FULL PRESCRIBING INFORMATION
WARNING:
RISK OF SERIOUS CARDIOVASCULAR and GASTROINTESTINAL EVENTS
Cardiovascular Risk Nonsteroidal anti-inflammatory drugs (NSAIDs) may cause an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk [see Warnings and Precautions (5.1)]. MOBIC is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery [see Contraindications (4.2) and Warnings and Precautions (5.1)]. Gastrointestinal Risk NSAIDs cause an increased risk of serious gastrointestinal (GI) adverse reactions including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events [see Warnings and Precautions (5.2)].
1.1 Osteoarthritis (OA) 1.2 Rheumatoid Arthritis (RA) 1.3 Juvenile Rheumatoid Arthritis (JRA) Pauciarticular and Polyarticular Course
1 INDICATIONS AND USAGE1.1 Osteoarthritis (OA) MOBIC is indicated for relief of the signs and symptoms of osteoarthritis [see Clinical Studies (14.1)].
1.2 Rheumatoid Arthritis (RA) MOBIC is indicated for relief of the signs and symptoms of rheumatoid arthritis [see Clinical Studies (14.1)].
1.3 Juvenile Rheumatoid Arthritis (JRA) Pauciarticular and Polyarticular Course MOBIC is indicated for relief of the signs and symptoms of pauciarticular or polyarticular course Juvenile Rheumatoid Arthritis in patients 2 years of age and older [see Clinical Studies (14.2)].
2.1 General Instructions 2.3 Rheumatoid Arthritis
2 DOSAGE AND ADMINISTRATION
2.1 General Instructions Carefully
consider the potential benefits and risks of MOBIC and other treatment
options before deciding to use MOBIC. Use the lowest effective dose for
the shortest duration consistent with individual patient treatment
goals [see Warnings and Precautions (5.4)]. After observing the response to initial therapy with MOBIC, adjust the dose to suit an individual patient's needs. In
adults, the maximum recommended daily oral dose of MOBIC is 15 mg
regardless of formulation. In patients with hemodialysis, a maximum
daily dosage of 7.5 mg is recommended [see Warnings and Precautions (5.6), Use in Specific Populations (8.7), and Clinical Pharmacology
( 12.3)]. MOBIC oral suspension 7.5 mg/5 mL or 15 mg/10 mL may be substituted for MOBIC tablets 7.5 mg or 15 mg, respectively. Shake the oral suspension gently before using. MOBIC may be taken without regard to timing of meals.
2.2 Osteoarthritis For
the relief of the signs and symptoms of osteoarthritis the recommended
starting and maintenance oral dose of MOBIC is 7.5 mg once daily. Some
patients may receive additional benefit by increasing the dose to 15 mg
once daily.
2.3 Rheumatoid Arthritis For the relief of
the signs and symptoms of rheumatoid arthritis, the recommended
starting and maintenance oral dose of MOBIC is 7.5 mg once daily. Some
patients may receive additional benefit by increasing the dose to 15 mg
once daily.
2.4 Juvenile Rheumatoid Arthritis (JRA) Pauciarticular and Polyarticular Course To improve dosing accuracy in smaller weight children, the use of the MOBIC oral suspension is recommended. MOBIC oral suspension is available in the strength of 7.5 mg/5 mL. For the treatment of juvenile rheumatoid arthritis, the recommended oral dose of MOBIC is 0.125 mg/kg once daily up to a maximum of 7.5 mg. There was no additional benefit demonstrated by increasing the dose above 0.125 mg/kg once daily in these clinical trials. Juvenile Rheumatoid Arthritis dosing using the oral suspension should be individualized based on the weight of the child:
0.125 mg/kg
| Weight | Dose (1.5 mg/mL) | Delivered dose |
| 12 kg (26 lb) | 1.0 mL | 1.5 mg |
| 24 kg (54 lb) | 2.0 mL | 3.0 mg |
| 36 kg (80 lb) | 3.0 mL | 4.5 mg |
| 48 kg (106 lb | 4.0 mL | 6.0 mg |
| ≥60 kg (132 lb) | 5.0 mL | 7.5 mg |
3 DOSAGE FORMS AND STRENGTHS
3 DOSAGE FORMS AND STRENGTHS Tablets: 7.5 mg: pastel yellow, round, biconvex, uncoated tablet containing meloxicam 7.5 mg. Impressed with the Boehringer Ingelheim logo on one side and the letter “M” on the other. 15 mg: pastel yellow, oblong, biconvex, uncoated tablet containing meloxicam 15 mg. Impressed with the tablet code “15” on one side and the letter “M” on the other. Oral Suspension: yellowish green tinged viscous suspension containing 7.5 mg meloxicam in 5 mL.4.1 Allergic Reactions 4.2 Coronary Surgery
4 CONTRAINDICATIONS4.1 Allergic Reactions MOBIC is contraindicated in patients with known hypersensitivity (e.g., anaphylactoid reactions and serious skin reactions) to meloxicam. MOBIC should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients [see Warnings and Precautions ( 5.7, 5.13)].
4.2 Coronary Surgery MOBIC is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery [see Warnings and Precautions (5.1)].
5.1 Cardiovascular Thrombotic Events 5.2 Gastrointestinal (GI) Effects - Risk of GI Ulceration, Bleeding, and Perforation 5.3 Hepatic Effects 5.4 Hypertension 5.5 Congestive Heart Failure and Edema 5.6 Renal Effects 5.7 Anaphylactoid Reactions 5.8 Adverse Skin Reactions 5.9 Pregnancy 5.12 Hematological Effects 5.13 Use in Patients with Pre-existing Asthma
5 WARNINGS AND PRECAUTIONS
5.1 Cardiovascular Thrombotic Events Clinical
trials of several COX-2 selective and nonselective NSAIDs of up to
three years’ duration have shown an increased risk of serious
cardiovascular (CV) thrombotic events, myocardial infarction, and
stroke, which can be fatal. All NSAIDs, both COX-2 selective and
nonselective, may have a similar risk. Patients with known CV disease
or risk factors for CV disease may be at greater risk. To minimize the
potential risk for an adverse CV event in patients treated with an
NSAID, the lowest effective dose should be used for the shortest
duration possible. Physicians and patients should remain alert for the
development of such events, even in the absence of previous CV
symptoms. Patients should be informed about the signs and/or symptoms
of serious CV events and the steps to take if they occur. Two
large, controlled, clinical trials of a COX-2 selective NSAID for the
treatment of pain in the first 10 to 14 days following CABG surgery
found an increased incidence of myocardial infarction and stroke [see
Contraindications (4.2)]. There is no consistent evidence that
concurrent use of aspirin mitigates the increased risk of serious CV
thrombotic events associated with NSAID use. The concurrent use of
aspirin and an NSAID does increase the risk of serious GI events [see
Warnings and Precautions (5.2)].
5.2 Gastrointestinal (GI) Effects - Risk of GI Ulceration, Bleeding, and Perforation NSAIDs,
including MOBIC, can cause serious gastrointestinal (GI) adverse events
including inflammation, bleeding, ulceration, and perforation of the
stomach, small intestine, or large intestine, which can be fatal. These
serious adverse events can occur at any time, with or without warning
symptoms, in patients treated with NSAIDs. Only one in five patients
who develop a serious upper GI adverse event on NSAID therapy is
symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by
NSAIDs, occur in approximately 1% of patients treated for 3 to 6
months, and in about 2% to 4% of patients treated for one year. These
trends continue with longer duration of use, increasing the likelihood
of developing a serious GI event at some time during the course of
therapy. However, even short-term therapy is not without risk. Prescribe
NSAIDs, including MOBIC, with extreme caution in those with a prior
history of ulcer disease or gastrointestinal bleeding. Patients with a
prior history of peptic ulcer disease and/or gastrointestinal bleeding
who use NSAIDs have a greater than 10-fold increased risk for
developing a GI bleed compared to patients with neither of these risk
factors. Other factors that increase the risk for GI bleeding in
patients treated with NSAIDs include concomitant use of oral
corticosteroids or anticoagulants, longer duration of NSAID therapy,
smoking, use of alcohol, older age, and poor general health status.
Most spontaneous reports of fatal GI events are in elderly or
debilitated patients and therefore, special care should be taken in
treating this population. To minimize the potential risk for an
adverse GI event in patients treated with an NSAID, use the lowest
effective dose for the shortest possible duration. Patients and
physicians should remain alert for signs and symptoms of GI ulceration
and bleeding during MOBIC therapy and promptly initiate additional
evaluation and treatment if a serious GI adverse event is suspected.
