MONTELUKAST SODIUM- montelukast sodium tablet, chewable
Method Pharmaceuticals, LLC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use MONTELUKAST SODIUM CHEWABLE TABLETS safely and effectively. See full prescribing information for MONTELUKAST SODIUM CHEWABLE TABLETS.
MONTELUKAST SODIUM chewable tablets, for oral use Initial U.S. Approval: 1998 WARNING: SERIOUS NEUROPSYCHIATRIC EVENTSSee full prescribing information for complete boxed warning.
RECENT MAJOR CHANGESINDICATIONS AND USAGEMontelukast sodium chewable tablets are a leukotriene receptor antagonist indicated for:
Limitations of Use:
DOSAGE AND ADMINISTRATIONAdministration (by indications):
Dosage (by age):
Patients with both asthma and allergic rhinitis should take only one dose daily in the evening ( 2.4). DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONSHypersensitivity to any component of montelukast sodium chewable tablets ( 4). WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (incidence ≥5% and greater than placebo listed in descending order of frequency): upper respiratory infection, fever, headache, pharyngitis, cough, abdominal pain, diarrhea, otitis media, influenza, rhinorrhea, sinusitis, otitis ( 6.1). To report SUSPECTED ADVERSE REACTIONS, contact Method Pharmaceuticals, LLC at 1-877-250-3427 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 3/2022 |
FULL PRESCRIBING INFORMATION
WARNING: SERIOUS NEUROPSYCHIATRIC EVENTS
Serious neuropsychiatric (NP) events have been reported with the use of montelukast sodium chewable tablets. The types of events reported were highly variable, and included, but were not limited to, agitation, aggression, depression, sleep disturbances, suicidal thoughts and behavior (including suicide). The mechanisms underlying NP events associated with montelukast sodium use are currently not well understood [see Warnings and Precautions ( 5.1)].
Because of the risk of NP events, the benefits of montelukast sodium may not outweigh the risks in some patients, particularly when the symptoms of disease may be mild and adequately treated with alternative therapies. Reserve use of montelukast sodium for patients with allergic rhinitis who have an inadequate response or intolerance to alternative therapies [see Indications and Usage ( 1.3)] . In patients with asthma or exercise-induced bronchoconstriction, consider the benefits and risks before prescribing montelukast sodium.
Discuss the benefits and risks of montelukast sodium with patients and caregivers when prescribing montelukast sodium. Advise patients and/or caregivers to be alert for changes in behavior or new NP symptoms when taking montelukast sodium. If changes in behavior are observed, or if new NP symptoms or suicidal thoughts and/or behavior occur, advise patients to discontinue montelukast sodium and contact a healthcare provider immediately [see Warnings and Precautions ( 5.1)] .
1 INDICATIONS AND USAGE
1.1 Asthma
Montelukast sodium chewable tablets are indicated for the prophylaxis and chronic treatment of asthma in adults and pediatric patients 2 years of age and older.
1.2 Exercise-Induced Bronchoconstriction (EIB)
Montelukast sodium chewable tablets are indicated for prevention of exercise-induced bronchoconstriction (EIB) in patients 6 years of age and older.
1.3 Allergic Rhinitis
Montelukast sodium chewable tablets are indicated for the relief of symptoms of seasonal allergic rhinitis in patients 2 years of age and older and perennial allergic rhinitis in patients 2 years of age and older. Because the benefits of montelukast sodium chewable tablets may not outweigh the risk of neuropsychiatric symptoms in patients with allergic rhinitis [see Warnings and Precautions ( 5.1)] , reserve use for patients who have an inadequate response or intolerance to alternative therapies.
2 DOSAGE AND ADMINISTRATION
2.1 Asthma
For asthma, administer montelukast sodium chewable tablets orally once daily in the evening, with or without food. There have been no clinical trials in patients with asthma to evaluate the relative efficacy of morning versus evening dosing.
The following doses are recommended:
Table 1: Recommended Dosage in Asthma
| Age
| Dose
|
| Pediatric patients 6 to 14 years of age
| one 5 mg chewable tablet
|
| Pediatric patients 2 to 5 years of age
| one 4 mg chewable tablet
|
Patients who miss a dose should not take the next dose at their regular time and should not take 2 doses at the same time.
2.2 Exercise-Induced Bronchoconstriction (EIB)
For prevention of EIB, administer a single dose of montelukast sodium chewable tablets orally at least 2 hours, before exercise.
The following doses are recommended:
Table 2: Recommended Dosage in Exercise-Induced Bronchoconstriction (EIB)
|
* Safety and effectiveness in patients younger than 6 years of age have not been established. |
|
| Age
| Dose
|
| Pediatric patients 6 to 14 years of age*
| one 5 mg chewable tablet
|
An additional dose of montelukast sodium chewable tablets should not be taken within 24 hours of a previous dose. Patients already taking montelukast sodium chewable tablets daily for another indication (including chronic asthma) should not take an additional dose to prevent EIB. All patients should have available for rescue a short-acting β-agonist.
Daily administration of montelukast sodium chewable tablets for the chronic treatment of asthma has not been established to prevent acute episodes of EIB.
2.3 Allergic Rhinitis
For allergic rhinitis, administer montelukast sodium chewable tablets orally once daily without regard to time of food ingestion. Time of administration in patients with allergic rhinitis can be individualized to suit patient needs.
The following doses for the treatment of symptoms of seasonal allergic rhinitis are recommended:
Table 3: Recommended Dosage in Seasonal Allergic Rhinitis
|
* Safety and effectiveness in patients younger than 2 years of age with seasonal allergic rhinitis have not been established. |
|
| Age
| Dose
|
| Pediatric patients 6 to 14 years of age
| one 5 mg chewable tablet
|
| Pediatric patients 2 to 5 years of age*
| one 4 mg chewable tablet
|
The following doses for the treatment of symptoms of perennial allergic rhinitis are recommended:
Table 4: Recommended Dosage in Perennial Allergic Rhinitis
| Age
| Dose
|
| Pediatric patients 6 to 14 years of age
| one 5 mg chewable tablet
|
| Pediatric patients 2 to 5 years of age
| one 4 mg chewable tablet
|
Patients who miss a dose should take the next dose at their regular time and should not take 2 doses at the same time.
3 DOSAGE FORMS AND STRENGTHS
- Montelukast Sodium Chewable Tablets USP, 5 mg are pink round tablets, debossed with '226' on one side and plain on the other side.
- Montelukast Sodium Chewable Tablets USP, 4 mg are pink oval tablets, debossed with '227' on one side and plain on the other side.
4 CONTRAINDICATIONS
Montelukast sodium chewable tablets are contraindicated in patients with hypersensitivity to any of its components.
5 WARNINGS AND PRECAUTIONS
5.1 Neuropsychiatric Events
Serious neuropsychiatric (NP) events have been reported with use of montelukast sodium. These postmarketing reports have been highly variable and included, but were not limited to, agitation, aggressive behavior or hostility, anxiousness, depression, disorientation, disturbance in attention, dream abnormalities, dysphemia (stuttering), hallucinations, insomnia, irritability, memory impairment, obsessive-compulsive symptoms, restlessness, somnambulism, suicidal thoughts and behavior (including suicide), tic, and tremor. NP events have been reported in adult, adolescent, and pediatric patients with and without a previous history of psychiatric disorder. NP events have been reported mostly during montelukast sodium treatment, but some were reported after montelukast sodium discontinuation. Animal studies showed that montelukast distributes into the brain in rats [see Clinical Pharmacology ( 12.3)] ; however, the mechanisms underlying montelukast sodium -associated NP events are currently not well understood. Based upon the available data, it is difficult to identify risk factors for or quantify the risk of NP events with montelukast sodium use.
Because of the risk of NP events, the benefits of montelukast sodium may not outweigh the risks in some patients, particularly when the symptoms of disease may be mild and adequately treated with alternative therapies. Reserve use of montelukast sodium for patients with allergic rhinitis who have an inadequate response or intolerance to alternative therapies [see Indications and Usage ( 1.3)] . In patients with asthma or exercise-induced bronchoconstriction, consider the benefits and risks before prescribing montelukast sodium.
