Cardiovascular Thrombotic Events
- Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use (see WARNINGS and PRECAUTIONS).
- Etodolac extended-release tablets, 400 mg, 500 mg and 600 mg are contraindicated in the setting of coronary artery bypass graft (CABG) surgery (see CONTRAINDICATIONS and WARNINGS).
Gastrointestinal Risk
- NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS).
DESCRIPTION
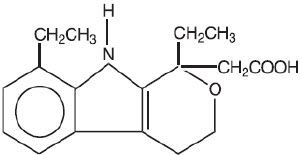
Etodolac Extended-Release Tablets contain etodolac, which is a member of the pyranocarboxylic acid group of nonsteroidal anti-inflammatory drugs (NSAIDs). Each tablet contains etodolac for oral administration. Etodolac is a racemic mixture of [+]S and [-]R-enantiomers. It is a white crystalline compound, insoluble in water, but soluble in alcohols, chloroform, dimethyl sulfoxide, and aqueous polyethylene glycol.
The chemical name is (±) 1,8-diethyl-1,3,4,9-tetrahydropyrano-[3,4-b]indole-1-acetic acid. The molecular weight is 287.37. Its molecular formula is C 17H 21NO 3 and it has the following structural formula:
The inactive ingredients in etodolac extended-release tablets include: HPMC 2910, hydroxypropyl methylcellulose, lactose anhydrous, magnesium stearate, microcrystalline cellulose, PEG 8000, polydextrose FCC, povidone, titanium dioxide and triacetin. In addition, the 500 mg and 600 mg tablets contain Indigo Carmine Lake and the 400 mg and 600 mg tablets contain Allura Red AC Lake and Sunset Yellow F.C.F. Lake. In addition, the 500 mg tablets contain yellow iron oxide.
Meets USP Dissolution Test 4.
CLINICAL PHARMACOLOGY
Pharmacodynamics
Etodolac extended-release tablets are a nonsteroidal anti-inflammatory drug (NSAID) that exhibits anti-inflammatory, analgesic, and antipyretic activities in animal models. The mechanism of action of etodolac extended-release tablets, like that of other NSAIDs, is not completely understood, but may be related to prostaglandin synthetase inhibition.
Pharmacokinetics
Absorption
Etodolac extended-release tablets and etodolac tablets both contain etodolac, but differ in their release characteristics. The systemic availability of etodolac from etodolac extended-release tablets is generally greater than 80%. Etodolac does not undergo significant first-pass metabolism following oral administration. After oral administration of etodolac extended-release tablets in doses up to 800 mg once daily, peak concentrations occur approximately 6 hours after dosing and are dose proportional for both total and free etodolac.
Table 1 shows the comparison of etodolac pharmacokinetic parameters after the administration of etodolac tablets and etodolac extended-release tablets.
Table 2 shows the etodolac pharmacokinetic parameters in various populations. The data from patients with renal and hepatic impairment were obtained following administration of (immediate-release) etodolac tablets.
| Mean (CV)% * | ||
|---|---|---|
| Pharmacokinetic Parameters | Etodolac Tablets | Etodolac Extended-Release Tablets |
|
||
| Extent of Oral Absorption (Bioavailability) [F] | ≥ 80% | ≥ 80% |
| Time to Peak Concentration (T max), h | 1.4 (61%) | 6.7 (47%) |
| Oral Clearance (CL/F), mL/h/kg | 49.1 (33%) | 46.8 (37%) |
| Apparent Volume of Distribution (Vd/F), mL/kg | 393 (29%) | 566 (26%) |
| Terminal Half-Life (t½), h | 6.4 (22%) | 8.4 (30%) |
| Etodolac Extended-Release Tablets | Etodolac Tablets | |||||||
|---|---|---|---|---|---|---|---|---|
| PK Parameters | Normal Healthy Adults | Healthy Males | Healthy Females | Elderly
(> 65 yr) | Hemodialysis
†
(24 to 65) (n=9) | Renal
Impairment † | Hepatic
Impairment † |
|
| (18 to 44)
‡
(n=116) | (18 to 43)
(n=102) | (25 to 44)
(n=14) | (66 to 88)
(n=24 | Dialysis On | Dialysis Off | (46 to 73)
(n=10) | (34 to 60)
(n=9) |
|
| NA = not available | ||||||||
| T max, h | 6.7
(47%) * | 6.8
(45%) | 4.5
(56%) | 6.2
(51%) | 1.7
(88%) | 0.9
(67%) | 2.1
(46%) | 1.1
(15%) |
| Oral Clearance, mL/h/kg (CL/F) | 46.8
(37%) | 46.8
(37%) | 47.2
(38%) | 51.6
(40%) | NA | NA | 58.3
(19%) | 42.0
(43%) |
| Apparent Volume of Distribution, mL/kg (Vd/F) | 566
(26%) | 580
(26%) | 459
(28%) | 552
(34%) | NA | NA | NA | NA |
| Terminal Half-Life, h | 8.4
(30%) | 8.4
(29%) | 7.6
(45%) | 7.8
(26%) | 5.1
(22%) | 7.5
(34%) | NA | 5.7
(24%) |
Food/Antacid Effects
Food has no significant effect on the extent of etodolac extended-release tablets absorption, however, food significantly increased C max (54%) following a 600 mg dose.
The extent of absorption of etodolac is not affected when etodolac is administered with antacid. Coadministration, with an antacid, decreases the peak concentration reached by about 15 to 20% with no measurable effect on time-to-peak.
Distribution
The mean apparent volume of distribution (Vd/F) of etodolac following administration of etodolac extended-release tablets is 566 mL/kg. Etodolac is more than 99% bound to plasma proteins, primarily to albumin, and is independent of etodolac concentration over the dose range studied. It is not known whether etodolac is excreted in human milk. However, based on its physical-chemical properties, excretion into breast milk is expected.
