INDIACTIONS AND USAGE
To reduce the development of drug-resistant bacteria and maintain the effectiveness of azithromycin and other antibacterial drugs, azithromycin should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Azithromycin is a macrolide antibacterial drug indicated for the treatment of patients with mild to moderate infections caused by susceptible strains of the designated microorganisms in the specific conditions listed below. Recommended dosages and durations of therapy in adult and pediatric patient populations vary in these indications. [see Dosage and Administration (2)]
1.1 Adult Patients
Acute bacterial exacerbations of chronic bronchitis due to Haemophilus influenzae , Moraxella catarrhalis, or Streptococcus pneumoniae .
Acute bacterial sinusitis due to Haemophilus influenzae , Moraxella catarrhalis. or Streptococcus pneumoniae .
Community-acquired pneumonia due to Chlamydophila pneumoniae , Haemophilus influenzae , Mycoplasma pneumoniae, or Streptococcus pneumoniae in patients appropriate for oral therapy.
Pharyngitis/tonsillitis caused by Streptococcus pyogenes as an alternative to first-line therapy in individuals who cannot use first-line therapy.
Uncomplicated skin and skin structure infections due to Staphylococcus aureus , Streptococcus pyogenes , or Streptococcus agalactiae .
Urethritis and cervicitis due to Chlamydia trachomatis or Neisseria gonorrhoeae .
Genital ulcer disease in men due to Haemophilus ducreyi (chancroid). Due to the small number of women included in clinical trials, the efficacy of azithromycin in the treatment of chancroid in women has not been established.
1.2 Pediatric Patients
[see Use in Specific Populations (8.4) and Clinical Studies (14.2)]
Acute otitis media (>6 months of age) caused by Haemophilus influenzae , Moraxella catarrhalis, or Streptococcus pneumoniae
Community-acquired pneumonia (>6 months of age) due to Chlamydophila pneumoniae , Haemophilus influenzae , Mycoplasma pneumonia , or Streptococcus pneumoniae in patients appropriate for oral therapy.
Pharyngitis/tonsillitis (> 2 years of age) caused by Streptococcus pyogenes as an alternative to first-line therapy in individuals who cannot use first-line therapy.
1.3 Limitations of Use
Azithromycin should not be used in patients with pneumonia who are judged to be inappropriate for oral therapy because of moderate to severe illness or risk factors such as any of the following:
patients with cystic fibrosis,
patients with nosocomial infections,
patients with known or suspected bacteremia,
patients requiring hospitalization,
elderly or debilitated patients, or
patients with significant underlying health problems that may compromise their ability to respond to their illness (including immunodeficiency or functional asplenia).
DOSAGE AND ADMIISTRATION
2.1 Adult Patients
Infection*
Recommended Dose/Duration of Therapy
Community-acquired pneumonia
Pharyngitis/tonsillitis (second-line therapy)
Skin/skin structure (uncomplicated)
500 mg as a single dose on Day 1,
followed by 250 mg once daily on
Days 2 through 5
Acute bacterial exacerbations of chronic
obstructive pulmonary disease
500 mg once daily for 3 days
OR
500 mg as a single dose on Day 1,
followed by 250 mg once daily on
Days 2 through 5
Acute bacterial sinusitis
500 mg once daily for 3 days
Genital ulcer disease (chancroid)
One single 1 gram dose
Non-gonococcal urethritis and cervicitis
One single 1 gram dose
Gonococcal urethritis and cervicitis
One single 2 gram dose
*DUE TO THE INDICATED ORGANISMS [see Indications and Usage (1.1)]
Azithromycin tablets can be taken with or without food.
2.2 Pediatric Patients1
Infection*
Recommended Dose/Duration of Therapy
Acute otitis media
30 mg/kg as a single dose or 10 mg/kg once daily for 3 days or 10 mg/kg as a single dose on Day 1 followed by 5 mg/kg/day on Days 2 through 5.
Acute bacterial sinusitis
10 mg/kg once daily for 3 days.
Community-acquired pneumonia
10 mg/kg as a single dose on Day 1 followed by 5 mg/kg once daily on Days 2 through 5.
Pharyngitis/tonsillitis
12 mg/kg once daily for 5 days.
*DUE TO THE INDICATED ORGANISMS [see Indications and Usage (1.2)] 1 see dosing tables below for maximum doses evaluated by indication
Azithromycin for oral suspension can be taken with or without food.
PEDIATRIC DOSAGE GUIDELINES FOR OTITIS MEDIA, ACUTE BACTERIAL SINUSITIS, AND COMMUNITY-ACQUIRED PNEUMONIA(Age 6 months and above, [see Use in Specific Populations (8.4)])Based on Body Weight
*Effectiveness of the 3-day or 1-day regimen in pediatric patients with community-acquired pneumonia has not been established.
OTITIS MEDIA AND COMMUNITY-ACQUIRED PNEUMONIA:
(5-Day Regimen)*
Dosing Calculated on 10 mg/kg/day Day 1 and
5 mg/kg/day Days 2 to 5.
Weight
100 mg/5 mL
200 mg/5 mL
Total mL per Treatment Course
Total mg per Treatment Course
Kg
Lbs.
Day 1
Days 2 to 5
Day 1
Days 2 to 5
5
11
2.5 mL;
(½ tsp)
1.25 mL;
( ¼ tsp)
7.5 mL
150 mg
10
22
5 mL; (1tsp)
2.5 mL;
(½ tsp)
15 mL
300 mg
20
44
5 mL;
(1 tsp)
2.5 mL;
(½ tsp)
15 mL
600 mg
30
66
7.5 mL;
(1½ tsp)
3.75 mL;
(¾ tsp)
22.5 mL
900 mg
40
88
10 mL;
(2 tsp)
5 mL;
(1 tsp)
30 mL
1200 mg
50 and above
110 and above
12.5 mL; (2½ tsp)
6.25 mL;
(1¼ tsp)
37.5 mL
1500 mg
*Effectiveness of the 5-day or 1-day regimen in pediatric patients with acute bacterial sinusitis has not been established.
OTITIS MEDIA AND ACUTE BACTERIAL SINUSITIS:
(3-Day Regimen)*
Dosing Calculated on 10 mg/kg/day.
Weight
100 mg/5 mL
200 mg/5 mL
Total mL per
Total mg per
Kg
Lbs.
Days 1 to 3
Days 1 to 3
Treatment Course
Treatment Course
5
11
2.5 mL;
(1/2 tsp)
7.5 mL
150 mg
10
22
5 mL;
(1 tsp)
15 mL
300 mg
20
44
5 mL
(1 tsp)
15 mL
600 mg
30
66
7.5 mL
(1 ½ tsp)
22.5 mL
900 mg
40
88
10 mL
(2 tsp)
30 mL
1200 mg
50 and above
110 and above
12.5 mL
(2 ½ tsp)
37.5 mL
1500 mg
OTITIS MEDIA: (1-Day Regimen)
Dosing Calculated on 30 mg/kg as a single dose.
