Label: DOXORUBICIN HYDROCHLORIDE injection, solution
- NDC Code(s): 62756-826-40, 62756-827-40
- Packager: Sun Pharmaceutical Industries, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated January 17, 2022
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use doxorubicin hydrochloride safely and effectively. See full prescribing information for doxorubicin hydrochloride injection.
DOXORUBICIN hydrochloride injection, USP for intravenous use
Initial U.S. Approval: 1974
WARNING: CARDIOMYOPATHY, SECONDARY MALIGNANCIES, EXTRAVASATION AND TISSUE NECROSIS, and SEVERE MYELOSUPPRESSION
See full prescribing information for complete boxed warning.
- Cardiomyopathy: Myocardial damage can occur with doxorubicin hydrochloride with incidences from 1% to 20% for cumulative doses from 300 mg/m2 to 500 mg/m2 when doxorubicin hydrochloride is administered every 3 weeks. The risk of cardiomyopathy is further increased with concomitant cardiotoxic therapy. Assess left ventricular ejection fraction (LVEF) before and regularly during and after treatment with doxorubicin hydrochloride. (5.1)
- Secondary Malignancies: Secondary acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) occur at a higher incidence in patients treated with anthracyclines, including doxorubicin hydrochloride. (5.2)
- Extravasation and Tissue Necrosis: Extravasation of doxorubicin hydrochloride can result in severe local tissue injury and necrosis requiring wide excision and skin grafting. Immediately terminate the drug, and apply ice to the affected area. (5.3)
- Severe myelosuppression resulting in serious infection, septic shock, requirement for transfusions, hospitalization, and death may occur. (5.4)
INDICATIONS AND USAGE
Doxorubicin hydrochloride (HCl) is an anthracycline topoisomerase II inhibitor indicated: (1)
- as a component of multiagent adjuvant chemotherapy for treatment of women with axillary lymph node involvement following resection of primary breast cancer (1.1).
- for the treatment of: acute lymphoblastic leukemia, acute myeloblastic leukemia, Hodgkin lymphoma, Non-Hodgkin lymphoma, metastatic breast cancer, metastatic Wilms’ tumor, metastatic neuroblastoma, metastatic soft tissue sarcoma, metastatic bone sarcomas, metastatic ovarian carcinoma, metastatic transitional cell bladder carcinoma, metastatic thyroid carcinoma, metastatic gastric carcinoma, metastatic bronchogenic carcinoma (1.2).
DOSAGE AND ADMINISTRATION
- Single agent: 60 to 75 mg/m2 given intravenously every 21 days (2.1).
- In combination therapy: 40 to 75 mg/m2 given intravenously every 21 to 28 days (2.1).
- Discontinue doxorubicin hydrochloride in patients who develop signs or symptoms of cardiomyopathy (2.2).
- Reduce dose in patients with hepatic impairment (2.2).
