AFLURIA- influenza a virus a/singapore/gp1908/2015 ivr-180a (h1n1) antigen (propiolactone inactivated), influenza a virus a/singapore/infimh-16-0019/2016 ivr-186 (h3n2) antigen (propiolactone inactivated) and influenza b virus b/maryland/15/2016 antigen (propiolactone inactivated) injection, suspension
Seqirus Pty Ltd
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use AFLURIA safely and effectively. See full prescribing information for AFLURIA.
AFLURIA, Influenza Vaccine Suspension for Intramuscular Injection 2018-2019 Season Initial U.S. Approval: 2007 INDICATIONS AND USAGEDOSAGE AND ADMINISTRATIONFor intramuscular (IM) injection only, by needle and syringe (5 years of age and older) or by PharmaJet® Stratis® Needle-Free Injection System (18 through 64 years of age). A single dose is 0.5 mL. (2)
DOSAGE FORMS AND STRENGTHSCONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact Seqirus at 1 855 358 8966 or VAERS at 1-800-822-7967 or www.vaers.hhs.gov. USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION. Revised: 4/2018 |
|||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
AFLURIA® is an inactivated influenza vaccine indicated for active immunization against influenza disease caused by influenza virus subtypes A and type B present in the vaccine. AFLURIA is approved for use in persons 5 years of age and older.
2 DOSAGE AND ADMINISTRATION
For intramuscular (IM) injection only, by needle and syringe (5 years of age and older) or by PharmaJet® Stratis® Needle-Free Injection System (18 through 64 years of age). A single dose is 0.5 mL.
The dose and schedule for AFLURIA are presented in Table 1.
| Age | Schedule |
|---|---|
|
|
| 5 years through 8 years | One dose or two doses at least 1 month apart * |
| 9 years and older | One dose |
Shake thoroughly and inspect visually before use. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever suspension and container permit. If either of these conditions exists, the vaccine should not be administered.
May be administered by needle and syringe (5 years of age and older) or PharmaJet Stratis Needle-Free Injection System (18 through 64 years of age only).
When using the single-dose pre-filled syringe, shake the syringe thoroughly and administer the dose immediately.
When using the multi-dose vial, shake the vial thoroughly before withdrawing each dose, and administer the dose immediately.
- Needle and Syringe: Draw up the exact dose using a separate sterile needle and syringe for each individual patient. It is recommended that small syringes (0.5 mL or 1 mL) be used to minimize any product loss.
- PharmaJet Stratis Needle-Free Injection System: For instructions on withdrawal of a 0.5 mL dose and use of the PharmaJet Stratis Needle-Free Injection System, refer to the Instructions For Use for the PharmaJet Stratis Needle-Free Injection System.
The preferred site for intramuscular injection is the deltoid muscle of the upper arm.
Between uses, return the multi-dose vial to the recommended storage conditions between 2-8°C (36–46°F). Do not freeze. Discard if the vaccine has been frozen.
3 DOSAGE FORMS AND STRENGTHS
AFLURIA is a sterile suspension for intramuscular injection (see Description [11]).
AFLURIA is supplied in two presentations:
- 0.5 mL pre-filled syringe (single dose).
- 5 mL multi-dose vial (ten 0.5 mL doses).
4 CONTRAINDICATIONS
AFLURIA is contraindicated in individuals with known severe allergic reactions (e.g., anaphylaxis) to any component of the vaccine including egg protein, or to a previous dose of any influenza vaccine (see Description [11]).
5 WARNINGS AND PRECAUTIONS
5.1 Fever and Febrile Seizures
Administration of CSL's 2010 Southern Hemisphere influenza vaccine was associated with postmarketing reports of increased rates of fever and febrile seizures in children predominantly below the age of 5 years as compared to previous years; these increased rates were confirmed by postmarketing studies. Febrile events were also observed in children 5 through 8 years of age.
5.2 Guillain-Barré Syndrome
If Guillain-Barré Syndrome (GBS) has occurred within 6 weeks of previous influenza vaccination, the decision to give AFLURIA should be based on careful consideration of the potential benefits and risks.
The 1976 swine influenza vaccine was associated with an increased frequency of GBS. Evidence for a causal relation of GBS with subsequent vaccines prepared from other influenza viruses is unclear. If influenza vaccine does pose a risk, it is probably slightly more than one additional case per 1 million persons vaccinated.
5.3 Preventing and Managing Allergic Reactions
Appropriate medical treatment and supervision must be available to manage possible anaphylactic reactions following administration of the vaccine.
6 ADVERSE REACTIONS
In children 5 through 17 years of age, the most common injection-site reactions observed in clinical studies with AFLURIA administered by needle and syringe were pain (≥60%), redness (≥20%) and swelling (≥10%). The most common systemic adverse events were headache, myalgia (≥20%), irritability, malaise and fever (≥10%).
In adults 18 through 64 years of age, the most common injection-site adverse reactions observed in clinical studies with AFLURIA administered by needle and syringe were tenderness (≥60%), pain (≥40%), swelling (≥20%), redness and itching (≥10%). The most common systemic adverse events observed were muscle aches (≥30%), headache and malaise (≥20%).
In adults 18 through 64 years of age, using the PharmaJet Stratis Needle-Free Injection System, the most common injection-site adverse reactions observed in a clinical study with AFLURIA up to 7 days post-vaccination were tenderness (≥80%), swelling, pain, redness (≥60%), itching (≥20%) and bruising (≥10%). The most common systemic adverse events within this period were myalgia, malaise (≥30%) and headache (≥20%).
In adults 65 years of age and older, the most common injection-site adverse reactions observed in clinical studies with AFLURIA administered by needle and syringe were tenderness (≥30%) and pain (≥10%). No systemic adverse reactions occurred in ≥10% of subjects in this age group.
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a vaccine cannot be directly compared to rates in the clinical studies of another vaccine and may not reflect the rates observed in clinical practice.
Children
In clinical studies, AFLURIA has been administered to, and safety information collected for, 3,009 children ages 6 months through 17 years. The exposure in children includes 1,601 aged 6 months to less than 5 years, 756 children ages 5 years to less than 9 years and 652 children ages 9 years through 17 years. Clinical safety data for AFLURIA in children are presented from three clinical studies (Studies 1, 2 and 3). Data from a comparator-controlled trial (Study 1) are presented, followed by pooled data from two open label studies (Studies 2 and 3). Subjects 6 months through 8 years of age received one or two vaccinations, administered by needle and syringe, as determined by previous vaccination history (for further details on clinical study design, dosing and demographics see Clinical Studies [14]).
