient individually, taking into account the patient's severity of pain, patient response, prior analgesic treatment experience, and risk factors for addiction, abuse, and misuse [see Warnings and Precautions (5.1)].
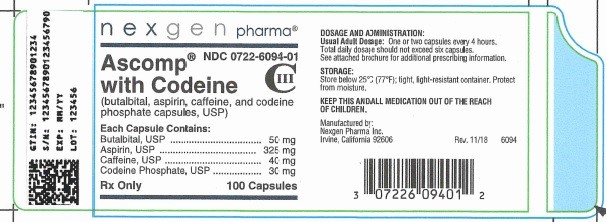
3 DOSAGE FORMS AND STRENGTHS
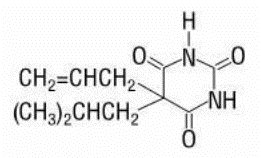
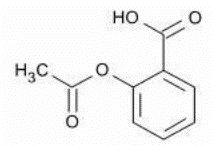
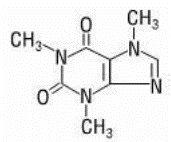
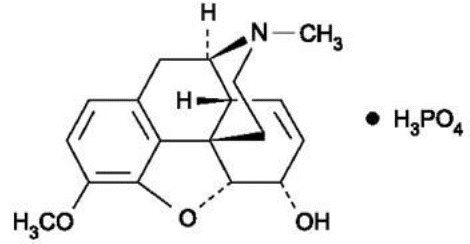
Capsules: Butalbital, 50 mg, Aspirin, 325 mg, Caffeine, 40 mg, Codeine Phosphate, 30 mg
Blue cap with a yellow body. Body is imprinted with "B 074" in black ink.
4 CONTRAINDICATIONS
ASCOMP with CODEINE is contraindicated for:
- •
- All children younger than 12 years of age [see Warnings and Precautions (5.4)]
- •
- Postoperative management in children younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Warnings and Precautions (5.5)].
ASCOMP with CODEINE is also contraindicated in patients with:
- •
- Significant respiratory depression [see Warnings and Precautions (5.8)]
- •
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions (5.8)]
- •
- Concurrent use of monoamine oxidase inhibitors (MAOIs) or use of MAOIs within the last 14 days [see Warnings and Precautions (5.9)/Drug Interactions (7)].
- •
- Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions (5.13)]
- •
- Hypersensitivity or intolerance to aspirin, caffeine, butalbital, or codeine.
- •
- Hemophilia [see Warnings and Precautions (5.17)]
- •
- Reye’s Syndrome [see Warnings and Precautions (5.18)]
- •
- Known allergy to nonsteroidal anti-inflammatory drugs (NSAIDs) [see Warnings and Precautions (5.19)]
- •
- Syndrome of asthma, rhinitis, and nasal polyps [see Warnings and Precautions (5.19)]
5 WARNINGS AND PRECAUTIONS
5.1 Addiction, Abuse, and Misuse
ASCOMP with CODEINE contains codeine. Codeine in combination with butalbital, aspirin, and caffeine is a Schedule III controlled substance. As ASCOMP with CODEINE contains butalbital and codeine, it exposes users to the risks of addiction, abuse, and misuse [see Drug Abuse and Dependence (9)].
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed ASCOMP with CODEINE. Addiction can occur at recommended dosages and if the drug is misused or abused.
Assess each patient’s risk for addiction, abuse, or misuse prior to prescribing ASCOMP with CODEINE, and monitor all patients receiving ASCOMP with CODEINE for the development of these behaviors and conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the proper management of pain in any given patient. Patients at increased risk may be prescribed opioids such as ASCOMP with CODEINE but use in such patients necessitates intensive counseling about the risks and proper use of ASCOMP with CODEINE along with intensive monitoring for signs of addiction, abuse, and misuse.
Opioids and barbiturates are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing ASCOMP with CODEINE. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on the proper disposal of unused drug [see Patient Counseling Information (17)]. Contact local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
5.2 Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS)
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the Food and Drug Administration (FDA) has required a Risk Evaluation and Mitigation Strategy (REMS) for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to healthcare providers. Healthcare providers are strongly encouraged to do all of the following:
- •
- Complete a REMS-compliant education program offered by an accredited provider of continuing education (CE) or another education program that includes all the elements of the FDA Education Blueprint for Health Care Providers Involved in the Management or Support of Patients with Pain.
- •
- Discuss the safe use, serious risks, and proper storage and disposal of opioid analgesics with patients and/or their caregivers every time these medicines are prescribed. The Patient Counseling Guide (PCG) can be obtained at this link: www.fda.gov/OpioidAnalgesicREMSPCG.
- •
- Emphasize to patients and their caregivers the importance of reading the Medication Guide that they will receive from their pharmacist every time an opioid analgesic is dispensed to them.
- •
- Consider using other tools to improve patient, household, and community safety, such as patient-prescriber agreements that reinforce patient-prescriber responsibilities.
To obtain further information on the opioid analgesic REMS and for a list of accredited REMS CME/CE, call 1-800-503-0784, or log on to www.opioidanalgesicrems.com. The FDA Blueprint can be found at www.fda.gov/OpioidAnalgesicREMSBlueprint.
5.3 Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient’s clinical status [see Overdosage (10)]. Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of ASCOMP with CODEINE, the risk is greatest during the initiation of therapy or following a dosage increase.
Monitor patients closely for respiratory depression, especially within the first 24-72 hours of initiating therapy with and following dosage increases of ASCOMP with CODEINE.
To reduce the risk of respiratory depression, proper dosing and titration of ASCOMP with CODEINE are essential [see Dosage and Administration (2.1)]. Overestimating the ASCOMP with CODEINE dosage when converting patients from another opioid product can result in a fatal overdose with the first dose.
Accidental ingestion of ASCOMP with CODEINE, especially by children, can result in respiratory depression and death due to an overdose of codeine and butalbital.
Opioids can cause sleep-related breathing disorders including central sleep apnea (CSA) and sleep-related hypoxemia. Opioid use increases the risk of CSA in a dose-dependent fashion. In patients who present with CSA, consider decreasing the opioid dosage using best practices for opioid taper [see Dosage and Administration (2.3)].
5.4 Risks from Concomitant Use with Benzodiazepines or Other CNS Depressants
Profound sedation, respiratory depression, coma, and death may result from the concomitant use of ASCOMP with CODEINE with benzodiazepines or other CNS depressants (e.g., non-benzodiazepine sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol). Because of these risks, reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioid analgesics alone. Because of similar pharmacological properties, it is reasonable to expect similar risk with the concomitant use of other CNS depressant drugs with opioid analgesics [see Drug Interactions (7)].
If the decision is made to prescribe a benzodiazepine or other CNS depressant concomitantly with an opioid analgesic, prescribe the lowest effective dosages and minimum durations of concomitant use. In patients already receiving an opioid analgesic, prescribe a lower initial dose of the benzodiazepine or other CNS depressant than indicated in the absence of an opioid, and titrate based on clinical response. If an opioid analgesic is initiated in a patient already taking a benzodiazepine or other CNS depressant, prescribe a lower initial dose of the opioid analgesic, and titrate based on clinical response. Follow patients closely for signs and symptoms of respiratory depression and sedation.
Advise both patients and caregivers about the risks of respiratory depression and sedation when ASCOMP with CODEINE is used with benzodiazepines or other CNS depressants (including alcohol and illicit drugs). Advise patients not to drive or operate heavy machinery until the effects of concomitant use of the benzodiazepine or other CNS depressant have been determined. Screen patients for risk of substance use disorders, including opioid abuse and misuse, and warn them of the risk for overdose and death associated with the use of additional CNS depressants including alcohol and illicit drugs [see Drug Interactions (7) and Patient Counseling Information (17)].
5.5 Ultra-Rapid Metabolism of Codeine and Other Risk Factors for Life-Threatening Respiratory Depression in Children
Life-threatening respiratory depression and death have occurred in children who received codeine. Codeine is subject to variability in metabolism based upon CYP2D6 genotype (described below), which can lead to an increased exposure to the active metabolite morphine. Based upon postmarketing reports, children younger than 12 years old appear to be more susceptible to the respiratory depressant effects of codeine, particularly if there are risk factors for respiratory depression. For example, many reported cases of death occurred in the postoperative period following tonsillectomy and/or adenoidectomy, and many of the children had evidence of being ultra-rapid metabolizers of codeine. Furthermore, children with obstructive sleep apnea who are treated with codeine for post-tonsillectomy and/or adenoidectomy pain may be particularly sensitive to its respiratory depressant effect. Because of the risk of life-threatening respiratory depression and death:
- •
- ASCOMP with CODEINE is contraindicated for all children younger than 12 years of age [see Contraindications (4)].
- •
- ASCOMP with CODEINE is contraindicated for post-operative management in pediatric patients younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Contraindications (4)].
- •
- Avoid the use of ASCOMP with CODEINE in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of codeine unless the benefits outweigh the risks. Risk factors include conditions associated with hypoventilation, such as postoperative status, obstructive sleep apnea, obesity, severe pulmonary disease, neuromuscular disease, and concomitant use of other medications that cause respiratory depression.
- •
- As with adults, when prescribing ASCOMP with CODEINE for adolescents, healthcare providers should choose the lowest effective dose for the shortest period of time and inform patients and caregivers about these risks and the signs of morphine overdose [see Use in Specific Populations (8.4), Overdosage (10)]
Nursing Mothers
At least one death was reported in a nursing infant who was exposed to high levels of morphine in breast milk because the mother was an ultra-rapid metabolizer of codeine. Breastfeeding is not recommended during treatment with ASCOMP with CODEINE [see Use in Specific Populations (8.2)].
