RISEDRONATE SODIUM- risedronate sodium tablet, delayed release
Teva Pharmaceuticals USA, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use risedronate sodium delayed-release tablets safely and effectively. See full prescribing information for risedronate sodium delayed-release tablets.
RISEDRONATE sodium delayed-release tablets for oral use Initial U.S. Approval: 1998 INDICATIONS AND USAGERisedronate sodium delayed-release tablets are a bisphosphonate in a delayed-release formulation and is indicated for treatment of postmenopausal osteoporosis (1.1) Limitations of Use Optimal duration of use has not been determined. For patients at low-risk for fracture, consider drug discontinuation after 3 to 5 years of use (1.2) DOSAGE AND ADMINISTRATIONOne 35 mg delayed-release tablet once-a-week (2.1) Instruct patients to:
DOSAGE FORMS AND STRENGTHSDelayed-release tablets: 35 mg (3) CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (greater than 5%) include: diarrhea, influenza, arthralgia, back pain, and abdominal pain (6.1) Hypersensitivity reactions (angioedema, generalized rash, bullous skin reactions, Stevens-Johnson syndrome, and toxic epidermal necrolysis), and eye inflammation (iritis, uveitis) have been reported rarely (6.2) To report SUSPECTED ADVERSE REACTIONS, contact TEVA USA, PHARMACOVIGILANCE at 1-866-832-8537 or drug.safety@tevapharm.com; or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSUSE IN SPECIFIC POPULATIONSRisedronate sodium delayed-release tablets are not recommended for use in patients with severe renal impairment (creatinine clearance less than 30 mL/min) (5.6, 8.6, 12.3) Risedronate sodium delayed-release tablets are not indicated for use in pediatric patients (8.4) See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 6/2017 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Postmenopausal Osteoporosis
Risedronate sodium delayed-release tablets are indicated for the treatment of osteoporosis in postmenopausal women. In postmenopausal women, risedronate sodium has been shown to reduce the incidence of vertebral fractures and a composite endpoint of nonvertebral osteoporosis-related fractures [see Clinical Studies (14.1)].
1.2 Important Limitations of Use
The optimal duration of use has not been determined. The safety and effectiveness of risedronate sodium delayed-release tablets for the treatment of osteoporosis are based on clinical data of one year duration. All patients on bisphosphonate therapy should have the need for continued therapy re-evaluated on a periodic basis. Patients at low-risk for fracture should be considered for drug discontinuation after 3 to 5 years of use. Patients who discontinue therapy should have their risk for fracture re-evaluated periodically.
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Postmenopausal Osteoporosis [see Indications and Usage (1.1)]
The recommended regimen is:
- one 35 mg delayed-release tablet orally, taken once-a-week
2.2 Important Administration Instructions
Instruct patients to do the following:
- Take risedronate sodium delayed-release tablets in the morning immediately following breakfast. Risedronate sodium delayed-release tablets should be taken immediately following breakfast and not under fasting conditions because of a higher risk of abdominal pain if taken before breakfast when fasting.
- Swallow risedronate sodium delayed-release tablets whole while in an upright position and with at least 4 ounces of plain water to facilitate delivery to the stomach. Avoid lying down for 30 minutes after taking the medication [see Warnings and Precautions (5.2)].
- Do not chew, cut, or crush risedronate sodium delayed-release tablets.
2.3 Recommendations for Calcium and Vitamin D Supplementation
Instruct patients to take supplemental calcium and vitamin D if dietary intake is inadequate [see Warnings and Precautions (5.3)] and to take calcium supplements, antacids, magnesium-based supplements or laxatives, and iron preparations at a different time of the day as they interfere with the absorption of risedronate sodium delayed-release tablets.
3 DOSAGE FORMS AND STRENGTHS
Delayed-release tablets: 35 mg, white to off-white, oval, enteric-coated, biconvex unscored tablet, debossed with "T21" on one side of the tablet and plain on the other side.
4 CONTRAINDICATIONS
Risedronate sodium delayed-release tablets are contraindicated in patients with the following conditions:
- Abnormalities of the esophagus which delay esophageal emptying such as stricture or achalasia [see Warnings and Precautions (5.2)]
- Inability to stand or sit upright for at least 30 minutes [see Dosage and Administration (2), Warnings and Precautions (5.2)]
- Hypocalcemia [see Warnings and Precautions (5.3)]
- Known hypersensitivity to any component of this product. Angioedema, generalized rash, bullous skin reactions, Stevens-Johnson syndrome and toxic epidermal necrolysis have been reported [see Adverse Reactions (6.2)]
5 WARNINGS AND PRECAUTIONS
5.1 Drug Products With the Same Active Ingredient
Risedronate sodium delayed-release tablets contain the same active ingredient found in Actonel®. A patient being treated with Actonel should not receive risedronate sodium delayed-release tablets.
5.2 Upper Gastrointestinal Adverse Reactions
Risedronate sodium delayed-release tablets, like other bisphosphonates administered orally, may cause local irritation of the upper gastrointestinal mucosa. Because of these possible irritant effects and a potential for worsening of the underlying disease, caution should be used when risedronate sodium delayed-release tablets are given to patients with active upper gastrointestinal problems (such as known Barrett’s esophagus, dysphagia, other esophageal diseases, gastritis, duodenitis or ulcers) [see Contraindications (4), Adverse Reactions (6.1), Information for Patients (17)].
Esophageal adverse experiences, such as esophagitis, esophageal ulcers and esophageal erosions, occasionally with bleeding and rarely followed by esophageal stricture or perforation, have been reported in patients receiving treatment with oral bisphosphonates. In some cases, these have been severe and required hospitalization. Physicians should therefore be alert to any signs or symptoms signaling a possible esophageal reaction and patients should be instructed to discontinue risedronate sodium delayed-release tablets and seek medical attention if they develop dysphagia, odynophagia, retrosternal pain or new or worsening heartburn.
The risk of severe esophageal adverse experiences appears to be greater in patients who lie down after taking oral bisphosphonates and/or who fail to swallow it with the recommended 4 ounces of water, and/or who continue to take oral bisphosphonates after developing symptoms suggestive of esophageal irritation. Therefore, it is very important that the full dosing instructions are provided to, and understood by, the patient [see Dosage and Administration (2)]. In patients who cannot comply with dosing instructions due to mental disability, therapy with risedronate sodium delayed-release tablets should be used under appropriate supervision.
There have been postmarketing reports of gastric and duodenal ulcers with oral bisphosphonate use, some severe and with complications, although no increased risk was observed in controlled clinical trials.
5.3 Mineral Metabolism
Hypocalcemia has been reported in patients taking risedronate sodium delayed-release tablets. Treat hypocalcemia and other disturbances of bone and mineral metabolism should be effectively treated before starting risedronate sodium delayed-release tablets therapy. Instruct patients to take supplemental calcium and vitamin D if their dietary intake is inadequate. Adequate intake of calcium and vitamin D is important in all patients [see Contraindications (4), Adverse Reactions (6.1), Information for Patients (17)].
5.4 Jaw Osteonecrosis
Osteonecrosis of the jaw (ONJ), which can occur spontaneously, is generally associated with tooth extraction and/or local infection with delayed healing, and has been reported in patients taking bisphosphonates, including risedronate. Known risk factors for osteonecrosis of the jaw include invasive dental procedures (for example, tooth extraction, dental implants, boney surgery), diagnosis of cancer, concomitant therapies (for example, chemotherapy, corticosteroids, angiogenesis inhibitors), poor oral hygiene, and co-morbid disorders (for example, periodontal and/or other preexisting dental disease, anemia, coagulopathy, infection, ill-fitting dentures). The risk of ONJ may increase with duration of exposure to bisphosphonates.
