KALETRA- lopinavir and ritonavir capsule, liquid filled
AbbVie Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use KALETRA safely and effectively. See full prescribing information for KALETRA.
KALETRA (lopinavir/ritonavir) capsules, liquid filled for oral use Initial U.S. Approval: 2000 RECENT MAJOR CHANGES
INDICATIONS AND USAGEKALETRA is an HIV-1 protease inhibitor indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection in adults and pediatric patients (14 days and older). (1) DOSAGE AND ADMINISTRATIONCapsules: Must be taken with food. (2) Do not use once daily administration of KALETRA in:
Adult Patients:
Pediatric Patients:
Concomitant Therapy in Adults and Pediatric Patients: Dose adjustments of KALETRA may be needed when co-administering with efavirenz, nevirapine, or nelfinavir. (2.1, 2.2) DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONSThe following have been observed in patients receiving KALETRA:
ADVERSE REACTIONSCommonly reported adverse reactions to KALETRA included diarrhea, nausea, vomiting, hypertriglyceridemia and hypercholesterolemia. (6.1) DRUG INTERACTIONSSee 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 10/2020 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
KALETRA is indicated in combination with other antiretroviral agents for the treatment of HIV-1 infection in adults and pediatric patients 14 days and older.
- Genotypic or phenotypic testing and/or treatment history should guide the use of KALETRA. The number of baseline lopinavir resistance-associated substitutions affects the virologic response to KALETRA [see Microbiology (12.4)].
2 DOSAGE AND ADMINISTRATION
KALETRA capsules must be taken with food.
2.1 Dosage Recommendations in Adults
- KALETRA capsules 400/100 mg (given as three 133/33 mg capsules) twice daily.
- KALETRA capsules 800/200 mg (given as six 133/33 mg capsules) once daily in patients with less than three lopinavir resistance-associated substitutions.
Once daily administration of KALETRA is not recommended for adult patients with three or more of the following lopinavir resistance-associated substitutions: L10F/I/R/V, K20M/N/R, L24I, L33F, M36I, I47V, G48V, I54L/T/V, V82A/C/F/S/T, and I84V [see Microbiology (12.4)].
KALETRA should not be administered once daily in combination with carbamazepine, phenobarbital, or phenytoin [see Drug Interactions (7)].
Concomitant therapy: Efavirenz, Nevirapine, or Nelfinavir
[see Clinical Pharmacology (12.3) and Drug Interactions (7.3)]
KALETRA capsules should not be administered as a once-daily regimen in combination with efavirenz, nevirapine, or nelfinavir.
- A dose increase is recommended for all patients who use KALETRA capsules. The recommended dose of KALETRA capsules is 533/133 mg twice daily (given as four 133/33 mg capsules twice daily taken with food) when used in combination with efavirenz, nevirapine, or nelfinavir.
2.2 Dosage Recommendations in Pediatric Patients
KALETRA capsules should not be administered once daily in pediatric patients less than 18 years of age.
For children less than 12 years of age who weigh greater than 40 kg or for children greater than 12 years of age, the maximum dose of 400/100 mg twice daily (given as three 133/33 mg capsules twice daily taken with food) is recommended.
The use of KALETRA oral solution is recommended for children 14 days to 12 years of age who weigh less than 40 kg and in those children who cannot swallow capsules. Please refer to the KALETRA oral solution full prescribing information for pediatric dosage and administration and other important information for these children.
Concomitant Therapy: Efavirenz, Nevirapine, or Nelfinavir
- A dose increase is recommended for all pediatric patients who use KALETRA capsules. For children weighing more than 45 kg, the recommended dose of KALETRA capsules is 533/133 mg twice daily (given as four 133/33 mg capsules twice daily taken with food) when used in combination with efavirenz, nevirapine, or nelfinavir.
3 DOSAGE FORMS AND STRENGTHS
KALETRA (lopinavir/ritonavir) capsules are orange soft gelatin capsules imprinted with the “a” logo and the code PK. KALETRA is available as 133.3 mg lopinavir/33.3 mg ritonavir capsules.
4 CONTRAINDICATIONS
- KALETRA is contraindicated in patients with previously demonstrated clinically significant hypersensitivity (e.g., toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, urticaria, angioedema) to any of its ingredients, including ritonavir.
- KALETRA is contraindicated with drugs that are highly dependent on CYP3A for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening reactions [see Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
- Alpha 1- Adrenoreceptor Antagonist: alfuzosin
- Antianginal: ranolazine
- Antiarrhythmic: dronedarone
- Anti-gout: colchicine
- Antipsychotics: lurasidone, pimozide
- Ergot Derivatives: dihydroergotamine, ergotamine, methylergonovine
- GI Motility Agent: cisapride
- Hepatitis C direct acting antiviral: elbasvir/grazoprevir
- HMG-CoA Reductase Inhibitors: lovastatin, simvastatin
- Microsomal triglyceride transfer protein (MTTP) Inhibitor: lomitapide
- PDE5 Inhibitor: sildenafil (Revatio®) when used for the treatment of pulmonary arterial hypertension
- Sedative/Hypnotics: triazolam, orally administered midazolam
- KALETRA is contraindicated with drugs that are potent CYP3A inducers where significantly reduced lopinavir plasma concentrations may be associated with the potential for loss of virologic response and possible resistance and cross-resistance [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)].
- Anticancer Agents: apalutamide
- Antimycobacterial: rifampin
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Serious Adverse Reactions Due to Drug Interactions
Initiation of KALETRA, a CYP3A inhibitor, in patients receiving medications metabolized by CYP3A or initiation of medications metabolized by CYP3A in patients already receiving KALETRA, may increase plasma concentrations of medications metabolized by CYP3A. Initiation of medications that inhibit or induce CYP3A may increase or decrease concentrations of KALETRA, respectively. These interactions may lead to:
- Clinically significant adverse reactions, potentially leading to severe, life-threatening, or fatal events from greater exposures of concomitant medications.
- Clinically significant adverse reactions from greater exposures of KALETRA.
- Loss of therapeutic effect of KALETRA and possible development of resistance.
See Table 5 for steps to prevent or manage these possible and known significant drug interactions, including dosing recommendations [see Drug Interactions (7)]. Consider the potential for drug interactions prior to and during KALETRA therapy; review concomitant medications during KALETRA therapy, and monitor for the adverse reactions associated with the concomitant medications [see Contraindications (4) and Drug Interactions (7)].
5.2 Pancreatitis
Pancreatitis has been observed in patients receiving KALETRA therapy, including those who developed marked triglyceride elevations. In some cases, fatalities have been observed. Although a causal relationship to KALETRA has not been established, marked triglyceride elevations are a risk factor for development of pancreatitis [see Warnings and Precautions (5.8)]. Patients with advanced HIV-1 disease may be at increased risk of elevated triglycerides and pancreatitis, and patients with a history of pancreatitis may be at increased risk for recurrence during KALETRA therapy.