CYP2D6 Genetic Variability: Ultra-rapid metabolizer
Some individuals may be ultra-rapid metabolizers because of a specific CYP2D6 genotype (gene duplications denoted as *1/*1xN or *1/*2xN). The prevalence of this CYP2D6 phenotype varies widely and has been estimated at 1 to 10% for Whites (European, North American), 3 to 4% for Blacks (African Americans), 1 to 2% for East Asians (Chinese, Japanese, Korean), and may be greater than 10% in certain racial/ethnic groups (i.e., Oceanian, Northern African, Middle Eastern, Ashkenazi Jews, Puerto Rican).
These individuals convert codeine into its active metabolite, morphine, more rapidly and completely than other people. This rapid conversion results in higher than expected serum morphine levels. Even at labeled dosage regimens, individuals who are ultra-rapid metabolizers may have life-threatening or fatal respiratory depression or experience signs of overdose (such as extreme sleepiness, confusion, or shallow breathing) [see Overdosage (10)]. Therefore, individuals who are ultra-rapid metabolizers should not use ASCOMP with CODEINE.
5.6 Neonatal Opioid Withdrawal Syndrome
Prolonged use of ASCOMP with CODEINE during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for a prolonged period of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Use in Specific Populations (8.1, 8.2), Patient Counseling Information (17)].
5.7 Risks of Interactions with Drugs Affecting Cytochrome P450 Isoenzymes
The effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with codeine are complex. Use of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with ASCOMP with CODEINE requires careful consideration of the effects on codeine and the active metabolite, morphine.
Cytochrome P450 3A4 Interaction
The concomitant use of ASCOMP with CODEINE with all cytochrome P450 3A4 inhibitors, such as macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), and protease inhibitors (e.g., ritonavir) or discontinuation of a cytochrome P450 3A4 inducer such as rifampin, carbamazepine, and phenytoin, may result in an increase in codeine plasma concentrations with subsequently greater metabolism by cytochrome P450 2D6, resulting in greater morphine levels, which could increase or prolong adverse reactions and may cause potentially fatal respiratory depression.
The concomitant use of ASCOMP with CODEINE with all cytochrome P450 3A4 inducers or discontinuation of a cytochrome P450 3A4 inhibitor may result in lower codeine levels, greater norcodeine levels, and less metabolism via 2D6 with resultant lower morphine levels. This may be associated with a decrease in efficacy, and in some patients, may result in signs and symptoms of opioid withdrawal.
Follow patients receiving ASCOMP with CODEINE and any CYP3A4 inhibitor or inducer for signs and symptoms that may reflect opioid toxicity and opioid withdrawal when ASCOMP with CODEINE is used in conjunction with inhibitors and inducers of CYP3A4.
If concomitant use of a CYP3A4 inhibitor is necessary or if a CYP3A4 inducer is discontinued, consider dosage reduction of ASCOMP with CODEINE until stable drug effects are achieved. Monitor patients for respiratory depression and sedation at frequent intervals.
If concomitant use of a CYP3A4 inducer is necessary or if a CYP3A4 inhibitor is discontinued, consider increasing the ASCOMP with CODEINE dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. [see Drug Interactions (7)].
Risks of Concomitant Use or Discontinuation of Cytochrome P450 2D6 Inhibitors
The concomitant use of ASCOMP with CODEINE with all cytochrome P450 2D6 inhibitors (e.g., amiodarone, quinidine) may result in an increase in codeine plasma concentrations and a decrease in active metabolite morphine plasma concentration which could result in an analgesic efficacy reduction or symptoms of opioid withdrawal.
Discontinuation of a concomitantly used cytochrome P450 2D6 inhibitor may result in a decrease in codeine plasma concentration and an increase in active metabolite morphine plasma concentration which could increase or prolong adverse reactions and may cause potentially fatal respiratory depression.
Follow patients receiving ASCOMP with CODEINE and any CYP2D6 inhibitor for signs and symptoms that may reflect opioid toxicity and opioid withdrawal when ASCOMP with CODEINE are used in conjunction with inhibitors of CYP2D6.
If concomitant use with a CYP2D6 inhibitor is necessary, follow the patient for signs of reduced efficacy or opioid withdrawal and consider increasing the ASCOMP with CODEINE dosage. After stopping use of a CYP2D6 inhibitor, consider reducing the ASCOMP with CODEINE dosage and follow the patient for signs and symptoms of respiratory depression or sedation. [see Drug Interactions (7)].
5.8 Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of ASCOMP with CODEINE in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
Patients with Chronic Pulmonary Disease: ASCOMP with CODEINE-treated patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or pre-existing respiratory depression are at increased risk of decreased respiratory drive including apnea, even at recommended dosages of ASCOMP with CODEINE [see Warnings and Precautions (5.8)].
Elderly, Cachectic, or Debilitated Patients: Life-threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients because they may have altered pharmacokinetics or altered clearance compared to younger, healthier patients [see Warnings and Precautions (5.8)].
Monitor such patients closely, particularly when initiating and titrating ASCOMP with CODEINE and when ASCOMP with CODEINE is given concomitantly with other drugs that depress respiration [see Warnings and Precautions (5.3)]. Alternatively, consider the use of non-opioid analgesics in these patients.
5.9 Interaction with Monoamine Oxidase Inhibitors
Monoamine oxidase inhibitors (MAOIs) may potentiate the effects of morphine, codeine’s active metabolite, including respiratory depression, coma, and confusion. ASCOMP with CODEINE should not be used in patients taking MAOIs or within 14 days of stopping such treatment.
5.10 Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
5.11 Severe Hypotension
ASCOMP with CODEINE may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions (7)]. Monitor these patients for signs of hypotension after initiating or titrating the dosage of ASCOMP with CODEINE. In patients with circulatory shock, ASCOMP with CODEINE may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of ASCOMP with CODEINE in patients with circulatory shock.
5.12 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
In patients who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors), ASCOMP with CODEINE may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with ASCOMP with CODEINE.
Opioids may also obscure the clinical course in a patient with a head injury. Avoid the use of ASCOMP with CODEINE in patients with impaired consciousness or coma.
5.13 Risks of Use in Patients with Gastrointestinal Conditions Including Peptic Ulcer Disease
ASCOMP with CODEINE is contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
The codeine in ASCOMP with CODEINE may cause spasm of the sphincter of Oddi. Opioids may cause increases in serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis for worsening symptoms.
Patients with a history of active peptic ulcer disease should avoid using aspirin, which can cause gastric mucosal irritation and bleeding.
The aspirin in ASCOMP with CODEINE can cause GI side effects including stomach pain, heartburn, nausea, vomiting, and gross GI bleeding. Although minor upper GI symptoms, such as dyspepsia, are common and can occur anytime during therapy, physicians should remain alert for signs of ulceration and bleeding, even in the absence of previous GI symptoms. Physicians should inform patients about the signs and symptoms of GI side effects and what steps to take if they occur.
5.14 Increased Risk of Seizures in Patients with Seizure Disorders
The codeine in ASCOMP with CODEINE may increase the frequency of seizures in patients with seizure disorders and may increase the risk of seizures occurring in other clinical settings associated with seizures. Monitor patients with a history of seizure disorders for worsened seizure control during ASCOMP with CODEINE therapy.
5.15 Withdrawal
Do not abruptly discontinue ASCOMP with Codeine in a patient physically dependent on opioids. Rapid tapering of butalbital, aspirin, caffeine, and codeine phosphate capsules in a patient physically dependent on opioids may lead to a withdrawal syndrome and return of pain [see Dosage and Administration (2.3), Drug Abuse and Dependence (9.3)].
Additionally, avoid the use of mixed agonist/antagonist (e.g., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who are receiving a full opioid agonist analgesic, including ASCOMP with CODEINE. In these patients, mixed agonist/antagonist and partial agonist analgesics may reduce the analgesic effect and/or precipitate withdrawal symptoms. [see Drug Interactions (7)].
When discontinuing ASCOMP with CODEINE in a physically-dependent patient, gradually taper the dosage [see Dosage and Administration (2.3)]. Abrupt discontinuation of butalbital can cause seizures [see Drug Abuse and Dependence ( 9.3)].
5.16 Risks of Driving and Operating Machinery
ASCOMP with CODEINE may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of ASCOMP with CODEINE and know how they will react to the medication.
5.17 Coagulation Abnormalities and Bleeding Risks
Even low doses of aspirin can inhibit platelet function leading to an increase in bleeding time. This can adversely affect patients with inherited (i.e. hemophilia) or acquired (i.e. liver disease or vitamin K deficiency) bleeding disorders. Aspirin is contraindicated in patients with hemophilia.
Aspirin administered pre-operatively may prolong the bleeding time.
Patients who consume three or more alcoholic drinks every day should be counseled about the bleeding risks involved with chronic, heavy alcohol use while taking aspirin.
5.18 Reye’s Syndrome
Aspirin should not be used in children or teenagers for viral infections, with or without fever, because of the risk of Reye syndrome with concomitant use of aspirin in certain viral illnesses.
5.19 Allergy
Aspirin is contraindicated in patients with known allergy to nonsteroidal anti-inflammatory drug products (NSAIDs) and in patients with the syndrome of asthma, rhinitis, and nasal polyps. Aspirin may cause severe urticaria, angioedema, or bronchospasm (asthma).
5.20 Drug/Laboratory Test Interactions
Aspirin: Aspirin may interfere with the following laboratory determinations in blood: serum amylase, fasting blood glucose, cholesterol, protein, serum glutamic-oxalacetic transaminase (SGOT), uric acid, prothrombin time and bleeding time. Aspirin may interfere with the following laboratory determinations in urine: glucose, 5-hydroxy-indoleacetic acid, Gerhardt ketone, vanillylmandelic acid (VMA), uric acid, diacetic acid, and spectrophotometric detection of barbiturates.
Codeine: Codeine may increase serum amylase levels.
