Label: QUALAQUIN- quinine sulfate capsule
-
Contains inactivated NDC Code(s)
NDC Code(s): 16590-595-30, 16590-595-60, 16590-595-90 - Packager: STAT RX USA LLC
- This is a repackaged label.
- Source NDC Code(s): 13310-153
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: New Drug Application
Drug Label Information
Updated March 18, 2010
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use QUALAQUIN® safely and effectively. See full prescribing information for QUALAQUIN®.
QUALAQUIN® (quinine sulfate) Capsules, USP for Oral use
Initial U.S. Approval: 2005
BOXED WARNING (See full prescribing information for complete boxed warning)WARNING:
QUALAQUIN® use for the treatment or prevention of nocturnal leg cramps may result in serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP). Chronic renal impairment associated with the development of TTP has been reported. The risk associated with QUALAQUIN use in the absence of evidence of its effectiveness in the treatment or prevention of nocturnal leg cramps outweighs any potential benefit (see WARNINGS).RECENT MAJOR CHANGES
Boxed Warning 11/2009 Warnings and Precautions Thrombocytopenia (5.2) 11/2009 Drug Interactions Effects of Drugs on Quinine Pharmacokinetics (7.1) 11/2009 INDICATIONS AND USAGE
QUALAQUIN® (quinine sulfate) is a cinchona alkaloid indicated for treatment of uncomplicated Plasmodium falciparum malaria (1).
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
- 324 mg hard gelatin, clear cap/clear body capsules, imprinted with 'AR 102' (3).
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Not indicated for the prevention or treatment of nocturnal leg cramps. Risk of serious and life-threatening adverse reactions (1, 5.1).
- Thrombocytopenia, including ITP and HUS/TTP, has been reported. Discontinue drug (5.2).
- QT prolongation and ventricular arrhythmias. Avoid concomitant use with drugs known to prolong QT interval (5.3).
- Avoid concomitant use with rifampin. QUALAQUIN treatment failures have been reported (5.4).
- Avoid concomitant use with neuromuscular blocking agents. QUALAQUIN may potentiate neuromuscular blockade and cause respiratory depression (5.5).
- Serious and life threatening hypersensitivity reactions. Discontinue drug (4, 5.6).
- Atrial fibrillation and flutter. Paradoxical increase in ventricular rate may occur. Closely monitor digoxin levels if used concomitantly (5.7).
- Hypoglycemia. Monitor for signs and symptoms (5.8).
ADVERSE REACTIONS
Most common adverse reactions are a cluster of symptoms called "cinchonism", which occurs to some degree in almost all patients taking quinine: headache, vasodilation and sweating, nausea, tinnitus, hearing impairment, vertigo or dizziness, blurred vision, disturbance in color perception, vomiting, diarrhea, abdominal pain, deafness, blindness, and disturbances in cardiac rhythm or conduction (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Mutual Pharmaceutical Company, Inc. at 1-888-351-3786 or drugsafety@urlpharma.com or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Interacting Drug Interaction Drugs known to prolong QT interval (e.g., Class IA and Class III antiarrhythmic agents). QUALAQUIN prolongs QT interval, ECG abnormalities including QT prolongation and Torsades des Pointes. Avoid concomitant use (5.3). Other antimalarials (e.g., halofantrine, mefloquine). ECG abnormalities including QT prolongation. Avoid concomitant use (5.3, 7.2). CYP3A4 inducers or inhibitors Alteration in plasma quinine concentration. Monitor for lack of efficacy or increased adverse events of quinine (7.1). CYP3A4 and CYP2D6 substrates Quinine is an inhibitor of CYP3A4 and CYP2D6. Monitor for lack of efficacy or increased adverse events of the co-administered drug (7.1). Digoxin Increased digoxin plasma concentration (5.8, 7.1). USE IN SPECIFIC POPULATIONS
- Renal impairment: Reduce dose and dosing frequency for patients with severe chronic renal impairment (2.2, 8.6, 12.3).
- Hepatic impairment: Closely monitor for adverse events (8.7, 12.3).
- Pregnancy: Based on animal data may cause fetal harm. Use only if the potential benefit justifies the risk (8.1).
- Nursing Mothers: Exercise caution when administering to a nursing woman (8.3).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 11/2009
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING:
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Uncomplicated P. falciparum Malaria
2.2 Renal Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Use of QUALAQUIN for Treatment or Prevention of Nocturnal Leg Cramps
5.2 Thrombocytopenia
5.3 QT Prolongation and Ventricular Arrhythmias
5.4 Concomitant Use of Rifampin
5.5 Concomitant Use of Neuromuscular Blocking Agents
5.6 Hypersensitivity
5.7 Atrial Fibrillation and Flutter
5.8 Hypoglycemia
6 ADVERSE REACTIONS
6.1 Overall
7 DRUG INTERACTIONS
7.1 Effects of Drugs and Other Substances on Quinine Pharmacokinetics
7.2 Effects of Quinine on the Pharmacokinetics of Other Drugs
7.3 Drug/Laboratory Interactions
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Labor and Delivery
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
16 HOW SUPPLIED / STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage
17 PATIENT COUNSELING INFORMATION
17.1 Dosing Instructions
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING:
QUALAQUIN® use for the treatment or prevention of nocturnal leg cramps may result in serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP). Chronic renal impairment associated with the development of TTP has been reported. The risk associated with QUALAQUIN use in the absence of evidence of its effectiveness in the treatment or prevention of nocturnal leg cramps outweighs any potential benefit (see WARNINGS).
-
1 INDICATIONS AND USAGE
QUALAQUIN (quinine sulfate) is an antimalarial drug indicated only for treatment of uncomplicated Plasmodium falciparum malaria. Quinine sulfate has been shown to be effective in geographical regions where resistance to chloroquine has been documented [see Clinical Studies (14)].
QUALAQUIN oral capsules are not approved for:
- Treatment of severe or complicated P. falciparum malaria.
- Prevention of malaria.
- Treatment or prevention of nocturnal leg cramps [see Warnings and Precautions (5.1)].
-
2 DOSAGE AND ADMINISTRATION
2.1 Treatment of Uncomplicated P. falciparum Malaria
For treatment of uncomplicated P. falciparum malaria in adults: Orally, 648 mg (two capsules) every 8 hours for 7 days [see Clinical Studies (14)].
QUALAQUIN should be taken with food to minimize gastric upset [see Clinical Pharmacology (12.3)].
2.2 Renal Impairment
In patients with acute uncomplicated malaria and severe chronic renal impairment, the following dosage regimen is recommended: one loading dose of 648 mg QUALAQUIN followed 12 hours later by maintenance doses of 324 mg every 12 hours.
The effects of mild and moderate renal impairment on the safety and pharmacokinetics of quinine sulfate are not known [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
QUALAQUIN is contraindicated in patients with the following:
- Prolonged QT interval. One case of a fatal ventricular arrhythmia was reported in an elderly patient with a prolonged QT interval at baseline, who received quinine sulfate intravenously for P. falciparum malaria [see Warnings and Precautions (5.3)].
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency.
- Hemolysis can occur in patients with G6PD deficiency receiving quinine.
