SPL UNCLASSIFIED
FOR INTRAVENOUS USE ONLY. NOT FOR DIRECT INTRAVENOUS INJECTION. NITROGLYCERIN INJECTION MUST BE DILUTED IN DEXTROSE (5%) INJECTION OR SODIUM CHLORIDE (0.9%) INJECTION PRIOR TO ITS INFUSION (SEE DOSAGE & ADMINISTRATION SECTION). THE ADMINISTRATION SET USED FOR INFUSION WILL AFFECT THE AMOUNT OF NITROGLYCERIN INJECTION DELIVERED TO THE PATIENT. (SEE WARNINGS, AND DOSAGE & ADMINISTRATION SECTIONS).
CAUTIONS
SEVERAL PREPARATIONS OF NITROGLYCERIN FOR INJECTION ARE AVAILABLE. THEY DIFFER IN CONCENTRATION AND/OR VOLUME PER VIAL. WHEN SWITCHING FROM ONE PRODUCT TO ANOTHER, ATTENTION MUST BE PAID TO THE DILUTION AND DOSAGE AND ADMINISTRATION INSTRUCTIONS.
DESCRIPTION
Nitroglycerin is 1,2,3-propanetriol trinitrate, an organic nitrate whose structural formula is:
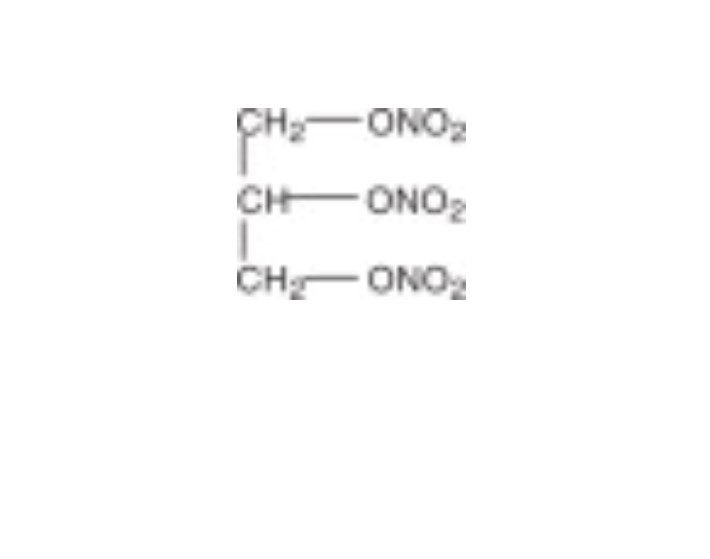
whose empiric formula is C3H5N3O9, and whose molecular weight is 227.09. The organic nitrates are vasodilators, active on both arteries and veins.
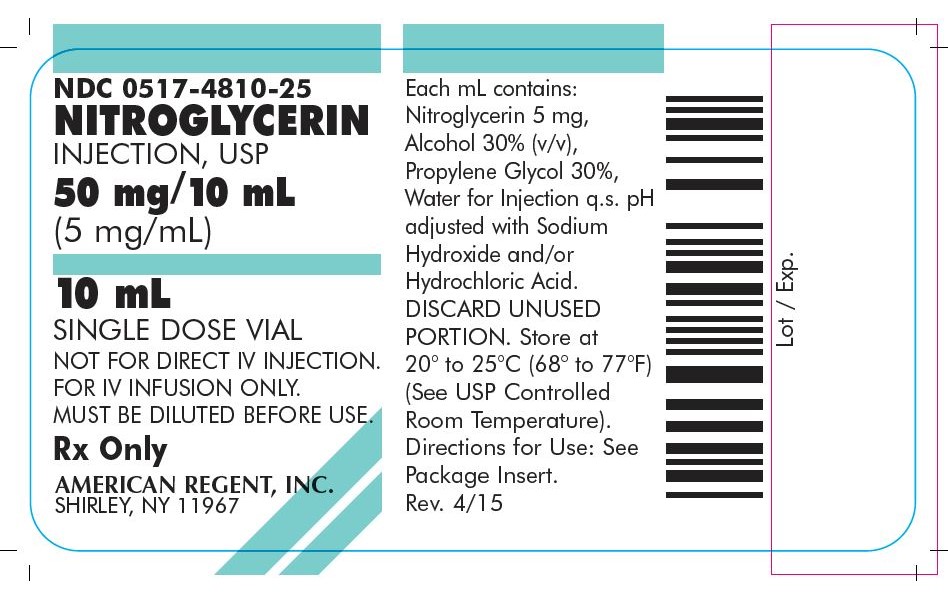
Nitroglycerin Injection, USP is a clear, practically colorless additive solution for intravenous infusion after dilution. Each mL contains: Nitroglycerin 5 mg, Alcohol 30% (v/v), Propylene Glycol 30%, and Water for Injection q.s. pH (range 3.0 to 6.5) may have been adjusted with Sodium Hydroxide and/or Hydrochloric Acid.