Study 1 included 1,468 subjects for safety analysis, ages 6 months through 17 years, randomized to receive AFLURIA (735 subjects) or another U.S.-licensed trivalent inactivated influenza vaccine (manufactured by Sanofi Pasteur, Inc.) (733 subjects).
Study 2 included 1,976 subjects for safety analysis, ages 6 months through 17 years. All subjects received AFLURIA.
Study 3 included 298 subjects for safety analysis, ages 6 months through 8 years. All subjects received AFLURIA.
The safety assessment was similar for the three pediatric studies. Local (injection site) adverse reactions and systemic adverse events were solicited for 7 days post-vaccination (Tables 2 and 3). Unsolicited adverse events were collected for 30 days post-vaccination. All adverse events are presented regardless of any treatment causality assigned by study investigators.
Among the pediatric studies, there were no vaccine-related deaths or vaccine-related serious adverse events reported in children 5 years of age and older.
In this section, safety data from the pediatric studies are limited to children 5 years of age and older. AFLURIA is not approved for use in children less than 5 years of age. See Warnings and Precautions [5.1] and Use in Specific Populations [8.4] for risks of AFLURIA in children less than 5 years of age.
In the comparator-controlled trial (Study 1), the rate of fever after the first dose of AFLURIA in subjects aged 5 through 8 years was 16% as compared to 8% in subjects who received the comparator. The rate of fever in subjects aged 9 through 17 years following a single dose of AFLURIA was 6% as compared to 4% in subjects who received the comparator. In all three pediatric studies, the rates of fever in subjects aged 5 through 8 years who received AFLURIA were lower after dose 2 than dose 1.
Data in Tables 2 and 3 are presented for children 5 years and older.
| Percentage * of Subjects in each Age Group Reporting Event | ||||
|---|---|---|---|---|
| Subjects 5 through 8 years | Subjects 9 through 17 years | |||
| AFLURIA N=161 † | Comparator N=165 † | AFLURIA N=254 † | Comparator N=250 † |
|
|
||||
| After the First Dose | ||||
| Local Adverse Reactions | ||||
| Pain | 63 | 60 | 66 | 60 |
| Redness | 23 | 27 | 17 | 17 |
| Induration | 17 | 17 | 15 | 16 |
| Systemic Adverse Events | ||||
| Myalgia | 34 | 30 | 40 | 37 |
| Malaise | 24 | 13 | 22 | 20 |
| Headache | 21 | 19 | 27 | 26 |
| Any Fever | 16 | 8 | 6 | 4 |
| Fever ≥102.2°F | 5 | 1 | 3 | 1 |
| Nausea/Vomiting | 12 | 8 | 9 | 10 |
| Diarrhea | 7 | 7 | 8 | 10 |
| AFLURIA N=39 † | Comparator N=53 † | |||
| After the Second Dose | ||||
| Local Adverse Reactions | ||||
| Pain | 36 | 38 | - | - |
| Redness | 10 | 19 | - | - |
| Induration | 8 | 17 | - | - |
| Systemic Adverse Events | ||||
| Diarrhea | 13 | 6 | - | - |
| Headache | 13 | 13 | - | - |
| Myalgia | 13 | 17 | - | - |
| Malaise | 5 | 8 | - | - |
| Nausea/Vomiting | 3 | 8 | - | - |
| Any Fever Fever ≥102.2°F | 0 0 | 2 0 | - - | - - |
| Percentage * of Subjects in each Age Group Reporting Event | |||
|---|---|---|---|
| Studies 2 and 3 Subjects 5 through 8 years | Study 2 Subjects 9 through 17 years |
||
| Dose 1 N=82-595 † | Dose 2 N=82-426 † | Dose 1 N=397 † |
|
|
|||
| Local Adverse Reactions | |||
| Pain | 61 | 56 | 68 |
| Erythema | 24 | 23 | 17 |
| Swelling | 17 | 17 | 13 |
| Systemic Adverse Events | |||
| Irritability ‡ | 18 | 16 | - |
| Headache | 16 | 10 | 27 |
| Malaise or feeling generally unwell § | 16 | 8 | 17 |
| Any Fever | 13 | 6 | 5 |
| Fever ≥ 102.2°F | 3 | 2 | 1 |
| General Muscle Ache (Myalgia) | 12 | 8 | 20 |
| Nausea/Vomiting § | 7 | 3 | 5 |
| Vomiting/Diarrhea ‡ | 5 | 6 | - |
| Loss of appetite ‡ | 5 | 4 | - |
| Diarrhea § | 4 | 2 | 5 |
In Study 1, unsolicited adverse events that occurred in ≥ 5% of subjects who received AFLURIA in ages 5 years through 8 years following the first or second dose included cough (15%) and pyrexia (9%). Unsolicited adverse events that occurred in ≥ 5% of subjects who received AFLURIA in ages 9 years through 17 years following the first dose included cough (7%), oropharyngeal pain (7%), headache (7%) and nasal congestion (6%).
In Studies 2 and 3, unsolicited adverse events that occurred in ≥ 5% of subjects ages 5 years through 8 years after the first or second dose included the following: upper respiratory tract infection (13%), cough (10%), rhinorrhea (7%), headache (5%), nasopharyngitis (5%) and pyrexia (5%). Unsolicited adverse events that occurred in ≥ 5% of subjects who received AFLURIA in ages 9 years through 17 years following the first dose included upper respiratory tract infection (9%) and headache (8%).
Adults
In clinical studies comparing AFLURIA to placebo or a comparator trivalent inactivated influenza vaccine, a single dose of AFLURIA was administered to, and safety information collected for, 11,104 subjects ages 18 through 64 years and 836 subjects ages 65 years and older. Clinical safety data for AFLURIA in adults are presented from three clinical studies (Studies 4 through 6) conducted in the US and one clinical study (Study 7) conducted in the UK
Study 4 included 1,357 subjects for safety analysis, ages 18 through 64 years, randomized to receive AFLURIA (1,089 subjects) or placebo (268 subjects) (see Clinical Studies [14]).