6 ADVERSE REACTIONS
The following serious adverse reactions are described, or described in greater detail, in other sections:
- •
- Addiction, Abuse, and Misuse [see Warnings and Precautions (5.1)]
- •
- Life-Threatening Respiratory Depression [see Warnings and Precautions (5.3)]
- •
- Interactions with Benzodiazepines or Other CNS Depressants [see Warnings and Precautions (5.4)
- •
- Ultra-Rapid Metabolism of Codeine and Other Risk Factors for Life-Threatening Respiratory Depression in Children [see Warnings and Precautions (5.5)]
- •
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.6)]
- •
- Adrenal Insufficiency [see Warnings and Precautions (5.10)]
- •
- Severe Hypotension [see Warnings and Precautions (5.11)]
- •
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.13)]
- •
- Seizures [see Warnings and Precautions (5.14)]
- •
- Withdrawal [see Warnings and Precautions (5.15)]
- •
- Coagulation Abnormalities and Bleeding [see Warnings and Precautions (5.17)]
- •
- Reye’s Syndrome [see Warnings and Precautions (5.18)]
- •
- Allergy [see Warnings and Precautions (5.19)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Incidence in Controlled Clinical Trials:
The following table summarizes the incidence rates of the adverse events reported by at least 1% of the Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules treated patients in controlled clinical trials comparing Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules to placebo, and provides a comparison to the incidence rates reported by the placebo-treated patients.
The prescriber should be aware that these figures cannot be used to predict the incidence of side effects in the course of usual medical practice where patient characteristics and other factors differ from those that prevailed in the clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigations involving different treatments, uses, and investigators.
|
Adverse Events Reported by at Least 1% of Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules Treated Patients During Placebo Controlled Clinical Trials Incidence Rate of Adverse Events |
||
|
Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules (N=382) |
Placebo (N =377) |
| ||
|
2.4% |
|
|
2.6% |
|
|
1.0% |
|
| ||
|
3.7% |
|
Other Adverse Events Reported During Controlled Clinical Trials
The listing that follows represents the proportion of the 382 patients exposed to Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules while participating in the controlled clinical trials who reported, on at least one occasion, an adverse event of the type cited. All reported adverse events, except those already presented in the previous table, are included. It is important to emphasize that, although the adverse events reported did occur while the patient was receiving Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules, the adverse events were not necessarily caused by Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules.
Adverse events are classified by body system and frequency. “Frequent” is defined as an adverse event which occurred in at least 1/100 (1%) of the patients; all adverse events listed in the previous table are frequent. “Infrequent” is defined as an adverse event that occurred in less than 1/100 patients but at least 1/1000 patients. All adverse events tabulated below are classified as infrequent.
Central Nervous: headache, shaky feeling, tingling, agitation, fainting, fatigue, heavy eyelids, high energy, hot spells, numbness, and sluggishness.
Autonomic Nervous: dry mouth and hyperhidrosis.
Gastrointestinal: vomiting, difficulty swallowing, and heartburn.
Cardiovascular: tachycardia.
Musculoskeletal: leg pain and muscle fatigue.
Genitourinary: diuresis.
Miscellaneous: pruritus, fever, earache, nasal congestion, and tinnitus.
The following adverse drug reactions have been reported with the components of ASCOMP with CODEINE.
Potential effects of high dosage are listed in the [see Overdosage (10)] section of this insert.
Aspirin: occult blood loss, hemolytic anemia, iron deficiency anemia, gastric distress, heartburn, nausea, peptic ulcer, prolonged bleeding time, acute airway obstruction, renal toxicity when taken in high doses for prolonged periods, impaired urate excretion, hepatitis.
Caffeine: cardiac stimulation, irritability, tremor, dependence, nephrotoxicity, hyperglycemia.
Codeine: nausea, vomiting, drowsiness, lightheadedness, constipation, pruritus.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Central Nervous: abuse, addiction, anxiety, depression, disorientation, hallucination, hyperactivity, insomnia, libido decrease, nervousness, neuropathy, psychosis, sedation, sexual activity increase, slurred speech, twitching, unconsciousness, vertigo.
Autonomic Nervous: epistaxis, flushing, miosis, salivation.
Gastrointestinal: anorexia, appetite increased, constipation, diarrhea, esophagitis, gastroenteritis, gastrointestinal spasm, hiccup, mouth burning, pyloric ulcer.
Cardiovascular: chest pain, hypotensive reaction, palpitations, syncope.
Skin: erythema, erythema multiforme, exfoliative dermatitis, hives, rash, toxic epidermal necrolysis.
Urinary: kidney impairment, urinary difficulty.
Miscellaneous: allergic reaction, anaphylactic shock, cholangiocarcinoma, drug interaction with erythromycin (stomach upset), edema.
Serotonin syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs.
Adrenal insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use.
Anaphylaxis: Anaphylaxis has been reported with ingredients contained in ASCOMP with CODEINE.
Androgen deficiency: Cases of androgen deficiency have occurred with chronic use of opioids [see Clinical Pharmacology (12.2)].
7 DRUG INTERACTIONS
Table 1 includes clinically significant drug interactions with ASCOMP with CODEINE.
Table 1: Clinically Significant Drug Interactions with ASCOMP with CODEINE
|
Inhibitors of CYP3A4 |
|
|
Clinical Impact: |
The concomitant use of ASCOMP with CODEINE with CYP3A4 inhibitors may result in an increase in codeine plasma concentrations with subsequently greater metabolism by cytochrome CYP2D6, resulting in greater morphine levels, which could increase or prolong adverse reactions and may cause potentially fatal respiratory depression, particularly when an inhibitor is added after a stable dose of ASCOMP with CODEINE is achieved. After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, it may result in lower codeine levels, greater norcodeine levels, and less metabolism via 2D6 with resultant lower morphine levels [see Clinical Pharmacology (12.3)], resulting in decreased opioid efficacy or a withdrawal syndrome in patients who had developed physical dependence to codeine. |
|
Intervention: |
If concomitant use with CYP3A4 inhibitor is necessary, consider dosage reduction of ASCOMP with CODEINE until stable drug effects are achieved. Monitor patients for respiratory depression and sedation at frequent intervals. If a CYP3A4 inhibitor is discontinued, consider increasing the ASCOMP with CODEINE dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. |
|
Examples: |
Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g. ketoconazole), protease inhibitors (e.g., ritonavir) |
|
CYP3A4 Inducers |
|
|
Clinical Impact: |
The concomitant use of ASCOMP with CODEINE and CYP3A4 inducers can result in lower codeine levels, greater norcodeine levels, and less metabolism via 2D6 with resultant lower morphine levels [see Clinical Pharmacology (12.3)], resulting in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence [see Warnings and Precautions (5.15)]. After stopping a CYP3A4 inducer, as the effects of the inducer decline, the codeine plasma concentration may increase with subsequently greater metabolism by cytochrome CYP2D6, resulting in greater morphine levels [see Clinical Pharmacology (12.3)], which could increase or prolong both the therapeutic effects and adverse reactions, and may cause serious respiratory depression. |
|
Intervention: |
If concomitant use of a CYP3A4 inducer is necessary, follow the patient for reduced efficacy and signs of opioid withdrawal and consider increasing the ASCOMP with CODEINE dosage as needed. If a CYP3A4 inducer is discontinued, consider ASCOMP with CODEINE dosage reduction, and monitor for signs of respiratory depression and sedation at frequent intervals. |
|
Examples: |
Rifampin, carbamazepine, phenytoin |
|
Inhibitors of CYP2D6 |
|
|
Clinical Impact: |
Codeine in ASCOMP with CODEINE is metabolized by CYP2D6 to form morphine. The concomitant use of ASCOMP with CODEINE and CYP2D6 inhibitors can increase the plasma concentration of codeine, but can decrease the plasma concentrations of active metabolite morphine which could result in reduced analgesic efficacy or symptoms of opioid withdrawal, particularly when an inhibitor is added after a stable dose of ASCOMP with CODEINE is achieved [see Clinical Pharmacology (12.3)]. After stopping a CYP2D6 inhibitor, as the effects of the inhibitor decline, the codeine plasma concentration will decrease but the active metabolite morphine plasma concentration will increase, which could increase or prolong adverse reactions and may cause potentially fatal respiratory depression [see Clinical Pharmacology (12.3)]. |
|
Intervention: |
If concomitant use with a CYP2D6 inhibitor is necessary, or if a CYP2D6 inhibitor is discontinued after concomitant use, consider dosage adjustment of ASCOMP with CODEINE and monitor patients closely at frequent intervals. If concomitant use with CYP2D6 inhibitors is necessary, follow the patient for reduced efficacy or signs and symptoms of opioid withdrawal and consider increasing the ASCOMP with CODEINE as needed. After stopping use of a CYP2D6 inhibitor, consider reducing the ASCOMP with CODEINE and monitor the patient for signs and symptoms of respiratory depression or sedation. |
|
Examples: |
paroxetine, fluoxetine, bupropion, quinidine |
|
Benzodiazepines and other Central Nervous System (CNS) Depressants |
|
|
Clinical Impact: |
Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants including alcohol, increases the risk of respiratory depression, profound sedation, coma, and death. |
|
Intervention: |
Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients closely for signs of respiratory depression and sedation [see Warnings and Precautions (5.4)]. |
|
Examples: |
Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids, alcohol. |
|
Serotonergic Drugs |
|
|
Clinical Impact: |
The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome. |
|
Intervention: |
If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue ASCOMP with CODEINE if serotonin syndrome is suspected. |
|
Examples: |
Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5HT3 receptor antagonists, drugs that effect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue). |
|
Monoamine Oxidase Inhibitors (MAOIs) |
|
|
Clinical Impact: |
MAOI interactions with opioids may manifest as serotonin syndrome or opioid toxicity (e.g., respiratory depression, coma) [see Warnings and Precautions (5.9)]. |
|
Intervention: |
