FULL PRESCRIBING INFORMATION
2 DOSAGE AND ADMINISTRATION
2.1 Dosage in Psoriasis
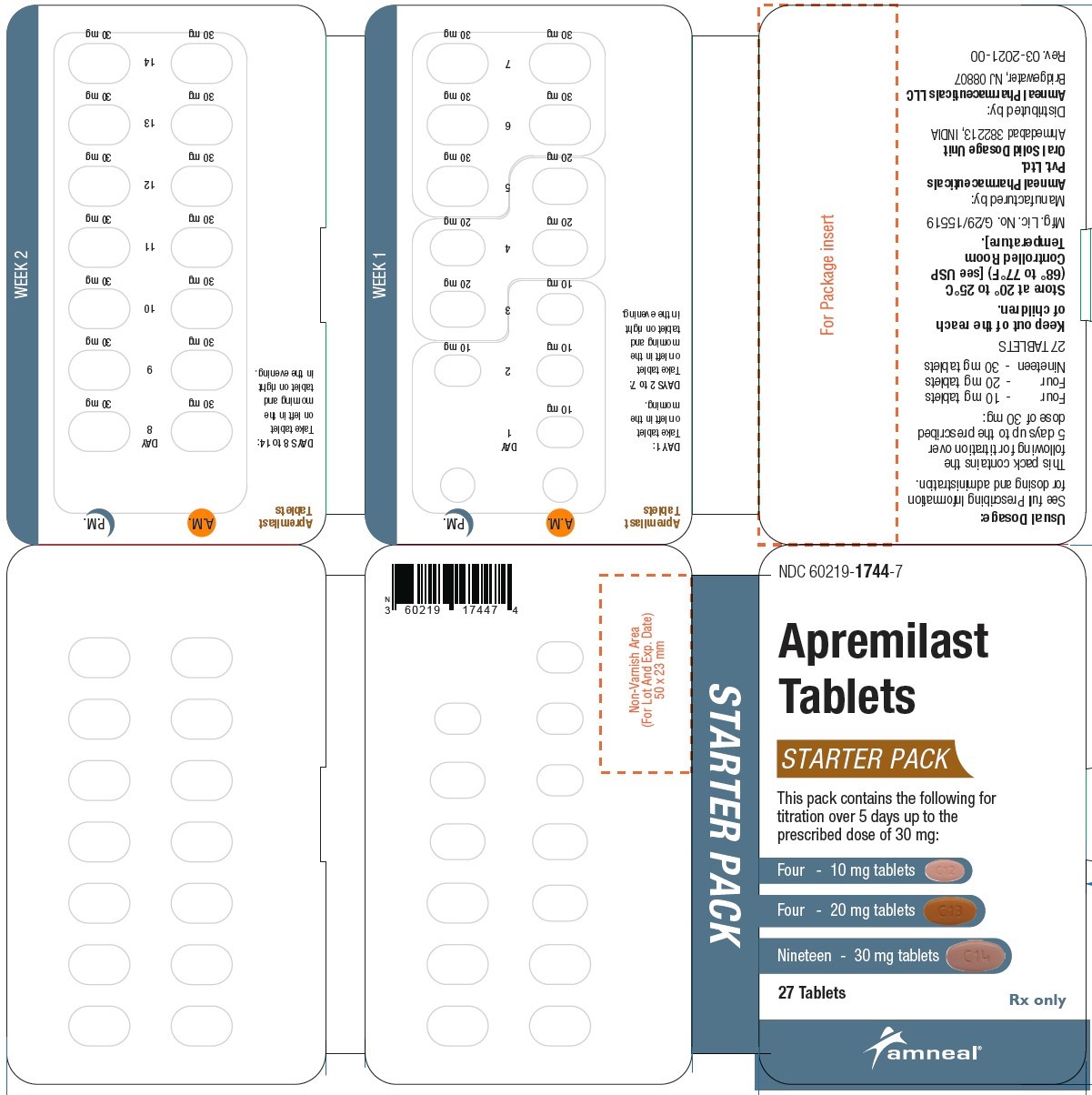
The recommended initial dosage titration of apremilast tablets from Day 1 to Day 5 is shown in Table 1. Following the 5-day titration, the recommended maintenance dosage is 30 mg twice daily taken orally starting on Day 6. This titration is intended to reduce the gastrointestinal symptoms associated with initial therapy.
