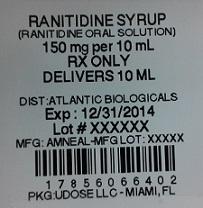
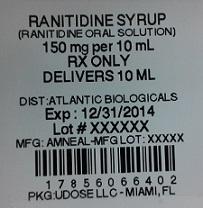
Label: RANITIDINE solution
-
Contains inactivated NDC Code(s)
NDC Code(s): 17856-0664-2, 17856-0664-4 - Packager: Atlantic Biologicals Corps
- This is a repackaged label.
- Source NDC Code(s): 65162-664
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated June 15, 2010
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
DESCRIPTION
The active ingredient in Ranitidine Oral Solution is ranitidine hydrochloride (HCl), USP, a histamine H -receptor antagonist. Chemically it is N[2-[[[5-[(dimethylamino)methyl]-2-furanyl]methyl]thio]ethyl]-N′-methyl-2-nitro-1,1-ethenediamine, HCl. It has the following structure: 2
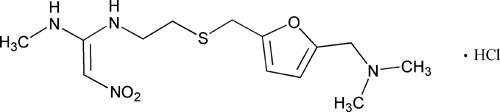
The empirical formula is C H N O S•HCl, representing a molecular weight of 350.87. 132243
Ranitidine HCl is a white to pale yellow, granular substance that is soluble in water. It has a slightly bitter taste and sulfurlike odor.
Each 1 mL of Ranitidine Oral Solution contains 16.8 mg of ranitidine HCl equivalent to 15 mg of ranitidine. Ranitidine Oral Solution also contains the inactive ingredients butylparaben, dibasic sodium phosphate, hypromellose, monobasic sodium phosphate, natural peppermint extract, propylene glycol, propylparaben, purified water, saccharin sodium, sodium chloride, and sorbitol solution.
-
CLINICAL PHARMACOLOGY
Ranitidine hydrochloride is a competitive, reversible inhibitor of the action of histamine at the histamine H -receptors, including receptors on the gastric cells. Ranitidine hydrochloride does not lower serum Ca in hypercalcemic states. Ranitidine hydrochloride is not an anticholinergic agent. 2++
Pharmacokinetics
: Ranitidine hydrochloride is 50% absorbed after oral administration, compared to an intravenous (IV) injection with mean peak levels of 440 to 545 ng/mL occurring 2 to 3 hours after a 150-mg dose. The oral solution formulation is bioequivalent to the tablets. Absorption is not significantly impaired by the administration of food or antacids. Propantheline slightly delays and increases peak blood levels of ranitidine hydrochloride, probably by delaying gastric emptying and transit time. In one study, simultaneous administration of high-potency antacid (150 mmol) in fasting subjects has been reported to decrease the absorption of ranitidine hydrochloride. Absorption
The volume of distribution is about 1.4 L/kg. Serum protein binding averages 15%. Distribution:
In humans, the N-oxide is the principal metabolite in the urine; however, this amounts to <4% of the dose. Other metabolites are the S-oxide (1%) and the desmethyl ranitidine (1%). The remainder of the administered dose is found in the stool. Studies in patients with hepatic dysfunction (compensated cirrhosis) indicate that there are minor, but clinically insignificant, alterations in ranitidine half-life, distribution, clearance, and bioavailability. Metabolism:
The principal route of excretion is the urine, with approximately 30% of the orally administered dose collected in the urine as unchanged drug in 24 hours. Renal clearance is about 410 mL/min, indicating active tubular excretion. The elimination half-life is 2.5 to 3 hours. Four patients with clinically significant renal function impairment (creatinine clearance 25 to 35 mL/min) administered 50 mg of ranitidine intravenously had an average plasma half-life of 4.8 hours, a ranitidine clearance of 29 mL/min, and a volume of distribution of 1.76 L/kg. In general, these parameters appear to be altered in proportion to creatinine clearance (see ). Excretion:DOSAGE AND ADMINISTRATION
The plasma half-life is prolonged and total clearance is reduced in the elderly population due to a decrease in renal function. The elimination half-life is 3 to 4 hours. Peak levels average 526 ng/mL following a 150-mg twice daily dose and occur in about 3 hours (see and ). Geriatrics:PRECAUTIONS: Geriatric UseDOSAGE AND ADMINISTRATION: Dosage Adjustment for Patients With Impaired Renal Function
