FULL PRESCRIBING INFORMATION
WARNING: NEPHROTOXICITY, OTOTOXICITY AND EMBRYO-FETAL TOXICITY
Nephrotoxicity
Tobramycin for Injection can result in acute kidney injury, including acute renal failure. Risk factors that may contribute to nephrotoxicity include tobramycin accumulation (increasing serum trough levels), high peak concentrations (above 12 mcg/mL), total cumulative dose, advanced age, volume depletion and concurrent or sequential use of other nephrotoxic drugs. Avoid concurrent or sequential use of other potentially nephrotoxic drugs. Monitor serum tobramycin levels and renal function in all patients during drug treatment. Reduce the dose or discontinue the Tobramycin for Injection if renal impairment occurs [see Warnings and Precautions (5.1)].
Ototoxicity
Tobramycin for Injection can cause irreversible auditory and vestibular toxicity that may continue to develop after the drug has been discontinued. Risk factors include high serum concentrations, prolonged therapy, renal impairment, concurrent and sequential use of other nephrotoxic or ototoxic drugs (e.g. aminoglycosides), and extremes of age. Avoid concurrent or sequential use with other potentially ototoxic drugs. Monitor for signs and symptoms of auditory and vestibular toxicity. Reduce the dose or discontinue the Tobramycin for Injection if renal impairment occurs. Discontinue the Tobramycin for Injection if ototoxicity occurs. [see Warnings and Precautions (5.2)].
Neuromuscular Blockade
Aminoglycosides have been associated with neuromuscular blockade. During therapy with Tobramycin for Injection, monitor for adverse reactions associated with neuromuscular blockade, particularly in high-risk patients, such as patients with underlying neuromuscular disorders (including myasthenia gravis) or in patients concomitantly receiving neuromuscular blocking agents [see Warnings and Precautions (5.5)].
Embryo-Fetal Toxicity
Tobramycin and other aminoglycosides can cause fetal harm when administered to a pregnant woman. If Tobramycin for Injection is used during pregnancy or if the patient becomes pregnant while taking tobramycin, apprise the patient of the potential hazard to the fetus [see Warnings and Precautions (5.3) and Use in Specific Populations (8.1)].
1 INDICATIONS AND USAGE
1.1 Septicemia
Tobramycin for Injection is indicated for the treatment of septicemia caused by susceptible isolates of P. aeruginosa, E. coli, and Klebsiella spp., in adult and pediatric patients.
1.2 Lower Respiratory Tract Infections
Tobramycin for Injection is indicated for the treatment of lower respiratory tract infections caused by susceptible isolates of P. aeruginosa, Klebsiella spp., Enterobacter spp., Serratia spp., E. coli, and S. aureus in adult and pediatric patients.
1.3 Central Nervous System Infections (Meningitis)
Tobramycin for Injection is indicated for the treatment of bacterial meningitis caused by susceptible bacteria in adult and pediatric patients.
1.4 Intra-abdominal Infections
Tobramycin for Injection is indicated for the treatment of intra-abdominal infections, including peritonitis, caused by susceptible isolates of E. coli, Klebsiella spp., and Enterobacter spp. in adult and pediatric patients.
1.5 Skin and Skin Structure Infections
Tobramycin for Injection is indicated for the treatment of skin and skin structure infections caused by susceptible isolates of P. aeruginosa, Proteus spp., E. coli, Klebsiella spp., Enterobacter spp., and S. aureus in adult and pediatric patients.
1.6 Bone Infections
Tobramycin for Injection is indicated for the treatment of bone infections caused by susceptible isolates of P. aeruginosa, Proteus spp., E. coli, Klebsiella spp., Enterobacter spp., and S. aureus in adult and pediatric patients
1.7 Complicated and Recurrent Urinary Tract Infections
Tobramycin for Injection is indicated for the treatment of complicated urinary tract infections caused by susceptible isolates of P. aeruginosa, Proteus spp., (indole-positive and indole-negative), E. coli, Klebsiella spp., Enterobacter spp., Serratia spp., S. aureus, Providencia spp., and Citrobacter spp. in adult and pediatric patients
1.8 Usage
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Tobramycin for Injection and other antibacterial drugs, Tobramycin for Injection should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
2 DOSAGE AND ADMINISTRATION
2.1 Important Preparation and Administration Instructions
Pharmacy Bulk Package-Not for Direct Infusion
Tobramycin for Injection Pharmacy Bulk Package is intended for dispensing of single doses to many patients in a hospital pharmacy admixture service. It should only be prepared in an aseptic work area, such as a laminar flow hood. Tobramycin for Injection Pharmacy Bulk Package vial must be reconstituted and diluted prior to intravenous administration [see Dosage and Administration (2.8)]. After reconstitution, the closure may be penetrated only one time using a suitable sterile transfer device or dispensing set, which allows measured dispensing of the contents. Use of a syringe and needle is not recommended as it may cause leakage. After penetration, the entire contents of the bulk vial must be dispensed within 24 hours. Do not administer Tobramycin for Injection as a direct, undiluted intravenous injection.