Weight
200 mg/5 mL
Total mL per
Total mg per
Kg
Lbs.
1-Day Regimen
Treatment Course
Treatment Course
5
11
3.75 mL; (¾ tsp)
3.75 mL
150 mg
10
22
7.5 mL; (1 ½ tsp)
7.5 mL
300 mg
20
44
15 mL; (3 tsp)
15 mL
600 mg
30
66
22.5 mL; (4 ½ tsp)
22.5 mL
900 mg
40
88
30 mL; (6 tsp)
30 mL
1200 mg
50 and above
110 and
above
37.5 mL; (7 ½ tsp)
37.5 mL
1500 mg
The safety of re-dosing azithromycin in pediatric patients who vomit after receiving 30 mg/kg as a single dose has not been established. In clinical studies involving 487 patients with acute otitis media given a single 30 mg/kg dose of azithromycin, eight patients who vomited within 30 minutes of dosing were re-dosed at the same total dose.
Pharyngitis/Tonsillitis: The recommended dose of azithromycin tablets for children with pharyngitis/tonsillitis is 12 mg/kg once daily for 5 days. (See chart below.)
PEDIATRIC DOSAGE GUIDELINES FOR PHARYNGITIS/TONSILLITIS (Age 2 years and above, [see Use in Specific Populations (8.4)]) Based on Body Weight
PHARYNGITIS/TONSILLITIS: (5-Day Regimen)
Dosing Calculated on 12 mg/kg/day for 5 days.
Weight
200 mg/5 mL
Total mL per
Total mg per
Kg
Lbs.
Day 1 to 5
Treatment Course
Treatment
Course
8
18
2.5 mL (½ tsp)
12.5 mL
500 mg
17
37
5 mL (1 tsp)
25 mL
1000 mg
25
55
7.5 mL (1½ tsp)
37.5 mL
1500 mg
33
73
10 mL (2 tsp)
50 mL
2000 mg
40
88
12.5 mL (2½ tsp)
62.5 mL
2500 mg
DOSAGE FORMS AND STRENGTHS
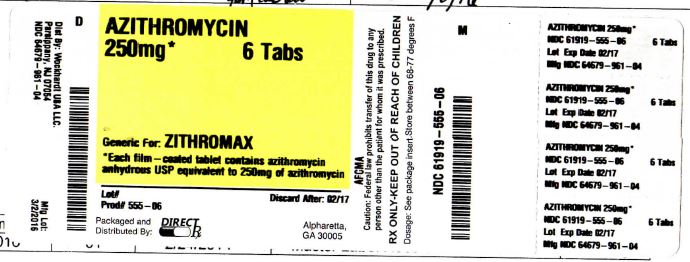
Azithromycin tablets 250 mg are supplied as white film-coated oval shaped biconvex tablets debossed with W961 on one side and other side plain containing anhydrous azithromycin 250 mg.
Azithromycin tablets 500 mg are supplied as white film-coated oval shaped biconvex tablets debossed with W964 on one side and other side plain containing anhydrous azithromycin 500 mg.
CONTRAINDICATIONS
4.1 Hypersensitivity
Azithromycin tablets are contraindicated in patients with known hypersensitivity to azithromycin, erythromycin, any macrolide or ketolide drug.
4.2 Hepatic Dysfunction
Azithromycin tablets are contraindicated in patients with a history of cholestatic jaundice/hepatic dysfunction associated with prior use of azithromycin.
WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
Serious allergic reactions, including angioedema, anaphylaxis, and dermatologic reactions including Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported in patients on azithromycin therapy. [see Contraindications (4.1)]
Fatalities have been reported. Despite initially successful symptomatic treatment of the allergic symptoms, when symptomatic therapy was discontinued, the allergic symptoms recurred soon thereafter in some patients without further azithromycin exposure. These patients required prolonged periods of observation and symptomatic treatment. The relationship of these episodes to the long tissue half-life of azithromycin and subsequent prolonged exposure to antigen is presently unknown.
If an allergic reaction occurs, the drug should be discontinued and appropriate therapy should be instituted. Physicians should be aware that allergic symptoms may reappear when symptomatic therapy has been discontinued.
5.2 Hepatotoxicity
Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure have been reported, some of which have resulted in death. Discontinue azithromycin immediately if signs and symptoms of hepatitis occur.
5.3 QT Prolongation
Prolonged cardiac repolarization and QT interval, imparting a risk of developing cardiac arrhythmia and torsades de pointes, have been seen with treatment with macrolides, including azithromycin. Cases of torsades de pointes have been spontaneously reported during postmarketing surveillance in patients receiving azithromycin. Providers should consider the risk of QT prolongation which can be fatal when weighing the risks and benefits of azithromycin for at-risk groups including:
patients with known prolongation of the QT interval, a history of torsades de pointes, congenital long QT syndrome, bradyarrhythmias or uncompensated heart failure
patients on drugs known to prolong the QT interval
patients with ongoing proarrhythmic conditions such as uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia, and in patients receiving Class IA (quinidine, procainamide) or Class III (dofetilide, amiodarone, sotalol) antiarrhythmic agents.
Elderly patients may be more susceptible to drug-associated effects on the QT interval.
5.4 Clostridium difficile-Associated Diarrhea (CDAD)
Clostridium difficile-associated diarrhea has been reported with use of nearly all antibacterial agents, including azithromycin, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon, leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antibacterial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
5.5 Exacerbation of myasthenia gravis
Exacerbation of symptoms of myasthenia gravis and new onset of myasthenic syndrome have been reported in patients receiving azithromycin therapy.
5.6 Use in Sexually Transmitted Infections
Azithromycin at the recommended dose, should not be relied upon to treat syphilis. Antibacterial agents used to treat non-gonococcal urethritis may mask or delay the symptoms of incubating syphilis. All patients with sexually transmitted urethritis or cervicitis should have a serologic test for syphilis and appropriate testing for gonorrhea performed at the time of diagnosis. Appropriate antibacterial therapy and follow-up tests for these diseases should be initiated if infection is confirmed.
5.7 Development of Drug-Resistant Bacteria
Prescribing azithromycin in the absence of a proven or strongly suspected bacterial infection is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In clinical trials, most of the reported side effects were mild to moderate in severity and were reversible upon discontinuation of the drug. Potentially serious adverse reactions of angioedema and cholestatic jaundice were reported. Approximately 0.7% of the patients (adults and pediatric patients) from the 5-day multiple-dose clinical trials discontinued azithromycin therapy because of treatment-related adverse reactions. In adults given 500 mg/day for 3 days, the discontinuation rate due to treatment-related adverse reactions was 0.6%. In clinical trials in pediatric patients given 30 mg/kg, either as a single dose or over 3 days, discontinuation from the trials due to treatment-related adverse reactions was approximately 1%. Most of the adverse reactions leading to discontinuation were related to the gastrointestinal tract, e.g., nausea, vomiting, diarrhea, or abdominal pain [see Clinical Studies (14.2)].