Discuss the benefits and risks of montelukast sodium use with patients and caregivers when prescribing montelukast sodium. Advise patients and/or caregivers to be alert for changes in behavior or for new NP symptoms when taking montelukast sodium. If changes in behavior are observed, or if new NP symptoms or suicidal thoughts and/or behavior occur, advise patients to discontinue montelukast sodium and contact a healthcare provider immediately. In many cases, symptoms resolved after stopping montelukast sodium therapy; however, in some cases symptoms persisted after discontinuation of montelukast sodium. Therefore, continue to monitor and provide supportive care until symptoms resolve. Re-evaluate the benefits and risks of restarting treatment with montelukast sodium if such events occur .
5.2 Acute Asthma
Montelukast sodium is not indicated for use in the reversal of bronchospasm in acute asthma attacks, including status asthmaticus. Patients should be advised to have appropriate rescue medication available. Therapy with montelukast sodium can be continued during acute exacerbations of asthma. Patients who have exacerbations of asthma after exercise should have available for rescue a short-acting inhaled β-agonist.
5.3 Concomitant Corticosteroid Use
While the dose of inhaled corticosteroid may be reduced gradually under medical supervision, montelukast sodium should not be abruptly substituted for inhaled or oral corticosteroids.
5.4 Aspirin Sensitivity
Patients with known aspirin sensitivity should continue avoidance of aspirin or non-steroidal anti-inflammatory agents while taking montelukast sodium. Although montelukast sodium is effective in improving airway function in asthmatics with documented aspirin sensitivity, it has not been shown to truncate bronchoconstrictor response to aspirin and other non-steroidal anti-inflammatory drugs in aspirin-sensitive asthmatic patients [see Clinical Studies ( 14.1)] .
5.5 Eosinophilic Conditions
Patients with asthma on therapy with montelukast sodium may present with systemic eosinophilia, sometimes presenting with clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition which is often treated with systemic corticosteroid therapy. These events have been sometimes associated with the reduction of oral corticosteroid therapy. Physicians should be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients. A causal association between montelukast sodium and these underlying conditions has not been established [see Adverse Reactions ( 6.2)] .
5.6 Risk in Patients with Phenylketonuria
Montelukast sodium contains aspartame, a source of phenylalanine. Phenylalanine can be harmful to patients with phenylketonuria (PKU). Each 4 mg and 5 mg chewable tablet contains 0.38 mg and 0.47 mg of phenylalanine, respectively. Before prescribing montelukast sodium to a patient with PKU, consider the combined daily amount of phenylalanine from all sources, including montelukast sodium.
6 ADVERSE REACTIONS
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Neuropsychiatric Events [see Warnings and Precautions ( 5.1)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. In the following description of clinical trials experience, adverse reactions are listed regardless of causality assessment.
The most common adverse reactions (incidence ≥ 5% and greater than placebo; listed in descending order of frequency) in controlled clinical trials were: upper respiratory infection, fever, headache, pharyngitis, cough, abdominal pain, diarrhea, otitis media, influenza, rhinorrhea, sinusitis, otitis.
Adults and Adolescents 15 Years of Age and Older with Asthma
Montelukast sodium has been evaluated for safety in approximately 2,950 adult and adolescent patients 15 years of age and older in clinical trials. In placebo-controlled clinical trials, the following adverse experiences reported with montelukast sodium occurred in greater than or equal to 1% of patients and at an incidence greater than that in patients treated with placebo:
Table 5: Adverse Experiences Occurring in ≥ 1% of Patients with an Incidence Greater than that in Patients Treated with Placebo
|
* Number of patients tested (montelukast sodium and placebo, respectively): ALT and AST, 1,935, 1,170; pyuria, 1,924, 1,159. |
||
| Montelukast Sodium 10 mg/day
(%) (n=1,955) | Placebo
(%) (n=1,180) |
|
| Body As A Whole
| ||
| Pain, abdominal
| 2.9
| 2.5
|
| Asthenia/fatigue
| 1.8
| 1.2
|
| Fever
| 1.5
| 0.9
|
| Trauma
| 1.0
| 0.8
|
| Digestive System Disorders
| ||
| Dyspepsia
| 2.1
| 1.1
|
| Pain, dental
| 1.7
| 1.0
|
| Gastroenteritis, infectious
| 1.5
| 0.5
|
| Nervous System/Psychiatric
| ||
| Headache
| 18.4
| 18.1
|
| Dizziness
| 1.9
| 1.4
|
| Respiratory System Disorders
| ||
| Influenza
| 4.2
| 3.9
|
| Cough
| 2.7
| 2.4
|
| Congestion, nasal
| 1.6
| 1.3
|
| Skin/Skin Appendages Disorder
| ||
| Rash
| 1.6
| 1.2
|
| Laboratory Adverse Experiences *
| ||
| ALT increased
| 2.1
| 2.0
|
| AST increased
| 1.6
| 1.2
|
| Pyuria
| 1.0
| 0.9
|
The frequency of less common adverse events was comparable between montelukast sodium and placebo.
The safety profile of montelukast sodium, when administered as a single dose for prevention of EIB in adult and adolescent patients 15 years of age and older, was consistent with the safety profile previously described for montelukast sodium.
Cumulatively, 569 patients were treated with montelukast sodium for at least 6 months, 480 for one year, and 49 for two years in clinical trials. With prolonged treatment, the adverse reaction profile did not significantly change.
Pediatric Patients 6 to 14 Years of Age with Asthma
Montelukast sodium has been evaluated for safety in 476 pediatric patients 6 to 14 years of age. Cumulatively, 289 pediatric patients were treated with montelukast sodium for at least 6 months, and 241 for one year or longer in clinical trials. The safety profile of montelukast sodium in the 8-week, double-blind, pediatric efficacy trial was generally similar to the adult safety profile. In pediatric patients 6 to 14 years of age receiving montelukast sodium, the following events occurred with a frequency ≥ 2% and more frequently than in pediatric patients who received placebo: pharyngitis, influenza, fever, sinusitis, nausea, diarrhea, dyspepsia, otitis, viral infection, and laryngitis. The frequency of less common adverse reactions was comparable between montelukast sodium and placebo. With prolonged treatment, the adverse reaction profile did not significantly change.
The safety profile of montelukast sodium, when administered as a single dose for prevention of EIB in pediatric patients 6 years of age and older, was consistent with the safety profile previously described for montelukast sodium.
In studies evaluating growth rate, the safety profile in these pediatric patients was consistent with the safety profile previously described for montelukast sodium. In a 56-week, double-blind study evaluating growth rate in pediatric patients 6 to 8 years of age receiving montelukast sodium, the following reactions not previously observed with the use of montelukast sodium in this age group occurred with a frequency ≥2% and more frequently than in pediatric patients who received placebo: headache, rhinitis (infective), varicella, gastroenteritis, atopic dermatitis, acute bronchitis, tooth infection, skin infection, and myopia.
Pediatric Patients 2 to 5 Years of Age with Asthma
Montelukast sodium has been evaluated for safety in 573 pediatric patients 2 to 5 years of age in single- and multiple-dose studies. Cumulatively, 426 pediatric patients 2 to 5 years of age were treated with montelukast sodium for at least 3 months, 230 for 6 months or longer, and 63 patients for one year or longer in clinical trials. In pediatric patients 2 to 5 years of age receiving montelukast sodium, the following reactions occurred with a frequency ≥ 2% and more frequently than in pediatric patients who received placebo: fever, cough, abdominal pain, diarrhea, headache, rhinorrhea, sinusitis, otitis, influenza, rash, ear pain, gastroenteritis, eczema, urticaria, varicella, pneumonia, dermatitis, and conjunctivitis.
Adults and Adolescents 15 Years of Age and Older with Seasonal Allergic Rhinitis
Montelukast sodium has been evaluated for safety in 2,199 adult and adolescent patients 15 years of age and older in clinical trials. Montelukast sodium administered once daily in the morning or in the evening had a safety profile similar to that of placebo. In placebo-controlled clinical trials, the following event was reported with montelukast sodium with a frequency ≥ 1% and at an incidence greater than placebo: upper respiratory infection, 1.9% of patients receiving montelukast sodium vs. 1.5% of patients receiving placebo. In a 4-week, placebo-controlled clinical study, the safety profile was consistent with that observed in 2-week studies. The incidence of somnolence was similar to that of placebo in all studies.
