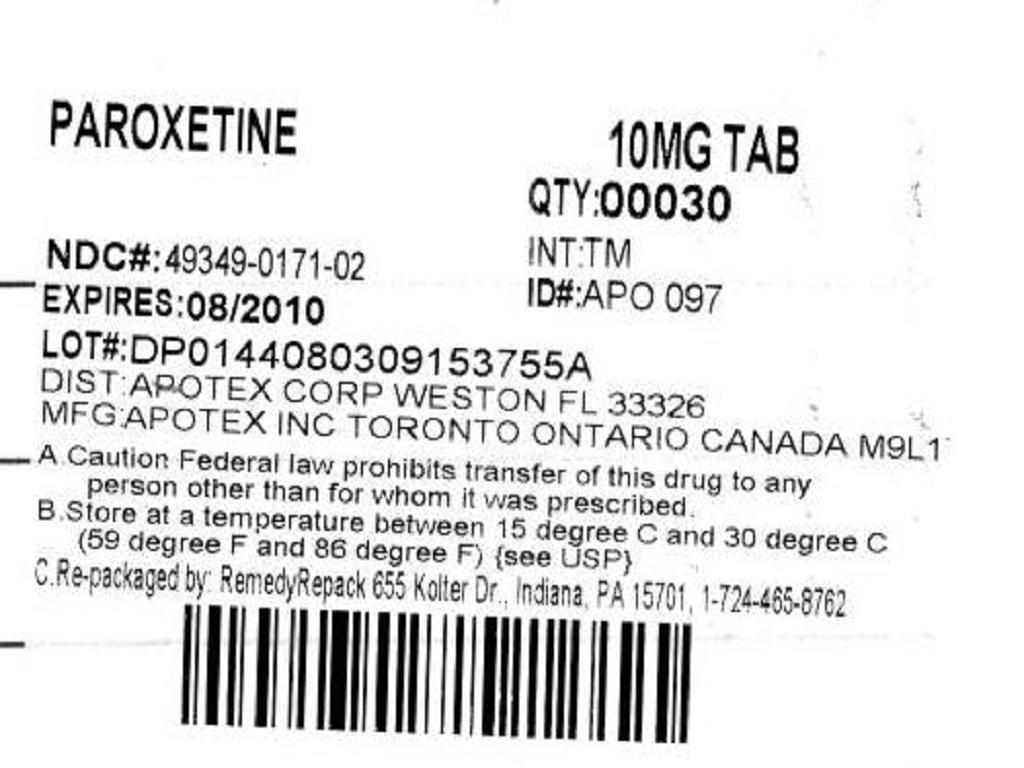
PAROXETINE- paroxetine tablet
REMEDYREPACK INC.
----------
DESCRIPTION
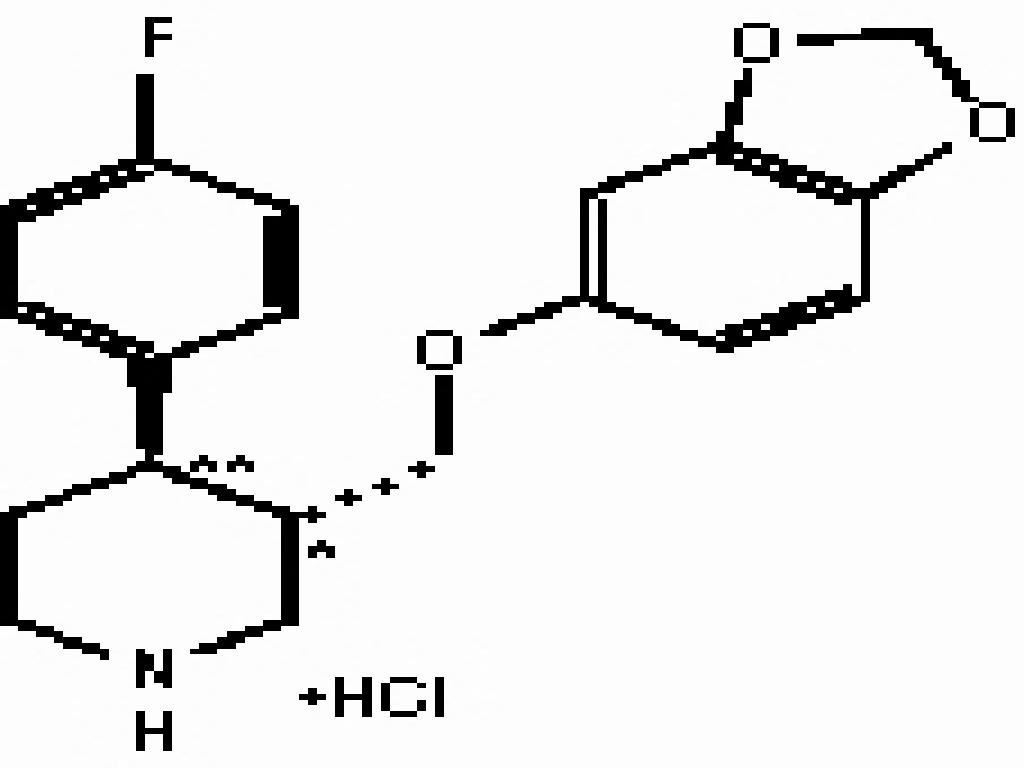
Paroxetine hydrochloride is an orally administered psychotropic drug. It is the hydrochloride salt of a phenylpiperidine compound identified chemically as (-)-trans-4R-(4'-fluorophenyl)-3S-[(3',4'-methylenedioxyphenoxy) methyl] piperidine hydrochloride anhydrous and has the empirical formula of C19H20FNO3HCl. The molecular weight is 365.8 (anhydrous) (329.4 as free base). The structural formula of paroxetine hydrochloride is:
Paroxetine hydrochloride is an odorless, off-white powder, having a melting point range of 116to 120and a solubility of 5.4 mg/mL in water.
Paroxetine tablets USP comply with USP Related Impurities Test 1.
CLINICAL PHARMACOLOGY
Pharmacodynamics
Because the relative potencies of paroxetine's major metabolites are at most 1/50 of the parent compound, they are essentially inactive.
Pharmacokinetics
Paroxetine hydrochloride is completely absorbed after oral dosing of a solution of the hydrochloride salt. The mean elimination half-life is approximately 21 hours (CV 32%) after oral dosing of 30 mg tablets of paroxetine daily for 30 days. Paroxetine is extensively metabolized and the metabolites are considered to be inactive. Nonlinearity in pharmacokinetics is observed with increasing doses. Paroxetine metabolism is mediated in part by CYP2D6, and the metabolites are primarily excreted in the urine and to some extent in the feces. Pharmacokinetic behavior of paroxetine has not been evaluated in subjects who are deficient in CYP2D6 (poor metabolizers).
Absorption and Distribution
Paroxetine is equally bioavailable from the oral suspension and tablet.
Paroxetine hydrochloride is completely absorbed after oral dosing of a solution of the hydrochloride salt. In a study in which normal male subjects (n = 15) received 30 mg tablets daily for 30 days, steady-state paroxetine concentrations were achieved by approximately 10 days for most subjects, although it may take substantially longer in an occasional patient. At steady state, mean values of Cmax, Tmax,Cmin, and Twere 61.7 ng/mL (CV 45%), 5.2 hr. (CV 10%), 30.7 ng/mL (CV 67%), and 21.0 hours (CV 32%), respectively. The steady-state Cmax and Cmin values were about 6 and 14 times what would be predicted from single-dose studies. Steady-state drug exposure based on AUC0-24 was about 8 times greater than would have been predicted from single-dose data in these subjects. The excess accumulation is a consequence of the fact that 1 of the enzymes that metabolizes paroxetine is readily saturable.
The effects of food on the bioavailability of paroxetine were studied in subjects administered a single dose with and without food. AUC was only slightly increased (6%) when drug was administered with food but the Cmax was 29% greater, while the time to reach peak plasma concentration decreased from 6.4 hours post-dosing to 4.9 hours.
Paroxetine distributes throughout the body, including the CNS, with only 1% remaining in the plasma.
Approximately 95% and 93% of paroxetine is bound to plasma protein at 100 ng/mL and 400 ng/mL, respectively. Under clinical conditions, paroxetine concentrations would normally be less than 400 ng/mL. Paroxetine does not alter the in vitro protein binding of phenytoin or warfarin.
Metabolism and Excretion
The mean elimination half-life is approximately 21 hours (CV 32%) after oral dosing of 30 mg tablets daily for 30 days of paroxetine hydrochloride. In steady-state dose proportionality studies involving elderly and nonelderly patients, at doses of 20 mg to 40 mg daily for the elderly and 20 mg to 50 mg daily for the nonelderly, some nonlinearity was observed in both populations, again reflecting a saturable metabolic pathway. In comparison to Cmin values after 20 mg daily, values after 40 mg daily were only about 2 to 3 times greater than doubled.
Paroxetine is extensively metabolized after oral administration. The principal metabolites are polar and conjugated products of oxidation and methylation, which are readily cleared. Conjugates with glucuronic acid and sulfate predominate, and major metabolites have been isolated and identified. Data indicate that the metabolites have no more than 1/50 the potency of the parent compound at inhibiting serotonin uptake. The metabolism of paroxetine is accomplished in part by CYP2D6. Saturation of this enzyme at clinical doses appears to account for the nonlinearity of paroxetine kinetics with increasing dose and increasing duration of treatment. The role of this enzyme in paroxetine metabolism also suggests potential drug-drug interactions (see PRECAUTIONS).
Approximately 64% of a 30-mg oral solution dose of paroxetine was excreted in the urine with 2% as the parent compound and 62% as metabolites over a 10-day post-dosing period. About 36% was excreted in the feces (probably via the bile), mostly as metabolites and less than 1% as the parent compound over the 10-day post-dosing period.
