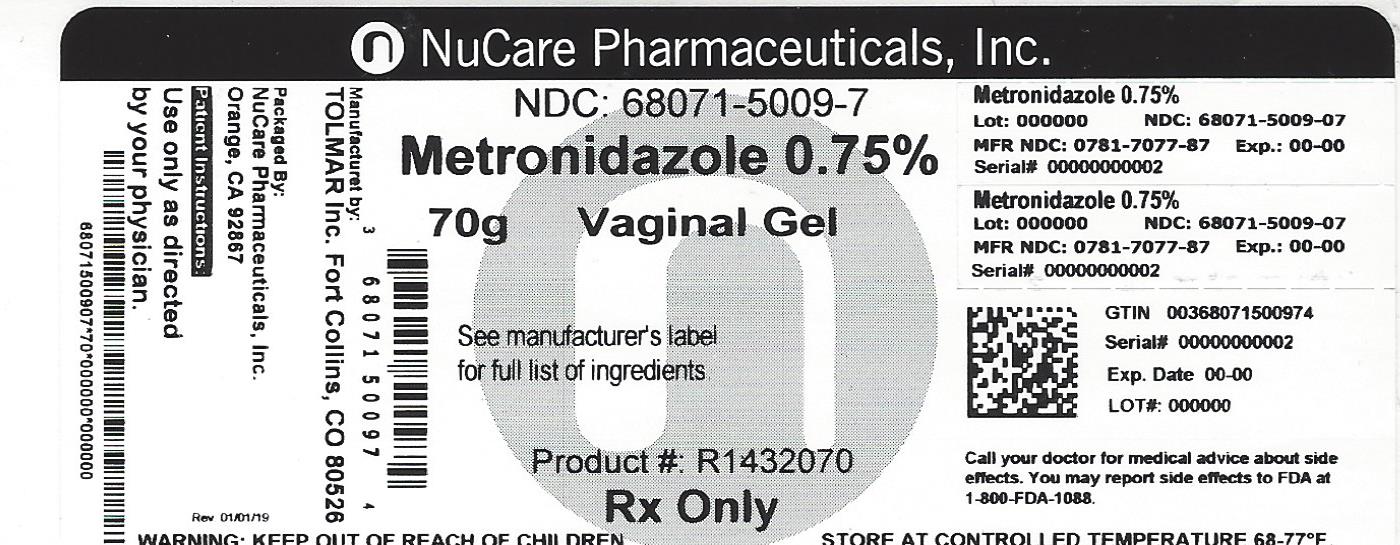
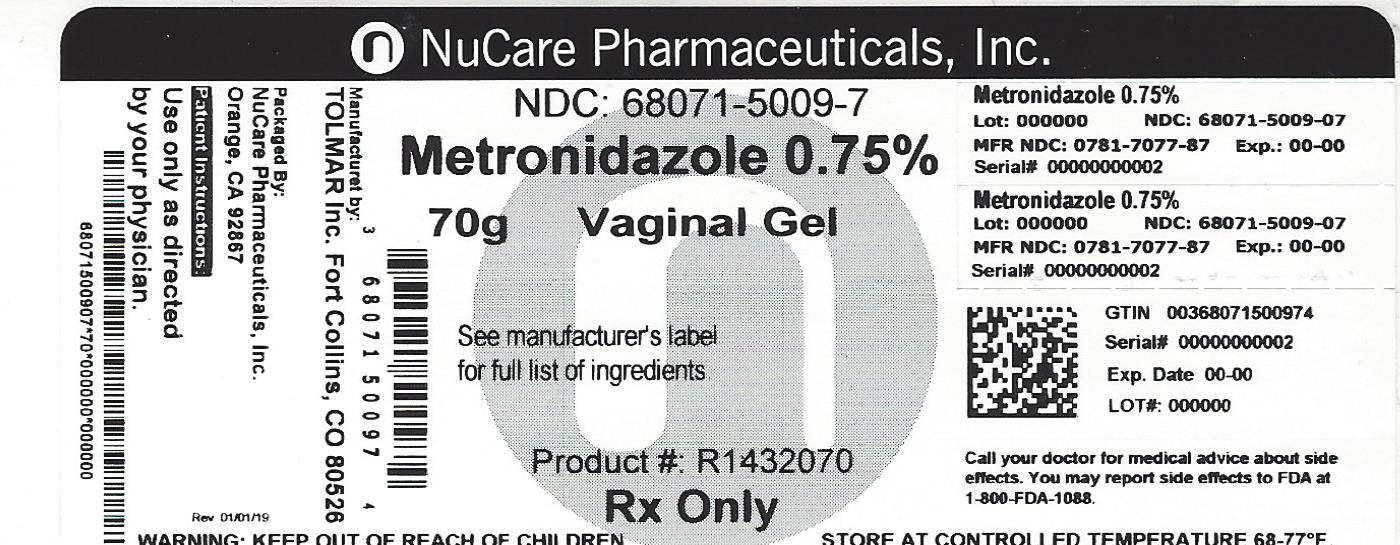
Label: METRONIDAZOLE gel
-
Contains inactivated NDC Code(s)
NDC Code(s): 68071-5009-7 - Packager: NuCare Pharmaceuticals,Inc.