Pediatric Patients 2 to 14 Years of Age with Seasonal Allergic Rhinitis
Montelukast sodium has been evaluated in 280 pediatric patients 2 to 14 years of age in a 2-week, multicenter, double-blind, placebo-controlled, parallel-group safety study. Montelukast sodium administered once daily in the evening had a safety profile similar to that of placebo. In this study, the following reactions occurred with a frequency ≥ 2% and at an incidence greater than placebo: headache, otitis media, pharyngitis, and upper respiratory infection.
Adults and Adolescents 15 Years of Age and Older with Perennial Allergic Rhinitis
Montelukast sodium has been evaluated for safety in 3,357 adult and adolescent patients 15 years of age and older with perennial allergic rhinitis of whom 1,632 received montelukast sodium in two, 6-week, clinical studies. Montelukast sodium administered once daily had a safety profile consistent with that observed in patients with seasonal allergic rhinitis and similar to that of placebo. In these two studies, the following events were reported with montelukast sodium with a frequency ≥ 1% and at an incidence greater than placebo: sinusitis, upper respiratory infection, sinus headache, cough, epistaxis, and increased ALT. The incidence of somnolence was similar to that of placebo.
Pediatric Patients 2 to 14 Years of Age with Perennial Allergic Rhinitis
The safety in patients 2 to 14 years of age with perennial allergic rhinitis is supported by the safety in patients 2 to 14 years of age with seasonal allergic rhinitis. The safety in patients 6 to 23 months of age is supported by data from pharmacokinetic and safety and efficacy studies in asthma in this pediatric population and from adult pharmacokinetic studies.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of montelukast sodium. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders
increased bleeding tendency, thrombocytopenia
Immune system disorders
hypersensitivity reactions including anaphylaxis, hepatic eosinophilic infiltration
Psychiatric disorders
including, but not limited to, agitation, aggressive behavior or hostility, anxiousness, depression, disorientation, disturbance in attention, dream abnormalities, dysphemia (stuttering), hallucinations, insomnia, irritability, memory impairment, obsessive-compulsive symptoms, restlessness, somnambulism, suicidal thinking and behavior (including suicide), tic, and tremor [see Boxed Warning, Warnings and Precautions ( 5.1)]
Nervous system disorders
drowsiness, paraesthesia/hypoesthesia, seizures
Cardiac disorders
palpitations
Respiratory, thoracic and mediastinal disorders
epistaxis, pulmonary eosinophilia
Gastrointestinal disorders
diarrhea, dyspepsia, nausea, pancreatitis, vomiting
Hepatobiliary disorders
Cases of cholestatic hepatitis, hepatocellular liver-injury, and mixed-pattern liver injury have been reported in patients treated with montelukast sodium. Most of these occurred in combination with other confounding factors, such as use of other medications, or when montelukast sodium was administered to patients who had underlying potential for liver disease such as alcohol use or other forms of hepatitis.
Skin and subcutaneous tissue disorders
angioedema, bruising, erythema multiforme, erythema nodosum, pruritus, Stevens-Johnson syndrome/toxic epidermal necrolysis, urticaria
Musculoskeletal and connective tissue disorders
arthralgia, myalgia including muscle cramps
Renal and urinary disorders
enuresis in children
General disorders and administration site conditions
edema.
Patients with asthma on therapy with montelukast sodium may present with systemic eosinophilia, sometimes presenting with clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition which is often treated with systemic corticosteroid therapy. These events have been sometimes associated with the reduction of oral corticosteroid therapy. Physicians should be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients [see Warnings and Precautions ( 5.5)] .
7 DRUG INTERACTIONS
No dose adjustment is needed when montelukast sodium is co-administered with theophylline, prednisone, prednisolone, oral contraceptives, fexofenadine, digoxin, warfarin, gemfibrozil, itraconazole, thyroid hormones, sedative hypnotics, non-steroidal anti-inflammatory agents, benzodiazepines, decongestants, and Cytochrome P450 (CYP) enzyme inducers [see Clinical Pharmacology ( 12.3)] .
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Available data from published prospective and retrospective cohort studies over decades with montelukast use in pregnant women have not established a drug-associated risk of major birth defects [see Data]. In animal reproduction studies, no adverse developmental effects were observed with oral administration of montelukast to pregnant rats and rabbits during organogenesis at doses approximately 100 and 110 times, respectively, the maximum recommended human daily oral dose (MRHDOD) based on AUCs [see Data].
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Poorly or moderately controlled asthma in pregnancy increases the maternal risk of perinatal adverse outcomes such as preeclampsia and infant prematurity, low birth weight, and small for gestational age.
Data
Human Data
Published data from prospective and retrospective cohort studies have not identified an association with montelukast sodium use during pregnancy and major birth defects. Available studies have methodologic limitations, including small sample size, in some cases retrospective data collection, and inconsistent comparator groups.
Animal Data
In embryo-fetal development studies, montelukast administered to pregnant rats and rabbits during organogenesis (gestation days 6 to 17 in rats and 6 to 18 in rabbits) did not cause any adverse developmental effects at maternal oral doses up to 400 and 300 mg/kg/day in rats and rabbits, respectively (approximately 100 and 110 times the AUC in humans at the MRHDOD, respectively).
8.2 Lactation
A published clinical lactation study reports the presence of montelukast in human milk. Data available on the effects of the drug on infants, either directly [see Use in Specific Populations ( 8.4)] or through breast milk, do not suggest a significant risk of adverse events from exposure to montelukast sodium. The effects of the drug on milk production are unknown. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for montelukast sodium and any potential adverse effects on the breastfed infant from montelukast sodium or from the underlying maternal condition.
8.4 Pediatric Use
Safety and effectiveness of montelukast sodium for asthma have been established in pediatric patients 6 to 14 years of age. Use of montelukast sodium for this indication is supported by evidence from well-controlled studies. Safety and efficacy data in this age group are similar to those seen in adults [see Adverse Reactions ( 6.1), Clinical Pharmacology, Specific Populations ( 12.3), and Clinical Studies ( 14.1, 14.2)].
The effectiveness of montelukast sodium for the treatment of seasonal allergic rhinitis in pediatric patients 2 to 14 years of age and for the treatment of perennial allergic rhinitis in pediatric patients 2 to 14 years of age have been established and is supported by extrapolation from the demonstrated effectiveness in patients 15 years of age and older with allergic rhinitis as well as the assumption that the disease course, pathophysiology and the drug's effect are substantially similar among these populations.
The safety of montelukast sodium 4 mg chewable tablets in pediatric patients 2 to 5 years of age with asthma has been demonstrated by adequate and well-controlled data [see Adverse Reactions (6.1)]. Effectiveness of montelukast sodium in this age group is extrapolated from the demonstrated effectiveness in patients 6 years of age and older with asthma and is based on similar pharmacokinetic data, as well as the assumption that the disease course, pathophysiology and the drug's effect are substantially similar among these populations. Effectiveness in this age group is supported by exploratory efficacy assessments from a large, well-controlled safety study conducted in patients 2 to 5 years of age.
The safety of montelukast sodium 4 mg and 5 mg chewable tablets in pediatric patient 2 to 14 years with allergic rhinitis is supported by data from studies conducted in pediatric patients aged 2 to 14 years with asthma. A safety study in pediatric patients 2 to 14 years of age with seasonal allergic rhinitis demonstrated a similar safety profile [see Adverse Reactions ( 6.1)] .
The safety and effectiveness in pediatric patients below the age of 12 months with asthma, 6 months with perennial allergic rhinitis, and 6 years with exercise-induced bronchoconstriction have not been established.
Growth Rate in Pediatric Patients
A 56-week, multi-center, double-blind, randomized, active- and placebo-controlled parallel group study was conducted to assess the effect of montelukast sodium on growth rate in 360 patients with mild asthma, aged 6 to 8 years. Treatment groups included montelukast sodium 5 mg once daily, placebo, and beclomethasone dipropionate administered as 168 mcg twice daily with a spacer device. For each subject, a growth rate was defined as the slope of a linear regression line fit to the height measurements over 56 weeks. The primary comparison was the difference in growth rates between montelukast sodium and placebo groups. Growth rates, expressed as least-squares (LS) mean (95% CI) in cm/year, for the montelukast sodium, placebo, and beclomethasone treatment groups were 5.67 (5.46, 5.88), 5.64 (5.42, 5.86), and 4.86 (4.64, 5.08), respectively. The differences in growth rates, expressed as least-squares (LS) mean (95% CI) in cm/year, for montelukast sodium minus placebo, beclomethasone minus placebo, and montelukast sodium minus beclomethasone treatment groups were 0.03 (-0.26, 0.31), -0.78 (-1.06, -0.49); and 0.81 (0.53, 1.09), respectively. Growth rate (expressed as mean change in height over time) for each treatment group is shown in FIGURE 1.