- Known hypersensitivity reactions to quinine.
- These include, but are not limited to, the following [see Warnings and Precautions (5.6)]:
- Thrombocytopenia
- Idiopathic thrombocytopenia purpura (ITP) and Thrombotic thrombocytopenic purpura (TTP)
- Hemolytic uremic syndrome (HUS)
- Blackwater fever (acute intravascular hemolysis, hemoglobinuria, and hemoglobinemia)
- These include, but are not limited to, the following [see Warnings and Precautions (5.6)]:
- Known hypersensitivity to mefloquine or quinidine: cross-sensitivity to quinine has been documented [see Warnings and Precautions (5.6)].
- Myasthenia gravis. Quinine has neuromuscular blocking activity, and may exacerbate muscle weakness.
- Optic neuritis. Quinine may exacerbate active optic neuritis [see Adverse Reactions (6)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Use of QUALAQUIN for Treatment or Prevention of Nocturnal Leg Cramps
QUALAQUIN may cause unpredictable serious and life-threatening hematologic reactions including thrombocytopenia and hemolytic-uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP) in addition to hypersensitivity reactions, QT prolongation, serious cardiac arrhythmias including torsades de pointes, and other serious adverse events requiring medical intervention and hospitalization. Chronic renal impairment associated with the development of TTP, and fatalities have also been reported. The risk associated with the use of QUALAQUIN in the absence of evidence of its effectiveness for treatment or prevention of nocturnal leg cramps, outweighs any potential benefit in treating and/or preventing this benign, self-limiting condition [see Boxed Warning and Contraindications (4)].
5.2 Thrombocytopenia
Quinine-induced thrombocytopenia is an immune-mediated disorder. Severe cases of thrombocytopenia that are fatal or life threatening have been reported, including cases of HUS/TTP. Chronic renal impairment associated with the development of TTP has also been reported. Thrombocytopenia usually resolves within a week upon discontinuation of quinine. If quinine is not stopped, a patient is at risk for fatal hemorrhage. Upon re-exposure to quinine from any source, a patient with quinine-dependent antibodies could develop thrombocytopenia that is more rapid in onset and more severe than the original episode.
5.3 QT Prolongation and Ventricular Arrhythmias
QT interval prolongation has been a consistent finding in studies which evaluated electrocardiographic changes with oral or parenteral quinine administration, regardless of age, clinical status, or severity of disease. The maximum increase in QT interval has been shown to correspond with peak quinine plasma concentration [see Clinical Pharmacology (12.2)]. Quinine sulfate has been rarely associated with potentially fatal cardiac arrhythmias, including torsades de pointes, and ventricular fibrillation.
QUALAQUIN is not recommended for use with other drugs known to cause QT prolongation, including Class IA antiarrhythmic agents (e.g., quinidine, procainamide, disopyramide), and Class III antiarrhythmic agents (e.g., amiodarone, sotalol, dofetilide).
The use of macrolide antibiotics such as erythromycin should be avoided in patients receiving QUALAQUIN. Fatal torsades de pointes was reported in an elderly patient who received concomitant quinine, erythromycin, and dopamine. Although a causal relationship between a specific drug and the arrhythmia was not established in this case, erythromycin is a CYP3A4 inhibitor and could potentially increase quinine plasma levels when used concomitantly. A related macrolide antibiotic, troleandomycin, has been shown to increase quinine exposure in a pharmacokinetic study [see Drug Interactions (7.1)].
Quinine may inhibit the metabolism of certain drugs that are CYP3A4 substrates and are known to cause QT prolongation, e.g., astemizole, cisapride, terfenadine, pimozide, halofantrine and quinidine. Torsades de pointes has been reported in patients who received concomitant quinine and astemizole. Therefore, concurrent use of QUALAQUIN with these medications, or drugs with similar properties, should be avoided [see Drug Interactions (7.2)].
Concomitant administration of QUALAQUIN with the antimalarial drugs, mefloquine or halofantrine, may result in electrocardiographic abnormalities, including QT prolongation, and increase the risk for torsades de pointes or other serious ventricular arrhythmias. Concurrent use of QUALAQUIN and mefloquine may also increase the risk of seizures [see Drug Interactions (7.2)].
QUALAQUIN should also be avoided in patients with known prolongation of QT interval and in patients with clinical conditions known to prolong the QT interval, such as uncorrected hypokalemia, bradycardia, and certain cardiac conditions [see Contraindications (4)].
5.4 Concomitant Use of Rifampin
Treatment failures may result from the concurrent use of rifampin with QUALAQUIN, due to decreased plasma concentrations of quinine, and concomitant use of these medications should be avoided [see Drug Interactions (7.1)].
5.5 Concomitant Use of Neuromuscular Blocking Agents
The use of neuromuscular blocking agents should be avoided in patients receiving QUALAQUIN. In one patient who received pancuronium during an operative procedure, subsequent administration of quinine resulted in respiratory depression and apnea. Although there are no clinical reports with succinylcholine or tubocurarine, quinine may also potentiate neuromuscular blockade when used with these drugs [see Drug Interactions (7.2)].
5.6 Hypersensitivity
Serious hypersensitivity reactions reported with quinine sulfate include anaphylactic shock, anaphylactoid reactions, urticaria, serious skin rashes, including Stevens-Johnson syndrome and toxic epidermal necrolysis, angioedema, facial edema, bronchospasm, and pruritus.
A number of other serious adverse reactions reported with quinine, including thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS), thrombocytopenia, immune thrombocytopenic purpura (ITP), blackwater fever, disseminated intravascular coagulation, leukopenia, neutropenia, granulomatous hepatitis, and acute interstitial nephritis may also be due to hypersensitivity reactions.
QUALAQUIN should be discontinued in case of any signs or symptoms of hypersensitivity [see Contraindications (4)].
5.7 Atrial Fibrillation and Flutter
QUALAQUIN should be used with caution in patients with atrial fibrillation or atrial flutter. A paradoxical increase in ventricular response rate may occur with quinine, similar to that observed with quinidine. If digoxin is used to prevent a rapid ventricular response, serum digoxin levels should be closely monitored, because digoxin levels may be increased with use of quinine [see Drug Interactions (7.2)].
-
6 ADVERSE REACTIONS
6.1 Overall
Quinine can adversely affect almost every body system. The most common adverse events associated with quinine use are a cluster of symptoms called "cinchonism", which occurs to some degree in almost all patients taking quinine. Symptoms of mild cinchonism include headache, vasodilation and sweating, nausea, tinnitus, hearing impairment, vertigo or dizziness, blurred vision, and disturbance in color perception. More severe symptoms of cinchonism are vomiting, diarrhea, abdominal pain, deafness, blindness, and disturbances in cardiac rhythm or conduction. Most symptoms of cinchonism are reversible and resolve with discontinuation of quinine.
The following ADVERSE REACTIONS have been reported with quinine sulfate. Most of these reactions are thought to be uncommon, but the actual incidence is unknown:
General: fever, chills, sweating, flushing, asthenia, lupus-like syndrome, and hypersensitivity reactions.
