FULL PRESCRIBING INFORMATION
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. INVEGA® (paliperidone) Extended-Release Tablets is not approved for the treatment of patients with dementia-related psychosis. [see Warnings and Precautions (5.1)]
1 INDICATIONS AND USAGE
1.1 Schizophrenia
INVEGA® (paliperidone) Extended-Release Tablets are indicated for the acute and maintenance treatment of schizophrenia [see Clinical Studies (14)].
2 DOSAGE AND ADMINISTRATION
2.1 Schizophrenia
The recommended dose of INVEGA® (paliperidone) Extended-Release Tablets for the treatment of schizophrenia is 6 mg once daily, administered in the morning. Initial dose titration is not required. Although it has not been systematically established that doses above 6 mg have additional benefit, there was a general trend for greater effects with higher doses. This must be weighed against the dose-related increase in adverse reactions. Thus, some patients may benefit from higher doses, up to 12 mg/day, and for some patients, a lower dose of 3 mg/day may be sufficient. Dose increases above 6 mg/day should be made only after clinical reassessment and generally should occur at intervals of more than 5 days. When dose increases are indicated, increments of 3 mg/day are recommended. The maximum recommended dose is 12 mg/day.
In a longer-term study, INVEGA® has been shown to be effective in delaying time to relapse in patients with schizophrenia who were stabilized on INVEGA® for 6 weeks [see Clinical Studies (14)]. INVEGA® should be prescribed at the lowest effective dose for maintaining clinical stability and the physician should periodically reevaluate the long-term usefulness of the drug in individual patients.
2.2 Schizoaffective Disorder
The recommended dose of INVEGA® (paliperidone) Extended-Release Tablets for the treatment of schizoaffective disorder is 6 mg once daily, administered in the morning. Initial dose titration is not required. Some patients may benefit from lower or higher doses within the recommended dose range of 3 to 12 mg once daily. A general trend for greater effects was seen with higher doses. This trend must be weighed against dose-related increase in adverse reactions. Dosage adjustment, if indicated, should occur only after clinical reassessment. Dose increases, if indicated, generally should occur at intervals of more than 4 days. When dose increases are indicated, increments of 3 mg/day are recommended. The maximum recommended dose is 12 mg/day.
2.3 Administration Instructions
INVEGA® can be taken with or without food. Clinical trials establishing the safety and efficacy of INVEGA® were carried out in patients without regard to food intake.
INVEGA® must be swallowed whole with the aid of liquids. Tablets should not be chewed, divided, or crushed. The medication is contained within a nonabsorbable shell designed to release the drug at a controlled rate. The tablet shell, along with insoluble core components, is eliminated from the body; patients should not be concerned if they occasionally notice in their stool something that looks like a tablet.
2.4 Use with Risperidone
Concomitant use of INVEGA® with risperidone has not been studied. Since paliperidone is the major active metabolite of risperidone, consideration should be given to the additive paliperidone exposure if risperidone is coadministered with INVEGA®.
2.5 Dosage in Special Populations
Renal Impairment
Dosing must be individualized according to the patient's renal function status. For patients with mild renal impairment (creatinine clearance ≥ 50 mL/min to < 80 mL/min), the recommended initial dose of INVEGA® is 3 mg once daily. The dose may then be increased to a maximum of 6 mg once daily based on clinical response and tolerability. For patients with moderate to severe renal impairment (creatinine clearance ≥ 10 mL/min to < 50 mL/min), the recommended initial dose of INVEGA® is 1.5 mg once daily, which may be increased to a maximum of 3 mg once daily after clinical reassessment. As INVEGA® has not been studied in patients with creatinine clearance below 10 mL/min, use is not recommended in such patients. [See Clinical Pharmacology (12.3)]
Hepatic Impairment
For patients with mild to moderate hepatic impairment, (Child-Pugh Classification A and B), no dose adjustment is recommended [see Clinical Pharmacology (12.3)]. INVEGA® has not been studied in patients with severe hepatic impairment.
Elderly
Because elderly patients may have diminished renal function, dose adjustments may be required according to their renal function status. In general, recommended dosing for elderly patients with normal renal function is the same as for younger adult patients with normal renal function. For patients with moderate to severe renal impairment (creatinine clearance 10 mL/min to < 50 mL/min), the maximum recommended dose of INVEGA® is 3 mg once daily [see Renal Impairment above].
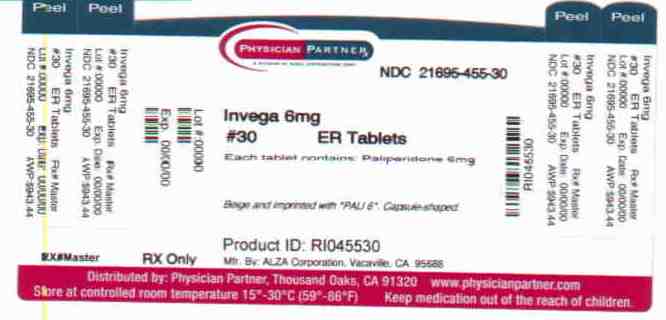
3 DOSAGE FORMS AND STRENGTHS
INVEGA® Extended-Release Tablets are available in the following strengths and colors: 1.5 mg (orange-brown), 3 mg (white), 6 mg (beige), and 9 mg (pink). All tablets are capsule shaped and are imprinted with either "PAL 1.5", "PAL 3", "PAL 6", or "PAL 9".
4 CONTRAINDICATIONS
Hypersensitivity reactions, including anaphylactic reactions and angioedema, have been observed in patients treated with risperidone and paliperidone. INVEGA® (paliperidone) is a metabolite of risperidone and is therefore contraindicated in patients with a known hypersensitivity to either paliperidone or risperidone, or to any of the excipients in INVEGA®.
5 WARNINGS AND PRECAUTIONS
5.1 Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. INVEGA® (paliperidone) is not approved for the treatment of dementia-related psychosis [see Boxed Warning].
5.2 Cerebrovascular Adverse Reactions, Including Stroke, in Elderly Patients With Dementia-Related Psychosis
In placebo-controlled trials with risperidone, aripiprazole, and olanzapine in elderly subjects with dementia, there was a higher incidence of cerebrovascular adverse reactions (cerebrovascular accidents and transient ischemic attacks) including fatalities compared to placebo-treated subjects. INVEGA® was not marketed at the time these studies were performed. INVEGA® is not approved for the treatment of patients with dementia-related psychosis [see also Boxed Warning and Warnings and Precautions (5.1)].
5.3 Neuroleptic Malignant Syndrome
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with antipsychotic drugs, including paliperidone. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases in which the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system pathology.
The management of NMS should include: (1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy; (2) intensive symptomatic treatment and medical monitoring; and (3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient appears to require antipsychotic drug treatment after recovery from NMS, reintroduction of drug therapy should be closely monitored, since recurrences of NMS have been reported.
5.4 QT Prolongation
Paliperidone causes a modest increase in the corrected QT (QTc) interval. The use of paliperidone should be avoided in combination with other drugs that are known to prolong QTc including Class 1A (e.g., quinidine, procainamide) or Class III (e.g., amiodarone, sotalol) antiarrhythmic medications, antipsychotic medications (e.g., chlorpromazine, thioridazine), antibiotics (e.g., gatifloxacin, moxifloxacin), or any other class of medications known to prolong the QTc interval. Paliperidone should also be avoided in patients with congenital long QT syndrome and in patients with a history of cardiac arrhythmias.
Certain circumstances may increase the risk of the occurrence of torsade de pointes and/or sudden death in association with the use of drugs that prolong the QTc interval, including (1) bradycardia; (2) hypokalemia or hypomagnesemia; (3) concomitant use of other drugs that prolong the QTc interval; and (4) presence of congenital prolongation of the QT interval.
The effects of paliperidone on the QT interval were evaluated in a double-blind, active-controlled (moxifloxacin 400 mg single dose), multicenter QT study in adults with schizophrenia and schizoaffective disorder, and in three placebo- and active-controlled 6-week, fixed-dose efficacy trials in adults with schizophrenia.