Figure 1: Change in Height (cm) from Randomization Visit by Scheduled Week (Treatment Group Mean ± Standard Error* of the Mean)
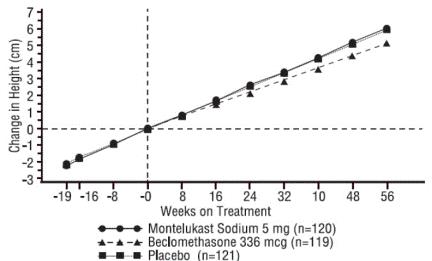
*The standard errors of the treatment group means in change in height are too small to be visible on the plot
8.5 Geriatric Use
Of the total number of subjects in clinical studies of montelukast, 3.5% were 65 years of age and over, and 0.4% were 75 years of age and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. The pharmacokinetic profile and the oral bioavailability of a single 10 mg oral dose of montelukast are similar in elderly and younger adults. The plasma half-life of montelukast is slightly longer in the elderly. No dosage adjustment in the elderly is required.
8.7 Hepatic Impairment
No dosage adjustment is required in patients with mild-to-moderate hepatic insufficiency [see Clinical Pharmacology ( 12.3)] .
8.6 Renal Impairment
No dosage adjustment is recommended in patients with renal insufficiency [see Clinical Pharmacology ( 12.3)] .
10 OVERDOSAGE
No specific information is available on the treatment of overdosage with montelukast sodium. In the event of overdose, it is reasonable to employ the usual supportive measures; e.g., remove unabsorbed material from the gastrointestinal tract, employ clinical monitoring, and institute supportive therapy, if required. It is not known whether montelukast is removed by peritoneal dialysis or hemodialysis.
11 DESCRIPTION
Montelukast sodium, the active ingredient in montelukast sodium chewable tablets, USP, is a selective and orally active leukotriene receptor antagonist that inhibits the cysteinyl leukotriene CysLT 1 receptor.
Montelukast sodium is described chemically as [ R-( E)]-1-[[[1-[3-[2-(7-chloro-2-quinolinyl) ethenyl]phenyl]-3-[2-(1-hydroxy-1-methylethyl)phenyl]propyl]thio]methyl]cyclopropaneacetic acid, monosodium salt.
The empirical formula is C 35H 35ClNNaO 3S, and its molecular weight is 608.18. The structural formula is:
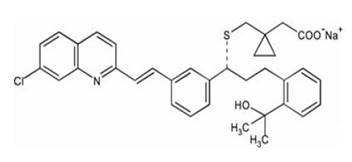
Montelukast sodium is a hygroscopic, optically active, white to off-white powder. Montelukast sodium is freely soluble in ethanol, methanol, and water and practically insoluble in acetonitrile. Each 4 mg and 5 mg montelukast sodium chewable tablet, USP contains 4.2 and 5.2 mg montelukast sodium, respectively, which are equivalent to 4 and 5 mg of montelukast, respectively. Both chewable tablets contain the following inactive ingredients: mannitol, microcrystalline cellulose, hydroxypropyl cellulose, red ferric oxide, croscarmellose sodium, cherry flavor, aspartame, and magnesium stearate.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The cysteinyl leukotrienes (LTC 4, LTD 4, LTE 4) are products of arachidonic acid metabolism and are released from various cells, including mast cells and eosinophils. These eicosanoids bind to cysteinyl leukotriene (CysLT) receptors. The CysLT type-1 (CysLT 1) receptor is found in the human airway (including airway smooth muscle cells and airway macrophages) and on other pro-inflammatory cells (including eosinophils and certain myeloid stem cells). CysLTs have been correlated with the pathophysiology of asthma and allergic rhinitis. In asthma, leukotriene-mediated effects include airway edema, smooth muscle contraction, and altered cellular activity associated with the inflammatory process. In allergic rhinitis, CysLTs are released from the nasal mucosa after allergen exposure during both early- and late-phase reactions and are associated with symptoms of allergic rhinitis.
Montelukast is an orally active compound that binds with high affinity and selectivity to the CysLT 1 receptor (in preference to other pharmacologically important airway receptors, such as the prostanoid, cholinergic, or β-adrenergic receptor). Montelukast inhibits physiologic actions of LTD 4 at the CysLT 1 receptor without any agonist activity.
12.2 Pharmacodynamics
Montelukast causes inhibition of airway cysteinyl leukotriene receptors as demonstrated by the ability to inhibit bronchoconstriction due to inhaled LTD 4 in asthmatics. Doses as low as 5 mg cause substantial blockage of LTD 4-induced bronchoconstriction. In a placebo-controlled, crossover study (n=12), montelukast sodium inhibited early- and late-phase bronchoconstriction due to antigen challenge by 75% and 57%, respectively.
The effect of montelukast sodium on eosinophils in the peripheral blood was examined in clinical trials. In patients with asthma aged 2 years and older who received montelukast sodium, a decrease in mean peripheral blood eosinophil counts ranging from 9% to 15% was noted, compared with placebo, over the double-blind treatment periods. In patients with seasonal allergic rhinitis aged 15 years and older who received montelukast sodium, a mean increase of 0.2% in peripheral blood eosinophil counts was noted, compared with a mean increase of 12.5% in placebo-treated patients, over the double-blind treatment periods; this reflects a mean difference of 12.3% in favor of montelukast sodium. The relationship between these observations and the clinical benefits of montelukast noted in the clinical trials is not known [see Clinical Studies ( 14)] .
12.3 Pharmacokinetics
Montelukast is rapidly absorbed following oral administration. After administration of the 10 mg film-coated tablet to fasted adults, the mean peak montelukast plasma concentration (C max) is achieved in 3 to 4 hours (T max). The mean oral bioavailability is 64%. The oral bioavailability and C max are not influenced by a standard meal in the morning.
For the 5 mg chewable tablet, the mean C max is achieved in 2 to 2.5 hours after administration to adults in the fasted state. The mean oral bioavailability is 73% in the fasted state versus 63% when administered with a standard meal in the morning.
For the 4 mg chewable tablet, the mean C max is achieved 2 hours after administration in pediatric patients 2 to 5 years of age in the fasted state.
The 4 mg oral granule formulation is bioequivalent to the 4 mg chewable tablet when administered to adults in the fasted state.
The safety and effectiveness of montelukast sodium in patients with asthma were demonstrated in clinical trials in which the 10 mg film-coated tablet and 5 mg chewable tablet formulations were administered in the evening without regard to the time of food ingestion. The safety of montelukast sodium in patients with asthma was also demonstrated in clinical trials in which the 4 mg chewable tablet and 4 mg oral granule formulations were administered in the evening without regard to the time of food ingestion. The safety and effectiveness of montelukast sodium chewable tablets in patients with seasonal allergic rhinitis were demonstrated in clinical trials in which the 10 mg film-coated tablet was administered in the morning or evening without regard to the time of food ingestion.
The comparative pharmacokinetics of montelukast when administered as two 5 mg chewable tablets versus one 10 mg film-coated tablet have not been evaluated.
Distribution
Montelukast is more than 99% bound to plasma proteins. The steady state volume of distribution of montelukast averages 8 to 11 liters. Orally administered montelukast distributes into the brain in rats.
Elimination
The plasma clearance of montelukast averages 45 mL/min in healthy adults. Following an oral dose of radiolabeled montelukast, 86% of the radioactivity was recovered in 5 day fecal collections and < 0.2% was recovered in urine. Coupled with estimates of montelukast oral bioavailability, this indicates that montelukast and its metabolites are excreted almost exclusively via the bile.