Apremilast tablets can be administered without regard to meals. Do not crush, split, or chew the tablets.
Table 1: Dosage Titration Schedule
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 |
Day 6 & thereafter |
|||||
| AM | AM | PM | AM | PM | AM | PM | AM | PM | AM | PM |
| 10 mg | 10 mg | 10 mg | 10 mg | 20 mg | 20 mg | 20 mg | 20 mg | 30 mg | 30 mg | 30 mg |
2.2 Dosage Adjustment in Patients with Severe Renal Impairment
Apremilast tablets dosage should be reduced to 30 mg once daily in patients with severe renal impairment (creatinine clearance (CLcr) of less than 30 mL per minute estimated by the Cockcroft–Gault equation) [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. For initial dosage titration in this group, it is recommended that apremilast tablets be titrated using only the AM schedule listed in Table 1 and the PM doses be skipped.
3 DOSAGE FORMS AND STRENGTHS
Apremilast tablets are available as oval shaped, film coated tablets in the following dosage strengths:
- Apremilast Tablets, 10 mg are supplied as pink colored, oval shaped, film-coated tablets, debossed with “C12” on one side and plain on other side.
- Apremilast Tablets, 20 mg are supplied as brown colored, oval shaped, film-coated tablet, debossed with "C13” on one side and plain on other side.
- Apremilast Tablets, 30 mg are supplied as beige colored, oval shaped, film-coated tablets, debossed with “C14" on one side and plain on other side.
4 CONTRAINDICATIONS
Apremilast tablets are contraindicated in patients with a known hypersensitivity to apremilast or to any of the excipients in the formulation [see Adverse Reactions (6.1)].
5 WARNINGS AND PRECAUTIONS
5.1 Diarrhea, Nausea, and Vomiting
There have been postmarketing reports of severe diarrhea, nausea, and vomiting associated with the use of apremilast. Most events occurred within the first few weeks of treatment. In some cases, patients were hospitalized. Patients 65 years of age or older and patients taking medications that can lead to volume depletion or hypotension may be at a higher risk of complications from severe diarrhea, nausea, or vomiting. Monitor patients who are more susceptible to complications of diarrhea or vomiting. Patients who reduced dosage or discontinued apremilast generally improved quickly. Consider apremilast dose reduction or suspension if patients develop severe diarrhea, nausea, or vomiting.
5.2 Depression
Treatment with apremilast is associated with an increase in adverse reactions of depression. Before using apremilast in patients with a history of depression and/or suicidal thoughts or behavior prescribers should carefully weigh the risks and benefits of treatment with apremilast in such patients. Patients, their caregivers, and families should be advised of the need to be alert for the emergence or worsening of depression, suicidal thoughts or other mood changes, and if such changes occur to contact their healthcare provider. Prescribers should carefully evaluate the risks and benefits of continuing treatment with apremilast if such events occur.
Psoriasis: During the 0 to 16 week placebo-controlled period of the 3 controlled clinical trials, 1.3% (12/920) of subjects treated with apremilast reported depression compared to 0.4% (2/506) treated with placebo. During the clinical trials, 0.1% (1/1,308) of subjects treated with apremilast discontinued treatment due to depression compared with none in placebo-treated subjects (0/506). Depression was reported as serious in 0.1% (1/1,308) of subjects exposed to apremilast, compared to none in placebo-treated subjects (0/506). Instances of suicidal behavior have been observed in 0.1% (1/1,308) of subjects while receiving apremilast, compared to 0.2% (1/506) in placebo-treated subjects. In the clinical trials, one subject treated with apremilast attempted suicide while one who received placebo committed suicide.
5.3 Weight Decrease
During the controlled period of the trials in psoriasis, weight decrease between 5% to 10% of body weight occurred in 12% (96/784) of subjects treated with apremilast compared to 5% (19/382) treated with placebo. Weight decrease of ≥ 10% of body weight occurred in 2% (16/784) of subjects treated with apremilast 30 mg twice daily compared to 1% (3/382) subjects treated with placebo.
Patients treated with apremilast should have their weight monitored regularly. If unexplained or clinically significant weight loss occurs, weight loss should be evaluated, and discontinuation of apremilast should be considered [see Adverse Reactions (6.1)].