Hematologic: agranulocytosis, hypoprothrombinemia, thrombocytopenia, disseminated intravascular coagulation, hemolytic anemia; hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura, petechiae, ecchymosis, hemorrhage, coagulopathy, blackwater fever, leukopenia, neutropenia, pancytopenia, aplastic anemia, and lupus anticoagulant.
Neuropsychiatric: headache, diplopia, confusion, altered mental status, seizures, coma, disorientation, tremors, restlessness, ataxia, acute dystonic reaction, aphasia, and suicide.
Dermatologic: cutaneous rashes, including urticarial, papular, or scarlatinal rashes, pruritus, bullous dermatitis, exfoliative dermatitis, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, fixed drug eruption, photosensitivity reactions, allergic contact dermatitis, acral necrosis, and cutaneous vasculitis.
Respiratory: asthma, dyspnea, pulmonary edema.
Cardiovascular: chest pain, vasodilatation, hypotension, postural hypotension, tachycardia, bradycardia, palpitations, syncope, atrioventricular block, atrial fibrillation, irregular rhythm, unifocal premature ventricular contractions, nodal escape beats, U waves, QT prolongation, ventricular fibrillation, ventricular tachycardia, torsades de pointes, and cardiac arrest.
Gastrointestinal: nausea, vomiting, diarrhea, abdominal pain, gastric irritation, and esophagitis.
Hepatobiliary: granulomatous hepatitis, hepatitis, jaundice, and abnormal liver function tests.
Metabolic: hypoglycemia and anorexia.
Musculoskeletal: myalgias and muscle weakness.
Renal: hemoglobinuria, renal failure, renal impairment, and acute interstitial nephritis.
Special Senses: visual disturbances, including blurred vision with scotomata, sudden loss of vision, photophobia, diplopia, night blindness, diminished visual fields, fixed pupillary dilatation, disturbed color vision, optic neuritis, blindness, vertigo, tinnitus, hearing impairment, and deafness.
-
7 DRUG INTERACTIONS
7.1 Effects of Drugs and Other Substances on Quinine Pharmacokinetics
Quinine is a P-gp substrate and is primarily metabolized by CYP3A4. Other enzymes, including CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP2E1 may contribute to the metabolism of quinine [see Clinical Pharmacology (12.3)].
Antacids: Antacids containing aluminum and/or magnesium may delay or decrease absorption of quinine. Concomitant administration of these antacids with QUALAQUIN should be avoided.
Antiepileptics (AEDs) (carbamazepine, phenobarbital, and phenytoin): Carbamazepine, phenobarbital, and phenytoin are CYP3A4 inducers and may decrease quinine plasma concentrations if used concurrently with QUALAQUIN.
Cholestyramine: In 8 healthy subjects who received quinine sulfate 600 mg with or without 8 grams of cholestyramine resin, no significant difference in quinine pharmacokinetic parameters was seen.
Cigarette Smoking (CYP1A2 inducer): In healthy male heavy smokers, the mean quinine AUC following a single 600 mg dose was 44% lower, the mean Cmax was 18% lower, and the elimination half-life was shorter (7.5 hours versus 12 hours) than in their non-smoking counterparts. However, in malaria patients who received the full 7-day course of quinine therapy, cigarette smoking produced only a 25% decrease in median quinine AUC and a 16.5% decrease in median Cmax, suggesting that the already reduced clearance of quinine in acute malaria could have diminished the metabolic induction effect of smoking. Because smoking did not appear to influence the therapeutic outcome in malaria patients, it is not necessary to increase the dose of quinine in the treatment of acute malaria in heavy cigarette smokers.
Grapefruit juice (P-gp/CYP3A4 inhibitor): In a pharmacokinetic study involving 10 healthy subjects, the administration of a single 600 mg dose of quinine sulfate with grapefruit juice (full-strength or half-strength) did not significantly alter the pharmacokinetic parameters of quinine. QUALAQUIN may be taken with grapefruit juice.
Histamine H2-receptor blockers [cimetidine, ranitidine (nonspecific CYP450 inhibitors)]: In healthy subjects who were given a single oral 600 mg dose of quinine sulfate after pretreatment with cimetidine (200 mg three times daily and 400 mg at bedtime for 7 days) or ranitidine (150 mg twice daily for 7 days), the apparent oral clearance of quinine decreased and the mean elimination half-life increased significantly when given with cimetidine but not with ranitidine. Compared to untreated controls, the mean AUC of quinine increased by 20% with ranitidine and by 42% with cimetidine (p<0.05) without a significant change in mean quinine Cmax. When quinine is to be given concomitantly with a histamine H2-receptor blocker, the use of ranitidine is preferred over cimetidine. Although cimetidine and ranitidine may be used concomitantly with QUALAQUIN, patients should be monitored closely for adverse events associated with quinine.
Isoniazid: Isoniazid 300 mg/day pretreatment for 1 week did not significantly alter the pharmacokinetic parameter values of quinine. Adjustment of QUALAQUIN dosage is not necessary when isoniazid is given concomitantly.
Ketoconazole (CYP3A4 inhibitor): In a crossover study, healthy subjects (N=9) who received a single oral dose of quinine hydrochloride (500 mg) concomitantly with ketoconazole (100 mg twice daily for 3 days) had a mean quinine AUC that was higher by 45% and a mean oral clearance of quinine that was 31% lower than after receiving quinine alone. Although no change in the QUALAQUIN dosage regimen is necessary with concomitant ketoconazole, patients should be monitored closely for adverse reactions associated with quinine.
Macrolide antibiotics (erythromycin, troleandomycin) (CYP3A4 inhibitors): In a crossover study (N=10), healthy subjects who received a single oral 600 mg dose of quinine sulfate with the macrolide antibiotic, troleandomycin (500 mg every 8 hours) exhibited a 87% higher mean quinine AUC, a 45% lower mean oral clearance of quinine, and a 81% lower formation clearance of the main metabolite, 3-hydroxyquinine, than when quinine was given alone. Therefore, concomitant administration of troleandomycin with QUALAQUIN should be avoided.
Erythromycin was shown to inhibit the metabolism of quinine in vitro using human liver microsomes. Therefore, concomitant administration of erythromycin with QUALAQUIN is likely to increase plasma quinine concentrations, and should be avoided [see Warnings and Precautions (5.3)].
Oral contraceptives (estrogen, progestin): In 7 healthy females who were using single-ingredient progestin or combination estrogen-containing oral contraceptives, the pharmacokinetic parameters of a single 600 mg dose of quinine sulfate were not altered in comparison to those observed in 7 age-matched female control subjects not using oral contraceptives.
Rifampin (CYP3A4 inducer): In patients with uncomplicated P. falciparum malaria who received quinine sulfate 10 mg/kg concomitantly with rifampin 15 mg/kg/day for 7 days (N=29), the median AUC of quinine between days 3 and 7 of therapy was 75% lower as compared to those who received quinine monotherapy. In healthy subjects (N=9) who received a single oral 600 mg dose of quinine sulfate after 2 weeks of pretreatment with rifampin 600 mg/day, the mean quinine AUC and Cmax decreased by 85% and 55%, respectively. Therefore the concomitant administration of rifampin with QUALAQUIN should be avoided [see Warnings and Precautions (5.4)].
