WARNING
This product is intended for use by physicians who are experienced in the administration of allergenic extracts and the emergency care of anaphylaxis or for use under the guidance of an allergy specialist.
Patients should be instructed to recognize adverse reaction symptoms and cautioned to contact the physician’s office if reaction symptoms occur. As with all allergenic extracts, severe systemic reactions may occur. In certain individuals, these reactions may rarely result in death. Patients should be observed for 20 to 30 minutes following treatment, and emergency measures, as well as personnel trained in their use, should be immediately available in the event of a life-threatening reaction. Patients with unstable asthma or steroid dependent asthmatics and patients with underlying cardiovascular disease are at greater risk. Adverse events are to be reported to Med Watch (1-800-FDA-1088), Adverse Event Reporting , Food and Drug Administration, 5600 Fishers Lane, Rockville, MD 20852-9787.
This product should not be injected intravenously. Deep subcutaneous routes have proven to be safe. Patients receiving beta-blockers may not be responsive to epinephrine or inhaled bronchodilators. Respiratory obstruction not responding to parenteral or inhaled bronchodilators may require theophylline, oxygen, intubation and the use of life support systems. Parenteral fluid and/or plasma expanders may be utilized for the treatment of shock. Adrenocorticosteroids may be administered parenterally or intravenously.
Refer to WARNINGS, PRECAUTIONS, and ADVERSE REACTIONS sections below.
DESCRIPTION
Sterile therapeutic extracts are supplied in either Phenol Saline Diluent or in Diluent containing Glycerin 50% (v/v) for subcutaneous injection. Inactive ingredients may include: Sodium Chloride for isotonicity, Glycerin, and Sodium Bicarbonate as buffering agents. These products are compounded and diluted on a w/v or PNU basis. Pollens are individually extracted from pure pollen extracted in a phenol-preserved sodium bicarbonate solution. Short Ragweed and Mixed (Tall and Short) Ragweed extracts are standardized by Antigen E content and so labeled. The Antigen E content of extracts containing Short Ragweed at a concentration more dilute than a weight/volume ratio of 1:10 are obtained by calculating the Antigen E content based on the assay value of more concentrated extract. Pollen extracts are filtered aseptically and, after final packaging, they are tested for sterility and safety. Molds are individually extracted from pure powdered inactivated mold source material extracted in phenol preserved saline. Mold extracts are filtered aseptically and after final packaging are tested for sterility and safety. Molds are present in all inhabited places at all seasons of the year; they are so ubiquitous that they are prevalent at times when common allergic pollens and other inhalants are not. In the home and surroundings, molds are found in upholstered furniture, mattresses, drapes, cellar and storage room dust, woolens, leather goods, fruits, meats, cheeses, garden soil and on plants. Spores, mycelial fragments and mold residues are thus inhaled, contacted and ingested continuously.
Miscellaneous inhalants and epidermals are individually extracted in phenol preserved saline, filtered aseptically and after final packaging are tested for sterility and safety.
CLINICAL PHARMACOLOGY
The treatment consists of the subcutaneous injection of gradually increasing doses of the allergens to which the patient is allergic. It has been demonstrated that this method of treatment induces an increased tolerance to the allergens responsible for the symptoms on subsequent exposure. The exact relationships between allergen, skin-sensitizing antibody (IgE) and the blocking antibody (IgG) have not been precisely established. Clinically confirmed immunological studies have adduced evidence of the efficacy of hyposensitization therapy.
Numerous controlled studies have demonstrated the clinical efficacy of immunotherapy with cat, dust mites and some pollen extracts. Nevertheless, responses are variable, and in a few studies patients reported no appreciable benefit.
Extracts containing Short Ragweed pollen bear a labeled potency declaration in terms of Antigen E content. Numerous studies have confirmed Antigen E (AgE) as the major antigen associated with Short Ragweed pollinosis.1 Therefore, it is essential that the physician be aware of AgE content of allergenic extract administered for hyposensitization therapy.
