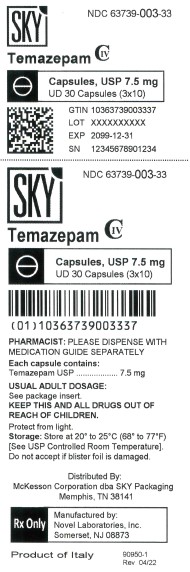
Label: TEMAZEPAM capsule
- NDC Code(s): 63739-003-33
- Packager: McKesson Corporation dba SKY Packaging
- This is a repackaged label.
- Source NDC Code(s): 67877-148
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: CIV
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated December 14, 2023
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
- temazepam 7.5mg-header
-
DESCRIPTION
Temazepam is a benzodiazepine hypnotic agent. The chemical name is 7-chloro-1,3-dihydro-3-hydroxy-1-methyl-5-phenyl-2H-1, 4-benzodiazepin-2-one, and the structural formula is:
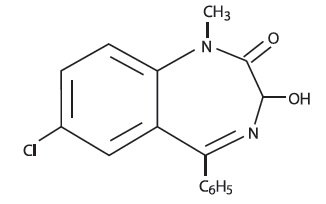
C 16H 13ClN 2O 2 MW = 300.74
Temazepam is a white, crystalline substance, very slightly soluble in water and sparingly soluble in alcohol USP.Temazepam Capsules, USP 7.5 mg, are for oral administration.
7.5 mg Capsules
Active Ingredient: temazepam USP
7.5 mg Capsules
Inactive Ingredients: Corn starch, lactose anhydrous, magnesium stearate, sodium lauryl sulfate, FD&C Red #40 and titanium dioxide.May also include: sodium lauryl sulfate. Imprinting ink may contain ammonium hydroxide, ethanol, isopropyl alcohol, butanol, shellac, potassium hydroxide, propylene glycol, and black iron oxide.
-
CLINICAL PHARMACOLOGY
Pharmacokinetics
In a single and multiple dose absorption, distribution, metabolism, and excretion (ADME) study, using 3H labeled drug, temazepam was well absorbed and found to have minimal (8%) first pass metabolism. There were no active metabolites formed and the only significant metabolite present in blood was the O-conjugate. The unchanged drug was 96% bound to plasma proteins. The blood level decline of the parent drug was biphasic with the short half-life ranging from 0.4 to 0.6 hours and the terminal half-life from 3.5 to 18.4 hours (mean 8.8 hours), depending on the study population and method of determination. Metabolites were formed with a half-life of 10 hours and excreted with a half-life of approximately 2 hours. Thus, formation of the major metabolite is the rate limiting step in the biodisposition of Temazepam. There is no accumulation of metabolites. A dose-proportional relationship has been established for the area under the plasma concentration/time curve over the 15 to 30 mg dose range.
Temazepam was completely metabolized through conjugation prior to excretion; 80% to 90% of the dose appeared in the urine. The major metabolite was the O-conjugate of temazepam (90%); the O-conjugate of N-desmethyl temazepam was a minor metabolite (7%).
Bioavailability, Induction, and Plasma Levels
Following ingestion of a 30 mg Temazepam capsule, measurable plasma concentrations were achieved 10 to 20 minutes after dosing with peak plasma levels ranging from 666 to 982 ng/mL (mean 865 ng/mL) occurring approximately 1.2 to 1.6 hours (mean 1.5 hours) after dosing.
In a 7 day study, in which subjects were given a 30 mg Temazepam capsule 1 hour before retiring, steady-state (as measured by the attainment of maximal trough concentrations) was achieved by the third dose. Mean plasma levels of Temazepam (for days 2 to 7) were 260±210 ng/mL at 9 hours and 75±80 ng/mL at 24 hours after dosing. A slight trend toward declining 24 hour plasma levels was seen after day 4 in the study, however, the 24 hour plasma levels were quite variable.
At a dose of 30 mg once-a-day for 8 weeks, no evidence of enzyme induction was found in man.
Elimination Rate of Benzodiazepine Hypnotics and Profile of Common Untoward Effects
The type and duration of hypnotic effects and the profile of unwanted effects during administration of benzodiazepine hypnotics may be influenced by the biologic half-life of the administered drug and for some hypnotics, the half-life of any active metabolites formed. Benzodiazepine hypnotics have a spectrum of half-lives from short (<4 hours) to long (>20 hours). When half-lives are long, drug (and for some drugs their active metabolites) may accumulate during periods of nightly administration and be associated with impairments of cognitive and/or motor performance during waking hours; the possibility of interaction with other psychoactive drugs or alcohol will be enhanced. In contrast, if half-lives are shorter, drug (and, where appropriate, its active metabolites) will be cleared before the next dose is ingested, and carry-over effects related to excessive sedation or CNS depression should be minimal or absent. However, during nightly use for an extended period, pharmacodynamic tolerance or adaptation to some effects of benzodiazepine hypnotics may develop. If the drug has a short elimination half-life, it is possible that a relative deficiency of the drug, or, if appropriate, its active metabolites (i.e., in relationship to the receptor site) may occur at some point in the interval between each night’s use. This sequence of events may account for 2 clinical findings reported to occur after several weeks of nightly use of rapidly eliminated benzodiazepine hypnotics, namely, increased wakefulness during the last third of the night, and the appearance of increased signs of daytime anxiety.
