Rx only
| PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION |
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Vancomycin Hydrochloride for Injection, USP and other antibacterial drugs, Vancomycin Hydrochloride for Injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
DESCRIPTION
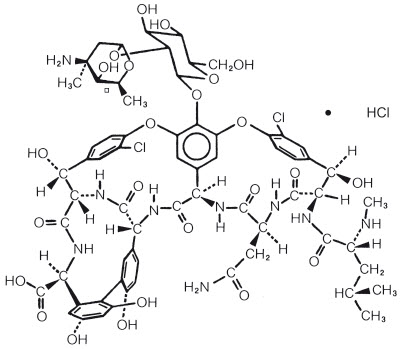
Vancomycin Hydrochloride for Injection, USP is a white, almost white, or tan lyophilized powder, for preparing intravenous (IV) infusions, in Pharmacy Bulk Package bottles containing the equivalent of 5 g or 10 g vancomycin base. 500 mg of the base are equivalent to 0.34 mmol. When reconstituted with Sterile Water for Injection to a concentration of 50 mg/mL for the 5 g Pharmacy Bulk Package bottle and 100 mg/mL for the 10 g Pharmacy Bulk Package bottle, a clear solution is achieved with the pH of the solution between 2.5 and 4.5. Vancomycin Hydrochloride for Injection, USP should be administered intravenously in diluted solution (see DOSAGE AND ADMINISTRATION). Vancomycin is a tricyclic glycopeptide antibiotic derived from Amycolatopsis orientalis (formerly Nocardia orientalis). The chemical name for vancomycin hydrochloride is 3S-[3R*,6S*(S*),7S*,22S*,23R*,26R*,36S*,38aS*]]-3-(2-Amino-2-oxoethyl)-44-[[2-O-(3-amino-2,3,6-trideoxy-3-C-methyl-α-L-lyxo-hexopyranosyl)-ß-D-glucopyranosyl]oxy]-10,19-dichloro-2,3,4,5,6,7,23,24,25,26,36,37,38,38a-tetradecahydro-7,22,28,30,32-pentahydroxy-6-[[4-methyl-2-(methylamino)-1-oxopentyl]amino]-2,5,24,38,39-pentaoxo-22H-8,11:18,21-dietheno-23,36-(iminomethano)-13,16:31,35-dimetheno-1H,16H-[1,6,9]oxadiazacyclohexadecino[4,5-m][10,2,16]-benzoxadiazacyclotetracosine-26-carboxylic acid, monohydrochloride. The molecular formula is C66H75Cl2N9O24∙HCl and the molecular weight is 1,485.74. Vancomycin hydrochloride has the following structural formula:
A pharmacy bulk package is a container of a sterile preparation for parenteral use that contains many single doses. The contents of this pharmacy bulk package are intended for use by a pharmacy admixture service for addition to suitable parenteral fluids in the preparation of admixtures for intravenous infusion (See DOSAGE AND ADMINISTRATION, Directions for Proper Use of Pharmacy Bulk Package). AFTER RECONSTITUTION, FURTHER DILUTION IS REQUIRED. NOT FOR DIRECT INFUSION.
CLINICAL PHARMACOLOGY
Vancomycin is poorly absorbed after oral administration.
In subjects with normal kidney function, multiple intravenous dosing of 1 g of vancomycin (15 mg/kg) infused over 60 minutes produces mean plasma concentrations of approximately 63 mcg/mL immediately after the completion of infusion, mean plasma concentrations of approximately 23 mcg/mL 2 hours after infusion, and mean plasma concentrations of approximately 8 mcg/mL 11 hours after the end of the infusion. Multiple dosing of 500 mg infused over 30 minutes produces mean plasma concentrations of about 49 mcg/mL at the completion of infusion, mean plasma concentrations of about 19 mcg/mL 2 hours after infusion, and mean plasma concentrations of about 10 mcg/mL 6 hours after infusion. The plasma concentrations during multiple dosing are similar to those after a single dose.
The mean elimination half-life of vancomycin from plasma is 4 to 6 hours in subjects with normal renal function. In the first 24 hours, about 75% of an administered dose of vancomycin is excreted in urine by glomerular filtration. Mean plasma clearance is about 0.058 L/kg/h, and mean renal clearance is about 0.048 L/kg/h. Renal dysfunction slows excretion of vancomycin. In anephric patients, the average half-life of elimination is 7.5 days. The distribution coefficient is from 0.3 to 0.43 L/kg. There is no apparent metabolism of the drug. About 60% of an intraperitoneal dose of vancomycin administered during peritoneal dialysis is absorbed systemically in 6 hours. Serum concentrations of about 10 mcg/mL are achieved by intraperitoneal injection of 30 mg/kg of vancomycin. However, the safety and efficacy of the intraperitoneal use of vancomycin has not been established in adequate and well-controlled trials (see PRECAUTIONS).