Do not use ASCOMP with CODEINE in patients taking MAOIs or within 14 days of stopping such treatment. If urgent use of an opioid is necessary, use test doses and frequent titration of small doses of other opioids (such as oxycodone, hydrocodone, oxymorphone, hydrocodone, or buprenorphine) to treat pain while closely monitoring blood pressure and signs and symptoms of CNS and respiratory depression. |
|
Examples: |
phenelzine, tranylcypromine, linezolid |
|
Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics |
|
|
Clinical Impact: |
May reduce the analgesic effect of ASCOMP with CODEINE and/or precipitate withdrawal symptoms. |
|
Intervention: |
Avoid concomitant use. |
|
Examples: |
butorphanol, nalbuphine, pentazocine, buprenorphine, |
|
Muscle Relaxants |
|
|
Clinical Impact: |
Codeine may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. |
|
Intervention: |
Monitor patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of ASCOMP with CODEINE and/or the muscle relaxant as necessary. |
|
Diuretics |
|
|
Clinical Impact: |
Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. |
|
Intervention: |
Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed. The effectiveness of diuretics in patients with underlying renal or cardiovascular disease may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow and salt and fluid retention. |
|
Anticholinergic Drugs |
|
|
Clinical Impact: |
The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. |
|
Intervention: |
Monitor patients for signs of urinary retention or reduced gastric motility when ASCOMP with CODEINE is used concomitantly with anticholinergic drugs. |
|
Anticoagulants |
|
|
Clinical Impact: |
Aspirin may enhance the effects of anticoagulants. Concurrent use may increase the risk of bleeding. Aspirin can also displace warfarin from protein binding sides, leading to prolongation of both the prothrombin time and the bleeding time. |
|
Intervention: |
Monitor patients for signs of bleeding. |
|
Examples: |
Warfarin, heparin, enoxaparin, clopidogrel, prasugrel, rivaroxaban, apixaban |
|
Uricosuric Agents |
|
|
Clinical Impact: |
Aspirin inhibits the uricosuric effects of uricosuric agents. |
|
Intervention: |
Avoid concomitant use. |
|
Examples: |
Probenecid |
|
Carbonic Anhydrase Inhibitors |
|
|
Clinical Impact: |
Concurrent use with aspirin can lead to high serum concentrations of the carbonic anhydrase inhibitor and cause toxicity due to competition at the renal tubule for secretion. |
|
Intervention: |
Consider reducing the dose of the carbonic anhydrase inhibitor and monitor patient for any adverse effects from the carbonic anhydrase inhibitor. |
|
Examples: |
Acetazolamide, methazolamide |
|
Methotrexate |
|
|
Clinical Impact: |
Aspirin may enhance the toxicity of methotrexate by displacing it from its plasma protein binding sites and/or reducing its renal clearance. |
|
Intervention: |
Use caution if using concomitantly, especially in elderly patients or patients with renal impairment. Monitor patients for methotrexate toxicity. |
|
Nephrotoxic Agents |
|
|
Clinical Impact: |
Concomitant use with aspirin may lead to additive nephrotoxicity due to the inhibition of renal prostaglandins by aspirin. Also, the plasma concentration of aspirin is increased by conditions that reduce the glomerular filtration rate or tubular secretion. |
|
Intervention: |
Use ASCOMP with CODEINE with caution if used concomitantly with nephrotoxic agents. Closely monitor the renal function of patients. |
|
Examples: |
Aminoglycosides, amphotericin B, systemic bacitracin, cisplatin, cyclosporine, foscarnet, or parenteral vancomycin |
|
Angiotensin Converting Enzyme (ACE) Inhibitors |
|
|
Clinical Impact: |
The hyponatremic and hypotensive effects of ACE inhibitors may be diminished by the concomitant administration of aspirin due to its indirect effect on the renin-angiotensin conversion pathway. |
|
Intervention: |
Use caution if using concomitantly. Monitor the blood pressure and renal function of patients. |
|
Examples: |
Ramipril, captopril |
|
Beta Blockers |
|
|
Clinical Impact: |
The hypotensive effects of beta blockers may be diminished by the concomitant administration of aspirin due to inhibition of renal prostaglandins, leading to decreased renal blood flow, and salt and fluid retention. |
|
Intervention: |
Use caution if using concomitantly. Monitor the blood pressure and renal function of patients. |
|
Examples: |
Metoprolol, propranolol |
|
Hypoglycemic Agents |
|
|
Clinical Impact: |
Aspirin may increase the serum glucose-lowering action of insulin and sulfonylureas leading to hypoglycemia. |
|
Intervention: |
Patients should be advised to consult a physician if any signs or symptoms of hypoglycemia occur. |
|
Examples: |
Insulin, glimepiride, glipizide |
|
Anticonvulsants |
|
|
Clinical Impact: |
Aspirin can displace protein-bound phenytoin and valproic acid, leading to a decrease in the total concentration of phenytoin and an increase in serum valproic acid levels. |
|
Intervention: |
Use caution if using concomitantly. |
|
Examples: |
Phenytoin, valproic acid |
|
Nonsteroidal Anti-inflammatory Drugs (NSAIDs) |
|
|
Clinical Impact: |
Concurrent use with aspirin may increase the risk of bleeding or lead to decreased renal function. Aspirin may enhance serious side effects and toxicity of ketorolac by displacing it from its plasma protein binding sites and/or reducing its renal clearance. |
|
Intervention: |
Avoid concomitant use. |
|
Examples: |
Ketorolac, ibuprofen, naproxen, diclofenac |
|
Corticosteroids |
|
|
Clinical Impact: |
In patients receiving concomitant corticosteroids and chronic use of aspirin, withdrawal of corticosteroids may result in salicylism because corticosteroids enhance renal clearance of salicylates and their withdrawal is followed by return to normal rates of renal clearance. |
|
Intervention: |
Avoid concomitant use. |
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Prolonged use of opioid analgesics during pregnancy may cause neonatal opioid withdrawal syndrome [see Warnings and Precautions (5.6)]. Use of aspirin, including ASCOMP with CODEINE, during the third trimester of pregnancy increases the risk of premature closure of the fetal ductus arteriosus. Avoid use of NSAIDs, including ASCOMP with CODEINE, in pregnant women starting at 30 weeks of gestation (third trimester). Available data with ASCOMP with CODEINE in pregnant women is insufficient to inform a drug-associated risk for major birth defects and miscarriage. Animal reproduction studies have not been conducted with the combination of butalbital, acetaminophen, caffeine, and codeine phosphate capsules or with butalbital alone. In animal reproduction studies, codeine administration during organogenesis has been shown to produce delayed ossification in the offspring of mice at 2.8 times maximum recommended human dose (MRHD) of 180 mg/day, embryolethal and fetotoxic effects in the offspring of rats and hamsters at approximately 4 to 6 times the MRHD, and cranial malformations/cranioschisis in the offspring of hamsters between 2 and 8 times the MRHD [see Data]. Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as aspirin, resulted in increased pre-and post-implantation loss.
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Although ASCOMP with CODEINE was not implicated in the birth defect, a female infant was born with lissencephaly, pachygyria and heterotopic gray matter. The infant was born 8 weeks prematurely to a woman who had taken an average of 90 ASCOMP with CODEINE each month from the first few days of pregnancy. The child’s development was mildly delayed and from one year of age she had partial simple motor seizures.
Withdrawal seizures were reported in a two-day-old male infant whose mother had taken a butalbital-containing drug during the last 2 months of pregnancy. Butalbital was found in the infant’s serum. The infant was given phenobarbital 5 mg/kg, which was tapered without further seizure or other withdrawal symptoms.
Studies of aspirin use in pregnant women have not shown that aspirin increases the risk of abnormalities when administered during the first trimester of pregnancy. In controlled studies involving 41,337 pregnant women and their offspring, there was no evidence that aspirin taken during pregnancy caused stillbirth, neonatal death or reduced birth weight. In controlled studies of 50,282 pregnant women and their offspring, aspirin administration in moderate and heavy doses during the first four lunar months of pregnancy showed no teratogenic effect.
Therapeutic doses of aspirin in pregnant women close to term may cause bleeding in mother, fetus, or neonate. During the last 6 months of pregnancy, regular use of aspirin in high doses may prolong pregnancy and delivery.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Prolonged use of opioid analgesics during pregnancy for medical or nonmedical purposes can result in physical dependence in the neonate and neonatal opioid withdrawal syndrome shortly after birth.
Neonatal opioid withdrawal syndrome presents as irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea and failure to gain weight. The onset, duration, and severity of neonatal opioid withdrawal syndrome vary based on the specific opioid used, duration of use, timing and amount of last maternal use, and rate of elimination of the drug by the newborn. Observe newborns for symptoms of neonatal opioid withdrawal syndrome and manage accordingly [see Warnings and Precautions (5.6)].
Labor or Delivery
There are no studies on the effects of ASCOMP with CODEINE during labor or delivery. In animal studies, NSAIDS, including aspirin, inhibit prostaglandin synthesis, cause delayed parturition, and increase the incidence of stillbirth.
Opioids such as codeine cross the placenta and may produce respiratory depression and psycho-physiologic effects in neonates. An opioid antagonist, such as naloxone, must be available for reversal of opioid-induced respiratory depression in the neonate. ASCOMP with CODEINE is not recommended for use in pregnant women during or immediately prior to labor, when other analgesic techniques are more appropriate. Opioid analgesics, including ASCOMP with CODEINE, can prolong labor through actions which temporarily reduce the strength, duration, and frequency of uterine contractions. However, this effect is not consistent and may be offset by an increased rate of cervical dilation, which tends to shorten labor. Monitor neonates exposed to opioid analgesics during labor for signs of excess sedation and respiratory depression.
Aspirin should be avoided one week prior to and during labor and delivery because it can result in excessive blood loss at delivery. Prolonged gestation and prolonged labor due to prostaglandin inhibition have been reported.
Salicylates readily cross the placenta and by inhibiting prostaglandin synthesis, may cause constriction of ductus arteriosus resulting in pulmonary hypertension and increased fetal mortality and, possibly other untoward fetal effects. Aspirin use in pregnancy can also result in alteration in maternal and neonatal hemostasis mechanisms. Maternal aspirin use during later stages of pregnancy may cause low birth weight, increased incidence of intracranial hemorrhage in premature infants, stillbirths and neonatal death. Use during pregnancy, especially in the third trimester, should be avoided.