The solution is sterile, non-pyrogenic, and nonexplosive.
CLINICAL PHARMACOLOGY
The principal pharmacological action of Nitroglycerin Injection is relaxation of vascular smooth muscle and consequent dilatation of peripheral arteries and veins, especially the latter. Dilatation of the veins promotes peripheral pooling of blood and decreases venous return to the heart, thereby reducing left ventricular end-diastolic pressure and pulmonary capillary wedge pressure (preload). Arteriolar relaxation reduces systemic vascular resistance, systolic arterial pressure, and mean arterial pressure (afterload). Dilatation of the coronary arteries also occurs. The relative importance of preload reduction, afterload reduction, and coronary dilatation remains undefined.
Dosing regimens for most chronically used drugs are designed to provide plasma concentrations that are continuously greater than a minimally effective concentration. This strategy is inappropriate for organic nitrates. Several well-controlled clinical trials have used exercise testing to assess the anti-anginal efficacy of continuously-delivered nitrates. In the large majority of these trials, active agents were indistinguishable from placebo after 24 hours (or less) of continuous therapy. Attempts to overcome nitrate tolerance by dose escalation, even to doses far in excess of those used acutely, have consistently failed. Only after nitrates have been absent from the body for several hours has their anti-anginal efficacy been restored.
Pharmacokinetics:
The volume of distribution of nitroglycerin is about 3 L/kg, and nitroglycerin is cleared from this volume at extremely rapid rates, with a resulting serum half-life of about 3 minutes. The observed clearance rates (close to 1 L/kg/min) greatly exceed hepatic blood flow; known sites of extrahepatic metabolism include red blood cells and vascular walls.
The first products in the metabolism of nitroglycerin are inorganic nitrate and the 1,2- and 1,3- dinitroglycerols. The dinitrates are less effective vasodilators than nitroglycerin, but they are longer-lived in the serum, and their net contribution to the overall effect of chronic nitroglycerin regimens is not known. The dinitrates are further metabolized to (non-vasoactive) mononitrates and, ultimately, to glycerol and carbon dioxide.
To avoid development of tolerance to nitroglycerin, drug-free intervals of 10-12 hours are known to be sufficient; shorter intervals have not been well studied. In one well-controlled clinical trial, subjects receiving nitroglycerin appeared to exhibit a rebound or withdrawal effect, so that their exercise tolerance at the end of the daily drug-free interval was less than that exhibited by the parallel group receiving placebo.
Clinical Trials:
Blinded, placebo-controlled trials of intravenous nitroglycerin have not been reported, but multiple investigators have reported open-label studies, and there are scattered reports of studies in which intravenous nitroglycerin was tested in blinded fashion against sodium nitroprusside.
In each of these studies, therapeutic doses of intravenous nitroglycerin were found to reduce systolic and diastolic arterial blood pressure. The heart rate was usually increased, presumably as a reflexive response to the fall in blood pressure. Coronary perfusion pressure was usually, but not always, maintained.
Intravenous nitroglycerin reduced central venous pressure (CVP), right atrial pressure (RAP), pulmonary arterial pressure (PAP), pulmonary-capillary wedge pressure (PCWP), pulmonary vascular resistance (PVR), and systemic vascular resistance (SVR). When these parameters were elevated, reducing them toward normal usually caused a rise in cardiac output. Conversely, intravenous nitroglycerin usually reduced cardiac output when it was given to patients whose CVP, RAP, PAP, PCWP, PVR, AND SVR were all normal.
Most clinical trials of intravenous nitroglycerin have been brief; they have typically followed hemodynamic parameters during a single surgical procedure. In one careful study, one of the few that lasted more than a few hours, continuous intravenous nitroglycerin had lost almost all of its hemodynamic effect after 48 hours. In the same study, patients who received nitroglycerin infusions for only 12 hours out of each 24 demonstrated no similar attenuation of effect. These results are consistent with those seen in multiple large, double-blind, placebo-controlled trials of other formulations of nitroglycerin and other nitrates.
INDICATIONS & USAGE
Nitroglycerin Injection is indicated for treatment of peri-operative hypertension; for control of congestive heart failure in the setting of acute myocardial infarction; for treatment of angina pectoris in patients who have not responded to sublingual nitroglycerin and β-blockers; and for induction of intraoperative hypotension.
CONTRAINDICATIONS
Allergic reactions to organic nitrates are extremely rare, but they do occur. Nitroglycerin Injection is contraindicated in patients who are allergic to it.
In patients with pericardial tamponade, restrictive cardiomyopathy, or constrictive pericarditis, cardiac output is dependent upon venous return. Intravenous nitroglycerin is contraindicated in patients with these conditions.