There are no significant differences in the pharmacokinetic parameter values for ranitidine in pediatric patients (from 1 month up to 16 years of age) and healthy adults when correction is made for body weight. The average bioavailability of ranitidine given orally to pediatric patients is 48% which is comparable to the bioavailability of ranitidine in the adult population. All other pharmacokinetic parameter values (t , Vd, and CL) are similar to those observed with intravenous ranitidine use in pediatric patients. Estimates of C and T are displayed in Table 1. Pediatrics:1/2maxmax
Table 1. Ranitidine Pharmacokinetics in Pediatric
Patients Following Oral DosingPopulation (age)
n Dosage Form (dose)
C (ng/mL) max
T (hours) max
Gastric or duodenal ulcer(3.5 to 16 years) 12 Tablets(1 to 2 mg/kg) 54 to 492 2.0 Otherwise healthy requiring Ranitidine Oral Solution(0.7 to 14 years, Single dose) 10 Oral Solution(2 mg/kg) 244 1.61 Otherwise healthy requiring Ranitidine Oral Solution(0.7 to 14 years, Multiple dose) 10 Oral Solution(2 mg/kg) 320 1.66 -
Plasma clearance measured in 2 neonatal patients (less than 1 month of age) was considerably lower (3 mL/min/kg) than children or adults and is likely due to reduced renal function observed in this population (see and ). PRECAUTIONS: Pediatric UseDOSAGE AND ADMINISTRATION: Pediatric Use
PHARMACODYNAMICS
Serum concentrations necessary to inhibit 50% of stimulated gastric acid secretion are estimated to be 36 to 94 ng/mL. Following a single oral dose of 150 mg, serum concentrations of ranitidine hydrochloride are in this range up to 12 hours. However, blood levels bear no consistent relationship to dose or degree of acid inhibition.
Ranitidine Oral Solution inhibits both daytime and nocturnal basal gastric acid secretions as well as gastric acid secretion stimulated by food, betazole, and pentagastrin, as shown in Table 2. Antisecretory Activity:1. Effects on Acid Secretion:
Table 2. Effect of Ranitidine Oral Solution on Gastric Acid Secretion Time After Dose, h % Inhibition of Gastric Acid Output by Dose, mg 75-80 100 150 200 Basal Up to 4 99 95 Nocturnal Up to 13 95 96 92 Betazole Up to 3 97 99 Pentagastrin Up to 5 58 72 72 80 Meal Up to 3 73 79 95 Basal Up to 4 75-80 100 150 200 -
It appears that basal-, nocturnal-, and betazole-stimulated secretions are most sensitive to inhibition by Ranitidine Oral Solution, responding almost completely to doses of 100 mg or less, while pentagastrin- and food-stimulated secretions are more difficult to suppress.
2.Effects on Other Gastrointestinal Secretions:
: Ranitidine Oral Solution does not affect pepsin secretion. Total pepsin output is reduced in proportion to the decrease in volume of gastric juice. Pepsin
: Ranitidine Oral Solution has no significant effect on pentagastrin-stimulated intrinsic factor secretion. Intrinsic Factor
: Ranitidine Oral Solution has little or no effect on fasting or postprandial serum gastrin. Serum Gastrin
Other Pharmacologic Actions:
-
1. Gastric bacterial flora—increase in nitrate-reducing organisms, significance not known.
-
2. Prolactin levels—no effect in recommended oral or intravenous (IV) dosage, but small, transient, dose-related increases in serum prolactin have been reported after IV bolus injections of 100 mg or more.
-
3. Other pituitary hormones—no effect on serum gonadotropins, TSH, or GH. Possible impairment of vasopressin release.
-
4. No change in cortisol, aldosterone, androgen, or estrogen levels.
-
5. No antiandrogenic action.
-
6. No effect on count, motility, or morphology of sperm.
Oral doses of 6 to 10 mg/kg per day in 2 or 3 divided doses maintain gastric pH>4 throughout most of the dosing interval. Pediatrics:
In a multicenter, double-blind, controlled, US study of endoscopically diagnosed duodenal ulcers, earlier healing was seen in the patients treated with Ranitidine Oral Solution as shown in Table 3. Clinical Trials:Active Duodenal Ulcer:
Table 3. Duodenal Ulcer Patient Healing Rates Ranitidine Oral Solution* Placebo* Number Entered Healed/ Evaluable Number Entered Healed/ Evaluable Outpatients 195 69/182(38%)† 188 31/164(19%) Week 2 Week 4 137/187(73%)† 76/168(45%) *All patients were permitted p.r.n. antacids for relief of pain.