Some studies have indicated that for most patients a cumulative Antigen E dosage of less than 0.1 unit is not immunizing (sufficient to stimulate specific IgG antibodies).2 This, however, does not suggest that 0.1 unit is a maximum tolerated dose. Most moderately sensitive patients may tolerate a dosage of ten to fifty times greater. If results with this product are unsatisfactory with exquisitely sensitive patients who cannot tolerate an immunizing dose, the physician should consider alternative therapy.
One well-controlled study demonstrated that standard immunotherapy (gradually increasing doses of antigen given subcutaneously to a maximum tolerated peak dose) using crude ragweed extract of known Antigen E potency, was significantly superior to placebo and low dose immunotherapy (0.1 units AgE cumulative dose) in amelioration of symptoms associated with ragweed hay fever. These patients received a cumulative dose of 18-350 units Antigen E (median = 84.9 units). The maximum single dose ranged from 3.7 to 46.8 units (median = 11.1 units) prior to the ragweed hay fever season.10
Patients for this study were sensitive to Ragweed Antigen E, as determined by intradermal skin testing at a dose of 0.01 units AgE/mL. A series of 24 weekly injections were administered. Forty-seven percent of the patients experienced at least one systemic reaction with an average of 1.2 systemic reactions per patient. None of the patients were able to achieve the expected maximum dose (90 units of Antigen E) in the 24 weekly injection dosage schedule.
INDICATIONS AND USAGE
Hyposensitization (injection) therapy is a treatment for patients exhibiting allergic reactions to seasonal pollens, dust, molds, animal danders, various other inhalants, and in situations where the offending allergen cannot be avoided.
Prior to initiation of therapy, the clinical sensitivity should be established by careful evaluation of the patient’s history confirmed by diagnostic skin testing. Hyposensitization should not be prescribed for sensitivities to allergens which can easily be avoided.
CONTRAINDICATIONS
A patient should not be immunized with preparations of allergens to which the patient has not demonstrated symptoms, IgE antibodies, positive skin tests, or properly controlled challenge testing. In most cases, immunotherapy is not indicated for those allergens that can be eliminated or minimized by environmental control.
Patients on beta-blockers are not candidates for immunotherapy, as they can be non-responsive to beta-agonists that may be required to reverse a systemic reaction (also see WARNINGS AND ADVERSE REACTIONS).
In the presence of active symptoms such as rhinitis, wheezing, dyspnea, etc., the indication of immunotherapy must be weighed carefully against the risk of temporarily aggravating the symptoms by the injection itself.
Also, there is some evidence, although inconclusive, that routine immunizations may exacerbate autoimmune diseases.3,4,5 Hyposensitization should be given cautiously to patients with this predisposition. Patients with severe cardiorespiratory symptoms are at an additional risk during a systemic reaction. The physician must weigh risk to benefit in these cases.
WARNINGS
Patients should always be observed for at least 20-30 minutes after any injection. In the event of a marked systemic reaction, application of a tourniquet above the injection site and administration of 0.2 mL to 1 mL (0.01 mg/kg) of Epinephrine Injection (1:1,000) is recommended. Maximal recommended dose for children between 2 and 12 years is 0.5 mL. The tourniquet is then gradually released at 15 minute intervals. Patients under treatment with beta-blockers may be refractory to the usual dose of epinephrine.
Volume expanders and vasopressor agents may be required to reverse hypotension. Inhalation bronchodilators and parenteral aminophylline may be required to reverse bronchospasm. In cases of respiratory obstruction, oxygen and intubation may be necessary. Life-threatening reaction unresponsive to the above may require cardiopulmonary resuscitation.
DO NOT GIVE INTRAVENOUSLY
After inserting the needle, but before injecting the dose, pull plunger of the syringe slightly. If blood returns in the syringe, discard the syringe and contents and repeat injection at another site.
Bulk concentrated extracts must be diluted for initial therapy.