WARNINGS
Amplification of the vasodilatory effects of nitroglycerin by sildenafil can result in severe hypotension. The time course and dose dependence of this interaction have not been studied. Appropriate supportive care has not been studied, but it seems reasonable to treat this as a nitrate overdose, with elevation of the extremities and with volume expansion.
Nitroglycerin readily migrates into many plastics, including the polyvinyl chloride (PVC) plastics commonly used for intravenous administration sets. Nitroglycerin absorption by PVC tubing is increased when the tubing is long, the flow rates are low, and the nitroglycerin concentration of the solution is high. The delivered fraction of the solution's original nitroglycerin content has been 20-60% in published studies using PVC tubing; the fraction varies with time during a single infusion, and no simple correction factor can be used. PVC tubing has been used in most published studies of intravenous nitroglycerin, but the reported doses have been calculated by simply multiplying the flow rate of the solution by the solution's original concentration of nitroglycerin. The actual doses delivered have been less, sometimes much less, than those reported.
Some in-line intravenous filters also absorb nitroglycerin; these filters should be avoided.
Because of the problem of nitroglycerin absorption by polyvinyl chloride (PVC) tubing, Nitroglycerin Injection should be used with the least absorptive infusion tubing (i.e., non-PVC tubing) available.
DOSING INSTRUCTIONS MUST BE FOLLOWED WITH CARE. WHEN THE APPROPRIATE INFUSION SETS ARE USED, THE CALCULATED DOSE WILL BE DELIVERED TO THE PATIENT, BECAUSE THE LOSS OF NITROGLYCERIN INJECTION SEEN WITH STANDARD PVC TUBING WILL BE AVOIDED. THE DOSAGES REPORTED IN PUBLISHED STUDIES UTILIZED GENERAL-USE PVC ADMINISTRATION SETS, AND RECOMMENDED DOSES BASED ON THIS EXPERIENCE WILL BE TOO HIGH WHEN THE LOW-ABSORBING INFUSION SETS ARE USED.
PRECAUTIONS
General:
Severe hypotension and shock may occur with even small doses of nitroglycerin. This drug should therefore be used with caution in patients who may be volume depleted or who, for whatever reason, are already hypotensive. Hypotension induced by nitroglycerin may be accompanied by paradoxical bradycardia and increased angina pectoris.
Nitrate therapy may aggravate the angina caused by hypertrophic cardiomyopathy.
As tolerance to other forms of nitroglycerin develops, the effect of sublingual nitroglycerin on exercise tolerance, although still observable, is somewhat blunted.
In industrial workers who have had long-term exposure to unknown (presumably high) doses of organic nitrates, tolerance clearly occurs. Chest pain, acute myocardial infarction, and even sudden death have occurred during temporary withdrawal of nitrates from these workers, demonstrating the existence of true physical dependence.
Some clinical trials in angina patients have provided nitroglycerin for about 12 continuous hours of every 24- hour day. During the nitrate-free intervals in some of these trials, anginal attacks have been more easily provoked than before treatment, and patients have demonstrated hemodynamic rebound and decreased exercise tolerance. The importance of these observations to the routine, clinical use of intravenous nitroglycerin is not known.
Lower concentrations of nitroglycerin increase the potential precision of dosing, but these concentrations increase the total fluid volume that must be delivered to the patient. Total fluid load may be a dominant consideration in patients with compromised function of the heart, liver, and/or kidneys.
Nitroglycerin infusions should be administered only via a pump that can maintain a constant infusion rate.
Intracoronary injection of nitroglycerin infusions has not been studied.
Laboratory Tests:
Because of the propylene glycol content of intravenous nitroglycerin, serum triglyceride assays that rely on glycerol oxidase may give falsely elevated results in patients receiving this medication.
Drug Interactions:
The vasodilating effects of nitroglycerin may be additive with those of other vasodilators.
Administration of nitroglycerin infusions through the same infusion set as blood can result in pseudoagglutination and hemolysis. More generally, nitroglycerin in 5% dextrose or sodium chloride 0.9% should not be mixed with any other medication of any kind.
Intravenous nitroglycerin interferes, at least in some patients, with the anticoagulant effect of heparin. In patients receiving intravenous nitroglycerin, concomitant heparin therapy should be guided by frequent measurement of the activated partial thromboplastin time.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
Animal carcinogenesis studies with injectable nitroglycerin have not been performed.
Rats receiving up to 434 mg/kg/day of dietary nitroglycerin for 2 years developed dose-related fibrotic and neoplastic changes in liver, including carcinomas, and interstitial cell tumors in testes. At high doses, the incidences of hepatocellular carcinomas in both sexes were 52% vs. 0% in controls, and incidences of testicular tumors were 52% vs. 8% in controls. Lifetime dietary administration of up to 1058 mg/kg/day of nitroglycerin was not tumorigenic in mice.