2.2 Dosage for Adult Patients with Normal Renal Function
Tobramycin for Injection may be given intramuscularly or intravenously. Recommended dosages are the same for both routes. The recommended dosage is as follows:
Adult Patients
Adults with Serious Infections
3 mg/kg/day administered in 3 equal doses of 1 mg/kg every 8 hours.
Adults with Life-Threatening Infections
Up to 5 mg/kg/day may be administered in 3 or 4 equal doses (see Table 1). The dosage should be reduced to 3 mg/kg/day as soon as clinically indicated. To prevent increased toxicity due to excessive serum concentrations, dosage should not exceed 5 mg/kg/day unless serum concentrations are monitored [see Boxed Warning, Warnings and Precautions (5.2)].
| For
Patient Weighing | Usual Dose for
Serious Infections 1 mg/kg Every 8 hours (h) |
||
| kg | lb | (Total, 3 mg/kg/day) | |
| mg/dose | mL/dose* | ||
| q8h | |||
| 120 | 264 | 120 mg | 3 mL |
| 115 | 253 | 115 mg | 2.9 mL |
| 110 | 242 | 110 mg | 2.75 mL |
| 105 | 231 | 105 mg | 2.6 mL |
| 100 | 220 | 100 mg | 2.5 mL |
| 95 | 209 | 95 mg | 2.4 mL |
| 90 | 198 | 90 mg | 2.25 mL |
| 85 | 187 | 85 mg | 2.1 mL |
| 80 | 176 | 80 mg | 2 mL |
| 75 | 165 | 75 mg | 1.9 mL |
| 70 | 154 | 70 mg | 1.75 mL |
| 65 | 143 | 65 mg | 1.6 mL |
| 60 | 132 | 60 mg | 1.5 mL |
| 55 | 121 | 55 mg | 1.4 mL |
| 50 | 110 | 50 mg | 1.25 mL |
| 45 | 99 | 45 mg | 1.1 mL |
| 40 | 88 | 40 mg | 1 mL |
|
*Applicable to all product forms except the Tobramycin Injection, USP, (Pediatric). |
|||||
| For
Patient Weighing | Maximum Dose for Life-
Threatening Infections (Reduce as soon as possible) 1.66 mg/kg Every 8 hours |
||||
| kg | lb | (Total, 5 mg/kg/day) | |||
| mg/dose | mL/dose* | ||||
| Every 8h | |||||
| 120 | 264 | 200 mg | 5 mL | ||
| 115 | 253 | 191 mg | 4.75 mL | ||
| 110 | 242 | 183 mg | 4.5 mL | ||
| 105 | 231 | 175 mg | 4.4 mL | ||
| 100 | 220 | 166 mg | 4.2 mL | ||
| 95 | 209 | 158 mg | 4 mL | ||
| 90 | 198 | 150 mg | 3.75 mL | ||
| 85 | 187 | 141 mg | 3.5 mL | ||
| 80 | 176 | 133 mg | 3.3 mL | ||
| 75 | 165 | 125 mg | 3.1 mL | ||
| 70 | 154 | 116 mg | 2.9 mL | ||
| 65 | 143 | 108 mg | 2.7 mL | ||
| 60 | 132 | 100 mg | 2.5 mL | ||
| 55 | 121 | 91 mg | 2.25 mL | ||
| 50 | 110 | 83 mg | 2.1 mL | ||
| 45 | 99 | 75 mg | 1.9 mL | ||
| 40 | 88 | 66 mg | 1.6 mL | ||
2.3 Dosage for Pediatric Patients
2.4 Duration of Treatment for Adult and Pediatric Patients
The usual duration of treatment for adult and pediatric patients is 7 to10 days. A longer course of therapy may be necessary in complicated infections. In such cases, monitoring of renal, auditory, and vestibular functions is advised, because neurotoxicity is more likely to occur when treatment is extended longer than 10 days.
