FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
Budesonide extended-release tablets are indicated for the induction of remission in patients with active, mild to moderate ulcerative colitis.
2 DOSAGE AND ADMINISTRATION
2.1 Mild to Moderate Ulcerative Colitis
The recommended dosage for the induction of remission in adult patients with active, mild to moderate ulcerative colitis is 9 mg taken orally once daily in the morning with or without food for up to 8 weeks. Budesonide extended-release tablets should be swallowed whole and not chewed, crushed or broken.
2.2 CYP3A4 Inhibitors
If concomitant administration with ketoconazole, or any other CYP3A4 inhibitor, is indicated, patients should be closely monitored for increased signs and/or symptoms of hypercorticism. Avoid grapefruit juice, which is known to inhibit CYP3A4, when taking budesonide extended-release tablets. In these cases, discontinuation of budesonide extended- release tablets or the CYP3A4 inhibitor should be considered [seeDrug Interactions (7)and Clinical Pharmacology (12.3)].
3 DOSAGE FORMS AND STRENGTHS
White, round, biconvex extended-release tablets debossed with “MX9”. Each extended-release tablet contains 9 mg budesonide.
4 CONTRAINDICATIONS
Budesonide extended-release tablets are contraindicated in patients with hypersensitivity to budesonide or any of the ingredients of budesonide extended-release tablets. Anaphylactic reactions have occurred with other budesonide formulations [see Adverse Reactions (6.2)].
5 WARNINGS AND PRECAUTIONS
5.1 Hypercorticism and Adrenal Axis Suppression
When glucocorticosteroids are used chronically, systemic effects such as hypercorticism and adrenal suppression may occur. Glucocorticosteroids can reduce the response of the hypothalamus-pituitary-adrenal (HPA) axis to stress. In situations where patients are subject to surgery or other stress situations, supplementation with a systemic glucocorticosteroid is recommended. Since budesonide extended-release tablets are a glucocorticosteroid, general warnings concerning glucocorticoids should be followed.
5.2 Transferring Patients from Systemic Glucocorticosteroid Therapy
Care is needed in patients who are transferred from glucocorticosteroid treatment with higher systemic effects to glucocorticosteroids with lower systemic effects, such as budesonide extended-release tablets, since symptoms attributed to withdrawal of steroid therapy, including those of acute adrenal suppression or benign intracranial hypertension, may develop. Adrenocortical function monitoring may be required in these patients, and the dose of glucocorticosteroid treatment with high systemic effects should be reduced cautiously.
5.3 Immunosuppression
Patients who are on drugs that suppress the immune system are more susceptible to infection than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in susceptible patients or patients on immunosuppressant doses of glucocorticosteroids. In patients who have not had these diseases, particular care should be taken to avoid exposure.
How the dose, route, and duration of glucocorticosteroid administration affect the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior glucocorticosteroid treatment to the risk is also not known. If exposed, therapy with varicella zoster immune globulin (VZIG) or pooled intravenous immunoglobulin (IVIG), as appropriate, may be indicated. If exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated. (See prescribing information for VZIG and IG.) If chickenpox develops, treatment with antiviral agents may be considered.
Glucocorticosteroids should be used with caution, if at all, in patients with active or quiescent tuberculosis infection, untreated fungal, bacterial, systemic viral or parasitic infections.
Replacement of systemic glucocorticosteroids with budesonide extended-release tablets may unmask allergies (e.g., rhinitis and eczema), which were previously controlled by the systemic drug.
5.4 Increased Systemic Glucocorticoid Susceptibility
Reduced liver function affects the elimination of glucocorticosteroids, and increased systemic availability of oral budesonide has been demonstrated in patients with liver cirrhosis [seeUse in Specific Populations (8.6).
6 ADVERSE REACTIONS
Systemic glucocorticosteroid use may result in the following:
- •
- Hypercorticism and Adrenal Suppression [see Warnings and Precautions (5.1)]
- •
- Symptoms of steroid withdrawal in those patients transferring from Systemic Glucocorticosteroid Therapy [see Warnings and Precautions (5.2)]
- •
- Immunosuppression [see Warnings and Precautions (5.3)]
- •
- Increased Systemic Glucocorticoid Susceptibility [see Warnings and Precautions (5.4)]
- •
- Other Glucocorticosteroid Effects [see Warnings and Precautions (5.5)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of budesonide extended-release tablets have been evaluated in controlled and open-label clinical trials which enrolled a combined total of 1,105 patients with ulcerative colitis.
In two 8-week, placebo-controlled studies in patients with active disease (Study 1 and Study 2), a total of 255 patients received budesonide extended-release tablets 9 mg, 254 patients received budesonide extended-release tablets 6 mg, and 258 patients received placebo. They ranged in age from 18-77 years (mean=43), 56% were male, and 75% were Caucasian. The most common adverse reactions were headache, nausea, decreased blood cortisol, upper abdominal pain, fatigue, flatulence, abdominal distension, acne, urinary tract infection, arthralgia, and constipation. The adverse reactions occurring in 2% or more of patients on therapy with budesonide extended-release tablets 9 mg are summarized in Table 1.
Table 1. Summary of Adverse Reactions in Two Placebo-Controlled Trials Experienced by at Least 2% of the Budesonide Extended-Release Tablets 9 mg Group (Studies 1 and 2)
|
Budesonide extended- release tablets 9 mg
|
Budesonide extended- release tablets 6 mg
|
Placebo
|
|
|
Headache |
29 (11.4) |
37 (14.6) |
27 (10.5) |
|
Nausea |
13 (5.1) |
12 (4.7) |
11 (4.3) |
|
Decreased blood cortisol |
11 (4.3) |
6 (2.4) |
1 (0.4) |
|
Upper abdominal pain |
10 (3.9) |
8 (3.1) |
5 (1.9) |
|
Fatigue |
8 (3.1) |
5 (2.0) |
5 (1.9) |
|
Flatulence |
6 (2.4) |
8 (3.1) |
5 (1.9) |
|
Abdominal distension |
6 (2.4) |
4 (1.6) |
2 (0.8) |
|
Acne |
6 (2.4) |
2 (0.8) |
5 (1.9) |
|
Urinary tract infection |
5 (2.0) |
1 (0.4) |
1 (0.4) |
|
Arthralgia |
5 (2.0) |
5 (2.0) |
4 (1.6) |
|
Constipation |
5 (2.0) |
1 (0.4) |
2 (0.8) |
Of budesonide extended-release tablets 9 mg patients, a total of 15% discontinued treatment due to any adverse event (including adverse reactions) compared with 17% in the placebo group.
Table 2 summarizes the percentages of patients reporting glucocorticoid-related effects in the 2 placebo-controlled studies.
Table 2. Summary of Glucocorticoid-Related Effects in Two Placebo-Controlled Trials (Studies 1 and 2)
|
Budesonide extended- release tablets 9 mg
|
Budesonide extended- release tablets 6 mg
|
Placebo
|
|
|
Overall |
26 (10.2) |
19 (7.5) |
27 (10.5) |
|
Mood changes |
9 (3.5) |
10 (3.9) |
11 (4.3) |
|
Sleep changes |
7 (2.7) |
10 (3.9) |
12 (4.7) |
|
Insomnia |
6 (2.4) |
6 (2.4) |
8 (3.1) |
|
Acne |
6 (2.4) |
2 (0.8) |
5 (1.9) |
|
Moon face |
3 (1.2) |
3 (1.2) |
4 (1.6) |
|
Fluid retention |
2 (0.8) |
3 (1.2) |
3 (1.2) |
|
Hirsutism |
1 (0.4) |
0 |
0 |
|
Striae rubrae |
0 |
0 |
2 (0.8) |
|
Flushing |
0 |
1 (0.4) |
3 (1.2) |
No clinically significant differences were observed with respect to the overall percentages of patients with any glucocorticoid-related effects between budesonide extended-release tablets and placebo after 8 weeks of induction therapy.
Study 3 was an open-label study evaluating budesonide extended-release tablets 9 mg once daily for 8 weeks in 60 patients who had previously completed an 8-week induction study (Study 1) but had not achieved remission. Among patients who took budesonide extended-release tablets 9 mg up to 16 weeks cumulatively across Study 1 and Study 3 combined, similar rates of adverse reactions and glucocorticoid-related effects were seen compared to those who took budesonide extended-release tablets 9 mg for 8 weeks in Study 1.
In Study 4, the safety of long-term treatment with budesonide extended-release tablets 6 mg was evaluated in a placebo-controlled 12-month maintenance study of 123 patients. Patients who had previously completed 8 weeks of therapy in any induction study (Study 1, 2, or 3) and were in remission were randomized to budesonide extended-release tablets 6 mg or placebo once daily for 12 months. In patients who took budesonide extended-release tablets 6 mg for up to 12 months, similar rates of adverse reactions were seen between placebo and budesonide extended-release tablets 6 mg. After up to 12 months of study treatment, 77% (27/35) of the patients in the budesonide extended-release tablets 6 mg and 74% (29/39) of the patients in the placebo treatment groups had normal bone density scans.
In Study 4, the glucocorticoid-related effects were similar in patients with up to 12 months of therapy with budesonide extended-release tablets 6 mg and placebo (Table 3).
Table 3. Summary of Glucocorticoid-Related Effects Over 12-Month Treatment (Study 4)
|
Budesonide extended- release tablets 6 mg
|
Placebo
|
|
|
Overall |
9 (14.5) |
7 (11.5) |
|
Insomnia |
4 (6.5) |
4 (6.6) |
|
Mood changes |
4 (6.5) |
2 (3.3) |
|
Moon face |
3 (4.8) |
3 (4.9) |
|
Sleep changes |
3 (4.8) |
3 (4.9) |
|
Acne |
3 (4.8) |
0 |
|
Hirsutism |
3 (4.8) |
0 |
|
Flushing |
1 (1.6) |
1 (1.6) |
|
Fluid retention |
1 (1.6) |
1 (1.6) |
6.2 Postmarketing Experience
In addition to adverse events reported from clinical trials, the following adverse reactions have been identified during post-approval use of oral budesonide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These events have been chosen for inclusion due to either their seriousness, frequency of reporting or causal connection to budesonide extended-release tablets, or a combination of these factors.
Gastrointestinal Disorders: diarrhea, rectal bleeding
General Disorders and Administrative Site Conditions: peripheral edema
Immune System Disorders: anaphylactic reactions
Musculoskeletal and Connective Tissue Disorders: muscle cramps/spasms
Nervous System Disorders: benign intracranial hypertension, dizziness
Psychiatric Disorders: mood swings
Skin and Subcutaneous Tissue Disorders: rash
Vascular Disorders: increased blood pressure
7 DRUG INTERACTIONS
7.1 Interaction with CYP3A4 Inhibitors
Concomitant oral administration of ketoconazole (a known inhibitor of CYP3A4 activity in the liver and in the intestinal mucosa) caused an eight-fold increase of the systemic exposure to oral budesonide. If treatment with inhibitors of CYP3A4 activity (such as ketoconazole, itraconazole, ritonavir, indinavir, saquinavir, erythromycin) is indicated, discontinuation of budesonide extended-release tablets should be considered. After extensive intake of grapefruit juice (which inhibits CYP3A4 activity predominantly in the intestinal mucosa), the systemic exposure for oral budesonide increased about two times. Ingestion of grapefruit or grapefruit juice should be avoided in connection with budesonide extended-release tablets administration [seeDosage and Administration (2)and Clinical Pharmacology (12.3)].
7.2 Inhibitors of Gastric Acid Secretion
Since the dissolution of the coating of budesonide extended-release tablets is pH dependent, the release properties and uptake of the compound may be altered when budesonide extended-release tablets are used after treatment with gastric acid reducing agents (e.g., proton pump inhibitors (PPIs), H2 blockers and antacids).
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Limited published studies report on the use of budesonide in pregnant women; however, the data are insufficient to inform a drug-associated risk for major birth defects and miscarriage. There are clinical considerations (see Clinical Considerations). In animal reproduction studies with pregnant rats and rabbits, subcutaneous administration of budesonide during organogenesis at doses 0.5 times and 0.05 times, respectively, the maximum recommended human dose, resulted in increased fetal loss, decreased pup weights, and skeletal abnormalities. Maternal toxicity was observed in both rats and rabbits at these dose levels (see Data). Based on animal data, advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage of the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4%, and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
Published data suggest that increased disease activity is associated with the risk of developing adverse pregnancy outcomes in women with ulcerative colitis. Adverse pregnancy outcomes include preterm delivery (before 37 weeks of gestation), low birth weight (less than 2500 g) infants, and small for gestational age at birth.
Fetal/Neonatal Adverse Reactions
Hypoadrenalism may occur in infants born of mothers receiving corticosteroids during pregnancy. Infants should be carefully observed for signs of hypoadrenalism, such as poor feeding, irritability, weakness, and vomiting, and managed accordingly [see Warnings and Precautions (5.1)].
Data
Animal Data
Budesonide was teratogenic and embryolethal in rabbits and rats. In an embryo-fetal development study in pregnant rats dosed subcutaneously with budesonide during the period of organogenesis from gestation days 6-15 there were effects on fetal development and survival at subcutaneous doses up to approximately 500 mcg/kg in rats (approximately 0.5 times the maximum recommended human dose on a body surface area basis). In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis from gestation days 6-18, there was an increase in maternal abortion, and effects on fetal development and reduction in litter weights at subcutaneous doses up to approximately 25 mcg/kg in rabbits (approximately 0.05 times the maximum recommended human dose on a body surface area basis). Maternal toxicity, including reduction in body weight gain, was observed at subcutaneous doses of 5 mcg/kg in rabbits (approximately 0.01 times the maximum recommended human dose on a body surface area basis) and 500 mcg/kg in rats (approximately 0.5 times the maximum recommended human dose on a body surface area basis).
In a peri-and post-natal development study, rats dosed subcutaneously with budesonide during the period of Day 15 post coitum to Day 21 postpartum, budesonide had no effects on delivery but did have an effect on growth and development of offspring. In addition, offspring survival was reduced, and surviving offspring had decreased mean body weights at birth and during lactation at exposures 0.02 times the MRHD (on a mg/m2 basis at maternal subcutaneous doses of 20 mcg/kg/day and higher). These findings occurred in the presence of maternal toxicity.
8.2 Lactation
Risk Summary
Lactation studies have not been conducted with budesonide extended-release tablets or other oral budesonide products and no information is available on the effects of budesonide on the breastfed infant or the effects of the drug on milk production. One published study reports that budesonide is present in human milk following maternal inhalation of budesonide (see Data). The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for budesonide extended-release tablets and any potential adverse effects on the breastfed infant from budesonide extended-release tablets, or from the underlying maternal condition.
Data
One published study reports that budesonide is present in human milk following maternal inhalation of budesonide which resulted in infant doses approximately 0.3% to 1% of the maternal weight-adjusted dosage and a milk/plasma ratio ranging between 0.4 and 0.5. Budesonide plasma concentrations were not detected, and no adverse events were noted in the breastfed infants following maternal use of inhaled budesonide. The recommended daily dose of budesonide extended-release tablets is higher (9 mg daily) compared with inhaled budesonide (up to 800 mcg daily) given to mothers in the above described study.
The maximum budesonide plasma concentration following a 9 mg daily dose (in both single-and repeated-dose pharmacokinetic studies) of oral budesonide is approximately 5 to 10 nmol/L which is up to 10 times higher than the 1 to 2 nmol/L for a 800 mcg daily dose of inhaled budesonide at steady state in the above inhalation study. Assuming the coefficient of extrapolation between the inhaled and oral doses is constant across all dose levels, at therapeutic doses of budesonide extended-release tablets, budesonide exposure to the nursing child may be up to 10 times higher than that by budesonide inhalation.
8.4 Pediatric Use
Safety and effectiveness of budesonide extended-release tablets in pediatric patients have not been established. Glucocorticosteroids, such as budesonide extended-release tablets, may cause a reduction of growth velocity in pediatric patients.
8.5 Geriatric Use
Clinical studies of budesonide extended-release tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, budesonide extended-release tablets should be used cautiously in elderly patients due to the potential for decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
Patients with moderate to severe liver disease should be monitored for increased signs and/or symptoms of hypercorticism. Discontinuing the use of budesonide extended-release tablets should be considered in these patients [seeWarnings and Precautions (5.4)].
10 OVERDOSAGE
Reports of acute toxicity and/or death following overdosage of glucocorticosteroids are rare. Treatment consists of immediate gastric lavage or emesis followed by supportive and symptomatic therapy.
If glucocorticosteroids are used at excessive doses for prolonged periods, systemic glucocorticosteroid effects, such as hypercorticism and adrenal suppression may occur. For chronic overdosage in the face of severe disease requiring continuous steroid therapy, the dosage may be reduced temporarily.
Single oral budesonide doses of 200 and 400 mg/kg were lethal in female and male mice, respectively. The signs of acute toxicity were decreased motor activity, piloerection and generalized edema.
11 DESCRIPTION
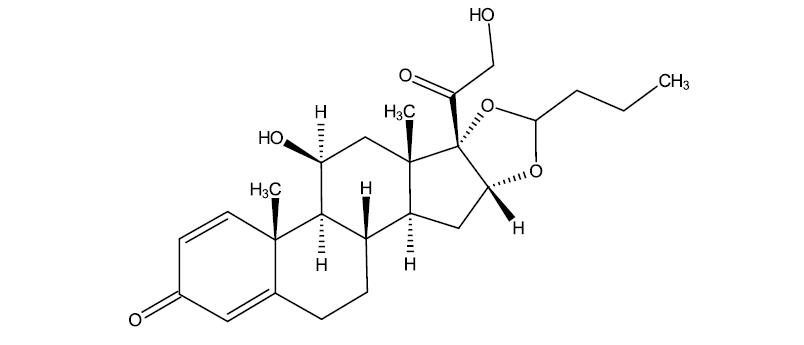
Budesonide extended-release tablets, for oral administration, contain budesonide, a synthetic corticosteroid, as the active ingredient. Budesonide is designated chemically as (RS)-11β, 16α, 17,21 tetrahydroxypregna-1,4-diene-3,20-dione cyclic 16,17-acetal with butyraldehyde.
Budesonide is provided as a mixture of two epimers (22R and 22S). The empirical formula of budesonide is C25H34O6 and its molecular weight is 430.5. Its structural formula is:
Budesonide is a white to off-white, odorless, crystalline powder that is practically insoluble in water, sparingly soluble in alcohol, and freely soluble in chloroform.
Budesonide extended-release tablets, a delayed and extended-release tablet, are coated with a polymer film, which breaks down at or above pH 7. The tablet core contains budesonide with polymers that provide for extended release of budesonide.
Each tablet contains the following inactive ingredients: stearic acid, lecithin, microcrystalline cellulose, hydroxypropyl cellulose, lactose, silicon dioxide, magnesium stearate, methacrylic acid copolymer types A and B, talc, triethyl citrate, and titanium dioxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Budesonide has a high topical glucocorticosteroid (GCS) activity and substantial first-pass elimination. The formulation contains budesonide in an extended-release tablet core. The tablet core is enteric coated to protect dissolution in gastric juice which delays budesonide release until exposure to a pH ≥7 in the small intestine. Upon disintegration of the coating, the core matrix provides extended release of budesonide in a time dependent manner.
12.2 Pharmacodynamics
Budesonide has a high glucocorticoid effect and a weak mineralocorticoid effect, and the affinity of budesonide to GCS receptors, which reflects the intrinsic potency of the drug, is about 200-fold that of cortisol and 15-fold that of prednisolone.
Treatment with systemically active GCS, including budesonide extended-release tablets, is associated with a suppression of endogenous cortisol concentrations and an impairment of the hypothalamus-pituitary-adrenal (HPA) axis function. Markers, indirect and direct, of this are cortisol levels in plasma or urine and response to ACTH stimulation.
In a study assessing the response to ACTH stimulation test in patients treated with budesonide extended-release tablets 9 mg once daily, the proportion of patients with abnormal response was 47% at 4 weeks and 79% at 8 weeks.
12.3 Pharmacokinetics
Absorption
Following single oral administration of budesonide extended-release tablets 9 mg in healthy subjects, peak plasma concentration (Cmax) was 1.35 ± 0.96 ng/mL, the time to peak concentration (Tmax) on average was 13.3 ± 5.9 hours, although it varied across different individual patients, and the area under the plasma concentration time curve (AUC) was approximately 16.43 ± 10.52 ng·hr/mL. The pharmacokinetic parameters of budesonide extended-release tablets 9 mg have a high degree of variability among subjects. There was no accumulation of budesonide with respect to both AUC and Cmax following 7 days of budesonide extended-release tablets 9 mg once daily dosing.
Food Effect
A food-effect study involving administration of budesonide extended-release tablets to healthy volunteers under fasting conditions and with a high-fat meal indicated that the Cmax was decreased by 27% while there was no significant decrease in AUC. Additionally, a mean delay in absorption lag time of 2.4 hours was observed under fed conditions.
Distribution
The mean volume of distribution (VSS) of budesonide varies between 2.2 and 3.9 L/kg in healthy subjects and in patients. Plasma protein binding is estimated to be 85 to 90% in the concentration range 1 to 230 nmol/L, independent of gender. The erythrocyte/plasma partition ratio at clinically relevant concentrations is about 0.8.
Elimination
Metabolism
Following absorption, budesonide is subject to high first-pass metabolism (80-90%). In vitro experiments in human liver microsomes demonstrate that budesonide is rapidly and extensively biotransformed, mainly by CYP3A4, to its 2 major metabolites, 6β-hydroxy budesonide and 16α-hydroxy prednisolone. The glucocorticoid activity of these metabolites is negligible (<1/100) in relation to that of the parent compound.
In vivo investigations with intravenous doses in healthy subjects are in agreement with the in vitro findings and demonstrate that budesonide has a high plasma clearance, 0.9-1.8 L/min. These high plasma clearance values approach the estimated liver blood flow, and, accordingly, suggest that budesonide is a high hepatic clearance drug.
The plasma elimination half-life, t1/2, after administration of intravenous doses ranges between 2 and 3.6 hours.
Excretion
Budesonide is excreted in urine and feces in the form of metabolites. After oral as well as intravenous administration of micronized [3H]-budesonide, approximately 60% of the recovered radioactivity is found in urine. The major metabolites, including 6β-hydroxy budesonide and 16α-hydroxy prednisolone, are mainly renally excreted, intact or in conjugated forms. No unchanged budesonide is detected in urine.
Specific Populations
Patients with Renal Impairment
The pharmacokinetics of budesonide in patients with renal impairment have not been studied. Intact budesonide is not renally excreted, but metabolites are to a large extent, and might therefore reach higher levels in patients with impaired renal function. However, these metabolites have negligible corticosteroid activity as compared with budesonide (<1/100).
Patients with Hepatic Impairment
In patients with liver cirrhosis, systemic availability of orally administered budesonide correlates with disease severity and is, on average, 2.5-fold higher compared with healthy controls. Patients with mild liver disease are minimally affected. Patients with severe liver dysfunction were not studied. Absorption parameters were not altered, and for the intravenous dose, no significant differences in CL or VSS were observed.
Drug Interaction Studies
Budesonide is metabolized via CYP3A4. Potent inhibitors of CYP3A4 can increase the plasma levels of budesonide several-fold. Co-administration of ketoconazole results in an eight-fold increase in AUC of budesonide, compared to budesonide alone. Grapefruit juice, an inhibitor of gut mucosal CYP3A, approximately doubles the systemic exposure of oral budesonide. Conversely, induction of CYP3A4 can result in the lowering of budesonide plasma levels [see Dosage and Administration (2) and Drug Interactions (7)].
Oral contraceptives containing ethinyl estradiol, which are also metabolized by CYP3A4, do not affect the pharmacokinetics of budesonide. Budesonide does not affect the plasma levels of oral contraceptives (i.e., ethinyl estradiol).
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity
Carcinogenicity studies with budesonide were conducted in rats and mice. In a two-year study in Sprague-Dawley rats, budesonide caused a statistically significant increase in the incidence of gliomas in male rats at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). In addition, there were increased incidences of primary hepatocellular tumors in male rats at 25 mcg/kg (approximately 0.023 times the maximum recommended human dose on a body surface area basis) and above. No tumorigenicity was seen in female rats at oral doses up to 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). In an additional two-year study in male Sprague-Dawley rats, budesonide caused no gliomas at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). However, it caused a statistically significant increase in the incidence of hepatocellular tumors at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). The concurrent reference glucocorticosteroids (prednisolone and triamcinolone acetonide) showed similar findings. In a 91-week study in mice, budesonide caused no treatment-related carcinogenicity at oral doses up to 200 mcg/kg (approximately 0.1 times the maximum recommended human dose on a body surface area basis).
Mutagenesis
Budesonide was not genotoxic in the Ames test, the mouse lymphoma cell forward gene mutation (TK+/-) test, the human lymphocyte chromosome aberration test, the Drosophila melanogaster sex-linked recessive lethality test, the rat hepatocycte unscheduled DNA synthesis (UDS) test and the mouse micronucleus test.
Impairment of Fertility
In rats, budesonide had no effect on fertility at subcutaneous doses up to 80 mcg/kg (approximately 0.07 times the maximum recommended human dose on a body surface area basis). However, it caused a decrease in prenatal viability and viability in pups at birth and during lactation, along with a decrease in maternal body weight gain, at subcutaneous doses of 20 mcg/kg (approximately 0.02 times the maximum recommended human dose on a body surface area basis) and above. No such effects were noted at 5 mcg/kg (approximately 0.005 times the maximum recommended human dose on a body surface area basis).
14 CLINICAL STUDIES
Induction of Remission in Active, Mild to Moderate Ulcerative Colitis
Two similarly designed, randomized, double-blind, placebo-controlled studies were conducted in a total of 970 adult patients with active, mild to moderate ulcerative colitis (UC) which was defined as an Ulcerative Colitis Disease Activity Index (UCDAI of ≥4 and ≤10). Eight hundred ninety-nine of these patients had histology consistent with active UC; this was considered the primary analysis population. UCDAI is a four-component scale (total score of 0 to 12) that encompasses the clinical assessments of stool frequency, rectal bleeding, mucosal appearance and physician’s rating of disease activity (score of 0 to 3 for each of the components).
The baseline median UCDAI score in both studies was 7.
In Study 1, 56% of patients were male, and the median age was 42 years. In Study 2, 57% of patients were male, and the median age was 44 years. In Study 1, 50% of patients were Caucasian, 7% were African American, and 34% were Asian. In Study 2, more than 99% were Caucasian.
Both studies compared budesonide extended-release tablets 9 mg and 6 mg with placebo and included an active reference arm (a mesalamine 2.4 g in Study 1 and a budesonide* 9 mg not approved for the treatment of UC in Study 2). The primary endpoint was induction of remission after 8 weeks of treatment. Remission was defined as a UCDAI score of ≤1, with subscores of 0 for rectal bleeding, stool frequency, and mucosal appearance and with a ≥1 point reduction in an endoscopy-only score.2 In both studies, budesonide extended-release tablets 9 mg extended-release tablets demonstrated superiority to placebo in inducing remission (Table 4).
Table 4. Induction of Remission in Studies 1 and 2
|
Treatment Group |
Study 1
|
Study 2
|
|
Budesonide extended-release tablets 9 mg |
22/123 (17.9) |
19/109 (17.4) |
|
Budesonide extended-release tablets 6 mg |
16/121 (13.2) |
9/109 (8.3) |
|
Reference arm* |
15/124 (12.1) |
13/103 (12.6) |
|
Placebo |
9/121 (7.4) |
4/89 (4.5) |
|
Treatment difference between budesonide extended-release tablets 9 mg and placebo (95% CI)† |
10.4% (2.2%, 18.7%) |
12.9% (4.6%, 21.3%) |
Remission is defined as a UCDAI score of ≤1, with subscores of 0 for rectal bleeding, stool frequency, and mucosal appearance and with a ≥1 point reduction in an endoscopy-only score.2
The primary analysis population included only patients that had histology consistent with active UC.
CI=Confidence Interval
*The reference arm in Study 1 is a delayed release mesalamine 2.4 g; the reference arm in Study 2 is a budesonide 9 mg not approved for the treatment of UC.
†p<0.025 for budesonide extended-release tablets 9 mg vs. placebo in both Studies 1 and 2 based on the Chi-square test (alpha=0.025)
15 REFERENCES
- 1.
- Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ. 1989;298:82-6.
16 HOW SUPPLIED/STORAGE AND HANDLING
Budesonide extended-release tablets 9 mg are white, round, biconvex tablets and debossed with “MX9”. They are supplied as follows:
- NDC 68682-309-30 Bottles of 30 tablets
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Keep container tightly closed. Protect from light and moisture.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Patients being treated with budesonide extended-release tablets should receive the following information and instructions. This information is intended to aid the patient in the safe and effective use of budesonide extended-release tablets.
Hypercorticism and Adrenal Suppression
Patients should be advised that budesonide extended-release tablets may cause systemic glucocorticosteroid effects of hypercorticism and adrenal suppression. Patients should taper slowly from systemic corticosteroids if transferring to budesonide extended-release tablets [see Warnings and Precautions (5.1) and (5.2)].
Immunosuppression
Patients who are on immunosuppressant doses of glucocorticosteroids should be warned to avoid exposure to chickenpox or measles and, if exposed, to consult their physician immediately. If exposure to such a person occurs, and the patient has not had chickenpox or been properly vaccinated, a physician should be consulted immediately. Patients should be informed of potential worsening of existing tuberculosis, fungal, bacterial, viral, or parasitic infections, or ocular herpes simplex [see Warnings and Precautions (5.3)].
How to Take Budesonide Extended-Release Tablets
Budesonide extended-release tablets should be swallowed whole with water and NOT CHEWED, CRUSHED, OR BROKEN. Patients should be advised to avoid the consumption of grapefruit juice for the duration of their budesonide extended-release tablets therapy [see Dosage and Administration (2)].
Pregnancy
Advise female patients that budesonide extended-release tablets may cause fetal harm and to inform their healthcare provider with a known or suspected pregnancy [see Use in Specific Populations (8.1)].
Distributed by:
Oceanside Pharmaceuticals, a division of
Bausch Health US, LLC
Bridgewater, NJ 08807 USA
Manufactured by:
Cosmo S.p.A.
Milan, 20020 Italy
By license of Cosmo Technologies Ltd., Dublin, Ireland
U.S. Patent Numbers: 7,410,651; 7,431,943; 8,293,273; 8,784,888; 8,895,064; 9,132,093; 9,192,581; 9,320,716; 9,532,954; 9,592,203; 9,737,489; 10,052,286; 10,064,878; 10,105,374; 10,143,698; 10,154,964; 10,172,799; 10,307,375 and RE43799
© 2020 Bausch Health Companies Inc. or its affiliates
9628701
70014816
Patient Information
Budesonide (bew DEH no side)
extended release tablets
What are budesonide extended-release tablets?
- •
- Budesonide extended release tablets are a prescription corticosteroid medicine used to help get active mild to moderate ulcerative colitis (UC) under control (induce remission).
- •
- It is not known if budesonide extended release tablets are safe and effective in children.
Who should not take budesonide extended release tablets?
Do not take budesonide extended release tablets if:
- •
- you are allergic to budesonide or any of the ingredients in budesonide extended release tablets. See the end of this leaflet for a complete list of ingredients in budesonide extended release tablets.
What should I tell my healthcare provider before taking budesonide extended release tablets?
Before you take budesonide extended release tablets tell your healthcare provider about all of your medical conditions, including if you:
- •
- have liver problems.
- •
- are planning to have surgery.
- •
- have chickenpox or measles or have recently been near anyone with chickenpox or measles.
- •
- have an infection.
- •
- have or had a family history of diabetes, cataracts or glaucoma.
- •
- have or had tuberculosis.
- •
- have high blood pressure (hypertension).
- •
- have decreased bone mineral density (osteoporosis).
- •
- have stomach ulcers.
- •
- are pregnant or plan to become pregnant. Budesonide extended release tablets may harm your unborn baby. Tell your healthcare provider if you are pregnant or think you are pregnant.
- •
- are breastfeeding or plan to breastfeed. Budesonide extended release tablets can pass into your breast milk and may harm your baby. You and your healthcare provider should decide if you will take budesonide extended release tablets or breastfeed. You should not do both.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Budesonide extended release tablets and other medicines may affect each other causing side effects.
Especially tell your healthcare provider if you take another medicine that contains corticosteroids for other conditions, such as allergies or asthma.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
How should I take budesonide extended release tablets?
- •
- Take budesonide extended release tablets exactly as your healthcare provider tells you to take them.
- •
- Take budesonide extended release tablets 1 time each day in the morning with or without food.
- •
- Take budesonide extended release tablets whole with water. Do not chew, crush, or break budesonide extended release tablets before swallowing.
- •
- If you take too much of budesonide extended release tablets, call your healthcare provider right away or go to the nearest hospital emergency room.
What should I avoid while taking budesonide extended release tablets?
- •
- Do not eat grapefruit or drink grapefruit juice while taking budesonide extended release tablets. Eating grapefruit or drinking grapefruit juice can increase the level of budesonide extended release tablets in your blood.
What are the possible side effects of budesonide extended release tablets?
Budesonide extended release tablets may cause serious side effects, including:
- •
- Effects of having too much corticosteroid medicine in your blood (hypercorticism). Long-time use of budesonide extended release tablets can cause you to have too much glucocorticosteroid medicine in your blood. Tell your healthcare provider if you have any of the following signs and symptoms of hypercorticism:
- o
- acne
- o
- bruise easily
- o
- rounding of your face (moon face)
- o
- ankle swelling
- o
- thicker or more hair on your body and face
- o
- a fatty pad or hump between your shoulders (buffalo hump)
- o
- pink or purple stretch marks on the skin of your abdomen, thighs, breasts and arms
Adrenal suppression. When budesonide extended-release tablets are taken for a long period of time (chronic use), the adrenal glands do not make enough steroid hormones (adrenal suppression). Tell your healthcare provider if you are under stress or have any symptoms of adrenal suppression during treatment with budesonide extended release tablets including:
- o
- tiredness
- o
- weakness
- o
- nausea
- o
- vomiting
- o
- low blood pressure
- •
- Immune system effects and a higher chance of infections.
- Budesonide extended release tablets weaken your immune system. Taking medicines that weaken your immune system makes you more likely to get infections. Avoid contact with people who have contagious diseases such as chickenpox or measles, while taking budesonide extended release tablets.
- Tell your healthcare provider about any signs or symptoms of infection during treatment with budesonide extended release tablets, including:
- o
- fever
- o
- pain
- o
- aches
- o
- chills
- o
- feeling tired
- o
- nausea and vomiting
- •
- Worsening of allergies. If you take certain other corticosteroid medicines to treat allergies, switching to budesonide extended release tablets may cause your allergies to come back. These allergies may include eczema (a skin disease) or rhinitis (inflammation inside your nose). Tell your healthcare provider if any of your allergies become worse while taking budesonide extended release tablets.
The most common side effects of budesonide extended release tablets include:
- •
- headache
- •
- nausea
- •
- decreased blood cortisol levels
- •
- stomach-area pain
- •
- tiredness
- •
- stomach or intestinal gas
- •
- bloating
- •
- acne
- •
- urinary tract infection
- •
- joint pain
- •
- constipation
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of budesonide extended release tablets. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store budesonide extended release tablets?
- •
- Store budesonide extended release tablets at room temperature, between 68° to 77°F (20° to 25°C).
- •
- Keep the bottle tightly closed to protect budesonide extended release tablets from light and moisture.
Keep budesonide extended release tablets and all medicines out of the reach of children.
General information about the safe and effective use of budesonide extended release tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use budesonide extended release tablets for a condition for which it was not prescribed. Do not give budesonide extended release tablets to other people, even if they have the same symptoms you have. It may harm them.
You can ask your healthcare provider or pharmacist for information about budesonide extended release tablets that is written for health professionals.
For more information call 1-800-321-4576.
What are the ingredients in budesonide extended release tablets?
Active Ingredient: budesonide
Inactive ingredients: stearic acid, lecithin, microcrystalline cellulose, hydroxypropyl cellulose, lactose, silicon dioxide, magnesium stearate, methacrylic acid copolymer types A and B, talc, triethyl citrate, and titanium dioxide.
Distributed by:
Oceanside Pharmaceuticals, a division of
Bausch Health US, LLC
Bridgewater, NJ 08807 USA
Manufactured by:
Cosmo S.p.A.
Milan, 20020 Italy
By license of Cosmo Technologies Ltd., Dublin, Ireland
U.S. Patent Numbers: U.S. Patent Numbers: 7,410,651; 7,431,943; 8,293,273; 8,784,888; 8,895,064; 9,132,093; 9,192,581; 9,320,716; 9,532,954; 9,592,203; 9,737,489; 10,052,286; 10,064,878; 10,105,374; 10,143,698; 10,154,964; 10,172,799; 10,307,375 and RE43799
© 2020 Bausch Health Companies Inc. or its affiliates
This Patient Information has been approved by the U.S. Food and Drug Administration.
9628701 70014816
Revised: 04/2020