HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use REYATAZ safely and effectively. See full prescribing information for REYATAZ.
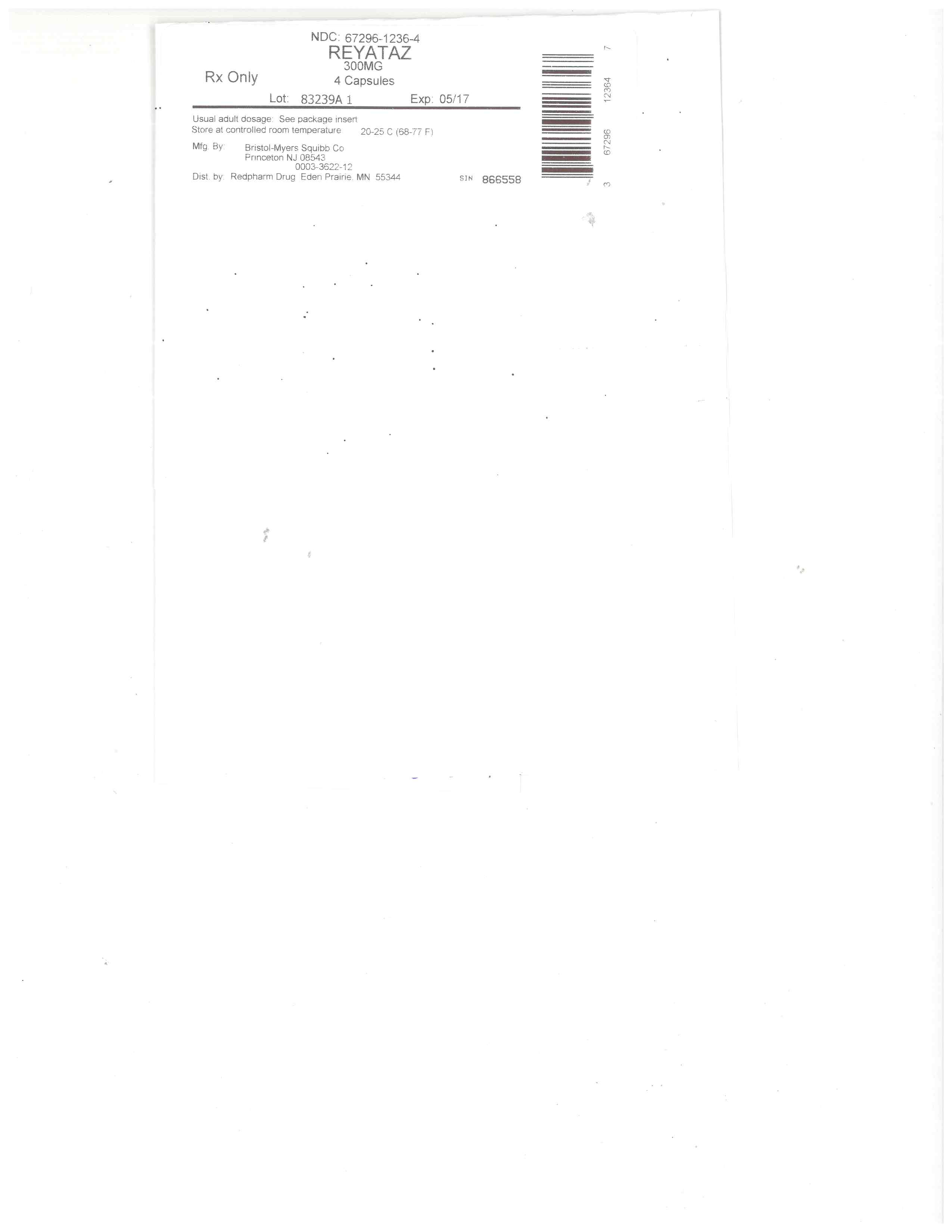
REYATAZ ® (atazanavir) capsules, for oral use
REYATAZ ® (atazanavir) oral powder
Initial U.S. Approval: 2003
RECENT MAJOR CHANGES
Indications and Usage (1) 9/2015
Dosage and Administration,
Overview (2.1) 9/2015
Dosage and Administration of REYATAZ
Oral Powder in Pediatric Patients (2.4) 9/2015
Contraindications (4) 9/2016
INDICATIONS AND USAGE
REYATAZ is a protease inhibitor indicated for use in combination with other antiretroviral agents for the treatment of HIV-1 infection for patients 3 months and older weighing at least 5 kg. (1)
DOSAGE AND ADMINISTRATION
•
Treatment-naive adults: REYATAZ 300 mg with ritonavir 100 mg once daily with food or REYATAZ 400 mg once daily with food. (2.2)
•
Treatment-experienced adults: REYATAZ 300 mg with ritonavir 100 mg once daily with food. (2.2)
•
Pediatric patients: REYATAZ capsule dosage is based on body weight not to exceed the adult dose and must be taken with food. (2.3)
•
REYATAZ oral powder: Must be taken with ritonavir and food and should not be used in pediatric patients who weigh less than 5 kg. (2.4)
•
Pregnancy: REYATAZ 300 mg with ritonavir 100 mg once daily with food, with dosing modifications for some concomitant medications. (2.5)
•
Dosing modifications: may be required for concomitant therapy (2.2, 2.3, 2.4, 2.5), renal impairment(2.6), and hepatic impairment (2.7).
DOSAGE FORMS AND STRENGTHS
•
Capsules: 150 mg, 200 mg, 300 mg. (3, 16)
•
Oral powder: 50 mg packet. (3, 16)
CONTRAINDICATIONS
•
REYATAZ is contraindicated in patients with previously demonstrated hypersensitivity (eg, Stevens-Johnson syndrome, erythema multiforme, or toxic skin eruptions) to any of the components of this product. (4)
•
Coadministration with alfuzosin, triazolam, orally administered midazolam, ergot derivatives, rifampin, irinotecan, lurasidone (if REYATAZ is coadministered with ritonavir), lovastatin, simvastatin, indinavir, cisapride, pimozide, St. John’s wort, nevirapine, and sildenafil when dosed as REVATIO ®. (4)
WARNINGS AND PRECAUTIONS
•
Cardiac conduction abnormalities: PR interval prolongation may occur in some patients. ECG monitoring should be considered in patients with preexisting conduction system disease or when administered with other drugs that may prolong the PR interval. (5.1, 7.3, 12.2, 17)
•
Severe Skin Reactions: Discontinue if severe rash develops. (5.2, 17)
•
Hyperbilirubinemia: Most patients experience asymptomatic increases in indirect bilirubin, which is reversible upon discontinuation. Do not dose reduce. If a concomitant transaminase increase occurs, evaluate for alternative etiologies. (5.3)
•
Phenylketonuria: REYATAZ oral powder contains phenylalanine which can be harmful to patients with phenylketonuria. (5.4)
•
Hepatotoxicity: Patients with hepatitis B or C infection are at risk of increased transaminases or hepatic decompensation. Monitor hepatic laboratory tests prior to therapy and during treatment.(2.7, 5.5, 8.8)
•
Nephrolithiasis and cholelithiasis have been reported. Consider temporary interruption or discontinuation. (5.6)
•
The concomitant use of REYATAZ/ritonavir and certain other medications may result in known or potentially significant drug interactions. Consult the full prescribing information prior to and during treatment for potential drug interactions. (5.7, 7.3)
•
Patients receiving REYATAZ may develop new onset or exacerbations of diabetes mellitus/hyperglycemia (5.8), immune reconstitution syndrome (5.9), and redistribution/accumulation of body fat (5.10).
•
Hemophilia: Spontaneous bleeding may occur and additional factor VIII may be required. (5.11)
ADVERSE REACTIONS
Most common adverse reactions (≥2%) are nausea, jaundice/scleral icterus, rash, headache, abdominal pain, vomiting, insomnia, peripheral neurologic symptoms, dizziness, myalgia, diarrhea, depression, and fever. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Bristol-Myers Squibb at 1-800-721-5072 or FDA at 1-800-FDA-1088 or WWW.FDA.GOV/MEDWATCH.
DRUG INTERACTIONS
Coadministration of REYATAZ can alter the concentration of other drugs and other drugs may alter the concentration of atazanavir. The potential drug-drug interactions must be considered prior to and during therapy. (4, 7, 12.3)
USE IN SPECIFIC POPULATIONS
•
Pregnancy: Available human and animal data suggest that atazanavir does not increase the risk of major birth defects overall compared to the background rate. (8.1)
•
Lactation: Breastfeeding is not recommended. (8.2)
•
Hepatitis B or C co-infection: Monitor liver enzymes. (5.5, 6.1)
•
Renal impairment: REYATAZ is not recommended for use in treatment-experienced patients with end stage renal disease managed with hemodialysis. (2.6, 8.7)
•
Hepatic impairment: REYATAZ is not recommended in patients with severe hepatic impairment. REYATAZ/ritonavir is not recommended in patients with any degree of hepatic impairment. (2.7, 8.8)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 9/2016
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Overview
2.2 Dosage of REYATAZ in Adult Patients
2.3 Dosage of REYATAZ Capsules in Pediatric Patients
2.4 Dosage and Administration of REYATAZ Oral Powder in Pediatric Patients
2.5 Dosage Adjustments in Pregnant Patients
2.6 Dosage in Patients with Renal Impairment
2.7 Dosage Adjustments in Patients with Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Conduction Abnormalities
5.2 Severe Skin Reactions
5.3 Hyperbilirubinemia
5.4 Patients with Phenylketonuria
5.5 Hepatotoxicity
5.6 Nephrolithiasis and Cholelithiasis
5.7 Risk of Serious Adverse Reactions Due to Drug Interactions
5.8 Diabetes Mellitus/Hyperglycemia
5.9 Immune Reconstitution Syndrome
5.10 Fat Redistribution
5.11 Hemophilia
5.12 Resistance/Cross-Resistance
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Potential for REYATAZ to Affect Other Drugs
7.2 Potential for Other Drugs to Affect REYATAZ
7.3 Established and Other Potentially Significant Drug Interactions
7.4 Drugs with No Observed Interactions with REYATAZ
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Age/Gender
8.7 Impaired Renal Function
8.8 Impaired Hepatic Function
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Adult Patients without Prior Antiretroviral Therapy
14.2 Adult Patients with Prior Antiretroviral Therapy
14.3 Pediatric Patients
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
*
Sections or subsections omitted from the full prescribing information are not listed.
1 INDICATIONS AND USAGE
REYATAZ® (atazanavir) is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection for patients 3 months and older weighing at least 5 kg.
Limitations of Use:
•
REYATAZ is not recommended for use in pediatric patients below the age of 3 months due to the risk of kernicterus.
•
Use of REYATAZ/ritonavir in treatment-experienced patients should be guided by the number of baseline primary protease inhibitor resistance substitutions [see MICROBIOLOGY (12.4)].
2 DOSAGE AND ADMINISTRATION
2.1 Overview
•
REYATAZ capsules and oral powder must be taken with food.
•
Do not open the capsules.
•
The recommended oral dosage of REYATAZ depends on the treatment history of the patient and the use of other coadministered drugs. When coadministered with H 2-receptor antagonists or proton-pump inhibitors, dose separation may be required [see DOSAGE AND ADMINISTRATION (2.2, 2.3, 2.4, 2.5) and DRUG INTERACTIONS (7)].
•
REYATAZ capsules without ritonavir are not recommended for treatment-experienced adult or pediatric patients with prior virologic failure [see CLINICAL STUDIES (14)].
•
REYATAZ oral powder must be taken with ritonavir and is not recommended for use in children who weigh less than 5 kg [see DOSAGE AND ADMINISTRATION (2.4)].
•
Efficacy and safety of REYATAZ with ritonavir when ritonavir is administered in doses greater than 100 mg once daily have not been established. The use of higher ritonavir doses may alter the safety profile of atazanavir (cardiac effects, hyperbilirubinemia) and, therefore, is not recommended. Prescribers should consult the complete prescribing information for ritonavir when using ritonavir.
2.2 Dosage of REYATAZ in Adult Patients
Table 1 displays the recommended dosage of REYATAZ capsules in treatment-naive and treatment-experienced adults. Table 1 also displays recommended dosage of REYATAZ and ritonavir when given concomitantly with other antiretroviral drugs and H2-receptor antagonists (H2RA). Ritonavir is required with several REYATAZ dosage regimens (see the ritonavir complete prescribing information about the safe and effective use of ritonavir). The use of REYATAZ in treatment-experienced adult patients without ritonavir is not recommended.
Table 1: Recommended REYATAZ and Ritonavir Dosage in Adultsa,b
a See DRUG INTERACTIONS (7) for instructions concerning coadministration of acid reducing medications (eg, H2RA or proton pump inhibitors [PPIs]), and other antiretroviral drugs (eg, efavirenz, tenofovir, and didanosine).
b For adult patients who cannot swallow the capsules, REYATAZ oral powder is taken once daily with food at the same recommended adult dosage as the capsules along with ritonavir.
REYATAZ Once Daily
Dosage
Ritonavir Once Daily
Dosage
Treatment-Naive Adult Patients
recommended regimen
300 mg
100 mg
unable to tolerate ritonavir
400 mg
N/A
in combination with efavirenz
400 mg
100 mg
Treatment-Experienced Adult Patients
recommended regimen
300 mg
100 mg
in combination with both H2RA and tenofovir
400 mg
100 mg
2.3 Dosage of REYATAZ Capsules in Pediatric Patients
The recommended daily dosage of REYATAZ capsules and ritonavir in pediatric patients (6 years of age to less than 18 years of age) is based on body weight (see Table 2).
Table 2: Recommended Dosage of REYATAZ Capsules and Ritonavir in Pediatric Patients (6 to less than 18 years of age)a,b
a Administer REYATAZ capsules and ritonavir simultaneously with food.
b The same recommendations regarding the timing and maximum doses of concomitant PPIs and H2RAs in adults also apply to pediatric patients. See DRUG INTERACTIONS (7) for instructions concerning coadministration of acid reducing medications (eg, H2RA or PPIs), and other antiretroviral drugs (eg, efavirenz, tenofovir, and didanosine).
c In treatment-experienced patients, REYATAZ capsules must be administered with ritonavir.
Body weight
REYATAZ Daily Dosage
Ritonavir Daily Dosage
Treatment-Naive and Treatment-Experiencedc
Less than 15 kg
Capsules not recommended
N/A
15 kg to less than 20 kg
150 mg
100 mg
20 kg to less than 40 kg
200 mg
100 mg
At least 40 kg
300 mg
100 mg
Treatment-Naive, at least 13 years old and cannot tolerate ritonavirc
At least 40 kg
400 mg
N/A
2.4 Dosage and Administration of REYATAZ Oral Powder in Pediatric Patients
REYATAZ oral powder is for use in treatment-naive or treatment-experienced pediatric patients who are at least 3 months of age and weighing at least 5 kg. REYATAZ oral powder must be mixed with food or beverage for administration and ritonavir must be given immediately afterwards. Table 3 displays the recommended dosage of REYATAZ oral powder and ritonavir.
Table 3: Recommended Dosage of REYATAZ Oral Powder and Ritonavir in Pediatric Patients (at least 3 months of age and weighing at least 5 kg)a,b
a The same recommendations regarding the timing and maximum doses of concomitant PPIs and H2RAs in adults also apply to pediatric patients. See DRUG INTERACTIONS (7) for instructions concerning coadministration of acid reducing medications (eg, H2RA or PPIs), and other antiretroviral drugs (eg, efavirenz, tenofovir, and didanosine).
b For pediatric patients at least 25 kg who cannot swallow REYATAZ capsules, 300 mg (6 packets) REYATAZ oral powder is taken once daily with food along with 100 mg ritonavir.
c Only patients weighing 5 to less than 10 kg who do not tolerate the 200 mg (4 packets) dose of REYATAZ oral powder and have not previously taken an HIV protease inhibitor, may take 150 mg (3 packets) REYATAZ oral powder with close HIV viral load monitoring.
d Each packet contains 50 mg of REYATAZ.
Body Weight
Daily Dosage of REYATAZ
Oral Powder
Daily Dosage of Ritonavir
Oral Solution
5 kg to less than 15 kg
200 mg (4 packets)c,d
80 mg
15 kg to less than 25 kg
250 mg (5 packets)d
80 mg
Instructions for Mixing REYATAZ Oral Powder [see FDA-approved Instructions for Use]
•
Determine the number of packets (3, 4, 5 or 6 packets) that are needed.
•
Prior to mixing, tap the packet to settle the powder.
•
It is preferable to mix REYATAZ oral powder with food such as applesauce or yogurt. Mixing REYATAZ oral powder with a beverage (milk, infant formula, or water) may be used for infants who can drink from a cup. For young infants (less than 6 months) who cannot eat solid food or drink from a cup, REYATAZ oral powder should be mixed with infant formula and given using an oral dosing syringe. Administration of REYATAZ and infant formula using an infant bottle is not recommended because full dose may not be delivered.
•
Use a clean pair of scissors to cut each packet along the dotted line.
•
Mixing with food: Using a spoon, mix the recommended number of REYATAZ oral powder packets with a minimum of one tablespoon of food (such as applesauce or yogurt). Feed the mixture to the infant or young child. Add an additional one tablespoon of food to the small container, mix, and feed the child the residual mixture.
•
Mixing with a beverage such as milk or water in a small drinking cup: Using a spoon, mix the recommended number of REYATAZ oral powder packets with a minimum of 30 mL of the beverage. Have the child drink the mixture. Add an additional 15 mL more of beverage to the drinking cup, mix, and have the child drink the residual mixture. If water is used, food should also be taken at the same time.
•
Mixing with liquid infant formula using an oral dosing syringe and a small medicine cup: Using a spoon, mix the recommended number of REYATAZ oral powder packets with 10 mL of prepared liquid infant formula. Draw up the full amount of the mixture into an oral syringe and administer into either right or left inner cheek of infant. Pour another 10 mL of formula into the medicine cup to rinse off remaining REYATAZ oral powder in cup. Draw up residual mixture into the syringe and administer into either right or left inner cheek of infant.
•
Administer ritonavir immediately following REYATAZ powder administration.
•
Administer the entire dosage of REYATAZ oral powder (mixed in the food or beverage) within one hour of preparation (may leave the mixture at room temperature during this one hour period). Ensure that the patient eats or drinks all the food or beverage that contains the powder. Additional food may be given after consumption of the entire mixture.
2.5 Dosage Adjustments in Pregnant Patients
Table 4 includes the recommended dosage of REYATAZ capsules and ritonavir in treatment-naive and treatment-experienced pregnant patients. In these patients, REYATAZ must be administered with ritonavir. There are no dosage adjustments for postpartum patients (see Table 1 for the recommended REYATAZ dosage in adults). [See USE IN SPECIFIC POPULATIONS (8.1).]
Table 4: Recommended Dosage of REYATAZ and Ritonavir in Pregnant Patientsa
a See DRUG INTERACTIONS (7) for instructions concerning coadministration of acid reducing medications (eg, H2RA or PPIs), and other antiretroviral drugs (eg, efavirenz, tenofovir, and didanosine).
b REYATAZ is not recommended for treatment-experienced pregnant patients during the second and third trimester taking REYATAZ with both tenofovir and H2RA.
REYATAZ
Once Daily
Dosage
Ritonavir
Once Daily
Dosage
Treatment-Naive and Treatment-Experienced
Recommended Regimen
300 mg
100 mg
Treatment-Experienced During the Second or Third Trimester When Coadministered with either H2RA or Tenofovirb
In combination with either H2RA or tenofovir
400 mg
100 mg
2.6 Dosage in Patients with Renal Impairment
For patients with renal impairment, including those with severe renal impairment who are not managed with hemodialysis, no dose adjustment is required for REYATAZ. Treatment-naive patients with end stage renal disease managed with hemodialysis should receive REYATAZ 300 mg with ritonavir 100 mg. REYATAZ is not recommended in HIV-treatment-experienced patients with end stage renal disease managed with hemodialysis. [See USE IN SPECIFIC POPULATIONS (8.7).]
2.7 Dosage Adjustments in Patients with Hepatic Impairment
Table 5 displays the recommended REYATAZ dosage in treatment-naive patients with hepatic impairment. The use of REYATAZ in patients with severe hepatic impairment (Child-Pugh Class C) is not recommended. The coadministration of REYATAZ with ritonavir in patients with any degree of hepatic impairment is not recommended.
Table 5: Recommended Dosage of REYATAZ Capsules in Treatment-Naive Adults with Hepatic Impairment
REYATAZ Once Daily Dosage
Mild hepatic impairment (Child-Pugh Class A)
400 mg
Moderate hepatic impairment (Child-Pugh Class B)
300 mg
Severe hepatic impairment (Child-Pugh Class C)
REYATAZ with or without ritonavir is not recommended
3 DOSAGE FORMS AND STRENGTHS
REYATAZ Capsules:
•
150 mg capsule with blue cap and powder blue body, printed with white ink “BMS 150 mg” on the cap and with blue ink “3624” on the body.
•
200 mg capsule with blue cap and blue body, printed with white ink “BMS 200 mg” on the cap and with white ink “3631” on the body.
•
300 mg capsule with red cap and blue body, printed with white ink “BMS 300 mg” on the cap and with white ink “3622” on the body.
REYATAZ Oral Powder:
•
50 mg of atazanavir as an oral powder in a packet.
4 CONTRAINDICATIONS
REYATAZ is contraindicated:
•
in patients with previously demonstrated clinically significant hypersensitivity (eg, Stevens-Johnson syndrome, erythema multiforme, or toxic skin eruptions) to any of the components of REYATAZ capsules or REYATAZ oral powder [see WARNINGS AND PRECAUTIONS (5.2)].
•
when coadministered with drugs that are highly dependent on CYP3A or UGT1A1 for clearance, and for which elevated plasma concentrations of the interacting drugs are associated with serious and/or life-threatening events (see Table 6).
•
when coadministered with drugs that strongly induce CYP3A and may lead to lower exposure and loss of efficacy of REYATAZ (see Table 6).
Table 6 displays drugs that are contraindicated with REYATAZ.
Table 6: Drugs that are Contraindicated with REYATAZ (Information in the table applies to REYATAZ with or without ritonavir, unless otherwise indicated)
a See DRUG INTERACTIONS, TABLE 16 (7) for parenterally administered midazolam.
b See DRUG INTERACTIONS, TABLE 16 (7) for sildenafil when dosed as VIAGRA® for erectile dysfunction.
