Label: CLARINEX- desloratadine tablet, film coated
-
Contains inactivated NDC Code(s)
NDC Code(s): 21695-815-10 - Packager: Rebel Distributors Corp
- This is a repackaged label.
- Source NDC Code(s): 0085-1264
- Category: HUMAN PRESCRIPTION DRUG LABEL
Drug Label Information
Updated September 23, 2010
If you are a healthcare professional or from the pharmaceutical industry please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
CLARINEX (desloratadine) Tablets are light blue, round, film coated tablets containing 5 mg desloratadine, an antihistamine, to be administered orally. It also contains the following excipients: dibasic calcium phosphate dihydrate USP, microcrystalline cellulose NF, corn starch NF, talc USP, carnauba wax NF, white wax NF, coating material consisting of lactose monohydrate, hypromellose, titanium dioxide, polyethylene glycol, and FD&C Blue #2 Aluminum Lake.
CLARINEX Syrup is a clear orange colored liquid containing 0.5 mg/1 mL desloratadine. The syrup contains the following inactive ingredients: propylene glycol USP, sorbitol solution USP, citric acid (anhydrous) USP, sodium citrate dihydrate USP, sodium benzoate NF, disodium edetate USP, purified water USP. It also contains granulated sugar, natural and artificial flavor for bubble gum and FDC Yellow #6 dye.
The CLARINEX RediTabs® brand of desloratadine orally-disintegrating tablets are light red, flat-faced, round, speckled tablets with an "A" debossed on one side for the 5 mg tablets and a "K" debossed on one side for the 2.5 mg tablets. Each RediTabs Tablet contains either 5 mg or 2.5 mg of desloratadine. It also contains the following inactive ingredients: mannitol USP, microcrystalline cellulose NF, pregelatinized starch, NF, sodium starch glycolate, NF, magnesium stearate NF, butylated methacrylate copolymer, crospovidone, NF, aspartame NF, citric acid USP, sodium bicarbonate USP, colloidal silicon dioxide, NF, ferric oxide red NF and tutti frutti flavoring.
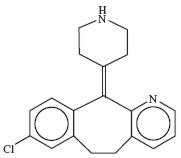
Desloratadine is a white to off-white powder that is slightly soluble in water, but very soluble in ethanol and propylene glycol. It has an empirical formula: C19H19ClN2 and a molecular weight of 310.8. The chemical name is 8-chloro-6,11-dihydro-11-(4-piperdinylidene)-5H-benzo[5,6]cyclohepta[1,2-b]pyridine and has the following structure:
-
CLINICAL PHARMACOLOGY
Mechanism of Action
Desloratadine is a long-acting tricyclic histamine antagonist with selective H1-receptor histamine antagonist activity. Receptor binding data indicate that at a concentration of 2–3 ng/mL (7 nanomolar), desloratadine shows significant interaction with the human histamine H1-receptor. Desloratadine inhibited histamine release from human mast cells in vitro.
Results of a radiolabeled tissue distribution study in rats and a radioligand H1-receptor binding study in guinea pigs showed that desloratadine did not readily cross the blood brain barrier.
Pharmacokinetics
Absorption
Following oral administration of desloratadine 5 mg once daily for 10 days to normal healthy volunteers, the mean time to maximum plasma concentrations (Tmax) occurred at approximately 3 hours post dose and mean steady state peak plasma concentrations (Cmax) and area under the concentration-time curve (AUC) of 4 ng/mL and 56.9 ng∙hr/mL were observed, respectively. Neither food nor grapefruit juice had an effect on the bioavailability (Cmax and AUC) of desloratadine.
The pharmacokinetic profile of CLARINEX Syrup was evaluated in a three-way crossover study in 30 adult volunteers. A single dose of 10 mL of CLARINEX Syrup containing 5 mg of desloratadine was bioequivalent to a single dose of 5 mg CLARINEX Tablet. Food had no effect on the bioavailability (AUC and Cmax) of CLARINEX Syrup.
The pharmacokinetic profile of CLARINEX RediTabs Tablets was evaluated in a three-way crossover study in 24 adult volunteers. A single CLARINEX RediTabs Tablet containing 5 mg of desloratadine was bioequivalent to a single 5 mg CLARINEX RediTabs Tablet (original formulation) for both desloratadine and 3-hydroxydesloratadine. Water had no effect on the bioavailability (AUC and Cmax) of CLARINEX RediTabs Tablets.
Distribution
Desloratadine and 3-hydroxydesloratadine are approximately 82% to 87% and 85% to 89%, bound to plasma proteins, respectively. Protein binding of desloratadine and 3-hydroxydesloratadine was unaltered in subjects with impaired renal function.
