FULL PRESCRIBING INFORMATION
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term studies. These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients over age 24; there was a reduction in risk with antidepressant use in patients aged 65 and older [see Warnings and Precautions (5.1)].
In patients of all ages who are started on antidepressant therapy, monitor closely for worsening, and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber [see Warnings and Precautions (5.1)].
Duloxetine is not approved for use in pediatric patients [see Use in Specific Populations (8.4)].
1 INDICATIONS AND USAGE
1.1 Major Depressive Disorder
Duloxetine delayed-release capsules are indicated for the treatment of major depressive disorder (MDD). The efficacy of duloxetine was established in four short term and one maintenance trial in adults [see CLINICAL STUDIES (14.1)].
A major depressive episode (DSM-IV) implies a prominent and relatively persistent (nearly every day for at least 2 weeks) depressed or dysphoric mood that usually interferes with daily functioning, and includes at least 5 of the following 9 symptoms: depressed mood, loss of interest in usual activities, significant change in weight and/or appetite, insomnia or hypersomnia, psychomotor agitation or retardation, increased fatigue, feelings of guilt or worthlessness, slowed thinking or impaired concentration, or a suicide attempt or suicidal ideation.
1.2 Generalized Anxiety Disorder
Duloxetine delayed-release capsules are indicated for the treatment of generalized anxiety disorder (GAD). The efficacy of duloxetine was established in three short-term trials and one maintenance trial in adults [see ]. Duloxetine delayed-release capsules are indicated for the treatment of generalized anxiety disorder (GAD). The efficacy of duloxetine was established in three short-term trials and one maintenance trial in adults [see CLINICAL STUDIES (14.2) ].
Generalized anxiety disorder is defined by the DSM-IV as excessive anxiety and worry, present more days than not, for at least 6 months. The excessive anxiety and worry must be difficult to control and must cause significant distress or impairment in normal functioning. It must be associated with at least 3 of the following 6 symptoms: restlessness or feeling keyed up or on edge, being easily fatigued, difficulty concentrating or mind going blank, irritability, muscle tension, and/or sleep disturbance.Generalized anxiety disorder is defined by the DSM-IV as excessive anxiety and worry, present more days than not, for at least 6 months. The excessive anxiety and worry must be difficult to control and must cause significant distress or impairment in normal functioning. It must be associated with at least 3 of the following 6 symptoms: restlessness or feeling keyed up or on edge, being easily fatigued, difficulty concentrating or mind going blank, irritability, muscle tension, and/or sleep disturbance.
1.3 Diabetic Peripheral Neuropathic Pain
Duloxetine delayed-release capsules are indicated for the management of neuropathic pain (DPNP) associated with diabetic peripheral neuropathy [see CLINICAL STUDIES (14.3)].
1.5 Chronic Musculoskeletal Pain
Duloxetine delayed-release capsules are indicated for the management of chronic musculoskeletal pain. This has been established in studies in patients with chronic low back pain (CLBP) and chronic pain due to osteoarthritis [see Clinical Studies ( 14.5) ].
2 DOSAGE AND ADMINISTRATION
Duloxetine delayed-release capsules should be swallowed whole and should not be chewed or crushed, nor should the capsule be opened and its contents sprinkled on food or mixed with liquids. All of these might affect the enteric coating. Duloxetine delayed-release capsules should be given without regard to meals.
2.1 Initial Treatment
Major Depressive Disorder - Duloxetine delayed-release capsules should be administered at a total dose of 40 mg/day (given as 20 mg twice daily) to 60 mg/day (given either once daily or as 30 mg twice daily). For some patients, it may be desirable to start at 30 mg once daily for 1 week, to allow patients to adjust to the medication before increasing to 60 mg once daily. While a 120 mg/day dose was shown to be effective, there is no evidence that doses greater than 60 mg/day confer any additional benefits. The safety of doses above 120 mg/day has not been adequately evaluated [see Clinical Studies ( 14.1) ].
Generalized Anxiety Disorder - For most patients, the recommended starting dose for duloxetine delayed-release capsules are 60 mg administered once daily. For some patients, it may be desirable to start at 30 mg once daily for 1 week, to allow patients to adjust to the medication before increasing to 60 mg once daily. While a 120 mg once daily dose was shown to be effective, there is no evidence that doses greater than 60 mg/day confer additional benefit. Nevertheless, if a decision is made to increase the dose beyond 60 mg once daily, dose increases should be in increments of 30 mg once daily. The safety of doses above 120 mg once daily has not been adequately evaluated [see Clinical Studies ( 14.2) ]
Diabetic Peripheral Neuropathic Pain - The recommended dose for duloxetine delayed-release capsules is 60 mg administered once daily. There is no evidence that doses higher than 60 mg confer additional significant benefit and the higher dose is clearly less well tolerated [see Clinical Studies ( 14.3) ]. For patients for whom tolerability is a concern, a lower starting dose may be considered.
Since diabetes is frequently complicated by renal disease, a lower starting dose and gradual increase in dose should be considered for patients with renal impairment [see Dosage and Administration ( 2.3), Use In Specific Population (8.10), and Clinical Pharmacology (12.3) ].
Chronic Musculoskeletal Pain — The recommended dose for duloxetine delayed-release capsules is 60 mg once daily. Dosing may be started at 30 mg for one week, to allow patients to adjust to the medication before increasing to 60 mg once daily. There is no evidence that higher doses confer additional benefit, even in patients who do not respond to a 60 mg dose, and higher doses are associated with a higher rate of adverse reactions [see Clinical Studies ( 14.5) ].
2.2 Maintenance/Continuation/Extended Treatment
Major Depressive Disorder — It is generally agreed that acute episodes of major depression require several months or longer of sustained pharmacologic therapy. Maintenance of efficacy in MDD was demonstrated with duloxetine delayed-release capsules as monotherapy. Duloxetine delayed-release capsules should be administered at a total dose of 60 mg once daily. Patients should be periodically reassessed to determine the need for maintenance treatment and the appropriate dose for such treatment [see Clinical Studies ( 14.1)].
Generalized Anxiety Disorder — It is generally agreed that episodes of generalized anxiety disorder require several months or longer of sustained pharmacological therapy. Maintenance of efficacy in GAD was demonstrated with duloxetine as monotherapy. Duloxetine delayed-release capsules should be administered in a dose range of 60 to 120 mg once daily. Patients should be periodically reassessed to determine the continued need for maintenance treatment and the appropriate dose for such treatment [see Clinical Studies ( 14.2) ].
Diabetic Peripheral Neuropathic Pain — As the progression of diabetic peripheral neuropathy is highly variable and management of pain is empirical, the effectiveness of duloxetine delayed-release capsules must be assessed individually. Efficacy beyond 12 weeks has not been systematically studied in placebo-controlled trials.
Chronic Musculoskeletal Pain — The efficacy of duloxetine delayed-release capsules has not been established in placebo-controlled studies beyond 13 weeks.
2.3 Dosing in Special Populations
Hepatic Insufficiency —It is recommended that duloxetine delayed-release capsules should ordinarily not be administered to patients with any hepatic insufficiency [see Warnings and Precautions ( 5.14) and UseIn Specific Populations ( 8.9) ].
Severe Renal Impairment — Duloxetine delayed-release capsules are not recommended for patients with end-stage renal disease or severe renal impairment (estimated creatinine clearance <30 mL/min) [see Warnings and Precautions ( 5.14) and Use In Specific Populations ( 8.10) ].
Elderly Patients — No dose adjustment is recommended for elderly patients on the basis of age. As with any drug, caution should be exercised in treating the elderly. When individualizing the dosage in elderly patients, extra care should be taken when increasing the dose [see Use In Specific Populations ( 8.5) ].
Pregnant Women — There are no adequate and well-controlled studies in pregnant women; therefore, duloxetine delayed-release capsules should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus [see Use In Specific Populations ( 8.1) ].
Nursing Mothers — Because the safety of duloxetine in infants is not known, nursing while on duloxetine delayed-release capsules are not recommended [see Use In Specific Populations ( 8.3) ].
2.4 Discontinuing Duloxetine
Symptoms associated with discontinuation of duloxetine delayed-release capsules and other SSRIs and SNRIs have been reported. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible [see WARNINGS AND PRECAUTIONS (5.7)].
2.5 Switching a Patient To or From a Monoamine Oxidase Inhibitor (MAOI) Intended to Treat Psychiatric Disorders
At least 14 days should elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with duloxetine delayed-release capsules. Conversely, at least 5 days should be allowed after stopping duloxetine delayed-release capsules before starting an MAOI intended to treat psychiatric disorders [see CONTRAINDICATIONS (4.1)].
2.6 Use of Duloxetine with Other MAOIs such as Linezolid or Methylene Blue
Do not start duloxetine in a patient who is being treated with linezolid or intravenous methylene blue because there is an increased risk of serotonin syndrome. In a patient who requires more urgent treatment of a psychiatric condition, other interventions, including hospitalization, should be considered [see CONTRAINDICATIONS (4.1)].
In some cases, a patient already receiving duloxetine therapy may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of serotonin syndrome in a particular patient, duloxetine should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for symptoms of serotonin syndrome for 5 days or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with duloxetine may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue [see WARNINGS AND PRECAUSTIONS (5.4)].
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with duloxetine is unclear. The clinician should, nevertheless, be aware of the possibility of emergent symptoms of serotonin syndrome with such use [see WARNINGS AND PRECAUSTIONS (5.4)].
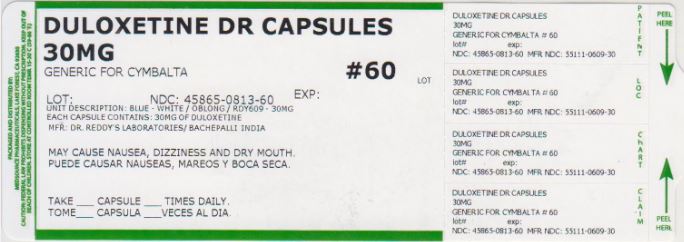
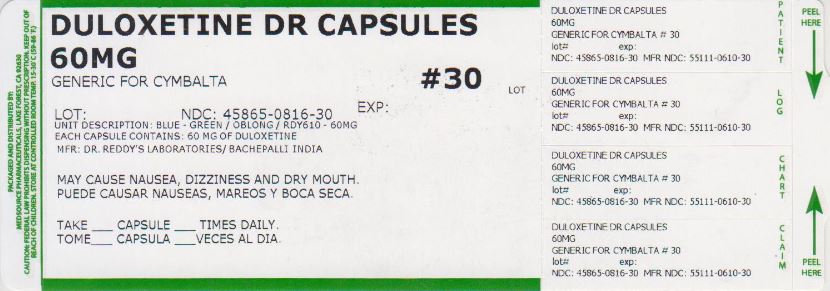
3 DOSAGE FORM AND STRENGTHS
Duloxetine delayed-release capsules are available as:
20 mg opaque green coloured cap and opaque green coloured body imprinted with "RDY608"
30 mg opaque blue coloured cap and opaque white coloured body imprinted with "RDY609"
60 mg opaque blue coloured cap and opaque green coloured body imprinted with "RDY610"
4 CONTRAINDICATIONS
4.1 Monoamine Oxidase Inhibitors (MAOIs)
The use of MAOIs intended to treat psychiatric disorders with duloxetine or within 5 days of stopping treatment with duloxetine is contraindicated because of an increased risk of serotonin syndrome. The use of duloxetine within 14 days of stopping an MAOI intended to treat psychiatric disorders is also contraindicated [see DOSAGE AND ADMINISTRATION (2.5) and WARNINGS AND PRECAUSTIONS (5.4).
Starting duloxetine in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue is also contraindicated because of an increased risk of serotonin syndrome [see DOSAGE AND ADMINISTRATION (2.6) and WARNINGS AND PRECAUSTIONS (5.4).
5 WARNINGS AND PRECAUTIONS
5.1 Suicidal Thoughts and Behaviors in Adolescents and Young Adults
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment.
Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk of differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk of differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
| Age Range | Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated |
|---|---|
| Increases Compared to Placebo | |
| <18 | 14 additional cases |
| 18-24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25-64 | 1 fewer case |
| ≥65 | 6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that discontinuation can be associated with certain symptoms [see and for descriptions of the risks of discontinuation of duloxetine ]. If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that discontinuation can be associated with certain symptoms [see DOSAGE AND ADMINISTRATION (2.4) and WARNINGS AND PRECAUTIONS (5.7) for descriptions of the risks of discontinuation of duloxetine ].
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for duloxetine should be written for the smallest quantity of capsules consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder — A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that duloxetine is not approved for use in treating bipolar depression.