† <0.0001. P
In these studies, patients treated with Ranitidine Oral Solution reported a reduction in both daytime and nocturnal pain, and they also consumed less antacid than the placebo-treated patients.
Table 4. Mean Daily Doses of Antacid Ulcer Healed Ulcer Not Healed Ranitidine Oral Solution 0.06 0.71 Placebo 0.71 1.43 Foreign studies have shown that patients heal equally well with 150 mg b.i.d. and 300 mg h.s. (85% versus 84%, respectively) during a usual 4-week course of therapy. If patients require extended therapy of 8 weeks, the healing rate may be higher for 150 mg b.i.d. as compared to 300 mg h.s. (92% versus 87%, respectively).
Studies have been limited to short-term treatment of acute duodenal ulcer. Patients whose ulcers healed during therapy had recurrences of ulcers at the usual rates.
Ranitidine has been found to be effective as maintenance therapy for patients following healing of acute duodenal ulcers. In 2 independent, double-blind, multicenter, controlled trials, the number of duodenal ulcers observed was significantly less in patients treated with Ranitidine Oral Solution (150 mg h.s.) than in patients treated with placebo over a 12-month period. Maintenance Therapy in Duodenal Ulcer:
Table 5. Duodenal Ulcer Prevalence Double-Blind, Multicenter, Placebo-Controlled Trials Multicenter Trial Drug Duodenal Ulcer Prevalence No. of Patients 0-4Months 0-8Months 0-12Months USA RAN 20%* 24%* 35%* 138 PLC 44% 54% 59% 139 Foreign RAN 12%* 21%* 28%* 174 PLC 56% 64% 68% 165 % = Life table estimate.
* = <0.05 (Ranitidine Oral Solution versus comparator). P
RAN = ranitidine (Ranitidine Oral Solution).
PLC = placebo.
As with other H -antagonists, the factors responsible for the significant reduction in the prevalence of duodenal ulcers include prevention of recurrence of ulcers, more rapid healing of ulcers that may occur during maintenance therapy, or both. 2
: In a multicenter, double-blind, controlled, US study of endoscopically diagnosed gastric ulcers, earlier healing was seen in the patients treated with Ranitidine Oral Solution as shown in Table 6. Gastric Ulcer
Table 6. Gastric Ulcer Patient Healing Rates Ranitidine Oral Solution* Placebo* Number Entered Healed/ Evaluable Number Entered Healed/ Evaluable Outpatients 92 16/83(19%) 94 10/83(12%) Week 2 Week 4 50/73(68%)† 35/69(51%) *All patients were permitted p.r.n. antacids for relief of pain.
† = 0.009. P
In this multicenter trial, significantly more patients treated with Ranitidine Oral Solution became pain free during therapy.
: In 2 multicenter, double-blind, randomized, placebo-controlled, 12-month trials conducted in patients whose gastric ulcers had been previously healed, Ranitidine Oral Solution 150 mg h.s. was significantly more effective than placebo in maintaining healing of gastric ulcers. Maintenance of Healing of Gastric Ulcers
Ranitidine hydrochloride inhibits gastric acid secretion and reduces occurrence of diarrhea, anorexia, and pain in patients with pathological hypersecretion associated with Zollinger-Ellison syndrome, systemic mastocytosis, and other pathological hypersecretory conditions (e.g., postoperative, "short-gut" syndrome, idiopathic). Use of Ranitidine Oral Solution was followed by healing of ulcers in 8 of 19 (42%) patients who were intractable to previous therapy. Pathological Hypersecretory Conditions (such as Zollinger-Ellison syndrome):
In 2 multicenter, double-blind, placebo-controlled, 6-week trials performed in the United States and Europe, Ranitidine Oral Solution 150 mg b.i.d. was more effective than placebo for the relief of heartburn and other symptoms associated with GERD. Ranitidine-treated patients consumed significantly less antacid than did placebo-treated patients. Gastroesophageal Reflux Disease (GERD):
The US trial indicated that Ranitidine Oral Solution 150 mg b.i.d. significantly reduced the frequency of heartburn attacks and severity of heartburn pain within 1 to 2 weeks after starting therapy. The improvement was maintained throughout the 6-week trial period. Moreover, patient response rates demonstrated that the effect on heartburn extends through both the day and night time periods.