Other Clinical Pharmacology Information
Specific Populations
Renal and Liver Disease
Increased plasma concentrations of paroxetine occur in subjects with renal and hepatic impairment. The mean plasma concentrations in patients with creatinine clearance below 30 mL/min. was approximately 4 times greater than seen in normal volunteers. Patients with creatinine clearance of 30 to 60 mL/min. and patients with hepatic functional impairment had about a 2-fold increase in plasma concentrations (AUC, Cmax).
The initial dosage should therefore be reduced in patients with severe renal or hepatic impairment, and upward titration, if necessary, should be at increased intervals (see DOSAGE AND ADMINISTRATION).
Elderly Patients
In a multiple-dose study in the elderly at daily paroxetine doses of 20, 30, and 40 mg, Cmin concentrations were about 70% to 80% greater than the respective Cmin concentrations in nonelderly subjects. Therefore the initial dosage in the elderly should be reduced (see DOSAGE AND ADMINISTRATION).
Drug-Drug Interactions
In vitro drug interaction studies reveal that paroxetine inhibits CYP2D6. Clinical drug interaction studies have been performed with substrates of CYP2D6 and show that paroxetine can inhibit the metabolism of drugs metabolized by CYP2D6 including desipramine, risperidone, and atomoxetine (see PRECAUTIONSDrug Interactions).
Clinical Trials
Major Depressive Disorder
The efficacy of paroxetine as a treatment for major depressive disorder has been established in 6 placebo-controlled studies of patients with major depressive disorder (aged 18 to 73). In these studies, paroxetine was shown to be significantly more effective than placebo in treating major depressive disorder by at least 2 of the following measures: Hamilton Depression Rating Scale (HDRS), the Hamilton depressed mood item, and the Clinical Global Impression (CGI)-Severity of Illness. Paroxetine was significantly better than placebo in improvement of the HDRS sub-factor scores, including the depressed mood item, sleep disturbance factor, and anxiety factor.
A study of outpatients with major depressive disorder who had responded to paroxetine (HDRS total score <8) during an initial 8-week open-treatment phase and were then randomized to continuation on paroxetine or placebo for 1 year demonstrated a significantly lower relapse rate for patients taking paroxetine (15%) compared to those on placebo (39%). Effectiveness was similar for male and female patients.
Obsessive Compulsive Disorder
The effectiveness of paroxetine in the treatment of obsessive compulsive disorder (OCD) was demonstrated in two 12-week multicenter placebo-controlled studies of adult outpatients (Studies 1 and 2). Patients in all studies had moderate to severe OCD (DSM-IIIR) with mean baseline ratings on the Yale Brown Obsessive Compulsive Scale (YBOCS) total score ranging from 23 to 26. Study 1, a dose-range finding study where patients were treated with fixed doses of 20, 40, or 60 mg of paroxetine/day demonstrated that daily doses of paroxetine 40 and 60 mg are effective in the treatment of OCD. Patients receiving doses of 40 and 60 mg paroxetine experienced a mean reduction of approximately 6 and 7 points, respectively, on the YBOCS total score which was significantly greater than the approximate 4-point reduction at 20 mg and a 3-point reduction in the placebo-treated patients. Study 2 was a flexible-dose study comparing paroxetine (20 to 60 mg daily) with clomipramine (25 to 250 mg daily). In this study, patients receiving paroxetine experienced a mean reduction of approximately 7 points on the YBOCS total score, which was significantly greater than the mean reduction of approximately 4 points in placebo-treated patients.
The following table provides the outcome classification by treatment group on Global Improvement items of the Clinical Global Impression (CGI) scale for Study 1.
Outcome Classification (%) on CGI-Gloval Improvement Itemfor Completers in Study 1OutcomePlaceboParoxetine 20 mgParoxetine 40 mgParoxetine 60 mgClassification(n=74)(n=75)(n=66)(n=66)Worse14%7%7%3%No Change44%35%22%19%Minimally Improved24%33%29%34%Much Improved11%18%22%24%Very Much7%7%20%20%ImprovedSubgroup analyses did not indicate that there were any differences in treatment outcomes as a function of age or gender.
The long-term maintenance effects of paroxetine in OCD were demonstrated in a long-term extension to Study 1. Patients who were responders on paroxetine during the 3-month double-blind phase and a 6-month extension on open-label paroxetine (20 to 60 mg/day) were randomized to either paroxetine or placebo in a 6-month double-blind relapse prevention phase. Patients randomized to paroxetine were significantly less likely to relapse than comparably treated patients who were randomized to placebo.
Panic Disorder
The effectiveness of paroxetine in the treatment of panic disorder was demonstrated in three 10- to 12-week multicenter, placebo-controlled studies of adult outpatients (Studies 1-3). Patients in all studies had panic disorder (DSM-IIIR), with or without agoraphobia. In these studies, paroxetine was shown to be significantly more effective than placebo in treating panic disorder by at least 2 out of 3 measures of panic attack frequency and on the Clinical Global Impression Severity of Illness score.
Study 2 was a 12-week flexible-dose study comparing paroxetine (10 to 60 mg daily) and placebo. At endpoint, 51% of paroxetine patients were free of panic attacks compared to 32% of placebo-treated patients.
Study 3 was a 12-week flexible-dose study comparing paroxetine (10 to 60 mg daily) to placebo in patients concurrently receiving standardized cognitive behavioral therapy. At endpoint, 33% of the paroxetine-treated patients showed a reduction to 0 or 1 panic attacks compared to 14% of placebo patients.
In both Studies 2 and 3, the mean paroxetine dose for completers at endpoint was approximately 40 mg/day of paroxetine.
Long-term maintenance effects of paroxetine in panic disorder were demonstrated in an extension to Study 1. Patients who were responders during the 10-week double-blind phase and during a 3-month double-blind extension phase were randomized to either paroxetine (10, 20, or 40 mg/day) or placebo in a 3-month double-blind relapse prevention phase. Patients randomized to paroxetine were significantly less likely to relapse than comparably treated patients who were randomized to placebo.
Subgroup analyses did not indicate that there were any differences in treatment outcomes as a function of age or gender.
Social Anxiety Disorder
The effectiveness of paroxetine in the treatment of social anxiety disorder was demonstrated in three 12-week, multicenter, placebo-controlled studies (Studies 1, 2, and 3) of adult outpatients with social anxiety disorder (DSM-IV). In these studies, the effectiveness of paroxetine compared to placebo was evaluated on the basis of (1) the proportion of responders, as defined by a Clinical Global Impression (CGI) Improvement score of 1 (very much improved) or 2 (much improved), and (2) change from baseline in the Liebowitz Social Anxiety Scale (LSAS).
Studies 1 and 2 were flexible-dose studies comparing paroxetine (20 to 50 mg daily) and placebo. Paroxetine demonstrated statistically significant superiority over placebo on both the CGI Improvement responder criterion and the Liebowitz Social Anxiety Scale (LSAS). In Study 1, for patients who completed to week 12, 69% of paroxetine-treated patients compared to 29% of placebo-treated patients were CGI Improvement responders. In Study 2, CGI Improvement responders were 77% and 42% for the paroxetine- and placebo-treated patients, respectively.
Subgroup analyses generally did not indicate differences in treatment outcomes as a function of age, race, or gender.
Generalized Anxiety Disorder
The effectiveness of paroxetine in the treatment of Generalized Anxiety Disorder (GAD) was demonstrated in two 8-week, multicenter, placebo-controlled studies (Studies 1 and 2) of adult outpatients with Generalized Anxiety Disorder (DSM-IV).
Study 1 was an 8-week study comparing fixed paroxetine doses of 20 mg or 40 mg/day with placebo. Doses of 20 mg or 40 mg of paroxetine were both demonstrated to be significantly superior to placebo on the Hamilton Rating Scale for Anxiety (HAM-A) total score. There was not sufficient evidence in this study to suggest a greater benefit for the 40 mg/day dose compared to the 20 mg/day dose.
Study 2 was a flexible-dose study comparing paroxetine (20 mg to 50 mg daily) and placebo. Paroxetine demonstrated statistically significant superiority over placebo on the Hamilton Rating Scale for Anxiety (HAM-A) total score. A third study, also flexible-dose comparing paroxetine (20 mg to 50 mg daily), did not demonstrate statistically significant superiority of paroxetine over placebo on the Hamilton Rating Scale for Anxiety (HAM-A) total score, the primary outcome.
Subgroup analyses did not indicate differences in treatment outcomes as a function of race or gender. There were insufficient elderly patients to conduct subgroup analyses on the basis of age.
In a longer-term trial, 566 patients meeting DSM-IV criteria for Generalized Anxiety Disorder, who had responded during a single-blind, 8-week acute treatment phase with 20 to 50 mg/day of paroxetine, were randomized to continuation of paroxetine at their same dose, or to placebo, for up to 24 weeks of observation for relapse. Response during the single-blind phase was defined by having a decrease ofpoints compared to baseline on the CGI-Severity of Illness scale, to a score ofRelapse during the double-blind phase was defined as an increase ofpoints compared to baseline on the CGI-Severity of Illness scale to a score ofor withdrawal due to lack of efficacy. Patients receiving continued paroxetine experienced a significantly lower relapse rate over the subsequent 24 weeks compared to those receiving placebo.
INDICATIONS & USAGE
Major Depressive Disorder
Paroxetine is indicated for the treatment of major depressive disorder.
The efficacy of paroxetine in the treatment of a major depressive episode was established in 6-week controlled trials of outpatients whose diagnoses corresponded most closely to the DSM-III category of major depressive disorder (see CLINICAL PHARMACOLOGY
The effects of paroxetine in hospitalized depressed patients have not been adequately studied.
The efficacy of paroxetine in maintaining a response in major depressive disorder for up to 1 year was demonstrated in a placebo-controlled trial (see CLINICAL PHARMACOLOGYClinical Trials). Nevertheless, the physician who elects to use paroxetine for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient.