5.4 Drug Interactions
Co-administration of strong cytochrome P450 enzyme inducer, rifampin, resulted in a reduction of systemic exposure of apremilast, which may result in a loss of efficacy of apremilast. Therefore, the use of cytochrome P450 enzyme inducers (e.g., rifampin, phenobarbital, carbamazepine, phenytoin) with apremilast is not recommended [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
6 ADVERSE REACTIONS
The following adverse reactions are described elsewhere in the labeling:
- Diarrhea, Nausea, and Vomiting [see Warnings and Precautions (5.1)]
- Depression [see Warnings and Precautions (5.2)]
- Weight Decrease [see Warnings and Precautions (5.3)]
- Drug Interactions [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Psoriasis Clinical Trials The safety of apremilast was assessed in 1,426 subjects in 3 randomized, double-blind, placebo-controlled trials in adult subjects with moderate to severe plaque psoriasis who were candidates for phototherapy or systemic therapy. Subjects were randomized to receive apremilast 30 mg twice daily or placebo twice daily. Titration was used over the first 5 days [see Dosage and Administration (2.1)]. Subjects ranged in age from 18 to 83 years, with an overall median age of 46 years.
Diarrhea, nausea, and upper respiratory tract infection were the most commonly reported adverse reactions. The most common adverse reactions leading to discontinuation for subjects taking apremilast were nausea (1.6%), diarrhea (1.0%), and headache (0.8%). The proportion of subjects with psoriasis who discontinued treatment due to any adverse reaction was 6.1% for subjects treated with apremilast 30 mg twice daily and 4.1% for placebo-treated subjects.
Table 3: Adverse Reactions Reported in ≥ 1% of Subjects on Apremilast and With Greater Frequency Than in Subjects on Placebo; up to Day 112 (Week 16)
|
Preferred Term |
Placebo (N=506) n (%) |
Apremilast 30 mg BID (N=920) n (%) |
|
Diarrhea |
32 (6) |
160 (17) |
|
Nausea |
35 (7) |
155 (17) |
|
Upper respiratory tract infection |
31 (6) |
84 (9) |
|
Tension headache |
21 (4) |
75 (8) |
|
Headache |
19 (4) |
55 (6) |
|
Abdominal pain* |
11 (2) |
39 (4) |
|
Vomiting |
8 (2) |
35 (4) |
|
Fatigue |
9 (2) |
29 (3) |
|
Dyspepsia |
6 (1) |
29 (3) |
|
Decreased appetite |
5 (1) |
26 (3) |
|
Insomnia |
4 (1) |
21 (2) |
|
Back pain |
4 (1) |
20 (2) |
|
Migraine |
5 (1) |
19 (2) |
|
Frequent bowel movements |
1 (0) |
17 (2) |
|
Depression |
2 (0) |
12 (1) |
|
Bronchitis |
2 (0) |
12 (1) |
|
Tooth abscess |
0 (0) |
10 (1) |
|
Folliculitis |
0 (0) |
9 (1) |
|
Sinus headache |
0 (0) |
9 (1) |
|
*Two subjects treated with apremilast experienced serious adverse reaction of abdominal pain. |
||
Severe worsening of psoriasis (rebound) occurred in 0.3% (4/1,184) subjects following discontinuation of treatment with apremilast.
7 DRUG INTERACTIONS
7.1 Strong CYP450 Inducers
Apremilast exposure is decreased when apremilast is co-administered with strong CYP450 inducers (such as rifampin) and may result in loss of efficacy [see Warnings and Precautions (5.3) and Clinical Pharmacology (12.3)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to apremilast during pregnancy. Information about the registry can be obtained by calling 1-877-311-8972.
Risk Summary
Available pharmacovigilance data with apremilast use in pregnant women have not established a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes, but these data are extremely limited. Based on findings from animal reproduction studies, apremilast may increase the risk for fetal loss. In animal embryo-fetal development studies, the administration of apremilast to pregnant cynomolgus monkeys during organogenesis resulted in dose-related increases in abortion/embryo-fetal death at dose exposures 2.1-times the maximum recommended human therapeutic dose (MRHD) and no adverse effect at an exposure of 1.4-times the MRHD. When administered to pregnant mice, during organogenesis there were no apremilast-induced malformations up to exposures 4.0-times the MRHD (see Data). Advise pregnant women of the potential risk of fetal loss. Consider pregnancy planning and prevention for females of reproductive potential.