This should include discontinuation of MOBIC until a serious GI adverse
event is ruled out. For high-risk patients, consider alternate
therapies that do not involve NSAIDs.
5.3 Hepatic Effects Borderline
elevations of one or more liver tests may occur in up to 15% of
patients taking NSAIDs including MOBIC. These laboratory abnormalities
may progress, may remain unchanged, or may be transient with continuing
therapy. Notable elevations of ALT or AST (approximately three or more
times the upper limit of normal) have been reported in approximately 1%
of patients in clinical trials with NSAIDs. In addition, rare cases of
severe hepatic reactions, including jaundice and fatal fulminant
hepatitis, liver necrosis and hepatic failure, some of them with fatal
outcomes have been reported [see Adverse Reactions (6.1)]. A
patient with symptoms and/or signs suggesting liver dysfunction, or in
whom an abnormal liver test has occurred, should be evaluated for
evidence of the development of a more severe hepatic reaction while on
therapy with MOBIC. If clinical signs and symptoms consistent with
liver disease develop, or if systemic manifestations occur (e.g.,
eosinophilia, rash, etc.), discontinue MOBIC [see Use in Specific
Populations (8.6) and Clinical Pharmacology (12.3)].
5.4 Hypertension NSAIDs,
including MOBIC, can lead to onset of new hypertension or worsening of
pre-existing hypertension, either of which may contribute to the
increased incidence of CV events. NSAIDs, including MOBIC, should be
used with caution in patients with hypertension. Blood pressure (BP)
should be monitored closely during the initiation of NSAID treatment
and throughout the course of therapy. Patients taking ACE inhibitors, thiazides, or loop diuretics may have impaired response to these therapies when taking NSAIDs.
5.5 Congestive Heart Failure and Edema Fluid
retention and edema have been observed in some patients taking NSAIDs.
Use MOBIC with caution in patients with fluid retention, hypertension,
or heart failure.
5.6 Renal Effects Long-term
administration of NSAIDs, including MOBIC, can result in renal
papillary necrosis, renal insufficiency, acute renal failure, and other
renal injury. Renal toxicity has also been seen in patients in whom
renal prostaglandins have a compensatory role in the maintenance of
renal perfusion. In these patients, administration of a nonsteroidal
anti-inflammatory drug may cause a dose-dependent reduction in
prostaglandin formation and, secondarily, in renal blood flow, which
may precipitate overt renal decompensation. Patients at greatest risk
of this reaction are those with impaired renal function, heart failure,
liver dysfunction, those taking diuretics, ACE-inhibitors, and
angiotensin II receptor antagonists, and the elderly. Discontinuation
of NSAID therapy is usually followed by recovery to the pretreatment
state. A pharmacokinetic study in patients with mild and
moderate renal impairment revealed that no dosage adjustments in these
patient populations are required. Patients with severe renal impairment
have not been studied. The use of MOBIC in patients with severe renal
impairment with CrCl less than 20 mL/min is not recommended. A study
performed in patients on hemodialysis revealed that although overall
Cmax was diminished in this population, the proportion of free drug not
bound to plasma was increased. Therefore it is recommended that
meloxicam dosage in this population not exceed 7.5 mg per day. Closely
monitor the renal function of patients with impaired renal function who
are taking MOBIC [see Dosage and Administration (2.1), Use in Specific
Populations (8.7), and Clinical Pharmacology (12.3)]. Use
caution when initiating treatment with MOBIC in patients with
considerable dehydration. It is advisable to rehydrate patients first
and then start therapy with MOBIC. Caution is also recommended in
patients with pre-existing kidney disease. The extent to which
metabolites may accumulate in patients with renal impairment has not
been studied with MOBIC. Because some MOBIC metabolites are excreted by
the kidney, monitor patients with significant renal impairment closely.
5.7 Anaphylactoid Reactions As
with other NSAIDs, anaphylactoid reactions have occurred in patients
without known prior exposure to MOBIC. MOBIC should not be given to
patients with the aspirin triad. This symptom complex typically occurs
in asthmatic patients who experience rhinitis with or without nasal
polyps, or who exhibit severe, potentially fatal bronchospasm after
taking aspirin or other NSAIDs [see Contraindications (4.1) and
Warnings and Precautions (5.12)]. Seek emergency help in cases where an
anaphylactoid reaction occurs.
5.8 Adverse Skin Reactions NSAIDs,
including MOBIC, can cause serious skin adverse events such as
exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic
epidermal necrolysis (TEN), which can be fatal. These serious events
may occur without warning. Inform patients about the signs and symptoms
of serious skin manifestations and discontinue use of the drug at the
first appearance of skin rash or any other sign of hypersensitivity.
5.9 Pregnancy Starting
at 30 weeks gestation, avoid the use of MOBIC because it may cause
premature closure of the ductus arteriosus [see Use in Specific
Populations (8.1) and Patient Counseling Information (17.8)].
5.10 Corticosteroid Treatment MOBIC
cannot be expected to substitute for corticosteroids or to treat
corticosteroid insufficiency. Abrupt discontinuation of corticosteroids
may lead to disease exacerbation. Slowly taper patients on prolonged
corticosteroid therapy if a decision is made to discontinue
corticosteroids.
5.11 Masking of Inflammation and Fever The
pharmacological activity of MOBIC in reducing fever and inflammation
may diminish the utility of these diagnostic signs in detecting
complications of presumed noninfectious, painful conditions.
5.12 Hematological Effects Anemia
may occur in patients receiving NSAIDs, including MOBIC. This may be
due to fluid retention, occult or gross GI blood loss, or an
incompletely described effect upon erythropoiesis. Patients on
long-term treatment with NSAIDs, including MOBIC, should have their
hemoglobin or hematocrit checked if they exhibit any signs or symptoms
of anemia. NSAIDs inhibit platelet aggregation and have been
shown to prolong bleeding time in some patients. Unlike aspirin, their
effect on platelet function is quantitatively less, of shorter
duration, and reversible. Carefully monitor patients treated with MOBIC
who may be adversely affected by alterations in platelet function, such
as those with coagulation disorders or patients receiving
anticoagulants.
5.13 Use in Patients with Pre-existing Asthma Patients
with asthma may have aspirin-sensitive asthma. The use of aspirin in
patients with aspirin-sensitive asthma has been associated with severe
bronchospasm, which can be fatal. Since cross reactivity, including
bronchospasm, between aspirin and other NSAIDs has been reported in
such aspirin-sensitive patients, MOBIC should not be administered to
patients with this form of aspirin sensitivity and should be used with
caution in patients with pre-existing asthma.
5.14 Monitoring Because serious GI tract ulcerations and bleeding can occur without warning symptoms, physicians should monitor for signs or symptoms of GI bleeding. Patients on long-term treatment with NSAIDs should have their CBC and a chemistry profile checked periodically. If clinical signs and symptoms consistent with liver or renal disease develop, systemic manifestations occur (e.g., eosinophilia, rash, etc.) or if abnormal liver tests persist or worsen, MOBIC should be discontinued.
6.1 Clinical Trials Experience
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The following serious adverse reactions are discussed elsewhere in the labeling: Cardiovascular thrombotic events [see Boxed Warning and Warnings and Precautions (5.1)] Gastrointestinal effects – risk of GI ulceration, bleeding, and perforation [see Boxed Warning and Warnings and Precautions (5.2)] Hepatic effects [see Warnings and Precautions (5.3)] Hypertension [see Warnings and Precautions (5.4)] Congestive heart failure and edema [see Warnings and Precautions (5.5)] Renal effects [see Warnings and Precautions (5.6)] Anaphylactoid reactions [see Warnings and Precautions (5.7)] Adverse skin reactions [see Warnings and Precautions (5.8)] 6.1 Clinical Trials Experience Adults Osteoarthritis and Rheumatoid Arthritis The MOBIC Phase 2/3 clinical trial database includes 10,122 OA patients and 1012 RA patients treated with MOBIC 7.5 mg/day, 3505 OA patients and 1351 RA patients treated with MOBIC 15 mg/day. MOBIC at these doses was administered to 661 patients for at least 6 months and to 312 patients for at least one year. Approximately 10,500 of these patients were treated in ten placebo- and/or active-controlled osteoarthritis trials and 2363 of these patients were treated in ten placebo- and/or active-controlled rheumatoid arthritis trials. Gastrointestinal (GI) adverse events were the most frequently reported adverse events in all treatment groups across MOBIC trials. A 12-week multicenter, double-blind, randomized trial was conducted in patients with osteoarthritis of the knee or hip to compare the efficacy and safety of MOBIC with placebo and with an active control. Two 12-week multicenter, double-blind, randomized trials were conducted in patients with rheumatoid arthritis to compare the efficacy and safety of MOBIC with placebo. Table 1a depicts adverse events that occurred in greater than or equal to 2% of the MOBIC treatment groups in a 12-week placebo- and active-controlled osteoarthritis trial. Table 1b depicts adverse events that occurred in greater than or equal to 2% of the MOBIC treatment groups in two 12-week placebo-controlled rheumatoid arthritis trials.