Metabolism
Etodolac metabolites do not contribute significantly to the pharmacological activity of etodolac extended-release tablets.
Following administration of immediate-release etodolac, several metabolites have been identified in human plasma and urine. Other metabolites remain to be identified. The metabolites include 6-, 7-, and 8- hydroxylated etodolac and etodolac glucuronide. After a single dose of 14C-etodolac, hydroxylated metabolites accounted for less than 10% of total drug in serum. On chronic dosing, hydroxylated-etodolac metabolites do not accumulate in the plasma of patients with normal renal function. The extent of accumulation of hydroxylated-etodolac metabolites in patients with renal dysfunction has not been studied. The role, if any, of a specific cytochrome P450 system in the metabolism of etodolac is unknown. The hydroxylated-etodolac metabolites undergo further glucuronidation followed by renal excretion and partial elimination in the feces.
Excretion
The mean oral clearance of etodolac following oral etodolac extended-release tablets dosing is 47 (±17) mL/h/kg. The terminal half-life (t ½) of etodolac after etodolac extended-release tablets administration is 8.4 hours compared to 6.4 hours for etodolac tablets. Approximately 1% of an etodolac tablet dose is excreted unchanged in the urine, with 72% of the dose excreted into the urine as parent drug plus metabolites:
| -etodolac, unchanged | 1% |
| -etodolac glucuronide | 13% |
| -hydroxylated metabolites (6-, 7-, and 8-OH) | 5% |
| -hydroxylated metabolite glucuronides | 20% |
| -unidentified metabolites | 33% |
Fecal excretion accounted for 16% of the dose.
Special Populations
Geriatric
In clinical studies, age was not shown to have any effect on half-life or protein binding, and demonstrated no change in expected drug accumulation. No dosage adjustment is generally necessary in the elderly on the basis of pharmacokinetics. The elderly may need dosage adjustment, however, as they may be more sensitive to antiprostaglandin effects than younger patients (see PRECAUTIONS, Geriatric Use).
Pediatric
The pharmacokinetics of etodolac extended-release tablets were assessed in an open-label, 12-week clinical trial which included plasma sampling for population pharmacokinetics. Seventy-two (72) patients, 6 to 16 years of age, with juvenile rheumatoid arthritis, received etodolac extended-release tablets in doses of 13.3 to 21.3 mg/kg given as 400 to 1000 mg once daily. The results from a population pharmacokinetic analysis based on the 59 subjects who completed the trial are as follows:
| Parameter | JRA * (Age: 6 to 16) † n = 59 |
|---|---|
| Oral Clearance (CL/F), mL/h/kg | 47.8 (38%) |
| Apparent Volume of Distribution (Vd/F), mL/kg | 78.9 (61%) |
| Half-life (t ½), h | 12.1 (75%) |
While similar, the pharmacokinetic parameters for children with juvenile rheumatoid arthritis did not directly correlate with adult pharmacokinetic data in rheumatoid arthritis. In the population pharmacokinetic analysis, body weights below 50 kg were found to correlate with CL/F (see DOSAGE AND ADMINISTRATION).
Race
Pharmacokinetic differences due to race have not been identified. Clinical studies included patients of many races, all of whom responded in a similar fashion.
Hepatic Insufficiency
The pharmacokinetics of etodolac following administration of etodolac extended-release tablets have not been investigated in subjects with hepatic insufficiency. Following administration of etodolac tablets, the plasma protein binding and disposition of total and free etodolac were unchanged in the presence of compensated hepatic cirrhosis. Although no dosage adjustment is generally required in patients with chronic hepatic diseases, etodolac clearance is dependent on liver function and could be reduced in patients with severe hepatic failure.
Renal Insufficiency
The pharmacokinetics of etodolac following administration of etodolac extended-release tablets have not been investigated in subjects with renal insufficiency. Etodolac renal clearance following administration of etodolac tablets was unchanged in the presence of mild-to-moderate renal failure (creatinine clearance, 37 to 88 mL/min). Although renal elimination is a significant pathway of excretion for etodolac metabolites, no dosing adjustment in patients with mild-to-moderate renal dysfunction is generally necessary. Etodolac plasma protein binding decreases in patients with severe renal deficiency. Etodolac should be used with caution in such patients because, as with other NSAIDs, it may further decrease renal function in some patients. Etodolac is not significantly removed from the blood in patients undergoing hemodialysis.
CLINICAL STUDIES
Arthritis
The use of etodolac extended-release tablets in managing the signs and symptoms of osteoarthritis of the knee and rheumatoid arthritis was assessed in double-blind, randomized, parallel, controlled clinical trials in 1552 patients. In these trials, etodolac extended-release tablets, given once daily, provided efficacy comparable to immediate-release etodolac.
The safety, efficacy, and pharmacokinetics of etodolac extended-release tablets were assessed in an open-label, 12-week clinical trial. Seventy-two (72) patients, 6 to 16 years of age, with juvenile rheumatoid arthritis, received etodolac extended-release tablets in doses of 400 to 1000 mg (13.3 to 21.3 mg/kg body weight) once daily. At these doses, etodolac extended-release tablets controlled the signs and symptoms of juvenile rheumatoid arthritis. Based on the results of this study, the safety profile of etodolac extended-release tablets (at doses not exceeding 20 mg/kg) appeared to be similar to that observed in the adult arthritic patients in clinical trials. (See PRECAUTIONS, Pediatric Use).
