FULL PRESCRIBING INFORMATION
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Zmax and other antibacterial drugs, Zmax should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria.
1 INDICATIONS AND USAGE
Zmax is indicated for the treatment with mild to moderate infections caused by susceptible isolates of the designated microorganisms in the specific conditions listed below. [See CLINICAL STUDIES (14)]
Acute bacterial sinusitis in adults due to Haemophilus influenzae, Moraxella catarrhalis or Streptococcus pneumoniae.
Community-acquired pneumonia in adults and pediatric patients six months of age or older due to Chlamydophila pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae or Streptococcus pneumoniae, in patients appropriate for oral therapy. Pediatric use in this indication is based on extrapolation of adult efficacy. [See USE IN SPECIFIC POPULATIONS (8.4)]
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Zmax and other antibacterial drugs, Zmax should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Appropriate culture and susceptibility tests should be performed before treatment to determine the causative organism and its susceptibility to Zmax. [See Clinical Pharmacology (12.4)] Therapy with Zmax may be initiated before results of these tests are known; once the results become available, antimicrobial therapy should be adjusted accordingly.
2 DOSAGE AND ADMINISTRATION
2.1 Adults
Zmax should be taken as a single 2 g dose. Zmax provides a full course of antibacterial therapy in a single oral dose. It is recommended that Zmax be taken on an empty stomach (at least 1 hour before or 2 hours following a meal).
2.2 Pediatric patients
For pediatric patients 6 months and older, Zmax should be taken as a single dose of 60 mg/kg (equivalent to 27 mg/lb) body weight. The Zmax dose in mL is equivalent to the child's weight in lb (1 mL/lb dose, see Table 1 below), for a body weight of less than 75 lb (34 kg). It is recommended that Zmax be taken on an empty stomach (at least 1 hour before or 2 hours following a meal).
Pediatric patients weighing 75 lb (34 kg) or more should receive the adult dose (2 g).
| Dosing Calculated on 1 mL/lb, Dose 1 mL of Suspension for every 1 lb of Body Weight for Children <75 lb (34 kg)* | |||
| Weight | 1 mL/lb Dose | ||
| Lb | Kg | Dose | Volume |
| (mg) | (mL) | ||
|
|||
| 10 | 5 | 270 | 10 |
| 15 | 7 | 405 | 15 |
| 20 | 9 | 540 | 20 |
| 25 | 11 | 675 | 25 |
| 30 | 14 | 810 | 30 |
| 35 | 16 | 945 | 35 |
| 40 | 18 | 1080 | 40 |
| 45 | 20 | 1215 | 45 |
| 50 | 23 | 1350 | 50 |
| 55 | 25 | 1485 | 55 |
| 60 | 27 | 1620 | 60 |
| 65 | 30 | 1755 | 65 |
| 70 | 32 | 1890 | 70 |
| ≥75 | 34 | 2000 | Consume entire contents of bottle |
2.3 Additional treatment after vomiting with Zmax
In the event that a patient vomits within 5 minutes of administration, the health care provider should consider additional antibiotic treatment since there would be minimal absorption of azithromycin. Since insufficient data exist on absorption of azithromycin if a patient vomits between 5 and 60 minutes following administration, alternative therapy should be considered. Neither a second dose of Zmax nor alternative treatment is warranted if vomiting occurs ≥60 minutes following administration, in patients with normal gastric emptying. In patients with delayed gastric emptying, alternative therapy should be considered.
2.4 Instructions for the pharmacist
Constitute with 60 mL of water and replace cap. Shake bottle well before dispensing. Do not refrigerate. Constituted suspension should be consumed within 12 hours.
For pediatric dosing in patients weighing less than 75 lb (34 kg), use of a dosing device is recommended. The pharmacist should inform the patient's caregiver that any suspension remaining after dosing MUST be discarded.
3 DOSAGE FORMS AND STRENGTHS
Each bottle of Zmax contains azithromycin dihydrate equivalent to 2 g of azithromycin. After constitution with 60 mL of water, each mL of suspension contains 27 mg of azithromycin. The suspension is a white or off-white color and has a cherry/banana flavor.
4 CONTRAINDICATIONS
Zmax is contraindicated in patients with known hypersensitivity to azithromycin, erythromycin or any macrolide or ketolide antibiotic. [SEE WARNINGS AND PRECAUTIONS (5.1)]
5 WARNINGS AND PRECAUTIONS
5.1 Allergic and skin reactions
Serious allergic reactions, including angioedema, anaphylaxis, Stevens Johnson syndrome and toxic epidermal necrolysis have been reported rarely in patients on azithromycin therapy using other formulations. Although rare, fatalities have been reported. Despite initially successful symptomatic treatment of the allergic symptoms, when symptomatic therapy was discontinued, the allergic symptoms recurred soon thereafter in some patients without further azithromycin exposure. These patients required prolonged periods of observation and symptomatic treatment. The relationship of these episodes to the long tissue half-life of azithromycin and subsequent exposure to antigen has not been determined.
If an allergic reaction occurs, appropriate therapy should be instituted. Physicians should be aware that reappearance of the allergic symptoms may occur when symptomatic therapy is discontinued.
5.2 Clostridium difficile-associated diarrhea
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Zmax, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.3 Exacerbation of myasthenia gravis
Exacerbation of symptoms of myasthenia gravis and new onset of myasthenic syndrome have been reported in patients receiving azithromycin therapy.
5.4 Gastrointestinal Disturbances
A higher incidence of gastrointestinal adverse events (8 of 19 subjects) was observed when Zmax was administered to a limited number of subjects with GFR< 10 mL/min [See USE IN SPECIFIC POPULATIONS (8.6)]
5.5 Prolongation of the QT interval
Prolonged cardiac repolarization and QT interval, imparting a risk of developing cardiac arrhythmia and torsades de pointes, have been seen in treatment with other macrolides. A similar effect with azithromycin cannot be completely ruled out in patients at increased risk for prolonged cardiac repolarization.
6 ADVERSE REACTIONS
6.1 Clinical studies experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults:
The data described below reflect exposure to Zmax in 728 adult patients. All patients received a single 2 g oral dose of Zmax. The population studied had community-acquired pneumonia and acute bacterial sinusitis.