2.5 Dosage in Patients with Cystic Fibrosis or Burns
In patients with cystic fibrosis, altered pharmacokinetics may result in reduced serum concentrations of aminoglycosides. An initial dosing regimen of 10 mg/kg/day in 4 equally divided doses is suggested as a guide. The serum concentrations of tobramycin should be monitored during treatment due to wide inter-patient variability.
Similarly, altered pharmacokinetics may result in reduced serum concentrations in patients with extensive burns. Monitoring tobramycin serum concentration in these patients is especially important as a basis for determination of appropriate dosage [see Dosage and Administration (2.9)].
2.6 Dosage for Patients with Renal Impairment
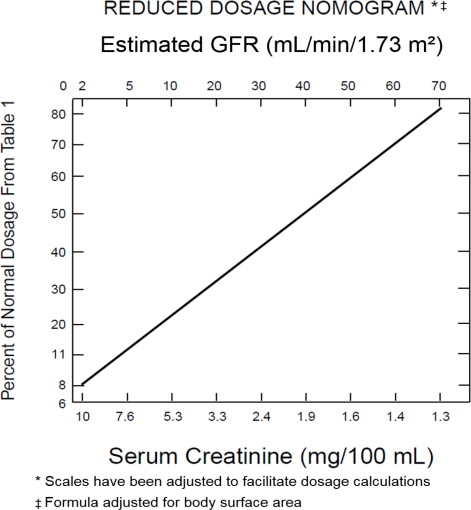
Following a loading dose of 1 mg/kg, subsequent dosage in these patients must be adjusted, either with reduced doses administered at 8-hour intervals or with normal doses given at prolonged intervals. Both of these methods are suggested as guides and dose should be adjusted based on serum concentration. The dosage adjustment for patients with renal impairment are based on either the creatinine clearance level or the serum creatinine level of the patient because these values correlate with the half-life of tobramycin. The dosage schedule derived from either method should be used in conjunction with careful clinical and laboratory observations of the patient and serum tobramycin concentration monitoring and should be modified as necessary. Neither method should be used when dialysis is being performed.
Reduced dosage at 8-hour intervals
When the creatinine clearance rate is less than or equal to 70 mL per minute or when the serum creatinine value is known, the amount of the reduced dose can be determined by multiplying the normal dose in adult patients from Table 1 by the percent of the normal dosage from the accompanying nomogram in Figure 1 below.
2.7 Dosage in Obese Patients
The appropriate dose may be calculated by using the patient's estimated lean body weight plus 40% of the excess as the weight on which to determine the dose in mg/kg.
2.8 Instructions for Preparation and Intravenous Administration
Tobramycin for Injection is supplied as a dry powder in a pharmacy bulk package vial that
contains the equivalent of 1.2 g of tobramycin. The contents of the vial must be reconstituted and diluted prior to intravenous administration as follows:
- Reconstitute the contents of the pharmacy bulk package vial aseptically with 30 mL of Sterile Water for Injection, USP to provide a reconstituted solution containing 40 mg of tobramycin per mL.
- Dilute the reconstituted pharmacy bulk vial prior to intravenous administration by adding a specified volume of the reconstituted solution to 50 to 100 mL (for adult doses) of diluent (0.9% Sodium Chloride Injection or 5% Dextrose Injection) for each patient. For pediatric patients, the volume of diluent should be proportionately less than for adults.
- After penetration, entire contents of pharmacy bulk vial should be dispensed within 24 hours.
- Visually inspect for particulate matter and discoloration prior to administration The diluted solution should be intravenously infused over a period of 20 to 60 minutes. Intravenous infusion periods of less than 20 minutes are not recommended because peak serum concentrations may exceed 12 mcg/mL [see Dosage and Administration (2.9)].
2.9 Measurement of Serum Concentrations of Tobramycin
Measure peak and trough serum tobramycin concentrations periodically during therapy to assure adequate concentrations and to avoid potentially toxic concentrations in all patients, especially in patients with renal impairment [see Dosage and Administration (2.6)]. Avoid peak serum concentrations above 12 mcg/mL. Rising trough concentrations (above 2 mcg/mL) may indicate tissue accumulation. Such accumulation may result in ototoxicity and nephrotoxicity [Warnings and Precautions (5.1, 5.2)].
A useful guideline is to measure serum concentrations after 2 or 3 doses, so that the dosage could be adjusted if necessary, and at 3- to 4-day intervals during therapy. In the event of changing renal function, obtain more frequent serum tobramycin concentrations and adjust the dosage or dosage interval according to the guidelines provided [see Dosage and Administration (2.6)].