In the QT study (n = 141), the 8 mg dose of immediate-release oral paliperidone (n=50) showed a mean placebo-subtracted increase from baseline in QTcLD of 12.3 msec (90% CI: 8.9; 15.6) on day 8 at 1.5 hours post-dose. The mean steady-state peak plasma concentration for this 8 mg dose of paliperidone immediate-release was more than twice the exposure observed with the maximum recommended 12 mg dose of INVEGA® (Cmax ss = 113 ng/mL and 45 ng/mL, respectively, when administered with a standard breakfast). In this same study, a 4 mg dose of the immediate-release oral formulation of paliperidone, for which Cmax ss = 35 ng/mL, showed an increased placebo-subtracted QTcLD of 6.8 msec (90% CI: 3.6; 10.1) on day 2 at 1.5 hours post-dose. None of the subjects had a change exceeding 60 msec or a QTcLD exceeding 500 msec at any time during this study.
For the three fixed-dose efficacy studies in subjects with schizophrenia, electrocardiogram (ECG) measurements taken at various time points showed only one subject in the INVEGA® 12 mg group had a change exceeding 60 msec at one time-point on Day 6 (increase of 62 msec). No subject receiving INVEGA® had a QTcLD exceeding 500 msec at any time in any of these three studies.
5.5 Tardive Dyskinesia
A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to predict which patients will develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing tardive dyskinesia and the likelihood that it will become irreversible appear to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase, but the syndrome can develop after relatively brief treatment periods at low doses, although this is uncommon.
There is no known treatment for established tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment itself may suppress (or partially suppress) the signs and symptoms of the syndrome and may thus mask the underlying process. The effect of symptomatic suppression on the long-term course of the syndrome is unknown.
Given these considerations, INVEGA® should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that is known to respond to antipsychotic drugs. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient treated with INVEGA®, drug discontinuation should be considered. However, some patients may require treatment with INVEGA® despite the presence of the syndrome.
5.6 Hyperglycemia and Diabetes Mellitus
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with all atypical antipsychotics. These cases were, for the most part, seen in post-marketing clinical use and epidemiologic studies, not in clinical trials, and there have been few reports of hyperglycemia or diabetes in trial subjects treated with INVEGA®. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of treatment-emergent hyperglycemia-related adverse events in patients treated with the atypical antipsychotics. Because INVEGA® was not marketed at the time these studies were performed, it is not known if INVEGA® is associated with this increased risk.
Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the suspect drug.
5.7 Hyperprolactinemia
Like other drugs that antagonize dopamine D2 receptors, paliperidone elevates prolactin levels and the elevation persists during chronic administration. Paliperidone has a prolactin-elevating effect similar to that seen with risperidone, a drug that is associated with higher levels of prolactin than other antipsychotic drugs.
Hyperprolactinemia, regardless of etiology, may suppress hypothalamic GnRH, resulting in reduced pituitary gonadotrophin secretion. This, in turn, may inhibit reproductive function by impairing gonadal steroidogenesis in both female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating compounds. Long-standing hyperprolactinemia when associated with hypogonadism may lead to decreased bone density in both female and male subjects.
Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin dependent in vitro, a factor of potential importance if the prescription of these drugs is considered in a patient with previously detected breast cancer. An increase in the incidence of pituitary gland, mammary gland, and pancreatic islet cell neoplasia (mammary adenocarcinomas, pituitary and pancreatic adenomas) was observed in the risperidone carcinogenicity studies conducted in mice and rats [see Nonclinical Toxicology (13.1)]. Neither clinical studies nor epidemiologic studies conducted to date have shown an association between chronic administration of this class of drugs and tumorigenesis in humans, but the available evidence is too limited to be conclusive.
5.8 Potential for Gastrointestinal Obstruction
Because the INVEGA® tablet is non-deformable and does not appreciably change in shape in the gastrointestinal tract, INVEGA® should ordinarily not be administered to patients with pre-existing severe gastrointestinal narrowing (pathologic or iatrogenic, for example: esophageal motility disorders, small bowel inflammatory disease, "short gut" syndrome due to adhesions or decreased transit time, past history of peritonitis, cystic fibrosis, chronic intestinal pseudoobstruction, or Meckel's diverticulum). There have been rare reports of obstructive symptoms in patients with known strictures in association with the ingestion of drugs in non-deformable controlled-release formulations. Because of the controlled-release design of the tablet, INVEGA® should only be used in patients who are able to swallow the tablet whole [see Dosage and Administration (2.3) and Patient Counseling Information (17.8)].
A decrease in transit time, e.g., as seen with diarrhea, would be expected to decrease bioavailability and an increase in transit time, e.g., as seen with gastrointestinal neuropathy, diabetic gastroparesis, or other causes, would be expected to increase bioavailability. These changes in bioavailability are more likely when the changes in transit time occur in the upper GI tract.
5.9 Orthostatic Hypotension and Syncope
Paliperidone can induce orthostatic hypotension and syncope in some patients because of its alpha-blocking activity. In pooled results of the three placebo-controlled, 6-week, fixed-dose trials in subjects with schizophrenia, syncope was reported in 0.8% (7/850) of subjects treated with INVEGA® (3 mg, 6 mg, 9 mg, 12 mg) compared to 0.3% (1/355) of subjects treated with placebo. INVEGA® should be used with caution in patients with known cardiovascular disease (e.g., heart failure, history of myocardial infarction or ischemia, conduction abnormalities), cerebrovascular disease, or conditions that predispose the patient to hypotension (e.g., dehydration, hypovolemia, and treatment with antihypertensive medications). Monitoring of orthostatic vital signs should be considered in patients who are vulnerable to hypotension.
5.10 Leukopenia, Neutropenia, and Agranulocytosis
Class Effect: In clinical trial and/or postmarketing experience, events of leukopenia/neutropenia have been reported temporally related to antipsychotic agents, including INVEGA®. Agranulocytosis has also been reported.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of INVEGA® should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count <1000/mm3) should discontinue INVEGA® and have their WBC followed until recovery.
5.11 Potential for Cognitive and Motor Impairment
Somnolence was reported in subjects treated with INVEGA® [see Adverse Reactions (6.1, 6.2)]. Antipsychotics, including INVEGA®, have the potential to impair judgment, thinking, or motor skills. Patients should be cautioned about performing activities requiring mental alertness, such as operating hazardous machinery or operating a motor vehicle, until they are reasonably certain that paliperidone therapy does not adversely affect them.
5.12 Seizures
During premarketing clinical trials in subjects with schizophrenia (the three placebo-controlled, 6-week, fixed-dose studies and a study conducted in elderly schizophrenic subjects), seizures occurred in 0.22% of subjects treated with INVEGA® (3 mg, 6 mg, 9 mg, 12 mg) and 0.25% of subjects treated with placebo. Like other antipsychotic drugs, INVEGA® should be used cautiously in patients with a history of seizures or other conditions that potentially lower the seizure threshold. Conditions that lower the seizure threshold may be more prevalent in patients 65 years or older.
5.13 Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use. Aspiration pneumonia is a common cause of morbidity and mortality in patients with advanced Alzheimer's dementia. INVEGA® and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia.
5.14 Suicide
The possibility of suicide attempt is inherent in psychotic illnesses, and close supervision of high-risk patients should accompany drug therapy. Prescriptions for INVEGA® should be written for the smallest quantity of tablets consistent with good patient management in order to reduce the risk of overdose.
5.15 Priapism
Drugs with alpha-adrenergic blocking effects have been reported to induce priapism. Priapism has been reported with INVEGA® during postmarketing surveillance. Severe priapism may require surgical intervention.
5.16 Thrombotic Thrombocytopenic Purpura (TTP)
No cases of TTP were observed during clinical studies with paliperidone. Although cases of TTP have been reported in association with risperidone administration, the relationship to risperidone therapy is unknown.