Obsessive Compulsive Disorder
Paroxetine is indicated for the treatment of obsessions and compulsions in patients with obsessive compulsive disorder (OCD) as defined in the DSM-IV. The obsessions or compulsions cause marked distress, are time-consuming, or significantly interfere with social or occupational functioning.
The efficacy of paroxetine was established in two 12-week trials with obsessive compulsive outpatients whose diagnoses corresponded most closely to the DSM-IIIR category of obsessive compulsive disorder (see CLINICAL PHARMACOLOGYClinical Trials).
Obsessive compulsive disorder is characterized by recurrent and persistent ideas, thoughts, impulses, or images (obsessions) that are ego-dystonic and/or repetitive, purposeful, and intentional behaviors (compulsions) that are recognized by the person as excessive or unreasonable.
Long-term maintenance of efficacy was demonstrated in a 6-month relapse prevention trial. In this trial, patients assigned to paroxetine showed a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGYClinical Trials). Nevertheless, the physician who elects to use paroxetine for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient (see DOSAGE AND ADMINISTRATION).
Panic Disorder
Paroxetine is indicated for the treatment of panic disorder, with or without agoraphobia, as defined in DSM-IV. Panic disorder is characterized by the occurrence of unexpected panic attacks and associated concern about having additional attacks, worry about the implications or consequences of the attacks, and/or a significant change in behavior related to the attacks.
The efficacy of paroxetine was established in three 10- to 12-week trials in panic disorder patients whose diagnoses corresponded to the DSM-IIIR category of panic disorder (see CLINICAL PHARMACOLOGYClinical Trials).
Long-term maintenance of efficacy was demonstrated in a 3-month relapse prevention trial. In this trial, patients with panic disorder assigned to paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGYClinical Trials). Nevertheless, the physician who prescribes paroxetine for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient.
Social Anxiety Disorder
Paroxetine is indicated for the treatment of social anxiety disorder, also known as social phobia, as defined in DSM-IV (300.23). Social anxiety disorder is characterized by a marked and persistent fear of 1 or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others. Exposure to the feared situation almost invariably provokes anxiety, which may approach the intensity of a panic attack. The feared situations are avoided or endured with intense anxiety or distress. The avoidance, anxious anticipation, or distress in the feared situation(s) interferes significantly with the person's normal routine, occupational or academic functioning, or social activities or relationships, or there is marked distress about having the phobias. Lesser degrees of performance anxiety or shyness generally do not require psychopharmacological treatment.
The efficacy of paroxetine was established in three 12-week trials in adult patients with social anxiety disorder (DSM-IV). Paroxetine has not been studied in children or adolescents with social phobia (see CLINICAL PHARMACOLOGYClinical Trials).
The effectiveness of paroxetine in long-term treatment of social anxiety disorder, i.e., for more than 12 weeks, has not been systematically evaluated in adequate and well-controlled trials. Therefore, the physician who elects to prescribe paroxetine for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient (see DOSAGE AND ADMINISTRATION).
Generalized Anxiety Disorder
Paroxetine is indicated for the treatment of Generalized Anxiety Disorder (GAD), as defined in DSM-IV. Anxiety or tension associated with the stress of everyday life usually does not require treatment with an anxiolytic.
The efficacy of paroxetine in the treatment of GAD was established in two 8-week placebo-controlled trials in adults with GAD. Paroxetine has not been studied in children or adolescents with Generalized Anxiety Disorder (see CLINICAL PHARMACOLOGYClinical Trials).
Generalized Anxiety Disorder (DSM-IV) is characterized by excessive anxiety and worry (apprehensive expectation) that is persistent for at least 6 months and which the person finds difficult to control. It must be associated with at least 3 of the following 6 symptoms: Restlessness or feeling keyed up or on edge, being easily fatigued, difficulty concentrating or mind going blank, irritability, muscle tension, sleep disturbance.
The efficacy of paroxetine in maintaining a response in patients with Generalized Anxiety Disorder, who responded during an 8-week acute treatment phase while taking paroxetine and were then observed for relapse during a period of up to 24 weeks, was demonstrated in a placebo-controlled trial (see CLINICAL PHARMACOLOGYClinical Trials). Nevertheless, the physician who elects to use paroxetine for extended periods should periodically re-evaluate the long-term usefulness of the drug for the individual patient (see DOSAGE AND ADMINISTRATION).
CONTRAINDICATIONS
Concomitant use in patients taking either monoamine oxidase inhibitors (MAOIs) or thioridazine is contraindicated (see WARNINGS and PRECAUTIONS).
Concomitant use in patients taking pimozide is contraindicated (see PRECAUTIONS).
Paroxetine is contraindicated in patients with a hypersensitivity to paroxetine or any of the inactive ingredients in paroxetine.
WARNINGS
Clinical Worsening and Suicide Risk
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
Table 1
Age RangeDrug-Placebo Difference in Numberof Cases of Suicidality per 1000Patients TreatedDrug-Related Increases<1814 additional cases18-245 additional casesDrug-Related Decreases25-641 fewer case6 fewer casesNo suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that abrupt discontinuation can be associated with certain symptoms (see PRECAUTIONS and DOSAGE AND ADMINISTRATION - Discontinuation of Treatment with Paroxetine, for a description of the risks of discontinuation of paroxetine).
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for paroxetine should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder
Potential for Interaction With Monoamine Oxidase Inhibitors
In patients receiving another serotonin reuptake inhibitor drug in combination with a monoamine oxidase inhibitor (MAOI), there have been reports of serious, sometimes fatal, reactions including hyperthermia, rigidity, myoclonus, autonomic instability with possible rapid fluctuations of vital signs, and mental status changes that include extreme agitation progressing to delirium and coma. These reactions have also been reported in patients who have recently discontinued that drug and have been started on an MAOI. Some cases presented with features resembling neuroleptic malignant syndrome. While there are no human data showing such an interaction with paroxetine, limited animal data on the effects of combined use of paroxetine and MAOIs suggest that these drugs may act synergistically to elevate blood pressure and evoke behavioral excitation. Therefore, it is recommended that paroxetine not be used in combination with an MAOI, or within 14 days of discontinuing treatment with an MAOI. At least 2 weeks should be allowed after stopping paroxetine before starting an MAOI.
Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome may occur with use of paroxetine, particularly with concomitant use of serotonergic drugs (including triptans) and with drugs which impair metabolism of serotonin (including MAOIs). Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile blood pressure, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination) and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea).
The concomitant use of paroxetine with MAOIs intended to treat depression is contraindicated (see CONTRAINDICATIONS and WARNINGSPotential for Interaction with Monoamine Oxidase Inhibitors).
If concomitant use of paroxetine with a 5-hydroxytryptamine receptor agonist (triptan) is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases (see PRECAUTIONSDrug Interactions).
The concomitant use of paroxetine with serotonin precursors (such as tryptophan) is not recommended (see PRECAUTIONSDrug Interactions).
Potential Interaction With Thioridazine
Thioridazine administration alone produces prolongation of the QTc interval, which is associated with serious ventricular arrhythmias, such as torsade de pointesarrhythmias, and sudden death. This effect appears to be dose related.
An in vivo study suggests that drugs which inhibit CYP2D6, such as paroxetine, will elevate plasma levels of thioridazine. Therefore, it is recommended that paroxetine not be used in combination with thioridazine (see CONTRAINDICATIONS and PRECAUTIONS).
Usage in Pregnancy
Teratogenic Effects
Epidemiological studies have shown that infants born to women who had first trimester paroxetine exposure had an increased risk of cardiovascular malformations, primarily ventricular and atrial septal defects (VSDs and ASDs). In general, septal defects range from those that are symptomatic and may require surgery to those that are asymptomatic and may resolve spontaneously. If a patient becomes pregnant while taking paroxetine, she should be advised of the potential harm to the fetus. Unless the benefits of paroxetine to the mother justify continuing treatment, consideration should be given to either discontinuing paroxetine therapy or switching to another antidepressant (see PRECAUTIONSDiscontinuation of Treatment with Paroxetine). For women who intend to become pregnant or are in their first trimester of pregnancy, paroxetine should only be initiated after consideration of the other available treatment options.
Animal Findings
Reproduction studies were performed at doses up to 50 mg/kg/day in rats and 6 mg/kg/day in rabbits administered during organogenesis. These doses are approximately 8 (rat) and 2 (rabbit) times the MRHD on an mg/m2 basis. These studies have revealed no evidence of teratogenic effects. However, in rats, there was an increase in pup deaths during the first 4 days of lactation when dosing occurred during the last trimester of gestation and continued throughout lactation. This effect occurred at a dose of 1 mg/kg/day or approximately one-sixth of the MRHD on an mg/m2 basis. The no-effect dose for rat pup mortality was not determined. The cause of these deaths is not known.
Nonteratogenic Effects
Neonates exposed to paroxetine hydrochloride and other SSRIs or serotonin and norepinephrine reuptake inhibitors (SNRIs), late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding. Such complications can arise immediately upon delivery. Reported clinical findings have included respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypotonia, hypertonia, hyperreflexia, tremor, jitteriness, irritability, and constant crying. These features are consistent with either a direct toxic effect of SSRIs and SNRIs or, possibly, a drug discontinuation syndrome. It should be noted that, in some cases, the clinical picture is consistent with serotonin syndrome (see WARNINGSPotential for Interaction With Monoamine Oxidase Inhibitors).
There have also been postmarketing reports of premature births in pregnant women exposed to paroxetine or other SSRIs.
When treating a pregnant woman with paroxetine during the third trimester, the physician should carefully consider both the potential risks and benefits of treatment (see DOSAGE AND ADMINISTRATION).
Physicians should note that in a prospective longitudinal study of 201 women with a history major depression who were euthymic at the beginning of pregnancy, women who discontinued antidepressant medication during pregnancy were more likely to experience a relapse of major depression than women who continued antidepressant medication.