Total systemic and renal clearance of vancomycin may be reduced in the elderly. Vancomycin is approximately 55% serum protein bound as measured by ultrafiltration at vancomycin serum concentrations of 10 to 100 mcg/mL. After IV administration of vancomycin, inhibitory concentrations are present in pleural, pericardial, ascitic, and synovial fluids; in urine; in peritoneal dialysis fluid; and in atrial appendage tissue. Vancomycin does not readily diffuse across normal meninges into the spinal fluid; but, when the meninges are inflamed, penetration into the spinal fluid occurs.
MICROBIOLOGY
The bactericidal action of vancomycin results primarily from inhibition of cell-wall biosynthesis. In addition, vancomycin alters bacterial-cell-membrane permeability and RNA synthesis. There is no cross-resistance between vancomycin and other antibiotics. Vancomycin is not active in vitro against gram-negative bacilli, mycobacteria, or fungi.
Synergy
The combination of vancomycin and an aminoglycoside acts synergistically in vitro against many strains of Staphylococcus aureus, Streptococcus bovis, enterococci, and the viridans group streptococci.
Vancomycin has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Aerobic gram-positive microorganisms
Diphtheroids
Enterococci (e.g., Enterococcus faecalis)
Staphylococci, including Staphylococcus aureus and Staphylococcus epidermidis (including heterogeneous methicillin-resistant strains)
Streptococcus bovis
Viridans group streptococci
The following in vitro data are available, but their clinical significance is unknown.
Vancomycin exhibits in vitro MIC's of 1 mcg/mL or less against most (≥90%) strains of streptococci listed below and MIC's of 4 mcg/mL or less against most (≥90%) strains of other listed microorganisms; however, the safety and effectiveness of vancomycin in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobic gram-positive microorganisms
Listeria monocytogenes
Streptococcus pyogenes
Streptococcus pneumoniae (including penicillin-resistant strains)
Streptococcus agalactiae
Anaerobic gram-positive microorganisms
Actinomyces species
Lactobacillus species
INDICATIONS AND USAGE
Vancomycin Hydrochloride for Injection, USP is indicated for the treatment of serious or severe infections caused by susceptible strains of methicillin-resistant (ß-lactam-resistant) staphylococci. It is indicated for penicillin-allergic patients, for patients who cannot receive or who have failed to respond to other drugs, including the penicillins or cephalosporins, and for infections caused by vancomycin-susceptible organisms that are resistant to other antimicrobial drugs. Vancomycin Hydrochloride for Injection, USP is indicated for initial therapy when methicillin-resistant staphylococci are suspected, but after susceptibility data are available, therapy should be adjusted accordingly.
Vancomycin Hydrochloride for Injection, USP is effective in the treatment of staphylococcal endocarditis. Its effectiveness has been documented in other infections due to staphylococci, including septicemia, bone infections, lower respiratory tract infections, skin and skin structure infections. When staphylococcal infections are localized and purulent, antibiotics are used as adjuncts to appropriate surgical measures.
Vancomycin Hydrochloride for Injection, USP has been reported to be effective alone or in combination with an aminoglycoside for endocarditis caused by S. viridans or S. bovis. For endocarditis caused by enterococci (e.g., E. faecalis), vancomycin has been reported to be effective only in combination with an aminoglycoside.
Vancomycin Hydrochloride for Injection, USP has been reported to be effective for the treatment of diphtheroid endocarditis. Vancomycin Hydrochloride for Injection, USP has been used successfully in combination with either rifampin, an aminoglycoside, or both in early-onset prosthetic valve endocarditis caused by S. epidermidis or diphtheroids.
Specimens for bacteriologic cultures should be obtained in order to isolate and identify causative organisms and to determine their susceptibilities to vancomycin.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Vancomycin Hydrochloride for Injection, USP and other antibacterial drugs, Vancomycin Hydrochloride for Injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
The parenteral form of vancomycin hydrochloride may be administered orally for treatment of antibiotic-associated pseudomembranous colitis produced by C. difficile and for staphylococcal enterocolitis. Parenteral administration of vancomycin hydrochloride alone is of unproven benefit for these indications. Vancomycin is not effective by the oral route for other types of infection.
CONTRAINDICATIONS
Vancomycin hydrochloride for injection is contraindicated in patients with known hypersensitivity to this antibiotic.