5.17 Body Temperature Regulation
Disruption of the body's ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing INVEGA® to patients who will be experiencing conditions which may contribute to an elevation in core body temperature, e.g., exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration.
5.18 Antiemetic Effect
An antiemetic effect was observed in preclinical studies with paliperidone. This effect, if it occurs in humans, may mask the signs and symptoms of overdosage with certain drugs or of conditions such as intestinal obstruction, Reye's syndrome, and brain tumor.
5.19 Use in Patients with Concomitant Illness
Clinical experience with INVEGA® in patients with certain concomitant illnesses is limited [see Clinical Pharmacology (12.3)].
Patients with Parkinson's Disease or Dementia with Lewy Bodies are reported to have an increased sensitivity to antipsychotic medication. Manifestations of this increased sensitivity include confusion, obtundation, postural instability with frequent falls, extrapyramidal symptoms, and clinical features consistent with the neuroleptic malignant syndrome.
INVEGA® has not been evaluated or used to any appreciable extent in patients with a recent history of myocardial infarction or unstable heart disease. Patients with these diagnoses were excluded from premarketing clinical trials. Because of the risk of orthostatic hypotension with INVEGA®, caution should be observed in patients with known cardiovascular disease [see Warnings and Precautions (5.9)].
6 ADVERSE REACTIONS
The following are discussed in more detail in other sections of the labeling:
- Increased mortality in elderly patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions (5.1)]
- Cerebrovascular adverse events, including stroke, in elderly patients with dementia-related psychosis [see Warnings and Precautions (5.2)]
- Neuroleptic malignant syndrome [see Warnings and Precautions (5.3)]
- QT prolongation [see Warnings and Precautions (5.4)]
- Tardive dyskinesia [see Warnings and Precautions (5.5)]
- Hyperglycemia and diabetes mellitus [see Warnings and Precautions (5.6)]
- Hyperprolactinemia [see Warnings and Precautions (5.7)]
- Potential for Gastrointestinal Obstruction [see Warnings and Precautions (5.8)]
- Orthostatic hypotension and syncope [see Warnings and Precautions (5.9)]
- Leukopenia, neutropenia, and agranulocytosis [see Warnings and Precautions (5.10)]
- Potential for cognitive and motor impairment [see Warnings and Precautions (5.11)]
- Seizures [see Warnings and Precautions (5.12)]
- Dysphagia [see Warnings and Precautions (5.13)]
- Suicide [see Warnings and Precautions (5.14)]
- Priapism [see Warnings and Precautions (5.15)]
- Thrombotic thrombocytopenic purpura (TTP) [see Warnings and Precautions (5.16)]
- Disruption of body temperature regulation [see Warnings and Precautions (5.17)]
- Antiemetic effect [see Warnings and Precautions (5.18)]
- Increased sensitivity in patients with Parkinson's disease or those with dementia with Lewy bodies [see Warnings and Precautions (5.19)]
- Diseases or conditions that could affect metabolism or hemodynamic responses [see Warnings and Precautions (5.19)]
The most common adverse reactions in clinical trials in subjects with schizophrenia (reported in 5% or more of subjects treated with INVEGA® and at least twice the placebo rate in any of the dose groups) were extrapyramidal symptoms, tachycardia, and akathisia. The most common adverse reactions in clinical trials in patients with schizoaffective disorder (reported in 5% or more of subjects treated with INVEGA® and at least twice the placebo rate) were extrapyramidal symptoms, somnolence, dyspepsia, constipation, weight increased, and nasopharyngitis.
The most common adverse reactions that were associated with discontinuation from clinical trials in subjects with schizophrenia (causing discontinuation in 2% of INVEGA®-treated subjects) were nervous system disorders. The most common adverse reactions that were associated with discontinuation from clinical trials in subjects with schizoaffective disorder were gastrointestinal disorders, which resulted in discontinuation in 1% of INVEGA®-treated subjects. [See Adverse Reactions (6.4)].
The safety of INVEGA® was evaluated in 1205 adult subjects with schizophrenia who participated in three placebo-controlled, 6-week, double-blind trials, of whom 850 subjects received INVEGA® at fixed doses ranging from 3 mg to 12 mg once daily. The information presented in this section was derived from pooled data from these three trials. Additional safety information from the placebo-controlled phase of the long-term maintenance study, in which subjects received INVEGA® at daily doses within the range of 3 mg to 15 mg (n=104), is also included.
The safety of INVEGA® was also evaluated in 622 adult subjects with schizoaffective disorder who participated in two placebo-controlled, 6-week, double-blind trials. In one of these trials, 206 subjects were assigned to one of two dose levels of INVEGA®: 6 mg with the option to reduce to 3 mg (n = 108) or 12 mg with the option to reduce to 9 mg (n = 98) once daily. In the other study, 214 subjects received flexible doses of INVEGA® (3–12 mg once daily). Both studies included subjects who received INVEGA® either as monotherapy or as an adjunct to mood stabilizers and/or antidepressants. Adverse events during exposure to study treatment were obtained by general inquiry and recorded by clinical investigators using their own terminology. Consequently, to provide a meaningful estimate of the proportion of individuals experiencing adverse events, events were grouped in standardized categories using MedDRA terminology.
Throughout this section, adverse reactions are reported. Adverse reactions are adverse events that were considered to be reasonably associated with the use of INVEGA® (adverse drug reactions) based on the comprehensive assessment of the available adverse event information. A causal association for INVEGA® often cannot be reliably established in individual cases. Further, because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
6.1 Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials - Schizophrenia
Table 1 enumerates the pooled incidences of adverse reactions reported in the three placebo-controlled, 6-week, fixed-dose studies, listing those that occurred in 2% or more of subjects treated with INVEGA® in any of the dose groups, and for which the incidence in INVEGA®-treated subjects in any of the dose groups was greater than the incidence in subjects treated with placebo.
| Percent of Patients Reporting Event | |||||
| INVEGA® | |||||
| Placebo | 3 mg once daily | 6 mg once daily | 9 mg once daily | 12 mg once daily |
|
| Body System or Organ Class Dictionary-Derived Term | (N=355) | (N=127) | (N=235) | (N=246) | (N=242) |
|
|||||
| Total percentage of subjects with adverse reactions | 37 | 48 | 47 | 53 | 59 |
| Cardiac disorders | |||||
| Atrioventricular block first degree | 1 | 2 | 0 | 2 | 1 |
| Bundle branch block | 2 | 3 | 1 | 3 | <1 |
| Sinus arrhythmia | 0 | 2 | 1 | 1 | <1 |
| Tachycardia | 7 | 14 | 12 | 12 | 14 |
| Gastrointestinal disorders | |||||
| Abdominal pain upper | 1 | 1 | 3 | 2 | 2 |
| Dry mouth | 1 | 2 | 3 | 1 | 3 |
| Salivary hypersecretion | <1 | 0 | <1 | 1 | 4 |
| General disorders | |||||
| Asthenia | 1 | 2 | <1 | 2 | 2 |
| Fatigue | 1 | 2 | 1 | 2 | 2 |
| Nervous system disorders | |||||
| Akathisia | 4 | 4 | 3 | 8 | 10 |
| Dizziness | 4 | 6 | 5 | 4 | 5 |
| Extrapyramidal symptoms | 8 | 10 | 7 | 20 | 18 |
| Headache | 12 | 11 | 12 | 14 | 14 |
| Somnolence | 7 | 6 | 9 | 10 | 11 |
| Vascular disorders | |||||
| Orthostatic hypotension | 1 | 2 | 1 | 2 | 4 |
6.2 Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials – Schizoaffective Disorder
Table 2 enumerates the pooled incidences of adverse reactions reported in the two placebo-controlled 6-week studies, listing those that occurred in 2% or more of subjects treated with INVEGA® and for which the incidence in INVEGA®-treated subjects was greater than the incidence in subjects treated with placebo.