INDICATIONS AND USAGE
Carefully consider the potential benefits and risks of etodolac extended-release tablets and other treatment options before deciding to use etodolac extended-release tablets. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
Etodolac extended-release tablets are indicated:
- For relief of signs and symptoms of juvenile arthritis
- For relief of the signs and symptoms of rheumatoid arthritis
- For relief of the signs and symptoms of osteoarthritis
CONTRAINDICATIONS
Etodolac extended-release tablets are contraindicated in patients with known hypersensitivity to etodolac.
Etodolac extended-release tablets should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients (see WARNINGS, Anaphylactoid Reactions and PRECAUTIONS, Preexisting Asthma).
Etodolac extended-release tablets are contraindicated in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS).
WARNINGS
Cardiovascular Effects
Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as etodolac, increases the risk of serious gastrointestinal (GI) events (see WARNINGS).
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery found an increased incidence of myocardial infarction and stroke. NSAIDs are contraindicated in the setting of CABG (see CONTRAINDICATIONS).
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of etodolac extended-release tablets in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If etodolac extended-release tablets are used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
Hypertension
NSAIDs, including etodolac extended-release tablets, can lead to onset of new hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including etodolac extended-release tablets, should be used with caution in patients with hypertension. Blood pressure (BP) should be monitored closely during the initiation of NSAID treatment and throughout the course of therapy.
Heart Failure and Edema
The Coxib and traditional NSAID Trialists' Collaboration meta-analysis of randomized controlled trials demonstrated an approximately two-fold increase in hospitalizations for heart failure in COX-2 selective-treated patients and nonselective NSAID-treated patients compared to placebo-treated patients. In a Danish National Registry study of patients with heart failure, NSAID use increased the risk of MI, hospitalization for heart failure, and death.
Additionally, fluid retention and edema have been observed in some patients treated with NSAIDs. Use of etodolac may blunt the CV effects of several therapeutic agents used to treat these medical conditions [e.g., diuretics, ACE inhibitors, or angiotensin receptor blockers (ARBs)] (see Drug Interactions).
Avoid the use of etodolac extended-release tablets in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure. If etodolac extended-release tablets are used in patients with severe heart failure, monitor patients for signs of worsening heart failure.
Gastrointestinal Effects - Risk of Ulceration, Bleeding, and Perforation
NSAIDs, including etodolac extended-release tablets, can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3 to 6 months, and in about 2 to 4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
NSAIDs should be prescribed with extreme caution in those with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10-fold increased risk for developing a GI bleed compared to patients with neither of these risk factors. Other factors that increase the risk for GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population.
To minimize the potential risk for an adverse GI event in patients treated with an NSAID, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. This should include discontinuation of the NSAID until a serious GI adverse event is ruled out. For high risk patients, alternate therapies that do not involve NSAIDs should be considered.
Renal Effects
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a nonsteroidal anti-inflammatory drug may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
Renal pelvic transitional epithelial hyperplasia, a spontaneous change occurring with variable frequency, was observed with increased frequency in treated male rats in a 2-year chronic study.
Caution is recommended in patients with pre-existing kidney disease.
Advanced Renal Disease
No information is available from controlled clinical studies regarding the use of etodolac extended-release tablets in patients with advanced renal disease. Therefore, treatment with etodolac extended-release tablets is not recommended in these patients with advanced renal disease. If etodolac extended-release tablet therapy must be initiated, close monitoring of the patient's renal function is advisable.
Anaphylactoid Reactions
As with other NSAIDs, anaphylactoid reactions may occur in patients without known prior exposure to etodolac extended-release tablets. Etodolac extended-release tablets should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs (see CONTRAINDICATIONS and PRECAUTIONS, Preexisting Asthma). Emergency help should be sought in cases where an anaphylactoid reaction occurs.
Skin Reactions
NSAIDs, including etodolac extended-release tablets, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) has been reported in patients taking NSAIDs such as etodolac extended-release tablets. Some of these events have been fatal or life-threatening. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling. Other clinical manifestations may include hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis. Sometimes symptoms of DRESS may resemble an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its presentation, other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, discontinue etodolac extended-release tablets and evaluate the patient immediately.
Fetal Toxicity
Premature Closure of Fetal Ductus Arteriosus
Avoid use of NSAIDs, including etodolac extended-release tablets, in pregnant women at about 30 weeks gestation and later. NSAIDs including etodolac extended-release tablets, increase the risk of premature closure of the fetal ductus arteriosus at approximately this gestational age.
Oligohydramnios/Neonatal Renal Impairment
Use of NSAIDs, including etodolac extended-release tablets, at about 20 weeks gestation or later in pregnancy may cause fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation. Oligohydramnios is often, but not always, reversible with treatment discontinuation. Complications of prolonged oligohydramnios may, for example, include limb contractures and delayed lung maturation. In some postmarketing cases of impaired neonatal renal function, invasive procedures such as exchange transfusion or dialysis were required.
If NSAID treatment is necessary between about 20 weeks and 30 weeks gestation, limit etodolac extended-release tablets use to the lowest effective dose and shortest duration possible. Consider ultrasound monitoring of amniotic fluid if etodolac extended-release tablets treatment extends beyond 48 hours. Discontinue etodolac extended-release tablets if oligohydramnios occurs and follow up according to clinical practice [ see PRECAUTIONS; Pregnancy].
PRECAUTIONS
General
Etodolac extended-release tablets cannot be expected to substitute for corticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to disease exacerbation. Patients on prolonged corticosteroid therapy should have their therapy tapered slowly if a decision is made to discontinue corticosteroids.
The pharmacological activity of etodolac extended-release tablets in reducing fever and inflammation may diminish the utility of these diagnostic signs in detecting complications of presumed noninfectious, painful conditions.