WARNINGS
Infusion Reactions
Rapid bolus administration (e.g., over several minutes) may be associated with exaggerated hypotension, including shock and rarely cardiac arrest.
Vancomycin hydrochloride for injection should be administered in a diluted solution over a period of not less than 60 minutes to avoid rapid-infusion-related reactions. Stopping the infusion usually results in prompt cessation of these reactions.
Nephrotoxicity
Systemic vancomycin exposure may result in acute kidney injury (AKI). The risk of AKI increases as systemic exposure/serum levels increase. Monitor renal function in all patients receiving vancomycin, especially patients with underlying renal impairment, patients with co-morbidities that predispose to renal impairment and patients receiving concomitant therapy with a drug known to be nephrotoxic.
Ototoxicity
Ototoxicity has occurred in patients receiving vancomycin. It may be transient or permanent. It has been reported mostly in patients who have been given excessive doses, who have an underlying hearing loss, or who are receiving concomitant therapy with another ototoxic agent, such as an aminoglycoside. Vancomycin should be used with caution in patients with renal insufficiency because the risk of toxicity is appreciably increased by high, prolonged blood concentrations.
Dosage of vancomycin hydrochloride for injection must be adjusted for patients with renal dysfunction (see PRECAUTIONS and DOSAGE AND ADMINISTRATION).
Severe Dermatologic Reactions
Severe dermatologic reactions such as toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP), and linear IgA bullous dermatosis (LABD) have been reported in association with the use of vancomycin. Cutaneous signs or symptoms reported include skin rashes, mucosal lesions, and blisters.
Discontinue vancomycin hydrochloride for injection at the first appearance of signs and symptoms of TEN, SJS, DRESS, AGEP, or LABD.
Clostridium Difficile Associated Diarrhea (CDAD)
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including vancomycin hydrochloride for injection, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Hemorrhagic Occlusive Retinal Vasculitis (HORV)
Hemorrhagic occlusive retinal vasculitis, including permanent loss of vision, occurred in patients receiving intracameral or intravitreal administration of vancomycin during or after cataract surgery. The safety and efficacy of vancomycin administered by the intracameral or the intravitreal route have not been established by adequate and well-controlled trials. Vancomycin is not indicated for the prophylaxis of endophthalmitis.
PRECAUTIONS
Clinically significant serum concentrations have been reported in some patients being treated for active C. difficile-induced pseudomembranous colitis after multiple oral doses of vancomycin.
Prolonged use of vancomycin hydrochloride for injection may result in the overgrowth of nonsusceptible microorganisms. Careful observation of the patient is essential. If superinfection occurs during therapy, appropriate measures should be taken. In rare instances, there have been reports of pseudomembranous colitis due to C. difficile developing in patients who received intravenous vancomycin hydrochloride for injection.
Serial tests of auditory function may be helpful in order to minimize the risk of ototoxicity.
Reversible neutropenia has been reported in patients receiving vancomycin hydrochloride for injection (see ADVERSE REACTIONS). Patients who will undergo prolonged therapy with vancomycin hydrochloride for injection or those who are receiving concomitant drugs which may cause neutropenia should have periodic monitoring of the leukocyte count.
Vancomycin hydrochloride for injection is irritating to tissue and must be given by a secure IV route of administration. Pain, tenderness, and necrosis occur with intramuscular (IM) injection of vancomycin hydrochloride for injection or with inadvertent extravasation. Thrombophlebitis may occur, the frequency and severity of which can be minimized by administering the drug slowly as a dilute solution (2.5 to 5 g/L) and by rotation of venous access sites.
There have been reports that the frequency of infusion-related events (including hypotension, flushing, erythema, urticaria, and pruritus) increases with the concomitant administration of anesthetic agents. Infusion-related events may be minimized by the administration of vancomycin as a 60-minute infusion prior to anesthetic induction. The safety and efficacy of vancomycin administered by the intrathecal (intralumbar or intraventricular) route or by the intraperitoneal route have not been established by adequate and well controlled trials.
Reports have revealed that administration of sterile vancomycin by the intraperitoneal route during continuous ambulatory peritoneal dialysis (CAPD) has resulted in a syndrome of chemical peritonitis. To date, this syndrome has ranged from cloudy dialysate alone to a cloudy dialysate accompanied by variable degrees of abdominal pain and fever. This syndrome appears to be short-lived after discontinuation of intraperitoneal vancomycin.
Prescribing vancomycin hydrochloride for injection, in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
DRUG INTERACTIONS
Concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing (see Pediatric Use under PRECAUTIONS) and anaphylactoid reactions (see ADVERSE REACTIONS).