DOSAGE FORMS AND STRENGTHS
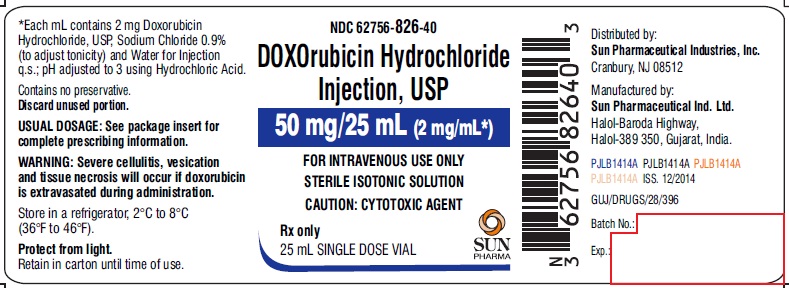
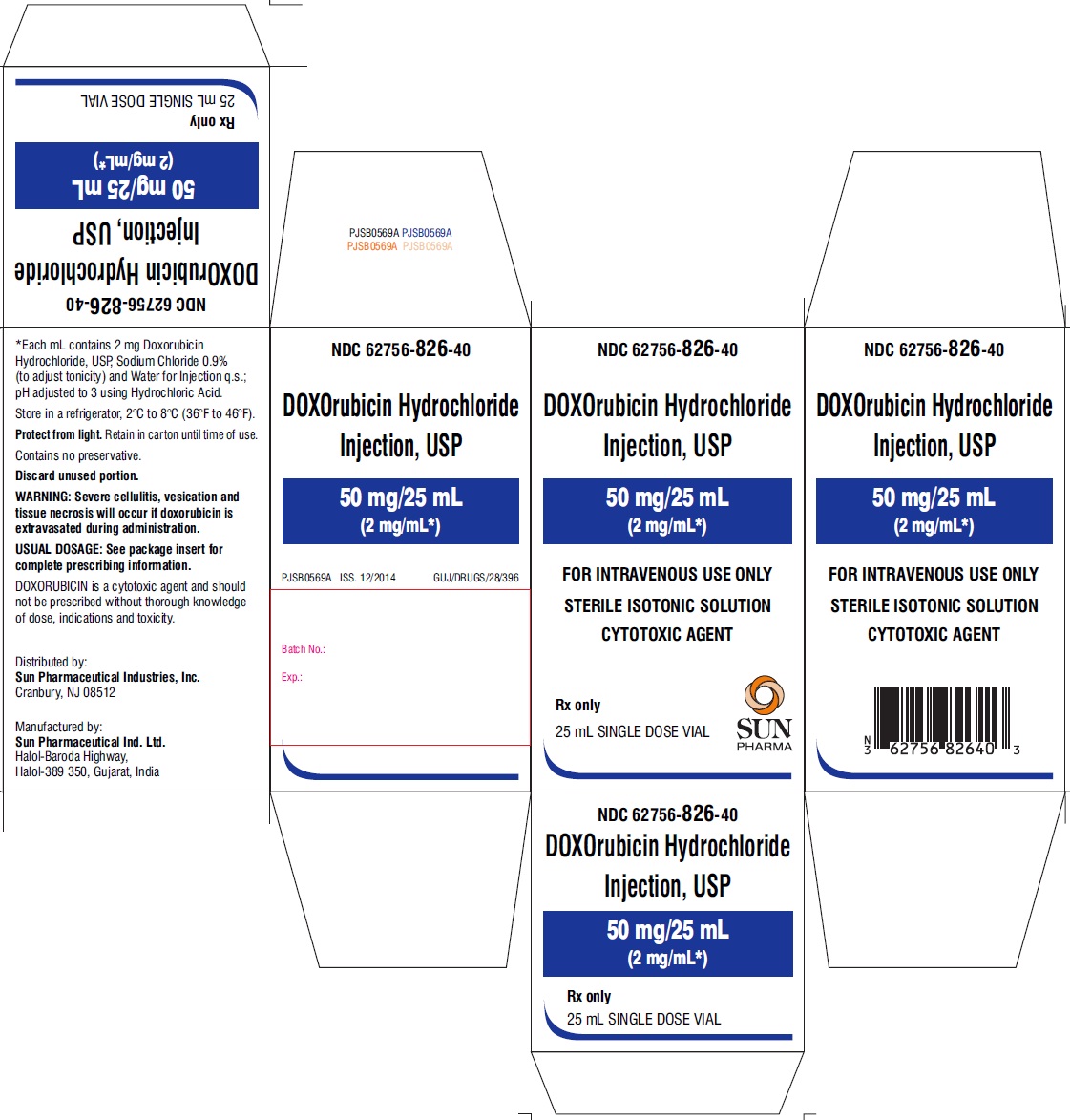
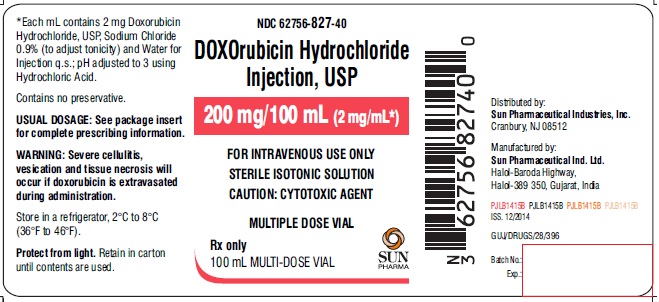
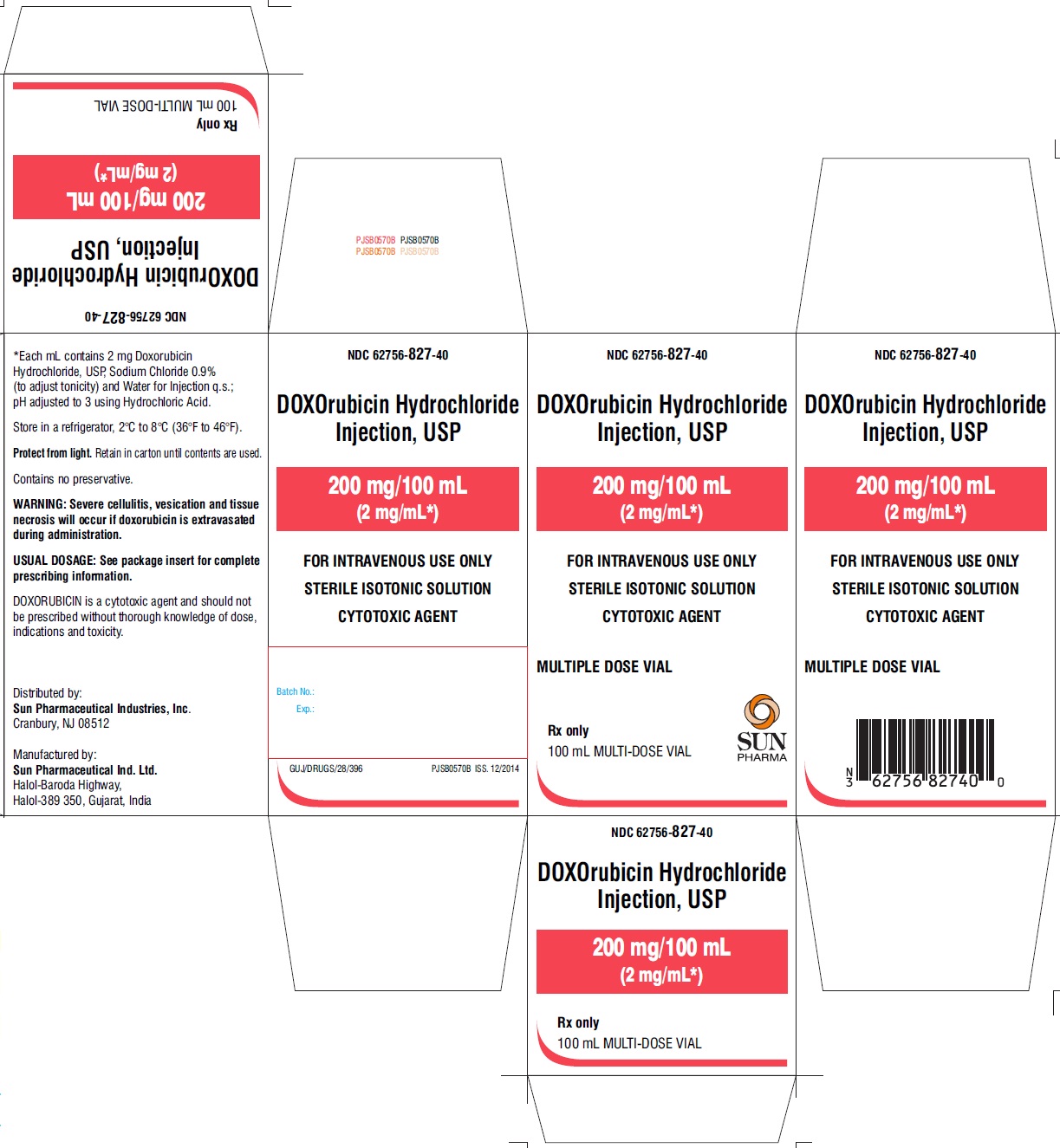
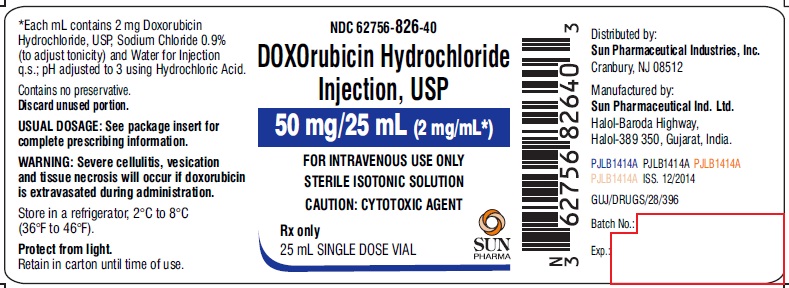
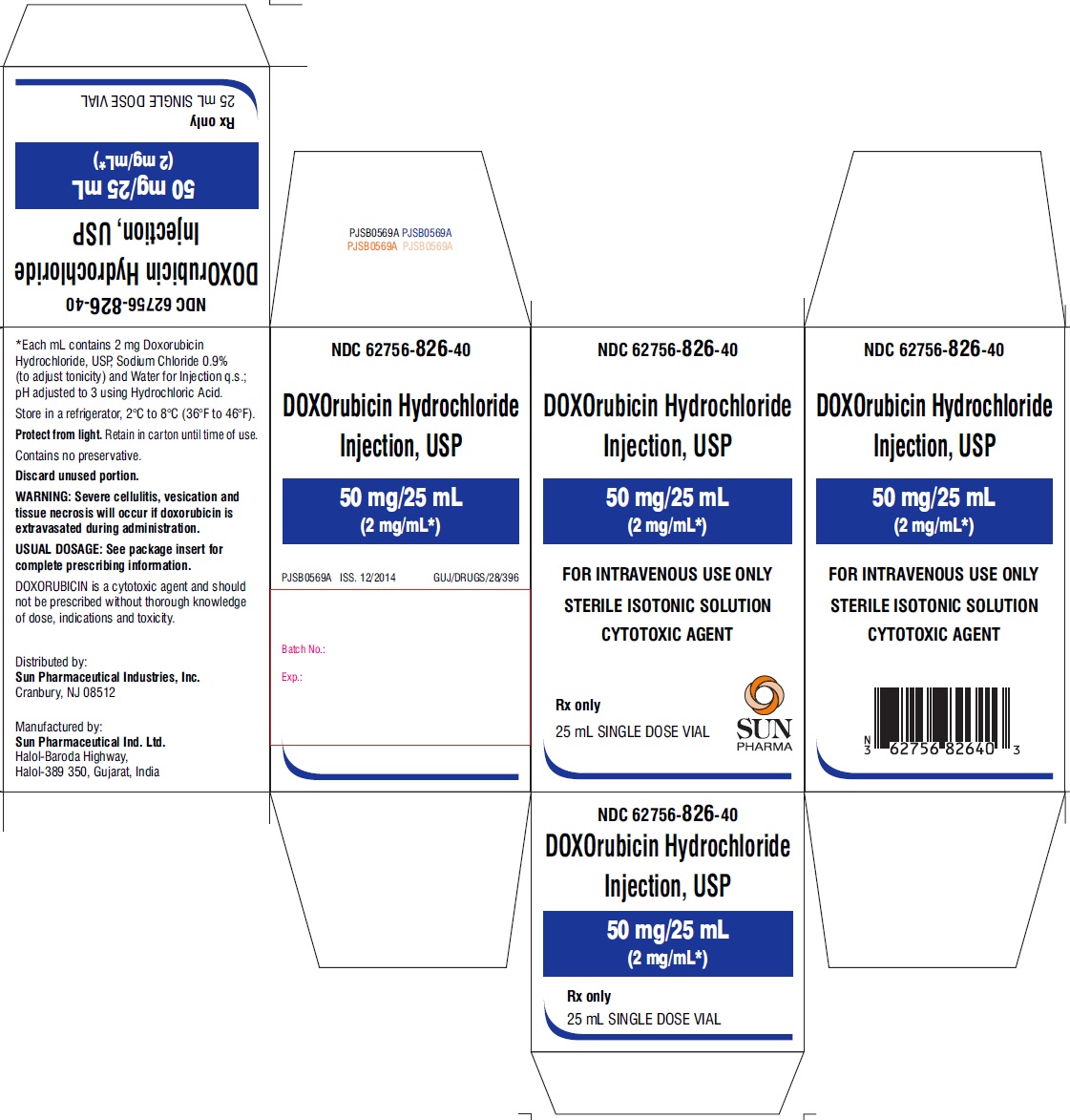
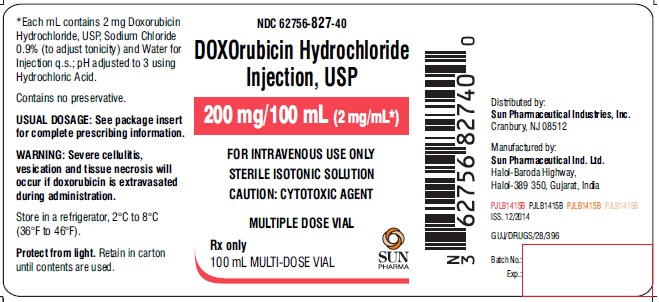
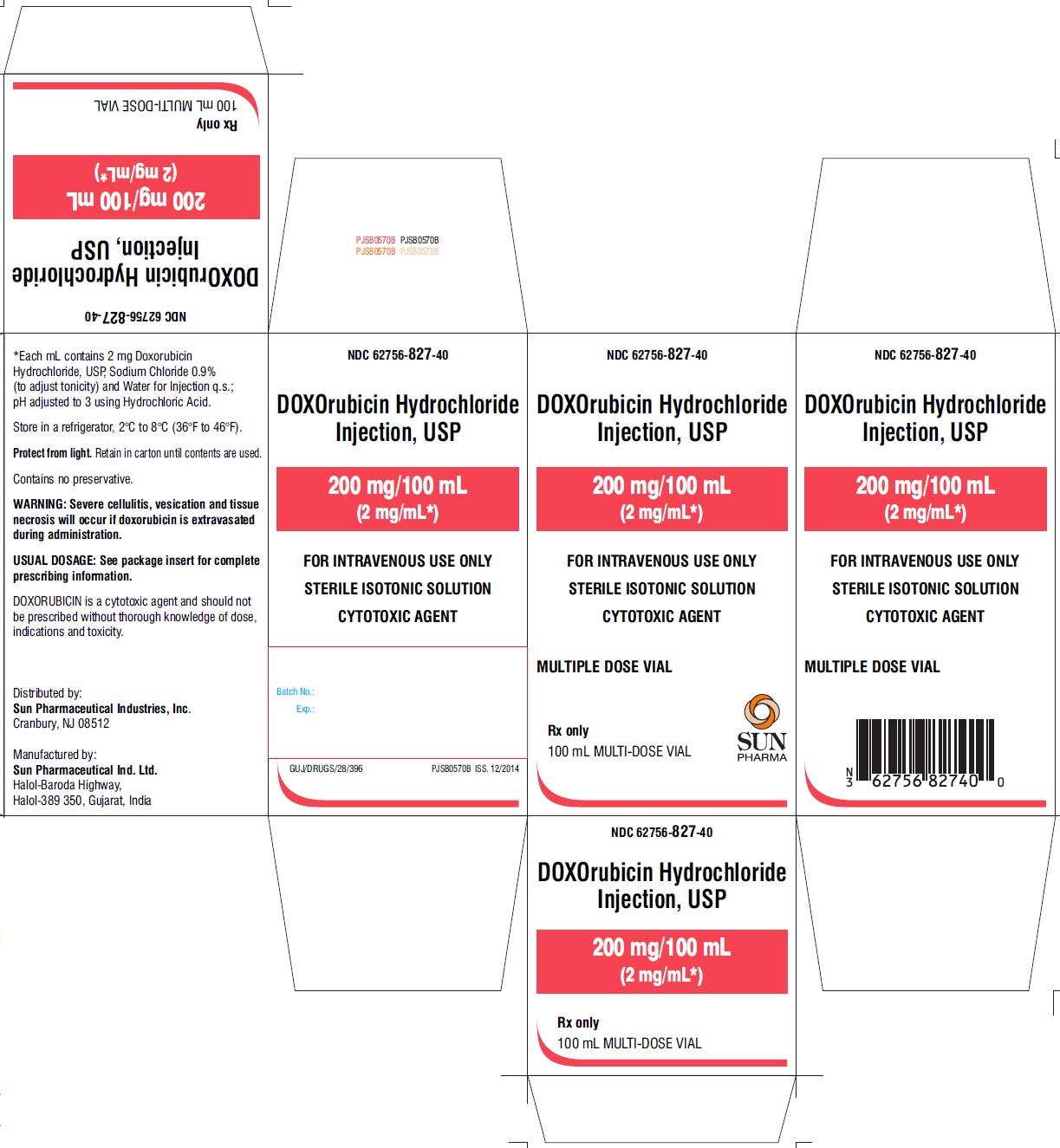
- Doxorubicin hydrochloride injection: Vials contain 50 mg/25 mL, and 200 mg/100 mL as a solution (3)
CONTRAINDICATIONS
- Severe myocardial insufficiency (4)
- Recent myocardial infarction (4)
- Severe persistent drug-induced myelosuppression (4)
- Severe hepatic impairment (4)
- Hypersensitivity to doxorubicin hydrochloride (4)
WARNINGS AND PRECAUTIONS
- Radiation-induced toxicity can be increased by the administration of doxorubicin hydrochloride. Radiation recall can occur in patients who receive doxorubicin hydrochloride after prior radiation therapy (5.7).
- Embryofetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of potential risk to the fetus (5.8).
ADVERSE REACTIONS
DRUG INTERACTIONS
- Avoid concurrent use of doxorubicin hydrochloride with inhibitors and inducers of CYP3A4, CYP2D6, and/or P-gp (7.1).
- Do not administer doxorubicin hydrochloride in combination with trastuzumab due to increased risk of cardiac dysfunction (5.1, 7.2).
USE IN SPECIFIC POPULATIONS
- Nursing Mothers: Discontinue drug or nursing taking into consideration importance of drug to mother (8.3).
- Pediatric Use: Recommend long-term follow-up cardiac evaluations due to risk of delayed cardiotoxicity (8.4).
- Females and Males of Reproductive Potential: May impair fertility. Counsel female and male patients on pregnancy planning and prevention (8.6).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 1/2022
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: CARDIOMYOPATHY, SECONDARY MALIGNANCIES, EXTRAVASATION AND TISSUE NECROSIS, and SEVERE MYELOSUPPRESSION
1 INDICATIONS AND USAGE
1.1 Adjuvant Breast Cancer
1.2 Other Cancers
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose
2.2 Dose Modifications
2.3 Preparation and Administration
2.4 Procedures for Proper Handling and Disposal
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Cardiomyopathy and Arrhythmias
5.2 Secondary Malignancies
5.3 Extravasation and Tissue Necrosis
5.4 Severe Myelosuppression
5.5 Use in Patients with Hepatic Impairment
5.6 Tumor Lysis Syndrome
5.7 Radiation Sensitization and Radiation Recall
5.8 Embryofetal Toxicity
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience in Breast Cancer
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Effect of CYP3A4 Inhibitors, Inducers and P-gp
7.2 Trastuzumab
7.3 Paclitaxel
7.4 Dexrazoxane
7.5 6-Mercaptopurine