Metabolism
Desloratadine (a major metabolite of loratadine) is extensively metabolized to 3-hydroxydesloratadine, an active metabolite, which is subsequently glucuronidated. The enzyme(s) responsible for the formation of 3-hydroxydesloratadine have not been identified. Data from clinical trials indicate that a subset of the general population has a decreased ability to form 3-hydroxydesloratadine, and are poor metabolizers of desloratadine. In pharmacokinetic studies (n=3748), approximately 6% of subjects were poor metabolizers of desloratadine (defined as a subject with an AUC ratio of 3-hydroxydesloratadine to desloratadine less than 0.1, or a subject with a desloratadine half-life exceeding 50 hours). These pharmacokinetic studies included subjects between the ages of 2 and 70 years, including 977 subjects aged 2–5 years, 1575 subjects aged 6–11 years, and 1196 subjects aged 12–70 years. There was no difference in the prevalence of poor metabolizers across age groups. The frequency of poor metabolizers was higher in Blacks (17%, n=988) as compared to Caucasians (2%, n=1462) and Hispanics (2%, n=1063). The median exposure (AUC) to desloratadine in the poor metabolizers was approximately 6-fold greater than in the subjects who are not poor metabolizers. Subjects who are poor metabolizers of desloratadine cannot be prospectively identified and will be exposed to higher levels of desloratadine following dosing with the recommended dose of desloratadine. In multidose clinical safety studies, where metabolizer status was identified, a total of 94 poor metabolizers and 123 normal metabolizers were enrolled and treated with CLARINEX Syrup for 15–35 days. In these studies, no overall differences in safety were observed between poor metabolizers and normal metabolizers. Although not seen in these studies, an increased risk of exposure-related adverse events in patients who are poor metabolizers cannot be ruled out.
Elimination
The mean elimination half-life of desloratadine was 27 hours. Cmax and AUC values increased in a dose proportional manner following single oral doses between 5 and 20 mg. The degree of accumulation after 14 days of dosing was consistent with the half-life and dosing frequency. A human mass balance study documented a recovery of approximately 87% of the 14C-desloratadine dose, which was equally distributed in urine and feces as metabolic products. Analysis of plasma 3-hydroxydesloratadine showed similar Tmax and half-life values compared to desloratadine.
Special Populations
Geriatric
In older subjects (≥ 65 years old; n=17) following multiple-dose administration of CLARINEX Tablets, the mean Cmax and AUC values for desloratadine were 20% greater than in younger subjects (< 65 years old). The oral total body clearance (CL/F) when normalized for body weight was similar between the two age groups. The mean plasma elimination half-life of desloratadine was 33.7 hr in subjects ≥ 65 years old. The pharmacokinetics for 3-hydroxydesloratadine appeared unchanged in older versus younger subjects. These age-related differences are unlikely to be clinically relevant and no dosage adjustment is recommended in elderly subjects.
Pediatric Subjects
In subjects 6 to 11 years old, a single dose of 5 mL of CLARINEX Syrup containing 2.5 mg of desloratadine resulted in desloratadine plasma concentrations similar to those achieved in adults administered a single 5 mg CLARINEX Tablet. In subjects 2 to 5 years old, a single dose of 2.5 mL of CLARINEX Syrup containing 1.25 mg of desloratadine resulted in desloratadine plasma concentrations similar to those achieved in adults administered a single 5 mg CLARINEX Tablet. However, the Cmax and AUCt of the metabolite (3-OH desloratadine) were 1.27 and 1.61 times higher for the 5 mg dose of syrup administered in adults compared to the Cmax and AUCt obtained in children 2–11 years of age receiving 1.25–2.5 mg of CLARINEX Syrup.
A single dose of either 2.5 mL or 1.25 mL of CLARINEX Syrup containing 1.25 mg or 0.625 mg, respectively, of desloratadine was administered to subjects 6 to 11 months of age and 12 to 23 months of age. The results of a population pharmacokinetic analysis indicated that a dose of 1 mg for subjects aged 6 to 11 months and 1.25 mg for subjects 12 to 23 months of age is required to obtain desloratadine plasma concentrations similar to those achieved in adults administered a single 5 mg dose of CLARINEX Syrup.
The CLARINEX RediTabs Tablet 2.5 mg tablet has not been evaluated in pediatric patients. Bioequivalence of the CLARINEX RediTabs Tablet and the original CLARINEX RediTabs Tablets was established in adults. In conjunction with the dose finding studies in pediatrics described, the pharmacokinetic data for CLARINEX RediTabs Tablet supports the use of the 2.5 mg dose strength in pediatric patients 6–11 years of age.
Renally Impaired
Desloratadine pharmacokinetics following a single dose of 7.5 mg were characterized in patients with mild (n=7; creatinine clearance 51–69 mL/min/1.73 m2), moderate (n=6; creatinine clearance 34–43 mL/min/1.73 m2), and severe (n=6; creatinine clearance 5–29 mL/min/1.73 m2) renal impairment or hemodialysis-dependent (n=6) patients. In patients with mild and moderate renal impairment, median Cmax and AUC values increased by approximately 1.2- and 1.9-fold, respectively, relative to subjects with normal renal function. In patients with severe renal impairment or who were hemodialysis dependent, Cmax and AUC values increased by approximately 1.7- and 2.5-fold, respectively. Minimal changes in 3-hydroxydesloratadine concentrations were observed. Desloratadine and 3-hydroxydesloratadine were poorly removed by hemodialysis. Plasma protein binding of desloratadine and 3-hydroxydesloratadine was unaltered by renal impairment. Dosage adjustment for patients with renal impairment is recommended (see DOSAGE AND ADMINISTRATION section).
