DESCRIPTION
Tramadol hydrochloride tablets, USP are a centrally acting analgesic. The chemical name for tramadol hydrochloride is (±)cis-2-[(dimethylamino)methyl]-1-(3methoxyphenyl) cyclohexanol hydrochloride. Its structural formula is:
The molecular formula of tramadol hydrochloride is C16H25NO2•HCl and its molecular weight is 299.8.
Tramadol hydrochloride is a white, bitter, crystalline and odorless powder. It is readily soluble in water and ethanol and has a pKa of 9.41. The n-octanol/water log partition coefficient (logP) is 1.35 at pH 7.
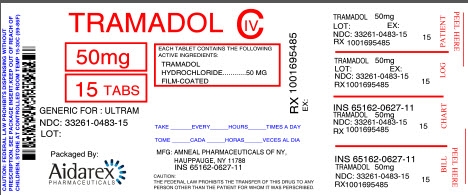
Each tramadol hydrochloride tablet, USP intended for oral administration contains 50 mg of tramadol hydrochloride. In addition, it also contains the following inactive ingredients: hypromellose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polysorbate 80, pregelatinized starch, sodium starch glycolate, and titanium dioxide.
CLINICAL PHARMACOLOGY
PHARMACODYNAMICS
Tramadol Hydrochloride contains tramadol, a centrally acting synthetic opioid analgesic. Although its mode of action is not completely understood, from animal tests, at least two complementary mechanisms appear applicable: binding of parent and M1 metabolite to μ-opioid receptors and weak inhibition of re-uptake of norepinephrine and serotonin.
Opioid activity is due to both low affinity binding of the parent compound and higher affinity binding of the O-demethylated metabolite M1 to μ-opioid receptors. In animal models, M1 is up to 6 times more potent than tramadol in producing analgesia and 200 times more potent in μ-opioid binding. Tramadol-induced analgesia is only partially antagonized by the opiate antagonist naloxone in several animal tests. The relative contribution of both tramadol and M1 to human analgesia is dependent upon the plasma concentrations of each compound (see CLINICAL PHARMACOLOGY, Pharmacokinetics).
Tramadol has been shown to inhibit reuptake of norepinephrine and serotonin in vitro, as have some other opioid analgesics. These mechanisms may contribute independently to the overall analgesic profile of tramadol hydrochloride. Analgesia in humans begins approximately within one hour after administration and reaches a peak in approximately two to three hours.
Apart from analgesia, tramadol hydrochloride administration may produce a constellation of symptoms (including dizziness, somnolence, nausea, constipation, sweating and pruritus) similar to that of other opioids. In contrast to morphine, tramadol has not been shown to cause histamine release. At therapeutic doses, tramadol hydrochloride has no effect on heart rate, left-ventricular function or cardiac index. Orthostatic hypotension has been observed.
PHARMACOKINETICS
The analgesic activity of tramadol hydrochloride is due to both parent drug and the M1 metabolite (see CLINICAL PHARMACOLOGY, Pharmacodynamics). Tramadol is administered as a racemate and both the [-] and [+] forms of both tramadol and M1 are detected in the circulation. Linear pharmacokinetics have been observed following multiple doses of 50 and 100 mg to steady-state.
Absorption
The mean absolute bioavailability of a 100 mg oral dose is approximately 75%. The mean peak plasma concentration of racemic tramadol and M1 occurs at two and three hours, respectively, after administration in healthy adults. In general, both enantiomers of tramadol and M1 follow a parallel time course in the body following single and multiple doses although small differences (∼ 10%) exist in the absolute amount of each enantiomer present.
Steady-state plasma concentrations of both tramadol and M1 are achieved within two days with four times per day dosing. There is no evidence of self-induction (see Figure 1 and Table 1 below).
Figure 1: Mean Tramadol and M1 Plasma Concentration Profiles after a Single 100 mg Oral Dose and after Twenty-Nine 100 mg Oral Doses of Tramadol HCl given four times per day
Table 1 Mean (%CV) Pharmacokinetic Parameters for Racemic Tramadol and M1 Metabolite
| Population/ Dosage Regimena | Parent Drug/ Metabolite | PeakConc. (ng/mL) | Time to Peak (hrs) | Clearence/Fb
(mL/min/Kg) | t1/2 (hrs) |
| Healthy Adults, 100 mg qid, MD p.o. | Tramadol M1 | 592 (30) 110 (29) | 2.3 (61) 2.4 (46) | 5.90 (25) c | 6.7 (15) 7.0 (14) |
| Healthy Adults, 100 mg SD p.o. | Tramadol M1 | 308 (25) 55.0 (36) | 1.6 (63) 3.0 (51) | 8.50 (31) c | 5.6 (20) 6.7 (16) |
| Geriatric, (>75 yrs) 50 mg SD p.o. | Tramadol M1 | 208 (31) d | 2.1 (19) d | 6.89 (25) c | 7.0 (23) d |
| Hepatic Impaired, 50 mg SD p.o. | Tramadol M1 | 217 (11) 19.4 (12) | 1.9 (16) 9.8 (20) | 4.23 (56) c | 13.3 (11) 18.5 (15) |
| Renal Impaired, CLcr10-30 mL/min 100 mg SD i.v | Tramadol M1 | c c | c c | 4.23 (54) c | 10.6 (31) 11.5 (40) |
| Renal Impaired, CLcr<5mL/min 100 mg SD i.v | Tramadol M1 | c c | c c | 3.73 (17) c | 11.0 (29) 16.9 (18) |
a SD = Single dose, MD = Multiple dose, p.o.= Oral administration, i.v.= Intravenous administration, q.i.d. = Four times daily
b F represents the oral bioavailability of tramadol
c Not applicable
d Not measured
Food Effects
Oral administration of tramadol hydrochloride with food does not significantly affect its rate or extent of absorption, therefore, tramadol hydrochloride can be administered without regard to food.
