GELNIQUE- oxybutynin gel
Actavis Pharma, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use GELNIQUE 3% safely and effectively. See full prescribing information for GELNIQUE 3%.
GELNIQUE 3% (oxybutynin) gel 3%, for topical use Initial U.S. Approval: 1975 RECENT MAJOR CHANGESWarnings and Precautions, Central Nervous System Effects (5.5) 07/2015 INDICATIONS AND USAGEGELNIQUE 3% is a muscarinic receptor antagonist indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency. (1) DOSAGE AND ADMINISTRATIONDOSAGE FORMS AND STRENGTHSGel; 3% (3) CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (≥ 3%) are dry mouth, and application site reactions. (6.1)
DRUG INTERACTIONS
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 7/2015 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
GELNIQUE 3% (oxybutynin) gel 3% is a muscarinic receptor antagonist indicated for the treatment of overactive bladder with symptoms of urge urinary incontinence, urgency, and frequency [see Clinical Studies (14)].
2 DOSAGE AND ADMINISTRATION
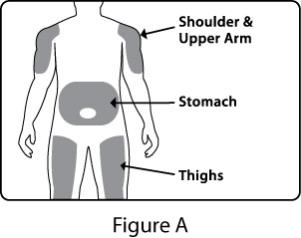
The recommended dosage is three pumps of GELNIQUE 3% (84 mg/day) applied once daily to clean, dry, intact skin on the abdomen, or upper arms/shoulders, or thighs. Apply immediately after actuating the dose. Application sites may be rotated to reduce the potential for local site reactions [see Adverse Reactions (6.1)]. GELNIQUE 3% is for topical application only and should not be ingested.
Wash hands immediately after product application. Patients should cover the application site with clothing after the gel has dried if direct skin-to-skin contact at the application site is anticipated [see Warnings and Precautions (5.3)].
4 CONTRAINDICATIONS
The use of GELNIQUE 3% is contraindicated in patients with the following conditions:
- Urinary retention [see Warnings and Precautions (5.1)].
- Gastric retention [see Warnings and Precautions (5.2)].
- Uncontrolled narrow-angle glaucoma [see Warnings and Precautions (5.8)].
5 WARNINGS AND PRECAUTIONS
5.1 Urinary Retention
Use GELNIQUE 3% with caution in patients with clinically significant bladder outflow obstruction because of the risk of urinary retention.
5.2 Use in Patients with Gastrointestinal Disorders
Use GELNIQUE 3% with caution in patients with gastrointestinal obstructive disorders because of the risk of gastric retention.
GELNIQUE 3%, like other anticholinergic drugs, may decrease gastrointestinal motility and should be used with caution in patients with conditions such as ulcerative colitis or intestinal atony.
GELNIQUE 3% should be used with caution in patients who have gastroesophageal reflux and/or who are concurrently taking drugs (such as bisphosphonates) that can cause or exacerbate esophagitis.
5.3 Skin Transference
Transfer of oxybutynin to another person can occur when vigorous bare skin-to-skin contact is made with the application site. To minimize the potential transfer of oxybutynin from treated skin to another person, patients should cover the application site with clothing after the gel has dried if direct skin-to-skin contact at the application site is anticipated [see Clinical Pharmacology (12.3)]. Patients should wash their hands immediately after application of GELNIQUE 3%.
5.4 Flammable Gel
GELNIQUE 3% is an alcohol-based gel and is therefore flammable. Avoid open fire or smoking until gel has dried.
5.5 Central Nervous System Effects
Drugs containing oxybutynin are associated with anticholinergic central nervous system (CNS) effects. A variety of CNS anticholinergic effects have been reported, including headache, dizziness, somnolence, confusion and hallucinations . Patients should be monitored for signs of anticholinergic CNS effects, particularly after beginning treatment. Advise patients not to drive or operate heavy machinery until they know how GELNIQUE 3% affects them. If a patient experiences anticholinergic CNS effects, drug discontinuation should be considered.
5.6 Myasthenia Gravis
Administer GELNIQUE 3% with caution in patients with myasthenia gravis, a disease characterized by decreased cholinergic activity at the neuromuscular junction.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trial of another drug and may not reflect the rates observed in practice.
The safety of GELNIQUE 3% was evaluated in 626 patients (210 randomized to GELNIQUE 3% 56 mg/day, 214 randomized to GELNIQUE 3% 84 mg/day and 202 randomized to placebo) during a randomized, placebo-controlled, double-blind, 12-week clinical efficacy and safety study. A subset of these 626 patients (N = 77) participated in the 24-week open-label safety extension that followed the placebo-controlled study. Of the 77 patients in the safety extension, 24 were randomized to placebo gel during the double-blind, placebo-controlled 12-week study. In the combined double-blind, placebo-controlled study and the open-label safety extension, a total of 441 patients were exposed to at least one dose of GELNIQUE 3%. 364 patients received at least 12 weeks of GELNIQUE 3% treatment and 66 patients received an additional 24 weeks of GELNIQUE 3% treatment during the open-label safety extension. The study population primarily consisted of women (87%) of Caucasian descent (87%) with an average age of 59 years who had overactive bladder with urge urinary incontinence.
Table 1 lists adverse reactions (ARs), regardless of causality, that were reported in the randomized, double-blind, placebo-controlled 12-week study at an incidence greater than placebo and in greater than 3% of patients treated with GELNIQUE 3%.
Overall, 672 ARs were experienced by 51.9% of patients. Majority of the ARs were mild to moderate in intensity. The AR most commonly reported was dry mouth which was experienced by a greater proportion of patients in the oxybutynin group than the placebo group (26 patients [12.1%] in the oxybutynin 84 mg group, 10 patients [5.0%] in the placebo group). Application site erythema was the next most commonly reported AR (8 patients [3.7%] in the oxybutynin 84 mg group and 2 patients [1.0%] in the placebo group). Other commonly reported ARs experienced by more patients in the oxybutynin groups compared with placebo were application site rash (7 patients [3.3%] in the oxybutynin 84 mg group and 1 patient [0.5%] in the placebo group); application site pruritus (6 patients [2.8%] in the oxybutynin 84 mg group and 1 patient [0.5%] in the placebo group). The overall rate of application site adverse reactions of any kind was 14.2% in patients receiving GELNIQUE 3% as compared to 3.7% in patients receiving placebo. Other cholinergic AEs < 2% in occurrence include dry eyes and blurred vision.
There were no deaths during the study. There were no clinically meaningful changes in vital signs, laboratory values, or ECG examinations over the course of the study.
| Treatment Group | ||
| Preferred Term* | Oxybutynin
84 mg/day (N = 214) | Placebo
(N = 202) |
| n (%) | n (%) | |
| Dry mouth | 26 (12.1) | 10 (5.0) |
| Application site erythema | 8 (3.7) | 2 (1.0) |
| Application site rash | 7 (3.3) | 1 (0.5) |
* Each patient is counted only once within each treatment, body system and preferred term. All percentages are based on number of patients in the ITT population within each treatment group as denominator.
During the 24-week open-label safety extension, the most commonly reported ARs were urinary tract infection and nasopharyngitis reported in 4 patients each (5.2%), followed by conjunctivitis and application site erythema (both occurred in 3 patients [3.9%]). One patient prematurely discontinued due to the application site erythema and pruritus (both considered to be of mild severity).
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of GELNIQUE. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Nervous System Disorders: dizziness, somnolence, confusion
Psychiatric Disorders: hallucinations
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B.
There are no adequate and well-controlled studies of topical or oral oxybutynin use in pregnant women. Reproduction studies using oxybutynin chloride in the hamster, rabbit, rat, and mouse have shown no evidence of impaired fertility or harm to the fetus. The safety of GELNIQUE 3% administration to women who are or who may become pregnant has not been established. Therefore, GELNIQUE 3% should not be given to pregnant women unless, in the judgment of the physician, the probable clinical benefits outweigh the possible hazards.
8.2 Labor and Delivery
GELNIQUE 3% has not been studied for use during labor and delivery. Treatment should only be given if clearly needed.
8.3 Nursing Mothers
It is not known whether oxybutynin is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when GELNIQUE 3% is administered to a nursing woman.
8.4 Pediatric Use
The safety and effectiveness of GELNIQUE 3% have not been established in pediatric patients.
8.5 Geriatric Use
Of the 424 patients exposed to GELNIQUE 3% in the randomized, double-blind, placebo-controlled 12-week study, 182 patients (34%) were 65 years of age and older. No overall differences in safety or effectiveness were observed between these patients and younger patients.
10 OVERDOSAGE
Overdosage with oxybutynin has been associated with anticholinergic effects including central nervous system excitation, flushing, fever, dehydration, cardiac arrhythmia, vomiting, exhaustion, heat sensitivity, and urinary retention. Oral ingestion of 100 mg oxybutynin chloride in association with alcohol has been reported in a 13-year-old who experienced memory loss, and in a 34-year-old who developed stupor, followed by disorientation and agitation on awakening, dilated pupils, dry skin, cardiac arrhythmia, and retention of urine. Both patients recovered fully with symptomatic treatment. If overexposure occurs, monitor patients until symptoms resolve.
11 DESCRIPTION
Oxybutynin is an antispasmodic, antimuscarinic agent. GELNIQUE 3% is a topical, homogeneous, very lightly to moderately opalescent, translucent colorless to slightly colored gel, without particles. The product is a hydroalcoholic gel containing 30 mg oxybutynin per gram of gel. GELNIQUE 3% is available in a 0.92 gram (1 mL) unit dose that contains 28 mg oxybutynin. Oxybutynin is delivered as a racemate of R- and S-isomers. Chemically, oxybutynin base is d, l (racemic) 4-(Diethylamino)-2-butynyl (±)-α-phenylcyclohexaneglycolate.
The empirical formula of oxybutynin base is C22H31NO3. Its structural formula is:
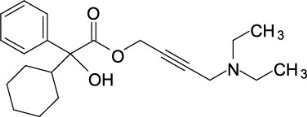
Oxybutynin is a white powder with a molecular weight of 357.
Inactive ingredients in GELNIQUE 3% are diethylene glycol monoethyl ether, NF; alcohol, USP; hydroxypropyl cellulose, NF; propylene glycol, NF; butylated hydroxytoluene, NF; HCl 0.1 M, NF; and purified water, USP.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Oxybutynin is a racemic (50:50) mixture of R- and S- isomers. Antimuscarinic activity resides predominantly with the R-isomer.
Oxybutynin acts as a competitive antagonist of acetylcholine at postganglionic muscarinic receptors, resulting in relaxation of bladder smooth muscle. The active metabolite, N-desethyloxybutynin, has pharmacological activity on the human detrusor muscle that is similar to that of oxybutynin in in vitro studies. In patients with conditions characterized by involuntary detrusor contractions, cystometric studies have demonstrated that oxybutynin increases maximum urinary bladder capacity and increases the volume to first detrusor contraction.
12.3 Pharmacokinetics
Oxybutynin is transported across intact skin and into the systemic circulation by passive diffusion across the stratum corneum. Steady-state concentrations are achieved within 3 days of continuous dosing.
Absorption
Absorption of oxybutynin is similar when GELNIQUE 3% is applied to the abdomen, upper arm/shoulders or thighs. The pharmacokinetic parameters and mean plasma concentrations during a randomized, crossover study of the three recommended application sites in 25 healthy men and women are shown in Table 2 and Figure 1, respectively.
| Application Site | AUC0-t
(ng·h/mL) | Cmax (ng/mL) | T max (h) |
| Abdomen | 284.1 | 6.3 | 24 |
| Thigh | 286.9 | 5.8 | 36 |
| Upper Arm/Shoulder | 329.1 | 8.8 | 24 |
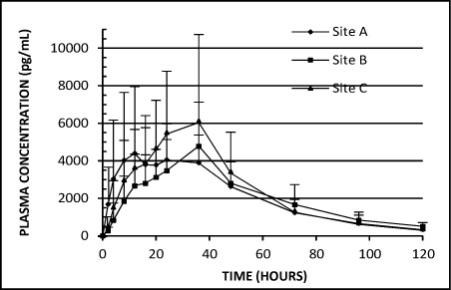
Figure 1: Mean (including SD) plasma oxybutynin concentrations versus time after application of GELNIQUE 3% to the abdomen (Site A), thigh (Site B), and upper arm/shoulder (Site C) (N = 25).
Distribution
Oxybutynin is widely distributed in body tissues following systemic absorption. The volume of distribution was estimated to be 193 L after intravenous administration of 5 mg oxybutynin chloride.
Metabolism
Oxybutynin is metabolized primarily by the cytochrome P450 enzyme systems, particularly CYP3A4, found mostly in the liver and gut wall. Metabolites include N-desethyloxybutynin (DEO), which is pharmacologically active and phenylcyclohexylglycolic acid, which is pharmacologically inactive.
Transdermal administration of oxybutynin bypasses the first-pass gastrointestinal and hepatic metabolism, reducing the formation of the N-desethyloxybutynin metabolite. Only small amounts of CYP3A4 are found in skin, limiting pre-systemic metabolism during transdermal absorption. The AUC ratio of N-desethyloxybutynin metabolite to parent compound following multiple transdermal applications is approximately 1:1 for GELNIQUE 3%. The apparent half-life was approximately 30 hours.
Excretion
Oxybutynin undergoes extensive hepatic metabolism, with less than 0.1% of the administered dose excreted unchanged in the urine. Less than 0.1% of the administered dose is excreted as the metabolite N-desethyloxybutynin.
Person-to-Person Transference
The potential for dermal transfer of oxybutynin from a treated person to an untreated person was evaluated in a single-dose study where subjects dosed with GELNIQUE 3% engaged in vigorous contact with an untreated partner for 15 minutes, either with (N = 14 couples) or without (N = 14 couples) clothing covering the application area. The untreated partners not protected by clothing demonstrated low detectable plasma concentrations of oxybutynin (mean Cmax = 0.65 ng/mL). Only one of the 14 untreated subjects participating in the clothing-to-skin contact regimen had very low measurable oxybutynin plasma concentrations (Cmax = 0.06 ng/mL) during the 24 hours following contact with treated subjects; oxybutynin was not detectable with the remaining 13 untreated subjects. Regardless of the low exposure observed in this study, patients should avoid skin-to-skin contact with partners after applying the gel.
Use of Sunscreen
The effect of sunscreen on the absorption of oxybutynin when applied 30 minutes before or 30 minutes after GELNIQUE 3% application was evaluated in a single-dose randomized crossover study (N = 20). Concomitant application of sunscreen, either before or after GELNIQUE 3% application, had no effect on the systemic exposure of oxybutynin.
Showering
The effect of showering on the absorption of oxybutynin was evaluated in a randomized, steady-state crossover study under conditions of no shower, or showering 1, 2 or 6 hours after GELNIQUE 3% application (N = 22). The results of the study indicate that showering one hour after administration does not affect the overall systemic exposure to oxybutynin.
Race
The effect of race on the pharmacokinetics of GELNIQUE 3% has not been studied.
Geriatric Patients
Available data suggest that there are no significant differences in the pharmacokinetics of oxybutynin based on geriatric status in patients following administration of GELNIQUE 3% [see Use in Specific Populations (8.5)].
Pediatric Patients
The pharmacokinetics of oxybutynin and N-desethyloxybutynin following application of GELNIQUE 3% has not been evaluated in individuals younger than 18 years of age [see Use in Specific Populations (8.4)].
Gender
Available data suggest that there are no significant differences in the pharmacokinetics of oxybutynin based on gender in healthy volunteers following administration of GELNIQUE 3%.
Renal Impairment
There is limited experience with the use of GELNIQUE 3% in patients with renal insufficiency [see Use in Specific Populations (8.6)].
Hepatic Impairment
There is limited experience with the use of GELNIQUE 3% in patients with hepatic insufficiency [see Use in Specific Populations (8.7)].
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A 24-month study in rats at dosages of oxybutynin chloride of 20, 80, and 160 mg/kg showed no evidence of carcinogenicity. These doses are approximately 6, 25, and 50 times the maximum exposure in humans taking an oral dose, based on body surface area. Oxybutynin chloride showed no increase of mutagenic activity when tested in Schizosaccharomyces pompholiciformis, Saccharomyces cerevisiae, and Salmonella typhimurium test systems. Reproduction studies with oxybutynin chloride in the mouse, rat, hamster, and rabbit showed no evidence of impaired fertility.
14 CLINICAL STUDIES
The efficacy and safety of GELNIQUE 3% were evaluated in a single randomized, double-blind, placebo-controlled, multicenter 12-week study in patients with urinary frequency and urge and mixed urinary incontinence with a predominance of urge incontinence episodes. This was followed by an open-label safety extension. Key entry criteria included adults with overactive bladder (OAB) symptoms for at least 3 months who were either treatment-naïve or had demonstrated a beneficial response to anticholinergic treatment for OAB. Subjects were randomly assigned to receive 84 mg/day oxybutynin, 56 mg/day oxybutynin, or placebo. A total of 214 patients received 84 mg/day oxybutynin, 210 patients received 56 mg/day oxybutynin, and 202 patients received placebo gel. The majority of patients were Caucasian (87%) and female (87%), with a mean age of 59 years (range: 19 to 89 years). The primary efficacy endpoint was the change from baseline to week 12 in the number of urinary incontinence episodes (UIE) per week, as determined from a 3‑day patient daily diary.
Patients treated with GELNIQUE 3% (84 mg) experienced a statistically significant decrease in the number of urinary incontinence episodes per week from baseline to endpoint (the primary efficacy endpoint) compared with placebo (p = 0.0445) and patients treated with the 56 mg dose did not show statistically significant efficacy. Statistically significant improvements in daily urinary frequency (p = 0.0010) and urinary void volume (p < 0.0001) were also seen with GELNIQUE 3% (84 mg) relative to placebo. The mean difference from placebo for GELNIQUE 3% (84 mg) was -2.3 for urinary incontinence episodes per week in a group of patients with a mean of greater than 40 incontinence episodes per week at baseline. Mean and median change from baseline in weekly incontinence episodes (primary endpoint), daily urinary frequency, and urinary void volume (secondary endpoints) between placebo and GELNIQUE 3% are summarized in Table 3.
| Parameter | Placebo
(N = 202) | GELNIQUE 3% (84 mg/day)
(N = 214) |
||
| Mean (SD) | Median | Mean (SD) | Median | |
| Weekly Urinary Incontinence Episodes | ||||
| Baseline | 45.8 (31.87) | 40.9 | 43.6 (27.90) | 37.3 |
| Reduction | -18.1 (28.81) | -14.0 | -20.4 (24.39) | -16.4 |
| Mean difference [GELNIQUE 3% – placebo] (SE) | -2.3 (2.65) | |||
| P-value† vs. placebo | 0.0445‡ | |||
| Daily Urinary Frequency | ||||
| Baseline | 11.5 (3.34) | 11.0 | 11.3 (2.87) | 10.7 |
| Reduction | -1.9 (3.34) | - 1.7 | - 2.6 (2.66) | - 2.3 |
| Mean difference [GELNIQUE 3% - placebo] (SE) | - 0.7 (0.30) | |||
| P-value† vs. placebo | 0.0010§ | |||
| Urinary Void Volume (mL) | ||||
| Baseline | 184.5 (85.71) | 173.4 | 196.9 (88.11) | 189.2 |
| Increase | 9.8 (64.98) | 5.7 | 32.7 (77.25) | 26.6 |
| Mean difference [GELNIQUE 3% – placebo] (SE) | 23.0 (7.24) | |||
| P-value† vs. placebo | < 0.0001§ | |||
¶ Last-Observation-Carried-Forward imputation for missing data
† P-value is based on ANCOVA analysis on rank-transformed data
‡ Comparison is significant if p ≤ 0.05
§ Comparison is significant if p ≤ 0.0125, adjusting for multiplicity
16 HOW SUPPLIED/STORAGE AND HANDLING
GELNIQUE 3% (oxybutynin) gel 3% is supplied in a metered-dose pump dispenser composed of an inner aluminum laminated foil liner encased in a rigid plastic bottle with a plastic cap. The nozzle of the pump dispenser is sealed by a removable cap attached to the actuator by a plastic string.
How Supplied
NDC 52544-041-54 100 mL (92 g) metered pump dispenser containing 90 metered 0.92 g (1 mL) pumps delivering 28 mg oxybutynin per pump actuation.
Storage
Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F). See USP controlled room temperature. Protect from moisture and humidity.
17 PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Patient Information)
Instructions for Use
Inform patients of the following:
- GELNIQUE 3% is for topical application only and should not be ingested. Keep out of reach of children.
- GELNIQUE 3% should be applied once daily to clean, dry, intact skin on the abdomen, or upper arms/shoulders, or thighs.
- Do not use any GELNIQUE 3% that came out while priming.
- Apply immediately after actuating the dose.
- Application sites may be rotated to reduce the potential for local site reactions.
- GELNIQUE 3% should not be applied to recently shaved skin surfaces. Avoid skin with open sores, wounds, irritation, scars, and tattoos.
- Do not apply the gel to the breasts or genital area.
- Discard used pump dispensers in household trash in a manner that prevents accidental application or ingestion by children, pets, or others.
- Wash hands immediately after product application.
- Do not shower or immerse the application site in water for 1 hour after product application.
- Cover the application sites with clothing if skin-to-skin contact at the application site is anticipated.
- Alcohol based gels are flammable. Avoid open fire or smoking until the gel has dried.
- If you get the gel in your eyes, thoroughly rinse your eyes right away with warm, clean water to flush out any gel. Seek medical attention if needed.
Important Anticholinergic Adverse Reactions
Patients should be informed that anticholinergic (antimuscarinic) agents, such as GELNIQUE 3%, may produce clinically significant adverse reactions related to anticholinergic pharmacological activity. Heat prostration (due to decreased sweating) can occur when anticholinergics such as GELNIQUE 3% are used in a hot environment. Because anticholinergic (antimuscarinic) agents, such as GELNIQUE 3%, may produce dizziness or blurred vision, patients should be advised to exercise caution in decisions to engage in potentially dangerous activities until this product's effects have been determined. Patients should be informed that alcohol may enhance the drowsiness caused by anticholinergic (antimuscarinic) agents such as GELNIQUE 3%.
For all medical inquiries contact:
ACTAVIS
Medical Communications
Parsippany, NJ 07054
1-800-272-5525
Distributed By:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USA
Content Updated: July 2015
FDA-approved patient labeling
Patient Information
GELNIQUE [Gel-nēk] 3%
(oxybutynin) gel 3%
Topical
Important: For use on the skin only (topical). Do not get GELNIQUE 3% in or near your eyes, nose, or mouth.
Read this Patient Information carefully before you use GELNIQUE 3% and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment.
What is GELNIQUE 3%?
GELNIQUE 3% is a prescription medicine used to treat the symptoms of overactive bladder including:
- a strong need to urinate with leaking or wetting accidents (urge urinary incontinence)
- a strong need to urinate right away (urgency)
- urinating often (frequency)
It is not known if GELNIQUE 3% is safe or effective in children.
Who should not use GELNIQUE 3%?
Do not use GELNIQUE 3% if:
- Your bladder does not empty or does not empty completely when you urinate (urinary retention).
- Your stomach empties slowly or incompletely after a meal (gastric retention).
- You have high pressure in your eye (uncontrolled narrow-angle glaucoma).
- You have an allergy to oxybutynin or any of the ingredients in GELNIQUE 3%. See the end of this leaflet for a complete list of ingredients in GELNIQUE 3%.
Talk to your healthcare provider before taking this medicine if you have any of these conditions.
What should I tell my doctor before using GELNIQUE 3%?
Before you use GELNIQUE 3%, tell your doctor if you:
- have problems emptying your bladder completely
- have stomach problems including:
• constipation or difficulty in emptying your bowels
• inflamed bowels (ulcerative colitis)
• inflammation of the tube between your mouth and stomach (gastric reflux disease or esophagitis)
- have generalized muscle weakness (myasthenia gravis)
- are pregnant or are planning to become pregnant. It is not known if GELNIQUE 3% will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if GELNIQUE 3% passes into your breast milk. Talk to your doctor about the best way to feed your baby if you use GELNIQUE 3%.
Tell your doctor about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements.
GELNIQUE 3% may affect the way other medicines work, and other medicines may affect how GELNIQUE 3% works.
Especially tell your doctor if you take:
- medicines used to treat osteoporosis (Bisphosphonates)
- other medicines used to treat overactive bladder (Anticholinergic)
Ask your doctor if you are not sure if your medicine is one listed above.
Know the medicines you take. Keep a list of them to show your doctor or pharmacist when you get a new medicine.
How should I use GELNIQUE 3%?
GELNIQUE 3% is for skin use only.
- Use GELNIQUE 3% exactly as your doctor tells you to use it.
- GELNIQUE 3% should only be applied to dry intact skin on your stomach (abdomen), upper arms, or thighs.
- Do not put GELNIQUE 3% on recently shaved skin, open sores, scars, tattoos, or skin with rashes.
- Do not put GELNIQUE 3% on your breasts or genital area.
-
GELNIQUE 3% contains alcohol and is flammable. Avoid fire, flames, or smoking until the product has dried.
- Cover the application site with clothing after the gel has dried, if skin-to-skin contact between another person and the application site is expected.
- After applying GELNIQUE 3%, wash your hands with soap and water right away.
- GELNIQUE 3% may be used with sunscreen.
- If you get GELNIQUE 3% in your eyes: Rinse your eyes well right away with clean and warm water. Seek medical attention if needed.
How to use the GELNIQUE 3% pump:
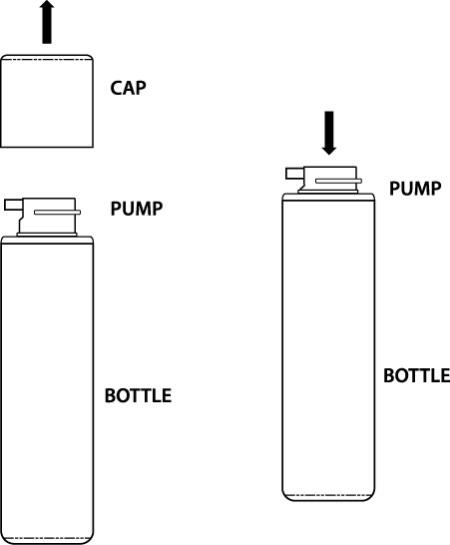
You must prime the pump before you use it for the first time.
To prime the pump:
- To prime the GELNIQUE 3% pump, hold the pump upright and fully press down (depress) the pump 4 times. Now GELNIQUE 3% is ready to use.
- Do not use any product that came out while priming.
Applying GELNIQUE 3%:
1. Selecting your application site:
Apply GELNIQUE 3% only to 1 of the shaded areas shown in the figure below: (See Figure A).
- stomach area (abdomen)
- upper arms
- shoulders
- thighs
- Wash the area where GELNIQUE 3% will be applied with mild soap and water. Allow the area to dry completely.
- Wash your hands with soap and water.
- Application sites may be rotated to reduce the potential for local site reactions.
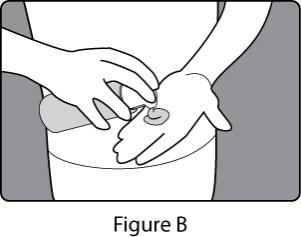
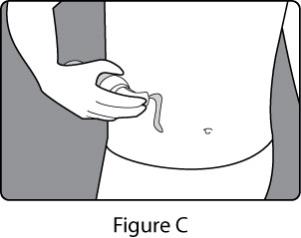
2. Dispensing your dose of GELNIQUE 3%:
-
Place your hand under the pump. Press the pump all the way down 3 times (See Figure B). You can also place the pump right over the application site then press the pump all the way down 3 times to dispense your dose (See Figure C).
- You should apply GELNIQUE 3% right after you dispense your dose.
- Wash your hands with soap and water right away.
What should I avoid while using GELNIQUE 3%?
- Do not take a bath, swim, shower, exercise, or get the application site wet for 1 hour after you apply your dose.
- GELNIQUE 3% can cause dizziness or blurred vision. Do not drive, operate heavy machinery, or do other dangerous activities until you know how GELNIQUE 3% affects you.
- You should not drink alcohol while using GELNIQUE 3%. It can increase your chances of getting serious side effects.
What are the possible side effects of GELNIQUE 3%?
The most common side effects of GELNIQUE 3% include:
- dry mouth
- urinary tract infections
- dry eyes
- blurry vision
- redness, rash, itching, pain at the application site
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of GELNIQUE 3%. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
How should I store GELNIQUE 3%?
- Store GELNIQUE 3% at room temperature between 68ºF to 77ºF (20ºC to 25ºC).
Keep GELNIQUE 3% and all medicines out of the reach of children.
General information about the safe and effective use of GELNIQUE 3%.
Medicines are sometimes prescribed for conditions that are not mentioned in the patient information leaflet. Do not use GELNIQUE 3% for a condition for which it was not prescribed. Do not give GELNIQUE 3% to other people, even if they have the same symptoms you have. It may harm them.
This Patient Information leaflet summarizes the most important information about GELNIQUE 3%. If you would like more information about GELNIQUE 3%, talk with your doctor. You can ask your pharmacist or doctor for information about GELNIQUE 3% that is written for health professionals.
For more information go to www.gelnique.com or call 1-800-272-5525.
What are the ingredients in GELNIQUE 3%?
Active ingredient: oxybutynin
Inactive ingredients: diethylene glycol monoethyl ether, NF; alcohol, USP; hydroxypropyl cellulose, NF; propylene glycol, NF; butylated hydroxytoluene, NF; HCl 0.1 M, NF; and purified water, USP.
This Patient Information has been approved by the U.S. Food and Drug Administration.
For all medical inquiries contact:
ACTAVIS
Medical Communications
Parsippany, NJ 07054
1-800-272-5525
Distributed By:
Actavis Pharma, Inc.
Parsippany, NJ 07054 USA
Content Updated: January 2013
219404-01
| GELNIQUE
oxybutynin gel |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Actavis Pharma, Inc. (119723554) |