The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
In an embryo-fetal developmental study, pregnant cynomolgus monkeys were administered apremilast at doses of 20, 50, 200, or 1,000 mg/kg/day during the period of organogenesis (gestation Days 20 through 50). There was a dose-related increase in spontaneous abortions, with most abortions occurring during Weeks 3 to 4 of dosing in the first trimester, at doses approximately 2.1-times the MRHD and greater (on an area under the curve [AUC] basis at doses ≥ 50 mg/kg/day). No abortifacient effects were observed at a dose approximately 1.4-times the MRHD (on an AUC basis at a dose of 20 mg/kg/day). Although, there was no evidence for a teratogenic effect at doses of 20 mg/kg/day and greater when examined at day 100, aborted fetuses were not examined.
In an embryo-fetal development study in mice, apremilast was administered at doses of 250, 500, or 750 mg/kg/day to dams during organogenesis (gestation Day 6 through 15). In a combined fertility and embryo-fetal development study in mice, apremilast was administered at doses of 10, 20, 40, or 80 mg/kg/day starting 15 days before cohabitation and continuing through gestation Day 15. No teratogenic findings attributed to apremilast were observed in either study; however, there was an increase in postimplantation loss at doses corresponding to a systemic exposure of 2.3-times the MRHD and greater (≥ 20 mg/kg/day). At doses of ≥ 20 mg/kg/day skeletal variations included incomplete ossification sites of tarsals, skull, sternebra, and vertebrae. No effects were observed at a dose approximately 1.3-times the MRHD (10 mg/kg/day).
Apremilast distributed across the placenta into the fetal compartment in mice and monkeys.
In a pre- and postnatal study in mice, apremilast was administered to pregnant female mice at doses of 10, 80, or 300 mg/kg/day from Day 6 of gestation through Day 20 of lactation, with weaning on Day 21. Dystocia, reduced viability, and reduced birth weights occurred at doses corresponding to ≥ 4.0-times the MRHD (on an AUC basis at doses ≥ 80 mg/kg/day). No adverse effects occurred at a dose 1.3-times the MRHD (10 mg/kg/day). There was no evidence for functional impairment of physical development, behavior, learning ability, immune competence, or fertility in the offspring at doses up to 7.5-times the MRHD (on an AUC basis at a dose of 300 mg/kg/day).
8.2 Lactation
Risk Summary
There are no data on the presence of apremilast in human milk, the effects on the breastfed infant, or the effects on milk production. However, apremilast was detected in the milk of lactating mice. When a drug is present in animal milk, it is likely that the drug will be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for apremilast and any potential adverse effects on the breastfed infant from apremilast or from the underlying maternal condition.
Data
In mice, following a single oral administration of 10 mg/kg to dams on postpartum day 13, apremilast concentrations in milk were approximately 1.5-times that of simultaneously collected blood samples.
8.4 Pediatric Use
The safety and effectiveness of apremilast in pediatric patients less than18 years of age have not been established.
8.5 Geriatric Use
Of the 1,257 subjects who enrolled in two placebo-controlled psoriasis trials (PSOR 1 and PSOR 2), a total of 108 psoriasis subjects were 65 years of age and older, including 9 subjects who were 75 years of age and older. No overall differences were observed in the efficacy and safety in elderly subjects ≥ 65 years of age and younger adult subjects < 65 years of age in the clinical trials.
8.6 Renal Impairment
Apremilast pharmacokinetics were characterized in subjects with mild, moderate, and severe renal impairment as defined by a creatinine clearance of 60 to 89, 30 to 59, and less than 30 mL per minute, respectively, by the Cockcroft–Gault equation. While no dose adjustment is needed in patients with mild or moderate renal impairment, the dose of apremilast should be reduced to 30 mg once daily in patients with severe renal impairment [see Dosage and Administration (2.2) and Clinical Pharmacology (12.3)].
10 OVERDOSAGE
In case of overdose, patients should seek immediate medical help. Patients should be managed by symptomatic and supportive care should there be an overdose.
11 DESCRIPTION
The active ingredient in apremilast tablets is apremilast. Apremilast is a phosphodiesterase 4 (PDE4) inhibitor. Apremilast is known chemically as N-[2-[(1S)-1-(3-ethoxy-4-methoxyphenyl)-2-(methylsulfonyl)ethyl]-2,3-dihydro-1,3-dioxo-1H-isoindol-4-yl]acetamide. Its molecular formula is C22H24N2O7S and the molecular weight is 460.50 g/mol.