In several studies, the mean plasma half-life of montelukast ranged from 2.7 to 5.5 hours in healthy young adults. The pharmacokinetics of montelukast are nearly linear for oral doses up to 50 mg. During once-daily dosing with 10 mg montelukast, there is little accumulation of the parent drug in plasma (14%).
Metabolism
Montelukast is extensively metabolized. In studies with therapeutic doses, plasma concentrations of metabolites of montelukast are undetectable at steady state in adults and pediatric patients.
In vitro studies using human liver microsomes indicate that CYP3A4, 2C8, and 2C9 are involved in the metabolism of montelukast. At clinically relevant concentrations, 2C8 appears to play a major role in the metabolism of montelukast.
Special Populations
Patients with Hepatic Impairment
Patients with mild-to-moderate hepatic insufficiency and clinical evidence of cirrhosis had evidence of decreased metabolism of montelukast resulting in 41% (90% CI=7%, 85%) higher mean montelukast AUC following a single 10 mg dose. The elimination of montelukast was slightly prolonged compared with that in healthy subjects (mean half-life, 7.4 hours). No dosage adjustment is required in patients with mild-to-moderate hepatic insufficiency. The pharmacokinetics of montelukast sodium in patients with more severe hepatic impairment or with hepatitis have not been evaluated.
Patients with Renal Impairment
Since montelukast and its metabolites are not excreted in the urine, the pharmacokinetics of montelukast were not evaluated in patients with renal insufficiency. No dosage adjustment is recommended in these patients .
Male and Female Patients
The pharmacokinetics of montelukast are similar in males and females.
Racial Groups
Pharmacokinetic differences due to race have not been studied.
Adolescents and Pediatric Patients
Pharmacokinetic studies evaluated the systemic exposure of the 4 mg oral granule formulation in pediatric patients 6 to 23 months of age, the 4 mg chewable tablets in pediatric patients 2 to 5 years of age, the 5 mg chewable tablets in pediatric patients 6 to 14 years of age, and the 10 mg film-coated tablets in young adults and adolescents ≥15 years of age.
The plasma concentration profile of montelukast following administration of the 10 mg film-coated tablet is similar in adolescents ≥15 years of age and young adults. The 10 mg film-coated tablet is recommended for use in patients ≥15 years of age.
The mean systemic exposure of the 4 mg chewable tablet in pediatric patients 2 to 5 years of age and the 5 mg chewable tablets in pediatric patients 6 to 14 years of age is similar to the mean systemic exposure of the 10 mg film-coated tablet in adults. The 5 mg chewable tablet should be used in pediatric patients 6 to 14 years of age and the 4 mg chewable tablet should be used in pediatric patients 2 to 5 years of age.
In children 6 to 11 months of age, the systemic exposure to montelukast and the variability of plasma montelukast concentrations were higher than those observed in adults. Based on population analyses, the mean AUC (4,296 ng•hr/mL [range 1,200 to 7,153]) was 60% higher and the mean C max (667 ng/mL [range 201 to 1,058]) was 89% higher than those observed in adults (mean AUC 2,689 ng•hr/mL [range 1,521 to 4,595]) and mean C max (353 ng/mL [range 180 to 548]). The systemic exposure in children 12 to 23 months of age was less variable, but was still higher than that observed in adults. The mean AUC (3,574 ng•hr/mL [range 2,229 to 5,408]) was 33% higher and the mean C max (562 ng/mL [range 296 to 814]) was 60% higher than those observed in adults. Safety and tolerability of montelukast in a single-dose pharmacokinetic study in 26 children 6 to 23 months of age were similar to that of patients two years and above [see Adverse Reactions ( 6.1)] . The 4 mg oral granule formulation should be used for pediatric patients 12 to 23 months of age for the treatment of asthma, or for pediatric patients 6 to 23 months of age for the treatment of perennial allergic rhinitis. Since the 4 mg oral granule formulation is bioequivalent to the 4 mg chewable tablet, it can also be used as an alternative formulation to the 4 mg chewable tablet in pediatric patients 2 to 5 years of age.
Drug Interaction Studies
Theophylline, Prednisone, and Prednisolone
Montelukast sodium has been administered with other therapies routinely used in the prophylaxis and chronic treatment of asthma with no apparent increase in adverse reactions. In drug-interaction studies, the recommended clinical dose of montelukast did not have clinically important effects on the pharmacokinetics of the following drugs: theophylline, prednisone, and prednisolone.
Montelukast at a dose of 10 mg once daily dosed to pharmacokinetic steady state, did not cause clinically significant changes in the kinetics of a single intravenous dose of theophylline [predominantly a cytochrome P450 (CYP) 1A2 substrate]. Montelukast at doses of ≥ 100 mg daily dosed to pharmacokinetic steady state, did not cause any clinically significant change in plasma profiles of prednisone or prednisolone following administration of either oral prednisone or intravenous prednisolone.
Oral Contraceptives, fexofenadine, Digoxin, and Warfarin
In drug interaction studies, the recommended clinical dose of montelukast did not have clinically important effects on the pharmacokinetics of the following drugs: oral contraceptives (norethindrone 1 mg/ethinyl estradiol 35 mcg), digoxin, and warfarin. Montelukast at doses of ≥ 100 mg daily dosed to pharmacokinetic steady state did not significantly alter the plasma concentrations of either component of an oral contraceptive containing norethindrone 1 mg/ethinyl estradiol 35 mcg. Montelukast at a dose of 10 mg once daily dosed to pharmacokinetic steady state did not change the plasma concentration profile of fexofenadine did not change the pharmacokinetic profile or urinary excretion of immunoreactive digoxin; did not change the pharmacokinetic profile of warfarin (primarily a substrate of CYP2C9, 3A4 and 1A2) or influence the effect of a single 30 mg oral dose of warfarin on prothrombin time or the International Normalized Ratio (INR).
Thyroid Hormones, Sedative Hypnotics, Non-Steroidal Anti-Inflammatory Agents, Benzodiazepines, and Decongestants
Although additional specific interaction studies were not performed, montelukast sodium was used concomitantly with a wide range of commonly prescribed drugs in clinical studies without evidence of clinical adverse interactions. These medications included thyroid hormones, sedative hypnotics, non-steroidal anti-inflammatory agents, benzodiazepines, and decongestants.
Cytochrome P450 (CYP) Enzyme Inducers
Phenobarbital, which induces hepatic metabolism, decreased the area under the plasma concentration curve (AUC) of montelukast approximately 40% following a single 10 mg dose of montelukast. No dosage adjustment for montelukast sodium is recommended. It is reasonable to employ appropriate clinical monitoring when potent CYP enzyme inducers, such as phenobarbital or rifampin, are co-administered with montelukast sodium.
Effect of Montelukast on Cytochrome P450 (CYP) Enzymes
Montelukast is a potent inhibitor of CYP2C8 in vitro. However, data from a clinical drug-drug interaction study involving montelukast and rosiglitazone (a probe substrate representative of drugs primarily metabolized by CYP2C8) in 12 healthy individuals demonstrated that the pharmacokinetics of rosiglitazone are not altered when the drugs are coadministered, indicating that montelukast does not inhibit CYP2C8 in vivo. Therefore, montelukast is not anticipated to alter the metabolism of drugs metabolized by this enzyme (e.g., paclitaxel, rosiglitazone, and repaglinide). Based on further in vitro results in human liver microsomes, therapeutic plasma concentrations of montelukast do not inhibit CYP 3A4, 2C9, 1A2, 2A6, 2C19, or 2D6.
Cytochrome P450 (CYP) Enzyme Inhibitors
In vitro studies have shown that montelukast is a substrate of CYP 2C8, 2C9, and 3A4. Co-administration of montelukast with itraconazole, a strong CYP 3A4 inhibitor, resulted in no significant increase in the systemic exposure of montelukast. Data from a clinical drug-drug interaction study involving montelukast and gemfibrozil (an inhibitor of both CYP 2C8 and 2C9) demonstrated that gemfibrozil, at a therapeutic dose, increased the systemic exposure of montelukast by 4.4-fold. Co-administration of itraconazole, gemfibrozil, and montelukast did not further increase the systemic exposure of montelukast. Based on available clinical experience, no dosage adjustment of montelukast is required upon co-administration with gemfibrozil [see Overdosage ( 10)] .