Study 5 included 15,020 subjects for safety analysis, ages 18 through 64 years, randomized to receive AFLURIA (10,015 subjects) or placebo (5,005 subjects) (see Clinical Studies [14]).
Study 6 included 1,266 subjects for safety analysis, ages 65 years and older, randomized to receive AFLURIA (630 subjects) or another U.S.-licensed trivalent inactivated influenza vaccine (manufactured by Sanofi Pasteur Inc.) as an active comparator (636 subjects) (see Clinical Studies [14]). Study 7 included 275 subjects for safety analysis, ages 65 years and older, randomized to receive AFLURIA (206 subjects) or a UK-licensed trivalent inactivated influenza vaccine (manufactured by GSK) as an active comparator (69 subjects).
The safety assessment was identical for the four adult studies. Local (injection-site) adverse reactions and systemic adverse events were solicited for 5 days post-vaccination (Table 4, studies 4 through 6). Unsolicited adverse events were collected for 21 days post-vaccination. All adverse events are presented regardless of any treatment causality assigned by study investigators.
Among adult studies, there were no vaccine-related deaths or vaccine-related serious adverse events reported.
| Percentage * of Subjects in each Age Group Reporting Event | ||||||
|---|---|---|---|---|---|---|
| Study 4 Subjects 18 through 64 years | Study 5 Subjects 18 through 64 years | Study 6 Subjects ≥ 65 years |
||||
| AFLURIA N=1087-1088 † | Placebo N=266 † | AFLURIA N=10,015 † | Placebo N=5005 † | AFLURIA N=630 † | Comparator N=636 † |
|
|
||||||
| Local Adverse Reactions | ||||||
| Tenderness (Pain on touching) | 60 | 18 | 69 | 17 | 36 | 31 |
| Pain (without touching) | 40 | 9 | 48 | 11 | 15 | 14 |
| Redness | 16 | 8 | 4 | <1 | 3 | 1 |
| Swelling | 9 | 1 | 4 | <1 | 7 | 8 |
| Bruising | 5 | 1 | 1 | 1 | <1 | 1 |
| Systemic Adverse Events | ||||||
| Headache | 26 | 26 | 25 | 23 | 9 | 11 |
| Malaise | 19 | 19 | 29 | 26 | 7 | 6 |
| Muscle aches | 13 | 9 | 21 | 12 | 9 | 8 |
| Nausea | 6 | 9 | 7 | 6 | 2 | 1 |
| Chills/Shivering | 3 | 2 | 5 | 4 | 2 | 2 |
| Fever | 1 | 1 | 3 | 2 | <1 | 1 |
In Study 4, headache was the only unsolicited adverse event that occurred in ≥ 5% of subjects who received AFLURIA or placebo (8% versus 6%, respectively).
In Study 5, unsolicited adverse events that occurred in ≥ 5% of subjects who received AFLURIA or placebo included headache (AFLURIA 12%, placebo 11%) and oropharyngeal pain (AFLURIA 5%, placebo 5%).
In Study 6, headache was the only unsolicited adverse event that occurred in ≥ 5% of subjects who received AFLURIA (5%).
Studies 1 to 7 were all conducted when AFLURIA was administered by needle and syringe.
Additionally, safety information has been collected in a clinical study of AFLURIA administered using the PharmaJet Stratis Needle-Free Injection System (Study 8). Study 8 included 1,247 subjects for safety analysis, ages 18 through 64 years, randomized to receive AFLURIA by either the PharmaJet Stratis Needle-Free Injection System (624 subjects) or needle and syringe (623 subjects). No deaths or vaccine-related serious adverse events were reported in Study 8. Local (injection-site) adverse reactions and systemic adverse events were solicited for 7 days post-vaccination (Table 5).
| Percentage * of Subjects Reporting Event | ||
|---|---|---|
| Study 8 Subjects 18 through 64 years |
||
| AFLURIA | ||
| PharmaJet Stratis Needle-Free Injection System N=540-616 † | Needle and Syringe N=599-606 † |
|
|
||
| Local Adverse Reactions | ||
| Tenderness | 89 | 78 |
| Swelling | 65 | 20 |
| Pain | 64 | 49 |
| Redness | 60 | 19 |
| Itching ‡ | 28 | 10 |
| Bruising | 18 | 5 |
| Systemic Adverse Events | ||
| Myalgia | 36 | 36 |
| Malaise | 31 | 28 |
| Headache | 25 | 22 |
| Chills | 7 | 7 |
| Nausea | 7 | 7 |
| Vomiting | 1 | 2 |
| Fever | 0 | 0 |
In Study 8, no unsolicited adverse events occurred in ≥ 5% of subjects who received AFLURIA administered via PharmaJet Stratis Needle-Free Injection System up to 28 days post-vaccination.
6.2 Postmarketing Experience
Because postmarketing reporting of adverse reactions is voluntary and from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to vaccine exposure. The adverse reactions described have been included in this section because they: 1) represent reactions that are known to occur following immunizations generally or influenza immunizations specifically; 2) are potentially serious; or 3) have been reported frequently. These adverse reactions reflect experience in both children and adults and include those identified during post-approval use of AFLURIA outside the US since 1985.
Immune system disorders
Allergic or immediate hypersensitivity reactions including anaphylactic shock and serum sickness
6.3 Adverse Reactions Associated With Influenza Vaccination
Anaphylaxis has been reported after administration of AFLURIA. Egg protein can induce immediate hypersensitivity reactions among persons who have severe egg allergy. Allergic reactions include hives, angioedema, asthma, and systemic anaphylaxis (see Contraindications [4]).
Neurological disorders temporally associated with influenza vaccination, such as encephalopathy, optic neuritis/neuropathy, partial facial paralysis, and brachial plexus neuropathy, have been reported.
Microscopic polyangiitis (vasculitis) has been reported temporally associated with influenza vaccination.
7 DRUG INTERACTIONS
7.1 Concurrent Use With Other Vaccines
There are no data to assess the concomitant administration of AFLURIA with other vaccines. If AFLURIA is given at the same time as another injectable vaccine(s), the vaccine(s) should be administered in separate syringes and a separate arm should be used.