Hepatic Effects
Borderline elevations of one or more liver tests may occur in up to 15% of patients taking NSAIDs including etodolac extended-release tablets. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Notable elevations of ALT or AST (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. In addition, rare cases of severe hepatic reactions, including jaundice and fatal fulminant hepatitis, liver necrosis and hepatic failure, some of them with fatal outcomes have been reported.
A patient with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred, should be evaluated for evidence of the development of a more severe hepatic reaction while on therapy with etodolac extended-release tablets. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), etodolac extended-release tablets should be discontinued.
Hematological Effects
Anemia is sometimes seen in patients receiving NSAIDs, including etodolac extended-release tablets. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Patients on long-term treatment with NSAIDs, including etodolac extended-release tablets, should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia.
NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients. Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration, and reversible. Patients receiving etodolac extended-release tablets who may be adversely affected by alterations in platelet function, such as those with coagulation disorders or patients receiving anticoagulants, should be carefully monitored.
Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since cross reactivity, including bronchospasm, between aspirin and other nonsteroidal anti-inflammatory drugs has been reported in such aspirin-sensitive patients, etodolac extended-release tablets should not be administered to patients with this form of aspirin sensitivity and should be used with caution in patients with preexisting asthma.
Information for Patients
Patients should be informed of the following information before initiating therapy with an NSAID and periodically during the course of ongoing therapy. Patients should also be encouraged to read the NSAID Medication Guide that accompanies each prescription dispensed.
-
Cardiovascular Thrombotic Events
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately (see WARNINGS). - Etodolac extended-release tablets, like other NSAIDs, can cause GI discomfort and, rarely, serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, patients should be alert for the signs and symptoms of ulcerations and bleeding, and should ask for medical advice when observing any indicative sign or symptoms including epigastric pain, dyspepsia, melena, and hematemesis. Patients should be apprised of the importance of this follow-up (see WARNINGS, Gastrointestinal Effects - Risk of Ulceration, Bleeding, and Perforation).
-
Serious Skin Reactions, including DRESS
Advise patients to stop taking etodolac extended-release tablets immediately if they develop any type of rash or fever and to contact their healthcare provider as soon as possible [ see Warnings]. -
Heart Failure and Edema
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur (see WARNINGS). - Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If these occur, patients should be instructed to stop therapy and seek immediate medical therapy.
- Patients should be informed of the signs of an anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). If these occur, patients should be instructed to seek immediate emergency help (see WARNINGS).
-
Fetal Toxicity
Inform pregnant women to avoid use of etodolac extended-release tablets and other NSAIDs starting at 30 weeks gestation because of the risk of the premature closing of the fetal ductus arteriosus. If treatment with etodolac extended-release tablets is needed for a pregnant woman between about 20 to 30 weeks gestation, advise her that she may need to be monitored for oligohydramnios, if treatment continues for longer than 48 hours [ see WARNINGS; Fetal Toxicity, PRECAUTIONS; Pregnancy].
Laboratory Tests
Because serious GI tract ulcerations and bleeding can occur without warning symptoms, physicians should monitor for signs or symptoms of GI bleeding. Patients on long-term treatment with NSAIDs, should have their CBC and a chemistry profile checked periodically. If clinical signs and symptoms consistent with liver or renal disease develop, systemic manifestations occur (e.g., eosinophilia, rash, etc.) or if abnormal liver tests persist or worsen, etodolac extended-release tablets should be discontinued.
Drug Interactions
ACE-inhibitors
Reports suggest that NSAIDs may diminish the antihypertensive effect of ACE-inhibitors. This interaction should be given consideration in patients taking NSAIDs concomitantly with ACE-inhibitors.
Aspirin
When etodolac extended-release tablets are administered with aspirin, its protein binding is reduced, although the clearance of free etodolac is not altered. The clinical significance of this interaction is not known; however, as with other NSAIDs, concomitant administration of etodolac extended-release tablets and aspirin is not generally recommended because of the potential of increased adverse effects.
Cyclosporine and Digoxin
Etodolac extended-release tablets, like other NSAIDs, through effects on renal prostaglandins, may cause changes in the elimination of these drugs, leading to elevated serum levels of cyclosporine and digoxin and increased toxicity. Nephrotoxicity associated with cyclosporine may also be enhanced. Patients receiving these drugs who are given etodolac extended-release tablets, or any other NSAID, and particularly those patients with altered renal function, should be observed for the development of the specific toxicities of these drugs.
Furosemide
Clinical studies, as well as post marketing observations, have shown that etodolac extended-release tablets can reduce the natriuretic effect of furosemide and thiazides in some patients. This response has been attributed to inhibition of renal prostaglandin synthesis. During concomitant therapy with NSAIDs, the patient should be observed closely for signs of renal failure (see WARNINGS, Renal Effects), as well as to assure diuretic efficacy.
Lithium
NSAIDs have produced an elevation of plasma lithium levels and a reduction in renal lithium clearance. The mean minimum lithium concentration increased 15% and the renal clearance was decreased by approximately 20%. These effects have been attributed to inhibition of renal prostaglandin synthesis by the NSAID. Thus, when NSAIDs and lithium are administered concurrently, subjects should be observed carefully for signs of lithium toxicity.
Methotrexate
NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Caution should be used when NSAIDs are administered concomitantly with methotrexate.
Drug/Laboratory Test Interactions
The urine of patients who take etodolac can give a false-positive reaction for urinary bilirubin (urobilin) due to the presence of phenolic metabolites of etodolac. Diagnostic dip-stick methodology, used to detect ketone bodies in urine, has resulted in false-positive findings in some patients treated with etodolac. Generally, this phenomenon has not been associated with other clinically significant events. No dose relationship has been observed.