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of tumorigenicity was seen in carcinogenicity studies of either 2 years in Sprague-Dawley rats or 92 weeks in mice at oral gavage doses up to 200 mg/kg/day or 100 mg/kg/day, respectively. The estimated exposure in rats was approximately 120 and 75 times the AUC for adults and children, respectively, at the maximum recommended daily oral dose. The estimated exposure in mice was approximately 45 and 25 times the AUC for adults and children, respectively, at the maximum recommended daily oral dose.
Montelukast demonstrated no evidence of mutagenic or clastogenic activity in the following assays: the microbial mutagenesis assay, the V-79 mammalian cell mutagenesis assay, the alkaline elution assay in rat hepatocytes, the chromosomal aberration assay in Chinese hamster ovary cells, and in the in vivo mouse bone marrow chromosomal aberration assay.
In fertility studies in female rats, montelukast produced reductions in fertility and fecundity indices at an oral dose of 200 mg/kg (estimated exposure was approximately 70 times the AUC for adults at the maximum recommended daily oral dose). No effects on female fertility or fecundity were observed at an oral dose of 100 mg/kg (estimated exposure was approximately 20 times the AUC for adults at the maximum recommended daily oral dose). Montelukast had no effects on fertility in male rats at oral doses up to 800 mg/kg (estimated exposure was approximately 160 times the AUC for adults at the maximum recommended daily oral dose).
14 CLINICAL STUDIES
14.2 Exercise-Induced Bronchoconstriction (EIB)
Exercise-Induced Bronchoconstriction (Adults, Adolescents, and Pediatric Patients 6 years of age and older)
The efficacy of montelukast 10 mg, when given as a single dose 2 hours before exercise for the prevention of EIB was investigated in three (U.S. and Multinational), randomized, double-blind, placebo-controlled crossover studies that included a total of 160 adult and adolescent patients 15 years of age and older with EIB. Exercise challenge testing was conducted at 2 hours, 8.5 or 12 hours, and 24 hours following administration of a single dose of study drug (montelukast 10 mg or placebo). The primary endpoint was the mean maximum percent fall in FEV 1 following the 2 hours post-dose exercise challenge in all three studies (Study A, Study B, and Study C). In Study A, a single dose of montelukast 10 mg demonstrated a statistically significant protective benefit against EIB when taken 2 hours prior to exercise. Some patients were protected from EIB at 8.5 and 24 hours after administration; however, some patients were not. The results for the mean maximum percent fall at each timepoint in Study A are shown in TABLE 7 and are representative of the results from the other two studies.
Table 7: Mean Maximum Percent Fall in FEV 1 Following Exercise Challenge in Study A (N=47) ANOVA Model
|
*Least squares-mean |
|||
| Time of exercise challenge following medication administration
| Mean Maximum percent fall in FEV
1*
| Treatment difference % for Montelukast Sodium versus Placebo
(95% CI)* |
|
|
| Montelukast Sodium
| Placebo
|
|
| 2 hours
| 13
| 22
| -9 (-12, -5)
|
| 8.5 hours
| 12
| 17
| -5 (-9, -2)
|
| 24 hours
| 10
| 14
| -4 (-7, -1)
|
The efficacy of montelukast sodium chewable tablets, 5 mg, when given as a single dose 2 hours before exercise for the prevention of EIB, was investigated in one multinational, randomized, double-blind, placebo-controlled crossover study that included a total of 64 pediatric patients 6 to 14 years of age with EIB. Exercise challenge testing was conducted at 2 hours and 24 hours following administration of a single dose of study drug (montelukast 5 mg or placebo). The primary endpoint was the mean maximum percent fall in FEV 1 following the 2 hours post-dose exercise challenge. A single dose of montelukast 5 mg demonstrated a statistically significant protective benefit against EIB when taken 2 hours prior to exercise (TABLE 8). Similar results were shown at 24 hours post-dose (a secondary endpoint). Some patients were protected from EIB at 24 hours after administration; however, some patients were not. No timepoints were assessed between 2 and 24 hours post-dose.
Table 8: Mean Maximum Percent Fall in FEV 1 Following Exercise Challenge in Pediatric Patients (N=64) ANOVA Model
|
*Least squares-mean |
|||
| Time of exercise challenge following medication administration
| Mean Maximum percent fall in FEV
1*
| Treatment difference % for Montelukast Sodium versus Placebo (95%CI)*
|
|
| Montelukast Sodium
| Placebo
| ||
| 2 hours
| 15
| 20
| -5 (-9, -1)
|
| 24 hours
| 13
| 17
| -4 (-7, -1)
|
The efficacy of montelukast sodium for prevention of EIB in patients below 6 years of age has not been established.
Daily administration of montelukast sodium for the chronic treatment of asthma has not been established to prevent acute episodes of EIB.
In a 12-week, randomized, double-blind, parallel group study of 110 adult and adolescent asthmatics 15 years of age and older, with a mean baseline FEV 1 percent of predicted of 83% and with documented exercise-induced exacerbation of asthma, treatment with montelukast 10 mg, once daily in the evening, resulted in a statistically significant reduction in mean maximal percent fall in FEV 1 and mean time to recovery to within 5% of the pre-exercise FEV 1. Exercise challenge was conducted at the end of the dosing interval (i.e., 20 to 24 hours after the preceding dose). This effect was maintained throughout the 12-week treatment period indicating that tolerance did not occur. Montelukast sodium did not, however, prevent clinically significant deterioration in maximal percent fall in FEV 1 after exercise (i.e., ≥ 20% decrease from pre-exercise baseline) in 52% of patients studied. In a separate crossover study in adults, a similar effect was observed after two once-daily 10 mg doses of montelukast sodium.
In pediatric patients 6 to 14 years of age, using the 5 mg chewable tablet, a 2-day crossover study demonstrated effects similar to those observed in adults when exercise challenge was conducted at the end of the dosing interval (i.e., 20 to 24 hours after the preceding dose).
14.3 Allergic Rhinitis (Seasonal and Perennial)
The efficacy of montelukast sodium tablets for the treatment of seasonal allergic rhinitis was investigated in 5 similarly designed, randomized, double-blind, parallel-group, placebo- and active-controlled (loratadine) trials conducted in North America. The 5 trials enrolled a total of 5,029 patients, of whom 1,799 were treated with montelukast sodium tablets. Patients were 15 to 82 years of age with a history of seasonal allergic rhinitis, a positive skin test to at least one relevant seasonal allergen, and active symptoms of seasonal allergic rhinitis at study entry.
The period of randomized treatment was 2 weeks in 4 trials and 4 weeks in one trial. The primary outcome variable was mean change from baseline in daytime nasal symptoms score (the average of individual scores of nasal congestion, rhinorrhea, nasal itching, sneezing) as assessed by patients on a 0 to 3 categorical scale.
Four of the five trials showed a significant reduction in daytime nasal symptoms scores with montelukast sodium tablets, 10 mg compared with placebo. The results of one trial are shown below. The median age in this trial was 35.0 years (range 15 to 81); 65.4% were females and 34.6% were males. The ethnic/racial distribution in this study was 83.1% Caucasian, 6.4% other origins, 5.8% Black, and 4.8% Hispanic. The mean changes from baseline in daytime nasal symptoms score in the treatment groups that received montelukast sodium tablets, loratadine, and placebo are shown in TABLE 9. The remaining three trials that demonstrated efficacy showed similar results. Efficacy was demonstrated for seasonal allergies rhinitis when montelukast was administered in the morning or the evening.
Table 9: Effects of Montelukast Sodium on Daytime Nasal Symptoms Score* in a Placebo-and Active-controlled Trial in Patients with Seasonal Allergic Rhinitis (ANCOVA Model)
|
* Average of individual scores of nasal congestion, rhinorrhea, nasal itching, sneezing as assessed by patients on a 0 to 3 categorical scale. |
|||
|
† Statistically different from placebo (p≤0.001). |
|||
|
‡ The study was not designed for statistical comparison between montelukast sodium and the active control (loratadine). |
|||
| Treatment Group (N)
| Baseline Mean Score
| Mean Change from Baseline
| Difference Between Treatment and Placebo
(95% CI) Least-Squares Mean |
| Montelukast 10 mg (344)
| 2.09
| -0.39
| -0.13
† (-0.21, -0.06)
|
| Placebo (351)
| 2.10
| -0.26
| N.A.
|
| Active Control
‡
(Loratadine 10 mg) (599) | 2.06
| -0.46
| -0.24
† (-0.31, -0.17)
|
The efficacy of montelukast sodium tablets for the treatment of perennial allergic rhinitis was investigated in 2 randomized, double-blind, placebo-controlled studies conducted in North America and Europe. The two studies enrolled a total of 3,357 patients, of whom 1,632 received montelukast sodium 10 mg tablets. Patients 15 to 82 years of age with perennial allergic rhinitis as confirmed by history and a positive skin test to at least one relevant perennial allergen (dust mites, animal dander, and/or mold spores), who had active symptoms at the time of study entry, were enrolled.