Monitor renal function in patients receiving vancomycin and concurrent and/or sequential systemic or topical use of other potentially, neurotoxic and/or nephrotoxic drugs, such as amphotericin B, aminoglycosides, bacitracin, polymixin B, colistin, viomycin, or cisplatin.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Although no long-term studies in animals have been performed to evaluate carcinogenic potential, no mutagenic potential of vancomycin hydrochloride for injection was found in standard laboratory tests. No definitive fertility studies have been performed.
Pregnancy
Teratogenic Effects
Animal reproduction studies have not been conducted with vancomycin. It is not known whether vancomycin can affect reproduction capacity. In a controlled clinical study, the potential ototoxic and nephrotoxic effects of vancomycin on infants were evaluated when the drug was administered to pregnant women for serious staphylococcal infections complicating intravenous drug abuse. Vancomycin was found in cord blood. No sensorineural hearing loss or nephrotoxicity attributable to vancomycin was noted. One infant whose mother received vancomycin in the third trimester experienced conductive hearing loss that was not attributed to the administration of vancomycin. Because the number of patients treated in this study was limited and vancomycin was administered only in the second and third trimesters, it is not known whether vancomycin causes fetal harm. Vancomycin should be given to a pregnant woman only if clearly needed.
Nursing Mothers
Vancomycin hydrochloride for injection is excreted in human milk. Caution should be exercised when vancomycin hydrochloride for injection is administered to a nursing woman. Because of the potential for adverse events, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
In pediatric patients, it may be appropriate to confirm desired vancomycin serum concentrations. Concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing in pediatric patients (see PRECAUTIONS).
Geriatric Use
The natural decrement of glomerular filtration with increasing age may lead to elevated vancomycin serum concentrations if dosage is not adjusted. Vancomycin dosage schedules should be adjusted in elderly patients (see DOSAGE AND ADMINISTRATION).
Information for Patients
Severe Dermatologic Reactions
Advise patients about the signs and symptoms of serious skin manifestations. Instruct patients to stop vancomycin hydrochloride for injection immediately and promptly seek medical attention at the first signs or symptoms of skin rash, mucosal lesions and blisters (see WARNINGS).
Patients should be counseled that antibacterial drugs including vancomycin hydrochloride for injection, should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When vancomycin hydrochloride for injection, is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by vancomycin hydrochloride for injection, or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
ADVERSE REACTIONS
Infusion-Related Events
During or soon after rapid infusion of vancomycin hydrochloride for injection, patients may develop anaphylactoid reactions, including hypotension (see ANIMAL PHARMACOLOGY), wheezing, dyspnea, urticaria, or pruritus. Rapid infusion may also cause flushing of the upper body ("red neck") or pain and muscle spasm of the chest and back. These reactions usually resolve within 20 minutes but may persist for several hours. Such events are infrequent if vancomycin hydrochloride for injection is given by a slow infusion over 60 minutes. In studies of normal volunteers, infusion-related events did not occur when vancomycin hydrochloride for injection was administered at a rate of 10 mg/min or less.
Nephrotoxicity
Systemic vancomycin exposure may result in acute kidney injury (AKI). The risk of AKI increases as systemic exposure/serum levels increase.
Additional risk factors for AKI in patients receiving vancomycin include receipt of concomitant drugs known to be nephrotoxic, in patients with pre- existing renal impairment or with co-morbidities that predispose to renal impairment. Interstitial nephritis has also been reported in patients receiving vancomycin.
Gastrointestinal
Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see WARNINGS).
Ototoxicity
A few dozen cases of hearing loss associated with vancomycin have been reported. Most of these patients had kidney dysfunction or a preexisting hearing loss or were receiving concomitant treatment with an ototoxic drug. Vertigo, dizziness, and tinnitus have been reported rarely.
Hematopoietic
Reversible neutropenia, usually starting 1 week or more after onset of therapy with vancomycin or after a total dosage of more than 25 g, has been reported for several dozen patients. Neutropenia appears to be promptly reversible when vancomycin is discontinued. Thrombocytopenia has rarely been reported. Although a causal relationship has not been established, reversible agranulocytosis (granulocytes <500/mm3) has been reported rarely.
Miscellaneous
Patients have been reported to have had anaphylaxis, drug fever, nausea, chills, eosinophilia, rashes including exfoliative dermatitis, Stevens-Johnson syndrome (see WARNINGS, Severe Dermatologic Reactions), and vasculitis in association with the administration of vancomycin.