|
Placebo | INVEGA®
3–6 mg once-daily fixed-dose range | INVEGA®
9–12 mg once-daily fixed-dose range | INVEGA®
3–12 mg once-daily flexible-dose |
|
| Body System or Organ Class | (N=202) | (N=108) | (N=98) | (N=214) |
| Dictionary-Derived Term | ||||
| * Table includes adverse reactions that were reported in 2% or more of subjects in any of the INVEGA® dose groups and which occurred at greater incidence than in the placebo group. Data are pooled from two studies. One study included once-daily INVEGA® doses of 6 mg (with the option to reduce to 3 mg) and 12 mg (with the option to reduce to 9 mg). The second study included flexible once-daily doses of 3 to 12 mg. Among the 420 subjects treated with INVEGA®, 230 (55%) received INVEGA® as monotherapy and 190 (45%) received INVEGA® as an adjunct to mood stabilizers and/or antidepressants. Extrapyramidal symptoms includes the terms bradykinesia, drooling, dyskinesia, dystonia, hypertonia, muscle rigidity, muscle twitching, oculogyration, parkinsonian gait, parkinsonism, restlessness, and tremor. Somnolence includes the terms sedation and somnolence. Tachycardia includes the terms tachycardia, sinus tachycardia, and heart rate increased. | ||||
| Total percentage of subjects with adverse reactions | 32 | 48 | 50 | 43 |
| Cardiac disorders | ||||
| Tachycardia | 2 | 3 | 1 | 2 |
| Gastrointestinal disorders | ||||
| Abdominal discomfort/Abdominal pain upper | 1 | 1 | 0 | 3 |
| Constipation | 2 | 4 | 5 | 4 |
| Dyspepsia | 2 | 5 | 6 | 6 |
| Nausea | 6 | 8 | 8 | 5 |
| Stomach discomfort | 1 | 0 | 1 | 2 |
| General disorders | ||||
| Asthenia | 1 | 3 | 4 | <1 |
| Infections and Infestations | ||||
| Nasopharyngitis | 1 | 2 | 5 | 3 |
| Rhinitis | 0 | 1 | 3 | 1 |
| Upper respiratory tract infection | 1 | 2 | 2 | 2 |
| Investigations | ||||
| Weight increased | 1 | 5 | 4 | 4 |
| Metabolism and nutrition disorders | ||||
| Decreased appetite | <1 | 1 | 0 | 2 |
| Increased appetite | <1 | 3 | 2 | 2 |
| Musculoskeletal and connective tissue disorders | ||||
| Back pain | 1 | 1 | 1 | 3 |
| Myalgia | <1 | 2 | 4 | 1 |
| Nervous system disorders | ||||
| Akathisia | 4 | 4 | 6 | 6 |
| Dysarthria | 0 | 1 | 4 | 2 |
| Extrapyramidal symptoms | 8 | 20 | 17 | 12 |
| Somnolence | 5 | 12 | 12 | 8 |
| Psychiatric disorders | ||||
| Sleep disorder | <1 | 2 | 3 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Cough | 1 | 1 | 3 | 1 |
| Pharyngolaryngeal pain | <1 | 0 | 2 | 1 |
Monotherapy versus Adjunctive Therapy
The designs of the two placebo-controlled, 6-week, double-blind trials in subjects with schizoaffective disorder included the option for subjects to receive antidepressants (except monoamine oxidase inhibitors) and/or mood stabilizers (lithium, valproate, or lamotrigine). In the subject population evaluated for safety, 230 (55%) subjects received INVEGA® as monotherapy and 190 (45%) subjects received INVEGA® as an adjunct to mood stabilizers and/or antidepressants. When comparing these 2 subpopulations, only nausea occurred at a greater frequency (≥ 3% difference) in subjects receiving INVEGA® as monotherapy.
6.3 Other Adverse Reactions Observed During Premarketing Evaluation of INVEGA®
The following additional adverse reactions occurred in < 2% of INVEGA®-treated subjects in the above schizophrenia and schizoaffective disorder clinical trial datasets. The following also includes additional adverse reactions reported at any frequency by INVEGA®-treated subjects who participated in other clinical studies.
Cardiac disorders: bradycardia, bundle branch block left, palpitations
Endocrine disorders: hyperprolactinemia
Eye disorders: vision blurred
Gastrointestinal disorders: abdominal pain, flatulence, small intestinal obstruction, swollen tongue
General disorders: edema, edema peripheral
Immune system disorders: anaphylactic reaction
Infections and infestations: urinary tract infection
Investigations: electrocardiogram abnormal
Musculoskeletal and connective tissue disorders: arthralgia, pain in extremity
Nervous system disorders: cerebrovascular accident, convulsion, dizziness postural, grand mal convulsion, lethargy, syncope, transient ischemic attack, additional extrapyramidal symptoms (cogwheel rigidity, muscle spasms, musculoskeletal pain, torticollis, trismus)
Psychiatric disorders: agitation, nightmare
Reproductive system and breast disorders: amenorrhea, breast discharge, breast engorgement, breast tenderness, breast pain, erectile dysfunction, galactorrhea, gynecomastia, menstruation irregular, retrograde ejaculation
Respiratory, thoracic and mediastinal disorders: nasal congestion, pneumonia aspiration
Skin and subcutaneous tissue disorders: pruritus, rash, rash papular
Vascular disorders: hypotension, ischemia
6.4 Discontinuations Due to Adverse Reactions
Schizophrenia Trials
The percentages of subjects who discontinued due to adverse reactions in the three schizophrenia placebo-controlled, 6-week, fixed-dose studies were 3% and 1% in INVEGA®- and placebo-treated subjects, respectively. The most common reasons for discontinuation were nervous system disorders (2% and 0% in INVEGA®- and placebo-treated subjects, respectively).
Schizoaffective Disorder Trials
The percentages of subjects who discontinued due to adverse reactions in the two schizoaffective disorder placebo‑controlled 6-week studies were 1% and <1% in INVEGA®- and placebo-treated subjects, respectively. The most common reasons for discontinuation were gastrointestinal disorders (1% and 0% in INVEGA®- and placebo-treated subjects, respectively).
6.5 Dose-Related Adverse Reactions
Schizophrenia Trials
Based on the pooled data from the three placebo-controlled, 6-week, fixed-dose studies in subjects with schizophrenia, among the adverse reactions that occurred with a greater than 2% incidence in the subjects treated with INVEGA®, the incidences of the following adverse reactions increased with dose: somnolence, orthostatic hypotension, akathisia, dystonia, extrapyramidal disorder, hypertonia, parkinsonism, and salivary hypersecretion. For most of these, the increased incidence was seen primarily at the 12 mg dose, and, in some cases, the 9 mg dose.
Schizoaffective Disorder Trials
In a placebo-controlled, 6-week, high- and low-dose study in subjects with schizoaffective disorder, akathisia, dystonia, dysarthria, myalgia, nasopharyngitis, rhinitis, cough, and pharyngolaryngeal pain occurred more frequently (i.e., a difference of at least 2%) in subjects who received higher doses of INVEGA® compared with subjects who received lower doses.
6.6 Demographic Differences
An examination of population subgroups in the three placebo-controlled, 6-week, fixed-dose studies in subjects with schizophrenia and in the two placebo-controlled, 6-week studies in subjects with schizoaffective disorder did not reveal any evidence of clinically relevant differences in safety on the basis of gender or race alone; there was also no difference on the basis of age [see Use in Specific Populations (8.5)].