5.2 Hepatotoxicity
There have been reports of hepatic failure, sometimes fatal, in patients treated with duloxetine. These cases have presented as hepatitis with abdominal pain, hepatomegaly, and elevation of transaminase levels to more than twenty times the upper limit of normal with or without jaundice, reflecting a mixed or hepatocellular pattern of liver injury. Duloxetine should be discontinued in patients who develop jaundice or other evidence of clinically significant liver dysfunction and should not be resumed unless another cause can be established.
Cases of cholestatic jaundice with minimal elevation of transaminase levels have also been reported. Other postmarketing reports indicate that elevated transaminases, bilirubin, and alkaline phosphatase have occurred in patients with chronic liver disease or cirrhosis.
Duloxetine increased the risk of elevation of serum transaminase levels in development program clinical trials. Liver transaminase elevations resulted in the discontinuation of 0.3% (89/29,435) of duloxetine -treated patients. In most patients, the median time to detection of the transaminase elevation was about two months. In placebo-controlled trials in any indication, for patients with normal and abnormal baseline ALT values, elevation of ALT >3 times the upper limit of normal occurred in 1.37% (132/9611) of duloxetine -treated patients compared to 0.49% (35/7182 of placebo-treated patients. In placebo-controlled studies using a fixed dose design, there was evidence of a dose response relationship for ALT and AST elevation of >3 times the upper limit of normal and >5 times the upper limit of normal, respectively.
Because it is possible that duloxetine and alcohol may interact to cause liver injury or that duloxetine may aggravate pre-existing liver disease, duloxetine should not be prescribed to patients with substantial alcohol use or evidence of chronic liver disease.
5.3 Orthostatic Hypotension and Syncope
Orthostatic hypotension and syncope have been reported with therapeutic doses of duloxetine. Syncope and orthostatic hypotension tend to occur within the first week of therapy but can occur at any time during duloxetine treatment, particularly after dose increases. The risk of blood pressure decreases may be greater in patients taking concomitant medications that induce orthostatic hypotension (such as antihypertensives) or are potent CYP1A2 inhibitors [see and ] and in patients taking duloxetine at doses above 60 mg daily. Consideration should be given to discontinuing duloxetine in patients who experience symptomatic orthostatic hypotension and/or syncope during duloxetine therapy. Orthostatic hypotension and syncope have been reported with therapeutic doses of duloxetine. Syncope and orthostatic hypotension tend to occur within the first week of therapy but can occur at any time during duloxetine treatment, particularly after dose increases. The risk of blood pressure decreases may be greater in patients taking concomitant medications that induce orthostatic hypotension (such as antihypertensives) or are potent CYP1A2 inhibitors [see Warnings and Precautions ( 5.12) and Drug Interactions ( 7.1) ] and in patients taking duloxetine at doses above 60 mg daily. Consideration should be given to discontinuing duloxetine in patients who experience symptomatic orthostatic hypotension and/or syncope during duloxetine therapy.
5.4 Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with SNRIs and SSRIs, including duloxetine, alone but particularly with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. John’s Wort) and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome.
The concomitant use of duloxetine with MAOIs intended to treat psychiatric disorders is contraindicated. Duloxetine should also not be started in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with an MAOI such as linezolid or intravenous methylene blue in a patient taking duloxetine. Duloxetine should be discontinued before initiating treatment with the MAOI [see DOSAGE AND ADMINISTRATION ( 2.5, 2.6), and CONTRAINDICATIONS ( 4.1) ].
If concomitant use of duloxetine with other serotonergic drugs including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, tryptophan and St. John’s Wort is clinically warranted, patients should be made aware of a potential increased risk for serotonin syndrome, particularly during treatment initiation and dose increases. Treatment with duloxetine and any concomitant serotonergic agents, should be discontinued immediately if the above events occur and supportive symptomatic treatment should be initiated.
5.5 Abnormal Bleeding
SSRIs and SNRIs, including duloxetine , may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs, warfarin, and other anti-coagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to SSRIs and SNRIs use have ranged from ecchymoses, hematomas, epistaxis, and petechiae to life-threatening hemorrhages. SSRIs and SNRIs, including duloxetine , may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs, warfarin, and other anti-coagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to SSRIs and SNRIs use have ranged from ecchymoses, hematomas, epistaxis, and petechiae to life-threatening hemorrhages.
Patients should be cautioned about the risk of bleeding associated with the concomitant use of duloxetine and NSAIDs, aspirin, or other drugs that affect coagulation.Patients should be cautioned about the risk of bleeding associated with the concomitant use of duloxetine and NSAIDs, aspirin, or other drugs that affect coagulation.
5.6 Severe Skin Reactions
Severe skin reactions, including erythema multiforme and Stevens-Johnson Syndrome (SJS), can occur with duloxetine. The reporting rate of SJS associated with duloxetine use exceeds the general population background incidence rate for this serious skin reaction (1 to 2 cases per million person years). The reporting rate is generally accepted to be an underestimate due to underreporting.
Duloxetine should be discontinued at the first appearance of blisters, peeling rash, mucosal erosions, or any other sign of hypersensitivity if no other etiology can be identified.
5.7 Discontinuation of Treatment with Duloxetine
Discontinuation symptoms have been systematically evaluated in patients taking duloxetine. Following abrupt or tapered discontinuation in placebo-controlled clinical trials, the following symptoms occurred at 1% or greater and at a significantly higher rate in duloxetine -treated patients compared to those discontinuing from placebo: dizziness, headache, nausea, diarrhea, paresthesia, diarrhea, vomiting, insomnia, anxiety, hyperhidrosis and fatigue,
During marketing of other SSRIs and SNRIs (serotonin and norepinephrine reuptake inhibitors), there have been spontaneous reports of adverse events occurring upon discontinuation of these drugs, particularly when abrupt, including the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesias such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. Although these events are generally self-limiting, some have been reported to be severe.
Patients should be monitored for these symptoms when discontinuing treatment with duloxetine. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate [see DOSAGE AND ADMINISTRATION (2.4)].
5.8 Activation of Mania/Hypomania
In placebo-controlled trials in patients with major depressive disorder, activation of mania or hypomania was reported in 0.1% (2/2489) of duloxetine-treated patients and 0.1% (1/1625) of placebo-treated patients. No activation of mania or hypomania was reported in GAD, or chronic musculoskeletal pain placebo-controlled trials. Activation of mania or hypomania has been reported in a small proportion of patients with mood disorders who were treated with other marketed drugs effective in the treatment of major depressive disorder. As with these other agents, duloxetine should be used cautiously in patients with a history of mania.
5.9 Angle-Closure Glaucoma
Angle-Closure Glaucoma — The pupillary dilation that occurs following use of many antidepressant drugs including duloxetine may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
5.10 Seizures
Duloxetine has not been systematically evaluated in patients with a seizure disorder, and such patients were excluded from clinical studies. In placebo-controlled clinical trials, seizures/convulsions occurred in 0.03% (3/10,524) of patients treated with duloxetine and 0.01% (1/7699) of patients treated with placebo. Duloxetine should be prescribed with care in patients with a history of a seizure disorder.
5.11 Effect on Blood Pressure
In placebo-controlled clinical trials across indications from baseline to endpoint, duloxetine treatment was associated with mean increases of 0.5 mm Hg in systolic blood pressure and 0.8 mm Hg in diastolic blood pressure compared to mean decreases of 0.6 mm Hg systolic and 0.4 mm Hg diastolic in placebo-treated patients. There was no significant difference in the frequency of sustained (3 consecutive visits) elevated blood pressure. In a clinical pharmacology study designed to evaluate the effects of duloxetine on various parameters, including blood pressure at supratherapeutic doses with an accelerated dose titration, there was evidence of increases in supine blood pressure at doses up to 200 mg twice daily. At the highest 200 mg twice daily dose, the increase in mean pulse rate was 5.0 to 6.8 beats and increases in mean blood pressure were 4.7 to 6.8 mm Hg (systolic) and 4.5 to 7 mm Hg (diastolic) up to 12 hours after dosing.
Blood pressure should be measured prior to initiating treatment and periodically measured throughout treatment [see ADVERSE REACTIONS (6.7)]
5.12 Clinically Important Drug Interactions
Both CYP1A2 and CYP2D6 are responsible for duloxetine metabolism.
Potential for Other Drugs to Affect Duloxetine
CYP1A2 Inhibitors — Co-administration of duloxetine with potent CYP1A2 inhibitors should be avoided [see Drug Interactions (7.1)].
CYP2D6 Inhibitors — Because CYP2D6 is involved in duloxetine metabolism, concomitant use of duloxetine with potent inhibitors of CYP2D6 would be expected to, and does, result in higher concentrations (on average of 60%) of duloxetine [see Drug Interactions (7.2)].
Potential for Duloxetine to Affect Other Drugs
Drugs Metabolized by CYP2D6 — Co-administration of duloxetine with drugs that are extensively metabolized by CYP2D6 and that have a narrow therapeutic index, including certain antidepressants (tricyclic antidepressants [TCAs], such as nortriptyline, amitriptyline, and imipramine), phenothiazines and Type 1C antiarrhythmics (e.g., propafenone, flecainide), should be approached with caution. Plasma TCA concentrations may need to be monitored and the dose of the TCA may need to be reduced if a TCA is co-administered with duloxetine. Because of the risk of serious ventricular arrhythmias and sudden death potentially associated with elevated plasma levels of thioridazine, duloxetine and thioridazine should not be co-administered [see Drug Interactions (7.9)].
Other Clinically Important Drug Interactions
Alcohol —Use of duloxetine concomitantly with heavy alcohol intake may be associated with severe liver injury. For this reason, duloxetine should not be prescribed for patients with substantial alcohol use [see Warnings and Precautions (5.2) and Drug Interactions (7.15)].
CNS Acting Drugs — Given the primary CNS effects of duloxetine, it should be used with caution when it is taken in combination with or substituted for other centrally acting drugs, including those with a similar mechanism of action [see Warnings and Precautions ( 5.12) and Drug Interactions (7.16)] .
5.13 Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including duloxetine. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/Lhave been reported and appeared to be reversible when duloxetine was discontinued. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics or who are otherwise volume depleted may be at greater risk [see ]. Discontinuation of duloxetine should be considered in patients with symptomatic hyponatremia and appropriate medical intervention should be instituted. Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including duloxetine. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/Lhave been reported and appeared to be reversible when duloxetine was discontinued. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics or who are otherwise volume depleted may be at greater risk [see USE IN SPECIFIC POPULATIONS (8.5)]. Discontinuation of duloxetine should be considered in patients with symptomatic hyponatremia and appropriate medical intervention should be instituted.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. More severe and/or acute cases have been associated with hallucination, syncope, seizure, coma, respiratory arrest, and death.Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. More severe and/or acute cases have been associated with hallucination, syncope, seizure, coma, respiratory arrest, and death.
5.14 Use in Patients with Concomitant Illness
Clinical experience with duloxetine in patients with concomitant systemic illnesses is limited. There is no information on the effect that alterations in gastric motility may have on the stability of duloxetine’s enteric coating. In extremely acidic conditions, duloxetine, unprotected by the enteric coating, may undergo hydrolysis to form naphthol. Caution is advised in using duloxetine in patients with conditions that may slow gastric emptying (e.g., some diabetics).
Duloxetine has not been systematically evaluated in patients with a recent history of myocardial infarction or unstable coronary artery disease. Patients with these diagnoses were generally excluded from clinical studies during the product’s premarketing testing.
Hepatic Insufficiency – Duloxetine should ordinarily not be used in patients with hepatic insufficiency [see Dosage and Administration ( 2.3) , Warnings and Precautions ( 5.2) , and Use In Specific Populations ( 8.9) ].
Severe Renal Impairment — Duloxetine should ordinarily not be used in patients with end-stage renal disease or severe renal impairment (creatinine clearance <30 mL/min). Increased plasma concentration of duloxetine, and especially of its metabolites, occur in patients with end-stage renal disease (requiring dialysis) [see Dosage and Administration ( 2.3) and Use In Specific Populations ( 8.10) ].
Glycemic Control in Patients with Diabetes — As observed in DPNP trials, duloxetine treatment worsens glycemic control in some patients with diabetes. In three clinical trials of duloxetine for the management of neuropathic pain associated with diabetic peripheral neuropathy, the mean duration of diabetes was approximately 12 years, the mean baseline fasting blood glucose was 176 mg/dL, and the mean baseline hemoglobin A 1c (HbA 1c) was 7.8%. In the 12-week acute treatment phase of these studies, duloxetine was associated with a small increase in mean fasting blood glucose as compared to placebo. In the extension phase of these studies, which lasted up to 52 weeks, mean fasting blood glucose increased by 12 mg/dL in the duloxetine group and decreased by 11.5 mg/dL in the routine care group. HbA 1c increased by 0.5% in the duloxetine and by 0.2% in the routine care groups.