Data
Animal Data
Animal reproduction studies have not been conducted with the combination of Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules or with butalbital alone.
Codeine:
In a study in which pregnant hamsters were administered 150 mg/kg twice daily of codeine (oral; approximately 14 times the maximum recommended daily dose of 180 mg/day for adults on a mg/m2 basis) during organogenesis cranial malformations (i.e., meningoencephalocele) in several fetuses were reported; as well as the observation of increases in the percentage of resorptions per litter. Doses of 50 and 150 mg/kg, bid resulted in fetotoxicity as demonstrated by decreased fetal body weight. In an earlier study in hamsters, single oral doses of 73 to 360 mg/kg level on Gestation Day 8 (oral; approximately 4 to 16 times the maximum recommended daily dose of 180 mg/day for adults on a mg/m2 basis), reportedly produced cranioschisis in all of the fetuses examined.
In studies in rats, doses at the 120 mg/kg level (oral; approximately 6 times the maximum recommended daily dose of 180 mg/day for adults on a mg/m2 basis) during organogenesis, in the toxic range for the adult animal, were associated with an increase in embryo resorption at the time of implantation.
In pregnant mice, a single 100 mg/kg dose (subcutaneous; approximately 2.8 times the recommended daily dose of 180 mg/day for adults on a mg/mg2 basis) administered between Gestation Day 7 and 12 reportedly resulted in delayed ossification in the offspring.
No teratogenic effects were observed in rabbits administered up to 30 mg/kg (approximately 4 times the maximum recommended daily dose of 180 mg/day for adults on a mg/m2 basis) of codeine during organogenesis.
Codeine (30 mg/kg) administered subcutaneously to pregnant rats during pregnancy and for 25 days after delivery increased neonatal mortality at birth. This dose is 1.6 times the maximum recommended human dose of 180 mg/day on a body surface area comparison.
Caffeine:
In studies performed in adult animals, caffeine (as caffeine base) administered to pregnant mice as sustained release pellets at 50 mg/kg (less than the maximum recommended daily dose on a mg/m2 basis), during the period of organogenesis, caused a low incidence of cleft palate and exencephaly in the fetuses.
8.2 Lactation
Risk Summary
Codeine and its active metabolite, morphine, are present in human milk. There are published studies and cases that have reported excessive sedation, respiratory depression, and death in infants exposed to codeine via breast milk. Women who are ultra-rapid metabolizers of codeine achieve higher than expected serum levels of morphine, potentially leading to higher levels of morphine in breast milk that can be dangerous in their breastfed infants. In women with normal codeine metabolism (normal CYP2D6 activity), the amount of codeine secreted into human milk is low and dose-dependent.
There is no information on the effects of the codeine on milk production. Because of the potential for serious adverse reactions, including excess sedation, respiratory depression, and death in a breastfed infant, advise patients that breastfeeding is not recommended during treatment with ASCOMP with CODEINE (see Warnings and Precautions, 5.7).
The aspirin and caffeine in ASCOMP with CODEINE are also excreted in breast milk in small amounts. Adverse effects on platelet function in the nursing infant exposed to aspirin in breast milk may be a potential risk. Furthermore, nursing women are advised against aspirin use because of the possible development of Reye's Syndrome in their babies.
Barbiturates and caffeine are also excreted in breast milk in small amounts. Because of potential for serious adverse reactions in nursing infants from Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Clinical Considerations
If infants are exposed to ASCOMP with CODEINE through breast milk, they should be monitored for excess sedation and respiratory depression. Withdrawal symptoms can occur in breastfed infants when maternal administration of an opioid analgesic is stopped, or when breast-feeding is stopped.
8.3 Females and Males of Reproductive Potential
Infertility
Chronic use of opioids may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible [see Adverse Reactions (6.2), Clinical Pharmacology (12.2), Nonclincical Toxicology (13.1)].
Females
Based on the mechanism of action, the use of prostaglandin-mediated NSAIDs, including aspirin, may delay or prevent rupture of ovarian follicles, which has been associated with reversible infertility in some women. Published animal studies have shown that administration of prostaglandin synthesis inhibitors has the potential to disrupt prostaglandin-mediated follicular rupture required for ovulation. Small studies in women treated with NSAIDs have also shown a reversible delay in ovulation. Consider withdrawal of NSAIDs, including aspirin, in women who have difficulties conceiving or who are undergoing investigation of infertility.
8.4 Pediatric Use
Preparations containing aspirin should be kept out of the reach of children. Reye's Syndrome is a rare condition that affects the brain and liver and is most often observed in children given aspirin during a viral illness. Safety and effectiveness in pediatric patients have not been established.
The safety and effectiveness of ASCOMP with CODEINE in pediatric patients have not been established.
Life-threatening respiratory depression and death have occurred in children who received codeine [see Warnings and Precautions (5.5)]. In most of the reported cases, these events followed tonsillectomy and/or adenoidectomy, and many of the children had evidence of being ultra-rapid metabolizers of codeine (i.e., multiple copies of the gene for cytochrome P450 isoenzyme 2D6 or high morphine concentrations). Children with sleep apnea may be particularly sensitive to the respiratory depressant effects of codeine. Because of the risk of life-threatening respiratory depression and death:
- •
- ASCOMP with CODEINE is contraindicated for all children younger than 12 years of age [see Contraindications (4)].
- •
- ASCOMP with CODEINE is contraindicated for post-operative management in pediatric patients younger than 18 years of age following tonsillectomy and/or adenoidectomy [see Contraindications (4)].
- •
- Avoid the use of ASCOMP with CODEINE in adolescents 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of codeine unless the benefits outweigh the risks. Risk factors include conditions associated with hypoventilation, such as postoperative status, obstructive sleep apnea, obesity, severe pulmonary disease, neuromuscular disease, and concomitant use of other medications that cause respiratory depression. [see Warnings and Precautions (5.5)].
8.5 Geriatric Use
Clinical studies of Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Butalbital is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Elderly patients (aged 65 years or older) may have increased sensitivity to ASCOMP with CODEINE. In general, use caution when selecting a dosage for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
Respiratory depression is the chief risk for elderly patients treated with opioids and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration. Titrate the dosage of ASCOMP with CODEINE slowly in geriatric patients and monitor closely for signs of central nervous system and respiratory depression [see Warnings and Precautions (5.8)].
Components of this product are known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Elderly patients, compared to younger patients, are at greater risk for NSAID-associated serious cardiovascular, gastrointestinal, and/or renal adverse reactions. If the anticipated benefit for the elderly patient outweighs these potential risks, dose selection should start at the low end of the dosing range, and monitor patients for adverse effects [see Warnings and Precautions (5)].
8.6 Hepatic Impairment
No formal studies have been conducted in patients with hepatic impairment so the pharmacokinetics of aspirin, codeine and butalbital in this patient population are unknown. Start these patients cautiously with lower doses of ASCOMP with CODEINE or with longer dosing intervals and titrate slowly while carefully monitoring for side effects. In patients with severe hepatic disease, monitor effects of therapy with serial liver function tests.
8.7 Renal Impairment
ASCOMP with CODEINE contains aspirin, which should be avoided in patients with severe renal failure (glomerular filtration rate less than 10 mL/minute).
Codeine pharmacokinetics may be altered in patients with renal failure. Clearance may be decreased, and the metabolites may accumulate to much higher plasma levels in patients with renal failure as compared to patients with normal renal function. Start these patients cautiously with lower doses of ASCOMP with CODEINE or with longer dosing intervals and titrate slowly while carefully monitoring for side effects. In patients with renal disease, monitor effects of therapy with serial renal function tests.
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
ASCOMP with CODEINE contains codeine. Codeine in combination with butalbital, aspirin, and caffeine is a Schedule III controlled substance.
9.2 Abuse
ASCOMP with CODEINE contains codeine, a substance with a high potential for abuse similar to other opioids, including fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, and tapentadol. ASCOMP with CODEINE can be abused and is subject to misuse, addiction, and criminal diversion [see Warnings and Precautions (5.1)].
All patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Prescription drug abuse is the intentional non-therapeutic use of a prescription drug, even once, for its rewarding psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and includes: a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal.
“Drug-seeking” behavior is very common in persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing, or referral, repeated “loss” of prescriptions, tampering with prescriptions, and reluctance to provide prior medical records or contact information for other treating healthcare provider(s). “Doctor shopping” (visiting multiple prescribers to obtain additional prescriptions) is common among drug abusers and people suffering from untreated addiction. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with poor pain control.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Healthcare providers should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of opioids can occur in the absence of true addiction.
ASCOMP with CODEINE, like other opioids, can be diverted for non-medical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
Risks Specific to Abuse of ASCOMP with CODEINE
ASCOMP with CODEINE is for oral use only. Abuse of ASCOMP with CODEINE poses a risk of overdose and death. The risk is increased with concurrent abuse of ASCOMP with CODEINE with alcohol and other central nervous system depressants.
Parenteral drug abuse is commonly associated with transmission of infectious diseases such as hepatitis and HIV.
Butalbital
Barbiturates may be habit-forming. Tolerance, psychological dependence, and physical dependence may occur especially following prolonged use of high doses of barbiturates. The average daily dose for the barbiturate addict is usually about 1,500 mg. As tolerance to barbiturates develops, the amount needed to maintain the same level of intoxication increases; tolerance to a fatal dosage, however, does not increase more than twofold. As this occurs, the margin between an intoxication dosage and fatal dosage becomes smaller. The lethal dose of a barbiturate is far less if alcohol is also ingested. Major withdrawal symptoms (convulsions and delirium) may occur within 16 hours and last up to 5 days after abrupt cessation of these drugs. Intensity of withdrawal symptoms gradually declines over a period of approximately 15 days. Treatment of barbiturate dependence consists of cautious and gradual withdrawal of the drug. Barbiturate-dependent patients can be withdrawn by using a number of different withdrawal regimens. One method involves initiating treatment at the patient’s regular dosage level and gradually decreasing the daily dosage as tolerated by the patient.