For patients requiring invasive dental procedures, discontinuation of bisphosphonate treatment may reduce the risk for ONJ. Clinical judgment of the treating physician and/or oral surgeon should guide the management plan of each patient based on individual benefit/risk assessment.
Patients who develop ONJ while on bisphosphonate therapy should receive care by an oral surgeon. In these patients, extensive dental surgery to treat ONJ may exacerbate the condition. Discontinuation of bisphosphonate therapy should be considered based on individual benefit/risk assessment [see Adverse Reactions (6.2)].
5.5 Musculoskeletal Pain
In postmarketing experience, there have been reports of severe and occasionally incapacitating bone, joint, and/or muscle pain in patients taking bisphosphonates [see Adverse Reactions (6.2)]. The time to onset of symptoms varied from one day to several months after starting the drug. Most patients had relief of symptoms after stopping medication. A subset had recurrence of symptoms when rechallenged with the same drug or another bisphosphonate. Consider discontinuing use if severe symptoms develop.
5.6 Atypical Subtrochanteric and Diaphyseal Femoral Fractures
Atypical, low-energy, or low trauma fractures of the femoral shaft have been reported in bisphosphonate-treated patients. These fractures can occur anywhere in the femoral shaft from just below the lesser trochanter to above the supracondylar flare and are traverse or short oblique in orientation without evidence of comminution. Causality has not been established as these fractures also occur in osteoporotic patients who have not been treated with bisphosphonates.
Atypical femur fractures most commonly occur with minimal or no trauma to the affected area. They may be bilateral and many patients report prodromal pain in the affected area, usually presenting as dull, aching thigh pain, weeks to months before a complete fracture occurs. A number of reports note that patients were also receiving treatment with glucocorticoids (for example, prednisone) at the time of fracture.
Any patient with a history of bisphosphonate exposure who presents with thigh or groin pain should be suspected of having an atypical fracture and should be evaluated to rule out an incomplete femur fracture. Patients presenting with an atypical fracture should also be assessed for symptoms and signs of fracture in the contralateral limb. Interruption of bisphosphonate therapy should be considered, pending a risk/benefit assessment, on an individual basis.
6 ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Treatment of Postmenopausal Osteoporosis
Once-a-Week Dosing with risedronate sodium delayed-release tablets
The safety of risedronate sodium delayed-release tablet, 35 mg once-a-week in the treatment of postmenopausal osteoporosis was assessed in a 1 year, double-blind, multicenter study comparing risedronate sodium delayed-release tablet, 35 mg once-a-week to risedronate sodium immediate-release 5 mg daily in postmenopausal women 50 years of age or older. Risedronate sodium delayed-release tablets were administered either at least 30 minutes before (N = 308) or immediately following (N = 307) breakfast, and risedronate sodium immediate-release 5 mg daily (N = 307) was administered at least 30 minutes before breakfast. Patients with preexisting gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors, and H2 antagonists were included in this clinical trial. All women received daily supplementation with 1000 mg of elemental calcium plus 800 to 1000 international units vitamin D. As treatment with risedronate sodium delayed-release tablets resulted in a significantly higher incidence of abdominal pain when administered before breakfast under fasting conditions, safety results that follow refer only to risedronate sodium delayed-release tablet, 35 mg once-a-week immediately following breakfast and risedronate sodium immediate-release 5 mg daily.
The incidence of all-cause mortality was 0.0% in the risedronate sodium delayed-release tablet, 35 mg once-a-week group and 0.3% in the risedronate sodium immediate-release 5 mg daily group. The incidence of serious adverse reactions was 6.5% in the risedronate sodium delayed-release tablet, 35 mg once-a-week group and 7.2% in the risedronate sodium immediate-release 5 mg daily group. The percentage of patients who withdrew from the study due to adverse reactions was 9.1% in the risedronate sodium delayed-release tablet, 35 mg once-a-week group and 8.1% in the risedronate sodium immediate-release 5 mg daily group. The overall safety and tolerability profiles of the two dosing regimens were similar. Table 1 lists adverse reactions reported in greater than or equal to 2% of patients. Adverse reactions are shown without attribution of causality.
|
System Organ Class Preferred Term |
35 mg
Tablets |
5 mg
|
|
Weekly N = 307 |
Daily N = 307 |
|
|
% |
% |
|
|
Gastrointestinal disorders | ||
|
Diarrhea |
8.8 |
4.9 |
|
Abdominal pain |
5.2 |
2.9 |
|
Constipation |
4.9 |
2.9 |
|
Vomiting |
4.9 |
1.6 |
|
Dyspepsia |
3.9 |
3.9 |
|
Nausea |
3.6 |
3.9 |
|
Abdominal pain upper |
2.9 |
2.3 |
|
Infections and infestations | ||
|
Influenza |
7.2 |
6.2 |
|
Bronchitis |
3.9 |
4.2 |
|
Upper respiratory tract |
3.6 |
2.6 |
|
Musculoskeletal and connective tissue disorders | ||
|
Arthralgia |
6.8 |
7.8 |
|
Back pain |
6.8 |
5.9 |
|
Pain in extremity |
3.9 |
2.3 |
|
Musculoskeletal pain |
2.0 |
1.6 |
|
Muscle spasms |
1.0 |
2.3 |
|
Nervous system disorders | ||
|
Dizziness |
2.6 |
3.3 |
|
Headache |
2.6 |
4.9 |
Acute Phase Reactions: Symptoms consistent with acute phase reaction have been reported with bisphosphonate use. The overall incidence of acute phase reaction was 2.3% in the risedronate sodium delayed-release tablet, 35 mg once-a-week group and 1.3% in the risedronate sodium immediate-release 5 mg daily group. These incidence rates are based on reporting of one or more pre-specified acute phase reaction-like symptoms within 3 days of the first dose and for a duration of 7 days or less.
Gastrointestinal Adverse Reactions: Adverse reactions related to the upper gastrointestinal tract occurred in 16% of subjects treated with risedronate sodium delayed-release tablet, 35 mg once-a-week and 15% of subjects treated with risedronate sodium immediate-release 5 mg daily. The incidence of upper gastrointestinal tract adverse reactions in the risedronate sodium delayed-release tablet, 35 mg once-a-week and risedronate sodium immediate-release 5 mg daily groups were: abdominal pain (5.2% versus 2.9%), dyspepsia (3.9% versus 3.9%), upper abdominal pain (2.9% versus 2.3%), gastritis (1.0% versus 1.0%), and gastroesophageal reflux disease (1.0% versus 1.6%). Study discontinuation due to abdominal pain occurred in 1.3% of the risedronate sodium delayed-release tablet, 35 mg once-a-week group and 0.7% of the risedronate sodium immediate-release 5 mg daily group.
Musculoskeletal Adverse Reactions: Selected musculoskeletal adverse reactions were reported in 16% of subjects treated with risedronate sodium delayed-release tablet, 35 mg once-a-week and 15% of subjects treated with risedronate sodium immediate-release 5 mg daily. The incidence of musculoskeletal adverse reactions in the risedronate sodium delayed-release tablet, 35 mg once-a-week and risedronate sodium immediate-release 5 mg daily groups were: arthralgia (6.8% versus 7.8%), back pain (6.8% versus 5.9%), musculoskeletal pain (2.0% versus 1.6%), and myalgia (1.3% versus 1.0%).