In 2 additional US multicenter, double-blind, placebo-controlled, 2-week trials, Ranitidine Oral Solution 150 mg b.i.d. was shown to provide relief of heartburn pain within 24 hours of initiating therapy and a reduction in the frequency of severity of heartburn.
In 2 multicenter, double-blind, randomized, placebo-controlled, 12-week trials performed in the United States, Ranitidine Oral Solution 150 mg q.i.d. was significantly more effective than placebo in healing endoscopically diagnosed erosive esophagitis and in relieving associated heartburn. The erosive esophagitis healing rates were as follows: Erosive Esophagitis:
Healed/Evaluable Placebo* n = 229
Ranitidine Oral Solution 150 mg q.i.d.* n = 215
Week 4 43/198 (22%) 96/206 (47%)† Week 8 63/176 (36%) 142/200 (71%)† Week 12 92/159 (58%) 162/192 (84%)† *All patients were permitted p.r.n. antacids for relief of pain.
† <0.001 versus placebo. P
No additional benefit in healing of esophagitis or in relief of heartburn was seen with a ranitidine dose of 300 mg q.i.d.
: In 2 multicenter, double-blind, randomized, placebo-controlled, 48-week trials conducted in patients whose erosive esophagitis had been previously healed, Ranitidine Oral Solution 150 mg b.i.d. was significantly more effective than placebo in maintaining healing of erosive esophagitis. Maintenance of Healing of Erosive Esophagitis
-
-
INDICATIONS & USAGE
-
Ranitidine Oral Solution is indicated in:
- Short-term treatment of active duodenal ulcer. Most patients heal within 4 weeks. Studies available to date have not assessed the safety of ranitidine in uncomplicated duodenal ulcer for periods of more than 8 weeks.
- Maintenance therapy for duodenal ulcer patients at reduced dosage after healing of acute ulcers. No placebo-controlled comparative studies have been carried out for periods of longer than 1 year.
- The treatment of pathological hypersecretory conditions (e.g., Zollinger-Ellison syndrome and systemic mastocytosis).
- Short-term treatment of active, benign gastric ulcer. Most patients heal within 6 weeks and the usefulness of further treatment has not been demonstrated. Studies available to date have not assessed the safety of ranitidine in uncomplicated, benign gastric ulcer for periods of more than 6 weeks.
- Maintenance therapy for gastric ulcer patients at reduced dosage after healing of acute ulcers. Placebo-controlled studies have been carried out for 1 year.
- Treatment of GERD. Symptomatic relief commonly occurs within 24 hours after starting therapy with Ranitidine Oral Solution 150 mg b.i.d.
- Treatment of endoscopically diagnosed erosive esophagitis. Symptomatic relief of heartburn commonly occurs within 24 hours of therapy initiation with Ranitidine Oral Solution 150 mg q.i.d.
- Maintenance of healing of erosive esophagitis. Placebo-controlled trials have been carried out for 48 weeks.
Concomitant antacids should be given as needed for pain relief to patients with active duodenal ulcer; active, benign gastric ulcer; hypersecretory states; GERD; and erosive esophagitis.
-
-
CONTRAINDICATIONS
Ranitidine Oral Solution is contraindicated for patients known to have hypersensitivity to the drug or any of the ingredients (see ). PRECAUTIONS
-
PRECAUTIONS
: General
- Symptomatic response to therapy with Ranitidine Oral Solution does not preclude the presence of gastric malignancy.
- Since ranitidine hydrochloride is excreted primarily by the kidney, dosage should be adjusted in patients with impaired renal function (see ). Caution should be observed in patients with hepatic dysfunction since ranitidine hydrochloride is metabolized in the liver. DOSAGE AND ADMINISTRATION
- Rare reports suggest that ranitidine hydrochloride may precipitate acute porphyric attacks in patients with acute porphyria. Ranitidine hydrochloride should therefore be avoided in patients with a history of acute porphyria.
