COLESEVELAM HYDROCHLORIDE- colesevelam hydrochloride tablet, coated
AvKARE
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONColesevelam Hydrochloride Tablets
Rx Only These highlights do not include all the information needed to use colesevelam hydrochloride safely and effectively. See full prescribing information for colesevelam hydrochloride. COLESEVELAM hydrochloride tablets, for oral use Initial U.S. Approval: 2000 INDICATIONS AND USAGEColesevelam hydrochloride is a bile acid sequestrant indicated as an adjunct to diet and exercise to
Important Limitations of Use ( 1.3):
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSTablets: 625 mg ( 3) CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSIn clinical trials, the most common (incidence ≥2% and greater than placebo) adverse reactions with colesevelam hydrochloride included constipation, dyspepsia, and nausea. Post-marketing reports with concomitant colesevelam hydrochloride administration include:
Other post-marketing reports include bowel obstruction, dysphagia, esophageal obstruction, fecal impaction, hypertriglyceridemia, pancreatitis, and increased transaminases ( 5.5, 6.2, 7, 12.3).
To report SUSPECTED ADVERSE REACTIONS, contact AvKARE, Inc. at 1-855-361-3993; email drugsafety@avkare.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONSIn drug interaction studies, colesevelam hydrochloride reduced levels of cyclosporine, glimepiride, glipizide, glyburide, levothyroxine, olmesartan medoxomil, and oral contraceptives containing ethinyl estradiol and norethindrone. Colesevelam hydrochloride increased levels of metformin when coadministered with metformin extended release. There have been post-marketing reports of decreases in phenytoin levels in patients receiving phenytoin concomitantly with colesevelam hydrochloride and decreases in INR in patients receiving warfarin concomitantly with colesevelam hydrochloride ( 5.5, 7, 12.3). See 17 for PATIENT COUNSELING INFORMATION. Revised: 2/2016 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Primary Hyperlipidemia
Colesevelam hydrochloride is indicated as an adjunct to diet and exercise to reduce elevated low-density lipoprotein cholesterol (LDL-C) in adults with primary hyperlipidemia (Fredrickson Type IIa) as monotherapy or in combination with a hydroxymethyl-glutaryl-coenzyme A (HMG CoA) reductase inhibitor (statin).
Colesevelam hydrochloride is indicated as monotherapy or in combination with a statin to reduce LDL-C levels in boys and post-menarchal girls, 10 to 17 years of age, with heterozygous familial hypercholesterolemia if after an adequate trial of diet therapy the following findings are present:
a. LDL-C remains ≥190 mg/dL or
b. LDL-C remains ≥160 mg/dL and
- there is a positive family history of premature cardiovascular disease or
- two or more other CVD risk factors are present in the pediatric patient.
Lipid-altering agents should be used in addition to a diet restricted in saturated fat and cholesterol when response to diet and non-pharmacological interventions alone has been inadequate [see Clinical Studies (14.1)] .
In patients with coronary heart disease (CHD) or CHD risk equivalents such as diabetes mellitus, LDL-C treatment goals are <100 mg/dL. An LDL-C goal of <70 mg/dL is a therapeutic option on the basis of recent trial evidence. If LDL-C is at goal but the serum triglyceride (TG) value is >200 mg/dL, then non-HDL cholesterol (non-HDL-C) (total cholesterol [TC] minus high density lipoprotein cholesterol [HDL-C]) becomes a secondary target of therapy. The goal for non-HDL-C in persons with high serum TG is set at 30 mg/dL higher than that for LDL-C.
1.3 Important Limitations of Use
- Colesevelam hydrochloride should not be used for the treatment of type 1 diabetes or for the treatment of diabetic ketoacidosis.
- Colesevelam hydrochloride has not been studied in type 2 diabetes in combination with a dipeptidyl peptidase 4 inhibitor.
- Colesevelam hydrochloride has not been studied in pediatric patients with type 2 diabetes.
- Colesevelam hydrochloride has not been studied in Fredrickson Type I, III, IV, and V dyslipidemias.
- Colesevelam hydrochloride has not been studied in children younger than 10 years of age or in pre-menarchal girls.
2 DOSAGE AND ADMINISTRATION
2.1 Primary Hyperlipidemia
The recommended dose of colesevelam hydrochloride tablets in adults, whether used as monotherapy or in combination with a statin, is 6 tablets once daily or 3 tablets twice daily. Colesevelam hydrochloride tablets should be taken with a meal and liquid.
Colesevelam hydrochloride can be dosed at the same time as a statin or the two drugs can be dosed apart [see Clinical Studies (14.1)] .
After initiation of colesevelam hydrochloride, lipid levels should be analyzed within 4 to 6 weeks.