Controlled Trials Supporting Efficacy
Temazepam improved sleep parameters in clinical studies. Residual medication effects (“hangover”) were essentially absent. Early morning awakening, a particular problem in the geriatric patient, was significantly reduced.
Patients with chronic insomnia were evaluated in 2 week, placebo controlled sleep laboratory studies with temazepam at doses of 7.5 mg, 15 mg, and 30 mg, given 30 minutes prior to bedtime. There was a linear dose-response improvement in total sleep time and sleep latency, with significant drug-placebo differences at 2 weeks occurring only for total sleep time at the 2 higher doses, and for sleep latency only at the highest dose.
In these sleep laboratory studies, REM sleep was essentially unchanged and slow wave sleep was decreased. No measurable effects on daytime alertness or performance occurred following temazepam treatment or during the withdrawal period, even though a transient sleep disturbance in some sleep parameters was observed following withdrawal of the higher doses. There was no evidence of tolerance development in the sleep laboratory parameters when patients were given temazepam nightly for at least 2 weeks.
In addition, normal subjects with transient insomnia associated with first night adaptation to the sleep laboratory were evaluated in 24 hour, placebo controlled sleep laboratory studies with temazepam at doses of 7.5 mg, 15 mg, and 30 mg, given 30 minutes prior to bedtime. There was a linear dose-response improvement in total sleep time, sleep latency and number of awakenings, with significant drug-placebo differences occurring for sleep latency at all doses, for total sleep time at the 2 higher doses and for number of awakenings only at the 30 mg dose.
-
INDICATIONS & USAGE
Temazepam Capsules, USP are indicated for the short-term treatment of insomnia (generally 7 to 10 days). For patients with short-term insomnia, instructions in the prescription should indicate that Temazepam Capsules should be used for short periods of time (7 to 10 days).
The clinical trials performed in support of efficacy were 2 weeks in duration with the final formal assessment of sleep latency performed at the end of treatment.
-
CONTRAINDICATIONS
Benzodiazepines may cause fetal harm when administered to a pregnant woman. An increased risk of congenital malformations associated with the use of diazepam and chlordiazepoxide during the first trimester of pregnancy has been suggested in several studies. Transplacental distribution has resulted in neonatal CNS depression following the ingestion of therapeutic doses of a benzodiazepine hypnotic during the last weeks of pregnancy.
Reproduction studies in animals with temazepam were performed in rats and rabbits. In a perinatal-postnatal study in rats, oral doses of 60 mg/kg/day resulted in increasing nursling mortality. Teratology studies in rats demonstrated increased fetal resorptions at doses of 30 and 120 mg/kg in one study and increased occurrence of rudimentary ribs, which are considered skeletal variants, in a second study at doses of 240 mg/kg or higher. In rabbits, occasional abnormalities such as exencephaly and fusion or asymmetry of ribs were reported without dose relationship. Although these abnormalities were not found in the concurrent control group, they have been reported to occur randomly in historical controls. At doses of 40 mg/kg or higher, there was an increased incidence of the 13th rib variant when compared to the incidence in concurrent and historical controls.
Temazepam is contraindicated in women who are or may become pregnant. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Patients should be instructed to discontinue the drug prior to becoming pregnant. The possibility that a woman of childbearing potential may be pregnant at the time of institution of therapy should be considered.
-
WARNINGS
Risks from Concomitant Use with Opioids
Concomitant use of benzodiazepines, including temazepam, and opioids may result in profound sedation, respiratory depression,
coma, and death. Because of these risks, reserve concomitant prescribing of these drugs in patients for whom alternative
treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of
drug-related mortality compared to use of opioids alone. If a decision is made to prescribe temazepam concomitantly with
opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs
and symptoms of respiratory depression and sedation. In patients already receiving an opioid analgesic, prescribe a lower initial
dose of temazepam than indicated in the absence of an opioid and titrate based on clinical response. If an opioid is initiated in a
patient already taking temazepam, prescribe a lower initial dose of the opioid and titrate based upon clinical response.
Advise both patients and caregivers about the risks of respiratory depression and sedation when temazepam is used with
opioids. Advise patients not to drive or operate heavy machinery until the effects of concomitant use with the opioid have been
determined ( seePRECAUTIONS, Drug Interactions).