Pancreatitis should be considered if clinical symptoms (nausea, vomiting, abdominal pain) or abnormalities in laboratory values (such as increased serum lipase or amylase values) suggestive of pancreatitis occur. Patients who exhibit these signs or symptoms should be evaluated and KALETRA and/or other antiretroviral therapy should be suspended as clinically appropriate.
5.3 Hepatotoxicity
Patients with underlying hepatitis B or C or marked elevations in transaminase prior to treatment may be at increased risk for developing or worsening of transaminase elevations or hepatic decompensation with use of KALETRA.
There have been postmarketing reports of hepatic dysfunction, including some fatalities. These have generally occurred in patients with advanced HIV-1 disease taking multiple concomitant medications in the setting of underlying chronic hepatitis or cirrhosis. A causal relationship with KALETRA therapy has not been established.
Elevated transaminases with or without elevated bilirubin levels have been reported in HIV-1 mono-infected and uninfected patients as early as 7 days after the initiation of KALETRA in conjunction with other antiretroviral agents. In some cases, the hepatic dysfunction was serious; however, a definitive causal relationship with KALETRA therapy has not been established.
Appropriate laboratory testing should be conducted prior to initiating therapy with KALETRA and patients should be monitored closely during treatment. Increased AST/ALT monitoring should be considered in the patients with underlying chronic hepatitis or cirrhosis, especially during the first several months of KALETRA treatment [see Use in Specific Populations (8.6)].
5.4 QT Interval Prolongation
Postmarketing cases of QT interval prolongation and torsade de pointes have been reported although causality of KALETRA could not be established. Avoid use in patients with congenital long QT syndrome, those with hypokalemia, and with other drugs that prolong the QT interval [see Clinical Pharmacology (12.3)].
5.5 PR Interval Prolongation
Lopinavir/ritonavir prolongs the PR interval in some patients. Cases of second or third degree atrioventricular block have been reported. KALETRA should be used with caution in patients with underlying structural heart disease, pre-existing conduction system abnormalities, ischemic heart disease or cardiomyopathies, as these patients may be at increased risk for developing cardiac conduction abnormalities.
The impact on the PR interval of co-administration of KALETRA with other drugs that prolong the PR interval (including calcium channel blockers, beta-adrenergic blockers, digoxin and atazanavir) has not been evaluated. As a result, co-administration of KALETRA with these drugs should be undertaken with caution, particularly with those drugs metabolized by CYP3A. Clinical monitoring is recommended [see Drug Interactions (7), and Clinical Pharmacology (12.3)].
5.6 Diabetes Mellitus/Hyperglycemia
New onset diabetes mellitus, exacerbation of pre-existing diabetes mellitus, and hyperglycemia have been reported during post-marketing surveillance in HIV-1 infected patients receiving protease inhibitor therapy. Some patients required either initiation or dose adjustments of insulin or oral hypoglycemic agents for treatment of these events. In some cases, diabetic ketoacidosis has occurred. In those patients who discontinued protease inhibitor therapy, hyperglycemia persisted in some cases. Because these events have been reported voluntarily during clinical practice, estimates of frequency cannot be made and a causal relationship between protease inhibitor therapy and these events has not been established. Consider monitoring for hyperglycemia, new onset diabetes mellitus or an exacerbation of diabetes mellitus in patients treated with KALETRA.
5.7 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including KALETRA. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia [PCP], or tuberculosis) which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves’ disease, polymyositis, and Guillain-Barré syndrome) have also been reported to occur in the setting of immune reconstitution, however, the time to onset is more variable, and can occur many months after initiation of treatment.
5.8 Lipid Elevations
Treatment with KALETRA has resulted in large increases in the concentration of total cholesterol and triglycerides [see Adverse Reactions (6.1)]. Triglyceride and cholesterol testing should be performed prior to initiating KALETRA therapy and at periodic intervals during therapy. Lipid disorders should be managed as clinically appropriate, taking into account any potential drug-drug interactions with KALETRA and HMG-CoA reductase inhibitors [see Contraindications (4), Drug Interactions (7.3), and Clinical Pharmacology (12.3)].
5.9 Fat Redistribution
Redistribution/accumulation of body fat including central obesity, dorsocervical fat enlargement (buffalo hump), peripheral wasting, facial wasting, breast enlargement, and "cushingoid appearance" have been observed in patients receiving antiretroviral therapy. The mechanism and long-term consequences of these events are currently unknown. A causal relationship has not been established.
5.10 Patients with Hemophilia
Increased bleeding, including spontaneous skin hematomas and hemarthrosis have been reported in patients with hemophilia type A and B treated with protease inhibitors. In some patients additional factor VIII was given. In more than half of the reported cases, treatment with protease inhibitors was continued or reintroduced. A causal relationship between protease inhibitor therapy and these events has not been established.
5.11 Resistance/Cross-resistance
Because the potential for HIV-1 cross-resistance among protease inhibitors has not been fully explored in treatment-naïve patients, it is unknown what effect therapy with KALETRA will have on the activity of subsequently administered protease inhibitors [see Microbiology (12.4)].
6 ADVERSE REACTIONS
The following adverse reactions are discussed in greater detail in other sections of the labeling.
- QT Interval Prolongation, PR Interval Prolongation [see Warnings and Precautions (5.4, 5.5)]
- Drug Interactions [see Contraindications (4), Warnings and Precautions (5.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]
- Pancreatitis [see Warnings and Precautions (5.2)]
- Hepatotoxicity [see Warnings and Precautions (5.3), and Use in Specific Populations (8.6)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The safety of KALETRA has been investigated in about 2,600 patients in Phase II-IV clinical trials, of which about 700 have received a dose of 800/200 mg (6 capsules or 4 tablets) once daily. Along with nucleoside reverse transcriptase inhibitors (NRTIs), in some studies, KALETRA was used in combination with efavirenz or nevirapine.
In clinical studies the incidence of diarrhea in patients treated with either KALETRA capsules or tablets was greater in those patients treated once daily than in those patients treated twice daily. Any grade of diarrhea was reported by at least half of patients taking once daily Kaletra capsules or tablets. At the time of treatment discontinuation, 4.2-6.3% of patients taking once daily Kaletra and 1.8-3.7% of those taking twice daily Kaletra reported ongoing diarrhea.