Nitroglycerin was weakly mutagenic in Ames tests performed in two different laboratories. There was no evidence of mutagenicity in an in vivo dominant lethal assay with male rats treated with doses up to about 363 mg/kg/day, p.o., or in in vitro cytogenetic tests in rat and dog tissues.
In a three-generation reproduction study, rats received dietary nitroglycerin at doses up to about 434 mg/kg/day for six months prior to mating of the F0 generation with treatment continuing through successive F1 and F2 generations. The high-dose was associated with decreased feed intake and body weight gain in both sexes at all matings. No specific effect on the fertility of the F0 generation was seen. Infertility noted in subsequent generations, however, was attributed to increased interstitial cell tissue and aspermatogenesis in the high dose males. In this three-generation study there was no clear evidence of teratogenicity.
Pregnancy: Pregnancy Category C:
Animal teratology studies have not been conducted with nitroglycerin injection. Teratology studies in rats and rabbits, however, were conducted with topically applied nitroglycerin ointment at doses up to 80 mg/kg/day and 240 mg/kg/day, respectively. No toxic effects on dams or fetuses were seen at any dose tested. There are no adequate and well-controlled studies in pregnant women. Nitroglycerin should be given to a pregnant woman only if clearly needed.
Nursing Mothers:
It is not known whether nitroglycerin is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when nitroglycerin is administered to a nursing woman.
Pediatric Use:
Safety and effectiveness in children have not been established.
ADVERSE REACTIONS
Adverse reactions to nitroglycerin are generally dose-related and almost all of these reactions are the result of nitroglycerin's activity as a vasodilator. Headache, which may be severe, is the most commonly reported side effect. Headache may be recurrent with each daily dose, especially at higher doses. Transient episodes of lightheadedness, occasionally related to blood pressure changes, may also occur. Hypotension occurs infrequently, but in some patients it may be severe enough to warrant discontinuation of therapy. Syncope, crescendo angina, and rebound hypertension have been reported but are uncommon.
Extremely rarely, ordinary doses of organic nitrates have caused methemoglobinemia in normal-seeming patients. Methemoglobinemia is so infrequent at these doses that further discussion of its diagnosis and treatment is deferred (see OVERDOSAGE).
OVERDOSAGE
Hemodynamic Effects:
The ill effects of nitroglycerin overdose are generally the results of nitroglycerin's capacity to induce vasodilatation, venous pooling, reduced cardiac output, and hypotension. These hemodynamic changes may have protean manifestations, including increased intracranial pressure, with any or all of persistent throbbing headache, confusion, and moderate fever; vertigo; palpitation; visual disturbances; nausea and vomiting (possibly with colic and even bloody diarrhea); syncope (especially in the upright posture); air hunger and dyspnea, later followed by reduced ventilatory effort; diaphoresis, with the skin either flushed or cold and clammy; heart block and bradycardia; paralysis; coma; seizures; and death.
Laboratory determinations of serum levels of nitroglycerin and its metabolites are not widely available, and such determinations have, in any event, no established role in the management of nitroglycerin overdose.
No data are available to suggest physiological maneuvers (e.g., maneuvers to change the pH of the urine) that might accelerate elimination of nitroglycerin and its active metabolites. Similarly, it is not known which-if any-of these substances can usefully be removed from the body by hemodialysis.
No specific antagonist to the vasodilator effects of nitroglycerin is known, and no intervention has been subject to controlled study as a therapy of nitroglycerin overdose. Because the hypotension associated with nitroglycerin overdose is the result of venodilatation and arterial hypovolemia, prudent therapy in this situation should be directed toward increase in central fluid volume. Passive elevation of the patient's legs may be sufficient, but intravenous infusion of normal saline or similar fluid may also be necessary.
The use of epinephrine or other arterial vasoconstrictors in this setting is likely to do more harm than good.
In patients with renal disease or congestive heart failure, therapy resulting in central volume expansion is not without hazard. Treatment of nitroglycerin overdose in these patients may be subtle and difficult, and invasive monitoring may be required.
Methemoglobinemia:
Nitrate ions liberated during metabolism of nitroglycerin can oxidize hemoglobin into methemoglobin. Even in patients totally without cytochrome b5 reductase activity, however, and even assuming that the nitrate moieties of nitroglycerin are quantitatively applied to oxidation of hemoglobin, about 1 mg/kg of nitroglycerin should be required before any of these patients manifests clinically significant (≥10%) methemoglobinemia. In patients with normal reductase function, significant production of methemoglobin should require even larger doses of nitroglycerin. In one study in which 36 patients received 2-4 weeks of continuous nitroglycerin therapy at 3.1 to 4.4 mg/hr, the average methemoglobin level measured was 0.2%; this was comparable to that observed in parallel patients who received placebo.