Etodolac treatment is associated with a small decrease in serum uric acid levels. In clinical trials, mean decreases of 1 to 2 mg/dL were observed in arthritic patients receiving etodolac (600 mg to 1000 mg/day) after 4 weeks of therapy. These levels then remained stable for up to 1 year of therapy.
Carcinogenesis, Mutagenesis, and Impairment of Fertility
No carcinogenic effect of etodolac was observed in mice or rats receiving oral doses of 15 mg/kg/day (45 to 89 mg/m 2, respectively) or less for periods of 18 months or 2 years, respectively. Etodolac was not mutagenic in in vitro tests performed with S. typhimurium and mouse lymphoma cells as well as in an in vivo mouse micronucleus test. However, data from the in vitro human peripheral lymphocyte test showed an increase in the number of gaps (3% to 5% unstained regions in the chromatid without dislocation) among the etodolac-treated cultures (50 to 200 g/mL) compared to negative controls (2%); no other difference was noted between the controls and drug-treated groups. Etodolac showed no impairment of fertility in male and female rats up to oral doses of 16 mg/kg (94 mg/m 2). However, reduced implantation of fertilized eggs occurred in the 8 mg/kg group.
Pregnancy
Risk Summary
Use of NSAIDs, including etodolac extended-release tablets, can cause premature closure of the fetal ductus arteriosus and fetal renal dysfunction leading to oligohydramnios and, in some cases, neonatal renal impairment. Because of these risks, limit dose and duration of etodolac extended-release tablets use between about 20 and 30 weeks of gestation, and avoid etodolac extended-release tablets use at about 30 weeks of gestation and later in pregnancy [ see Warnings; Fetal Toxicity].
Premature Closure of Fetal Ductus Arteriosus
Use of NSAIDs, including etodolac extended-release tablets, at about 30 weeks gestation or later in pregnancy increases the risk of premature closure of the fetal ductus arteriosus.
Oligohydramnios/Neonatal Renal Impairment
Use of NSAIDs at about 20 weeks gestation or later in pregnancy has been associated with cases of fetal renal dysfunction leading to oligohydramnios, and in some cases, neonatal renal impairment.
Data from observational studies regarding other potential embryofetal risks of NSAID use in women in the first or second trimesters of pregnancy are inconclusive. Reproductive studies conducted in rats and rabbits have not demonstrated evidence of developmental abnormalities. However, animal reproduction studies are not always predictive of human response. Based on animal data, prostaglandins have been shown to have an important role in endometrial vascular permeability, blastocyst implantation, and decidualization. In animal studies, administration of prostaglandin synthesis inhibitors such as etodolac, resulted in increased pre- and post-implantation loss. Prostaglandins also have been shown to have an important role in fetal kidney development. In published animal studies, prostaglandin synthesis inhibitors have been reported to impair kidney development when administered at clinically relevant doses.
The estimated background risk of major birth defects and miscarriage for the indicated population(s) is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Clinical Considerations
Fetal/Neonatal Adverse Reactions
Premature Closure of Fetal Ductus Arteriosus:
Avoid use of NSAIDs in women at about 30 weeks gestation and later in pregnancy, because NSAIDs, including etodolac extended-release tablets, can cause premature closure of the fetal ductus arteriosus [
see
WARNINGS; Fetal Toxicity].
Oligohydramnios/Neonatal Renal Impairment
If an NSAID is necessary at about 20 weeks gestation or later in pregnancy, limit the use to the lowest effective dose and shortest duration possible. If etodolac extended-release tablets treatment extends beyond 48 hours, consider monitoring with ultrasound for oligohydramnios. If oligohydramnios occurs, discontinue etodolac extended-release tablets and follow up according to clinical practice [ see WARNINGS; Fetal Toxicity].
Data
Human Data
There are no adequate and well-controlled studies in pregnant women. Because of the known effects of nonsteroidal anti-inflammatory drugs on the fetal cardiovascular system (closure of ductus arteriosus), use during pregnancy (particularly late pregnancy) should be avoided.
Premature Closure of Fetal Ductus Arteriosus
Published literature reports that the use of NSAIDs at about 30 weeks of gestation and later in pregnancy may cause premature closure of the fetal ductus arteriosus.
Oligohydramnios/Neonatal Renal Impairment
Published studies and postmarketing reports describe maternal NSAID use at about 20 weeks gestation or later in pregnancy associated with fetal renal dysfunction leading to oligohydramnios, and in some cases, neonatal renal impairment. These adverse outcomes are seen, on average, after days to weeks of treatment, although oligohydramnios has been infrequently reported as soon as 48 hours after NSAID initiation. In many cases, but not all, the decrease in amniotic fluid was transient and reversible with cessation of the drug. There have been a limited number of case reports of maternal NSAID use and neonatal renal dysfunction without oligohydramnios, some of which were irreversible. Some cases of neonatal renal dysfunction required treatment with invasive procedures, such as exchange transfusion or dialysis.
Methodological limitations of these postmarketing studies and reports include lack of a control group; limited information regarding dose, duration, and timing of drug exposure; and concomitant use of other medications. These limitations preclude establishing a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAID use. Because the published safety data on neonatal outcomes involved mostly preterm infants, the generalizability of certain reported risks to the full-term infant exposed to NSAIDs through maternal use is uncertain.
Labor and Delivery
In rat studies with NSAIDs, as with other drugs known to inhibit prostaglandin synthesis, an increased incidence of dystocia, delayed parturition, and decreased pup survival occurred. The effects of etodolac extended-release tablets on labor and delivery in pregnant women are unknown.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from etodolac extended-release tablets, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
ADVERSE REACTIONS
A total of 1552 patients were exposed to etodolac extended-release tablets in controlled clinical studies of at least 4 weeks in length and using daily doses in the range of 400 to 1200 mg. In the tabulations below, adverse event rates are generally categorized based on the incidence of events in the first 30 days of treatment with etodolac extended-release tablets. As with other NSAIDs, the cumulative adverse event rates may increase significantly over time with extended therapy.