Tetracycline: In 8 patients with acute uncomplicated P. falciparum malaria who were treated with oral quinine sulfate (600 mg every 8 hours for 7 days) in combination with oral tetracycline (250 mg every 6 hours for 7 days), the mean plasma quinine concentrations were about two-fold higher than in 8 patients who received quinine monotherapy. Although tetracycline may be concomitantly administered with QUALAQUIN, patients should be monitored closely for adverse reactions associated with quinine sulfate.
Theophylline or aminophylline: In 20 healthy subjects who received multiple doses of QUALAQUIN (648 mg every 8 hours × 7 days) with a single 300 mg oral dose of theophylline, the quinine mean Cmax and AUC were increased by 13% and 14% respectively. Although no change in the QUALAQUIN dosage regimen is necessary with concomitant theophylline or aminophylline, patients should be monitored closely for adverse reactions associated with quinine.
7.2 Effects of Quinine on the Pharmacokinetics of Other Drugs
Results of in vivo drug interaction studies suggest that quinine has the potential to inhibit the metabolism of drugs that are substrates of CYP3A4 and CYP2D6. Quinine inhibits P-gp and has the potential to affect the transport of drugs that are P-gp substrates.
Anticonvulsants (carbamazepine, phenobarbital, and phenytoin): A single 600 mg oral dose of quinine sulfate increased the mean plasma Cmax, and AUC0–24 of single oral doses of carbamazepine (200 mg) and phenobarbital (120 mg) but not phenytoin (200 mg) in 8 healthy subjects. The mean AUC increases of carbamazepine, phenobarbital and phenytoin were 104%, 81% and 4%, respectively; the mean increases in Cmax were 56%, 53%, and 4%, respectively. Mean urinary recoveries of the three antiepileptics over 24 hours were also profoundly increased by quinine. If concomitant administration with carbamazepine or phenobarbital cannot be avoided, frequent monitoring of anticonvulsant drug concentrations is recommended. Additionally, patients should be monitored closely for adverse reactions associated with these anticonvulsants.
Astemizole (CYP3A4 substrate): Elevated plasma astemizole concentrations were reported in a subject who experienced torsades de pointes after receiving three doses of quinine sulfate for nocturnal leg cramps concomitantly with chronic astemizole 10 mg/day. The concurrent use of QUALAQUIN with astemizole and other CYP3A4 substrates with QT prolongation potential (e.g., cisapride, terfenadine, halofantrine, pimozide and quinidine) should also be avoided [see Warnings and Precautions (5.3)].
Atorvastatin (CYP3A4 substrate): Rhabdomyolysis with acute renal failure secondary to myoglobinuria was reported in a patient taking atorvastatin administered with a single dose of quinine. Quinine may increase plasma concentrations of atorvastatin, thereby increasing the risk of myopathy or rhabdomyolysis. Thus, clinicians considering combined therapy of QUALAQUIN with atorvastatin or other HMG-CoA reductase inhibitors ("statins") that are CYP3A4 substrates (e.g., simvastatin, lovastatin) should carefully weigh the potential benefits and risks of each medication. If QUALAQUIN is used concomitantly with any of these statins, lower starting and maintenance doses of the statin should be considered. Patients should also be monitored closely for any signs or symptoms of muscle pain, tenderness, or weakness, particularly during initial therapy. If marked creatine phosphokinase (CPK) elevation occurs or myopathy (defined as muscle aches or muscle weakness in conjunction with CPK values >10 times the upper limit of normal) is diagnosed or suspected, atorvastatin or other statin should be discontinued.
Desipramine (CYP2D6 substrate): Quinine (750 mg/day for 2 days) decreased the metabolism of desipramine in patients who were extensive CYP2D6 metabolizers, but had no effect in patients who were poor CYP2D6 metabolizers. Lower doses (80 mg to 400 mg) of quinine did not significantly affect the pharmacokinetics of other CYP2D6 substrates, namely, debrisoquine, dextromethorphan, and methoxyphenamine. Although clinical drug interaction studies have not been performed, antimalarial doses (greater than or equal to 600 mg) of quinine may inhibit the metabolism of other drugs that are CYP2D6 substrates (e.g., flecainide, debrisoquine, dextromethorphan, metoprolol, paroxetine). Patients taking medications that are CYP2D6 substrates with QUALAQUIN should be monitored closely for adverse reactions associated with these medications.
Digoxin (P-gp substrate): In 4 healthy subjects who received digoxin (0.5 to 0.75 mg/day) during treatment with quinine (750 mg/day), a 33% increase in mean steady state AUC of digoxin and a 35% reduction in the steady-state biliary clearance of digoxin were observed compared to digoxin alone. Thus, if QUALAQUIN is administered to patients receiving digoxin, plasma digoxin concentrations should be closely monitored, and the digoxin dose adjusted, as necessary [see Warnings and Precautions (5.7)].
Halofantrine: Although not studied clinically, quinine was shown to inhibit the metabolism of halofantrine in vitro using human liver microsomes. Therefore, concomitant administration of QUALAQUIN is likely to increase plasma halofantrine concentrations [see Warnings and Precautions (5.3)].
Mefloquine: In 7 healthy subjects who received mefloquine (750 mg) at 24 hours before an oral 600 mg dose of quinine sulfate, the AUC of mefloquine was increased by 22% compared to mefloquine alone. In this study, the QTc interval was significantly prolonged in the subjects who received mefloquine and quinine sulfate 24 hours apart. The concomitant administration of mefloquine and QUALAQUIN may produce electrocardiographic abnormalities (including QTc prolongation) and may increase the risk of seizures [see Warnings and Precautions (5.3)].
Midazolam (CYP3A4 substrate): In 23 healthy subjects who received multiple doses of QUALAQUIN 324 mg three times daily × 7 days with a single oral 2 mg dose of midazolam, the mean AUC and Cmax of midazolam and 1-hydroxymidazolam were not significantly affected. This finding indicates that 7-day dosing with QUALAQUIN 324 mg every 8 hours did not induce the metabolism of midazolam.
Neuromuscular blocking agents (pancuronium, succinylcholine, tubocurarine): In one report, quinine potentiated neuromuscular blockade in a patient who received pancuronium during an operative procedure, and subsequently (3 hours after receiving pancuronium) received quinine 1800 mg daily. Quinine may also enhance the neuromuscular blocking effects of succinylcholine and tubocurarine [see Warnings and Precautions (5.5)].
Theophylline or aminophylline (CYP1A2 substrate): In 19 healthy subjects who received multiple doses of QUALAQUIN 648 mg every 8 hours × 7 days with a single 300 mg oral dose of theophylline, the mean theophylline AUC was 10% lower than when theophylline was given alone. There was no significant effect on mean theophylline Cmax. Therefore, if QUALAQUIN is co-administered to patients receiving theophylline or aminophylline, plasma theophylline concentrations should be monitored frequently to ensure therapeutic concentrations.