Drug Class
Drugs within class that are contraindicated with REYATAZ
Clinical Comment
Alpha 1-Adrenoreceptor Antagonist
Alfuzosin
Potential for increased alfuzosin concentrations, which can result in hypotension.
Antimycobacterials
Rifampin
Rifampin substantially decreases plasma concentrations of atazanavir, which may result in loss of therapeutic effect and development of resistance.
Antineoplastics
Irinotecan
Atazanavir inhibits UGT1A1 and may interfere with the metabolism of irinotecan, resulting in increased irinotecan toxicities.
Antipsychotics
Lurasidone
Potential for serious and/or life-threatening reactions if REYATAZ is coadministered with ritonavir.
Pimozide
Potential for serious and/or life-threatening reactions such as cardiac arrhythmias.
Benzodiazepines
Triazolam, orally administered midazolama
Triazolam and orally administered midazolam are extensively metabolized by CYP3A4. Coadministration of triazolam or orally administered midazolam with REYATAZ may cause large increases in the concentration of these benzodiazepines. Potential for serious and/or life-threatening events such as prolonged or increased sedation or respiratory depression.
Ergot Derivatives
Dihydroergotamine, ergotamine, ergonovine, methylergonovine
Potential for serious and/or life-threatening events such as acute ergot toxicity characterized by peripheral vasospasm and ischemia of the extremities and other tissues.
GI Motility Agent
Cisapride
Potential for serious and/or life-threatening reactions such as cardiac arrhythmias.
Herbal Products
St. John’s wort (Hypericum perforatum)
Coadministration of St. John’s wort and REYATAZ may result in loss of therapeutic effect and development of resistance.
HMG-CoA Reductase Inhibitors
Lovastatin, simvastatin
Potential for serious reactions such as myopathy, including rhabdomyolysis.
PDE5 Inhibitor
Sildenafilb when dosed as REVATIO® for the treatment of pulmonary arterial hypertension
Potential for sildenafil-associated adverse events (which include visual disturbances, hypotension, priapism, and syncope).
Protease Inhibitors
Indinavir
Both REYATAZ and indinavir are associated with indirect (unconjugated) hyperbilirubinemia.
Non-nucleoside Reverse Transcriptase Inhibitors
Nevirapine
Nevirapine substantially decreases atazanavir exposure which may result in loss of therapeutic effect and development of resistance. Potential risk for nevirapine-associated adverse reactions due to increased nevirapine exposures.
Table 6: Drugs that are Contraindicated with REYATAZ (Information in the table applies to REYATAZ with or without ritonavir, unless otherwise indicated)
a See DRUG INTERACTIONS, TABLE 16 (7) for parenterally administered midazolam.
b See DRUG INTERACTIONS, TABLE 16 (7) for sildenafil when dosed as VIAGRA® for erectile dysfunction.
5 WARNINGS AND PRECAUTIONS
5.1 Cardiac Conduction Abnormalities
REYATAZ has been shown to prolong the PR interval of the electrocardiogram in some patients. In healthy volunteers and in patients, abnormalities in atrioventricular (AV) conduction were asymptomatic and generally limited to first-degree AV block. There have been reports of second-degree AV block and other conduction abnormalities [see ADVERSE REACTIONS (6.2) and OVERDOSAGE (10)]. In clinical trials that included electrocardiograms, asymptomatic first-degree AV block was observed in 5.9% of atazanavir-treated patients (n=920), 5.2% of lopinavir/ritonavir-treated patients (n=252), 10.4% of nelfinavir-treated patients (n=48), and 3.0% of efavirenz-treated patients (n=329). In Study AI424-045, asymptomatic first-degree AV block was observed in 5% (6/118) of atazanavir/ritonavir-treated patients and 5% (6/116) of lopinavir/ritonavir-treated patients who had on-study electrocardiogram measurements. Because of limited clinical experience in patients with preexisting conduction system disease (eg, marked first-degree AV block or second- or third-degree AV block). ECG monitoring should be considered in these patients. [See CLINICAL PHARMACOLOGY (12.2).]
5.2 Severe Skin Reactions
In controlled clinical trials, rash (all grades, regardless of causality) occurred in approximately 20% of patients treated with REYATAZ. The median time to onset of rash in clinical studies was 7.3 weeks and the median duration of rash was 1.4 weeks. Rashes were generally mild-to-moderate maculopapular skin eruptions. Treatment-emergent adverse reactions of moderate or severe rash (occurring at a rate of ≥2%) are presented for the individual clinical studies [see ADVERSE REACTIONS (6.1)]. Dosing with REYATAZ was often continued without interruption in patients who developed rash. The discontinuation rate for rash in clinical trials was <1%. Cases of Stevens-Johnson syndrome, erythema multiforme, and toxic skin eruptions, including drug rash, eosinophilia, and systemic symptoms (DRESS) syndrome, have been reported in patients receiving REYATAZ. [See CONTRAINDICATIONS (4) and ADVERSE REACTIONS (6.1).] REYATAZ should be discontinued if severe rash develops.
5.3 Hyperbilirubinemia
Most patients taking REYATAZ experience asymptomatic elevations in indirect (unconjugated) bilirubin related to inhibition of UDP-glucuronosyl transferase (UGT). This hyperbilirubinemia is reversible upon discontinuation of REYATAZ. Hepatic transaminase elevations that occur with hyperbilirubinemia should be evaluated for alternative etiologies. No long-term safety data are available for patients experiencing persistent elevations in total bilirubin >5 times the upper limit of normal (ULN). Alternative antiretroviral therapy to REYATAZ may be considered if jaundice or scleral icterus associated with bilirubin elevations presents cosmetic concerns for patients. Dose reduction of atazanavir is not recommended since long-term efficacy of reduced doses has not been established. [See ADVERSE REACTIONS (6.1).]
5.4 Patients with Phenylketonuria
Phenylalanine can be harmful to patients with phenylketonuria (PKU). REYATAZ oral powder contains phenylalanine (a component of aspartame). Each packet of REYATAZ oral powder contains 35 mg of phenylalanine. REYATAZ capsules do not contain phenylalanine.
5.5 Hepatotoxicity
Patients with underlying hepatitis B or C viral infections or marked elevations in transaminases before treatment may be at increased risk for developing further transaminase elevations or hepatic decompensation. In these patients, hepatic laboratory testing should be conducted prior to initiating therapy with REYATAZ and during treatment. [See ADVERSE REACTIONS (6.1) and USE IN SPECIFIC POPULATIONS (8.8).]
5.6 Nephrolithiasis and Cholelithiasis
Cases of nephrolithiasis and/or cholelithiasis have been reported during postmarketing surveillance in HIV-infected patients receiving REYATAZ therapy. Some patients required hospitalization for additional management and some had complications. Because these events were reported voluntarily during clinical practice, estimates of frequency cannot be made. If signs or symptoms of nephrolithiasis and/or cholelithiasis occur, temporary interruption or discontinuation of therapy may be considered. [See ADVERSE REACTIONS (6.2).]
5.7 Risk of Serious Adverse Reactions Due to Drug Interactions
Initiation of REYATAZ with ritonavir, a CYP3A inhibitor, in patients receiving medications metabolized by CYP3A or initiation of medications metabolized by CYP3A in patients already receiving REYATAZ with ritonavir, may increase plasma concentrations of medications metabolized by CYP3A. Initiation of medications that inhibit or induce CYP3A may increase or decrease concentrations of REYATAZ with ritonavir, respectively. These interactions may lead to:
•
clinically significant adverse reactions potentially leading to severe, life threatening, or fatal events from greater exposures of concomitant medications.
•
clinically significant adverse reactions from greater exposures of REYATAZ with ritonavir.
•
loss of therapeutic effect of REYATAZ with ritonavir and possible development of resistance.
See Table 16 for steps to prevent or manage these possible and known significant drug interactions, including dosing recommendations [see DRUG INTERACTIONS (7)]. Consider the potential for drug interactions prior to and during REYATAZ/ritonavir therapy; review concomitant medications during REYATAZ/ritonavir therapy; and monitor for the adverse reactions associated with the concomitant medications [see CONTRAINDICATIONS (4) and DRUG INTERACTIONS (7)].
5.8 Diabetes Mellitus/Hyperglycemia
New-onset diabetes mellitus, exacerbation of preexisting diabetes mellitus, and hyperglycemia have been reported during postmarketing surveillance in HIV-infected patients receiving protease inhibitor therapy. Some patients required either initiation or dose adjustments of insulin or oral hypoglycemic agents for treatment of these events. In some cases, diabetic ketoacidosis has occurred. In those patients who discontinued protease inhibitor therapy, hyperglycemia persisted in some cases. Because these events have been reported voluntarily during clinical practice, estimates of frequency cannot be made and a causal relationship between protease inhibitor therapy and these events has not been established. [See ADVERSE REACTIONS (6.2).]
5.9 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including REYATAZ. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jiroveci pneumonia, or tuberculosis), which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves’ disease, polymyositis, and Guillain-Barré syndrome) have also been reported to occur in the setting of immune reconstitution; however, the time to onset is more variable, and can occur many months after initiation of treatment.
5.10 Fat Redistribution
Redistribution/accumulation of body fat including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and “cushingoid appearance” have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
5.11 Hemophilia
There have been reports of increased bleeding, including spontaneous skin hematomas and hemarthrosis, in patients with hemophilia type A and B treated with protease inhibitors. In some patients additional factor VIII was given. In more than half of the reported cases, treatment with protease inhibitors was continued or reintroduced. A causal relationship between protease inhibitor therapy and these events has not been established.
5.12 Resistance/Cross-Resistance
Various degrees of cross-resistance among protease inhibitors have been observed. Resistance to atazanavir may not preclude the subsequent use of other protease inhibitors. [See MICROBIOLOGY (12.4).]
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling:
•
cardiac conduction abnormalities [see WARNINGS AND PRECAUTIONS (5.1)]
•
rash [see WARNINGS AND PRECAUTIONS (5.2)]
•
hyperbilirubinemia [see WARNINGS AND PRECAUTIONS (5.3)]
•
nephrolithiasis and cholelithiasis [see WARNINGS AND PRECAUTIONS (5.6)]
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.1 Clinical Trial Experience
Adverse Reactions in Treatment-Naive Adult Patients
The safety profile of REYATAZ in treatment-naive adults is based on 1625 HIV-1 infected patients in clinical trials. 536 patients received REYATAZ 300 mg with ritonavir 100 mg and 1089 patients received REYATAZ 400 mg or higher (without ritonavir).
The most common adverse reactions were nausea, jaundice/scleral icterus, and rash.
Selected clinical adverse reactions of moderate or severe intensity reported in ≥2% of treatment-naive patients receiving combination therapy including REYATAZ 300 mg with ritonavir 100 mg and REYATAZ 400 mg (without ritonavir) are presented in Tables 7 and 8, respectively.
Table 7: Selected Adverse Reactionsa of Moderate or Severe Intensity Reported in ≥2% of Adult Treatment-Naive Patients,b Study AI424-138
* None reported in this treatment arm.
a Includes events of possible, probable, certain, or unknown relationship to treatment regimen.
b Based on the regimen containing REYATAZ.
c Median time on therapy.
d As a fixed-dose combination: 300 mg tenofovir, 200 mg emtricitabine once daily.
96 weeksc
REYATAZ 300 mg with ritonavir
100 mg (once daily) and tenofovir
with emtricitabined
(n=441)
96 weeksc
lopinavir 400 mg with ritonavir
100 mg (twice daily) and tenofovir
with emtricitabined
(n=437)
Digestive System
Nausea
4%
8%
Jaundice/scleral icterus
5%
*
Diarrhea
2%
12%
Skin and Appendages
Rash
3%
2%
Table 8: Selected Adverse Reactionsa of Moderate or Severe Intensity Reported in ≥2% of Adult Treatment-Naive Patients,b Studies AI424-034, AI424-007, and AI424-008
* None reported in this treatment arm.
a Includes events of possible, probable, certain, or unknown relationship to treatment regimen.
b Based on regimens containing REYATAZ.
c Median time on therapy.
d Includes long-term follow-up.
e As a fixed-dose combination: 150 mg lamivudine, 300 mg zidovudine twice daily.
Study AI424-034
Studies AI424-007, -008
64 weeksc
REYATAZ
400 mg once daily
+ lamivudine +
zidovudinee
(n=404)
64 weeksc
efavirenz
600 mg once daily
+ lamivudine +
zidovudinee
(n=401)
120 weeksc,d
REYATAZ
400 mg once daily
+ stavudine +
lamivudine or
didanosine
(n=279)
73 weeksc,d
nelfinavir
750 mg TID or
1250 mg BID +
stavudine +
lamivudine or
didanosine
(n=191)
Body as a Whole
Headache
6%
6%
1%
2%
Digestive System
Nausea
14%
12%
6%
4%
Jaundice/scleral icterus
7%
*
7%
*
Vomiting
4%
7%
3%
3%
Abdominal pain
4%
4%
4%
2%
Diarrhea
1%
2%
3%
16%
Nervous System
Insomnia
3%
3%
<1%
*
Dizziness
2%
7%
<1%
*
Peripheral neurologic symptoms
<1%
1%
4%
3%
Skin and Appendages
Rash
7%
10%
5%
1%
Adverse Reactions in Treatment-Experienced Adult Patients
The safety profile of REYATAZ in treatment-experienced adults is based on 119 HIV-1 infected patients in clinical trials.
The most common adverse reactions are jaundice/scleral icterus and myalgia.
Selected clinical adverse reactions of moderate or severe intensity reported in ≥2% of treatment-experienced patients receiving REYATAZ/ritonavir are presented in Table 9.
Table 9: Selected Adverse Reactionsa of Moderate or Severe Intensity Reported in ≥2% of Adult Treatment-Experienced Patients,b Study AI424-045
* None reported in this treatment arm.
a Includes events of possible, probable, certain, or unknown relationship to treatment regimen.
b Based on the regimen containing REYATAZ.
c Median time on therapy.
d As a fixed-dose combination.
48 weeksc
REYATAZ/ritonavir 300/100 mg
once daily + tenofovir + NRTI
(n=119)
48 weeksc
lopinavir/ritonavir 400/100 mg
twice dailyd + tenofovir + NRTI
(n=118)
Body as a Whole
Fever
2%
*
Digestive System
Jaundice/scleral icterus
9%
*
Diarrhea
3%
11%
Nausea
3%
2%
Nervous System
Depression
2%
<1%
Musculoskeletal System
Myalgia
4%
*
Laboratory Abnormalities in Treatment-Naive Patients
The percentages of adult treatment-naive patients treated with combination therapy including REYATAZ 300 mg with ritonavir 100 mg and REYATAZ 400 mg (without ritonavir) with Grade 3–4 laboratory abnormalities are presented in Tables 10 and 11, respectively.
Table 10: Grade 3�4 Laboratory Abnormalities Reported in ≥2% of Adult Treatment-Naive Patients,a Study AI424-138
a Based on the regimen containing REYATAZ.
b Median time on therapy.
c ULN = upper limit of normal.
d As a fixed-dose combination: 300 mg tenofovir, 200 mg emtricitabine once daily.
96 weeksb
REYATAZ 300 mg
with ritonavir 100 mg
(once daily) and tenofovir
with emtricitabined
96 weeksb
lopinavir 400 mg
with ritonavir 100 mg
(twice daily) and tenofovir
with emtricitabined
Variable
Limitc
(n=441)
(n=437)
Chemistry
High
SGOT/AST
≥5.1 × ULN
3%
1%
SGPT/ALT
≥5.1 × ULN
3%
2%
Total Bilirubin
≥2.6 × ULN
44%
<1%
Lipase
≥2.1 × ULN
2%
2%
Creatine Kinase
≥5.1 × ULN
8%
7%
Total Cholesterol
≥240 mg/dL
11%
25%
Hematology
Low
Neutrophils
<750 cells/mm3
5%
2%
Table 11: Grade 3–4 Laboratory Abnormalities Reported in ≥2% of Adult Treatment-Naive Patients,a Studies AI424-034, AI424-007, and AI424-008
* None reported in this treatment arm.
a Based on regimen(s) containing REYATAZ.
b Median time on therapy.
c Includes long-term follow-up.
d ULN = upper limit of normal.
e As a fixed-dose combination: 150 mg lamivudine, 300 mg zidovudine twice daily.
Study AI424-034
Studies AI424-007, -008
64 weeksb
REYATAZ
400 mg
once daily
+ lamivudine
+ zidovudinee
64 weeksb
efavirenz
600 mg
once daily
+ lamivudine
+ zidovudinee
120 weeksb,c
REYATAZ
400 mg
once daily
+ stavudine
+ lamivudine or
+ stavudine
+ didanosine
73 weeksb,c
nelfinavir
750 mg TID or
1250 mg BID
+ stavudine
+ lamivudine or
+ stavudine
+ didanosine
Variable
Limitd
(n=404)
(n=401)
(n=279)
(n=191)
Chemistry
High
SGOT/AST
≥5.1 × ULN
2%
2%
7%
5%
SGPT/ALT
≥5.1 × ULN
4%
3%
9%
7%
Total Bilirubin
≥2.6 × ULN
35%
<1%
47%
3%
Amylase
≥2.1 × ULN
*
*
14%
10%
Lipase
≥2.1 × ULN
<1%
1%
4%
5%
Creatine
Kinase
≥5.1 × ULN
6%
6%
11%
9%
Total Cholesterol
≥240 mg/dL
6%
24%
19%
48%
Triglycerides
≥751 mg/dL
<1%
3%
4%
2%
Hematology
Low
Hemoglobin
<8.0 g/dL
5%
3%
<1%
4%
Neutrophils
<750 cells/mm3
7%
9%
3%
7%
Change in Lipids from Baseline in Treatment-Naive Patients
For Study AI424-138 and Study AI424-034, changes from baseline in LDL-cholesterol, HDL-cholesterol, total cholesterol, and triglycerides are shown in Tables 12 and 13, respectively.
Table 12: Lipid Values, Mean Change from Baseline, Study AI424-138
a REYATAZ 300 mg with ritonavir 100 mg once daily with the fixed-dose combination: 300 mg tenofovir, 200 mg emtricitabine once daily.
b Values obtained after initiation of serum lipid-reducing agents were not included in these analyses. At baseline, serum lipid-reducing agents were used in 1% in the lopinavir/ritonavir treatment arm and 1% in the REYATAZ/ritonavir arm. Through Week 48, serum lipid-reducing agents were used in 8% in the lopinavir/ritonavir treatment arm and 2% in the REYATAZ/ritonavir arm. Through Week 96, serum lipid-reducing agents were used in 10% in the lopinavir/ritonavir treatment arm and 3% in the REYATAZ/ritonavir arm.
c Lopinavir 400 mg with ritonavir 100 mg twice daily with the fixed-dose combination 300 mg tenofovir, 200 mg emtricitabine once daily.
d The change from baseline is the mean of within-patient changes from baseline for patients with both baseline and Week 48 or Week 96 values and is not a simple difference of the baseline and Week 48 or Week 96 mean values, respectively.
e Number of patients with LDL-cholesterol measured.
f Fasting.
REYATAZ/ritonavira,b
lopinavir/ritonavirb,c
Baseline
Week 48
Week 96
Baseline
Week 48
Week 96
mg/dL
mg/dL
Changed
mg/dL
Changed
mg/dL
mg/dL
Changed
mg/dL
Changed
(n=428e)
(n=372e)
(n=372e)
(n=342e)
(n=342e)
(n=424e)
(n=335e)
(n=335e)
(n=291e)
(n=291e)
LDL-Cholesterolf
92
105
+14%
105
+14%
93
111
+19%
110
+17%
HDL-Cholesterolf
37
46
+29%
44
+21%
36
48
+37%
46
+29%
Total Cholesterolf
149
169
+13%
169
+13%
150
187
+25%
186
+25%
Triglyceridesf
126
145
+15%
140
+13%
129
194
+52%
184
+50%
Table 13: Lipid Values, Mean Change from Baseline, Study AI424-034
a REYATAZ 400 mg once daily with the fixed-dose combination: 150 mg lamivudine, 300 mg zidovudine twice daily.
b Values obtained after initiation of serum lipid-reducing agents were not included in these analyses. At baseline, serum lipid-reducing agents were used in 0% in the efavirenz treatment arm and <1% in the REYATAZ arm. Through Week 48, serum lipid-reducing agents were used in 3% in the efavirenz treatment arm and 1% in the REYATAZ arm.
c Efavirenz 600 mg once daily with the fixed-dose combination: 150 mg lamivudine, 300 mg zidovudine twice daily.
d The change from baseline is the mean of within-patient changes from baseline for patients with both baseline and Week 48 values and is not a simple difference of the baseline and Week 48 mean values.
e Number of patients with LDL-cholesterol measured.
f Fasting.
REYATAZa,b
efavirenzb,c
Baseline
mg/dL
(n=383e)
Week 48
mg/dL
(n=283e)
Week 48
Changed
(n=272e)
Baseline
mg/dL
(n=378e)
Week 48
mg/dL
(n=264e)
Week 48
Changed
(n=253e)
LDL-Cholesterolf
98
98
+1%
98
114
+18%
HDL-Cholesterol
39
43
+13%
38
46
+24%
Total Cholesterol
164
168
+2%
162
195
+21%
Triglyceridesf
138
124
−9%
129
168
+23%
Laboratory Abnormalities in Treatment-Experienced Patients
The percentages of adult treatment-experienced patients treated with combination therapy including REYATAZ/ritonavir with Grade 3–4 laboratory abnormalities are presented in Table 14.
Table 14: Grade 3–4 Laboratory Abnormalities Reported in ≥2% of Adult Treatment-Experienced Patients, Study AI424-045a
a Based on regimen(s) containing REYATAZ.
b Median time on therapy.
c ULN = upper limit of normal.
d As a fixed-dose combination.