|
| Placebo | MOBIC 7.5 mg daily | MOBIC 15 mg daily | Diclofenac 100 mg daily |
| No. of Patients | 157 | 154 | 156 | 153 |
| Gastrointestinal | 17.2 | 20.1 | 17.3 | 28.1 |
| Abdominal pain | 2.5 | 1.9 | 2.6 | 1.3 |
| Diarrhea | 3.8 | 7.8 | 3.2 | 9.2 |
| Dyspepsia | 4.5 | 4.5 | 4.5 | 6.5 |
| Flatulence | 4.5 | 3.2 | 3.2 | 3.9 |
| Nausea | 3.2 | 3.9 | 3.8 | 7.2 |
| Body as a Whole |
|
|
|
|
| Accident household | 1.9 | 4.5 | 3.2 | 2.6 |
| Edema1 | 2.5 | 1.9 | 4.5 | 3.3 |
| Fall | 0.6 | 2.6 | 0.0 | 1.3 |
| Influenza-like symptoms | 5.1 | 4.5 | 5.8 | 2.6 |
| Central and Peripheral Nervous System |
|
|
|
|
| Dizziness | 3.2 | 2.6 | 3.8 | 2.0 |
| Headache | 10.2 | 7.8 | 8.3 | 5.9 |
| Respiratory |
|
|
|
|
| Pharyngitis | 1.3 | 0.6 | 3.2 | 1.3 |
| Upper respiratory tract infection | 1.9 | 3.2 | 1.9 | 3.3 |
| Skin |
|
|
|
|
| Rash2 | 2.5 | 2.6 | 0.6 | 2.0 |
|
| Placebo | MOBIC 7.5 mg daily | MOBIC 15 mg daily |
| No. of Patients | 469 | 481 | 477 |
| Gastrointestinal Disorders | 14.1 | 18.9 | 16.8 |
| Abdominal pain NOS2 | 0.6 | 2.9 | 2.3 |
| Dyspeptic signs and symptoms1 | 3.8 | 5.8 | 4.0 |
| Nausea2 | 2.6 | 3.3 | 3.8 |
| General Disorders and Administration Site Conditions |
|
|
|
| Influenza-like illness2 | 2.1 | 2.9 | 2.3 |
| Infection and Infestations |
|
|
|
| Upper respiratory tract infections-pathogen class unspecified1 | 4.1 | 7.0 | 6.5 |
| Musculoskeletal and Connective Tissue Disorders |
|
|
|
| Joint related signs and symptoms1 | 1.9 | 1.5 | 2.3 |
| Nervous System Disorders |
|
|
|
| Headaches NOS2 | 6.4 | 6.4 | 5.5 |
| Skin and Subcutaneous Tissue Disorders |
|
|
|
| Rash NOS2 | 1.7 | 1.0 | 2.1 |
|
| 4 to 6 Weeks Controlled Trials | 4 to 6 Weeks Controlled Trials | 6 Month Controlled Trials | 6 Month Controlled Trials |
|
| MOBIC 7.5 mg daily | MOBIC 15 mg daily | MOBIC 7.5 mg daily | MOBIC 15 mg daily |
| No. of Patients | 8955 | 256 | 169 | 306 |
| Gastrointestinal | 11.8 | 18.0 | 26.6 | 24.2 |
| Abdominal pain | 2.7 | 2.3 | 4.7 | 2.9 |
| Constipation | 0.8 | 1.2 | 1.8 | 2.6 |
| Diarrhea | 1.9 | 2.7 | 5.9 | 2.6 |
| Dyspepsia | 3.8 | 7.4 | 8.9 | 9.5 |
| Flatulence | 0.5 | 0.4 | 3.0 | 2.6 |
| Nausea | 2.4 | 4.7 | 4.7 | 7.2 |
| Vomiting | 0.6 | 0.8 | 1.8 | 2.6 |
| Body as a Whole |
|
|
|
|
| Accident household | 0.0 | 0.0 | 0.6 | 2.9 |
| Edema1 | 0.6 | 2.0 | 2.4 | 1.6 |
| Pain | 0.9 | 2.0 | 3.6 | 5.2 |
| Central and Peripheral Nervous System |
|
|
|
|
| Dizziness | 1.1 | 1.6 | 2.4 | 2.6 |
| Headache | 2.4 | 2.7 | 3.6 | 2.6 |
| Hematologic |
|
|
|
|
| Anemia | 0.1 | 0.0 | 4.1 | 2.9 |
| Musculoskeletal |
|
|
|
|
| Arthralgia | 0.5 | 0.0 | 5.3 | 1.3 |
| Back pain | 0.5 | 0.4 | 3.0 | 0.7 |
| Psychiatric |
|
|
|
|
| Insomnia | 0.4 | 0.0 | 3.6 | 1.6 |
| Respiratory |
|
|
|
|
| Coughing | 0.2 | 0.8 | 2.4 | 1.0 |
| Upper respiratory tract infection | 0.2 | 0.0 | 8.3 | 7.5 |
| Skin |
|
|
|
|
| Pruritus | 0.4 | 1.2 | 2.4 | 0.0 |
| Rash2 | 0.3 | 1.2 | 3.0 | 1.3 |
| Urinary |
|
|
|
|
| Micturition frequency | 0.1 | 0.4 | 2.4 | 1.3 |
| Urinary tract infection | 0.3 | 0.4 | 4.7 | 6.9 |
| Body as a Whole | allergic reaction, face edema, fatigue, fever, hot flushes, malaise, syncope, weight decrease, weight increase |
| Cardiovascular | angina pectoris, cardiac failure, hypertension, hypotension, myocardial infarction, vasculitis |
| Central and Peripheral Nervous System | convulsions, paresthesia, tremor, vertigo |
| Gastrointestinal | colitis, dry mouth, duodenal ulcer, eructation, esophagitis, gastric ulcer, gastritis, gastroesophageal reflux, gastrointestinal hemorrhage, hematemesis, hemorrhagic duodenal ulcer, hemorrhagic gastric ulcer, intestinal perforation, melena, pancreatitis, perforated duodenal ulcer, perforated gastric ulcer, stomatitis ulcerative |
| Heart Rate and Rhythm | arrhythmia, palpitation, tachycardia |
| Hematologic | leukopenia, purpura, thrombocytopenia |
| Liver and Biliary System | ALT increased, AST increased, bilirubinemia, GGT increased, hepatitis |
| Metabolic a nd Nutritional | dehydration |
| Psychiatric | abnormal dreaming, anxiety, appetite increased, confusion, depression, nervousness, somnolence |
| Respiratory | asthma, bronchospasm, dyspnea |
| Skin and Appendages | alopecia, angioedema, bullous eruption, photosensitivity reaction, pruritus, sweating increased, urticaria |
| Special Senses | abnormal vision, conjunctivitis, taste perversion, tinnitus |
| Urinary System | albuminuria, BUN increased, creatinine increased, hematuria, renal failure |
7.1 ACE-inhibitors 7.2 Aspirin 7.4 Lithium 7.5 Methotrexate 7.7 Warfarin
7 DRUG INTERACTIONS See also Clinical Pharmacology ( 12.3).
7.1 ACE-inhibitors NSAIDs
may diminish the antihypertensive effect of ACE-inhibitors. This
interaction should be given consideration in patients taking MOBIC concomitantly with ACE-inhibitors.
7.2 Aspirin When MOBIC is administered with aspirin (1000 mg three times daily) to healthy volunteers, an increase in the AUC (10%) and Cmax (24%) of meloxicam was noted. The clinical significance of this interaction is not known; however, as with other NSAIDs concomitant administration of meloxicam and aspirin is not generally recommended because of the potential for increased adverse effects. Concomitant administration of low-dose aspirin with MOBIC may result in an increased rate of GI ulceration or other complications, compared to use of MOBIC alone. MOBIC is not a substitute for aspirin for cardiovascular prophylaxis.
