DESCRIPTION
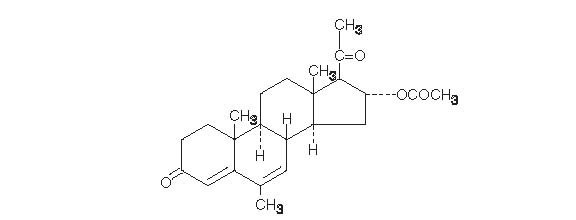
Megestrol acetate oral suspension, USP contains megestrol acetate, a synthetic derivative of the naturally occurring steroid hormone, progesterone. Megestrol acetate is a white, crystalline solid chemically designated as 17-Hydroxy-6-methylpregna-4,6-diene-3,20-dione acetate. Solubility at 37°C in water is 2 mcg per mL, solubility in plasma is 24 mcg per mL. Its molecular weight is 384.52.
The chemical formula is C24H32O4 and the structural formula is represented as follows:
Megestrol acetate oral suspension is supplied as an oral suspension containing 40 mg of micronized megestrol acetate per mL.
Megestrol acetate oral suspension contains the following inactive ingredients: alcohol (max 0.06% v/v from flavor), artificial lime flavor, citric acid monohydrate, docusate sodium, glycerin, natural and artificial lemon flavor, purified water, sodium benzoate, sodium citrate dihydrate, sucrose and xanthan gum.
Megestrol acetate oral suspension, 40 mg/mL complies with USP Dissolution Test 2.
CLINICAL PHARMACOLOGY
Several investigators have reported on the appetite enhancing property of megestrol acetate and its possible use in cachexia. The precise mechanism by which megestrol acetate produces effects in anorexia and cachexia is unknown at the present time.
There are several analytical methods used to estimate megestrol acetate plasma concentrations, including gas chromatography-mass fragmentography (GC-MF), high pressure liquid chromatography (HPLC) and radioimmunoassay (RIA). The GC-MF and HPLC methods are specific for megestrol acetate and yield equivalent concentrations. The RIA method reacts to megestrol acetate metabolites and is, therefore, non-specific and indicates higher concentrations than the GC-MF and HPLC methods. Plasma concentrations are dependent, not only on the method used, but also on intestinal and hepatic inactivation of the drug, which may be affected by factors such as intestinal tract motility, intestinal bacteria, antibiotics administered, body weight, diet and liver function.
The major route of drug elimination in humans is urine. When radiolabeled megestrol acetate was administered to humans in doses of 4 to 90 mg, the urinary excretion within 10 days ranged from 56.5 to 78.4% (mean 66.4%) and fecal excretion ranged from 7.7 to 30.3% (mean 19.8%). The total recovered radioactivity varied between 83.1 and 94.7% (mean 86.2%). Megestrol acetate metabolites which were identified in urine constituted 5 to 8% of the dose administered. Respiratory excretion as labeled carbon dioxide and fat storage may have accounted for at least part of the radioactivity not found in urine and feces.
Plasma steady state pharmacokinetics of megestrol acetate were evaluated in 10 adult, cachectic male patients with acquired immunodeficiency syndrome (AIDS) and an involuntary weight loss greater than 10% of baseline. Patients received single oral doses of 800 mg/day of megestrol acetate oral suspension for 21 days. Plasma concentration data obtained on day 21 were evaluated for up to 48 hours past the last dose.
Mean (±1SD) peak plasma concentration (Cmax) of megestrol acetate was 753 (±539) ng/mL. Mean area under the concentration time-curve (AUC) was 10476 (±7788) ng x hr/mL. Median Tmax value was five hours. Seven of 10 patients gained weight in three weeks.
Additionally, 24 adult, asymptomatic HIV seropositive male subjects were dosed once daily with 750 mg of megestrol acetate oral suspension. The treatment was administered for 14 days. Mean Cmax and AUC values were 490 (±238) ng/mL and 6779 (±3048) hr x ng/mL, respectively. The median Tmax value was three hours. The mean Cmin value was 202 (±101) ng/mL. The mean % of fluctuation value was 107 (±40).
The effect of food on the bioavailability of megestrol acetate oral suspension has not been evaluated.
INDICATIONS AND USAGE
Megestrol acetate oral suspension, USP is indicated for the treatment of anorexia, cachexia, or an unexplained, significant weight loss in patients with a diagnosis of acquired immunodeficiency syndrome (AIDS).
CONTRAINDICATIONS
History of hypersensitivity to megestrol acetate or any component of the formulation. Known or suspected pregnancy.