Hepatically Impaired
Desloratadine pharmacokinetics were characterized following a single oral dose in patients with mild (n=4), moderate (n=4), and severe (n=4) hepatic impairment as defined by the Child-Pugh classification of hepatic function and 8 subjects with normal hepatic function. Patients with hepatic impairment, regardless of severity, had approximately a 2.4-fold increase in AUC as compared with normal subjects. The apparent oral clearance of desloratadine in patients with mild, moderate, and severe hepatic impairment was 37%, 36%, and 28% of that in normal subjects, respectively. An increase in the mean elimination half-life of desloratadine in patients with hepatic impairment was observed. For 3-hydroxydesloratadine, the mean Cmax and AUC values for patients with hepatic impairment were not statistically significantly different from subjects with normal hepatic function. Dosage adjustment for patients with hepatic impairment is recommended (see DOSAGE AND ADMINISTRATION section).
Gender
Female subjects treated for 14 days with CLARINEX Tablets had 10% and 3% higher desloratadine Cmax and AUC values, respectively, compared with male subjects. The 3-hydroxydesloratadine Cmax and AUC values were also increased by 45% and 48%, respectively, in females compared with males. However, these apparent differences are not likely to be clinically relevant and therefore no dosage adjustment is recommended.
Race
Following 14 days of treatment with CLARINEX Tablets, the Cmax and AUC values for desloratadine were 18% and 32% higher, respectively, in Blacks compared with Caucasians. For 3-hydroxydesloratadine there was a corresponding 10% reduction in Cmax and AUC values in Blacks compared to Caucasians. These differences are not likely to be clinically relevant and therefore no dose adjustment is recommended.
Drug Interactions
In two controlled crossover clinical pharmacology studies in healthy male (n=12 in each study) and female (n=12 in each study) volunteers, desloratadine 7.5 mg (1.5 times the daily dose) once daily was coadministered with erythromycin 500 mg every 8 hours or ketoconazole 200 mg every 12 hours for 10 days. In three separate controlled, parallel group clinical pharmacology studies, desloratadine at the clinical dose of 5 mg has been coadministered with azithromycin 500 mg followed by 250 mg once daily for 4 days (n=18) or with fluoxetine 20 mg once daily for 7 days after a 23-day pretreatment period with fluoxetine (n=18) or with cimetidine 600 mg every 12 hours for 14 days (n=18) under steady state conditions to normal healthy male and female volunteers. Although increased plasma concentrations (Cmax and AUC 0–24 hrs) of desloratadine and 3-hydroxydesloratadine were observed (see Table 1), there were no clinically relevant changes in the safety profile of desloratadine, as assessed by electrocardiographic parameters (including the corrected QT interval), clinical laboratory tests, vital signs, and adverse events.
Table 1 Changes in Desloratadine and 3-Hydroxydesloratadine Pharmacokinetics in Healthy Male and Female Volunteers Desloratadine 3-Hydroxydesloratadine Cmax AUC
0–24 hrsCmax AUC
0–24 hrsErythromycin
(500 mg Q8h)+24% +14% +43% +40% Ketoconazole
(200 mg Q12h)+45% +39% +43% +72% Azithromycin
(500 mg day 1, 250 mg QD × 4 days)+15% +5% +15% +4% Fluoxetine
(20 mg QD)+15% +0% +17% +13% Cimetidine
(600 mg Q12h)+12% +19% -11% -3% Pharmacodynamics
Wheal and Flare
Human histamine skin wheal studies following single and repeated 5 mg doses of desloratadine have shown that the drug exhibits an antihistaminic effect by 1 hour; this activity may persist for as long as 24 hours. There was no evidence of histamine-induced skin wheal tachyphylaxis within the desloratadine 5 mg group over the 28-day treatment period. The clinical relevance of histamine wheal skin testing is unknown.
Effects on QTc
Single dose administration of desloratadine did not alter the corrected QT interval (QTc) in rats (up to 12 mg/kg, oral), or guinea pigs (25 mg/kg, intravenous). Repeated oral administration at doses up to 24 mg/kg for durations up to 3 months in monkeys did not alter the QTc at an estimated desloratadine exposure (AUC) that was approximately 955 times the mean AUC in humans at the recommended daily oral dose. See OVERDOSAGE section for information on human QTc experience.
Clinical Trials
Seasonal Allergic Rhinitis
The clinical efficacy and safety of CLARINEX Tablets were evaluated in over 2,300 patients 12 to 75 years of age with seasonal allergic rhinitis. A total of 1,838 patients received 2.5–20 mg/day of CLARINEX in four double-blind, randomized, placebo-controlled clinical trials of 2 to 4 weeks' duration conducted in the United States. The results of these studies demonstrated the efficacy and safety of CLARINEX 5 mg in the treatment of adult and adolescent patients with seasonal allergic rhinitis. In a dose ranging trial, CLARINEX 2.5–20 mg/day was studied. Doses of 5, 7.5, 10, and 20 mg/day were superior to placebo; and no additional benefit was seen at doses above 5.0 mg. In the same study, an increase in the incidence of somnolence was observed at doses of 10 mg/day and 20 mg/day (5.2% and 7.6%, respectively), compared to placebo (2.3%).