In controlled clinical trials with Zmax, the majority of the reported treatment-related adverse reactions were gastrointestinal in nature and mild to moderate in severity.
Overall, the most common treatment-related adverse reactions in adult patients receiving a single 2 g dose of Zmax were diarrhea/loose stools (12%), nausea (4%), abdominal pain (3%), headache (1%), and vomiting (1%). The incidence of treatment-related gastrointestinal adverse reactions was 17% for Zmax and 10% for pooled comparators.
Treatment-related adverse reactions following Zmax treatment that occurred with a frequency of <1% included the following:
Cardiovascular: palpitations, chest pain
Gastrointestinal: constipation, dyspepsia, flatulence, gastritis, oral moniliasis
Genitourinary: vaginitis
Nervous System: dizziness, vertigo
General: asthenia
Allergic: rash, pruritus, urticaria
Special Senses: taste perversion
Laboratory Abnormalities
In subjects with normal baseline values, the following clinically significant laboratory abnormalities (irrespective of drug relationship) were reported in Zmax clinical trials:
- -with an incidence of greater than or equal to 1%: reduced lymphocytes and increased eosinophils; reduced bicarbonate;
- -with an incidence of less than 1%: leukopenia, neutropenia, elevated bilirubin, AST, ALT, BUN, creatinine, alterations in potassium.
Where follow-up was provided, changes in laboratory tests appeared to be reversible.
Pediatric Patients:
The data described below reflect exposure to Zmax in 907 pediatric patients. The population was 3 months to 12 years of age. All patients received a single 60 mg/kg oral dose of Zmax.
As in adults, the most common treatment-related adverse reactions in pediatric subjects were gastrointestinal in nature. The pediatric subjects all received a single 60 mg/kg dose (equivalent to 27 mg/lb) of Zmax.
In a study with 450 pediatric subjects (ages 3 months to 48 months), vomiting (11%), diarrhea (10%) loose stools (9%), and abdominal pain (2%) were the most frequently reported treatment-related gastrointestinal adverse reactions. Many treatment related gastrointestinal adverse reactions with an incidence greater than 1% began on the day of dosing in these subjects [43% (68/160)] and most [53% (84/160)] resolved within 48 hours of onset. Treatment-related adverse events that were not gastrointestinal, occurring with a frequency ≥ 1% were: rash (5%), anorexia (2%), fever (2%), and dermatitis (2%).
In a second study of 337 pediatric subjects, ages 2 years to 12 years, the most frequently reported treatment-related adverse reactions also included vomiting (14%), diarrhea (7%), loose stools (2%), nausea (4%) and abdominal pain (4%).
A third study investigated the tolerability of two different concentrations of azithromycin oral suspension in 120 pediatric subjects (ages 3 months to 48 months), all of whom were treated with azithromycin. The study evaluated the hypothesis that a more dilute, less viscous formulation (the recommended 27 mg/mL concentration of Zmax) is less likely to induce vomiting in young children than a more concentrated suspension used in other pediatric studies. The vomiting rate for subjects taking the dilute concentration azithromycin was 3% (2/61). The rate was numerically lower but not statistically different from the vomiting for the more concentrated suspension Across both treatment arms, the only treatment-related adverse events with a frequency of ≥ 1% were vomiting (6%, 7/120) and diarrhea (2%, 2/120).
Treatment-related adverse reactions with a frequency of < 1% following Zmax treatment in all 907 pediatric subjects in the Phase 3 studies were:
Body as a whole: chills, fever, flu syndrome, headache;
Digestive: abnormal stools, constipation, dyspepsia, flatulence, gastritis, gastrointestinal disorder, hepatitis;
Hemic and Lymphatic: leukopenia;
Nervous System: agitation, emotional liability, hostility, hyperkinesia, insomnia, irritability, parasthesia, somnolence;
Respiratory: asthma, bronchitis, cough increased, dyspnea, pharyngitis, rhinitis;
Skin and Appendages: dermatitis, fungal dermatitis, maculopapular rash, pruritus, urticaria;
Special Senses: otitis media, taste perversion;
Urogenital: dysuria.
Laboratory Abnormalities
In subjects with normal baseline values, the following clinically significant laboratory abnormalities (irrespective of drug relationship) were reported in Zmax pediatric clinical trials:
- -with an incidence of greater than or equal to 1%: elevated eosinophils, BUN, and potassium; decreased lymphocytes; and alterations in neutrophils;
- -with an incidence of less than 1%: elevated SGOT, SGPT and creatinine; decreased potassium; and alterations in sodium and glucose.
6.2 Postmarketing experience with other azithromycin products
Because these reactions are reported voluntarily from a population of uncertain size, reliably estimating their frequency or establishing a causal relationship to drug exposure is not always possible.
Adverse events reported with azithromycin immediate release formulations during the postmarketing period for which a causal relationship may not be established include:
Allergic: arthralgia, edema, urticaria and angioedema
Cardiovascular: palpitations and arrhythmias including ventricular tachycardia and hypotension
There have been rare reports of QT prolongation and torsades de pointes.
Gastrointestinal: anorexia, constipation, dyspepsia, flatulence, vomiting/diarrhea rarely resulting in dehydration, pseudomembranous colitis, pancreatitis, oral candidiasis and rare reports of tongue discoloration
General: asthenia, paresthesia, fatigue, malaise and anaphylaxis (rarely fatal)
Genitourinary: interstitial nephritis, acute renal failure, moniliasis and vaginitis
Hematopoietic: thrombocytopenia, mild neutropenia
Liver/Biliary: abnormal liver function including hepatitis and cholestatic jaundice, as well as rare cases of hepatic necrosis and hepatic failure, some of which have resulted in death
Nervous System: convulsions, dizziness/vertigo, headache, somnolence, hyperactivity, nervousness, agitation and syncope
Psychiatric: aggressive reaction and anxiety
Skin/Appendages: pruritus, rash, photosensitivity, rarely serious skin reactions including erythema multiforme, Stevens-Johnson syndrome and toxic epidermal necrolysis
Special Senses: hearing disturbances including hearing loss, deafness and/or tinnitus and rare reports of taste/smell perversion and/or loss
7 DRUG INTERACTIONS
Warfarin
Although, in a study of 22 healthy men, a 5-day course of azithromycin did not affect the prothrombin time from a subsequently administered dose of warfarin, spontaneous post-marketing reports suggest that concomitant administration of azithromycin may potentiate the effects of oral anticoagulants. Prothrombin times should be carefully monitored while patients are receiving azithromycin and oral anticoagulants concomitantly.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects. Pregnancy Category B: Reproduction studies have been performed in rats and mice at doses up to moderately maternally toxic dose concentrations (i.e., 200 mg/kg/day). These daily doses in rats and mice, based on mg/m2, are estimated to be approximately equivalent to one or one-half of, respectively, the single adult oral dose of 2 g. In the animal studies, no evidence of harm to the fetus due to azithromycin was found. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, azithromycin should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
It is not known whether azithromycin is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when azithromycin is administered to a nursing woman.