Notwithstanding these observations, there are case reports of significant methemoglobinemia in association with moderate overdoses of organic nitrates. None of the affected patients had been thought to be unusually susceptible.
Methemoglobin levels are available from most clinical laboratories. The diagnosis should be suspected in patients who exhibit signs of impaired oxygen delivery despite adequate cardiac output and adequate arterial pO2. Classically, methemoglobinemic blood is described as chocolate brown, without color change on exposure to air.
When methemoglobinemia is diagnosed, the treatment of choice is methylene blue, 1-2 mg/kg intravenously.
DOSAGE & ADMINISTRATION
NOT FOR DIRECT INTRAVENOUS INJECTION
NITROGLYCERIN INJECTION IS A CONCENTRATED, POTENT DRUG WHICH MUST BE DILUTED IN DEXTROSE (5%) INJECTION OR SODIUM CHLORIDE (0.9%) INJECTION PRIOR TO ITS INFUSION. NITROGLYCERIN INJECTION SHOULD NOT BE MIXED WITH OTHER DRUGS.
Initial Dilution:
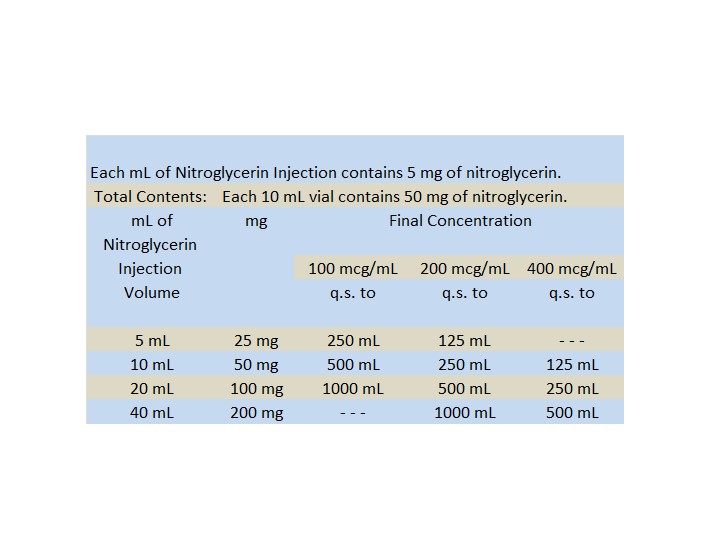
Aseptically transfer the contents of one nitroglycerin vial (50 mg of nitroglycerin) into a 500 mL glass bottle of either Dextrose (5%) Injection or Sodium Chloride Injection (0.9%). This yields a final concentration of 100 mcg/mL. Diluting 5 mg nitroglycerin into 100 mL will yield a final concentration of 50 mcg/mL.
Maintenance Dilution:
It is important to consider the fluid requirements of the patient as well as the expected duration of infusion in selecting the appropriate dilution of Nitroglycerin Injection.
After the initial dosage titration, the concentration of the solution may be increased, if necessary, to limit fluids given to the patient. The nitroglycerin concentration should not exceed 400 mcg/mL. See chart.
Note: If the concentration is adjusted, it is imperative to flush or replace the infusion set before a new concentration is utilized. If the set were not flushed or replaced, it could take minutes to hours, depending upon the flow rate and the dead space of the set, for the new concentration to reach the patient.
Invert the glass parenteral bottle several times to assure uniform dilution of the nitroglycerin.
Dosage is affected by the type of container and administration set used. See WARNINGS.
Although the usual starting adult dose range reported in clinical studies was 25 mcg/min or more, these studies used PVC administration sets. THE USE OF NON-ABSORBING TUBING WILL RESULT IN THE NEED FOR REDUCED DOSES.
If a peristaltic action infusion pump is used, an appropriate administration set should be selected with a drip chamber that delivers approximately 60 microdrops/mL. Table 1 and the Nitroglycerin Injection Dilution Table below may be used to calculate the nitroglycerin dilution and flow rate in microdrops/minute to achieve the desired Nitroglycerin Injection administration rate.
If a volumetric infusion pump is used, an appropriate volumetric infusion pump connector set should be selected. Table 1 below may still be used; however, flow rate will be determined directly by the infusion pump, independent of the drop size of the appropriate set drip chambers. Thus, the reference to ``microdrops/min′′ is not applicable, and the corresponding flow rate in mL/hr should be used to determine pump settings.
When using a non-absorbing infusion set, the initial dosage should be 5 mcg/min delivered through an infusion pump capable of exact and constant delivery of the drug. Subsequent titration must be adjusted to the clinical situation, with dose increments becoming more cautious as partial response is seen. Initial titration should be in 5 mcg/min increments, with increases every 3-5 minutes until some response is noted. If no response is seen at 20 mcg/min, increments of 10 and later 20 mcg/min can be used. Once a partial blood pressure response is observed, the dose increase should be reduced and the interval between increases should be lengthened.