False-positive tests for urine protein with MULTISTIX may occur during Ranitidine Oral Solution therapy, and therefore testing with sulfosalicylic acid is recommended. Laboratory Tests:®
: Although ranitidine hydrochloride has been reported to bind weakly to cytochrome P-450 in vitro, recommended doses of the drug do not inhibit the action of the cytochrome P-450–linked oxygenase enzymes in the liver. However, there have been isolated reports of drug interactions that suggest that Ranitidine Oral Solution may affect the bioavailability of certain drugs by some mechanism as yet unidentified (e.g., a pH-dependent effect on absorption or a change in volume of distribution). Drug Interactions
Increased or decreased prothrombin times have been reported during concurrent use of ranitidine and warfarin. However, in human pharmacokinetic studies with dosages of ranitidine up to 400 mg/day, no interaction occurred; ranitidine had no effect on warfarin clearance or prothrombin time. The possibility of an interaction with warfarin at dosages of ranitidine higher than 400 mg/day has not been investigated.
In a ranitidine-triazolam drug-drug interaction study, triazolam plasma concentrations were higher during b.i.d. dosing of ranitidine than triazolam given alone. The mean area under the triazolam concentration-time curve (AUC) values in 18- to 60-year-old subjects were 10% and 28% higher following administration of 75-mg and 150-mg ranitidine, respectively, than triazolam given alone. In subjects older than 60 years of age, the mean AUC values were approximately 30% higher following administration of 75-mg and 150-mg ranitidine. It appears that there were no changes in pharmacokinetics of triazolam and α-hydroxytriazolam, a major metabolite, and in their elimination. Reduced gastric acidity due to ranitidine may have resulted in an increase in the availability of triazolam. The clinical significance of this triazolam and ranitidine pharmacokinetic interaction is unknown.
There was no indication of tumorigenic or carcinogenic effects in life-span studies in mice and rats at dosages up to 2,000 mg/kg per day. Carcinogenesis, Mutagenesis, Impairment of Fertility:
Ranitidine was not mutagenic in standard bacterial tests ( ) for mutagenicity at concentrations up to the maximum recommended for these assays. Salmonella, Escherichia coli
In a dominant lethal assay, a single oral dose of 1,000 mg/kg to male rats was without effect on the outcome of 2 matings per week for the next 9 weeks.
Pregnancy Category B. Reproduction studies have been performed in rats and rabbits at doses up to 160 times the human dose and have revealed no evidence of impaired fertility or harm to the fetus due to Ranitidine Oral Solution. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed. Pregnancy:Teratogenic Effects:
Ranitidine hydrochloride is secreted in human milk. Caution should be exercised when Ranitidine Oral Solution is administered to a nursing mother. Nursing Mothers:
The safety and effectiveness of Ranitidine Oral Solution have been established in the age-group of 1 month to 16 years for the treatment of duodenal and gastric ulcers, gastroesophageal reflux disease and erosive esophagitis, and the maintenance of healed duodenal and gastric ulcer. Use of Ranitidine Oral Solution in this age-group is supported by adequate and well-controlled studies in adults, as well as additional pharmacokinetic data in pediatric patients and an analysis of the published literature (see and ). Pediatric Use:CLINICAL PHARMACOLOGY: PediatricsDOSAGE AND ADMINISTRATION: Pediatric Use
Safety and effectiveness in pediatric patients for the treatment of pathological hypersecretory conditions or the maintenance of healing of erosive esophagitis have not been established.
Safety and effectiveness in neonates (less than 1 month of age) have not been established (see ). CLINICAL PHARMACOLOGY: Pediatrics
Of the total number of subjects enrolled in US and foreign controlled clinical trials of oral formulations of ranitidine hydrochloride, for which there were subgroup analyses, 4,197 were 65 and over, while 899 were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Geriatric Use:
This drug is known to be substantially excreted by the kidney and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, caution should be exercised in dose selection, and it may be useful to monitor renal function (see and ). CLINICAL PHARMACOLOGY: Pharmacokinetics: GeriatricsDOSAGE AND ADMINISTRATION: Dosage Adjustment for Patients With Impaired Renal Function
-
ADVERSE REACTIONS
The following have been reported as events in clinical trials or in the routine management of patients treated with Ranitidine Oral Solution.
The relationship to therapy with Ranitidine Oral Solution has been unclear in many cases. Headache, sometimes severe, seems to be related to administration of Ranitidine Oral Solution.