8.4 Pediatric Use
Safety and effectiveness in the treatment of pediatric patients under 6 months of age have not been established.
Community-Acquired Pneumonia: The safety and effectiveness of Zmax have been established in pediatric patients 6 months of age or older with community-acquired pneumonia due to Chlamydophila pneumoniae, Mycoplasma pneumoniae, Haemophilus influenzae or Streptococcus pneumoniae. Use of Zmax for these patients is supported by evidence from adequate and well-controlled studies of Zmax in adults with additional safety and pharmacokinetic data in pediatric patients. [See DOSAGE AND ADMINISTRATION (2.2), ADVERSE REACTIONS (6), CLINICAL PHARMACOLOGY (12.3)]
8.5 Geriatric Use
Data collected from the azithromycin capsule and tablet formulations indicate that a dosage adjustment does not appear to be necessary for older patients with normal renal function (for their age) and hepatic function receiving treatment with Zmax.
In clinical trials of Zmax, 17% of subjects were at least 65 years of age (214/1292) and 5% of subjects (59/1292) were at least 75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects.
8.6 Renal Impairment
No dosage adjustment is recommended for patients GFR >10 mL/min. Caution should be exercised when Zmax is administered to patients with GFR <10 mL/min, due to a higher incidence of gastrointestinal adverse events (8 of 19 subjects) observed in a limited number of subjects with GFR <10 mL/min. [See CLINICAL PHARMACOLOGY (12)]
8.7 Gender
The impact of gender on the pharmacokinetics of azithromycin has not been evaluated for Zmax. However, previous studies have demonstrated no significant differences in the disposition of azithromycin between male and female subjects. No dosage adjustment of Zmax is recommended based on gender.
10 OVERDOSAGE
Adverse events experienced in higher than recommended doses were similar to those seen at normal doses. In the event of overdosage, general symptomatic and supportive measures are indicated as required.
11 DESCRIPTION
Zmax (azithromycin extended release) for oral suspension contains the active ingredient azithromycin (as azithromycin dihydrate), an azalide, a subclass of macrolide antibiotics. Azithromycin has the chemical name (2R,3S,4R,5R,8R,10R,11R,12S,13S,14R)13-[(2,6-Dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl) oxy]-2-ethyl-3,4,10-trihydroxy-3,5,6,8,10,12,14-heptamethyl-11-[[3,4,6-trideoxy-3- (dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-1-oxa-6-azacyclopentadecan-15-one. Azithromycin is derived from erythromycin; however, it differs chemically from erythromycin in that a methyl-substituted nitrogen atom is incorporated into the lactone ring. Its molecular formula is C38H72N2O12, and its molecular weight is 749.0. Azithromycin has the following structural formula:
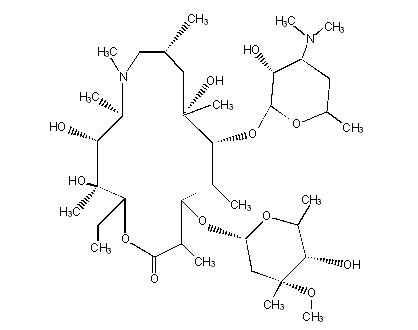
Azithromycin, as the dihydrate, is a white crystalline powder with a molecular formula of C38H72N2O12•2H2O and a molecular weight of 785.0.
Zmax is a single-dose, extended release formulation of microspheres for oral suspension containing azithromycin (as azithromycin dihydrate) and the following excipients: glyceryl behenate, poloxamer 407, sucrose, sodium phosphate tribasic anhydrous, magnesium hydroxide, hydroxypropyl cellulose, xanthan gum, colloidal silicon dioxide, titanium dioxide, artificial cherry flavor, and artificial banana flavor.
Note: Each bottle of Zmax 2 g for oral suspension contains approximately 148 mg of sodium and 19 g of sucrose. Constituted Zmax oral suspension contains approximately 2 mg/mL of sodium and 0.26 g/mL of sucrose.
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
Based on animal models of infection, the antimicrobial activity of azithromycin appears to correlate with the ratio of area under the concentration-time curve to minimum inhibitory concentration (AUC/MIC) for certain pathogens (S. pneumoniae and S. aureus). The principal pharmacokinetic/pharmacodynamic parameter best associated with clinical and microbiological cure has not been elucidated in clinical trials with Zmax.