Laboratory Test Findings:
Parathyroid hormone: The effect of risedronate sodium delayed-release tablet, 35 mg once-a-week and risedronate sodium immediate-release 5 mg daily on parathyroid hormone was evaluated in postmenopausal women with osteoporosis. At week 52, in subjects with normal levels at baseline, PTH levels greater than 65 pg/mL (upper limit of normal) were noted in 9% of subjects receiving risedronate sodium delayed-release tablet, 35 mg once-a-week and 8% of subjects receiving risedronate sodium immediate-release 5 mg daily. In subjects with normal levels at baseline, PTH levels greater than 97 pg/mL (1.5 times the upper limit of normal) were seen in 2% of subjects receiving risedronate sodium delayed-release tablet, 35 mg once-a-week and no subjects receiving risedronate sodium immediate-release 5 mg daily. There were no clinically significant differences between treatment groups for levels of calcium, phosphorus and magnesium.
Daily Dosing with risedronate sodium immediate-release 5 mg tablets
The safety of risedronate sodium immediate-release 5 mg once daily in the treatment of postmenopausal osteoporosis was assessed in four randomized, double-blind, placebo-controlled multinational trials of 3232 women aged 38 to 85 years with postmenopausal osteoporosis. The duration of the trials was up to three years, with 1619 patients exposed to placebo and 1613 patients exposed to risedronate sodium immediate-release 5 mg daily. Patients with preexisting gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors (PPIs), and H2 antagonists were included in these clinical trials. All women received 1000 mg of elemental calcium plus vitamin D supplementation up to 500 international units per day if their 25-hydroxyvitamin D3 level was below normal at baseline.
The incidence of all-cause mortality was 2.0% in the placebo group and 1.7% in the risedronate sodium immediate-release 5 mg daily group. The incidence of serious adverse reactions was 24.6% in the placebo group and 27.2% in the risedronate sodium immediate-release 5 mg daily group. The percentage of patients who withdrew from the study due to adverse reactions was 15.6% in the placebo group and 14.8% in the risedronate sodium immediate-release 5 mg daily group. The most common adverse reactions reported in greater than 10% of subjects were: back pain, arthralgia, abdominal pain and dyspepsia.
Gastrointestinal Adverse Reactions: The incidence of adverse reactions in the placebo and risedronate sodium immediate-release 5 mg daily groups were: abdominal pain (9.9% versus 12.2%), diarrhea (10.0% versus 10.8%), dyspepsia (10.6% versus 10.8%), and gastritis (2.3% versus 2.7%). Duodenitis and glossitis have been reported uncommonly in the risedronate sodium immediate-release 5 mg daily group (0.1% to 1%). In patients with active upper gastrointestinal disease at baseline, the incidence of upper gastrointestinal adverse reactions was similar between the placebo and risedronate sodium immediate-release 5 mg daily groups.
Musculoskeletal Adverse Reactions: The incidence of adverse reactions in the placebo and risedronate sodium immediate-release 5 mg daily groups were: back pain (26.1% versus 28.0%), arthralgia (22.1% versus 23.7%), myalgia (6.2% versus 6.7%), and bone pain (4.8% versus 5.3%).
Laboratory Test Findings: Throughout the Phase 3 studies, transient decreases from baseline in serum calcium (less than 1%) and serum phosphate (less than 3%) and compensatory increases in serum PTH levels (less than 30%) were observed within 6 months in patients in osteoporosis clinical trials treated with risedronate sodium immediate-release 5 mg daily. There were no significant differences in serum calcium, phosphate, or PTH levels between placebo and risedronate sodium immediate-release 5 mg daily at 3 years. Serum calcium levels below 8 mg/dL were observed in 18 patients, 9 (0.5%) in each treatment arm (placebo and risedronate sodium immediate-release 5 mg daily). Serum phosphorus levels below 2 mg/dL were observed in 14 patients, 3 (0.2%) treated with placebo and 11 (0.6%) treated with risedronate sodium immediate-release 5 mg daily. There have been rare reports (less than 0.1%) of abnormal liver function tests.
Endoscopic Findings: In the risedronate sodium immediate-release 5 mg daily clinical trials, endoscopic evaluation was encouraged in any patient with moderate-to-severe gastrointestinal complaints, while maintaining the blind. Endoscopies were performed on equal numbers of patients between the placebo and treated groups [75 (14.5%) placebo; 75 (11.9%) risedronate sodium immediate-release 5 mg daily]. Clinically important findings (perforations, ulcers, or bleeding) among this symptomatic population were similar between groups (51% placebo; 39% risedronate sodium immediate-release 5 mg daily).
6.2 Postmarketing Experience
The following adverse reactions have been reported with the use of risedronate sodium delayed-release. Because these adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity Reactions
Hypersensitivity and skin reactions have been reported, including angioedema, generalized rash, bullous skin reactions, Stevens-Johnson syndrome and toxic epidermal necrolysis.
Gastrointestinal Adverse Reactions
Reactions involving upper gastrointestinal irritation, such as esophagitis and esophageal or gastric ulcers, have been reported [see Warnings and Precautions (5.2)].
Musculoskeletal Pain
Bone, joint, or muscle pain, described as severe or incapacitating, have been reported rarely [see Warnings and Precautions (5.5)].
Eye Inflammation
Reactions of eye inflammation including iritis and uveitis have been reported rarely.
Jaw Osteonecrosis
Osteonecrosis of the jaw has been reported rarely [see Warnings and Precautions (5.4)].
Pulmonary
Asthma exacerbations
7 DRUG INTERACTIONS
Risedronate is not metabolized and does not induce or inhibit hepatic microsomal drug-metabolizing enzymes (for example, Cytochrome P450).
7.1 Calcium Supplements/Antacids
When risedronate sodium delayed-release tablets were administered following breakfast, the coadministration of a tablet containing 600 mg of elemental calcium and 400 international units vitamin D reduced risedronate bioavailability by approximately 38% [see Clinical Pharmacology (12.3)]. Calcium supplements, antacids, magnesium-based supplements or laxatives, and iron preparations interfere with the absorption of risedronate sodium delayed-release tablets and should not be taken together.
7.2 Histamine 2 (H2) Blockers and Proton Pump Inhibitors (PPIs)
Drugs that raise stomach pH (for example, PPIs or H2 blockers) may cause faster drug release from enteric coated (delayed-release) drug products such as risedronate sodium delayed-release tablets. Coadministration of risedronate sodium delayed-release tablets with the PPI, esomeprazole, increased risedronate bioavailability. The maximum plasma concentration (Cmax) and the area under the plasma concentration (AUC) were increased by 60 percent and 22 percent, respectively.
Concomitant administration of risedronate sodium delayed-release tablets and H2 blockers or PPIs is not recommended.
7.3 Hormone Therapy
Concomitant use of risedronate sodium delayed-release tablets with estrogens and estrogen agonist/antagonists has not been studied.
7.4 Aspirin/Non-Steroidal Anti-Inflammatory Drugs
In the Phase 3 study comparing risedronate sodium delayed-release tablet, 35 mg once-a-week immediately following breakfast and risedronate sodium 5 mg daily, 18% of NSAID users (any use) in both groups developed upper gastrointestinal adverse reactions. Among non-users, 13% of patients taking risedronate sodium delayed-release tablet, 35 mg once-a-week immediately following breakfast developed upper gastrointestinal adverse reactions, compared to 12% taking risedronate sodium 5 mg daily.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy category C
There are no adequate and well-controlled studies of risedronate sodium delayed-release tablets in pregnant women. Risedronate sodium delayed-release tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the mother and fetus.