Distribution
The volume of distribution of tramadol was 2.6 and 2.9 liters/kg in male and female subjects, respectively, following a 100 mg intravenous dose. The binding of tramadol to human plasma proteins is approximately 20% and binding also appears to be independent of concentration up to 10 μg/mL. Saturation of plasma protein binding occurs only at concentrations outside the clinically relevant range.
Metabolism
Tramadol is extensively metabolized after oral administration by a number of pathways, including CYP2D6 and CYP3A4, as well as by conjugation of parent and metabolites. Approximately 30% of the dose is excreted in the urine as unchanged drug, whereas 60% of the dose is excreted as metabolites. The remainder is excreted either as unidentified or as unextractable metabolites. The major metabolic pathways appear to be N- and O-demethylation and glucuronidation or sulfation in the liver. One metabolite (O-desmethyltramadol, denoted M1) is pharmacologically active in animal models. Formation of M1 is dependent on CYP2D6 and as such is subject to inhibition, which may affect the therapeutic response (see PRECAUTIONS, Drug Interaction).
Approximately 7% of the population has reduced activity of the CYP2D6 isoenzyme of cytochrome P-450. These individuals are "poor metabolizers" of debrisoquine, dextromethorphan, tricyclic antidepressants, among other drugs. Based on a population PK analysis of Phase I studies in healthy subjects, concentrations of tramadol were approximately 20% higher in "poor metabolizers" versus "extensive metabolizers", while M1 concentrations were 40% lower. Concomitant therapy with inhibitors of CYP2D6 such as fluoxetine, paroxetine and quinidine could result in significant drug interactions. In vitro drug interaction studies in human liver microsomes indicate that inhibitors of CYP2D6 such as fluoxetine and its metabolite norfluoxetine, amitriptyline and quinidine inhibit the metabolism of tramadol to various degrees, suggesting that concomitant administration of these compounds could result in increases in tramadol concentrations and decreased concentrations of M1. The full pharmacological impact of these alterations in terms of either efficacy or safety is unknown. Concomitant use of SEROTONIN re-uptake INHIBITORS and MAO INHIBITORS may enhance the risk of adverse events, including seizure (see WARNINGS) and serotonin syndrome.
Elimination
Tramadol is eliminated primarily through metabolism by the liver and the metabolites are eliminated primarily by the kidneys. The mean terminal plasma elimination half-lives of racemic tramadol and racemic M1 are 6.3 ± 1.4 and 7.4 ± 1.4 hours, respectively. The plasma elimination half-life of racemic tramadol increased from approximately six hours to seven hours upon multiple dosing.
Special Populations
Renal
Impaired renal function results in a decreased rate and extent of excretion of tramadol and its active metabolite, M1. In patients with creatinine clearances of less than 30 mL/min, adjustment of the dosing regimen is recommended (see DOSAGE AND ADMINISTRATION). The total amount of tramadol and M1 removed during a 4-hour dialysis period is less than 7% of the administered dose.
Hepatic
Metabolism of tramadol and M1 is reduced in patients with advanced cirrhosis of the liver, resulting in both a larger area under the concentration time curve for tramadol and longer tramadol and M1 elimination half-lives (13 hrs. for tramadol and 19 hrs. for M1). In cirrhotic patients, adjustment of the dosing regimen is recommended (see DOSAGE AND ADMINISTRATION).
Geriatric
Healthy elderly subjects aged 65 to 75 years have plasma tramadol concentrations and elimination half-lives comparable to those observed in healthy subjects less than 65 years of age. In subjects over 75 years, maximum serum concentrations are elevated (208 vs. 162 ng/mL) and the elimination half-life is prolonged (7 vs. 6 hours) compared to subjects 65 to 75 years of age. Adjustment of the daily dose is recommended for patients older than 75 years (see DOSAGE AND ADMINISTRATION).
Gender
The absolute bioavailability of tramadol was 73% in males and 79% in females. The plasma clearance was 6.4 mL/min/kg in males and 5.7 mL/min/kg in females following a 100 mg IV dose of tramadol. Following a single oral dose, and after adjusting for body weight, females had a 12% higher peak tramadol concentration and a 35% higher area under the concentration-time curve compared to males. The clinical significance of this difference is unknown.