Chemical peritonitis has been reported following intraperitoneal administration (see PRECAUTIONS)
POST MARKETING REPORTS
The following adverse reactions have been identified during post-approval use of vancomycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
To report SUSPECTED ADVERSE REACTIONS, contact Xellia Pharmaceuticals USA, LLC at 1-833-295-6953 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Skin and Subcutaneous Tissue Disorders
Severe dermatologic reactions such as toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), acute generalized exanthematous pustulosis (AGEP), and linear IgA bullous dermatosis (LABD) (see WARNINGS, Severe Dermatologic Reactions).
OVERDOSAGE
Supportive care is advised, with maintenance of glomerular filtration. Vancomycin is poorly removed by dialysis. Hemofiltration and hemoperfusion with polysulfone resin have been reported to result in increased vancomycin clearance. The median lethal intravenous dose is 319 mg/kg in rats and 400 mg/kg in mice.
To obtain up-to-date information about the treatment of overdose, a good resource is your certified Regional Poison Control Center. Telephone numbers of certified poison control centers are listed in the Physicians' Desk Reference (PDR). In managing overdosage, consider the possibility of multiple drug overdoses, interaction among drugs, and unusual drug kinetics in your patient.
DOSAGE AND ADMINISTRATION
The intent of the pharmacy bulk package for this product is for preparation of solutions for IV infusion only.
Infusion-related events are related to both the concentration and the rate of administration of vancomycin. Concentrations of no more than 5 mg/mL and rates of no more than 10 mg/min, are recommended in adults (see also age-specific recommendations). In selected patients in need of fluid restriction, a concentration up to 10 mg/mL may be used; use of such higher concentrations may increase the risk of infusion-related events. An infusion rate of 10 mg/min or less is associated with fewer infusion-related events (see ADVERSE REACTIONS). Infusion-related events may occur, however, at any rate or concentration.
Patients With Normal Renal Function
Adults
The usual daily intravenous dose is 2 g divided either as 500 mg every 6 hours or 1 g every 12 hours. Each dose should be administered at no more than 10 mg/min or over a period of at least 60 minutes, whichever is longer. Other patient factors, such as age or obesity, may call for modification of the usual intravenous daily dose.
Pediatric patients
The usual intravenous dosage of vancomycin is 10 mg/kg per dose given every 6 hours. Each dose should be administered over a period of at least 60 minutes. Close monitoring of serum concentrations of vancomycin may be warranted in these patients.
Neonates
In pediatric patients up to the age of 1 month, the total daily intravenous dosage may be lower. In neonates, an initial dose of 15 mg/kg is suggested, followed by 10 mg/kg every 12 hours for neonates in the 1st week of life and every 8 hours thereafter up to the age of 1 month. Each dose should be administered over 60 minutes. In premature infants, vancomycin clearance decreases as postconceptional age decreases.
Therefore, longer dosing intervals may be necessary in premature infants. Close monitoring of serum concentrations of vancomycin is recommended in these patients.
Patients With Impaired Renal Function and Elderly Patients
Dosage adjustment must be made in patients with impaired renal function. In premature infants and the elderly, greater dosage reductions than expected may be necessary because of decreased renal function. Measurement of vancomycin serum concentrations can be helpful in optimizing therapy, especially in seriously ill patients with changing renal function. Vancomycin serum concentrations can be determined by use of microbiologic assay, radioimmunoassay, fluorescence polarization immunoassay, fluorescence immunoassay, or high-pressure liquid chromatography. If creatinine clearance can be measured or estimated accurately, the dosage for most patients with renal impairment can be calculated using the following table. The dosage of vancomycin hydrochloride for injection per day in mg is about 15 times the glomerular filtration rate in mL/min (see following table).
| Creatinine Clearance mL/min | Vancomycin Dose mg/24 h |
|---|---|
| 100 | 1,545 |
| 90 | 1,390 |
| 80 | 1,235 |
| 70 | 1,080 |
| 60 | 925 |
| 50 | 770 |
| 40 | 620 |
| 30 | 465 |
| 20 | 310 |
| 10 | 155 |
The initial dose should be no less than 15 mg/kg, even in patients with mild to moderate renal insufficiency. The table is not valid for functionally anephric patients. For such patients, an initial dose of 15 mg/kg of body weight should be given to achieve prompt therapeutic serum concentrations. The dose required to maintain stable concentrations is 1.9 mg/kg/24 hr. In patients with marked renal impairment, it may be more convenient to give maintenance doses of 250 to 1,000 mg once every several days rather than administering the drug on a daily basis. In anuria, a dose of 1,000 mg every 7 to 10 days has been recommended. When only serum creatinine is known, the following formula (based on sex, weight and age of the patient) may be used to calculate creatinine clearance. Calculated creatinine clearances (mL/min) are only estimates. The creatinine clearance should be measured promptly.