7.3 Diuretics Clinical studies, as well as post marketing observations, have shown that NSAIDs can reduce the natriuretic effect of furosemide and
thiazides in some patients. This response has been attributed to
inhibition of renal prostaglandin synthesis. However, studies with
furosemide agents and meloxicam have not demonstrated a reduction in
natriuretic effect. Furosemide single and multiple dose pharmacodynamics and pharmacokinetics are not affected by multiple doses of meloxicam. Nevertheless, during concomitant therapy with
MOBIC, patients should be observed closely for signs of renal failure
[see Warnings and Precautions (5.6)], as well as to ensure diuretic efficacy.
7.4 Lithium In
a study conducted in healthy subjects, mean pre-dose lithium
concentration and AUC were increased by 21% in subjects receiving lithium doses ranging from 804 to 1072 mg twice daily with meloxicam 15 mg every day as compared to subjects receiving lithium alone.
These effects have been attributed to inhibition of renal prostaglandin
synthesis by MOBIC. Closely monitor patients on lithium treatment for signs of lithium toxicity when MOBIC is introduced, adjusted, or withdrawn.
7.5 Methotrexate NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. Therefore, NSAIDs may reduce the elimination of methotrexate, thereby enhancing the toxicity of methotrexate. Use caution when MOBIC is administered concomitantly with methotrexate [see Clinical Pharmacology (12.3)].
7.6 Cyclosporine MOBIC, like other NSAIDs, may affect renal prostaglandins, thereby altering the renal toxicity of certain drugs. Therefore, concomitant therapy with MOBIC may increase cyclosporine's nephrotoxicity. Use caution when MOBIC is administered concomitantly with cyclosporine.
7.7 Warfarin The effects of warfarin and NSAIDs on GI bleeding are synergistic, such that users of both drugs together have a risk of serious GI bleeding higher than users of either drug alone. Monitor anticoagulant activity, particularly in the first few days after initiating or changing MOBIC therapy in patients receiving warfarin or similar agents, since these patients are at an increased risk of bleeding than with the use of either drug alone. Use caution when administering MOBIC with warfarin since patients on warfarin may experience changes in INR and an increased risk of bleeding complications when a new medication is introduced [see Clinical Pharmacology (12.3)].
8.1 Pregnancy 8.7 Renal Impairment
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy Pregnancy Category C; Category D starting 30 weeks gestation There are no adequate and well-controlled studies in pregnant women. Meloxicam crosses the placental barrier. Prior to 30 weeks gestation, use MOBIC during pregnancy only if the potential benefit justifies the potential risk to the fetus. Starting at 30 weeks gestation, avoid MOBIC and other NSAIDs, in pregnant women as premature closure of the ductus arteriosus in the fetus may occur. If this drug is used during this time period in pregnancy, inform the patient of the potential hazard to a fetus [see Warnings and Precautions (5.9) and Patient Counseling Information (17.8)]. Teratogenic Effects Meloxicam was not teratogenic when administered to pregnant rats during fetal organogenesis at oral doses up to 4 mg/kg/day (2.6-fold greater than the maximum recommended human daily dose [MRHD] based on body surface area [BSA] comparison). Administration of meloxicam to pregnant rabbits throughout embryogenesis produced an increased incidence of septal defects of the heart at an oral dose of 60 mg/kg/day. The no effect level was 20 mg/kg/day (26-fold greater than the MRHD based on BSA conversion) . Nonteratogenic Effects In rats and rabbits, embryolethality occurred at oral meloxicam doses of 1 mg/kg/day and 5 mg/kg/day, respectively (0.65- and 6.5- fold greater, respectively, than the MRHD based on BSA comparison) when administered throughout organogenesis.
8.2 Labor and Delivery The effects of MOBIC on labor and delivery of pregnant women are unknown. Oral administration of meloxicam to pregnant rats during late gestation through lactation increased the incidence of dystocia, delayed parturition, and decreased offspring survival at meloxicam doses of 0.125 mg/kg/day or greater (at least 12.5 times lower than the maximum recommended human daily dose based on body surface area comparison).
8.3 Nursing Mothers
8.3 Nursing Mothers It is not known whether this drug is excreted in human milk; however, meloxicam was excreted in the milk of lactating rats at concentrations higher than those in plasma. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from MOBIC, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.8.4 Pediatric Use The safety and effectiveness of meloxicam in pediatric JRA patients from 2 to 17 years of age has been evaluated in three clinical trials [see Dosage and Administration (2.3), Adverse Reactions (6.1), and Clinical Studies (14.2)].
8.6 Hepatic Impairment 8.7 Renal Impairment
8.5 Geriatric Use As with any NSAID, caution should be exercised in treating the elderly (65 years and older). Of the total number of subjects in clinical studies, 5157 were age 65 and over (4044 in OA studies and 1113 in RA studies). No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.8.6 Hepatic Impairment No dose adjustment is necessary in patients with mild to moderate hepatic impairment. Patients with severe hepatic impairment have not been adequately studied. Since meloxicam is significantly metabolized in the liver; the use of meloxicam in these patients should be done with caution [see Warnings and Precautions (5.3) and Clinical Pharmacology (12.3)].
8.7 Renal Impairment No dose adjustment is necessary in patients with mild to moderate renal impairment. Patients with severe renal impairment have not been studied. The use of MOBIC in subjects with severe renal impairment is not recommended. Following a single dose of meloxicam, the free Cmax plasma concentrations were higher in patients with renal failure on chronic hemodialysis (1% free fraction) in comparison to healthy volunteers (0.3% free fraction). Therefore, it is recommended that meloxicam dosage in this population not exceed 7.5 mg per day. Hemodialysis did not lower the total drug concentration in plasma; therefore, additional doses are not necessary after hemodialysis. Meloxicam is not dialyzable [see Dosage and Administration (2.1), Warnings and Precautions (5.6), and Clinical Pharmacology (12.3)].
10 OVERDOSAGE There is limited experience with meloxicam overdose. Four cases have taken 6 to 11 times the highest recommended dose; all recovered. Cholestyramine is known to accelerate the clearance of meloxicam. Symptoms following acute NSAID overdose include lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Gastrointestinal bleeding can occur. Severe poisoning may result in hypertension, acute renal failure, hepatic dysfunction, respiratory depression, coma, convulsions, cardiovascular collapse, and cardiac arrest. Anaphylactoid reactions have been reported with therapeutic ingestion of NSAIDs, and may occur following an overdose. Patients should be managed with symptomatic and supportive care following an NSAID overdose. Administration of activated charcoal is recommended for patients who present 1 to 2 hours after overdose. For substantial overdose or severely symptomatic patients, activated charcoal may be administered repeatedly. Accelerated removal of meloxicam by 4 gm oral doses of cholestyramine given three times a day was demonstrated in a clinical trial. Administration of cholestyramine may be useful following an overdose. Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding. For additional information about overdose treatment, call a poison control center (1-800-222-1222).
11 DESCRIPTION Meloxicam, an oxicam derivative, is a member of the enolic acid group of nonsteroidal anti-inflammatory drugs (NSAIDs). Each pastel yellow MOBIC tablet contains 7.5 mg or 15 mg meloxicam for oral administration. Each bottle of MOBIC oral suspension contains 7.5 mg meloxicam per 5 mL. Meloxicam is chemically designated as 4-hydroxy-2-methyl-N-(5-methyl-2-thiazolyl)-2H-1,2- benzothiazine-3-carboxamide-1,1-dioxide. The molecular weight is 351.4. Its empirical formula is C14H13N3O4S2 and it has the following structural formula:
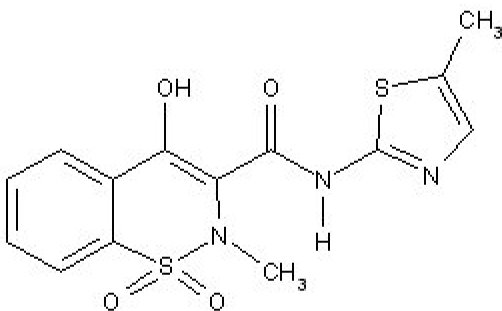
Meloxicam is a pastel yellow solid, practically insoluble in water, with higher solubility observed in strong acids and bases. It is very slightly soluble in methanol. Meloxicam has an apparent partition coefficient (log P)app = 0.1 in n-octanol/buffer pH 7.4. Meloxicam has pKa values of 1.1 and 4.2. MOBIC is available as a tablet for oral administration containing 7.5 mg or 15 mg meloxicam, and as an oral suspension containing 7.5 mg meloxicam per 5 mL. The inactive ingredients in MOBIC tablets include colloidal silicon dioxide, crospovidone, lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone, and sodium citrate dihydrate. The inactive ingredients in MOBIC oral suspension include colloidal silicon dioxide, hydroxyethylcellulose, sorbitol, glycerol, xylitol, monobasic sodium phosphate (dihydrate), saccharin sodium, sodium benzoate, citric acid (monohydrate), raspberry flavor, and purified water.