Some patients with normal or low left ventricular filling pressures or pulmonary capillary wedge pressure (e.g., angina patients without other complications) may be hypersensitive to the effects of nitroglycerin and may respond fully to doses as small as 5 mcg/min. These patients require especially careful titration and monitoring.
There is no fixed optimum dose of nitroglycerin. Due to variations in the responsiveness of individual patients to the drug, each patient must be titrated to the desired level of hemodynamic function. Therefore, continuous monitoring of physiologic parameters (i.e., blood pressure and heart rate in all patients, other measurements such as pulmonary capillary wedge pressure, as appropriate) MUST be performed to achieve the correct dose. Adequate systemic blood pressure and coronary perfusion pressure must be maintained.
Dilution:
Nitroglycerin Injection is supplied in 5 mg/mL solution. A dilution and administration scheme for Nitroglycerin Injection is shown in Table 1 below.
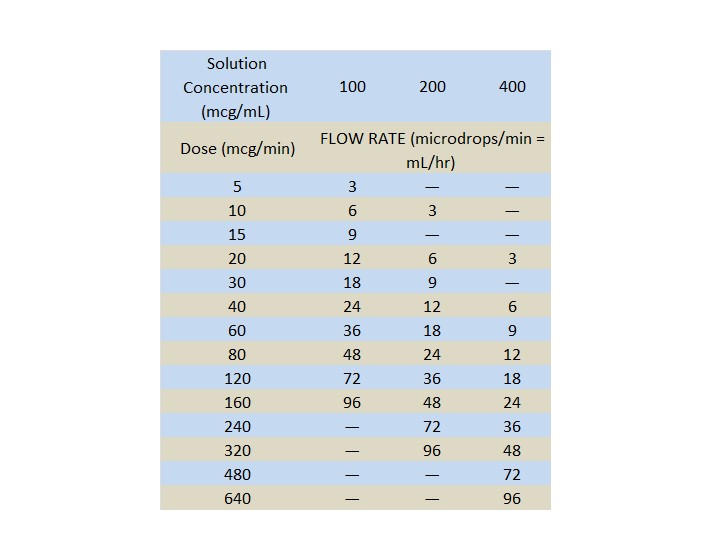
60 MICRODROPS = 1 mL
NITROGLYCERIN INJECTION DILUTION TABLE
(Diluent: Dextrose 5% Injection or Sodium Chloride Injection (0.9%))
NOTE: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit.
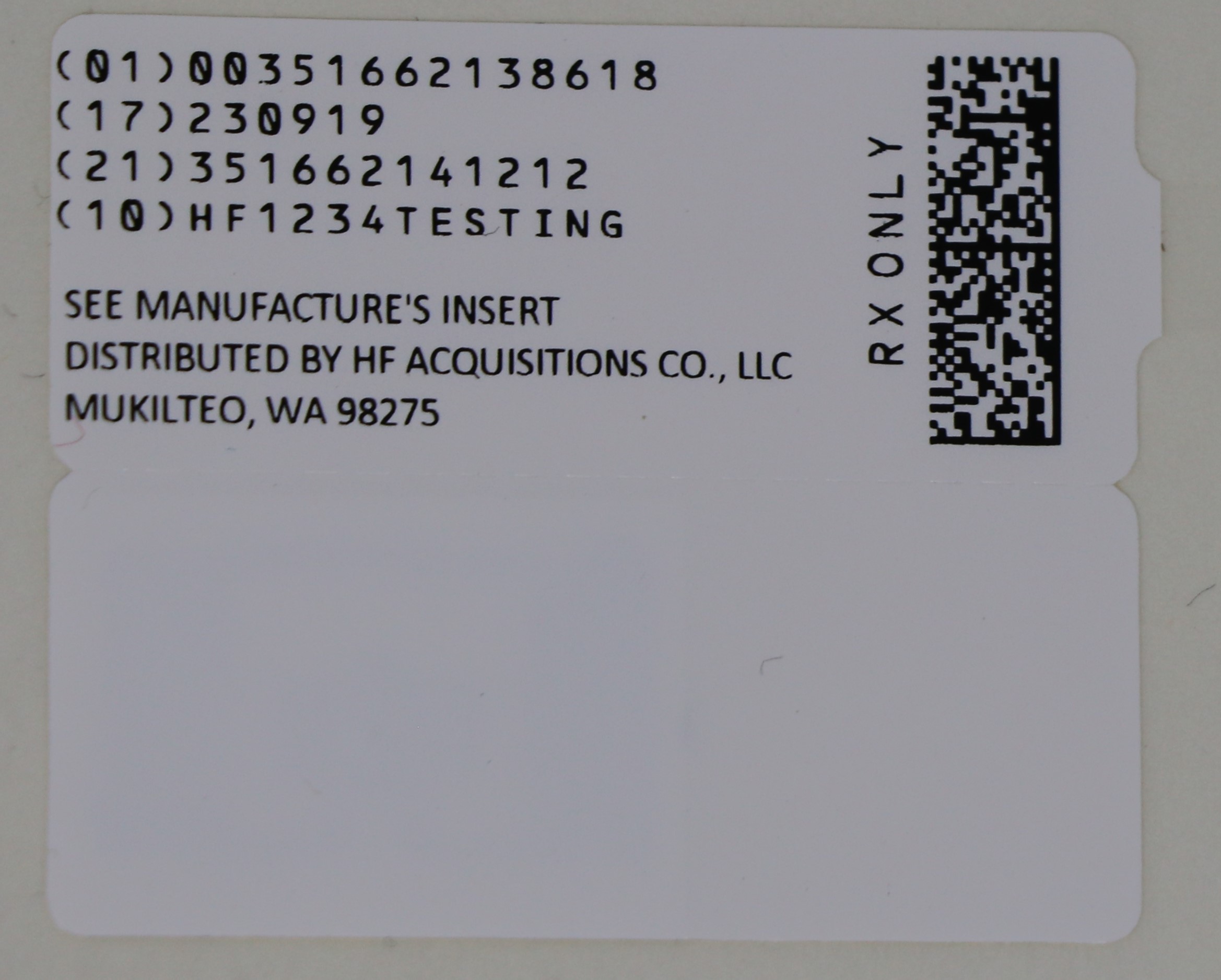
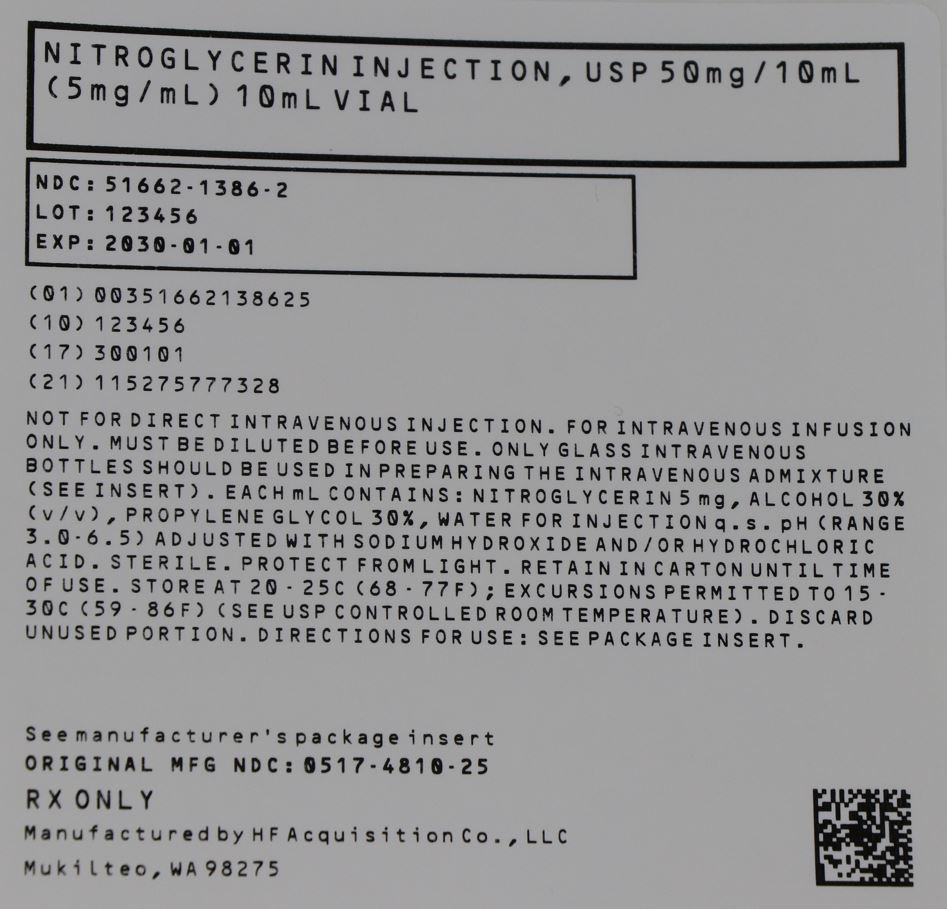