Commonly reported adverse reactions to KALETRA included diarrhea, nausea, vomiting, hypertriglyceridemia and hypercholesterolemia. Diarrhea, nausea and vomiting may occur at the beginning of the treatment while hypertriglyceridemia and hypercholesterolemia may occur later. The following have been identified as adverse reactions of moderate or severe intensity (Table 1):
| n | % | ||
| BLOOD AND LYMPHATIC SYSTEM DISORDERS | |||
| anemia* | 54 | 2.1 | |
| leukopenia and neutropenia* | 44 | 1.7 | |
| lymphadenopathy* | 35 | 1.3 | |
| CARDIAC DISORDERS | |||
| atherosclerosis such as myocardial infarction* | 10 | 0.4 | |
| atrioventricular block* | 3 | 0.1 | |
| tricuspid valve incompetence* | 3 | 0.1 | |
| EAR AND LABYRINTH DISORDERS | |||
| vertigo* | 7 | 0.3 | |
| tinnitus | 6 | 0.2 | |
| ENDOCRINE DISORDERS | |||
| hypogonadism* | 16 | 0.81 | |
| EYE DISORDERS | |||
| visual impairment* | 8 | 0.3 | |
| GASTROINTESTINAL DISORDERS | |||
| diarrhea* | 510 | 19.5 | |
| nausea | 269 | 10.3 | |
| vomiting* | 177 | 6.8 | |
| abdominal pain (upper and lower)* | 160 | 6.1 | |
| gastroenteritis and colitis* | 66 | 2.5 | |
| dyspepsia | 53 | 2.0 | |
| pancreatitis* | 45 | 1.7 | |
| Gastroesophageal Reflux Disease (GERD)* | 40 | 1.5 | |
| hemorrhoids | 39 | 1.5 | |
| flatulence | 36 | 1.4 | |
| abdominal distension | 34 | 1.3 | |
| constipation* | 26 | 1.0 | |
| stomatitis and oral ulcers* | 24 | 0.9 | |
| duodenitis and gastritis* | 20 | 0.8 | |
| gastrointestinal hemorrhage including rectal hemorrhage* | 13 | 0.5 | |
| dry mouth | 9 | 0.3 | |
| gastrointestinal ulcer* | 6 | 0.2 | |
| fecal incontinence | 5 | 0.2 | |
| GENERAL DISORDERS AND ADMINISTRATION SITE CONDITIONS | |||
| fatigue including asthenia* | 198 | 7.6 | |
| HEPATOBILIARY DISORDERS | |||
| hepatitis including AST, ALT, and GGT increases* | 91 | 3.5 | |
| hepatomegaly | 5 | 0.2 | |
| cholangitis | 3 | 0.1 | |
| hepatic steatosis | 3 | 0.1 | |
| IMMUNE SYSTEM DISORDERS | |||
| hypersensitivity including urticaria and angioedema* | 70 | 2.7 | |
| immune reconstitution syndrome | 3 | 0.1 | |
| INFECTIONS AND INFESTATIONS | |||
| upper respiratory tract infection* | 363 | 13.9 | |
| lower respiratory tract infection* | 202 | 7.7 | |
| skin infections including cellulitis, folliculitis, and furuncle* | 86 | 3.3 | |
| METABOLISM AND NUTRITION DISORDERS | |||
| hypercholesterolemia* | 192 | 7.4 | |
| hypertriglyceridemia* | 161 | 6.2 | |
| weight decreased* | 61 | 2.3 | |
| decreased appetite | 52 | 2.0 | |
| blood glucose disorders including diabetes mellitus* | 30 | 1.1 | |
| weight increased* | 20 | 0.8 | |
| lactic acidosis* | 11 | 0.4 | |
| increased appetite | 5 | 0.2 | |
| MUSCULOSKELETAL AND CONNECTIVE TISSUE DISORDERS | |||
| musculoskeletal pain including arthralgia and back pain* | 166 | 6.4 | |
| myalgia* | 46 | 1.8 | |
| muscle disorders such as weakness and spasms* | 34 | 1.3 | |
| rhabdomyolysis* | 18 | 0.7 | |
| osteonecrosis | 3 | 0.1 | |
| NERVOUS SYSTEM DISORDERS | |||
| headache including migraine* | 165 | 6.3 | |
| insomnia* | 99 | 3.8 | |
| neuropathy and peripheral neuropathy* | 51 | 2.0 | |
| dizziness* | 45 | 1.7 | |
| ageusia* | 19 | 0.7 | |
| convulsion* | 9 | 0.3 | |
| tremor* | 9 | 0.3 | |
| cerebral vascular event* | 6 | 0.2 | |
| PSYCHIATRIC DISORDERS | |||
| anxiety* | 101 | 3.9 | |
| abnormal dreams* | 19 | 0.7 | |
| libido decreased | 19 | 0.7 | |
| RENAL AND URINARY DISORDERS | |||
| renal failure* | 31 | 1.2 | |
| hematuria* | 20 | 0.8 | |
| nephritis* | 3 | 0.1 | |
| REPRODUCTIVE SYSTEM AND BREAST DISORDERS | |||
| erectile dysfunction* | 34 | 1.71 | |
| menstrual disorders - amenorrhea, menorrhagia* | 10 | 1.72 | |
| SKIN AND SUBCUTANEOUS TISSUE DISORDERS | |||
| rash including maculopapular rash* | 99 | 3.8 | |
| lipodystrophy acquired including facial wasting* | 58 | 2.2 | |
| dermatitis/rash including eczema and seborrheic dermatitis* | 50 | 1.9 | |
| night sweats* | 42 | 1.6 | |
| pruritus* | 29 | 1.1 | |
| alopecia | 10 | 0.4 | |
| capillaritis and vasculitis* | 3 | 0.1 | |
| VASCULAR DISORDERS | |||
| hypertension* | 47 | 1.8 | |
| deep vein thrombosis* | 17 | 0.7 | |
| *Represents a medical concept including several similar MedDRA PTs 1. Percentage of male population (N=2,038) 2. Percentage of female population (N=574) |
|||
Laboratory Abnormalities in Adults
The percentages of adult patients treated with combination therapy with Grade 3-4 laboratory abnormalities are presented in Table 2 (treatment-naïve patients) and Table 3 (treatment-experienced patients).
| Variable | Limit1 | |||||||
| Chemistry | High | |||||||
| Glucose | > 250 mg/dL | 2% | 2% | 4% | 3% | 1% | 0% | <1% |
| Uric Acid | > 12 mg/dL | 2% | 2% | 5% | 0% | 3% | <1% | 1% |
| SGOT/ AST2 | > 180 U/L | 2% | 4% | 10% | 5% | 3% | 1% | 2% |
| SGPT/ ALT2 | >215 U/L | 4% | 4% | 11% | 4% | 3% | 1% | 1% |
| GGT | >300 U/L | N/A | N/A | 10% | N/A | N/A | N/A | N/A |
| Total Cholesterol | >300 mg/dL | 9% | 5% | 27% | 3% | 3% | 4% | 3% |
| Triglycerides | >750 mg/dL | 9% | 1% | 29% | 5% | 4% | 3% | 6% |
| Amylase | >2 x ULN | 3% | 2% | 4% | 7% | 5% | N/A | N/A |
| Lipase | >2 x ULN | N/A | N/A | N/A | N/A | N/A | 3% | 5% |
| Chemistry | Low | |||||||
| Calculated Creatinine Clearance | <50 mL/min | N/A | N/A | N/A | N/A | N/A | 2% | 2% |
| Hematology | Low | |||||||
| Neutrophils | <0.75 x 109/L | 1% | 3% | 5% | 5% | 1% | 2% | 1% |
| 1 ULN = upper limit of the normal range; N/A = Not Applicable. 2 Criterion for Study 730 was >5x ULN (AST/ALT). |
||||||||
Adverse Reactions in Pediatric Patients
KALETRA oral solution dosed up to 300/75 mg per m2 has been studied in 100 pediatric patients 6 months to 12 years of age. The adverse reaction profile seen during Study 940 was similar to that for adult patients.