12.3 Pharmacokinetics
Zmax is an extended release microsphere formulation. Based on data obtained from studies evaluating the pharmacokinetics of azithromycin in healthy adult subjects a higher peak serum concentration (Cmax) and greater systemic exposure (AUC 0–24) of azithromycin are achieved on the day of dosing following a single 2 g dose of Zmax versus 1.5 g of azithromycin tablets administered over 3 days (500 mg/day) or 5 days (500 mg on day 1, 250 mg/day on days 2–5) [Table 2]. Consequently, due to these different pharmacokinetic profiles, Zmax is not interchangeable with azithromycin tablet 3-day and 5-day dosing regimens.
| Pharmacokinetic Parameter* | Azithromycin Regimen | ||
| Zmax [N=41]† | 3-day ‡
[N=12] | 5-day ‡
[N=12] |
|
| SD = standard deviation Cmax = maximum serum concentration Tmax = time to Cmax AUC = area under concentration vs. time curve t1/2 = terminal serum half-life |
|||
| Cmax (µg/mL) | 0.821 (0.281) | 0.441 (0.223) | 0.434 (0.202) |
| Tmax§ (hr) | 5.0 (2.0–8.0) | 2.5 (1.0–4.0) | 2.5 (1.0–6.0) |
| AUC0–24 (µg∙hr/mL) | 8.62 (2.34) | 2.58 (0.84) | 2.60 (0.71) |
| AUC0–∞¶ (µg∙hr/mL) | 20.0 (6.66) | 17.4 (6.2) | 14.9 (3.1) |
| t1/2 (hr) | 58.8 (6.91) | 71.8 (14.7) | 68.9 (13.8) |
Absorption
The bioavailability of Zmax relative to azithromycin immediate release (IR) (powder for oral suspension) was 83%. On average, peak serum concentrations were achieved approximately 2.5 hours later following Zmax administration and were lower by 57%, compared to 2 g azithromycin IR. Thus, single 2 g doses of Zmax and azithromycin IR are not bioequivalent and are not interchangeable.
Effect of food on absorption: A high-fat meal increased the rate and extent of absorption of a 2 g dose of Zmax (115% increase in Cmax, and 23% increase in AUC0–72) compared to the fasted state. A standard meal also increased the rate of absorption (119% increase in Cmax) and with less effect on the extent of absorption (12% increase in AUC0–72) compared to administration of a 2 g Zmax dose in the fasted state.
Effect of antacids: Following the administration of Zmax with an aluminum and magnesium hydroxide antacid, the rate and extent of azithromycin absorption were not altered.
Distribution
The serum protein binding of azithromycin is concentration dependent, decreasing from 51% at 0.02 µg/mL to 7% at 2 µg/mL. Following oral administration, azithromycin is widely distributed throughout the body with an apparent steady-state volume of distribution of 31.1 L/kg.
Azithromycin concentrates in fibroblasts, epithelial cells, macrophages, and circulating neutrophils and monocytes. Higher azithromycin concentrations in tissues than in plasma or serum have been observed. White blood cell and lung exposure data in humans following a single 2 g dose of Zmax in adults are shown in Table 3. Following a 2 g single dose of Zmax, azithromycin achieved higher exposure (AUC0–120) in mononuclear leukocytes (MNL) and polymorphonuclear leukocytes (PMNL) than in serum. The azithromycin exposure (AUC0–72) in lung tissue and alveolar cells (AC) was approximately 100 times that in serum; and the exposure in epithelial lining fluid (ELF) was also higher (approximately 2–3 times) than in serum. The clinical significance of this distribution data is unknown.
| A single 2 g dose of Zmax | ||||
| Abbreviation: WBC: white blood cells; MNL: mononuclear leukocytes; PMNL: polymorphonuclear leukocytes; ELF: Epithelial lining fluid | ||||
| WBC | Cmax (µg/mL) | AUC0–24 (µg∙hr/mL) | AUC0–120 (µg∙hr/mL) | Ct=120* (µg/mL) |
| MNL† | 116 (40.2) | 1790 (540) | 4710 (1100) | 16.2 (5.51) |
| PMNL† | 146 (66.0) | 2080 (650) | 10000 (2690) | 81.7 (23.3) |
| LUNG | Cmax (µg/mL) | AUC0–24 (µg∙hr/mL) | AUC0–72 (µg∙hr/mL) | |
| ALVEOLAR CELL‡ | 669 | 7028 | 20403 | - |
| ELF‡ | 3.2 | 17.6 | 131 | - |
| Cmax (µg/g) | AUC0–24 (µg∙hr/g) | AUC0–72 (µg∙hr/g) | ||
| LUNG TISSUE‡ | 37.9 | 505 | 1693 | - |
Following a regimen of 500 mg of azithromycin tablets on the first day and 250 mg daily for 4 days, only very low concentrations were noted in cerebrospinal fluid (less than 0.01 µg/mL) in the presence of non-inflamed meninges.
Metabolism
In vitro and in vivo studies to assess the metabolism of azithromycin have not been performed.
Excretion
Serum azithromycin concentrations following a single 2 g dose of Zmax declined in a polyphasic pattern with a terminal elimination half-life of 59 hours. The prolonged terminal half-life is thought to be due to a large apparent volume of distribution.
Biliary excretion of azithromycin, predominantly as unchanged drug, is a major route of elimination. Over the course of a week, approximately 6% of the administered dose appears as unchanged drug in urine.
Special Populations
Renal Impairment
Azithromycin pharmacokinetics were investigated in 42 adults (21 to 85 years of age) with varying degrees of renal impairment. Following the oral administration of a single 1.0 g dose of azithromycin (4 × 250 mg capsules), the mean Cmax and AUC0–120 were 5.1% and 4.2% higher, respectively in subjects with GFR 10 to 80 mL/min compared to subjects with normal renal function (GFR >80 mL/min). The mean Cmax and AUC0–120 were 61% and 35% higher, respectively in subjects with GFR <10 mL/min compared to subjects with normal renal function. (See Renal Impairment (8.6).)
Hepatic Impairment
The pharmacokinetics of azithromycin in subjects with hepatic impairment has not been established.
Pediatric Patients
The pharmacokinetics of azithromycin were characterized following a single 60 mg/kg dose of Zmax in pediatric patients aged 3 months to 16 years. Although there was high inter-patient variability in systemic exposure (AUC and Cmax) across the age groups studied, individual azithromycin AUC and Cmax values in pediatric patients were comparable to or higher than those following administration of 2 g Zmax in adults (Table 4). (See Pediatric Use (8.4).)