In order to measure the peak concentration, a serum sample should be drawn about 30 minutes following intravenous infusion or 1 hour after an intramuscular injection. Trough concentrations are measured by obtaining serum samples at 8 hours or just prior to the next dose of tobramycin. These suggested time intervals are intended only as guidelines and may vary according to institutional practices. It is important, however, that there be consistency within the individual patient program unless computerized pharmacokinetic dosing programs are available in the institution. These serum-concentration assays may be especially useful for monitoring the treatment of severely ill patients with changing renal function or of those infected with less susceptible organisms or those receiving maximum dosage.
3 DOSAGE FORMS AND STRENGTHS
Tobramycin for Injection, USP is supplied as a sterile dry powder in a pharmacy bulk package vial containing tobramycin sulfate equivalent to 1.2 g of tobramycin. The contents of the vial should be diluted with 30 mL of Sterile Water for Injection, USP, to provide a solution containing 40 mg of tobramycin per mL.
4 CONTRAINDICATIONS
Tobramycin for Injection is contraindicated in patients with a history of hypersensitivity to tobramycin or any other aminoglycoside [see Warnings and Precautions (5.4)].
5 WARNINGS AND PRECAUTIONS
5.1 Nephrotoxicity
Systemic exposure to Tobramycin for Injection and other aminoglycosides can cause nephrotoxicity, primarily manifested as acute tubular necrosis. Signs of nephrotoxicity include rising blood urea nitrogen (BUN) and creatinine (Cr), decreased urinary output, and sodium, potassium, bicarbonate, magnesium, phosphate and calcium urinary losses. Aminoglycoside-induced nephrotoxicity may occur during therapy but may not become apparent until the first few days after cessation of therapy and usually is reversible. The risk for nephrotoxicity increases with tobramycin accumulation (indicated by rising trough levels above 2 mcg/mL), excessive peak concentrations (above 12 mcg/mL), total cumulative dose, advanced age, volume depletion, concurrent or sequential use of other nephrotoxic drugs and in patients with diabetes. Monitor serum tobramycin concentrations in all patients and avoid peak levels above 12 mcg/mL and trough levels above 2 mcg/mL [see Dosage and Administration (2.9)]. Monitor renal function, serum electrolytes, potassium, sodium, magnesium, calcium and phosphate, urine output and urinalysis during therapy in all patients. Reduce the dose or discontinue treatment if renal impairment occurs.
5.2 Ototoxicity
Ototoxicity with use of Tobramycin for Injection
Tobramycin for Injection can cause both auditory and vestibular eighth nerve damage. The auditory changes are irreversible, are usually bilateral, and may be partial or total. Symptoms of ototoxicity can include dizziness, vertigo, tinnitus, roaring in the ears and hearing loss. Ototoxicity symptoms may manifest during therapy or after tobramycin has been discontinued. The risk of ototoxicity increases with higher peak and trough serum tobramycin concentrations, in patients who receive high doses or prolonged or prior treatment with tobramycin or other aminoglycosides, in patients with renal impairment, patients receiving with other nephrotoxic or ototoxic drugs and in the extremes of age. To decrease the risk of ototoxicity, use as short a duration of therapy as clinically appropriate, adequately hydrate patients, limit the use of other ototoxic drugs, and closely monitor tobramycin concentrations during therapy [see Dosage and Administration (2.9)]. Monitor patients for signs and symptoms of auditory or vestibular toxicity and consider serial audiograms in high-risk patients. Discontinue tobramycin in patients with evidence of auditory or vestibular toxicity.
Risk of Ototoxicity Due to Mitochondrial DNA Variants
Cases of ototoxicity with aminoglycosides have been observed in patients with certain variants in the mitochondrially encoded 12S rRNA gene (MT-RNR1), particularly the m.1555A>G variant. Ototoxicity occurred in some patients even when their aminoglycoside serum levels were within the recommended range. Mitochondrial DNA variants are present in less than 1% of the general US population, and the proportion of the variant carriers who may develop ototoxicity as well as the severity of ototoxicity is unknown. In case of known maternal history of ototoxicity due to aminoglycoside use or a known mitochondrial DNA variant in the patient, consider alternative treatments other than aminoglycosides unless the increased risk of permanent hearing loss is outweighed by the severity of infection and lack of safe and effective alternative therapies.