12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action The mechanism of action of meloxicam, like that of other NSAIDs, may be related to prostaglandin synthetase (cyclo-oxygenase) inhibition which is involved in the initial steps of the arachidonic acid cascade, resulting in the reduced formation of prostaglandins, thromboxanes and prostacylin. It is not completely understood how reduced synthesis of these compounds results in therapeutic efficacy.
12.3 Pharmacokinetics
12.3 Pharmacokinetics Absorption The absolute bioavailability of meloxicam capsules was 89% following a single oral dose of 30 mg compared with 30 mg IV bolus injection. Following single intravenous doses, dose-proportional pharmacokinetics were shown in the range of 5 mg to 60 mg. After multiple oral doses the pharmacokinetics of meloxicam capsules were dose-proportional over the range of 7.5 mg to 15 mg. Mean Cmax was achieved within four to five hours after a 7.5 mg meloxicam tablet was taken under fasted conditions, indicating a prolonged drug absorption. With multiple dosing, steady-state concentrations were reached by Day 5. A second meloxicam concentration peak occurs around 12 to 14 hours post-dose suggesting biliary recycling.
Meloxicam oral suspension doses of 7.5 mg/5 mL and 15 mg/10 mL have been found to be bioequivalent to meloxicam 7.5 mg and 15 mg capsules, respectively. Meloxicam capsules have been shown to be bioequivalent to MOBIC tablets.
|
|
| Steady State | Steady State | Steady State | Single Dose | Single Dose |
| Pharmacokinetic Parameters (% CV) |
| Healthy male adults (Fed)2 | Elderly males (Fed)2 | Elderly females (Fed)2 | Renal failure (Fasted) | Hepatic insufficiency (Fasted) |
|
|
| 7.5 mg3 tablets | 15 mg capsules | 15 mg capsules | 15 mg capsules | 15 mg capsules |
| N |
| 18 | 5 | 8 | 12 | 12 |
| Cmax | [µg/mL] | 1.05(20) | 2.3 (59) | 3.2 (24) | 0.59 (36) | 0.84 (29) |
| tmax | [h] | 4.9 (8) | 5 (12) | 6 (27) | 4 (65) | 10 (87) |
| t1/2 | [h] | 20.1(29) | 21 (34) | 24 (34) | 18 (46) | 16 (29) |
| CL/f | [mL/min] | 8.8 (29) | 9.9 (76) | 5.1 (22) | 19 (43) | 11 (44) |
| Vz/f4 | [L] | 14.7(32) | 15 (42) | 10 (30) | 26 (44) | 14 (29) |
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis: There was no increase in tumor incidence in long-term carcinogenicity studies in rats (104 weeks) and mice (99 weeks) administered meloxicam at oral doses up to 0.8 mg/kg/day in rats and up to 8.0 mg/kg/day in mice (up to 0.5- and 2.6-fold, respectively, the maximum recommended human daily dose based on body surface area comparison). Mutagenesis: Meloxicam was not mutagenic in an Ames assay, or clastogenic in a chromosome aberration assay with human lymphocytes and an in vivo micronucleus test in mouse bone marrow. Impairment of Fertility: Meloxicam did not impair male and female fertility in rats at oral doses up to 9 mg/kg/day in males and 5 mg/ kg/day in females (up to 5.8- and 3.2-fold greater, respectively, than the maximum recommended human daily dose based on body surface area comparison).
14.1 Osteoarthritis and Rheumatoid Arthritis 14.2 Juvenile Rheumatoid Arthritis (JRA) Pauciarticular and Polyarticular Course
14 CLINICAL STUDIES
14.1 Osteoarthritis and Rheumatoid Arthritis The use of MOBIC for the treatment of the signs and symptoms of osteoarthritis of the knee and hip was evaluated in a 12-week, double-blind, controlled trial. MOBIC (3.75 mg, 7.5 mg, and 15 mg daily) was compared to placebo. The four primary endpoints were investigator’s global assessment, patient global assessment, patient pain assessment, and total WOMAC score (a self-administered questionnaire addressing pain, function, and stiffness). Patients on MOBIC 7.5 mg daily and MOBIC 15 mg daily showed significant improvement in each of these endpoints compared with placebo. The use of MOBIC for the management of signs and symptoms of osteoarthritis was evaluated in six double-blind, active-controlled trials outside the U.S. ranging from 4 weeks’ to 6 months’ duration. In these trials, the efficacy of MOBIC, in doses of 7.5 mg/day and 15 mg/day, was comparable to piroxicam 20 mg/day and diclofenac SR 100 mg/day and consistent with the efficacy seen in the U.S. trial. The use of MOBIC for the treatment of the signs and symptoms of rheumatoid arthritis was evaluated in a 12-week, double-blind, controlled multinational trial. MOBIC (7.5 mg, 15 mg, and 22.5 mg daily) was compared to placebo. The primary endpoint in this study was the ACR20 response rate, a composite measure of clinical, laboratory, and functional measures of RA response. Patients receiving MOBIC 7.5 mg and 15 mg daily showed significant improvement in the primary endpoint compared with placebo. No incremental benefit was observed with the 22.5 mg dose compared to the 15 mg dose. 14.2 Juvenile Rheumatoid Arthritis (JRA) Pauciarticular and Polyarticular Course The use of MOBIC for the treatment of the signs and symptoms of pauciarticular or polyarticular course Juvenile Rheumatoid Arthritis in patients 2 years of age and older was evaluated in two 12-week, double-blind, parallel-arm, active-controlled trials. Both studies included three arms: naproxen and two doses of meloxicam. In both studies, meloxicam dosing began at 0.125 mg/kg/day (7.5 mg maximum) or 0.25 mg/kg/day (15 mg maximum), and naproxen dosing began at 10 mg/kg/day. One study used these doses throughout the 12-week dosing period, while the other incorporated a titration after 4 weeks to doses of 0.25 mg/kg/day and 0.375 mg/ kg/day (22.5 mg maximum) of meloxicam and 15 mg/kg/day of naproxen. The efficacy analysis used the ACR Pediatric 30 responder definition, a composite of parent and investigator assessments, counts of active joints and joints with limited range of motion, and erythrocyte sedimentation rate. The proportion of responders were similar in all three groups in both studies, and no difference was observed between the meloxicam dose groups.
16 HOW SUPPLIED/STORAGE AND HANDLING MOBIC is available as a pastel yellow, round, biconvex, uncoated tablet containing meloxicam 7.5 mg or as a pastel yellow, oblong, biconvex, uncoated tablet containing meloxicam 15 mg. The 7.5 mg tablet is impressed with the Boehringer Ingelheim logo on one side, and on the other side, the letter “M”. The 15 mg tablet is impressed with the tablet code “15” on one side and the letter “M” on the other. MOBIC is also available as a yellowish green tinged viscous oral suspension containing 7.5 mg meloxicam in 5 mL. MOBIC tablets 7.5 mg: NDC 0597-0029-01; Bottles of 100 MOBIC tablets 15 mg: NDC 0597-0030-01; Bottles of 100 MOBIC oral suspension 7.5 mg/5 mL: NDC 0597-0034-01; Bottles of 100 mL
Storage Store at 25°C (77°F); excursions permitted to 15°C-30°C (59°F-86°F). Keep MOBIC tablets in a dry place. Dispense tablets in a tight container. Keep oral suspension container tightly closed. Keep this and all medications out of the reach of children.
17 PATIENT COUNSELING INFORMATION 17.8 Effects During Pregnancy
17 PATIENT COUNSELING INFORMATION See FDA-approved Medication Guide Patients should be informed of the following information before initiating therapy with an NSAID and periodically during the course of ongoing therapy. 17.1 Medication Guide Inform
patients of the availability of a Medication Guide for NSAIDs that
accompanies each prescription dispensed, and instruct them to read the Medication Guide prior to using MOBIC.