| Treatment Group | Pharmacokinetic Parameters | |||
| Cmax
(µg/mL) | Tmax*
(hr) | AUC(0–24)
(µg∙hr/mL) | AUC(0–∞)
(µg∙hr/mL) |
|
| Empty stomach = dosed with Zmax at least 1 hour before or 2 hours after a meal (Groups I–VI) Fed = dosed with Zmax within 5 minutes of consuming an age-appropriate high-fat breakfast (Group VII) |
||||
| Group 1 (N = 6) [3 to 18 months] | 0.74 (0.20) | 3 (3–3) | 6.29 (1.17) | 14.1 (2.16) (n = 3) |
| Group 2† (N = 6) [>18 to 36 months] | 1.88† (0.50) | 3 (3–3) | 19.7† (5.35) | 37.3 (12.9) (n = 5) |
| Group 3 (N = 6) [>36 to 48 months] | 1.23 (0.42) | 3 (3–6) | 12.9 (3.79) | 22.4 (5.96) |
| Group 4 (N = 6) [>48 months to 8 years] | 1.13 (0.34) | 3 (3–6) | 13.0 (4.21) | 22.2 (6.89) |
| Group 5 (N = 6) [>8 to 12 years] | 1.65 (0.38) | 3 (3–6) | 16.0 (4.99) | 30.1 (10.7) |
| Group 6 (N = 6) [>12 to 16 years] | 0.98 (0.35) | 3 (3–6) | 11.0 (4.78) | 21.3 (9.37) |
| Pooled 1–6 (N = 36) [On an empty stomach] | 1.27 (0.53) | 3 (3–6) | 13.1 (5.78) | 25.2 (10.7) (n = 32) |
| Group 7‡ (N = 7) [Fed; 18 months to 8 years] | 1.41 (0.62) | 3 (1.5–3.1) | 7.43 (3.00) | 18.9 (3.57) (n = 3) |
Pharmacokinetic Interaction Studies
A drug interaction study was performed with Zmax and antacids. All other drug interaction studies were performed with azithromycin immediate release (IR) formulations (capsules and tablets, doses ranging from 500 to 1200 mg) and other drugs likely to be co-administered. The effects of co-administration of azithromycin on the pharmacokinetics of other drugs are shown in Table 5 and the effects of other drugs on the pharmacokinetics of azithromycin are shown in Table 6.
When used at therapeutic doses, azithromycin IR had a minimal effect on the pharmacokinetics of atorvastatin, carbamazepine, cetirizine, didanosine, efavirenz, fluconazole, indinavir, midazolam, nelfinavir, sildenafil, theophylline (intravenous and oral), triazolam, trimethoprim/sulfamethoxazole or zidovudine (Table 5). Although the drug interaction studies were not conducted with Zmax, similar modest effect as observed with IR formulation are expected since the total exposure to azithromycin is comparable for Zmax and other azithromycin IR regimens. Therefore, no dosage adjustment of drugs listed in Table 5 is recommended when co-administered with Zmax.
Nelfinavir significantly increased the Cmax and AUC of azithromycin following co-administration with azithromycin IR 1200 mg (Table 6). However, no dose adjustment of azithromycin is recommended when Zmax is co-administered with nelfinavir.
Pharmacokinetic and/or pharmacodynamic interactions with the drugs listed below have not been reported in clinical trials with azithromycin; however, no specific drug interaction studies have been performed to evaluate potential drug-drug interaction. Nonetheless, pharmacokinetic and/or pharmacodynamic interactions with these drugs have been observed with other macrolide products. Until further data are developed, careful monitoring of patients is advised when azithromycin and these drugs are used concomitantly: digoxin, ergotamine or dihydroergotamine, cyclosporine, hexobarbital and phenytoin.
| Co-administered Drug | Dose of Co-administered Drug | Dose of Azithromycin* | n | Ratio (with/without Azithromycin) of Co-administered Drug Pharmacokinetic Parameters (90% CI); No Effect = 1.00 | |
| Mean Cmax | Mean AUC | ||||
| Atorvastatin | 10 mg/day × 8 days | 500 mg/day PO on days 6–8 | 12 | 0.83 (0.63 to 1.08) | 1.01 (0.81 to 1.25) |
| Carbamazepine | 200 mg/day × 2 days, then 200 mg BID × 18 days | 500 mg/day PO for days 16–18 | 7 | 0.97 (0.88 to 1.06) | 0.96 (0.88 to 1.06) |
| Cetirizine | 20 mg/day × 11 days | 500 mg PO on day 7, then 250 mg/day on days 8–11 | 14 | 1.03 (0.93 to 1.14) | 1.02 (0.92 to 1.13) |
| Didanosine | 200 mg PO BID × 21 days | 1,200 mg/day PO on days 8–21 | 6 | 1.44 (0.85 to 2.43) | 1.14 (0.83 to 1.57) |
| Efavirenz | 400 mg/day × 7 days | 600 mg PO on day 7 | 14 | 1.04† | 0.95† |
| Fluconazole | 200 mg PO single dose | 1,200 mg PO single dose | 18 | 1.04 (0.98 to 1.11) | 1.01 (0.97 to 1.05) |
| Indinavir | 800 mg TID × 5 days | 1,200 mg PO on day 5 | 18 | 0.96 (0.86 to 1.08) | 0.90 (0.81 to 1.00) |
| Midazolam | 15 mg PO on day 3 | 500 mg/day PO × 3 days | 12 | 1.27 (0.89 to 1.81) | 1.26 (1.01 to 1.56) |
| Nelfinavir | 750 mg TID × 11 days | 1,200 mg PO on day 9 | 14 | 0.90 (0.81 to 1.01) | 0.85 (0.78 to 0.93) |
| Sildenafil | 100 mg on days 1 and 4 | 500 mg/day PO × 3 days | 12 | 1.16 (0.86 to 1.57) | 0.92 (0.75 to 1.12) |
| Theophylline | 4 mg/kg IV on days 1, 11, 25 | 500 mg PO on day 7, then 250 mg/day on days 8–11 | 10 | 1.19 (1.02 to 1.40) | 1.02 (0.86 to 1.22) |
| Theophylline | 300 mg PO BID × 15 days | 500 mg PO on day 6, then 250 mg/day on days 7–10 | 8 | 1.09 (0.92 to 1.29) | 1.08 (0.89 to 1.31) |
| Triazolam | 0.125 mg on day 2 | 500 mg PO on day 1, then 250 mg/day on day 2 | 12 | 1.06† | 1.02† |
| Trimethoprim/
Sulfamethoxazole | 160 mg/800 mg/day PO × 7 days | 1,200 mg PO on day 7 | 12 | 0.85 (0.75 to 0.97)/ 0.90 (0.78 to 1.03) | 0.87 (0.80 to 0.95)/ 0.96 (0.88 to 1.03) |
| Zidovudine | 500 mg/day PO × 21 days | 600 mg/day PO × 14 days | 5 | 1.12 (0.42 to 3.02) | 0.94 (0.52 to 1.70) |
| Zidovudine | 500 mg/day PO × 21 days | 1,200 mg/day PO × 14 days | 4 | 1.31 (0.43 to 3.97) | 1.30 (0.69 to 2.43) |
| Co-administered Drug | Dose of Co-administered Drug | Dose of Azithromycin* | n | Ratio (with/without co-administered drug) of Azithromycin Pharmacokinetic Parameters (90% CI); No Effect = 1.00 | |
| Mean Cmax | Mean AUC | ||||
| Efavirenz | 400 mg/day × 7 days | 600 mg PO on day 7 | 14 | 1.22 (1.04 to 1.42) | 0.92† |
| Fluconazole | 200 mg PO single dose | 1,200 mg PO single dose | 18 | 0.82 (0.66 to 1.02) | 1.07 (0.94 to 1.22) |
| Nelfinavir | 750 mg TID × 11 days | 1,200 mg PO on day 9 | 14 | 2.36 (1.77 to 3.15) | 2.12 (1.80 to 2.50) |
| Aluminum and Magnesium hydroxide | 20 mL regular strength, single dose | 2 g Zmax, single dose | 39 | 0.99 (0.93 to 1.06) | 0.99 (0.92 to 1.08) |
12.4 Microbiology
Mechanism of Action
Azithromycin acts by binding to the 50S ribosomal subunit of susceptible microorganisms, thus interfering with microbial protein synthesis. Nucleic acid synthesis is not affected.