In patients taking NSAIDs, including etodolac extended-release tablets, the most frequently reported adverse experiences occurring in approximately 1 to 10% of patients are:
gastrointestinal experiences including:
|
||
| abdominal pain | constipation | diarrhea |
| dyspepsia | flatulence | GI ulcers (gastric/duodenal) * |
| gross bleeding/perforation * | nausea | vomiting |
other events including:
| abnormal renal function * | anemia * | asthenia |
| dizziness | edema * | elevated liver enzymes * |
| headaches | hypertension | increased bleeding time * |
| infection | pharyngitis | pruritus |
| rashes | rhinitis | tinnitus * |
Additional NSAID Adverse Experiences Reported Occasionally with NSAIDs or Etodolac Extended-Release Tablets Include
Body as a whole - allergic reaction, anaphylactic/anaphylactoid reactions (including shock), chills, fever, sepsis
Cardiovascular system - congestive heart failure, flushing, palpitations, tachycardia, syncope, vasculitis (including necrotizing and allergic)
Digestive system - anorexia, cholestatic hepatitis, cholestatic jaundice, dry mouth, duodenitis, eructation, esophagitis, gastritis, gastric/peptic ulcers, glossitis, hepatic failure, hepatitis, hematemesis, intestinal ulceration, jaundice, liver necrosis, melena, pancreatitis, rectal bleeding, stomatitis
Hemic and lymphatic system - agranulocytosis, ecchymosis, eosinophilia, hemolytic anemia, leukopenia, neutropenia, pancytopenia, purpura, thrombocytopenia
Metabolic and nutritional - hyperglycemia in previously controlled diabetic patients
Nervous system - anxiety, confusion, depression, dream abnormalities, insomnia, nervousness, paresthesia, somnolence, tremors, vertigo
Respiratory system - asthma, dyspnea, pulmonary infiltration with eosinophilia
Skin and appendages - angioedema, cutaneous vasculitis with purpura, erythema multiforme, hyperpigmentation, sweating, urticaria, vesiculobullous rash
Special senses - blurred vision, photophobia, transient visual disturbances
Urogenital system - dysuria, elevated BUN, oliguria/polyuria, proteinuria, renal failure, renal insufficiency, renal papillary necrosis, serum creatinine increase, urinary frequency
Other NSAID Adverse Reactions, Which Occur Rarely Are
Body as a whole - anaphylactic reactions, appetite changes, death
Cardiovascular system - arrhythmia, cerebrovascular accident, hypotension, myocardial infarction
Digestive system - colitis, esophagitis with or without stricture or cardiospasm, thirst, ulcerative stomatitis
Hemic and lymphatic system - aplastic anemia, lymphadenopathy
Metabolic and nutritional - change in weight
Nervous system - coma, convulsions, hallucinations, meningitis
Respiratory - bronchitis, pneumonia, respiratory depression, sinusitis
Skin and appendages - alopecia, exfoliative dermatitis, maculopapular rash, photosensitivity, skin peeling, Stevens-Johnson syndrome, toxic epidermal necrosis
Special senses - conjunctivitis, deafness, hearing impairment, taste perversion
Urogenital system - cystitis, hematuria, interstitial nephritis, leukorrhea, renal calculus, uterine bleeding irregularities
OVERDOSAGE
Symptoms following acute NSAID overdose are usually limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Gastrointestinal bleeding can occur. Hypertension, acute renal failure, respiratory depression and coma may occur, but are rare. Anaphylactoid reactions have been reported with therapeutic ingestion of NSAIDs, and may occur following an overdose.
Patients should be managed by symptomatic and supportive care following an NSAID overdose. There are no specific antidotes. Emesis and/or activated charcoal (60 to 100 g in adults, 1 to 2 g/kg in children) and/or osmotic cathartic may be indicated in patients seen within 4 hours of ingestion with symptoms or following a large overdose (5 to 10 times the usual dose). Forced diuresis, alkalinization of the urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
DOSAGE AND ADMINISTRATION
Carefully consider the potential benefits and risks of etodolac extended-release tablets and other treatment options before deciding to use etodolac extended-release tablets. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
After observing the response to initial therapy with etodolac extended-release tablets, the dose and frequency should be adjusted to suit an individual patient's needs.
Juvenile Rheumatoid Arthritis
For the relief of the signs and symptoms of juvenile rheumatoid arthritis in patients 6 to 16 years of age, the recommended dose given orally once per day should be based on body weight, according to the following table:
| Body Weight Range (kg) | Dose |
|---|---|
| 20 to 30 | 400 mg Tablet × 1 |
| 31 to 45 | 600 mg Tablet × 1 |
| 46 to 60 | 400 mg Tablet × 2 |
| >60 | 500 mg Tablet × 2 |
Rheumatoid Arthritis and Osteoarthritis
For the relief of the signs and symptoms of osteoarthritis or rheumatoid arthritis, the recommended starting dose of etodolac extended-release tablets is 400 to 1000 mg given orally once per day.
As with other NSAIDs, the lowest effective dose should be sought for each patient. In chronic conditions, a therapeutic response to therapy with etodolac extended-release tablets is sometimes seen within one week of therapy, but most often is observed by two weeks.
HOW SUPPLIED
Etodolac extended-release tablets are available as:
400 mg tablets (pink, round, bi-convex, film coated tablet engraved with "T400" on one side and plain on the other side).