Abuse, Misuse, and Addiction
The use of benzodiazepines, including temazepam, exposes users to the risks of abuse, misuse, and addiction, which can lead to
overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the
maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances,
which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or
death ( seeDRUG ABUSE AND DEPENDENCE, Abuse).
Before prescribing temazepam and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction (e.g., using
a standardized screening tool). Use of temazepam, particularly in patients at elevated risk, necessitates counseling about the
risks and proper use of temazepam along with monitoring for signs and symptoms of abuse, misuse, and addiction. Prescribe the
lowest effective dosage; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse,
misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a
substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
Dependence and Withdrawal Reactions
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue temazepam or reduce the dosage (a
patient-specific plan should be used to taper the dose) ( seeDOSAGE AND ADMINISTRATION, Discontinuation or Dosage
Reduction of temazepam).
Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction
include those who take higher dosages, and those who have had longer durations of use.
Acute Withdrawal Reactions
The continued use of benzodiazepines, including temazepam, may lead to clinically significant physical dependence. Abrupt
discontinuation or rapid dosage reduction of temazepam after continued use , or administration of flumazenil (a benzodiazepine
antagonist) may precipitate acute withdrawal reactions, which can be life-threatening (e.g., seizures) ( seeDRUG ABUSEAND DEPENDENCE, Dependence).Protracted Withdrawal Syndrome
In some cases, benzodiazepine users have developed a protracted withdrawal syndrome with withdrawal symptoms lasting
weeks to more than 12 months ( seeDRUG ABUSE AND DEPENDENCE, Dependence).
Sleep disturbance may be the presenting manifestation of an underlying physical and/or psychiatric disorder. Consequently, a
decision to initiate symptomatic treatment of insomnia should only be made after the patient has been carefully evaluated. The
failure of insomnia to remit after 7 to 10 days of treatment may indicate the presence of a primary psychiatric and/or
medical illness that should be evaluated . Worsening of insomnia may be the consequence of an unrecognized psychiatric or
physical disorder as may the emergence of new abnormalities of thinking or behavior. Such abnormalities have also been
reported to occur in association with the use of drugs with central nervous system depressant activity, including those of the
benzodiazepine class. Because some of the worrisome adverse effects of benzodiazepines, including temazepam, appear to be
dose related ( seePRECAUTIONSandDOSAGE AND ADMINISTRATION), it is important to use the lowest possible effective dose.
Elderly patients are especially at risk.
Some of these changes may be characterized by decreased inhibition, e.g., aggressiveness and extroversion that seem out of
character, similar to that seen with alcohol. Other kinds of behavioral changes can also occur, for example, bizarre behavior,
agitation, hallucinations, and depersonalization. Complex behaviors such as “sleep-driving” (i.e., driving while not fully awake
after ingestion of a sedative-hypnotic, with amnesia for the event) have been reported. These events can occur in
sedative-hypnotic-naïve as well as in sedative-hypnotic-experienced persons. Although behaviors such as “sleep-driving” may
occur with temazepam alone at therapeutic doses, the use of alcohol and other CNS depressants with Temazepam appears to
increase the risk of such behaviors, as does the use of temazepam at doses exceeding the maximum recommended dose. Due
to the risk to the patient and the community, discontinuation of temazepam should be strongly considered for patients who report
a “sleep-driving” episode. Other complex behaviors (e.g., preparing and eating food, making phone calls, or having sex) have
been reported in patients who are not fully awake after taking a sedative-hypnotic. As with “sleep-driving”, patients usually do
not remember these events. Amnesia and other neuro-psychiatric symptoms may occur unpredictably. In primarily depressed
patients, worsening of depression, including suicidal thinking has been reported in association with the use of sedative/hypnotics.
It can rarely be determined with certainty whether a particular instance of the abnormal behaviors listed above is drug induced,
spontaneous in origin, or a result of an underlying psychiatric or physical disorder. Nonetheless, the emergence of any new
behavioral sign or symptom of concern requires careful and immediate evaluation.
Because temazepam can cause drowsiness and a decreased level of consciousness, patients, particularly the elderly, are at
higher risk of falls.
Severe Anaphylactic and Anaphylactoid Reactions
Rare cases of angioedema involving the tongue, glottis or larynx have been reported in patients after taking the first or
subsequent doses of sedative-hypnotics, including temazepam. Some patients have had additional symptoms such as dyspnea,
throat closing, or nausea and vomiting that suggest anaphylaxis. Some patients have required medical therapy in the emergency
department. If angioedema involves the tongue, glottis or larynx, airway obstruction may occur and be fatal.