5.15 Urinary Hesitation and Retention
Duloxetine is in a class of drugs known to affect urethral resistance. If symptoms of urinary hesitation develop during treatment with duloxetine, consideration should be given to the possibility that they might be drug-related.
In post marketing experience, cases of urinary retention have been observed. In some instances of urinary retention associated with duloxetine use, hospitalization and/or catheterization has been needed.
6 ADVERSE REACTIONS
6.1 Clinical Trial Data Sources
The data described below reflect exposure to duloxetine in placebo-controlled trials for MDD (N=2489), GAD (N=910), OA (N=239), CLBP (N=600) and DPNP (N=906). The population studied was 17 to 91 years of age; 65.5%, 62.5%, 61.5% and 42.9% female; and 86.5%, 81.2%, 86.2% and 74% Caucasian for MDD, GAD, OA and CLBP and DPNP respectively. Most patients received doses of a total of 60 to 120 mg per day [see CLINICAL STUDIES (14)].
The stated frequencies of adverse reactions represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse reaction of the type listed. A reaction was considered treatment-emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation. Reactions reported during the studies were not necessarily caused by the therapy, and the frequencies do not reflect investigator impression (assessment) of causality.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.2 Adverse Reactions Reported as Reasons for Discontinuation of Treatment in Placebo-Controlled Trials
Major Depressive Disorder — Approximately 9% (209/2327) of the patients who received duloxetine in placebo-controlled trials for MDD discontinued treatment due to an adverse reaction, compared with 4.7% (68/1460) of the patients receiving placebo. Nausea (duloxetine 1.3%, placebo 0.5%) was the only common adverse reaction reported as a reason for discontinuation and considered to be drug-related (i.e., discontinuation occurring in at least 1% of the duloxetine-treated patients and at a rate of at least twice that of placebo).
Generalized Anxiety Disorder — Approximately 15.3% (102/668) of the patients who received duloxetine in placebo-controlled trials for GAD discontinued treatment due to an adverse reaction, compared with 4% (20/495) for placebo. Common adverse reactions reported as a reason for discontinuation and considered to be drug-related (as defined above) included nausea (duloxetine 3.7%, placebo 0.2%), and vomiting (duloxetine 1.3%, placebo 0%), and dizziness (duloxetine 1%, placebo 0.2%).
Diabetic Peripheral Neuropathic Pain — Approximately 12.9% (117/906) of the patients who received duloxetine in placebo-controlled trials for DPNP discontinued treatment due to an adverse reaction, compared with 5.1% (23/448) for placebo. Common adverse reactions reported as a reason for discontinuation and considered to be drug-related (as defined above) included nausea (duloxetine 3.5%, placebo 0.7%), dizziness (duloxetine 1.2%, placebo 0.4%), and somnolence (duloxetine 1.1%, placebo 0%).
Chronic Pain due to Osteoarthritis — Approximately 16.3% (39/239) of the patients who received duloxetine in 13 week, placebo-controlled trials for chronic pain due to OA discontinued treatment due to an adverse reaction, compared with 5.6% (14/248) for placebo. Common adverse reactions reported as a reason for discontinuation and considered to be drug-related (as defined above) included nausea (duloxetine 2.9%, placebo 0.8%) and asthenia (duloxetine 1.3%, placebo 0%).
Chronic Low Back Pain — Approximately 16.5% (99/600) of the patients who received duloxetine in 13-week, placebo-controlled trials for CLBP discontinued treatment due to an adverse reaction, compared with 6.3% (28/441) for placebo. Common adverse reactions reported as a reason for discontinuation and considered to be drug-related (as defined above) included nausea (duloxetine 3%, placebo 0.7%), and somnolence (duloxetine 1%, placebo 0%).
6.3 Most Common Adverse Reactions
Pooled Trials for all Approved Indications — The most commonly observed adverse reactions in duloxetine -treated patients (incidence of at least 5% and at least twice the incidence in placebo patients) were nausea, dry mouth, somnolence, constipation, decreased appetite, and hyperhidrosis.
Diabetic Peripheral Neuropathic Pain — The most commonly observed adverse reactions in duloxetine treated patients (as defined above) were nausea, somnolence, decreased appetite, constipation, hyperhidrosis, and dry mouth.
Chronic Pain due to Osteoarthritis — The most commonly observed adverse reactions in duloxetine-treated patients (as defined above) were nausea, fatigue, and constipation.
Chronic Low Back Pain — The most commonly observed adverse reactions in duloxetine-treated patients (as defined above) were nausea, dry mouth, insomnia, somnolence, constipation, dizziness, and fatigue.
6.4 Adverse Reactions Occurring at an Incidence of 5% or More among Duloxetine-Treated Patients in Placebo-Controlled Trials
Table 2 gives the incidence of treatment-emergent adverse reactions in placebo-controlled trials for approved indications that occurred in 5% or more of patients treated with duloxetine and with an incidence greater than placebo.
Table 2: Treatment-Emergent Adverse Reactions: Incidence of 5% or More in Placebo-Controlled Trials of Approved Indications a
| Percentage of Patients Reporting Reaction | ||
| Adverse Reaction | Duloxetine(N=6020) | Placebo(N=3962) |
| Nausea | 24 | 8 |
| Headache | 14 | 13 |
| Dry mouth | 13 | 5 |
| Fatigue b | 10 | 5 |
| Somnolence c,e | 10 | 3 |
| Insomnia c,d | 10 | 6 |
| Dizziness | 10 | 5 |
| Constipation c | 10 | 4 |
| Diarrhea | 9 | 6 |
| Decreased appetite c,f | 8 | 2 |
| Hyperhidrosis | 7 | 2 |
a The inclusion of an event in the table is determined based on the percentages before rounding; however, the percentages displayed in the table are rounded to the nearest integer.
b Also includes asthenia
c Events for which there was a significant dose-dependent relationship in fixed-dose studies, excluding three MDD studies which did not have a placebo lead-in period or dose titration.
d Also includes middle insomnia, early morning awakening, and initial insomnia
e Also includes hypersomnia and sedation
f Also includes anorexia
6.5 Adverse Reactions Occurring at an Incidence of 2% or More Among Duloxetine-Treated Patients in Placebo-Controlled Trials
Pooled MDD and GAD Trials— Table 3 gives the incidence of treatment-emergent adverse reactions in MDD and GAD placebo-controlled trials for approved indications that occurred in 2% or more of patients treated with duloxetine and with an incidence greater than placebo.
Table 3: Treatment-Emergent Adverse Reactions: Incidence of 2% or More in MDD and GAD Placebo-Controlled Trials
| System Organ Class / Adverse Reaction | Percentage of Patients Reporting Reaction | |
| Duloxetine (N=2995) | Placebo (N=1955) | |
| Cardiac Disorders
Palpitations | 2 | 2 |
| Eye Disorders
Vision blurred | 3 | 2 |
| Gastrointestinal Disorders
Nausea Dry mouth Diarrhea Constipation b Abdominal pain c Vomiting |
25 15 10 10 4 5 |
9 6 7 4 4 2 |
| General Disorders and Administration Site Conditions
Fatigue d | 10 | 6 |
| Investigations
Weight decreased b | 2 | <1 |
| Metabolism and Nutrition Disorders
Decreased appetite e | 7 | 2 |
| Nervous System Disorders | ||
| Dizziness
Somnolence f Tremor | 10
10 3 | 6
4 <1 |
| Psychiatric Disorders | ||
| Insomnia
g
Agitation h Anxiety Libido decreased i Orgasm abnormal j Abnormal dreams k | 10
5 3 4 3 2 | 6
3 2 1 <1 1 |
| Reproductive System and Breast Disorders
Erectile dysfunction l Ejaculation delayed b,j Ejaculation disorder l,m |
4 3 2 |
1 <1 <1 |
| Respiratory, Thoracic, and Mediastinal Disorders
Yawning | 2 | <1 |
| Skin and Subcutaneous Tissue Disorders
Hyperhidrosis | 6 | 2 |
| Vascular Disorders
Hot Flush | 2 | <1 |
a The inclusion of an event in the table is determined based on the percentages before rounding; however, the percentages displayed in the table are rounded to the nearest integer.
b Events for which there was a significant dose-dependent relationship in fixed-dose studies, excluding three MDD studies which did not have a placebo lead-in period or dose titration.
c Also includes abdominal pain upper, abdominal pain lower, abdominal tenderness, abdominal discomfort, and gastrointestinal pain
d Also includes asthenia
e Also includes anorexia
fAlso includes hypersomnia and sedation
g Also includes middle insomnia, early morning awakening, and initial insomnia
h Also includes feeling jittery, nervousness, restlessness, tension, and psychomotor agitation
i Also includes loss of libido
j Also includes anorgasmia
k Also includes nightmare
l Male patients only
m Also includes ejaculation failure and ejaculation dysfunction
DPNP, OA, and CLBP — Table 4 gives the incidence of treatment-emergent adverse events that occurred in 2% or more of patients treated with duloxetine (determined prior to rounding) in the premarketing acute phase of DPNP, OA, and CLBP placebo-controlled trials and with an incidence greater than placebo.
Table 4: Treatment-Emergent Adverse Reactions Incidence of 2% or More in DPNP, OA, and CLBP Placebo-Controlled Trials a
| System Organ Class / Adverse Reaction | Percentage of Patients Reporting Reaction | |
| Duloxetine(N=2621) | Placebo(N=1672) | |
| Gastrointestinal Disorders | ||
| Nausea | 23 | 7 |
| Dry Mouth b | 11 | 3 |
| Constipation b | 10 | 3 |
| Diarrhea | 9 | 6 |
| Abdominal Pain c | 6 | 5 |
| Vomiting | 3 | 2 |
| Dyspepsia d | 2 | 1 |
| General Disorders and Administration Site Conditions
Fatigue e | 11 | 5 |
| Infections and Infestations | ||
| Nasopharyngitis | 5 | 4 |
| Upper Respiratory Tract Infection | 4 | 4 |
| Influenza | 3 | 2 |
| Metabolism and Nutrition Disorders
Decreased Appetite b,f | 9 | 1 |
| Musculoskeletal and Connective Tissue Disorders | ||
| Musculoskeletal Pain b,g | 4 | 4 |
| Muscle Spasms | 3 | 2 |
| Nervous System Disorders | ||
| Headache | 13 | 9 |
| Somnolence b,h | 12 | 3 |
| Dizziness | 10 | 5 |
| Paraesthesia i | 2 | 2 |
| Tremor b | 2 | <1 |
| Psychiatric Disorders
Insomnia b,j Agitation k | 10
3 | 6
<1 |
| Reproductive System and Breast Disorders
Erectile dysfunction b,j Ejaculation Disorder m | 4
2 | <1
<1 |
| Respiratory, Thoracic and Mediastinal Disorders | ||
| Cough | 3 | 2 |
| Oropharyngeal Pain b | 2 | 2 |
| Skin and Subcutaneous | ||
| Tissue Disorders | ||
| Hyperhidrosis | 6 | 1 |
| Vascular Disorders | ||
| Flushing n | 3 | 1 |
a The inclusion of an event in the table is determined based on the percentages before rounding; however, the percentages displayed in the table are rounded to the nearest integer.
b Incidence of 120 mg/day is significantly greater than the incidence for 60 mg/day.
c Also includes abdominal discomfort, abdominal pain lower, abdominal pain upper, abdominal tenderness and gastrointestinal pain
d Also includes stomach discomfort
e Also includes asthenia
f Also includes anorexia
g Also includes myalgia and neck pain
h Also includes hypersomnia and sedation
i Also includes hypoaesthesia, hypoaesthesia facial and paraethesia oral
j Also includes middle insomnia, early morning awakening, and initial insomnia
k Also includes feeling jittery, nervousness, restlessness, tension and psychomotor hyperactivity
l Male patients only (N=885 for duloxetine , 494 for placebo)
m Male patients only (N=885 for duloxetine , 494 for placebo). Also includes ejaculation failure
n Also includes hot flush
6.6 Effects on Male and Female Sexual Function
Changes in sexual desire, sexual performance and sexual satisfaction often occur as manifestations of psychiatric disorders or diabetes, but they may also be a consequence of pharmacologic treatment. Because adverse sexual reactions are presumed to be voluntarily underreported, the Arizona Sexual Experience Scale (ASEX), a validated measure designed to identify sexual side effects, was used prospectively in 4 MDD placebo-controlled trials. In these trials, as shown in Table 5 below, patients treated with duloxetine experienced significantly more sexual dysfunction, as measured by the total score on the ASEX, than did patients treated with placebo. Gender analysis showed that this difference occurred only in males. Males treated with duloxetine experienced more difficulty with ability to reach orgasm (ASEX Item 4) than males treated with placebo. Females did not experience more sexual dysfunction on duloxetine than on placebo as measured by ASEX total score. Negative numbers signify an improvement from a baseline level of dysfunction, which is commonly seen in depressed patients. Physicians should routinely inquire about possible sexual side effects.