3 DOSAGE FORMS AND STRENGTHS
- 625 mg tablets are off-white to pale yellow film-coated oval tablets, debossed with "L61" on one side and plain on the other side.
4 CONTRAINDICATIONS
Colesevelam hydrochloride is contraindicated in patients with
- A history of bowel obstruction [see Warnings and Precautions (5.4)]
- Serum TG concentrations >500 mg/dL [see Warnings and Precautions (5.2)]
- A history of hypertriglyceridemia-induced pancreatitis [see Warnings and Precautions (5.2)]
5 WARNINGS AND PRECAUTIONS
5.1 General
The effect of colesevelam hydrochloride on cardiovascular morbidity and mortality has not been determined.
5.2 Serum Triglycerides
Colesevelam hydrochloride, like other bile acid sequestrants, can increase serum TG concentrations.
Colesevelam hydrochloride had small effects on serum TG (median increase 5% compared to placebo) in trials of patients with primary hyperlipidemia [see Adverse Reactions (6.1) and Clinical Studies (14.1)] .
Hypertriglyceridemia of sufficient severity can cause acute pancreatitis. The long-term effect of hypertriglyceridemia on the risk of coronary artery disease is uncertain. Caution should be exercised when treating patients with TG levels greater than 300 mg/dL. Because most patients in the colesevelam hydrochloride clinical trials had baseline TG <300 mg/dL, it is unknown whether patients with more uncontrolled baseline hypertriglyceridemia would have greater increases in serum TG levels with colesevelam hydrochloride. In addition, the use of colesevelam hydrochloride is contraindicated in patients with TG levels >500 mg/dL [see Contraindications (4)] . Lipid parameters, including TG levels and non-HDL-C, should be obtained before starting colesevelam hydrochloride and periodically thereafter. Colesevelam hydrochloride should be discontinued if TG levels exceed 500 mg/dL or if the patient develops hypertriglyceridemia-induced pancreatitis [see Adverse Reactions (6.1)] .
5.3 Vitamin K or Fat-Soluble Vitamin Deficiencies Precautions
Bile acid sequestrants may decrease the absorption of fat-soluble vitamins A, D, E, and K. No specific clinical studies have been conducted to evaluate the effects of colesevelam hydrochloride on the absorption of co-administered dietary or supplemental vitamin therapy. In nonclinical safety studies, rats administered colesevelam hydrochloride at doses greater than 30-fold the projected human clinical dose experienced hemorrhage from vitamin K deficiency. Patients on oral vitamin supplementation should take their vitamins at least 4 hours prior to colesevelam hydrochloride. Caution should be exercised when treating patients with a susceptibility to deficiencies of vitamin K (e.g., patients on warfarin, patients with malabsorption syndromes) or other fat-soluble vitamins.
5.4 Gastrointestinal Disorders
Because of its constipating effects, colesevelam hydrochloride is not recommended in patients with gastroparesis, other gastrointestinal motility disorders, and in those who have had major gastrointestinal tract surgery and who may be at risk for bowel obstruction. Because of the tablet size, colesevelam hydrochloride tablets can cause dysphagia or esophageal obstruction and should be used with caution in patients with dysphagia or swallowing disorders.
5.5 Drug Interactions
Colesevelam hydrochloride reduces gastrointestinal absorption of some drugs. Drugs with a known interaction with colesevelam should be administered at least 4 hours prior to colesevelam hydrochloride. Drugs that have not been tested for interaction with colesevelam, especially those with a narrow therapeutic index, should also be administered at least 4 hours prior to colesevelam hydrochloride. Alternatively, the physician should monitor drug levels of the co-administered drug [see Drug Interactions (7) and Clinical Pharmacology (12.3)] .
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in clinical studies of another drug and may not reflect the rates observed in practice.
Primary Hyperlipidemia: In 7 double-blind, placebo-controlled, clinical trials, 807 patients with primary hyperlipidemia (age range 18 to 86 years, 50% women, 90% Caucasians, 7% Blacks, 2% Hispanics, 1% Asians) and elevated LDL-C were treated with colesevelam hydrochloride 1.5 g/day to 4.5 g/day from 4 to 24 weeks (total exposure 199 patient-years).