AFLURIA should not be mixed with any other vaccine in the same syringe or vial.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B: A reproductive and developmental toxicity study has been performed in female rats at a dose approximately 265 times the human dose (on a mg/kg basis) and revealed no evidence of impaired female fertility or harm to the fetus due to AFLURIA. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, AFLURIA should be given to a pregnant woman only if clearly needed.
In the reproductive and developmental toxicity study, the effect of AFLURIA on embryo-fetal and pre-weaning development was evaluated in pregnant rats. Animals were administered AFLURIA by intramuscular injection twice prior to gestation, once during the period of organogenesis (gestation day 6), and once later in pregnancy (gestation day 20), 0.5 mL/rat/occasion (approximately a 265-fold excess relative to the projected human dose on a body weight basis). No adverse effects on mating, female fertility, pregnancy, parturition, lactation parameters, and embryo-fetal or pre-weaning development were observed. There were no vaccine-related fetal malformations or other evidence of teratogenesis.
8.3 Nursing Mothers
AFLURIA has not been evaluated in nursing mothers. It is not known whether AFLURIA is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when AFLURIA is administered to a nursing woman.
8.4 Pediatric Use
AFLURIA is not approved for use in children less than 5 years of age. In a clinical study in which children received AFLURIA or a US-licensed comparator vaccine (Study 1, see Clinical Trials Experience, [6.1]), the incidence of fever in children 6 months through 35 months of age following the first and second doses of AFLURIA were 37% and 15%, respectively, as compared to 14% following each dose in the comparator group. Among children 3 years through 4 years of age, the incidence of fever following the first and second doses of AFLURIA were 32% and 14%, respectively, as compared to 11% and 16% in the comparator. In an open-label study (Study 2), fever, irritability, loss of appetite, and vomiting/diarrhea occurred more frequently in children 6 months through 35 months of age as compared to older children. Across three pediatric studies of AFLURIA (Studies 1, 2, and 3), 1.2% of eligible children (n=1,764) were discontinued from the second vaccination because of severe fever (≥ 104°F) within 48 hours of the first vaccination. Across the three pediatric studies, two children, a 7-month old and a 3-year old, experienced vaccine-related febrile seizures (rate of 0.07% across studies), one of which was serious.
Administration of CSL's 2010 Southern Hemisphere influenza vaccine was associated with increased rates of fever and febrile seizures, predominantly in children below the age of 5 years as compared to previous years, in postmarketing reports confirmed by postmarketing studies (see Warnings and Precautions [5.1]).
The PharmaJet Stratis Needle-Free Injection System is not approved as a method of administering AFLURIA to children and adolescents less than 18 years of age due to lack of adequate data supporting safety and effectiveness in this population.
8.5 Geriatric Use
In clinical studies, AFLURIA has been administered to, and safety information collected for, 836 subjects ages 65 years and older (see Clinical Trials Experience [6.1]). After administration of AFLURIA, hemagglutination-inhibiting antibody responses in persons 65 years of age and older were lower as compared to younger adult subjects (see Clinical Studies [14]).
The PharmaJet Stratis Needle-Free Injection System is not approved as a method of administering AFLURIA to adults 65 years of age and older due to lack of adequate data supporting safety and effectiveness in this population.
11 DESCRIPTION
AFLURIA, Influenza Vaccine for intramuscular injection, is a sterile, clear, colorless to slightly opalescent suspension with some sediment that resuspends upon shaking to form a homogeneous suspension. AFLURIA is prepared from influenza virus propagated in the allantoic fluid of embryonated chicken eggs. Following harvest, the virus is purified in a sucrose density gradient using continuous flow zonal centrifugation. The purified virus is inactivated with beta-propiolactone, and the virus particles are disrupted using sodium taurodeoxycholate to produce a "split virion". The disrupted virus is further purified and suspended in a phosphate buffered isotonic solution.
AFLURIA is standardized according to USPHS requirements for the 2018-2019 influenza season and is formulated to contain 45 mcg hemagglutinin (HA) per 0.5 mL dose in the recommended ratio of 15 mcg HA for each of the three influenza strains recommended for the 2018-2019 Northern Hemisphere influenza season: A/Singapore/GP1908/2015 IVR 180A (H1N1) (an A/Michigan/45/2015 – like virus), A/Singapore/INFIMH-16-0019/2016 IVR-186 (H3N2) (an A/Singapore/INFIMH-16-0019/2016 – like virus and B/Maryland/15/2016 (a B/Colorado/06/2017 – like virus).
Thimerosal, a mercury derivative, is not used in the manufacturing process for the single dose presentations; therefore these products contain no preservative. The multi-dose presentation contains thimerosal, added as a preservative; each 0.5 mL dose contains 24.5 mcg of mercury.
A single 0.5 mL dose of AFLURIA contains sodium chloride (4.1 mg), monobasic sodium phosphate (80 mcg), dibasic sodium phosphate (300 mcg), monobasic potassium phosphate (20 mcg), potassium chloride (20 mcg), and calcium chloride (0.5 mcg). From the manufacturing process, each 0.5 mL dose may also contain residual amounts of sodium taurodeoxycholate (≤ 10 ppm), ovalbumin (< 1 mcg), sucrose (< 10 mcg), neomycin sulfate (≤ 61.5 nanograms [ng]), polymyxin B (≤ 10.5 ng), and beta-propiolactone (≤ 2 ng).
The rubber tip cap and plunger used for the preservative-free, single-dose syringes and the rubber stoppers used for the multi-dose vial were not made with natural rubber latex.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Influenza illness and its complications follow infection with influenza viruses. Global surveillance of influenza identifies yearly antigenic variants. For example, since 1977 antigenic variants of influenza A (H1N1 and H3N2) and influenza B viruses have been in global circulation. Specific levels of hemagglutination inhibition (HI) antibody titers post-vaccination with inactivated influenza vaccine have not been correlated with protection from influenza virus. In some human studies, antibody titers of 1:40 or greater have been associated with protection from influenza illness in up to 50% of subjects.2,3
Antibody against one influenza virus type or subtype confers limited or no protection against another. Furthermore, antibody to one antigenic variant of influenza virus might not protect against a new antigenic variant of the same type or subtype. Frequent development of antigenic variants through antigenic drift is the virologic basis for seasonal epidemics and the reason for the usual change to one or more new strains in each year's influenza vaccine. Therefore, inactivated influenza vaccines are standardized to contain the HA of three strains (i.e., typically two type A and one type B) representing the influenza viruses likely to be circulating in the US during the upcoming winter.