| Men: | Weight (kg) × (140 – age in years) |
| 72 × serum creatinine concentration (mg/dL) | |
| Women: | 0.85 × above value |
The serum creatinine must represent a steady state of renal function. Otherwise, the estimated value for creatinine clearance is not valid. Such a calculated clearance is an overestimate of actual clearance in patients with conditions: (1) characterized by decreasing renal function, such as shock, severe heart failure, or oliguria; (2) in which a normal relationship between muscle mass and total body weight is not present, such as in obese patients or those with liver disease, edema, or ascites; and (3) accompanied by debilitation, malnutrition, or inactivity. The safety and efficacy of vancomycin administration by the intrathecal (intralumbar or intraventricular) routes have not been established. Intermittent infusion is the recommended method of administration.
Compatibility with Other Drugs and IV Fluids
The following diluents are physically and chemically compatible (with 4 g/L vancomycin hydrochloride):
5% Dextrose Injection, USP
5% Dextrose Injection and 0.9% Sodium Chloride Injection, USP
Lactated Ringer's Injection, USP
5% Dextrose and Lactated Ringer's Injection
Normosol®-M and 5% Dextrose
0.9% Sodium Chloride Injection, USP
Isolyte® E
Good professional practice suggests that compounded admixtures should be administered as soon after preparation as is feasible.
Vancomycin solution has a low pH and may cause physical instability of other compounds.
Mixtures of solutions of vancomycin and beta-lactam antibiotics have been shown to be physically incompatible. The likelihood of precipitation increases with higher concentrations of vancomycin. It is recommended to adequately flush the intravenous lines between the administrations of these antibiotics. It is also recommended to dilute solutions of vancomycin to 5 mg/mL or less.
Although intravitreal injection is not an approved route of administration for vancomycin, precipitation has been reported after intravitreal injection of vancomycin and ceftazidime for endophthalmitis using different syringes and needles. The precipitates dissolved gradually, with complete clearing of the vitreous cavity over two months and with improvement of visual acuity.
PREPARATION AND STABILITY
CAUTION: NOT TO BE DISPENSED AS A UNIT
DIRECTIONS FOR PROPER USE OF PHARMACY BULK PACKAGE
Not for direct infusion. The pharmacy bulk package is for use in the Pharmacy Admixture Service only in a suitable work area such as a laminar flow hood. Using aseptic technique, the closure may be penetrated only one time after reconstitution using a suitable sterile transfer device or dispensing set, which allows measured dispensing of the contents. Use of a syringe and needle is not recommended as it may cause leakage. After entry use entire contents of the Pharmacy Bulk Package bottle promptly. The entire contents of the Pharmacy Bulk Package bottle should be dispensed within 4 hours after initial entry. A maximum time of 4 hours from the initial entry may be allowed to complete fluid aliquoting/transferring operations. Discard the container no later than 4 hours after initial closure puncture. This time limit should begin with the introduction of solvent or diluent into the Pharmacy Bulk Package bottle.
Preparation and Stability
5 g Pharmacy Bulk Package bottle
At the time of use, reconstitute by adding 100 mL of Sterile Water for Injection to the 5 g Pharmacy Bulk Package bottle of dry, sterile vancomycin powder. The resultant solution will contain vancomycin equivalent to 500 mg/10 mL. AFTER RECONSTITUTION, FURTHER DILUTION IS REQUIRED.
Reconstituted solutions of vancomycin (500 mg/10 mL) must be further diluted in at least 100 mL of a suitable infusion solution. Doses of 1 gram/20 mL must be further diluted in at least 200 mL of a suitable infusion solution. The desired dose diluted in this manner should be administered by intermittent intravenous infusion over a period of at least 60 minutes.
10 g Pharmacy Bulk Package bottle
At the time of use, reconstitute by adding 95 mL of Sterile Water for Injection, USP to the 10 g bottle of dry, sterile vancomycin powder. The resultant solution will contain vancomycin equivalent to 500 mg/5 mL (1 g/10 mL). AFTER RECONSTITUTION, FURTHER DILUTION IS REQUIRED.
Reconstituted solutions of vancomycin (500 mg/5 mL) must be further diluted in at least 100 mL of a suitable infusion solution. For doses of 1 gram (10 mL), at least 200 mL of solution must be used. The desired dose diluted in this manner should be administered by intermittent IV infusion over a period of at least 60 minutes.
Parenteral drug products should be visually inspected for particulate matter and discoloration prior to administration, whenever solution and container permit.