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Females and Males of Reproductive Potential
8.7 Hepatic Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
15 REFERENCES
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: CARDIOMYOPATHY, SECONDARY MALIGNANCIES, EXTRAVASATION AND TISSUE NECROSIS, and SEVERE MYELOSUPPRESSION
- Cardiomyopathy: Myocardial damage, including acute left ventricular failure can occur with doxorubicin hydrochloride. The risk of cardiomyopathy is proportional to the cumulative exposure with incidence rates from 1% to 20% for cumulative doses ranging from 300 mg/m2 to 500 mg/m2 when doxorubicin hydrochloride is administered every 3 weeks. The risk of cardiomyopathy is further increased with concomitant cardiotoxic therapy. Assess LVEF before and regularly during and after treatment with doxorubicin hydrochloride [see Warnings and Precautions (5.1)].
- Secondary Malignancies: Secondary acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) occur at a higher incidence in patients treated with anthracyclines, including doxorubicin hydrochloride [see Warnings and Precautions (5.2)].
- Extravasation and Tissue Necrosis: Extravasation of doxorubicin hydrochloride can result in severe local tissue injury and necrosis requiring wide excision of the affected area and skin grafting. Immediately terminate the drug and apply ice to the affected area [see Warnings and Precautions (5.3)].
- Severe myelosuppression resulting in serious infection, septic shock, requirement for transfusions, hospitalization, and death may occur [see Warnings and Precautions (5.4)].
-
1 INDICATIONS AND USAGE
1.1 Adjuvant Breast Cancer
DOXOrubicin hydrochloride injection, USP is indicated as a c omponent of multi-a gent adjuvant chemotherapy for treat ment of wo men with axillary lymph node involve ment following resection of pri mary breast cancer [see Clinical Studies (14.1 ) ].
1.2 Other Cancers
DOXOrubicin hydrochloride injection, USP is indicated for the treat ment of
- acute ly mphoblastic leu ke mia
- acute m yeloblastic leuke mia
- Hodgkin lympho ma
- non-Hodgkin ly mpho ma (NHL)
- metastatic breast cancer
- metastatic Wil ms’ tumor
- metastatic neurobla stoma
- metastatic s oft tissue sa rco ma
- metastatic bone sarco ma
- metastatic o varian car cino ma
- metastatic t ransitional c ell bladder carcino ma
- metastatic t hyroid carcinoma
- metastatic gastric carcinoma
- metastatic bronchogenic carcinoma
-
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose
Adjuvant Breast Cancer
The recommended dose of doxorubicin hydrochloride is 60 mg/m2 administered as an intravenous bolus on day 1 of each 21-day treatment cycle, in combination with cyclophosphamide, for a total of four cycles [see Clinical Studies (14)].