Warfarin and oral anticoagulants: Cinchona alkaloids, including quinine, may have the potential to depress hepatic enzyme synthesis of vitamin K-dependent coagulation pathway proteins and may enhance the action of warfarin and other oral anticoagulants. Quinine may also interfere with the anticoagulant effect of heparin. Thus, in patients receiving these anticoagulants, the prothrombin time (PT), partial thromboplastin time (PTT), or international normalization ratio (INR) should be closely monitored as appropriate, during concurrent therapy with QUALAQUIN.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are extensive published data but few well-controlled studies of QUALAQUIN in pregnant women. Published data on over 1,000 pregnancy exposures to quinine did not show an increase in teratogenic effects over the background rate in the general population; however the majority of these exposures were not in the first trimester. In developmental and reproductive toxicity studies, central nervous system (CNS) and ear abnormalities and increased fetal deaths occurred in some species when pregnant animals received quinine at doses about 1 to 4 times the human clinical dose. Quinine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
P. falciparum malaria carries a higher risk of morbidity and mortality in pregnant women than in the general population. Pregnant women with P. falciparum malaria have an increased incidence of fetal loss (including spontaneous abortion and stillbirth), preterm labor and delivery, intrauterine growth retardation, low birth weight, and maternal death. Therefore, treatment of malaria in pregnancy is important.
Hypoglycemia, due to increased pancreatic secretion of insulin, has been associated with quinine use, particularly in pregnant women.
Quinine crosses the placenta with measurable blood concentrations in the fetus. In 8 women who delivered live infants 1 to 6 days after starting quinine therapy, umbilical cord plasma quinine concentrations were between 1.0 and 4.6 mg/L (mean 2.4 mg/L) and the mean (±SD) ratio of cord plasma to maternal plasma quinine concentrations was 0.32 ± 0.14. Quinine levels in the fetus may not be therapeutic. If congenital malaria is suspected after delivery, the infant should be evaluated and treated appropriately.
A study from Thailand (1999) of women with P. falciparum malaria who were treated with oral quinine sulfate 10 mg/kg 3 times daily for 7 days at anytime in pregnancy reported no significant difference in the rate of stillbirths at >28 weeks of gestation in women treated with quinine (10 of 633 women [1.6%]) as compared with a control group without malaria or exposure to antimalarial drugs during pregnancy (40 of 2201 women [1.8%]). The overall rate of congenital malformations (9 of 633 offspring [1.4%]) was not different for women who were treated with quinine sulfate compared with the control group (38 of 2201 offspring [1.7%]). The spontaneous abortion rate was higher in the control group (10.9%) than in women treated with quinine sulfate (3.5%) [OR = 3.1; 95% CI 2.1-4.7]. An epidemiologic survey that included 104 mother-child pairs exposed to quinine during the first 4 months of pregnancy, found no increased risk of structural birth defects was seen (2 fetal malformations [1.9%]). Rare and isolated case reports describe deafness and optic nerve hypoplasia in children exposed in utero due to maternal ingestion of high doses of quinine.
In animal developmental studies conducted in multiple animal species, pregnant animals received quinine by the subcutaneous or intramuscular route at dose levels similar to the maximum recommended human dose (based on body surface area). In rabbits, chinchillas, and dogs, there were increases in fetal death in utero. Rabbit offspring had increased rates of degenerated auditory nerve and spiral ganglion; chinchilla offspring had increased rates of growth restriction in utero; and both rabbit and chinchilla offspring had increased rates of CNS anomalies such as anencephaly and microcephaly. Guinea pig offspring had increased rates of hemorrhage and mitochondrial change in the cochlea. There were no teratogenic findings in rats and monkeys.
8.2 Labor and Delivery
There is no evidence that quinine causes uterine contractions at the doses recommended for the treatment of malaria. In doses several-times higher than those used to treat malaria, quinine may stimulate the pregnant uterus.
8.3 Nursing Mothers
There is limited information on the safety of quinine in breastfed infants. No toxicity was reported in infants in a single study where oral quinine sulfate (10 mg/kg every 8 hours for 1 to 10 days) was administered to 25 lactating women. It is estimated from this study that breastfed infants would receive less than 2 to 3 mg per day of quinine base (< 0.4% of the maternal dose) via breast milk [see Clinical Pharmacology (12.3)].
Although quinine is generally considered compatible with breastfeeding, the risks and benefits to infant and mother should be assessed. Caution should be exercised when administered to a nursing woman.
If malaria is suspected in the infant, appropriate evaluation and treatment should be provided. Plasma quinine levels may not be therapeutic in infants of nursing mothers receiving QUALAQUIN.
8.4 Pediatric Use
The safety and efficacy of QUALAQUIN in pediatric patients under the age of 16 has not been established.
8.5 Geriatric Use
Clinical studies of quinine sulfate did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
8.6 Renal Impairment
Clearance of quinine is decreased in patients with severe chronic renal failure. The dosage and dosing frequency should be reduced [see Dosage and Administration (2.2), Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Close monitoring is recommended for patients with impaired liver function, as it may increase exposure to quinine [see Clinical Pharmacology (12.3)].
-
10 OVERDOSAGE
Quinine overdose can be associated with serious complications, including visual impairment, hypoglycemia, cardiac arrhythmias, and death. Visual impairment can range from blurred vision and defective color perception, to visual field constriction and permanent blindness. Cinchonism occurs in virtually all patients with quinine overdose. Symptoms range from headache, nausea, vomiting, abdominal pain, diarrhea, tinnitus, vertigo, hearing impairment, sweating, flushing, and blurred vision, to deafness, blindness, serious cardiac arrhythmias, hypotension, and circulatory collapse. Central nervous system toxicity (drowsiness, disturbances of consciousness, ataxia, convulsions, respiratory depression and coma) has also been reported with quinine overdose, as well as pulmonary edema and adult respiratory distress syndrome.
Most toxic reactions are dose-related; however, some reactions may be idiosyncratic because of the variable sensitivity of patients to the toxic effects of quinine. A lethal dose of quinine has not been clearly defined, but fatalities have been reported after the ingestion of 2 to 8 grams in adults.
Quinine, like quinidine, has Class I antiarrhythmic properties. The cardiotoxicity of quinine is due to its negative inotropic action, and to its effect on cardiac conduction, resulting in decreased rates of depolarization and conduction, and increased action potential and effective refractory period. ECG changes observed with quinine overdose include sinus tachycardia, PR prolongation, T wave inversion, bundle branch block, an increased QT interval, and a widening of the QRS complex. Quinine's alpha-blocking properties may result in hypotension and further exacerbate myocardial depression by decreasing coronary perfusion. Quinine overdose has been also associated with hypotension, cardiogenic shock, and circulatory collapse, ventricular arrhythmias, including ventricular tachycardia, ventricular fibrillation, idioventricular rhythm, and torsades de pointes, as well as bradycardia, and atrioventricular block [see Warnings and Precautions (5), Clinical Pharmacology (12.3)].
Quinine is rapidly absorbed, and attempts to remove residual quinine sulfate from the stomach by gastric lavage may not be effective. Multiple-dose activated charcoal has been shown to decrease plasma quinine concentrations [see Clinical Pharmacology (12.3)].
Forced acid diuresis, hemodialysis, charcoal column hemoperfusion, and plasma exchange were not found to be effective in significantly increasing quinine elimination in a series of 16 patients.