PRECAUTIONS
General
Activation of Mania/Hypomania
During premarketing testing, hypomania or mania occurred in approximately 1.0% of unipolar patients treated with paroxetine compared to 1.1% of active-control and 0.3% of placebo-treated unipolar patients. In a subset of patients classified as bipolar, the rate of manic episodes was 2.2% for paroxetine and 11.6% for the combined active-control groups. As with all drugs effective in the treatment of major depressive disorder, paroxetine should be used cautiously in patients with a history of mania.
Seizures
During premarketing testing, seizures occurred in 0.1% of patients treated with paroxetine, a rate similar to that associated with other drugs effective in the treatment of major depressive disorder. Paroxetine should be used cautiously in patients with a history of seizures. It should be discontinued in any patient who develops seizures.
Discontinuation of Treatment With Paroxetine
Recent clinical trials supporting the various approved indications for paroxetine employed a taper-phase regimen, rather than an abrupt discontinuation of treatment. The taper-phase regimen used in GAD clinical trials involved an incremental decrease in the daily dose by 10 mg/day at weekly intervals. When a daily dose of 20 mg/day was reached, patients were continued on this dose for 1 week before treatment was stopped.
With this regimen in those studies, the following adverse events were reported at an incidence of 2% or greater for paroxetine and were at least twice that reported for placebo: Abnormal dreams, paresthesia, and dizziness. In the majority of patients, these events were mild to moderate and were self-limiting and did not require medical intervention.
During marketing of paroxetine and other SSRIs and SNRIs, there have been spontaneous reports of adverse events occurring, upon the discontinuation of these drugs (particularly when abrupt), including the following: Dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesias such as electric shock sensations and tinnitus), anxiety, confusion, headache, lethargy, emotional lability, insomnia, and hypomania. While these events are generally self-limiting, there have been reports of serious discontinuation symptoms.
Patients should be monitored for these symptoms when discontinuing treatment with paroxetine. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate (see DOSAGE AND ADMINISTRATION).
See also PRECAUTIONSPediatric Use, for adverse events reported upon discontinuation of treatment with paroxetine in pediatric patients.
Akathisia
The use of paroxetine or other SSRIs has been associated with the development of akathisia, which is characterized by an inner sense of restlessness and psychomotor agitation such as an inability to sit or stand still usually associated with subjective distress. This is most likely to occur within the first few weeks of treatment.
Hyponatremia
Several cases of hyponatremia have been reported. The hyponatremia appeared to be reversible when paroxetine was discontinued. The majority of these occurrences have been in elderly individuals, some in patients taking diuretics or who were otherwise volume depleted.
Abnormal Bleeding
Published case reports have documented the occurrence of bleeding episodes in patients treated with psychotropic agents that interfere with serotonin reuptake. Subsequent epidemiological studies, both of the case-control and cohort design, have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding. In 2 studies, concurrent use of a nonsteroidal anti-inflammatory drug (NSAID) or aspirin potentiated the risk of bleeding (see Drug Interactions). Although these studies focused on upper gastrointestinal bleeding, there is reason to believe that bleeding at other sites may be similarly potentiated. Patients should be cautioned regarding the risk of bleeding associated with the concomitant use of paroxetine with NSAIDs, aspirin, or other drugs that affect coagulation.
Use in Patients With Concomitant Illness
Clinical experience with paroxetine in patients with certain concomitant systemic illness is limited. Caution is advisable in using paroxetine in patients with diseases or conditions that could affect metabolism or hemodynamic responses.
As with other SSRIs, mydriasis has been infrequently reported in premarketing studies with paroxetine. A few cases of acute angle closure glaucoma associated with paroxetine therapy have been reported in the literature. As mydriasis can cause acute angle closure in patients with narrow angle glaucoma, caution should be used when paroxetine is prescribed for patients with narrow angle glaucoma.
Paroxetine has not been evaluated or used to any appreciable extent in patients with a recent history of myocardial infarction or unstable heart disease. Patients with these diagnoses were excluded from clinical studies during the product's premarket testing. Evaluation of electrocardiograms of 682 patients who received paroxetine in double-blind, placebo-controlled trials, however, did not indicate that paroxetine is associated with the development of significant ECG abnormalities. Similarly, paroxetine does not cause any clinically important changes in heart rate or blood pressure.
Increased plasma concentrations of paroxetine occur in patients with severe renal impairment (creatinine clearance <30 mL/min.) or severe hepatic impairment. A lower starting dose should be used in such patients (see DOSAGE AND ADMINISTRATION).
INFORMATION FOR PATIENTS
Paroxetine tablets USP should not be chewed or crushed, and should be swallowed whole.
Patients should be cautioned about the risk of serotonin syndrome with the concomitant use of paroxetine and triptans, tramadol, or other serotonergic agents.
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with paroxetine and should counsel them in its appropriate use. A patient Medication Guide about "Antidepressant Medicines, Depression and other Serious Mental Illness, and Suicidal Thoughts or Actions" is available for paroxetine tablets USP. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking paroxetine tablets USP.
Clinical Worsening and Suicide Risk
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient's prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient's presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
Drugs That Interfere With Hemostasis (NSAIDs, Aspirin, Warfarin, etc.)
Patients should be cautioned about the concomitant use of paroxetine and NSAIDs, aspirin, or other drugs that affect coagulation since the combined use of psychotropic drugs that interfere with serotonin reuptake and these agents has been associated with an increased risk of bleeding.
Interference With Cognitive and Motor Performance
Any psychoactive drug may impair judgment, thinking, or motor skills. Although in controlled studies paroxetine has not been shown to impair psychomotor performance, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that therapy with paroxetine does not affect their ability to engage in such activities.
Completing Course of Therapy
While patients may notice improvement with treatment with paroxetine in 1 to 4 weeks, they should be advised to continue therapy as directed.
Concomitant Medication
Patients should be advised to inform their physician if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions.
Alcohol
Although paroxetine has not been shown to increase the impairment of mental and motor skills caused by alcohol, patients should be advised to avoid alcohol while taking paroxetine.
Pregnancy
Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during therapy. (See WARNINGSUsage in Pregnancy: Teratogenic and Nonteratogenic Effects).
Nursing
Patients should be advised to notify their physician if they are breast-feeding an infant (see PRECAUTIONSNursing Mothers).
DRUG INTERACTIONS
Tryptophan
As with other serotonin reuptake inhibitors, an interaction between paroxetine and tryptophan may occur when they are coadministered. Adverse experiences, consisting primarily of headache, nausea, sweating, and dizziness, have been reported when tryptophan was administered to patients taking paroxetine. Consequently, concomitant use of paroxetine with tryptophan is not recommended (see WARNINGSSerotonin Syndrome).
Monoamine Oxidase Inhibitors
See CONTRAINDICATIONS and WARNINGS.
Pimozide
In a controlled study of healthy volunteers, after paroxetine was titrated to 60 mg daily, co-administration of a single dose of 2 mg pimozide was associated with mean increases in pimozide AUC of 151% and Cmax of 62%, compared to pimozide administered alone. Due to the narrow therapeutic index of pimozide and its known ability to prolong the QT interval, concomitant use of pimozide and paroxetine is contraindicated (see CONTRAINDICATIONS).
Serotonergic Drugs
Based on the mechanism of action of paroxetine hydrochloride and the potential for serotonin syndrome, caution is advised when paroxetine is coadministered with other drugs or agents that may affect the serotonergic neurotransmitter systems, such as triptans, linezolid (an antibiotic which is a reversible non-selective MAOI), lithium, tramadol, or St. John's Wort (see WARNINGSSerotonin Syndrome). The concomitant use of paroxetine with other SSRIs, SNRIs or tryptophan is not recommended (see PRECAUTIONSDrug Interactions, Tryptophan).
Thioridazine
See CONTRAINDICATIONS and WARNINGS.
Warfarin
Preliminary data suggest that there may be a pharmacodynamic interaction (that causes an increased bleeding diathesis in the face of unaltered prothrombin time) between paroxetine and warfarin. Since there is little clinical experience, the concomitant administration of paroxetine and warfarin should be undertaken with caution (see Drugs That Interfere With Hemostasis).
Triptans
There have been rare postmarketing reports of serotonin syndrome with the use of an SSRI and a triptan. If concomitant use of paroxetine with a triptan is clinically warranted, careful observation of the patient is advised, particularly during treatment initiation and dose increases (see WARNINGSSerotonin Syndrome).
Drugs Affecting Hepatic Metabolism
The metabolism and pharmacokinetics of paroxetine may be affected by the induction or inhibition of drug-metabolizing enzymes.
Cimetidine
Cimetidine inhibits many cytochrome P450 (oxidative) enzymes. In a study where paroxetine (30 mg once daily) was dosed orally for 4 weeks, steady-state plasma concentrations of paroxetine were increased by approximately 50% during coadministration with oral cimetidine (300 mg three times daily) for the final week. Therefore, when these drugs are administered concurrently, dosage adjustment of paroxetine after the 20-mg starting dose should be guided by clinical effect. The effect of paroxetine on cimetidine's pharmacokinetics was not studied.
Phenobarbital
Phenobarbital induces many cytochrome P450 (oxidative) enzymes. When a single oral 30-mg dose of paroxetine was administered at phenobarbital steady state (100 mg once daily for 14 days), paroxetine AUC and T
Phenytoin
When a single oral 30-mg dose of paroxetine was administered at phenytoin steady state (300 mg once daily for 14 days), paroxetine AUC and TPostmarketing Reports).