6.7 Extrapyramidal Symptoms (EPS)
Pooled data from the three placebo-controlled, 6-week, fixed-dose studies in subjects with schizophrenia provided information regarding treatment-emergent EPS. Several methods were used to measure EPS: (1) the Simpson-Angus global score (mean change from baseline) which broadly evaluates Parkinsonism, (2) the Barnes Akathisia Rating Scale global clinical rating score (mean change from baseline) which evaluates akathisia, (3) use of anticholinergic medications to treat emergent EPS (Table 3), and (4) incidence of spontaneous reports of EPS (Table 4). For the Simpson-Angus Scale, spontaneous EPS reports and use of anticholinergic medications, there was a dose-related increase observed for the 9 mg and 12 mg doses. There was no difference observed between placebo and INVEGA® 3 mg and 6 mg doses for any of these EPS measures.
| Percentage of Patients | |||||
| INVEGA® | |||||
| Placebo | 3 mg | 6 mg | 9 mg | 12 mg | |
| once daily | once daily | once daily | once daily | ||
| EPS Group | (N=355) | (N=127) | (N=235) | (N=246) | (N=242) |
|
|||||
| Parkinsonism * | 9 | 11 | 3 | 15 | 14 |
| Akathisia † | 6 | 6 | 4 | 7 | 9 |
| Use of anticholinergic medications ‡ | 10 | 10 | 9 | 22 | 22 |
| Percentage of Patients | |||||
| INVEGA® | |||||
| Placebo | 3 mg | 6 mg | 9 mg | 12 mg | |
| once daily | once daily | once daily | once daily | ||
| EPS Group | (N=355) | (N=127) | (N=235) | (N=246) | (N=242) |
| Dyskinesia group includes: Dyskinesia, extrapyramidal disorder, muscle twitching, tardive dyskinesia Dystonia group includes: Dystonia, muscle spasms, oculogyration, trismus Hyperkinesia group includes: Akathisia, hyperkinesia Parkinsonism group includes: Bradykinesia, cogwheel rigidity, drooling, hypertonia, hypokinesia, muscle rigidity, musculoskeletal stiffness, parkinsonism Tremor group includes: Tremor |
|||||
| Overall percentage of patients with EPS-related AE | 11 | 13 | 10 | 25 | 26 |
| Dyskinesia | 3 | 5 | 3 | 8 | 9 |
| Dystonia | 1 | 1 | 1 | 5 | 5 |
| Hyperkinesia | 4 | 4 | 3 | 8 | 10 |
| Parkinsonism | 2 | 3 | 3 | 7 | 6 |
| Tremor | 3 | 3 | 3 | 4 | 3 |
Compared to data from the studies in schizophrenia, pooled data from the two placebo-controlled 6-week studies in subjects with schizoaffective disorder showed similar types and frequencies of EPS as measured by rating scales, anticholinergic medication use, and spontaneous reports of EPS-related adverse events. For subjects with schizoaffective disorder, there was no dose-related increase in EPS observed for parkinsonism with the Simpson-Angus scale or akathisia with the Barnes Akathisia Rating Scale. There was a dose-related increase observed with spontaneous EPS reports of hyperkinesia and dystonia and in the use of anticholinergic medications.
Table 5 shows the EPS data from the pooled schizoaffective disorder trials.
| Percentage of Patients | ||||
| INVEGA® | ||||
| Placebo | 3–6 mg once-daily fixed-dose range | 9–12 mg once-daily fixed-dose range | 3–12 mg once-daily flexible dose |
|
| EPS Group | (N=202) | (N=108) | (N=98) | (N=214) |
| Dyskinesia group includes: Dyskinesia, muscle twitching Dystonia group includes: Dystonia, muscle spasms, oculogyration Hyperkinesia group includes: Akathisia, hyperkinesia, restlessness Parkinsonism group includes: Bradykinesia, drooling, hypertonia, muscle rigidity, muscle tightness, musculoskeletal stiffness, parkinsonian gait, parkinsonism Tremor group includes: Tremor |
||||
| Overall percentage of patients with EPS-related AE | 11 | 23 | 22 | 17 |
| Dyskinesia | 1 | 3 | 1 | 1 |
| Dystonia | 1 | 2 | 3 | 2 |
| Hyperkinesia | 5 | 5 | 8 | 7 |
| Parkinsonism | 3 | 14 | 7 | 7 |
| Tremor | 3 | 12 | 11 | 5 |
Dystonia
Class Effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
6.8 Laboratory Test Abnormalities
In the pooled data from the three placebo-controlled, 6-week, fixed-dose studies in subjects with schizophrenia and from the two placebo-controlled, 6-week studies in subjects with schizoaffective disorder, between-group comparisons revealed no medically important differences between INVEGA® and placebo in the proportions of subjects experiencing potentially clinically significant changes in routine serum chemistry, hematology, or urinalysis parameters. Similarly, there were no differences between INVEGA® and placebo in the incidence of discontinuations due to changes in hematology, urinalysis, or serum chemistry, including mean changes from baseline in fasting glucose, insulin, c-peptide, triglyceride, HDL, LDL, and total cholesterol measurements. However, INVEGA® was associated with increases in serum prolactin [see Warnings and Precautions (5.7)].
6.9 Weight Gain
Schizophrenia Trials
In the pooled data from the three placebo-controlled, 6-week, fixed-dose studies in subjects with schizophrenia, the proportions of subjects meeting a weight gain criterion of ≥ 7% of body weight were compared, revealing a similar incidence of weight gain for INVEGA® 3 mg and 6 mg (7% and 6%, respectively) compared with placebo (5%), and a higher incidence of weight gain for INVEGA® 9 mg and 12 mg (9% and 9%, respectively).
Schizoaffective Disorder Trials
In the pooled data from the two placebo-controlled, 6-week studies in subjects with schizoaffective disorder, a higher percentage of INVEGA®-treated subjects (5%) had an increase in body weight of ≥ 7% compared with placebo-treated subjects (1%). In the study that examined high- and low-dose groups, the increase in body weight of ≥ 7% was 3% in the low-dose group, 7% in the high-dose group, and 1% in the placebo group.
6.10 Other Findings Observed During Clinical Trials
The safety of INVEGA® was also evaluated in a long-term trial designed to assess the maintenance of effect with INVEGA® in adults with schizophrenia [see Clinical Studies (14)]. In general, adverse reaction types, frequencies, and severities during the initial 14-week open-label phase of this study were comparable to those observed in the 6-week, placebo-controlled, fixed-dose studies. Adverse reactions reported during the long-term double-blind phase of this study were similar in type and severity to those observed in the initial 14-week open-label phase.
6.11 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of INVEGA®; because these reactions were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency: angioedema, priapism, swollen tongue, tardive dyskinesia, urinary incontinence, urinary retention.
7 DRUG INTERACTIONS
7.1 Potential for INVEGA® to Affect Other Drugs
Given the primary CNS effects of paliperidone [see Adverse Reactions (6.1, 6.2)], INVEGA® should be used with caution in combination with other centrally acting drugs and alcohol. Paliperidone may antagonize the effect of levodopa and other dopamine agonists.
Because of its potential for inducing orthostatic hypotension, an additive effect may be observed when INVEGA® is administered with other therapeutic agents that have this potential [see Warnings and Precautions (5.9)].
Paliperidone is not expected to cause clinically important pharmacokinetic interactions with drugs that are metabolized by cytochrome P450 isozymes. In vitro studies in human liver microsomes showed that paliperidone does not substantially inhibit the metabolism of drugs metabolized by cytochrome P450 isozymes, including CYP1A2, CYP2A6, CYP2C8/9/10, CYP2D6, CYP2E1, CYP3A4, and CYP3A5. Therefore, paliperidone is not expected to inhibit clearance of drugs that are metabolized by these metabolic pathways in a clinically relevant manner. Paliperidone is also not expected to have enzyme inducing properties.
Paliperidone is a weak inhibitor of P-glycoprotein (P-gp) at high concentrations. No in vivo data are available and the clinical relevance is unknown.
Pharmacokinetic interaction between lithium and INVEGA® is unlikely.
In a clinical study, subjects on a stable dose of valproate showed comparable valproate average plasma concentrations when 3–15 mg of INVEGA® was added to their existing valproate treatment.