In clinical trials for the reduction of LDL-C, 68% of patients receiving colesevelam hydrochloride vs. 64% of patients receiving placebo reported an adverse reaction.
| Number of Patients (%) | ||
|---|---|---|
| Colesevelam Hydrochloride
N=807 | Placebo
N=258 |
|
| Constipation | 89 (11.0) | 18 (7.0) |
| Dyspepsia | 67 (8.3) | 9 (3.5) |
| Nausea | 34 (4.2) | 10 (3.9) |
| Accidental injury | 30 (3.7) | 7 (2.7) |
| Asthenia | 29 (3.6) | 5 (1.9) |
| Pharyngitis | 26 (3.2) | 5 (1.9) |
| Flu syndrome | 26 (3.2) | 8 (3.1) |
| Rhinitis | 26 (3.2) | 8 (3.1) |
| Myalgia | 17 (2.1) | 1 (0.4) |
Pediatric Patients 10 to 17 Years of Age: In an 8-week double-blind, placebo-controlled study boys and post-menarchal girls, 10 to 17 years of age, with heterozygous familial hypercholesterolemia (heFH) (n=129), were treated with colesevelam hydrochloride tablets (1.9 to 3.8 g, daily) or placebo tablets [see Clinical Studies (14.1)] .
| Number of Patients (%) | ||
|---|---|---|
| Colesevelam Hydrochloride
N=129 | Placebo
N=65 |
|
| Nasopharyngitis | 8 (6.2) | 3 (4.6) |
| Headache | 5 (3.9) | 2 (3.1) |
| Fatigue | 5 (3.9) | 1 (1.5) |
| Creatine Phosphokinase Increase | 3 (2.3) | 0 (0.0) |
| Rhinitis | 3 (2.3) | 0 (0.0) |
| Vomiting | 3 (2.3) | 1 (1.5) |
The reported adverse reactions during the additional 18-week open-label treatment period with colesevelam hydrochloride 3.8 g per day were similar to those during the double-blind period and included headache (7.6%), nasopharyngitis (5.4%), upper respiratory tract infection (4.9%), influenza (3.8%), and nausea (3.8%) [see Clinical Studies (14.1)] .
Hypertriglyceridemia: Colesevelam hydrochloride resulted in a median increase in serum TG of 5% compared to placebo (p=0.42) in a 24-week monotherapy lipid-lowering trial [see Clinical Studies (14.1)] .
6.2 Post-Marketing Experience
The following additional adverse reactions have been identified during post-approval use of colesevelam hydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Drug Interactions with concomitant colesevelam hydrochloride administration include:
- Increased seizure activity or decreased phenytoin levels in patients receiving phenytoin. Phenytoin should be administered 4 hours prior to colesevelam hydrochloride.
- Reduced International Normalized Ratio (INR) in patients receiving warfarin therapy. In warfarin-treated patients, INR should be monitored frequently during colesevelam hydrochloride initiation then periodically thereafter.
- Elevated thyroid-stimulating hormone (TSH) in patients receiving thyroid hormone replacement therapy. Thyroid hormone replacement should be administered 4 hours prior to colesevelam hydrochloride [see Drug Interactions (7)] .
Gastrointestinal Adverse Reactions
Bowel obstruction (in patients with a history of bowel obstruction or resection), dysphagia or esophageal obstruction (occasionally requiring medical intervention), fecal impaction, pancreatitis, abdominal distension, exacerbation of hemorrhoids, and increased transaminases.
7 DRUG INTERACTIONS
Table 4 lists the drugs that have been tested in in vitro binding, in vivo drug interaction studies with colesevelam and/or drugs with post-marketing reports consistent with potential drug-drug interactions. Orally administered drugs that have not been tested for interaction with colesevelam, especially those with a narrow therapeutic index, should also be administered at least 4 hours prior to colesevelam hydrochloride. Alternatively, the physician should monitor drug levels of the co-administered drug.
|
|
| Drugs with a known interaction with colesevelam:
Decrease in exposure of co-administered drug | cyclosporine *, glimepiride †, glipizide †, glyburide †, levothyroxine †, olmesartan medoxomil †, and oral contraceptives containing ethinyl estradiol and norethindrone † |
| Drugs with a known interaction with colesevelam:
Increase in exposure of coadministered drug | metformin extended release (ER) ‡ |
| Drug(s) with post-marketing reports consistent with potential drug-drug interactions when co-administered with colesevelam hydrochloride | phenytoin †, warfarin § |
| Drugs that do not interact with colesevelam based on in vitro or in vivo testing | aspirin, atenolol, cephalexin, ciprofloxacin, digoxin, enalapril, fenofibrate, lovastatin, metformin, metoprolol, phenytoin †, pioglitazone, rosiglitazone, quinidine, repaglinide, sitagliptin, valproic acid, verapamil, warfarin § |
In an in vivo drug interaction study, colesevelam hydrochloride and warfarin co-administration had no effect on warfarin drug levels. This study did not assess the effect of colesevelam hydrochloride and warfarin co-administration on INR. In post-marketing reports, concomitant use of colesevelam hydrochloride and warfarin has been associated with reduced INR. Therefore, in patients on warfarin therapy, the INR should be monitored before initiating colesevelam hydrochloride and frequently enough during early colesevelam hydrochloride therapy to ensure that no significant alteration in INR occurs. Once the INR is stable, continue to monitor the INR at intervals usually recommended for patients on warfarin [see Post-Marketing Experience (6.2)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B. There are no adequate and well-controlled studies of colesevelam use in pregnant women. Animal reproduction studies in rats and rabbits revealed no evidence of fetal harm. Requirements for vitamins and other nutrients are increased in pregnancy. However, the effect of colesevelam on the absorption of fat-soluble vitamins has not been studied in pregnant women. This drug should be used during pregnancy only if clearly needed.