In two 4-week studies of 924 patients (aged 15 to 75 years) with seasonal allergic rhinitis and concomitant asthma, CLARINEX Tablets 5 mg once daily improved rhinitis symptoms, with no decrease in pulmonary function. This supports the safety of administering CLARINEX Tablets to adult patients with seasonal allergic rhinitis with mild to moderate asthma.
CLARINEX Tablets 5 mg once daily significantly reduced the Total Symptom Scores (the sum of individual scores of nasal and non-nasal symptoms) in patients with seasonal allergic rhinitis. See Table 2.
Table 2 TOTAL SYMPTOM SCORE (TSS) Changes in a 2-Week Clinical Trial in Patients with Seasonal Allergic Rhinitis Treatment Group
(n)Mean Baseline*
(sem)Change from Baseline†
(sem)Placebo Comparison
(P-value)- *
- At baseline, a total nasal symptom score (sum of 4 individual symptoms) of at least 6 and a total non-nasal symptom score (sum of 4 individual symptoms) of at least 5 (each symptom scored 0 to 3 where 0=no symptom and 3=severe symptoms) was required for trial eligibility. TSS ranges from 0=no symptoms to 24=maximal symptoms.
- †
- Mean reduction in TSS averaged over the 2-week treatment period.
CLARINEX 5.0 mg (171) 14.2 (0.3) -4.3 (0.3) P<0.01 Placebo (173) 13.7 (0.3) -2.5 (0.3) There were no significant differences in the effectiveness of CLARINEX Tablets 5 mg across subgroups of patients defined by gender, age, or race.
Perennial Allergic Rhinitis
The clinical efficacy and safety of CLARINEX Tablets 5 mg were evaluated in over 1,300 patients 12 to 80 years of age with perennial allergic rhinitis. A total of 685 patients received 5 mg/day of CLARINEX in two double-blind, randomized, placebo-controlled clinical trials of 4 weeks' duration conducted in the United States and internationally. In one of these studies CLARINEX Tablets 5 mg once daily was shown to significantly reduce symptoms of perennial allergic rhinitis (Table 3).
Table 3 TOTAL SYMPTOM SCORE (TSS) Changes in a 4-Week Clinical Trial in Patients with Perennial Allergic Rhinitis Treatment Group
(n)Mean Baseline*
(sem)Change from Baseline†
(sem)Placebo Comparison
(P-value)- *
- At baseline, average of total symptom score (sum of 5 individual nasal symptoms and 3 non-nasal symptoms, each symptom scored 0 to 3 where 0=no symptom and 3=severe symptoms) of at least 10 was required for trial eligibility. TSS ranges from 0=no symptoms to 24=maximal symptoms.
- †
- Mean reduction in TSS averaged over the 4-week treatment period.
CLARINEX 5.0 mg (337) 12.37 (0.18) -4.06 (0.21) P=0.01 Placebo (337) 12.30 (0.18) -3.27 (0.21) Chronic Idiopathic Urticaria
The efficacy and safety of CLARINEX Tablets 5 mg once daily was studied in 416 chronic idiopathic urticaria patients 12 to 84 years of age, of whom 211 received CLARINEX. In two double-blind, placebo-controlled, randomized clinical trials of six weeks' duration, at the pre-specified one-week primary time point evaluation, CLARINEX Tablets significantly reduced the severity of pruritus when compared to placebo (Table 4). Secondary endpoints were also evaluated and during the first week of therapy CLARINEX Tablets 5 mg reduced the secondary endpoints, "Number of Hives" and the "Size of the Largest Hive," when compared to placebo.
Table 4 PRURITUS SYMPTOM SCORE Changes in the First Week of a Clinical Trial in Patients with Chronic Idiopathic Urticaria Treatment Group
(n)Mean Baseline
(sem)Change from Baseline*
(sem)Placebo Comparison
(P-value)Pruritus scored 0 to 3 where 0=no symptom to 3=maximal symptom. - *
- Mean reduction in pruritus averaged over the first week of treatment.
CLARINEX 5.0 mg (115) 2.19 (0.04) -1.05 (0.07) P<0.01 Placebo (110) 2.21 (0.04) -0.52 (0.07) The clinical safety of CLARINEX Syrup was documented in three, 15-day, double-blind, placebo-controlled safety studies in pediatric subjects with a documented history of allergic rhinitis, chronic idiopathic urticaria, or subjects who were candidates for antihistamine therapy. In the first study, 2.5 mg of CLARINEX Syrup was administered to 60 pediatric subjects 6 to 11 years of age. The second study evaluated 1.25 mg of CLARINEX Syrup administered to 55 pediatric subjects 2 to 5 years of age. In the third study, 1.25 mg of CLARINEX Syrup was administered to 65 pediatric subjects 12 to 23 months of age and 1.0 mg of CLARINEX Syrup was administered to 66 pediatric subjects 6 to 11 months of age. The results of these studies demonstrated the safety of CLARINEX Syrup in pediatric subjects 6 months to 11 years of age.