5.3 Embryo-Fetal Toxicity
Aminoglycosides, including Tobramycin for Injection, can cause fetal harm when administered to a pregnant woman. Aminoglycosides cross the placenta. Streptomycin, another aminoglycoside, has been associated with several reports of total, irreversible, bilateral congenital deafness in pediatric patients whose mothers received streptomycin during pregnancy. Apprise patients of potential hazard to the fetus if Tobramycin for Injection is used during pregnancy or if the patient becomes pregnant while taking Tobramycin for Injection [see Use in Specific Populations (8.1)].
5.4 Allergic Reactions
Serious and fatal allergic reactions including anaphylaxis and dermatologic reactions including exfoliative dermatitis, toxic epidermal necrolysis, erythema multiforme, and Stevens-Johnson Syndrome have been reported in patients on tobramycin therapy [see Contraindications (4) and Adverse Reactions (6)].
If an allergic reaction occurs, discontinue Tobramycin for Injection and institute appropriate therapy. A history of hypersensitivity to other aminoglycosides is a contraindication to the use of Tobramycin for Injection, because cross-allergenicity among aminoglycosides has been demonstrated [see Contraindications (4)].
5.5 Neuromuscular Blockade and Other Neurologic Adverse Reactions
Neuromuscular blockade with respiratory paralysis and respiratory failure may occur following administration of aminoglycosides. Neuromuscular blockade, respiratory failure, and prolonged respiratory paralysis may occur more commonly and be more severe in patients with myasthenia gravis or Parkinson's disease and in patients concomitantly receiving neuromuscular blocking agents such as succinylcholine. If neuromuscular blockade occurs following the administration of Tobramycin for Injection, it may be reversed by the administration of calcium salts but mechanical assistance may be necessary. Other manifestations of neurotoxicity may include numbness, skin tingling, muscle twitching, and convulsions.
5.6 Clostridioides difficile-Associated Diarrhea (CDAD)
Clostridioides difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Tobramycin for Injection, USP, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antibacterial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.7 Risk of Development of Drug-Resistant Bacteria
Prescribing Tobramycin for Injection, USP in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
5.8 Macular Necrosis
Tobramycin for Injection is not approved for intraocular and/or subconjunctival use. Macular necrosis has been reported following intraocular and/ or subconjunctival administration of aminoglycosides, including tobramycin.
5.9 Inactivation by Beta-Lactam Antibacterials
The inactivation of tobramycin and other aminoglycosides by ß-lactam-type antibacterials (penicillins, cephalosporins) has been demonstrated in vitro and in patients with severe renal impairment. Such inactivation has not been found in patients with normal renal function who have been given the drugs by separate routes of administration.
6 ADVERSE REACTIONS
The following serious adverse reactions are described below and elsewhere in the labeling:
- Nephrotoxicity [see Boxed Warning and Warnings and Precautions (5.1)]
- Ototoxicity [see Boxed Warning and Warnings and Precautions (5.2)]
- Embryo-Fetal Toxicity [see Boxed Warning and Warnings and Precautions (5.3)]
- Allergic Reactions [see Warnings and Precautions (5.4)]
- Neuromuscular Blockade [see Warnings and Precautions (5.5)]
The following adverse reactions associated with the use of Tobramycin for Injection were identified in clinical studies or postmarketing reports. Because some of these reactions were reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System Disorders: anemia, granulocytopenia, leukopenia, leukocytosis, eosinophilia and thrombocytopenia
Ear and Labyrinth Disorders: Tinnitus, hearing loss, vertigo
Gastrointestinal Disorders: nausea, vomiting, diarrhea
General Disorders and Administration Site Conditions: fever, lethargy, pain at the injection site
Immune system disorders: Anaphylaxis, hypersensitivity reactions
Laboratory Investigations: elevated blood urea nitrogen, elevated serum creatinine, hyponatremia, hypokalemia, hypomagnesemia, hypocalcemia, hypophosphatemia, urinary casts, increased serum transaminases (AST, ALT); increased serum LDH and bilirubin
Nervous System Disorders: headache, numbness, paresthesia, muscle twitching, convulsions, mental confusion, and disorientation
Skin and Subcutaneous Tissue Disorders: rash, itching, urticaria
7 DRUG INTERACTIONS
7.1 Drugs with Nephrotoxic or Ototoxic Potential
Avoid concurrent and/or sequential use of Tobramycin for Injection with other drugs with nephrotoxic and/or ototoxic potential.