Patients who develop angioedema after treatment with temazepam should not be rechallenged with the drug. -
PRECAUTIONS
General
Since the risk of the development of oversedation, dizziness, confusion, and/or ataxia increases substantially with larger doses of benzodiazepines in elderly and debilitated patients, 7.5 mg of temazepam is recommended as the initial dosage for such patients.
Temazepam should be administered with caution in severely depressed patients or those in whom there is any evidence of latent depression; it should be recognized that suicidal tendencies may be present and protective measures may be necessary.
The usual precautions should be observed in patients with impaired renal or hepatic function and in patients with chronic pulmonary insufficiency.
If temazepam is to be combined with other drugs having known hypnotic properties or CNS-depressant effects, consideration should be given to potential additive effects.
The possibility of a synergistic effect exists with the co-administration of temazepam and diphenhydramine. One case of stillbirth at term has been reported 8 hours after a pregnant patient received temazepam and diphenhydramine. A cause and effect relationship has not yet been determined ( see CONTRAINDICATIONS).
Information for Patients
Advise the patient to read the FDA approved patient labeling (Medication Guide).
Risks from Concomitant Use with Opioids
Advise both patients and caregivers about the risks of potentially fatal respiratory depression and sedation when temazepam is
used with opioids and not to use such drugs concomitantly unless supervised by a healthcare provider. Advise patients not to
drive or operate heavy machinery until the effects of concomitant use with the opioid have been determined ( see WARNINGS,
Risks from Concomitant Use with Opioids and PRECAUTIONS, Drug Interactions).
Abuse, Misuse, and Addiction
Inform patients that the use of temazepam, even at recommended dosages, exposes users to risks of abuse, misuse, and
addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid
analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse,
and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug
( seeWARNINGS, Abuse, Misuse, and AddictionandDRUG ABUSE AND DEPENDENCE).
Withdrawal Reactions
Inform patients that the continued use of temazepam may lead to clinically significant physical dependence and that abrupt
discontinuation or rapid dosage reduction of temazepam may precipitate acute withdrawal reactions, which can be
life-threatening. Inform patients that in some cases, patients taking benzodiazepines have developed a protracted withdrawal
syndrome with withdrawal symptoms lasting weeks to more than 12 months. Instruct patients that discontinuation or dosage
reduction of temazepam may require a slow taper ( seeWARNINGS, Dependence and Withdrawal ReactionsandDRUG
ABUSE AND DEPENDENCE).
“Sleep-Driving” and Other Complex Behaviors
There have been reports of people getting out of bed after taking a sedative-hypnotic and driving their cars while not fully awake,
often with no memory of the event. If a patient experiences such an episode, it should be reported to his or her doctor
immediately, since “sleep-driving” can be dangerous. This behavior is more likely to occur when temazepam is taken with
alcohol or other central nervous system depressants ( seeWARNINGS). Other complex behaviors (e.g., preparing and eating food,
making phone calls, or having sex) have been reported in patients who are not fully awake after taking a sedative-hypnotic. As
with “sleep-driving”, patients usually do not remember these events.
Advise patients that increased drowsiness and decreased consciousness may increase the risk of falls in some patients.Laboratory Tests
The usual precautions should be observed in patients with impaired renal or hepatic function and in patients with chronic pulmonary insufficiency. Abnormal liver function tests as well as blood dyscrasias have been reported with benzodiazepines.
Drug Interactions
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different
receptor sites in the CNS that control respiration. Benzodiazepines interact at GABAA sites and opioids interact primarily at mu
receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen
opioid-related respiratory depression exists. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and
monitor patients closely for respiratory depression and sedation.
The pharmacokinetic profile of Temazepam does not appear to be altered by orally administered cimetidine dosed according to
labeling.Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies were conducted in rats at dietary temazepam doses up to 160 mg/kg/day for 24 months and in mice at dietary doses of 160 mg/kg/day for 18 months. No evidence of carcinogenicity was observed although hyperplastic liver nodules were observed in female mice exposed to the highest dose. The clinical significance of this finding is not known. Fertility in male and female rats was not adversely affected by temazepam. No mutagenicity tests have been done with temazepam.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when temazepam is administered to a nursing woman.
Geriatric Use
Clinical studies of temazepam did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in response between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy commonly observed in this population. Temazepam 7.5 mg is recommended as the initial dosage for patient aged 65 and over since the risk of the development of oversedation, dizziness, confusion, ataxia and/or falls increases substantially with larger doses of benzodiazepines in elderly and debilitated patients.