CLINICAL STUDIES
Tramadol hydrochloride has been given in single oral doses of 50, 75 and 100 mg to patients with pain following surgical procedures and pain following oral surgery (extraction of impacted molars).
In single-dose models of pain following oral surgery, pain relief was demonstrated in some patients at doses of 50 mg and 75 mg. A dose of 100 mg tramadol hydrochloride tended to provide analgesia superior to codeine sulfate 60 mg, but it was not as effective as the combination of aspirin 650 mg with codeine phosphate 60 mg.
Tramadol hydrochloride has been studied in three long-term controlled trials involving a total of 820 patients, with 530 patients receiving tramadol hydrochloride. Patients with a variety of chronic painful conditions were studied in double-blind trials of one to three months duration. Average daily doses of approximately 250 mg of tramadol hydrochloride in divided doses were generally comparable to five doses of acetaminophen 300 mg with codeine phosphate 30 mg (TYLENOL® with Codeine #3) daily, five doses of aspirin 325 mg with codeine phosphate 30 mg daily, or two to three doses of acetaminophen 500 mg with oxycodone hydrochloride 5 mg (TYLOX® ) daily.
Titration Trials
In a randomized, blinded clinical study with 129 to 132 patients per group, a 10-day titration to a daily tramadol hydrochloride dose of 200 mg (50 mg four times per day), attained in 50 mg increments every 3 days, was found to result in fewer discontinuations due to dizziness or vertigo than titration over only 4 days or no titration.
INDICATIONS AND USAGE
Tramadol hydrochloride tablets, USP are indicated for the management of moderate to moderately severe pain in adults.
CONTRAINDICATIONS
Tramadol hydrochloride tablets, USP should not be administered to patients who have previously demonstrated hypersensitivity to tramadol, any other component of this product or opioids. Tramadol hydrochloride tablets, USP are contraindicated in any situation where opioids are contraindicated, including acute intoxication with any of the following: alcohol, hypnotics, narcotics, centrally acting analgesics, opioids or psychotropic drugs. Tramadol hydrochloride tablets, USP may worsen central nervous system and respiratory depression in these patients.
WARNINGS
Seizure Risk
Seizures have been reported in patients receiving Tramadol hydrochloride within the recommended dosage range. Spontaneous post-marketing reports indicate that seizure risk is increased with doses of tramadol hydrochloride above the recommended range.
Concomitant use of tramadol hydrochloride increases the seizure risk in patients taking:
- Selective serotonin re-uptake inhibitors (SSRI antidepressants or anorectics),
- Tricyclic antidepressants (TCAs), and other tricyclic compounds (e.g., cyclobenzaprine , promethazine, etc.), or
- Other opioids.
Administration of tramadol hydrochloride may enhance the seizure risk in patients taking:
- MAO inhibitors (see alsoWARNINGS, Use with MAO Inhibitors and Serotonin Re-Uptake Inhibitors),
- Neuroleptics, or
- Other drugs that reduce the seizure threshold.
Risk of convulsions may also increase in patients with epilepsy, those with a history of seizures, or in patients with a recognized risk for seizure (such as head trauma, metabolic disorders, alcohol and drug withdrawal, CNS infections). In tramadol hydrochloride overdose, naloxone administration may increase the risk of seizure.
Suicide Risk
- Do not prescribe tramadol hydrochloride for patients who are suicidal or addiction-prone.
- Prescribe tramadol hydrochloride tablets with caution for patients who are taking tranquilizers or antidepressant drug and patients who use alcohol in excess and who suffer from emotional disturbance or depression.
The judicious prescribing of tramadol is essential to the safe use of this drug. With patients who are depressed or suicidal, consideration should be given to the use of nonnarcotic analgesics.
Tramadol-related deaths have occurred in patients with previous histories of emotional disturbances or suicidal ideation or attempts as well as histories of misuse of tranquilizers, alcohol, and other CNS-active drugs (see WARNINGS, Risk of Overdosage).
Serotonin Syndrome Risk
The development of a potentially life-threatening serotonin syndrome may occur with the use of tramadol products, including tramadol hydrochloride, particularly with concomitant use of serotonergic drugs such as SSRIs, SNRIs, TCAs, MAOIs, and triptans, with drugs which impair metabolism of serotonin (including MAOIs), and with drugs which impair metabolism of tramadol (CYP2D6 and CYP3A4 inhibitors). This may occur within the recommended dose (seeCLINICAL PHARMACOLOGY, Pharmacokinetics).
Serotonin syndrome may include mental-status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination) and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
Anaphylactoid Reactions
Serious and rarely fatal anaphylactoid reactions have been reported in patients receiving therapy with tramadol hydrochloride. When these events do occur it is often following the first dose. Other reported allergic reactions include pruritus, hives, bronchospasm, angioedema, toxic epidermal necrolysis and Stevens-Johnson syndrome. Patients with a history of anaphylactoid reactions to codeine and other opioids may be at increased risk and therefore should not receive tramadol hydrochloride (see CONTRAINDICATIONS).