In animal reproduction studies, colesevelam revealed no evidence of fetal harm when administered to rats and rabbits at doses 50 and 17 times the maximum human dose, respectively. Because animal reproduction studies are not always predictive of human response, this drug should be used in pregnancy only if clearly needed.
8.3 Nursing Mothers
Colesevelam hydrochloride is not expected to be excreted in human milk because colesevelam hydrochloride is not absorbed systemically from the gastrointestinal tract.
8.4 Pediatric Use
The safety and effectiveness of colesevelam hydrochloride as monotherapy or in combination with a statin were evaluated in children, 10 to 17 years of age with heFH [see Clinical Studies (14.1)] . The adverse reaction profile was similar to that of patients treated with placebo. In this limited controlled study, there were no significant effects of growth, sexual maturation, fat-soluble vitamin levels or clotting factors in the adolescent boys or girls relative to placebo [see Adverse Reactions (6.1)] .
Due to tablet size, colesevelam hydrochloride for oral suspension is recommended for use in the pediatric population.
Dose adjustments are not required when colesevelam hydrochloride is administered to children 10 to 17 years of age.
Colesevelam hydrochloride has not been studied in children younger than 10 years of age or in pre-menarchal girls.
8.5 Geriatric Use
Primary Hyperlipidemia: Of the 1350 patients enrolled in the hyperlipidemia clinical studies, 349 (26%) were ≥65 years old, and 58 (4%) were ≥75 years old. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Hepatic Impairment
No special considerations or dosage adjustments are recommended when colesevelam hydrochloride is administered to patients with hepatic impairment.
To report SUSPECTED ADVERSE REACTIONS contact AvKARE, Inc. at 1-855-361-3993; email drugsafety@avkare.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
10 OVERDOSAGE
Doses of colesevelam hydrochloride in excess of 4.5 g/day have not been tested. Because colesevelam hydrochloride is not absorbed, the risk of systemic toxicity is low. However, excessive doses of colesevelam hydrochloride may cause more severe local gastrointestinal effects (e.g., constipation) than recommended doses.
11 DESCRIPTION
Colesevelam hydrochloride is a non-absorbed, polymeric, lipid-lowering and glucose-lowering agent intended for oral administration. Colesevelam hydrochloride is a high-capacity bile acid-binding molecule.
Colesevelam hydrochloride is poly(allylamine hydrochloride) cross-linked with epichlorohydrin and alkylated with 1-bromodecane and (6-bromohexyl)-trimethylammonium bromide. The chemical name (IUPAC) of colesevelam hydrochloride is allylamine polymer with 1-chloro-2,3-epoxypropane, [6-(allylamino)-hexyl]trimethylammonium chloride and N-allyldecylamine, hydrochloride. The chemical structure of colesevelam hydrochloride is represented by the following formula:
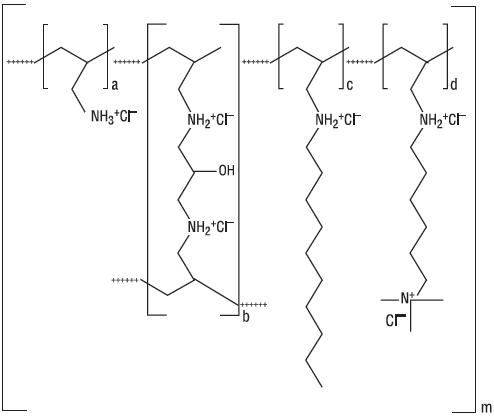
wherein (a) represents allyl amine monomer units that have not been alkylated by either of the 1-bromodecane or (6-bromohexyl)-trimethylammonium bromide alkylating agents or cross-linked by epichlorohydrin; (b) represents allyl amine units that have undergone cross-linking with epichlorohydrin; (c) represents allyl amine units that have been alkylated with a decyl group; (d) represents allyl amine units that have been alkylated with a (6-trimethylammonium) hexyl group, and m represents a number ≥100 to indicate an extended polymer network. A small amount of the amines are dialkylated, and are not depicted in the formula above. No regular order of the groups is implied by the structure; cross-linking and alkylation are expected to occur randomly along the polymer chains. A large amount of the amines are protonated. The polymer is depicted in the hydrochloride form; a small amount of the halides are bromide. Colesevelam hydrochloride is hydrophilic and insoluble in water.