-
ADVERSE REACTIONS
During controlled clinical studies in which 1076 patients received temazepam at bedtime, the drug was well tolerated. Side effects were usually mild and transient. Adverse reactions occurring in 1% or more of patients are presented in the following table:
Temazepam % Incidence (n=1076)
Placebo % Incidence (n=783)
Drowsiness
9.1
5.6
Headache
8.5
9.1
Fatigue
4.8
4.7
Nervousness
4.6
8.2
Lethargy
4.5
3.4
Dizziness
4.5
3.3
Nausea
3.1
3.8
Hangover
2.5
1.1
Anxiety
2.0
1.5
Depression
1.7
1.8
Dry Mouth
1.7
2.2
Diarrhea
1.7
1.1
Abdominal Discomfort
1.5
1.9
Euphoria
1.5
0.4
Weakness
1.4
0.9
Confusion
1.3
0.5
Blurred Vision
1.3
1.3
Nightmares
1.2
1.7
Vertigo
1.2
0.8
The following adverse events have been reported less frequently (0.5% to 0.9%):
Central Nervous System - anorexia, ataxia, equilibrium loss, tremor, increased dreaming
Cardiovascular - dyspnea, palpitations Gastrointestinal – vomiting
Musculoskeletal – backache
Special Senses - hyperhidrosis, burning eyes
Amnesia, hallucinations, horizontal nystagmus, and paradoxical reactions including restlessness, overstimulation and agitation were rare (less than 0.5%).
-
DRUG ABUSE AND DEPENDENCE
Controlled Substance
Temazepam is a Schedule IV controlled substance.
Abuse
Temazepam is a benzodiazepine and a CNS depressant with a potential for abuse and addiction. Abuse is the intentional,
non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects. Misuse is the intentional use, for
therapeutic purposes, of a drug by an individual in a way other than prescribed by a healthcare provider or for whom it was not
prescribed. Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to
take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority
to drug use than other activities and obligations), and possible tolerance or physical dependence. Even taking benzodiazepines as
prescribed may put patients at risk for abuse and misuse of their medication. Abuse and misuse of benzodiazepines may lead to
addiction.
Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended
dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with
an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death. Benzodiazepines are
often sought by individuals who abuse drugs and other substances, and by individuals with addictive disorders (see WARNINGS,
Abuse, Misuse, and Addiction).
The following adverse reactions have occurred with benzodiazepine abuse and/or misuse: abdominal pain, amnesia, anorexia,
anxiety, aggression, ataxia, blurred vision, confusion, depression, disinhibition, disorientation, dizziness, euphoria, impaired
concentration and memory, indigestion, irritability, muscle pain, slurred speech, tremors, and vertigo.
The following severe adverse reactions have occurred with benzodiazepine abuse and/or misuse: delirium, paranoia, suicidal
ideation and behavior, seizures, coma, breathing difficulty, and death. Death is more often associated with polysubstance use
(especially benzodiazepines with other CNS depressants such as opioids and alcohol).Dependence
Physical Dependence
Temazepam may produce physical dependence from continued therapy. Physical dependence is a state that develops as a result
of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt
discontinuation or a significant dose reduction of a drug. Abrupt discontinuation or rapid dosage reduction of benzodiazepines or
administration of flumazenil, a benzodiazepine antagonist, may precipitate acute withdrawal reactions, including seizures, which
can be life-threatening. Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or
rapid dosage reduction include those who take higher dosages (i.e., higher and/or more frequent doses) and those who have had
longer durations of use ( seeWARNINGS, Dependence and Withdrawal Reactions).
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue Temazepam or reduce the dosage ( seeDOSAGE
and ADMINISTRATION, Discontinuation or Dosage Reduction of TemazepamandWARNINGS, Dependence and
Withdrawal Reactions).
Acute Withdrawal Signs and Symptoms
Acute withdrawal signs and symptoms associated with benzodiazepines have included abnormal involuntary movements,
anxiety, blurred vision, depersonalization, depression, derealization, dizziness, fatigue, gastrointestinal adverse reactions (e.g.,
nausea, vomiting, diarrhea, weight loss, decreased appetite), headache, hyperacusis, hypertension, irritability, insomnia, memory
impairment, muscle pain and stiffness, panic attacks, photophobia, restlessness, tachycardia, and tremor. More severe acute
withdrawal signs and symptoms including life-threatening reactions, have included catatonia, convulsions, delirium tremens,
depression, hallucinations, mania, psychosis, seizures, and suicidality.
Protracted Withdrawal Syndrome
Protracted withdrawal syndrome with benzodiazepines is characterized by anxiety, cognitive impairment, depression, insomnia,
formication, motor symptoms (e.g., weakness, tremor, muscle twitches), paresthesia, and tinnitus that persists beyond 4 to 6
weeks after initial benzodiazepine withdrawal. Protracted withdrawal symptoms may last weeks to more than 12 months. As a
result, there may be difficulty in differentiating withdrawal symptoms from potential re-emergence or continuation of symptoms
for which the benzodiazepine was being used.