Respiratory Depression
Administer tramadol hydrochoride cautiously in patients at risk for respiratory depression. In these patients alternative non-opioid analgesics should be considered. When large doses of tramadol hydrochloride are administered with anesthetic medications or alcohol, respiratory depression may result. Respiratory depression should be treated as an overdose. If naloxone is to be administered, use cautiously because it may precipitate seizures (see WARNINGS, Seizure Risk and OVERDOSAGE).
Interaction With Central Nervous System (CNS) Depressants
Tramadol hydrochloride should be used with caution and in reduced dosages when administered to patients receiving CNS depressants such as alcohol, opioids, anesthetic agents, narcotics, phenothiazines, tranquilizers or sedative hypnotics. Tramadol hydrochloride increases the risk of CNS and respiratory depression in these patients.
Interactions with Alcohol and Drugs of Abuse
Tramadol may be expected to have additive effects when used in conjunction with alcohol, other opioids, or illicit drugs that cause central nervous system depression.
Increased Intracranial Pressure or Head Trauma
Tramadol hydrochloride should be used with caution in patients with increased intracranial pressure or head injury. The respiratory depressant effects of opioids include carbon dioxide retention and secondary elevation of cerebrospinal fluid pressure, and may be markedly exaggerated in these patients. Additionally, pupillary changes (miosis) from tramadol may obscure the existence, extent, or course of intracranial pathology. Clinicians should also maintain a high index of suspicion for adverse drug reaction when evaluating altered mental status in these patients if they are receiving tramadol hydrochloride (see WARNINGS, Respiratory Depression).
Use in Ambulatory Patients
Tramadol hydrochloride may impair the mental and or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery. The patient using this drug should be cautioned accordingly.
Use With MAO Inhibitors and Serotonin Re-uptake Inhibitors
Use tramadol hydrochloride with great caution in patients taking monoamine oxidase inhibitors. Animal studies have shown increased deaths with combined administration. Concomitant use of tramadol hydrochloride with MAO inhibitors or SSRI’s increases the risk of adverse events, including seizure and serotonin syndrome.
Misuse, Abuse and Diversion
Tramadol has mu-opioid agonist activity. Tramadol hydrochloride® can be sought by drug abusers and people with addiction disorders and may be subject to criminal diversion. The possibility of illegal or illicit use should be considered when prescribing or dispensing tramadol hydrochloride® in situations where the physician or pharmacist is concerned about an increased risk of misuse, abuse, or diversion. Misuse or abuse poses a significant risk to the abuser that could result in overdose and death (see DRUG ABUSE AND DEPENDENCE and OVERDOSAGE).
Concerns about abuse, addiction, and diversion should not prevent the proper management of pain. The development of addiction to opioid analgesics in properly managed patients with pain has been reported to be rare. However, data are not available to establish the true incidence of addiction in chronic pain patients.
Risk of Overdosage
Patients taking tramadol should be warned not to exceed the dose recommended by their physician. Tramadol products in excessive doses, either alone or in combination with other CNS depressants, including alcohol, are a cause of drug-related deaths. Patients should be cautioned about the concomitant use of tramadol products and alcohol because of potentially serious CNS additive effects of these agents. Because of its added depressant effects, tramadol should be prescribed with caution for those patients whose medical condition requires the concomitant administration of sedatives, tranquilizers, muscle relaxants, antidepressants, or other CNS depressant drugs. Patients should be advised of the additive depressant effects of these combinations.
Serious potential consequences of overdosage with tramadol hydrochloride (tramadol hydrochloride) tablets are central nervous system depression, respiratory depression and death. Some deaths have occurred as a consequence of the accidental ingestion of excessive quantities of tramadol alone or in combination with other drugs. In treating an overdose, primary attention should be given to maintaining adequate ventilation along with general supportive treatment (see OVERDOSAGE).
Withdrawal
Withdrawal symptoms may occur if tramadol hydrochloride is discontinued abruptly (see also DRUG ABUSE AND DEPENDENCE). Reported symptoms have included anxiety, sweating, insomnia, rigors, pain, nausea, tremors, diarrhea, upper respiratory symptoms, piloerection, and rarely hallucinations. Other symptoms that have been reported less frequently with tramadol hydrchloride discontinuation include panic attacks, severe anxiety, and paresthesias. Clinical experience suggests that withdrawal symptoms may be avoided by tapering tramadol hydrochloride at the time of discontinuation.
PRECAUTIONS
Acute Abdominal Conditions
The administration of tramadol hydrochloride may complicate the clinical assessment of patients with acute abdominal conditions.
Use in Renal and Hepatic Disease
Impaired renal function results in a decreased rate and extent of excretion of tramadol and its active metabolite, M1. In patients with creatinine clearances of less than 30 mL/min, dosing reduction is recommended (see DOSAGE AND ADMINISTRATION). Metabolism of tramadol and M1 is reduced in patients with advanced cirrhosis of the liver. In cirrhotic patients, dosing reduction is recommended (see DOSAGE AND ADMINISTRATION).