- This is a repackaged label.
- Source NDC Code(s): 0781-7077
- Category: HUMAN PRESCRIPTION DRUG LABEL
Drug Label Information
Updated February 19, 2021
If you are a healthcare professional or from the pharmaceutical industry please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
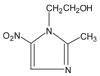
DESCRIPTION
Metronidazole vaginal gel USP, 0.75% is the intravaginal dosage form of the synthetic antibacterial agent, metronidazole, USP at a concentration of 0.75%. Metronidazole is a member of the imidazole class of antibacterial agents and is classified therapeutically as an antiprotozoal and antibacterial agent. Chemically, metronidazole is a 2-methyl-5-nitroimidazole-1-ethanol. It has a chemical formula of C 6H 9N 3O 3, a molecular weight of 171.16, and has the following structure:
Metronidazole vaginal gel USP, 0.75% is a gelled, purified water solution, containing metronidazole at a concentration of 7.5 mg/g (0.75%). The gel is formulated at pH 5.5. The gel also contains carbopol 974P, edetate disodium, methylparaben, propylene glycol, propylparaben and sodium hydroxide.
Each applicator full of 5 grams of vaginal gel contains approximately 37.5 mg of metronidazole.
-
CLINICAL PHARMACOLOGY
Normal Subjects:
Following a single, intravaginal 5 gram dose of metronidazole vaginal gel (equivalent to 37.5 mg of metronidazole) to 12 normal subjects, a mean maximum serum metronidazole concentration of 237 ng/mL was reported (range: 152 to 368 ng/mL). This is approximately 2% of the mean maximum serum metronidazole concentration reported in the same subjects administered a single, oral 500 mg dose of metronidazole (mean C max = 12,785 ng/mL, range: 10,013 to 17,400 ng/mL). These peak concentrations were obtained in 6 to 12 hours after dosing with metronidazole vaginal gel and 1 to 3 hours after dosing with oral metronidazole.
The extent of exposure [area under the curve (AUC)] of metronidazole, when administered as a single intravaginal 5 gram dose of metronidazole vaginal gel (equivalent to 37.5 mg of metronidazole), was approximately 4% of the AUC of a single oral 500 mg dose of metronidazole (4977 ng-hr/mL and approximately 125,000 ng-hr/mL, respectively).
Dose-adjusted comparisons of AUCs demonstrated that, on a mg to mg comparison basis, the absorption of metronidazole, when administered vaginally, was approximately half that of an equivalent oral dosage.
Patients with Bacterial Vaginosis:
Following single and multiple 5 gram doses of metronidazole vaginal gel to 4 patients with bacterial vaginosis, a mean maximum serum metronidazole concentration of 214 ng/mL on day one and 294 ng/mL (range: 228 to 349 ng/mL) on day five were reported. Steady state metronidazole serum concentrations following oral dosages of 400 to 500 mg BID have been reported to range from 6,000 to 20,000 ng/mL.
MICROBIOLOGY
The intracellular targets of action of metronidazole on anaerobes are largely unknown. The 5-nitro group of metronidazole is reduced by metabolically active anaerobes, and studies have demonstrated that the reduced form of the drug interacts with bacterial DNA. However, it is not clear whether interaction with DNA alone is an important component in the bactericidal action of metronidazole on anaerobic organisms.
Culture and sensitivity testing of bacteria are not routinely performed to establish the diagnosis of bacterial vaginosis. (See INDICATIONS AND USAGE.)
Standard methodology for the susceptibility testing of the potential bacterial vaginosis pathogens, Gardnerella vaginalis, Mobiluncus spp., and Mycoplasma hominis, has not been defined. Nonetheless, metronidazole is an antimicrobial agent active in vitro against most strains of the following organisms that have been reported to be associated with bacterial vaginosis:
-
Bacteroides spp.