Withhold allergenic extracts temporarily or reduce the dose in patients with any one of the following conditions:
- Severe rhinitis or asthma symptoms;
- Infection or flu accompanied by fever;
- Exposure to excessive amounts of clinically relevant allergen prior to therapy.
Patients with unstable asthma or steroid dependent asthmatics and patients with underlying cardiovascular disease are at greater risk. See PRECAUTIONS AND ADVERSE REACTIONS.
TRANSFER OF PATIENTS
From pyridine extracted alum complexed allergenic extracts to aqueous extracts and glycerinated: In order to avoid untoward reaction, it is recommended that therapy be initiated as though patients were previously untreated. The first dose should be related to the patient’s sensitivity, determined by history and confirmed by skin testing.
From unstandardized aqueous extracts to standardized aqueous extracts and glycerinated: The physician should establish the potency relationship, perhaps by comparative skin testing at equal concentration, prior to injecting the first standardized dose.
From aqueous alum precipitated or modified extracts to aqueous extracts and glycerinated: Since this subject has not been studied, it is recommended that therapy be initiated as if the patient were not previously treated.
PRECAUTIONS
INFORMATION TO PATIENTS:
Patients should be instructed to describe any active allergic symptoms such as rhinitis, wheezing, dyspnea, etc. prior to injection including any late reactions from previous administration. Patients should be instructed to remain in the office for 20 to 30 minutes after injection to monitor for adverse reactions. Also, see ADVERSE REACTIONS and WARNINGS Sections.
If the protective action of allergenic extract injections is considered essential for the patient’s welfare, appropriate symptomatic therapy with antihistaminic, adrenergic or other drugs might be needed either prior to or in conjunction with the allergenic extract injections.
GENERAL:
- Objective assessment of pulmonary function such as Peak Expiratory Flow Rate (PEFR) before allergen administration may be useful in unstable asthmatic to reduce the chances of exacerbation of the patient’s asthma.
- Store allergenic extracts between 2° and 8°C at all times, even during use.
- Injections are to be given subcutaneously with the usual sterile precautions using a tuberculin syringe.
- Care must be taken to avoid injecting into a blood vessel. Pull gently on syringe plunger to determine if a blood vessel has been entered (See WARNINGS).
- Allergenic extracts slowly become less potent with age. During the course of treatment, it may be necessary to continue therapy with a vial of extract bearing a later expiration date. The initial dose of the extract bearing the later expiration date should be lowered to a safe, non-reaction eliciting level which can be confirmed by comparative skin testing using end-point titration.
- Use standard aseptic precautions when making dilutions. The first dose of the new extract should be reduced to at least 25% of the amount of the dosage from the previous extract.
- Extracts in 50% glycerin can cause discomfort at the site of the injection.
PREGNANCY - CATEGORY C:
Animal reproduction studies have not been conducted with allergenic extracts. It is also not known whether allergenic extracts can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
Controlled studies of hyposensitization with moderate to high doses of allergenic extracts during conception and all trimesters of pregnancy have failed to demonstrate any risk to the fetus or to the mother. However, on the basis of histamine’s known ability to contract uterine muscle, the release of significant amounts of histamine from allergen exposure or hyposensitization overdose should be avoided on theoretical grounds. Therefore, allergenic extracts should be used cautiously in a pregnant woman and only if clearly needed.
PEDIATRIC USE:
Children can receive the same dose as adults, however, to minimize the discomfort associated with dose volume it may be advisable to reduce the volume of the dose by one-half and administer the injection at two different sites.
NURSING MOTHERS:
It is not known if allergens administered subcutaneously appear in human milk. Because many drugs are excreted in human milk, caution should be exercised when allergenic extracts are administered to a nursing woman.
DRUG INTERACTIONS:
Drugs can interfere with the performance of skin tests.6
Antihistamines: Response to mediator (histamine) released by allergens is suppressed by antihistamines. The length of suppression varies and is dependent on individual patient, type of antihistamine and length of time the patient has been on antihistamines. The duration of this suppression may be as little as 24 hours (chlorpheniramine), and can be as long as 40 days (astemizole).