Drugs Metabolized by CYP2D6
Many drugs, including most drugs effective in the treatment of major depressive disorder (paroxetine, other SSRIs and many tricyclics), are metabolized by the cytochrome P450 isozyme CYP2D6. Like other agents that are metabolized by CYP2D6, paroxetine may significantly inhibit the activity of this isozyme. In most patients (>90%), this CYP2D6 isozyme is saturated early during dosing with paroxetine. In 1 study, daily dosing of paroxetine (20 mg once daily) under steady-state conditions increased single dose desipramine (100 mg) Cmax, AUC, and Tby an average of approximately 2-, 5-, and 3-fold, respectively. Concomitant use of paroxetine with risperidone, a CYP2D6 substrate has also been evaluated. In 1 study, daily dosing of paroxetine 20 mg in patients stabilized on risperidone (4 to 8 mg/day) increased mean plasma concentrations of risperidone approximately 4-fold, decreased 9-hydroxyrisperidone concentrations approximately 10%, and increased concentrations of the active moiety (the sum of risperidone plus 9-hydroxyrisperidone) approximately 1.4-fold. The effect of paroxetine on the pharmacokinetics of atomoxetine has been evaluated when both drugs were at steady state. In healthy volunteers who were extensive metabolizers of CYP2D6, paroxetine 20 mg daily was given in combination with 20 mg atomoxetine every 12 hours. This resulted in increases in steady state atomoxetine AUC values that were 6- to 8-fold greater and in atomoxetine Cmax values that were 3- to 4-fold greater than when atomoxetine was given alone. Dosage adjustment of atomoxetine may be necessary and it is recommended that atomoxetine be initiated at a reduced dose when it is given with paroxetine.
Concomitant use of paroxetine with other drugs metabolized by cytochrome CYP2D6 has not been formally studied but may require lower doses than usually prescribed for either paroxetine or the other drug.
Therefore, coadministration of paroxetine with other drugs that are metabolized by this isozyme, including certain drugs effective in the treatment of major depressive disorder (e.g., nortriptyline, amitriptyline, imipramine, desipramine, and fluoxetine), phenothiazines, risperidone, and Type 1C antiarrhythmics (e.g., propafenone, flecainide, and encainide), or that inhibit this enzyme (e.g., quinidine), should be approached with caution.
However, due to the risk of serious ventricular arrhythmias and sudden death potentially associated with elevated plasma levels of thioridazine, paroxetine and thioridazine should not be coadministered (see CONTRAINDICATIONS and WARNINGS).
At steady state, when the CYP2D6 pathway is essentially saturated, paroxetine clearance is governed by alternative P450 isozymes that, unlike CYP2D6, show no evidence of saturation (see PRECAUTIONSTricyclic Antidepressants).
Drugs Metabolized by Cytochrome CYP3A4
An in vivo interaction study involving the coadministration under steady-state conditions of paroxetine and terfenadine, a substrate for cytochrome CYP3A4, revealed no effect of paroxetine on terfenadine pharmacokinetics. In addition, in vitro studies have shown ketoconazole, a potent inhibitor of CYP3A4 activity, to be at least 100 times more potent than paroxetine as an inhibitor of the metabolism of several substrates for this enzyme, including terfenadine, astemizole, cisapride, triazolam, and cyclosporine. Based on the assumption that the relationship between paroxetine's in vitro Ki and its lack of effect on terfenadine's in vivo clearance predicts its effect on other CYP3A4 substrates, paroxetine's extent of inhibition of CYP3A4 activity is not likely to be of clinical significance.
Tricyclic Antidepressants (TCAs)
Caution is indicated in the coadministration of tricyclic antidepressants (TCAs) with paroxetine, because paroxetine may inhibit TCA metabolism. Plasma TCA concentrations may need to be monitored, and the dose of TCA may need to be reduced, if a TCA is coadministered with paroxetine (see PRECAUTIONSDrugs Metabolized by Cytochrome CYP2D6).
Drugs Highly Bound to Plasma Protein
Because paroxetine is highly bound to plasma protein, administration of paroxetine to a patient taking another drug that is highly protein bound may cause increased free concentrations of the other drug, potentially resulting in adverse events. Conversely, adverse effects could result from displacement of paroxetine by other highly bound drugs.
Drugs That Interfere With Hemostasis (NSAIDs, Aspirin, Warfarin, etc.)
Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies of the case-control and cohort design that have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding have also shown that concurrent use of an NSAID or aspirin potentiated the risk of bleeding. Thus, patients should be cautioned about the use of such drugs concurrently with paroxetine.
Alcohol
Although paroxetine does not increase the impairment of mental and motor skills caused by alcohol, patients should be advised to avoid alcohol while taking paroxetine.
Lithium
A multiple-dose study has shown that there is no pharmacokinetic interaction between paroxetine and lithium carbonate. However, due to the potential for serotonin syndrome, caution is advised when paroxetine is coadministered with lithium.
Digoxin
The steady-state pharmacokinetics of paroxetine was not altered when administered with digoxin at steady state. Mean digoxin AUC at steady state decreased by 15% in the presence of paroxetine. Since there is little clinical experience, the concurrent administration of paroxetine and digoxin should be undertaken with caution.
Diazepam
Under steady-state conditions, diazepam does not appear to affect paroxetine kinetics. The effects of paroxetine on diazepam were not evaluated.
Procyclidine
Daily oral dosing of paroxetine (30 mg once daily) increased steady-state AUC0-24, Cmax, and Cmin values of procyclidine (5 mg oral once daily) by 35%, 37% and 67%, respectively, compared to procyclidine alone at steady state. If anticholinergic effects are seen, the dose of procyclidine should be reduced.
Beta-Blockers
In a study where propranolol (80 mg twice daily) was dosed orally for 18 days, the established steady-state plasma concentrations of propranolol were unaltered during coadministration with paroxetine (30 mg once daily) for the final 10 days. The effects of propranolol on paroxetine have not been evaluated (see ADVERSE REACTIONSPostmarketing Reports).
Theophylline
Reports of elevated theophylline levels associated with treatment with paroxetine have been reported. While this interaction has not been formally studied, it is recommended that theophylline levels be monitored when these drugs are concurrently administered.
Fosamprenavir/Ritonavir
Co-administration of fosamprenavir/ritonavir with paroxetine significantly decreased plasma levels of paroxetine. Any dose adjustment should be guided by clinical effect (tolerability and efficacy).
Electroconvulsive Therapy (ECT)
There are no clinical studies of the combined use of ECT and paroxetine.
CARCINOGENESIS & MUTAGENESIS & IMPAIRMENT OF FERTILITY
Carcinogenesis
Two-year carcinogenicity studies were conducted in rodents given paroxetine in the diet at 1, 5, and 25 mg/kg/day (mice) and 1, 5, and 20 mg/kg/day (rats). These doses are up to 2.4 (mouse) and 3.9 (rat) times the maximum recommended human dose (MRHD) for major depressive disorder, social anxiety disorder, and GAD on a mg/m2 basis. Because the MRHD for major depressive disorder is slightly less than that for OCD (50 mg versus 60 mg), the doses used in these carcinogenicity studies were only 2.0 (mouse) and 3.2 (rat) times the MRHD for OCD. There was a significantly greater number of male rats in the high-dose group with reticulum cell sarcomas (1/100, 0/50, 0/50, and 4/50 for control, low-, middle-, and high-dose groups, respectively) and a significantly increased linear trend across dose groups for the occurrence of lymphoreticular tumors in male rats. Female rats were not affected. Although there was a dose-related increase in the number of tumors in mice, there was no drug-related increase in the number of mice with tumors. The relevance of these findings to humans is unknown.
Mutagenesis
Paroxetine produced no genotoxic effects in a battery of 5 in vitro and 2 in vivo assays that included the following: Bacterial mutation assay, mouse lymphoma mutation assay, unscheduled DNA synthesis assay, and tests for cytogenetic aberrations in vivo in mouse bone marrow and in vitro in human lymphocytes and in a dominant lethal test in rats.
Impairment of Fertility
PREGNANCY
Pregnancy Category D
See WARNINGS-Usage in Pregnancy: Teratogenic and Nonteratogenic Effects.
NURSING MOTHERS
Like many other drugs, paroxetine is secreted in human milk, and caution should be exercised when paroxetine is administered to a nursing woman.
PEDIATRIC USE
Safety and effectiveness in the pediatric population have not been established (see BOX WARNING and WARNINGSClinical Worsening and Suicide Risk). Three placebo-controlled trials in 752 pediatric patients with MDD have been conducted with paroxetine, and the data were not sufficient to support a claim for use in pediatric patients. Anyone considering the use of paroxetine in a child or adolescent must balance the potential risks with the clinical need.
In placebo-controlled clinical trials conducted with pediatric patients, the following adverse events were reported in at least 2% of pediatric patients treated with paroxetine and occurred at a rate at least twice that for pediatric patients receiving placebo: emotional lability (including self-harm, suicidal thoughts, attempted suicide, crying, and mood fluctuations), hostility, decreased appetite, tremor, sweating, hyperkinesia, and agitation.
Events reported upon discontinuation of treatment with paroxetine in the pediatric clinical trials that included a taper phase regimen, which occurred in at least 2% of patients who received paroxetine and which occurred at a rate at least twice that of placebo, were: emotional lability (including suicidal ideation, suicide attempt, mood changes, and tearfulness), nervousness, dizziness, nausea, and abdominal pain (see Discontinuation of Treatment With Paroxetine).
ADVERSE REACTIONS
Associated With Discontinuation of Treatment
Twenty percent (1,199/6,145) of patients treated with paroxetine in worldwide clinical trials in major depressive disorder and 16.1% (84/522), 11.8% (64/542), 9.4% (44/469), and 10.7% (79/735) of patients treated with paroxetine in worldwide trials in social anxiety disorder, OCD, panic disorder, and GAD respectively, discontinued treatment due to an adverse event. The most common events (associated with discontinuation and considered to be drug related (i.e., those events associated with dropout at a rate approximately twice or greater for paroxetine compared to placebo) included the following:
Major Depressive OCDPanicSocial AnxietyGeneralized AnxietyDisorderDisorderDisorderDisorderParoxe-PlaceboParoxe-Plac-Paroxe-Plac-Paroxe-PlaceboParoxe-PlacebotinetineebotineebotinetineCNSSomnolence2.3%0.7%1.9%0.3%3.4%0.3%2.0%0.2%Insomnia1.7%0%1.3%0.3%3.1%0%Agitation1.1%0.5%Tremor1.1%0.3%1.7%0%Anxiety1.1%0%Dizziness1.5%0%1.9%0%1.0%0.2%Gastroin- testinalConstipation1.1%0%Nausea3.2%1.1%1.9%0%3.2%1.2%4.0%0.3%2.0%0.2%Diarrhea1.0%0.3%Dry mouth1.0%0.3%Vomiting1.0%0.3%1.0%0%Flatulence1.0%0.3%OtherAsthenia1.6%0.4%1.9%0.4%2.5%0.6%1.8%0.2%Abnormal1.6%0%2.1%0%4.9%0.6%2.5%0.5%ejaculation 1Sweating1.0%0.3%1.1%0%1.1%0.2%Impotence11.5%0%Libido Decreased1.0%0%Where numbers are not provided the incidence of the adverse events in patients treated with paroxetine was not >1% or was not greater than or equal to 2 times the incidence of placebo.