- in bottles of 100, NDC 60429-313-01
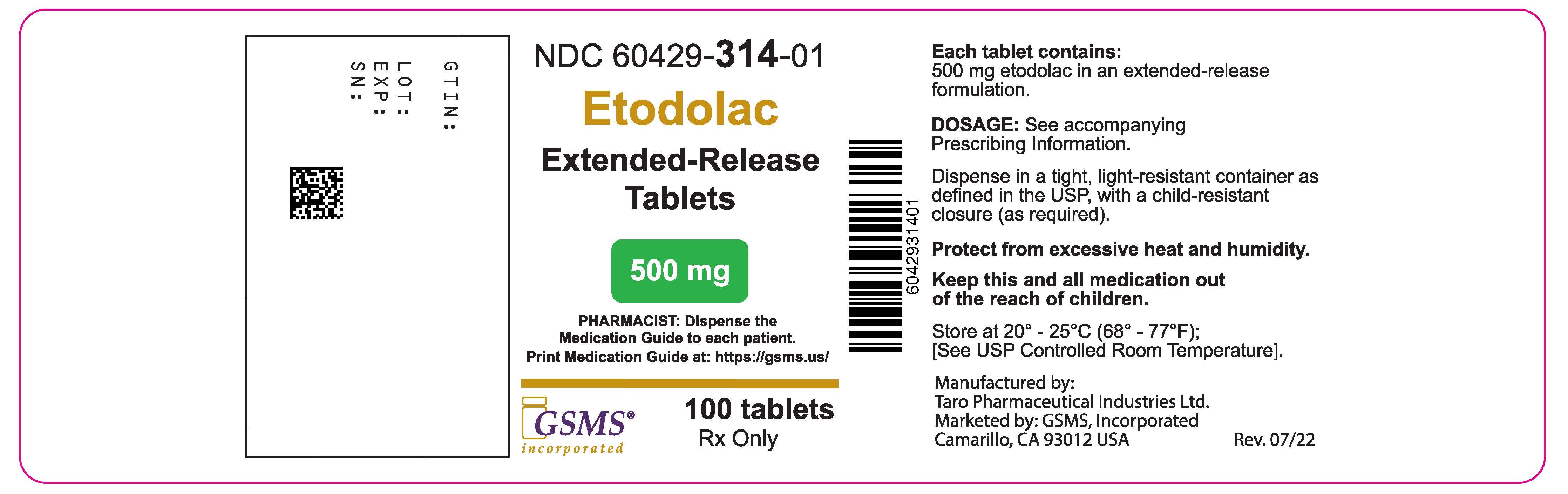
500 mg tablets (green, oblong, normal convex, film coated tablet engraved with "T500" on one side and plain on the other side).
- in bottles of 100, NDC 60429-314-01
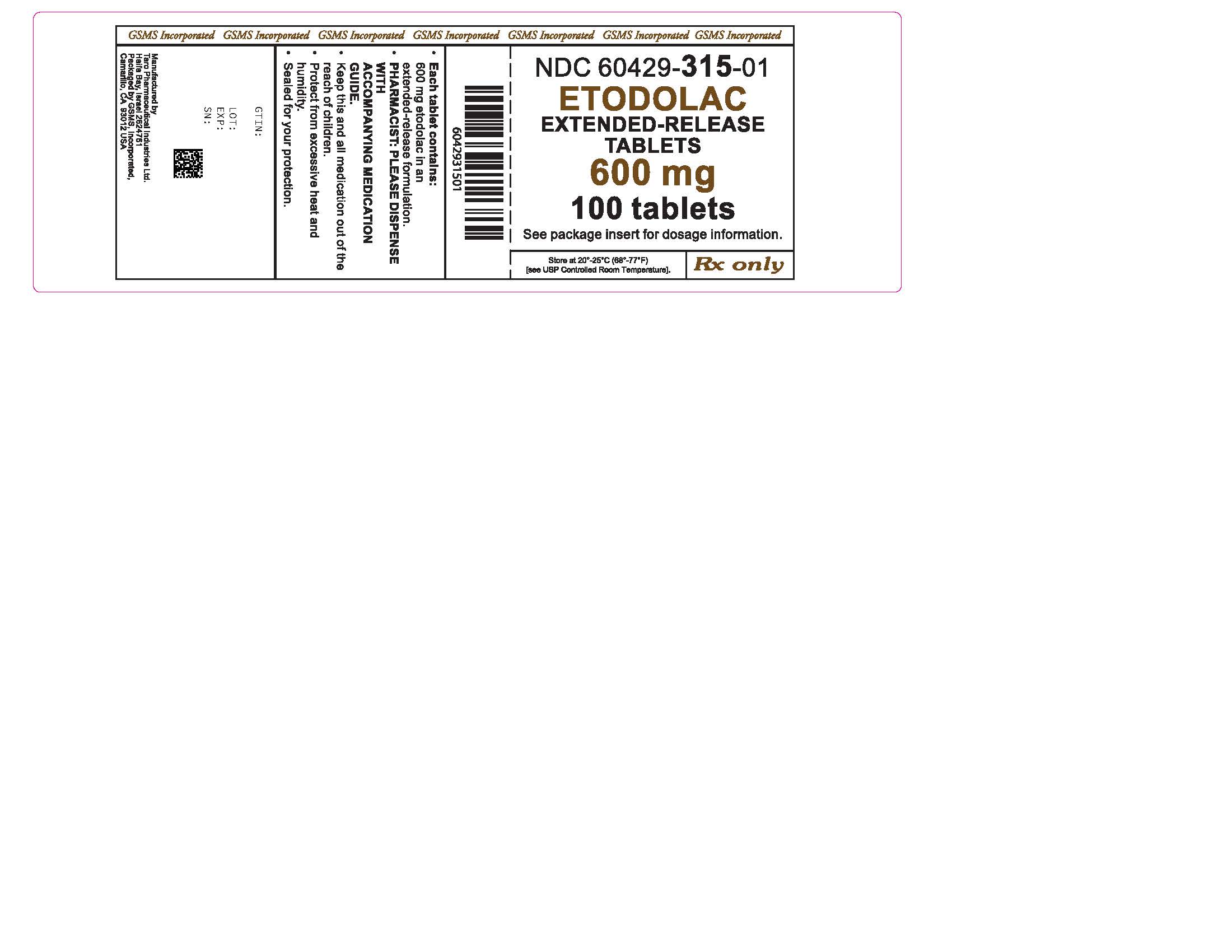
600 mg tablets (grey, oval, bi-convex, film coated tablet engraved with "T600" on one side and plain on the other side).