Adults
Multiple-dose regimens: Overall, the most common treatment-related adverse reactions in adult patients receiving multiple-dose regimens of azithromycin were related to the gastrointestinal system with diarrhea/loose stools (4 to 5%), nausea (3%), and abdominal pain (2 to 3%) being the most frequently reported.
No other adverse reactions occurred in patients on the multiple-dose regimens of azithromycin with a frequency greater than 1%. Adverse reactions that occurred with a frequency of 1% or less included the following:
Cardiovascular: Palpitations, chest pain.
Gastrointestinal: Dyspepsia, flatulence, vomiting, melena, and cholestatic jaundice.
Genitourinary: Monilia, vaginitis, and nephritis.
Nervous System: Dizziness, headache, vertigo, and somnolence.
General: Fatigue.
Allergic: Rash, pruritus, photosensitivity, and angioedema.
Single 1-gram dose regimen:
Overall, the most common adverse reactions in patients receiving a single-dose regimen of 1 gram of azithromycin were related to the gastrointestinal system and were more frequently reported than in patients receiving the multiple-dose regimen.
Adverse reactions that occurred in patients on the single 1-gram dosing regimen of azithromycin with a frequency of 1% or greater included diarrhea/loose stools (7%), nausea (5%), abdominal pain (5%), vomiting (2%), dyspepsia (1%), and vaginitis (1%).
Single 2-gram dose regimen:
Overall, the most common adverse reactions in patients receiving a single 2-gram dose of azithromycin were related to the gastrointestinal system. Adverse reactions that occurred in patients in this study with a frequency of 1% or greater included nausea (18%), diarrhea/loose stools (14%), vomiting (7%), abdominal pain (7%), vaginitis (2%), dyspepsia (1%), and dizziness (1%). The majority of these complaints were mild in nature.
Pediatric Patients
Single and Multiple-dose regimens: The types of adverse reactions in pediatric patients were comparable to those seen in adults, with different incidence rates for the dosage regimens recommended in pediatric patients.
Acute Otitis Media: For the recommended total dosage regimen of 30 mg/kg, the most frequent adverse reactions (≥1%) attributed to treatment were diarrhea, abdominal pain, vomiting, nausea, and rash [see Dosage and Administration (2) and Clinical Studies (14.2)].
The incidence, based on dosing regimen, is described in the table below: Dosage Regimen
Diarrhea %
Abdominal Pain %
Vomiting %
Nausea %
Rash %
1-day
4.3%
1.4%
4.9%
1%
1%
3-day
2.6%
1.7%
2.3%
0.4%
0.6%
5-day
1.8%
1.2%
1.1%
0.5%
0.4%
Community-Acquired Pneumonia: For the recommended dosage regimen of 10 mg/kg on Day 1 followed by 5 mg/kg on Days 2 to 5, the most frequent adverse reactions attributed to treatment were diarrhea/loose stools, abdominal pain, vomiting, nausea, and rash.
The incidence is described in the table below: Dosage Regimen
Diarrhea/Loose stools %
Abdominal Pain %
Vomiting %
Nausea %
Rash %
5-day
5.8%
1.9%
1.9%
1.9%
1.6%
Pharyngitis/tonsillitis: For the recommended dosage regimen of 12 mg/kg on Days 1 to 5, the most frequent adverse reactions attributed to treatment were diarrhea, vomiting, abdominal pain, nausea, and headache.
The incidence is described in the table below: Dosage Regimen
Diarrhea
%
Abdominal Pain %
Vomiting %
Nausea %
Rash %
Headache %
5-day
5.4%
3.4%
5.6%
1.8%
0.7%
1.1%
With any of the treatment regimens, no other adverse reactions occurred in pediatric patients treated with azithromycin tablets with a frequency greater than 1%. Adverse reactions that occurred with a frequency of 1% or less included the following:
Cardiovascular: Chest pain.
Gastrointestinal: Dyspepsia, constipation, anorexia, enteritis, flatulence, gastritis, jaundice, loose stools, and oral moniliasis.
Hematologic and Lymphatic: Anemia and leukopenia.
Nervous System: Headache (otitis media dosage), hyperkinesia, dizziness nervousness, and insomnia.
General: Fever, face edema, fatigue, fungal infection, malaise, and pain.
Allergic: Rash and allergic reaction.
Respiratory: Increased cough, pharyngitis, pleural effusion, and rhinitis.
Skin and Appendages: Eczema, fungal dermatitis, pruritus, sweating, urticaria, and vesiculobullous rash.
Special Senses: Conjunctivitis.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of azithromycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse reactions reported with azithromycin during the postmarketing period in adult and/or pediatric patients for which a causal relationship may not be established include:
Allergic: Arthralgia, edema, urticaria, and angioedema.
Cardiovascular: Arrhythmias including ventricular tachycardia and hypotension. There have been reports of QT prolongation and torsades de pointes.
Gastrointestinal: Anorexia, constipation, dyspepsia, flatulence, vomiting/diarrhea, pseudomembranous colitis, pancreatitis, oral candidiasis, pyloric stenosis, and reports of tongue discoloration.
General: Asthenia, paresthesia, fatigue, malaise, and anaphylaxis.
Genitourinary: Interstitial nephritis and acute renal failure and vaginitis.
Hematopoietic: Thrombocytopenia.
Liver/Biliary: Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure [see Warnings and Precautions (5.2)].
Nervous System: Convulsions, dizziness/vertigo, headache, somnolence, hyperactivity, nervousness, agitation, and syncope.
Psychiatric: Aggressive reaction and anxiety.
Skin/Appendages: Pruritus, serious skin reactions including erythema multiforme, Stevens-Johnson Syndrome and toxic epidermal necrolysis.
Special Senses: Hearing disturbances including hearing loss, deafness and/or tinnitus, and reports of taste/smell perversion and/or loss.
6.3 Laboratory Abnormalities
Adults:
Clinically significant abnormalities (irrespective of drug relationship) occurring during the clinical trials were reported as follows: with an incidence of greater than 1%: decreased hemoglobin, hematocrit, lymphocytes, neutrophils, and blood glucose; elevated serum creatine phosphokinase, potassium, ALT, GGT, AST, BUN, creatinine, blood glucose, platelet count, lymphocytes, neutrophils, and eosinophils; with an incidence of less than 1%: leukopenia, neutropenia, decreased sodium, potassium, platelet count, elevated monocytes, basophils, bicarbonate, serum alkaline phosphatase, bilirubin, LDH, and phosphate. The majority of subjects with elevated serum creatinine also had abnormal values at baseline. When follow-up was provided, changes in laboratory tests appeared to be reversible.