WARNINGS
Megestrol acetate may cause fetal harm when administered to a pregnant woman. For animal data on fetal effects, (see PRECAUTIONS: Carcinogenesis, Mutagenesis, Impairment of Fertility: Impairment of Fertility). There are no adequate and well-controlled studies in pregnant women. If this drug is used during pregnancy, or if the patient becomes pregnant while taking (receiving) this drug, the patient should be apprised of the potential hazard to the fetus. Women of childbearing potential should be advised to avoid becoming pregnant.
Megestrol acetate is not intended for prophylactic use to avoid weight loss.
(See also PRECAUTIONS: Carcinogenesis, Mutagenesis, and Impairment of Fertility section.)
The glucocorticoid activity of megestrol acetate oral suspension has not been fully evaluated. Clinical cases of new onset diabetes mellitus, exacerbation of pre-existing diabetes mellitus, and overt Cushing’s Syndrome have been reported in association with the chronic use of megestrol acetate. In addition, clinical cases of adrenal insufficiency have been observed in patients receiving or being withdrawn from chronic megestrol acetate therapy in the stressed and non-stressed state. Furthermore, adrenocorticotropin (ACTH) stimulation testing has revealedthe frequent occurrence of asymptomatic pituitary-adrenal suppression in patients treated with chronic megestrol acetate therapy. Therefore, the possibility of adrenal insufficiency should be considered in any patient receiving or being withdrawn from chronic megestrol acetate therapy who presents with symptoms and/or signs suggestive of hypoadrenalism (e.g., hypotension, nausea, vomiting, dizziness, or weakness) in either the stressed or non-stressed state. Laboratory evaluation for adrenal insufficiency and consideration of replacement or stress doses of a rapidly acting glucocorticoid are strongly recommended in such patients. Failure to recognize inhibition of the hypothalamic-pituitary-adrenal axis may result in death. Finally, in patients who are receiving or being withdrawn from chronic megestrol acetate therapy, consideration should be given to the use of empiric therapy with stress doses of a rapidly acting glucocorticoid in conditions of stress or serious intercurrent illness (e.g., surgery, infection).
OVERDOSAGE
No serious unexpected side effects have resulted from studies involving megestrol acetate oral suspension administered in dosages as high as 1200 mg/day. In post-marketing experience, limited reports of overdose have been received. Signs and symptoms reported in the context of overdose included diarrhea, nausea, abdominal pain, shortness of breath, cough, unsteady gait, listlessness, and chest pain. There is no specific antidote for overdose with megestrol acetate oral suspension. In case of overdose, appropriate supportive measures should be taken. Megestrol acetate has not been tested for dialyzability, however, due to its low solubility it is postulated that dialysis would not be an effective means of treating overdose
DOSAGE AND ADMINISTRATION
The recommended adult initial dosage of megestrol acetate oral suspension is 800 mg/day (20 mL/day). Shake container well before using.
In clinical trials evaluating different dose schedules, daily doses of 400 and 800 mg/day were found to be clinically effective.
HOW SUPPLIED
Megestrol acetate oral suspension, USP is available as a milky white, lemon-lime flavored oral suspension containing 40 mg of micronized megestrol acetate per mL.
DESCRIPTION OF CLINICAL STUDIES
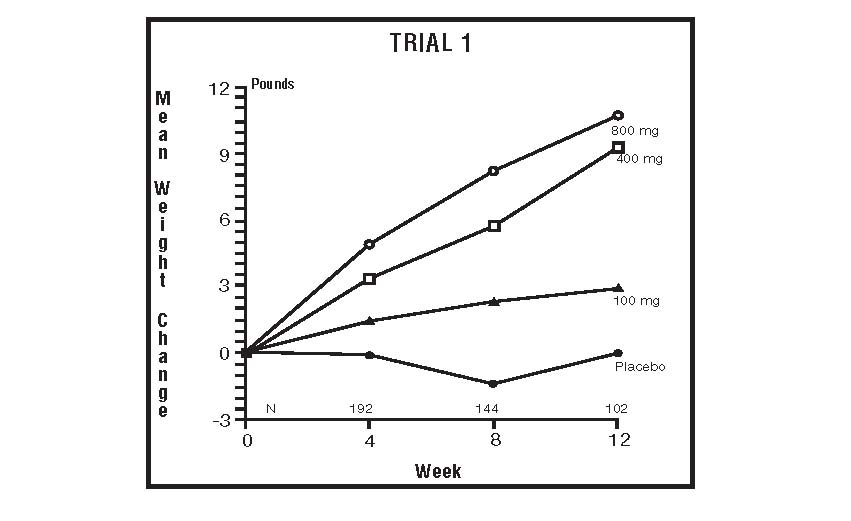
The clinical efficacy of megestrol acetate oral suspension was assessed in two clinical trials. One was a multicenter, randomized, double-blind, placebo-controlled study comparing megestrol acetate (MA) at doses of 100 mg, 400 mg, and 800 mg per day versus placebo in AIDS patients with anorexia/cachexia and significant weight loss. Of the 270 patients entered on study, 195 met all inclusion/exclusion criteria, had at least two additional post baseline weight measurements over a 12 week period or had one post baseline weight measurement but dropped out for therapeutic failure. The percent of patients gaining five or more pounds at maximum weight gain in 12 study weeks was statistically significantly greater for the 800 mg (64%) and 400 mg (57%) MA-treated groups than for the placebo group (24%). Mean weight increased from baseline to last evaluation in 12 study weeks in the 800 mg MA-treated group by 7.8 pounds, the 400 mg MA group by 4.2 pounds, the 100 mg MA group by 1.9 pounds and decreased in the placebo group by 1.6 pounds. Mean weight changes at 4, 8 and 12 weeks for patients evaluable for efficacy in the two clinical trials are shown graphically. Changes in body composition during the 12 study weeks as measured by bioelectrical impedance analysis showed increases innon-water body weight in the MA-treated groups (see CLINICAL STUDIES table). In addition, edema developed or worsened in only 3 patients.