| Male Patients * | Female Patients * | |||
|---|---|---|---|---|
| Duloxetine | Placebo | Duloxetine | Placebo | |
| (n=175) | (n=83) | (n=241) | (n=126) | |
| ASEX Total (Items 1-5) | 0.56 † | -1.07 | -1.15 | -1.07 |
| Item 1 — Sex drive | -0.07 | -0.12 | -0.32 | -0.24 |
| Item 2 — Arousal | 0.01 | -0.26 | -0.21 | -0.18 |
| Item 3 — Ability to achieve | 0.03 | -0.25 | -0.17 | -0.18 |
| erection (men); Lubrication (women) | ||||
| Item 4 — Ease of reaching orgasm | 0.40 ‡ | -0.24 | -0.09 | -0.13 |
| Item 5 — Orgasm satisfaction | 0.09 | -0.13 | -0.11 | -0.17 |
6.7 Vital Sign Changes
In placebo-controlled clinical trials across approved indications for change from baseline to endpoint, duloxetine treatment was associated with mean increases of 0.07 mm Hg in systolic blood pressure and 0.62 mm Hg in diastolic blood pressure compared to mean decreases of 1.31 mm Hg systolic and 0.73 mm Hg diastolic in placebo-treated patients. There was no significant difference in the frequency of sustained (3 consecutive visits) elevated blood pressure [see WARNINGS AND PRECAUTIONS ( 5.3 and 5.10 ) ].
Duloxetine treatment, for up to 26 weeks in placebo-controlled trials typically caused a small increase in heart rate across approved indications, typically caused a small increase in heart rate for change from baseline to endpoint compared to placebo of up to 1.40 beats per minute.
6.8 Weight Changes
In placebo-controlled clinical trials, MDD and GAD patients treated with duloxetine for up to 10 weeks experienced a mean weight loss of approximately 0.5 kg, compared with a mean weight gain of approximately 0.2 kg in placebo-treated patients. In studies of DPNP, OA, and CLBP patients treated with duloxetine for up to 26 weeks experienced a mean weight loss of approximately 0.6 kg, compared with a mean weight gain of approximately 0.2 kg in placebo-treated patients. In one long-term CLBP 54-week study (13-week, placebo-controlled acute phase and 41-week, uncontrolled extension phase), duloxetine patients had a mean weight decrease of 0.6 kg in 13 weeks of acute phase compared to study entry, then a mean weight increase of 1.4 kg in 41 weeks of extension phase compared to end of acute phase.
6.9 Laboratory Changes
Duloxetine treatment in placebo-controlled clinical trials across approved indications,, was associated with small mean increases from baseline to endpoint in ALT, AST, CPK, and alkaline phosphatase; infrequent, modest, transient, abnormal values were observed for these analytes in duloxetine -treated patients when compared with placebo-treated patients [see WARNINGS AND PRECAUTIONS (5.2)].
6.10 Electrocardiogram Changes
The effect of duloxetine 160 mg and 200 mg administered twice daily to steady state was evaluated in a randomized, double-blinded, two-way crossover study in 117 healthy female subjects. No QT interval prolongation was detected. Duloxetine appears to be associated with concentration-dependent but not clinically meaningful QT shortening.
6.11 Other Adverse Reactions Observed During the Premarketing and Postmarketing Clinical Trial Evaluation of Duloxetine
Following is a list of treatment-emergent adverse reactions reported by patients treated with duloxetine in clinical trials. In clinical trials of all indications, 29,435 patients were treated with duloxetine . Of these,30.4% (8953) took duloxetine for at least 6 months, and 14.7% (4317) for at least one year. The following listing is not intended to include reactions (1) already listed in previous tables or elsewhere in labeling, (2) for which a drug cause was remote, (3) which were so general as to be uninformative, (4) which were not considered to have significant clinical implications, or (5) which occurred at a rate equal to or less than placebo.
Reactions are categorized by body system according to the following definitions: frequent adverse reactions are those occurring in at least 1/100 patients; infrequent adverse reactions are those occurring in 1/100 to 1/1000 patients; rare reactions are those occurring in fewer than 1/1000 patients.
Cardiac Disorders — Frequent: palpitations; Infrequent: myocardial infarction and tachycardia.
Ear and Labyrinth Disorders — Frequent: vertigo; Infrequent: ear pain and tinnitus.
Endocrine Disorders — Infrequent: hypothyroidism.
Eye Disorders — Frequent: vision blurred; Infrequent: diplopia and visual disturbance.
Gastrointestinal Disorders — Frequent: flatulence; Infrequent: eructation, gastritis, halitosis, and stomatitis; Rare: gastric ulcer, hematochezia, and melena.
General Disorders and Administration Site Conditions — Frequent: chills/rigors; Infrequent: feeling abnormal, feeling hot and/or cold, malaise, and thirst; Rare: gait disturbance.
Infections and Infestations — Infrequent: gastroenteritis and laryngitis.
Investigations — Frequent: weight increased; Infrequent: blood cholesterol increased.
Metabolism and Nutrition Disorders — Infrequent: dehydration and hyperlipidemia; Rare: dyslipidemia.
Musculoskeletal and Connective Tissue Disorders — Frequent: musculoskeletal pain; Infrequent: muscle tightness and muscle twitching.
Nervous System Disorders — Frequent: dysgeusia, lethargy, and parasthesia/hypoesthesia; Infrequent: disturbance in attention, dyskinesia, and myoclonus; and poor quality sleep, Rare: dysarthria.
Psychiatric Disorders — Frequent: abnormal dreams and sleep disorder; Infrequent: apathy, bruxism, disorientation/confusional state, irritability, mood swings, and suicide attempt; Rare: completed suicide.
Renal and Urinary Disorders — Infrequent: dysuria, micturition urgency, nocturia, polyuria, and urine odor abnormal.
Reproductive System and Breast Disorders — Frequent: anorgasmia/orgasm abnormal; Infrequent: menopausal symptoms, and sexual disfunction.
Respiratory, Thoracic and Mediastinal Disorders — Frequent: yawning; Infrequent: throat tightness.
Skin and Subcutaneous Tissue Disorders — Infrequent: cold sweat, dertermatitis contact erythema, increased tendency to bruise, night sweats, and photosensitivity reaction; Rare: ecchymosis.
Vascular Disorders — Frequent: hot flush; Infrequent: flushing, orthostatic hypotension, and peripheral coldness.
6.12 Postmarketing Spontaneous Reports
The following adverse reactions have been identified during postapproval use of duloxetine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse reactions reported since market introduction that were temporally related to duloxetine therapy and not mentioned elsewhere in labeling include: anaphylactic reaction, aggression and anger (particularly early in treatment or after treatment discontinuation), angioneurotic edema, angle-closure glaucoma, extrapyramidal disorder, galactorrhea, gynecological bleeding, hallucinations, hyperglycemia, hyperprolactinemia, hypersensitivity, hypertensive crisis, muscle spasm, rash, restless legs syndrome, seizures upon treatment discontinuation, supraventricular arrhythmia, tinnitus (upon treatment discontinuation), trismus, and urticaria.
7 DRUG INTERACTIONS
Both CYP1A2 and CYP2D6 are responsible for duloxetine metabolism.
7.1 Inhibitors of CYP1A2
Concomitant use of duloxetine (40 mg once daily) with paroxetine (20 mg once daily) increased the concentration of duloxetine AUC by about 60%, and greater degrees of inhibition are expected with higher doses of paroxetine. Similar effects would be expected with other potent CYP2D6 inhibitors (e.g., fluoxetine, quinidine) [see WARNINGS AND PRECAUTIONS ( 5.12) ].
7.2 Inhibitors of CYP2D6
Concomitant use of duloxetine (40 mg QD) with paroxetine (20 mg QD) increased the concentration of duloxetine AUC by about 60%, and greater degrees of inhibition are expected with higher doses of paroxetine. Similar effects would be expected with other potent CYP2D6 inhibitors (e.g., fluoxetine, quinidine) [see Warnings and Precautions (5.12) ].
7.3 Dual Inhibition of CYP1A2 and CYP2D6
Concomitant administration of duloxetine 40 mg twice daily with fluvoxamine 100 mg, a potent CYP1A2 inhibitor, to CYP2D6 poor metabolizer subjects (n=14) resulted in a 6-fold increase in duloxetine AUC and C max.
7.4 Drugs that Interfere with Hemostasis (e.g., NSAIDs, Aspirin, and Warfarin)
Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies of the case-control and cohort design that have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. These studies have also shown that concurrent use of an NSAID or aspirin may potentiate this risk of bleeding. Altered anticoagulant effects, including increased bleeding, have been reported when SSRIs or SNRIs are coadministered with warfarin. Concomitant administration of warfarin (2 to 9 mg once daily) under steady state conditions with duloxetine 60 or 120 mg once daily for up to 14 days in healthy subjects (n=15) did not significantly change INR from baseline (mean INR changes ranged from 0.05 to +0.07). The total warfarin (protein bound plus free drug) pharmacokinetics (AUC τ,ss, C max,ss or t max,ss) for both R- and S-warfarin were not altered by duloxetine. Because of the potential effect of duloxetine on platelets, patients receiving warfarin therapy should be carefully monitored when duloxetine is initiated or discontinued [see WARNINGS AND PRECAUTIONS (5.5)].
7.5 Lorazepam
Under steady-state conditions for duloxetine (60 mg Q 12 hours) and lorazepam (2 mg Q 12 hours), the pharmacokinetics of duloxetine were not affected by co-administration.
7.6 Temazepam
Under steady-state conditions for duloxetine (20 mg qhs) and temazepam (30 mg qhs), the pharmacokinetics of duloxetine were not affected by co-administration.
7.7 Drugs that Affect Gastric Acidity
Duloxetine has an enteric coating that resists dissolution until reaching a segment of the gastrointestinal tract where the pH exceeds 5.5. In extremely acidic conditions, duloxetine , unprotected by the enteric coating, may undergo hydrolysis to form naphthol. Caution is advised in using duloxetine in patients with conditions that may slow gastric emptying (e.g., some diabetics). Drugs that raise the gastrointestinal pH may lead to an earlier release of duloxetine . However, co-administration of duloxetine with aluminum- and magnesium-containing antacids (51 mEq) or duloxetine with famotidine, had no significant effect on the rate or extent of duloxetine absorption after administration of a 40 mg oral dose. It is unknown whether the concomitant administration of proton pump inhibitors affects duloxetine absorption [see Warnings and Precautions (5.14)]
7.8 Drugs Metabolized by CYP1A2
In vitro drug interaction studies demonstrate that duloxetine does not induce CYP1A2 activity. Therefore, an increase in the metabolism of CYP1A2 substrates (e.g., theophylline, caffeine) resulting from induction is not anticipated, although clinical studies of induction have not been performed. Duloxetine is an inhibitor of the CYP1A2 isoform in in vitro studies, and in two clinical studies the average (90% confidence interval) increase in theophylline AUC was 7% (1%-15%) and 20% (13%-27%) when co-administered with duloxetine (60 mg twice daily).
7.9 Drugs Metabolized by CYP2D6
Duloxetine is a moderate inhibitor of CYP2D6. When duloxetine was administered (at a dose of 60 mg twice daily) in conjunction with a single 50 mg dose of desipramine, a CYP2D6 substrate, the AUC of desipramine increased 3-fold [see Warnings and Precautions ( 5.12) ]
7.10 Drugs Metabolized by CYP2C9
Results of in vitro studies demonstrate that duloxetine does not inhibit activity. In a clinical study, the pharmacokinetics of S-warfarin, a CYP2C9 substrate, were not significantly affected by duloxetine [see DRUG INTERACTIONS (7.4)].
7.11 Drugs Metabolized by CYP3A
Results of in vitro studies demonstrate that duloxetine does not inhibit or induce CYP3A activity. Therefore, an increase or decrease in the metabolism of CYP3A substrates (e.g., oral contraceptives and other steroidal agents) resulting from induction or inhibition is not anticipated, although clinical studies have not been performed.