48 weeksb
48 weeksb
REYATAZ/ritonavir
300/100 mg once daily +
tenofovir + NRTI
lopinavir/ritonavir
400/100 mg twice dailyd + tenofovir + NRTI
Variable
Limitc
(n=119)
(n=118)
Chemistry
High
SGOT/AST
≥5.1 × ULN
3%
3%
SGPT/ALT
≥5.1 × ULN
4%
3%
Total Bilirubin
≥2.6 × ULN
49%
<1%
Lipase
≥2.1 × ULN
5%
6%
Creatine Kinase
≥5.1 × ULN
8%
8%
Total Cholesterol
≥240 mg/dL
25%
26%
Triglycerides
≥751 mg/dL
8%
12%
Glucose
≥251 mg/dL
5%
<1%
Hematology
Low
Platelets
<50,000 cells/mm3
2%
3%
Neutrophils
<750 cells/mm3
7%
8%
Change in Lipids from Baseline in Treatment-Experienced Patients
For Study AI424-045, changes from baseline in LDL-cholesterol, HDL-cholesterol, total cholesterol, and triglycerides are shown in Table 15. The observed magnitude of dyslipidemia was less with REYATAZ/ritonavir than with lopinavir/ritonavir. However, the clinical impact of such findings has not been demonstrated.
Table 15: Lipid Values, Mean Change from Baseline, Study AI424-045
a REYATAZ 300 mg once daily + ritonavir + tenofovir + 1 NRTI.
b Values obtained after initiation of serum lipid-reducing agents were not included in these analyses. At baseline, serum lipid-reducing agents were used in 4% in the lopinavir/ritonavir treatment arm and 4% in the REYATAZ/ritonavir arm. Through Week 48, serum lipid-reducing agents were used in 19% in the lopinavir/ritonavir treatment arm and 8% in the REYATAZ/ritonavir arm.
c Lopinavir/ritonavir (400/100 mg) BID + tenofovir + 1 NRTI.
d The change from baseline is the mean of within-patient changes from baseline for patients with both baseline and Week 48 values and is not a simple difference of the baseline and Week 48 mean values.
e Number of patients with LDL-cholesterol measured.
f Fasting.
REYATAZ/ritonavira,b
lopinavir/ritonavirb,c
Baseline
mg/dL
(n=111e)
Week 48
mg/dL
(n=75e)
Week 48
Changed
(n=74e)
Baseline
mg/dL
(n=108e)
Week 48
mg/dL
(n=76e)
Week 48
Changed
(n=73e)
LDL-Cholesterolf
108
98
−10%
104
103
+1%
HDL-Cholesterol
40
39
−7%
39
41
+2%
Total Cholesterol
188
170
−8%
181
187
+6%
Triglyceridesf
215
161
−4%
196
224
+30%
Adverse Reactions in Pediatric Patients: REYATAZ Capsules
The safety and tolerability of REYATAZ Capsules with and without ritonavir have been established in pediatric patients at least 6 years of age from the open-label, multicenter clinical trial PACTG 1020A.
The safety profile of REYATAZ in pediatric patients (6 to less than 18 years of age) taking the capsule formulation was generally similar to that observed in clinical studies of REYATAZ in adults. The most common Grade 2–4 adverse events (≥5%, regardless of causality) reported in pediatric patients were cough (21%), fever (18%), jaundice/scleral icterus (15%), rash (14%), vomiting (12%), diarrhea (9%), headache (8%), peripheral edema (7%), extremity pain (6%), nasal congestion (6%), oropharyngeal pain (6%), wheezing (6%), and rhinorrhea (6%). Asymptomatic second-degree atrioventricular block was reported in <2% of patients. The most common Grade 3–4 laboratory abnormalities occurring in pediatric patients taking the capsule formulation were elevation of total bilirubin (≥3.2 mg/dL, 58%), neutropenia (9%), and hypoglycemia (4%). All other Grade 3–4 laboratory abnormalities occurred with a frequency of less than 3%.
Adverse Reactions in Pediatric Patients: REYATAZ Oral Powder
The data described below reflect exposure to REYATAZ oral powder in 155 subjects weighing at least 5 kg to less than 35 kg, including 134 patients exposed for 48 weeks. These data are from two pooled open-label, multi-center clinical trials in treatment-naive and treatment-experienced pediatric patients (AI424-397 [PRINCE I] and AI424-451 [PRINCE II]). Age ranged from 3 months to 10 years of age. In these studies 51% were female and 49% were male. All patients received ritonavir and 2 nucleoside reverse transcriptase inhibitors (NRTIs).
The safety profile of REYATAZ in pediatric patients taking REYATAZ oral powder was generally similar to that observed in clinical studies of REYATAZ in pediatric patients taking REYATAZ capsules. The most common Grade 3–4 laboratory abnormalities occurring in pediatric patients weighing 5 kg to less than 35 kg taking REYATAZ oral powder were increased amylase (33%), neutropenia (9%), increased SGPT/ALT (9%), elevation of total bilirubin (≥2.6 times ULN, 16%), and increased lipase (8%). All other Grade 3–4 laboratory abnormalities occurred with a frequency of less than 3%.
Adverse Reactions in Patients Co-Infected with Hepatitis B and/or Hepatitis C Virus
In study AI424-138, 60 patients treated with REYATAZ/ritonavir 300 mg/100 mg once daily, and 51 patients treated with lopinavir/ritonavir 400 mg/100 mg twice daily, each with fixed dose tenofovir-emtricitabine, were seropositive for hepatitis B and/or C at study entry. ALT levels >5 times ULN developed in 10% (6/60) of the REYATAZ/ritonavir-treated patients and 8% (4/50) of the lopinavir/ritonavir-treated patients. AST levels >5 times ULN developed in 10% (6/60) of the REYATAZ/ritonavir-treated patients and none (0/50) of the lopinavir/ritonavir-treated patients.
In study AI424-045, 20 patients treated with REYATAZ/ritonavir 300 mg/100 mg once daily, and 18 patients treated with lopinavir/ritonavir 400 mg/100 mg twice daily, were seropositive for hepatitis B and/or C at study entry. ALT levels >5 times ULN developed in 25% (5/20) of the REYATAZ/ritonavir-treated patients and 6% (1/18) of the lopinavir/ritonavir-treated patients. AST levels >5 times ULN developed in 10% (2/20) of the REYATAZ/ritonavir-treated patients and 6% (1/18) of the lopinavir/ritonavir-treated patients.
In studies AI424-008 and AI424-034, 74 patients treated with 400 mg of REYATAZ once daily, 58 who received efavirenz, and 12 who received nelfinavir were seropositive for hepatitis B and/or C at study entry. ALT levels >5 times ULN developed in 15% of the REYATAZ-treated patients, 14% of the efavirenz-treated patients, and 17% of the nelfinavir-treated patients. AST levels >5 times ULN developed in 9% of the REYATAZ-treated patients, 5% of the efavirenz-treated patients, and 17% of the nelfinavir-treated patients. Within REYATAZ and control regimens, no difference in frequency of bilirubin elevations was noted between seropositive and seronegative patients. [See WARNINGS AND PRECAUTIONS (5.3).]
6.2 Postmarketing Experience
The following events have been identified during postmarketing use of REYATAZ. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Body as a Whole: edema
Cardiovascular System: second-degree AV block, third-degree AV block, left bundle branch block, QTc prolongation [see WARNINGS AND PRECAUTIONS (5.1)]
Gastrointestinal System: pancreatitis
Hepatic System: hepatic function abnormalities
Hepatobiliary Disorders: cholelithiasis [see WARNINGS AND PRECAUTIONS (5.5)], cholecystitis, cholestasis
Metabolic System and Nutrition Disorders: diabetes mellitus, hyperglycemia [see WARNINGS AND PRECAUTIONS (5.8)]
Musculoskeletal System: arthralgia
Renal System: nephrolithiasis [see WARNINGS AND PRECAUTIONS (5.6)], interstitial nephritis
Skin and Appendages: alopecia, maculopapular rash [see CONTRAINDICATIONS (4) and WARNINGS AND PRECAUTIONS (5.2)], pruritus, angioedema
7 DRUG INTERACTIONS
7.1 Potential for REYATAZ to Affect Other Drugs
Atazanavir is an inhibitor of CYP3A and UGT1A1. Coadministration of REYATAZ and drugs primarily metabolized by CYP3A or UGT1A1 may result in increased plasma concentrations of the other drug that could increase or prolong its therapeutic and adverse effects.
Atazanavir is a weak inhibitor of CYP2C8. Use of REYATAZ without ritonavir is not recommended when coadministered with drugs highly dependent on CYP2C8 with narrow therapeutic indices (eg, paclitaxel, repaglinide). When REYATAZ with ritonavir is coadministered with substrates of CYP2C8, clinically significant interactions are not expected [see CLINICAL PHARMACOLOGY, TABLE 22 (12.3)].
The magnitude of CYP3A-mediated drug interactions on coadministered drug may change when REYATAZ is coadministered with ritonavir. See the complete prescribing information for ritonavir for information on drug interactions with ritonavir.
7.2 Potential for Other Drugs to Affect REYATAZ
Atazanavir is a CYP3A4 substrate; therefore, drugs that induce CYP3A4 may decrease atazanavir plasma concentrations and reduce REYATAZ’s therapeutic effect.
Atazanavir solubility decreases as pH increases. Reduced plasma concentrations of atazanavir are expected if proton-pump inhibitors, antacids, buffered medications, or H2-receptor antagonists are administered with REYATAZ [see DOSAGE AND ADMINISTRATION (2.2, 2.3, 2.4, and 2.5)].
7.3 Established and Other Potentially Significant Drug Interactions
Table 16 provides dosing recommendations in adults as a result of drug interactions with REYATAZ. These recommendations are based on either drug interaction studies or predicted interactions due to the expected magnitude of interaction and potential for serious events or loss of efficacy.
Table 16: Established and Other Potentially Significant Drug Interactions: Alteration in Dose or Regimen May Be Recommended Based on Drug Interaction Studiesa or Predicted Interactions (Information in the table applies to REYATAZ with or without ritonavir, unless otherwise indicated)
Concomitant Drug Class:
Specific Drugs Effect on Concentration of Atazanavir or Concomitant Drug Clinical Comment
a For magnitude of interactions see CLINICAL PHARMACOLOGY, TABLES 21 AND 22 (12.3).
b See CONTRAINDICATIONS (4), TABLE 6 for orally administered midazolam.
c In combination with atazanavir 300 mg and ritonavir 100 mg once daily.
d In combination with atazanavir 400 mg once daily.
HIV Antiviral Agents
Nucleoside Reverse Transcriptase Inhibitors (NRTIs):
didanosine buffered formulations
enteric-coated (EC) capsules
↓ atazanavir
↓ didanosine
Coadministration of REYATAZ with didanosine buffered tablets resulted in a marked decrease in atazanavir exposure. It is recommended that REYATAZ be given (with food) 2 h before or 1 h after didanosine buffered formulations. Simultaneous administration of didanosine EC and REYATAZ with food results in a decrease in didanosine exposure. Thus, REYATAZ and didanosine EC should be administered at different times.
Nucleotide Reverse Transcriptase Inhibitors:
tenofovir disoproxil fumarate
↓ atazanavir
↑ tenofovir
Tenofovir may decrease the AUC and Cmin of atazanavir. When coadministered with tenofovir in adults, it is recommended that REYATAZ 300 mg be given with ritonavir 100 mg and tenofovir 300 mg (all as a single daily dose with food). REYATAZ increases tenofovir concentrations. The mechanism of this interaction is unknown. Higher tenofovir concentrations could potentiate tenofovir-associated adverse reactions, including renal disorders. Patients receiving REYATAZ and tenofovir should be monitored for tenofovir-associated adverse reactions. For pregnant women taking REYATAZ with ritonavir and tenofovir, see DOSAGE AND ADMINISTRATION (2.5).
Non-nucleoside Reverse Transcriptase Inhibitors (NNRTIs):
efavirenz
↓ atazanavir
Efavirenz decreases atazanavir exposure.
In treatment-naive adult patients:
If REYATAZ is combined with efavirenz, REYATAZ 400 mg (two 200-mg capsules) should be administered with ritonavir 100 mg simultaneously once daily with food, and efavirenz 600 mg should be administered once daily on an empty stomach, preferably at bedtime.
In treatment-experienced adult patients:
Coadministration of REYATAZ with efavirenz in treatment-experienced patients is not recommended due to decreased atazanavir exposure.
Protease Inhibitors:
saquinavir (soft gelatin capsules)
↑ saquinavir
Appropriate dosing recommendations for this combination, with or without ritonavir, with respect to efficacy and safety have not been established. In a clinical study, saquinavir 1200 mg coadministered with REYATAZ 400 mg and tenofovir 300 mg (all given once daily) plus nucleoside analogue reverse transcriptase inhibitors did not provide adequate efficacy [see CLINICAL STUDIES (14.2)].
ritonavir
↑ atazanavir
If REYATAZ is coadministered with ritonavir, it is recommended that REYATAZ 300 mg once daily be given with ritonavir 100 mg once daily with food in adults. See the complete prescribing information for ritonavir for information on drug interactions with ritonavir.
others
↑ other protease inhibitor
Although not studied, the coadministration of REYATAZ/ritonavir and an additional protease inhibitor would be expected to increase exposure to the other protease inhibitor. Such coadministration is not recommended.
HCV Antiviral Agents
Protease Inhibitors:
boceprevir
↓ atazanavir
↓ ritonavir
Concomitant administration of boceprevir and atazanavir/ritonavir resulted in reduced steady-state exposures to atazanavir and ritonavir. Coadministration of REYATAZ/ritonavir and boceprevir is not recommended.
Other Agents
Antacids and buffered medications
↓ atazanavir
Reduced plasma concentrations of atazanavir are expected if antacids, including buffered medications, are administered with REYATAZ. REYATAZ should be administered 2 hours before or 1 hour after these medications.
Antiarrhythmics:
amiodarone, bepridil, lidocaine (systemic), quinidine
↑ amiodarone, bepridil, lidocaine (systemic), quinidine
Coadministration with REYATAZ has the potential to produce serious and/or life-threatening adverse events and has not been studied. Caution is warranted and therapeutic concentration monitoring of these drugs is recommended if they are used concomitantly with REYATAZ.
Anticoagulants:
warfarin
↑ warfarin
Coadministration with REYATAZ has the potential to produce serious and/or life-threatening bleeding and has not been studied. It is recommended that International Normalized Ratio (INR) be monitored.
Antidepressants:
tricyclic antidepressants
↑ tricyclic antidepressants
Coadministration with REYATAZ has the potential to produce serious and/or life-threatening adverse events and has not been studied. Concentration monitoring of these drugs is recommended if they are used concomitantly with REYATAZ.
trazodone
↑ trazodone
Concomitant use of trazodone and REYATAZ with or without ritonavir may increase plasma concentrations of trazodone. Nausea, dizziness, hypotension, and syncope have been observed following coadministration of trazodone and ritonavir. If trazodone is used with a CYP3A4 inhibitor such as REYATAZ, the combination should be used with caution and a lower dose of trazodone should be considered.
Antiepileptics:
carbamazepine
↓ atazanavir
↑ carbamazepine
Plasma concentrations of atazanavir may be decreased when carbamazepine is administered with REYATAZ without ritonavir. Coadministration of carbamazepine and REYATAZ without ritonavir is not recommended. Ritonavir may increase plasma levels of carbamazepine. If patients beginning treatment with REYATAZ/ritonavir have been titrated to a stable dose of carbamazepine, a dose reduction for carbamazepine may be necessary.
phenytoin, phenobarbital
↓ atazanavir
↓ phenytoin
↓ phenobarbital
Plasma concentrations of atazanavir may be decreased when phenytoin or phenobarbital is administered with REYATAZ without ritonavir. Coadministration of phenytoin or phenobarbital and REYATAZ without ritonavir is not recommended. Ritonavir may decrease plasma levels of phenytoin and phenobarbital. When REYATAZ with ritonavir is coadministered with either phenytoin or phenobarbital, a dose adjustment of phenytoin or phenobarbital may be required.
lamotrigine
↓ lamotrigine
Coadministration of lamotrigine and REYATAZ with ritonavir may decrease lamotrigine plasma concentrations. Dose adjustment of lamotrigine may be required when coadministered with REYATAZ and ritonavir. Coadministration of lamotrigine and REYATAZ without ritonavir is not expected to decrease lamotrigine plasma concentrations. No dose adjustment of lamotrigine is required when coadministered with REYATAZ without ritonavir.
Antifungals:
ketoconazole, itraconazole
REYATAZ/ritonavir:
↑ ketoconazole
↑ itraconazole
Coadministration of ketoconazole has only been studied with REYATAZ without ritonavir (negligible increase in atazanavir AUC and Cmax). Due to the effect of ritonavir on ketoconazole, high doses of ketoconazole and itraconazole (>200 mg/day) should be used cautiously with REYATAZ/ritonavir.
voriconazole
REYATAZ/ritonavir in subjects with a functional CYP2C19 allele:
↓ voriconazole
↓ atazanavir
REYATAZ/ritonavir in subjects without a functional CYP2C19 allele:
↑ voriconazole
↓ atazanavir
The use of voriconazole in patients receiving REYATAZ/ritonavir is not recommended unless an assessment of the benefit/risk to the patient justifies the use of voriconazole. Patients should be carefully monitored for voriconazole-associated adverse reactions and loss of either voriconazole or atazanavir efficacy during the coadministration of voriconazole and REYATAZ/ritonavir. Coadministration of voriconazole with REYATAZ (without ritonavir) may affect atazanavir concentrations; however, no data are available.
Antigout:
colchicine
↑ colchicine
The coadministration of REYATAZ with colchicine in patients with renal or hepatic impairment is not recommended.
Recommended adult dosage of colchicine when administered with REYATAZ:
Treatment of gout flares:
0.6 mg (1 tablet) for 1 dose, followed by 0.3 mg (half tablet) 1 hour later. Not to be repeated before 3 days.
Prophylaxis of gout flares:
If the original regimen was 0.6 mg twice a day, the regimen should be adjusted to 0.3 mg once a day.
If the original regimen was 0.6 mg once a day, the regimen should be adjusted to 0.3 mg once every other day.
Treatment of familial Mediterranean fever (FMF):
Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day).
Antimycobacterials:
rifabutin
↑ rifabutin
A rifabutin dose reduction of up to 75% (eg, 150 mg every other day or 3 times per week) is recommended. Increased monitoring for rifabutin-associated adverse reactions including neutropenia is warranted.
Antipsychotics:
quetiapine and lurasidone
↑ quetiapine
Init.iation of REYATAZ with ritonavir in patients taking quetiapine:
Consider alternative antiretroviral therapy to avoid increases in quetiapine exposures. If coadministration is necessary, reduce the quetiapine dose to 1/6 of the current dose and monitor for quetiapine-associated adverse reactions. Refer to the quetiapine prescribing information for recommendations on adverse reaction monitoring.
Initiation of quetiapine in patients taking REYATAZ with ritonavir:
Refer to the quetiapine prescribing information for initial dosing and titration of quetiapine.
REYATAZ
↑ lurasidone
REYATAZ without ritonavir
If coadministration is necessary, reduce the lurasidone dose. Refer to the lurasidone prescribing information for concomitant use with moderate CYP3A4 inhibitors
REYATAZ/ritonavir
↑ lurasidone
REYATAZ/ritonavir
Use of lurasidone is contraindicated.
Benzodiazepines:
parenterally administered midazolamb
↑ midazolam
Concomitant use of parenteral midazolam with REYATAZ may increase plasma concentrations of midazolam. Coadministration should be done in a setting which ensures close clinical monitoring and appropriate medical management in case of respiratory depression and/or prolonged sedation. Dosage reduction for midazolam should be considered, especially if more than a single dose of midazolam is administered. Coadministration of oral midazolam with REYATAZ is CONTRAINDICATED.
Calcium channel blockers:
diltiazem
↑ diltiazem and desacetyl-diltiazem
Caution is warranted. A dose reduction of diltiazem by 50% should be considered. ECG monitoring is recommended. Coadministration of REYATAZ/ritonavir with diltiazem has not been studied.
felodipine, nifedipine, nicardipine, and verapamil
↑ calcium channel blocker
Caution is warranted. Dose titration of the calcium channel blocker should be considered. ECG monitoring is recommended.
Endothelin receptor antagonists:
bosentan
↓ atazanavir
↑ bosentan
Plasma concentrations of atazanavir may be decreased when bosentan is administered with REYATAZ without ritonavir. Coadministration of bosentan and REYATAZ without ritonavir is not recommended.
Coadministration of bosentan in adult patients on REYATAZ/ritonavir:
For patients who have been receiving REYATAZ/ritonavir for at least 10 days, start bosentan at 62.5 mg once daily or every other day based on individual tolerability.
Coadministration of REYATAZ/ritonavir in adult patients on bosentan:
Discontinue bosentan at least 36 hours before starting REYATAZ/ritonavir. At least 10 days after starting REYATAZ/ritonavir, resume bosentan at 62.5 mg once daily or every other day based on individual tolerability.
HMG-CoA reductase inhibitors:
atorvastatin, rosuvastatin
↑ atorvastatin
↑ rosuvastatin
Titrate atorvastatin dose carefully and use the lowest necessary dose. Rosuvastatin dose should not exceed 10 mg/day. The risk of myopathy, including rhabdomyolysis, may be increased when HIV protease inhibitors, including REYATAZ, are used in combination with these drugs.
H2‑Receptor antagonists
↓ atazanavir
Plasma concentrations of atazanavir were substantially decreased when REYATAZ 400 mg once daily was administered simultaneously with famotidine 40 mg twice daily in adults, which may result in loss of therapeutic effect and development of resistance.
In treatment-naive adult patients:
REYATAZ 300 mg with ritonavir 100 mg once daily with food should be administered simultaneously with, and/or at least 10 hours after, a dose of the H2-receptor antagonist (H2RA). An H2RA dose comparable to famotidine 20 mg once daily up to a dose comparable to famotidine 40 mg twice daily can be used with REYATAZ 300 mg with ritonavir 100 mg in treatment-naive patients.
OR
For patients unable to tolerate ritonavir, REYATAZ 400 mg once daily with food should be administered at least 2 hours before and at least 10 hours after a dose of the H2RA. No single dose of the H2RA should exceed a dose comparable to famotidine 20 mg, and the total daily dose should not exceed a dose comparable to famotidine 40 mg. The use of REYATAZ without ritonavir in pregnant women is not recommended.