For Oral Administration
Oral vancomycin is used in treating antibiotic-associated pseudomembranous colitis caused by C. difficile and for staphylococcal enterocolitis. Vancomycin is not effective by the oral route for other types of infections. The usual adult total daily dosage is 500 mg to 2 g given in 3 or 4 divided doses for 7 to 10 days. The total daily dose in children is 40 mg/kg of body weight in 3 or 4 divided doses for 7 to 10 days. The total daily dosage should not exceed 2 g. The appropriate dose may be diluted in 1 oz of water and given to the patients to drink. Common flavoring syrups may be added to the solution to improve the taste for oral administration. The diluted solution may be administered via a nasogastric tube.
HOW SUPPLIED
| NDC No. | |
|---|---|
| 70594-047-01 | Vancomycin Hydrochloride for Injection, USP equivalent to 5 g vancomycin in a Pharmacy Bulk Package Bottle, packaged individually |
| 70594-048-01 | Vancomycin Hydrochloride for Injection, USP equivalent to 10 g vancomycin in a Pharmacy Bulk Package Bottle, packaged individually |
Store dry powder at 20° to 25°C (68° to 77°F) [see USP Controlled Room temperature] in original container.
Vancomycin Hydrochloride for Injection USP, 5 g/vial is a white, almost white or tan solid in a clear glass vial with a yellow flip off cap.
Vancomycin Hydrochloride for Injection USP, 10 g/vial is a white, almost white or tan solid in a clear glass vial with a black flip off cap.
Bottle stoppers do not contain natural rubber latex.
ANIMAL PHARMACOLOGY
In animal studies, hypotension and bradycardia occurred in dogs receiving an intravenous infusion of vancomycin hydrochloride 25 mg/kg, at a concentration of 25 mg/mL and an infusion rate of 13.3 mL/min.
REFERENCES
- Moellering RC, Krogstad DJ, Greenblatt DJ: Vancomycin therapy in patients with impaired renal function: A nomogram for dosage. Ann Inter Med 1981;94:343.
Manufactured for:
Xellia Pharmaceuticals USA, LLC
Buffalo Grove, IL 60089
Made in Denmark
Revised: February 2022
2504-D
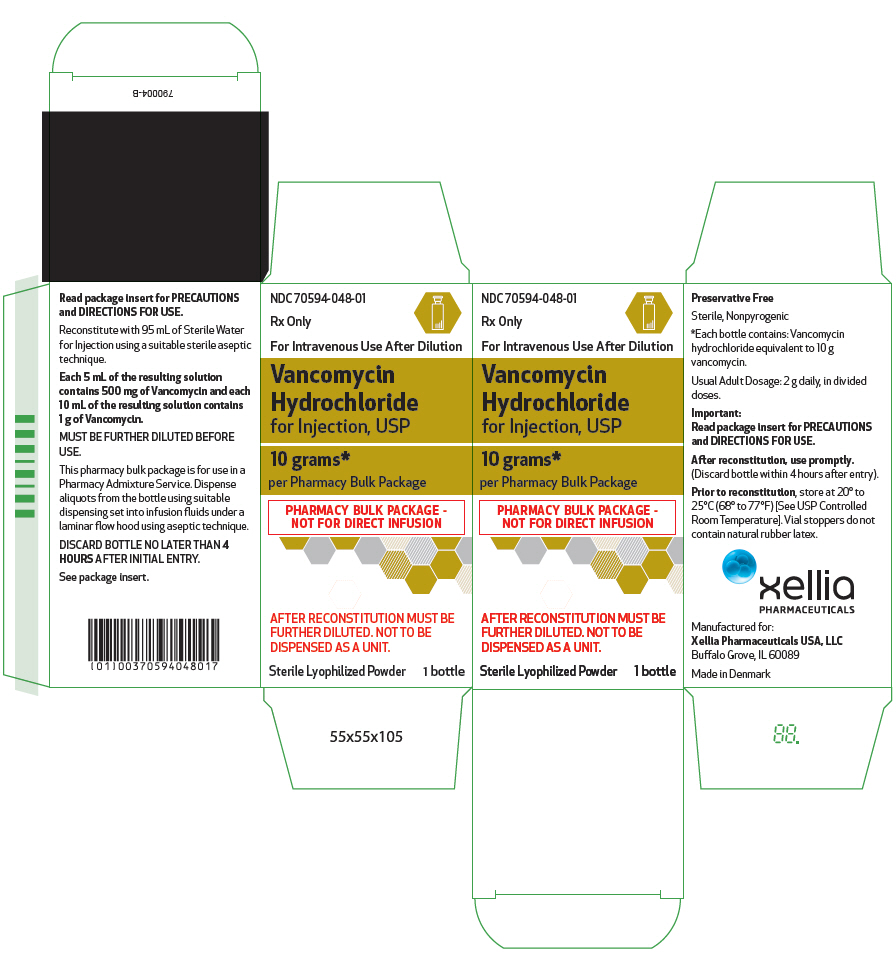
PRINCIPAL DISPLAY PANEL - 10 gram Bottle Carton
NDC 70594-048-01
Rx Only
For Intravenous Use After Dilution
Vancomycin
Hydrochloride
for Injection, USP
10 grams*
per Pharmacy Bulk Package
PHARMACY BULK PACKAGE -
NOT FOR DIRECT INFUSION
AFTER RECONSTITUTION MUST BE
FURTHER DILUTED. NOT TO BE
DISPENSED AS A UNIT.