7.12 Drugs Metabolized by CYP2C19
Results of in vitro studies demonstrate that duloxetine does not inhibit CYP2C19 activity at therapeutic concentrations. Inhibition of the metabolism of CYP2C19 substrates is therefore not anticipated, although clinical studies have not been performed.
7.13 Monoamine Oxidase Inhibitors
[see DOSAGE AND ADMINISTRATION (2.5), CONTRAINDICATIONS (4.1), and WARNINGS AND PRECAUTIONS (5.4)].
7.14 Serotonergic Drugs
[see DOSAGE AND ADMINISTRATION ( 2.5, 2.6), CONTRAINDICATIONS (4.1) , and WARNINGS AND PRECAUTIONS ( 5.4) ].
7.15 Alcohol
When duloxetine and ethanol were administered several hours apart so that peak concentrations of each would coincide, duloxetine did not increase the impairment of mental and motor skills caused by alcohol.
In the duloxetine clinical trials database, three duloxetine -treated patients had liver injury as manifested by ALT and total bilirubin elevations, with evidence of obstruction. Substantial intercurrent ethanol use was present in each of these cases, and this may have contributed to the abnormalities seen [see Warnings and Precautions ( 5.2 and 5.12) ].
7.17 Drugs Highly Bound to Plasma Protein
Because duloxetine is highly bound to plasma protein, administration of duloxetine to a patient taking another drug that is highly protein bound may cause increased free concentrations of the other drug, potentially resulting in adverse reactions. However, coadministration of duloxetine (60 or 120 mg) with warfarin (2 to 9 mg), a highly protein-bound drug, did not result in significant changes in INR and in the pharmacokinetics of either total S-or total R-warfarin (protein bound plus free drug) [see DRUG INTERACTIONS (7.4)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects, Pregnancy Category C — In animal reproduction studies, duloxetine has been shown to have adverse effects on embryo/fetal and postnatal development.
When duloxetine was administered orally to pregnant rats and rabbits during the period of organogenesis, there was no evidence of teratogenicity at doses up to 45 mg/kg/day (7 times the maximum recommended human dose [MRHD, 60 mg/day] and 4 times the human dose of 120 mg/day on a mg/m 2 basis, in rat; 15 times the MRHD and 7 times the human dose of 120 mg/day on a mg/m 2 basis in rabbit). However, fetal weights were decreased at this dose, with a no-effect dose of 10 mg/kg/day (2 times the MRHD and ≈1 times the human dose of 120 mg/day on a mg/m 2 basis in rats; 3 times the MRHD and 2 times the human dose of 120 mg/day on a mg/m 2 basis in rabbits).
When duloxetine was administered orally to pregnant rats throughout gestation and lactation, the survival of pups to 1 day postpartum and pup body weights at birth and during the lactation period were decreased at a dose of 30 mg/kg/day (5 times the MRHD and 2 times the human dose of 120 mg/day on a mg/m 2 basis); the no-effect dose was 10 mg/kg/day. Furthermore, behaviors consistent with increased reactivity, such as increased startle response to noise and decreased habituation of locomotor activity, were observed in pups following maternal exposure to 30 mg/kg/day. Post-weaning growth and reproductive performance of the progeny were not affected adversely by maternal duloxetine treatment.
There are no adequate and well-controlled studies in pregnant women; therefore, duloxetine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nonteratogenic Effects — Neonates exposed to SSRIs or serotonin and norepinephrine reuptake inhibitors (SNRIs), late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are consistent with either a direct toxic effect of SSRIs and SNRIs or, possibly, a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome [see WARNINGS AND PRECAUTIONS (5.4)] .
When treating pregnant women with duloxetine during the third trimester, the physician should carefully consider the potential risks and benefits of treatment. The physician may consider tapering duloxetine in the third trimester [see DOSAGE AND ADMINISTRATION (2.3)] .
.
8.2 Labor and Delivery
The effect of duloxetine on labor and delivery in humans is unknown. Duloxetine should be used during labor and delivery only if the potential benefit justifies the potential risk to the fetus.
8.3 Nursing Mothers
Duloxetine is excreted into the milk of lactating women. The estimated daily infant dose on a mg/kg basis is approximately 0.14% of the maternal dose. Because the safety of duloxetine in infants is not known, nursing while on duloxetine is not recommended. However, if the physician determines that the benefit of duloxetine therapy for the mother outweighs any potential risk to the infant, no dosage adjustment is required as lactation did not influence duloxetine pharmacokinetics.
The disposition of duloxetine was studied in 6 lactating women who were at least 12 weeks postpartum. Duloxetine 40 mg twice daily was given for 3.5 days. Like many other drugs, duloxetine is detected in breast milk, and steady state concentrations in breast milk are about one-fourth those in plasma. The amount of duloxetine in breast milk is approximately 7 mcg/day while on 40 mg BID dosing. The excretion of duloxetine metabolites into breast milk was not examined. Because the safety of duloxetine in infants is not known, nursing while on duloxetine is not recommended [ see Dosage and Administration (2.3)].
8.4 Pediatric Use
Safety and effectiveness in the pediatric population has not been established [see Boxed Warning and Warnings and Precautions (5. 1)].
Decreased appetite and weight loss have been observed in association with the use of SSRIs and SNRls. Perform regular monitoring of weight and growth in children and adolescents treated with an SNRI such as duloxetine delayed-release capsules.
Duloxetine administration to young rats from post-natal day 21 (weaning) through post-natal day 90 (adult) resulted in decreased body weights that persisted into adulthood, but recovered when drug treatment was discontinued; slightly delayed (~1.5 days) sexual maturation in females, without any effect on fertility; and a delay in learning a complex task in adulthood, which was not observed after drug treatment was discontinued. These effects were observed at the high dose of 45 mg/kg/day; the no-effect-level was 20 mg/kg/day.
Information describing two additional clinical studies performed by Eli Lilly and Company that failed to demonstrate pediatric efficacy is approved for Eli Lilly and Company's Duloxetine Delayed-Release Capsules. However, due to Eli Lilly and Company's marketing exclusivity rights, this drug product is not labeled with that pediatric information.
8.5 Geriatric Use
Of the 2,418 patients in premarketing clinical studies of duloxetine for MDD, 5.9% (143) were 65 years of age or over. Of the 1041 patients in CLBP premarketing studies, 21.2% (221) were 65 years of age or over. Of the 487 patients in OA premarketing studies, 40.5% (197) were 65 years of age or over. Of the 1,074 patients in the DPNP premarketing studies, 33% (357) were 65 years of age or over. Premarketing clinical studies of GAD did not include sufficient numbers of subjects age 65 or over to determine whether they respond differently from younger subjects. In the MDD and DPNP, OA and CLBP studies, no overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. SSRIs and SNRIs, including duloxetine have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse event [see Warnings and Precautions (5.13)].
The pharmacokinetics of duloxetine after a single dose of 40 mg were compared in healthy elderly females (65 to 77 years) and healthy middle-age females (32 to 50 years). There was no difference in the C max, but the AUC of duloxetine was somewhat (about 25%) higher and the half-life about 4 hours longer in the elderly females. Population pharmacokinetic analyses suggest that the typical values for clearance decrease by approximately 1% for each year of age between 25 to 75 years of age; but age as a predictive factor only accounts for a small percentage of between-patient variability. Dosage adjustment based on the age of the patient is not necessary [see Dosage and Administration (2.3)].
8.6 Gender
Duloxetine's half-life is similar in men and women. Dosage adjustment based on gender is not necessary.
8.7 Smoking Status
Duloxetine bioavailability (AUC) appears to be reduced by about one-third in smokers. Dosage modifications are not recommended for smokers.
8.9 Hepatic Insufficiency
Patients with clinically evident hepatic insufficiency have decreased duloxetine metabolism and elimination. After a single 20 mg dose of duloxetine , 6 cirrhotic patients with moderate liver impairment (Child-Pugh Class B) had a mean plasma duloxetine clearance about 15% that of age- and gender-matched healthy subjects, with a 5-fold increase in mean exposure (AUC). Although C max was similar to normals in the cirrhotic patients, the half-life was about 3 times longer [ see Dosage and Administration (2.3) and Warnings and Precautions (5.14) ].
8.10 Severe Renal Impairment
Limited data are available on the effects of duloxetine in patients with end-stage renal disease (ESRD). After a single 60 mg dose of duloxetine , C max and AUC values were approximately 100% greater in patients with end-stage renal disease receiving chronic intermittent hemodialysis than in subjects with normal renal function. The elimination half-life, however, was similar in both groups. The AUCs of the major circulating metabolites, 4-hydroxy duloxetine glucuronide and 5-hydroxy, 6-methoxy duloxetine sulfate, largely excreted in urine, were approximately 7- to 9-fold higher and would be expected to increase further with multiple dosing. Population PK analyses suggest that mild to moderate degrees of renal dysfunction (estimated CrCl 30-80 mL/min) have no significant effect on duloxetine apparent clearance [see Dosage and Administration ( 2.3) and Warnings and Precautions (5.14) ].
9 DRUG ABUSE AND DEPENDENCE
9.2 Abuse
In animal studies, duloxetine did not demonstrate barbiturate-like (depressant) abuse potential.
While duloxetine has not been systematically studied in humans for its potential for abuse, there was no indication of drug-seeking behavior in the clinical trials. However, it is not possible to predict on the basis of premarketing experience the extent to which a CNS active drug will be misused, diverted, and/or abused once marketed. Consequently, physicians should carefully evaluate patients for a history of drug abuse and follow such patients closely, observing them for signs of misuse or abuse of duloxetine (e.g., development of tolerance, incrementation of dose, drug-seeking behavior).
10 OVERDOSAGE
10.1 Signs and Symptoms
In postmarketing experience, fatal outcomes have been reported for acute overdoses, primarily with mixed overdoses, but also with duloxetine only, at doses as low as 1000 mg. Signs and symptoms of overdose (duloxetine alone or with mixed drugs) included somnolence, coma, serotonin syndrome, seizures, syncope, tachycardia, hypotension, hypertension and vomiting.
10.2 Management of Overdose
There is no specific antidote to duloxetine, but if serotonin syndrome ensues, specific treatment (such as with cyproheptadine and/or temperature control) may be considered. In case of acute overdose, treatment should consist of those general measures employed in the management of overdose with any drug.
An adequate airway, oxygenation, and ventilation should be assured, and cardiac rhythm and vital signs should be monitored. Induction of emesis is not recommended. Gastric lavage with a large-bore orogastric tube with appropriate airway protection, if needed, may be indicated if performed soon after ingestion or in symptomatic patients.
Activated charcoal may be useful in limiting absorption of duloxetine from the gastrointestinal tract. Administration of activated charcoal has been shown to decrease AUC and C max by an average of one-third, although some subjects had a limited effect of activated charcoal. Due to the large volume of distribution of this drug, forced diuresis, dialysis, hemoperfusion, and exchange transfusion are unlikely to be beneficial.
In managing overdose, the possibility of multiple drug involvement should be considered. A specific caution involves patients who are taking or have recently taken duloxetine and might ingest excessive quantities of a TCA. In such a case, decreased clearance of the parent tricyclic and/or its active metabolite may increase the possibility of clinically significant sequelae and extend the time needed for close medical observation [see WARNINGS AND PRECAUTIONS (5.4) and DRUG INTERACTIONS (7)]. The physician should consider contacting a poison control center for additional information on the treatment of any overdose. Telephone numbers for certified poison control centers are listed in the Physicians' Desk Reference (PDR).
11 DESCRIPTION
Duloxetine hydrochloride is a selective serotonin and norepinephrine reuptake inhibitor (SSNRI) for oral administration. Its chemical designation is (+)-( S)- N-methyl-γ-(1-naphthyloxy)-2-thiophenepropylamine hydrochloride. The molecular formula is C 18H 19NOS•HCl, which corresponds to a molecular weight of 333.88. The structural formula is:
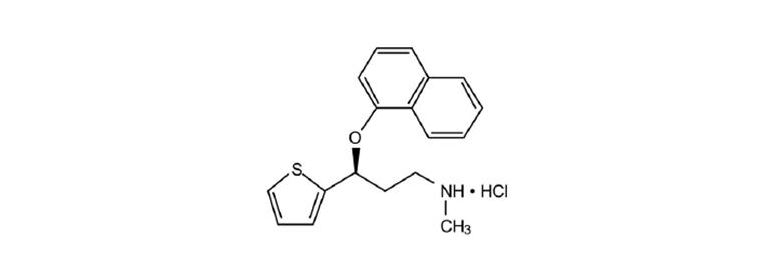
Duloxetine hydrochloride USP is a off-white to cream crystalline solid, soluble in methanol and chloroform slightly soluble in water.