Colesevelam hydrochloride tablets are off-white to pale yellow film-coated oval tablets, debossed with "L61" on one side and plain on the other side, containing 625 mg colesevelam hydrochloride. In addition, each tablet contains the following inactive ingredients: colloidal silicon dioxide, copovidone, hypromellose, magnesium stearate, microcrystalline cellulose, polyethylene glycol, and talc.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Primary Hyperlipidemia: Colesevelam hydrochloride, the active pharmaceutical ingredient in colesevelam hydrochloride tablets, is a non-absorbed, lipid-lowering polymer that binds bile acids in the intestine, impeding their re-absorption. As the bile acid pool becomes depleted, the hepatic enzyme, cholesterol 7-α-hydroxylase, is up-regulated, which increases the conversion of cholesterol to bile acids. This causes an increased demand for cholesterol in the liver cells, resulting in the dual effect of increasing transcription and activity of the cholesterol biosynthetic enzyme, HMG-CoA reductase, and increasing the number of hepatic LDL receptors. These compensatory effects result in increased clearance of LDL-C from the blood, resulting in decreased serum LDL-C levels. Serum TG levels may increase or remain unchanged.
12.2 Pharmacodynamics
A maximum therapeutic response to the lipid-lowering effects of colesevelam hydrochloride was achieved within 2 weeks and was maintained during long-term therapy.
12.3 Pharmacokinetics
Absorption: Colesevelam hydrochloride is a hydrophilic, water-insoluble polymer that is not hydrolyzed by digestive enzymes and is not absorbed.
Distribution: Colesevelam hydrochloride is not absorbed, and therefore, its distribution is limited to the gastrointestinal tract.
Metabolism: Colesevelam hydrochloride is not metabolized systemically and does not interfere with systemic drug-metabolizing enzymes such as cytochrome P-450.
Excretion: In 16 healthy volunteers, an average of 0.05% of administered radioactivity from a single 14C-labeled colesevelam hydrochloride dose was excreted in the urine.
Drug Interactions: Drug interactions between colesevelam and concomitantly administered drugs were screened through in vitro studies and confirmed in in vivo studies. In vitro studies demonstrated that cephalexin, metformin, and ciprofloxacin had negligible binding to colesevelam hydrochloride. Therefore, an in vivo pharmacokinetic interaction of colesevelam hydrochloride with these drugs is unlikely. Colesevelam hydrochloride was found to have no significant effect on the bioavailability of aspirin, atenolol, digoxin, enalapril, fenofibrate, lovastatin, metoprolol, phenytoin, pioglitazone, quinidine, rosiglitazone, sitagliptin, valproic acid, and warfarin. The results of additional in vivo drug interactions of colesevelam hydrochloride are presented in Table 5.
| Drug | Dose | Co-administered | 1 hr prior to Colesevelam Hydrochloride | 4 hr prior to Colesevelam Hydrochloride | |||
|---|---|---|---|---|---|---|---|
| AUC 0 to ∞ | C max | AUC 0 to ∞ | C max | AUC 0 to ∞ | C max | ||
| N/A — Not Available | |||||||
|
|||||||
| Cyclosporine † | 200 mg | -34% | -44% | N/A | N/A | N/A | N/A |
| Ethinyl Estradiol ठ| 0.035 mg | -24% | -24% | -18% | -1% | -12% | 0% |
| Glimepiride § | 4 mg | -18% | -8% | N/A | N/A | -6% | 3% |
| Glipizide § | 20 mg | -12% | -13% | N/A | N/A | -4% | 0% |
| Glyburide § | 3 mg | -32% | -47% | -20% | -15% | -7% | 4% |
| Levothyroxine § | 600 mcg | -22% | -33% | 6% | -2% | 1% | 8% |
| Metformin ER ¶ | 1500 mg | 44% | 8% | N/A | N/A | N/A | N/A |
| Norethindrone ठ| 1 mg | -1% | -20% | 5% | -3% | 6% | 7% |
| Olmesartan Medoxomil § | 40 mg | -39% | -28% | N/A | N/A | -15% | -4% |
| Repaglinide | 2 mg | -7% | -19% | -6% | -1% | N/A | N/A |
| Verapamil sustained-release | 240 mg | -31% | -11% | N/A | N/A | N/A | N/A |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis: A 104-week carcinogenicity study with colesevelam hydrochloride was conducted in CD-1 mice, at oral dietary doses up to 3 g/kg/day. This dose was approximately 50 times the maximum recommended human dose of 4.5 g/day, based on body weight, mg/kg. There were no significant drug-induced tumor findings in male or female mice. In a 104-week carcinogenicity study with colesevelam hydrochloride in Harlan Sprague-Dawley rats, a statistically significant increase in the incidence of pancreatic acinar cell adenoma was seen in male rats at doses >1.2 g/kg/day (approximately 20 times the maximum human dose, based on body weight, mg/kg) (trend test only). A statistically significant increase in thyroid C-cell adenoma was seen in female rats at 2.4 g/kg/day (approximately 40 times the maximum human dose, based on body weight, mg/kg).