Tolerance
Tolerance to Temazepam may develop from continued therapy. Tolerance is a physiological state characterized by a reduced
response to a drug after repeated administration (i.e., a higher dose of a drug is required to produce the same effect that was
once obtained at a lower dose). Tolerance to the therapeutic effect of Temazepam may develop; however, little tolerance develops
to the amnestic reactions and other cognitive impairments caused by benzodiazepines. -
OVERDOSAGE
Manifestations of acute overdosage of temazepam can be expected to reflect the CNS effects of the drug and include somnolence, confusion, and coma, with reduced or absent reflexes, respiratory depression, and hypotension. The oral LD50 of temazepam was 1963 mg/kg in mice, 1833 mg/kg in rats, and >2400 mg/kg in rabbits.
Treatment
If the patient is conscious, vomiting should be induced mechanically or with emetics. Gastric lavage should be employed utilizing concurrently a cuffed endotracheal tube if the patient is unconscious to prevent aspiration and pulmonary complications. Maintenance of adequate pulmonary ventilation is essential. The use of pressor agents intravenously may be necessary to combat hypotension. Fluids should be administered intravenously to encourage diuresis. The value of dialysis has not been determined. If excitation occurs, barbiturates should not be used. It should be borne in mind that multiple agents may have been ingested. Flumazenil (Romazicon®)*, a specific benzodiazepine receptor antagonist, is indicated for the complete or partial reversal of the sedative effects of benzodiazepines and may be used in situations when an overdose with a benzodiazepine is known or suspected. Prior to the administration of flumazenil, necessary measures should be instituted to secure airway, ventilation, and intravenous access. Flumazenil is intended as an adjunct to, not as a substitute for, proper management of benzodiazepine overdose. Patients treated with flumazenil should be monitored for re-sedation, respiratory depression, and other residual benzodiazepine effects for an appropriate period after treatment. The prescriber should be aware of a risk of seizure in association with flumazenil treatment, particularly in long-term benzodiazepine users and in cyclic antidepressant overdose. The complete flumazenil package insert including CONTRAINDICATIONS, WARNINGS, and PRECAUTIONS should be consulted prior to use.
Up-to-date information about the treatment of overdose can often be obtained from a certified Regional Poison Control Center.
-
DOSAGE AND ADMINISTRATION
While the recommended usual adult dose is 15 mg before retiring, 7.5 mg may be sufficient for some patients, and others may need 30 mg. In transient insomnia, a 7.5 mg dose may be sufficient to improve sleep latency. In elderly or debilitated patients, it is recommended that therapy be initiated with 7.5 mg until individual responses are determined.
Discontinuation or Dosage Reduction of Temazepam Capsules
To reduce the risk of withdrawal reactions, use a gradual taper to discontinue temazepam capsules or reduce the dosage. If a
patient develops withdrawal reactions, consider pausing the taper or increasing the dosage to the previous tapered dosage level.
Subsequently decrease the dosage more slowly (see WARNINGS, Dependence and Withdrawal ReactionsandDRUG ABUSE
AND DEPENDENCE: Dependence). -
HOW SUPPLIED
Temazepam Capsules USP
7.5 mg
Pink opaque cap and white opaque body, imprinted “7.5 mg” on cap and “Novel 120” on the body in black ink.
Box of 3 x 10 UD 30 NDC 63739-003-33
Dispense in a well-closed, light-resistant container with a child-resistant closure.
Storage: Store at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature].Manufactured by:
Novel Laboratories, Inc.
Somerset, NJ 08873Distributed by:
McKesson Corporation dba SKY Packaging
Memphis, TN 38133
Rev. 04/2022
21359-1
-
MEDICATION GUIDE
MEDICATION GUIDE
TEMAZEPAM ( tem az’ e pam) Capsules, C-IVWhat is the most important information I should know about
temazepam?
• temazepam is a benzodiazepine medicine. Taking
benzodiazepines with opioid medicines, alcohol, or other central
nervous system (CNS) depressants (including street drugs) can
cause severe drowsiness, breathing problems (respiratory
depression), coma and death. Get emergency help right away if any
of the following happens:
° shallow or slowed breathing
° breathing stops (which may lead to the heart stopping)
° excessive sleepiness (sedation)Do not drive or operate heavy machinery until you know how taking
temazepam and opioids affects you.
° Risk of abuse, misuse, and addiction. There is a risk of abuse,
misuse, and addiction with benzodiazepines including temazepam
which can lead to overdose and serious side effects including
coma and death. Serious side effects including coma and death
have happened in people who have abused or misused
benzodiazepines, including temazepam. These serious side
effects may also include delirium, paranoia, suicidal thoughts or
actions, seizures, and difficulty breathing. Call your healthcare
provider or go to the nearest hospital emergency room right
away if you get any of these serious side effects.