-
INDICATIONS AND USAGE
Seasonal Allergic Rhinitis
CLARINEX is indicated for the relief of the nasal and non-nasal symptoms of seasonal allergic rhinitis in patients 2 years of age and older.
- CONTRAINDICATIONS
-
PRECAUTIONS
Carcinogenesis, Mutagenesis, Impairment of Fertility
The carcinogenic potential of desloratadine was assessed using a loratadine study in rats and a desloratadine study in mice. In a 2-year study in rats, loratadine was administered in the diet at doses up to 25 mg/kg/day (estimated desloratadine and desloratadine metabolite exposures were approximately 30 times the AUC in humans at the recommended daily oral dose). A significantly higher incidence of hepatocellular tumors (combined adenomas and carcinomas) was observed in males given 10 mg/kg/day of loratadine and in males and females given 25 mg/kg/day of loratadine. The estimated desloratadine and desloratadine metabolite exposures in rats given 10 mg/kg of loratadine were approximately 7 times the AUC in humans at the recommended daily oral dose. The clinical significance of these findings during long-term use of desloratadine is not known.
In a 2-year dietary study in mice, males and females given up to 16 mg/kg/day and 32 mg/kg/day desloratadine, respectively, did not show significant increases in the incidence of any tumors. The estimated desloratadine and metabolite exposures in mice at these doses were 12 and 27 times, respectively, the AUC in humans at the recommended daily oral dose.
In genotoxicity studies with desloratadine, there was no evidence of genotoxic potential in a reverse mutation assay (Salmonella/E. coli mammalian microsome bacterial mutagenicity assay) or in two assays for chromosomal aberrations (human peripheral blood lymphocyte clastogenicity assay and mouse bone marrow micronucleus assay).
There was no effect on female fertility in rats at desloratadine doses up to 24 mg/kg/day (estimated desloratadine and desloratadine metabolite exposures were approximately 130 times the AUC in humans at the recommended daily oral dose). A male specific decrease in fertility, demonstrated by reduced female conception rates, decreased sperm numbers and motility, and histopathologic testicular changes, occurred at an oral desloratadine dose of 12 mg/kg in rats (estimated desloratadine exposures were approximately 45 times the AUC in humans at the recommended daily oral dose). Desloratadine had no effect on fertility in rats at an oral dose of 3 mg/kg/day (estimated desloratadine and desloratadine metabolite exposures were approximately 8 times the AUC in humans at the recommended daily oral dose).
Pregnancy Category C
Desloratadine was not teratogenic in rats at doses up to 48 mg/kg/day (estimated desloratadine and desloratadine metabolite exposures were approximately 210 times the AUC in humans at the recommended daily oral dose) or in rabbits at doses up to 60 mg/kg/day (estimated desloratadine exposures were approximately 230 times the AUC in humans at the recommended daily oral dose). In a separate study, an increase in pre-implantation loss and a decreased number of implantations and fetuses were noted in female rats at 24 mg/kg (estimated desloratadine and desloratadine metabolite exposures were approximately 120 times the AUC in humans at the recommended daily oral dose). Reduced body weight and slow righting reflex were reported in pups at doses of 9 mg/kg/day or greater (estimated desloratadine and desloratadine metabolite exposures were approximately 50 times or greater than the AUC in humans at the recommended daily oral dose). Desloratadine had no effect on pup development at an oral dose of 3 mg/kg/day (estimated desloratadine and desloratadine metabolite exposures were approximately 7 times the AUC in humans at the recommended daily oral dose). There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, desloratadine should be used during pregnancy only if clearly needed.
Nursing Mothers
Desloratadine passes into breast milk; therefore a decision should be made whether to discontinue nursing or to discontinue desloratadine, taking into account the importance of the drug to the mother.
Pediatric Use
The recommended dose of CLARINEX Syrup in the pediatric population is based on cross-study comparison of the plasma concentration of CLARINEX in adults and pediatric subjects. The safety of CLARINEX Syrup has been established in 246 pediatric subjects aged 6 months to 11 years in three placebo-controlled clinical studies. Since the course of seasonal and perennial allergic rhinitis and chronic idiopathic urticaria and the effects of CLARINEX are sufficiently similar in the pediatric and adult populations, it allows extrapolation from the adult efficacy data to pediatric patients. The effectiveness of CLARINEX Syrup in these age groups is supported by evidence from adequate and well-controlled studies of CLARINEX Tablets in adults. The safety and effectiveness of CLARINEX Tablets or CLARINEX Syrup have not been demonstrated in pediatric patients less than 6 months of age.
The CLARINEX RediTabs Tablet 2.5 mg tablet has not been evaluated in pediatric patients. Bioequivalence of the CLARINEX RediTabs Tablet and the previously marketed RediTabs Tablet was established in adults. In conjunction with the dose finding studies in pediatrics described, the pharmacokinetic data for CLARINEX RediTabs Tablet supports the use of the 2.5 mg dose strength in pediatric patients 6–11 years of age.
Geriatric Use
Clinical studies of desloratadine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy (see CLINICAL PHARMACOLOGY – Special Populations).