Annual revaccination with the current vaccine is recommended because immunity declines during the year after vaccination and circulating strains of influenza virus change from year to year.1
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
AFLURIA has not been evaluated for carcinogenic or mutagenic potential, or male infertility in animals. A reproductive study of female rats vaccinated with AFLURIA revealed no impairment of fertility (see Pregnancy, 8.1).
14 CLINICAL STUDIES
14.1 Efficacy Against Laboratory-Confirmed Influenza
In Study 5, the efficacy of AFLURIA was demonstrated in a randomized, observer-blind, placebo-controlled study conducted in 15,044 subjects. Healthy subjects 18 through 64 years of age were randomized in a 2:1 ratio to receive a single dose of AFLURIA (enrolled subjects: 10,033; evaluable subjects: 9,889) or placebo (enrolled subjects: 5,011; evaluable subjects: 4,960). The mean age of all randomized subjects was 35.5 years. 54.4% were female and 90.2% were White. Laboratory-confirmed influenza was assessed by active and passive surveillance of influenza-like illness (ILI) beginning 2 weeks post-vaccination until the end of the influenza season, approximately 6 months post-vaccination. ILI was defined as at least one respiratory symptom (e.g., cough, sore throat, nasal congestion) and at least one systemic symptom (e.g., oral temperature of 100.0°F or higher, feverishness, chills, body aches). Nasal and throat swabs were collected from subjects who presented with an ILI for laboratory confirmation by viral culture and real-time reverse transcription polymerase chain reaction. Influenza virus strain was further characterized using gene sequencing and pyrosequencing.
Attack rates and vaccine efficacy, defined as the relative reduction in the influenza infection rate for AFLURIA compared to placebo, were calculated using the per protocol population. Vaccine efficacy against laboratory-confirmed influenza infection due to influenza A or B virus strains contained in the vaccine was 60% with a lower limit of the 95% CI of 41% (Table 6).
| Subjects * | Laboratory-Confirmed Influenza Cases | Influenza Infection Rate | Vaccine Efficacy † | ||
|---|---|---|---|---|---|
| N | N | n/N % | % | Lower Limit of the 95% CI | |
| Abbreviations: CI, confidence interval | |||||
| Vaccine-matched Strains | |||||
| AFLURIA | 9889 | 58 | 0.59 | 60 | 41 |
| Placebo | 4960 | 73 | 1.47 | ||
| Any Influenza Virus Strain | |||||
| AFLURIA | 9889 | 222 | 2.24 | 42 | 28 |
| Placebo | 4960 | 192 | 3.87 | ||
14.2 Immunogenicity in Children – Administration via Needle and Syringe
Study 1 was a randomized, observer-blind, comparator-controlled study to evaluate the immunological non-inferiority of AFLURIA to a U.S.-licensed trivalent inactivated influenza vaccine (manufactured by Sanofi Pasteur, Inc.) in subjects 6 months through 17 years of age. Study vaccines were administered by needle and syringe. Results are presented for children 5 through 17 years of age (Table 7). A total of 832 subjects (aged 5 through 17 years) were enrolled. Subjects were randomized in a 1:1 ratio to receive AFLURIA (enrolled subjects: 417; evaluable subjects: 383) or the comparator vaccine (enrolled subjects: 415; evaluable subjects: 383).
Children 6 months through 8 years of age with no history of influenza vaccination received 2 doses approximately 28 days apart. Children 6 months through 8 years of age with a history of influenza vaccination and children 9 years of age and older received 1 dose. Children 6 months through 35 months of age received 0.25 mL of AFLURIA or comparator influenza vaccine, and children 3 years of age and older received 0.5 mL of AFLURIA or comparator influenza vaccine. Nearly equal proportions of subjects were male (49.9%) and female (50.1%), and the majority were White (85.0%) or Black (10.3%).
Immunogenicity assessments were performed prior to vaccination and at 21 days after vaccination. The co-primary endpoints were HI Geometric Mean Titer (GMT) ratios (adjusted for baseline HI titers) and the difference in seroconversion rates for each vaccine strain 21 days after the final vaccination. Pre-specified non-inferiority criteria required that the upper bound of the 2-sided 95% CI of the GMT ratio (Comparator/AFLURIA) did not exceed 1.5 and the upper bound of the 2-sided 95% CI of the seroconversion rate difference (Comparator minus AFLURIA) did not exceed 10.0% for each strain. As shown in Table 7, non-inferiority of AFLURIA to the comparator vaccine was demonstrated in the per protocol population for influenza A subtypes A(H1N1) and A(H3N2), but not for influenza type B. For influenza type B, non-inferiority was demonstrated for HI GMTs, but not for seroconversion rates. Note that the study was powered to assess the pre-specified non-inferiority criteria based on 1400 evaluable subjects. Analysis of the 761 subjects aged 5 through 17 years reduced the power of the study and widened the confidence intervals. In the pre-specified analysis, AFLURIA was not inferior to the comparator vaccine for all three virus strains. Post-hoc analyses of immunogenicity by gender did not demonstrate significant differences between males and females. The study was not sufficiently diverse to assess differences between races or ethnicities.
| Post-vaccination GMT | GMT Ratio * | Seroconversion % † | Difference | Met both pre-defined non-inferiority criteria? ‡ | |||
|---|---|---|---|---|---|---|---|
| Strain | Comparator N=381 | AFLURIA N=380 | Comparator over AFLURIA (95% CI) | Comparator N=381 | AFLURIA N=380 | Comparator minus AFLURIA (95% CI) |
|
| Abbreviations: CI, confidence interval; GMT, geometric mean titer. | |||||||
|
|||||||
| A(H1N1) | 526.2 | 507.4 | 1.03 (0.88, 1.21) | 62.7 | 62.6 | 0.1 (-6.8, 7.0) | Yes |
| A(H3N2) | 1060.0 | 961.3 | 1.07 (0.94, 1.23) | 72.2 | 69.7 | 2.4 (-4.0, 8.9) | Yes |
| B | 123.3 | 110.1 | 1.10 (0.94, 1.29) | 75.1 | 70.0 | 5.1 (-1.3, 11.4) | No |
14.3 Immunogenicity in Adults and Older Adults – Administration via Needle and Syringe
Two randomized, controlled clinical studies of AFLURIA evaluated the immune responses by measuring HI antibody titers to each virus strain in the vaccine in adults as compared to placebo (adults 18 through 64 years) or another U.S.-licensed trivalent influenza vaccine (adults ≥ 65 years). In these studies, post-vaccination immunogenicity was evaluated on sera obtained 21 days after administration of a single dose of AFLURIA.