Mutagenesis: Colesevelam hydrochloride and 4 degradants present in the drug substance have been evaluated for mutagenicity in the Ames test and a mammalian chromosomal aberration test. The 4 degradants and an extract of the parent compound did not exhibit genetic toxicity in an in vitro bacterial mutagenesis assay in S.typhimurium and E. coli (Ames assay) with or without rat liver metabolic activation. An extract of the parent compound was positive in the Chinese Hamster Ovary (CHO) cell chromosomal aberration assay in the presence of metabolic activation and negative in the absence of metabolic activation. The results of the CHO cell chromosomal aberration assay with 2 of the 4 degradants, decylamine HCl and aminohexyltrimethyl ammonium chloride HCl, were equivocal in the absence of metabolic activation and negative in the presence of metabolic activation. The other 2 degradants, didecylamine HCl and 6-decylaminohexyltrimethyl ammonium chloride HCl, were negative in the presence and absence of metabolic activation.
13.2 Animal Toxicology and/or Pharmacology
Reproductive Toxicology Studies
Reproduction studies have been performed in rats and rabbits at doses up to 3 g/kg/day and 1 g/kg/day, respectively (approximately 50 and 17 times the maximum human dose, based on body weight, mg/kg) and have revealed no evidence of harm to the fetus due to colesevelam hydrochloride.
14 CLINICAL STUDIES
14.1 Primary Hyperlipidemia
Colesevelam hydrochloride reduces TC, LDL-C, apolipoprotein B (Apo B), and non-HDL-C when administered alone or in combination with a statin in patients with primary hyperlipidemia.
Approximately 1600 patients were studied in 9 clinical trials with treatment durations ranging from 4 to 50 weeks. With the exception of one open-label, uncontrolled, long-term extension study, all studies were multicenter, randomized, double-blind, and placebo-controlled. A maximum therapeutic response to colesevelam hydrochloride was achieved within 2 weeks and was maintained during long-term therapy.
Monotherapy: In a study in patients with LDL-C between 130 mg/dL and 220 mg/dL (mean 158 mg/dL), colesevelam hydrochloride was given for 24 weeks in divided doses with the morning and evening meals.
As shown in Table 6, the mean LDL-C reductions were 15% and 18% at the 3.8 g and 4.5 g doses. The respective mean TC reductions were 7% and 10%. The mean Apo B reductions were 12% in both treatment groups. Colesevelam hydrochloride at both doses increased HDL-C by 3%. Increases in TG of 9 to 10% were observed at both colesevelam hydrochloride doses but the changes were not statistically different from placebo.
| Grams/Day | N | TC | LDL-C | Apo B | HDL-C * | Non-HDL-C | TG * |
|---|---|---|---|---|---|---|---|
| Placebo | 88 | +1 | 0 | 0 | -1 | +1 | +5 |
| 3.8 g (6 tablets) | 95 | -7 † | -15 † | -12 † | +3 † | -10 † | +10 |
| 4.5 g (7 tablets) | 94 | -10 † | -18 † | -12 † | +3 | -13 † | +9 |
In a study in 98 patients with LDL-C between 145 mg/dL and 250 mg/dL (mean 169 mg/dL), colesevelam hydrochloride 3.8 g was given for 6 weeks as a single dose with breakfast, as a single dose with dinner, or as divided doses with breakfast and dinner. The mean LDL-C reductions were 18%, 15%, and 18% for the 3 dosing regimens, respectively. The reductions with these 3 regimens were not statistically different from one another.
Combination Therapy: Co-administration of colesevelam hydrochloride and a statin (atorvastatin, lovastatin, or simvastatin) in 3 clinical studies demonstrated an additive reduction of LDL-C. The mean baseline LDL-C was 184 mg/dL in the atorvastatin study (range 156 to 236 mg/dL), 171 mg/dL in the lovastatin study (range 115 to 247 mg/dL), and 188 mg/dL in the simvastatin study (range 148 to 352 mg/dL). As demonstrated in Table 7, colesevelam hydrochloride doses of 2.3 g to 3.8 g resulted in an additional 8% to 16% reduction in LDL-C above that seen with the statin alone.