9.3 Dependence
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs and may develop at different rates for different effects.
Physical dependence results in withdrawal symptoms after abrupt discontinuation or a significant dosage reduction of a drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone, nalmefene), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
Do not abruptly discontinue ASCOMP with Codeine in a patient physically dependent on opioids. Rapid tapering of ASCOMP with Codeine in a patient physically dependent on opioids may lead to serious withdrawal symptoms, uncontrolled pain, and suicide. Rapid discontinuation has also been associated with attempts to find other sources of opioid analgesics, which may be confused with drug-seeking for abuse.
When discontinuing ASCOMP with Codeine, gradually taper the dosage using a patient-specific plan that considers the following: the dose of ASCOMP with Codeine the patient has been taking, the duration of treatment, and the physical and psychological attributes of the patient. To improve the likelihood of a successful taper and minimize withdrawal symptoms, it is important that the opioid tapering schedule is agreed upon by the patient. In patients taking opioids for a long duration at high doses, ensure that a multimodal approach to pain management, including mental health support (if needed), is in place prior to initiating an opioid analgesic taper [see Dosage and Administration (2.3), Warnings and Precautions (5.15)].
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal signs [see Use in Specific Populations (8.1, 8.2)].
10 OVERDOSAGE
Clinical Presentation
Acute overdose with ASCOMP with CODEINE can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, hypotension, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Clinical Pharmacology (12.2)].
Signs and Symptoms
Acute Barbiturate Poisoning:
Symptoms include drowsiness, confusion, and coma; respiratory depression; hypotension; hypovolemic shock.
Acute Aspirin Poisoning:
Symptoms include hyperpnea; acid-base disturbances with development of metabolic acidosis; vomiting and abdominal pain; tinnitus, hyperthermia; hypoprothrombinemia; restlessness; delirium; convulsions.
Acute Caffeine Poisoning:
Symptoms include insomnia, restlessness, tremor, and delirium; tachycardia and extrasystoles.
Codeine:
Acute overdose with codeine can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, and, in some cases, pulmonary edema, bradycardia, hypotension, partial or complete airway obstruction, atypical snoring, and death. Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations [see Clinical Pharmacology (12.2)].
Treatment of Overdose
In case of overdose, priorities are the reestablishment of a patent and protected airway and institution of assisted or controlled ventilation, if needed. Employ other supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema as indicated. Cardiac arrest or arrhythmias will require advanced life-support techniques.
The opioid antagonists, naloxone or nalmefene, are specific antidotes to respiratory depression resulting from opioid overdose. For clinically significant respiratory or circulatory depression secondary to codeine phosphate overdose, administer an opioid antagonist. Opioid antagonists should not be administered in the absence of clinically significant respiratory or circulatory depression secondary to codeine overdose.
Because the duration of opioid reversal is expected to be less than the duration of action of codeine in ASCOMP with CODEINE, carefully monitor the patient until spontaneous respiration is reliably re-established. If the response to an opioid antagonist is suboptimal or only brief in nature, administer additional antagonist as directed by the product’s prescribing information.
In an individual physically dependent on opioids, administration of the recommended usual dosage of the antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. If a decision is made to treat serious respiratory depression in the physically dependent patient, administration of the antagonist should be begun with care and by titration with smaller than usual doses of the antagonist.
Treatment consists primarily of management of barbiturate intoxication, reversal of the effects of codeine, and the correction of the acid-base imbalance due to salicylism. Vomiting should be induced mechanically or with emetics in the conscious patient. Gastric lavage may be used if the pharyngeal and laryngeal reflexes are present and if less than 4 hours have elapsed since ingestion. A cuffed endotracheal tube should be inserted before gastric lavage of the unconscious patient and when necessary to provide assisted respiration. Diuresis, alkalinization of the urine, and correction of electrolyte disturbances should be accomplished through administration of intravenous fluids such as1% sodium bicarbonate and 5% dextrose in water.
Meticulous attention should be given to maintaining adequate pulmonary ventilation. The value of vasopressor agents such as Norepinephrine or Phenylephrine Hydrochloride in treating hypotension is questionable since they increase vasoconstriction and decrease blood flow. However, if prolonged support of blood pressure is required, Norepinephrine Bitartrate (Levophed®) may be given I.V. with the usual precautions and serial blood pressure monitoring. In severe cases of intoxication, peritoneal dialysis, hemodialysis, or exchange transfusion may be lifesaving. Hypoprothrombinemia should be treated with vitamin K, intravenously.
Methemoglobinemia over 30% should be treated with methylene blue by slow intravenous administration.
Naloxone, a narcotic antagonist, can reverse respiratory depression and coma associated with opioid overdose. Typically, a dose of 0.4 to 2 mg is given parenterally and may be repeated if an adequate response is not achieved. Since the duration of action of codeine may exceed that of the antagonist, the patient should be kept under continued surveillance and repeated doses of the antagonist should be administered as needed to maintain adequate respiration. A narcotic antagonist should not be administered in the absence of clinically significant respiratory or cardiovascular depression.
11 DESCRIPTION
ASCOMP with CODEINE (butalbital, aspirin, caffeine, and codeine phosphate, USP) is supplied in capsule form for oral administration.
Each capsule contains the following active ingredients:
Butalbital, USP……………..50mg
Aspirin, USP………………..325mg
Caffeine, USP………………40mg
Codeine phosphate, USP…...30mg
Butalbital (5-allyl-5-isobutylbarbituric acid) is a short-to intermediate-acting barbiturate. It has a molecular formula of: C11H16N2O3, with a molecular weight of 224.26, and the following structural formula:
Aspirin (benzoic acid, 2-(acetyloxy)-) is a nonsteroidal anti-inflammatory drug. It has a molecular formula of C9H8O4 with a molecular weight of 180.6, and the following structural formula:
Caffeine (1,3,7-trimethylxanthine), a methylxanthine, is a central nervous system stimulant. It has a molecular formula of C8H10N4O2 with a molecular weight of 194.19, and the following structural formula:
Codeine phosphate (7,8-Didehydro-4,5α-epoxy-3-methoxy-17-methylmorphinan-6α-ol phosphate (1:1) (salt) hemihydrate) is an opioid agonist. It has a molecular formula of C18H24NO7P with an anhydrous molecular weight of 397.37, and the following structural formula:
Inactive Ingredients: Corn Starch, D&C Red No. 28, D&C Yellow No. 10, FD&C Blue No. 1, FD&C Red No. 40, Gelatin, Microcrystalline Cellulose, Sodium Lauryl Sulfate, Stearic Acid, Talc, and Titanium Dioxide.
The capsules are printed with edible black ink.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Butalbital, a barbiturate, is a GABAA receptor agonist and may inhibit excitatory AMPA receptors.
Aspirin is a nonsteroidal anti-inflammatory drug and a non-selective irreversible inhibitor of cyclooxygenases.
Caffeine is a methylxanthine and Central Nervous System (CNS) stimulant. The exact mechanism with respect to the indication is not clear; however, the effects of caffeine may be due to antagonism of adenosine receptors.
Codeine is an opioid agonist relatively selective for the mu-opioid receptor, but with a much weaker affinity than morphine. The analgesic properties of codeine have been speculated to come from its conversion to morphine, although the exact mechanism of analgesic action remains unknown.
12.2 Pharmacodynamics
Effects on the Central Nervous System
Butalbital, a barbiturate, is a central nervous system (CNS) depressant that can produce sedation, respiratory depression, and euphoria. The potential impact of butalbital on painful stimuli is not clear, and in some individuals, barbiturates may increase reaction to painful stimuli.
Codeine produces respiratory depression by direct action on brain stem respiratory centers. The respiratory depression involves a reduction in the responsiveness of the brain stem respiratory centers to both increases in carbon dioxide tension and electrical stimulation.
Codeine causes miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdose but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origins may produce similar findings). Marked mydriasis rather than miosis may be seen due to hypoxia in overdose situations.
Aspirin works by inhibiting the body’s production of prostaglandins, including prostaglandins involved in inflammation. Prostaglandins cause pain sensations by stimulating muscle contractions and dilating blood vessels throughout the body. In the CNS, aspirin works on the hypothalamus heat-regulating center to reduce fever, however, other mechanisms may be involved.
Effects on the Gastrointestinal Tract and Other Smooth Muscle
Codeine causes a reduction in motility associated with an increase in smooth muscle tone in the antrum of the stomach and duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone may be increased to the point of spasm, resulting in constipation. Other opioid-induced effects may include a reduction in biliary and pancreatic secretions, spasm of sphincter of Oddi, and transient elevations in serum amylase.
Aspirin can produce gastrointestinal injury (lesions, ulcers) through a mechanism that is not yet completely understood but may involve a reduction in eicosanoid synthesis by the gastric mucosa. Decreased production of prostaglandins may compromise the defenses of the gastric mucosa and the activity of substances involved in tissue repair and ulcer healing.
Effects on the Cardiovascular System
Butalbital may decrease blood pressure and heart rate when administered at sedative and hypnotic doses.
Codeine produces peripheral vasodilation which may result in orthostatic hypotension or syncope. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, sweating. and/or orthostatic hypotension.
Aspirin affects platelet aggregation by irreversibly inhibiting prostaglandin cyclooxygenase. This effect lasts for the life of the platelet and prevents the formation of the platelet aggregating factor, thromboxane A2. Nonacetylated salicylates do not inhibit this enzyme and have no effect on platelet aggregation. At somewhat higher doses, aspirin reversibly inhibits the formation of prostaglandin 12 (prostacyclin), which is an arterial vasodilator and inhibits platelet aggregation.