Tricyclic Antidepressants: These exert a potent and sustained decrease of skin reactivity to histamine which may last for a few weeks.
Beta2 Agonists: Oral terbutaline and parenteral ephedrine, in general, have been shown to decrease allergen induced wheal.
Dopamine: Intravenous infusion of dopamine may inhibit skin test responses.
Beta Blocking Agents: Propranolol can significantly increase skin test reactivity (See WARNINGS).
Other Drugs: Short acting steroids, inhaled beta2 agonists, theophylline and cromolyn do not seem to affect skin test response.
ADVERSE REACTIONS
Anaphylaxis and deaths following the injection of mite and other extracts have been reported by The British Committee on Safety in Medicine.7 Fatalities from immunotherapy in the United States since 1945 have been extensively reviewed by Lockey, R. F., et al8 and more recently by Reid, M. J. et al.9
With careful attention to dosage and administration, such reactions occur infrequently, but it must be remembered that allergenic extracts are highly potent to sensitive individuals and OVERDOSE could result in anaphylactic symptoms. Therefore, it is imperative that physicians administering allergenic extracts understand and be prepared for the treatment of severe reactions.
Local: Reactions at the site of injection may be immediate or delayed. Immediate wheal and erythema reactions are ordinarily of little consequence; but if very large, may be the first manifestation of a systemic reaction. If large local reactions occur, the patient should be observed for systemic symptoms for which treatment is outlined below.
Delayed reactions start several hours after injection with local edema, erythema, itching or pain. They are usually at their peak at 24 hours and usually require no treatment. Antihistamine drugs may be administered orally.
The next therapeutic dose should be reduced to the dose which did not elicit a reaction, and subsequent doses increased more slowly; i.e., use of intermediate dilutions.
Systemic: Systemic reactions are characterized by one or more of the following symptoms: Sneezing, mild to severe generalized urticaria, itching other than at the injection site, extensive or generalized edema, wheezing, asthma, dyspnea, cyanosis, tachycardia, lacrimation, marked perspiration, cough, hypotension, syncope and upper airway obstruction. Symptoms may progress to shock and death. Patients should always be observed for at least 20 to 30 minutes after any injection. Volume expanders and vasopressor agents may be required to reverse hypotension. Inhalational bronchodilators and parenteral aminophylline may be required to reverse bronchospasm. Severe airway obstruction, unresponsive to bronchodilator, may require tracheal intubation and use of oxygen. In the event of a marked systemic reaction, application of a tourniquet above the injection site and the administration of 0.2 mL to 1 mL of Epinephrine Injection (1:1,000) are recommended. Maximal recommended dose for children under 2 years of age is 0.3 mL. Maximal recommended dose for children between 2 and 12 years of age is 0.5 mL. The tourniquet should not be left in place without loosening for 90 seconds every 15 minutes.
The next therapeutic injection of extract should be reduced to the dose which did not elicit a reaction, and subsequent doses increased more slowly; i.e., use of intermediate dilutions.
OVERDOSAGE
Signs and symptoms of overdose are typically local and systemic reactions. For a description and management of overdose reactions, refer to “Adverse Reaction” section above.
DOSAGE AND ADMINISTRATION
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
When diluting bulk extracts, use of Sterile Diluent for Allergenic Extracts or Sterile Diluent for Allergenic Extracts Normal Saline with HSA (albumin saline) is recommended. Dilutions should be made with sterile disposable syringes using aseptic technique. Commonly, 10 fold dilutions are used to achieve a desired concentration for initiation and continuation of immunotherapy. For example, transferring 0.5 mL of a 10,000 PNU/mL extract into 4.5 mL of diluent will yield 5 mL of extract at 1,000 PNU/mL. For weight volume products, a 1:100 w/v dilution may be prepared from a 1:10 w/v by transferring 0.5 mL of the 1:10 w/v to 4.5 mL of diluent. Prepare as many additional serial dilutions as necessary to reach the appropriate concentration.