- in bottles of 100, NDC 60429-315-01
Mfd. by: Taro Pharmaceutical Industries Ltd.
Haifa Bay, Israel 2624761
Dist. by:
Taro Pharmaceuticals U.S.A., Inc.
Hawthorne, NY 10532
Revised: March 2021
Marketed/Packaged by:
GSMS, Inc.
Camarillo, CA USA 93012
| Medication Guide for Nonsteroidal Anti-inflammatory Drugs (NSAIDs) | ||||
|---|---|---|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | ||||
|
What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)? |
||||
| NSAIDs can cause serious side effects, including: | ||||
|
||||
| The risk of getting an ulcer or bleeding increases with: | ||||
|
||||
|
| |||
| NSAIDs should only be used: | ||||
|
||||
| What are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain. |
||||
| Who should not take NSAIDs? | ||||
Do not take NSAIDs:
|
||||
Before taking NSAIDs, tell your healthcare provider about all of your medical conditions, including if you:
|
||||
| Tell your healthcare provider about all of the medicines you take, including prescription or over-the-counter medicines, vitamins or herbal supplements. NSAIDs and some other medicines can interact with each other and cause serious side effects. Do not start taking any new medicine without talking to your healthcare provider first. | ||||
| What are the possible side effects of NSAIDs? | ||||
| NSAIDs can cause serious side effects, including: | ||||
| See " What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?" | ||||
|
||||
| Get emergency help right away if you get any of the following symptoms: | ||||
|
|
|||
| Stop taking your NSAID and call your healthcare provider right away if you get any of the following symptoms: | ||||
|
|
|||
| If you take too much of your NSAID, call your healthcare provider or get medical help right away. | ||||
| These are not all the possible side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs. | ||||
| Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | ||||
Other information about NSAIDs
|
||||
| General information about the safe and effective use of NSAIDs | ||||
| Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them. | ||||
| If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals. | ||||
Mfd. by: Taro Pharmaceutical Industries Ltd., Haifa Bay, Israel 2624761
Dist. by:
Taro Pharmaceuticals U.S.A., Inc., Hawthorne, NY 10532
Revised: March 2021
Marketed/Packaged by:
GSMS, Inc.
Camarillo, CA USA 93012
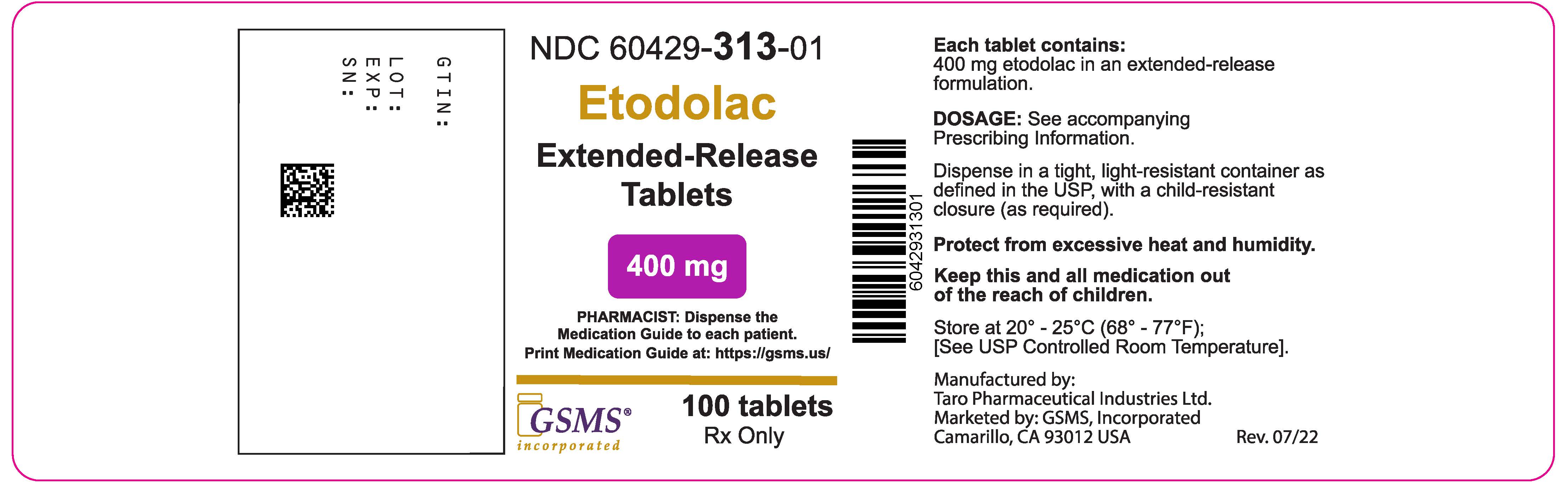
PRINCIPAL DISPLAY PANEL - 400 mg Tablet Bottle Label
NDC 60429-313-01
100 Tablets
Etodolac
Extended-Release
Tablets 400 mg
Pharmacist: Please dispense with
accompanying Medication Guide.
Rx only