17.2 Cardiovascular Effects NSAIDs including MOBIC may cause serious CV side effects, such as MI or stroke, which may result in hospitalization and even death.
Although serious CV events can occur without warning symptoms, patients
should be alert for the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and should ask for medical advice when observing any indicative sign or symptoms. Patients should be apprised of the importance of this follow-up [see Warnings and Precautions (5.1)].
17.3 Gastrointestinal Effects NSAIDs including MOBIC, can cause GI discomfort and, rarely, serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, patients
should be alert for the signs and symptoms of ulcerations and bleeding,
and should ask for medical advice when observing any indicative sign
or symptoms including epigastric pain, dyspepsia, melena, and
hematemesis. Patients should be apprised of the importance of this follow-up [see Warnings and Precautions (5.2)].
17.4 Hepatotoxicity Inform
patients of the warning signs and symptoms of hepatotoxicity (e.g.,
nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant
tenderness, and "flu like" symptoms). If these occur, instruct patients
to stop therapy and seek immediate medical therapy [see Warnings and Precautions (5.3)].
17.5 Adverse Skin Reactions NSAIDs including MOBIC, can cause serious skin side effects such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which may result in hospitalization and even death. Although serious skin reactions may occur without
warning, patients should be alert for the signs and symptoms of skin
rash and blisters, fever, or other signs of hypersensitivity such as
itching, and should ask for medical advice when observing any
indicative signs or symptoms. Advise patients to stop the drug immediately
if they develop any type of rash and contact their physicians as soon
as possible [see Warnings and Precautions (5.8)].
17.6 Weight Gain and Edema Advise patients to promptly report signs or symptoms of unexplained weight gain or edema to their physicians [see Warnings and Precautions (5.5)].
17.7 Anaphylactoid Reactions Inform
patients of the signs of an anaphylactoid reaction (e.g., difficulty
breathing, swelling of the face or throat). Instruct patients seek immediate emergency help [see Warnings and Precautions (5.7)].
17.8 Effects During Pregnancy Starting at 30 weeks gestation, MOBIC should be avoided as premature closure of the ductus arteriosus in the fetus may occur [see Warnings and Precautions (5.9) and Use in Specific Populations (8.1)]. Please address medical inquiries to (800) 542-6257 or (800) 459-9906 TTY. Distributed by: Boehringer Ingelheim Pharmaceuticals, Inc. Ridgefield, CT 06877 USA Licensed from: Boehringer Ingelheim International GmbH ©Copyright 2010 Boehringer Ingelheim International GmbH ALL RIGHTS RESERVED 10003990/06 OT1400GD2810 090340141-7 OT1407E
Medication Guide for Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) (See the end of this Medication Guide for a list of prescription NSAID medicines.) What is the most important information I should know about medicines called Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)? NSAID medicines may increase the chance of a heart attack or stroke that can lead to death. This chance increases: - with longer use of NSAID medicines - in people who have heart disease NSAID medicines should never be used right before or after a heart surgery called a "coronary artery bypass graft (CABG)." NSAID medicines can cause ulcers and bleeding in the stomach and intestines at any time during treatment. Ulcers and bleeding: - can happen without warning symptoms - may cause death The chance of a person getting an ulcer or bleeding increases with: - taking medicines called "corticosteroids" and "anticoagulants" - longer use - smoking - drinking alcohol - older age - having poor health NSAID medicines should only be used: - exactly as prescribed - at the lowest dose possible for your treatment - for the shortest time needed What are Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)? NSAID medicines are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as: - different types of arthritis - menstrual cramps and other types of short-term pain Who should not take a Non-Steroidal Anti-Inflammatory Drug (NSAID)? Do not take an NSAID medicine: - if you had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAID medicine - for pain right before or after heart bypass surgery Tell your healthcare provider: - about all of your medical conditions. - about all of the medicines you take. NSAIDs and some other medicines can interact with each other and cause serious side effects. Keep a list of your medicines to show to your healthcare provider and pharmacist. - if you are pregnant. NSAID medicines should not be used by pregnant women late in their pregnancy. - if you are breastfeeding. Talk to your doctor. What are the possible side effects of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)? Serious side effects include: - heart attack - stroke - high blood pressure - heart failure from body swelling (fluid retention) - kidney problems including kidney failure - bleeding and ulcers in the stomach and intestine - low red blood cells (anemia) - life-threatening skin reactions - life-threatening allergic reactions - liver problems including liver failure - asthma attacks in people who have asthma Other side effects include: - stomach pain - constipation - diarrhea - gas - heartburn - nausea - vomiting - dizziness Get emergency help right away if you have any of the following symptoms: - shortness of breath or trouble breathing - chest pain - weakness in one part or side of your body - slurred speech - swelling of the face or throat Stop your NSAID medicine and call your healthcare provider right away if you have any of the following symptoms: - nausea - more tired or weaker than usual - itching - your skin or eyes look yellow - stomach pain - flu-like symptoms - vomit blood - there is blood in your bowel movement or it is black and sticky like tar - unusual weight gain - skin rash or blisters with fever - swelling of the arms and legs, hands and feet These are not all the side effects with NSAID medicines. Talk to your healthcare provider or pharmacist for more information about NSAID medicines. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. Other information about Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) - Aspirin is an NSAID medicine but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines. - Some of these NSAID medicines are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
| Generic Name | Tradename |
| Celecoxib | Celebrex |
| Diclofenac | Cataflam, Voltaren, Arthrotec (combined with misoprostol) |
| Diflunisal | Dolobid |
| Etodolac | Lodine, Lodine XL |
| Fenoprofen | Nalfon, Nalfon 200 |
| Flurbiprofen | Ansaid |
| Ibuprofen | Motrin, Tab-Profen, Vicoprofen* (combined with hydrocodone), Combunox (combined with oxycodone) |
| Indomethacin | Indocin, Indocin SR, Indo-Lemmon, Indomethagan |
| Ketoprofen | Oruvail |
| Ketorolac | Toradol |
| Mefenamic Acid | Ponstel |
| Meloxicam | Mobic |
| Nabumetone | Relafen |
| Naproxen | Naprosyn, Anaprox, Anaprox DS, EC-Naprosyn, Naprelan, Naprapac (copackaged with lansoprazole) |
| Oxaprozin | Daypro |
| Piroxicam | Feldene |
| Sulindac | Clinoril |
| Tolmetin | Tolectin, Tolectin DS, Tolectin 600 |
Vicoprofen contains the same dose of ibuprofen as over-the-counter (OTC) NSAIDs, and is usually used for less than 10 days to treat pain. The OTC NSAID label warns that long term continuous use may increase the risk of heart attack or stroke. This Medication Guide has been approved by the U.S. Food and Drug Administration.
NDC 0597-0029-01 ATTENTION DISPENSER: Disperse with separately provided Medication Guide. Mobic (meloxicam) tablets 7.5 mg 100 tablets Dosage: Read accompanying prescribing information. RX only Boehringer Ingelheim EXP. LOT
Store at 25 degree C (77 degree F); excursions permitted to 15 degree - 30 degree C (59 degree - 86 degree F.) Dispense in a tight container.Keep in a dry place. Keep out of reach of children. Mfd. by: Boehringer Ingelheim (BI) Promeco, S.A de C.V. Mexico City,Mexico Lic. from: BI Int'l GmbH Mkd. by: BI Pharmaceuticals, Inc. Ridgefield, CT 06877 USA C2009 BI Int'l GmbH L1411A
Trepadone (U.S. patent pending) capsules by oral administration. A specially formulated Medical Food product, consisting of a proprietary blend of amino acids, glucosamine, chondroitin sulfate, fish oil, and polyphenol ingredients in specific proportions, for the dietary management of the metabolic processes associated with pain disorders and inflammatory conditions. (PD) (IC), particularly diseases associated with joint pain. Must be administered under physician supervision.
Medical Foods
Medical Food products are often used in hospitals (e.g., for burn victims or kidney dialysis patients) and outside of a hospital setting under a physician’s care for the dietary management of diseases in patients with particular medical or metabolic needs due to their disease or condition. Congress defined "Medical Food" in the Orphan Drug Act and Amendments of 1988 as "a food which is formulated to be consumed or administered enterally [or orally] under the supervision of a physician and which is intended for the specific dietary management of a disease or condition for which distinctive nutritional requirements, based on recognized scientific principles, are established by medical evaluation." Medical Foods are complex formulated products, requiring sophisticated and exacting technology. Trepadone has been developed, manufactured, and labeled in accordance with both the statutory and the FDA regulatory definition of a Medical Food. Trepadone must be used while the patient is under the ongoing care of a physician.