Information for Patients
Patients should be instructed to use CLARINEX Tablets as directed. As there are no food effects on bioavailability, patients can be instructed that CLARINEX Tablets, Syrup, or RediTabs Tablets may be taken without regard to meals. Patients should be advised not to increase the dose or dosing frequency, as studies have not demonstrated increased effectiveness at higher doses and somnolence may occur. Phenylketonurics: CLARINEX RediTabs Tablets contain phenylalanine 2.9 mg per 5 mg CLARINEX RediTabs Tablet or 1.4 mg per 2.5 mg CLARINEX RediTabs Tablet.
-
ADVERSE REACTIONS
Adults and Adolescents
Allergic Rhinitis
In multiple-dose placebo-controlled trials, 2,834 patients ages 12 years or older received CLARINEX Tablets at doses of 2.5 mg to 20 mg daily, of whom 1,655 patients received the recommended daily dose of 5 mg. In patients receiving 5 mg daily, the rate of adverse events was similar between CLARINEX and placebo-treated patients. The percent of patients who withdrew prematurely due to adverse events was 2.4% in the CLARINEX group and 2.6% in the placebo group. There were no serious adverse events in these trials in patients receiving desloratadine. All adverse events that were reported by greater than or equal to 2% of patients who received the recommended daily dose of CLARINEX Tablets (5.0 mg once-daily), and that were more common with CLARINEX Tablets than placebo, are listed in Table 5.
Table 5 Incidence of Adverse Events Reported by 2% or More of Adult and Adolescent Allergic Rhinitis Patients in Placebo-Controlled, Multiple-Dose Clinical Trials with the Tablet Formulation of CLARINEX Adverse Experience CLARINEX Tablets 5 mg
(n=1,655)Placebo
(n=1,652)Pharyngitis 4.1% 2.0% Dry Mouth 3.0% 1.9% Myalgia 2.1% 1.8% Fatigue 2.1% 1.2% Somnolence 2.1% 1.8% Dysmenorrhea 2.1% 1.6% The frequency and magnitude of laboratory and electrocardiographic abnormalities were similar in CLARINEX and placebo-treated patients.
There were no differences in adverse events for subgroups of patients as defined by gender, age, or race.
Chronic Idiopathic Urticaria
In multiple-dose, placebo-controlled trials of chronic idiopathic urticaria, 211 patients ages 12 years or older received CLARINEX Tablets and 205 received placebo. Adverse events that were reported by greater than or equal to 2% of patients who received CLARINEX Tablets and that were more common with CLARINEX than placebo were (rates for CLARINEX and placebo, respectively): headache (14%, 13%), nausea (5%, 2%), fatigue (5%, 1%), dizziness (4%, 3%), pharyngitis (3%, 2%), dyspepsia (3%, 1%), and myalgia (3%, 1%).
Pediatrics
Two hundred and forty-six pediatric subjects 6 months to 11 years of age received CLARINEX Syrup for 15 days in three placebo-controlled clinical trials. Pediatric subjects aged 6 to 11 years received 2.5 mg once a day, subjects aged 1 to 5 years received 1.25 mg once a day, and subjects 6 to 11 months of age received 1.0 mg once a day. In subjects 6 to 11 years of age, no individual adverse event was reported by 2 percent or more of the subjects. In subjects 2 to 5 years of age, adverse events reported for CLARINEX and placebo in at least 2 percent of subjects receiving CLARINEX Syrup and at a frequency greater than placebo were fever (5.5%, 5.4%), urinary tract infection (3.6%, 0%), and varicella (3.6%, 0%). In subjects 12 months to 23 months of age, adverse events reported for the CLARINEX product and placebo in at least 2 percent of subjects receiving CLARINEX Syrup and at a frequency greater than placebo were fever (16.9%, 12.9%), diarrhea (15.4%, 11.3%), upper respiratory tract infections (10.8%, 9.7%), coughing (10.8%, 6.5%), appetite increased (3.1%, 1.6%), emotional lability (3.1%, 0%), epistaxis (3.1%, 0%), parasitic infection (3.1%, 0%), pharyngitis (3.1%, 0%), rash maculopapular (3.1%, 0%). In subjects 6 months to 11 months of age, adverse events reported for CLARINEX and placebo in at least 2 percent of subjects receiving CLARINEX Syrup and at a frequency greater than placebo were upper respiratory tract infections (21.2%, 12.9%), diarrhea (19.7%, 8.1%), fever (12.1%, 1.6%), irritability (12.1%, 11.3%), coughing (10.6%, 9.7%), somnolence (9.1%, 8.1%), bronchitis (6.1%, 0%), otitis media (6.1%, 1.6%), vomiting (6.1%, 3.2%), anorexia (4.5%, 1.6%), pharyngitis (4.5%, 1.6%), insomnia (4.5%, 0%), rhinorrhea (4.5%, 3.2%), erythema (3.0%, 1.6%), and nausea (3.0%, 0%). There were no clinically meaningful changes in any electrocardiographic parameter, including the QTc interval. Only one of the 246 pediatric subjects receiving CLARINEX Syrup in the clinical trials discontinued treatment because of an adverse event.