Bisphosphonates are incorporated into the bone matrix, from which they are gradually released over periods of weeks to years. The amount of bisphosphonate incorporation into adult bone, and hence, the amount available for release back into the systemic circulation, is directly related to the dose and duration of bisphosphonate use. There are no data on fetal risk in humans. However, there is a theoretical risk of fetal harm, predominantly skeletal, if a woman becomes pregnant after completing a course of bisphosphonate therapy. The impact of variables such as time between cessation of bisphosphonate therapy to conception, the particular bisphosphonate used, and the route of administration (intravenous versus oral) on this risk has not been studied.
In animal studies, pregnant rats received risedronate sodium during organogenesis at doses 1 to 26 times the human Paget’s disease dose of 30 mg/day. Survival of neonates was decreased in rats treated during gestation with oral doses approximately 5 times the human dose and body weight was decreased in neonates from dams treated with approximately 26 times the human dose. The number of fetuses exhibiting incomplete ossification of sternebrae or skull from dams treated with approximately 2.5 times the human dose was significantly increased compared to controls. Both incomplete ossification and unossified sternebrae were increased in rats treated with oral doses approximately 5 times the human dose. A low incidence of cleft palate was observed in fetuses from female rats treated with oral doses approximately equal to the human dose. The relevance of this finding to human use of risedronate sodium delayed-release tablets is unclear.
No significant fetal ossification effects were seen in rabbits treated with oral doses approximately 7 times the human dose (the highest dose tested). However, 1 of 14 litters were aborted and 1 of 14 litters were delivered prematurely.
Similar to other bisphosphonates, treatment during mating and gestation with doses of risedronate sodium approximately the same as the human Paget’s disease dose of 30 mg/day resulted in periparturient hypocalcemia and mortality in pregnant rats allowed to deliver.
Dosing multiples provided above are based on the recommended human Paget’s disease dose of 30 mg/day and normalized using body surface area (mg/m2). Actual animal doses were 3.2, 7.1 and 16 mg/kg/day in the rat and 10 mg/kg/day in the rabbit.
8.3 Nursing Mothers
Risedronate was detected in feeding pups exposed to lactating rats for a 24 hour period post-dosing, indicating a small degree of lacteal transfer. It is not known whether risedronate sodium is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from risedronate sodium delayed-release tablets, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Risedronate sodium delayed-release tablets are not indicated for use in pediatric patients.
The safety and effectiveness of risedronate sodium immediate-release was assessed in a one-year, randomized, double-blind, placebo-controlled study of 143 pediatric patients (94 received risedronate) with osteogenesis imperfecta (OI). The enrolled population was predominantly patients with mild OI (85% Type-I), aged 4 to less than 16 years, 50% male and 82% Caucasian, with a mean lumbar spine BMD Z-score of -2.08 (2.08 standard deviations below the mean for age-matched controls). Patients received either a 2.5 mg (less than or equal to 30 kg body weight) or 5 mg (greater than 30 kg body weight) daily oral dose. After one year, an increase in lumbar spine BMD in the risedronate sodium immediate-release group compared to the placebo group was observed. However, treatment with risedronate sodium immediate-release did not result in a reduction in the risk of fracture in pediatric patients with OI. In risedronate sodium immediate-release treated subjects, no mineralization defects were noted in paired bone biopsy specimens obtained at baseline and month 12.
The overall safety profile of risedronate in OI patients treated for up to 12 months was generally similar to that of adults with osteoporosis. However, there was an increased incidence of vomiting compared to placebo. In this study, vomiting was observed in 15% of children treated with risedronate sodium immediate-release and 6% of patients treated with placebo. Other adverse reactions reported in greater than or equal to 10% of patients treated with risedronate sodium immediate-release and with a higher frequency than placebo were: pain in the extremity (21% with risedronate sodium immediate-release versus 16% with placebo), headache (20% versus 8%), back pain (17% versus 10%), pain (15% versus 10%), upper abdominal pain (11% versus 8%), and bone pain (10% versus 4%).
8.5 Geriatric Use
Of the patients receiving risedronate sodium delayed-release tablets in postmenopausal osteoporosis studies, 59% were 65 and over, while 13% were 75 and over. No overall differences in safety or effectiveness were observed between these patients and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
8.6 Renal Impairment
Risedronate sodium delayed-release tablets are not recommended for use in patients with severe renal impairment (creatinine clearance less than 30 mL/min) because of lack of clinical experience. No dosage adjustment is necessary in patients with a creatinine clearance greater than or equal to 30 mL/min.
10 OVERDOSAGE
Decreases in serum calcium and phosphorus following substantial overdose may be expected in some patients. Signs and symptoms of hypocalcemia may also occur in some of these patients. While milk or antacids containing calcium may be given to bind risedronate sodium immediate-release and reduce absorption of the drug, the impact of this intervention for risedronate sodium delayed-release tablets has not been evaluated.
In cases of substantial overdose, gastric lavage may be considered to remove unabsorbed drug. Standard procedures that are effective for treating hypocalcemia, including the administration of calcium intravenously, would be expected to restore physiologic amounts of ionized calcium and to relieve signs and symptoms of hypocalcemia.
Lethality after single oral doses of risedronate was seen in female rats at 903 mg/kg and male rats at 1703 mg/kg. The minimum lethal dose in mice and rabbits was 4000 mg/kg and 1000 mg/kg, respectively. These values represent 320 to 620 times the human Paget’s disease dose of 30 mg/day based on surface area (mg/m2).
11 DESCRIPTION
Risedronate sodium delayed-release tablets contain a pH-sensitive enteric coating and a chelating agent (EDTA).
Risedronate is a pyridinyl bisphosphonate that inhibits osteoclast-mediated bone resorption and modulates bone metabolism. Each risedronate sodium delayed-release tablet for oral administration contains the equivalent of 35 mg of anhydrous risedronate sodium in the form of the monohydrate. The chemical name of risedronate sodium is [1-hydroxy-2-(3-pyridinyl)ethylidene]bis[phosphonic acid] monosodium salt. The chemical structure of risedronate sodium monohydrate is the following:
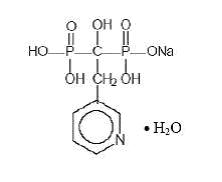
C7H10NO7P2Na•H2O M.W. Monohydrate: 323.10 Anhydrous: 305.10
Risedronate sodium monohydrate is a white to off-white powder. It is soluble in water and in aqueous solutions, and essentially insoluble in common organic solvents.
Inactive Ingredients
Colloidal silicon dioxide, edetate disodium, magnesium stearate, methacrylic acid copolymer, microcrystalline cellulose, polysorbate 80, sodium starch glycolate, stearic acid, talc, and triethyl citrate.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Risedronate has an affinity for hydroxyapatite crystals in bone and acts as an antiresorptive agent. At the cellular level, risedronate inhibits osteoclasts. The osteoclasts adhere normally to the bone surface, but show evidence of reduced active resorption (for example, lack of ruffled border). Histomorphometry in rats, dogs, and minipigs showed that risedronate treatment reduces bone turnover (activation frequency, that is, the rate at which bone remodeling sites are activated) and bone resorption at remodeling sites.