In treatment-experienced adult patients:
Whenever an H2RA is given to a patient receiving REYATAZ with ritonavir, the H2RA dose should not exceed a dose comparable to famotidine 20 mg twice daily, and the REYATAZ and ritonavir doses should be administered simultaneously with, and/or at least 10 hours after, the dose of the H2RA.
•
REYATAZ 300 mg with ritonavir 100 mg once daily (all as a single dose with food) if taken with an H2RA.
•
REYATAZ 400 mg with ritonavir 100 mg once daily (all as a single dose with food) if taken with both tenofovir and an H2RA.
•
REYATAZ 400 mg with ritonavir 100 mg once daily (all as a single dose with food) if taken with either tenofovir or an H2RA for pregnant women during the second and third trimester. REYATAZ is not recommended for pregnant women during the second and third trimester taking REYATAZ with both tenofovir and an H2RA.
Hormonal contraceptives:
ethinyl estradiol and norgestimate or norethindrone
↓ ethinyl estradiol
↑ norgestimatec
↑ ethinyl estradiol
↑ norethindroned
Use with caution if coadministration of REYATAZ or REYATAZ/ritonavir with oral contraceptives is considered. If an oral contraceptive is administered with REYATAZ plus ritonavir, it is recommended that the oral contraceptive contain at least 35 mcg of ethinyl estradiol. If REYATAZ is administered without ritonavir, the oral contraceptive should contain no more than 30 mcg of ethinyl estradiol.
Potential safety risks include substantial increases in progesterone exposure. The long-term effects of increases in concentration of the progestational agent are unknown and could increase the risk of insulin resistance, dyslipidemia, and acne.
Coadministration of REYATAZ or REYATAZ/ritonavir with other hormonal contraceptives (eg, contraceptive patch, contraceptive vaginal ring, or injectable contraceptives) or oral contraceptives containing progestogens other than norethindrone or norgestimate, or less than 25 mcg of ethinyl estradiol, has not been studied; therefore, alternative methods of contraception are recommended.
Immunosuppressants:
cyclosporine, sirolimus, tacrolimus
↑ immunosuppressants
Therapeutic concentration monitoring is recommended for these immunosuppressants when coadministered with REYATAZ.
Inhaled beta agonist:
salmeterol
↑ salmeterol
Coadministration of salmeterol with REYATAZ is not recommended. Concomitant use of salmeterol and REYATAZ may result in increased risk of cardiovascular adverse reactions associated with salmeterol, including QT prolongation, palpitations, and sinus tachycardia.
Inhaled/nasal steroid:
fluticasone
REYATAZ
↑ fluticasone
Concomitant use of fluticasone propionate and REYATAZ (without ritonavir) may increase plasma concentrations of fluticasone propionate. Use with caution. Consider alternatives to fluticasone propionate, particularly for long-term use.
REYATAZ/ritonavir
↑ fluticasone
Concomitant use of fluticasone propionate and REYATAZ/ritonavir may increase plasma concentrations of fluticasone propionate, resulting in significantly reduced serum cortisol concentrations. Systemic corticosteroid effects, including Cushing’s syndrome and adrenal suppression, have been reported during postmarketing use in patients receiving ritonavir and inhaled or intranasally administered fluticasone propionate. Coadministration of fluticasone propionate and REYATAZ/ritonavir is not recommended unless the potential benefit to the patient outweighs the risk of systemic corticosteroid side effects [see WARNINGS AND PRECAUTIONS (5.1)].
Macrolide antibiotics:
clarithromycin
↑ clarithromycin
↓ 14-OH clarithromycin
↑ atazanavir
Increased concentrations of clarithromycin may cause QTc prolongations; therefore, a dose reduction of clarithromycin by 50% should be considered when it is coadministered with REYATAZ. In addition, concentrations of the active metabolite 14-OH clarithromycin are significantly reduced; consider alternative therapy for indications other than infections due to Mycobacterium avium complex. Coadministration of REYATAZ/ritonavir with clarithromycin has not been studied.
Opioids:
Buprenorphine
↑ buprenorphine
↑ norbuprenorphine
Coadministration of buprenorphine and REYATAZ with or without ritonavir increases the plasma concentration of buprenorphine and norbuprenorphine. Coadministration of REYATAZ plus ritonavir with buprenorphine warrants clinical monitoring for sedation and cognitive effects. A dose reduction of buprenorphine may be considered. Coadministration of buprenorphine and REYATAZ with ritonavir is not expected to decrease atazanavir plasma concentrations. Coadministration of buprenorphine and REYATAZ without ritonavir may decrease atazanavir plasma concentrations. The coadministration of REYATAZ and buprenorphine without ritonavir is not recommended.
PDE5 inhibitors:
sildenafil, tadalafil, vardenafil
↑ sildenafil
↑ tadalafil
↑ vardenafil
Coadministration with REYATAZ has not been studied but may result in an increase in PDE5 inhibitor-associated adverse reactions, including hypotension, syncope, visual disturbances, and priapism.
Use of PDE5 inhibitors for pulmonary arterial hypertension (PAH):
Use of REVATIO ® (sildenafil) for the treatment of pulmonary hypertension (PAH) is contraindicated with REYATAZ [see CONTRAINDICATIONS (4)].
The following dose adjustments are recommended for the use of ADCIRCA ® (tadalafil) with REYATAZ:
Coadministration of ADCIRCA ® in patients on REYATAZ (with or without ritonavir):
•
For patients receiving REYATAZ (with or without ritonavir) for at least one week, start ADCIRCA ® at 20 mg once daily. Increase to 40 mg once daily based on individual tolerability.
Coadministration of REYATAZ (with or without ritonavir) in patients on ADCIRCA ®:
•
Avoid the use of ADCIRCA ® when starting REYATAZ (with or without ritonavir). Stop ADCIRCA ® at least 24 hours before starting REYATAZ (with or without ritonavir). At least one week after starting REYATAZ (with or without ritonavir), resume ADCIRCA ® at 20 mg once daily. Increase to 40 mg once daily based on individual tolerability.
Use of PDE5 inhibitors for erectile dysfunction:
Use VIAGRA ® (sildenafil) with caution at reduced doses of 25 mg every 48 hours with increased monitoring for adverse events.
Use CIALIS ® (tadalafil) with caution at reduced doses of 10 mg every 72 hours with increased monitoring for adverse events.
REYATAZ/ritonavir: Use vardenafil with caution at reduced doses of no more than 2.5 mg every 72 hours with increased monitoring for adverse reactions.
REYATAZ: Use vardenafil with caution at reduced doses of no more than 2.5 mg every 24 hours with increased monitoring for adverse reactions.
Proton-pump inhibitors:
omeprazole
↓ atazanavir
Plasma concentrations of atazanavir were substantially decreased when REYATAZ 400 mg or REYATAZ 300 mg/ritonavir 100 mg once daily was administered with omeprazole 40 mg once daily in adults, which may result in loss of therapeutic effect and development of resistance.
In treatment-naive adult patients:
The proton-pump inhibitor (PPI) dose should not exceed a dose comparable to omeprazole 20 mg and must be taken approximately 12 hours prior to the REYATAZ 300 mg with ritonavir 100 mg dose.
In treatment-experienced adult patients:
The use of PPIs in treatment-experienced patients receiving REYATAZ is not recommended.
7.4 Drugs with No Observed Interactions with REYATAZ
No clinically significant drug interactions were observed when REYATAZ was coadministered with methadone, fluconazole, acetaminophen, atenolol, or the nucleoside reverse transcriptase inhibitors lamivudine or zidovudine [see CLINICAL PHARMACOLOGY, TABLES 21 AND 22 (12.3)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to REYATAZ during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
Atazanavir has been evaluated in a limited number of women during pregnancy. Available human and animal data suggest that atazanavir does not increase the risk of major birth defects overall compared to the background rate [see DATA]. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. No treatment-related malformations were observed in rats and rabbits, for which the atazanavir exposures were 0.7-1.2 times of those at the human clinical dose (300 mg/day atazanavir boosted with 100 mg/day ritonavir). When atazanavir was administered to rats during pregnancy and throughout lactation, reversible neonatal growth retardation was observed [see DATA].
Clinical Considerations
Dose Adjustments during Pregnancy and the Postpartum Period
•
REYATAZ must be administered with ritonavir in pregnant women.
•
For pregnant patients, no dosage adjustment is required for REYATAZ with the following exceptions:
•
For treatment-experienced pregnant women during the second or third trimester, when REYATAZ is coadministered with either an H 2-receptor antagonist or tenofovir, REYATAZ 400 mg with ritonavir 100 mg once daily is recommended. There are insufficient data to recommend a REYATAZ dose for use with both an H 2-receptor antagonist and tenofovir in treatment-experienced pregnant women.
•
No dosage adjustment is required for postpartum patients. However, patients should be closely monitored for adverse events because atazanavir exposures could be higher during the first 2 months after delivery [see DOSAGE AND ADMINISTRATION (2.5) and CLINICAL PHARMACOLOGY (12.3)].
Maternal Adverse Reactions
Cases of lactic acidosis syndrome, sometimes fatal, and symptomatic hyperlactatemia have occurred in pregnant women using REYATAZ in combination with nucleoside analogues, which are associated with an increased risk of lactic acidosis syndrome.
Hyperbilirubinemia occurs frequently in patients who take REYATAZ [see WARNINGS AND PRECAUTIONS (5.3)], including pregnant women [see DATA].
Advise pregnant women of the potential risks of lactic acidosis syndrome and hyperbilirubinemia.
Fetal/Neonatal Adverse Reactions
All infants, including neonates exposed to REYATAZ in utero, should be monitored for the development of severe hyperbilirubinemia during the first few days of life [see DATA].
Data
Human Data
In clinical trial AI424-182, REYATAZ/ritonavir (300/100 mg or 400/100 mg) in combination with zidovudine/lamivudine was administered to 41 HIV-infected pregnant women during the second or third trimester. Among the 39 women who completed the study, 38 women achieved an HIV RNA less than 50 copies/mL at time of delivery. Six of 20 (30%) women on REYATAZ/ritonavir 300/100 mg and 13 of 21 (62%) women on REYATAZ/ritonavir 400/100 mg experienced hyperbilirubinemia (total bilirubin greater than or equal to 2.6 times ULN). There were no cases of lactic acidosis observed in clinical trial AI424-182.
Atazanavir drug concentrations in fetal umbilical cord blood were approximately 12% to 19% of maternal concentrations. Among the 40 infants born to 40 HIV-infected pregnant women, all had test results that were negative for HIV-1 DNA at the time of delivery and/or during the first 6 months postpartum. All 40 infants received antiretroviral prophylactic treatment containing zidovudine. No evidence of severe hyperbilirubinemia (total bilirubin levels greater than 20 mg/dL) or acute or chronic bilirubin encephalopathy was observed among neonates in this study. However, 10/36 (28%) infants (6 greater than or equal to 38 weeks gestation and 4 less than 38 weeks gestation) had bilirubin levels of 4 mg/dL or greater within the first day of life.
Lack of ethnic diversity was a study limitation. In the study population, 33/40 (83%) infants were Black/African American, who have a lower incidence of neonatal hyperbilirubinemia than Caucasians and Asians. In addition, women with Rh incompatibility were excluded, as well as women who had a previous infant who developed hemolytic disease and/or had neonatal pathologic jaundice (requiring phototherapy).
Additionally, of the 38 infants who had glucose samples collected in the first day of life, 3 had adequately collected serum glucose samples with values of less than 40 mg/dL that could not be attributed to maternal glucose intolerance, difficult delivery, or sepsis.
Based on prospective reports from the APR of approximately 1600 live births following exposure to atazanavir-containing regimens (including 1037 live births in infants exposed in the first trimester and 569 exposed in second/third trimesters), there was no difference between atazanavir and overall birth defects compared with the background birth defect rate. In the U.S. general population, the estimated background risk of major birth defects in clinically recognized pregnancies is 2-4%.
Animal Data
In animal reproduction studies, there was no evidence of mortality or teratogenicity in offspring born to animals at systemic drug exposure levels (AUC) 0.7 (in rabbits) to 1.2 (in rats) times those observed at the human clinical dose (300 mg/day atazanavir boosted with 100 mg/day ritonavir). In pre- and postnatal development studies in the rat, atazanavir caused neonatal growth retardation during lactation that reversed after weaning. Maternal drug exposure at this dose was 1.3 times the human exposure at the recommended clinical exposure. Minimal maternal toxicity occurred at this exposure level.
8.2 Lactation
Risk Summary
The Centers for Disease Control and Prevention recommend that HIV-1 infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV-1. Atazanavir has been detected in human milk. No data are available regarding atazanavir effects on milk production. Atazanavir was present in the milk of lactating rats and was associated with neonatal growth retardation that reversed after weaning.
Because of both the potential for HIV-1 transmission and the potential for serious adverse reactions in breastfed infants, advise women not to breastfeed.
8.4 Pediatric Use
REYATAZ is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection in pediatric patients 3 months of age and older weighing at least 5 kg. REYATAZ is not recommended for use in pediatric patients below the age of 3 months due to the risk of kernicterus [see INDICATIONS AND USAGE (1)]. All REYATAZ contraindications, warnings, and precautions apply to pediatric patients [see CONTRAINDICATIONS (4) and WARNINGS AND PRECAUTIONS (5)].
The safety, pharmacokinetic profile, and virologic response of REYATAZ in pediatric patients at least 3 months of age and older weighing at least 5 kg were established in three open-label, multicenter clinical trials: PACTG 1020A, AI424-451, and AI424-397 [see CLINICAL PHARMACOLOGY (12.3) and CLINICAL STUDIES (14.3)]. The safety profile in pediatric patients was generally similar to that observed in adults [see ADVERSE REACTIONS (6.1)]. See DOSAGE AND ADMINISTRATION (2.3, 2.4) for dosing recommendations for the use of REYATAZ capsules and REYATAZ oral powder in pediatric patients.
8.5 Geriatric Use
Clinical studies of REYATAZ did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. Based on a comparison of mean single-dose pharmacokinetic values for Cmax and AUC, a dose adjustment based upon age is not recommended. In general, appropriate caution should be exercised in the administration and monitoring of REYATAZ in elderly patients reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Age/Gender
A study of the pharmacokinetics of atazanavir was performed in young (n=29; 18-40 years) and elderly (n=30; ≥65 years) healthy subjects. There were no clinically significant pharmacokinetic differences observed due to age or gender.
8.7 Impaired Renal Function
REYATAZ is not recommended for use in HIV-treatment-experienced patients with end stage renal disease managed with hemodialysis [see DOSAGE AND ADMINISTRATION (2.6) and CLINICAL PHARMACOLOGY (12.3)].
8.8 Impaired Hepatic Function
REYATAZ is not recommended for use in patients with severe hepatic impairment. REYATAZ/ritonavir is not recommended in patients with any degree of hepatic impairment [see DOSAGE AND ADMINISTRATION (2.7) and CLINICAL PHARMACOLOGY (12.3)].
10 OVERDOSAGE
Human experience of acute overdose with REYATAZ is limited. Single doses up to 1200 mg (three times the 400 mg maximum recommended dose) have been taken by healthy volunteers without symptomatic untoward effects. A single self-administered overdose of 29.2 g of REYATAZ in an HIV-infected patient (73 times the 400-mg recommended dose) was associated with asymptomatic bifascicular block and PR interval prolongation. These events resolved spontaneously. At REYATAZ doses resulting in high atazanavir exposures, jaundice due to indirect (unconjugated) hyperbilirubinemia (without associated liver function test changes) or PR interval prolongation may be observed [see WARNINGS AND PRECAUTIONS (5.1, 5.3) and CLINICAL PHARMACOLOGY (12.2)].
Treatment of overdosage with REYATAZ should consist of general supportive measures, including monitoring of vital signs and ECG, and observations of the patient’s clinical status. If indicated, elimination of unabsorbed atazanavir should be achieved by emesis or gastric lavage. Administration of activated charcoal may also be used to aid removal of unabsorbed drug. There is no specific antidote for overdose with REYATAZ. Since atazanavir is extensively metabolized by the liver and is highly protein bound, dialysis is unlikely to be beneficial in significant removal of this medicine.
11 DESCRIPTION
The active ingredient in REYATAZ capsules and oral powder is atazanavir sulfate, which is an HIV-1 protease inhibitor.
The chemical name for atazanavir sulfate is (3S,8S,9S,12S)-3,12-Bis(1,1-dimethylethyl)-8-hydroxy-4,11-dioxo-9-(phenylmethyl)-6-[[4-(2-pyridinyl)phenyl]methyl]-2,5,6,10,13-pentaazatetradecanedioic acid dimethyl ester, sulfate (1:1). Its molecular formula is C38H52N6O7•H2SO4, which corresponds to a molecular weight of 802.9 (sulfuric acid salt). The free base molecular weight is 704.9. Atazanavir sulfate has the following structural formula:
[Reyataz Chemical Structure]
Atazanavir sulfate is a white to pale-yellow crystalline powder. It is slightly soluble in water
(4-5 mg/mL, free base equivalent) with the pH of a saturated solution in water being about 1.9 at 24 ± 3°C.
REYATAZ Capsules are available for oral administration in strengths of 150 mg, 200 mg, or 300 mg of atazanavir, which are equivalent to 170.8 mg, 227.8 mg, or 341.69 mg of atazanavir sulfate, respectively. The capsules also contain the following inactive ingredients: crospovidone, lactose monohydrate, and magnesium stearate. The capsule shells contain the following inactive ingredients: gelatin, FD&C Blue No. 2, titanium dioxide, black iron oxide, red iron oxide, and yellow iron oxide. The capsules are printed with ink containing shellac, titanium dioxide, FD&C Blue No. 2, isopropyl alcohol, ammonium hydroxide, propylene glycol, n-butyl alcohol, simethicone, and dehydrated alcohol.
REYATAZ oral powder comes in a packet containing 50 mg of atazanavir equivalent to 56.9 mg of atazanavir sulfate in 1.5 g of powder. The powder is off-white to pale yellow and contains the following inactive ingredients: aspartame, sucrose, and orange-vanilla flavor.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Atazanavir is an HIV-1 antiretroviral drug [see MICROBIOLOGY (12.4)].
12.2 Pharmacodynamics
Cardiac Electrophysiology
Concentration- and dose-dependent prolongation of the PR interval in the electrocardiogram has been observed in healthy volunteers receiving atazanavir. In a placebo-controlled study (AI424-076), the mean (±SD) maximum change in PR interval from the predose value was 24 (±15) msec following oral dosing with 400 mg of atazanavir (n=65) compared to 13 (±11) msec following dosing with placebo (n=67). The PR interval prolongations in this study were asymptomatic. There is limited information on the potential for a pharmacodynamic interaction in humans between atazanavir and other drugs that prolong the PR interval of the electrocardiogram [see WARNINGS AND PRECAUTIONS (5.1)].
Electrocardiographic effects of atazanavir were determined in a clinical pharmacology study of 72 healthy subjects. Oral doses of 400 mg (maximum recommended dosage) and 800 mg (twice the maximum recommended dosage) were compared with placebo; there was no concentration-dependent effect of atazanavir on the QTc interval (using Fridericia’s correction). In 1793 HIV-infected patients receiving antiretroviral regimens, QTc prolongation was comparable in the atazanavir and comparator regimens. No atazanavir-treated healthy subject or HIV-infected patient in clinical trials had a QTc interval >500 msec [see WARNINGS AND PRECAUTIONS (5.1)].
12.3 Pharmacokinetics
The pharmacokinetics of atazanavir were evaluated in healthy adult volunteers and in HIV-infected patients after administration of REYATAZ 400 mg once daily and after administration of REYATAZ 300 mg with ritonavir 100 mg once daily (see Table 17).
Table 17: Steady-State Pharmacokinetics of Atazanavir in Healthy Subjects or HIV-Infected Patients in the Fed State
a n=26.
b n=12.
400 mg once daily
300 mg with ritonavir
100 mg once daily
Parameter
Healthy
Subjects
(n=14)
HIV-Infected
Patients
(n=13)
Healthy
Subjects
(n=28)
HIV-Infected
Patients
(n=10)
Cmax (ng/mL)
Geometric mean (CV%)
5199 (26)
2298 (71)
6129 (31)
4422 (58)
Mean (SD)
5358 (1371)
3152 (2231)
6450 (2031)
5233 (3033)
Tmax (h)
Median
2.5
2.0
2.7
3.0
AUC (ng•h/mL)
Geometric mean (CV%)
28132 (28)
14874 (91)
57039 (37)
46073 (66)
Mean (SD)
29303 (8263)
22262 (20159)
61435 (22911)
53761 (35294)
T-half (h)
Mean (SD)
7.9 (2.9)
6.5 (2.6)
18.1 (6.2)a
8.6 (2.3)
Cmin (ng/mL)
Geometric mean (CV%)
159 (88)
120 (109)
1227 (53)
636 (97)
Mean (SD)
218 (191)
273 (298)b
1441 (757)
862 (838)
Figure 1 displays the mean plasma concentrations of atazanavir at steady state after REYATAZ 400 mg once daily (as two 200-mg capsules) with a light meal and after REYATAZ 300 mg (as two 150-mg capsules) with ritonavir 100 mg once daily with a light meal in HIV-infected adult patients.
Figure 1: Mean (SD) Steady-State Plasma Concentrations of Atazanavir 400 mg (n=13) and 300 mg with Ritonavir (n=10) for HIV-Infected Adult Patients
[Reyataz Fig 1]
Absorption
Atazanavir is rapidly absorbed with a Tmax of approximately 2.5 hours. Atazanavir demonstrates nonlinear pharmacokinetics with greater than dose-proportional increases in AUC and Cmax values over the dose range of 200 to 800 mg once daily. Steady state is achieved between Days 4 and 8, with an accumulation of approximately 2.3 fold.
Food Effect
Administration of REYATAZ with food enhances bioavailability and reduces pharmacokinetic variability. Administration of a single 400-mg dose of REYATAZ with a light meal (357 kcal, 8.2 g fat, 10.6 g protein) resulted in a 70% increase in AUC and 57% increase in Cmax relative to the fasting state. Administration of a single 400-mg dose of REYATAZ with a high-fat meal (721 kcal, 37.3 g fat, 29.4 g protein) resulted in a mean increase in AUC of 35% with no change in Cmax relative to the fasting state. Administration of REYATAZ with either a light meal or high-fat meal decreased the coefficient of variation of AUC and Cmax by approximately one-half compared to the fasting state.