The chemical structure is:
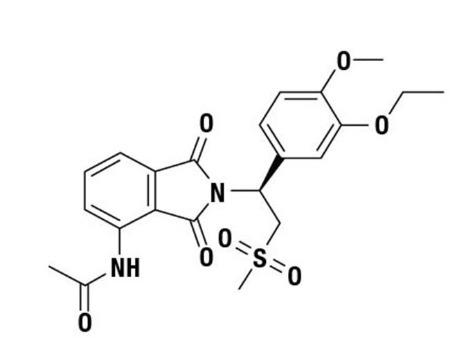
Apremilast is a white to pale yellow powder. It is soluble in acetone and practically insoluble in water.
Apremilast tablets are supplied in 10 mg, 20 mg, and 30 mg strengths for oral administration. Each tablet contains apremilast as the active ingredient and the following inactive ingredients: croscarmellose sodium, ferrosoferric oxide (30 mg), iron oxide red, iron oxide yellow (20 mg and 30 mg), lactose monohydrate, magnesium stearate, polyethylene glycol, polyvinyl alcohol, talc and titanium dioxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Apremilast is an oral small-molecule inhibitor of phosphodiesterase 4 (PDE4) specific for cyclic adenosine monophosphate (cAMP). PDE4 inhibition results in increased intracellular cAMP levels. The specific mechanism(s) by which apremilast exerts its therapeutic action is not well defined.
12.3 Pharmacokinetics
Absorption
Apremilast when taken orally is absorbed with an absolute bioavailability of ~73%, with peak plasma concentrations (Cmax) occurring at a median time (tmax) of ~2.5 hours. Co-administration with food does not alter the extent of absorption of apremilast.
Distribution
Human plasma protein binding of apremilast is approximately 68%. Mean apparent volume of distribution (Vd) is 87 L.
Metabolism
Following oral administration in humans, apremilast is a major circulating component (45%) followed by inactive metabolite M12 (39%), a glucuronide conjugate of O-demethylated apremilast. It is extensively metabolized in humans with up to 23 metabolites identified in plasma, urine and feces. Apremilast is metabolized by both cytochrome (CYP) oxidative metabolism with subsequent glucuronidation and non-CYP mediated hydrolysis. In vitro, CYP metabolism of apremilast is primarily mediated by CYP3A4, with minor contributions from CYP1A2 and CYP2A6.
Elimination
The plasma clearance of apremilast is about 10 L/hr in healthy subjects, with a terminal elimination half-life of approximately 6 to 9 hours. Following oral administration of radio-labeled apremilast, about 58% and 39% of the radioactivity is recovered in urine and feces, respectively, with about 3% and 7% of the radioactive dose recovered as apremilast in urine and feces, respectively.
Specific Populations
Hepatic Impairment: The pharmacokinetics of apremilast is not affected by moderate or severe hepatic impairment.
Renal Impairment: The pharmacokinetics of apremilast is not affected by mild or moderate renal impairment. In 8 subjects with severe renal impairment administered a single dose of 30 mg apremilast, the AUC and Cmax of apremilast increased by approximately 88% and 42%, respectively [see Dosage and Administration (2.2) and Use in Specific Populations (8.6)].
Age: A single oral dose of 30-mg apremilast was studied in young adults and elderly healthy subjects. The apremilast exposure in elderly subjects (65 to 85 years of age) was about 13% higher in AUC and about 6% higher in Cmax than in young subjects (18 to 55 years of age) [see Use in Specific Populations (8.5)].
Gender: In pharmacokinetic studies in healthy volunteers, the extent of exposure in females was about 31% higher and Cmax was about 8% higher than that in male subjects.
Race and Ethnicity: The pharmacokinetics of apremilast in Chinese and Japanese healthy male subjects is comparable to that in Caucasian healthy male subjects. In addition, apremilast exposure is similar among Hispanic Caucasians, non-Hispanic Caucasians, and African Americans.