12.2 Pharmacodynamics
Risedronate treatment decreases the elevated rate of bone turnover that is typically seen in postmenopausal osteoporosis. In clinical trials, administration of risedronate sodium immediate-release to postmenopausal women resulted in decreases in biochemical markers of bone turnover, including urinary deoxypyridinoline/creatinine and urinary collagen cross-linked N-telopeptide (markers of bone resorption) and serum bone-specific alkaline phosphatase (a marker of bone formation). At the 5 mg daily dose, decreases in deoxypyridinoline/creatinine were evident within 14 days of treatment. Changes in bone formation markers were observed later than changes in resorption markers, as expected, due to the coupled nature of bone resorption and bone formation; decreases in bone-specific alkaline phosphatase of about 20% were evident within 3 months of treatment. Bone turnover markers reached a nadir of about 40% below baseline values by the sixth month of treatment and remained stable with continued treatment for up to 3 years. Bone turnover is decreased as early as 14 days and maximally within about 6 months of treatment, with achievement of a new steady-state that more nearly approximates the rate of bone turnover seen in premenopausal women. In a 1 year study comparing risedronate sodium delayed-release tablet, 35 mg weekly taken immediately after breakfast versus risedronate sodium immediate-release 5 mg daily oral dosing regimens in postmenopausal women, mean decreases from baseline at 1 year in urinary collagen cross-linked N-telopeptide were 47% in the risedronate sodium delayed-release tablet, 35 mg once-a-week following breakfast group and 42% in the risedronate sodium immediate-release 5 mg daily group. In addition, serum bone-specific alkaline phosphatase at 1 year was reduced by 33% in the risedronate sodium delayed-release tablet, 35 mg once-a-week following breakfast group and 32% in the risedronate sodium immediate-release 5 mg daily group.
12.3 Pharmacokinetics
Absorption
The mean absolute oral bioavailability of the 30 mg risedronate sodium immediate-release tablet taken 4 hours prior to a meal is 0.63% (90% confidence interval [CI]: 0.54% to 0.75%) and is similar to an oral solution. The time to peak concentration (Tmax) for risedronate sodium delayed-release tablet is approximately 3 hours when administered in the morning 4 hours prior to a meal.
Food Effect
In a crossover pharmacokinetic study, the bioavailability of risedronate sodium delayed-release tablets, 35 mg decreased by approximately 30% when administered immediately after a high-fat breakfast compared to administration in the morning 4 hours before a meal.
The bioavailability of the risedronate sodium delayed-release tablet, 35 mg administered after a high-fat breakfast was similar to risedronate sodium 35 mg immediate-release tablet dosed 4 hours before a meal in one study and was approximately 2 to 4 fold greater than the immediate-release 35 mg tablet administered 30 minutes prior to a high-fat breakfast.
In a separate study, risedronate sodium delayed-release tablets administered after dinner exhibited approximately 87% increase in risedronate exposure compared to administration following a breakfast. The safety and efficacy of dosing risedronate sodium delayed-release tablets after dinner has not been evaluated [see Dosage and Administration (2)].
Distribution
The mean steady-state volume of distribution for risedronate is 13.8 L/kg in humans. Human plasma protein binding of drug is about 24%. Preclinical studies in rats and dogs dosed intravenously with single doses of [14C] risedronate indicate that approximately 60% of the dose is distributed to bone. The remainder of the dose is excreted in the urine. After multiple oral dosing in rats, the uptake of risedronate in soft tissues was in the range of 0.001% to 0.01%.
Metabolism
There is no evidence of systemic metabolism of risedronate.
Excretion
In young healthy subjects, approximately half of the absorbed dose of risedronate was excreted in urine within 24 hours, and 85% of an intravenous dose was recovered in the urine over 28 days. Based on simultaneous modeling of serum and urine data for the risedronate sodium immediate-release tablets, mean renal clearance was 105 mL/min (CV = 34%) and mean total clearance was 122 mL/min (CV = 19%), with the difference primarily reflecting nonrenal clearance or clearance due to adsorption to bone. The renal clearance is not concentration dependent, and there is a linear relationship between renal clearance and creatinine clearance. Unabsorbed drug is eliminated unchanged in feces. In osteopenic postmenopausal women, the terminal exponential half-life was 561 hours, mean renal clearance was 52 mL/min (CV = 25%), and mean total clearance was 73 mL/min (CV = 15%).
Specific Populations
Pediatric: Risedronate sodium delayed-release tables are not indicated for use in pediatric patients [see Pediatric Use (8.4)].
Geriatric: Effect of age on bioavailability of risedronate sodium delayed-release tablets has not been evaluated. Based on data from risedronate immediate-release tablet, bioavailability and disposition of risedronate are similar in elderly (greater than 60 years of age) and younger subjects. No dosage adjustment is necessary.
Race: Pharmacokinetic differences due to race have not been studied. The clinical trial of risedronate sodium delayed-release tablets was conducted mostly in Caucasians.
Renal Impairment: Risedronate is excreted unchanged primarily via the kidney. As compared to persons with normal renal function, the renal clearance of risedronate was decreased by about 70% in patients with creatinine clearance of approximately 30 mL/min. Risedronate sodium delayed-release tablets are not recommended for use in patients with severe renal impairment (creatinine clearance less than 30 mL/min). No dosage adjustment is necessary in patients with a creatinine clearance greater than or equal to 30 mL/min.
Hepatic Impairment: No studies have been performed to assess risedronate’s safety or efficacy in patients with hepatic impairment. Risedronate is not metabolized in rat, dog, and human liver preparations. Insignificant amounts (less than 0.1% of intravenous dose) of drug are excreted in the bile in rats. Therefore, dosage adjustment is unlikely to be needed in patients with hepatic impairment.
Drug Interactions: Risedronate is not metabolized and does not induce or inhibit hepatic microsomal drug-metabolizing enzymes (for example, Cytochrome P450).
Calcium supplement: A Phase 1 single-dose, cross-over study in 101 postmenopausal women evaluated the relative bioavailability of risedronate sodium delayed-release tablet, 35 mg taken after breakfast and following a 600 mg elemental calcium/400 international units vitamin D supplement, compared to risedronate sodium delayed-release tablets alone taken after breakfast without calcium or vitamin D supplementation. The addition of the calcium/vitamin D supplement following the meal resulted in an approximate 38% reduction in the amount of risedronate absorbed [see Drug Interactions (7)].
Proton Pump Inhibitors: A Phase 1, 2-period, cross-over study in 60 healthy postmenopausal female subjects evaluated the relative bioavailability of a single dose risedronate sodium delayed-release tablet, 35 mg taken after breakfast following 6 days of esomeprazole magnesium delayed release 40 mg capsules. On Day 6, esomeprazole 40 mg capsule was administered with 240 mL water one hour before breakfast and risedronate sodium delayed-release tablet, 35 mg was administered with 240 mL water within 10 minutes after a standard breakfast. The Cmax and AUCinf of risedronate were increased by 60 percent and 22 percent, respectively, in presence of esomeprazole.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
In a 104 week carcinogenicity study, rats were administered daily oral doses up to approximately 8 times the human Paget’s disease dose of 30 mg/day. There were no significant drug-induced tumor findings in male or female rats. The high dose male group was terminated early in the study (Week 93) due to excessive toxicity, and data from this group were not included in the statistical evaluation of the study results. In an 80 week carcinogenicity study, mice were administered daily oral doses approximately 6.5 times the human dose. There were no significant drug-induced tumor findings in male or female mice.
Mutagenesis
Risedronate did not exhibit genetic toxicity in the following assays: In vitro bacterial mutagenesis in Salmonella and E. coli (Ames assay), mammalian cell mutagenesis in CHO/HGPRT assay, unscheduled DNA synthesis in rat hepatocytes and an assessment of chromosomal aberrations in vivo in rat bone marrow. Risedronate was positive in a chromosomal aberration assay in CHO cells at highly cytotoxic concentrations (greater than 675 mcg/mL, survival of 6% to 7%). When the assay was repeated at doses exhibiting appropriate cell survival (29%), there was no evidence of chromosomal damage.