Spectrum of Activity
Azithromycin has been shown to be active against most isolates of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Aerobic and facultative Gram-positive microorganisms
Streptococcus pneumoniae
NOTE: Erythromycin- and penicillin-resistant Gram-positive isolates may demonstrate cross-resistance to azithromycin.
Aerobic and facultative Gram-negative microorganisms
Haemophilus influenzae
Moraxella catarrhalis
Beta-lactamase production should not affect azithromycin activity.
"Other" microorganisms
Chlamydophila pneumoniae
Mycoplasma pneumoniae
The following in vitro data are available, but their clinical significance is unknown.
At least 90% of the following microorganisms exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the azithromycin susceptible breakpoints of <4 µg/mL. However, the safety and effectiveness of azithromycin in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled trials.
Aerobic and facultative Gram-positive microorganisms
Staphylococcus aureus
Streptococcus agalactiae
Streptococcus pyogenes
Streptococci (Groups C, F, G)
Viridans group streptococci
Aerobic and facultative Gram-negative microorganisms
Bordetella pertussis
Legionella pneumophila
Anaerobic microorganisms
Peptostreptococcus species
Prevotella bivia
"Other" microorganisms
Ureaplasma urealyticum
Susceptibility Testing Methods:
When available, the clinical microbiology laboratory should provide cumulative results of in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial.
Dilution techniques:
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method1,3 (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of azithromycin powder. The MIC values should be interpreted according to criteria provided in Table 7.
Diffusion techniques:
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure2,3 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 15-µg azithromycin to test the susceptibility of microorganisms to azithromycin. The disk diffusion interpretive criteria are provided in Table 7.
| Minimum Inhibitory Concentrations (µg/mL) | Disk Diffusion (zone diameters in mm) |
|||||
| Pathogen | S | I | R* | S | I | R* |
|
||||||
| Haemophilus influenzae | ≤ 4 | -- | -- | ≥ 12 | -- | -- |
| Streptococcus pneumoniae | ≤ 0.5 | 1 | ≥ 2 | ≥ 18 | 14–17 | ≤ 13 |
No interpretive criteria have been established for testing Moraxella catarrhalis. This species is not usually tested.
A report of "susceptible" indicates that the pathogen is likely to be inhibited if the antimicrobial compound reaches the concentrations usually achievable. A report of "intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone, which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound reaches the concentrations usually achievable; other therapy should be selected.
Quality Control:
Standardized susceptibility test procedures require the use of quality control microorganisms to determine if the test was performed correctly. Standard azithromycin powder should provide the range of values noted in Table 8. Quality control (QC) microorganisms are specific strains of organisms with intrinsic biological properties. QC strains are very stable strains, which will give a standard and repeatable susceptibility pattern. The specific strains used for microbiological quality control are not clinically significant.
| QC Strain | Minimum Inhibitory Concentrations (µg/mL) | Disk Diffusion (zone diameters in mm) |
| Haemophilus influenzae
ATCC 49247 | 1.0–4.0 | 13–21 |
| Streptococcus pneumoniae
ATCC 49619 | 0.06–0.25 | 19–25 |
13 NONCLINICAL TOXICOLOGY
13. 1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed to evaluate carcinogenic potential. Azithromycin has shown no mutagenic potential in standard laboratory tests: mouse lymphoma assay, human lymphocyte clastogenic assay, and mouse bone marrow clastogenic assay. No evidence of impaired fertility due to azithromycin was found in rats given daily doses up to 10 mg/kg (approximately 0.05 times the single 2 g oral adult human dose on a mg/m2 basis).
13. 2 Animal Toxicology and/or Pharmacology
Phospholipidosis (intracellular phospholipid accumulation) has been observed in some tissues of mice, rats, and dogs given multiple doses of azithromycin. It has been demonstrated in numerous organ systems (e.g., eye, dorsal root ganglia, liver, gallbladder, kidney, spleen, and/or pancreas) in dogs treated with azithromycin at doses which, expressed on the basis of mg/m2, are approximately one-sixth the recommended adult dose, and in rats treated at doses approximately one-fourth the recommended adult dose. This effect has been shown to be reversible after cessation of azithromycin treatment. Based on the pharmacokinetic data, phospholipidosis has been seen in the rat (50 mg/kg/day dose) at the observed maximal plasma concentration of 1.3 µg/mL (1.6 times the observed Cmax of 0.821 µg/mL at the adult dose of 2 g.) Similarly, it has been shown in the dog (10 mg/kg/day dose) at the observed maximal serum concentration of 1 µg/mL (1.2 times the observed Cmax of 0.821 µg/mL at the adult dose of 2 g).