In multiple-dose clinical trials involving more than 5000 patients, four patients discontinued therapy because of treatment-related liver enzyme abnormalities and one because of a renal function abnormality.
Pediatric Patients:
One, Three, and Five Day Regimens Laboratory data collected from comparative clinical trials employing two 3-day regimens (30 mg/kg or 60 mg/kg in divided doses over 3 days), or two 5-day regimens (30 mg/kg or 60 mg/kg in divided doses over 5 days) were similar for regimens of azithromycin and all comparators combined, with most clinically significant laboratory abnormalities occurring at incidences of 1 to 5%. Laboratory data for patients receiving 30 mg/kg as a single dose were collected in one single center trial. In that trial, an absolute neutrophil count between 500 to 1500 cells/mm3 was observed in 10/64 patients receiving 30 mg/kg as a single dose, 9/62 patients receiving 30 mg/kg given over 3 days, and 8/63 comparator patients. No patient had an absolute neutrophil count <500 cells/mm3.
In multiple-dose clinical trials involving approximately 4700 pediatric patients, no patients discontinued therapy because of treatment-related laboratory abnormalities.
DRUG INTERACTIONS
7.1 Nelfinavir
Co-administration of nelfinavir at steady-state with a single oral dose of azithromycin resulted in increased azithromycin serum concentrations. Although a dose adjustment of azithromycin is not recommended when administered in combination with nelfinavir, close monitoring for known adverse reactions of azithromycin, such as liver enzyme abnormalities and hearing impairment, is warranted [see Adverse Reactions (6)].
7.2 Warfarin
Spontaneous postmarketing reports suggest that concomitant administration of azithromycin may potentiate the effects of oral anticoagulants such as warfarin, although the prothrombin time was not affected in the dedicated drug interaction study with azithromycin and warfarin. Prothrombin times should be carefully monitored while patients are receiving azithromycin and oral anticoagulants concomitantly.
7.3 Potential Drug-Drug Interactions with Macrolides
Interactions with digoxin or phenytoin have not been reported in clinical trials with azithromycin; however, no specific drug interaction studies have been performed to evaluate potential drug-drug interactions. However, drug interactions have been observed with other macrolide products. Until further data are developed regarding drug interactions when digoxin or phenytoin are used concomitantly with azithromycin careful monitoring of patients is advised.
USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects: Pregnancy Category B: Reproduction studies have been performed in rats and mice at doses up to moderately maternally toxic dose concentrations (i.e., 200 mg/kg/day). These daily doses in rats and mice, based on body surface area, are estimated to be 4 and 2 times, respectively, an adult daily dose of 500 mg. In the animal studies, no evidence of harm to the fetus due to azithromycin was found. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, azithromycin should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
Azithromycin has been reported to be excreted in human breast milk in small amounts. Caution should be exercised when azithromycin is administered to a nursing woman.
8.4 Pediatric Use
[see Clinical Pharmacology (12.3), Indications and Usage (1.2), and Dosage and Administration (2.2)]
Safety and effectiveness in the treatment of pediatric patients with acute otitis media, acute bacterial sinusitis and community-acquired pneumonia under 6 months of age have not been established. Use of azithromycin for the treatment of acute bacterial sinusitis and community-acquired pneumonia in pediatric patients (6 months of age or greater) is supported by adequate and well-controlled trials in adults
Pharyngitis/Tonsillitis: Safety and effectiveness in the treatment of pediatric patients with pharyngitis/tonsillitis under 2 years of age have not been established.
8.5 Geriatric Use
In multiple-dose clinical trials of oral azithromycin, 9% of patients were at least 65 years of age (458/4949) and 3% of patients (144/4949) were at least 75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in response between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Elderly patients may be more susceptible to development of torsades de pointes arrhythmias than younger patients. [see WARNINGS AND PRECAUTIONS (5.3)].
OVERDOSAGE
Adverse reactions experienced at higher than recommended doses were similar to those seen at normal doses particularly nausea, diarrhea, and vomiting. In the event of overdosage, general symptomatic and supportive measures are indicated as required.
DESCRIPTION
Azithromycin tablets, USP contain the active ingredient azithromycin, a macrolide antibacterial drug, for oral administration. Azithromycin has the chemical name (2R,3S,4R,5R,8R,10R,11R,12S,13S,14R)-13-[(2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranosyl)oxy]-2-ethyl-3,4,10-trihydroxy-3,5,6,8,10,12,14-heptamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy]-1-oxa-6-azacyclopentadecan-15-one. Azithromycin is derived from erythromycin; however, it differs chemically from erythromycin in that a methyl-substituted nitrogen atom is incorporated into the lactone ring. Its molecular formula is C38H72N2O12, and its molecular weight is 749. Azithromycin has the following structural formula:
Structure
Anhydrous azithromycin USP is a white amorphous powder with a molecular formula of C38H72N2O12 and a molecular weight of 749.
Azithromycin tablet, USP is supplied for oral administration as white, film-coated, oval shaped biconvex tablets containing anhydrous azithromycin 250 mg or 500 mg and the following inactive ingredients: microcrystalline cellulose, corn starch, croscarmellose sodium, magnesium trisilicate, magnesium stearate, colloidal silicon dioxide, hydroxypropyl cellulose, sodium lauryl sulfate, hypromellose, titanium dioxide and polyethylene glycol.
CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Azithromycin is a macrolide antibacterial drug [see Microbiology (12.4)].
12.2 Pharmacodynamics
Based on animal models of infection, the antibacterial activity of azithromycin appears to correlate with the ratio of area under the concentration-time curve to minimum inhibitory concentration (AUC/MIC) for certain pathogens (S. pneumoniae and S. aureus). The principal pharmacokinetic/pharmacodynamic parameter best associated with clinical and microbiological cure has not been elucidated in clinical trials with azithromycin.
Cardiac Electrophysiology
QTc interval prolongation was studied in a randomized, placebo-controlled parallel trial in 116 healthy subjects who received either chloroquine (1000 mg) alone or in combination with oral azithromycin (500 mg, 1000 mg, and 1500 mg once daily). Co-administration of azithromycin increased the QTc interval in a dose- and concentration-dependent manner. In comparison to chloroquine alone, the maximum mean (95% upper confidence bound) increases in QTcF were 5 (10) ms, 7 (12) ms and 9 (14) ms with the co-administration of 500 mg, 1000 mg and 1500 mg azithromycin, respectively.
12.3 Pharmacokinetics
Following oral administration of a single 500 mg dose (two 250 mg tablets) to 36 fasted healthy male volunteers, the mean (SD) pharmacokinetic parameters were AUC0-72 =4.3 (1.2) mcg•h/mL; Cmax=0.5 (0.2) mcg/mL; Tmax =2.2 (0.9) hours. Two azithromycin 250 mg tablets are bioequivalent to a single 500 mg tablet. In a two-way crossover study, 12 adult healthy volunteers (6 males, 6 females) received 1500 mg of azithromycin administered in single daily doses over either 5 days (two 250 mg tablets on day 1, followed by one 250 mg tablet on days 2 to 5) or 3 days (500 mg per day for days 1 to 3). Due to limited serum samples on day 2 (3-day regimen) and days 2 to 4 (5-day regimen), the serum concentration-time profile of each subject was fit to a 3-compartment model and the AUC0-∞ for the fitted concentration profile was comparable between the 5-day and 3-day regimens.