Impairment of Fertility
In female rats, ovulation was inhibited at an oral dose approximately 5 times the human dose. Decreased implantation was noted in female rats treated with doses approximately 2.5 times the human dose. In male rats, testicular and epididymal atrophy and inflammation were noted at approximately 13 times the human dose. Testicular atrophy was also noted in male rats after 13 weeks of treatment at oral doses approximately 5 times the human dose. There was moderate-to-severe spermatid maturation block after 13 weeks in male dogs at an oral dose approximately 8 times the human dose. These findings tended to increase in severity with increased dose and exposure time.
Dosing multiples provided above are based on the recommended human Paget’s disease dose of 30 mg/day and normalized using body surface area (mg/m2). Actual doses were 24 mg/kg/day in rats, 32 mg/kg/day in mice, and 8, 16 and 40 mg/kg/day in dogs.
13.2 Animal Toxicology and/or Pharmacology
Risedronate demonstrated potent anti-osteoclast, antiresorptive activity in ovariectomized rats and minipigs. Bone mass and biomechanical strength were increased dose-dependently at daily oral doses up to 4 and 25 times the recommended human dose of 5 mg/day for rats and minipigs, respectively. Risedronate treatment maintained the positive correlation between BMD and bone strength and did not have a negative effect on bone structure or mineralization. In intact dogs, risedronate induced positive bone balance at the level of the bone remodeling unit at oral doses ranging from 0.5 to 1.5 times the human dose of 5 mg/day.
In dogs treated with an oral dose approximately 5 times the human dose of 5 mg/day, risedronate caused a delay in fracture healing of the radius. The observed delay in fracture healing is similar to other bisphosphonates. This effect did not occur at a dose approximately 0.5 times the human daily dose.
The Schenk rat assay, based on histologic examination of the epiphyses of growing rats after drug treatment, demonstrated that risedronate did not interfere with bone mineralization even at the highest dose tested, which was approximately 3500 times the lowest antiresorptive dose in this model (1.5 mcg/kg/day) and approximately 800 times the human dose of 5 mg/day. This indicates that risedronate sodium delayed-release tablets administered at the therapeutic dose is unlikely to induce osteomalacia.
Dosing multiples provided above are based on the recommended human osteoporosis dose of 5 mg/day and normalized using body surface area (mg/m2).
14 CLINICAL STUDIES
14.1 Treatment of Osteoporosis in Postmenopausal Women
The efficacy of risedronate sodium delayed-release tablet, 35 mg once-a-week in the treatment of postmenopausal osteoporosis was demonstrated in a randomized, double-blind, active-control trial of approximately 900 subjects. All patients in this study received supplemental calcium (1000 mg/day) and vitamin D (800 to 1000 international units/day). The primary efficacy endpoint was percent change in lumbar spine bone mineral density at 1 year.
Risedronate sodium delayed-release tablet, 35 mg once-a-week administered after breakfast was shown to be non-inferior to risedronate sodium immediate-release 5 mg daily. Table 2 presents the primary efficacy analysis, percent change in lumbar spine BMD, in the intent-to-treat population with last observation carried forward (LOCF).
|
Risedronate sodium immediate-release 5 mg Daily
|
Risedronate sodium delayed-release Tablet, 35 mg Once-a-Week Following Breakfast N = 307 |
|
|
Primary Efficacy (LOCF) n LS Mean (95% CI) LS Mean Difference†
|
270 3.1‡ (2.7, 3.5) |
261 3.3‡ (2.9, 3.7) -0.2 (-0.8, 0.3) |
|
N = number of intent-to-treat patients within specified treatment; n = number of patients with values at the visit. |
||
Fracture efficacy with risedronate sodium immediate-release 5 mg daily
The fracture efficacy of risedronate sodium immediate-release 5 mg daily in the treatment of postmenopausal osteoporosis was demonstrated in 2 large, randomized, placebo-controlled, double-blind studies that enrolled a total of almost 4000 postmenopausal women under similar protocols. The Multinational study (VERT MN) (risedronate sodium immediate-release 5 mg daily, N = 408) was conducted primarily in Europe and Australia; a second study was conducted in North America (VERT NA) (risedronate sodium immediate-release 5 mg daily, N = 821). Patients were selected on the basis of radiographic evidence of previous vertebral fracture, and therefore, had established disease. The average number of prevalent vertebral fractures per patient at study entry was 4 in VERT MN, and 2.5 in VERT NA, with a broad range of baseline BMD levels. All patients in these studies received supplemental calcium 1000 mg/day. Patients with low 25-hydroxyvitamin D3 levels (approximately 40 nmol/L or less) also received 500 international units/day supplemental vitamin D.
Effect on Vertebral Fractures
Fractures of previously undeformed vertebrae (new fractures) and worsening of preexisting vertebral fractures were diagnosed radiographically; some of these fractures were also associated with symptoms (that is, clinical fractures). Spinal radiographs were scheduled annually and prospectively planned analyses were based on the time to a patient’s first diagnosed fracture. The primary endpoint for these studies was the incidence of new and worsening vertebral fractures across the period of 0 to 3 years. Risedronate sodium immediate-release 5 mg daily significantly reduced the incidence of new and worsening vertebral fractures and of new vertebral fractures in both VERT NA and VERT MN at all time points (Table 3). The reduction in risk seen in the subgroup of patients who had 2 or more vertebral fractures at study entry was similar to that seen in the overall study population.
|
||||
|
VERT NA |
Proportion of Patients with Fracture (%)* | |||
|
Placebo N = 678 |
Risedronate N = 696 |
Absolute Risk Reduction (%) |
Relative Risk Reduction (%) |
|
|
New and Worsening 0 to 1 Year 0 to 2 Years 0 to 3 Years |
7.2 12.8 18.5 |
3.9 8.0 13.9 |
3.3 4.8 4.6 |
49 42 33 |
|
New 0 to 1 Year 0 to 2 Years 0 to 3 Years |
6.4 11.7 16.3 |
2.4 5.8 11.3 |
4.0 5.9 5.0 |
65 55 41 |
|
VERT MN |
Placebo N = 346 |
Risedronate sodium 5 mg N = 344 |
Absolute Risk Reduction (%) |
Relative Risk Reduction (%) |
|
New and Worsening 0 to 1 Year 0 to 2 Years 0 to 3 Years |
15.3 28.3 34.0 |
8.2 13.9 21.8 |
7.1 14.4 12.2 |
50 56 46 |
|
New 0 to 1 Year 0 to 2 Years 0 to 3 Years |
13.3 24.7 29.0 |
5.6 11.6 18.1 |
7.7 13.1 10.9 |
61 59 49 |
Effect on Osteoporosis-Related Nonvertebral Fractures
In VERT MN and VERT NA, a prospectively planned efficacy endpoint was defined consisting of all radiographically confirmed fractures of skeletal sites accepted as associated with osteoporosis. Fractures at these sites were collectively referred to as osteoporosis-related nonvertebral fractures. Risedronate sodium immediate-release 5 mg daily significantly reduced the incidence of nonvertebral osteoporosis-related fractures over 3 years in VERT NA (8% versus 5%; relative risk reduction 39%) and reduced the fracture incidence in VERT MN from 16% to 11%. There was a significant reduction from 11% to 7% when the studies were combined, with a corresponding 36% reduction in relative risk. Figure 1 shows the overall results as well as the results at the individual skeletal sites for the combined studies.