7.2 Diuretics
Some diuretics can enhance aminoglycoside toxicity by altering concentrations in serum and tissue and causing dehydration. Monitor serum concentrations, renal function, serum electrolytes, sodium, magnesium, calcium and phosphate, urine output and urinalysis, and signs of auditory or vestibular toxicity in patients concomitantly administered diuretics.
7.3 Drugs with Neuromuscular Blockade or Neurotoxic Potential
Prolonged respiratory paralysis may occur in patients concomitantly receiving neuromuscular blocking agents with Tobramycin for Injection [see Boxed Warning, Warnings and Precautions (5.5)]. If neuromuscular blockade occurs, it may be reversed by the administration of calcium salts but mechanical assistance may be necessary. In addition, avoid concurrent and/or sequential use of Tobramycin for Injection with other neurotoxic drugs.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Aminoglycosides, including Tobramycin for Injection, can cause fetal harm when administered to a pregnant woman. Published literature reports that use of streptomycin, an aminoglycoside, can cause total, irreversible, bilateral congenital deafness when administered to a pregnant woman [see Warnings and Precautions (5.3)]. In animal reproduction studies with subcutaneous administration of tobramycin in pregnant rats and rabbits during organogenesis, there were no adverse developmental outcomes at doses up to 3.2 times and 1.3 times the maximum recommended clinical dose based on body surface area; however, ototoxicity was not evaluated in the offspring from these studies (see Data). Advise pregnant women of the potential risk to a fetus.
The estimated background risk of major birth defects and miscarriage for the indicated populations are unknown. All pregnancies have a background risk of birth defects, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20% respectively.
Data
Animal Data
Subcutaneous administration of tobramycin at doses of up to 100 mg/kg/day (rat) or 20 mg/kg/day (rabbit) during organogenesis was not associated with adverse developmental outcomes. These doses are 3.2 and 1.3 times the maximum recommended clinical daily dose of 5 mg/kg based on body surface area. Doses of tobramycin ≥40 mg/kg/day were maternally toxic to rabbits and precluded the evaluation of adverse developmental outcomes. Ototoxicity was not evaluated in offspring during nonclinical reproductive toxicity studies with tobramycin.
8.2 Lactation
Risk Summary
Limited published data with Tobramycin for Injection in lactating women indicate that tobramycin is present in human milk. There are no data on the effects of Tobramycin for Injection on milk production. Tobramycin may cause alteration in the intestinal flora of the breastfeeding infant. Advise a woman to monitor the breastfed infant for loose or bloody stools and candidiasis (thrush, diaper rash).
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Tobramycin for Injection and any potential adverse effects on the breastfed infant from Tobramycin for Injection or from the underlying maternal condition.
8.4 Pediatric Use
Use Tobramycin for Injection with caution in premature infants and neonates because of their renal immaturity and the resulting prolongation of serum half-life. For pediatric dosing information [see Dosage and Administration (2.3)]. Similar to adults, monitor renal function and serum tobramycin concentrations in pediatric patients receiving Tobramycin for Injection.
8.5 Geriatric Use
Elderly patients may be at a higher risk of developing nephrotoxicity and ototoxicity while receiving Tobramycin for Injection [see Warnings and Precautions (5.1)].
Tobramycin is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function and serum tobramycin levels [see Dosage and Administration (2.6) and Warnings and Precautions (5.1)].
8.6 Patients with Renal Impairment
The dosage schedule of Tobramycin for Injection should be adjusted according to the degree of renal impairment and serum concentration [see Dosage and Administration (2.6)]. In patients undergoing hemodialysis, 25% to 70% of the administered dose may be removed, depending on the duration and type of dialysis.
10 OVERDOSAGE
10.1 Signs and Symptoms
Acute overdosage with Tobramycin for Injection can result in more severe manifestations of the types of toxicities known to occur with recommended doses, e.g., renal damage, ototoxicity, neuromuscular blockade. The severity of the signs and symptoms following a tobramycin overdose are dependent on the dose administered, the patient's renal function, state of hydration, age and whether or not other medications with similar toxicities are being administered concurrently. [see Warnings and Precautions (5.1, 5.2, 5.5)] for signs and symptoms related to neurotoxicity, nephrotoxicity and neuromuscular blockade; and Adverse Reactions (6)].
If tobramycin were ingested, toxicity would be less likely because aminoglycosides are minimally absorbed from an intact gastrointestinal tract.