Each capsule contains enteric-coated pellets of 22.4, 33.7, or 67.3 mg of duloxetine hydrochloride equivalent to 20, 30, or 60 mg of duloxetine, respectively. These enteric-coated pellets are designed to prevent degradation of the drug in the acidic environment of the stomach. Inactive Ingredients include: ammonia, FD&C Blue 2, gelatin, glycine, hypromellose phthalate, hypromellose, iron oxide yellow, propylene glycol, shellac, sodium lauryl sulfate, sucrose, sugar spheres (contains sugar and corn starch), talc, titanium dioxide, and triethyl citrate. The 20 mg capsules also contain black iron oxide and potassium hydroxide. The 60 mg capsules also contain potassium hydroxide.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Although the exact mechanisms of the antidepressant, central pain inhibitory and anxiolytic actions of duloxetine in humans are unknown, these actions are believed to be related to its potentiation of serotonergic and noradrenergic activity in the CNS.
12.2 Pharmacodynamics
Preclinical studies have shown that duloxetine is a potent inhibitor of neuronal serotonin and norepinephrine reuptake and a less potent inhibitor of dopamine reuptake. Duloxetine has no significant affinity for dopaminergic, adrenergic, cholinergic, histaminergic, opioid, glutamate, and GABA receptors in vitro. Duloxetine does not inhibit monoamine oxidase (MAO).
Duloxetine is in a class of drugs known to affect urethral resistance. If symptoms of urinary hesitation develop during treatment with duloxetine, consideration should be given to the possibility that they might be drug-related.
12.3 Pharmacokinetics
Duloxetine has an elimination half-life of about 12 hours (range 8 to 17 hours) and its pharmacokinetics are dose proportional over the therapeutic range. Steady-state plasma concentrations are typically achieved after 3 days of dosing. Elimination of duloxetine is mainly through hepatic metabolism involving two P450 isozymes, CYP1A2 and CYP2D6.
Absorption and Distribution — Orally administered duloxetine is well absorbed. There is a median 2-hour lag until absorption begins (T lag), with maximal plasma concentrations (C max) of duloxetine occurring 6 hours post dose. Food does not affect the C max of duloxetine, but delays the time to reach peak concentration from 6 to 10 hours and it marginally decreases the extent of absorption (AUC) by about 10%. There is a 3-hour delay in absorption and a one-third increase in apparent clearance of duloxetine after an evening dose as compared to a morning dose.
The apparent volume of distribution averages about 1640 L. Duloxetine is highly bound (>90%) to proteins in human plasma, binding primarily to albumin and α 1-acid glycoprotein. The interaction between duloxetine and other highly protein bound drugs has not been fully evaluated. Plasma protein binding of duloxetine is not affected by renal or hepatic impairment.
Metabolism and Elimination — Biotransformation and disposition of duloxetine in humans have been determined following oral administration of 14C-labeled duloxetine. Duloxetine comprises about 3% of the total radiolabeled material in the plasma, indicating that it undergoes extensive metabolism to numerous metabolites. The major biotransformation pathways for duloxetine involve oxidation of the naphthyl ring followed by conjugation and further oxidation. Both CYP1A2 and CYP2D6 catalyze the oxidation of the naphthyl ring in vitro. Metabolites found in plasma include 4-hydroxy duloxetine glucuronide and 5-hydroxy, 6-methoxy duloxetine sulfate. Many additional metabolites have been identified in urine, some representing only minor pathways of elimination. Only trace (<1% of the dose) amounts of unchanged duloxetine are present in the urine. Most (about 70%) of the duloxetine dose appears in the urine as metabolites of duloxetine ; about 20% is excreted in the feces. Duloxetine undergoes extensive metabolism, but the major circulating metabolites have not been shown to contribute significantly to the pharmacologic activity of duloxetine.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis — Duloxetine was administered in the diet to mice and rats for 2 years.
In female mice receiving duloxetine at 140 mg/kg/day (11 times the maximum recommended human dose [MRHD, 60 mg/day] and 6 times the human dose of 120 mg/day on a mg/m 2 basis), there was an increased incidence of hepatocellular adenomas and carcinomas. The no-effect dose was 50 mg/kg/day (4 times the MRHD and 2 times the human dose of 120 mg/day on a mg/m 2 basis). Tumor incidence was not increased in male mice receiving duloxetine at doses up to 100 mg/kg/day (8 times the MRHD and 4 times the human dose of 120 mg/day on a mg/m 2 basis).
In rats, dietary doses of duloxetine up to 27 mg/kg/day in females (4 times the MRHD and 2 times the human dose of 120 mg/day on a mg/m 2 basis) and up to 36 mg/kg/day in males (6 times the MRHD and 3 times the human dose of 120 mg/day on a mg/m 2 basis) did not increase the incidence of tumors.
Mutagenesis — Duloxetine was not mutagenic in the in vitro bacterial reverse mutation assay (Ames test) and was not clastogenic in an in vivo chromosomal aberration test in mouse bone marrow cells. Additionally, duloxetine was not genotoxic in an in vitro mammalian forward gene mutation assay in mouse lymphoma cells or in an in vitro unscheduled DNA synthesis (UDS) assay in primary rat hepatocytes, and did not induce sister chromatid exchange in Chinese hamster bone marrow in vivo.
14 CLINICAL STUDIES
14.1 Major Depressive Disorder
The efficacy of duloxetine as a treatment for depression was established in 4 randomized, double-blind, placebo-controlled, fixed-dose studies in adult outpatients (18 to 83 years) meeting DSM-IV criteria for major depression. In 2 studies, patients were randomized to duloxetine 60 mg once daily (N=123 and N=128, respectively) or placebo (N=122 and N=139, respectively) for 9 weeks; in the third study, patients were randomized to duloxetine 20 or 40 mg twice daily (N=86 and N=91, respectively) or placebo (N=89) for 8 weeks; in the fourth study, patients were randomized to duloxetine 40 or 60 mg twice daily (N=95 and N=93, respectively) or placebo (N=93) for 8 weeks. There is no evidence that doses greater than 60 mg/day confer additional benefits.
In all 4 studies, duloxetine demonstrated superiority over placebo as measured by improvement in the 17-item Hamilton Depression Rating Scale (HAMD-17) total score.
In all of these clinical studies, analyses of the relationship between treatment outcome and age, gender, and race did not suggest any differential responsiveness on the basis of these patient characteristics.
In another study, 533 patients meeting DSM-IV criteria for MDD received duloxetine 60 mg once daily during an initial 12-week open-label treatment phase. Two hundred and seventy-eight patients who responded to open label treatment (defined as meeting the following criteria at weeks 10 and 12: a HAMD-17 total score ≤9, Clinical Global Impressions of Severity (CGI-S) ≤2, and not meeting the DSM IV criteria for MDD) were randomly assigned to continuation of duloxetine at the same dose (N=136) or to placebo (N=142) for 6 months. Patients on duloxetine experienced a statistically significantly longer time to relapse of depression than did patients on placebo. Relapse was defined as an increase in the CGI–S score of ≥2 points compared with that obtained at week 12, as well as meeting the DSM-IV criteria for MDD at 2 consecutive visits at least 2 weeks apart, where the 2-week temporal criterion had to be satisfied at only the second visit. The effectiveness of duloxetine in hospitalized patients with major depressive disorder has not been studied.
14.2 Generalized Anxiety Disorder
The efficacy of duloxetine in the treatment of generalized anxiety disorder (GAD) was established in 1 fixed-dose randomized, double-blind, placebo-controlled trial and 2 flexible-dose randomized, double-blind, placebo-controlled trials in adult outpatients between 18 and 83 years of age meeting the DSM-IV criteria for GAD.
In 1 flexible-dose study and in the fixed-dose study, the starting dose was 60 mg once daily were down titration to 30 mg once daily was allowed for tolerability reasons before increasing it to 60 mg once daily. Fifteen percent of patients were down titrated. One flexible-dose study had a starting dose of 30 mg once daily for 1 week before increasing it to 60 mg once daily.
The 2 flexible-dose studies involved dose titration with duloxetine doses ranging from 60 mg once daily to 120 mg once daily (N=168 and N=162) compared to placebo (N=159 and N=161) over a 10-week treatment period. The mean dose for completers at endpoint in the flexible-dose studies was 104.75 mg/day. The fixed-dose study evaluated duloxetine doses of 60 mg once daily (N=168) and 120 mg once daily (N=170) compared to placebo (N=175) over a 9-week treatment period. While a 120 mg/day dose was shown to be effective, there is no evidence that doses greater than 60 mg/day confer additional benefit.
In all 3 studies, duloxetine demonstrated superiority over placebo as measured by greater improvement in the Hamilton Anxiety Scale (HAM-A) total score and by the Sheehan Disability Scale (SDS) global functional impairment score. The SDS is a widely used and well-validated scale that measures the extent emotional symptoms disrupt patient functioning in 3 life domains: work/school, social life/leisure activities and family life/home responsibilities.
In another study, 887 patients meeting DSM-IV-TR criteria for GAD received duloxetine 60 mg to 120 mg once daily during an initial 26-week open-label treatment phase. Four hundred and twenty-nine patients who responded to open-label treatment (defined as meeting the following criteria at weeks 24 and 26: a decrease from baseline HAM-A total score by at least 50% to a score no higher than 11, and a Clinical Global Impressions of Improvement [CGI-Improvement] score of 1 or 2) were randomly assigned to continuation of duloxetine at the same dose (N = 216) or to placebo (N = 213) and were observed for relapse. Of the patients randomized, 73% had been in a responder status for at least 10 weeks. Relapse was defined as an increase in CGI-Severity score at least 2 points to a score ≥4 and a MINI (Mini-International Neuropsychiatric Interview) diagnosis of GAD (excluding duration), or discontinuation due to lack of efficacy. Patients taking duloxetine experienced a statistically significantly longer time to relapse of GAD than did patients taking placebo.
Subgroup analyses did not indicate that there were any differences in treatment outcomes as a function of age or gender.
14.3 Diabetic Peripheral Neuropathic Pain
The efficacy of duloxetine for the management of neuropathic pain associated with diabetic peripheral neuropathy was established in 2 randomized, 12-week, double-blind, placebo-controlled, fixed-dose studies in adult patients having diabetic peripheral neuropathic pain for at least 6 months. Study DPNP-1 and Study DPNP-2 enrolled a total of 791 patients of whom 592 (75%) completed the studies. Patients enrolled had Type I or II diabetes mellitus with a diagnosis of painful distal symmetrical sensorimotor polyneuropathy for at least 6 months. The patients had a baseline pain score of ≥4 on an 11-point scale ranging from 0 (no pain) to 10 (worst possible pain). Patients were permitted up to 4 g of acetaminophen per day as needed for pain, in addition to duloxetine. Patients recorded their pain daily in a diary.
Both studies compared duloxetine 60 mg once daily or 60 mg twice daily with placebo. DPNP-1 additionally compared duloxetine 20 mg with placebo. A total of 457 patients (342 duloxetine , 115 placebo) were enrolled in DPNP-1 and a total of 334 patients (226 duloxetine, 108 placebo) were enrolled in DPNP-2. Treatment with duloxetine 60 mg one or two times a day statistically significantly improved the endpoint mean pain scores from baseline and increased the proportion of patients with at least a 50% reduction in pain score from baseline. For various degrees of improvement in pain from baseline to study endpoint, Figures 1 and 2 show the fraction of patients achieving that degree of improvement. The figures are cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as week 1, which persisted throughout the study.
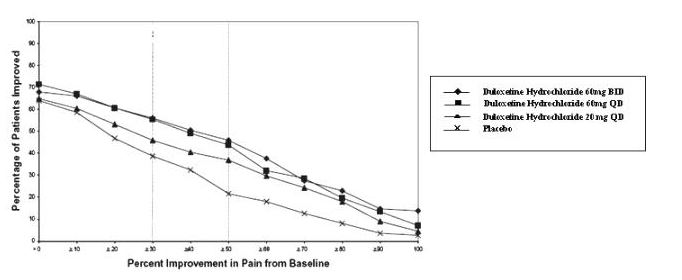
Figure 1: Percentage of Patients Achieving Various Levels of Pain Relief as Measured by 24-Hour Average Pain Severity - DPNP-1
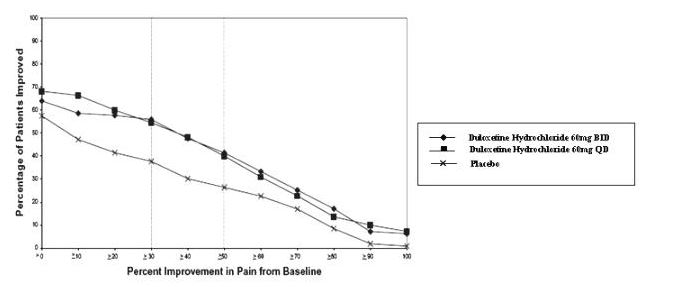
Figure 2: Percentage of Patients Achieving Various Levels of Pain Relief as Measured by 24-Hour Average Pain Severity - DPNP-2
14.5 Chronic Musculoskeletal Pain
Duloxetine is indicated for the management of chronic musculoskeletal pain. This has been established in studies in patients with chronic low back pain and chronic pain due to osteoarthritis.