Starting dose for immunotherapy is related directly to a patient’s sensitivity as determined by carefully executed skin testing. Degree of sensitivity can be established by determination of D50.11 A general rule is to begin at 1/10 of the dose that produces sum of erythema of 50 mm (approximately a 2+ positive skin test reaction).
For example, if a patient exhibits a 2+ intradermal reaction to 1 AU/mL, the first dose should be no higher than 0.05 mL of 0.1 AU/mL. Dosage may be increased by 0.05 mL each time until 0.5 mL is reached, at which time the next 10-fold more concentrated dilution can be used, beginning with 0.05 mL, if no untoward reaction is observed.
Interval between doses in the early stages of immunotherapy is no more than once to twice a week, and may gradually be increased to once every two weeks. Generally, maintenance injections may be given as infrequently as once every two weeks to once a month.
Injections are given subcutaneously, preferably in the arm. It is advantageous to give injections in alternate arms and routinely in the same area. In some patients, a local tolerance to the allergen may develop thus preventing a possible severe local reaction.
Formal stability studies for diluted and undiluted forms of unstandardized extracts have not been performed; therefore, it is recommended that minimal amounts of the concentrate be diluted so that the diluted product is used up within a relatively short period of time; i.e., preferably not more than four weeks.
PRE-SEASONAL METHOD OF TREATMENT
Treatment of hay fever by the pre-seasonal method should be started 6-10 weeks prior to the usual onset of symptoms. Therapy should be started early enough to permit a graduated series of doses at 2-7 day intervals. It is recommended that the larger doses be spaced 5-7 days apart.
Some physicians continue therapy into or through the season by repeating a reduced or MAINTENANCE dose at weekly or biweekly intervals. If during the season, hay fever symptoms develop, relief may be provided by giving supplemental treatment. If the last dose was well-tolerated and not more than 2 weeks has elapsed since it was given, this dose may be given again and repeated every 4 to 7 days.
PERENNIAL TREATMENT
The patient’s tolerance to the offending pollen or pollens is first established by the injection of a series of graduated doses as outlined in the PRE-SEASONAL METHOD, not necessarily given pre-seasonally, since perennial therapy may be begun at any time. After completion of the ascending series of injections, from 1/4 to 1/2 of the highest well-tolerated dose is continued at 2 to 3 week intervals throughout the year. Shortly before the usual onset of symptoms (4 to 5 weeks prior to the season) the interval between injections is shortened and the dosage is gradually increased, according to the Pre-Seasonal schedule, until maximum well-tolerated dose is again attained. This top dose should be reached just before the usual onset of symptoms at which time the treatment is discontinued. If patient’s symptoms persist, therapy may be continued at a reduced dosage level, usually 1/4 to 1/2 of the top dose.
DOSAGE ADJUSTMENTS
For Products Containing Short Ragweed.
In transferring patients from unstandardized to standardized product, the physician should establish the potency relationships, perhaps by comparative skin testing, prior to injecting the first standardized dose.
AgE is important in adjusting dosage of Short Ragweed extracts to accurately transfer a patient from older extracts to fresher material. In such cases, the dosage of AgE should be considered in addition to the W/V dilution or protein nitrogen units. Antigen E concentration continuously declines in Short Ragweed Pollen extracts at a rate that varies with the formulation of the product. Aqueous extracts retain Antigen E potency less effectively than glycerin 50% (v/v) extracts. These differences are reflected in the expiration date declared on the vial. The continuous decline should be considered. Also, where ragweed is a component of an allergen mixture, clinical response to the other components must be considered in adjustment of dosage based on AgE content alone. The usual course of immunotherapy is three to five years.
Caution: A small percent of individuals allergic to Short Ragweed are more sensitive to minor antigens such as Ra3 Ra5 than AgE. There is no correlation between the amount of these antigens and either AgE or PNU content.
NOTE: For extracts of Short Ragweed or equal part mixture of Short and Tall Ragweed refer to AgE dosage schedule. The AgE content for those products is indicated on the vial label. The physician may use the formula below to determine the AgE dosage for each injection.