PAIN DISORDERS (PD) INFLAMMATORY CONDITIONS (IC)
PD and IC as a Metabolic Deficiency Disease
A critical component of the definition of a Medical Food is the requirement for a distinctive nutritional deficiency. FDA scientists have proposed a physiologic definition of a distinctive nutritional deficiency as follows: “the dietary management of patients with specific diseases requires, in some instances, the ability to meet nutritional requirements that differ substantially from the needs of healthy persons. For example, in establishing the recommended dietary allowances for general, healthy population, the Food and Nutrition Board of the Institute of Medicine National Academy of Sciences, recognized that different or distinctive physiologic requirements may exist for certain persons with "special nutritional needs arising from metabolic disorders, chronic diseases, injuries, premature birth, other medical conditions and drug therapies. Thus, the distinctive nutritional needs associated with a disease reflects the total amount needed by a healthy person to support life or maintain homeostasis, adjusted for the distinctive changes in the nutritional needs of the patient as a result of the effects of the disease process on absorption, metabolism and excretion.” It was also proposed that in patients with certain disease states who respond to nutritional therapies, a physiologic deficiency of the nutrient is assumed to exist. For example, if a patient with pain disorders responds to a tryptophan formulation by decreasing perceived pain, a deficiency of tryptophan is assumed to exist.
Patients with pain disorders and inflammatory conditions are known to have nutritional deficiencies of tryptophan, choline, arginine, GABA, flavonoids, and certain antioxidants. Patients with pain disorders and inflammatory conditions frequently exhibit reduced plasma levels of tryptophan and GABA and have been shown to respond to oral administration of GABA, arginine, tryptophan, or a 5-hydoxytryptophan formulation. Research has shown that tryptophan, arginine or GABA reduced diets result in a fall of circulating tryptophan, arginine, and/or GABA. Patients with pain disorders frequently exhibit activation of the degradation pathways that increases the turnover of GABA, arginine and/or tryptophan leading to a reduced level of production of serotonin, GABA or nitric oxide for a given precursor blood level. Patients with pain disorders and inflammatory conditions are known to have nutritional deficiencies of glucosamine and chondroitin sulfate. Patients with pain disorders and inflammatory conditions frequently exhibit reduced plasma levels of glucosamine and chondroitin sulfate and have been shown to respond to oral administration of glucosamine and chondroitin sulfate formulation. Patients with pain disorders and inflammatory conditions are known to have nutritional deficiencies of prostaglandin precursors such as omega-3 free fatty acids. Patients with pain disorders and inflammatory conditions frequently exhibit reduced plasma levels of prostaglandin precursors and have been shown to respond to oral administration of prostaglandin precursors, such as the Omega-3 free fatty acids, particularly in the form of fish oils. Research has also shown that a genetic predisposition to accelerated degradation of prostaglandins can lead to increased precursor requirements in certain patients with pain disorders and inflammatory conditions.
Choline is required to fully potentiate acetylcholine synthesis by brain neurons. A deficiency of choline leads to reduced acetylcholine production by the neurons. Flavonoids potentiate the production of acetylcholine by the neurons thereby reducing pain. Diets deficient in flavonoid rich foods and choline result in inadequate flavonoid concentrations, impeding acetylcholine production in certain patients with pain disorders and/or inflammatory conditions. Acetylcholine in pre-synaptic ganglia is necessary for the production of serotonin and nitric oxide in post-synaptic ganglia. Provision of tryptophan, arginine, GABA, choline and flavonoids with antioxidants, in specific proportions can restore the production of beneficial serotonin, nitric oxide, and acetylcholine, thereby reducing the perception of pain and reducing inflammation. L-Histidine is known to produce brain histamine that stimulates production of ACTH.
PRODUCT DESCRIPTION
Primary Ingredients
Trepadone consists of a proprietary blend of amino acids, prostaglandin precursors in the form of omega-3 free fatty acids, glucosamine, chondroitin sulfate, cocoa, caffeine, cinnamon, and flavonoids in specific proportions. These ingredients fall into the category of Generally Regarded as Safe” (GRAS) as defined by the Food and Drug Administration (FDA) (Sections 201(s) and 409 of the Federal Food, Drug, and Cosmetic Act). A GRAS substance is distinguished from a food additive on the basis of the common knowledge about the safety of the substance for its intended use. The standard for an ingredient to achieve GRAS status requires not only technical demonstration of non-toxicity and safety, but also general recognition of safety through widespread usage and agreement of that safety by experts in the field. Many ingredients have been determined by the U.S. Food and Drug Administration (FDA) to be GRAS, and are listed as such by regulation, in Volume 21 Code of Federal Regulations (CFR) Sections 182, 184, and 186.
Amino Acids
Amino Acids are the building blocks of protein. All amino acids are GRAS listed as they have been ingested by humans for many thousands of years. The doses of the amino acids in Trepadone are equivalent to those found in the usual human diet. Patients with pain disorders may require an increased amount of certain amino acids that cannot be obtained from normal diet alone. Tryptophan, for example, is an obligatory amino acid. The body cannot make tryptophan and must obtain tryptophan from the diet. Tryptophan is needed to produce serotonin. Serotonin is required to reduce pain. Patients with pain disorders and inflammatory conditions have altered serotonin metabolism. Some patients with pain disorders and inflammatory conditions have a resistance to the use of tryptophan that is similar to the mechanism found in insulin resistance. Patients with pain disorders and inflammatory conditions cannot acquire sufficient tryptophan from the diet to alter the perception of pain and the inflammatory process without ingesting a prohibitively large amount of calories, particularly calories from protein.
Chondroitin Sulfate and Glucosamine
Chondroitin sulfate and glucosamine are the building blocks of joint cartilage and are GRAS listed as they have been ingested by humans for thousands of years. The doses of the chondroitin sulfate and glucosamine in Trepadone are equivalent to those found in the usual human diet. Patients with pain disorders, particularly of the joints, may require an increased amount of chondroitin sulfate and glucosamine that cannot be obtained from normal diet alone. Patients with pain disorders and inflammatory conditions, particularly of the joints have altered chondroitin sulfate and glucosamine metabolism. Some patients with pain disorders and inflammatory conditions of the joints have a resistance to the use of chondroitin sulfate and glucosamine. Patients with pain disorders and inflammatory conditions of the joints cannot acquire sufficient chondroitin sulfate and glucosamine from the diet to alter the pain and the inflammatory process of the joint without ingesting a prohibitively large amount of calories, particularly calories from protein.
Omega-3 Free Fatty Acids in the Form of Fish Oil
Omega-3 Free Fatty Acids in the Form of Fish Oil are the building blocks of prostaglandin precursors that control the inflammatory process. Omega-3 Free Fatty Acids in the Form of Fish Oil are GRAS listed as they have been ingested by humans for thousands of years. The doses of the Omega-3 Free Fatty Acids in the Form of Fish Oil in Trepadone are equivalent to those found in the usual human diet. Patients with pain disorders, particularly of the joints, may require an increased amount of Omega-3 Free Fatty Acids in the Form of Fish Oil that cannot be obtained from normal diet alone. Patients with pain disorders and inflammatory conditions, particularly of the joints have altered prostaglandin metabolism. Some patients with pain disorders and inflammatory conditions exhibit a resistance to the use of Omega-3 Free Fatty Acids in the Form of Fish Oil. Patients with pain disorders and inflammatory conditions of the joints cannot acquire sufficient Omega-3 Free Fatty Acids in the Form of Fish Oil from the diet to alter the pain and the inflammatory process of the joint without ingesting a prohibitively large amount of calories.
Flavonoids
Flavonoids are a group of phytochemical compounds found in all vascular plants including fruits and vegetables. They are a part of a larger class of compounds known as polyphenols. Many of the therapeutic or health benefits of colored fruits and vegetables, cocoa, red wine, and green tea are directly related to their flavonoid content. The specially formulated flavonoids found in Trepadone cannot be obtained from conventional foods in the necessary proportions to elicit a therapeutic response.
Other Ingredients
Trepadone contains the following inactive or other ingredients, as fillers, excipients, and colorings: magnesium stearate, microcrystalline cellulose, Maltodextrin NF, gelatin (as the capsule material).