Observed During Clinical Practice
The following spontaneous adverse events have been reported during the marketing of desloratadine: tachycardia, palpitations, rare cases of hypersensitivity reactions (such as rash, pruritus, urticaria, edema, dyspnea, and anaphylaxis), psychomotor hyperactivity, seizures, and elevated liver enzymes including bilirubin, and very rarely, hepatitis.
- DRUG ABUSE AND DEPENDENCE
-
OVERDOSAGE
Information regarding acute overdosage is limited to experience from clinical trials conducted during the development of the CLARINEX product. In a dose ranging trial, at doses of 10 mg and 20 mg/day somnolence was reported.
Single daily doses of 45 mg were given to normal male and female volunteers for 10 days. All ECGs obtained in this study were manually read in a blinded fashion by a cardiologist. In CLARINEX-treated subjects, there was an increase in mean heart rate of 9.2 bpm relative to placebo. The QT interval was corrected for heart rate (QTc) by both the Bazett and Fridericia methods. Using the QTc (Bazett) there was a mean increase of 8.1 msec in CLARINEX-treated subjects relative to placebo. Using QTc (Fridericia) there was a mean increase of 0.4 msec in CLARINEX-treated subjects relative to placebo. No clinically relevant adverse events were reported.
In the event of overdose, consider standard measures to remove any unabsorbed drug. Symptomatic and supportive treatment is recommended. Desloratadine and 3-hydroxy-desloratadine are not eliminated by hemodialysis.
Lethality occurred in rats at oral doses of 250 mg/kg or greater (estimated desloratadine and desloratadine metabolite exposures were approximately 120 times the AUC in humans at the recommended daily oral dose). The oral median lethal dose in mice was 353 mg/kg (estimated desloratadine exposures were approximately 290 times the human daily oral dose on a mg/m2 basis). No deaths occurred at oral doses up to 250 mg/kg in monkeys (estimated desloratadine exposures were approximately 810 times the human daily oral dose on a mg/m2 basis).
-
DOSAGE AND ADMINISTRATION
Adults and children 12 years of age and over
The recommended dose of CLARINEX Tablets or CLARINEX RediTabs Tablets is one 5 mg tablet once daily or the recommended dose of CLARINEX Syrup is 2 teaspoonfuls (5 mg in 10 mL) once daily.
Children 6 to 11 years of age
The recommended dose of CLARINEX Syrup is 1 teaspoonful (2.5 mg in 5 mL) once daily or the recommended dose of CLARINEX RediTabs Tablets is one 2.5 mg tablet once daily.