Study 4 was a randomized, double-blinded, placebo-controlled, multi-center study in healthy subjects ages 18 through 64 years. A total of 1,357 subjects were vaccinated (1,089 subjects with AFLURIA and 268 with a placebo). Subjects who received AFLURIA were vaccinated using either the preservative-free or thimerosal-containing presentation. The evaluable population consisted of 1,341 subjects (1,077 in the AFLURIA group and 264 in the placebo group). The mean age of the entire evaluable population receiving AFLURIA was 38 years. 62.5% of subjects were female, 81.3% were White, 12.1% were Black, and 6.2% were Asian.
Serum HI antibody responses to AFLURIA met the pre-specified co-primary endpoint criteria for all three virus strains (Table 8). Similar responses were observed between genders. The study was not sufficiently diverse to assess immunogenicity by race or ethnicity.
| Strain Variable | AFLURIA N=1077 value (95% CI) | Placebo N=264 value (95% CI) |
|---|---|---|
|
||
| A(H1N1) | ||
| HI Titer ≥ 1:40 * | 97.8% (96.7, 98.6) | 74.6% (68.9, 79.8) |
| Seroconversion Rate (%) † | 48.7% (45.6, 51.7) | 2.3% (0.8, 4.9) |
| A(H3N2) | ||
| HI Titer ≥ 1:40 * | 99.9% (99.5, 100.0) | 72.0% (66.1, 77.3) |
| Seroconversion Rate (%) † | 71.5% (68.7, 74.2) | 0.0% (N/A) |
| B | ||
| HI Titer ≥ 1:40 * | 94.2% (92.7, 95.6) | 47.0% (40.8, 53.2) |
| Seroconversion Rate (%) † | 69.7% (66.9, 72.5) | 0.4% (< 0.1, 2.1) |
Study 6 was a randomized, observer-blind, comparator-controlled study that enrolled 1,268 subjects 65 years of age and older (Table 9). This study compared the immune response following administration of AFLURIA to that following a US-licensed trivalent inactivated influenza vaccine (manufactured by Sanofi Pasteur Inc.). Subjects were randomized in a 1:1 ratio to receive a single vaccination of AFLURIA (enrolled subjects: 631; evaluable subjects: 605) or the comparator vaccine (enrolled subjects: 637; evaluable subjects: 610). Immunogenicity assessments were performed prior to vaccination and at 21 days after vaccination. Most of the subjects in the per-protocol immunogenicity population were female (56.7%) and White (97.4%). 2.0% were Black and less than 1.0% were of other races or ethnicities.
The co-primary endpoints were HI GMT ratios (adjusted for baseline HI titers) and the difference in seroconversion rates for each vaccine strain 21 days after vaccination. Pre-specified non-inferiority criteria required that the upper bound of the 2-sided 95% CI of the GMT ratio (Comparator/AFLURIA) did not exceed 1.5 and the upper bound of the 2-sided 95% CI of the seroconversion rate difference (Comparator minus AFLURIA) did not exceed 10.0% for each strain. As shown in Table 9, non-inferiority of AFLURIA to the comparator vaccine was demonstrated in the per protocol population for influenza A subtypes A(H1N1) and A(H3N2), but not for influenza type B. For the B strain, non-inferiority was demonstrated for HI GMTs, but not for seroconversion rates. Post-hoc analyses of immunogenicity by gender did not demonstrate significant differences between males and females. The study was not sufficiently diverse to assess differences between races or ethnicities.
| Post-vaccination GMT | GMT Ratio * | Seroconversion % † | Difference | Met both pre-defined non-inferiority criteria? | |||
|---|---|---|---|---|---|---|---|
| Strain | Comparator N=610 | AFLURIA N=605 | Comparator over AFLURIA (95% CI) | Comparator N=610 | AFLURIA N=605 | Comparator minus AFLURIA (95% CI) |
|
| Abbreviations: CI, confidence interval; GMT, geometric mean titer. | |||||||
| A(H1N1) | 59.2 | 59.4 | 1.04 (0.92, 1.18) | 43.0 | 38.8 | 4.1 (-1.4, 9.6) | Yes |
| A(H3N2) | 337.7 | 376.8 | 0.95 (0.83, 1.08) | 68.7 | 69.4 | -0.7 (-5.9, 4.5) | Yes |
| B | 33.4 | 30.4 | 1.12 (1.01, 1.25) | 34.4 | 29.3 | 5.2 (-0.1, 10.4) | No |
14.4 Immunogenicity in Adults – Administration via PharmaJet Stratis Needle-Free Injection System
Study 8 was a randomized, comparator-controlled non-inferiority study that enrolled 1,250 subjects 18 through 64 years of age. This study compared the immune response following administration of AFLURIA when delivered IM using either the PharmaJet Stratis Needle-Free Injection System or needle and syringe. Immunogenicity assessments were performed prior to vaccination and at 28 days after vaccination in the immunogenicity population (1,130 subjects, 562 PharmaJet Stratis Needle-Free Injection System group, 568 needle and syringe group). The co-primary endpoints were HI GMT ratios for each vaccine strain and the absolute difference in seroconversion rates for each vaccine strain 28 days after vaccination. As shown in Table 10, non-inferiority of administration of AFLURIA by the PharmaJet Stratis Needle-Free Injection System compared to administration of AFLURIA by needle and syringe was demonstrated in the immunogenicity population for all strains. Post-hoc analyses of immunogenicity by age showed that younger subjects (18 through 49 years) elicited higher immunological responses than older subjects (50 through 64 years). Post-hoc analyses of immunogenicity according to gender and body mass index did not reveal significant influences of these variables on immune responses. The study population was not sufficiently diverse to assess immunogenicity by race or ethnicity.