10.2 Treatment
In all cases of suspected overdosage with Tobramycin for Injection, call your Regional Poison Control Center or the National Poison Control center at 1-800-222-1222 or www.poison.org to obtain the most up-to-date information about the treatment of overdose. This recommendation is made because, in general, information regarding the treatment of overdosage may change more rapidly than the package insert.
Management of Tobramycin for Injection overdosage is symptomatic and supportive. Maintain airway, provide adequate hydration and monitor renal function, serum electrolytes, and tobramycin concentrations until the serum tobramycin level falls below 2 mcg/mL.
Tobramycin is removed by hemodialysis.
11 DESCRIPTION
Tobramycin sulfate, a water-soluble aminoglycoside antibacterial, drug derived from the actinomycete Streptomyces tenebrarius. Tobramycin for Injection, USP is supplied as a sterile powder in a pharmacy bulk package vial for intravenous use. It is intended for reconstitution with 30 mL of Sterile Water for Injection, USP. Each vial contains tobramycin sulfate equivalent to 1.2 g of tobramycin. After reconstitution, the solution will contain 40 mg of tobramycin per mL. The product contains no preservative or sodium bisulfite.
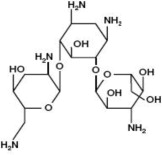
Tobramycin sulfate is O-3-amino-3-deoxy-α-D-glucopyranosyl-(1→4)-O-[2,6-diamino-2,3,6-trideoxy-α-D-ribo-hexopyranosyl-(1→6)]-2-deoxy-L-streptamine, sulfate (2:5)(salt) and has the molecular formula (C18H37N5O9)2•5H2SO4. The molecular weight is 1425.42 g/mol. The molecular weight of the free base is 467.51 g/mol. The structural formula of tobramycin, free base, is as follows:
Figure 2: Tobramycin Structure
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Tobramycin sulfate is an aminoglycoside antibacterial drug [see Microbiology (12.4)].
12.3 Pharmacokinetics
In patients with normal renal function, except neonates, tobramycin administered every 8 hours does not accumulate in serum. The serum elimination half-life in patients with normal renal function is 2 hours. However, in patients with renal impairment and in neonates, serum concentrations of the antibacterial are usually higher and can be measured for longer periods of time than in adults with normal renal function. Thus, the dosage of Tobramycin for Injection for patients with renal impairment and neonates must be adjusted accordingly [see Dosage and Administration (2.3, 2.6)].
Absorption
Following intramuscular administration, peak serum concentrations of tobramycin occur between 30 and 90 minutes. Following an intramuscular dose of 1 mg/kg of body weight, maximum serum concentrations reach about 4 mcg/mL, and measurable concentrations persist for as long as 8 hours. Therapeutic serum concentrations are generally considered to range from 4 to 6 mcg/mL. When Tobramycin for Injection is administered by intravenous infusion over a 1-hour period, the serum concentrations are similar to those obtained by intramuscular administration. Tobramycin is poorly absorbed from the gastrointestinal tract.
Distribution
Based on ultrafiltration studies, practically no serum protein binding of tobramycin occurs.
Tobramycin can be detected in tissues and body fluids after parenteral administration. Concentrations of tobramycin in bile and stools ordinarily have been low, which suggests minimal biliary excretion. The concentration of tobramycin in cerebrospinal fluid following parenteral administration is low, and concentrations are dependent on dose, rate of penetration, and degree of meningeal inflammation. Tobramycin has also been detected in sputum, peritoneal fluid, synovial fluid, and abscess fluids, and it crosses the placental membranes. Concentrations in the renal cortex are several times higher than serum concentrations.
Metabolism
Following parenteral administration, minimal, metabolic transformation occurs, and tobramycin is eliminated almost exclusively by glomerular filtration.
Excretion
Peak urine concentrations ranging from 75 to 100 mcg/mL have been observed following the intramuscular injection of a single dose of 1 mg/kg. After several days of treatment, the amount of tobramycin excreted in the urine approaches the daily dose administered. Renal clearance is similar to that of endogenous creatinine. In patients with normal renal function, up to 84% of the dose is recoverable from the urine in 8 hours and up to 93% in 24 hours. When renal function is impaired, excretion of tobramycin is slowed, and accumulation of the drug may cause toxic blood concentrations.
12.4 Microbiology
Mechanism of Action
Tobramycin is an aminoglycoside that inhibits protein synthesis by binding to the aminoacyl site (A) of the 16S RNA within the bacterial 30S ribosomal subunit. Tobramycin is bactericidal against susceptible bacteria.