7.2 Potential for Other Drugs to Affect INVEGA®
Paliperidone is not a substrate of CYP1A2, CYP2A6, CYP2C9, and CYP2C19, so that an interaction with inhibitors or inducers of these isozymes is unlikely. While in vitro studies indicate that CYP2D6 and CYP3A4 may be minimally involved in paliperidone metabolism, in vivo studies do not show decreased elimination by these isozymes and they contribute to only a small fraction of total body clearance. In vitro studies have shown that paliperidone is a P-gp substrate.
Co-administration of INVEGA® 6 mg once daily with carbamazepine 200 mg twice daily caused a decrease of approximately 37% in the mean steady-state Cmax and AUC of paliperidone. This decrease is caused, to a substantial degree, by a 35% increase in renal clearance of paliperidone. A minor decrease in the amount of drug excreted unchanged in the urine suggests that there was little effect on the CYP metabolism or bioavailability of paliperidone during carbamazepine co-administration. On initiation of carbamazepine, the dose of INVEGA® should be re-evaluated and increased if necessary. Conversely, on discontinuation of carbamazepine, the dose of INVEGA® should be re-evaluated and decreased if necessary.
Paliperidone is metabolized to a limited extent by CYP2D6 [see Clinical Pharmacology (12.3)]. In an interaction study in healthy subjects in which a single 3 mg dose of INVEGA® was administered concomitantly with 20 mg per day of paroxetine (a potent CYP2D6 inhibitor), paliperidone exposures were on average 16% (90% CI: 4, 30) higher in CYP2D6 extensive metabolizers. Higher doses of paroxetine have not been studied. The clinical relevance is unknown.
Co-administration of a single dose of INVEGA® 12 mg with divalproex sodium extended-release tablets (two 500 mg tablets once daily) resulted in an increase of approximately 50% in the Cmax and AUC of paliperidone. Dosage reduction for INVEGA® should be considered when INVEGA® is co-administered with valproate after clinical assessment.
Pharmacokinetic interaction between lithium and INVEGA® is unlikely.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C.
There are no adequate and well controlled studies of INVEGA® in pregnant women. INVEGA® should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Use of first generation antipsychotic drugs during the last trimester of pregnancy has been associated with extrapyramidal symptoms in the neonate. These symptoms are usually self-limited. It is not known whether paliperidone, when taken near the end of pregnancy, will lead to similar neonatal signs and symptoms.
In animal reproduction studies, there were no increases in fetal abnormalities when pregnant rats and rabbits were treated during the period of organogenesis with up to 8 times the maximum recommended human dose of paliperidone (on a mg/m2 basis).
In rat reproduction studies with risperidone, which is extensively converted to paliperidone in rats and humans, there were increases in pup deaths seen at oral doses which are less than the maximum recommended human dose of risperidone on a mg/m2 basis (see risperidone package insert).
8.3 Nursing Mothers
Paliperidone is 9-hydroxyrisperidone, the active metabolite of risperidone. In animal studies, risperidone and 9-hydroxyrisperidone were excreted in milk. Risperidone and 9-hydroxyrisperidone are also excreted in human breast milk. Caution should be exercised when INVEGA® is administered to a nursing woman. The known benefits of breastfeeding should be weighed against the unknown risks of infant exposure to paliperidone.
8.4 Pediatric Use
Safety and effectiveness of INVEGA® in patients < 18 years of age have not been established.
8.5 Geriatric Use
The safety, tolerability, and efficacy of INVEGA® were evaluated in a 6-week placebo-controlled study of 114 elderly subjects with schizophrenia (65 years of age and older, of whom 21 were 75 years of age and older). In this study, subjects received flexible doses of INVEGA® (3 mg to 12 mg once daily). In addition, a small number of subjects 65 years of age and older were included in the 6-week placebo-controlled studies in which adult schizophrenic subjects received fixed doses of INVEGA® (3 mg to 15 mg once daily) [see Clinical Studies (14)]. There were no subjects ≥ 65 years of age in the schizoaffective disorder studies.
Overall, of the total number of subjects in schizophrenia clinical studies of INVEGA® (n = 1796), including those who received INVEGA® or placebo, 125 (7.0%) were 65 years of age and older and 22 (1.2%) were 75 years of age and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in response between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
This drug is known to be substantially excreted by the kidney and clearance is decreased in patients with moderate to severe renal impairment [see Clinical Pharmacology (12.3)], who should be given reduced doses. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Dosage and Administration (2.5)].
8.6 Renal Impairment
Dosing must be individualized according to the patient's renal function status [see Dosage and Administration (2.5)].
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
Paliperidone has not been systematically studied in animals or humans for its potential for abuse. It is not possible to predict the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of INVEGA® misuse or abuse (e.g., development of tolerance, increases in dose, drug-seeking behavior).
10 OVERDOSAGE
10.1 Human Experience
While experience with paliperidone overdose is limited, among the few cases of overdose reported in pre-marketing trials, the highest estimated ingestion of INVEGA® was 405 mg. Observed signs and symptoms included extrapyramidal symptoms and gait unsteadiness. Other potential signs and symptoms include those resulting from an exaggeration of paliperidone's known pharmacological effects, i.e., drowsiness and somnolence, tachycardia and hypotension, and QT prolongation. Torsade de pointes and ventricular fibrillation have been reported in a patient in the setting of overdose.
Paliperidone is the major active metabolite of risperidone. Overdose experience reported with risperidone can be found in the OVERDOSAGE section of the risperidone package insert.
10.2 Management of Overdosage
There is no specific antidote to paliperidone, therefore, appropriate supportive measures should be instituted and close medical supervision and monitoring should continue until the patient recovers. Consideration should be given to the extended-release nature of the product when assessing treatment needs and recovery. Multiple drug involvement should also be considered.
In case of acute overdose, establish and maintain an airway and ensure adequate oxygenation and ventilation. Gastric lavage (after intubation if patient is unconscious) and administration of activated charcoal together with a laxative should be considered.
The possibility of obtundation, seizures, or dystonic reaction of the head and neck following overdose may create a risk of aspiration with induced emesis.
Cardiovascular monitoring should commence immediately, including continuous electrocardiographic monitoring for possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide, and quinidine carry a theoretical hazard of additive QT-prolonging effects when administered in patients with an acute overdose of paliperidone. Similarly the alpha-blocking properties of bretylium might be additive to those of paliperidone, resulting in problematic hypotension.
Hypotension and circulatory collapse should be treated with appropriate measures, such as intravenous fluids and/or sympathomimetic agents (epinephrine and dopamine should not be used, since beta stimulation may worsen hypotension in the setting of paliperidone-induced alpha blockade). In cases of severe extrapyramidal symptoms, anticholinergic medication should be administered.
11 DESCRIPTION
Paliperidone, the active ingredient in INVEGA® Extended-Release Tablets, is a psychotropic agent belonging to the chemical class of benzisoxazole derivatives. INVEGA® contains a racemic mixture of (+)- and (-)- paliperidone. The chemical name is (±)-3-[2-[4-(6-fluoro-1,2-benzisoxazol-3-yl)-1-piperidinyl]ethyl]-6,7,8,9-tetrahydro-9-hydroxy-2-methyl-4H-pyrido[1,2-a]pyrimidin-4-one. Its molecular formula is C23H27FN4O3 and its molecular weight is 426.49. The structural formula is:
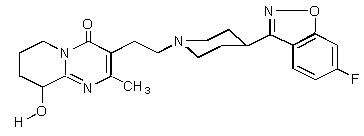
Paliperidone is sparingly soluble in 0.1N HCl and methylene chloride; practically insoluble in water, 0.1N NaOH, and hexane; and slightly soluble in N,N-dimethylformamide.
INVEGA® (paliperidone) Extended-Release Tablets are available in 1.5 mg (orange-brown), 3 mg (white), 6 mg (beige), and 9 mg (pink) strengths. INVEGA® utilizes OROS® osmotic drug-release technology [see Description (11.1)].