| Dose/Day | N | TC | LDL-C | Apo B | HDL-C * | Non-HDL-C | TG * |
|---|---|---|---|---|---|---|---|
| Atorvastatin Trial (4-week) | |||||||
| Placebo | 19 | +4 | +3 | -3 | +4 | +4 | +10 |
| Atorvastatin 10 mg | 18 | -27 † | -38 † | -32 † | +8 | -35 † | -24 † |
| Colesevelam Hydrochloride 3.8 g/ Atorvastatin 10 mg | 18 | -31 † | -48 † | -38 † | +11 | -40 † | -1 |
| Atorvastatin 80 mg | 20 | -39 † | -53 † | -46 † | +6 | -50 † | -33 † |
| Simvastatin Trial (6-week) | |||||||
| Placebo | 33 | -2 | -4 | -4 † | -3 | -2 | +6 † |
| Simvastatin 10 mg | 35 | -19 † | -26 † | -20 † | +3 † | -24 † | -17 † |
| Colesevelam Hydrochloride 3.8 g/ Simvastatin 10 mg | 34 | -28 † | -42 † | -33 † | +10 † | -37 † | -12 † |
| Simvastatin 20 mg | 39 | -23 † | -34 † | -26 † | +7 † | -30 † | -12 † |
| Colesevelam Hydrochloride 2.3 g/ Simvastatin 20 mg | 37 | -29 † | -42 † | -32 † | +4 † | -37 † | -12 † |
| Lovastatin Trial (4-week) | |||||||
| Placebo | 26 | +1 | 0 | 0 | +1 | +1 | +1 |
| Lovastatin 10 mg | 26 | -14 † | -22 † | -16 † | +5 | -19 † | 0 |
| Colesevelam Hydrochloride 2.3 g/ Lovastatin 10 mg Together | 27 | -21 † | -34 † | -24 † | +4 | -27 † | -1 |
| Colesevelam Hydrochloride 2.3 g/ Lovastatin 10 mg Apart | 23 | -21 † | -32 † | -24 † | +2 | -28 † | -2 |
In all 3 studies, the LDL-C reduction achieved with the combination of colesevelam hydrochloride and any given dose of statin therapy was statistically superior to that achieved with colesevelam hydrochloride or that dose of the statin alone. The LDL-C reduction with atorvastatin 80 mg was not statistically significantly different from the combination of colesevelam hydrochloride 3.8 g and atorvastatin 10 mg.
The effect of colesevelam hydrochloride when added to fenofibrate was assessed in 122 patients with mixed hyperlipidemia (Fredrickson Type IIb). Inclusion in the study required LDL-C ≥115 mg/dL and TG 150 mg/dL to 749 mg/dL. Patients were treated with 160 mg of fenofibrate during an 8-week open-label run-in period and then randomly assigned to receive fenofibrate 160 mg plus either colesevelam hydrochloride 3.8 g or placebo for 6 weeks of double-blind treatment. The overall mean LDL-C at the start of randomized treatment was 144 mg/dL. The results of the study are summarized in Table 8.
| Treatment | N | TC | LDL-C | Apo B | HDL-C | Non-HDL-C | TG † |
|---|---|---|---|---|---|---|---|
| Placebo + Fenofibrate 160 mg | 61 | 2 | 2 | 1 | -1 | 2 | -3 |
| Colesevelam Hydrochloride + Fenofibrate 160 mg | 61 | -6 ‡ | -10 ‡ | -7 ‡ | 0 | -8 ‡ | 6 |
Pediatric Therapy: The safety and efficacy of colesevelam hydrochloride in pediatric patients were evaluated in an 8-week, multi-center, randomized, double-blind, placebo-controlled, parallel-group study followed by an open-label phase, in 194 boys and post-menarchal girls 10 to 17 years of age (mean age 14.1 years) with heterozygous familial hypercholesterolemia (heFH), taking a stable dose of an FDA-approved statin (with LDL-C >130 mg/dL) or naïve to lipid-lowering therapy (with LDL-C >160 mg/dL). This study had 3 periods: a single-blind, placebo stabilization period; an 8-week, randomized, double-blind, parallel-group, placebo-controlled treatment period; and an 18-week, open-label treatment period. Forty-seven (24%) patients were taking statins and 147 (76%) patients were statin-naïve at screening. The mean baseline LDL-C at Day 1 was approximately 199 mg/dL.
During the double-blind treatment period, patients were assigned randomly to treatment: colesevelam hydrochloride 3.8 g/day (n=64), colesevelam hydrochloride 1.9 g/day (n=65), or placebo (n=65). In total, 186 patients completed the double-blind treatment period. After 8 weeks of treatment, colesevelam hydrochloride 3.8 g/day significantly decreased plasma levels of LDL-C, non-HDL-C, TC, and Apo B and significantly increased HDL-C. A moderate, non-statistically significant increase in TG was observed versus placebo (Table 9).
| Treatment Difference | TC
(N=128) | LDL-C
(N=128) | Apo B
(N=124) | HDL-C
(N=128) | Non-HDL-C
(N=128) | TG
*
(N=128) |
|---|---|---|---|---|---|---|
|
||||||
| Colesevelam Hydrochloride 3.8 g vs. Placebo | -7 † | -13 † | -8 † | +6 † | -11 † | +5 |
During the open-label treatment period patients were treated with colesevelam hydrochloride 3.8 g/day. In total, 173 (89%) patients completed 26 weeks of treatment. Results at Week 26 were consistent with those at Week 8.