Rarely, malaise, dizziness, somnolence, insomnia, and vertigo. Rare cases of reversible mental confusion, agitation, depression, and hallucinations have been reported, predominantly in severely ill elderly patients. Rare cases of reversible blurred vision suggestive of a change in accommodation have been reported. Rare reports of reversible involuntary motor disturbances have been received. Central Nervous System:
As with other H -blockers, rare reports of arrhythmias such as tachycardia, bradycardia, atrioventricular block, and premature ventricular beats. Cardiovascular:2
Constipation, diarrhea, nausea/vomiting, abdominal discomfort/pain, and rare reports of pancreatitis. Gastrointestinal:
There have been occasional reports of hepatocellular, cholestatic, or mixed hepatitis, with or without jaundice. In such circumstances, ranitidine should be immediately discontinued. These events are usually reversible, but in rare circumstances death has occurred. Rare cases of hepatic failure have also been reported. In normal volunteers, SGPT values were increased to at least twice the pretreatment levels in 6 of 12 subjects receiving 100 mg q.i.d. intravenously for 7 days, and in 4 of 24 subjects receiving 50 mg q.i.d. intravenously for 5 days. Hepatic:
Rare reports of arthralgias and myalgias. Musculoskeletal:
Blood count changes (leukopenia, granulocytopenia, and thrombocytopenia) have occurred in a few patients. These were usually reversible. Rare cases of agranulocytosis, pancytopenia, sometimes with marrow hypoplasia, and aplastic anemia and exceedingly rare cases of acquired immune hemolytic anemia have been reported. Hematologic:
Controlled studies in animals and man have shown no stimulation of any pituitary hormone by ranitidine hydrochloride and no antiandrogenic activity, and cimetidine-induced gynecomastia and impotence in hypersecretory patients have resolved when Ranitidine Oral Solution has been substituted. However, occasional cases of impotence and loss of libido have been reported in male patients receiving Ranitidine Oral Solution, but the incidence did not differ from that in the general population. Rare cases of breast symptoms and consitions, including galactorrhea and gynecomastis, have been reported in both males and females. Endocrine:
Rash, including rare cases of erythema multiforme. Rare cases of alopecia and vasculitis. Integumentary:
A large epidemiological study suggested an increased risk of developing pneumonia in current users of histamine-2-receptor antagonists (H RAs) compared to patients who had stopped H RA treatment, with an observed adjusted relative risk of 1.63 (95% Cl, 1.07-2.48). However, a causal relationship between use of H RAs and pneumonia has not been established. Respiratory:222
Rare cases of hypersensitivity reactions (e.g., bronchospasm, fever, rash, eosinophilia), anaphylaxis, angioneurotic edema, and small increases in serum creatinine. Other:
-
OVERDOSAGE
There has been limited experience with overdosage. Reported acute ingestions of up to 18 g orally have been associated with transient adverse effects similar to those encountered in normal clinical experience (see ). In addition, abnormalities of gait and hypotension have been reported. ADVERSE REACTIONS
When overdosage occurs, the usual measures to remove unabsorbed material from the gastrointestinal tract, clinical monitoring, and supportive therapy should be employed.
Studies in dogs receiving dosages of Ranitidine Oral Solution in excess of 225 mg/kg per day have shown muscular tremors, vomiting, and rapid respiration. Single oral doses of 1,000 mg/kg in mice and rats were not lethal. Intravenous LD values in mice and rats were 77 and 83 mg/kg, respectively. 50
-
DOSAGE & ADMINISTRATION
The current recommended adult dosage of Ranitidine Oral Solution for duodenal ulcer is 150 mg or 10 mL of oral solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) twice daily. An alternative dosage of 300 mg or 20 mL of oral solution (4 teaspoonfuls of solution equivalent to 300 mg of ranitidine) once daily after the evening meal or at bedtime can be used for patients in whom dosing convenience is important. The advantages of one treatment regimen compared to the other in a particular patient population have yet to be demonstrated (see Smaller doses have been shown to be equally effective in inhibiting gastric acid secretion in US studies, and several foreign trials have shown that 100 mg twice daily is as effective as the 150-mg dose. Active Duodenal Ulcer:Clinical Trials: Active Duodenal Ulcer).