AgE dosage can be monitored by using the following formula:
W/V compounded products:
Labeled AgE X Dose (mL) = dose in AgE
PNU compounded products:
Labeled AgE/mL X dose in PNU = dose in AgE
Labeled PNU/mL
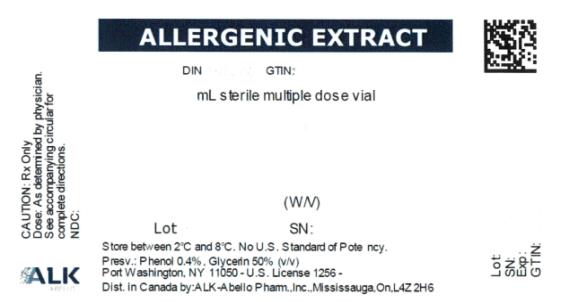
HOW SUPPLIED
- Concentrate in multiple dose vials:
- Sterile Diluent for Allergenic Extracts (Phenol Saline) is supplied in vials of 4.5 mL, 9.0 mL, 30 mL and 100 mL.
10 mL and 50 mL, single antigens or specified mixtures, potency expressed in PNU/mL (up to and including 100,000 PNU/mL) or W/V (up to and including 1:10 W/V), aqueous or in 50% glycerin, to be diluted prior to use. 1:10 w/v short ragweed extracts contain ≥ 300 units/mL of AgE.
STORAGE: To maintain stability of allergenic extracts, proper storage conditions are essential. Bulk concentrates and diluted extracts are to be stored at 2° to 8° C even during use. Bulk or diluted extracts are not to be frozen. Do not use after the expiration date shown on the vial label.
REFERENCES
- Norman, P.S. et al: Immunotherapy of hayfever with ragweed antigen E. Comparisons with whole pollen extract and placebo. J. Allergy 42:93, 1968.
- Van Metre, T.E. et al: A controlled study of the effectiveness of the Rinkel method of immunotherapy for ragweed pollen hayfever. J. Allergy Clin. Immunol. 65:288, 1980.
- Umetsu, D.T. et al: Serum sickness triggered by anaphylaxis: a complication of immunotherapy. J. Allergy Clin. Immunol. 76:713, 1985.
- Phannphak, P. and Kohler, P.F.: Onset of polyarteritis nodosa during allergic hyposenitization treatment. Am. J. Med. 68:479, 1980.
- Kohler, P.F.: Immune complexes and allergic disease. In: Middleton et al: Allergy Principles and Practice 3rd Ed. St. Louis: CV Mosby, 1988:167.
- Bousquet, J.: In vivo methods for the study of allergy: skin test, techniques, and interpretation. In: Middleton et al: Allergy Principles and Practice 3rd Ed. St. Louis: CV Mosby, 1988:167.
- Committee on the Safety of Medicines. CSM update: desensitising vaccines. Brit Med. J. 293:948,1986.
- Lockey, R.F. et al: Fatalities from immunotherapy (IT) and skin testing (ST). J. Allergy Clin. Immunol. 79:660, 1987.
- Reid, M.J. et al: Survey of fatalities from skin testing and immunotherapy. 1985-1989. J. Allergy Clin. Immunol.;92:6, 1993.
- Van Metre, T.E. et al: A controlled study of the effectiveness of the Rinkel method and the current standard method of immunotherapy for ragweed pollen hayfever. J. Allergy Clin. Immunol. 66:500, 1980.
- Turkeltaub, P.C., Rastogi, S.C., Baer, H., et al: A standardized quantitative skin-test assay of allergen potency and stability: studies on the allergen dose-response curve and effect of wheal, erythema, and patient selection on assay results, J. Allergy Clin. Immunol. 70:343, 1982.
Revised April 2017 158M
© ALK-Abelló, Inc.
Distributed in Canada by:
ALK-Abelló Pharmaceuticals, Inc.
#35-151 Brunel Road
Mississauga, Ontario
Canada L4Z 2H6