Children 12 months to 5 years of age
The recommended dose of CLARINEX Syrup is ½ teaspoonful (1.25 mg in 2.5 mL) once daily.
Children 6 to 11 months of age
The recommended dose of CLARINEX Syrup is 2 mL (1.0 mg) once daily.
The age-appropriate dose of CLARINEX Syrup should be administered with a commercially available measuring dropper or syringe that is calibrated to deliver 2 mL and 2.5 mL (½ teaspoon).
In adult patients with liver or renal impairment, a starting dose of one 5 mg tablet every other day is recommended based on pharmacokinetic data. Dosing recommendation for children with liver or renal impairment cannot be made due to lack of data.
-
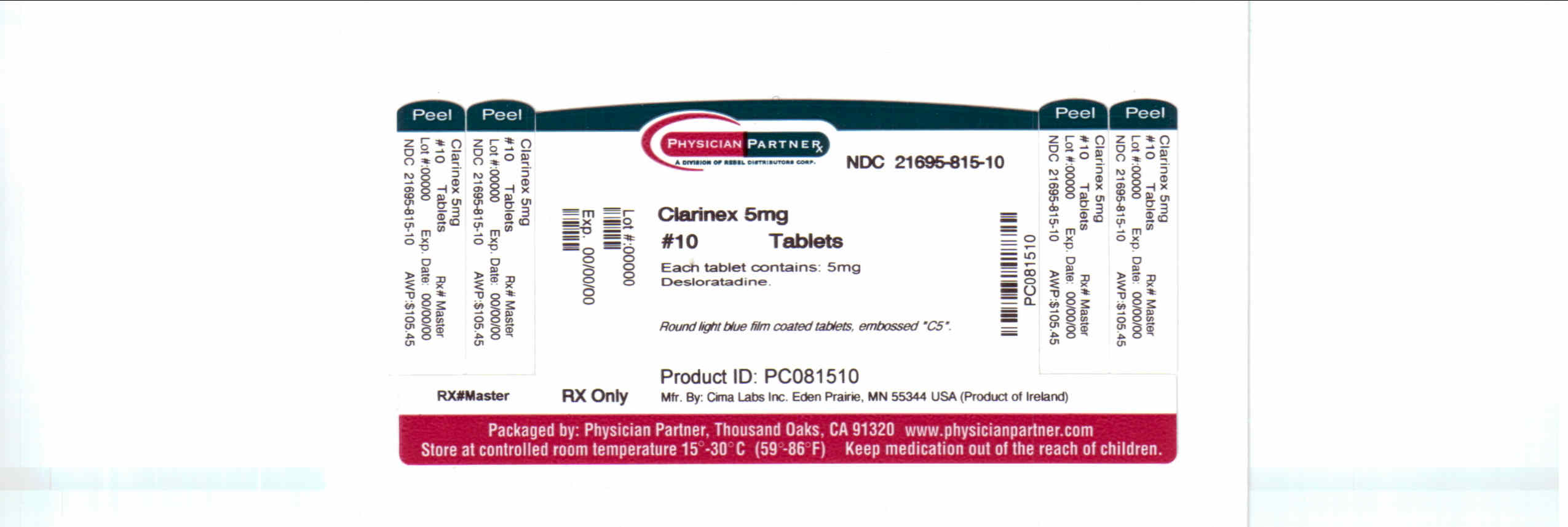
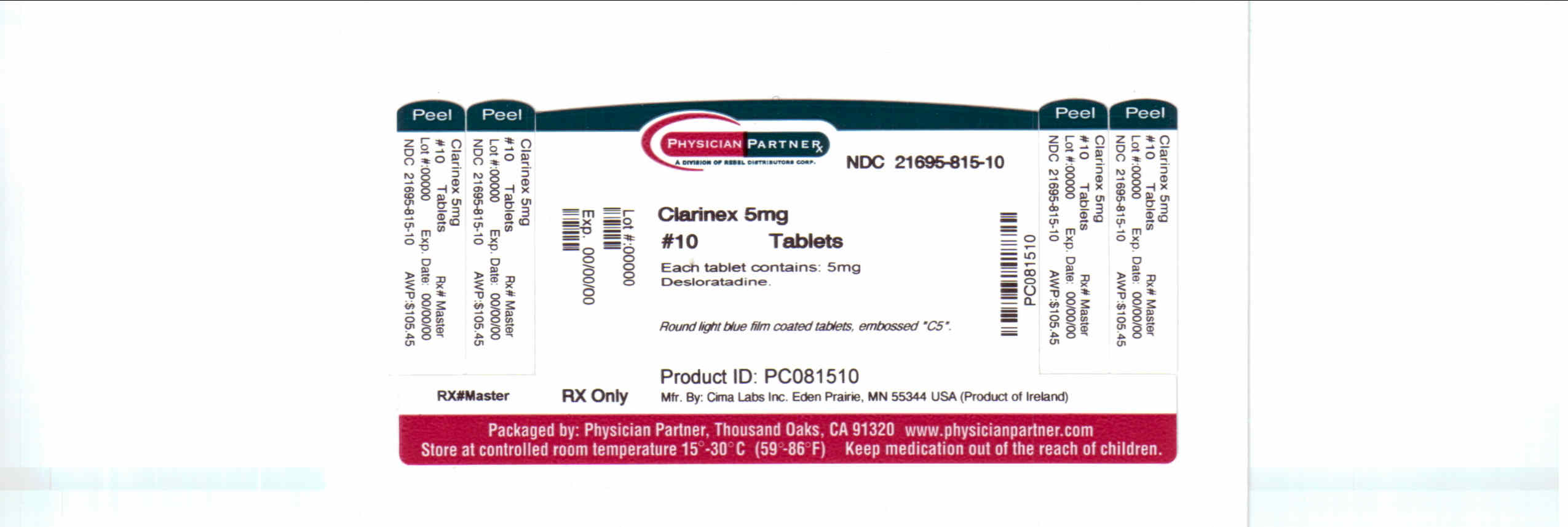
HOW SUPPLIED
CLARINEX Tablets
Embossed "C5", light blue film coated tablets; that are packaged in high-density polyethylene plastic bottles of 10 (NDC 21695-815-10).
Protect Unit-of-Use packaging and Unit Dose-Hospital Pack from excessive moisture.
Store at 25°C (77°F); excursions permitted to 15°–30°C (59°–86°F) [see USP Controlled Room Temperature]. Heat sensitive. Avoid exposure at or above 30°C (86°F).
- SPL UNCLASSIFIED SECTION
- Principal Display Panel
-
INGREDIENTS AND APPEARANCE
CLARINEX
desloratadine tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:21695-815(NDC:0085-1264) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength Desloratadine (UNII: FVF865388R) (Desloratadine - UNII:FVF865388R) Desloratadine 5 mg Inactive Ingredients Ingredient Name Strength dibasic calcium phosphate dihydrate (UNII: O7TSZ97GEP) CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) STARCH, CORN (UNII: O8232NY3SJ) talc (UNII: 7SEV7J4R1U) CARNAUBA WAX (UNII: R12CBM0EIZ) WHITE WAX (UNII: 7G1J5DA97F) lactose monohydrate (UNII: EWQ57Q8I5X) HYPROMELLOSES (UNII: 3NXW29V3WO) titanium dioxide (UNII: 15FIX9V2JP) polyethylene glycol (UNII: 3WJQ0SDW1A) FD&C BLUE NO. 2 (UNII: L06K8R7DQK) Product Characteristics Color blue (LIGHT BLUE) Score no score Shape ROUND (ROUND) Size 6mm Flavor Imprint Code C5 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:21695-815-10 10 in 1 BOTTLE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date NDA NDA021297 02/08/2002 Labeler - Rebel Distributors Corp (118802834) Establishment Name Address ID/FEI Business Operations Rebel Distributors Corp 118802834 RELABEL, REPACK