Metastatic Disease, Leukemia, or Lymphoma
- The recommended dose of doxorubicin hydrochloride when used as a single agent is 60 to 75 mg/m2 intravenously every 21 days.
- The recommended dose of doxorubicin hydrochloride, when administered in combination with other chemotherapy drugs, is 40 to 75 mg/m2 intravenously every 21 to 28 days.
- Consider use of the lower doxorubicin dose in the recommended dose range or longer intervals between cycles for heavily pretreated patients, elderly patients, or obese patients.
- Cumulative doses above 550 mg/m2 are associated with an increased risk of cardiomyopathy [see Warnings and Precautions (5.1)].
2.2 Dose Modifications
Cardiac Impairment
Discontinue doxorubicin in patients who develop signs or symptoms of cardiomyopathy.
Hepatic Impairment
Doxorubicin hydrochloride is contraindicated in patients with severe hepatic impairment (Child-Pugh Class C or serum bilirubin >5 mg/dL) [see Contraindications (4)].
Decrease the dose of doxorubicin hydrochloride in patients with elevated serum total bilirubin concentrations as follows:
Serum bilirubin concentration
Doxorubicin Hydrochloride Dose reduction
1.2 to 3 mg/dL
50 %
3.1 to 5 mg/dL
75 %
greater than 5 mg/dL
Do not initiate doxorubicin hydrochloride
Discontinue doxorubicin hydrochloride
[see Warnings and Precautions (5.5) and Use in Specific Population (8.7)]
2.3 Preparation and Administration
Preparation for Continuous Intravenous Infusion
Dilute doxorubicin hydrochloride solution in 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP. Protect from light following preparation until completion of infusion.
Administration
Visually inspect parenteral drug products for particulate matter and discoloration prior to administration, whenever solution and container permit. Discard if the solution is discolored, cloudy, or contains particulate matter.
Storage of vials of doxorubicin hydrochloride injection under refrigerated conditions can result in the formation of a gelled product. Place gelled product at room temperature [15º to 30ºC (59º to 86ºF)] for 2 to 4 hours to return the product to a slightly viscous, mobile solution.
Administration by Intravenous Injection:
- Administer doxorubicin hydrochloride as an intravenous injection through a central intravenous line or a secure and free-flowing peripheral venous line containing 0.9% Sodium Chloride Injection, USP, 0.45% Sodium Chloride Injection, USP, or 5% Dextrose Injection, USP.
- Administer doxorubicin hydrochloride intravenously over 3 to 10 minutes. Decrease the rate of doxorubicin hydrochloride administration if erythematous streaking along the vein proximal to the site of infusion or facial flushing occur.
Administration by Continuous Intravenous Infusion:
- Infuse only through a central catheter. Decrease the rate of doxorubicin hydrochloride administration if erythematous streaking along the vein proximal to the site of infusion or facial flushing occur.
- Protect from light from preparation for infusion until completion of infusion.
Management of Suspected Extravasation
Discontinue doxorubicin hydrochloride for burning or stinging sensation or other evidence indicating perivenous infiltration or extravasation. Manage confirmed or suspected extravasation as follows:
- Do not remove the needle until attempts are made to aspirate extravasated fluid.
- Do not flush the line.
- Avoid applying pressure to the site.
- Apply ice to the site intermittently for 15 min 4 times a day for 3 days.
- If the extravasation is in an extremity, elevate the extremity.
- In adults, consider administration of dexrazoxane [see Warnings and Precautions (5.3)].
Incompatibility with Other Drugs
Do not admix doxorubicin hydrochloride with other drugs. If doxorubicin hydrochloride is mixed with heparin or fluorouracil a precipitate may form. Avoid contact with alkaline solutions which can lead to hydrolysis of doxorubicin hydrochloride.
2.4 Procedures for Proper Handling and Disposal
Handle and dispose of doxorubicin hydrochloride consistent with recommendations for the handling and disposal of hazardous drugs.1
Treat accidental contact with the skin or eyes immediately by copious lavage with water, or soap and water, or sodium bicarbonate solution. Do not abrade the skin by using a scrub brush. Seek medical attention.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Doxorubicin hydrochloride is contraindicated in patients with:
- Severe myocardial insufficiency [see Warnings and Precautions (5.1)]
- Recent (occurring within the past 4 to 6 weeks) myocardial infarction [see Warnings and Precautions (5.1)]
- Severe persistent drug-induced myelosuppression [see Warnings and Precautions (5.4)]
- Severe hepatic impairment (defined as Child Pugh Class C or serum bilirubin level greater than 5 mg/dL) [see Warnings and Precautions (5.5)]
- Severe hypersensitivity reaction to doxorubicin hydrochloride including anaphylaxis [see Adverse Reactions (6.2)]
-
5 WARNINGS AND PRECAUTIONS
5.1 Cardiomyopathy and Arrhythmias
Cardiomyopathy
Doxorubicin hydrochloride can result in myocardial damage, including acute left ventricular failure. The risk of cardiomyopathy is generally proportional to the cumulative exposure. Include prior doses of other anthracyclines or anthracenediones in calculations of total cumulative dosage for doxorubicin hydrochloride. Cardiomyopathy may develop during treatment or up to several years after completion of treatment and can include decrease in LVEF and signs and symptoms of congestive heart failure (CHF). The probability of developing cardiomyopathy is estimated to be 1 to 2% at a total cumulative dose of 300 mg/m2 of doxorubicin hydrochloride, 3 to 5% at a dose of 400 mg/m2, 5 to 8% at a dose of 450 mg/m2, and 6 to 20% at a dose of 500 mg/m2, when doxorubicin hydrochloride is administered every 3 weeks. There is an additive or potentially synergistic increase in the risk of cardiomyopathy in patients who have received radiotherapy to the mediastinum or concomitant therapy with other known cardiotoxic agents such as cyclophosphamide and trastuzumab.
Pericarditis and myocarditis have also been reported during or following doxorubicin hydrochloride treatment.
Assess left ventricular cardiac function (e.g., MUGA or echocardiogram) prior to initiation of doxorubicin hydrochloride, during treatment to detect acute changes, and after treatment to detect delayed cardiotoxicity. Increase the frequency of assessments as the cumulative dose exceeds 300 mg/m2. Use the same method of assessment of LVEF at all time points [see Use in Specific Populations (8.4)].
Consider the use of dexrazoxane to reduce the incidence and severity of cardiomyopathy due to doxorubicin hydrochloride administration in patients who have received a cumulative doxorubicin hydrochloride dose of 300 mg/m2 and who will continue to receive doxorubicin hydrochloride.
Arrhythmias
Doxorubicin hydrochloride can result in arrhythmias, including life-threatening arrhythmias, during or within a few hours after doxorubicin hydrochloride administration and at any time point during treatment. Tachyarrhythmias, including sinus tachycardia, premature ventricular contractions, and ventricular tachycardia, as well as bradycardia may occur. Electrocardiographic changes including non-specific ST-T wave changes, atrioventricular and bundle-branch block can also occur. These electrocardiographic changes may be transient and self-limited and may not require dose-modifications of doxorubicin hydrochloride.
5.2 Secondary Malignancies
The risk of developing secondary acute myelogenous leukemia (AML) and myelodysplastic syndrome (MDS) is increased following treatment with doxorubicin hydrochloride. Cumulative incidences ranged from 0.2% at five years to 1.5% at 10 years in two separate trials involving the adjuvant treatment of women with breast cancer. These leukemias generally occur within 1 to 3 years of treatment.
5.3 Extravasation and Tissue Necrosis
Extravasation of doxorubicin hydrochloride can result in severe local tissue injury manifesting as blistering, ulceration, and necrosis requiring wide excision of the affected area and skin grafting. When given via a peripheral venous line, infuse doxorubicin over 10 minutes or less to minimize the risk of thrombosis or perivenous extravasation. If signs or symptoms of extravasation occur, immediately terminate the injection or infusion [see Dosage and Administration (2.3)]. Extravasation may be present in patients who do not experience a stinging or burning sensation or when blood return is present on aspiration of the infusion needle. If extravasation is suspected, apply ice to the site intermittently for 15 minutes, 4 times a day for 3 days. If appropriate, administer dexrazoxane at the site of extravasation as soon as possible and within the first 6 hours after extravasation.