Antacid should be given as needed for relief of pain (see ). CLINICAL PHARMACOLOGY: Pharmacokinetics
The current recommended adult dosage is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) at bedtime. Maintenance of Healing of Duodenal Ulcers:
The current recommended adult dosage is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) twice a day. In some patients it may be necessary to administer Ranitidine Oral Solution 150-mg doses more frequently. Dosages should be adjusted to individual patient needs, and should continue as long as clinically indicated. Dosages up to 6 g/day have been employed in patients with severe disease. Pathological Hypersecretory Conditions (such as Zollinger-Ellison syndrome):
The current recommended adult dosage is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) twice a day. Benign Gastric Ulcer:
The current recommended adult dosage is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) at bedtime. Maintenance of Healing of Gastric Ulcers:
The current recommended adult dosage is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) twice a day. GERD:
The current recommended adult dosage is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) 4 times a day. Erosive Esophagitis:
The current recommended adult dosage is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) twice a day. Maintenance of Healing of Erosive Esophagitis:
The safety and effectiveness of Ranitidine Oral Solution have been established in the age-group of 1 month to 16 years. There is insufficient information about the pharmacokinetics of ranitidine hydrochloride in neonatal patients (less than 1 month of age) to make dosing recommendations. Pediatric Use:
The following 3 subsections provide dosing information for each of the pediatric indications.
The recommended oral dose for the treatment of active duodenal and gastric ulcers is 2 to 4 mg/kg twice daily to a maximum of 300 mg/day. This recommendation is derived from adult clinical studies and pharmacokinetic data in pediatric patients. Treatment of Duodenal and Gastric Ulcers:
The recommended oral dose for the maintenance of healing of duodenal and gastric ulcers is 2 to 4 mg/kg once daily to a maximum of 150 mg/day. This recommendation is derived from adult clinical studies and pharmacokinetic data in pediatric patients. Maintenance of Healing of Duodenal and Gastric Ulcers:
Although limited data exist for these conditions in pediatric patients, published literature supports a dosage of 5 to 10 mg/kg per day, usually given as 2 divided doses. Treatment of GERD and Erosive Esophagitis:
On the basis of experience with a group of subjects with severely impaired renal function treated with ranitidine hydrochloride, the recommended dosage in patients with a creatinine clearance <50 mL/min is 150 mg or 10 mL of Ranitidine Oral Solution (2 teaspoonfuls of solution equivalent to 150 mg of ranitidine) every 24 hours. Should the patient's condition require, the frequency of dosing may be increased to every 12 hours or even further with caution. Hemodialysis reduces the level of circulating ranitidine. Ideally, the dosing schedule should be adjusted so that the timing of a scheduled dose coincides with the end of hemodialysis. Dosage Adjustment for Patients With Impaired Renal Function:
Elderly patients are more likely to have decreased renal function, therefore caution should be exercised in dose selection, and it may be useful to monitor renal function (see and ). CLINICAL PHARMACOLOGY: Pharmacokinetics: GeriatricsPRECAUTIONS: Geriatric Use
- RANITIDINE SOLUTION
-
INGREDIENTS AND APPEARANCE
RANITIDINE
ranitidine solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:17856-0664(NDC:65162-664) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength RANITIDINE HYDROCHLORIDE (UNII: BK76465IHM) (RANITIDINE - UNII:884KT10YB7) RANITIDINE 15 mg in 1 mL Inactive Ingredients Ingredient Name Strength BUTYLPARABEN (UNII: 3QPI1U3FV8) SODIUM PHOSPHATE, DIBASIC (UNII: GR686LBA74) HYPROMELLOSES (UNII: 3NXW29V3WO) SODIUM PHOSPHATE, MONOBASIC (UNII: 3980JIH2SW) PEPPERMINT (UNII: V95R5KMY2B) PROPYLENE GLYCOL (UNII: 6DC9Q167V3) PROPYLPARABEN (UNII: Z8IX2SC1OH) WATER (UNII: 059QF0KO0R) SACCHARIN SODIUM (UNII: SB8ZUX40TY) SODIUM CHLORIDE (UNII: 451W47IQ8X) SORBITOL (UNII: 506T60A25R) Product Characteristics Color Score Shape Size Flavor PEPPERMINT Imprint Code Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:17856-0664-2 10 mL in 1 CUP 2 NDC:17856-0664-4 1 mL in 1 SYRINGE Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078312 03/12/2010 Labeler - Atlantic Biologicals Corps (047437707) Registrant - Atlantic Biologicals Corps (047437707) Establishment Name Address ID/FEI Business Operations Atlantic Biologicals Corps 047437707 RELABEL(17856-0664) , REPACK(17856-0664)