Phospholipidosis was also observed in neonatal rats dosed for 18 days at 30 mg/kg/day, which is less than the pediatric dose of 60 mg/kg on a mg/m2 basis, but was not observed in neonatal rats treated for 10 days at 40 mg/kg/day with mean maximal serum concentrations of 1.86 µg/ml, approximately 1.5 times the Cmax of 1.27 µg/ml at the pediatric dose. Phospholipidosis has been observed in neonatal dogs (10 mg/kg/day) at maximum mean whole blood concentrations of 3.54 µg/ml, approximately 3 times the pediatric dose Cmax.
The significance of the finding for animals and for humans is unknown.
14 CLINICAL STUDIES
Acute Bacterial Maxillary Sinusitis
Adult subjects with a diagnosis of acute bacterial maxillary sinusitis were evaluated in a randomized, double-blind, multicenter study; a maxillary sinus tap was performed on all subjects at baseline. Clinical evaluations were conducted for all subjects at the TOC visit, 7 to 14 days post-treatment. Two hundred seventy (270) subjects were treated with a single 2 g oral dose of Zmax and 268 subjects were treated with levofloxacin, 500 mg orally QD for 10 days. A subject was considered a cure if signs and symptoms related to the acute infection had resolved, or if clinical improvement was such that no additional antibiotics were deemed necessary. The clinical response for the primary population, Clinical Per Protocol Subjects, is presented below.
| ZMAX | LEVOFLOXACIN | |
| RESPONSE AT TOC | N = 255 | N = 254 |
| CURE | 241 (94.5%) | 236 (92.9%) |
| FAILURE | 14 (5.5%) | 18 (7.1%) |
Clinical response by pathogen in the Bacteriologic Per Protocol population is presented below.
| Zmax | Levofloxacin | |||
| Pathogen | N | Cure | N | Cure |
| S. pneumoniae | 37 | 36 (97.3%) | 39 | 36 (92.3%) |
| H. influenzae | 27 | 26 (96.3%) | 30 | 30 (100.0%) |
| M. catarrhalis | 8 | 8 (100.0%) | 11 | 10 (90.9%) |
Community-Acquired Pneumonia
Adult subjects with a diagnosis of mild-to-moderate community-acquired pneumonia were evaluated in two, randomized, double-blind, multicenter studies. In both studies, clinical and microbiologic evaluations were conducted for all subjects at the Test of Cure (TOC) visit, 7 to 14 days post-treatment. In the first study, 247 subjects were treated with a single 2 g oral dose of Zmax and 252 subjects were treated with clarithromycin extended release, 1 g orally QD for 7 days. In the second study, 211 subjects were treated with a single 2.0 g oral dose of Zmax and 212 subjects were treated with levofloxacin, 500 mg orally QD for 7 days. A patient was considered a cure if signs and symptoms related to the acute infection had resolved, or if clinical improvement was such that no additional antibiotics were deemed necessary; in addition, the chest x-ray performed at the TOC visit was to be either improved or stable. The clinical response at TOC for the primary population, Clinical Per Protocol Subjects, is presented in the table below.
| ZMAX | COMPARATOR | |
| ZMAX VS. CLARITHROMYCIN EXTENDED RELEASE | N=202 | N=209 |
| CURE | 187 (92.6%) | 198 (94.7%) |
| FAILURE | 15 (7.4%) | 11 (5.3%) |
| ZMAX VS. LEVOFLOXACIN | N=174 | N=189 |
| CURE | 156 (89.7%) | 177 (93.7%) |
| FAILURE | 18 (10.3%) | 12 (6.3%) |
Clinical response by pathogen in the Bacteriologic Per Protocol population, across both studies, is presented below:
| Pathogen | Zmax | Comparators | ||
| N | Cure | N | Cure | |
| S. pneumoniae | 33 | 28 (84.8%) | 39 | 35 (89.7%) |
| H. influenzae | 30 | 28 (93.3%) | 34 | 31 (91.2%) |
| C. pneumoniae | 40 | 37 (92.5%) | 53 | 50 (94.3%) |
| M. pneumoniae | 33 | 30 (90.9%) | 39 | 38 (97.4%) |
15 REFERENCES
- Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard – Seventh Edition. 2006. CLSI Document M7-A7 [ISBN 1-56238-587-9]. CLSI, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2006.
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard – Ninth Edition. CLSI Document M2-A9 (ISBN 1-56238-586-0). CLSI, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2006.
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing; Eighteenth Informational Supplement. 2008. CLSI Document M100-S18 [ISBN 1-56238-653-0]. CLSI, 940 West Valley Road, Suite 1400, Wayne, Pennsylvania 19087-1898 USA, 2008.
16 HOW SUPPLIED/STORAGE AND HANDLING
NDC 21695-444-60 for pediatric use is supplied in bottles containing 2 g of azithromycin and should be constituted with 60 mL of water.
Storage
Before constitution, store dry powder at or below 30°C (86°F).
After constitution, store suspension at 25°C (77°F); excursions permitted to 15–30°C (59–86°F) [see USP Controlled Room Temperature]. Do not refrigerate or freeze.
Constituted suspension should be consumed within 12 hours. For adult patients, the entire bottle should be consumed. For pediatric patients, any suspension remaining after dosing MUST be discarded.
17 PATIENT COUNSELING INFORMATION
See FDA-approved Patient Labeling (17.2)
17.1 General Patient Counseling
- Patients should be instructed to take Zmax on an empty stomach (at least 1 hour before or 2 hours following a meal).
- To ensure accurate dosing for children, use of a dosing spoon, medicine syringe, or cup is recommended.
- Patients should be told that Zmax needs time to work, so the patient may not feel better right away. If the patient's symptoms do not improve in a few days, the patient or their guardian should call their doctor.
- Patients should be instructed to immediately contact a physician if any signs of an allergic reaction occur.
- Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
- Patients who vomit within the first hour should contact their health care provider about further treatment.