5.4 Severe Myelosuppression
Doxorubicin hydrochloride can cause myelosuppression. In Study 1, the incidence of severe myelosuppression was: grade 4 leukopenia (0.3%), grade 3 leukopenia (3%), and grade 4 thrombocytopenia (0.1%). A dose-dependent, reversible neutropenia is the predominant manifestation of hematologic toxicity from doxorubicin hydrochloride. When doxorubicin hydrochloride is administered every 21 days, the neutrophil count reaches its nadir 10 to 14 days after administration with recovery usually occurring by the 21st day.
Obtain baseline assessment of blood counts and carefully monitor patients during treatment for possible clinical complications due to myelosuppression.
5.5 Use in Patients with Hepatic Impairment
The clearance of doxorubicin is decreased in patients with elevated serum bilirubin with an increased risk of toxicity [see Use in Specific Populations (8.7) and Clinical Pharmacology (12.3)]. Reduce the dose of doxorubicin hydrochloride in patients with serum bilirubin levels of 1.2 to 5 mg/dL [see Dosage and Administration (2.2)]. Doxorubicin is contraindicated in patients with severe hepatic impairment (defined as Child Pugh Class C or serum bilirubin level greater than 5 mg/dL) [see Contraindications (4)]. Obtain liver tests including SGOT, SGPT, alkaline phosphatase, and bilirubin prior to and during doxorubicin hydrochloride therapy.
5.6 Tumor Lysis Syndrome
Doxorubicin hydrochloride may induce tumor lysis syndrome in patients with rapidly growing tumors. Evaluate blood uric acid levels, potassium, calcium, phosphate, and creatinine after initial treatment. Hydration, urine alkalinization, and prophylaxis with allopurinol to prevent hyperuricemia may minimize potential complications of tumor lysis syndrome.
5.7 Radiation Sensitization and Radiation Recall
Doxorubicin hydrochloride can increase radiation-induced toxicity to the myocardium, mucosa, skin, and liver. Radiation recall, including but not limited to cutaneous and pulmonary toxicity, can occur in patients who receive doxorubicin hydrochloride after prior radiation therapy.
5.8 Embryofetal Toxicity
Doxorubicin hydrochloride can cause fetal harm when administered to a pregnant woman. Doxorubicin hydrochloride was teratogenic and embryotoxic in rats and rabbits at doses lower than the recommended human dose.
If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus [see Use in Specific Populations (8.1)].
Advise female patients of reproductive potential to use highly effective contraception during treatment with doxorubicin hydrochloride and for 6 months after treatment. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking doxorubicin hydrochloride [see Use in Specific Populations (8.1) and (8.6)].
-
6 ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections of the labeling.
- Cardiomyopathy and Arrhythmias [see Warnings and Precautions (5.1)]
- Secondary Malignancies [see Warnings and Precautions (5.2)]
- Extravasation and Tissue Necrosis [see Warnings and Precautions (5.3)]
- Severe Myelosuppression [see Warnings and Precautions (5.4)]
- Tumor Lysis Syndrome [see Warnings and Precautions (5.6)]
- Radiation Sensitization and Radiation Recall [see Warnings and Precautions (5.7)]
6.1 Clinical Trial Experience in Breast Cancer
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety data below were collected from 1492 women who received doxorubicin hydrochloride at a dose of 60 mg/m2 and cyclophosphamide at a dose of 600 mg/m2 (AC) every 3 weeks for 4 cycles for the adjuvant treatment of axillary lymph node positive breast cancer. The median number of cycles received was 4. Selected adverse reactions reported in this study are provided in Table 1. No treatment-related deaths were reported in patients on either arm of the study.
- *
- Includes pooled data from patients who received either AC alone for 4 cycles, or who were treated with AC for 4 cycles followed by 3 cycles of CMF
Table 1. Selected Adverse Reactions in Patients with Early Breast
Cancer Involving Axillary Lymph Nodes
AC*
Conventional
CMF
N=1492
N=739
Adverse reactions, % of patients
Leukopenia
Grade 3 (1,000 to 1,999 /mm3)
3.4
9.4
Grade 4 (<1000 /mm3)
0.3
0.3
Thrombocytopenia
Grade 3 (25,000 to 49,999 /mm3)
0
0.3
Grade 4 (<25,000 /mm3)
0.1
0
Shock, sepsis
2
1
Systemic infection
2
1
Vomiting
Vomiting ≤12 hours
34
25
Vomiting >12 hours
37
12
Intractable
5
2
Alopecia
92
71
Cardiac dysfunction
Asymptomatic
0.2
0.1
Transient
0.1
0
Symptomatic
0.1
0
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of doxorubicin hydrochloride. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiac – cardiogenic shock
Cutaneous – Skin and nail hyperpigmentation, oncolysis, rash, itching, photosensitivity, urticaria, acral erythema, palmar plantar erythrodysesthesia
Gastrointestinal – Nausea, mucositis, stomatitis, necrotizing colitis, typhlitis, gastric erosions, gastrointestinal tract bleeding, hematochezia, esophagitis, anorexia, abdominal pain, dehydration, diarrhea, hyperpigmentation of the oral mucosa
Hypersensitivity – Anaphylaxis
Laboratory Abnormalities – Increased alanine aminotransferase, increased aspartate aminotransferase
Neurological – Peripheral sensory and motor neuropathy, seizures, coma
Ocular – Conjunctivitis, keratitis, lacrimation
Vascular – Phlebosclerosis, phlebitis/thrombophlebitis, hot flashes, thromboembolism
Other – Malaise/asthenia, fever, chills, weight gain
-
7 DRUG INTERACTIONS
7.1 Effect of CYP3A4 Inhibitors, Inducers and P-gp
Doxorubicin is a major substrate of cytochrome P450 CYP3A4 and CYP2D6, and P-glycoprotein (P-gp). Clinically significant interactions have been reported with inhibitors of CYP3A4, CYP2D6, and/or P-gp (e.g., verapamil), resulting in increased concentration and clinical effect of doxorubicin. Inducers of CYP3A4 (e.g., phenobarbital, phenytoin, St. John’s Wort) and P-gp inducers may decrease the concentration of doxorubicin. Avoid concurrent use of doxorubicin hydrochloride with inhibitors and inducers of CYP3A4, CYP2D6, or P-gp.
7.2 Trastuzumab
Concurrent use of trastuzumab and doxorubicin hydrochloride results in an increased risk of cardiac dysfunction. Avoid concurrent administration of doxorubicin and trastuzumab. The appropriate interval for administering doxorubicin following trastuzumab therapy has not been determined [see Warnings and Precautions (5.1)].
7.3 Paclitaxel
Paclitaxel, when given prior to doxorubicin hydrochloride, increases the plasma-concentrations of doxorubicin and its metabolites. Administer doxorubicin hydrochloride prior to paclitaxel if used concomitantly.
7.4 Dexrazoxane
Do not administer dexrazoxane as a cardioprotectant at the initiation of doxorubicin hydrochloridecontaining chemotherapy regimens. In a randomized trial in women with metastatic breast cancer, initiation of dexrazoxane with doxorubicin hydrochloride-based chemotherapy resulted in a significantly lower tumor response rate (48% vs. 63%; p=0.007) and shorter time to progression than in women who received doxorubicin hydrochloride-based chemotherapy alone.
7.5 6-Mercaptopurine
Doxorubicin hydrochloride may potentiate 6-mercaptopurine-induced hepatotoxicity. In 11 patients with refractory leukemia treated with 6-mercaptopurine (500 mg/m2 intravenously daily for 5 days per cycle every 2 to 3 weeks) and doxorubicin hydrochloride (50 mg/m2 intravenous once per cycle every 2 to 3 weeks) alone or with vincristine and prednisone, all developed hepatic dysfunction manifested by elevations of total serum bilirubin, alkaline phosphatase and aspartate aminotransferase.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category D
Risk Summary
Doxorubicin hydrochloride can cause fetal harm when administered to a pregnant woman. Doxorubicin hydrochloride was teratogenic and embryotoxic in rats and rabbits at doses approximately 0.07 times (based on body surface area) the recommended human dose of 60 mg/m2. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus.
Animal Data
Doxorubicin hydrochloride was teratogenic and embryotoxic at doses of 0.8 mg/kg/day (about 0.07 times the recommended human dose based on body surface area) when administered during the period of organogenesis in rats. Teratogenicity and embryotoxicity were also seen using discrete periods of treatment. The most susceptible was the 6- to 9-day gestation period at doses of 1.25 mg/kg/day and greater. Characteristic malformations included esophageal and intestinal atresia, tracheo-esophageal fistula, hypoplasia of the urinary bladder, and cardiovascular anomalies. Doxorubicin hydrochloride was embryotoxic (increase in embryofetal deaths) and abortifacient at 0.4 mg/kg/day (about 0.07 times the recommended human dose based on body surface area) in rabbits when administered during the period of organogenesis.