Coadministration of a single 300-mg dose of REYATAZ and a 100-mg dose of ritonavir with a light meal (336 kcal, 5.1 g fat, 9.3 g protein) resulted in a 33% increase in the AUC and a 40% increase in both the Cmax and the 24-hour concentration of atazanavir relative to the fasting state. Coadministration with a high-fat meal (951 kcal, 54.7 g fat, 35.9 g protein) did not affect the AUC of atazanavir relative to fasting conditions and the Cmax was within 11% of fasting values. The 24-hour concentration following a high-fat meal was increased by approximately 33% due to delayed absorption; the median Tmaxincreased from 2.0 to 5.0 hours. Coadministration of REYATAZ with ritonavir with either a light or a high-fat meal decreased the coefficient of variation of AUC and Cmax by approximately 25% compared to the fasting state.
Distribution
Atazanavir is 86% bound to human serum proteins and protein binding is independent of concentration. Atazanavir binds to both alpha-1-acid glycoprotein (AAG) and albumin to a similar extent (89% and 86%, respectively). In a multiple-dose study in HIV-infected patients dosed with REYATAZ 400 mg once daily with a light meal for 12 weeks, atazanavir was detected in the cerebrospinal fluid and semen. The cerebrospinal fluid/plasma ratio for atazanavir (n=4) ranged between 0.0021 and 0.0226 and seminal fluid/plasma ratio (n=5) ranged between 0.11 and 4.42.
Metabolism
Atazanavir is extensively metabolized in humans. The major biotransformation pathways of atazanavir in humans consisted of monooxygenation and dioxygenation. Other minor biotransformation pathways for atazanavir or its metabolites consisted of glucuronidation, N-dealkylation, hydrolysis, and oxygenation with dehydrogenation. Two minor metabolites of atazanavir in plasma have been characterized. Neither metabolite demonstrated in vitro antiviral activity. In vitro studies using human liver microsomes suggested that atazanavir is metabolized by CYP3A.
Elimination
Following a single 400-mg dose of 14C-atazanavir, 79% and 13% of the total radioactivity was recovered in the feces and urine, respectively. Unchanged drug accounted for approximately 20% and 7% of the administered dose in the feces and urine, respectively. The mean elimination half-life of atazanavir in healthy volunteers (n=214) and HIV-infected adult patients (n=13) was approximately 7 hours at steady state following a dose of 400 mg daily with a light meal.
Specific Populations
Renal Impairment
In healthy subjects, the renal elimination of unchanged atazanavir was approximately 7% of the administered dose. REYATAZ has been studied in adult subjects with severe renal impairment (n=20), including those on hemodialysis, at multiple doses of 400 mg once daily. The mean atazanavir Cmaxwas 9% lower, AUC was 19% higher, and Cmin was 96% higher in subjects with severe renal impairment not undergoing hemodialysis (n=10), than in age-, weight-, and gender-matched subjects with normal renal function. In a 4-hour dialysis session, 2.1% of the administered dose was removed. When atazanavir was administered either prior to, or following hemodialysis (n=10), the geometric means for Cmax, AUC, and Cmin were approximately 25% to 43% lower compared to subjects with normal renal function. The mechanism of this decrease is unknown. REYATAZ is not recommended for use in HIV-treatment-experienced patients with end stage renal disease managed with hemodialysis [see DOSAGE AND ADMINISTRATION (2.6)].
Hepatic Impairment
REYATAZ has been studied in adult subjects with moderate-to-severe hepatic impairment (14 Child-Pugh B and 2 Child-Pugh C subjects) after a single 400-mg dose. The mean AUC(0-∞) was 42% greater in subjects with impaired hepatic function than in healthy volunteers. The mean half-life of atazanavir in hepatically impaired subjects was 12.1 hours compared to 6.4 hours in healthy volunteers. A dose reduction to 300 mg is recommended for patients with moderate hepatic impairment (Child-Pugh Class B) who have not experienced prior virologic failure as increased concentrations of atazanavir are expected. REYATAZ is not recommended for use in patients with severe hepatic impairment. The pharmacokinetics of REYATAZ in combination with ritonavir has not been studied in subjects with hepatic impairment; thus, coadministration of REYATAZ with ritonavir is not recommended for use in patients with any degree of hepatic impairment [see DOSAGE AND ADMINISTRATION (2.7)].
Pediatrics
The pharmacokinetic parameters for atazanavir at steady state in pediatric patients taking the powder formulation are summarized in Table 18 by weight ranges [see DOSAGE AND ADMINISTRATION (2.4)].
Table 18: Steady-State Pharmacokinetics of Atazanavir (powder formulation) with Ritonavir in HIV-Infected Pediatric Patients
Body Weight
(range in kg) [n]
atazanavir/ritonavir
Dose (mg)
Cmax ng/mL
Geometric Mean
(CV%)
AUC ng•h/mL
Geometric Mean
(CV%)
Cmin ng/mL
Geometric Mean
(CV%)
5 to <10 [20]
150/80
4131 (55%)
32503 (61%)
336 (76%)
5 to <10 [10]
200/80
4466 (59%)
39519 (54%)
550 (60%)
10 to <15 [18]
200/80
5197 (53%)
50305 (67%)
572 (111%)
15 to <25 [32]
250/80
5394 (46%)
55687 (45%)
686 (68%)
25 to <35 [8]
300/100
4209 (52%)
44329 (63%)
468 (104%)
The pharmacokinetic parameters for atazanavir at steady state in pediatric patients taking the capsule formulation were predicted by a population pharmacokinetic model and are summarized in Table 19 by weight ranges that correspond to the recommended doses [see DOSAGE AND ADMINISTRATION (2.3)].
Table 19: Predicted Steady-State Pharmacokinetics of Atazanavir (capsule formulation) with Ritonavir in HIV-Infected Pediatric Patients
Body Weight
(range in kg)
atazanavir/ritonavir
Dose (mg)
Cmax ng/mL
Geometric Mean
(CV%)
AUC ng•h/mL
Geometric Mean
(CV%)
Cmin ng/mL
Geometric Mean
(CV%)
15 to <20
150/100
5213 (78.7%)
42902 (77.0%)
504 (99.5%)
20 to <40
200/100
4954 (81.7%)
42999 (78.5%)
562 (98.9%)
≥40
300/100
5040 (84.6%)
46777 (80.6%)
691 (98.5%)
Pregnancy
The pharmacokinetic data from HIV-infected pregnant women receiving REYATAZ Capsules with ritonavir are presented in Table 20.
Table 20: Steady-State Pharmacokinetics of Atazanavir with Ritonavir in HIV-Infected Pregnant Women in the Fed State
a Available data during the 2nd trimester are limited.
b Atazanavir peak concentrations and AUCs were found to be approximately 28% to 43% higher during the postpartum period (4-12 weeks) than those observed historically in HIV-infected, non-pregnant patients. Atazanavir plasma trough concentrations were approximately 2.2-fold higher during the postpartum period when compared to those observed historically in HIV-infected, non-pregnant patients.
c Cmin is concentration 24 hours post-dose.
Atazanavir 300 mg with ritonavir 100 mg
Pharmacokinetic Parameter
2nd Trimester
(n=5a)
3rd Trimester
(n=20)
Postpartumb
(n=34)
Cmax ng/mL
Geometric mean (CV%)
3078.85
(50)
3291.46
(48)
5721.21
(31)
AUC ng•h/mL
Geometric mean (CV%)
27657.1
(43)
34251.5
(43)
61990.4
(32)
Cmin ng/mLc
Geometric mean (CV%)
538.70
(46)
668.48
(50)
1462.59
(45)
Drug Interaction Data
Atazanavir is a metabolism-dependent CYP3A inhibitor, with a Kinact value of 0.05 to 0.06 min−1 and Kivalue of 0.84 to 1.0 µM. Atazanavir is also a direct inhibitor for UGT1A1 (Ki=1.9 µM) and CYP2C8 (Ki=2.1 µM).
Atazanavir has been shown in vivo not to induce its own metabolism nor to increase the biotransformation of some drugs metabolized by CYP3A. In a multiple-dose study, REYATAZ decreased the urinary ratio of endogenous 6β-OH cortisol to cortisol versus baseline, indicating that CYP3A production was not induced.
Clinically significant interactions are not expected between atazanavir and substrates of CYP2C19, CYP2C9, CYP2D6, CYP2B6, CYP2A6, CYP1A2, or CYP2E1. Clinically significant interactions are not expected between atazanavir when administered with ritonavir and substrates of CYP2C8. See the complete prescribing information for ritonavir for information on other potential drug interactions with ritonavir.
Based on known metabolic profiles, clinically significant drug interactions are not expected between REYATAZ and dapsone, trimethoprim/sulfamethoxazole, azithromycin, or erythromycin. REYATAZ does not interact with substrates of CYP2D6 (eg, nortriptyline, desipramine, metoprolol).
Drug interaction studies were performed with REYATAZ and other drugs likely to be coadministered and some drugs commonly used as probes for pharmacokinetic interactions. The effects of coadministration of REYATAZ on the AUC, Cmax, and Cmin are summarized in Tables 21 and 22. Neither didanosine EC nor diltiazem had a significant effect on atazanavir exposures (see Table 22 for effect of atazanavir on didanosine EC or diltiazem exposures). REYATAZ did not have a significant effect on the exposures of didanosine (when administered as the buffered tablet), stavudine, or fluconazole. For information regarding clinical recommendations, see DRUG INTERACTIONS (7).
Table 21: Drug Interactions: Pharmacokinetic Parameters for Atazanavir in the Presence of Coadministered Drugsa
Coadministered
Drug Coadministered Drug
Dose/Schedule REYATAZ
Dose/Schedule Ratio (90% Confidence Interval) of Atazanavir
Pharmacokinetic Parameters with/without
Coadministered Drug;
No Effect = 1.00
Cmax AUC Cmin
a Data provided are under fed conditions unless otherwise noted.
b All drugs were given under fasted conditions.
c REYATAZ 300 mg plus ritonavir 100 mg once daily coadministered with famotidine 40 mg twice daily resulted in atazanavir geometric mean Cmax that was similar and AUC and Cmin values that were 1.79- and 4.46-fold higher relative to REYATAZ 400 mg once daily alone.
d Similar results were noted when famotidine 20 mg BID was administered 2 hours after and 10 hours before atazanavir 300 mg and ritonavir 100 mg plus tenofovir 300 mg.
e Atazanavir/ritonavir/tenofovir was administered after a light meal.
f Study was conducted in HIV-infected individuals.
g Compared with atazanavir 400 mg historical data without nevirapine (n=13), the ratio of geometric means (90% confidence intervals) for Cmax, AUC, and Cmin were 1.42 (0.98, 2.05), 1.64 (1.11, 2.42), and 1.25 (0.66, 2.36), respectively, for atazanavir/ritonavir 300/100 mg; and 2.02 (1.42, 2.87), 2.28 (1.54, 3.38), and 1.80 (0.94, 3.45), respectively, for atazanavir/ritonavir 400/100 mg.
h Parallel group design; n=23 for atazanavir/ritonavir plus nevirapine, n=22 for atazanavir 300 mg/ritonavir 100 mg without nevirapine. Subjects were treated with nevirapine prior to study entry.
i Omeprazole 40 mg was administered on an empty stomach 2 hours before REYATAZ.
j Omeprazole 20 mg was administered 30 minutes prior to a light meal in the morning and REYATAZ 300 mg plus ritonavir 100 mg in the evening after a light meal, separated by 12 hours from omeprazole.
k REYATAZ 300 mg plus ritonavir 100 mg once daily separated by 12 hours from omeprazole 20 mg daily resulted in increases in atazanavir geometric mean AUC (10%) and Cmin (2.4-fold), with a decrease in Cmax (29%) relative to REYATAZ 400 mg once daily in the absence of omeprazole (study days 1–6).
l Omeprazole 20 mg was given 30 minutes prior to a light meal in the morning and REYATAZ 400 mg plus ritonavir 100 mg once daily after a light meal, 1 hour after omeprazole. Effects on atazanavir concentrations were similar when REYATAZ 400 mg plus ritonavir 100 mg was separated from omeprazole 20 mg by 12 hours.
m REYATAZ 400 mg plus ritonavir 100 mg once daily administered with omeprazole 20 mg once daily resulted in increases in atazanavir geometric mean AUC (32%) and Cmin (3.3-fold), with a decrease in Cmax (26%) relative to REYATAZ 400 mg once daily in the absence of omeprazole (study days 1–6).
n Compared with atazanavir 400 mg QD historical data, administration of atazanavir/ritonavir 300/100 mg QD increased the atazanavir geometric mean values of Cmax, AUC, and Cmin by 18%, 103%, and 671%, respectively.
o Note that similar results were observed in studies where administration of tenofovir and REYATAZ was separated by 12 hours.
p Ratio of atazanavir plus ritonavir plus tenofovir to atazanavir plus ritonavir. Atazanavir 300 mg plus ritonavir 100 mg results in higher atazanavir exposure than atazanavir 400 mg (see footnote o). The geometric mean values of atazanavir pharmacokinetic parameters when coadministered with ritonavir and tenofovir were: Cmax = 3190 ng/mL, AUC = 34459 ng•h/mL, and Cmin = 491 ng/mL. Study was conducted in HIV-infected individuals.
NA = not available.
atenolol
50 mg QD, d 7–11 (n=19)
and d 19–23
400 mg QD, d 1–11
(n=19)
1.00
(0.89, 1.12)
0.93
(0.85, 1.01)
0.74
(0.65, 0.86)
boceprevir
800 mg TID, d 1–6, 25–31
300 mg QD/ritonavir 100 mg QD,
d 10–31
atazanavir: 0.75
(0.64-0.88)
ritonavir: 0.73
(0.64-0.83)
atazanavir: 0.65
(0.55-0.78)
ritonavir: 0.64
(0.58-0.72)
atazanavir: 0.51
(0.44-0.61)
ritonavir: 0.55
(0.45-0.67)
clarithromycin
500 mg BID, d 7–10 (n=29)
and d 18–21
400 mg QD, d 1–10
(n=29)
1.06
(0.93, 1.20)
1.28
(1.16, 1.43)
1.91
(1.66, 2.21)
didanosine (ddI) (buffered tablets) plus stavudine (d4T)b
ddI: 200 mg × 1 dose,
d4T: 40 mg × 1 dose (n=31)
400 mg × 1 dose simultaneously with ddI and d4T
(n=31)
0.11
(0.06, 0.18)
0.13
(0.08, 0.21)
0.16
(0.10, 0.27)
ddI: 200 mg × 1 dose,
d4T: 40 mg × 1 dose (n=32)
400 mg × 1 dose 1 h after ddI + d4T
(n=32)
1.12
(0.67, 1.18)
1.03
(0.64, 1.67)
1.03
(0.61, 1.73)
efavirenz
600 mg QD, d 7–20
(n=27)
400 mg QD, d 1–20
(n=27)
0.41
(0.33, 0.51)
0.26
(0.22, 0.32)
0.07
(0.05, 0.10)
600 mg QD, d 7–20
(n=13)
400 mg QD, d 1–6 (n=23)
then 300 mg/ritonavir 100 mg QD,
2 h before efavirenz, d 7–20
(n=13)
1.14
(0.83, 1.58)
1.39
(1.02, 1.88)
1.48
(1.24, 1.76)
600 mg QD, d 11–24 (pm)
(n=14)
300 mg QD/ritonavir 100 mg QD,
d 1–10 (pm) (n=22),
then 400 mg QD/ritonavir 100 mg QD, d 11–24 (pm), (simultaneously with efavirenz)
(n=14)
1.17
(1.08, 1.27)
1.00
(0.91, 1.10)
0.58
(0.49, 0.69)
famotidine
40 mg BID, d 7–12
(n=15)
400 mg QD, d 1–6 (n=45), d 7–12 (simultaneous administration)
(n=15)
0.53
(0.34, 0.82)
0.59
(0.40, 0.87)
0.58
(0.37, 0.89)
40 mg BID, d 7–12
(n=14)
400 mg QD (pm), d 1–6 (n=14),
d 7–12 (10 h after, 2 h before famotidine)
(n=14)
1.08
(0.82, 1.41)
0.95
(0.74, 1.21)
0.79
(0.60, 1.04)
40 mg BID, d 11–20
(n=14)c
300 mg QD/ritonavir 100 mg QD,
d 1–10 (n=46),
d 11–20d(simultaneous administration)
(n=14)
0.86
(0.79, 0.94)
0.82
(0.75, 0.89)
0.72
(0.64, 0.81)
20 mg BID, d 11–17
(n=18)
300 mg QD/ritonavir 100 mg QD/tenofovir 300 mg QD,
d 1–10 (am) (n=39),
d 11–17 (am) (simultaneous administration with am famotidine) (n=18)d,e
0.91
(0.84, 0.99)
0.90
(0.82, 0.98)
0.81
(0.69, 0.94)
40 mg QD (pm), d 18–24
(n=20)
300 mg QD/ritonavir 100 mg QD/tenofovir 300 mg QD,
d 1–10 (am)
(n=39),
d 18–24 (am) (12 h after pm famotidine)
(n=20)e
0.89
(0.81, 0.97)
0.88
(0.80, 0.96)
0.77
(0.63, 0.93)
40 mg BID, d 18–24
(n=18)
300 mg QD/ritonavir 100 mg QD/tenofovir 300 mg QD, d 1–10 (am) (n=39),
d 18–24 (am) (10 h after pm famotidine and 2 h before am famotidine) (n=18)e
0.74
(0.66, 0.84)
0.79
(0.70, 0.88)
0.72
(0.63, 0.83)
40 mg BID, d 11–20
(n=15)
300 mg QD/ritonavir 100 mg QD, d 1–10 (am) (n=46),
then 400 mg QD/ritonavir 100 mg QD, d 11–20 (am) (n=15)
1.02
(0.87, 1.18)
1.03
(0.86, 1.22)
0.86
(0.68, 1.08)
ketoconazole
200 mg QD, d 7–13
(n=14)
400 mg QD, d 1–13
(n=14)
0.99
(0.77, 1.28)
1.10
(0.89, 1.37)
1.03
(0.53, 2.01)
nevirapinef,g
200 mg BID, d 1–23
(n=23)
300 mg QD/ritonavir 100 mg QD,
d 4–13, then
400 mg QD/ritonavir 100 mg QD, d 14–23 (n=23)h
0.72
(0.60, 0.86)
1.02
(0.85, 1.24)
0.58
(0.48, 0.71)
0.81
(0.65, 1.02)
0.28
(0.20, 0.40)
0.41
(0.27, 0.60)
omeprazole
40 mg QD, d 7–12
(n=16)i
400 mg QD,
d 1–6 (n=48),
d 7–12 (n=16)
0.04
(0.04, 0.05)
0.06
(0.05, 0.07)
0.05
(0.03, 0.07)
40 mg QD, d 11
–20
(n=15)i
300 mg QD/ritonavir 100 mg QD,
d 1–20 (n=15)
0.28
(0.24, 0.32)
0.24
(0.21, 0.27)
0.22
(0.19, 0.26)
20 mg QD, d 17–23 (am)
(n=13)
300 mg QD/ritonavir 100 mg QD,
d 7–16 (pm) (n=27),
d 17–23 (pm) (n=13)j,k
0.61
(0.46, 0.81)
0.58
(0.44, 0.75)
0.54
(0.41, 0.71)
20 mg QD, d 17–23 (am)
(n=14)
300 mg QD/ritonavir 100 mg QD,
d 7–16 (am) (n=27), then
400 mg QD/ritonavir 100 mg QD, d 17–23 (am) (n=14)l,m
0.69
(0.58, 0.83)
0.70
(0.57, 0.86)
0.69
(0.54, 0.88)
pitavastatin
4 mg QD
for 5 days
300 mg QD for 5 days
1.13
(0.96, 1.32)
1.06
(0.90, 1.26)
NA
rifabutin
150 mg QD, d 15–28
(n=7)
400 mg QD, d 1–28
(n=7)
1.34
(1.14, 1.59)
1.15
(0.98, 1.34)
1.13
(0.68, 1.87)
rifampin
600 mg QD, d 17–26
(n=16)
300 mg QD/ritonavir 100 mg QD,
d 7–16 (n=48),
d 17–26 (n=16)
0.47
(0.41, 0.53)
0.28
(0.25, 0.32)
0.02
(0.02, 0.03)
ritonavirn
100 mg QD, d 11–20
(n=28)
300 mg QD, d 1–20
(n=28)
1.86
(1.69, 2.05)
3.38
(3.13, 3.63)
11.89
(10.23, 13.82)
tenofoviro
300 mg QD, d 9–16
(n=34)
400 mg QD, d 2–16
(n=34)
0.79
(0.73, 0.86)
0.75
(0.70, 0.81)
0.60
(0.52, 0.68)
300 mg QD, d 15–42
(n=10)
300 mg/ritonavir 100 mg QD, d 1–42
(n=10)
0.72p
(0.50, 1.05)
0.75q
(0.58, 0.97)
0.77q
(0.54, 1.10)
voriconazole
(Subjects with at least one functional CYP2C19 allele)
200 mg BID, d 2–3, 22–30;
400 mg BID, d 1, 21
(n=20)
300 mg/ritonavir 100 mg QD, d 11–30
(n=20)
0.87
(0.80, 0.96)
0.88
(0.82, 0.95)
0.80
(0.72, 0.90)
voriconazole
(Subjects without a functional CYP2C19 allele)
50 mg BID, d 2–3, 22–30;
100 mg BID, d 1, 21
(n=8)
300 mg/ritonavir 100 mg QD, d 11–30
(n=8)
0.81
(0.66, 1.00)
0.80
(0.65, 0.97)
0.69
(0.54, 0.87)
Table 22: Drug Interactions: Pharmacokinetic Parameters for Coadministered Drugs in the Presence of REYATAZa
Coadministered
Drug Coadministered Drug
Dose/Schedule REYATAZ
Dose/Schedule Ratio (90% Confidence Interval) of Coadministered Drug Pharmacokinetic Parameters with/without
REYATAZ;
No Effect = 1.00
Cmax AUC Cmin
a Data provided are under fed conditions unless otherwise noted.
b 400 mg ddI EC and REYATAZ were administered together with food on Days 8 and 19.
c Upon further dose normalization of ethinyl estradiol 25 mcg with atazanavir relative to ethinyl estradiol 35 mcg without atazanavir, the ratio of geometric means (90% confidence intervals) for Cmax, AUC, and Cmin were 0.82 (0.73, 0.92), 1.06 (0.95, 1.17), and 1.35 (1.11, 1.63), respectively.
d Upon further dose normalization of ethinyl estradiol 35 mcg with atazanavir/ritonavir relative to ethinyl estradiol 25 mcg without atazanavir/ritonavir, the ratio of geometric means (90% confidence intervals) for Cmax, AUC, and Cmin were 1.17 (1.03, 1.34), 1.13 (1.05, 1.22), and 0.88 (0.77, 1.00), respectively.
e All subjects were on a 28 day lead-in period; one full cycle of Ortho Tri-Cyclen®. Ortho Tri-Cyclen® contains 35 mcg of ethinyl estradiol. Ortho Tri-Cyclen® LO contains 25 mcg of ethinyl estradiol. Results were dose normalized to an ethinyl estradiol dose of 35 mcg.
f 17-deacetyl norgestimate is the active component of norgestimate.
g (R)-methadone is the active isomer of methadone.
h Study was conducted in HIV-infected individuals.
i Subjects were treated with nevirapine prior to study entry.
j Omeprazole was used as a metabolic probe for CYP2C19. Omeprazole was given 2 hours after REYATAZ on Day 7; and was given alone 2 hours after a light meal on Day 20.
k Not the recommended therapeutic dose of atazanavir.
l When compared to rifabutin 150 mg QD alone d1–10 (n=14). Total of rifabutin + 25-O-desacetyl-rifabutin: AUC 2.19 (1.78, 2.69).
m Rosiglitazone used as a probe substrate for CYP2C8.
n Mean ratio (with/without coadministered drug). ↑ indicates an increase in rosuvastatin exposure.
o The combination of atazanavir and saquinavir 1200 mg QD produced daily saquinavir exposures similar to the values produced by the standard therapeutic dosing of saquinavir at 1200 mg TID. However, the Cmax is about 79% higher than that for the standard dosing of saquinavir (soft gelatin capsules) alone at 1200 mg TID.
p Note that similar results were observed in a study where administration of tenofovir and REYATAZ was separated by 12 hours.
q Administration of tenofovir and REYATAZ was temporally separated by 12 hours.