With the prolonged half-life in these conditions, achievement of steady-state is delayed, so that it may take several days for elevated plasma concentrations to develop.
Information for Patients
- Patients should be informed that tramadol hydrochloride may cause seizures and/or serotonin syndrome with concomitant use of serotonergic agents (including SSRIs, SNRIs, and triptans) or drugs that significantly reduce the metabolic clearance of tramadol.
- Tramadol hydrochloride may impair mental or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery.
- Tramadol hydrochloride should not be taken with alcohol containing beverages.
- Tramadol hydrochloride should be used with caution when taking medications such as tranquilizers, hypnotics or other opiate containing analgesics.
- The patient should be instructed to inform the physician if they are pregnant, think they might become pregnant, or are trying to become pregnant (see PRECAUTIONS, Labor and Delivery).
- The patient should understand the single-dose and 24-hour dose limit and the time interval between doses, since exceeding these recommendations can result in respiratory depression, seizures and death.
Drug Interactions
CYP2D6 and CYP3A4 Inhibitors
Concomitant administration of CYP2D6 and/or CYP3A4 inhibitors (see CLINICAL PHARMACOLOGY, Pharmacokinetics), such as quinidine, fluoxetine, paroxetine and amitriptyline (CYP2D6 inhibitors), and ketoconazole and erythromycin (CYP3A4 inhibitors), may reduce metabolic clearance of tramadol increasing the risk for serious adverse events including seizures and serotonin syndrome.
Serotonergic Drugs
There have been postmarketing reports of serotonin syndrome with use of tramadol and SSRIs/SNRIs or MAOIs and α2-adrenergic blockers. Caution is advised when tramadol hydrochloride is coadministered with other drugs that may affect the serotonergic neurotransmitter systems, such as SSRIs, MAOIs, triptans, linezolid (an antibiotic which is a reversible non-selective MAOI), lithium, or St. John’s Wort. If concomitant treatment of tramadol hydrochloride with a drug affecting the serotonergic neurotransmitter system is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases (see WARNINGS, Serotonin Syndrome).
Triptans
Based on the mechanism of action of tramadol and the potential for serotonin syndrome, caution is advised when tramadol hydrochloride is coadministered with a triptan. If concomitant treatment of tramadol hydrochloride with a triptan is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases (see WARNINGS, Serotonin Syndrome).
Use With Carbamazepine
Patients taking carbamazepine may have a significantly reduced analgesic effect of tramadol hydrochloride. Because carbamazepine increases tramadol metabolism and because of the seizure risk associated with tramadol, concomitant administration of tramadol hydrochloride and carbamazepine is not recommended.
Use With Quinidine
Tramadol is metabolized to M1 by CYP2D6. Quinidine is a selective inhibitor of that isoenzyme, so that concomitant administration of quinidine and tramadol hydrochloride results in increased concentrations of tramadol and reduced concentrations of M1. The clinical consequences of these findings are unknown. In vitro drug interaction studies in human liver microsomes indicate that tramadol has no effect on quinidine metabolism.
Potential for Other Drugs to Affect Tramadol
In vitro drug interaction studies in human liver microsomes indicate that concomitant administration with inhibitors of CYP2D6 such as fluoxetine, paroxetine, and amitriptyline could result in some inhibition of the metabolism of tramadol. Administration of CYP3A4 inhibitors, such as ketoconazole and erythromycin, or inducers, such as rifampin and St. John’s Wort, with tramadol hydrochloride may affect the metabolism of tramadol leading to altered tramadol exposure.
Potential for Tramadol to Affect Other Drugs
In vitro studies indicate that tramadol is unlikely to inhibit the CYP3A4-mediated metabolism of other drugs when tramadol is administered concomitantly at therapeutic doses. Tramadol does not appear to induce its own metabolism in humans, since observed maximal plasma concentrations after multiple oral doses are higher than expected based on single-dose data. Tramadol is a mild inducer of selected drug metabolism pathways measured in animals.
Use With Cimetidine
Concomitant administration of tramadol hydrochloride with cimetidine does not result in clinically significant changes in tramadol pharmacokinetics. Therefore, no alteration of the tramadol hydrochloride dosage regimen is recommended.
Use With Digoxin and Warfarin
Post-marketing surveillance has revealed rare reports of digoxin toxicity and alteration of warfarin effect, including elevation of prothrombin times.
Carcinogenesis, Mutagenesis, Impairment of Fertility
A slight, but statistically significant, increase in two common murine tumors, pulmonary and hepatic, was observed in a mouse carcinogenicity study, particularly in aged mice. Mice were dosed orally up to 30 mg/kg (90 mg/m2 or 0.36 times the maximum daily human dosage of 246 mg/m2) for approximately two years, although the study was not done with the Maximum Tolerated Dose. This finding is not believed to suggest risk in humans. No such finding occurred in a rat carcinogenicity study (dosing orally up to 30 mg/kg, 180 mg/m2, or 0.73 times the maximum daily human dosage).