-
11 DESCRIPTION
QUALAQUIN (quinine sulfate) is a cinchona alkaloid chemically described as cinchonan-9-ol, 6'-methoxy-, (8α, 9R)-, sulfate (2:1) (salt), dihydrate with a molecular formula of (C20H24N2O2)2•H2SO4•2H2O and a molecular weight of 782.96.
The structural formula of quinine sulfate is:
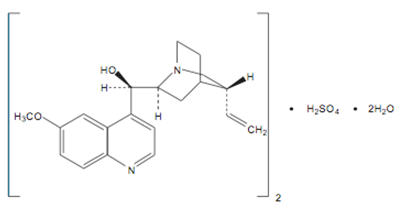
Quinine sulfate occurs as a white, crystalline powder that darkens on exposure to light. It is odorless and has a persistent very bitter taste. It is only slightly soluble in water, alcohol, chloroform, and ether.
QUALAQUIN is supplied for oral administration as capsules containing 324 mg of the active ingredient quinine sulfate USP, equivalent to 269 mg free base. Inactive ingredients: corn starch, magnesium stearate, and talc.
-
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
QTc interval prolongation was evaluated in a crossover pharmacokinetic study in healthy subjects (N=24) who received single oral doses of QUALAQUIN (324 mg and 648 mg). The mean ± SD maximum QTc change from baseline around the quinine Tmax was 10 ± 19 msec and 12 ± 18 msec, respectively for the 324 mg and 648 mg doses. There were no subjects who had a QTc interval greater than 500 msec, or had a maximum QTc change from baseline of greater than 60 msec [see Warnings and Precautions (5.3)].
12.3 Pharmacokinetics
Absorption
The oral bioavailability of quinine is 76 to 88% in healthy adults. Quinine exposure is higher in patients with malaria than in healthy subjects. After a single oral dose of quinine sulfate, the mean quinine Tmax was longer, and mean AUC and Cmax were higher in patients with uncomplicated P. falciparum malaria than in healthy subjects, as shown in Table 1 below.
TABLE 1 Pharmacokinetic Parameters of Quinine in Healthy Subjects and Patients with Uncomplicated P. falciparum Malaria after a Single Dose* of Oral Quinine Sulfate Capsules Healthy Subjects
(N = 23)
Mean ± SDUncomplicated P. falciparum Malaria Patients
(N = 15)
Mean ± SD- *
- Quinine Sulfate dose was 648 mg (approximately 8.7 mg/kg) in healthy subjects; and 10 mg/kg in patients with malaria
Dose (mg/kg)* 8.7 10 Tmax (h) 2.8 ± 0.8 5.9 ± 4.7 Cmax (mcg/mL) 3.2 ± 0.7 8.4 AUC0–12 (mcg*h/mL) 28.0 73.0 QUALAQUIN capsules may be administered without regard to meals. When a single oral 324 mg capsule of QUALAQUIN was administered to healthy subjects (N=26) with a standardized high-fat breakfast, the mean Tmax of quinine was prolonged to about 4.0 hours, but the mean Cmax and AUC0-24h were similar to those achieved when QUALAQUIN capsule was given under fasted conditions [see Dosage and Administration (2.1)].
Distribution
In patients with malaria, the volume of distribution (Vd/F) decreases in proportion to the severity of the infection. In published studies with healthy subjects who received a single oral 600 mg dose of quinine sulfate, the mean Vd/F ranged from 2.5 to 7.1 L/kg.
Quinine is moderately protein-bound in blood in healthy subjects, ranging from 69 to 92%. During active malarial infection, protein binding of quinine is increased to 78 to 95%, corresponding to the increase in α1-acid glycoprotein that occurs with malaria infection.
Intra-erythrocytic levels of quinine are approximately 30 to 50% of the plasma concentration.
Quinine penetrates relatively poorly into the cerebrospinal fluid (CSF) in patients with cerebral malaria, with CSF concentration approximately 2 to 7% of plasma concentration.
In one study, quinine concentrations in placental cord blood and breast milk were approximately 32% and 31%, respectively, of quinine concentrations in maternal plasma. The estimated total dose of quinine secreted into breast milk was less than 2 to 3 mg per day [see Use in Specific Populations (8.1, 8.3)].
Metabolism
Quinine is metabolized almost exclusively via hepatic oxidative cytochrome P450 (CYP) pathways, resulting in four primary metabolites, 3-hydroxyquinine, 2´-quinone, O-desmethylquinine, and 10,11-dihydroxydihydroquinine. Six secondary metabolites result from further biotransformation of the primary metabolites. The major metabolite, 3-hydroxyquinine, is less active than the parent drug. In vitro studies using human liver microsomes and recombinant P450 enzymes have shown that quinine is metabolized mainly by CYP3A4. Depending on the in vitro experimental conditions, other enzymes, including CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP2E1 were shown to have some role in the metabolism of quinine.
Elimination/Excretion
Quinine is eliminated primarily via hepatic biotransformation. Approximately 20% of quinine is excreted unchanged in urine. Because quinine is reabsorbed when the urine is alkaline, renal excretion of the drug is twice as rapid when the urine is acidic than when it is alkaline.
In various published studies, healthy subjects who received a single oral 600 mg dose of quinine sulfate exhibited a mean plasma clearance ranging from 0.08 to 0.47 L/h/kg (median value: 0.17 L/h/kg) with a mean plasma elimination half-life of 9.7 to 12.5 hours.
In 15 patients with uncomplicated malaria who received a 10 mg/kg oral dose of quinine sulfate, the mean total clearance of quinine was slower (approximately 0.09 L/h/kg) during the acute phase of the infection, and faster (approximately 0.16 L/h/kg) during the recovery or convalescent phase.
Extracorporeal Elimination: Administration of multiple-dose activated charcoal (50 grams administered 4 hours after quinine dosing followed by 3 further doses over the next 12 hours) decreased the mean quinine elimination half-life from 8.2 to 4.6 hours, and increased the mean quinine clearance by 56% (from 11.8 L/h to 18.4 L/h) in 7 healthy adult subjects who received a single oral 600 mg dose of quinine sulfate. Likewise, in 5 symptomatic patients with acute quinine poisoning who received multiple-dose activated charcoal (50 grams every 4 hours), the mean quinine elimination half-life was shortened to 8.1 hours in comparison to a half-life of approximately 26 hours in patients who did not receive activated charcoal [see Overdosage (10)].
In 6 patients with quinine poisoning, forced acid diuresis did not change the half-life of quinine elimination (25.1 ± 4.6 hours vs. 26.5 ± 5.8 hours), or the amount of unchanged quinine recovered in the urine, in comparison to 8 patients not treated in this manner [see Overdosage (10)].
Specific Populations
Pediatric Patients: The pharmacokinetics of quinine in children (1.5 to 12 years old) with uncomplicated P. falciparum malaria appear to be similar to that seen in adults with uncomplicated malaria. Furthermore, as seen in adults, the mean total clearance and the volume of distribution of quinine were reduced in pediatric patients with malaria as compared to the healthy pediatric controls. Table 2 below provides a comparison of the mean ± SD pharmacokinetic parameters of quinine in pediatric patients vs. healthy pediatric controls.