1. Incidence corrected for gender.
Commonly Observed Adverse Events
Major Depressive Disorder
The most commonly observed adverse events associated with the use of paroxetine (incidence of 5% or greater and incidence for paroxetine at least twice that for placebo, derived from Table 2) were: Asthenia, sweating, nausea, decreased appetite, somnolence, dizziness, insomnia, tremor, nervousness, ejaculatory disturbance, and other male genital disorders.
Obsessive Compulsive Disorder
The most commonly observed adverse events associated with the use of paroxetine (incidence of 5% or greater and incidence for paroxetine at least twice that of placebo, derived from Table 3) were: Nausea, dry mouth, decreased appetite, constipation, dizziness, somnolence, tremor, sweating, impotence, and abnormal ejaculation.
Panic Disorder
The most commonly observed adverse events associated with the use of paroxetine (incidence of 5% or greater and incidence for paroxetine at least twice that for placebo, derived from Table 3) were: Asthenia, sweating, decreased appetite, libido decreased, tremor, abnormal ejaculation, female genital disorders, and impotence.
Social Anxiety Disorder
The most commonly observed adverse events associated with the use of paroxetine (incidence of 5% or greater and incidence for paroxetine at least twice that for placebo, derived from Table 3) were: Sweating, nausea, dry mouth, constipation, decreased appetite, somnolence, tremor, libido decreased, yawn, abnormal ejaculation, female genital disorders, and impotence.
Generalized Anxiety Disorder
The most commonly observed adverse events associated with the use of paroxetine (incidence of 5% or greater and incidence for paroxetine at least twice that for placebo, derived from Table 4) were: Asthenia, infection, constipation, decreased appetite, dry mouth, nausea, libido decreased, somnolence, tremor, sweating, and abnormal ejaculation.
Incidence in Controlled Clinical Trials
The prescriber should be aware that the figures in the tables following cannot be used to predict the incidence of side effects in the course of usual medical practice where patient characteristics and other factors differ from those that prevailed in the clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigations involving different treatments, uses, and investigators. The cited figures, however, do provide the prescribing physician with some basis for estimating the relative contribution of drug and nondrug factors to the side effect incidence rate in the populations studied.
Major Depressive Disorder
Table 2 enumerates adverse events that occurred at an incidence of 1% or more among paroxetine-treated patients who participated in short-term (6-week) placebo-controlled trials in which patients were dosed in a range of 20 mg to 50 mg/day. Reported adverse events were classified using a standard COSTART-based Dictionary terminology.
Table 2. Treatment-Emergent Adverse Experience Incidence in Placebo-Controlled Clinical Trials for Major Depressive Disorder1
Body SystemPreferred TermParoxetine (n = 421)Placebo (n = 421)Body as a WholeHeadache18%17%Asthenia15%6%CardiovascularPalpitation3%1%Vasodilation3%1%DermatologicSweating11%2%Rash2%1%GastrointestinalNausea26%9%Dry Mouth18%12%Constipation14%9%Diarrhea12%8%Decreased Appetite6%2%Flatulence4%2%Oropharynx Disorder22%0%Dyspepsia2%1%MusculoskeletalMyopathy2%1%Myalgia2%1%Myasthenia1%0%Nervous SystemSomnolence23%9%Dizziness13%6%Insomnia13%6%Tremor8%2%Nervousness5%3%Anxiety5%3%Paresthesia4%2%Libido Decreased3%0%Drugged Feeling2%1%Confusion1%0%RespirationYawn4%0%Special SensesBlurred Vision4%1%Taste Perversion2%0%Urogenital SystemEjaculatory Disturbance3,413%0%Other Male Genital Disorders3,510%0%Urinary Frequency3%1%Urination Disorder63%0%Female Genital Disorders3,72%0%1. Events reported by at least 1% of patients treated with paroxetine are included, except the following events which had an incidence on placeboparoxetine: Abdominal pain, agitation, back pain, chest pain, CNS stimulation, fever, increased appetite, myoclonus, pharyngitis, postural hypotension, respiratory disorder (includes mostlycold symptomsorURI), trauma, and vomiting.
2. Includes mostlylump in throatandtightness in throat.
3. Percentage corrected for gender.
4. Mostlyejaculatory delay.
5. Includesanorgasmia,erectile difficulties,delayed ejaculation/orgasm,andsexual dysfunction,andimpotence.
6. Includes mostlydifficulty with micturitionandurinary hesitancy.
7. Includes mostlyanorgasmiaanddifficulty reaching climax/orgasm.
Obsessive Compulsive Disorder, Panic Disorder, and Social Anxiety Disorder
Table 3 enumerates adverse events that occurred at a frequency of 2% or more among OCD patients on paroxetine who participated in placebo-controlled trials of 12-weeks duration in which patients were dosed in a range of 20 mg to 60 mg/day or among patients with panic disorder on paroxetine who participated in placebo-controlled trials of 10- to 12-weeks duration in which patients were dosed in a range of 10 mg to 60 mg/day or among patients with social anxiety disorder on paroxetine who participated in placebo-controlled trials of 12-weeks duration in which patients were dosed in a range of 20 mg to 50 mg/day.
Table 3. Treatment-Emergent Adverse Experience Incidence in Placebo-Controlled Clinical Trials for Obsessive Compulsive Disorder, Panic Disorder, and Social Anxiety Disorder1
Obsessive CompulsiveBodyPreferredDisorderPanic DisorderSocial Anxiety DisorderSystemTermParoxetinePlacebo(n Paroxetine (n Placebo(n Paroxetine (n Placebo(n=542)=265)=469)=324)=425)(n=339)Body as aAsthenia22%14%14%5%22%14%WholeAbdominal Pain4%3%Chest Pain3%2%Back Pain3%2%Chills2%1%2%1%Trauma3%1%Cardiovas-Vasodilation4%1%cularPalpitation2%0%Derma-Sweating9%3%14%6%9%2%tologicRash3%2%Gastro-Nausea23%10%23%17%25%7%intestinalDry Mouth18%9%18%11%9%3%Constipation16%6%8%5%5%2%Diarrhea10%10%12%7%9%6%Decreased9%3%7%3%8%2%AppetiteDyspepsia4%2%Flatulence4%2%Increased4%3%2%1%AppetiteVomiting2%1%Musculo-Myalgia4%3%skeletalNervousSystemInsomnia24%13%18%10%21%16%Somnolence24%7%19%11%22%5%Dizziness12%6%14%10%11%7%Tremor11%1%9%1%9%1%Nervousness9%8%8%7%Libido Decreased 7%4%9%1%12%1%Agitation5%4%3%1%Anxiety5%4%5%4%Abnormal Dreams 4%1%--Concentration3%2%4%1%ImpairedDepersonalization 3%0%--Myoclonus3%0%3%2%2%1%Amnesia2%1%RespiratorySystemRhinits----3%0%----Pharyngitis4%2%Yawn5%1%SpecialSensesAbnormal Vision4%2%----4%1%Taste Perversion2%0%UrogenitalSystemAbnormal23%1%21%1%28%1%Ejaculation2Dysmenorrhea5%4%Female Genital3%0%9%1%9%1%Disorder2Impotence28%1%5%0%5%1%Urinary3%1%2%0%FrequencyUrination3%0%ImpairedUrinary Tract2%1%2%1%Infection1. Events reported by at least 2% of OCD, panic disorder, and social anxiety disorder in patients treated with paroxetine are included, except the following events which had an incidence on placebo[OCD]: Abdominal pain, agitation, anxiety, back pain, cough increased, depression, headache, hyperkinesia, infection, paresthesia, pharyngitis, respiratory disorder, rhinitis, and sinusitis. [panic disorder]: Abnormal dreams, abnormal vision, chest pain, cough increased, depersonalization, depression, dysmenorrhea, dyspepsia, flu syndrome, headache, infection, myalgia, nervousness, palpitation, paresthesia, pharyngitis, rash, respiratory disorder, sinusitis, taste perversion, trauma, urination impaired, and vasodilation. [social anxiety disorder]: Abdominal pain, depression, headache, infection, respiratory disorder, and sinusitis.
2. Percentage corrected for gender.
Generalized Anxiety Disorder
Table 4 enumerates adverse events that occurred at a frequency of 2% or more among GAD patients on paroxetine who participated in placebo-controlled trials of 8-weeks duration in which patients were dosed in a range of 10 mg/day to 50 mg/day.