Effects on the Endocrine System
Opioids inhibit the secretion of adrenocorticotropic hormone (ACTH), cortisol, and luteinizing hormone (LH) in humans [see Adverse Reactions (6.2)]. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon.
Chronic use of opioids may influence the hypothalamic-pituitary-gonadal axis, leading to androgen deficiency that may manifest as low libido, impotence, erectile dysfunction, amenorrhea, or infertility. The causal role of opioids in the clinical syndrome of hypogonadism is unknown because the various medical, physical, lifestyle, and psychological stressors that may influence gonadal hormone levels have not been adequately controlled in studies conducted to date [see Adverse Reactions (6.2)].
Effects on the Immune System
Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. Overall, the effects of opioids appear to be modestly immunosuppressive.
Concentration–Efficacy Relationships
The minimum effective analgesic concentration will vary widely among patients, especially among patients who have been previously treated with potent agonist opioids. The minimum effective analgesic concentration of codeine for any individual patient may increase over time due to an increase in pain, the development of a new pain syndrome and/or the development of analgesic tolerance [see Dosage and Administration (2.1, 2.2)].
Concentration–Adverse Reaction Relationships
There is a relationship between increasing codeine plasma concentration and increasing frequency of dose-related opioid adverse reactions such as nausea, vomiting, CNS effects, and respiratory depression. In opioid-tolerant patients, the situation may be altered by the development of tolerance to opioid-related adverse reactions [see Dosage and Administration (2.1, 2.2, 2.3)].
12.3 Pharmacokinetics
Bioavailability:
The bioavailability of the components of the fixed combination of ASCOMP with CODEINE is identical to their bioavailability when Fiorinal (Butalbital, Aspirin, and Caffeine Capsules,) and Codeine are administered separately in equivalent molar doses. The behavior of the individual components is described below.
Aspirin
Absorption
The systemic availability of aspirin after an oral dose is highly dependent on the dosage form, the presence of food, the gastric emptying time, gastric pH, antacids, buffering agents, and particle size. These factors affect not necessarily the extent of absorption of total salicylates but more the stability of aspirin prior to absorption.
Distribution
During the absorption process and after absorption, aspirin is mainly hydrolyzed to salicylic acid and distributed to all body tissues and fluids, including fetal tissues, breast milk, and the central nervous system (CNS). Highest concentrations are found in plasma, liver, renal cortex, heart, and lung. In plasma, about 50%-80% of the salicylic acid and its metabolites are loosely bound to plasma proteins.
Elimination
Metabolism
The biotransformation of aspirin occurs primarily in the hepatocytes. The major metabolites are salicyluric acid (75%), the phenolic and acyl glucuronides of salicylate (15%), and gentisic and gentisuric acid (1%). The bioavailability of the aspirin component of ASCOMP with CODEINE is equivalent to that of a solution except for a slower rate of absorption. A peak concentration of 8.8 mcg/mL was obtained at 40 minutes after a 650 mg dose.
Excretion
The clearance of total salicylates is subject to saturable kinetics; however, first-order elimination kinetics are still a good approximation for doses up to 650 mg. The plasma half-life for aspirin is about 12 minutes and for salicylic acid and/or total salicylates is about 3 hours.
The elimination of therapeutic doses is through the kidneys either as salicylic acid or other biotransformation products. The renal clearance is greatly augmented by an alkaline urine as is produced by concurrent administration of sodium bicarbonate or potassium citrate.
Codeine
Absorption
Codeine is readily absorbed from the gastrointestinal tract. The bioavailability of the codeine component of ASCOMP with CODEINE is equivalent to that of a solution. Peak concentrations of 198 ng/mL were obtained at 1 hour after a 60 mg dose. At therapeutic doses, the analgesic effect reaches a peak within 2 hours and persists between 4 and 6 hours.
Distribution
It is rapidly distributed from the intravascular spaces to the various body tissues, with preferential uptake by parenchymatous organs such as the liver, spleen, and kidney. Codeine crosses the blood-brain barrier and is found in fetal tissue and breast milk. The plasma concentration does not correlate with brain concentration or relief of pain; however, codeine is not bound to plasma proteins and does not accumulate in body tissues.
Elimination
Metabolism
About 70-80% of administered dose of codeine is metabolized by conjugation with glucuronic acid to codeine-6glucuronide (C6G) and via O-demethylation to morphine (about 5-10%) and N-demethylation to norcodeine (about 10%) respectively. UDP-glucuronosyltransferase (UGT) 2B7 and 2B4 are the major enzymes mediating glucuronidation of codeine to C6G. Cytochrome P450 2D6 is the major enzyme responsible for conversion of codeine to morphine and P450 3A4 is the major enzyme mediating conversion of codeine to norcodeine. Morphine and norcodeine are further metabolized by conjugation with glucuronic acid. The glucuronide metabolites of morphine are morphine-3-glucuronide (M3G) and morphine-6-glucuronide (M6G). Morphine and M6G are known to have analgesic activity in humans. The analgesic activity of C6G in humans is unknown. Norcodeine and M3G are generally not considered to possess analgesic properties.
Excretion
The plasma half-life is about 2.9 hours. The elimination of codeine is primarily via the kidneys, and about 90% of an oral dose is excreted by the kidneys within 24 hours of dosing. The urinary secretion products consist of free and glucuronide-conjugated codeine (about 70%), free and conjugated norcodeine (about 10%), free and conjugated morphine (about 10%), normorphine (4%), and hydrocodone (1%). The remainder of the dose is excreted in the feces.
Butalbital
Absorption
Butalbital is well absorbed from the gastrointestinal tract. The bioavailability of the butalbital component of ASCOMP with CODEINE is equivalent to that of a solution except for a decrease in the rate of absorption. A peak concentration of 2,020 ng/mL is obtained at about 1.5 hours after a 100 mg dose.
Distribution
Butalbital is expected to distribute to most of the tissues in the body. Barbiturates, in general, may appear in breast milk and readily cross the placental barrier. They are bound to plasma and tissue proteins to a varying degree and binding increases directly as a function of lipid solubility.
The in vitro plasma protein binding of butalbital is 45% over the concentration range of 0.5 to 20 mcg/mL. This falls within the range of plasma protein binding (20% to 45%) reported with other barbiturates such as phenobarbital, pentobarbital, and secobarbital sodium. The plasma-to-blood concentration ratio was almost unity indicating that there is no preferential distribution of butalbital into either plasma or blood cells.
Elimination
Elimination of butalbital is primarily via the kidney (59% to 88% of the dose) as unchanged drug or metabolites. The plasma half-life is about 35 hours. Urinary excretion products included parent drug (about 3.6% of the dose), 5-isobutyl-5-(2,3-dihydroxypropyl) barbituric acid (about 24% of the dose), 5-allyl-5(3-hydroxy2-methyl-1-propyl) barbituric acid (about 4.8% of the dose), products with the barbituric acid ring hydrolyzed with excretion of urea (about 14% of the dose), as well as unidentified materials. Of the material excreted in the urine, 32% was conjugated.
Caffeine
Absorption
Like most xanthines, caffeine is rapidly absorbed and distributed in all body tissues and fluids, including the CNS, fetal tissues, and breast milk. The bioavailability of the caffeine component for ASCOMP with CODEINE is equivalent to that of a solution except for a slightly longer time to peak. A peak concentration of 1,660 ng/mL was obtained in less than an hour for an 80 mg dose.
Distribution
Caffeine is distributed in all body tissues and fluids, including the CNS, fetal tissues, and breast milk.
Elimination
Caffeine is cleared rapidly through metabolism and excretion in the urine.
Metabolism
Caffeine is mainly metabolized by CYP1A2. Other enzymes, including CYP2E1, CYP3A4, CYP2C8 and CYP2C9 may play a minor role in its metabolism. Hepatic biotransformation prior to excretion results in about equal amounts of 1-methylxanthine and 1-methyluric acid.
Excretion
Of the 70% of the dose that has been recovered in the urine, only 3% was unchanged drug. The plasma half-life is about 3 hours.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term studies in animals to evaluate the carcinogenic potential of the combination of butalbital, aspirin, caffeine, and codeine or butalbital alone have not been conducted.
Administration of aspirin for 68 weeks at 0.5 percent in the feed of rats was not carcinogenic.
Two-year carcinogenicity studies with codeine sulfate have been conducted in F344/N rats and B6C3F1 mice. There was no evidence of carcinogenicity in male and female rats, respectively, at dietary doses up to 70 and 80 mg/kg/day of codeine sulfate (approximately 4 times the maximum recommended daily dose of 180 mg/day for adults on a mg/m2 basis) for two years. Similarly, there was no evidence of carcinogenicity activity in male and female mice at dietary doses up to 400 mg/kg/day of codeine sulfate (approximately 10 times the maximum recommended daily dose of 180 mg/day for adults on a mg/m2 basis) for two years.
In a 2-year study in Sprague-Dawley rats, caffeine (as caffeine base) administered in drinking water was not carcinogenic in male rats at doses up to 102 mg/kg or in female rats at doses up to 170 mg/kg (approximately 4 and 7 times, respectively, the maximum human daily dose on a mg/m2 basis). In an 18-month study in C57BL/6 mice, no evidence of tumorigenicity was seen at dietary doses up to 55 mg/kg (equivalent to the MHDD on a mg/m2 basis).
Mutagenesis
There are no genetic toxicology data for butalbital.
Codeine sulfate was not mutagenic in the in vitro bacterial reverse mutation assay or clastogenic in the in vitro Chinese hamster ovary cell chromosome aberration assay.
Aspirin is not mutagenic in the Ames Salmonella assay; however, aspirin did induce chromosome aberrations in cultured human fibroblasts.