*Total AUC for the entire 3-day and 5-day regimens.
3-Day Regimen
5-Day Regimen
Pharmacokinetic Parameter [mean (SD)]
Day 1
Day 3
Day 1
Day 5
Cmax (serum, mcg/mL)
0.44 (0.22)
0.54 (0.25)
0.43 (0.20)
0.24 (0.06)
Serum AUC0-∞ (mcg•hr/mL)
17.4 (6.2)*
14.9 (3.1)*
Serum T1/2
71.8 hr
68.9 hr
Absorption
The absolute bioavailability of azithromycin 250 mg capsules is 38%.
In a two-way crossover study in which 12 healthy subjects received a single 500 mg dose of azithromycin (two 250 mg tablets) with or without a high fat meal, food was shown to increase Cmax by 23% but had no effect on AUC.
When azithromycin oral suspension was administered with food to 28 adult healthy male subjects, Cmax increased by 56% and AUC was unchanged.
Distribution
The serum protein binding of azithromycin is variable in the concentration range approximating human exposure, decreasing from 51% at 0.02 mcg/mL to 7% at 2 mcg/mL.
The antibacterial activity of azithromycin is pH related and appears to be reduced with decreasing pH, However, the extensive distribution of drug to tissues may be relevant to clinical activity.
Azithromycin has been shown to penetrate into human tissues, including skin, lung, tonsil, and cervix. Extensive tissue distribution was confirmed by examination of additional tissues and fluids (bone, ejaculum, prostate, ovary, uterus, salpinx, stomach, liver, and gallbladder). As there are no data from adequate and well-controlled studies of azithromycin treatment of infections in these additional body sites, the clinical significance of these tissue concentration data is unknown.
Following a regimen of 500 mg on the first day and 250 mg daily for 4 days, very low concentrations were noted in cerebrospinal fluid (less than 0.01 mcg/mL) in the presence of noninflamed meninges.
Metabolism
In vitro and in vivo studies to assess the metabolism of azithromycin have not been performed.
Elimination
Plasma concentrations of azithromycin following single 500 mg oral and IV doses declined in a polyphasic pattern resulting in a mean apparent plasma clearance of 630 mL/min and terminal elimination half-life of 68 hours. The prolonged terminal half-life is thought to be due to extensive uptake and subsequent release of drug from tissues. Biliary excretion of azithromycin, predominantly as unchanged drug, is a major route of elimination. Over the course of a week, approximately 6% of the administered dose appears as unchanged drug in urine.
Specific Populations
Renal Insufficiency
Azithromycin pharmacokinetics was investigated in 42 adults (21 to 85 years of age) with varying degrees of renal impairment. Following the oral administration of a single 1 g dose of azithromycin (4 x 250 mg capsules), mean Cmax and AUC0-120 increased by 5.1% and 4.2%, respectively, in subjects with mild to moderate renal impairment (GFR 10 to 80 mL/min) compared to subjects with normal renal function (GFR >80 mL/min). The mean Cmax and AUC0-120 increased 61% and 35%, respectively, in subjects with severe renal impairment (GFR <10 mL/min) compared to subjects with normal renal function (GFR >80 mL/min).
Hepatic Insufficiency
The pharmacokinetics of azithromycin in subjects with hepatic impairment has not been established.
Gender
There are no significant differences in the disposition of azithromycin between male and female subjects. No dosage adjustment is recommended based on gender.
Geriatric Patients
Pharmacokinetic parameters in older volunteers (65 to 85 years old) were similar to those in young adults (18 to 40 years old) for the 5-day therapeutic regimen. Dosage adjustment does not appear to be necessary for older patients with normal renal and hepatic function receiving treatment with this dosage regimen [see Geriatric Use (8.5)].
Pediatric Patients
In two clinical studies, azithromycin for oral suspension was dosed at 10 mg/kg on day 1, followed by 5 mg/kg on days 2 through 5 in two groups of pediatric patients (aged 1 to 5 years and 5 to 15 years, respectively). The mean pharmacokinetic parameters on day 5 were Cmax =0.216 mcg/mL, Tmax =1.9 hours, and AUC0-24 =1.822 mcg•hr/mL for the 1- to 5-year-old group and were Cmax =0.383 mcg/mL, Tmax =2.4 hours, and AUC0-24 =3.109 mcg•hr/mL for the 5- to 15-year-old group.
In another study, 33 pediatric patients received doses of 12 mg/kg/day (maximum daily dose 500 mg) for 5 days, of whom 31 patients were evaluated for azithromycin pharmacokinetics following a low fat breakfast. In this study, azithromycin concentrations were determined over a 24 hour period following the last daily dose. Patients weighing above 41.7 kg received the maximum adult daily dose of 500 mg. Seventeen patients (weighing 41.7 kg or less) received a total dose of 60 mg/kg. The following table shows pharmacokinetic data in the subset of pediatric patients who received a total dose of 60 mg/kg.
Pharmacokinetic Parameter [mean (SD)]
5-Day Regimen (12 mg/kg for 5 days)
N
17
Cmax (mcg/mL)
0.5 (0.4)
Tmax (hr)
2.2 (0.8)
AUC0-24(mcg•hr/mL)
3.9 (1.9)
Single dose pharmacokinetics of azithromycin in pediatric patients given doses of 30 mg/kg have not been studied [see Dosage and Administration (2)].
Drug interaction studies were performed with azithromycin and other drugs likely to be co-administered. The effects of co-administration of azithromycin on the pharmacokinetics of other drugs are shown in Table 1 and the effects of other drugs on the pharmacokinetics of azithromycin are shown in Table 2.
Co-administration of azithromycin at therapeutic doses had a modest effect on the pharmacokinetics of the drugs listed in Table 1. No dosage adjustment of drugs listed in Table 1 is recommended when co-administered with azithromycin.
Co-administration of azithromycin with efavirenz or fluconazole had a modest effect on the pharmacokinetics of azithromycin. Nelfinavir significantly increased the Cmax and AUC of azithromycin. No dosage adjustment of azithromycin is recommended when administered with drugs listed in Table 2 [see Drug Interactions (7.3)].