Studies in Chronic Low Back Pain — The efficacy of duloxetine in chronic low back pain (CLBP) was assessed in two double-blind, placebo-controlled, randomized clinical trials of 13-weeks duration (Study CLBP-1 and Study CLBP-2), and one of 12-weeks duration (CLBP 3). CLBP-1 and CLBP-3 demonstrated efficacy of duloxetine in the treatment of chronic low back pain. Patients in all studies had no signs of radiculopathy or spinal stenosis.
Study CLBP-1: Two hundred thirty-six adult patients (N=115 on duloxetine, N=121 on placebo) enrolled and 182 (77%) completed 13-week treatment phase. After 7 weeks of treatment, duloxetine patients with less than 30% reduction in average daily pain and who were able to tolerate duloxetine 60 mg once daily had their dose of duloxetine, in a double-blinded fashion, increased to 120 mg once daily for the remainder of the study. Patients had a mean baseline pain rating of 6 on a numerical rating scale ranging from 0 (no pain) to 10 (worst possible pain). After 13 weeks of treatment, patients taking duloxetine 60 to 120 mg daily had a significantly greater pain reduction compared to placebo. Randomization was stratified by the patients’ baseline NSAIDs-use status. Subgroup analyses did not indicate that there were differences in treatment outcomes as a function of NSAIDs use.
Study CLBP-2: Four hundred and four patients were randomized to receive fixed doses of duloxetine daily or a matching placebo (N=59 on duloxetine 20 mg, N=116 on duloxetine 60 mg, N=112 on duloxetine 120 mg, N=117 on placebo) and 267 (66%) completed the entire 13-week study. After 13 weeks of treatment, none of the three duloxetine doses showed a statistically significant difference in pain reduction compared to placebo.
Study CLBP-3: Four hundred and one patients were randomized to receive fixed doses of duloxetine 60 mg daily or placebo (N=198 on duloxetine, N=203 on placebo), and 303 (76%) completed the study. Patients had a mean baseline pain rating of 6 on a numerical rating scale ranging from 0 (no pain) to 10 (worst possible pain). After 12 weeks of treatment, patients taking duloxetine 60 mg daily had significantly greater pain reduction compared to placebo.
For various degrees of improvement in pain from baseline to study endpoint, Figures 5 and 6 show the fraction of patients in CLBP-1 and CLBP-3 achieving that degree of improvement. The figures are cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned the value of 0% improvement.
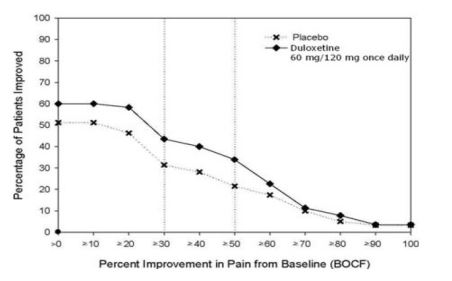
Figure 5: Percentage of Patients Achieving Various Levels of Pain Relief as Measured by 24-Hour Average Pain Severity – CLBP-1
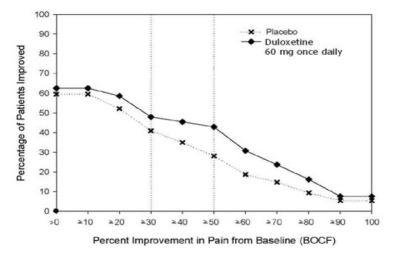
Figure 6: Percentage of Patients Achieving Various Levels of Pain Relief as Measured by 24-Hour Average Pain Severity – CLBP-3
Studies in Chronic Pain Due to Osteoarthritis —The efficacy of duloxetine in chronic pain due to osteoarthritis was assessed in 2 double-blind, placebo-controlled, randomized clinical trials of 13-weeks duration (Study OA-1 and Study OA-2). All patients in both studies fulfilled the ACR clinical and radiographic criteria for classification of idiopathic osteoarthritis of the knee. Randomization was stratified by the patients’ baseline NSAIDs-use status. Patients assigned to duloxetine started treatment in both studies at a dose of 30 mg once daily for one week. After the first week, the dose of duloxetine was increased to 60 mg once daily. After 7 weeks of treatment with duloxetine 60 mg once daily, in OA-1 patients with sub-optimal response to treatment (<30% pain reduction) and tolerated duloxetine 60 mg once daily had their dose increased to 120 mg. However, in OA-2, all patients, regardless of their response to treatment after 7 weeks, were re-randomized to either continue receiving duloxetine 60 mg once daily or have their dose increased to 120 mg once daily for the remainder of the study. Patients in the placebo treatment groups in both studies received a matching placebo for the entire duration of studies. For both studies, efficacy analyses were conducted using 13-week data from the combined duloxetine 60 mg and 120 mg once daily treatment groups compared to the placebo group.
Study OA-1: Two hundred fifty-six patients (N=128 on duloxetine, N=128 on placebo) enrolled and 204 (80%) completed the study. Patients had a mean baseline pain rating of 6 on a numerical rating scale ranging from 0 (no pain) to 10 (worst possible pain). After 13 weeks of treatment, patients taking duloxetine had significantly greater pain reduction. Subgroup analyses did not indicate that there were differences in treatment outcomes as a function of NSAIDs use.
Study OA-2: Two hundred thirty-one patients (N=111 on duloxetine, N=120 on placebo) enrolled and 173 (75%) completed the study. Patients had a mean baseline pain of 6 on a numerical rating scale ranging from 0 (no pain) to 10 (worst possible pain). After 13 weeks of treatment, patients taking duloxetine did not show a significantly greater pain reduction.
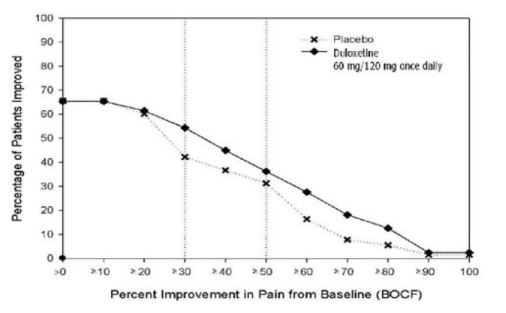
Figure 7: Percentage of Patients Achieving Various Levels of Pain Relief as Measured by 24-Hour Average Pain Severity – OA-1
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Duloxetine delayed-release capsules USP, 20 mg are white to off-white spherical enteric coated pellets filled in size '4' hard gelatin capsules with opaque green colored cap and opaque green colored body, imprinted 'RDY608' on cap and '20mg' on body with black ink. They are supplied in bottles of 60's, 1000's and unit dose package of 30 (3 × 10).
Bottles of 60 NDC 55111-608-60
Bottles of 1000 NDC 55111-608-10
Unit-dose Package of 30 (3 × 10) NDC 55111-608-81
Duloxetine delayed-release capsules USP, 30 mg are white to off-white spherical enteric coated pellets filled in size '3' hard gelatin capsules with opaque blue coloured cap and opaque white colored body, imprinted 'RDY609' on cap and '30mg' on body with golden yellow ink. They are supplied in bottles of 30's, 90's, 1000's and unit dose package of 30 (3 x 10).
Bottles of 30 NDC 55111-609-30
Bottles of 90 NDC 55111-609-90
Bottles of 1000 NDC 55111-609-10
Unit-dose Package of 30 (3 × 10) NDC 55111-609-81
Duloxetine delayed-release capsules USP, 60 mg are white to off-white spherical enteric coated pellets filled in size '1' hard gelatin capsules with opaque blue colored cap and opaque green colored body, imprinted 'RDY610' on cap and '60mg' on body with white ink. They are supplied in bottles of 30's, 90's, 1000's and unit dose package of 30 (3 × 10).
Bottles of 30 NDC 55111-610-30
Bottles of 90 NDC 55111-610-90
Bottles of 1000 NDC 55111-610-10
Unit-dose Package of 30 (3 × 10) NDC 55111-610-81
17 PATIENT COUNSELING INFORMATION
See FDA-approved Medication Guide
17.1 Information on Medication Guide
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with duloxetine and should counsel them in its appropriate use. A patient Medication Guide is available for duloxetine. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide before starting duloxetine and each time their prescription is renewed, and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking duloxetine.
17.2 Suicidal Thoughts and Behaviors
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to observe for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication [see BOXED WARNING, and WARNING AND PRECAUTIONS (5.1)].
17.3 Medication Administration
Duloxetine should be swallowed whole and should not be chewed or crushed, nor should the capsule be opened and its contents be sprinkled on food or mixed with liquids. All of these might affect the enteric coating.
17.4 Continuing the Therapy Prescribed
While patients may notice improvement with duloxetine therapy in 1 to 4 weeks, they should be advised to continue therapy as directed.
17.5 Hepatotoxicity
Patients should be informed that severe liver problems, sometimes fatal, have been reported in patients treated with duloxetine. Patients should be instructed to talk to their healthcare provider if they develop itching, right upper belly pain, dark urine, or yellow skin/eyes while taking duloxetine, which may be signs of liver problems. Patients should talk to their healthcare provider about their alcohol consumption. Use of duloxetine with heavy alcohol intake may be associated with severe liver injury [see WARNINGS AND PRECAUTIONS ( 5.2)].
17.6 Alcohol
Although duloxetine does not increase the impairment of mental and motor skills caused by alcohol, use of duloxetine concomitantly with heavy alcohol intake may be associated with severe liver injury. For this reason, Duloxetine should not be prescribed for patients with substantial alcohol use [see WARNINGS AND PRECAUTIONS ( 5.2) and DRUG INTERACTIONS ( 7.15)] .
17.7 Orthostatic Hypotension and Syncope
Patients should be advised of the risk of orthostatic hypotension and syncope, especially during the period of initial use and subsequent dose escalation, and in association with the use of concomitant drugs that might potentiate the orthostatic effect of duloxetine [see WARNINGS AND PRECAUTIONS ( 5.3) ].
17.8 Serotonin Syndrome
Patients should be cautioned about the risk of serotonin syndrome with the concomitant use of duloxetine and other serotonergic agents including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, tryptophan and St. John’s Wort [see CONTRAINDICATIONS ( 4.1), WARNINGS AND PRECAUTIONS (5.4), and DRUG INTERACTIONS (7.14)] .
Patients should be advised of the signs and symptoms associated with serotonin syndrome that may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular changes (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be cautioned to seek medical care immediately if they experience these symptoms.
17.9 Abnormal Bleeding
Patients should be cautioned about the concomitant use of duloxetine and NSAIDs, aspirin, warfarin, or other drugs that affect coagulation since combined use of psychotropic drugs that interfere with serotonin reuptake and these agents has been associated with an increased risk of bleeding [see W ARNINGS AND PRECAUTIONS ( 5.5) ].
17.10 Severe Skin Reactions
Patients should be cautioned that duloxetine may cause serious skin reactions. This may need to be treated in a hospital and may be life-threatening. Patients should be counseled to call their doctor right away or get emergency help if they have skin blisters, peeling rash, sores in their mouth, hives, or any other allergic reactions [see Warnings and Precautions ( 5.6) ].
17.11 Discontinuation of Tratment
Patients should be instructed that discontinuation of duloxetine may be associated with symptoms such as dizziness, headache, nausea, diarrhea, paresthesia, irritability, vomiting, insomnia, anxiety, hyperhidrosis, and fatigue, and should be advised not to alter their dosing regimen, or stop taking duloxetine without consulting their physician [see WARNINGS AND PRECAUTIONS (5.7)].
17.12 Activation of Mania or Hypomania
Patients with depressive symptoms should be adequately screened for risk of bipolar disorder (e.g. family history of suicide, bipolar disorder, and depression) prior to initiating treatment with duloxetine. Patients should be advised to report any signs or symptoms of a manic reaction such as greatly increased energy, severe trouble sleeping, racing thoughts, reckless behavior, talking more or faster than usual, unusually grand ideas, and excessive happiness or irritability [see WARNINGS AND PRECAUTIONS (5.8)].