NA = not available.
acetaminophen
1 gm BID, d 1–20
(n=10)
300 mg QD/ritonavir 100 mg QD,
d 11–20 (n=10)
0.87
(0.77, 0.99)
0.97
(0.91, 1.03)
1.26
(1.08, 1.46)
atenolol
50 mg QD, d 7–11 (n=19)
and d 19–23
400 mg QD, d 1–11
(n=19)
1.34
(1.26, 1.42)
1.25
(1.16, 1.34)
1.02
(0.88, 1.19)
boceprevir
800 mg TID,
d 1–6, 25–31
300 mg QD/ritonavir 100 mg QD,
d 10–31
0.93
(0.80, 1.08)
0.95
(0.87, 1.05)
0.82
(0.68, 0.98)
clarithromycin
500 mg BID, d 7–10 (n=21)
and d 18–21
400 mg QD, d 1–10
(n=21)
1.50
(1.32, 1.71)
OH-clarithromycin:
0.28
(0.24, 0.33)
1.94
(1.75, 2.16)
OH-clarithromycin:
0.30
(0.26, 0.34)
2.60
(2.35, 2.88)
OH-clarithromycin:
0.38
(0.34, 0.42)
ddI (enteric-coated [EC] capsules)b
400 mg d 1 (fasted), d 8 (fed)
(n=34)
400 mg QD,
d 2–8
(n=34)
0.64
(0.55, 0.74)
0.66
(0.60, 0.74)
1.13
(0.91, 1.41)
400 mg d 1 (fasted), d 19 (fed)
(n=31)
300 mg QD/ritonavir 100 mg QD, d 9–19
(n=31)
0.62
(0.52, 0.74)
0.66
(0.59, 0.73)
1.25
(0.92, 1.69)
diltiazem
180 mg QD, d 7–11 (n=28)
and d 19–23
400 mg QD, d 1–11
(n=28)
1.98
(1.78, 2.19)
desacetyl-diltiazem:
2.72
(2.44, 3.03)
2.25
(2.09, 2.16)
desacetyl-diltiazem:
2.65
(2.45, 2.87)
2.42
(2.14, 2.73)
desacetyl-diltiazem:
2.21
(2.02, 2.42)
ethinyl estradiol & norethindronec
Ortho-Novum®7/7/7 QD, d 1–29
(n=19)
400 mg QD,
d 16–29
(n=19)
ethinyl estradiol: 1.15
(0.99, 1.32)
norethindrone: 1.67
(1.42, 1.96)
ethinyl estradiol: 1.48
(1.31, 1.68)
norethindrone: 2.10
(1.68, 2.62)
ethinyl estradiol: 1.91
(1.57, 2.33)
norethindrone: 3.62
(2.57, 5.09)
ethinyl estradiol & norgestimated
Ortho Tri-Cyclen® QD, d 1–28 (n=18),
then Ortho Tri-Cyclen® LO QD, d 29–42e
(n=14)
300 mg QD/ritonavir 100 mg QD,
d 29–42
(n=14)
ethinyl estradiol:
0.84
(0.74, 0.95)
17-deacetyl norgestimate:f
1.68
(1.51, 1.88)
ethinyl estradiol:
0.81
(0.75, 0.87)
17-deacetyl
norgestimate:f
1.85
(1.67, 2.05)
ethinyl estradiol:
0.63
(0.55, 0.71)
17-deacetyl norgestimate:f
2.02
(1.77, 2.31)
methadone
Stable maintenance
dose, d 1–15
(n=16)
400 mg QD, d 2–15
(n=16)
(R)-methadoneg
0.91
(0.84, 1.0)
total: 0.85
(0.78, 0.93)
(R)-methadoneg
1.03
(0.95, 1.10)
total: 0.94
(0.87, 1.02)
(R)-methadoneg
1.11
(1.02, 1.20)
total: 1.02
(0.93, 1.12)
nevirapineh,i
200 mg BID, d 1–23
(n=23)
300 mg QD/ritonavir 100 mg QD,
d 4–13, then
400 mg QD/ritonavir 100 mg QD,
d 14–23
(n=23)
1.17
(1.09, 1.25)
1.21
(1.11, 1.32)
1.25
(1.17, 1.34)
1.26
(1.17, 1.36)
1.32
(1.22, 1.43)
1.35
(1.25, 1.47)
omeprazolej
40 mg single dose, d 7 and d 20
(n=16)
400 mg QD, d 1–12
(n=16)
1.24
(1.04, 1.47)
1.45
(1.20, 1.76)
NA
rifabutin
300 mg QD, d 1–10
then 150 mg QD, d 11–20
(n=3)
600 mg QD,k
d 11–20
(n=3)
1.18
(0.94, 1.48)
25-O-desacetyl-rifabutin: 8.20
(5.90, 11.40)
2.10
(1.57, 2.79)
25-O-desacetyl-rifabutin: 22.01
(15.97, 30.34)
3.43
(1.98, 5.96)
25-O-desacetyl-rifabutin: 75.6
(30.1, 190.0)
150 mg twice weekly, d 1–15
(n=7)
300 mg QD/ritonavir 100 mg QD,
d 1–17
(n=7)
2.49l
(2.03, 3.06)
25-O-desacetyl-rifabutin: 7.77
(6.13, 9.83)
1.48l
(1.19, 1.84)
25-O-desacetyl-rifabutin: 10.90
(8.14, 14.61)
1.40l
(1.05, 1.87)
25-O-desacetyl-rifabutin: 11.45
(8.15, 16.10)
pitavastatin
4 mg QD
for 5 days
300 mg QD
for 5 days
1.60
(1.39, 1.85)
1.31
(1.23, 1.39)
NA
rosiglitazonem
4 mg single dose, d 1, 7, 17
(n=14)
400 mg QD, d 2–7, then
300 mg QD/ritonavir 100 mg QD,
d 8–17
(n=14)
1.08
(1.03, 1.13)
0.97
(0.91, 1.04)
1.35
(1.26, 1.44)
0.83
(0.77, 0.89)
NA
NA
rosuvastatin
10 mg single dose
300 mg QD/ritonavir 100 mg QD for 7 days
↑ 7-foldn
↑ 3-foldn
NA
saquinaviro(soft gelatin capsules)
1200 mg QD, d 1–13
(n=7)
400 mg QD, d 7–13
(n=7)
4.39
(3.24, 5.95)
5.49
(4.04, 7.47)
6.86
(5.29, 8.91)
tenofovirp
300 mg QD, d 9–16 (n=33)
and d 24–30
(n=33)
400 mg QD, d 2–16
(n=33)
1.14
(1.08, 1.20)
1.24
(1.21, 1.28)
1.22
(1.15, 1.30)
300 mg QD, d 1–7 (pm) (n=14)
d 25–34 (pm) (n=12)
300 mg QD/ritonavir 100 mg QD, d 25–34 (am)
(n=12)q
1.34
(1.20, 1.51)
1.37
(1.30, 1.45)
1.29
(1.21, 1.36)
voriconazole
(Subjects with at least one functional CYP2C19 allele)
200 mg BID, d 2–3, 22–30; 400 mg BID, d 1, 21
(n=20)
300 mg/ritonavir 100 mg QD, d 11–30
(n=20)
0.90
(0.78, 1.04)
0.67
(0.58, 0.78)
0.61
(0.51, 0.72)
voriconazole
(Subjects without a functional CYP2C19 allele)
50 mg BID, d 2–3, 22–30; 100 mg BID, d 1, 21
(n=8)
300 mg/ritonavir 100 mg QD, d 11–30
(n=8)
4.38
(3.55, 5.39)
5.61
(4.51, 6.99)
7.65
(5.71, 10.2)
lamivudine + zidovudine
150 mg lamivudine + 300 mg zidovudine BID, d 1–12
(n=19)
400 mg QD, d 7–12
(n=19)
lamivudine: 1.04
(0.92, 1.16)
zidovudine: 1.05
(0.88, 1.24)
zidovudine
glucuronide: 0.95
(0.88, 1.02)
lamivudine: 1.03
(0.98, 1.08)
zidovudine: 1.05
(0.96, 1.14)
zidovudine glucuronide: 1.00
(0.97, 1.03)
lamivudine: 1.12
(1.04, 1.21)
zidovudine: 0.69
(0.57, 0.84)
zidovudine glucuronide: 0.82
(0.62, 1.08)
12.4 Microbiology
Mechanism of Action
Atazanavir (ATV) is an azapeptide HIV-1 protease inhibitor (PI). The compound selectively inhibits the virus-specific processing of viral Gag and Gag-Pol polyproteins in HIV-1 infected cells, thus preventing formation of mature virions.
Antiviral Activity in Cell Culture
Atazanavir exhibits anti-HIV-1 activity with a mean 50% effective concentration (EC50) in the absence of human serum of 2 to 5 nM against a variety of laboratory and clinical HIV-1 isolates grown in peripheral blood mononuclear cells, macrophages, CEM-SS cells, and MT-2 cells. ATV has activity against HIV-1 Group M subtype viruses A, B, C, D, AE, AG, F, G, and J isolates in cell culture. ATV has variable activity against HIV-2 isolates (1.9-32 nM), with EC50 values above the EC50 values of failure isolates. Two-drug combination antiviral activity studies with ATV showed no antagonism in cell culture with NNRTIs (delavirdine, efavirenz, and nevirapine), PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir), NRTIs (abacavir, didanosine, emtricitabine, lamivudine, stavudine, tenofovir, zalcitabine, and zidovudine), the HIV-1 fusion inhibitor enfuvirtide, and two compounds used in the treatment of viral hepatitis, adefovir and ribavirin, without enhanced cytotoxicity.
Resistance
In Cell Culture: HIV-1 isolates with a decreased susceptibility to ATV have been selected in cell culture and obtained from patients treated with ATV or atazanavir/ritonavir (ATV/RTV). HIV-1 isolates with 93- to 183-fold reduced susceptibility to ATV from three different viral strains were selected in cell culture by 5 months. The substitutions in these HIV-1 viruses that contributed to ATV resistance include I50L, N88S, I84V, A71V, and M46I. Changes were also observed at the protease cleavage sites following drug selection. Recombinant viruses containing the I50L substitution without other major PI substitutions were growth impaired and displayed increased susceptibility in cell culture to other PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir). The I50L and I50V substitutions yielded selective resistance to ATV and amprenavir, respectively, and did not appear to be cross-resistant.
Clinical Studies of Treatment-Naive Patients: Comparison of Ritonavir-Boosted REYATAZ vs. Unboosted REYATAZ: Study AI424-089 compared REYATAZ 300 mg once daily with ritonavir 100 mg vs. REYATAZ 400 mg once daily when administered with lamivudine and extended-release stavudine in HIV-infected treatment-naive patients. A summary of the number of virologic failures and virologic failure isolates with ATV resistance in each arm is shown in Table 23.
Table 23: Summary of Virologic Failuresa at Week 96 in Study AI424-089: Comparison of Ritonavir Boosted REYATAZ vs. Unboosted REYATAZ: Randomized Patients
a Virologic failure includes patients who were never suppressed through Week 96 and on study at Week 96, had virologic rebound or discontinued due to insufficient viral load response.
b Percentage of Virologic Failure Isolates with genotypic and phenotypic data.
c Mixture of I50I/L emerged in 2 other ATV 400 mg-treated patients. Neither isolate was phenotypically resistant to ATV.
REYATAZ 300 mg
+
ritonavir 100 mg
(n=95)
REYATAZ 400 mg
(n=105)
Virologic Failure (≥50 copies/mL) at Week 96
15 (16%)
34 (32%)
Virologic Failure with Genotypes and Phenotypes Data
5
17
Virologic Failure Isolates with ATV-resistance at Week 96
0/5 (0%)b
4/17 (24%)b
Virologic Failure Isolates with I50L Emergence at Week 96c
0/5 (0%)b
2/17 (12%)b
Virologic Failure Isolates with Lamivudine Resistance at Week 96
2/5 (40%)b
11/17 (65%)b
Clinical Studies of Treatment-Naive Patients Receiving REYATAZ 300 mg with Ritonavir 100 mg: In Phase III study AI424-138, an as-treated genotypic and phenotypic analysis was conducted on samples from patients who experienced virologic failure (HIV-1 RNA ≥400 copies/mL) or discontinued before achieving suppression on ATV/RTV (n=39; 9%) and LPV/RTV (n=39; 9%) through 96 weeks of treatment. In the ATV/RTV arm, one of the virologic failure isolates had a 56-fold decrease in ATV susceptibility emerge on therapy with the development of PI resistance-associated substitutions L10F, V32I, K43T, M46I, A71I, G73S, I85I/V, and L90M. The NRTI resistance-associated substitution M184V also emerged on treatment in this isolate conferring emtricitabine resistance. Two ATV/RTV-virologic failure isolates had baseline phenotypic ATV resistance and IAS-defined major PI resistance-associated substitutions at baseline. The I50L substitution emerged on study in one of these failure isolates and was associated with a 17-fold decrease in ATV susceptibility from baseline and the other failure isolate with baseline ATV resistance and PI substitutions (M46M/I and I84I/V) had additional IAS-defined major PI substitutions (V32I, M46I, and I84V) emerge on ATV treatment associated with a 3-fold decrease in ATV susceptibility from baseline. Five of the treatment failure isolates in the ATV/RTV arm developed phenotypic emtricitabine resistance with the emergence of either the M184I (n=1) or the M184V (n=4) substitution on therapy and none developed phenotypic tenofovir disoproxil resistance. In the LPV/RTV arm, one of the virologic failure patient isolates had a 69-fold decrease in LPV susceptibility emerge on therapy with the development of PI substitutions L10V, V11I, I54V, G73S, and V82A in addition to baseline PI substitutions L10L/I, V32I, I54I/V, A71I, G73G/S, V82V/A, L89V, and L90M. Six LPV/RTV virologic failure isolates developed the M184V substitution and phenotypic emtricitabine resistance and two developed phenotypic tenofovir disoproxil resistance.
Clinical Studies of Treatment-Naive Patients Receiving REYATAZ 400 mg without Ritonavir: ATV-resistant clinical isolates from treatment-naive patients who experienced virologic failure on REYATAZ 400 mg treatment without ritonavir often developed an I50L substitution (after an average of 50 weeks of ATV therapy), often in combination with an A71V substitution, but also developed one or more other PI substitutions (eg, V32I, L33F, G73S, V82A, I85V, or N88S) with or without the I50L substitution. In treatment-naive patients, viral isolates that developed the I50L substitution, without other major PI substitutions, showed phenotypic resistance to ATV but retained in cell culture susceptibility to other PIs (amprenavir, indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir); however, there are no clinical data available to demonstrate the effect of the I50L substitution on the efficacy of subsequently administered PIs.
Clinical Studies of Treatment-Experienced Patients: In studies of treatment-experienced patients treated with ATV or ATV/RTV, most ATV-resistant isolates from patients who experienced virologic failure developed substitutions that were associated with resistance to multiple PIs and displayed decreased susceptibility to multiple PIs. The most common protease substitutions to develop in the viral isolates of patients who failed treatment with ATV 300 mg once daily and RTV 100 mg once daily (together with tenofovir and an NRTI) included V32I, L33F/V/I, E35D/G, M46I/L, I50L, F53L/V, I54V, A71V/T/I, G73S/T/C, V82A/T/L, I85V, and L89V/Q/M/T. Other substitutions that developed on ATV/RTV treatment including E34K/A/Q, G48V, I84V, N88S/D/T, and L90M occurred in less than 10% of patient isolates. Generally, if multiple PI resistance substitutions were present in the HIV-1 virus of the patient at baseline, ATV resistance developed through substitutions associated with resistance to other PIs and could include the development of the I50L substitution. The I50L substitution has been detected in treatment-experienced patients experiencing virologic failure after long-term treatment. Protease cleavage site changes also emerged on ATV treatment but their presence did not correlate with the level of ATV resistance.
Clinical Studies of Pediatric Subjects in AI424-397 (PRINCE I) and AI424-451 (PRINCE II): Treatment-emergent ATV/RTV resistance-associated amino acid substitution M36I in the protease was detected in the virus of one subject among treatment failures in AI424-397. In addition, three known resistance-associated substitutions for other PIs arose in the viruses from one subject each (L19I/R, H69K/R, and I72I/V). Reduced susceptibility to ATV, RTV, or ATV/RTV was not seen with these viruses. In AI424-451, ATV/RTV resistance-associated substitutions G16E, V82A/I/T, I84V, and/or L90M arose in the viruses of two subjects. The virus population harboring the M46M/V, V82V/I, I84I/V, and L90L/M substitutions acquired phenotypic resistance to RTV (RTV phenotypic fold-change of 3.5, with a RTV cutoff of 2.5-fold change). However, these substitutions did not result in phenotypic resistance to ATV (ATV phenotypic fold-change of <1.8, with an ATV cutoff of 2.2-fold change). Secondary PI resistance-associated amino acid substitutions also arose in the viruses of one subject each, including V11V/I, D30D/G, E35E/D, K45K/R, L63P/S, and I72I/T. Q61D and Q61E/G emerged in the viruses of two subjects who failed treatment with ATV/RTV. Viruses from nine subjects in the two studies developed NRTI resistance-associated substitutions: K65K/R (n=1), M184V (n=7), and T215I (n=1).
Cross-Resistance
Cross-resistance among PIs has been observed. Baseline phenotypic and genotypic analyses of clinical isolates from ATV clinical trials of PI-experienced patients showed that isolates cross-resistant to multiple PIs were cross-resistant to ATV. Greater than 90% of the isolates with substitutions that included I84V or G48V were resistant to ATV. Greater than 60% of isolates containing L90M, G73S/T/C, A71V/T, I54V, M46I/L, or a change at V82 were resistant to ATV, and 38% of isolates containing a D30N substitution in addition to other changes were resistant to ATV. Isolates resistant to ATV were also cross-resistant to other PIs with >90% of the isolates resistant to indinavir, lopinavir, nelfinavir, ritonavir, and saquinavir, and 80% resistant to amprenavir. In treatment-experienced patients, PI-resistant viral isolates that developed the I50L substitution in addition to other PI resistance-associated substitution were also cross-resistant to other PIs.
Baseline Genotype/Phenotype and Virologic Outcome Analyses
Genotypic and/or phenotypic analysis of baseline virus may aid in determining ATV susceptibility before initiation of ATV/RTV therapy. An association between virologic response at 48 weeks and the number and type of primary PI resistance-associated substitutions detected in baseline HIV-1 isolates from antiretroviral-experienced patients receiving ATV/RTV once daily or lopinavir (LPV)/RTV twice daily in Study AI424-045 is shown in Table 24.
Overall, both the number and type of baseline PI substitutions affected response rates in treatment-experienced patients. In the ATV/RTV group, patients had lower response rates when 3 or more baseline PI substitutions, including a substitution at position 36, 71, 77, 82, or 90, were present compared to patients with 1–2 PI substitutions, including one of these substitutions.
Table 24: HIV RNA Response by Number and Type of Baseline PI Substitution, Antiretroviral-Experienced Patients in Study AI424-045, As-Treated Analysis
a Primary substitutions include any change at D30, V32, M36, M46, I47, G48, I50, I54, A71, G73, V77, V82, I84, N88, and L90.
b Results should be interpreted with caution because the subgroups were small.
c There were insufficient data (n<3) for PI substitutions V32I, I47V, G48V, I50V, and F53L.