*-90% Confidence interval not reported
Table 1. Drug Interactions: Pharmacokinetic Parameters for Co-administered Drugs in the Presence of Azithromycin
Co-administered Drug
Dose of Co-administered Drug
Dose of Azithromycin
n
Ratio (with/without azithromycin) of
Co-administered Drug Pharmacokinetic
Parameters (90% CI); No Effect = 1
Mean Cmax
Mean AUC
Atorvastatin
10 mg/day for
8 days
500 mg/day orally on days 6 to 8
12
0.83
(0.63 to 1.08)
1.01
(0.81 to 1.25)
Carbamazepine
200 mg/day for 2 days,
then 200 mg twice a day for 18 days
500 mg/day orally for days 16 to 18
7
0.97
(0.88 to 1.06)
0.96
(0.88 to 1.06)
Cetirizine
20 mg/day for
11 days
500 mg orally on day 7,
then 250 mg/day on days 8 to 11
14
1.03
(0.93 to 1.14)
1.02
(0.92 to 1.13)
Didanosine
200 mg orally twice a day for 21 days
1200 mg/day orally on days 8 to 21
6
1.44
(0.85 to 2.43)
1.14
(0.83 to 1.57)
Efavirenz
400 mg/day for 7 days
600 mg orally on day 7
14
1.04*
0.95*
Fluconazole
200 mg orally single dose
1200 mg orally single dose
18
1.04
(0.98 to 1.11)
1.01
(0.97 to 1.05)
Indinavir
800 mg three times a day for 5 days
1200 mg orally on
day 5
18
0.96
(0.86 to 1.08)
0.90
(0.81 to 1)
Midazolam
15 mg orally on
day 3
500 mg/day orally for
3 days
12
1.27
(0.89 to 1.81)
1.26
(1.01 to 1.56)
Nelfinavir
750 mg three times a day for 11 days
1,200 mg orally on
day 9
14
0.90
(0.81 to 1.01)
0.85
(0.78 to 0.93)
Sildenafil
100 mg on days 1 and 4
500 mg/day orally for
3 days
12
1.16
(0.86 to 1.57)
0.92
(0.75 to 1.12)
Theophylline
4 mg/kg IV on days 1, 11, 25
500 mg orally on day 7, 250 mg/day on
days 8 to 11
10
1.19
(1.02 to 1.40)
1.02
(0.86 to 1.22)
Theophylline
300 mg orally twice a day for 15 days
500 mg orally on day 6, then 250 mg/day on days 7 to 10
8
1.09
(0.92 to 1.29)
1.08
(0.89 to 1.31)
Triazolam
0.125 mg on day 2
500 mg orally on day 1, then 250 mg/day on
day 2
12
1.06*
1.02*
Trimethoprim/ Sulfamethoxazole
160 mg/800 mg/day orally for
7 days
1200 mg orally on
day 7
12
0.85
(0.75 to 0.97)/0.90
(0.78 to 1.03)
0.87
(0.80 to 0.95)/0.96
(0.88 to 1.03)
Zidovudine
500 mg/day orally for 21 days
600 mg/day orally for
14 days
5
1.12
(0.42 to 3.02)
0.94
(0.52 to 1.70)
Zidovudine
500 mg/day orally for 21 days
1200 mg/day orally for 14 days
4
1.31
(0.43 to 3.97)
1.30
(0.69 to 2.43)
* -90% Confidence interval not reported
Table 2. Drug Interactions: Pharmacokinetic Parameters for Azithromycin in the Presence of Co-administered Drugs [see Drug Interactions (7)].
Co-administered Drug
Dose of Co-administered Drug
Dose of Azithromycin
n
Ratio (with/without co-administered drug) of Azithromycin Pharmacokinetic Parameters (90% CI); No Effect = 1
Mean Cmax
Mean AUC
Efavirenz
400 mg/day for 7 days
600 mg orally on day 7
14
1.22
(1.04 to 1.42)
0.92*
Fluconazole
200 mg orally single dose
1,200 mg orally single dose
18
0.82
(0.66 to 1.02)
1.07
(0.94 to 1.22)
Nelfinavir
750 mg three times a day for 11 days
1,200 mg orally on day 9
14
2.36
(1.77 to 3.15)
2.12
(1.80 to 2.50)
12.4 Microbiology
Mechanism of Action
Azithromycin acts by binding to the 50S ribosomal subunit of susceptible microorganisms and interferes with bacterial protein synthesis. Nucleic acid synthesis is not affected.
Cross Resistance
Azithromycin demonstrates cross resistance with erythromycin resistant Gram positive isolates.
Azithromycin has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical [see Indications and Usage (1)].
Gram-Positive Bacteria
Staphylococcus aureus
Streptococcus agalactiae
Streptococcus pneumoniae
Streptococcus pyogenes
Gram-Negative Bacteria
Haemophilus ducreyi
Haemophilus influenzae
Moraxella catarrhalis
Neisseria gonorrhoeae
Other Bacteria
Chlamydophila pneumoniae
Chlamydia trachomatis
Mycoplasma pneumoniae
The following in vitro data are available, but their clinical significance is unknown. Azithromycin exhibits in vitro minimal inhibitory concentrations (MICs) of 4 mcg/ml or less against most (≥90%) isolates of the following bacteria; however, the safety and effectiveness of azithromycin in treating clinical infections due to these bacteria have not been established in adequate and well-controlled trials.
Gram-Positive Bacteria
Beta-hemolytic streptococci (Groups C, F, G)
Viridans group streptococci
Gram-Negative Bacteria
Bordetella pertussis
Legionella pneumophila
Anaerobic Bacteria
Prevotella bivia
Peptostreptococcus species
Other Bacteria
Ureaplasma urealyticum
Susceptibility Testing Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility test results for antibacterial drugs used in resident hospitals to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting an antibacterial drug product for treatment.
Dilution Techniques
Quantitative methods are used to determine minimal inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antibacterial compounds. The MICs should be determined using a standardized test method1,2,3 (broth or agar). The MIC values should be interpreted according to criteria provided in Table 1.
Diffusion Techniques
Quantitative methods that require measurement of zone diameters can also provide reproducible estimates of the susceptibility of bacteria to antibacterial compounds. The zone size provides an estimate of the susceptibility of bacteria to antibacterial compounds. The zone size should be determined using a standardized method2,3. This procedure uses paper disk impregnated with 15 mcg azithromycin to test the susceptibility of bacteria to azithromycin. The disk diffusion interpretive criteria are provided in Table 1.
a Clarithromycin is used for susceptibility testing due to its better solubility
b Insufficient information is available to determine Intermediate or Resistant interpretive criteria
Table 1: Susceptibility Test Interpretive Criteria for Azithromycina
Pathogen
Minimum Inhibitory Concentrations (mcg/mL)
Disk Diffusion (zone diameter in mm)
S
I
R
S
I
R
Haemophilus influenzaeb
≤4
-
-
≥12
-
-
Staphylococcus aureus
≤2
4
≥8
≥18
14 to 17
≤13
Streptococci including S. pneumoniae
≤0.5
1
≥2
≥18
14 to 17
≤13
The ability to correlate MIC values and plasma drug levels is difficult as azithromycin concentrates in macrophages and tissues. [see Clinical Pharmacology (12)]
A report of "Susceptible" indicates that the pathogen is likely to inhibit growth of the pathogen if the antibacterial compound reaches the concentration at the infection site necessary to inhibit growth of the pathogen. A report of "Intermediate" indicates that the result should be considered equivocal, and if the microorganism is not fully susceptible to alternative clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated. This category also provides a buffer zone that prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the antibacterial is not likely to inhibit growth of the pathogen if the antibacterial compound reaches the concentrations usually achievable at the infection site; other therapy should be selected.