TABLE 2 Quinine Pharmacokinetic Parameters Following the First 10 mg/kg Quinine Sulfate Oral Dose in Healthy Pediatric Controls and Pediatric Patients with Acute Uncomplicated P. falciparum Malaria Healthy Pediatric Controls*
(N = 5)
Mean ± SDP. falciparum Malaria Pediatric Patients1
(N = 15)
Mean ± SD- *
- age 1.5 to 12 years
Tmax (h) 2.0 4.0 Cmax (mcg/mL) 3.4 ± 1.18 7.5 ± 1.1 Half-life (h) 3.2 ± 0.3 12.1 ± 1.4 Total CL (L/h/kg) 0.30 ± 0.04 0.06 ± 0.01 Vd (L/kg) 1.43 ± 0.18 0.87 ± 0.12 Geriatric Patients: Following a single oral dose of 600 mg quinine sulfate, the mean AUC was about 38% higher in 8 healthy elderly subjects (65 to 78 years old) than in 12 younger subjects (20 to 35 years old). The mean Tmax and Cmax were similar in elderly and younger subjects after a single oral dose of quinine sulfate 600 mg. The mean oral clearance of quinine was significantly decreased, and the mean elimination half-life was significantly increased in elderly subjects compared with younger subjects (0.06 vs. 0.08 L/h/kg, and 18.4 hours vs. 10.5 hours, respectively). Although there was no significant difference in the renal clearance of quinine between the two age groups, elderly subjects excreted a larger proportion of the dose in urine as unchanged drug than younger subjects (16.6% vs. 11.2%). Although an alteration in the QUALAQUIN dosage regimen is not needed, elderly patients should be closely monitored for adverse reactions associated with quinine.
Renal Impairment: Following a single oral 600 mg dose of quinine sulfate in otherwise healthy subjects with severe chronic renal failure not receiving any form of dialysis (mean serum creatinine = 9.6 mg/dL), the median AUC was higher by 195% and the median Cmax was higher by 79% than in subjects with normal renal function (mean serum creatinine = 1 mg/dL). The mean plasma half-life in subjects with severe chronic renal impairment was prolonged to 26 hours compared to 9.7 hours in the healthy controls. Computer assisted modeling and simulation indicates that in patients with malaria and severe chronic renal failure, a dosage regimen consisting of one loading dose of 648 mg QUALAQUIN followed 12 hours later by a maintenance dosing regimen of 324 mg every 12 hours will provide adequate systemic exposure to quinine [see Dosage and Administration (2.2)]. The effects of mild and moderate renal impairment on the pharmacokinetics and safety of quinine sulfate are not known.
Negligible to minimal amounts of circulating quinine in the blood are removed by hemodialysis or hemofiltration. In subjects with chronic renal failure (CRF) on hemodialysis, only about 6.5% of quinine is removed in 1 hour. Plasma quinine concentrations do not change during or shortly after hemofiltration in subjects with CRF [see Overdosage (10)].
Hepatic Impairment: In otherwise healthy subjects with moderate hepatic impairment (Child-Pugh B; N=9) who received a single oral 600 mg dose of quinine sulfate, the mean AUC increased by 55% without a significant change in mean Cmax, as compared to healthy volunteer controls (N=6). In subjects with hepatitis, the absorption of quinine was prolonged, the elimination half-life was increased, the apparent volume of distribution was higher, but there was no significant difference in weight-adjusted clearance. Therefore, in patients with mild to moderate hepatic impairment, dosage adjustment is not needed, but patients should be monitored closely for adverse effects of quinine [see Use in Specific Populations (8.7)]. No pharmacokinetic data are available for patients with severe hepatic impairment (Child-Pugh C).
12.4 Microbiology
Mechanism of Action
Quinine inhibits nucleic acid synthesis, protein synthesis, and glycolysis in Plasmodium falciparum and can bind with hemazoin in parasitized erythrocytes. However, the precise mechanism of the antimalarial activity of quinine sulfate is not completely understood.
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Mutagenesis
Genotoxicity studies of quinine were positive in the Ames bacterial mutation assay with metabolic activation and in the sister chromatid exchange assay in mice. The sex-linked recessive lethal test performed in Drosophila, the in vivo mouse micronucleus assay, and the chromosomal aberration assay in mice and Chinese hamsters were negative.
-
14 CLINICAL STUDIES
Quinine has been used worldwide for hundreds of years in the treatment of malaria. Thorough searches of the published literature identified over 1300 references to the treatment of malaria with quinine, and from these, 21 randomized, active-controlled studies were identified which evaluated oral quinine monotherapy or combination therapy for treatment of uncomplicated P. falciparum malaria. Over 2900 patients from malaria-endemic areas were enrolled in these studies, and more than 1400 patients received oral quinine. The following conclusions were drawn from review of these studies:
In areas where multi-drug resistance of P. falciparum is increasing, such as Southeast Asia, cure rates with 7 days of oral quinine monotherapy were at least 80%; while cure rates for 7 days of oral quinine combined with an antimicrobial agent (tetracycline or clindamycin) were greater than 90%. In areas where multi-drug resistance of the parasite was not as widespread, cure rates with 7 days of quinine monotherapy ranged from 86 to 100%. Cure was defined as initial clearing of parasitemia within 7 days without recrudescence by day 28 after treatment initiation. P. falciparum malaria that is clinically resistant to quinine has been reported in some areas of South America, Southeast Asia, and Bangladesh, and quinine may not be as effective in those areas.
Completion of a 7-day oral quinine treatment regimen may be limited by drug intolerance, and shorter courses (3 days) of quinine combination therapy have been used. However, the published data from randomized, controlled clinical trials for shorter regimens of oral quinine in conjunction with tetracycline, doxycycline, or clindamycin for treatment of uncomplicated P. falciparum malaria is limited, and these shorter course combination regimens may not be as effective as the longer regimens.
- 16 HOW SUPPLIED / STORAGE AND HANDLING
-
17 PATIENT COUNSELING INFORMATION
See FDA-approved Medication Guide (17.2)
17.1 Dosing Instructions
Patients should be instructed to:
- Take all of the medication as directed.
- Take no more of the medication than the amount prescribed.
- Take with food to minimize possible gastrointestinal irritation.
If a dose is missed, patients should also be instructed not to double the next dose. If more than 4 hours has elapsed since the missed dose, the patient should wait and take the next dose as previously scheduled.
-
MEDICATION GUIDE
MEDICATION GUIDE
QUALAQUIN®
(kwol-a-kwin)(Quinine Capsules, USP)
Read the Medication Guide that comes with QUALAQUIN® before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment. You and your healthcare provider should talk about QUALAQUIN® when you start taking it and at regular checkups. QUALAQUIN® is not approved for the treatment of night-time leg cramps.
What is the most important information I should know about QUALAQUIN®?
QUALAQUIN® used to treat or prevent leg cramps may cause serious side effects or even death.
- QUALAQUIN® may cause your blood cell (platelet) to drop causing serious bleeding problems. In some cases, kidney injury can also occur.
- QUALAQUIN® may cause problems with the heart rhythm that can lead to death.
- QUALAQUIN® may cause serious allergic reactions.
Call your healthcare provider right away if you have:
- easy bruising
- severe nose bleed
- blood in urine or stool
- bleeding gums
- appearance of unusual purple, brown or red spots on your skin (bleeding under your skin)
- rash
- hives
- severe itching
- sever flushing
- swelling of your face
- trouble breathing
- chest pain
- rapid heartbeat
- irregular heart rhythm
- weakness
- sweating
- nervousness
Taking QUALAQUIN® with some other medicines can increase the chance of serious side effects. Tell your health care provider if you take any other medicines.
Certain medicines can cause the blood levels of QUALAQUIN® to be too high or too low in your body. It is important for you to tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements.
QUALAQUIN® and other medicines may affect each other causing serious side effects or even death. Even medicines that you may take for a short period of time, such as antibiotics, can mix in your blood with QUALAQUIN® and cause serious side effects or death. Do not start taking a new medicine without telling your healthcare provider or pharmacist.
What is QUALAQUIN®?
QUALAQUIN® is a prescription medication used to treat uncomplicated malaria caused by the parasite Plasmodium falciparum.
QUALAQUIN® is NOT approved to:
- Prevent malaria
- Treat severe or complicated malaria
- Prevent or treat night-time leg cramps
It is not known if QUALAQUIN® is safe and works in children younger than 16 years old.
Who should not take QUALAQUIN®?
Do not take QUALAQUIN® if you:
- Have certain heart rhythm problems (Atrial fibrillation) or abnormal electrocardiogram (ECG) (QT prolongation).
- Have low levels of an enzyme called Glucose-6-phosphate dehydrogenase (G6PD).
- Have an autoimmune disease (myasthenia gravis) that leads to muscle weakness.
- Have had allergic reactions to quinine, quinidine, or mefloquine (Lariam®).
- Have had serious side effects to quinine (QUALAQUIN®), such as low platelets, which are necessary for your blood to clot.
- Have an inflammation of the nerve important for vision (optic neuritis).
What should I tell my healthcare provider before starting QUALAQUIN®?
Before you take QUALAQUIN®, tell your doctor or health care provider if you:
- Have heart problems.
- Have kidney problems.
- Have liver problems.
- Have any other medical condition.
- Are pregnant or could be pregnant. Treatment of malaria is important because it can be a serious disease for a pregnant woman and her unborn baby. Your doctor can tell you more about the benefits and risks of taking this medication during pregnancy. Low blood sugar (hypoglycemia) can be seen in pregnant women while taking QUALAQUIN®. This can include sweating, weakness, nausea, vomiting, or confusion. You and your doctor can decide if QUALAQUIN® is right for you.
- Are breast-feeding. Small amounts of QUALAQUIN® can pass into the breast milk. You and your healthcare provider can decide if you should breastfeed while taking QUALAQUIN®.
Tell your healthcare provider about all the medicines you take, including prescription medicines, vitamins and herbal supplements. See "What is the most important information I should know about QUALAQUIN®?
How should I take QUALAQUIN®?
- Take QUALAQUIN® exactly as your healthcare provider tells you to take it.
- You healthcare provider will tell you how many QUALAQUIN® capsules to take and when to take them.
- To lower the chance of stomach upset, take this medication WITH FOOD.
- Finish all the QUALAQUIN® that is prescribed even if you feel better. Do not stop taking the medication without talking to your healthcare provider.
- Do not take more than the amount prescribed. Do not take more than 2 capsules at one time or more than 3 doses in one day. If you take more than the prescribed dose, call your healthcare provider right away. If you forget to take QUALAQUIN®, do NOT double the next dose. If it has been more than 4 hours since the missed dose, just wait and take the regular dose at the next scheduled time. Call your healthcare provider if you are not sure what to do.
- If you take too much QUALAQUIN® call your healthcare provider or go to the nearest emergency room right away.
Call your healthcare provider right away if:
- If you feel worse, or if you do not start feeling better within 1 or 2 days of starting to take QUALAQUIN®.
- If your fever comes back after finishing treatment with QUALAQUIN®.
What are the possible side effects of QUALAQUIN®?
QUALAQUIN® may cause serious side effects.
- See "What is the most important information I should know about QUALAQUIN®" section.
- Low blood sugar (hypoglycemia). This can include sweating, weakness, nausea, vomiting, or confusion. If you experience symptoms of low blood sugar, drink some fruit juice or eat a snack, and call your healthcare provider.
Common side effects with QUALAQUIN® include:
- Headache
- Sweating
- Flushing
- Nausea
- Ringing in your ears
- Hearing loss
- Dizziness (vertigo)
- Blurred vision
- Change in how you see color
Less common side effects with QUALAQUIN® include:
- Vomiting
- Diarrhea
- Stomach pain
- Deafness
- Blindness
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of QUALAQUIN®. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store QUALAQUIN®?
- Keep the capsules in a tightly closed container.
- Do not refrigerate or freeze.
- Store at 20° to 25°C (68º to 77°F).
Keep QUALAQUIN® out of reach of children.
General Information about QUALAQUIN®
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use QUALAQUIN® for a condition for which it was not prescribed. Do not give QUALAQUIN® to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about QUALAQUIN®. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about QUALAQUIN® that is written for healthcare professionals.
For more information, go to www.QUALAQUIN.com or call 1-888-351-3786.
What are the ingredients in QUALAQUIN®?
Active Ingredients: Quinine Sulfate, USP
Inactive Ingredients: Corn starch, magnesium stearate, talc
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured for:
AR SCIENTIFIC, INC.
Philadelphia, PA 19124 USA
by:
MUTUAL PHARMACEUTICAL COMPANY, INC.
Philadelphia, PA 19124 USARev 11, December 2009
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
QUALAQUIN
quinine sulfate capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:16590-595(NDC:13310-153) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength QUININE SULFATE (UNII: KF7Z0E0Q2B) (QUININE - UNII:A7V27PHC7A) QUININE SULFATE 324 mg Product Characteristics Color white (CLEAR) Score no score Shape CAPSULE Size 22mm Flavor Imprint Code AR;102 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:16590-595-30 30 in 1 BOTTLE 2 NDC:16590-595-60 60 in 1 BOTTLE 3 NDC:16590-595-90 90 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021799 08/12/2005 Labeler - STAT RX USA LLC (786036330) Establishment Name Address ID/FEI Business Operations STAT RX USA LLC 786036330 repack, relabel

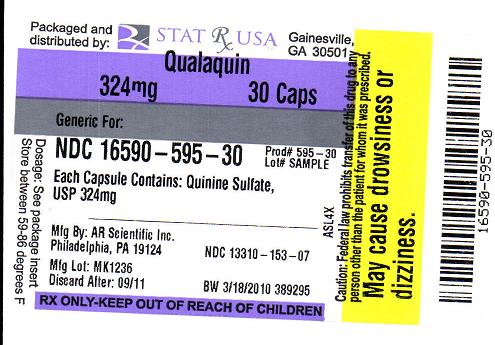
 QUALAQUIN 324MG LABEL IMAGE
QUALAQUIN 324MG LABEL IMAGE