16 HOW SUPPLIED/STORAGE AND HANDLING
Colesevelam hydrochloride tablets, 625 mg, are supplied as off-white to pale yellow film-coated oval tablets, debossed with "L61" on one side and plain on the other side. Colesevelam hydrochloride tablets are available as follows:
- Bottles of 180 – NDC 42291-147-18
17 PATIENT COUNSELING INFORMATION
Dosing: Patients should be advised to take colesevelam hydrochloride tablets with a meal and liquid. Colesevelam hydrochloride can be taken as 6 tablets once daily or 3 tablets twice daily [see Dosage and Administration (2)].
Drug interactions: Drugs with a known interaction with colesevelam (e.g., cyclosporine, glimepiride, glipizide, glyburide, levothyroxine, olmesartan medoxomil, oral contraceptives) should be administered at least 4 hours prior to colesevelam hydrochloride. In an in vivo drug interaction study, there was no significant effect on the bioavailability of phenytoin; however, due to its narrow therapeutic index and post-marketing reports consistent with potential drug-drug interactions, phenytoin should be administered at least 4 hours prior to colesevelam hydrochloride. Drugs that have not been tested for interaction with colesevelam, especially those with a narrow therapeutic index, should also be administered at least 4 hours prior to colesevelam hydrochloride. Alternatively the physician should monitor blood levels of the coadministered drug. Patients receiving concomitant metformin ER and colesevelam should be monitored for clinical response as is usual for the use of anti-diabetes drugs [see Drug Interactions (7)].
Gastrointestinal: Colesevelam hydrochloride can cause constipation. Colesevelam hydrochloride is contraindicated in patients with a history of bowel obstruction. Colesevelam hydrochloride is not recommended in patients who may be at risk of bowel obstruction, including patients with gastroparesis, other gastrointestinal motility disorders, or a history of major gastrointestinal surgery. Patients should be instructed to consume a diet that promotes bowel regularity. Patients should be instructed to promptly discontinue colesevelam hydrochloride and seek medical attention if severe abdominal pain or severe constipation occurs. Because of the tablet size, colesevelam hydrochloride tablets can cause dysphagia or esophageal obstruction and should be used with caution in patients with dysphagia or swallowing disorders [see Warnings and Precautions (5.4)] .
Hypertriglyceridemia and pancreatitis: Patients should be instructed to discontinue colesevelam hydrochloride and seek prompt medical attention if the hallmark symptoms of acute pancreatitis occur (e.g., severe abdominal pain with or without nausea and vomiting) [see Warnings and Precautions (5.2)] .
17.1 Primary Hyperlipidemia
Patients should be advised to adhere to their National Cholesterol Education Program (NCEP)-recommended diet.
Hypertriglyceridemia and cardiovascular disease: Patients should be informed that colesevelam hydrochloride may increase serum triglyceride concentrations and that the long-term effect of hypertriglyceridemia on the risk of coronary artery disease is uncertain [see Warnings and Precautions (5.2)] .
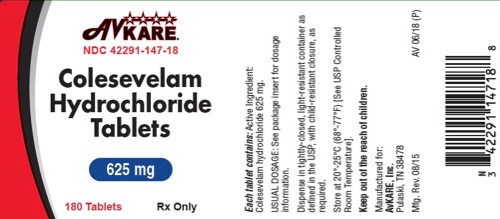
PRINCIPAL DISPLAY PANEL - 180 Tablet Bottle Label
AvKARE ®
NDC 42291-147-18
Colesevelam
Hydrochloride
Tablets
625 mg
180 Tablets Rx Only
Each tablet contains: Active Ingredient:
Colesevelam hydrochloride 625 mg.
USUAL DOSAGE: See package insert for dosage
information.
Dispense in tightly-closed, light-resistant container as
defined in the USP, with child-resistant closure, as
required.
Store at 20°-25°C (68°-77°F) [See USP Controlled
Room Temperature].
Keep out of the reach of children.
Manufactured for:
AvKARE, Inc.
Pulaski, TN 38478
Mfg. Rev. 08/15 AV 06/18 (P)
| COLESEVELAM HYDROCHLORIDE
colesevelam hydrochloride tablet, coated |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - AvKARE (796560394) |