Table 4. Treatment-Emergent Adverse Experience Incidence in Placebo-Controlled Clinical Trials for Generalized Anxiety Disorder1
Body SystemPreferred TermGeneralized Anxiety DisorderParoxetine (n = 735)Placebo (n = 529)Body as a WholeAsthenia14%6%Headache17%14%Infection6%3%Abdominal PainTraumaCardiovascularVasodilation3%1%DermatologicSweating6%2%GastrointestinalNausea20%5%Dry Mouth11%5%Constipation10%2%Diarrhea9%7%Decreased Appetite5%1%Vomiting3%2%DyspepsiaNervous SystemInsomnia11%8%Somnolence15%5%Dizziness6%5%Tremor5%1%Nervousness4%3%Libido Decreased9%2%Abnormal DreamsRespiratory SystemRespiratory Disorder7%5%Sinusitis4%3%Yawn4%Special SensesAbnormal Vision2%1%Urogenital SystemAbnormal Ejaculation225%2%Female Genital Disorder24%1%Impotence24%3%1. Events reported by at least 2% of GAD in patients treated with paroxetine are included, except the following events which had an incidence on placeboparoxetine [GAD]: Abdominal pain, back pain, trauma, dyspepsia, myalgia, and pharyngitis.
2. Percentage corrected for gender.
Dose Dependency of Adverse Events
A comparison of adverse event rates in a fixed-dose study comparing 10, 20, 30, and 40 mg/day of paroxetine with placebo in the treatment of major depressive disorder revealed a clear dose dependency for some of the more common adverse events associated with use of paroxetine, as shown in the following table:
Table 5. Treatment-Emergent Adverse Experience Incidence in a Dose-Comparison Trial in the Treatment of Major Depressive Disorder*
Body System/Preferred TermPlaceboParoxetinen = 5110 mg n = 10220 mg n = 10430 mg n = 101 40 mg n=102Body as a WholeAsthenia0.0%2.9%10.6%13.9%12.7%DermatologySweating2.0%1.0%6.7%8.9%11.8%GastrointestinalConstipation5.9%4.9%7.7%9.9%12.7%Decreased Appetite2.0%2.0%5.8%4.0%4.9%Diarrhea7.8%9.8%19.2%7.9%14.7%Dry Mouth2.0%10.8%18.3%15.8%20.6%Nausea13.7%14.7%26.9%34.7%36.3%Nervous SystemAnxiety0.0%2.0%5.8%5.9%5.9%Dizziness3.9%6.9%6.7%8.9%12.7%Nervousness0.0%5.9%5.8%4.0%2.9%Paresthesia0.0%2.9%1.0%5.0%5.9%Somnolence7.8%12.7%18.3%20.8%21.6%Tremor0.0%0.0%7.7%7.9%14.7%Special SensesBlurred Vision2.0%2.9%2.9%2.0%7.8%Urogenital SystemAbnormal Ejaculation0.0%5.8%6.5%10.6%13.0%Impotence0.0%1.9%4.3%6.4%1.9%Male Genital Disorders0.0%3.8%8.7%6.4%3.7%* Rule for including adverse events in table: Incidence at least 5% for 1 of paroxetine groups andtwice the placebo incidence for at least 1 paroxetine group.
In a fixed-dose study comparing placebo and 20, 40, and 60 mg of paroxetine in the treatment of OCD, there was no clear relationship between adverse events and the dose of paroxetine to which patients were assigned. No new adverse events were observed in the group treated with 60 mg paroxetine compared to any of the other treatment groups.
In a fixed-dose study comparing placebo and 10, 20, and 40 mg of paroxetine in the treatment of panic disorder, there was no clear relationship between adverse events and the dose of paroxetine to which patients were assigned, except for asthenia, dry mouth, anxiety, libido decreased, tremor, and abnormal ejaculation. In flexible-dose studies, no new adverse events were observed in patients receiving 60 mg of paroxetine compared to any of the other treatment groups.
In a fixed-dose study comparing placebo and 20, 40, and 60 mg of paroxetine in the treatment of social anxiety disorder, for most of the adverse events, there was no clear relationship between adverse events and the dose of paroxetine to which patients were assigned.
In a fixed-dose study comparing placebo and 20 and 40 mg of paroxetine in the treatment of generalized anxiety disorder, for most of the adverse events, there was no clear relationship between adverse events and the dose of paroxetine to which patients were assigned, except for the following adverse events: Asthenia, constipation, and abnormal ejaculation.
Adaptation to Certain Adverse Events
Over a 4- to 6-week period, there was evidence of adaptation to some adverse events with continued therapy (e.g., nausea and dizziness), but less to other effects (e.g., dry mouth, somnolence, and asthenia).
Male and Female Sexual Dysfunction With SSRIs
Although changes in sexual desire, sexual performance, and sexual satisfaction often occur as manifestations of a psychiatric disorder, they may also be a consequence of pharmacologic treatment. In particular, some evidence suggests that selective serotonin reuptake inhibitors (SSRIs) can cause such untoward sexual experiences.
Reliable estimates of the incidence and severity of untoward experiences involving sexual desire, performance, and satisfaction are difficult to obtain, however, in part because patients and physicians may be reluctant to discuss them. Accordingly, estimates of the incidence of untoward sexual experience and performance cited in product labeling, are likely to underestimate their actual incidence.
In placebo-controlled clinical trials involving more than 3,200 patients, the ranges for the reported incidence of sexual side effects in males and females with major depressive disorder, OCD, panic disorder, social anxiety disorder, and GAD are displayed in Table 6.
Table 6. Incidence of Sexual Adverse Events in Controlled Clinical Trials
ParoxetinePlacebon (males)14461042Decreased Libido6-15%0-5%Ejaculatory Disturbance13-28%0-2%Impotence2-9%0-3%n (females)18221340Decreased Libido0-9%0-2%Orgasmic Disturbance2-9%0-1%There are no adequate and well-controlled studies examining sexual dysfunction with paroxetine treatment.
Paroxetine treatment has been associated with several cases of priapism. In those cases with a known outcome, patients recovered without sequelae.
While it is difficult to know the precise risk of sexual dysfunction associated with the use of SSRIs, physicians should routinely inquire about such possible side effects.
Weight and Vital Sign Changes
Significant weight loss may be an undesirable result of treatment with paroxetine for some patients but, on average, patients in controlled trials had minimal (about 1 pound) weight loss versus smaller changes on placebo and active control. No significant changes in vital signs (systolic and diastolic blood pressure, pulse and temperature) were observed in patients treated with paroxetine in controlled clinical trials.
ECG Changes
In an analysis of ECGs obtained in 682 patients treated with paroxetine and 415 patients treated with placebo in controlled clinical trials, no clinically significant changes were seen in the ECGs of either group.
Liver Function Tests
In placebo-controlled clinical trials, patients treated with paroxetine exhibited abnormal values on liver function tests at no greater rate than that seen in placebo-treated patients. In particular, the paroxetine-versus-placebo comparisons for alkaline phosphatase, SGOT, SGPT, and bilirubin revealed no differences in the percentage of patients with marked abnormalities.
Hallucinations
In pooled clinical trials of immediate-release paroxetine hydrochloride, hallucinations were observed in 22 of 9089 patients receiving drug and 4 of 3187 patients receiving placebo.
Other Events Observed During the Premarketing Evaluation of Paroxetine
During its premarketing assessment in major depressive disorder, multiple doses of paroxetine were administered to 6,145 patients in phase 2 and 3 studies. The conditions and duration of exposure to paroxetine varied greatly and included (in overlapping categories) open and double-blind studies, uncontrolled and controlled studies, inpatient and outpatient studies, and fixed-dose, and titration studies. During premarketing clinical trials in OCD, panic disorder, social anxiety disorder, and generalized anxiety disorder, 542, 469, 522, and 735 patients, respectively, received multiple doses of paroxetine. Untoward events associated with this exposure were recorded by clinical investigators using terminology of their own choosing. Consequently, it is not possible to provide a meaningful estimate of the proportion of individuals experiencing adverse events without first grouping similar types of untoward events into a smaller number of standardized event categories.
In the tabulations that follow, reported adverse events were classified using a standard COSTART-based Dictionary terminology. The frequencies presented, therefore, represent the proportion of the 9,089 patients exposed to multiple doses of paroxetine who experienced an event of the type cited on at least 1 occasion while receiving paroxetine. All reported events are included except those already listed in Tables 2 to 4, those reported in terms so general as to be uninformative and those events where a drug cause was remote. It is important to emphasize that although the events reported occurred during treatment with paroxetine, they were not necessarily caused by it.
Body as a Whole
Cardiovascular System
Digestive System
Endocrine System
Rare: Diabetes mellitus, goiter, hyperthyroidism, hypothyroidism, thyroiditis.
Hemic and Lymphatic Systems
Metabolic and Nutritional
Musculoskeletal System
Nervous System
Respiratory System
Skin and Appendages
Special Senses
Urogenital System
Postmarketing Reports
Voluntary reports of adverse events in patients taking paroxetine that have been received since market introduction and not listed above that may have no causal relationship with the drug include acute pancreatitis, elevated liver function tests (the most severe cases were deaths due to liver necrosis, and grossly elevated transaminases associated with severe liver dysfunction), Guillain-Barrsyndrome, toxic epidermal necrolysis, priapism, syndrome of inappropriate ADH secretion, symptoms suggestive of prolactinemia and galactorrhea, neuroleptic malignant syndromepurpura). There has been a case report of an elevated phenytoin level after 4 weeks of paroxetine and phenytoin coadministration. There has been a case report of severe hypotension when paroxetine was added to chronic metoprolol treatment.
DRUG ABUSE AND DEPENDENCE
Controlled Substance Class
Paroxetine is not a controlled substance.
Physical and Psychologic Dependence
Paroxetine has not been systematically studied in animals or humans for its potential for abuse, tolerance or physical dependence. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for history of drug abuse, and such patients should be observed closely for signs of misuse or abuse of paroxetine (e.g., development of tolerance, incrementations of dose, drug-seeking behavior).
OVERDOSAGE
Human Experience
Since the introduction of paroxetine in the United States, 342 spontaneous cases of deliberate or accidental overdosage during paroxetine treatment have been reported worldwide (circa 1999). These include overdoses with paroxetine alone and in combination with other substances. Of these, 48 cases were fatal and of the fatalities, 17 appeared to involve paroxetine alone. Eight fatal cases that documented the amount of paroxetine ingested were generally confounded by the ingestion of other drugs or alcohol or the presence of significant comorbid conditions. Of 145 non-fatal cases with known outcome, most recovered without sequelae. The largest known ingestion involved 2,000 mg of paroxetine (33 times the maximum recommended daily dose) in a patient who recovered.