8.3 Nursing Mothers
Doxorubicin has been detected in the milk of at least one lactating patient [see Clinical Pharmacology (12.3)]. Because of the potential for serious adverse reactions in nursing infants from doxorubicin hydrochloride, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Based on postmarketing reports, pediatric patients treated with doxorubicin hydrochloride are at risk for developing late cardiovascular dysfunction. Risk factors include young age at treatment (especially < 5 years), high cumulative doses and receipt of combined modality therapy. Long-term periodic cardiovascular monitoring is recommended for all pediatric patients who have received doxorubicin hydrochloride. Doxorubicin hydrochloride, as a component of intensive chemotherapy regimens administered to pediatric patients, may contribute to prepubertal growth failure and may also contribute to gonadal impairment, which is usually temporary.
There are no recommended dose adjustments based on age. Doxorubicin clearance was increased in patients aged 2 years to 20 years as compared to adults, while doxorubicin clearance was similar in children less than 2 years as compared to adults [see Clinical Pharmacology (12.3)].
8.5 Geriatric Use
Clinical experience in patients who were 65 years of age and older who received doxorubicin hydrochloride-based chemotherapy regimens for metastatic breast cancer showed no overall differences in safety and effectiveness compared with younger patients.
8.6 Females and Males of Reproductive Potential
Contraception
Females
Doxorubicin hydrochloride can cause fetal harm when administered during pregnancy. Advise female patients of reproductive potential to use highly effective contraception during treatment with doxorubicin hydrochloride and for 6 months after treatment. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking doxorubicin hydrochloride [see Use in Specific Populations (8.1)].
Males
Doxorubicin hydrochloride may damage spermatozoa and testicular tissue, resulting in possible genetic fetal abnormalities. Males with female sexual partners of reproductive potential should use effective contraception during and for 6 months after treatment [see Nonclinical Toxicology (13.1)].
Infertility
Females
In females of reproductive potential, doxorubicin hydrochloride may cause infertility and result in amenorrhea. Premature menopause can occur. Recovery of menses and ovulation is related to age at treatment [see Nonclinical Toxicology (13.1)].
Males
Doxorubicin hydrochloride may result in oligospermia, azoospermia, and permanent loss of fertility. Sperm counts have been reported to return to normal levels in some men. This may occur several years after the end of therapy.
8.7 Hepatic Impairment
The clearance of doxorubicin was reduced in patients with elevated serum bilirubin levels. Reduce the dose of doxorubicin hydrochloride in patients with serum bilirubin levels greater than 1.2 mg/dL [See Dosage and Administration (2.2) and Warnings and Precautions (5.5)].
Doxorubicin hydrochloride is contraindicated in patients with severe hepatic impairment (defined as Child Pugh Class C or serum bilirubin levels greater than 5 mg/dL) [see Contraindications (4)].
-
10 OVERDOSAGE
Few cases of overdose have been described. A 58-year-old man with acute lymphoblastic leukemia received 10-fold overdose of doxorubicin hydrochloride (300 mg/m2) in one day. He was treated with charcoal filtration, hemopoietic growth factor (G-CSF), proton pump inhibitor and antimicrobial prophylaxis. The patient suffered sinus tachycardia, grade 4 neutropenia and thrombocytopenia for 11 days, severe mucositis and sepsis. The patient recovered completely 26 days after the overdose. A 17-year-old girl with osteogenic sarcoma received 150 mg of doxorubicin hydrochloride daily for 2 days (intended dose was 50 mg per day for 3 days). The patient developed severe mucositis on days 4 to 7 after the overdose and chills and pyrexia on day 7. The patient was treated with antibiotics and platelets and recovered 18 days after overdose.
-
11 DESCRIPTION
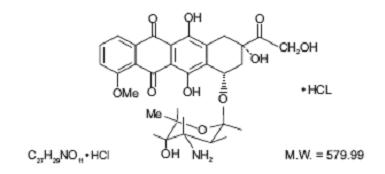
Doxorubicin hydrochloride is a cytotoxic, anthracycline, topoisomerase II inhibitor isolated from cultures of Streptomyces peucetius var. caesius. Chemically, doxorubicin hydrochloride is: 5,12-Naphthacenedione, 10-[(3-amino-2,3,6-trideoxy-α-L-lyxo-hexopyranosyl)oxy]-7,8,9,10 tetrahydro-6,8,11-trihydroxy-8-(hydroxylacetyl)-1-methoxy-, hydrochloride (8S-cis)-. The chemical structure of doxorubicin hydrochloride is:
DOXOrubicin hydrochloride injection, USP is a clear, red-orange, sterile, isotonic aqueous solution provided in vials containing 50 mg/25 mL or 200 mg/100 mL of doxorubicin hydrochloride. The drug product has demonstrated inherent antimicrobial activity suitable for a multiple dose presentation. Each milliliter of solution contains 2 mg of doxorubicin hydrochloride. Inactive ingredients include sodium chloride 0.9% and water for injection quantity sufficient. The pH of the solution is adjusted to 3 with hydrochloric acid.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The cytotoxic effect of doxorubicin hydrochloride on malignant cells and its toxic effects on various organs are thought to be related to nucleotide base intercalation and cell membrane lipid binding activities of doxorubicin. Intercalation inhibits nucleotide replication and action of DNA and RNA polymerases. The interaction of doxorubicin with topoisomerase II to form DNA-cleavable complexes appears to be an important mechanism of doxorubicin hydrochloride cytocidal activity.
12.3 Pharmacokinetics
Pharmacokinetic studies conducted in patients with various types of tumors have shown that doxorubicin follows multiphasic disposition after intravenous injection. The distribution half-life is approximately 5 minutes, while the terminal half-life is 20 to 48 hours. In four patients, doxorubicin demonstrated dose-independent pharmacokinetics across a dose range of 30 to 70 mg/m2.
Distribution
Steady-state distribution volume ranges from 809 to 1214 L/m2. Binding of doxorubicin and its major metabolite, doxorubicinol, to plasma proteins is about 75% and is independent of plasma concentration of doxorubicin up to 1.1 mcg/mL.
Doxorubicin was measured in the milk of one lactating patient after therapy with 70 mg/m2 of doxorubicin hydrochloride given as a 15-minute intravenous infusion. The peak milk concentration at 24 hours after treatment was 4.4-fold greater than the corresponding plasma concentration.
Doxorubicin was detectable in the milk up to 72 hours.
Doxorubicin does not cross the blood brain barrier.
Metabolism
Enzymatic reduction at the 7 position and cleavage of the daunosamine sugar yields aglycones which are accompanied by free radical formation, the local production of which may contribute to the cardiotoxic activity of doxorubicin hydrochloride. Disposition of doxorubicinol in patients is formation rate limited, with the terminal half-life of doxorubicinol being similar to doxorubicin. The relative exposure of doxorubicinol, i.e., the ratio between the AUC of doxorubicinol and the AUC of doxorubicin is approximately 0.5.
Excretion
Plasma clearance is in the range 324 to 809 mL/min/m2 and is predominately by metabolism and biliary excretion. Approximately 40% of the dose appears in the bile in 5 days, while only 5 to 12% of the drug and its metabolites appear in the urine during the same time period. In urine, <3% of the dose was recovered as doxorubicinol over 7 days.
Systemic clearance of doxorubicin is significantly reduced in obese women with ideal body weight greater than 130%. There was a significant reduction in clearance without any change in volume of distribution in obese patients when compared with normal patients with less than 115% ideal body weight.
Pediatric patients
Following administration of doses ranging from 10 to 75 mg/m2 of doxorubicin hydrochloride to 60 children and adolescents ranging from 2 months to 20 years of age, doxorubicin clearance averaged 1443 ± 114 mL/min/m2. Further analysis demonstrated that clearance in 52 children greater than 2 years of age (1540 mL/min/m2) was increased compared with adults. However, clearance in infants younger than 2 years of age (813 mL/min/m2) was decreased compared with older children and approached the range of clearance values determined in adults [see Use in Specific Populations (8.4)].
Patient Gender
There is no recommended dose adjustment based on gender. A published clinical study involving 6 men and 21 women with no prior anthracycline therapy reported a significantly higher median doxorubicin clearance in men compared to women (1088 mL/min/m2 versus 433 mL/min/m2). However, the terminal half-life of doxorubicin was longer in men compared to women (54 versus 35 hours).