Virologic Response = HIV RNA <400 copies/mLb
Number and Type of Baseline PI
Substitutionsa
ATV/RTV
(n=110)
LPV/RTV
(n=113)
3 or more primary PI substitutions includingc:
D30N
75% (6/8)
50% (3/6)
M36I/V
19% (3/16)
33% (6/18)
M46I/L/T
24% (4/17)
23% (5/22)
I54V/L/T/M/A
31% (5/16)
31% (5/16)
A71V/T/I/G
34% (10/29)
39% (12/31)
G73S/A/C/T
14% (1/7)
38% (3/8)
V77I
47% (7/15)
44% (7/16)
V82A/F/T/S/I
29% (6/21)
27% (7/26)
I84V/A
11% (1/9)
33% (2/6)
N88D
63% (5/8)
67% (4/6)
L90M
10% (2/21)
44% (11/25)
Number of baseline primary PI substitutionsa
All patients, as-treated
58% (64/110)
59% (67/113)
0–2 PI substitutions
75% (50/67)
75% (50/67)
3–4 PI substitutions
41% (14/34)
43% (12/28)
5 or more PI substitutions
0% (0/9)
28% (5/18)
The response rates of antiretroviral-experienced patients in Study AI424-045 were analyzed by baseline phenotype (shift in susceptibility in cell culture relative to reference, Table 25). The analyses are based on a select patient population with 62% of patients receiving an NNRTI-based regimen before study entry compared to 35% receiving a PI-based regimen. Additional data are needed to determine clinically relevant break points for REYATAZ.
Table 25: Baseline Phenotype by Outcome, Antiretroviral-Experienced Patients in Study AI424-045, As-Treated Analysis
Virologic Response = HIV RNA <400 copies/mLb
Baseline Phenotypea ATV/RTV
(n=111) LPV/RTV
(n=111)
a Fold change susceptibility in cell culture relative to the wild-type reference.
b Results should be interpreted with caution because the subgroups were small.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Long-term carcinogenicity studies in mice and rats were carried out with atazanavir for two years. In the mouse study, drug-related increases in hepatocellular adenomas were found in females at 360 mg/kg/day. The systemic drug exposure (AUC) at the NOAEL (no observable adverse effect level) in females, (120 mg/kg/day) was 2.8 times and in males (80 mg/kg/day) was 2.9 times higher than those in humans at the clinical dose (300 mg/day atazanavir boosted with 100 mg/day ritonavir, non-pregnant patients). In the rat study, no drug-related increases in tumor incidence were observed at doses up to 1200 mg/kg/day, for which AUCs were 1.1 (males) or 3.9 (females) times those measured in humans at the clinical dose.
Mutagenesis
Atazanavir tested positive in an in vitro clastogenicity test using primary human lymphocytes, in the absence and presence of metabolic activation. Atazanavir tested negative in the in vitro Ames reverse-mutation assay, in vivo micronucleus and DNA repair tests in rats, and in vivo DNA damage test in rat duodenum (comet assay).
Impairment of Fertility
At the systemic drug exposure levels (AUC) 0.9 (in male rats) or 2.3 (in female rats) times that of the human clinical dose, (300 mg/day atazanavir boosted with 100 mg/day ritonavir) significant effects on mating, fertility, or early embryonic development were not observed.
14 CLINICAL STUDIES
14.1 Adult Patients without Prior Antiretroviral Therapy
Study AI424-138: a 96-week study comparing the antiviral efficacy and safety of REYATAZ/ritonavir with lopinavir/ritonavir, each in combination with fixed-dose tenofovir-emtricitabine in HIV-1 infected treatment-naive subjects. Study AI424-138 was a 96-week, open-label, randomized, multicenter study, comparing REYATAZ (300 mg once daily) with ritonavir (100 mg once daily) to lopinavir with ritonavir (400/100 mg twice daily), each in combination with fixed-dose tenofovir with emtricitabine (300/200 mg once daily), in 878 antiretroviral treatment-naive treated patients. Patients had a mean age of 36 years (range: 19-72), 49% were Caucasian, 18% Black, 9% Asian, 23% Hispanic/Mestizo/mixed race, and 68% were male. The median baseline plasma CD4+ cell count was 204 cells/mm3 (range: 2 to 810 cells/mm3) and the mean baseline plasma HIV-1 RNA level was 4.94 log10 copies/mL (range: 2.60 to 5.88 log10 copies/mL). Treatment response and outcomes through Week 96 are presented in Table 26.
Table 26: Outcomes of Treatment Through Week 96 in Treatment-Naive Adults (Study AI424-138)
a As a fixed-dose combination: 300 mg tenofovir, 200 mg emtricitabine once daily.
b Patients achieved HIV RNA <50 copies/mL at Week 96. Roche Amplicor®, v1.5 ultra-sensitive assay.
c Pre-specified ITT analysis at Week 48 using as-randomized cohort: ATV/RTV 78% and LPV/RTV 76% (difference estimate: 1.7% [95% confidence interval: −3.8%, 7.1%]).
d Pre-specified ITT analysis at Week 96 using as-randomized cohort: ATV/RTV 74% and LPV/RTV 68% (difference estimate: 6.1% [95% confidence interval: 0.3%, 12.0%]).
e Includes viral rebound and failure to achieve confirmed HIV RNA <50 copies/mL through Week 96.
f Includes lost to follow-up, patient’s withdrawal, noncompliance, protocol violation, and other reasons.
REYATAZ
300 mg + ritonavir 100 mg
(once daily) with tenofovir/emtricitabine
(once daily)a
(n=441)
lopinavir
400 mg + ritonavir 100 mg
(twice daily) with tenofovir/emtricitabine
(once daily)a
(n=437)
Outcome
96 Weeks
96 Weeks
Responderb,c,d
75%
68%
Virologic failuree
17%
19%
Rebound
8%
10%
Never suppressed through Week 96
9%
9%
Death
1%
1%
Discontinued due to adverse event
3%
5%
Discontinued for other reasonsf
4%
7%
Through 96 weeks of therapy, the proportion of responders among patients with high viral loads (ie, baseline HIV RNA ≥100,000 copies/mL) was comparable for the REYATAZ/ritonavir (165 of 223 patients, 74%) and lopinavir/ritonavir (148 of 222 patients, 67%) arms. At 96 weeks, the median increase from baseline in CD4+ cell count was 261 cells/mm3 for the REYATAZ/ritonavir arm and 273 cells/mm3 for the lopinavir/ritonavir arm.
Study AI424-034: REYATAZ once daily compared to efavirenz once daily, each in combination with fixed-dose lamivudine + zidovudine twice daily. Study AI424-034 was a randomized, double-blind, multicenter trial comparing REYATAZ (400 mg once daily) to efavirenz (600 mg once daily), each in combination with a fixed-dose combination of lamivudine (3TC) (150 mg) and zidovudine (ZDV) (300 mg) given twice daily, in 810 antiretroviral treatment-naive patients. Patients had a mean age of 34 years (range: 18 to 73), 36% were Hispanic, 33% were Caucasian, and 65% were male. The mean baseline CD4+ cell count was 321 cells/mm3 (range: 64 to 1424 cells/mm3) and the mean baseline plasma HIV-1 RNA level was 4.8 log10 copies/mL (range: 2.2 to 5.9 log10 copies/mL). Treatment response and outcomes through Week 48 are presented in Table 27.
Table 27: Outcomes of Randomized Treatment Through Week 48 in Treatment-Naive Adults (Study AI424-034)
a Patients achieved and maintained confirmed HIV RNA <400 copies/mL (<50 copies/mL) through Week 48. Roche Amplicor® HIV-1 Monitor™ Assay, test version 1.0 or 1.5 as geographically appropriate.
b Includes viral rebound and failure to achieve confirmed HIV RNA <400 copies/mL through Week 48.
c Includes lost to follow-up, patient’s withdrawal, noncompliance, protocol violation, and other reasons.
d As a fixed-dose combination: 150 mg lamivudine, 300 mg zidovudine twice daily.
Outcome
REYATAZ
400 mg once daily
+ lamivudine
+ zidovudined
(n=405)
efavirenz
600 mg once daily
+ lamivudine
+ zidovudined
(n=405)
Respondera
67% (32%)
62% (37%)
Virologic failureb
20%
21%
Rebound
17%
16%
Never suppressed through Week 48
3%
5%
Death
–
<1%
Discontinued due to adverse event
5%
7%
Discontinued for other reasonsc
8%
10%
Through 48 weeks of therapy, the proportion of responders among patients with high viral loads (ie, baseline HIV RNA ≥100,000 copies/mL) was comparable for the REYATAZ and efavirenz arms. The mean increase from baseline in CD4+ cell count was 176 cells/mm3 for the REYATAZ arm and 160 cells/mm3for the efavirenz arm.
Study AI424-008: REYATAZ 400 mg once daily compared to REYATAZ 600 mg once daily, and compared to nelfinavir 1250 mg twice daily, each in combination with stavudine and lamivudine twice daily. Study AI424-008 was a 48-week, randomized, multicenter trial, blinded to dose of REYATAZ, comparing REYATAZ at two dose levels (400 mg and 600 mg once daily) to nelfinavir (1250 mg twice daily), each in combination with stavudine (40 mg) and lamivudine (150 mg) given twice daily, in 467 antiretroviral treatment-naive patients. Patients had a mean age of 35 years (range: 18 to 69), 55% were Caucasian, and 63% were male. The mean baseline CD4+ cell count was 295 cells/mm3 (range: 4 to 1003 cells/mm3) and the mean baseline plasma HIV-1 RNA level was 4.7 log10 copies/mL (range: 1.8 to 5.9 log10 copies/mL). Treatment response and outcomes through Week 48 are presented in Table 28.
Table 28: Outcomes of Randomized Treatment Through Week 48 in Treatment-Naive Adults (Study AI424-008)
a Patients achieved and maintained confirmed HIV RNA <400 copies/mL (<50 copies/mL) through Week 48. Roche Amplicor® HIV-1 Monitor™ Assay, test version 1.0 or 1.5 as geographically appropriate.
b Includes viral rebound and failure to achieve confirmed HIV RNA <400 copies/mL through Week 48.
c Includes lost to follow-up, patient’s withdrawal, noncompliance, protocol violation, and other reasons.
Outcome
REYATAZ
400 mg once daily +
lamivudine + stavudine
(n=181)
nelfinavir
1250 mg twice daily +
lamivudine + stavudine
(n=91)
Respondera
67% (33%)
59% (38%)
Virologic failureb
24%
27%
Rebound
14%
14%
Never suppressed through Week 48
10%
13%
Death
<1%
–
Discontinued due to adverse event
1%
3%
Discontinued for other reasonsc
7%
10%
Through 48 weeks of therapy, the mean increase from baseline in CD4+ cell count was 234 cells/mm3for the REYATAZ 400-mg arm and 211 cells/mm3 for the nelfinavir arm.
14.2 Adult Patients with Prior Antiretroviral Therapy
Study AI424-045: REYATAZ once daily + ritonavir once daily compared to REYATAZ once daily + saquinavir (soft gelatin capsules) once daily, and compared to lopinavir + ritonavir twice daily, each in combination with tenofovir + one NRTI. Study AI424-045 was a randomized, multicenter trial comparing REYATAZ (300 mg once daily) with ritonavir (100 mg once daily) to REYATAZ (400 mg once daily) with saquinavir soft gelatin capsules (1200 mg once daily), and to lopinavir + ritonavir (400/100 mg twice daily), each in combination with tenofovir and one NRTI, in 347 (of 358 randomized) patients who experienced virologic failure on HAART regimens containing PIs, NNRTIs, and NRTIs. The mean time of prior exposure to antiretrovirals was 139 weeks for PIs, 85 weeks for NNRTIs, and 283 weeks for NRTIs. The mean age was 41 years (range: 24 to 74); 60% were Caucasian, and 78% were male. The mean baseline CD4+ cell count was 338 cells/mm3 (range: 14 to 1543 cells/mm3) and the mean baseline plasma HIV-1 RNA level was 4.4 log10 copies/mL (range: 2.6 to 5.88 log10 copies/mL).
Treatment outcomes through Week 48 for the REYATAZ/ritonavir and lopinavir/ritonavir treatment arms are presented in Table 29. REYATAZ/ritonavir and lopinavir/ritonavir were similar for the primary efficacy outcome measure of time-averaged difference in change from baseline in HIV RNA level. Study AI424-045 was not large enough to reach a definitive conclusion that REYATAZ/ritonavir and lopinavir/ritonavir are equivalent on the secondary efficacy outcome measure of proportions below the HIV RNA lower limit of quantification [see MICROBIOLOGY, TABLES 24 AND 25 (12.4)].
Table 29: Outcomes of Treatment Through Week 48 in Study AI424-045 (Patients with Prior Antiretroviral Experience)
a Time-averaged difference through Week 48 for HIV RNA; Week 48 difference in HIV RNA percentages and CD4+ mean changes, REYATAZ/ritonavir vs lopinavir/ritonavir; CI = 97.5% confidence interval for change in HIV RNA; 95% confidence interval otherwise.
b Roche Amplicor® HIV-1 Monitor™ Assay, test version 1.5.
c Protocol-defined primary efficacy outcome measure.
d Based on patients with baseline and Week 48 CD4+ cell count measurements (REYATAZ/ritonavir, n=85; lopinavir/ritonavir, n=93).
e Patients achieved and maintained confirmed HIV-1 RNA <400 copies/mL (<50 copies/mL) through Week 48.
Outcome
REYATAZ 300 mg + ritonavir 100 mg once daily + tenofovir + 1 NRTI
(n=119)
lopinavir/ritonavir
(400/100 mg) twice daily
+ tenofovir + 1 NRTI
(n=118)
Differencea
(REYATAZ-lopinavir/ritonavir)
(CI)
HIV RNA Change from Baseline (log10copies/mL)b
−1.58
−1.70
+0.12c
(−0.17, 0.41)
CD4+ Change from Baseline (cells/mm3)d
116
123
−7
(−67, 52)
Percent of Patients Respondinge
HIV RNA <400 copies/mLb
55%
57%
−2.2%
(−14.8%, 10.5%)
HIV RNA <50 copies/mLb
38%
45%
−7.1%
(−19.6%, 5.4%)
No patients in the REYATAZ/ritonavir treatment arm and three patients in the lopinavir/ritonavir treatment arm experienced a new-onset CDC Category C event during the study.
In Study AI424-045, the mean change from baseline in plasma HIV-1 RNA for REYATAZ 400 mg with saquinavir (n=115) was −1.55 log10 copies/mL, and the time-averaged difference in change in HIV-1 RNA levels versus lopinavir/ritonavir was 0.33. The corresponding mean increase in CD4+ cell count was 72 cells/mm3. Through 48 weeks of treatment, the proportion of patients in this treatment arm with plasma HIV-1 RNA <400 (<50) copies/mL was 38% (26%). In this study, coadministration of REYATAZ and saquinavir did not provide adequate efficacy [see DRUG INTERACTIONS (7)].
Study AI424-045 also compared changes from baseline in lipid values. [See ADVERSE REACTIONS (6.1).]
Study AI424-043: Study AI424-043 was a randomized, open-label, multicenter trial comparing REYATAZ (400 mg once daily) to lopinavir/ritonavir (400/100 mg twice daily), each in combination with two NRTIs, in 300 patients who experienced virologic failure to only one prior PI-containing regimen. Through 48 weeks, the proportion of patients with plasma HIV-1 RNA <400 (<50) copies/mL was 49% (35%) for patients randomized to REYATAZ (n=144) and 69% (53%) for patients randomized to lopinavir/ritonavir (n=146). The mean change from baseline was −1.59 log10 copies/mL in the REYATAZ treatment arm and −2.02 log10 copies/mL in the lopinavir/ritonavir arm. Based on the results of this study, REYATAZ without ritonavir was inferior to lopinavir/ritonavir in PI-experienced patients with prior virologic failure and is not recommended for such patients.
14.3 Pediatric Patients
Pediatric Trials with REYATAZ Capsules
Assessment of the pharmacokinetics, safety, tolerability, and virologic response of REYATAZ capsules was based on data from the open-label, multicenter clinical trial PACTG 1020A which included patients from 6 years to 21 years of age. In this study, 105 patients (43 antiretroviral-naive and 62 antiretroviral-experienced) received once daily REYATAZ capsule formulation, with or without ritonavir, in combination with two NRTIs.
One-hundred five (105) patients (6 to less than 18 years of age) treated with the REYATAZ capsule formulation, with or without ritonavir, were evaluated. Using an ITT analysis, the overall proportions of antiretroviral-naive and -experienced patients with HIV RNA <400 copies/mL at Week 96 were 51% (22/43) and 34% (21/62), respectively. The overall proportions of antiretroviral-naive and -experienced patients with HIV RNA <50 copies/mL at Week 96 were 47% (20/43) and 24% (15/62), respectively. The median increase from baseline in absolute CD4 count at 96 weeks of therapy was 335 cells/mm3 in antiretroviral-naive patients and 220 cells/mm3 in antiretroviral-experienced patients.
Pediatric Trials with REYATAZ Oral Powder
Assessment of the pharmacokinetics, safety, tolerability, and virologic response of REYATAZ oral powder was based on data from two open-label, multicenter clinical trials.
•
AI424-397 (PRINCE I): In pediatric patients from 3 months to less than 6 years of age
•
AI424-451 (PRINCE II): In pediatric patients from 3 months to less than 11 years of age
In these studies 155 patients (59 antiretroviral-naive and 96 antiretroviral-experienced) received once daily REYATAZ oral powder and ritonavir, in combination with two NRTIs.
For inclusion in both trials, treatment-naive patients had to have genotypic sensitivity to REYATAZ and two NRTIs, and treatment-experienced patients had to have documented genotypic and phenotypic sensitivity at screening to REYATAZ and at least 2 NRTIs. Patients exposed only to antiretrovirals in utero or intrapartum were considered treatment-naive. Patients who received REYATAZ or REYATAZ/ritonavir at any time prior to study enrollment or who had a history of treatment failure on two or more protease inhibitors were excluded from the trials.
One hundred thirty-four (134) patients from both studies weighing 5 kg to less than 35 kg treated with REYATAZ oral powder with ritonavir were evaluated. Patients 5 kg to less than 10 kg received either 150 mg or 200 mg REYATAZ and 80 mg ritonavir oral solution; patients 10 kg to less than 15 kg received 200 mg REYATAZ and 80 mg ritonavir oral solution; patients 15 kg to less than 25 kg received 250 mg REYATAZ and 80 mg ritonavir oral solution; and patients 25 kg to less than 35 kg received 300 mg REYATAZ and 100 mg ritonavir.
Using a modified ITT analysis, the overall proportions of antiretroviral-naive and antiretroviral-experienced patients with HIV RNA <400 copies/mL at Week 48 were 79% (41/52) and 62% (51/82), respectively in patients who received REYATAZ oral powder with ritonavir. The overall proportions of antiretroviral-naive and antiretroviral-experienced patients with HIV RNA <50 copies/mL at Week 48 were 54% (28/52) and 50% (41/82), respectively in patients who received REYATAZ oral powder with ritonavir. The median increase from baseline in absolute CD4 count (percent) at 48 weeks of therapy (last observation carried forward) was 215 cells/mm3 (6%) in antiretroviral-naive patients and 133 cells/mm3 (4%) in antiretroviral-experienced patients who received REYATAZ oral powder with ritonavir.
16 HOW SUPPLIED/STORAGE AND HANDLING
REYATAZ Capsules
REYATAZ® (atazanavir) capsules are available in the following strengths and configurations of plastic bottles with child-resistant closures.
* 150 mg atazanavir equivalent to 170.8 mg atazanavir sulfate.
200 mg atazanavir equivalent to 227.8 mg atazanavir sulfate.
300 mg atazanavir equivalent to 341.69 mg atazanavir sulfate.
Product Strength*
Capsule Shell Color (cap/body)
Markings on Capsule
(ink color)
Capsules per Bottle
NDC Number
cap
body
150 mg
blue/powder blue
BMS 150 mg (white)
3624
(blue)
60
150 mg
200 mg
blue/blue
BMS 200 mg (white)
3631
(white)
60
200 mg
300 mg
red/blue
BMS 300 mg
(white)
3622
(white)
30
300 mg
Store REYATAZ capsules at 25°C (77°F); excursions permitted to 15°C-30°C (59°F-86°F) [see USP Controlled Room Temperature].
REYATAZ Oral Powder
REYATAZ oral powder is an orange-vanilla flavored powder, packed in child-resistant packets. Each packet contains 50 mg of atazanavir equivalent to 56.9 mg of atazanavir sulfate in 1.5 g of powder. REYATAZ oral powder is supplied in cartons (NDC 0003-3638-10) of 30 packets each. [See DOSAGE AND ADMINISTRATION (2.4).]
Store REYATAZ oral powder below 30°C (86°F). Once the REYATAZ oral powder is mixed with food or beverage, it may be kept at room temperature 20°C to 30°C (68°F-86°F) for up to 1 hour prior to administration. Store REYATAZ oral powder in the original packet and do not open until ready to use.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (PATIENT INFORMATION and INSTRUCTIONS FOR USE).
REYATAZ is not a cure for HIV infection and patients may continue to experience illnesses associated with HIV infection, including opportunistic infections. Tell patients that sustained decreases in plasma HIV RNA have been associated with a reduced risk of progression to AIDS and death. Advise patients to remain under the care of a healthcare provider while using REYATAZ.
HIV Transmission
Advise patients to avoid doing things that can spread HIV infection to others.
•
Do not share or reuse needles or other injection equipment.
•
Do not share personal items that can have blood or body fluids on them, like toothbrushes and razor blades.
•
Do not have any kind of sex without protection. Always practice safer sex by using a latex or polyurethane condom to lower the chance of sexual contact with semen, vaginal secretions, or blood.
•
Do not breastfeed. REYATAZ can be passed to your baby in your breast milk and it is not known whether it could harm your baby. Also, mothers with HIV should not breastfeed because HIV can be passed to the baby in breast milk.
Cardiac Conduction Abnormalities
Inform patients that atazanavir may produce changes in the electrocardiogram (eg, PR prolongation). Tell patients to consult their healthcare provider if they are experiencing symptoms such as dizziness or lightheadedness [see WARNINGS AND PRECAUTIONS (5.1)].
Severe Skin Reaction
Inform patients that there have been reports of severe skin reactions (eg, Stevens-Johnson syndrome, erythema multiforme, and toxic skin eruptions) with REYATAZ use. Advise patients that if signs or symptoms of severe skin reactions or hypersensitivity reactions develop, they must discontinue REYATAZ and seek medical evaluation immediately [see WARNINGS AND PRECAUTIONS (5.2) and ADVERSE REACTIONS (6.1)].
Hyperbilirubinemia
Inform patients that asymptomatic elevations in indirect bilirubin have occurred in patients receiving REYATAZ. This may be accompanied by yellowing of the skin or whites of the eyes and alternative antiretroviral therapy may be considered if the patient has cosmetic concerns [see WARNINGS AND PRECAUTIONS (5.3)].
Patients with Phenylketonuria
Advise caregivers of patients with phenylketonuria that REYATAZ oral powder contains phenylalanine [see WARNINGS AND PRECAUTIONS (5.4)].
Nephrolithiasis and Cholelithiasis
Inform patients that kidney stones and/or gallstones have been reported with REYATAZ use. Some patients with kidney stones and/or gallstones required hospitalization for additional management and some had complications. Discontinuation of REYATAZ may be necessary as part of the medical management of these adverse events [see WARNINGS AND PRECAUTIONS (5.6)].
Drug Interactions
REYATAZ may lead to significant interaction with some drugs; therefore, advise patients to report the use of any other prescription, nonprescription medication, or herbal products, particularly St. John’s wort, to their healthcare provider prior to use [see CONTRAINDICATIONS (4), WARNINGS AND PRECAUTIONS (5.7)].
Fat Redistribution
Inform patients that redistribution or accumulation of body fat may occur in patients receiving antiretroviral therapy including protease inhibitors and that the cause and long-term health effects of these conditions are not known at this time.
Dosing Instructions
Advise patients to take REYATAZ with food every day and take other concomitant antiretroviral therapy as prescribed. REYATAZ must always be used in combination with other antiretroviral drugs. Advise patients that they should not alter the dose or discontinue therapy without consulting with their healthcare provider. Tell patients if a dose of REYATAZ is missed, they should take the dose as soon as possible and then return to their normal schedule; however, if a dose is skipped the patient should not double the next dose.
Pregnancy
Inform pregnant patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to REYATAZ during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry [see USE IN SPECIFIC POPULATIONS (8.1)].
PATIENT PACKAGE INSERT
PATIENT INFORMATION
REYATAZ® (RAY-ah-taz)
(atazanavir)
capsules
REYATAZ® (RAY-ah-taz)
(atazanavir)
oral powder
Important: Ask your healthcare provider or pharmacist about medicines that should not be taken with REYATAZ. For more information, see “Who should not take REYATAZ?” and “What should I tell my healthcare provider before taking REYATAZ?”
What is REYATAZ?
REYATAZ is a prescription HIV-1 (Human Immunodeficiency Virus-type 1) medicine that is used with other antiretroviral medicines to treat HIV-1 infection in adults and children 3 months of age and older and who weigh at least 11 pounds (5 kg). HIV-1 is the virus that causes AIDS (Acquired Immunodeficiency Syndrome).
REYATAZ should not be used in children younger than 3 months of age.
When used with other antiretroviral medicines to treat HIV-1 infection, REYATAZ may help:
•
reduce the amount of HIV-1 in your blood. This is called “viral load”.
•
increase the number of CD4+ (T) cells in your blood that help fight off other infections.
Reducing the amount of HIV-1 and increasing the CD4+ (T) cells in your blood may help improve your immune system. This may reduce your risk of death or getting infections that can happen when your immune system is weak (opportunistic infections).
REYATAZ does not cure HIV-1 infection or AIDS. You must keep taking HIV-1 medicines to control HIV-1 infection and decrease HIV-related illnesses.
Avoid doing things that can spread HIV-1 infection to others:
•
Do not share or reuse needles or other injection equipment.
•
Do not share personal items that can have blood or body fluids on them, like toothbrushes and razor blades.
•
Do not have any kind of sex without protection. Always practice safer sex by using a latex or polyurethane condom to lower the chance of sexual contact with any body fluids such as semen, vaginal secretions, or blood.
Ask your healthcare provider if you have any questions about how to prevent passing HIV-1 to other people.
Who should not take REYATAZ?
Do not take REYATAZ if you:
•
are allergic to atazanavir or any of the ingredients in REYATAZ. See the end of this leaflet for a complete list of ingredients in REYATAZ.
•
are taking any of the following medicines. Taking REYATAZ with these medicines may affect how REYATAZ works. REYATAZ may cause serious life-threatening side effects or death when used with these medicines:
o
alfuzosin (UROXATRAL ®)
o
cisapride (PROPULSID ®)
o
ergot medicines including:
▪
ergotamine tartrate (CAFERGOT ®, MIGERGOT ®, ERGOMAR ®, ERGOSTAT ®, MEDIHALER ®, Ergotamine, WIGRAINE ®, WIGRETTES ®)
▪
dihydroergotamine mesylate (D.H.E. 45 ®, MIGRANAL ®)
▪
methylergonovine (METHERGINE ®)
o
indinavir (CRIXIVAN ®)
o
irinotecan (CAMPTOSAR ®)
o
lurasidone (LATUDA ®) if REYATAZ is used with ritonavir (NORVIR ®)
o
lovastatin (ADVICOR ®, ALTOPREV ®, MEVACOR ®)
o
midazolam (VERSED ®), when taken by mouth for sedation
o
nevirapine (VIRAMUNE ®, VIRAMUNE XR ®)
o
pimozide (ORAP ®)
o
rifampin (RIFADIN ®, RIFAMATE®, RIFATER ®, RIMACTANE ®)
o
sildenafil (REVATIO ®), when used for the treatment of pulmonary arterial hypertension
o
simvastatin (SIMCOR ®, VYTORIN ®, ZOCOR ®)
o
St. John’s wort (Hypericum perforatum)
o
triazolam (HALCION ®)
Serious problems can happen if you or your child takes any of the medicines listed above with REYATAZ.
What should I tell my healthcare provider before taking REYATAZ?
Before taking REYATAZ, tell your healthcare provider if you:
•
have heart problems
•
have liver problems, including hepatitis B or C virus infection
•
have phenylketonuria (PKU). REYATAZ oral powder contains phenylalanine as part of the artificial sweetener aspartame. The artificial sweetener can be harmful to people with PKU.
•
are receiving dialysis treatment
•
have diabetes
•
have hemophilia
•
have any other medical conditions
•
are pregnant or plan to become pregnant. Talk to your healthcare provider about taking REYATAZ during your pregnancy or if you are planning to become pregnant while you are taking REYATAZ.
o
Hormonal forms of birth control, such as injections, vaginal rings or implants, contraceptive patch, and some birth control pills may not work during treatment with REYATAZ. Talk to your healthcare provider about forms of birth control that may be used during treatment with REYATAZ.
o
Pregnancy Registry. There is a pregnancy registry for women who take antiretroviral medicines during pregnancy. The purpose of this registry is to collect information about the health of you and your baby. Talk to your healthcare provider about how you can take part in this registry.
o
After your baby is born, tell your healthcare provider if your baby’s skin or the white part of the eyes turns yellow.
•
are breastfeeding or plan to breastfeed. Do not breastfeed if you are taking REYATAZ. You should not breastfeed if you have HIV-1 because of the risk of passing HIV-1 to your baby. REYATAZ can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Some medicines interact with REYATAZ. Keep a list of your medicines to show your healthcare provider and pharmacist. You can ask your healthcare provider or pharmacist for a list of medicines that interact with REYATAZ. Do not start taking a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take REYATAZ with other medicines.
How should I take REYATAZ?
•
Take REYATAZ exactly as your healthcare provider tells you to.
•
Do not change your dose or stop taking REYATAZ unless your healthcare provider tells you to.
•
Stay under the care of your healthcare provider during treatment with REYATAZ.
•
REYATAZ must be used with other antiretroviral medicines.
•
Take REYATAZ 1 time each day.
•
REYATAZ comes as capsules and oral powder.
•
Take REYATAZ capsules and oral powder with food.
•
Swallow the capsules whole. Do not open the capsules.
•
REYATAZ oral powder must be mixed with food or liquid. Your child’s healthcare provider will prescribe the right dose of REYATAZ based on your child’s weight.
•
REYATAZ oral powder must be taken with ritonavir.
•
If you miss a dose of REYATAZ, take it as soon as you remember. Then take the next dose at your regular time. Do not take 2 doses at the same time.
•
If you take too much REYATAZ, call your healthcare provider or go to the nearest hospital emergency room right away.
When your supply of REYATAZ starts to run low, get more from your healthcare provider or pharmacy. It is important not to run out of REYATAZ. The amount of HIV-1 in your blood may increase if the medicine is stopped for even a short time. The virus may become resistant to REYATAZ and harder to treat.
What are the possible side effects of REYATAZ?
REYATAZ can cause serious side effects, including:
•
A change in the way your heart beats (heart rhythm change). Tell your healthcare provider right away if you get dizzy or lightheaded. These could be symptoms of a heart problem.
•
Skin rash. Skin rash is common with REYATAZ but can sometimes be severe. Skin rash usually goes away within 2 weeks without any change in treatment. Severe rash may develop in association with other symptoms which could be serious. If you develop a severe rash or a rash with any of the following symptoms, stop taking REYATAZ and call your healthcare provider right away:
o
general feeling of discomfort or “flu-like” symptoms
o
fever
o
muscle or joint aches
o
red or inflamed eyes, like “pink eye” (conjunctivitis)
o
blisters
o
mouth sores
o
swelling of your face
o
painful, warm, or red lump under your skin
•
Yellowing of your skin or the white part of your eyes is common with REYATAZ, and is usually not harmful in adults and infants older than 3 months of age; but it could also be a symptom of a serious problem. These effects may be due to increases in bilirubin levels in your blood (bilirubin is made by the liver). Although these effects may not be damaging to your liver, skin, or eyes, tell your healthcare provider right away if your skin or the white part of your eyes turns yellow.
•
Liver problems. If you have liver problems, including hepatitis B or C infection, your liver problems may get worse when you take REYATAZ. Your healthcare provider will do blood tests to check your liver before you start REYATAZ and during treatment. Tell your healthcare provider right away if you get any of the following symptoms:
o
dark “tea-colored” urine
o
your skin or the white part of your eyes turns yellow
o
light colored stools
o
nausea
o
itching
o
stomach-area pain
•
Kidney stones have happened in some people who take REYATAZ. Tell your healthcare provider right away if you get symptoms of kidney stones which may include, pain in your low back or low stomach-area, blood in your urine, or pain when you urinate.
•
Gallbladder problems have happened in some people who take REYATAZ. Tell your healthcare provider right away if you get symptoms of gallbladder problems which may include:
o
pain in the right or middle upper stomach area
o
fever
o
nausea and vomiting
o
your skin or the white part of your eyes turns yellow
•
Diabetes and high blood sugar (hyperglycemia) have happened or have worsened in some people who take protease inhibitor medicines like REYATAZ. Some people have had to start taking medicine to treat diabetes or have had to change their diabetes medicine.
•
Changes in your immune system (Immune Reconstitution Syndrome) can happen when you start taking HIV-1 medicines. Your immune system may get stronger and begin to fight infections that have been hidden in your body for a long time. Tell your healthcare provider if you start having new symptoms after starting REYATAZ.
•
Changes in body fat can happen in people taking HIV-1 medicines. These changes may include increased amount of fat in the upper back and neck (“buffalo hump”), breast, and around the main part of your body (trunk). Loss of fat from the legs, arms, and face may also happen. The exact cause and long-term health effects of these conditions are not known.
•
Increased bleeding problems in people with hemophilia have happened when taking protease inhibitors like REYATAZ.
The most common side effects of REYATAZ include:
•
nausea
•
headache
•
stomach-area pain
•
vomiting
•
trouble sleeping
•
numbness, tingling, or burning of hands or feet
•
dizziness
•
muscle pain
•
diarrhea
•
depression
•
fever
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of REYATAZ. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store REYATAZ?
REYATAZ capsules:
•
Store REYATAZ capsules at room temperature, between 68°F to 77°F (20°C to 25°C).
•
Keep capsules in a tightly closed container.
REYATAZ oral powder:
•
Store REYATAZ oral powder below 86°F (30°C).
•
Store REYATAZ oral powder in the original packet. Do not open until ready to use.
•
After REYATAZ oral powder is mixed with food or liquid it may be kept at room temperature 68°F to 86°F (20°C to 30°C) for up to 1 hour. Take REYATAZ oral powder within 1 hour after mixing with food or liquid.
Keep REYATAZ and all medicines out of the reach of children.
General information about the safe and effective use of REYATAZ
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use REYATAZ for a condition for which it was not prescribed. Do not give REYATAZ to other people, even if they have the same symptoms that you have. It may harm them. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about REYATAZ that is written for health professionals.
For more information, go to www.reyataz.com or call 1-800-321-1335.
What are the ingredients in REYATAZ?
Active ingredient: atazanavir sulfate
Inactive ingredients:
REYATAZ capsules: crospovidone, lactose monohydrate, and magnesium stearate. The capsule shells contain gelatin, FD&C Blue No. 2, titanium dioxide, black iron oxide, red iron oxide, and yellow iron oxide. The capsules are printed with ink containing shellac, titanium dioxide, FD&C Blue No. 2, isopropyl alcohol, ammonium hydroxide, propylene glycol, n-butyl alcohol, simethicone, and dehydrated alcohol.
REYATAZ oral powder: aspartame, sucrose, and orange-vanilla flavor.
Distributed by:
Bristol-Myers Squibb Company, Princeton, NJ 08543 USA.
Product of Ireland
REYATAZ® is a registered trademark of Bristol-Myers Squibb Company. Other brands listed are the trademarks of their respective owners and are not trademarks of Bristol-Myers Squibb Company.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Revised: September 2016
INSTRUCTIONS FOR USE
Instructions for Use
REYATAZ® (RAY-ah-taz)
(atazanavir)
oral powder
Read this Instructions for Use before you prepare your child’s first dose of REYATAZ oral powder, each time you get a refill, and as needed. There may be new information. This information does not take the place of talking to your child’s healthcare provider about their medical condition or treatment. Ask your child’s healthcare provider or pharmacist if you have questions about how to mix or give a dose of REYATAZ oral powder.
Important information:
•
For more information about REYATAZ oral powder, see the Patient Information leaflet.
•
REYATAZ oral powder must be mixed with food or liquid. If REYATAZ oral powder is mixed with water, the child must eat food right after taking REYATAZ oral powder.
•
REYATAZ oral powder must be taken with ritonavir.
•
Talk with your child’s healthcare provider to help decide the best schedule for giving your child REYATAZ oral powder.
Instructions for mixing REYATAZ oral powder:
REYATAZ oral powder should be mixed with food such as applesauce or yogurt, instead of a liquid (milk, infant formula, or water) in young children and infants who can take food.
•
Infants less than 6 months old and who cannot eat solid food or drink from a cup should be given REYATAZ oral powder mixed with infant formula using an oral dosing syringe.
•
REYATAZ oral powder that is mixed in infant formula or liquid should not be given using a baby bottle.
When preparing REYATAZ oral powder with either food or liquid, choose a clean, flat work surface. Place a clean paper towel on the work surface. Place the supplies you will need on the paper towel.
Wash and dry your hands before and after preparing REYATAZ oral powder.
Preparing a dose of REYATAZ oral powder mixed with food:
Before you prepare a dose of REYATAZ oral powder mixed with food, gather the following supplies:
•
paper towel
•
tablespoon
•
small clean container (such as a small cup or bowl)
•
a food such as applesauce or yogurt
•
the correct number of packets of REYATAZ oral powder needed for the prescribed dose
Step 1. Place at least 1 tablespoon of a food such as applesauce or yogurt in the small container (see Figure A).
[Reyataz Figure A]
Figure A
Step 2. Tap the packet of REYATAZ oral powder to settle the contents to the bottom of the packet (see Figure B).
[Reyataz Figure B]
Figure B
Step 3. Using a clean pair of scissors, cut open the packet on the dotted line (see Figure C).
[Reyataz Figure C]
Figure C
Step 4. Empty the contents of the packet into the small container onto the food (see Figure D).
[Reyataz Figure D]
Figure D
Repeat Steps 2 through 4 for each packet of REYATAZ oral powder needed for the total prescribed dose.
Step 5. Use a tablespoon to gently mix the powder and the food together (see Figure E).
[Reyataz Figure E]
Figure E
Steps 6 through 8 must be completed within 1 hour of mixing the medicine.
Step 6. Use the tablespoon or a small spoon to feed the REYATAZ oral powder and food mixture to your child. Look in your child’s mouth to make sure that all of the mixture is swallowed.
Step 7. Add 1 tablespoon more of food to the empty container and gently stir to mix with any contents that may still be in the container.
Step 8. Use the tablespoon or a small spoon to feed your child the mixture, making sure your child has swallowed all of the mixture.
Step 9. Give your child ritonavir as prescribed right after taking REYATAZ oral powder.
Step 10. Wash the container and tablespoon. Allow the container and spoon to dry. Throw away the paper towel and clean the work surface.
Preparing a dose of REYATAZ oral powder mixed with liquid in a small drinking cup:
Before you prepare a dose of REYATAZ oral powder mixed with liquid in a small drinking cup, gather the following supplies:
•
paper towel
•
spoon
•
30 milliliter (mL) medicine cup (ask your pharmacist for this). See Figure F.
•
small drinking cup
•
liquid such as milk or water
•
the correct number of packets of REYATAZ oral powder needed for the prescribed dose
[Reyataz Figure F]
Figure F
Step 1. Using the 30 mL medicine cup, pour at least 30 mL of liquid into the small drinking cup (see Figure G).
[Reyataz Figure G]
Figure G
Step 2. Tap the packet of REYATAZ oral powder to settle the contents to the bottom of the packet (see Figure H).
[Reyataz Figure H]
Figure H
Step 3. Using a clean pair of scissors, cut open the packet on the dotted line (see Figure I).
[Reyataz Figure I]
Figure I
Step 4. Empty the contents of the packet into the small drinking cup (see Figure J).
[Reyataz Figure J]
Figure J
Repeat Steps 2 through 4 for each packet of REYATAZ oral powder needed for the total prescribed dose.
Step 5. Hold the small drinking cup with one hand. With your other hand, use the spoon to gently mix the powder and the liquid (see Figure K).
[Reyataz Figure K]
Figure K
Steps 6 and 7 must be completed within 1 hour of mixing the medicine.
Step 6. Have your child drink all of the mixture in the small drinking cup.
Step 7. To make sure there is no mixture left in the small drinking cup add 15 mL more liquid to the small drinking cup:
•
Stir with the spoon.
•
Repeat Step 6 above.
If REYATAZ oral powder is mixed with water, your child must eat food right after taking REYATAZ oral powder.
Step 8. Give your child ritonavir as prescribed right after taking REYATAZ oral powder.
Step 9. Wash the small drinking cup, medicine cup, and spoon. Allow the small drinking cup, medicine cup, and spoon to dry. Throw away the paper towel and clean the work surface.
Preparing a dose of REYATAZ oral powder mixed with liquid infant formula using an oral dosing syringe and a small medicine cup:
Before you prepare a dose of REYATAZ oral powder mixed with infant formula using an oral dosing syringe, gather the following supplies:
•
paper towel
•
small spoon
•
30 milliliter (mL) medicine cup (ask your pharmacist for this). See Figure L.
•
10 mL oral dosing syringe (ask your pharmacist for this). See Figure L.
•
infant formula
•
the correct number of packets of REYATAZ oral powder needed for the prescribed dose
[Reyataz Figure L]
Figure L
Step 1. Prepare the infant formula according to the directions on the infant formula package.
Step 2. Pour 10 mL of infant formula into the medicine cup (see Figure M).
[Reyataz Figure M]
Figure M
Step 3. Tap the packet of REYATAZ oral powder to settle the contents to the bottom of the packet (see Figure N).
[Reyataz Figure N]
Figure N
Step 4. Using a clean pair of scissors, cut open the packet on the dotted line (see Figure O).
[Reyataz Figure O]
Figure O
Step 5. Empty the contents of the packet into the medicine cup (see Figure P).
[Reyataz Figure P]
Figure P
Repeat Steps 3 through 5 for each packet of REYATAZ oral powder needed for the total prescribed dose.
Step 6. Hold the medicine cup with one hand. With your other hand, use the small spoon to gently mix the powder and the infant formula (see Figure Q).
[Reyataz Figure Q]
Figure Q
Steps 7 through 9 must be completed within 1 hour of mixing the medicine.
Step 7. Draw up the powder and infant formula mixture into the oral dosing syringe as follows:
•
Check that the plunger is completely pushed into barrel of the syringe (see Figure R).
[Reyataz Figure R]
Figure R
•
Place the tip of the syringe into the powder and infant formula mixture in the medicine cup (see Figure S).
[Reyataz Figure S]
Figure S
•
Slowly pull back on the plunger and draw up 10 mL of the mixture (see Figure T).
[Reyataz Figure T]
Figure T
Step 8. Place the tip of the oral dosing syringe in your baby’s mouth along the inner cheek on either the right or left side (see Figure U). Slowly push on the plunger to give your baby all of the REYATAZ oral powder and infant formula mixture.
•
Draw up any remaining mixture with the oral dosing syringe and repeat until all of the mixture has been given to the baby.
[Reyataz Figure U]
Figure U
Step 9. To make sure there is no mixture left in the medicine cup or syringe:
•
Repeat Step 1 above to add 10 mL more infant formula to the medicine cup
•
Stir with a small spoon.
•
Then repeat Steps 7 through 8 above.
To make sure that your baby gets all of the medicine, do not give REYATAZ oral powder in a baby bottle.
Step 10. Give your baby ritonavir as prescribed right after taking REYATAZ oral powder.
Step 11. Remove the plunger from the oral dosing syringe. Wash the medicine cup, spoon, and oral dosing syringe. Allow the medicine cup, spoon, and oral dosing syringe to dry. Throw away the paper towel and clean the work surface.
How should I store REYATAZ oral powder?
•
Store REYATAZ oral powder below 86°F (30°C).
•
Store REYATAZ oral powder in the original packet. Do not open until ready to use.
•
After REYATAZ oral powder is mixed with food or liquid, it may be kept at room temperature 68°F to 86°F (20°C to 30°C) for up to 1 hour. Take REYATAZ oral powder within 1 hour after mixing with food or liquid.
Keep REYATAZ oral powder and all medicines out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Distributed by:
Bristol-Myers Squibb Company
Princeton, NJ 08543 USA
Product of Ireland
Revised: September 2016