Drug Interactions
In vitro data: Apremilast is not an inhibitor of CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP2E1, or CYP3A4 and not an inducer of CYP1A2, CYP2B6, CYP2C9, CYP2C19, or CYP3A4. Apremilast is a substrate, but not an inhibitor of P-glycoprotein (P-gp) and is not a substrate or an inhibitor of organic anion transporter (OAT)1 and OAT3, organic cation transporter (OCT)2, organic anion transporting polypeptide (OATP)1B1 and OATP1B3, or breast cancer resistance protein (BCRP).
Drug interaction studies were performed with apremilast and CYP3A4 substrates (oral contraceptive containing ethinyl estradiol and norgestimate), CYP3A and P-gp inhibitor (ketoconazole), CYP450 inducer (rifampin) and frequently co-administered drug in this patient population (methotrexate).
No significant pharmacokinetic interactions were observed when 30-mg oral apremilast was administered with either oral contraceptive, ketoconazole, or methotrexate. Co-administration of the CYP450 inducer rifampin (600 mg once daily for 15 days) with a single oral dose of 30-mg apremilast resulted in reduction of apremilast AUC and Cmax by 72% and 43%, respectively [see Warnings and Precautions (5.3) and Drug Interactions (7.1)].
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies were conducted in mice and rats with apremilast to evaluate its carcinogenic potential. No evidence of apremilast-induced tumors was observed in mice at oral doses up to 8.8-times the Maximum Recommended Human Dose (MRHD) on an AUC basis (1,000 mg/kg/day) or in rats at oral doses up to approximately 0.08- and 1.1-times the MRHD, (20 mg/kg/day in males and 3 mg/kg/day in females, respectively).
Apremilast tested negative in the Ames assay, in vitro chromosome aberration assay of human peripheral blood lymphocytes, and the in vivo mouse micronucleus assay.
In a fertility study of male mice, apremilast at oral doses up to approximately 3-times the MRHD based on AUC (up to 50 mg/kg/day) produced no effects on male fertility. In a fertility study of female mice, apremilast was administered at oral doses of 10, 20, 40, or 80 mg/kg/day. At doses ≥ 1.8-times the MRHD (≥ 20 mg/kg/day), estrous cycles were prolonged, due to lengthening of diestrus which resulted in a longer interval until mating. Mice that became pregnant at doses of 20 mg/kg/day and greater also had increased incidences of early postimplantation losses. There was no effect of apremilast approximately 1.0-times the MRHD (10 mg/kg/day).
14 CLINICAL STUDIES
14.2 Psoriasis
Two multicenter, randomized, double-blind, placebo-controlled trials (Studies PSOR-1 and PSOR-2) enrolled a total of 1,257 subjects 18 years of age and older with moderate to severe plaque psoriasis [body surface area (BSA) involvement of ≥ 10%, static Physician Global Assessment (sPGA) of ≥ 3 (moderate or severe disease), Psoriasis Area and Severity Index (PASI) score ≥ 12, candidates for phototherapy or systemic therapy]. Subjects were allowed to use low-potency topical corticosteroids on the face, axilla and groin.
Study PSOR-1 enrolled 844 subjects and Study PSOR-2 enrolled 413 subjects. In both studies, subjects were randomized 2:1 to apremilast 30 mg BID or placebo for 16 weeks. Both studies assessed the proportion of subjects who achieved PASI-75 at Week 16 and the proportion of subjects who achieved a sPGA score of clear (0) or almost clear (1) at Week 16. Across both studies, subjects ranged in age from 18 to 83 years, with an overall median age of 46 years. The mean baseline BSA involvement was 25.19% (median 21.0%), the mean baseline PASI score was 19.07 (median 16.80), and the proportion of subjects with sPGA score of 3 (moderate) and 4 (severe) at baseline were 70.0% and 29.8%, respectively. Approximately 30% of all subjects had received prior phototherapy and 54% had received prior conventional systemic and/or biologic therapy for the treatment of psoriasis with 37% receiving prior conventional systemic therapy and 30% receiving prior biologic therapy. Approximately one-third of subjects had not received prior phototherapy, conventional systemic nor biologic therapy.
Clinical Response in Subjects with Plaque Psoriasis
The proportion of subjects who achieved PASI-75 responses, and sPGA score of clear (0) or almost clear (1), are presented in Table 7.