-
Gardnerella vaginalis
-
Mobiluncus spp.
-
Peptostreptococcus spp.
-
-
INDICATIONS & USAGE
Metronidazole vaginal gel USP, 0.75% is indicated in the treatment of bacterial vaginosis (formerly referred to as Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis).
-
NOTE: For purposes of this indication, a clinical diagnosis of bacterial vaginosis is usually defined by the presence of a homogeneous vaginal discharge that (a) has a pH of greater than 4.5, (b) emits a “fishy” amine odor when mixed with a 10% KOH solution, and (c) contains clue cells on microscopic examination. Gram’s stain results consistent with a diagnosis of bacterial vaginosis include (a) markedly reduced or absent Lactobacillus morphology, (b) predominance of Gardnerella morphotype, and (c) absent or few white blood cells.
Other pathogens commonly associated with vulvovaginitis, e.g., Trichomonas vaginalis, Chlamydia trachomatis, N. gonorrhoeae, Candida albicans, and Herpes simplex virus should be ruled out.
-
- CONTRAINDICATIONS
-
WARNINGS
Convulsive Seizures and Peripheral Neuropathy:
Convulsive seizures and peripheral neuropathy, the latter characterized mainly by numbness or paresthesia of an extremity, have been reported in patients treated with oral or intravenous metronidazole. The appearance of abnormal neurologic signs demands the prompt discontinuation of metronidazole vaginal gel therapy. Metronidazole vaginal gel should be administered with caution to patients with central nervous system diseases.
Psychotic Reactions:
Psychotic reactions have been reported in alcoholic patients who were using oral metronidazole and disulfiram concurrently. Metronidazole vaginal gel should not be administered to patients who have taken disulfiram within the last two weeks.
-
PRECAUTIONS
Metronidazole vaginal gel USP, 0.75% affords minimal peak serum levels and systemic exposure (AUCs) of metronidazole compared to 500 mg oral metronidazole dosing. Although these lower levels of exposure are less likely to produce the common reactions seen with oral metronidazole, the possibility of these and other reactions cannot be excluded presently. Data from well-controlled trials directly comparing metronidazole administered orally to metronidazole administered vaginally are not available.
General:
Patients with severe hepatic disease metabolize metronidazole slowly. This results in the accumulation of metronidazole and its metabolites in the plasma. Accordingly, for such patients, metronidazole vaginal gel should be administered cautiously.
Known or previously unrecognized vaginal candidiasis may present more prominent symptoms during therapy with metronidazole vaginal gel. Approximately 6-10% of patients treated with metronidazole vaginal gel USP, 0.75% developed symptomatic Candida vaginitis during or immediately after therapy.
Disulfiram-like reaction to alcohol has been reported with oral metronidazole, thus the possibility of such a reaction occurring while on metronidazole vaginal gel therapy cannot be excluded.
Metronidazole vaginal gel USP, 0.75% contains ingredients that may cause burning and irritation of the eye. In the event of accidental contact with the eye, rinse the eye with copious amounts of cool tap water.
INFORMATION FOR PATIENTS
The patient should be cautioned about drinking alcohol while being treated with metronidazole vaginal gel. While blood levels are significantly lower with metronidazole vaginal gel USP, 0.75% than with usual doses of oral metronidazole, a possible interaction with alcohol cannot be excluded.
The patient should be instructed not to engage in vaginal intercourse during treatment with this product.
DRUG INTERACTIONS
Oral metronidazole has been reported to potentiate the anticoagulant effect of warfarin and other coumarin anticoagulants, resulting in a prolongation of prothrombin time. This possible drug interaction should be considered when metronidazole vaginal gel is prescribed for patients on this type of anticoagulant therapy.
In patients stabilized on relatively high doses of lithium, short-term oral metronidazole therapy has been associated with elevation of serum lithium levels and, in a few cases, signs of lithium toxicity.
Use of cimetidine with oral metronidazole may prolong the half-life and decrease plasma clearance of metronidazole.
DRUG & OR LABORATORY TEST INTERACTIONS
Metronidazole may interfere with certain types of determinations of serum chemistry values, such as aspartate aminotransferase (AST, SGOT), alanine aminotransferase (ALT, SGPT), lactate dehydrogenase (LDH), triglycerides, and glucose hexokinase. Values of zero may be observed. All of the assays in which interference has been reported involve enzymatic coupling of the assay to oxidation-reduction of nicotinamide-adenine dinucleotides (NAD + NADH). Interference is due to the similarity in absorbance peaks of NADH (340 nm) and metronidazole (322 nm) at pH 7.
CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
Metronidazole has shown evidence of carcinogenic activity in a number of studies involving chronic oral administration in mice and rats. Prominent among the effects in the mouse was the promotion of pulmonary tumorigenesis. This has been observed in all six reported studies in that species, including one study in which the animals were dosed on an intermittent schedule (administration during every fourth week only). At very high dose levels (approximately 500 mg/kg/day), there was a statistically significant increase in the incidence of malignant liver tumors in males. Also, the published results of one of the mouse studies indicate an increase in the incidence of malignant lymphomas as well as pulmonary neoplasms associated with lifetime feeding of the drug. All these effects are statistically significant. Several long-term oral dosing studies in the rat have been completed. There were statistically significant increases in the incidence of various neoplasms, particularly in mammary and hepatic tumors, among female rats administered metronidazole over those noted in the concurrent female control groups. Two lifetime tumorigenicity studies in hamsters have been performed and reported to be negative.
These studies have not been conducted with 0.75% metronidazole vaginal gel, which would result in significantly lower systemic blood levels than those obtained with oral formulations.
Although metronidazole has shown mutagenic activity in a number of in vitro assay systems, studies in mammals ( in vivo) have failed to demonstrate a potential for genetic damage.
Fertility studies have been performed in mice up to six times the recommended human oral dose (based on mg/m 2) and have revealed no evidence of impaired fertility.
PREGNANCY
Teratogenic Effects:
Pregnancy Category B
There has been no experience to date with the use of metronidazole vaginal gel USP, 0.75% in pregnant patients. Metronidazole crosses the placental barrier and enters the fetal circulation rapidly. No fetotoxicity or teratogenicity was observed when metronidazole was administered orally to pregnant mice at six times the recommended human dose (based on mg/m 2); however, in a single small study where the drug was administered intraperitoneally, some intrauterine deaths were observed. The relationship of these findings to the drug is unknown.
There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, and because metronidazole is a carcinogen in rodents, this drug should be used during pregnancy only if clearly needed.
NURSING MOTHERS
Specific studies of metronidazole levels in human milk following intravaginally administered metronidazole have not been performed. However, metronidazole is secreted in human milk in concentrations similar to those found in plasma following oral administration of metronidazole.
Because of the potential for tumorigenicity shown for metronidazole in mouse and rat studies, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
-
ADVERSE REACTIONS
Clinical Trials
There were no deaths or serious adverse events related to drug therapy in clinical trials involving 800 non-pregnant women who received metronidazole vaginal gel USP, 0.75%.
In a randomized, single-blind clinical trial of 505 non-pregnant women who received metronidazole vaginal gel USP, 0.75% once or twice a day, 2 patients (one from each regimen) discontinued therapy early due to drug-related adverse events. One patient discontinued drug because of moderate abdominal cramping and loose stools, while the other patient discontinued drug because of mild vaginal burning. These symptoms resolved after discontinuation of drug.
Medical events judged to be related, probably related, or possibly related to administration of metronidazole vaginal gel USP, 0.75% once or twice a day were reported for 195/505 (39%) patients. The incidence of individual adverse reactions were not significantly different between the two regimens. Unless percentages are otherwise stipulated, the incidence of individual adverse reactions listed below was less than 1%:
Reproductive:
-
Vaginal discharge (12%),
-
Symptomatic Candida cervicitis/vaginitis (10%),
-
Vulva/vaginal irritative symptoms (9%),
-
Pelvic discomfort (3%).
Gastrointestinal:
-
Gastrointestinal discomfort (7%),
-
Nausea and/or vomiting (4%),
-
Unusual taste (2%),
-
Diarrhea/loose stools (1%),
-
Decreased appetite (1%),
-
Abdominal bloating/gas; thirsty, dry mouth.
Neurologic:
-
Headache (5%),
-
Dizziness (2%),
-
Depression.
Dermatologic:
-
Generalized itching or rash.
Other:
-
Unspecified cramping (1%),
-
Fatigue,
-
Darkened urine.
In previous clinical trials submitted for approved labeling of metronidazole vaginal gel USP, 0.75% the following was also reported:
Laboratory:
-
Increased/decreased white blood cell counts (1.7%).