Sterile Lyophilized Powder
1 bottle
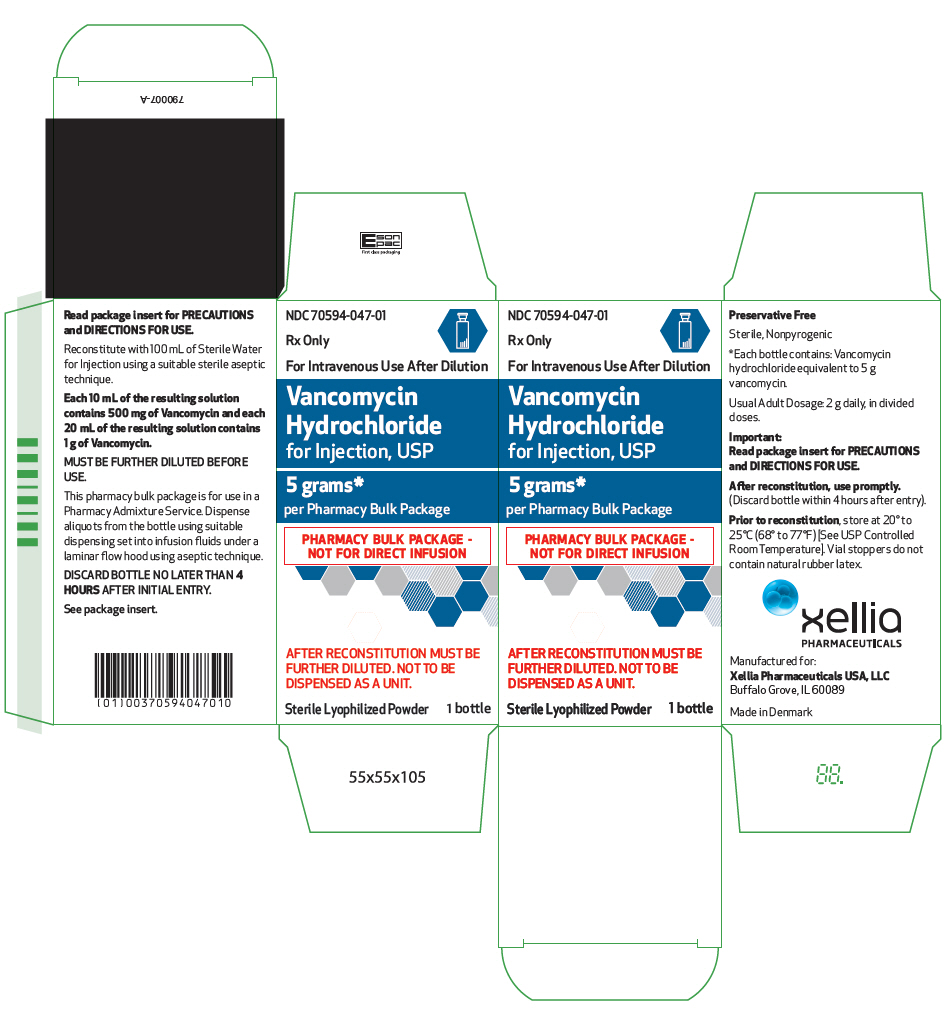
PRINCIPAL DISPLAY PANEL - 5 gram Bottle Carton
NDC 70594-047-01
Rx Only
For Intravenous Use After Dilution
Vancomycin
Hydrochloride
for Injection, USP
5 grams*
per Pharmacy Bulk Package
PHARMACY BULK PACKAGE -
NOT FOR DIRECT INFUSION
AFTER RECONSTITUTION MUST BE
FURTHER DILUTED. NOT TO BE
DISPENSED AS A UNIT.
Sterile Lyophilized Powder
1 bottle