Resistance
Resistance to aminoglycosides includes production of aminoglycoside modifying enzymes (AMEs), alteration of the ribosomal target through production of 16S rRNA methyltransferases, up-regulation of efflux pumps and reduced permeability into bacterial cell due to loss of outer membrane porins. Aminoglycosides are generally not active against most gram-positive organisms, including Streptococcus pyogenes, Streptococcus pneumoniae, and enterococci. Cross-resistance between aminoglycosides may occur.
Interaction with Other Antimicrobials
In vitro studies have shown that an aminoglycoside combined with an antibacterial that interferes with cell-wall synthesis, such as penicillin, results in a synergistic bactericidal effect in some isolates of Enterococcus faecalis. This combination is not synergistic against other closely related organisms, e.g., Enterococcus faecium. Species-level identification of enterococci alone cannot be used to predict susceptibility. Susceptibility testing and tests for antibacterial synergism must be performed.
Antimicrobial Activity
Tobramycin has been shown to be active against most isolates of the following bacteria both in vitro and in clinical infections [see Indications and Usage (1)]:
Gram-positive bacteria
Staphylococcus aureus
Gram-negative bacteria
Citrobacter species
Enterobacter species
Escherichia coli
Klebsiella species
Morganella morganii
Pseudomonas aeruginosa
Proteus mirabilis
Proteus vulgaris
Providencia species
Serratia species
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies in animals have not been conducted with Tobramycin for Injection.
Mutagenesis
Tobramycin has been evaluated for genotoxicity in a battery of in vitro and in vivo tests. The Ames bacterial reversion test, conducted with 5 tester strains, failed to show a significant increase in revertants with or without metabolic activation in all strains. Tobramycin was negative in the mouse lymphoma forward mutation assay, did not induce chromosomal aberrations in Chinese hamster ovary cells, and was negative in the mouse micronucleus test.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Tobramycin for Injection, USP is supplied as a sterile dry powder containing tobramycin sulfate equivalent to 1.2 g tobramycin in a 50 mL Pharmacy Bulk Package Vial packaged in trays of 6.
| Product Code | Unit of Sale | Strength | Each |
| NP300351 | NDC 63323-303-55 Unit of 6 | 1.2 g in 50 mL | NDC 63323-303-21 50 mL Pharmacy Bulk Package Vial |
Vial stoppers do not contain natural rubber latex.
16.2 Storage and Handling
Prior to reconstitution, the vial should be stored at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature]. After reconstitution, the solution should be kept in a refrigerator and used within 96 hours. If kept at room temperature, the solution must be used within 24 hours [see Dosage and Administration (2.1, 2.8)].
17 PATIENT COUNSELING INFORMATION
Serious Allergic Reactions
Advise patients that serious allergic reactions could occur with Tobramycin for Injection. Advise patients to report fever, swelling, difficulty breathing, wheezing, decrease blood pressure or dizziness, or skin rash. If an allergic reaction occurs, discontinue the drug and institute appropriate therapy immediately.
Impairment of Kidney Function
Advise patients that Tobramycin for Injection may cause impairment in kidney function and that periodic blood draws are required to monitor kidney function and tobramycin drug levels.
Hearing Loss and Impaired Balance
Advise patients that Tobramycin for Injection may cause serious and irreversible hearing loss and impaired balance. Advise patients to report hearing loss, ringing or roaring in the ears, dizziness or imbalance.
Antibacterial Resistance
Counsel patients that antibacterial drugs, including Tobramycin for Injection should be used to treat bacterial infections only. They do not treat viral infections (e.g., the common cold). When Tobramycin for Injection is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be administered exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Tobramycin for Injection or other antibacterial drugs in the future.
Diarrhea
Counsel patients that diarrhea is a common problem caused by antibacterials, and it usually ends when the antibacterial is discontinued. Sometimes after starting treatment with antibacterials, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as 2 or more months after having taken their last dose of the antibacterial. If this occurs, patients should contact their physician as soon as possible.
Embryofetal Toxicity
Advise pregnant women that aminoglycosides, including Tobramycin for Injection, can cause irreversible congenital deafness when administered to a pregnant woman [see Warnings and Precautions (5.3) and Use in Specific Populations (8.1)].
Lactation
Advise a woman to monitor their breastfed infants for diarrhea and/or bloody stools [see Use in Specific Populations (8.2)].
Novaplus is a registered trademark of Vizient, Inc.
Manufactured by:
Fresenius Kabi
Lake Zurich, IL 60047
www.fresenius-kabi.com/us
451027D