Dysgeusia (22%), vomiting (21%), and diarrhea (12%) were the most common adverse reactions of any severity reported in pediatric patients treated with combination therapy for up to 48 weeks in Study 940. A total of 8 patients experienced adverse reactions of moderate to severe intensity. The adverse reactions meeting these criteria and reported for the 8 subjects include: hypersensitivity (characterized by fever, rash and jaundice), pyrexia, viral infection, constipation, hepatomegaly, pancreatitis, vomiting, alanine aminotransferase increased, dry skin, rash, and dysgeusia. Rash was the only event of those listed that occurred in 2 or more subjects (N = 3).
KALETRA oral solution and soft gelatin capsules dosed at higher than recommended doses including 400/100 mg per m2 (without concomitant NNRTI) and 480/120 mg per m2 (with concomitant NNRTI) have been studied in 26 pediatric patients 7 to 18 years of age in Study 1038. Patients also had saquinavir mesylate added to their regimen at Week 4. Rash (12%), blood cholesterol abnormal (12%) and blood triglycerides abnormal (12%) were the only adverse reactions reported in greater than 10% of subjects. Adverse drug reactions of moderate to severe intensity occurring in 2 or more subjects included rash (N=3), blood triglycerides abnormal (N=3), and electrocardiogram QT prolonged (N=2). Both subjects with QT prolongation had additional predisposing conditions such as electrolyte abnormalities, concomitant medications, or pre-existing cardiac abnormalities.
Laboratory Abnormalities in Pediatric Patients
The percentages of pediatric patients treated with combination therapy including KALETRA with Grade 3-4 laboratory abnormalities are presented in Table 4.
| Variable | Limit1 | |
| Chemistry | High | |
| Sodium | > 149 mEq/L | 3% |
| Total Bilirubin | ≥ 3.0 x ULN | 3% |
| SGOT/AST | > 180 U/L | 8% |
| SGPT/ALT | > 215 U/L | 7% |
| Total Cholesterol | > 300 mg/dL | 3% |
| Amylase | > 2.5 x ULN | 7%2 |
| Chemistry | Low | |
| Sodium | < 130 mEq/L | 3% |
| Hematology | Low | |
| Platelet Count | < 50 x 109/L | 4% |
| Neutrophils | < 0.40 x 109/L | 2% |
| 1 ULN = upper limit of the normal range. 2 Subjects with Grade 3-4 amylase confirmed by elevations in pancreatic amylase. |
||
6.2 Postmarketing Experience
The following adverse reactions have been reported during postmarketing use of KALETRA. Because these reactions are reported voluntarily from a population of unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to KALETRA exposure.
Redistribution/accumulation of body fat has been reported [see Warnings and Precautions (5.9)].
Bradyarrhythmias. First-degree AV block, second-degree AV block, third-degree AV block, QTc interval prolongation, torsades (torsade) de pointes [see Warnings and Precautions (5.4, 5.5)].
Toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome and erythema multiforme.
7 DRUG INTERACTIONS
7.1 Potential for KALETRA to Affect Other Drugs
Lopinavir/ritonavir is an inhibitor of CYP3A and may increase plasma concentrations of agents that are primarily metabolized by CYP3A. Agents that are extensively metabolized by CYP3A and have high first pass metabolism appear to be the most susceptible to large increases in AUC (> 3-fold) when co-administered with KALETRA. Thus, co-administration of KALETRA with drugs highly dependent on CYP3A for clearance and for which elevated plasma concentrations are associated with serious and/or life-threatening events is contraindicated. Co-administration with other CYP3A substrates may require a dose adjustment or additional monitoring as shown in Table 5.
Additionally, KALETRA induces glucuronidation.
Published data suggest that lopinavir is an inhibitor of OATP1B1.
These examples are a guide and not considered a comprehensive list of all possible drugs that may interact with lopinavir/ritonavir. The healthcare provider should consult appropriate references for comprehensive information.
7.2 Potential for Other Drugs to Affect Lopinavir
Lopinavir/ritonavir is a CYP3A substrate; therefore, drugs that induce CYP3A may decrease lopinavir plasma concentrations and reduce KALETRA’s therapeutic effect. Although not observed in the KALETRA/ketoconazole drug interaction study, co-administration of KALETRA and other drugs that inhibit CYP3A may increase lopinavir plasma concentrations.
7.3 Established and Other Potentially Significant Drug Interactions
Table 5 provides a listing of established or potentially clinically significant drug interactions. Alteration in dose or regimen may be recommended based on drug interaction studies or predicted interaction [see Contraindications (4), Warnings and Precautions (5.1), and Clinical Pharmacology (12.3)] for magnitude of interaction.