° You can develop an addiction even if you take temazepam as
prescribed by your healthcare provider
° Take temazepam exactly as your healthcare provider
prescribed.
° Do not share your temazepam with other people.
° Keep temazepam in a safe place and away from children.• Physical dependence and withdrawal reactions. temazepam can
cause physical dependence and withdrawal reactions.
° Do not suddenly stop taking temazepam. Stopping temazepam
suddenly can cause serious and life-threatening side effects,
including, unusual movements, responses, or expressions,
seizures, sudden and severe mental or nervous system changes,
depression, seeing or hearing things that others do not see or hear,
an extreme increase in activity or talking, losing touch with reality,
and suicidal thoughts or actions. Call your healthcare provider or
go to the nearest hospital emergency room right away if you
get any of these symptoms.
° Some people who suddenly stop benzodiazepines have
symptoms that can last for several weeks to more than
12 months , including, anxiety, trouble remembering, learning, or
concentrating, depression, problems sleeping, feeling like insects
are crawling under your skin, weakness, shaking, muscle
twitching, burning or prickling feeling in your hands, arms, legs or
feet, and ringing in your ears.
° Physical dependence is not the same as drug addiction. Your
healthcare provider can tell you more about the differences
between physical dependence and drug addiction.
° Do not take more temazepam than prescribed or take temazepam
for longer than prescribed.• After taking temazepam, you may get up out of bed while not being
fully awake and do an activity that you do not know you are doing. The
next morning, you may not remember that you did anything during the
night. You have a higher chance for doing these activities if you drink
alcohol or take other medicines that make you sleepy with
temazepam. Reported activities include:
° driving a car (“sleep driving”)
° making and eating food
° talking on the phone
° having sex
° sleep-walking
Call your healthcare provider right away if you find out that you have
done any of the above activities after taking temazepam.What is temazepam?
• Temazepam is a prescription sleep medicine. Temazepam is used in
adults for the short-term (usually 7 to 10 days) treatment of a sleep
problem called insomnia. Symptoms of insomnia include trouble falling
asleep and waking up often during the night.
• Temazepam is a federal controlled substance (C-IV) because it
can be abused or lead to dependence. Keep temazepam in a safe
place to prevent misuse and abuse. Selling or giving away temazepam
may harm others, and is against the law. Tell your healthcare provider
if you have ever abused or been dependent on alcohol, prescription
medicines or street drugs.
• It is not known if temazepam is safe and effective in children.
• It is not known if temazepam is safe and effective for use longer than
2 weeksDo not take temazepam if you:
• are allergic to temazepam or any of the ingredients in temazepam
capsules. See the end of this Medication Guide for a complete list of
ingredients in temazepam capsules.Before you take temazepam, tell your healthcare provider about all of
your medical conditions, including if you:
• have a history of depression, mental illness or, suicidal thoughts
• have a history of drug or alcohol abuse or addiction
• have lung disease or breathing problems
• are pregnant or plan to become pregnant. Temazepam may cause birth
defects or harm your unborn baby.
• are breastfeeding, or plan to breastfeed. Temazepam may pass
through your breast milk and may harm your baby. Talk to your
healthcare provider about the best way to feed your baby if you take
temazepam.
Tell your healthcare provider about all of the medicines you take,
including prescription and over-the-counter medicines, vitamins, and
herbal supplements.Taking temazepam with certain other medicines can cause side effects or
affect how well temazepam or the other medicines work. Do not start or
stop other medicines without talking to your healthcare provider.
Do not take temazepam with other medicines that can make you sleepy
unless your healthcare provider tells you to.
How should I take temazepam?
• See “What is the most important information I should know about
temazepam?”
• Take temazepam exactly as your healthcare providers tell you to take
it. Take temazepam right before you get into bed.
• Do not take temazepam unless you are able to get a full night’s sleep
before you must be active again.
• If you take too much temazepam or overdose, get emergency
treatment right away.What are the possible side effects of temazepam?
Temazepam may cause serious side effects, including:
• See “What is the most important information I should know about
temazepam?”
• Abnormal thoughts and behavior. Symptoms include more outgoing
or aggressive behavior than normal, confusion, agitation,
hallucinations, worsening of depression, and suicidal thoughts.
• Severe allergic reactions. Symptoms include swelling of the tongue
or throat, trouble breathing, and nausea and vomiting. Get emergency
medical help right away if you have these symptoms after taking
temazepam.
Temazepam can make you sleepy or dizzy and can slow your thinking
and motor skills.
° Do not drive, operate heavy machinery, or do other dangerous
activities until you know how temazepam affects you.