| Baseline GMT | Post-vaccination GMT | GMT Ratio * | Seroconversion % † | Difference | Met both pre-defined non-inferiority criteria? ‡ | ||||
|---|---|---|---|---|---|---|---|---|---|
| Strain | Needle and Syringe N=568 | PharmaJet Stratis Needle-Free Injection System N=562 | Needle and Syringe N=568 | PharmaJet Stratis Needle-Free Injection System N=562 | Needle and Syringe over PharmaJet Stratis Needle-Free Injection System (95% CI) | Needle and Syringe N=568 | PharmaJet Stratis Needle-Free Injection System N=562 | Needle and Syringe minus PharmaJet Stratis Needle-Free Injection System (95% CI) |
|
| Abbreviations: CI, confidence interval; GMT, geometric mean titer | |||||||||
|
|||||||||
| A(H1N1) | 79.5 | 83.7 | 280.6 | 282.9 | 0.99 (0.88, 1.12) | 38.4 | 37.5 | 0.8 (-4.8, 6.5) | Yes |
| A(H3N2) | 75.4 | 68.1 | 265.9 | 247.3 | 1.08 (0.96, 1.21) | 45.1 | 43.8 | 1.3 (-4.5, 7.1) | Yes |
| B | 12.6 | 13.5 | 39.7 | 42.5 | 0.94 (0.83, 1.06) | 35.2 | 34.9 | 0.3 (-5.2, 5.9) | Yes |
15 REFERENCES
- Centers for Disease Control and Prevention. Prevention and Control of Influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2010;59 (RR-8):1-62.
- Hannoun C, Megas F, Piercy J. Immunogenicity and Protective Efficacy of Influenza Vaccination. Virus Res 2004;103:133-138.
- Hobson D, Curry RL, Beare AS, et al. The Role of Serum Hemagglutination-Inhibiting Antibody in Protection against Challenge Infection with Influenza A2 and B Viruses. J Hyg Camb 1972;70:767-777.
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Each product presentation includes a package insert and the following components:
| Presentation | Carton NDC Number | Components |
|---|---|---|
| Pre-Filled Syringe | 33332-018-01 |
|
| Multi-Dose Vial | 33332-118-10 |
|
16.2 Storage and Handling
- Store refrigerated at 2–8°C (36–46°F).
- Do not freeze. Discard if product has been frozen.
- Protect from light.
- Do not use AFLURIA beyond the expiration date printed on the label.
- Once the stopper of the multi-dose vial has been pierced the vial must be discarded within 28 days.
17 PATIENT COUNSELING INFORMATION
- Inform the vaccine recipient or guardian of the potential benefits and risks of immunization with AFLURIA.
- Inform the vaccine recipient or guardian that AFLURIA is an inactivated vaccine that cannot cause influenza but stimulates the immune system to produce antibodies that protect against influenza, and that the full effect of the vaccine is generally achieved approximately 3 weeks after vaccination.