Quality Control
Standardized susceptibility test procedures require the use of laboratory controls to monitor and ensure the accuracy and precision of supplies and reagents used in the assay, and the techniques of the individuals performing the test1,2,3. Standard azithromycin powder should provide the following range of MIC values provided in Table 2. For the diffusion technique using the 15-mcg azithromycin disk the criteria provided in Table 2 should be achieved.
Table 2: Acceptable Quality Control Ranges for Susceptibility Testing
*ATCC = American Type Culture Collection
Quality Control Organism
Minimum Inhibitory Concentrations (mcg/mL)
Disk Diffusion (zone diameters in mm)
Staphylococcus aureus ATCC* 25923
Not Applicable
21 to 26
Staphylococcus aureus ATCC 29213
0.5 to 2
Not Applicable
Haemophilus Influenzae ATCC 49247
1 to 4
13 to 21
Streptococcus pneumoniae ATCC 49619
0.06 to 0.25
19 to 25
Close
NON CLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals have not been performed to evaluate carcinogenic potential. Azithromycin has shown no mutagenic potential in standard laboratory tests: mouse lymphoma assay, human lymphocyte clastogenic assay, and mouse bone marrow clastogenic assay. No evidence of impaired fertility due to azithromycin was found in rats given daily doses up to 10 mg/kg (approximately 0.2 times an adult daily dose of 500 mg based on body surface area).
13.2 Animal Toxicology and/or Pharmacology
Phospholipidosis (intracellular phospholipid accumulation) has been observed in some tissues of mice, rats, and dogs given multiple doses of azithromycin. It has been demonstrated in numerous organ systems (e.g., eye, dorsal root ganglia, liver, gallbladder, kidney, spleen, and/or pancreas) in dogs and rats treated with azithromycin at doses which, expressed on the basis of body surface area, are similar to or less than the highest recommended adult human dose. This effect has been shown to be reversible after cessation of azithromycin treatment. Based on the pharmacokinetic data, phospholipidosis has been seen in the rat (50 mg/kg/day dose) at the observed maximal plasma concentration of 1.3 mcg/mL (1.6 times the observed Cmax of 0.821 mcg/mL at the adult dose of 2 g). Similarly, it has been shown in the dog (10 mg/kg/day dose) at the observed maximal serum concentration of 1 mcg/mL (1.2 times the observed Cmax of 0.821 mcg/mL at the adult dose of 2 g). Phospholipidosis was also observed in neonatal rats dosed for 18 days at 30 mg/kg/day, which is less than the pediatric dose of 60 mg/kg based on body surface area. It was not observed in neonatal rats treated for 10 days at 40 mg/kg/day with mean maximal serum concentrations of 1.86 mcg/mL, approximately 1.5 times the Cmax of 1.27 mcg/mL at the pediatric dose. Phospholipidosis has been observed in neonatal dogs (10 mg/kg/day) at maximum mean whole blood concentrations of 3.54 mcg/mL, approximately 3 times the pediatric dose Cmax. The significance of these findings for animals and for humans is unknown.
CLINICAL STUDIES
14.1 Adult Patients
Acute Bacterial Exacerbations of Chronic Bronchitis
In a randomized, double-blind controlled clinical trial of acute exacerbation of chronic bronchitis (AECB), azithromycin (500 mg once daily for 3 days) was compared with clarithromycin (500 mg twice daily for 10 days). The primary endpoint of this trial was the clinical cure rate at Days 21 to 24. For the 304 patients analyzed in the modified intent-to-treat analysis at the Days 21 to 24 visit, the clinical cure rate for 3 days of azithromycin was 85% (125/147) compared to 82% (129/157) for 10 days of clarithromycin.
The following outcomes were the clinical cure rates at the Days 21 to 24 visit for the bacteriologically evaluable patients by pathogen:
Pathogen
Azithromycin (3 Days)
Clarithromycin (10 Days)
S. pneumoniae
29/32 (91%)
21/27 (78%)
H. influenzae
12/14 (86%)
14/16 (88%)
M. catarrhalis
11/12 (92%)
12/15 (80%)
Acute Bacterial Sinusitis
In a randomized, double-blind, double-dummy controlled clinical trial of acute bacterial sinusitis, azithromycin (500 mg once daily for 3 days) was compared with amoxicillin/clavulanate (500/125 mg three times a day for 10 days). Clinical response assessments were made at Day 10 and Day 28. The primary endpoint of this trial was prospectively defined as the clinical cure rate at Day 28. For the 594 patients analyzed in the modified intent to treat analysis at the Day 10 visit, the clinical cure rate for 3 days of azithromycin was 88% (268/303) compared to 85% (248/291) for 10 days of amoxicillin/clavulanate. For the 586 patients analyzed in the modified intent to treat analysis at the Day 28 visit, the clinical cure rate for 3 days of azithromycin was 71.5% (213/298) compared to 71.5% (206/288), with a 97.5% confidence interval of –8.4 to 8.3, for 10 days of amoxicillin/clavulanate.
In an open label, non-comparative study requiring baseline transantral sinus punctures, the following outcomes were the clinical success rates at the Day 7 and Day 28 visits for the modified intent to treat patients administered 500 mg of azithromycin once daily for 3 days with the following pathogens:
Clinical Success Rates of Azithromycin (500 mg per day for 3 Days) Pathogen
Day 7
Day28
S. pneumoniae
23/26 (88%)
21/25 (84%)
H. influenzae
28/32 (87%)
24/32 (75%)
M. catarrhalis
14/15 (93%)
13/15 (87%)
14.2 Pediatric Patients
From the perspective of evaluating pediatric clinical trials, Days 11 to 14 were considered on-therapy evaluations because of the extended half-life of azithromycin. Days 11 to 14 data are provided for clinical guidance. Days 24 to 32 evaluations were considered the primary test of cure endpoint.