Commonly reported adverse events associated with paroxetine overdosage include somnolence, coma, nausea, tremor, tachycardia, confusion, vomiting, and dizziness. Other notable signs and symptoms observed with overdoses involving paroxetine (alone or with other substances) include mydriasis, convulsions (including status epilepticus), ventricular dysrhythmias (including torsade de pointes), hypertension, aggressive reactions, syncope, hypotension, stupor, bradycardia, dystonia, rhabdomyolysis, symptoms of hepatic dysfunction (including hepatic failure, hepatic necrosis, jaundice, hepatitis, and hepatic steatosis), serotonin syndrome, manic reactions, myoclonus, acute renal failure, and urinary retention.
Overdosage Management
Treatment should consist of those general measures employed in the management of overdosage with any drugs effective in the treatment of major depressive disorder.
Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. General supportive and symptomatic measures are also recommended. Induction of emesis is not recommended. Gastric lavage with a large-bore orogastric tube with appropriate airway protection, if needed, may be indicated if performed soon after ingestion, or in symptomatic patients.
Activated charcoal should be administered. Due to the large volume of distribution of this drug, forced diuresis, dialysis, hemoperfusion, and exchange transfusion are unlikely to be of benefit. No specific antidotes for paroxetine are known.
A specific caution involves patients who are taking or have recently taken paroxetine who might ingest excessive quantities of a tricyclic antidepressant. In such a case, accumulation of the parent tricyclic and/or an active metabolite may increase the possibility of clinically significant sequelae and extend the time needed for close medical observation (see PRECAUTIONSDrugs Metabolized by Cytochrome CYP2D6).
In managing overdosage, consider the possibility of multiple drug involvement. The physician should consider contacting a poison control center for additional information on the treatment of any overdose. Telephone numbers for certified poison control centers are listed in the Physicians' Desk Reference (PDR).
DOSAGE & ADMINISTRATION
Major Depressive Disorder
Usual Initial Dosage
Paroxetine should be administered as a single daily dose with or without food, usually in the morning. The recommended initial dose is 20 mg/day. Patients were dosed in a range of 20 to 50 mg/day in the clinical trials demonstrating the effectiveness of paroxetine in the treatment of major depressive disorder. As with all drugs effective in the treatment of major depressive disorder, the full effect may be delayed. Some patients not responding to a 20-mg dose may benefit from dose increases, in 10-mg/day increments, up to a maximum of 50 mg/day. Dose changes should occur at intervals of at least 1 week.
Maintenance Therapy
There is no body of evidence available to answer the question of how long the patient treated with paroxetine should remain on it. It is generally agreed that acute episodes of major depressive disorder require several months or longer of sustained pharmacologic therapy. Whether the dose needed to induce remission is identical to the dose needed to maintain and/or sustain euthymia is unknown.
Systematic evaluation of the efficacy of paroxetine has shown that efficacy is maintained for periods of up to 1 year with doses that averaged about 30 mg.
Obsessive Compulsive Disorder
Usual Initial Dosage
Paroxetine should be administered as a single daily dose with or without food, usually in the morning. The recommended dose of paroxetine in the treatment of OCD is 40 mg daily. Patients should be started on 20 mg/day and the dose can be increased in 10-mg/day increments. Dose changes should occur at intervals of at least 1 week. Patients were dosed in a range of 20 to 60 mg/day in the clinical trials demonstrating the effectiveness of paroxetine in the treatment of OCD. The maximum dosage should not exceed 60 mg/day.
Maintenance Therapy
Long-term maintenance of efficacy was demonstrated in a 6-month relapse prevention trial. In this trial, patients with OCD assigned to paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGYClinical Trials). OCD is a chronic condition, and it is reasonable to consider continuation for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Panic Disorder
Usual Initial Dosage
Paroxetine should be administered as a single daily dose with or without food, usually in the morning. The target dose of paroxetine in the treatment of panic disorder is 40 mg/day. Patients should be started on 10 mg/day. Dose changes should occur in 10-mg/day increments and at intervals of at least 1 week. Patients were dosed in a range of 10 to 60 mg/day in the clinical trials demonstrating the effectiveness of paroxetine. The maximum dosage should not exceed 60 mg/day.
Maintenance Therapy
Long-term maintenance of efficacy was demonstrated in a 3-month relapse prevention trial. In this trial, patients with panic disorder assigned to paroxetine demonstrated a lower relapse rate compared to patients on placebo (see CLINICAL PHARMACOLOGYClinical Trials). Panic disorder is a chronic condition, and it is reasonable to consider continuation for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Social Anxiety Disorder
Usual Initial Dosage
Paroxetine should be administered as a single daily dose with or without food, usually in the morning. The recommended and initial dosage is 20 mg/day. In clinical trials the effectiveness of paroxetine was demonstrated in patients dosed in a range of 20 to 60 mg/day. While the safety of paroxetine has been evaluated in patients with social anxiety disorder at doses up to 60 mg/day, available information does not suggest any additional benefit for doses above 20 mg/day (see CLINICAL PHARMACOLOGYClinical Trials).
Maintenance Therapy
There is no body of evidence available to answer the question of how long the patient treated with paroxetine should remain on it. Although the efficacy of paroxetine beyond 12 weeks of dosing has not been demonstrated in controlled clinical trials, social anxiety disorder is recognized as a chronic condition, and it is reasonable to consider continuation of treatment for a responding patient. Dosage adjustments should be made to maintain the patient on the lowest effective dosage, and patients should be periodically reassessed to determine the need for continued treatment.
Generalized Anxiety Disorder
Usual Initial Dosage
Paroxetine should be administered as a single daily dose with or without food, usually in the morning. In clinical trials the effectiveness of paroxetine was demonstrated in patients dosed in a range of 20 to 50 mg/day. The recommended starting dosage and the established effective dosage is 20 mg/day. There is not sufficient evidence to suggest a greater benefit to doses higher than 20 mg/day. Dose changes should occur in 10 mg/day increments and at intervals of at least 1 week.
Maintenance Therapy
Systematic evaluation of continuing paroxetine for periods of up to 24 weeks in patients with Generalized Anxiety Disorder who had responded while taking paroxetine during an 8-week acute treatment phase has demonstrated a benefit of such maintenance (see CLINICAL PHARMACOLOGYClinical Trials). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Special Populations
Treatment of Pregnant Women During the Third Trimester
Neonates exposed to paroxetine and other SSRIs or SNRIs, late in the third trimester have developed complications requiring prolonged hospitalization, respiratory support, and tube feeding (see WARNINGS). When treating pregnant women with paroxetine during the third trimester, the physician should carefully consider the potential risks and benefits of treatment. The physician may consider tapering paroxetine in the third trimester.
Dosage for Elderly or Debilitated Patients, and Patients With Severe Renal or Hepatic Impairment
The recommended initial dose is 10 mg/day for elderly patients, debilitated patients, and/or patients with severe renal or hepatic impairment. Increases may be made if indicated. Dosage should not exceed 40 mg/day.
Switching Patients to or From a Monoamine Oxidase Inhibitor
At least 14 days should elapse between discontinuation of an MAOI and initiation of therapy with paroxetine. Similarly, at least 14 days should be allowed after stopping paroxetine before starting an MAOI.
Discontinuation of Treatment With Paroxetine
Symptoms associated with discontinuation of paroxetine have been reported (see PRECAUTIONS). Patients should be monitored for these symptoms when discontinuing treatment, regardless of the indication for which paroxetine is being prescribed. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate.
HOW SUPPLIED
Paroxetine tablets USP are supplied as white to off-white, oval, film-coated tablets as follows:
10 mg scored tablets imprintedAPOwith a partial bisect on one side and097
20 mg scored tablets imprintedAPOwith a partial bisect score on one side and083
30 mg unscored tablets imprintedAPOon one side and084
40 mg unscored tablets imprintedAPOon one side and101
STORAGE AND HANDLING
Store at 20to 25(68to 77to 30(59to 86[see USP Controlled Room Temperature].
Dispense in a tight, light-resistant container [see USP].
APOTEX INC.
PAROXETINE TABLETS USP
10 mg, 20 mg, 30 mg and 40 mg
Manufactured by: Manufactured for:
Apotex Inc. Apotex Corp.
Toronto, Ontario Weston, Florida
Canada M9L 1T9 33326
Rev. 3
Revised: May 2007
SPL MEDGUIDE
Antidepressant Medicines, Depression and other Serious Mental Illnesses, and
Suicidal Thoughts or Actions
Read the Medication Guide that comes with you or your family member's antidepressant medicine. This Medication Guide is only about the risk of suicidal thoughts and actions with antidepressant medicines. Talk to your, or your family member's, healthcare provider about:
- all risks and benefits of treatment with antidepressant medicines
- all treatment choices for depression or other serious mental illness
- What is the most important information I should know about antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions?
1. Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults when the medicine is first started.
2. Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) bipolar illness (also called manic-depressive illness) or suicidal thoughts or actions.
3. How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is first started or when the dose is changed.
Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
- Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling very agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
- What else do I need to know about antidepressant medicines?
Never stop an antidepressant medicine without first talking to a healthcare provider. Stopping an antidepressant medicine suddenly can cause other symptoms.
Antidepressants are medicines used to treat depression and other illnesses. It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants.
Antidepressant medicines have other side effects. Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member.
Antidepressant medicines can interact with other medicines. Know all of the medicines that you or your family member takes. Keep a list of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider.
Not all antidepressant medicines prescribed for children are FDA approved for use in children. Talk to your child's healthcare provider for more information.
- This Medication Guide has been approved by the U.S. Food and Drug Administration for all antidepressants.
Revised: May 2007
| PAROXETINE
paroxetine tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - REMEDYREPACK INC. (829572556) |