| Concomitant Drug Class: Drug Name | Effect on Concentration of Lopinavir or Concomitant Drug | Clinical Comment |
| HIV-1 Antiviral Agents | ||
| HIV-1 Protease Inhibitor: fosamprenavir/ritonavir | ↓ amprenavir ↓ lopinavir | An increased rate of adverse reactions has been observed with co-administration of these medications. Appropriate doses of the combinations with respect to safety and efficacy have not been established. |
| HIV-1 Protease Inhibitor: indinavir* | ↑ indinavir | Decrease indinavir dose to 600 mg twice daily, when co-administered with KALETRA 400/100 mg twice daily. KALETRA once daily has not been studied in combination with indinavir. |
| HIV-1 Protease Inhibitor: nelfinavir* | ↑ nelfinavir ↑ M8 metabolite of nelfinavir ↓ lopinavir | Increase KALETRA dose to 533/133 mg and decrease nelfinavir dose to 1000 mg twice daily, when co-administered. KALETRA once-daily in combination with nelfinavir is not recommended [see Dosage and Administration (2.1)]. |
| HIV-1 Protease Inhibitor: ritonavir* | ↑ lopinavir | Appropriate doses of additional ritonavir in combination with KALETRA with respect to safety and efficacy have not been established. |
| HIV-1 Protease Inhibitor: saquinavir | ↑ saquinavir | The saquinavir dose is 1000 mg twice daily (with no additional ritonavir), when co-administered with KALETRA 400/100 mg twice daily. KALETRA once daily has not been studied in combination with saquinavir. |
| HIV-1 Protease Inhibitor: tipranavir* | ↓ lopinavir | Co-administration with tipranavir (500 mg twice daily) and ritonavir (200 mg twice daily) is not recommended. |
| HIV CCR5 – Antagonist: maraviroc* | ↑ maraviroc | When co-administered, patients should receive 150 mg twice daily of maraviroc. For further details see complete prescribing information for maraviroc. |
| Non-nucleoside Reverse Transcriptase Inhibitors: efavirenz*, nevirapine* | ↓ lopinavir | Increase the dose of KALETRA capsules to 533/133 mg when KALETRA capsule is co-administered with efavirenz or nevirapine. KALETRA once daily in combination with efavirenz or nevirapine is not recommended [see Dosage and Administration (2.1)]. |
| Non-nucleoside Reverse Transcriptase Inhibitor: delavirdine | ↑ lopinavir | Appropriate doses of the combination with respect to safety and efficacy have not been established. |
| Nucleoside Reverse Transcriptase Inhibitor: didanosine | It is recommended that didanosine be administered on an empty stomach; therefore, didanosine should be given one hour before or two hours after KALETRA capsules (given with food). | |
| Nucleoside Reverse Transcriptase Inhibitor: tenofovir disoproxil fumarate* | ↑ tenofovir | Patients receiving KALETRA and tenofovir should be monitored for adverse reactions associated with tenofovir. |
| Nucleoside Reverse Transcriptase Inhibitors: abacavir, zidovudine | ↓ abacavir ↓ zidovudine | The clinical significance of this potential interaction is unknown. |
| Other Agents | ||
| Alpha 1- Adrenoreceptor Antagonist: alfuzosin | ↑ alfuzosin | Contraindicated due to potential hypotension [see Contraindications (4)]. |
| Antianginal: ranolazine | ↑ ranolazine | Contraindicated due to potential for serious and/or life-threatening reactions [see Contraindications (4)]. |
| Antiarrhythmics: dronedarone | ↑ dronedarone | Contraindicated due to potential for cardiac arrhythmias [see Contraindications (4)]. |
| Antiarrhythmics: e.g. amiodarone, bepridil, lidocaine (systemic), quinidine | ↑ antiarrhythmics | Caution is warranted and therapeutic concentration monitoring (if available) is recommended for antiarrhythmics when co-administered with KALETRA. |
| Anticancer Agents: abemaciclib, apalutamide, dasatinib, encorafenib, ibrutinib, ivosidenib, neratinib, nilotinib, venetoclax, vinblastine, vincristine | ↑ anticancer agents ↓ lopinavir/ritonavir# | Apalutamide is contraindicated due to potential for loss of virologic response and possible resistance to KALETRA or to the class of protease inhibitors [see Contraindications (4)]. Avoid co-administration of encorafenib or ivosidenib with KALETRA due to potential risk of serious adverse events such as QT interval prolongation. If co-administration of encorafenib with KALETRA cannot be avoided, modify dose as recommended in encorafenib USPI. If co-administration of ivosidenib with KALETRA cannot be avoided, reduce ivosidenib dose to 250 mg once daily. Avoid use of neratinib, venetoclax or ibrutinib with KALETRA. For vincristine and vinblastine, consideration should be given to temporarily withholding the ritonavir-containing antiretroviral regimen in patients who develop significant hematologic or gastrointestinal side effects when KALETRA is administered concurrently with vincristine or vinblastine. If the antiretroviral regimen must be withheld for a prolonged period, consideration should be given to initiating a revised regimen that does not include a CYP3A or P-gp inhibitor. A decrease in the dosage or an adjustment of the dosing interval of nilotinib and dasatinib may be necessary for patients requiring co-administration with strong CYP3A inhibitors such as KALETRA. Please refer to the nilotinib and dasatinib prescribing information for dosing instructions. |
| Anticoagulants: warfarin, rivaroxaban |
↑↓ warfarin ↑ rivaroxaban | Concentrations of warfarin may be affected. Initial frequent monitoring of the INR during KALETRA and warfarin co-administration is recommended. Avoid concomitant use of rivaroxaban and KALETRA. Co-administration of KALETRA and rivaroxaban may lead to increased risk of bleeding. |
| Anticonvulsants: carbamazepine, phenobarbital, phenytoin | ↓ lopinavir ↓ phenytoin | KALETRA may be less effective due to decreased lopinavir plasma concentrations in patients taking these agents concomitantly and should be used with caution. KALETRA once daily in combination with carbamazepine, phenobarbital, or phenytoin is not recommended. In addition, co-administration of phenytoin and KALETRA may cause decreases in steady-state phenytoin concentrations. Phenytoin levels should be monitored when co-administering with KALETRA. |
| Anticonvulsants: lamotrigine, valproate | ↓ lamotrigine ↓ or ↔ valproate | A dose increase of the lamotrigine or valproate may be needed when co-administered with KALETRA and therapeutic concentration monitoring for lamotrigine may be indicated; particularly during dosage adjustments. |
| Antidepressant: bupropion | ↓ bupropion ↓ active metabolite, hydroxybupropion | Patients receiving KALETRA and bupropion concurrently should be monitored for an adequate clinical response to bupropion. |
| Antidepressant: trazodone | ↑ trazodone | Adverse reactions of nausea, dizziness, hypotension and syncope have been observed following co-administration of trazodone and ritonavir. A lower dose of trazodone should be considered. |
| Anti-infective: clarithromycin | ↑ clarithromycin | For patients with renal impairment adjust clarithromycin dose as follows:
No dose adjustment for patients with normal renal function is necessary. |
| Antifungals: ketoconazole*, itraconazole, voriconazole, isavuconazonium sulfate* | ↑ ketoconazole ↑ itraconazole ↓ voriconazole ↑isavuconazonium | High doses of ketoconazole (> 200 mg/day) or itraconazole (> 200 mg/day) are not recommended. The coadministration of voriconazole and KALETRA should be avoided unless an assessment of the benefit/risk to the patient justifies the use of voriconazole. Isavuconazonium and Kaletra should be coadministered with caution. Alternative antifungal therapies should be considered in these patients. |