In the study in which efficacy was demonstrated, the median age was 35 years (range 15 to 81); 64.1% were females and 35.9% were males. The ethnic/racial distribution in this study was 83.2% Caucasian, 8.1% Black, 5.4% Hispanic, 2.3% Asian, and 1.0% other origins. Montelukast sodium 10 mg tablets once daily was shown to significantly reduce symptoms of perennial allergic rhinitis over a 6-week treatment period (TABLE 10); in this study the primary outcome variable was mean change from baseline in daytime nasal symptoms score (the average of individual scores of nasal congestion, rhinorrhea, and sneezing).
Table 10: Effects of Montelukast Sodium on Daytime Nasal Symptoms Score* in a Placebo-controlled Trial in Patients with Perennial Allergic Rhinitis (ANCOVA Model)
|
* Average of individual scores of nasal congestion, rhinorrhea, sneezing as assessed by patients on a 0 to 3 categorical scale. |
|||
|
† Statistically different from placebo (p≤0.001). |
|||
| Treatment Group (N)
| Baseline
Mean Score | Mean Change from Baseline
| Difference Between Treatment
and Placebo (95% CI) Least- Squares Mean |
| Montelukast 10 mg (1,000)
| 2.09
| -0.42
| -0.08
† (-0.12, -0.04)
|
| Placebo (980)
| 2.10
| -0.35
| N.A.
|
The other 6-week study evaluated montelukast 10 mg (n = 626), placebo (n = 609), and an active-control (cetirizine 10 mg; n = 120). The primary analysis compared the mean change from baseline in daytime nasal symptoms score for montelukast sodium vs. placebo over the first 4 weeks of treatment; the study was not designed for statistical comparison between montelukast sodium and the active-control. The primary outcome variable included nasal itching in addition to nasal congestion, rhinorrhea, and sneezing. The estimated difference between montelukast sodium and placebo was -0.04 with a 95% CI of (-0.09, 0.01). The estimated difference between the active-control and placebo was -0.10 with a 95% CI of (-0.19, -0.01).
16 HOW SUPPLIED/STORAGE AND HANDLING
Montelukast Sodium Chewable Tablets USP, 4 mg are pink oval tablets, debossed with '227' on one side and plain on the other side.
NDC 58657-715-30 unit of use high-density polyethylene (HDPE) bottles of 30 with a polypropylene child-resistant cap, an aluminum foil induction seal, and silica gel desiccant
NDC 58657-715-90 unit of use high-density polyethylene (HDPE) bottles of 90 with a polypropylene child-resistant cap, an aluminum foil induction seal, and silica gel desiccant
Montelukast Sodium Chewable Tablets USP, 5 mg pink round tablets, debossed with '226' on one side and plain on the other side.
NDC 58657-716-30 unit of use high-density polyethylene (HDPE) bottles of 30 with a polypropylene child-resistant cap, an aluminum foil induction seal, and silica gel desiccant
NDC 58657-716-90 unit of use high-density polyethylene (HDPE) bottles of 90 with a polypropylene child-resistant cap, an aluminum foil induction seal, and silica gel desiccant
Storage
Store at 25°C (77°F), excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Protect from moisture and light. Store in original package.
17 PATIENT COUNSELING INFORMATION
For the chewable tablets, advise the patient and/or caregiver to read the FDA-approved patient labeling (Medication Guide).
- Advise patients about the potential risk for serious neuropsychiatric symptoms and behavioral changes with montelukast sodium use [see Warnings and Precautions ( 5.1)] .
- Discuss the benefits and risks of montelukast sodium with patients when prescribing or continuing treatment with montelukast sodium [see Warnings and Precautions ( 5.1)] .
- Advise patients to monitor for changes in behavior or neuropsychiatric symptoms in patients taking montelukast sodium [see Warnings and Precautions ( 5.1)] .
- Instruct patients to discontinue montelukast sodium and contact a healthcare provider immediately if changes in behavior or thinking that are not typical for the patient occur, or if the patient develops suicidal ideation or suicidal behavior [see Warnings and Precautions ( 5.1)] .
- Advise patients to take montelukast sodium daily as prescribed, even when they are asymptomatic, as well as during periods of worsening asthma, and to contact their physicians if their asthma is not well controlled.
- Advise patients that oral montelukast sodium is not for the treatment of acute asthma attacks. They should have appropriate short-acting inhaled β-agonist medication available to treat asthma exacerbations. Patients who have exacerbations of asthma after exercise should be instructed to have available for rescue a short-acting inhaled β-agonist. Daily administration of montelukast sodium for the chronic treatment of asthma has not been established to prevent acute episodes of EIB [see Warnings and Precautions ( 5.2)] .
- Advise patients to seek medical attention if short-acting inhaled bronchodilators are needed more often than usual, or if more than the maximum number of inhalations of short-acting bronchodilator treatment prescribed for a 24 hour period are needed.
- Instruct patients to continue other anti-asthma medications as prescribed unless instructed by a physician.
- Instruct patients with known aspirin sensitivity to continue avoidance of aspirin or non-steroidal anti-inflammatory agents while taking montelukast sodium [see Warnings and Precautions ( 5.4)] .
Graviti Pharmaceuticals Inc.,
Wilmington, Delaware-19801, USA.
Manufactured by:
Graviti Pharmaceuticals Pvt. Ltd.
Telangana-502307, INDIA.
Revised: 11/2021
MEDICATION GUIDE
Montelukast Sodium Chewable Tablets, USP
(mon te loo′kast soe′dee um)
What is the most important information I should know about montelukast sodium chewable tablets?
Serious mental health problems have happened in people taking montelukast sodium chewable tablets or even after treatment has stopped. This can happen in people with or without a history of mental health problems. Stop taking montelukast sodium chewable tablets and tell your healthcare provider right away if you or your child have any unusual changes in behavior or thinking, including any of these symptoms:
- agitation, including aggressive behavior or hostility
- hallucinations (seeing or hearing things that are not really there)
- suicidal thoughts and actions (including suicide)
- attention problems
- memory problems
- tremor
- bad or vivid dreams
- obsessive-compulsive symptoms
- trouble sleeping
- depression
- restlessness
- uncontrolled muscle movements
- disorientation (confusion)
- sleep walking
- feeling anxious
- stuttering
- irritability
What are montelukast sodium chewable tablets?
Montelukast sodium chewable tablets are a prescription medicine that blocks substances in the body called leukotrienes. This may help to improve symptoms of asthma and inflammation of the lining of the nose (allergic rhinitis). Montelukast sodium chewable tablets does not contain a steroid. Montelukast sodium chewable tablets are used to:
- Prevent asthma attacks and for the long-term treatment of asthma in adults and children ages 2 years and older. Do not take montelukast sodium chewable tablets if you need relief right away for a sudden asthma attack. If you have an asthma attack, you should follow the instructions your healthcare provider gave you for treating asthma attacks.
- Prevent exercise-induced asthma in people 6 years of age and older.
- Help control the symptoms of allergic rhinitis such as sneezing, stuffy nose, runny nose, and itching of the nose. Montelukast sodium chewable tablets are used to treat the following in people who have already taken other medicines that did not work well enough or in people who could not tolerate other medicines:
- outdoor allergies that happen part of the year (seasonal allergic rhinitis) in adults and children ages 2 years and older, and
- indoor allergies that happen all year (perennial allergic rhinitis) in adults and children ages 2 years and older.
Do not take montelukast sodium chewable tablets if you are allergic to any of its ingredients. See the end of this Medication Guide for a complete list of the ingredients in montelukast sodium chewable tablets.