Inactive ingredients are carnauba wax, cellulose acetate, hydroxyethyl cellulose, propylene glycol, polyethylene glycol, polyethylene oxides, povidone, sodium chloride, stearic acid, butylated hydroxytoluene, hypromellose, titanium dioxide, and iron oxides. The 3 mg tablets also contain lactose monohydrate and triacetin.
11.1 Delivery System Components and Performance
INVEGA® uses osmotic pressure to deliver paliperidone at a controlled rate. The delivery system, which resembles a capsule-shaped tablet in appearance, consists of an osmotically active trilayer core surrounded by a subcoat and semipermeable membrane. The trilayer core is composed of two drug layers containing the drug and excipients, and a push layer containing osmotically active components. There are two precision laser-drilled orifices on the drug-layer dome of the tablet. Each tablet strength has a different colored water-dispersible overcoat and print markings. In an aqueous environment, such as the gastrointestinal tract, the water-dispersible color overcoat erodes quickly. Water then enters the tablet through the semipermeable membrane that controls the rate at which water enters the tablet core, which, in turn, determines the rate of drug delivery. The hydrophilic polymers of the core hydrate and swell, creating a gel containing paliperidone that is then pushed out through the tablet orifices. The biologically inert components of the tablet remain intact during gastrointestinal transit and are eliminated in the stool as a tablet shell, along with insoluble core components.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Paliperidone is the major active metabolite of risperidone. The mechanism of action of paliperidone, as with other drugs having efficacy in schizophrenia, is unknown, but it has been proposed that the drug's therapeutic activity in schizophrenia is mediated through a combination of central dopamine Type 2 (D2) and serotonin Type 2 (5HT2A) receptor antagonism.
12.2 Pharmacodynamics
Paliperidone is a centrally active dopamine Type 2 (D2) antagonist and with predominant serotonin Type 2 (5HT2A) activity. Paliperidone is also active as an antagonist at α1 and α2 adrenergic receptors and H1 histaminergic receptors, which may explain some of the other effects of the drug. Paliperidone has no affinity for cholinergic muscarinic or β1- and β2-adrenergic receptors. The pharmacological activity of the (+)- and (-)- paliperidone enantiomers is qualitatively and quantitatively similar in vitro.
12.3 Pharmacokinetics
Following a single dose, the plasma concentrations of paliperidone gradually rise to reach peak plasma concentration (Cmax) approximately 24 hours after dosing. The pharmacokinetics of paliperidone following INVEGA® administration are dose-proportional within the available dose range. The terminal elimination half-life of paliperidone is approximately 23 hours.
Steady-state concentrations of paliperidone are attained within 4–5 days of dosing with INVEGA® in most subjects. The mean steady-state peak:trough ratio for an INVEGA® dose of 9 mg was 1.7 with a range of 1.2–3.1.
Following administration of INVEGA®, the (+) and (-) enantiomers of paliperidone interconvert, reaching an AUC (+) to (-) ratio of approximately 1.6 at steady state.
Absorption and Distribution
The absolute oral bioavailability of paliperidone following INVEGA® administration is 28%.
Administration of a 12 mg paliperidone extended-release tablet to healthy ambulatory subjects with a standard high-fat/high-caloric meal gave mean Cmax and AUC values of paliperidone that were increased by 60% and 54%, respectively, compared with administration under fasting conditions. Clinical trials establishing the safety and efficacy of INVEGA® were carried out in subjects without regard to the timing of meals. While INVEGA® can be taken without regard to food, the presence of food at the time of INVEGA® administration may increase exposure to paliperidone [see Dosage and Administration (2.3)].
Based on a population analysis, the apparent volume of distribution of paliperidone is 487 L. The plasma protein binding of racemic paliperidone is 74%.
Metabolism and Elimination
Although in vitro studies suggested a role for CYP2D6 and CYP3A4 in the metabolism of paliperidone, in vivo results indicate that these isozymes play a limited role in the overall elimination of paliperidone [see Drug Interactions (7)].
One week following administration of a single oral dose of 1 mg immediate-release 14C-paliperidone to 5 healthy volunteers, 59% (range 51% – 67%) of the dose was excreted unchanged into urine, 32% (26% – 41%) of the dose was recovered as metabolites, and 6% – 12% of the dose was not recovered. Approximately 80% of the administered radioactivity was recovered in urine and 11% in the feces. Four primary metabolic pathways have been identified in vivo, none of which could be shown to account for more than 10% of the dose: dealkylation, hydroxylation, dehydrogenation, and benzisoxazole scission.
Population pharmacokinetic analyses found no difference in exposure or clearance of paliperidone between extensive metabolizers and poor metabolizers of CYP2D6 substrates.
Special Populations
Renal Impairment
The dose of INVEGA® should be reduced in patients with moderate or severe renal impairment [see Dosage and Administration (2.5)]. The disposition of a single dose paliperidone 3 mg extended-release tablet was studied in subjects with varying degrees of renal function. Elimination of paliperidone decreased with decreasing estimated creatinine clearance. Total clearance of paliperidone was reduced in subjects with impaired renal function by 32% on average in mild (CrCl = 50 mL/min to < 80 mL/min), 64% in moderate (CrCl = 30 mL/min to < 50 mL/min), and 71% in severe (CrCl = 10 mL/min to < 30 mL/min) renal impairment, corresponding to an average increase in exposure (AUCinf) of 1.5 fold, 2.6 fold, and 4.8 fold, respectively, compared to healthy subjects. The mean terminal elimination half-life of paliperidone was 24 hours, 40 hours, and 51 hours in subjects with mild, moderate, and severe renal impairment, respectively, compared with 23 hours in subjects with normal renal function (CrCl ≥ 80 mL/min).
Hepatic Impairment
In a study in subjects with moderate hepatic impairment (Child-Pugh class B), the plasma concentrations of free paliperidone were similar to those of healthy subjects, although total paliperidone exposure decreased because of a decrease in protein binding. Consequently, no dose adjustment is required in patients with mild or moderate hepatic impairment. INVEGA® has not been studied in patients with severe hepatic impairment.
Elderly
No dosage adjustment is recommended based on age alone. However, dose adjustment may be required because of age-related decreases in creatinine clearance [see Renal Impairment above and Dosage and Administration (2.1, 2.5)].
Race
No dosage adjustment is recommended based on race. No differences in pharmacokinetics were observed in a pharmacokinetic study conducted in Japanese and Caucasians.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies of paliperidone have not been performed.
Carcinogenicity studies of risperidone, which is extensively converted to paliperidone in rats, mice, and humans, were conducted in Swiss albino mice and Wistar rats. Risperidone was administered in the diet at daily doses of 0.63 mg/kg, 2.5 mg/kg, and 10 mg/kg for 18 months to mice and for 25 months to rats. A maximum tolerated dose was not achieved in male mice. There were statistically significant increases in pituitary gland adenomas, endocrine pancreas adenomas, and mammary gland adenocarcinomas. The no-effect dose for these tumors was less than or equal to the maximum recommended human dose of risperidone on a mg/m2 basis (see risperidone package insert). An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be mediated by prolonged dopamine D2 antagonism and hyperprolactinemia. The relevance of these tumor findings in rodents in terms of human risk is unknown [see Warnings and Precautions (5.7)].
Mutagenesis
No evidence of genotoxic potential for paliperidone was found in the Ames reverse mutation test, the mouse lymphoma assay, or the in vivo rat micronucleus test.
Impairment of Fertility
In a study of fertility, the percentage of treated female rats that became pregnant was not affected at oral doses of paliperidone of up to 2.5 mg/kg/day. However, pre- and post-implantation loss was increased, and the number of live embryos was slightly decreased, at 2.5 mg/kg, a dose that also caused slight maternal toxicity. These parameters were not affected at a dose of 0.63 mg/kg, which is half of the maximum recommended human dose on a mg/m2 basis.