Greater percentages of MA-treated patients in the 800 mg group (89%), the 400 mg group (68%) and the 100 mg group (72%), than in the placebo group (50%), showed an improvement in appetite at last evaluation during the 12 study weeks. A statistically significant difference was observed between the 800 mg MA-treated group and the placebo group in the change in caloric intake from baseline to time of maximum weight change. Patients were asked to assess weight change, appetite, appearance, and overall perception of well-being in a 9 question survey. At maximum weight change only the 800 mg MA-treated group gave responses that were statistically significantly more favorable to all questions when compared to the placebo-treated group. A dose response was noted in the survey with positive responses correlating with higher dose for all questions.
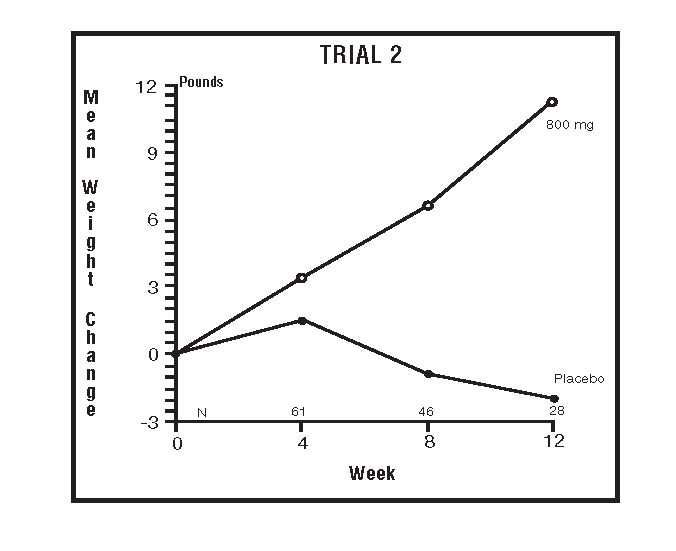
The second trial was a multicenter, randomized, double-blind, placebo-controlled study comparing megestrol acetate 800 mg/day versus placebo in AIDS patients with anorexia/cachexia and significant weight loss. Of the 100 patients entered on study, 65 met all inclusion/exclusion criteria, had at least two additional post baseline weight measurements over a 12 week period or had one post baseline weight measurement but dropped out for therapeutic failure. Patients in the 800 mg MA-treated group had a statistically significantly larger increase in mean maximum weight change than patients in the placebo group. From baseline to study week 12, mean weight increased by 11.2 pounds in the MA-treated group and decreased 2.1 pounds in the placebo group. Changes in body composition as measured by bioelectrical impedance analysis showed increases in non-water weight in the MA-treated group (see CLINICAL STUDIES table). No edema was reported in the MA-treated group. A greater percentage of MA-treated patients (67%) than placebo-treated patients (38%) showed an improvement in appetite at last evaluation during the 12 study weeks; this difference was statistically significant. There were no statistically significant differences between treatment groups in mean caloric change or in daily caloric intake at time to maximum weight change. In the same 9 question survey referenced in the first trial, patients’ assessments of weight change, appetite, appearance, and overall perception of well-being showed increases in mean scores in MA-treated patients as compared to the placebo group.
In both trials, patients tolerated the drug well and no statistically significant differences were seen between the treatment groups with regard to laboratory abnormalities, , new opportunistic infections, lymphocyte counts, T4 counts, T8 counts, or skin reactivity tests (see ADVERSE REACTIONS).
The following figures are the results of mean weight changes for patients evaluable for efficacy in trials 1 and 2