Before taking montelukast sodium chewable tablets, tell your healthcare provider about all your medical conditions, including if you:
- are allergic to aspirin.
- have phenylketonuria. Montelukast sodium chewable tablets contain aspartame, a source of phenylalanine.
- have or have had mental health problems.
- are pregnant or plan to become pregnant. Talk to your healthcare provider if you are pregnant or plan to become pregnant, montelukast sodium chewable tablets may not be right for you.
- are breastfeeding or plan to breastfeed. It is not known if montelukast sodium passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby while taking montelukast sodium chewable tablets.
Tell your healthcare provider about all the medicines you take, including prescription and over the counter medicines, vitamins, and herbal supplements. Some medicines may affect how montelukast sodium chewable tablets works, or montelukast sodium chewable tablets may affect how your other medicines work.
How should I take montelukast sodium chewable tablets?
For anyone who takes montelukast sodium chewable tablets:
- Take montelukast sodium chewable tablets exactly as prescribed by your healthcare provider. Your healthcare provider will tell you how much montelukast sodium chewable tablets to take, and when to take it .
- Stop taking montelukast sodium chewable tablets and tell your healthcare provider right away if you or your child have any unusual changes in behavior or thinking.
- You can take montelukast sodium chewable tablets with food or without food.
- If you or your child misses a dose of montelukast sodium chewable tablets, just take the next dose at your regular time. Do not take 2 doses at the same time.
- If you take too much montelukast sodium chewable tablets, call your healthcare provider right away.
For adults and children 2 years of age and older with asthma:
- Take montelukast sodium chewable tablets 1 time each day, in the evening. Continue to take montelukast sodium chewable tablets every day for as long as your healthcare provider prescribes it, even if you have no asthma symptoms.
- Tell your healthcare provider right away if your asthma symptoms get worse, or if you need to use your rescue inhaler medicine more often for asthma attacks.
- Always have your rescue inhaler medicine with you for asthma attacks.
- Continue to take your other asthma medicines as prescribed unless your healthcare provider tells you to change how you take these medicines.
For people 6 years of age and older for the prevention of exercise-induced asthma:
- Take montelukast sodium chewable tablets at least 2 hours before exercise.
- Always have your rescue inhaler medicine with you for asthma attacks.
- If you take montelukast sodium chewable tablets every day for chronic asthma or allergic rhinitis, do not take another dose to prevent exercise-induced asthma. Talk to your healthcare provider about your treatment for exercise-induced asthma.
- Do not take 2 doses of montelukast sodium chewable tablets within 24 hours (1 day).
For anyone 2 years of age and older with seasonal allergic rhinitis, or for anyone 6 months of age and older with perennial allergic rhinitis:
- Take montelukast sodium chewable tablets 1 time each day, at about the same time each day.
What should I avoid while taking montelukast sodium chewable tablets?
If you have asthma and aspirin makes your asthma symptoms worse, continue to avoid taking aspirin or other medicines called non-steroidal anti-inflammatory drugs (NSAIDs) while taking montelukast sodium chewable tablets.
What are the possible side effects of montelukast sodium chewable tablets?
Montelukast sodium chewable tablets may cause serious side effects, including:
- See "What is the most important information I should know about montelukast sodium chewable tablets?"
- Increase in certain white blood cells (eosinophils) and possible inflamed blood vessels throughout the body (systemic vasculitis). Rarely, this can happen in people with asthma who take montelukast sodium chewable tablets. This sometimes happens in people who also take a steroid medicine by mouth that is being stopped or the dose is being lowered.
Tell your healthcare provider right away if you get one or more of these symptoms:
- a feeling of pins and needles or numbness of arms or legs
- rash
- severe inflammation (pain and swelling) of the sinuses (sinusitis)
- a flu-like illness
The most common side effects of montelukast sodium chewable tablets include:
- upper respiratory infection
- cough
- flu
- fever
- stomach pain
- runny nose
- headache
- diarrhea
- sinus infection
- sore throat
- earache or ear infection
These are not all the possible side effects of montelukast sodium chewable tablets. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store montelukast sodium chewable tablets?
- Store montelukast sodium chewable tablets at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep montelukast sodium chewable tablets in the package it comes in.
- Keep montelukast sodium chewable tablets in a dry place and keep it away from light.
- Keep montelukast sodium chewable tablets and all medicines out of reach of children.
General information about the safe and effective use of montelukast sodium chewable tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use montelukast sodium chewable tablets for a condition for which it was not prescribed. Do not give montelukast sodium chewable tablets to other people even if they have the same symptoms you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about montelukast sodium chewable tablets that is written for health professionals.
What are the ingredients in montelukast sodium chewable tablets?
Active ingredient: montelukast sodium
Inactive ingredients:
- 4 mg and 5 mg chewable tablets: mannitol, microcrystalline cellulose, hydroxypropyl cellulose, red ferric oxide, croscarmellose sodium, cherry flavor, aspartame, and magnesium stearate.
Graviti Pharmaceuticals Inc.,
Wilmington, Delaware-19801, USA.
Manufactured by:
Graviti Pharmaceuticals Pvt. Ltd.
Telangana-502307, INDIA.
This Medication Guide has been approved by the U.S. Food and Drug Administration
Revised: 11/2021
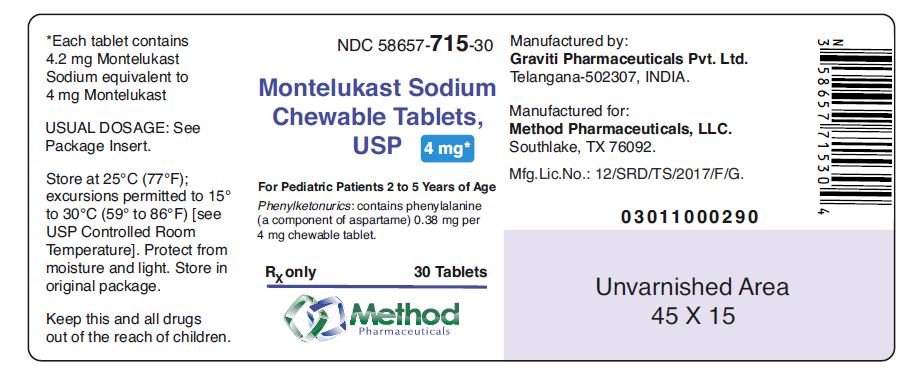
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 58657- 715-30
Montelukast Sodium Chewable Tablets, USP
4 mg*
For Pediatric Patients 2 to 5 Years of Age
Phenylketonurics: contains phenylalanine (a component of aspartame) 0.38 mg per 4 mg chewable tablet.
Rx only
30 Tablets
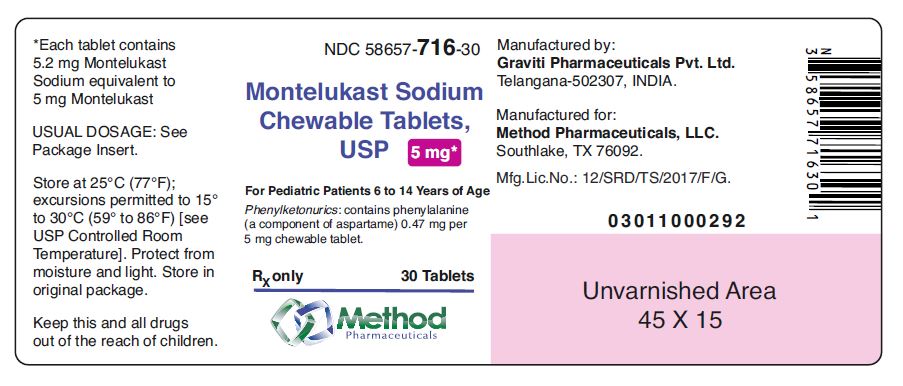
NDC 58657- 716-30
Montelukast Sodium Chewable Tablets, USP
4 mg*
For Pediatric Patients 2 to 5 Years of Age
Phenylketonurics: contains phenylalanine (a component of aspartame) 0.38 mg per 4 mg chewable tablet.
Rx only
30 Tablets
| MONTELUKAST SODIUM
montelukast sodium tablet, chewable |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| MONTELUKAST SODIUM
montelukast sodium tablet, chewable |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Method Pharmaceuticals, LLC (060216698) |