Caffeine (as caffeine base) increased the sister chromatid exchange (SCE) SCE/cell metaphase (exposure time dependent) in an in vivo mouse metaphase analysis. Caffeine also potentiated the genotoxicity of known mutagens and enhanced the micronuclei formation (5-fold) in folate-deficient mice. However, caffeine did not increase chromosomal aberrations in invitro Chinese hamster ovary cell (CHO) and human lymphocyte assays and was not mutagenic in an in vitro CHO/hypoxanthine guanine phosphoribosyltransferase (HGPRT) gene mutation assay, except at cytotoxic concentrations. In addition, caffeine was not clastogenic in an in vivo mouse micronucleus assay. Caffeine was negative in the in vitro bacterial reverse mutation assay (Ames test).
Impairment of Fertility
No adequate studies have been conducted in animals to characterize the impact of the combinations of butalbital, aspirin, caffeine, and codeine on fertility. There are also no data on butalbital alone or codeine alone.
Aspirin inhibits ovulation in rats.
Caffeine (as caffeine base) administered to male rats at 50 mg/kg/day subcutaneously (2 times the MHDD on a mg/m2 basis) for 4 days prior to mating with untreated females, caused decreased male reproductive performance in addition to causing embryotoxicity. In addition, long-term exposure to high oral doses of caffeine (3 g over 7 weeks) was toxic to rat testes as manifested by spermatogenic cell degeneration.
14 CLINICAL STUDIES
Evidence supporting the efficacy of Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules is derived from 2 multi-clinic trials that compared patients with tension headache randomly assigned to 4 parallel treatments: Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules, codeine, Butalbital, Aspirin, and Caffeine capsules, USP, and placebo. Response was assessed over the course of the first 4 hours of each of 2 distinct headaches, separated by at least 24 hours Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules proved statistically significantly superior to each of its components (butalbital, aspirin, caffeine, and codeine) and to placebo on measures of pain relief.
Evidence supporting the efficacy and safety of Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP Capsules in the treatment of multiple recurrent headaches is unavailable. Caution in this regard is required because codeine and butalbital are habit-forming and potentially abusable.
16 HOW SUPPLIED/STORAGE AND HANDLING
ASCOMP with CODEINE capsules have a plain blue opaque cap with a yellow opaque body imprinted with "B 074" in black ink. They are available in bottles of 100 capsules [NDC 0722-6094-01] and 500 capsules [NDC 0722-6094-05].
Store and Dispense
Below 25°C (77°F); tight container. Protect from moisture.
Store ASCOMP with Codeine securely and dispose of properly [see Patient Counseling Information (17)].
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (MEDICATION GUIDE).
Storage and Disposal
Because of the risks associated with accidental ingestion, misuse, and abuse, advise patients to store ASCOMP with Codeine securely, out of sight and reach of children, and in a location not accessible by others, including visitors to the home [see Warnings and Precautions (5.1, 5.2), Drug Abuse and Dependence (9.2)]. Inform patients that leaving ASCOMP with Codeine unsecured can pose a deadly risk to others in the home.
Advise patients and caregivers that when medicines are no longer needed, they should be disposed of promptly. Inform patients that medicine take-back options are the preferred way to safely dispose of most types of unneeded medicines. If no take back programs or DEA-registered collectors are available, instruct patients to dispose of ASCOMP with Codeine by following these four steps:
- • Mix ASCOMP with Codeine (do not crush) with an unpalatable substance such as dirt, cat litter, or used coffee grounds;
- • Place the mixture in a container such as a sealed plastic bag;
- • Throw the container in the household trash;
- • Delete all personal information on the prescription label of the empty bottle.
- Inform patients that they can visit www.fda.gov/drugdisposal for additional information on disposal of unused medicines.
Addiction, Abuse, and Misuse
Inform patients that the use of ASCOMP with CODEINE, even when taken as recommended, can result in addiction, abuse, and misuse, which can lead to overdose and death [see Warnings and Precautions (5.1)]. Instruct patients not to share ASCOMP with CODEINE with others and to take steps to protect ASCOMP with CODEINE from theft or misuse.
Life-Threatening Respiratory Depression
Inform patients of the risk of life-threatening respiratory depression, including information that the risk is greatest when starting ASCOMP with CODEINE or when the dosage is increased, and that it can occur even at recommended dosages [see Warnings and Precautions (5.3)]. Advise patients how to recognize respiratory depression and to seek medical attention if breathing difficulties develop.
Accidental Ingestion
Inform patients that accidental ingestion, especially by children, may result in respiratory depression or death.
Risks from Concomitant Use with Benzodiazepines and Other CNS Depressants
Inform patients and caregivers that potentially fatal additive effects may occur if ASCOMP with CODEINE is used with benzodiazepines or other CNS depressants, including alcohol, and not to use these concomitantly unless supervised by a health care provider [see Warnings and Precautions (5.4), Drug Interactions (7)].
Ultra-Rapid Metabolism of Codeine and Other Risk Factors for Life-threatening Respiratory Depression in
Children
Advise caregivers that ASCOMP with CODEINE is contraindicated in all children younger than 12 years of age and in children younger than 18 years of age following tonsillectomy and/or adenoidectomy. Advise caregivers of children 12-18 years of age receiving ASCOMP with CODEINE to monitor for signs of respiratory depression [see Warnings and Precautions (5.5)].
Serotonin Syndrome
Inform patients that opioids could cause a rare but potentially life-threatening condition resulting from concomitant administration of serotonergic drugs. Warn patients of the symptoms of serotonin syndrome and to seek medical attention right away if symptoms develop. Instruct patients to inform their healthcare providers if they are taking, or plan to take serotonergic medications. [see Drug Interactions (7)].
MAOI Interaction
Inform patients not to take ASCOMP with CODEINE while using any drugs that inhibit monoamine oxidase. Patients should not start MAOIs while taking ASCOMP with CODEINE [see Drug Interactions (7)].
Adrenal Insufficiency
Inform patients that opioids could cause adrenal insufficiency, a potentially life-threatening condition. Adrenal insufficiency may present with non-specific symptoms and signs such as nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. Advise patients to seek medical attention if they experience a constellation of these symptoms [see Warnings and Precautions (5.10)].
Important Administration Instructions
Instruct patients how to properly take ASCOMP with CODEINE. [see Dosage and Administration (2.2)]. Patients should take the drug only for as long as it is prescribed, in the amounts prescribed, and no more frequently than prescribed.
Important Discontinuation Instructions
- In order to avoid developing withdrawal symptoms, instruct patients not to discontinue ASCOMP with Codeine without first discussing a tapering plan with the prescriber [see Dosage and Administration (2.3)].
- Hypotension
Inform patients that ASCOMP with CODEINE may cause orthostatic hypotension and syncope. Instruct patients how to recognize symptoms of low blood pressure and how to reduce the risk of serious consequences should hypotension occur (e.g., sit or lie down, carefully rise from a sitting or lying position) [see Warnings and Precautions (5.11)].
Anaphylaxis
Inform patients that anaphylaxis has been reported with ingredients contained in ASCOMP with CODEINE. Advise patients how to recognize such a reaction and when to seek medical attention [see Contraindications (4), Adverse Reactions (6)].
Aspirin Allergy
Patients should be informed that ASCOMP with CODEINE contains aspirin and should not be taken by patients with an aspirin or NSAIDs allergy [see Warnings and Precautions (5.19)].
Pregnancy
Neonatal Opioid Withdrawal Syndrome
Inform female patients of reproductive potential that prolonged use of ASCOMP with CODEINE during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated [see Warnings and Precautions (5.6), Use in Specific Populations (8.1)].
Embryo-Fetal Toxicity
Inform female patients of reproductive potential that ASCOMP with CODEINE can (or may) cause fetal harm and to inform the healthcare provider of a known or suspected pregnancy [see Use in Specific Populations (8.1)].
Lactation
Advise women that breastfeeding is not recommended during treatment with ASCOMP with CODEINE [see Use in Specific Populations (8.2)].
Infertility
Inform patients that chronic use of opioids may cause reduced fertility. It is not known whether these effects on fertility are reversible [see Use in Specific Populations (8.3)].
Risk of Bleeding
Inform patients about the signs and symptoms of bleeding. Tell patients to notify their physician if they are prescribed any drug which may increase risk of bleeding.
Counsel patients who consume three or more alcoholic drinks daily about the bleeding risks involved with chronic, heavy alcohol use while taking aspirin [see Warnings and Precautions (5.17)].
Driving or Operating Heavy Machinery
Inform patients that ASCOMP with CODEINE may impair the ability to perform potentially hazardous activities such as driving a car or operating heavy machinery. Advise patients not to perform such tasks until they know how they will react to the medication [see Warnings and Precautions (5.16)].
Constipation
Advise patients of the potential for severe constipation, including management instructions and when to seek medical attention [see Adverse Reactions (6)].
Manufactured by: Nexgen Pharma, Inc., Irvine, CA 92606, USA
Rev. 12/2019
MEDICATION GUIDE
|
Medication Guide ASCOMP with CODEINE (AZ-komp) (Butalbital, Aspirin, Caffeine, and Codeine Phosphate, USP) capsules, CIII |
|
|
ASCOMP with CODEINE is:
|
|
|
Important information about ASCOMP with CODEINE:
|
|
|
Important Information Guiding Use in Pediatric Patients:
Do not give ASCOMP with CODEINE to a child or teenager with a viral illness. Reye syndrome, a life-threatening condition, can happen when aspirin (an ingredient in ASCOMP with CODEINE) is used in children and teenagers who have certain viral illnesses. Do not take ASCOMP with CODEINE if you have:
|
|
|
Before taking ASCOMP with CODEINE, tell your healthcare provider if you have a history of: |
|
|
|
|
|
|
Tell your healthcare provider if you are:
|
|
|
When taking ASCOMP with CODEINE:
|
|
|
While taking ASCOMP with CODEINE DO NOT:
|
|
|
The possible side effects of ASCOMP with CODEINE:
Get emergency medical help if you have:
These are not all the possible side effects of ASCOMP with CODEINE. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. For more information go to dailymed.nlm.nih.gov |
|
- This Medication Guide has been approved by the U.S. Food and Drug Administration. Issued: 12/2019