Table 7: Clinical Response at Week 16 in Studies PSOR-1 and PSOR-2
|
|
Study PSOR-1 |
Study PSOR-2 |
||
|
Placebo |
Apremilast 30 mg BID |
Placebo |
Apremilast 30 mg BID |
|
|
Na |
N=282 |
N=562 |
N=137 |
N=274 |
|
PASIb -75, n (%) |
15 (5.3) |
186 (33.1) |
8 (5.8) |
79 (28.8) |
|
sPGAc of Clear or Almost Clear, n (%) |
11 (3.9) |
122 (21.7) |
6 (4.4) |
56 (20.4) |
|
a N is number of randomized and treated patients. b PASI=Psoriasis Area and Severity Index. c sPGA=Static Physician Global Assessment. |
||||
The median time to loss of PASI-75 response among the subjects re-randomized to placebo at Week 32 during the Randomized Treatment Withdrawal Phase was 5.1 weeks.
16 HOW SUPPLIED/STORAGE AND HANDLING
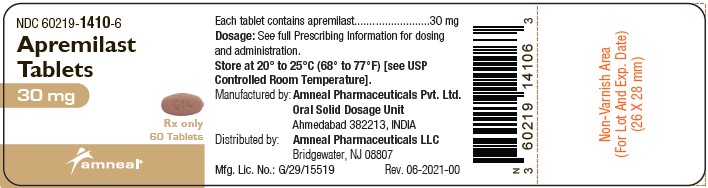
Apremilast Tablets, 10 mg are supplied as pink colored, oval shaped, film-coated tablets, debossed with “C12” on one side and plain on other side.
Apremilast Tablets, 20 mg are supplied as brown colored, oval shaped, film-coated tablet, debossed with "C13” on one side and plain on other side.
Apremilast Tablets, 30 mg are supplied as beige colored, oval shaped, film-coated tablets, debossed with “C14" on one side and plain on other side.
Tablets are supplied in the following strengths and package configurations:
|
Package Configuration |
Tablet Strength |
NDC number |
|
Bottles of 60 |
30 mg |
NDC 60219-1410-6 |
|
Two week starter pack |
13-tablet blister titration pack containing: (4) 10-mg, (4) 20-mg, and (5) 30-mg tablets with an additional (14) 30-mg tablets | NDC 60219-1744-7 |
Storage and Handling
Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
-
Diarrhea, Nausea, and Vomiting
Instruct patients to contact their healthcare provider if they experience severe diarrhea, nausea, or vomiting. Prescribers should advise patients of the potential complications of severe diarrhea, nausea, or vomiting. Consider apremilast tablets dose reduction or suspension if patients develop severe diarrhea, nausea, or vomiting [see Warnings and Precautions (5.1)].
-
Depression
Before using apremilast tablets in patients with a history of depression and/or suicidal thoughts or behavior, prescribers should carefully weigh the risks and benefits of treatment with apremilast tablets in such patients. Patients, their caregivers, and families should be advised of the need to be alert for the emergence or worsening of depression, suicidal thoughts or other mood changes, and if such changes occur to contact their healthcare provider. Prescribers should carefully evaluate the risks and benefits of continuing treatment with apremilast tablets if such events occur [see Warnings and Precautions (5.2)].
-
Weight Decrease
Patients treated with apremilast tablets should have their weight monitored regularly. If unexplained or clinically significant weight loss occurs, weight loss should be evaluated, and discontinuation of apremilast tablets should be considered [see Warnings and Precautions (5.3)].
-
Drug Interactions
The use of strong cytochrome P450 enzyme inducers (e.g., rifampin, phenobarbital, carbamazepine, phenytoin) with apremilast tablets is not recommended [see Warnings and Precautions (5.4), Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
- Instruct patients to take apremilast tablets only as prescribed.
- Advise patients apremilast tablets can be taken with or without food.
- Advise patients that the tablets should not be crushed, split, or chewed.
- Advise patients about the side effects associated with apremilast tablets [see Adverse Reactions (6.1)].
- Pregnancy
Inform patients that there is a pregnancy registry for pregnant women who have taken apremilast tablets during pregnancy. Advise patients to contact the registry at 1-877-311-8972 to enroll [see Use in Specific Populations (8.1)]. Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Advise females to inform their prescriber of a known or suspected pregnancy.
Manufactured by:
Amneal Pharmaceuticals Pvt. Ltd.
Oral Solid Dosage Unit
Ahmedabad 382213, INDIA
Distributed by:
Amneal Pharmaceuticals LLC
Bridgewater, NJ 08807
Rev. 03-2021-00