Other Metronidazole Formulations:
Other effects that have been reported in association with the use of topical (dermal) formulations of metronidazole include skin irritation, transient skin erythema, and mild skin dryness and burning. None of these adverse events exceeded an incidence of 2% of patients.
Metronidazole vaginal gel USP, 0.75% affords minimal peak serum levels and systemic exposure (AUC) of metronidazole compared to 500 mg oral metronidazole dosing. Although these lower levels of exposure are less likely to produce the common reactions seen with oral metronidazole, the possibility of these and other reactions cannot be excluded presently.
The following adverse reactions and altered laboratory tests have been reported with the oral or parenteral use of metronidazole:
-
Cardiovascular: Flattening of the T-wave may be seen in electrocardiographic tracings.
-
Central Nervous System: (See WARNINGS.) Headache, dizziness, syncope, ataxia, confusion, convulsive seizures, peripheral neuropathy, vertigo, incoordination, irritability, depression, weakness, insomnia.
-
Gastrointestinal: Abdominal discomfort, nausea, vomiting, diarrhea, an unpleasant metallic taste, anorexia, epigastric distress, abdominal cramping, constipation, “furry” tongue, glossitis, stomatitis, pancreatitis, and modification of taste of alcoholic beverages.
-
Genitourinary: Overgrowth of Candida in the vagina, dyspareunia, decreased libido, proctitis.
-
Hematopoietic: Reversible neutropenia, reversible thrombocytopenia.
-
Hypersensitivity Reactions: Urticaria; erythematous rash; flushing; nasal congestion; dryness of the mouth, vagina, or vulva; fever; pruritus; fleeting joint pains.
-
Renal: Dysuria, cystitis, polyuria, incontinence, a sense of pelvic pressure, darkened urine.
-
- OVERDOSAGE
- DOSAGE & ADMINISTRATION
- HOW SUPPLIED
-
CLINICAL STUDIES
In a randomized, single-blind clinical trial of non-pregnant women with bacterial vaginosis who received metronidazole vaginal gel USP, 0.75% daily for 5 days, the clinical cure rates for evaluable patients determined at 4 weeks after completion of therapy for the QD and BID regimens were 98/185 (53%) and 109/190 (57%), respectively.
Manufactured by
TOLMAR Inc.
Fort Collins, CO 80526 for
Sandoz Inc.
Princeton, NJ 0854004486 Rev. 6 11/16
-
SPL PATIENT PACKAGE INSERT
Metronidazole Vaginal Gel USP, 0.75%
DIRECTIONS FOR USE
1. Filling the applicator
- Remove cap and puncture metal seal on tube with the pointed tip of cap. (See Figure 1)
- Screw end of applicator onto tube. (See Figure 2)
- Gently squeeze the tube from the bottom to fill applicator. Plunger will stop when the applicator is full. (See Figure 3)
- Unscrew applicator and replace cap on tube.

Figure 1 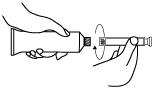
Figure 2 Figure 3 2. Inserting the applicator
- The applicator may be inserted while lying on your back with your knees bent or in any comfortable position.
- Hold filled applicator by barrel, and gently insert into vagina as far as it will comfortably go. (See Figure 4)
- Slowly press the plunger until it stops to deposit gel into vagina and then withdraw the applicator.
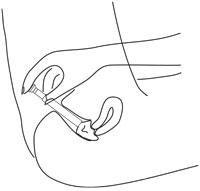
Figure 4
3. Care of the applicator
If physician prescribes twice-a-day dosing:
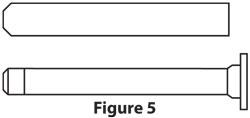
- After use, pull the plunger out of the barrel. (See Figure 5)
- Wash both plunger and barrel in warm soapy water and rinse thoroughly.
- To reassemble applicator, gently push plunger back into barrel.
IMPORTANT:
For once-a-day dosing, apply one applicator full at bedtime. For twice-a-day dosing, apply one applicator full each morning and evening for five days, or as directed by physician.
WARNINGS:
- If significant irritation develops from the use of this medication, discontinue use and consult your physician.
- Do not use during pregnancy except under the supervision of a physician.
- Keep this and all medications out of reach of children.
- For vaginal use only. Not for use in the eyes, on the skin or in the mouth.
Store at room temperature. Avoid exposure to extreme heat or cold. See end of carton and crimp end of tube for lot number and expiration date.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Manufactured by
TOLMAR Inc.
Fort Collins, CO 80526 for
Sandoz Inc.