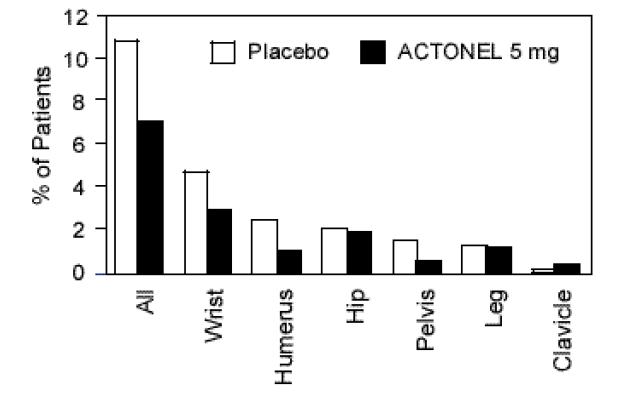
Figure 1: Nonvertebral Osteoporosis-Related Fractures Cumulative Incidence Over 3 Years Combined VERT MN and VERT NA
Histology/Histomorphometry
Bone biopsies from 110 postmenopausal women were obtained at endpoint in the VERT NA study. Patients had received placebo or daily risedronate sodium immediate-release (2.5 mg or 5 mg) for 2 to 3 years. Histologic evaluation (N = 103) showed no osteomalacia, impaired bone mineralization, or other adverse effects on bone in risedronate sodium immediate-release treated women. These findings demonstrate that bone formed during risedronate sodium immediate-release administration is of normal quality. The histomorphometric parameter mineralizing surface, an index of bone turnover, was assessed based upon baseline and post-treatment biopsy samples from 21 treated with placebo and 23 patients treated with risedronate sodium immediate-release 5 mg daily. Mineralizing surface decreased moderately in risedronate sodium immediate-release treated patients (median percent change: placebo, -21%; risedronate sodium immediate-release 5 mg daily, -74%), consistent with the known effects of treatment on bone turnover.
Effect on Height
In the two 3 year osteoporosis treatment studies, standing height was measured yearly by stadiometer. Both risedronate sodium immediate-release 5 mg daily and placebo-treated groups lost height during the studies. Patients who received risedronate sodium immediate-release 5 mg daily had a statistically significantly smaller loss of height than those who received placebo. In VERT MN, the median annual height change was -2.4 mm/yr in the placebo group compared to -1.3 mm/yr in the risedronate sodium immediate-release 5 mg daily group. In VERT NA, the median annual height change was -1.1 mm/yr in the placebo group compared to -0.7 mm/yr in the risedronate sodium immediate-release 5 mg daily group.
Effect on Bone Mineral Density
The results of 4 randomized, placebo-controlled trials in women with postmenopausal osteoporosis (VERT MN, VERT NA, BMD MN, BMD NA) demonstrate that risedronate sodium immediate-release 5 mg daily increases BMD at the spine, hip, and wrist compared to the effects seen with placebo. Table 4 displays the significant increases in BMD seen at the lumbar spine, femoral neck, femoral trochanter, and midshaft radius in these trials compared to placebo. In both VERT studies (VERT MN and VERT NA), risedronate sodium immediate-release 5 mg daily produced increases in lumbar spine BMD that were progressive over the 3 years of treatment, and were statistically significant relative to baseline and to placebo at 6 months and at all later time points.
|
||||||||
|
VERT MN† |
VERT NA† |
BMD MN‡ |
BMD NA‡ |
|||||
|
Placebo N = 323 |
5 mg N = 323 |
Placebo N = 599 |
5 mg N = 606 |
Placebo N = 161 |
5 mg N = 148 |
Placebo N = 191 |
5 mg N = 193 |
|
|
Lumbar Spine Femoral Neck Femoral Trochanter Midshaft Radius |
1.0 -1.4 -1.9 -1.5§ |
6.6 1.6 3.9 0.2§ |
0.8 -1.0 -0.5 -1.2§ |
5.0 1.4 3.0 0.1§ |
0.0 4.0 -1.1 1.3 -0.6 2.5 ND |
0.2 4.8 0.1 2.4 1.3 4.0 ND |
||
|
ND = analysis not done |
||||||||
16 HOW SUPPLIED/STORAGE AND HANDLING
Risedronate sodium delayed-release tablets are available as follows:
35 mg - white to off-white, oval, enteric-coated, biconvex unscored tablet, debossed with "T21" on one side of the tablet and plain on the other side, in unit-dose boxes of 4 (1 x 4) (NDC 0093-5509-44).
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide)
Instruct patients to read the Medication Guide before starting therapy with risedronate sodium delayed-release tablets and to re-read it each time the prescription is renewed.
Instruct patients that risedronate sodium delayed-release tablets and Actonel contain the same active ingredient and if they are taking Actonel, they should not take risedronate sodium delayed-release tablets [see Warnings and Precautions (5.1)].
Instruct patients to pay particular attention to the dosing instructions as clinical benefits may be compromised by failure to take the drug according to instructions.
Instruct patients to take risedronate sodium delayed-release tablets in the morning, while in an upright position (sitting or standing) with at least 4 ounces of plain water immediately following breakfast. Risedronate sodium delayed-release tablets should not be taken before breakfast.
Instruct patients to swallow risedronate sodium delayed-release tablets whole. Patients should not chew, cut, or crush the tablet because of a potential for oropharyngeal irritation, and because the tablet coating is an important part of the delayed-release formulation. Patients should not lie down for 30 minutes after taking the medication.
Instruct patients that if they develop symptoms of esophageal disease (such as difficulty or pain upon swallowing, retrosternal pain or severe persistent or worsening heartburn) they should consult their physician before continuing risedronate sodium delayed-release tablets [see Warnings and Precautions (5.2)].
If a dose of risedronate sodium delayed-release tablets, 35 mg once-a-week is missed, instruct the patient to take one tablet on the morning after they remember and return to taking one tablet once-a-week, as originally scheduled on their chosen day. Patients should not take 2 tablets on the same day.
Instruct patients to take supplemental calcium and vitamin D if dietary intake is inadequate [see Warnings and Precautions (5.3)].
Instruct patients to take calcium supplements, antacids, magnesium-based supplements or laxatives, and iron preparations at a different time of the day because they interfere with the absorption of risedronate sodium delayed-release tablets.
Remind patients to give all of their healthcare providers an accurate medication history. Instruct patients to tell all of their healthcare providers that they are taking risedronate sodium delayed-release tablets. Patients should be instructed that any time they have a medical problem they think may be from risedronate sodium delayed-release tablets they should talk to their doctor.
TEVA PHARMACEUTICALS USA, INC.
North Wales, PA 19454
Rev. C 4/2015
MEDICATION GUIDE
Risedronate Sodium (rih-SED-roe-nate SOE-dee-um) Delayed-Release Tablets
Read this Medication Guide that comes with risedronate sodium delayed-release tablets before you start taking them and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking with your doctor about your medical condition or your treatment. Talk to your doctor if you have any questions about risedronate sodium delayed-release tablets, there may be new information about it.
What is the most important information I should know about risedronate sodium delayed-release tablets?
Risedronate sodium delayed-release tablets can cause serious side effects including:
- Esophagus problems
- Low calcium levels in your blood (hypocalcemia)
- Severe jaw bone problems (osteonecrosis)
- Bone, joint, or muscle pain
- Unusual thigh bone fractures
1. Esophagus problems.
Some people who take risedronate sodium delayed-release tablets may develop problems in the esophagus (the tube that connects the mouth and the stomach). These problems include irritation, inflammation, or ulcers of the esophagus which may sometimes bleed.