Physical Description
Trepadone is a yellow to light brown powder. Trepadone contains L-Glutamine, L-Arginine, L-Histidine, and L-Serine, 5-Hydroxytryptophan as Griffonia Seed Extract, GABA, Choline Bitartrate, Cinnamon, Cocoa, Hydrolyzed Whey Protein, and Grape Seed Extract.
CLINICAL PHARMACOLOGY
Mechanism of Action
Trepadone acts by restoring and maintaining the balance of the neurotransmitters; GABA, nitric oxide, serotonin, and acetylcholine that are associated with pain disorders and inflammatory conditions. Trepadone stimulates the production ACTH to reduce inflammation. Trepadone stimulates the production prostaglandins to reduce inflammation. Trepadone stimulates the production joint cartilage.
Metabolism
The amino acids in Trepadone are primarily absorbed by the stomach and small intestines. All cells metabolize the amino acids in Trepadone. Circulating tryptophan, arginine and choline blood levels determine the production of serotonin, nitric oxide, and acetylcholine. The Omega-3 free fatty acids in Trepadone are primarily absorbed by the stomach and small intestines. Inflammatory cells metabolize the free fatty acids in Trepadone.
Excretion
Trepadone is not an inhibitor of cytochrome P450 1A2, 2C9, 2C19, 2D6, or 3A4. These isoenzymes are principally responsible for 95% of all detoxification of drugs, with CYP3A4 being responsible for detoxification of roughly 50% of drugs. Amino acids do not appear to have an effect on drug metabolizing enzymes. Free fatty acids, glucosamine, and chondroitin sulfate do not appear to have an effect on drug metabolizing enzymes
INDICATIONS FOR USE
Trepadone is intended for the clinical dietary management of the metabolic processes of pain disorders and inflammatory conditions, particularly those associated with joint pain.
CLINICAL EXPERIENCE
Administration of Trepadone has demonstrated significant reduction in symptoms of pain and inflammation in patients with acute and chronic pain when used for the dietary management of the metabolic processes associated with pain disorders and inflammatory conditions. Administration of Trepadone results in the induction and maintenance of pain relief in patients with pain disorders and inflammatory conditions associated with joint pain.
PRECAUTIONS AND CONTRAINDICATIONS
Trepadone is contraindicated in an extremely small number of patients with hypersensitivity to any of the nutritional components of Trepadone.
ADVERSE REACTIONS
Oral supplementation with L-tryptophan, L-arginine or choline at high doses up to 15 grams daily is generally well tolerated. The most common adverse reactions of higher doses — from 15 to 30 grams daily — are nausea, abdominal cramps, and diarrhea. Some patients may experience these symptoms at lower doses. The total combined amount of amino acids in each Trepadone capsule does not exceed 400 mg. The doses of chondroitin sulfate, glucosamine, and omega-3 free fatty acids are well tolerated. Large doses of free fatty acids can be associated with bleeding disorders.
DRUG INTERACTIONS
Trepadone does not directly influence the pharmacokinetics of prescription drugs. Clinical experience has shown that administration of Trepadone may allow for lowering the dose of coadministered drugs under physician supervision.
OVERDOSE
There is a negligible risk of overdose with Trepadone as the total dosage of amino acids in a one month supply (90 capsules) is less than 36 grams. Overdose symptoms may include diarrhea, weakness, and nausea. There is a negligible risk of overdose with Trepadone as the total dosage of glucosamine, chondroitin sulfate, and omega-3 free fatty acids in a one month supply (90 capsules) is less than 10 grams. Overdose symptoms may include diarrhea, weakness, and nausea.
POST-MARKETING SURVEILLANCE
Post-marketing surveillance has shown no serious adverse reactions. Reported cases of mild rash and itching may have been associated with allergies to Trepadone flavonoid ingredients, including cinnamon, cocoa, and chocolate. These reactions were transient in nature and subsided within 24 hours.
DOSAGE AND ADMINISTRATION
Recommended Administration
For the dietary management of the metabolic processes associated with pain disorders and inflammatory conditions, particularly joint pain. Take (2) capsules up to four times per day times daily or as directed by physician. As with most amino acid formulations Trepadone should be taken without food to increase the absorption of key ingredients.
How Supplied
Trepadone is supplied in green and yellow, size 0 capsules in bottles of 90 capsules.
Physician Supervision
Trepadone is a Medical Food product available by prescription only and must be used while the patient is under ongoing physician supervision.
U.S. patents pending.
Manufactured by Arizona Nutritional Supplements, Inc. Chandler AZ 85225
Distributed by Physician Therapeutics LLC, Los Angeles, CA 90077. www.ptlcentral.com
© Copyright 2003-2006, Physician Therapeutics LLC, all rights reserved
NDC # 68405-1003-02
NDC: 68405-1016-03
Storage
Store at room temperature, 59-86oF (15-30oC) Protect from light and moisture. Trepadone is supplied to physicians in a recyclable plastic bottle with a child-resistant cap.
PHYSICIAN THERAPEUTICS TREPADONE Medical Food Rx only 90 Capsules Directions for use: Must be administered under medical supervision. For adults only. As a Medical Food, take two (2) capsules four times daily in between meals. For the dietary management of osteoarthritis, tendonitis, and joint pain. Contains no added sugar, starch, wheat, yeast, preservatives, or flavor. Storage: Keep tightly closed in a cool dry place 8-32 Degree Centigrade (45-90 Degree F), relative humidity, below 50%. Warning: Keep this product out of the reach of children. NDC#68405-1016-03 Ingredients: Each serving (per 2 capsules) contains: Proprietary Amino Acid Blend L-Histadine, GABA, Hydrolyzed Whey Protein Glucosamine Omega - 3 FFA from Tuna Oil Chondroitin Sulfate Grape Seed Extract Cocoa (6% Theobromine) (fruit) Other indgredients: Gelatin. tricalcium phosphate, magnesium stearate, silicon dioxide, microcrystalline cellulose, FD and C yello #5, FD and C yellow #6, chlorophyllin copper complex, titanium dioxide. Distributed by: Physician Therapeutics LLC, Los Angeles, CA 90077 www.ptlcentral.com Patent Pending
For the Dietary Management of Joint Disorder.
Two capsules up to four times daily or as directed by physician. See product label and insert.
Trepadone Medical Food
PHYSICIAN THERAPEUTICS
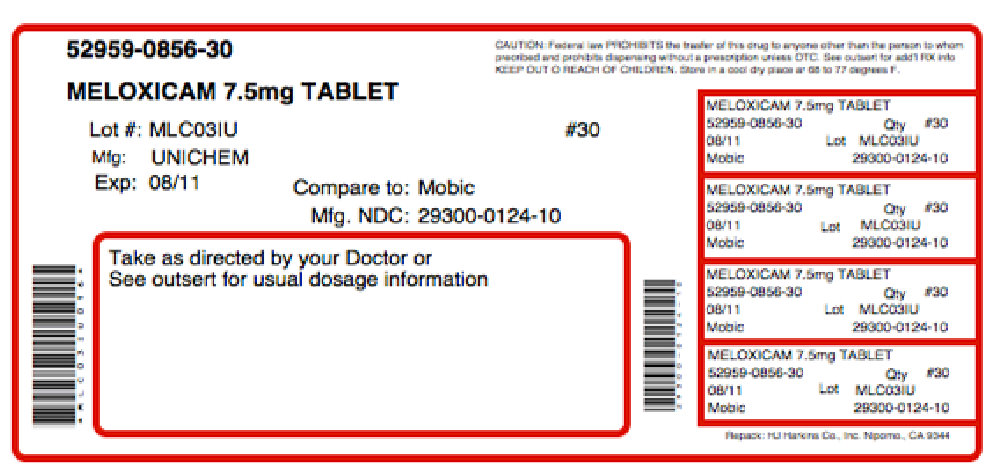
Trepadone Meloxicam 7.5 mg
A Convenience Packed Medical Food and Drug
Trepoxicam - 7.5
PHYSICIAN THERAPEUTICS
Trepadone 90 Capsules
Meloxicam 7.5 mg 30 Tablets
No Refills Without Physician Authorization
Rx only
NDC# 68405-036-36 of this co-pack
As prescribed by physician. See product label and product information insert.
Meloxicam 7.5 mg
Rx Drug
Manufactured and Distributed by Physician Therapeutics, A Division of Targeted Medical Pharma Inc. Los Angeles, CA 90077 www.ptlcentral.com
B-NDC# 68405-8036-36