Princeton, NJ 0854004486 Rev. 6 11/16
Metronidazole Vaginal Gel USP, 0.75%
INSTRUCCIONES PARA EL USO
1. Como llenar el aplicador
- Quite la tapa y con la punta de la misma perfore el sello metálico del tubo. (Véase Ilustración 1)
- Enrosque el extremo del aplicador en el tubo. (Véase Ilustración 2)
- Exprima el tubo suavemente desde abajo para llenar el aplicador. Cuando el aplicador esté lleno, el émbolo dejará de moverse. (Véase Ilustración 3)
- Desenrosque el aplicador y reponga la tapa en el tubo.
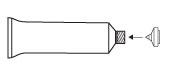
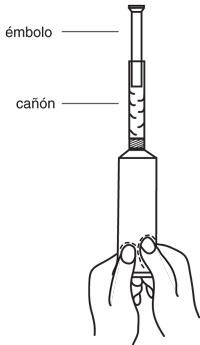
Ilustración 1 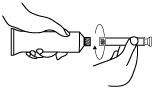
Ilustración 2 Ilustración 3 2. Como introducir el aplicador
- El aplicador puede introducirse estando acostada boca arriba con las rodillas dobladas, o en cualquier posición en que se sienta cómoda.
- Sostenga el aplicador lleno por su cañón, e introduzcalo suave y profundamente en la vagina de manera cómoda. (Véase Ilustración 4)
- Para depositar la gelatina dentro de la vagina, suavemente empuje el émbolo hasta que deje de moverse y entonces saque el aplicador.
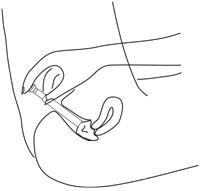
Ilustración 4
3. Como limpiar el aplicador
Si la prescripción médica indica una dosis de dos veces al día:
- Después de usar el aplicador, saque el émbolo del cañón. (Véase Ilustración 5)
- Lave el émbolo y el cañón con agua tibia y jabón y luego enjuaguelos completamente.
- Para volver a armar el aplicador, suavemente empuje el émbolo en su sitio dentro del cañón.
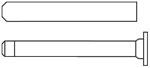
Ilustración 5
IMPORTANTE:
Para dosis de una vez al día, introduzca un aplicador lleno por la noche. Para dosis de dos veces al día, introduzca un aplicador lleno cada mañana y cada noche durante cinco días, o según las indicaciones de su médico.
ADVERTENCIAS:
- Si una irritación significante se desarrolla debida al uso de este medicamento, deje de usarlo y consulte a su médico.
- No lo utilice cuando esté embarazada, excepto bajo la supervisión de un médico.
- Mantenga éste y todo medicamento fuera del alcance de los niños.
- Para uso vaginal únicamente. No debe aplicarse a los ojos, en la piel, ni en la boca.
Guarde a una temperatura ambiente. Evite que se exponga al calor o frío excesivo. Vea la feche de vencimiento y el número del lote en la base del cartón y en el sello del tubo.
Llame a su doctor para opinión médica sobre efectos secundarios. Usted puede reportar los efectos secundarios a la FDA al 1-800-FDA-1088.
Manufactured by
TOLMAR Inc.
Fort Collins, CO 80526 for
Sandoz Inc.
Princeton, NJ 0854004486 Rev. 6 11/16
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
METRONIDAZOLE
metronidazole gelProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68071-5009(NDC:0781-7077) Route of Administration VAGINAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength METRONIDAZOLE (UNII: 140QMO216E) (METRONIDAZOLE - UNII:140QMO216E) METRONIDAZOLE 7.5 mg in 1 g Inactive Ingredients Ingredient Name Strength CARBOMER HOMOPOLYMER TYPE B (ALLYL PENTAERYTHRITOL CROSSLINKED) (UNII: HHT01ZNK31) METHYLPARABEN (UNII: A2I8C7HI9T) PROPYLPARABEN (UNII: Z8IX2SC1OH) EDETATE DISODIUM (UNII: 7FLD91C86K) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) SODIUM HYDROXIDE (UNII: 55X04QC32I) WATER (UNII: 059QF0KO0R) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68071-5009-7 70 g in 1 BOX; Type 0: Not a Combination Product 07/31/2019 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA077264 10/31/2006 Labeler - NuCare Pharmaceuticals,Inc. (010632300) Establishment Name Address ID/FEI Business Operations NuCare Pharmaceuticals,Inc. 010632300 relabel(68071-5009)