| Anti-gout: colchicine | ↑ colchicine | Contraindicated due to potential for serious and/or life-threatening reactions in patients with renal and/or hepatic impairment [see Contraindications (4)]. For patients with normal renal or hepatic function: Treatment of gout flares-co-administration of colchicine in patients on KALETRA: 0.6 mg (1 tablet) x 1 dose, followed by 0.3 mg (half tablet) 1 hour later. Dose to be repeated no earlier than 3 days. Prophylaxis of gout flares-co-administration of colchicine in patients on KALETRA: If the original colchicine regimen was 0.6 mg twice a day, the regimen should be adjusted to 0.3 mg once a day. If the original colchicine regimen was 0.6 mg once a day, the regimen should be adjusted to 0.3 mg once every other day. Treatment of familial Mediterranean fever (FMF)-co-administration of colchicine in patients on KALETRA: Maximum daily dose of 0.6 mg (may be given as 0.3 mg twice a day). |
| Antimycobacterial: rifampin | ↓ lopinavir | Contraindicated due to potential loss of virologic response and possible resistance to KALETRA or to the class of protease inhibitors or other co-administered antiretroviral agents [see Contraindications (4)]. |
| Antimycobacterial: bedaquiline | ↑ bedaquiline | Bedaquiline should only be used with KALETRA if the benefit of co-administration outweighs the risk. |
| Antimycobacterial: rifabutin* | ↑ rifabutin and rifabutin metabolite | Dosage reduction of rifabutin by at least 75% of the usual dose of 300 mg per day is recommended (i.e., a maximum dose of 150 mg every other day or three times per week). Increased monitoring for adverse reactions is warranted in patients receiving the combination. Further dosage reduction of rifabutin may be necessary. |
| Antiparasitic: atovaquone | ↓ atovaquone | Clinical significance is unknown; however, increase in atovaquone doses may be needed. |
| Antipsychotics: lurasidone pimozide | ↑ lurasidone ↑ pimozide | Contraindicated due to potential for serious and/or life-threatening reactions [see Contraindications (4)]. Contraindicated due to potential for serious and/or life-threatening reactions such as cardiac arrhythmias [see Contraindications (4)]. |
| Antipsychotics: quetiapine | ↑ quetiapine |
Initiation of KALETRA in patients taking quetiapine:
|
| Contraceptive: ethinyl estradiol* | ↓ ethinyl estradiol | Because contraceptive steroid concentrations may be altered when KALETRA is co-administered with oral contraceptives or with the contraceptive patch, alternative methods of nonhormonal contraception are recommended. |
| Dihydropyridine Calcium Channel Blockers: e.g. felodipine, nifedipine, nicardipine | ↑ dihydropyridine calcium channel blockers | Clinical monitoring of patients is recommended and a dose reduction of the dihydropyridine calcium channel blocker may be considered. |
| Endothelin Receptor Antagonists: bosentan | ↑ bosentan |
Co-administration of bosentan in patients on KALETRA:
|
| Ergot Derivatives: dihydroergotamine, ergotamine, methylergonovine | ↑ ergot derivatives | Contraindicated due to potential for acute ergot toxicity characterized by peripheral vasospasm and ischemia of the extremities and other tissues [see Contraindications (4)]. |
| GI Motility Agent: cisapride | ↑ cisapride | Contraindicated due to potential for cardiac arrhythmias [see Contraindications (4)]. |
| GnRH Receptor Antagonists: elagolix | ↑ elagolix ↓ lopinavir/ritonavir | Concomitant use of elagolix 200 mg twice daily and KALETRA for more than 1 month is not recommended due to potential risk of adverse events such as bone loss and hepatic transaminase elevations. Limit concomitant use of elagolix 150 mg once daily and KALETRA to 6 months. |
| Hepatitis C direct acting antiviral: elbasvir/grazoprevir | ↑ elbasvir/grazoprevir | Contraindicated due to increased risk of alanine transaminase (ALT) elevations [see Contraindications (4)]. |
| Hepatitis C direct acting antiviral: boceprevir* glecaprevir/pibrentasvir simeprevir* sofosbuvir/velpatasvir/voxilaprevir ombitasvir/paritaprevir/ ritonavir and dasabuvir* | ↓ lopinavir ↓ boceprevir ↓ ritonavir ↑ glecaprevir ↑ pibrentasvir ↑ simeprevir ↑ sofosbuvir ↑ velpatasvir ↑ voxilaprevir ↑ ombitasvir ↑ paritaprevir ↑ ritonavir ↔ dasabuvir | It is not recommended to co-administer KALETRA and boceprevir, glecaprevir/pibrentasvir, simeprevir, sofosbuvir/velpatasvir/voxilaprevir, or ombitasvir/paritaprevir/ritonavir and dasabuvir. |
| Herbal Products: St. John's Wort (hypericum perforatum) | ↓ lopinavir | Contraindicated due to potential for loss of virologic response and possible resistance to KALETRA or to the class of protease inhibitors [see Contraindications (4)]. |
| Lipid-modifying agents HMG-CoA Reductase Inhibitors: lovastatin simvastatin atorvastatin rosuvastatin Microsomal triglyceride transfer protein (MTTP) Inhibitor: lomitapide |
↑ lovastatin ↑ simvastatin ↑ atorvastatin ↑ rosuvastatin ↑ lomitapide |
Contraindicated due to potential for myopathy including rhabdomyolysis [see Contraindications (4)]. Use atorvastatin with caution and at the lowest necessary dose. Titrate rosuvastatin dose carefully and use the lowest necessary dose; do not exceed rosuvastatin 10 mg per day. Lomitapide is a sensitive substrate for CYP3A4 metabolism. CYP3A4 inhibitors increase the exposure of lomitapide, with strong inhibitors increasing exposure approximately 27-fold. Concomitant use of moderate or strong CYP3A4 inhibitors with lomitapide is contraindicated due to potential for hepatotoxicity [see Contraindications (4)]. |
| Immunosuppressants: e.g. cyclosporine, tacrolimus, sirolimus | ↑ immunosuppressants | Therapeutic concentration monitoring is recommended for immunosuppressant agents when co-administered with KALETRA. |
| Kinase Inhibitors: fostamatinib (also see anticancer agents above) | ↑ fostamatinib metabolite R406 | Monitor for toxicities of R406 such as hepatotoxicity and neutropenia. Fostamatinib dose reduction may be required. |
| Long-acting Beta- Adrenoceptor Agonist: salmeterol | ↑ salmeterol | Concurrent administration of salmeterol and KALETRA is not recommended. The combination may result in increased risk of cardiovascular adverse events associated with salmeterol, including QT prolongation, palpitations and sinus tachycardia. |
| Narcotic Analgesics: methadone*, fentanyl | ↓ methadone ↑ fentanyl | Dosage of methadone may need to be increased when co-administered with KALETRA. Careful monitoring of therapeutic and adverse effects (including potentially fatal respiratory depression) is recommended when fentanyl is concomitantly administered with KALETRA. |
| PDE5 Inhibitors: avanafil, sildenafil, tadalafil, vardenafil | ↑ avanafil ↑ sildenafil ↑ tadalafil ↑ vardenafil | Sildenafil when used for the treatment of pulmonary arterial hypertension (Revatio®) is contraindicated due to the potential for sildenafil-associated adverse events, including visual abnormalities, hypotension, prolonged erection, and syncope [see Contraindications (4)]. Do not use KALETRA with avanafil because a safe and effective avanafil dosage regimen has not been established. Particular caution should be used when prescribing sildenafil, tadalafil, or vardenafil in patients receiving KALETRA. Co-administration of KALETRA may result in an increase in PDE5 inhibitor associated adverse reactions including hypotension, syncope, visual changes and prolonged erection. Use of PDE5 inhibitors for pulmonary arterial hypertension (PAH): Sildenafil (Revatio®) is contraindicated [see Contraindications (4)]. The following dose adjustments are recommended for use of tadalafil (Adcirca®) with KALETRA: Co-administration of ADCIRCA in patients on KALETRA: In patients receiving KALETRA for at least one week, start ADCIRCA at 20 mg once daily. Increase to 40 mg once daily based upon individual tolerability. Co-administration of KALETRA in patients on ADCIRCA: Avoid use of ADCIRCA during the initiation of KALETRA. Stop ADCIRCA at least 24 hours prior to starting KALETRA. After at least one week following the initiation of KALETRA, resume ADCIRCA at 20 mg once daily. Increase to 40 mg once daily based upon individual tolerability. Use of PDE5 inhibitors for erectile dysfunction: It is recommended not to exceed the following doses:
Use with increased monitoring for adverse events. |
| Sedative/Hypnotics: triazolam, orally administered midazolamc | ↑ triazolam ↑ midazolam | Contraindicated due to potential for prolonged or increased sedation or respiratory depression [see Contraindications (4)]. |
| Sedative/Hypnotics: parenterally administered midazolam | ↑ midazolam | If KALETRA is co-administered with parenteral midazolam, close clinical monitoring for respiratory depression and/or prolonged sedation should be exercised and dosage adjustment should be considered. |
| Systemic/Inhaled/ Nasal/Ophthalmic Corticosteroids: e.g., betamethasone budesonide ciclesonide dexamethasone fluticasone methylprednisolone mometasone prednisone triamcinolone | ↓ lopinavir ↑ glucocorticoids | Coadministration with oral dexamethasone or other systemic corticosteroids that induce CYP3A may result in loss of therapeutic effect and development of resistance to lopinavir. Consider alternative corticosteroids. Coadministration with corticosteroids whose exposures are significantly increased by strong CYP3A inhibitors can increase the risk for Cushing’s syndrome and adrenal suppression. Alternative corticosteroids including beclomethasone and prednisolone (whose PK and/or PD are less affected by strong CYP3A inhibitors relative to other studied steroids) should be considered, particularly for long-term use. |
| * see Clinical Pharmacology (12.3) for magnitude of interaction. # refers to interaction with apalutamide. |
||
7.4 Drugs with No Observed or Predicted Interactions with KALETRA
Drug interaction or clinical studies reveal no clinically significant interaction between KALETRA and desipramine (CYP2D6 probe), etravirine, pitavastatin, pravastatin, stavudine, lamivudine, omeprazole, raltegravir, ranitidine, or rilpivirine.
Based on known metabolic profiles, clinically significant drug interactions are not expected between KALETRA and dapsone, trimethoprim/sulfamethoxazole, azithromycin, erythromycin, or fluconazole.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to KALETRA during pregnancy. Physicians are encouraged to register patients by calling the Antiretroviral Pregnancy Registry at 1-800-258-4263.
Available data from the Antiretroviral Pregnancy Registry show no difference in the risk of overall major birth defects compared to the background rate for major birth defects of 2.7% in the U.S. reference population of the Metropolitan Atlanta Congenital Defects Program (MACDP). No treatment-related malformations were observed when lopinavir in combination with ritonavir was administered to pregnant rats or rabbits; however embryonic and fetal developmental toxicities occurred in rats administered maternally toxic doses.
KALETRA was evaluated in 12 HIV-infected pregnant women in an open-label pharmacokinetic trial [see Clinical Pharmacology (12.3)]. No new trends in the safety profile were identified in pregnant women dosed with KALETRA compared to the safety described in non-pregnant adults, based on the review of these limited data.
Antiretroviral Pregnancy Registry Data: Based on prospective reports from the Antiretroviral Pregnancy Registry (APR) of over 3,000 exposures to lopinavir containing regimens (including over 1,000 exposed in the first trimester), there was no difference between lopinavir and overall birth defects compared with the background birth defect rate of 2.7% in the U.S. reference population of the Metropolitan Atlanta Congenital Defects Program. Based on prospective reports from the APR of over 5,000 exposures to ritonavir containing regimens (including over 2,000 exposures in the first trimester) there was no difference between ritonavir and overall birth defects compared with the U.S. background rate (MACDP). For both lopinavir and ritonavir, sufficient numbers of first trimester exposures have been monitored to detect at least a 1.5 fold increase in risk of overall birth defects and a 2 fold increase in risk of birth defects in the cardiovascular and genitourinary systems.
Embryonic and fetal developmental toxicities (early resorption, decreased fetal viability, decreased fetal body weight, increased incidence of skeletal variations and skeletal ossification delays) occurred in rats at a maternally toxic dosage. Based on AUC measurements, the drug exposures in rats at the toxic doses were approximately 0.7-fold for lopinavir and 1.8-fold for ritonavir for males and females that of the exposures in humans at the recommended therapeutic dose (400/100 mg twice daily). In a peri- and postnatal study in rats, a developmental toxicity (a decrease in survival in pups between birth and postnatal Day 21) occurred.
No embryonic and fetal developmental toxicities were observed in rabbits at a maternally toxic dosage. Based on AUC measurements, the drug exposures in rabbits at the toxic doses were approximately 0.6-fold for lopinavir and 1.0-fold for ritonavir that of the exposures in humans at the recommended therapeutic dose (400/100 mg twice daily).
8.2 Lactation
The Centers for Disease Control and Prevention recommend that HIV-1 infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV-1. Because of the potential for HIV-1 transmission in breastfed infants, advise women not to breastfeed.
8.3 Females and Males of Reproductive Potential
Use of KALETRA may reduce the efficacy of combined hormonal contraceptives. Advise patients using combined hormonal contraceptives to use an effective alternative contraceptive method or an additional barrier method of contraception [see Drug Interactions (7.3)].
8.4 Pediatric Use
The safety, efficacy, and pharmacokinetic profiles of KALETRA in pediatric patients below the age of 14 days have not been established. KALETRA should not be administered once daily in pediatric patients. The KALETRA Oral Solution full prescribing information should be consulted for information for young children who cannot swallow KALETRA Capsules.
An open-label, multi-center, dose-finding trial was performed to evaluate the pharmacokinetic profile, tolerability, safety and efficacy of KALETRA oral solution containing lopinavir 80 mg per mL and ritonavir 20 mg per mL at a dose of 300/75 mg per m2 twice daily plus two NRTIs in HIV-infected infants at least 14 days and less than 6 months of age. Results revealed that infants younger than 6 months of age generally had lower lopinavir AUC12 than older children (6 months to 12 years of age), however, despite the lower lopinavir drug exposure observed, antiviral activity was demonstrated as reflected in the proportion of subjects who achieved HIV-1 RNA less than 400 copies per mL at Week 24 [see Adverse Reactions (6.2), Clinical Pharmacology (12.3), and Clinical Studies (14.4 )].
Safety and efficacy in pediatric patients 6 months of age and older was demonstrated in a clinical trial in 100 patients. The clinical trial was an open-label, multicenter trial evaluating the pharmacokinetic profile, tolerability, safety, and efficacy of KALETRA oral solution containing lopinavir 80 mg per mL and ritonavir 20 mg per mL in 100 antiretroviral naïve and experienced pediatric patients ages 6 months to 12 years. Dose selection for patients 6 months to 12 years of age was based on the following results. The 230/57.5 mg per m2 oral solution twice daily regimen without nevirapine and the 300/75 mg per m2 oral solution twice daily regimen with nevirapine provided lopinavir plasma concentrations similar to those obtained in adult patients receiving the 400/100 mg twice daily regimen (without nevirapine) [see Adverse Reactions (6.2), Clinical Pharmacology (12.3), and Clinical Studies (14.4)].