Pharyngitis/Tonsillitis
In three double-blind controlled studies, conducted in the United States, azithromycin (12 mg/kg once a day for 5 days) was compared to penicillin V (250 mg three times a day for 10 days) in the treatment of pharyngitis due to documented Group A β-hemolytic streptococci (GABHS or S. pyogenes). Azithromycin was clinically and microbiologically statistically superior to penicillin at Day 14 and Day 30 with the following clinical success (i.e., cure and improvement) and bacteriologic efficacy rates (for the combined evaluable patient with documented GABHS):
Three U.S. Streptococcal Pharyngitis StudiesAzithromycin vs. Penicillin VEFFICACY RESULTS
Day 14
Day 30
Bacteriologic Eradication:
Azithromycin
323/340 (95%)
255/330 (77%)
Penicillin V
242/332 (73%)
206/325 (63%)
Clinical Success (cure plus improvement):
Azithromycin
336/343 (98%)
310/330 (94%)
Penicillin V
284/338 (84%)
241/325 (74%)
Approximately 1% of azithromycin-susceptible S. pyogenes isolates were resistant to azithromycin following therapy.
Acute Otitis Media
Efficacy using azithromycin given over 5 days (10 mg/kg on Day 1 followed by 5 mg/kg on Days 2 to 5).
Trial 1
In a double-blind, controlled clinical study of acute otitis media performed in the United States, azithromycin (10 mg/kg on Day 1 followed by 5 mg/kg on Days 2 to 5) was compared to amoxicillin/clavulanate potassium (4:1). For the 553 patients who were evaluated for clinical efficacy, the clinical success rate (i.e., cure plus improvement) at the Day 11 visit was 88% for azithromycin and 88% for the control agent. For the 521 patients who were evaluated at the Day 30 visit, the clinical success rate was 73% for azithromycin and 71% for the control agent.
Trial 2
In a non-comparative clinical and microbiologic trial performed in the United States, where significant rates of beta-lactamase producing organisms (35%) were found, 131 patients were evaluable for clinical efficacy. The combined clinical success rate (i.e., cure and improvement) at the Day 11 visit was 84% for azithromycin. For the 122 patients who were evaluated at the Day 30 visit, the clinical success rate was 70% for azithromycin.
Microbiologic determinations were made at the pre-treatment visit. Microbiology was not reassessed at later visits. The following clinical success rates were obtained from the evaluable group:
Day 11
Day 30
Pathogen
Azithromycin
Azithromycin
S. pneumoniae
61/74 (82%)
40/56 (71%)
H. influenzae
43/54 (80%)
30/47 (64%)
M. catarrhalis
28/35 (80%)
19/26 (73%)
S. pyogenes
11/11 (100%)
7/7 (100%)
Overall
177/217 (82%)
97/137 (73%)
Trial 3
In another controlled comparative clinical and microbiologic study of otitis media performed in the United States, azithromycin (10 mg/kg on Day 1 followed by 5 mg/kg on Days 2 to 5).was compared to amoxicillin/clavulanate potassium (4:1). This study utilized two of the same investigators as Protocol 2 (above), and these two investigators enrolled 90% of the patients in Protocol 3. For this reason, Protocol 3 was not considered to be an independent study. Significant rates of beta-lactamase producing organisms (20%) were found. Ninety-two (92) patients were evaluable for clinical and microbiologic efficacy. The combined clinical success rate (i.e., cure and improvement) of those patients with a baseline pathogen at the Day 11 visit was 88% for azithromycin vs. 100% for control; at the Day 30 visit, the clinical success rate was 82% for azithromycin vs. 80% for control.
Microbiologic determinations were made at the pre-treatment visit. Microbiology was not reassessed at later visits. At the Day 11 and Day 30 visits, The following clinical success rates were obtained from the evaluable group:
Day 11
Day 30
Pathogen
Azithromycin
Control
Azithromycin
Control
S. pneumoniae
25/29 (86%)
26/26 (100%)
22/28 (79%)
18/22 (82%)
H. influenzae
9/11 (82%)
9/9 (100%)
8/10 (80%)
6/8 (75%)
M. catarrhalis
7/7 (100%)
5/5 (100%)
5/5 (100%)
2/3 (66%)
S. pyogenes
2/2 (100%)
5/5 (100%)
2/2 (100%)
4/4 (100%)
Overall
43/49 (88%)
45/45 (100%)
37/45 (82%)
30/37 (81%)
Efficacy using azithromycin given over 3 days (10 mg/kg/day).
Trial 4
In a double-blind, controlled, randomized clinical study of acute otitis media in pediatric patients from 6 months to 12 years of age, azithromycin (10 mg/kg per day for 3 days) was compared to amoxicillin/clavulanate potassium (7:1) in divided doses q12h for 10 days. Each patient received active drug and placebo matched for the comparator.
For the 366 patients who were evaluated for clinical efficacy at the Day 12 visit, the clinical success rate (i.e., cure plus improvement) was 83% for azithromycin and 88% for the control agent. For the 362 patients who were evaluated at the Days 24 to 28 visit, the clinical success rate was 74% for azithromycin and 69% for the control agent.
Efficacy using azithromycin 30 mg/kg given as a single dose
Trial 5
A double-blind, controlled, randomized trial was performed at nine clinical centers. Pediatric patients from 6 months to 12 years of age were randomized 1:1 to treatment with either azithromycin (given at 30 mg/kg as a single dose on Day 1) or amoxicillin/clavulanate potassium (7:1), divided q12h for 10 days. Each child received active drug, and placebo matched for the comparator.
Clinical response (Cure, Improvement, Failure) was evaluated at End of Therapy (Days 12 to 16) and Test of Cure (Days 28 to 32). Safety was evaluated throughout the trial for all treated subjects. For the 321 subjects who were evaluated at End of Treatment, the clinical success rate (cure plus improvement) was 87% for azithromycin, and 88% for the comparator. For the 305 subjects who were evaluated at Test of Cure, the clinical success rate was 75% for both azithromycin and the comparator.
Trial 6
In a non-comparative clinical and microbiological trial, 248 patients from 6 months to 12 years of age with documented acute otitis media were dosed with a single oral dose of azithromycin (30 mg/kg on Day 1).
For the 240 patients who were evaluable for clinical modified Intent-to-Treat (MITT) analysis, the clinical success rate (i.e., cure plus improvement) at Day 10 was 89% and for the 242 patients evaluable at Days 24 to 28, the clinical success rate (cure) was 85%.
Presumed Bacteriologic Eradication
Day 10
Days 24 to 28
S. pneumoniae
70/76 (92%)
67/76 (88%)
H. influenzae
30/42 (71%)
28/44 (64%)
M. catarrhalis
10/10 (100%)
10/10 (100%)
Overall
110/128 (86%)
105/130 (81%)
STORAGE AND HANDLING
Azithromycin tablets, USP are supplied in the following strengths and package configurations:
Azithromycin tablets 250 mg are supplied as white film-coated oval shaped biconvex tablets debossed with W961 on one side and other side plain containing anhydrous azithromycin 250 mg.
Azithromycin tablets 500 mg are supplied as white film-coated oval shaped biconvex tablets debossed with W964 on one side and other side plain containing anhydrous azithromycin 500 mg.
Cartons of 3 blister cards (3 tablets per blister card)
Bottles of 500
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].