° Do not drink alcohol or take other drugs that may make you
sleepy or dizzy while taking temazepam talking to your
healthcare provider . When taken with alcohol or other drugs that
cause sleepiness or dizziness, temazepam may make your
sleepiness or dizziness much worse.The most common side effects of temazepam include:
• drowsiness
• headache
• tiredness
• nervousness
• dizziness
• nausea
You may still feel drowsy the next day after taking temazepam. Do not
drive or do other dangerous activities after taking temazepam until
you feel fully awake.
These are not all the possible side effects of temazepam. Call your doctor
for medical advice about side effects. You may report side effects to FDA at
1-800-FDA-1088.How should I store temazepam?
• Store temazepam at room temperature between 68°F to 77°F (20°C to
25°C).
• Keep temazepam and all medicines out of the reach of children.
General information about the safe and effective use of temazepam.
Medicines are sometimes prescribed for purposes other than those listed
in a Medication Guide. Do not use temazepam for a condition for which it
was not prescribed. Do not give temazepam to other people, even if they
have the same symptoms that you have. It may harm them. You can ask
your healthcare provider or pharmacist for information about temazepam
that is written for healthcare professionals.What are the ingredients in temazepam?
7.5mg Capsules
Active Ingredient: temazepam USP
7.5 mg Capsules
Inactive Ingredients: Corn starch, lactose anhydrous, magnesium stearate,
sodium lauryl sulfate, FD&C Red #40 and titanium dioxide.
May also include: sodium lauryl sulfate. Imprinting ink may contain
ammonium hydroxide, ethanol, isopropyl alcohol, butanol, shellac,
potassium hydroxide, propylene glycol, and black iron oxide.
If you would like more information, call Novel Laboratories, Inc. at
1-866-403-7592
This Medication Guide has been approved by the U.S. Food and Drug
Administration
Manufactured by:
Novel Laboratories, Inc
Somerset, NJ 08873
Distributed by:
McKesson Corporation dba SKY Packaging
Memphis, TN 38141
Rev. 04/2022
21359-1
-
BOXED WARNING
(What is this?)
BOXED WARNING
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE,
AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
• Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma,
and death. Reserve concomitant prescribing of these drugs in patients for whom alternative treatment options are
inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of
respiratory depression and sedation (see WARNINGS and PRECAUTIONS).
• The use of benzodiazepines, including Temazepam, exposes users to risks of abuse, misuse, and addiction, which
can lead to overdose or death. Abuse and misuse of benzodiazepines commonly involve concomitant use of other
medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse
outcomes. Before prescribing Temazepam and throughout treatment, assess each patient’s risk for abuse, misuse,
and addiction (see WARNINGS).
• The continued use of benzodiazepines, including Temazepam, may lead to clinically significant physical
dependence. The risks of dependence and withdrawal increase with longer treatment duration and higher daily
dose. Abrupt discontinuation or rapid dosage reduction of Restoril after continued use may precipitate acute
withdrawal reactions, which can be life-threatening. To reduce the risk of withdrawal reactions, use a gradual
taper to discontinue Temazepam or reduce the dosage (see DOSAGE AND ADMINISTRATION and WARNINGS). - temazepam
-
INGREDIENTS AND APPEARANCE
TEMAZEPAM
temazepam capsuleProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:63739-003(NDC:67877-148) Route of Administration ORAL DEA Schedule CIV Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TEMAZEPAM (UNII: CHB1QD2QSS) (TEMAZEPAM - UNII:CHB1QD2QSS) TEMAZEPAM 7.5 mg Inactive Ingredients Ingredient Name Strength STARCH, CORN (UNII: O8232NY3SJ) ANHYDROUS LACTOSE (UNII: 3SY5LH9PMK) MAGNESIUM STEARATE (UNII: 70097M6I30) SODIUM LAURYL SULFATE (UNII: 368GB5141J) FD&C RED NO. 40 (UNII: WZB9127XOA) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) AMMONIA (UNII: 5138Q19F1X) ALCOHOL (UNII: 3K9958V90M) ISOPROPYL ALCOHOL (UNII: ND2M416302) BUTYL ALCOHOL (UNII: 8PJ61P6TS3) SHELLAC (UNII: 46N107B71O) POTASSIUM HYDROXIDE (UNII: WZH3C48M4T) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) FERROSOFERRIC OXIDE (UNII: XM0M87F357) Product Characteristics Color white (white opaque body) , pink (pink opaque cap) Score no score Shape CAPSULE Size 19mm Flavor Imprint Code 7;5mg;Novel120 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:63739-003-33 3 in 1 BOX, UNIT-DOSE 11/04/2015 1 10 in 1 BLISTER PACK; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA071457 06/28/2012 Labeler - McKesson Corporation dba SKY Packaging (140529962) Establishment Name Address ID/FEI Business Operations Legacy Pharmaceutical Packaging, LLC 143213275 repack(63739-003)