A prospective multicenter, open-label trial evaluated the pharmacokinetic profile, tolerability, safety and efficacy of high-dose KALETRA with or without concurrent NNRTI therapy (Group 1: 400/100 mg per m2 twice daily plus 2 or more NRTIs; Group 2: 480/120 mg per m2 twice daily plus 1 or more NRTIs plus 1 NNRTI) in 26 children and adolescents at least 2 years to less than 18 years of age who had failed prior therapy. Patients also had saquinavir mesylate added to their regimen. This strategy was intended to assess whether higher than approved doses of KALETRA could overcome protease inhibitor cross-resistance. High doses of KALETRA exhibited a safety profile similar to those observed in previous trials; changes in HIV-1 RNA were less than anticipated; three patients had HIV-1 RNA less than 400 copies per mL at Week 48. CD4+ cell count increases were noted in the eight patients who remained on treatment for 48 weeks [see Adverse Reactions (6.2), and Clinical Pharmacology (12.3)].
A prospective multicenter, randomized, open-label study evaluated the efficacy and safety of twice-daily versus once-daily dosing of KALETRA tablets dosed by weight as part of combination antiretroviral therapy (cART) in virologically suppressed HIV-1 infected children (n=173). Children were eligible when they were aged < 18 years, ≥ 15 kg in weight, receiving cART that included KALETRA, HIV-1 ribonucleic acid (RNA) < 50 copies/mL for at least 24 weeks and able to swallow tablets. At week 24, efficacy (defined as the proportion of subjects with plasma HIV-1 RNA less than 50 copies per mL) was significantly higher in subjects receiving twice daily dosing compared to subjects receiving once daily dosing. The safety profile was similar between the two treatment arms although there was a greater incidence of diarrhea in the once daily treated subjects.
8.5 Geriatric Use
Clinical studies of KALETRA did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, appropriate caution should be exercised in the administration and monitoring of KALETRA in elderly patients reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
10 OVERDOSAGE
Human experience of acute overdosage with KALETRA is limited. Treatment of overdose with KALETRA should consist of general supportive measures including monitoring of vital signs and observation of the clinical status of the patient. There is no specific antidote for overdose with KALETRA. If indicated, elimination of unabsorbed drug should be achieved by emesis or gastric lavage. Administration of activated charcoal may also be used to aid in removal of unabsorbed drug. Since KALETRA is highly protein bound, dialysis is unlikely to be beneficial in significant removal of the drug.
11 DESCRIPTION
KALETRA (lopinavir/ritonavir) is a co-formulation of lopinavir and ritonavir. Lopinavir is an inhibitor of the HIV-1 protease. As co-formulated in KALETRA, ritonavir inhibits the CYP3A-mediated metabolism of lopinavir, thereby providing increased plasma levels of lopinavir.
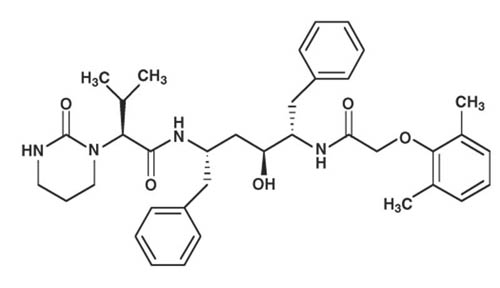
Lopinavir is chemically designated as [1S-[1R*,(R*), 3R*, 4R*]]-N-[4-[[(2,6-dimethylphenoxy)acetyl]amino]-3-hydroxy-5-phenyl-1-(phenylmethyl)pentyl]tetrahydro-alpha-(1-methylethyl)-2-oxo-1(2H)-pyrimidineacetamide. Its molecular formula is C37H48N4O5, and its molecular weight is 628.80. Lopinavir is a white to light tan powder. It is freely soluble in methanol and ethanol, soluble in isopropanol and practically insoluble in water. Lopinavir has the following structural formula:
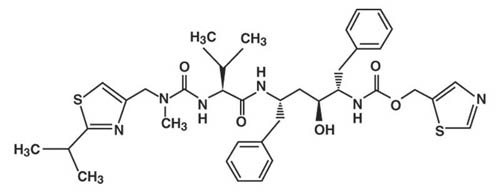
Ritonavir is chemically designated as 10-hydroxy-2-methyl-5-(1-methylethyl)-1- [2-(1-methylethyl)-4-thiazolyl]-3,6-dioxo-8,11-bis(phenylmethyl)-2,4,7,12-tetraazatridecan-13-oic acid, 5-thiazolylmethyl ester, [5S-(5R*,8R*,10R*,11R*)]. Its molecular formula is C37H48N6O5S2, and its molecular weight is 720.95. Ritonavir is a white to light tan powder. It is freely soluble in methanol and ethanol, soluble in isopropanol and practically insoluble in water. Ritonavir has the following structural formula:
KALETRA capsules are available for oral administration in a strength of 133.3 mg lopinavir and 33.3 mg ritonavir with the following inactive ingredients: FD&C Yellow No. 6, gelatin, glycerin, oleic acid, polyoxyl 35 castor oil, propylene glycol, sorbitol special, titanium dioxide, and water.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Lopinavir is an antiviral drug [see Microbiology (12.4)]. As co-formulated in KALETRA, ritonavir inhibits the CYP3A-mediated metabolism of lopinavir, thereby providing increased plasma levels of lopinavir.
12.2 Pharmacodynamics
The effect of KALETRA on QTcF interval was evaluated in a placebo and active (moxifloxacin 400 mg once daily) controlled crossover study in 39 healthy adults. The maximum mean time-matched (95% upper confidence bound) differences in QTcF interval from placebo after baseline-correction were 5.3 (8.1) and 15.2 (18.0) mseconds (msec) for 400/100 mg twice daily and supratherapeutic 800/200 mg twice daily KALETRA, respectively. KALETRA 800/200 mg twice daily resulted in a Day 3 mean Cmax approximately 2-fold higher than the mean Cmax observed with the approved once daily and twice daily KALETRA doses at steady state. The maximum mean (95% upper confidence bound) difference from placebo in the PR interval after baseline-correction were 24.9 (21.5, 28.3) and 31.9 (28.5, 35.3) msec for 400/100 mg twice daily and supratherapeutic 800/200 mg twice daily KALETRA, respectively [see Warnings and Precautions (5.4, 5.5)].
12.3 Pharmacokinetics
The pharmacokinetic properties of lopinavir co-administered with ritonavir have been evaluated in healthy adult volunteers and in HIV-1 infected patients; no substantial differences were observed between the two groups. