FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
BAT [Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) – (Equine)] is a mixture of immune globulin fragments indicated for the treatment of symptomatic botulism following documented or suspected exposure to botulinum neurotoxin serotypes A, B, C, D, E, F, or G in adults and pediatric patients.
The effectiveness of BAT is based on efficacy studies conducted in animal models of botulism.
2 DOSAGE AND ADMINISTRATION
BAT is for intravenous use only.
2.1 Dosage and Administration
- •
- Each vial of BAT contains a minimum potency for serotypes A, B, C, D, E, F, and G antitoxin [see Dosage Forms and Strengths (3 DOSAGE FORMS AND STRENGTHS
- •
- For adult, pediatric, and infant patient groups, administer a dose of BAT according to Table 1. For details on pediatric dosing by body weight see Table 2.
- •
- Administer all BAT doses after dilution 1:10 in normal saline by slow intravenous infusion according to the varying infusion rates in Table 1.
- •
- Monitor vital signs throughout the infusion. If tolerated, the infusion rate can be increased incrementally up to the maximum infusion rate, and continued for the remainder of the administration. Decrease infusion rate if the patient develops discomfort or infusion-related adverse reactions.
|
Patient Group |
Dose |
Starting Infusion Rate (first 30 minutes) |
Incremental Infusion Rate if Tolerated (every 30 minutes) |
Maximum Infusion Rate |
|
Adults (≥ 17 years) |
One vial |
0.5 mL/min |
Double the rate |
2 mL/min |
|
Pediatric (1 year to < 17 years) |
20 – 100% of adult dose |
0.01 mL/kg/min Do not exceed the adult rate. |
0.01 mL/kg/min |
0.03 mL/kg/min Do not exceed the adult rate |
|
Infants (< 1 year) |
10% of adult dose regardless of body weight |
0.01 mL/kg/min |
0.01 mL/kg/min |
0.03 mL/kg/min |
Calculate pediatric BAT dose by body weight according to Table 2.
|
Body Weight (kg) |
Percent of Adult Dose* (%) |
|
10-14 |
20** |
|
15-19 |
30 |
|
20-24 |
40 |
|
25-29 |
50 |
|
30-34 |
60 |
|
35-39 |
65 |
|
40-44 |
70 |
|
45-49 |
75 |
|
50-54 |
80 |
|
≥ 55 |
100 |
|
*Dosing guide is based on the Salisbury Rule (1):
Do not exceed 1 vial dose regardless of body weight. ** Minimum pediatric dose is 20% of adult dose. See Table 1 for infant dose. |
|
2.2 Preparation
- 1.
- Bring vial to room temperature.
- •
- If frozen, thaw vial by placing in a refrigerator at 36 to 46 °F (2 to 8 °C) until the contents are thawed for approximately 14 hours.
- •
- Product can be thawed rapidly by placing at room temperature for one hour followed by a water bath at 98.6 °F (37°C) until thawed.
- •
- Do not thaw this product in a microwave oven. Do not refreeze the vial.
- 2.
- Inspect vial to ensure there is no damage to the seal or vial. If damaged, discard the vial.
- 3.
- Do not shake the vial during preparation to avoid foaming.
- 4.
- Dilute 1:10 in 0.9% Sodium Chloride Injection, USP (saline) by adding BAT solution from the vial to the appropriate amount of saline in an IV bag. Do not use any other diluents. As the fill volume per vial varies by lot number (ranging from 10 to 26 milliliters per vial), 90 to 235 milliliters of saline will be required. Withdraw the entire contents of the vial to obtain the total volume in the vial. If a partial vial is required (for pediatric dosing), the entire content of the vial should be withdrawn to ensure accurate calculation of the dosage [Table 2].
- 5.
- Visually inspect the product for particulate matter and discoloration prior to administration. Do not use if the solution is turbid, cloudy, or contains particles other than a few translucent-to-white proteinaceous particulates.
- 6.
- Use an intravenous line with constant infusion pump. Use a 15-micron sterile, non-pyrogenic, low protein binding in-line filter.
- 7.
- BAT vials are for single use only and contain no preservative. Once punctured, use the vial contents to prepare the infusion bag and administer as soon as possible.
- 8.
- Discard any unused portion.
3 DOSAGE FORMS AND STRENGTHS
BAT is a sterile solution of purified F(ab')2 plus F(ab')2-related immune globulin fragments derived from equine plasma, containing antitoxin activity to botulinum neurotoxins A, B, C, D, E, F, and G.
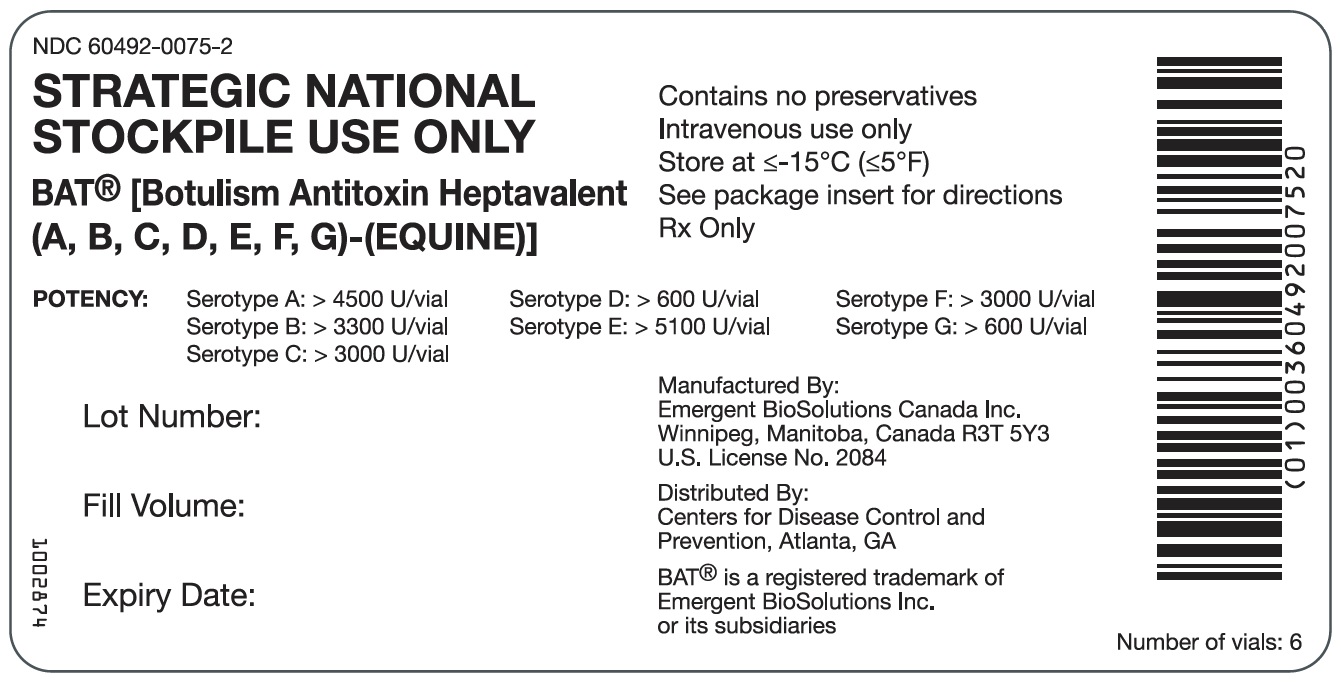
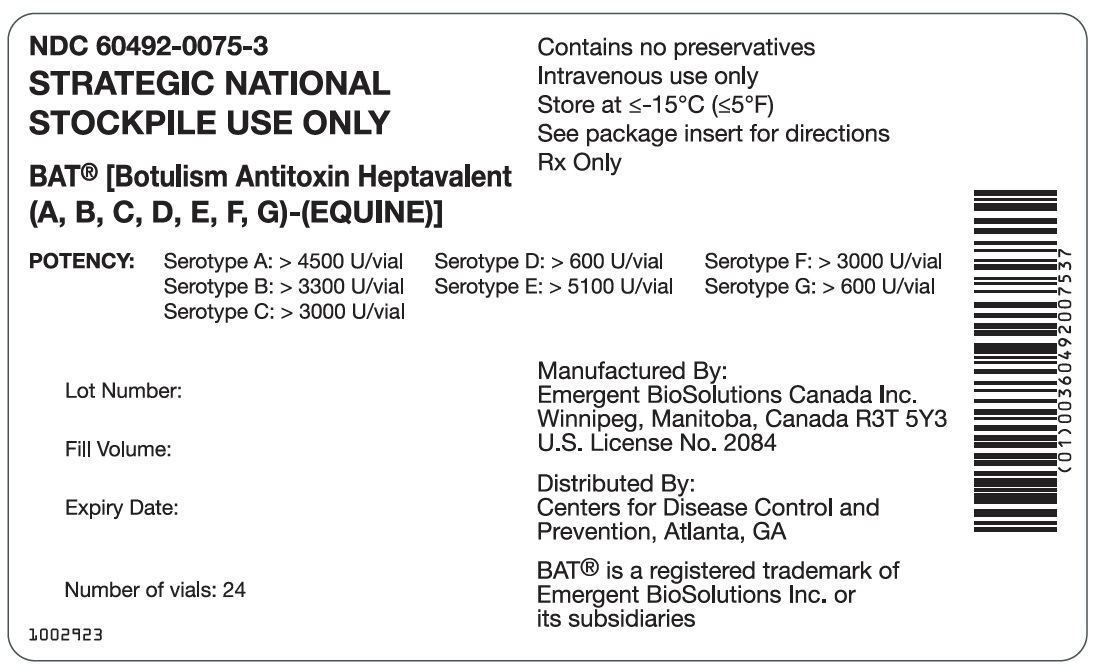
Each single-use vial, regardless of size or fill volume, contains a minimum antitoxin potency of:
- •
- 4,500 U serotype A antitoxin,
- •
- 3,300 U serotype B antitoxin,
- •
- 3,000 U serotype C antitoxin,
- •
- 600 U serotype D antitoxin,
- •
- 5,100 U serotype E antitoxin,
- •
- 3,000 U serotype F antitoxin, and
- •
- 600 U serotype G antitoxin.
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity Reactions
Severe hypersensitivity reactions, including anaphylactic and anaphylactoid reactions may occur following BAT administration. Patients who have had previous therapy with an equine-derived antivenom/antitoxin, with a history of hypersensitivity to horses, asthma, or hay fever are at a greater risk for developing severe hypersensitivity reactions to BAT. Administer BAT in a setting with appropriate equipment, medication including epinephrine, and personnel trained in the management of hypersensitivity, anaphylaxis, and shock.
Monitor all patients for signs and symptoms of acute allergic reaction (e.g. urticaria, pruritus, erythema, angioedema, bronchospasm with wheezing or cough, stridor, laryngeal edema, hypotension, tachycardia) during and following the BAT infusion. In case of hypersensitivity reaction, discontinue BAT administration immediately and administer appropriate emergency care. Have immediately available medications such as epinephrine for emergency treatment of acute hypersensitivity reactions.
For patients at risk for hypersensitivity reaction, begin BAT administration at the lowest rate achievable (< 0.01 mL/min) and monitor.
5.2 Delayed Allergic Reactions (Serum Sickness)
Delayed allergic reactions (serum sickness e.g. fever, urticarial or maculopapular rash, myalgia, arthralgia, and lymphadenopathy) may occur following BAT administration, typically 10-21 days after infusion. Monitor patients for signs and symptoms of delayed allergic reaction.
If a delayed allergic reaction (serum sickness) is suspected, administer appropriate medical care.
5.3 Infusion Reactions
Chills, fever, headaches, nausea, and vomiting can be related to the rate of infusion. Arthralgia, myalgia and fatigue or vasovagal reactions may also develop. Carefully observe patients for the onset of these infusion reactions throughout the infusion period and immediately following an infusion.
Reduce the rate of infusion if the patient experiences infusion reactions and administer symptomatic therapy. If symptoms worsen, discontinue the infusion and administer appropriate medical care.
5.4 Interference with Blood Glucose Testing
The maltose contained in BAT can interfere with some types of blood glucose monitoring systems i.e. those based on glucose dehydrogenase pyrroloquinoline-quinone (GDH-PQQ) method. This can result in falsely elevated glucose readings and inappropriate administration of insulin, resulting in life-threatening hypoglycemia. Cases of true hypoglycemia may go untreated if the hypoglycemic state is masked by falsely elevated results [see Drug Interactions (7 DRUG INTERACTIONS)].
5.5 Transmissible Infectious Agents
Because BAT is made from equine plasma, it may carry the risk of transmitting infectious agents e.g. viruses. The equine plasma pools are screened for the presence of certain infectious agents and the manufacturing process for BAT includes measures to inactivate and remove certain viruses [see Description (11 DESCRIPTION)]. Despite these measures, such products can still potentially transmit disease. No cases of transmission of viral diseases have been associated with the use of BAT.
Report all infections thought by a physician to have been transmitted by BAT to Emergent BioSolutions Canada Inc. at 1-800-768-2304. Discuss the risks and benefits of this product with the patient or their legal guardian before administering it to the patient [see Patient Counseling Information (17 PATIENT COUNSELING INFORMATION)].
6 ADVERSE REACTIONS
The most common adverse reactions observed in ≥ 5 % of healthy volunteers in clinical trials were headache, nausea, pruritus, and urticaria.
The most common adverse reactions reported in ≥ 1% of patients in a clinical study were pyrexia, rash, chills, nausea and edema.
The following serious adverse reactions are discussed in detail in other sections of the labeling:
- •
- Hypersensitivity reactions [see Warnings and Precautions (5.1 Hypersensitivity Reactions)]
- •
- Delayed allergic reactions/serum sickness [see Warnings and Precautions (5.2 Delayed Allergic Reactions (Serum Sickness)]
- •
- Infusion reactions [See Warnings and Precautions (5.3 Infusion Reactions)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In a randomized, double-blind, parallel arm trial conducted to evaluate the safety of BAT in healthy subjects, and to establish the pharmacokinetic profile of the seven botulinum antitoxin serotypes contained in BAT following intravenous (IV) administration, 40 subjects were randomized to receive either one (n=20) or two vials (n=20) of BAT.
In a second parallel arm, randomized, double-blind pharmacodynamic trial, 26 healthy subjects were randomized to receive either BAT in saline (n=16) or placebo (0.9% saline; n=10).
The most common adverse reactions in all healthy subjects were headache (9%), pruritus (5%), nausea (5%), and urticaria (5%). Other adverse reactions reported in less than 4% of subjects included pyrexia and throat discomfort. All reported adverse reactions were considered mild or moderate. No serious adverse reactions were reported. Two moderate acute allergic reactions that required premature termination of the infusion and treatment were reported. Reactions were predefined as mild if the subject was aware but could tolerate. Moderate reactions were predefined as discomfort enough to interfere with normal daily activity.
A total of 231 subjects with suspected or confirmed botulism were exposed to BAT in an open-label observational expanded access clinical study sponsored by the Centers for Disease Control and Prevention (CDC).
The majority of adult (213/216) and pediatric (13/15) subjects received one dose of BAT. Three adult subjects were exposed to a second dose of BAT, and two pediatric subjects each received two infant doses (10% of the adult dose). The administration of a second dose varied from seven hours to one month after the first dose.
Safety data was actively collected from treating physicians by the CDC. However, no on-site safety monitoring was performed, and the CDC relied on follow-up information provided by the treating physicians to determine the reporting frequencies for adverse reactions. Of the 231 subjects receiving BAT, safety information was available for 228 subjects. Adverse reactions were reported in 10% of all subjects. The most common adverse reactions were pyrexia (4%), rash (2%), chills (1%), nausea (1%), and edema (1%). Other adverse reactions were reported in less than 1% of subjects. No subject experienced anaphylaxis. One subject experienced a serious adverse reaction of hemodynamic instability characterized by bradycardia, tachycardia, and asystole during BAT administration. One subject experienced mild serum sickness (< 1%) with myalgia, arthralgia, and dark urine twelve days after BAT administration.
| System Organ Class | Preferred Term | Overall
(N=228) |
||
|---|---|---|---|---|
| No. of Events | No. of Subjects | % of Subjects | ||
|
ALL BODY SYSTEM |
OVERALL |
37 |
23 |
10.1 |
|
Cardiac disorders |
Cardiac arrest |
1 |
1 |
0.4 |
|
Bradycardia |
1 |
1 |
0.4 |
|
|
Tachycardia |
1 |
1 |
0.4 |
|
|
Gastrointestinal disorders |
Vomiting |
1 |
1 |
0.4 |
|
Nausea |
2 |
2 |
0.9 |
|
|
General disorders and administration site conditions |
Pyrexia |
9 |
9 |
3.9 |
|
Chest discomfort |
1 |
1 |
0.4 |
|
|
Edema |
2 |
2 |
0.9 |
|
|
Chills |
3 |
3 |
1.3 |
|
|
Feeling jittery |
1 |
1 |
0.4 |
|
|
Immune system disorders |
Serum Sickness |
1 |
1 |
0.4 |
|
Investigations |
Blood pressure increased |
1 |
1 |
0.4 |
|
White blood cell count increased |
1 |
1 |
0.4 |
|
|
Psychiatric disorders |
Agitation |
1 |
1 |
0.4 |
|
Anxiety |
1 |
1 |
0.4 |
|
|
Renal and urinary disorders |
Urinary retention |
1 |
1 |
0.4 |
|
Respiratory, thoracic and mediastinal disorders |
Bronchospasm |
1 |
1 |
0.4 |
|
Skin and subcutaneous tissue disorders |
Erythema |
1 |
1 |
0.4 |
|
Hyperhidrosis |
1 |
1 |
0.4 |
|
|
Rash |
4 |
4 |
1.8 |
|
|
Vascular disorders |
Hemodynamic instability |
1 |
1 |
0.4 |
|
Hypotension |
1 |
1 |
0.4 |
|
|
All adverse reactions were classified according to MedDRA Version 15.0 and are ranked according to medical significance within a given SOC. |
||||
6.2 Postmarketing Experience
The following hypersensitivity/allergic reactions have been reported in patients treated with BAT:
- •
- Anaphylactic shock
- •
- Angioedema
- •
- Urticaria
6.3 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. All subjects from the two clinical trials were tested for immunogenicity against BAT at baseline and at the end of the studies (Day 28) using a validated assay. Eleven subjects seroconverted during the course of the two trials. One subject from each clinical trial experienced a moderate allergic reaction during the administration of BAT. Both subjects were negative for anti-BAT antibodies at baseline and at the end of their respective studies. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to BAT with the incidence of antibodies to other products may be misleading.
7 DRUG INTERACTIONS
Drug Laboratory Interactions: Blood Glucose Testing
BAT contains maltose which can interfere with certain types of blood glucose monitoring systems [see Warnings and Precautions (5.4 Interference with Blood Glucose Testing)]. Only test systems that are glucose-specific should be used in patients receiving BAT. This interference can result in falsely elevated glucose readings that can lead to untreated hypoglycemia or to inappropriate insulin administration, resulting in life-threatening hypoglycemia.
The product information of the blood glucose testing system, including that of the test strips, should be carefully reviewed to determine if the system is appropriate for use with maltose-containing parenteral systems. If any uncertainty exists, contact the manufacturer of the testing system to determine if the system is appropriate for use with maltose-containing parenteral products.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
There are no human or animal data to establish the presence or absence of BAT associated risk.
8.2 Lactation
Risk Summary
There are no data to assess the presence or absence of BAT in human milk, the effects on the breastfed child or the effects on milk production/excretion.
Consider the developmental and health benefits of breastfeeding along with the mother’s clinical need for BAT and any potential adverse effects on the breastfed child from BAT or from the underlying maternal condition.
8.4 Pediatric Use
The effectiveness of BAT has not been established in pediatric patients. Limited pediatric safety data are available.
Fifteen pediatric subjects (age 10 days to 17 years; including 1 newborn, 3 infants and toddlers, 4 children and 7 adolescents) received BAT under the CDC expanded access clinical study. A 3-year old subject and an infant received two infant doses, and 13 pediatric subjects received one pediatric dose according to Salisbury Rule [Table 2].
Two adverse reactions were reported in two pediatric subjects. One subject experienced an adverse reaction of pyrexia following infusion of BAT, while the other subject experienced a serious adverse reaction of hemodynamic instability characterized by tachycardia, bradycardia, and asystole during infusion of BAT.
Dosing in pediatric patients is based on Salisbury Rule.
11 DESCRIPTION
BAT [Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) – (Equine)] is a sterile solution of F(ab’)2 and F(ab') 2-related antibody fragments prepared from plasma obtained from horses that have been immunized with a specific serotype of botulinum toxoid and toxin. To obtain the final heptavalent product, the seven antitoxin serotypes are blended. BAT is supplied in either a 20 or 50 milliliter vial size, with a fill volume ranging from 10 to 26 milliliters per vial. BAT is administered intravenously.
The manufacturing process for each antitoxin type includes cation-exchange chromatography to purify the immune globulin fraction, digestion with pepsin to produce F(ab')2 plus F(ab') 2-related immune globulin fragments, anion exchange chromatography to remove the pepsin as well as other impurities and filtration. In addition, the manufacturing process includes two viral inactivation/removal steps; solvent/detergent (S/D) treatment and virus filtration [Table 4].
The S/D treatment step is effective at inactivating known lipid-enveloped viruses such as equine encephalitis, equine arteritis, West Nile virus, equine infectious anemia, equine herpes virus, rabies, and equine influenza. The BAT manufacturing process also includes a robust filtration step that is effective in reducing the levels of some lipid-enveloped viruses (listed above) as well as non-enveloped viruses including equine rhinovirus, equine adenoviruses and adeno-associated viruses, and equine parvovirus.
| Enveloped | Non-enveloped | |||||||
|---|---|---|---|---|---|---|---|---|
|
Genome |
RNA |
RNA |
RNA |
DNA |
RNA |
DNA |
DNA |
RNA |
|
Virus |
XMuLV |
WNV |
BVDV |
PRV |
PI3 |
Ad2 |
Porcine Parvovirus |
EMC |
|
Family |
Retro |
Flavi |
Flavi |
Herpes |
Paramyxo |
Adeno |
Parvo |
Picorna |
|
Size (nm) |
80-110 |
40-70 |
50-70 |
150-200 |
100-200 |
70-90 |
18-24 |
25-30 |
|
Nanofiltration (log10) |
≥ 2.7 |
≥ 2.1 |
≥ 4.5 |
n.t. |
n.t. |
≥ 4.7 |
4.5 |
≥ 4.5 |
|
S/D (log10) |
≥ 4.3 |
≥ 5.1 |
n.t. |
≥ 5.1 |
≥ 5.5 |
n.t. |
n.t. |
n.t. |
|
Total Reduction (log10) |
≥ 7.0 |
≥ 7.2 |
≥ 4.5 |
≥ 5.1 |
≥ 5.5 |
≥ 4.7 |
4.5 |
≥ 4.5 |
|
XMuLV: Xenotropic Murine Leukemia Virus; specific model for equine infectious anemia, and a model for lipid-enveloped RNA viruses of similar size, such as vesicular stomatitis virus (Rhabdo family). WNV: West Nile Virus; relevant virus, and specific model for lipid-enveloped RNA viruses, including the arboviruses, which contains both Flavividae and Togaviridae and includes equine encephalitis viruses (Toga family) and equine viral arteritis (Arteri family, formerly a Toga virus). BVDV: Bovine Viral Diarrhea Virus; relevant virus, and specific model for lipid-enveloped RNA viruses, including the arboviruses, which contains both Flavividae and Togaviridae and includes equine encephalitis viruses (Toga family) and equine viral arteritis (Arteri family, formerly a Toga virus). PRV: Pseudorabies Virus; specific model for equine herpes viruses and non-specific model for lipid-enveloped viruses. PI3: Parainfluenza III Virus; model for lipid enveloped RNA viruses, and viruses of the similar family, orthomyxo, which includes equine influenza virus. Ad2: Adenovirus; specific model for equine adenovirus. EMC: Encephalomyocarditis Virus; specific model for equine parvovirus and adeno-associated virus, non-specific model for small lipid and non-lipid enveloped viruses. n.t.: not tested |
||||||||
BAT is formulated with 10% maltose and 0.03% polysorbate 80. The formulated bulk material contains approximately 3-7 g% (30-70 milligrams/milliliter) protein.
The product potency is expressed in units based on the mouse neutralization assay (MNA). Each unit of BAT is designed to neutralize 10,000 mouse intraperitoneal lethal dose 50% units (MIPLD50) of botulinum neurotoxin for serotype A, B, C, D, F, and G and 1,000 MIPLD50 of serotype E.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The mechanism of action of BAT is through passive immunization with equine polyclonal antibody fragments (primarily F(ab′)2 and Fab) against botulinum neurotoxin (BoNT) A, B, C, D, E, F, and G. In the circulation the polyclonal antibody fragments bind to free BoNT. This prevents the BoNT from interacting with ganglioside anchorage sites and protein receptors on the cholinergic nerve endings. In turn this prevents BoNT internalization into the target cells. The antibody/antigen complexes are then cleared from the circulation by the organs involved in processing immune complexes.
Experimental evidence concerning the amount of circulating antitoxin needed to counteract BoNT intoxication is not fully documented. The outcome of treatment depends, as it does with other comparable conditions, largely on the time interval elapsing after the onset of symptoms and antitoxin administration.
12.2 Pharmacodynamics
A proof-of-concept clinical dose-response trial was conducted using the extensor digitorum brevis (EDB) muscle of the foot as a model for measuring muscle paralysis after exposure to botulism toxin. In this model, BAT prevented subjects from experiencing a decrease in muscle function after exposure to botulinum neurotoxin (BoNT) serotypes A and B. Subjects treated with placebo (n=10) demonstrated a loss of greater than 50% EDB muscle function within 3 days of exposure to BoNT serotypes A and B. In the BAT arm of the trial (n=16), EDB muscle function was stable over time indicating that BAT was effective in preserving muscle function for up to 28 days following exposure to both BoNT serotype A and B.
12.3 Pharmacokinetics
The pharmacokinetics (PK) of the seven botulism antitoxin serotypes was determined in healthy human subjects following IV administration of either one (n=20) or two vials (n=20) of BAT. The various PK parameters are summarized in Table 5.
The PK parameters varied based upon the antitoxin serotype measured. Antitoxin serotypes D and E had the shortest half-lives. While antitoxin serotype B and C had the longest half-lives. The AUC0-∞ and Cmax values increased in a dose proportional fashion as the BAT dose increased from one to two vials. In addition, mean clearance values appeared to be similar between both treatment groups for the seven antitoxin serotypes, suggesting dose linearity of BAT over the dose range studied.
| Antitoxin
Serotype | Treatment Group | AUC0-∞
(U*hr/mL) | Cmax
(U/mL) | t1/2
(hr) | Cl
(mL/hr) | Vd
(mL) |
|---|---|---|---|---|---|---|
|
A |
1 Vial |
26.00 |
2.69 |
8.64 |
293 |
3637 |
|
2 Vials |
56.09 |
6.23 |
10.20 |
285 |
3993 |
|
|
B |
1 Vial |
29.30 |
1.90 |
34.20 |
196 |
9607 |
|
2 Vials |
62.55 |
4.28 |
57.10 |
181 |
14865 |
|
|
C |
1 Vial |
37.34 |
2.26 |
29.60 |
144 |
6066 |
|
2 Vials |
86.25 |
4.89 |
45.60 |
127 |
8486 |
|
|
D |
1 Vial |
7.62 |
0.81 |
7.51 |
137 |
1465 |
|
2 Vials |
14.83 |
1.60 |
7.77 |
151 |
1653 |
|
|
E |
1 Vial |
7.16 |
0.94 |
7.75 |
1250 |
14172 |
|
2 Vials |
15.66 |
1.75 |
7.32 |
1110 |
11596 |
|
|
F |
1 Vial |
31.40 |
2.37 |
14.10 |
169 |
3413 |
|
2 Vials |
63.19 |
4.29 |
18.20 |
168 |
4334 |
|
|
G |
1 Vial |
7.05 |
0.59 |
11.70 |
149 |
2372 |
|
2 Vials |
14.66 |
1.19 |
14.70 |
144 |
3063 |
|
|
AUC = Area Under the Concentration Curve; Cl = Clearance; Cmax = Maximum Serum Concentration; BAT = Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) – (Equine); t1/2 = Half-life; Tmax = Time to Maximum Serum Concentration; U = Unit; Vd = Volume of Distribution. |
||||||
13 NONCLINICAL TOXICOLOGY
13.2 Animal Toxicology and/or Pharmacology
Toxicological studies were not conducted for BAT or its components.
The evaluation of new treatment options for botulism using controlled human trials is unethical and infeasible. Therefore the effectiveness of BAT for treatment of botulism is based on well controlled efficacy studies conducted in guinea pigs and rhesus macaques.
Guinea Pig
In a controlled therapeutic efficacy study, guinea pigs were intoxicated with various BoNT serotypes (A, B, C, D, E, F or G) at a dose of 1.5x guinea pig intramuscular lethal dose 50% units (GPIMLD50) via intramuscular injection into the right hind limb. The animals were then treated with either placebo control or 1x scaled human dose of BAT (weight/weight based on an average human body weight of 70 kilograms), after the onset of moderate clinical signs of botulism (right hind limb weakness, salivation, lacrimation, weak limbs and noticeable changes in breathing rate or pattern). Treatment with BAT resulted in a statistically significant improvement in the survival rate of animals across all of the serotypes tested [Table 6].
| Neurotoxin Serotype | Treatment Group | Survival Rate (%) | Two-sided Fisher’s Exact Test (p-value) |
|---|---|---|---|
|
A |
1x BAT |
34/34 (100%) |
p<0.0001 |
|
Placebo Control |
0/34 (0%) |
||
|
B |
1x BAT |
34/34 (100%) |
p<0.0001 |
|
Placebo Control |
1/34 (3%) |
||
|
C |
1x BAT |
33/34 (97%) |
p<0.0001 |
|
Placebo Control |
4/34 (12%) |
||
|
D |
1x BAT |
33/34 (97%) |
p<0.0001 |
|
Placebo Control |
5/34 (15%) |
||
|
E |
1x BAT |
34/34 (100%) |
p<0.0001 |
|
Placebo Control |
0/34 (0%) |
||
|
F |
1x BAT |
34/34 (100%) |
p<0.0001 |
|
Placebo Control |
4/34 (12%) |
||
|
G |
1x BAT |
34/34 (100%) |
p<0.0001 |
|
Placebo Control |
17/34 (50%) |
||
|
BAT = Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) – (Equine). |
|||
Nonhuman Primate
In a controlled therapeutic efficacy study, rhesus macaques were intoxicated with BoNT serotype A delivered intravenously at a dose of 1.7x nonhuman primate intravenous lethal dose 50% (NHPLD50) units per kilogram of body weight. The animals were then treated with either placebo control or 1x scaled human dose of BAT (weight/weight based on an average human body weight of 70 kilograms), after the onset of clinical signs of botulism (ptosis, muscular weakness, or respiratory distress). Treatment with BAT resulted in a statistically significant improvement in the survival rate [Table 7].
| Treatment Group | Survival Rate (%) | Two-sided Fisher’s Exact Test (p-value) |
|---|---|---|
|
1x BAT |
14/30 (47%) |
p<0.0001 |
|
Placebo Control |
0/30 (0%) |
|
|
BAT = Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) – (Equine). |
||
14 CLINICAL STUDIES
The effectiveness of BAT is based on efficacy studies demonstrating a survival benefit in animal models of botulism [see Nonclinical Toxicology (13.2 Animal Toxicology and/or Pharmacology)]. The safety has been tested in healthy adults and patients with suspected botulism who were treated with BAT under an expanded access clinical study.
The pharmacokinetic, pharmacodynamic, and safety profiles of BAT have been evaluated in two clinical studies. In these clinical studies, BAT was shown to have an acceptable safety profile when one or two vials of BAT were administered intravenously to healthy subjects.
In a randomized, single-center, double-blind trial the pharmacokinetics and safety of BAT was evaluated in 40 healthy subjects receiving either one (n = 20) or two (n = 20) vials of BAT by IV infusion. Serum BAT levels were measured in the subjects using the Mouse Neutralization Assay (MNA) [see Clinical Pharmacology (12.3)].
In a randomized single center, double-blind trial the pharmacodynamics and safety of BAT was evaluated in 26 healthy subjects receiving either a single vial of BAT (n=16) or placebo (n=10) by IV infusion. The effects of BAT in preventing paralysis of the EDB foot muscle following administration of botulinum neurotoxin serotype A or B was determined [see Clinical Pharmacology (12.2)].
To provide additional support for the efficacy demonstrated in the animal models, a preliminary analysis of data from a Centers for Disease Control and Prevention (CDC) open-label, observational expanded access clinical study for the treatment of subjects with suspected or confirmed botulism with BAT was conducted. Across the 148 subjects treated with BAT in the period analyzed, 109 subjects had a final discharge diagnosis of suspected or confirmed botulism and were included in the analysis population. The median time from the onset of botulism symptoms to treatment with BAT was 3.6 days (range: 0.25 – 38 days). Early treatment (≤ 2 days after onset of symptoms) with BAT was associated with a shorter length of hospitalization, duration in intensive care unit (ICU) and duration of mechanical ventilation compared to later treatment [Table 8] and is consistent with the mechanism of action [see Clinical Pharmacology (12.1 Mechanism of Action)].
|
Time from Symptoms to Treatment |
Number of Patients (N) |
Mean Duration in Days (SD) |
|
|
Hospitalization |
≤ 2 Days |
14 |
12.4 (9.28) |
|
> 2 Days |
72 |
26.1 (26.37) |
|
|
ICU Stay |
≤ 2 Days |
13 |
9.2 (7.40) |
|
> 2 Days |
70 |
15.8 (18.76) |
|
|
Mechanical Ventilation |
≤ 2 Days |
9 |
11.6 (7.83) |
|
> 2 Days |
41 |
23.4 (21.11) |
15 REFERENCES
- 1.
- Lack JA, Stuart-Taylor ME. Calculation of drug dosage and body surface area of children. Br J Anaesth. 1997; 78:601-605.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
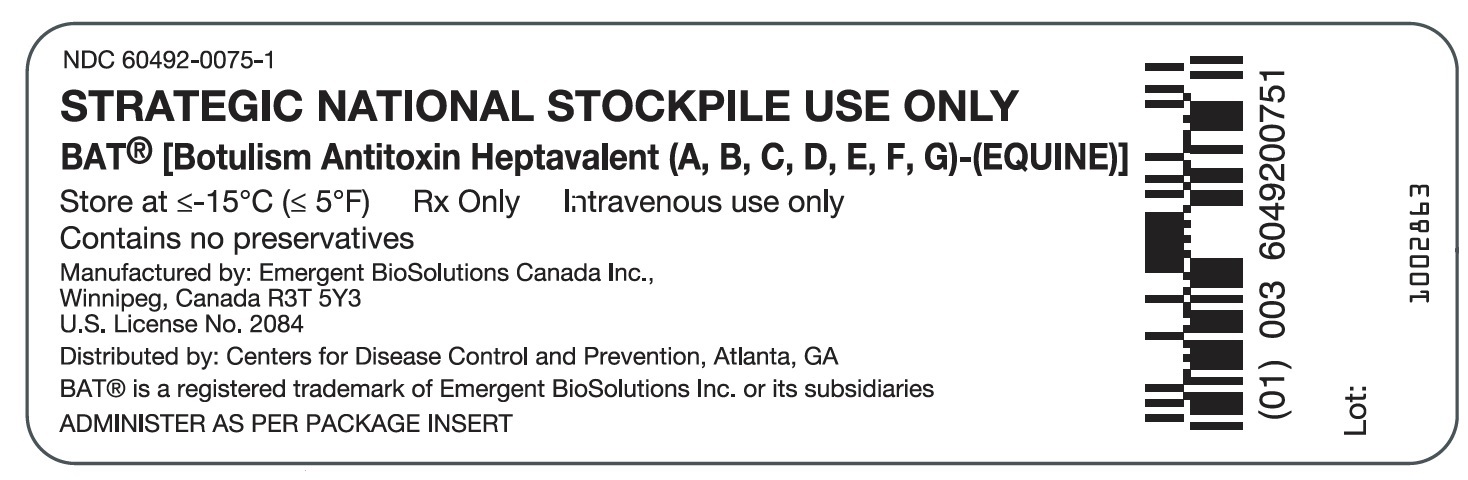
BAT is supplied in either 20 milliliter or 50 milliliter glass vials seated with a butyl rubber stopper and an aluminum seal with a plastic flip-top cap, with a fill volume ranging from 10 to 26 milliliters per vial. Each vial, regardless of size or fill volume contains a minimum potency of > 4,500 U serotype A antitoxin, > 3,300 U serotype B antitoxin, > 3000 U serotype C antitoxin, > 600 U serotype D antitoxin, > 5,100 U serotype E antitoxin, > 3,000 U serotype F antitoxin, and > 600 U serotype G antitoxin.
BAT is not made with natural rubber latex.
- NDC Number Product Description
- 60492-0075-2: A 50 milliliter single dose vial.
- 60492-0075-3: A 20 milliliter single dose vial.
- 60492-0075-4: A 50 milliliter single dose vial.
16.2 Storage and Handling
- •
- Store frozen at or below 5°F (≤ -15°C) until used.
- •
- Once thawed, Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) – (Equine) may be stored at 2-8°C (36-46°F) for a maximum of 36 months or until 48 months from the date of manufacture, whichever comes first. Do not refreeze.
- •
- Once punctured, use the vial contents to prepare the infusion bag and administer as soon as possible.
- •
- BAT vials are for single use only and contain no preservative. Discard any unused portion.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Patient Information).
- •
- Inform patients of the following:
- •
- BAT is prepared from equine plasma and may contain infectious agents such as viruses that can cause disease.
- •
- The risk that such products will transmit an infectious agent has been reduced by screening the horses for prior exposure to certain viruses, by testing for the presence of certain current viral infections, and by inactivating and/or removing certain viruses during manufacturing.
- •
- Despite these measures, such products can still potentially transmit disease.
- •
- There is also the possibility that unknown infectious agents may be present in such products.
- •
- Inform patients that persons who have received previous therapy with an equine-derived antivenom/antitoxin, have known allergies to horses, have asthma or get hay fever (seasonal allergies) may be at increased risk of hypersensitivity reactions and should only receive BAT if the benefits outweigh the risks.
- •
- Advise patients about the potential interference with non-glucose specific monitoring systems.
- •
- The maltose contained in BAT can interfere with some types of blood glucose monitoring systems.
- •
- Only testing systems that are glucose-specific should be used in patients receiving BAT.
- •
- This interference can result in falsely elevated glucose readings that can lead to untreated hypoglycemia or to inappropriate insulin administration, resulting in life-threatening hypoglycemia.
BAT® and any and all Emergent BioSolutions Inc. brand, product, service and feature names, logos and slogans are trademarks or registered trademarks of Emergent BioSolutions Inc. or its subsidiaries in the United States or other countries. All rights reserved.
Manufactured By:
Emergent BioSolutions Canada Inc.
155 Innovation Drive
Winnipeg, Manitoba
Canada, R3T 5Y3
U.S. License No. 2084
PATIENT INFORMATION
BAT® [Botulism Antitoxin Heptavalent (A, B, C, D, E, F, G) – (Equine)]
What is botulism?
Botulism is a muscle-paralyzing disease caused by a toxin made by a bacterium called Clostridium botulinum.
Botulism can cause the following conditions:
- •
- Double vision,
- •
- Blurred vision,
- •
- Drooping eyelids,
- •
- Slurred speech,
- •
- Difficulty swallowing,
- •
- Dry mouth,
- •
- Muscle weakness that spreads through the body,
- •
- Difficulty breathing.
Botulism can also cause paralysis and death. After a person is exposed to the toxin, problems can start as early as three hours or as late as a few days. It can take weeks or months to get better. During that time, many people need special care in the hospital.
The effectiveness of BAT has been studied in animals with botulism.
What is BAT?
BAT is a botulism antitoxin made from the plasma of horses. It contains antibody fragments which can neutralize botulism toxins. BAT may make the illness from botulism less severe. Treatment with BAT will not reverse the paralysis, but may decrease the duration and extent of paralysis.
Who should use BAT?
Your doctor may give you BAT if they suspect that you have been exposed to botulism toxin. You should get the treatment as quickly as possible to stop the progression of the illness.
Unless the benefits outweigh the risks, you should not receive BAT if you have a known history of allergies to horses or horse blood products, asthma or hay fever (seasonal allergies).
How will you receive BAT?
BAT is given as an injection into your vein. Your doctor will determine the dose of BAT. The treatment may take several hours to administer. Your doctor will decide if you need more than one injection.
What are the possible or reasonably likely side effects of BAT?
The most common side effects of BAT are:
- •
- Headache
- •
- Fever
- •
- Rash
- •
- Hives
- •
- Chills
- •
- Nausea
- •
- Swelling
Some people have a chilly feeling, difficulty breathing, and have a quick rise in body temperature within the first 20 to 60 minutes after getting BAT. This can be managed by your doctor.
BAT can cause allergic reactions. Tell your doctor or go to the emergency department right away if you have trouble breathing, swelling of your tongue or lips, or a very fast heart rate because this can be signs of a serious allergic reaction.
Tell your doctor if you get pains in your joints and back, fever, and a rash within one to three weeks after getting BAT. These can be signs of “serum sickness” and can last for a few weeks. Your doctor can give you medicine to help with serum sickness.
Talk to your doctor about any side effects that concern you. You can ask your doctor for additional prescribing information that is available to healthcare professionals.
What other information do you need to know about BAT?
BAT is made from horse plasma. The horses are carefully screened and the plasma is carefully cleaned, but there is a small risk that it may give you a virus. Talk to your doctor if you have any symptoms that concern you.
You may report side effects directly to Emergent BioSolutions Canada Inc. at 1-800-768-2304 or to the FDA’s MedWatch reporting system at 1-800-FDA-1088.
BAT® and any and all Emergent BioSolutions Inc. brand, product, service and feature names, logos and slogans are trademarks or registered trademarks of Emergent BioSolutions Inc. or its subsidiaries in the United States or other countries. All rights reserved.
Manufactured By:
Emergent BioSolutions Canada Inc.
155 Innovation Drive
Winnipeg, Manitoba
Canada, R3T 5Y3
US License No. 2084