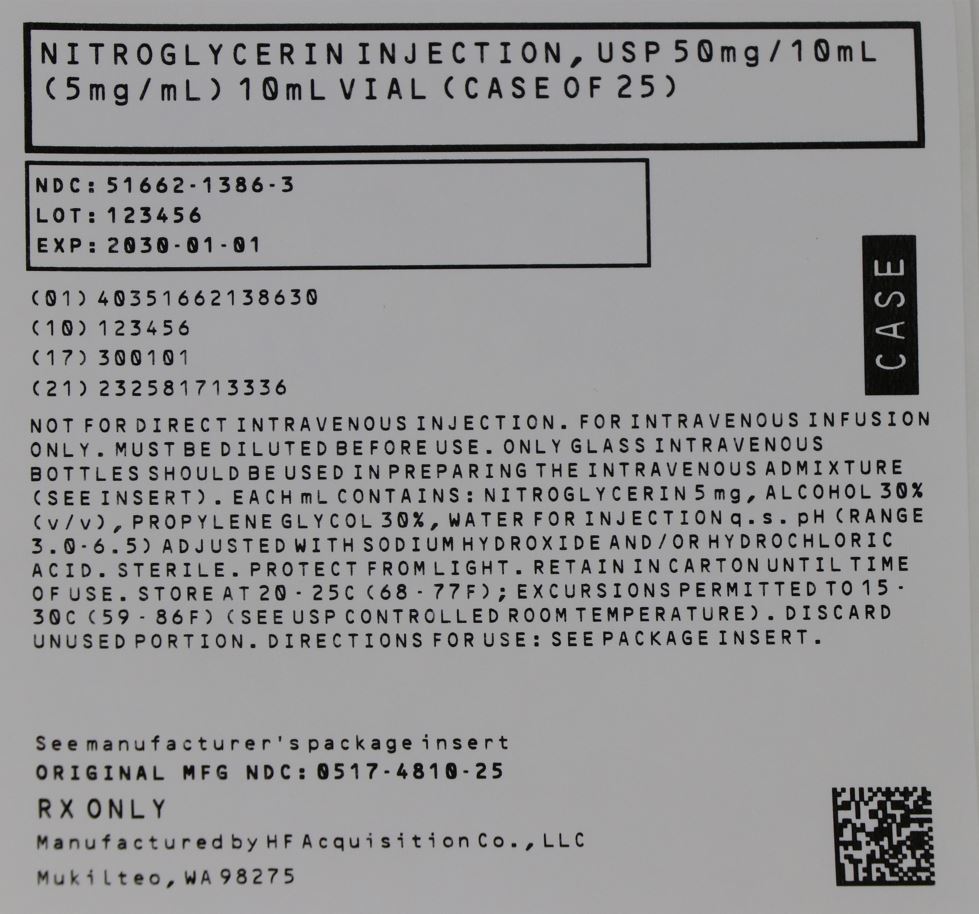
HOW SUPPLIED
NITROGLYCERIN INJECTION, USP is supplied in the following dosage forms.
NDC 51662-1386-1
NITROGLYCERIN INJECTION, USP 50mg/10mL (5mg/mL) 10mL VIAL
HF Acquisition Co LLC, DBA HealthFirst
Mukilteo, WA 98275
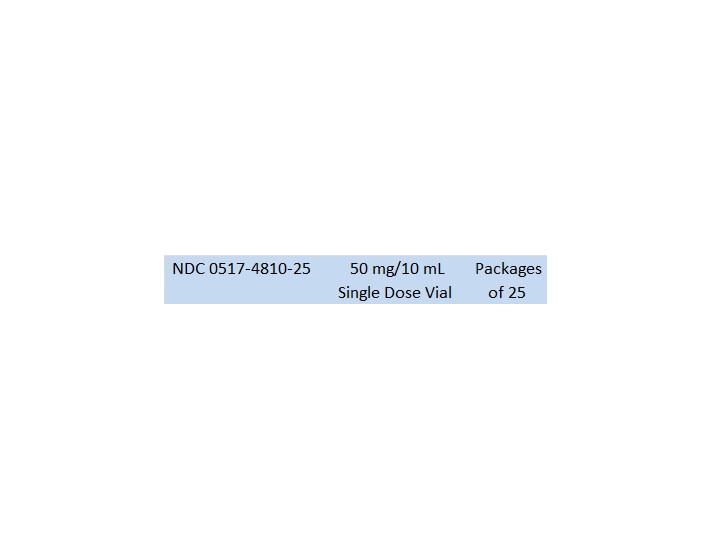
Also supplied in the following manufacture supplied dosage forms
Nitroglycerin Injection, USP, 5 mg/mL is available as follows:
PROTECT FROM LIGHT. RETAIN IN CARTON UNTIL TIME OF USE.
Store at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) (See USP Controlled Room Temperature).
DISCARD UNUSED PORTION.
AMERICAN
REGENT, INC.
SHIRLEY, NY 11967
IN4805
Rev. 11/05
MG #6925