- Keep bottle tightly closed. Store at room temperature. Use within 12 hours of constitution. Shake bottle well before use. Adult patients should consume the entire contents of the bottle; pediatric patients should take the recommended dose and MUST discard any unused portion.
- Patients should be advised that Zmax may be taken without regard to antacids containing magnesium hydroxide and/or aluminum hydroxide.
Patients should be counseled that antibacterial drugs including Zmax should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). Not taking the complete prescribed dose may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Zmax or other antibacterial drugs in the future.
Read the Patient Information that comes with Zmax ® carefully before you or your child take it. This leaflet does not take the place of talking with your doctor about you or your child's medical condition or treatment. Only your doctor can decide if Zmax is right for you or your child.
What is Zmax?
Zmax is an antibiotic that kills certain bacteria. Zmax is dosed differently from other antibiotics.
You take just one dose, one time.
- Day 1: Take Zmax in one dose. Zmax starts working.
- Days 2 – 3: As with most antibiotics, you may not feel better right away.
- After Day 3: Zmax continues to work over time. If your symptoms are not better, call your doctor.
Zmax is used in adults and in children over the age of 6 months against bacteria to treat certain kinds of pneumonia (lung infections)
Zmax is used in adults against bacteria to treat sinus infections.
Zmax only works against bacteria. It does not work against viruses, like the common cold or flu.
Zmax has not been studied in children under 6 months of age.
Who should not take Zmax?
- You or your child should not take Zmax if allergic to:
- anything in Zmax. See the end of this leaflet for a complete list of ingredients in Zmax.
- antibiotics like erythromycin or telithromycin (Ketek®).
Talk with your doctor or pharmacist if you have questions about your medicine allergies.
Before you start Zmax...
Tell your doctor about all your or your child's medical problems including if you or your child :
- have liver problems.
- have kidney problems.
- have myasthenia gravis.
- are pregnant, or might be pregnant. It is not known if Zmax could harm your baby.
- are breast-feeding.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. Especially tell your doctor if you or your child are taking warfarin (Coumadin®, Jantoven)
Know the medicines you take. Keep a list of your medicines and show it to your doctor or pharmacist when you get a new prescription.
Do I need to prepare Zmax?
- If you get Zmax in liquid form, it is ready to take.
- If you get Zmax as dry powder, you must add water to the bottle before you take it. To prepare Zmax:
- Open the bottle: To open the bottle, press down on the cap and twist.
- Use a measuring cup to add 60 mL (1/4 cup) water to the Zmax bottle.
- Tightly close the bottle and shake to mix it.
How do I take Zmax?
- Keep Zmax at room temperature between 59ºF to 86ºF (15º to 30ºC).
- Shake the bottle well before using.
- Take Zmax or give it to your child within 12 hours after it has been prepared by the pharmacy or you add water to the powder.
- Take Zmax or give it to your child exactly how your doctor prescribes it. This will help to treat you or your child's infection and decrease the chance that Zmax or other antibiotics will not work to treat infections in the future.
- Adults: take all the medicine in the bottle.
- Children: give your child the amount of Zmax prescribed by your doctor and throw away the rest of the medicine.
- To be sure that you give your child the right dose of Zmax, use a dosing spoon, medicine syringe, or cup.
- Take Zmax on an empty stomach (at least 1 hour before eating or 2 hours after eating).
- You can take antacids with Zmax.
- If you or your child throws up (vomits) within one hour of taking Zmax, call your doctor right away to see if more medicine is needed. Do not give your child more Zmax unless your doctor tells you to.
- If your child takes too much Zmax, call your doctor right away or go to the nearest hospital emergency room.
How will I know Zmax is working?
Zmax needs time to work, so you or your child may not feel better right away. If you or your child's symptoms do not get better in a few days, call your doctor.
What are possible side effects of Zmax?
Zmax may cause serious side effects. These happened in a small number of patients. Call your doctor right away or get emergency treatment if you or your child have any of the following:
-
Serious allergic reaction or serious skin reaction: Get emergency help right away if you or your child has:
- Hives, skin rash, sores in your mouth, or your skin blisters and peels
- Trouble swallowing,
- Swelling of your face, eyes, lips, tongue or throat
- Wheezing or trouble breathing
These symptoms could go away and then come back.
- Diarrhea: Call your doctor right away if you have diarrhea that does not go away, is severe, watery, or has blood in it. Diarrhea can occur as late as two or more months after you take an antibiotic such as Zmax.
- Abnormal heart rhythm. Tell your doctor right away if you or your child feel your heart beating in your chest or an abnormal heart beat, get dizzy or faint. This has been seen with other antibiotics like Zmax.
The most common side effects in adults are:
- Diarrhea/loose stools
- Nausea
- Stomach pain
- Headache
- Vomiting
The most common side effects in children are:
- Vomiting
- Diarrhea/loose stools
- Nausea
- Stomach pain
Tell your doctor if you have any side effects that bother your or your child, or that does not go away.
These are not all of the possible side effects with Zmax. For a list of all reported side effects, ask your doctor or pharmacist.
General information about Zmax
Doctors sometimes prescribe medicines for conditions that are not in the patient leaflets. Do not use Zmax for anything other than what your doctor prescribed. Do not give it to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet is a summary of the most important information about Zmax. For more information, talk with your doctor. You can ask your doctor or pharmacist for information about Zmax that is written for healthcare professionals. For more information, go to our website at www.zmaxinfo.com or call 1-800-438-1985.
What is in Zmax?
Active ingredient: azithromycin dihydrate
Inactive ingredients: glyceryl behenate, poloxamer 407, sucrose, sodium phosphate tribasic anhydrous, magnesium hydroxide, hydroxypropyl cellulose, xanthan gum, colloidal silicon dioxide, titanium dioxide, artificial cherry flavor, and artificial banana flavor
Brand names are registered trademarks of their respective owners.
Coumadin® is a registered trademark of Bristol-Myers Squibb, Inc.
Ketek® is a registered trademark of Aventis Pharmaceuticals Inc.
LAB-0384-3.0
June 2009
Repackaged by:
Rebel Distributors Corp
Thousand Oaks, CA 91320