Patients with hepatic impairment
The clearance of doxorubicin and doxorubicinol was reduced in patients with elevation in serum bilirubin [see Dosage and Administration (2.2) and Warnings and Precautions (5.5)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Doxorubicin hydrochloride treatment results in an increased risk of secondary malignancies based on postmarketing reports [see Warnings and Precautions (5.2)]. Doxorubicin hydrochloride was mutagenic in the in vitro Ames assay, and clastogenic in multiple in vitro assays (CHO cell, V79 hamster cell, human lymphoblast, and SCE assays) and the in vivo mouse micronucleus assay.
Doxorubicin hydrochloride decreased fertility in female rats at the doses of 0.05 and 0.2 mg/kg/day (approximately 0.005 and 0.02 times the recommended human dose, based on body surface area).
A single intravenous dose of 0.1 mg/kg doxorubicin hydrochloride (approximately 0.01 times the recommended human dose based on body surface area) was toxic to male reproductive organs in animal studies, producing testicular atrophy, diffuse degeneration of the seminiferous tubules, and oligospermia/hypospermia in rats. Doxorubicin hydrochloride induces DNA damage in rabbit spermatozoa and dominant lethal mutations in mice.
-
14 CLINICAL STUDIES
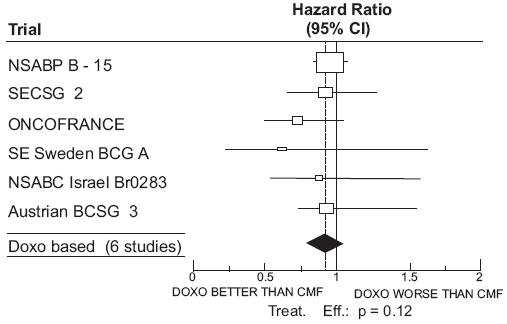
The clinical efficacy of doxorubicin hydrochloride-containing regimens for the post-operative, adjuvant treatment of surgically resected breast cancer was evaluated in a meta-analysis conducted by the Early Breast Cancer Trialists Collaborative Group (EBCTCG). The EBCTCG meta-analyses compared cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) to no chemotherapy (19 trials including 7,523 patients) and doxorubicin hydrochloride-containing regimens with CMF as an active control (6 trials including 3,510 patients). Data from the meta-analysis of trials comparing CMF to no therapy were used to establish the historical treatment effect size for CMF regimens. The major efficacy outcome measures were disease-free survival (DFS) and overall survival (OS).
Of the 3,510 women (2,157 received doxorubicin hydrochloride-containing regimens and 1,353 received CMF treatment) with early breast cancer involving axillary lymph nodes included in the six trials from the meta-analyses, approximately 70% were premenopausal and 30% were postmenopausal. At the time of the meta-analysis, 1,745 first recurrences and 1,348 deaths had occurred. The analyses demonstrated that doxorubicin hydrochloride-containing regimens retained at least 75% of the historical CMF adjuvant effect on DFS with a hazard ratio (HR) of 0.91 (95% CI, 0.82 to 1.01) and on OS with a HR of 0.91 (95% CI, 0.81 to 1.03). Results of these analyses for both DFS and OS are provided in Table 2 and Figures 1 and 2.
Table 2. Summary of Randomized Trials Comparing Doxorubicin Hydrochloride-Containing Regimens Versus CMF in Meta-Analysis - *
- a hazard ratio of less than 1 indicates that the treatment with doxorubicin hydrochloride-containing regimens is associated with lower risk of disease recurrences or death compared to the treatment with CMF.
- †
- Includes pooled data from patients who received either AC alone for 4 cycles, or who were treated with AC for 4 cycles followed by 3 cycles of CMF.
- ‡
- Patients received alternating cycles of AVb and CMF.
Study
(starting year)
Regimens
No. of Cycles
No. of Patients
Doxorubicin Hydrochloride-Containing
Regimens vs. CMF HR* (95% CI)
DFS
OS
NSABP B-15
(1984)
AC
4
1,562†
0.93 (0.82 to 1.06)
0.97 (0.83 to 1.12)
CMF
6
776
SECSG 2
(1976)
FAC
6
260
0.86 (0.66 to 1.13)
0.93 (0.69 to 1.26)
CMF
6
268
ONCOFRANCE
(1978)
FACV
12
138
0.71 (0.49 to 1.03)
0.65 (0.44 to 0.96)
CMF
12
113
SE Sweden BCG A
(1980)
AC
6
21
0.59 (0.22 to 1.61)
0.53 (0.21 to 1.37)
CMF
6
22
NSABC Israel Br0283
(1983)
AVbCMF‡
4
6
55
0.91 (0.53 to 1.57)
0.88 (0.47 to 1.63)
CMF
6
50
Austrian BCSG 3
(1984)
CMFVA
6
121
1.07 (0.73 to 1.55)
0.93 (0.64 to 1.35)
CMF
8
124
Combined Studies
Doxorubicin Hydrochloride-Containing Regimens
2,157
0.91 (0.82 to 1.01)
0.91 (0.81 to 1.03)
CMF
1,353
Abbreviations: DFS = disease free survival; OS = overall survival; AC = doxorubicin hydrochloride, cyclophosphamide; AVbCMF = doxorubicin hydrochloride, vinblastine, cyclophosphamide, methotrexate, 5-fluorouracil; CMF = cyclophosphamide, methotrexate, 5-fluorouracil; CMFVA = cyclophosphamide, methotrexate, 5-fluorouracil, vincristine, doxorubicin hydrochloride; FAC = 5-fluorouracil, doxorubicin hydrochloride, cyclophosphamide; FACV = 5-fluorouracil, doxorubicin hydrochloride, cyclophosphamide, vincristine; HR = hazard ratio; CI = confidence interval
Figure 1. Meta-analysis of Disease-Free Survival
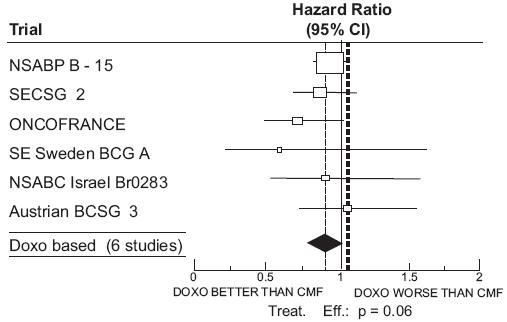
Figure 2. Meta-analysis of Overall Survival
- 15 REFERENCES
-
16 HOW SUPPLIED/STORAGE AND HANDLING
DOXOrubicin hydrochloride injection, USP is supplied in single-dose, colorless molded vial, with teflon coated gray chlorobutyl rubber stopper sealed with light blue flip-off aluminum seal, as a red-orange solution containing doxorubicin hydrochloride, USP 2 mg/mL in the following package strength:
NDC 62756-826-40: 50 mg in a 25 mL vial; individually boxed.
Store in a refrigerator, 2°C to 8°C (36°F to 46°F).
Protect from light. Retain in carton until time of use. Contains no preservative. Discard unused portion.
DOXOrubicin hydrochloride injection, USP is supplied in a sterile, multiple dose, colorless molded vial with gray chlorobutyl rubber stopper sealed with light blue flip-off aluminum seal, as a red-orange solution containing doxorubicin hydrochloride, USP 2 mg/mL in the following package strength:
NDC 62756-827-40: 200 mg in a 100 mL vial; individually boxed.
Store in a refrigerator, 2°C to 8°C (36°F to 46°F).
Protect from light. Retain in carton until contents are used. Contains no preservative.
Storage of doxorubicin hydrochloride injection under refrigerated conditions can result in the formation of a gelled product. Place gelled product at room temperature [15º to 30ºC (59º to 86ºF)] for 2 to 4 hours to return the product to a slightly viscous, mobile solution.
Handling and Disposal
Handle and dispose of doxorubicin hydrochloride injection consistent with recommendations for the handling and disposal of hazardous drugs.1
-
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling (Patient Information).
Inform patients of the following:
- Doxorubicin hydrochloride can cause irreversible myocardial damage. Advise patients to contact a healthcare provider for symptoms of heart failure during or after treatment with doxorubicin hydrochloride [see Warnings and Precautions (5.1)].
- There is an increased risk of treatment-related leukemia from doxorubicin hydrochloride [see Warnings and Precautions (5.2)].
- Doxorubicin hydrochloride can reduce the absolute neutrophil count resulting in an increased risk of infection. Advise patients to contact a healthcare provider for new onset fever or symptoms of infection [see Warnings and Precautions (5.4)].