The fertility of male rats was not affected at oral doses of paliperidone of up to 2.5 mg/kg/day, although sperm count and sperm viability studies were not conducted with paliperidone. In a subchronic study in Beagle dogs with risperidone, which is extensively converted to paliperidone in dogs and humans, all doses tested (0.31 mg/kg – 5.0 mg/kg) resulted in decreases in serum testosterone and in sperm motility and concentration. Serum testosterone and sperm parameters partially recovered, but remained decreased after the last observation (two months after treatment was discontinued).
14 CLINICAL STUDIES
14.1 Schizophrenia
The acute efficacy of INVEGA® (3 mg to 15 mg once daily) was established in three placebo-controlled and active-controlled (olanzapine), 6-week, fixed-dose trials in non-elderly adult subjects (mean age of 37) who met DSM-IV criteria for schizophrenia. Studies were carried out in North America, Eastern Europe, Western Europe, and Asia. The doses studied among these three trials included 3 mg/day, 6 mg/day, 9 mg/day, 12 mg/day, and 15 mg/day. Dosing was in the morning without regard to meals.
Efficacy was evaluated using the Positive and Negative Syndrome Scale (PANSS), a validated multi-item inventory composed of five factors to evaluate positive symptoms, negative symptoms, disorganized thoughts, uncontrolled hostility/excitement, and anxiety/depression. Efficacy was also evaluated using the Personal and Social Performance (PSP) scale. The PSP is a validated clinician-rated scale that measures personal and social functioning in the domains of socially useful activities (e.g., work and study), personal and social relationships, self-care, and disturbing and aggressive behaviors.
In all 3 studies (n = 1665), INVEGA® was superior to placebo on the PANSS at all doses. Mean effects at all doses were fairly similar, although the higher doses in all studies were numerically superior. INVEGA® was also superior to placebo on the PSP in these trials.
An examination of population subgroups did not reveal any evidence of differential responsiveness on the basis of gender, age (there were few patients over 65), or geographic region. There were insufficient data to explore differential effects based on race.
In a longer-term trial, adult outpatients meeting DSM-IV criteria for schizophrenia who had clinically responded (defined as PANSS score ≤ 70 or ≤ 4 on pre-defined PANSS subscales, as well as having been on a stable fixed dose of INVEGA® for the last two weeks of an 8-week run-in phase) were entered into a 6-week open-label stabilization phase where they received INVEGA® (doses ranging from 3 mg to 15 mg once daily). After the stabilization phase, patients were randomized in a double-blind manner to either continue on INVEGA® at their achieved stable dose, or to placebo, until they experienced a relapse of schizophrenia symptoms. Relapse was pre-defined as significant increase in PANSS (or pre-defined PANSS subscales), hospitalization, clinically significant suicidal or homicidal ideation, or deliberate injury to self or others. An interim analysis of the data showed a significantly longer time to relapse in patients treated with INVEGA® compared to placebo, and the trial was stopped early because maintenance of efficacy was demonstrated.
14.2 Schizoaffective Disorder
The acute efficacy of INVEGA® (3 mg to 12 mg once daily) in the treatment of schizoaffective disorder was established in two placebo-controlled, 6‑week trials in non-elderly adult subjects. Enrolled subjects 1) met DSM-IV criteria for schizoaffective disorder, as confirmed by the Structured Clinical Interview for DSM-IV Disorders, 2) had a Positive and Negative Syndrome Scale (PANSS) total score of at least 60, and 3) had prominent mood symptoms as confirmed by a score of at least 16 on the Young Mania Rating Scale and/or Hamilton Rating Scale for Depression. The population included subjects with schizoaffective bipolar and depressive types. In one of these trials, efficacy was assessed in 211 subjects who received flexible doses of INVEGA® (3-12 mg once daily). In the other study, efficacy was assessed in 203 subjects who were assigned to one of two dose levels of INVEGA®: 6 mg with the option to reduce to 3 mg (n = 105) or 12 mg with the option to reduce to 9 mg (n = 98) once daily. Both studies included subjects who received INVEGA® either as monotherapy [no mood stabilizers and/or antidepressants (55%)] or as an adjunct to mood stabilizers and/or antidepressants (45%). The most commonly used mood stabilizers were valproate and lithium. The most commonly used antidepressants were SSRIs and SNRIs. INVEGA® was dosed in the morning without regard to meals. Studies were carried out in the United States, Eastern Europe, Russia, and Asia.
Efficacy was evaluated using the PANSS, a validated multi-item inventory composed of five factors to evaluate positive symptoms, negative symptoms, disorganized thoughts, uncontrolled hostility/excitement, and anxiety/depression. As secondary outcomes, mood symptoms were evaluated using the Hamilton Depression Rating Scale (HAM-D-21) and the Young Mania Rating Scale (YMRS).
The INVEGA® group in the flexible-dose study (dosed between 3 and 12 mg/day, mean modal dose of 8.6 mg/day) and the higher dose group of INVEGA® in the 2 dose-level study (12 mg/day with option to reduce to 9 mg/day) were each superior to placebo in the PANSS. Numerical improvements in mood symptoms were also observed, as measured by the HAM-D-21 and YMRS. In the lower dose group of the 2 dose-level study (6 mg/day with option to reduce to 3 mg/day), INVEGA® was not significantly different from placebo as measured by the PANSS.
Taking the results of both studies together, INVEGA® improved the symptoms of schizoaffective disorder at endpoint relative to placebo when administered either as monotherapy or as an adjunct to mood stabilizers and/or antidepressants. An examination of population subgroups did not reveal any evidence of differential responsiveness on the basis of gender, age, or geographic region. There were insufficient data to explore differential effects based on race.
16 HOW SUPPLIED/STORAGE AND HANDLING
INVEGA® (paliperidone) Extended-Release Tablets are available in the following strengths and packages. All tablets are capsule-shaped.
6 mg tablets are beige and imprinted with "PAL 6", and are available in bottles of 30 (NDC 21695-455-30).
17 PATIENT COUNSELING INFORMATION
Physicians are advised to discuss the following issues with patients for whom they prescribe INVEGA®.
17.1 Orthostatic Hypotension
Patients should be advised that there is risk of orthostatic hypotension, particularly at the time of initiating treatment, re-initiating treatment, or increasing the dose [see Warnings and Precautions (5.9)].
17.2 Interference with Cognitive and Motor Performance
As INVEGA® has the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that INVEGA® therapy does not affect them adversely [see Warnings and Precautions (5.11)].
17.3 Pregnancy
Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during treatment with INVEGA® [see Use in Specific Populations (8.1)].
17.4 Nursing
Caution should be exercised when INVEGA® is administered to a nursing woman. The known benefits of breastfeeding should be weighed against the unknown risks of infant exposure to paliperidone. [See Use in Specific Populations (8.3)].
17.5 Concomitant Medication
Patients should be advised to inform their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs, as there is a potential for interactions [see Drug Interactions (7)].
17.6 Alcohol
Patients should be advised to avoid alcohol while taking INVEGA® [see Drug Interactions (7.1)].
17.7 Heat Exposure and Dehydration
Patients should be advised regarding appropriate care in avoiding overheating and dehydration [see Warnings and Precautions (5.17)].
17.8 Administration
Patients should be informed that INVEGA® should be swallowed whole with the aid of liquids. Tablets should not be chewed, divided, or crushed. The medication is contained within a nonabsorbable shell designed to release the drug at a controlled rate. The tablet shell, along with insoluble core components, is eliminated from the body; patients should not be concerned if they occasionally notice something that looks like a tablet in their stool [see Dosage and Administration (2.3)].
INVEGA® (paliperidone) Extended-Release Tablets
Manufactured by:
ALZA Corporation
Vacaville, CA 95688
OR
Janssen Cilag Manufacturing, LLC
Gurabo, Puerto Rico 00778
Manufactured for:
Janssen, Division of Ortho-McNeil-Janssen Pharmaceuticals, Inc.
Titusville, NJ 08560
OROS is a registered trademark of ALZA Corporation
Revised: January 2010
©Ortho-McNeil-Janssen Pharmaceuticals, Inc. 2007
Repackaged by:
Rebel Distributors Corp
Thousand Oaks, CA 91320