17.13 Angle-Closure Glaucoma
Patients should be advised that taking duloxetine can cause mild pupillary dilation, which in susceptible individuals, can lead to an episode of angle-closure glaucoma. Pre-existing glaucoma is almost always open-angle glaucoma because angle-closure glaucoma, when diagnosed, can be treated definitively with iridectomy. Open-angle glaucoma is not a risk factor for angle-closure glaucoma. Patients may wish to be examined to determine whether they are susceptible to angle-closure, and have a prophylactic procedure (e.g., iridectomy), if they are susceptible. [See Warnings and Precautions ( 5.9) ]
17.14 Seizures
Patients should be advised to inform their physician if they have a history of seizure disorder [see WARNINGS AND PRECAUTIONS (5.10)].
17.15 Effects on Blood Pressure
Patients should be cautioned that duloxetine may cause an increase in blood pressure [see WARNINGS AND PRECAUTIONS ( 5.11) ].
17.16 Concomitant Medications
Patients should be advised to inform their physicians if they are taking, or plan to take, any prescription or overthe-counter medications, since there is a potential for interactions [see Dosage and Administration ( 2.5), Contraindications (4.1) Warnings and Precautions ( 5.4 and 5.12), and Drug Interactions (7)].
17.17 Hyponatremia
Patients should be advised that hyponatremia has been reported as a result of treatment with SNRIs and SSRIs, including duloxetine. Patients should be advised of the signs and symptoms of hyponatremia [see Warnings and Precautions ( 5.13) ].
17.18 Concomitant Illness
Patients should be advised to inform their physicians about all of their medical conditions [see Warnings and Precautions (5.14)].
17.19 Urinary Hesitancy and Retention
Duloxetine is in a class of medicines that may affect urination. Patients should be instructed to consult with their healthcare provider if they develop any problems with urine flow [see Warnings and Precautions ( 5.15) ].
17.21 Interference with Psychomotor Performance
Any psychoactive drug may impair judgment, thinking, or motor skills. Although in controlled studies duloxetine has not been shown to impair psychomotor performance, cognitive function, or memory, it may be associated with sedation and dizziness. Therefore, patients should be cautioned about operating hazardous machinery including automobiles, until they are reasonably certain that duloxetine therapy does not affect their ability to engage in such activities.
MEDICATION GUIDE
DULOXETINE [doh-LOCKS-ah-teen]
(Duloxetine Delayed-Release Capsules USP)
Read the Medication Guide that comes with duloxetine before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment. Talk with your healthcare provider if there is something you do not understand or want to learn more about.
What is the most important information I should know about duloxetine delayed-release capsules?
Duloxetine and other antidepressant medicines may cause serious side effects, including:
1. Suicidal thoughts or actions:
- Duloxetine and other antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, or young adults within the first few months of treatment or when the dose is changed.
- Depression or other serious mental illnesses are the most important causes of suicidal thoughts or actions.
- Watch for these changes and call your healthcare provider right away if you notice:
- New or sudden changes in mood, behavior, actions, thoughts, or feelings, especially if severe.
- Pay particular attention to such changes when duloxetine is started or when the dose is changed.
Keep all follow-up visits with your healthcare provider and call between visits if you are worried about symptoms.
Call your healthcare provider right away if you have any of the following symptoms, or call 911 if an emergency, especially if they are new, worse, or worry you:
- attempts to commit suicide
- acting on dangerous impulses
- acting aggressive or violent
- thoughts about suicide or dying
- new or worse depression
- new or worse anxiety or panic attacks
- feeling agitated, restless, angry or irritable
- trouble sleeping
- an increase in activity or talking more than what is normal for you
- other unusual changes in behavior or mood
Call your healthcare provider right away if you have any of the following symptoms, or call 911 if an emergency. Duloxetine may be associated with these serious side effects:
2. Liver damage- symptoms may include:
- itching
- right upper abdominal pain
- dark urine
- hepatitis with yellow skin or eyes
- enlarged liver
- increased liver enzymes
3. Serotonin Syndrome -This condition can be life-threatening and may include.
- agitation, hallucinations, coma or other changes in mental status
- coordination problems or muscle twitching (overactive reflexes)
- racing heartbeat, high or low blood pressure
- sweating or fever
- nausea, vomiting, or diarrhea
- muscle rigidity
- dizziness
- flushing
- tremor
- seizures
4. Abnormal bleeding: Duloxetine and other antidepressant medicines may increase your risk of bleeding or bruising, especially if you take the blood thinner warfarin (Coumadin*, Jantoven*), a non-steroidal anti-inflammatory drug (NSAIDs, like ibuprofen or naproxen), or aspirin.
5. Severe skin reactions: Duloxetine may cause serious skin reactions that may require stopping its use. This may need to be treated in a hospital and may be life-threatening. Call your doctor right away or get emergency help if you have skin blisters, peeling rash, sores in the mouth, hives or any other allergic reactions.
6. Manic episodes:
- greatly increased energy
- severe trouble sleeping
- racing thoughts
- reckless behavior
- unusually grand ideas
- excessive happiness or irritability
- talking more or faster than usual
7. Visual Problems
-
eye pain
-
changes in vision
-
swelling or redness in or around the eye
Only some people are at risk for these problems. You may want to undergo an eye examination to see if you are at risk and receive preventative treatment if you are.
8. Seizures or convulsions
9. Changes in blood pressure. Monitor your blood pressure before starting and throughout treatment. Duloxetine may:
- increase your blood pressure.
- decrease your blood pressure when standing and cause dizziness or fainting, mostly when first starting duloxetine or when increasing the dose.
10. Low salt (sodium) levels in the blood. Elderly people may be at greater risk for this. Symptoms may include:
- headache
- weakness or feeling unsteady
- confusion, problems concentrating or thinking or memory problems
11. Problems with urination include:
- decreased urine flow
- unable to pass any urine
12. Changes in appetite or weight. Children and adolescents should have height and weight monitored during treatment.
Do not stop duloxetine delayed-release capsules without first talking to your healthcare provider. Stopping duloxetine delayed-release capsules too quickly or changing from another antidepressant too quickly may result in serious symptoms including:
- anxiety, irritability
- feeling tired or problems sleeping
- headache, sweating, dizziness
- electric shock-like sensations
- vomiting, nausea, diarrhea
What is duloxetine ?
Duloxetine is a prescription medicine used to treat depression. It is important to talk with your healthcare provider about the risks of treating depression and also the risks of not treating it. You should discuss all treatment choices with your healthcare provider. Duloxetine is also used to treat or manage:
- Major Depressive Disorder (MDD)
- Generalized Anxiety Disorder (GAD)
- Diabetic Peripheral Neuropathic Pain (DPNP)
- Chronic Musculoskeletal Pain
Talk to your healthcare provider if you do not think that your condition is getting better with duloxetine treatment.
Who should not take duloxetine delayed-release capsules?
Do NOT take duloxetine delayed-release capsules if you:
- take a Monoamine Oxidase Inhibitor (MAOI). Ask your healthcare provider or pharmacist if you are not sure if you take an MAOI, including the antibiotic linezolid.
- Do not take an MAOI within 5 days of stopping duloxetine unless directed to do so by your physician.
- Do not start duloxetine if you stopped taking an MAOI in the last 2 weeks unless directed to do so by your physician.
- People who take duloxetine close in time to an MAOI may have serious or even life-threatening side effects. Get medical help right away if you have any of these symptoms:
-
- high fever
- uncontrolled muscle spasms
- stiff muscles
- rapid changes in heart rate or blood pressure
- confusion
- loss of consciousness (pass out)
- take Mellaril* (thioridazine) because this can cause serious heart rhythm problems or sudden death
What should I tell my healthcare provider before taking duloxetine delayed-release capsules? Ask if you are not sure.
Before starting duloxetine , tell your healthcare provider if you:
- Are taking certain drugs such as:
- Triptans used to treat migraine headache
- Medicines used to treat mood, anxiety, psychotic or thought disorders, including tricyclics, lithium, buspirone, SSRIs, SNRIs or MAOIs
- Tramadol and fentanyl
- Cimetidine
- The antibiotics ciprofloxacin, enoxacin
- Medicine to control heart rate such as propafenone, flecainide, quinidine
- Theophylline
- The blood thinner warfarin (Coumadin*, Jantoven*)
- Non-steroidal anti-inflammatory drug (NSAID), like ibuprofen, naproxen or aspirin.
- Over-the-counter supplements such as tryptophan or St. John’s Wort
- have heart problems or high blood pressure
- have diabetes (Duloxetine treatment worsens the control of blood sugar in some patients with diabetes)
- have liver problems
- have kidney problems
- have glaucoma
- have or had seizures or convulsions
- have bipolar disorder or mania
- have low sodium levels in your blood
- have delayed stomach emptying
- have or had bleeding problems
- are pregnant or plan to become pregnant. It is not known if duloxetine will harm your unborn baby. Talk to your healthcare provider about the benefits and risks of treating depression or other conditions with duloxetine during pregnancy.
- are breast-feeding or plan to breast-feed. Some duloxetine may pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby while taking duloxetine.
Tell your healthcare provider about all the medicines that you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Duloxetine and some medicines may interact with each other, may not work as well, or may cause serious side effects.
Your healthcare provider or pharmacist can tell you if it is safe to take duloxetine with your other medicines. Do not start or stop any medicine while taking duloxetine without talking to your healthcare provider first.
If you take duloxetine delayed-release capsules, you should not take any other medicines that contain duloxetine.
How should I take duloxetine delayed-release capsules?
- Take duloxetine exactly as prescribed. Your healthcare provider may need to change the dose of duloxetine until it is the right dose for you.
- Do not open, break or chew the capsule; it must be swallowed whole.
- Duloxetine may be taken with or without food.
- If you miss a dose of duloxetine, take the missed dose as soon as you remember. If it is almost time for the next dose, skip the missed dose and take your next dose at the regular time. Do not take two doses of duloxetine at the same time.
- If you take too much duloxetine, call your healthcare provider or poison control center right away, or get emergency treatment.
- When switching from another antidepressant to duloxetine your doctor may want to lower the dose of the initial antidepressant first to potentially avoid side effects.
What should I avoid while taking duloxetine delayed-release capsules?
- Duloxetine can cause sleepiness or may affect your ability to make decisions, think clearly, or react quickly. You should not drive, operate heavy machinery, or do other dangerous activities until you know how duloxetine affects you.
- Use of duloxetine concomitantly with heavy alcohol intake may be associated with severe liver injury. Avoid heavy alcohol use while taking duloxetine.
What are the possible side effects of duloxetine delayed-release capsules?
Duloxetine may cause serious side effects, including all of those described in the section entitled “ What is the most important information I should know about duloxetine delayed-release capsules?
Common possible side effects in people who take duloxetine include:
- nausea
- dry mouth
- sleepiness
- fatigue
- loss of appetite
- increased sweating
- dizziness
Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of duloxetine. For more information, ask your healthcare provider or pharmacist.
CALL YOUR DOCTOR FOR MEDICAL ADVICE ABOUT SIDE EFFECTS. YOU MAY REPORT SIDE EFFECTS TO THE FDA AT 1-800-FDA1088.
How should I store duloxetine delayed-release capsules?
Store at 20°-25°C (68° - 77°F); [See USP Controlled Room Temperature].
Keep duloxetine delayed-release capsules and all medicines out of the reach of children.
General information about duloxetine
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use duloxetine for a condition for which it was not prescribed. Do not give duloxetine to other people, even if they have the same condition. It may harm them.
This Medication Guide summarizes the most important information about duloxetine. If you would like more information, talk with your healthcare provider. You may ask your healthcare provider or pharmacist for information about duloxetine that is written for healthcare professionals. For more information about duloxetine call 1-888-375-3784.
What are the ingredients in duloxetine delayed-release capsules?
Active ingredient: duloxetine hydrochloride USP
Inactive ingredients: ammonia, FD&C Blue 2, gelatin, glycine, hypromellose phthalate, hypromellose, iron oxide yellow, propylene glycol, shellac, sodium lauryl sulfate, sucrose, sugar spheres (contains sugar and corn starch), talc, titanium dioxide, and triethyl citrate. The 20 mg capsules also contain black iron oxide and potassium hydroxide. The 60 mg capsules also contain potassium hydroxide.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
To reorder additional Medication Guides, please contact Dr. Reddy's Customer Service at 1-866-733-3952
* The brands listed are trademarks of their respective owners and not trademarks of Dr. Reddy’s Laboratories Limited.
Rx only
Manufactured by
Dr. Reddy’s Laboratories Limited
Bachupally – 500 090 INDIA
Revised: 0914