- It is important that you take risedronate sodium delayed-release tablets exactly as prescribed to help lower your chance of getting esophagus problems. (See the section “How should I take risedronate sodium delayed-release tablets?”)
- Stop taking risedronate sodium delayed-release tablets and call your doctor right away if you get chest pain, new or worsening heartburn, or have trouble or pain when you swallow.
2. Low calcium levels in your blood (hypocalcemia).
Risedronate sodium delayed-release tablets may lower the calcium levels in your blood. If you have low blood calcium before you start taking risedronate sodium delayed-release tablets, it may get worse during treatment. Your low blood calcium must be treated before you take risedronate sodium delayed-release tablets. Most people with low blood calcium levels do not have symptoms, but some people may have symptoms. Call your doctor right away if you have symptoms of low blood calcium such as:
- Spasms, twitches, or cramps in your muscles
- Numbness or tingling in your fingers, toes, or around your mouth
Your doctor may prescribe calcium and vitamin D to help prevent low calcium levels in your blood, while you are taking risedronate sodium delayed-release tablets. Take calcium and vitamin D as your doctor tells you to.
3. Severe jaw bone problems (osteonecrosis).
Severe jaw bone problems may happen when you take risedronate sodium delayed-release tablets. Your doctor should examine your mouth before you start risedronate sodium delayed-release tablets. Your doctor may tell you to see your dentist before you start risedronate sodium delayed-release tablets. It is important for you to practice good mouth care during treatment with risedronate sodium delayed-release tablets.
4. Bone, joint, or muscle pain.
Some people who take risedronate sodium delayed-release tablets develop severe bone, joint, or muscle pain.
5. Unusual thigh bone fractures.
Some people have developed unusual fractures in their thigh bone. Symptoms of a fracture may include new or unusual pain in your hip, groin, or thigh.
Call your doctor right away if you have any of these side effects.
What are risedronate sodium delayed-release tablets?
Risedronate sodium delayed-release tablets are a prescription medicine used to treat osteoporosis in women after menopause.
It is not known how long risedronate sodium delayed-release tablets work for the treatment and prevention of osteoporosis. You should see your doctor regularly to determine if risedronate sodium delayed-release tablets are still right for you.
Risedronate sodium delayed-release tablets are not for use in children.
Who should not take risedronate sodium delayed-release tablets?
Do not take risedronate sodium delayed-release tablets if you:
- Have certain problems with your esophagus, the tube that connects your mouth and stomach
- Cannot sit or stand up for at least 30 minutes
- Have low blood calcium (hypocalcemia)
- Are allergic to any of the other ingredients in risedronate sodium delayed-release tablets. See the end of this leaflet for a complete list of ingredients in risedronate sodium delayed-release tablets.
What should I tell my healthcare provider before taking risedronate sodium delayed-release tablets?
Before you take risedronate sodium delayed-release tablets, tell your healthcare provider if you:
- Have problems swallowing
- Have stomach or digestive problems
- Have low blood calcium
- Plan to have dental surgery or teeth removed
- Have kidney problems
- Have been told you have trouble absorbing mineral in your stomach or intestines (malabsorption syndrome)
- Are pregnant or plan to become pregnant. It is not known if risedronate sodium delayed-release tablets can harm your unborn baby.
- Are breastfeeding or plan to breastfeed. It is not known if risedronate sodium passes into your breast milk and may harm your baby. You and your doctor should decide if you will take risedronate sodium delayed-release tablets or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements. Certain medicines may affect how risedronate sodium delayed-release tablets work.
Especially tell your doctor if you take:
- Actonel® or other medicines to treat osteoporosis
- calcium supplements
- antacids
- laxatives
- iron supplements
Ask your doctor or pharmacist for a list of these medications, if you are not sure.
Know the medicines you take. Keep a list of them to show your doctor and pharmacist when you get a new medicine.
How should I take risedronate sodium delayed-release tablets?
- Take risedronate sodium delayed-release tablets exactly as your doctor tells you.
- Take risedronate sodium delayed-release tablets 1 time a week right after breakfast. Choose a day of the week to take risedronate sodium delayed-release tablets that best fits your schedule.
- Take risedronate sodium delayed-release tablets with at least 4 ounces (about 1 half cup) of plain water.
- Swallow risedronate sodium delayed-release tablets whole. Do not chew, cut, or crush risedronate sodium delayed-release tablets before swallowing. If you cannot swallow risedronate sodium delayed-release tablets whole, tell your doctor. You may need a different medicine.
After swallowing risedronate sodium delayed-release tablets wait at least 30 minutes:
- Before you lie down. You may sit, stand or walk, and do normal activities like reading.
- Before you take other medicines, including antacids, calcium, and other supplements and vitamins.
Do not lie down for at least 30 minutes after you take risedronate sodium delayed-release tablets.
If you miss your weekly risedronate sodium delayed-release tablet dose, take risedronate sodium delayed-release tablets the morning after you remember then return to your normal schedule. Do not take 2 doses at the same time.
You should take calcium and vitamin D as directed by your doctor.
If you take too many risedronate sodium delayed-release tablets, call your doctor. Do not try to vomit. Do not lie down.
What are the possible side effects of risedronate sodium delayed-release tablets?
Risedronate sodium delayed-release tablets may cause serious side effects:
- See “What is the most important information I should know about risedronate sodium delayed-release tablets”.
The most common side effects of risedronate sodium delayed-release tablets include:
- diarrhea
- flu-like symptoms
- muscle pain
- back and joint pain
- upset stomach
- stomach area (abdominal) pain
You may get allergic reactions, such as hives, swelling of your face, lips, tongue, or throat.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of risedronate sodium delayed-release tablets. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store risedronate sodium delayed-release tablets?
- Store risedronate sodium delayed-release tablets between 68°F to 77°F (20°C to 25°C).
Keep risedronate sodium delayed-release tablets and all medicines out of the reach of children.
General information about the safe and effective use of risedronate sodium delayed-release tablets
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information Leaflet. Do not use risedronate sodium delayed-release tablets for a condition for which they were not prescribed. Do not give risedronate sodium delayed-release tablets to other people, even if they have the same symptoms you have. They may harm them.
This Medication Guide summarizes the most important information about risedronate sodium delayed-release tablets. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about risedronate sodium delayed-release tablets that is written for health professionals.
For more information, call 1-888-838-2872.
What are the ingredients in risedronate sodium delayed-release tablets?
Active ingredient: risedronate sodium
Inactive ingredients: Colloidal silicon dioxide, edetate disodium, magnesium stearate, methacrylic acid copolymer, microcrystalline cellulose, polysorbate 80, sodium starch glycolate, stearic acid, talc, and triethyl citrate.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
All brand names listed are the registered trademarks of their respective owners and are not trademarks of Teva Pharmaceuticals USA, Inc.
TEVA PHARMACEUTICALS USA, INC.
North Wales, PA 19454
Rev. A 12/2014
Package/Label Display Panel
Risedronate Sodium Delayed-Release Tablets (Once-a-Week) 35 mg, 4s Carton Text
NDC 0093-5509-44
Once-a-Week
RISEDRONATE SODIUM Delayed-release Tablets
35 mg
Each enteric-coated tablets contains the equivalent of 35 mg anhydrous risedronate sodium in the form of the monohydrate.
USUAL ADULT DOSAGE: Take as directed by prescriber. See package insert for full prescribing information.
PHARMACIST: Dispense the enclosed Medication Guide to each patient.
Rx only
4 TABLETS
TEVA
| RISEDRONATE SODIUM
risedronate sodium tablet, delayed release |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Labeler - Teva Pharmaceuticals USA, Inc. (001627975) |