- Instruct the vaccine recipient or guardian to report any severe or unusual adverse reactions to their healthcare provider.
- Provide the vaccine recipient or guardian with Vaccine Information Statements which are required by the National Childhood Vaccine Injury Act of 1986 to be given prior to immunization. These materials are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
- Instruct the vaccine recipient or guardian that annual revaccination is recommended.
Manufactured by:
Seqirus Pty Ltd
Parkville, Victoria, 3052, Australia
US License No. 2044
Distributed by:
Seqirus USA Inc.
25 Deforest Avenue, Summit, NJ 07901, USA 1-855-358-8966
AFLURIA is a registered trademark of Seqirus UK Limited or its affiliates.
PharmaJet® and STRATIS® are registered trademarks of PharmaJet.
Luer-Lok™ is a trademark of Becton, Dickinson and Company Corporation.
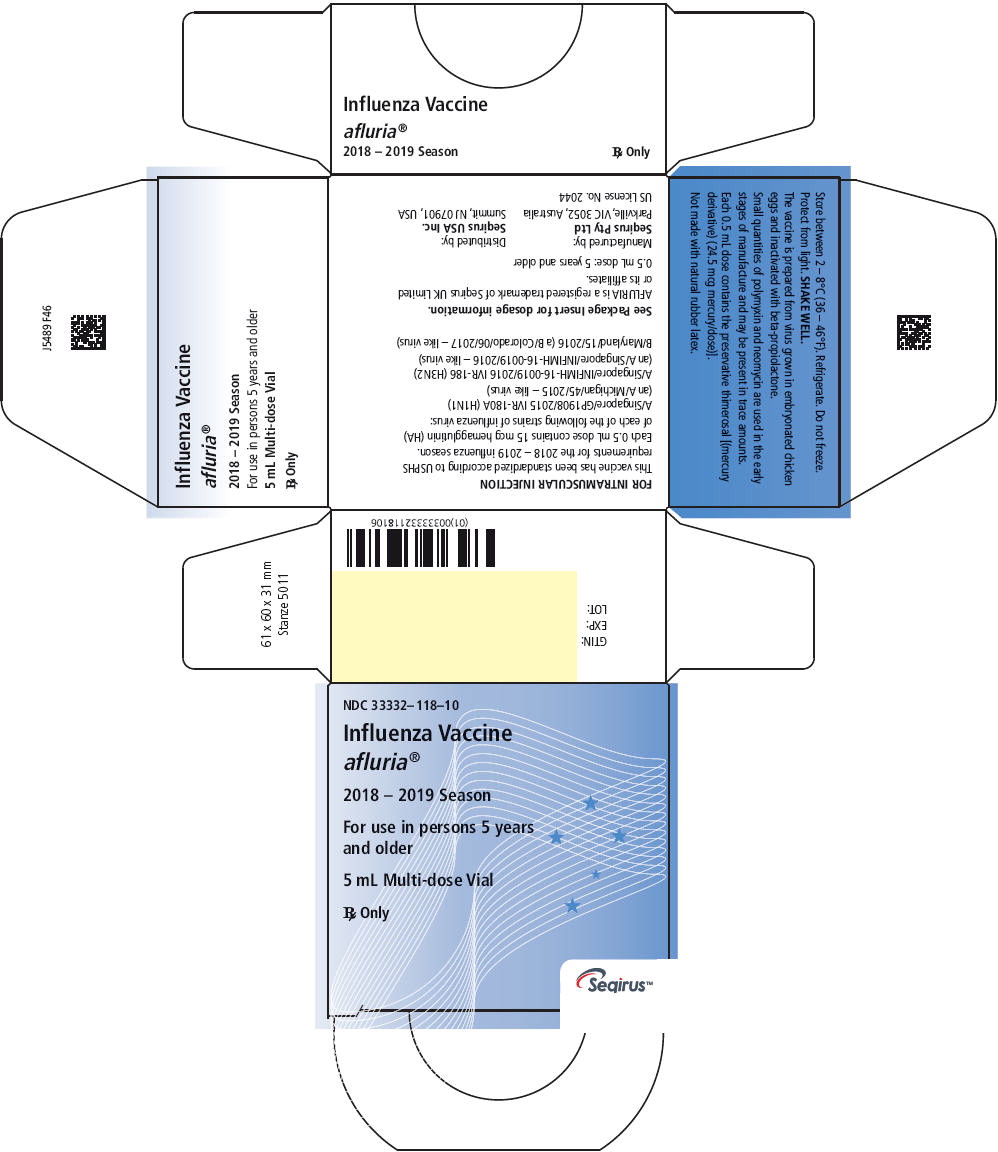
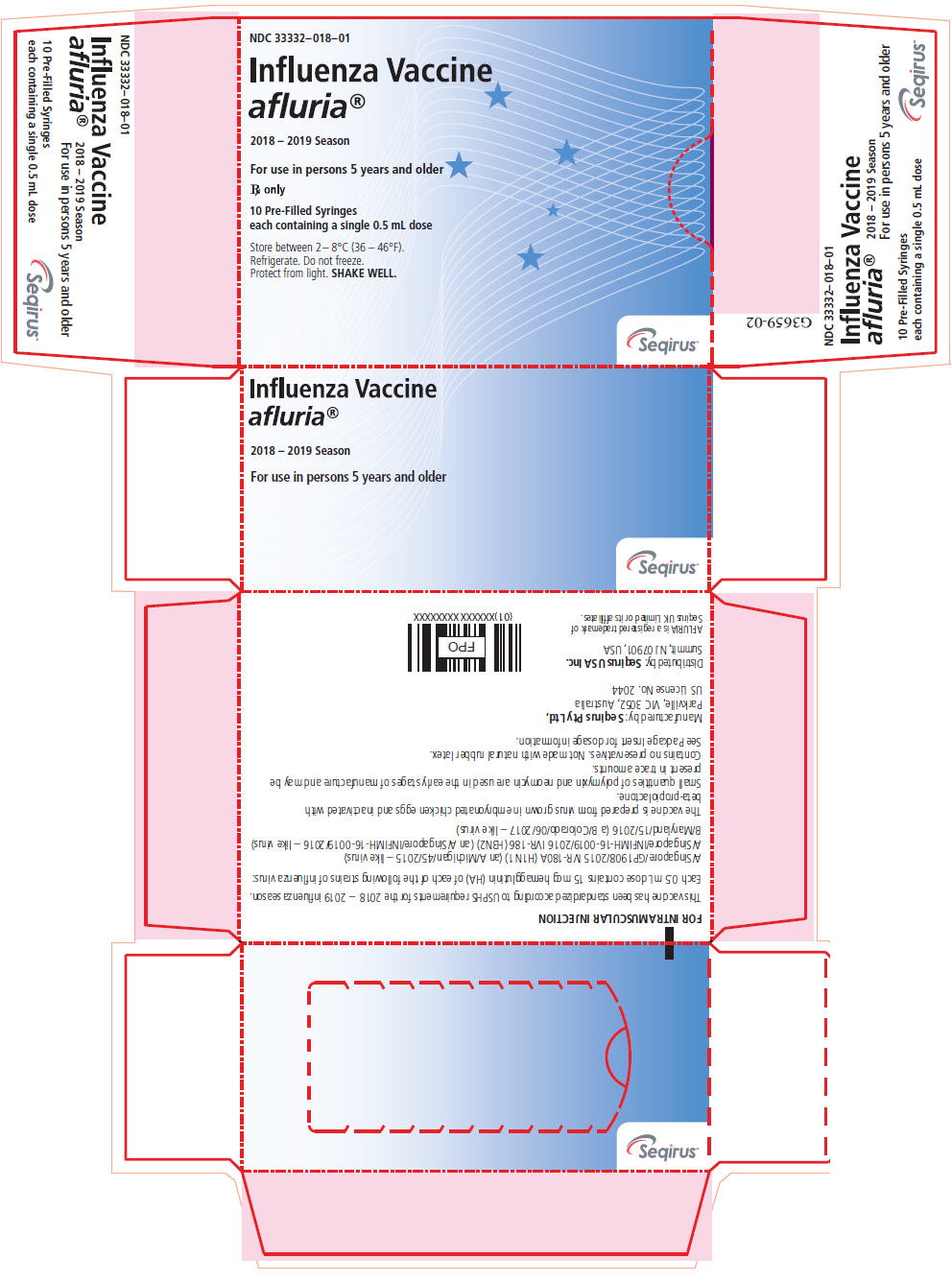
PRINCIPAL DISPLAY PANEL - 0.5 mL Syringe Carton
NDC 33332–018–01
Influenza Vaccine
afluria®
2018 – 2019 Season
For use in persons 5 years and older
Rx only
10 Pre-Filled Syringes
each containing a single 0.5 mL dose
Store between 2 – 8°C (36 – 46°F).
Refrigerate. Do not freeze.
Protect from light. SHAKE WELL.
Seqirus™
| AFLURIA
influenza a virus a/singapore/gp1908/2015 ivr-180a (h1n1) antigen (propiolactone inactivated), influenza a virus a/singapore/infimh-16-0019/2016 ivr-186 (h3n2) antigen (propiolactone inactivated) and influenza b virus b/maryland/15/2016 antigen (propiolactone inactivated) injection, suspension |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| AFLURIA
influenza a virus a/singapore/gp1908/2015 ivr-180a (h1n1) antigen (propiolactone inactivated), influenza a virus a/singapore/infimh-16-0019/2016 ivr-186 (h3n2) antigen (propiolactone inactivated) and influenza b virus b/maryland/15/2016 antigen (propiolactone inactivated) injection, suspension |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Seqirus Pty Ltd (747286735) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Seqirus Pty Ltd | 747286735 | MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| CSL Behring GmbH | 326530474 | MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| CSL Behring LLC | 058268293 | MANUFACTURE | |