Tramadol was not mutagenic in the following assays: Ames Salmonella microsomal activation test, CHO/HPRT mammalian cell assay, mouse lymphoma assay (in the absence of metabolic activation), dominant lethal mutation tests in mice, chromosome aberration test in Chinese hamsters, and bone marrow micronucleus tests in mice and Chinese hamsters. Weakly mutagenic results occurred in the presence of metabolic activation in the mouse lymphoma assay and micronucleus test in rats. Overall, the weight of evidence from these tests indicates that tramadol does not pose a genotoxic risk to humans.
No effects on fertility were observed for tramadol at oral dose levels up to 50 mg/kg (300 mg/m2) in male rats and 75 mg/kg (450 mg/m2) in female rats. These dosages are 1.2 and 1.8 times the maximum daily human dosage of 246 mg/m2, respectively.
Pregnancy, Teratogenic Effects: Pregnancy Category C
Tramadol has been shown to be embryotoxic and fetotoxic in mice, (120 mg/kg or 360 mg/m2), rats (≥25 mg/kg or 150 mg/m2) and rabbits (≥75 mg/kg or 900 mg/m2) at maternally toxic dosages, but was not teratogenic at these dose levels. These dosages on a mg/m2 basis are 1.4, ≥0.6, and ≥3.6 times the maximum daily human dosage (246 mg/m2) for mouse, rat and rabbit, respectively.
No drug-related teratogenic effects were observed in progeny of mice (up to 140 mg/kg or 420 mg/m2), rats (up to 80 mg/kg or 480 mg/m2) or rabbits (up to 300 mg/kg or 3600 mg/m2) treated with tramadol by various routes. Embryo and fetal toxicity consisted primarily of decreased fetal weights, skeletal ossification and increased supernumerary ribs at maternally toxic dose levels. Transient delays in developmental or behavioral parameters were also seen in pups from rat dams allowed to deliver. Embryo and fetal lethality were reported only in one rabbit study at 300 mg/kg (3600 mg/m2), a dose that would cause extreme maternal toxicity in the rabbit. The dosages listed for mouse, rat and rabbit are 1.7, 1.9 and 14.6 times the maximum daily human dosage (246 mg/m2), respectively.
Non-teratogenic Effects
Tramadol was evaluated in peri- and post-natal studies in rats. Progeny of dams receiving oral (gavage) dose levels of 50 mg/kg (300 mg/m2 or 1.2 times the maximum daily human tramadol dosage) or greater had decreased weights, and pup survival was decreased early in lactation at 80 mg/kg (480 mg/m2 or 1.9 and higher the maximum daily human dose).
There are no adequate and well-controlled studies in pregnant women. Tramadol hydrochloride should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Neonatal seizures, neonatal withdrawal syndrome, fetal death and still birth have been reported during post-marketing.
Labor and Delivery
Tramadol hydrochloride should not be used in pregnant women prior to or during labor unless the potential benefits outweigh the risks. Safe use in pregnancy has not been established. Chronic use during pregnancy may lead to physical dependence and post-partum withdrawal symptoms in the newborn (see DRUG ABUSE AND DEPENDENCE). Tramadol has been shown to cross the placenta. The mean ratio of serum tramadol in the umbilical veins compared to maternal veins was 0.83 for 40 women given tramadol during labor.
The effect of tramadol hydrochloride, if any, on the later growth, development, and functional maturation of the child is unknown.
Nursing Mothers
Tramadol hydrochloride is not recommended for obstetrical preoperative medication or for post-delivery analgesia in nursing mothers because its safety in infants and newborns has not been studied. Following a single IV 100 mg dose of tramadol, the cumulative excretion in breast milk within 16 hours postdose was 100 μg of tramadol (0.1% of the maternal dose) and 27 μg of M1.
Pediatric Use
The safety and efficacy of tramadol hydrochloride in patients under 16 years of age have not been established. The use of tramadol hydrochloride in the pediatric population is not recommended.
Geriatric Use
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function and of concomitant disease or other drug therapy. In patients over 75 years of age, daily doses in excess of 300 mg are not recommended (see CLINICAL PHARMACOLOGY and DOSAGE AND ADMINISTRATION).
A total of 455 elderly (65 years of age or older) subjects were exposed to tramadol hydrochloride in controlled clinical trials. Of those, 145 subjects were 75 years of age and older.
In studies including geriatric patients, treatment-limiting adverse events were higher in subjects over 75 years of age compared to those under 65 years of age. Specifically, 30% of those over 75 years of age had gastrointestinal treatment-limiting adverse events compared to 17% of those under 65 years of age. Constipation resulted in discontinuation of treatment in 10% of those over 75.
ADVERSE REACTIONS
Tramadol hydrochloride was administered to 550 patients during the double-blind or open-label extension periods in U.S. studies of chronic nonmalignant pain. Of these patients, 375 were 65 years old or older. Table 2 reports the cumulative incidence rate of adverse reactions by 7, 30 and 90 days for the most frequent reactions (5% or more by 7 days). The most frequently reported events were in the central nervous system and gastrointestinal system. Although the reactions listed in the table are felt to be probably related to tramadol hydrochloride administration, the reported rates also include some events that may have been due to underlying disease or concomitant medication. The overall incidence rates of adverse experiences in these trials were similar for tramadol hydrochloride and the active control groups, TYLENOL® with Codeine #3 (acetaminophen 300 mg with codeine phosphate 30 mg), and aspirin 325 mg with codeine phosphate 30 mg, however, the rates of withdrawals due to adverse events appeared to be higher in the tramadol hydrochloride groups.