- Doxorubicin hydrochloride can cause fetal harm when administered during pregnancy. Advise females of reproductive potential to use effective contraception during treatment with doxorubicin hydrochloride and for 6 months after treatment, and to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, during treatment with doxorubicin hydrochloride [see Warnings and Precautions (5.8) and Use in Specific Populations (8.6)].
- Doxorubicin hydrochloride may induce chromosomal damage in sperm, which may lead to loss of fertility and offspring with birth defects. Advise patients to use effective contraception during and for 6 months after treatment [see Warnings and Precautions (5.8 and Use in Specific Populations (8.6)].
- Doxorubicin hydrochloride can cause premature menopause in females and loss of fertility in males [see Use in Specific Populations (8.6)].
- Discontinue nursing while receiving doxorubicin hydrochloride [see Use in Specific Populations (8.3)].
- Doxorubicin hydrochloride can cause nausea, vomiting, diarrhea, mouth/oral pain and sores. Advise patients to contact a healthcare provider should they develop any severe symptoms that prevent them from eating and drinking [see Adverse Reactions (6)].
- Doxorubicin hydrochloride causes alopecia [see Adverse Reactions (6.1)].
- Doxorubicin hydrochloride can cause their urine to appear red for 1 to 2 days after administration.
-
Patient Information
DOXOrubicin (dok-suh-roo-buh-sin) Hydrochloride Injection, USP
for intravenous use
What is the most important information I should know about Doxorubicin?
Doxorubicin may cause serious side effects including:
-
Heart failure. Doxorubicin may cause heart muscle damage that may lead to heart failure, which is a condition in which the heart does not pump well. Heart failure is irreversible in some cases and can lead to death. Heart failure can happen during your treatment with doxorubicin or months to years after stopping treatment. Your risk of heart muscle damage increases with higher total amounts of doxorubicin hydrochloride that you receive in your lifetime. Your risk of heart failure is higher if you:
- already have other heart problems
- have had or are currently receiving radiation therapy to your chest
- have had treatment with certain other anti-cancer medicines
- take other medicines that can have severe side effects on your heart
Tell your doctor if you get any of these symptoms of heart failure during or after treatment with doxorubicin:
- extreme tiredness or weakness
- fast heartbeat
- shortness of breath
- swelling of your feet and ankles
Your doctor will do tests to check the strength of your heart muscle before, during, and after your treatment with doxorubicin.
- Risk of new cancers. You may have an increased risk of developing certain blood cancers called acute myelogenous leukemia (AML) or myelodysplastic syndrome (MDS) after treatment with doxorubicin. Talk with your doctor about your risk of developing new cancers if you take doxorubicin.
- Skin damage near the vein where doxorubicin is given (injection site reaction). Doxorubicin can damage the skin if it leaks out of the vein. Symptoms of infusion reaction include blisters and skin sores at injection site which may require skin grafts.
- Decreased blood cell counts. Doxorubicin can cause a decrease in neutrophils (a type of white blood cells important in fighting bacterial infections) and platelets (important for clotting and to control bleeding). This may lead to a serious infection, the need for blood transfusions, treatment in a hospital and death. Your doctor will check your blood cell count during your treatment with doxorubicin and after you have stopped your treatment. Call your doctor right away if you get a fever (temperature of 100.4 F or greater) or chills with shivering.
What is Doxorubicin?
Doxorubicin is a prescription medicine used to treat certain types of cancers. Doxorubicin may be used alone or along with other anti-cancer medicines.
Who should not receive Doxorubicin?
Do not receive Doxorubicin if:
- you have had a recent heart attack or have severe heart problems
- your blood cell counts (platelets, red blood cells, and white blood cells) are very low because of prior chemotherapy
- you have a severe liver problem
- you have had a serious allergic reaction to doxorubicin hydrochloride
What should I tell my doctor before receiving Doxorubicin?
Before you receive doxorubicin, tell your doctor if you:
- have heart problems including heart failure
- are currently receiving radiation therapy or plan to receive radiation to the chest
- have severe liver problems
- have had an allergic reaction to doxorubicin
- have any other medical conditions
- are pregnant or plan to become pregnant. Doxorubicin can harm your unborn baby. Women who are able to become pregnant and men who take doxorubicin should use effective birth control (contraception) during treatment and for 6 months after treatment. Talk to your doctor about birth control methods. If you or your partner becomes pregnant, tell your doctor right away.
- are breastfeeding or plan to breast feed. Doxorubicin can pass into your breast milk and harm your baby. You and your doctor should decide if you will receive doxorubicin or breastfeed. You should not do both.
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Doxorubicin can interact with other medicines. Do not start any new medicine before you talk with the doctor that prescribed doxorubicin.
Know the medicines you take. Keep a list to show your doctor and pharmacist each time you get a new medicine.
How will I receive Doxorubicin?
- Doxorubicin will be given to you into your vein.
What are the possible side effects of Doxorubicin?
Doxorubicin may cause serious side effects, including:
- See “What is the most important information I should know about Doxorubicin?”
Doxorubicin may cause lower sperm counts and sperm problems in men.
This could affect your ability to father a child and cause birth defects. Talk to your healthcare provider if this is a concern for you. Talk to your healthcare provider about family planning options that might be right for you.
Irreversible amenorrhea or early menopause. Your periods (menstrual cycle) may completely stop when you receive doxorubicin. Your periods may or may not return following treatment. Talk to your healthcare provider about family planning options that might be right for you.
The most common side effects of Doxorubicin include:
- Total hair loss (alopecia). Your hair may re-grow after your treatment.
- nausea
- vomiting
Other side effects:
- Red colored urine. You may have red colored urine for 1 to 2 days after your infusion of doxorubicin. This is normal. Tell your doctor if it does not stop in a few days, or if you see what looks like blood or blood clots in your urine.
- Darkening of your nails or separation of your nails from your nail bed.
- Easy bruising or bleeding.
- Call your doctor if you have severe symptoms that prevent you from eating or drinking, such as:
- nausea
- vomiting
- diarrhea
- mouth sores
Tell your doctor or nurse if you have any side effect that bothers you or that does not go away.
These are not all of the possible side effects of doxorubicin.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Doxorubicin.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet.
You can ask your pharmacist or doctor for information about doxorubicin that is written for health professionals.
For more information, call 1-800-818-4555.
What are the ingredients of Doxorubicin?
Active ingredient: doxorubicin hydrochloride
Inactive ingredients: 0.9% sodium chloride, water for injection and hydrochloric acid.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Distributed by:
Sun Pharmaceutical Industries, Inc.
Cranbury, NJ 08512
Manufactured by:
Sun Pharmaceutical Industries Ltd.
Halol-Baroda Highway,
Halol-389 350, Gujarat, India.
ISS. 12/2014PJPI0249B
-
Heart failure. Doxorubicin may cause heart muscle damage that may lead to heart failure, which is a condition in which the heart does not pump well. Heart failure is irreversible in some cases and can lead to death. Heart failure can happen during your treatment with doxorubicin or months to years after stopping treatment. Your risk of heart muscle damage increases with higher total amounts of doxorubicin hydrochloride that you receive in your lifetime. Your risk of heart failure is higher if you:
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - label -50 mg/25 mL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - carton - 50 mg/25 mL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - label - 200 mg/100 mL
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - carton - 200 mg/100 mL
-
INGREDIENTS AND APPEARANCE
DOXORUBICIN HYDROCHLORIDE
doxorubicin hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:62756-826 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DOXORUBICIN HYDROCHLORIDE (UNII: 82F2G7BL4E) (DOXORUBICIN - UNII:80168379AG) DOXORUBICIN HYDROCHLORIDE 2 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 9 mg in 1 mL WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:62756-826-40 1 in 1 BOX 02/20/2012 1 25 mL in 1 VIAL, SINGLE-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA091418 02/20/2012 DOXORUBICIN HYDROCHLORIDE
doxorubicin hydrochloride injection, solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:62756-827 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength DOXORUBICIN HYDROCHLORIDE (UNII: 82F2G7BL4E) (DOXORUBICIN - UNII:80168379AG) DOXORUBICIN HYDROCHLORIDE 2 mg in 1 mL Inactive Ingredients Ingredient Name Strength SODIUM CHLORIDE (UNII: 451W47IQ8X) 9 mg in 1 mL WATER (UNII: 059QF0KO0R) HYDROCHLORIC ACID (UNII: QTT17582CB) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:62756-827-40 1 in 1 BOX 02/20/2012 1 100 mL in 1 VIAL, MULTI-DOSE; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA091418 02/20/2012 Labeler - Sun Pharmaceutical Industries, Inc. (146974886) Establishment Name Address ID/FEI Business Operations Sun Pharmaceutical Industries Limited 725959238 ANALYSIS(62756-826, 62756-827) , MANUFACTURE(62756-826, 62756-827)