Table 2: Cumulative Incidence of Adverse Reactions for Tramadol Hydrochloride in Chronic Trials of Nonmalignant Pain (N=427)
| Up to 7 Days | Up to 30 Days | Up to 90 Days | |
| Dizziness/Vertigo | 26% | 31% | 33% |
| Nausea | 24% | 34% | 40% |
| Constipation | 24% | 38% | 46% |
| Headache | 18% | 26% | 32% |
| Somnolence | 16% | 23% | 25% |
| Vomiting | 9% | 13% | 17% |
| Pruritus | 8% | 10% | 11% |
| ‘CNS Stimulation’1 | 7% | 11% | 14% |
| Asthenia | 6% | 11% | 12% |
| Sweating | 6% | 7% | 9% |
| Dyspepsia | 5% | 9% | 13% |
| Dry Mouth | 5% | 9% | 10% |
| Diarrhea | 5% | 9% | 10% |
| 1 “CNS Stimulation” is a composite of nervousness, anxiety, agitation, tremor, spasticity, euphoria, emotional lability and hallucinations | |||
Incidence 1% to less than 5% possibly causally related: the following lists adverse reactions that occurred with an incidence of 1% to less than 5% in clinical trials, and for which the possibility of a causal relationship with tramadol hydrochloride exists.
Body as a Whole: Malaise.
Cardiovascular: Vasodilation.
Central Nervous System: Anxiety, Confusion, Coordination disturbance, Euphoria,
Miosis, Nervousness, Sleep disorder.
Gastrointestinal: Abdominal pain, Anorexia, Flatulence.
Musculoskeletal: Hypertonia.
Skin: Rash.
Special Senses: Visual disturbance.
Urogenital: Menopausal symptoms, Urinary frequency, Urinary retention.
Incidence less than 1%, possibly causally related: the following lists adverse reactions that occurred with an incidence of less than 1% in clinical trials and/or reported in post-marketing experience.
Body as a Whole: Accidental injury, Allergic reaction, Anaphylaxis, Death, Suicidal tendency, Weight loss, Serotonin syndrome (mental status change, hyperreflexia, fever, shivering, tremor, agitation, diaphoresis, seizures and coma).
Cardiovascular: Orthostatic hypotension, Syncope, Tachycardia.
Central Nervous System: Abnormal gait, Amnesia, Cognitive dysfunction, Depression, Difficulty in concentration, Hallucinations, Paresthesia, Seizure (see WARNINGS). Tremor.
Respiratory: Dyspnea.
Skin: Stevens-Johnson syndrome/Toxic epidermal necrolysis, Urticaria, Vesicles.
Special Senses: Dysgeusia.
Urogenital: Dysuria, Menstrual disorder.
Other adverse experiences, causal relationship unknown: A variety of other adverse events were reported infrequently in patients taking tramadol hydrochloride during clinical trials and/or reported in post-marketing experience. A causal relationship between tramadol hydrochloride and these events has not been determined. However, the most significant events are listed below as alerting information to the physician.
Cardiovascular: Abnormal ECG, Hypertension, Hypotension, Myocardial ischemia, Palpitations, Pulmonary edema, Pulmonary embolism.
Central Nervous System: Migraine, Speech disorders.
Gastrointestinal: Gastrointestinal bleeding, Hepatitis, Stomatitis, Liver failure.
Laboratory Abnormalities: Creatinine increase, Elevated liver enzymes, Hemoglobin decrease, Proteinuria.
Sensory: Cataracts, Deafness, Tinnitus.
DRUG ABUSE AND DEPENDENCE
Abuse
Tramadol has mu-opioid agonist activity. Tramadol hydrochloride tablets can be abused and may be subject to criminal diversion.
Addiction is a primary, chronic, neurobiologic disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. Drug addiction is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, use for non-medical purposes, and continued use despite harm or risk of harm, and craving. Drug addiction is a treatable disease, utilizing a multidisciplinary approach, but relapse is common.
“Drug-seeking” behavior is very common in addicts and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated “loss” of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). “Doctor shopping” to obtain additional prescriptions is common among drug abusers and people suffering from untreated addiction.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all addicts. In addition, abuse of tramadol hydrochloride can occur in the absence of true addiction and is characterized by misuse for non-medical purposes, often in combination with other psychoactive substances.
Concerns about abuse and addiction should not prevent the proper management of pain. However all patients treated with opioids require careful monitoring for signs of abuse and addiction, because use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Proper assessment of the patient and periodic re-evaluation of therapy are appropriate measures that help to limit the potential abuse of this product.
Tramadol hydrochloride tablets is intended for oral use only.
Dependence
Tolerance is the need for increasing doses of drugs to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Physical dependence is manifested by withdrawal symptoms after abrupt discontinuation of a drug or upon administration of an antagonist (see also WARNINGS, Withdrawal).
The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
Generally, tolerance and/or withdrawal are more likely to occur the longer a patient is on continuous therapy with tramadol hydrochloride tablets.
OVERDOSAGE
Acute overdosage with tramadol can be manifested by respiratory depression, somnolence progressing to stupor or coma, skeletal muscle flaccidity, cold and clammy skin, constricted pupils, seizures, bradycardia, hypotension, cardiac arrest, and death. Deaths due to overdose have been reported with abuse and misuse of tramadol (see WARNINGS, Misuse, Abuse, and Diversion). Review of case reports has indicated that the risk of fatal overdose is further increased when tramadol is abused concurrently with alcohol or other CNS depressants, including other opioids.
In the treatment of tramadol overdosage, primary attention should be given to the reestablishment of a patent airway and institution of assisted or controlled ventilation. Supportive measures (including oxygen and vasopressors) should be employed in the management of circulatory shock and pulmonary edema accompanying overdose as indicated. Cardiac arrest or arrhythmias may require cardiac massage or defibrillation.
While naloxone will reverse some, but not all, symptoms caused by overdosage with tramadol, the risk of seizures is also increased with naloxone administration. In animals convulsions following the administration of toxic doses of tramadol hydrochloride tablets could be suppressed with barbiturates or benzodiazepines but were increased with naloxone. Naloxone administration did not change the lethality of an overdose in mice. Hemodialysis is not expected to be helpful in an overdose because it removes less than 7% of the administered dose in a 4-hour dialysis period.
DOSAGE AND ADMINISTRATION
Adults (17 years of age and over)
For patients with moderate to moderately severe chronic pain not requiring rapid onset of analgesic effect, the tolerability of tramadol hydrochloride tablets, USP can be improved by initiating therapy with a titration regimen: The total daily dose may be increased by 50 mg as tolerated every 3 days to reach 200 mg/day (50 mg q.i.d.). After titration, tramadol hydrochloride tablets, USP 50 to 100 mg can be administered as needed for pain relief every 4 to 6 hours not to exceed 400 mg/day.
For the subset of patients for whom rapid onset of analgesic effect is required and for whom the benefits outweigh the risk of discontinuation due to adverse events associated with higher initial doses, tramadol hydrochloride tablets, USP 50 mg to 100 mg can be administered as needed for pain relief every four to six hours, not to exceed 400 mg per day.
Individualization of Dose
Good pain management practice dictates that the dose be individualized according to patient need using the lowest beneficial dose. Studies with tramadol in adults have shown that starting at the lowest possible dose and titrating upward will result in fewer discontinuations and increased tolerability.
- In all patients with creatinine clearance less than 30 mL/min, it is recommended that the dosing interval of tramadol hydrochloride tablets be increased to 12 hours, with a maximum daily dose of 200 mg. Since only 7% of an administered dose is removed by hemodialysis, dialysis patients can receive their regular dose on the day of dialysis.
- The recommended dose for adult patients with cirrhosis is 50 mg every 12 hours.
- In general, dose selection for an elderly patient over 65 years old should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function and of concomitant disease or other drug therapy. For elderly patients over 75 years old, total dose should not exceed 300 mg/day.
HOW SUPPLIED
Tramadol hydrochloride tablets, USP 50 mg are supplied as unscored, white, round film coated tablets debossed “AN” over “627”.
They are supplied as follows:
| 9 TABLET in a BOTTLE (33261-105-09) |
| 10 TABLET in a BOTTLE (33261-105-10) |
| 15 TABLET in a BOTTLE (33261-105-15) |
| 16 TABLET in a BOTTLE (33261-105-16) |
| 20 TABLET in a BOTTLE (33261-105-20) |
| 30 TABLET in a BOTTLE (33261-105-30) |
| 40 TABLET in a BOTTLE (33261-105-40) |
| 45 TABLET in a BOTTLE (33261-105-45) |
| 50 TABLET in a BOTTLE (33261-105-50) |
| 60 TABLET in a BOTTLE (33261-105-60) |
| 90 TABLET in a BOTTLE (33261-105-90) |
| 100 TABLET in a BOTTLE (33261-105-00) |
| 120 TABLET in a BOTTLE (33261-105-02) |
| 168 TABLET in a BOTTLE (33261-105-98) |
| 180 TABLET in a BOTTLE (33261-105-99) |
| 200 TABLET in a BOTTLE (33261-105-91) |
| 240 TABLET in a BOTTLE (33261-105-04) |
| 120 TABLET in a BOTTLE (33261-105-02) |
| 168 TABLET in a BOTTLE (33261-105-98) |
| 180 TABLET in a BOTTLE (33261-105-99) |
| 200 TABLET in a BOTTLE (33261-105-91) |
| 240 TABLET in a BOTTLE (33261-105-04) |
Dispense in a tight container as defined in the USP.
Store at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F).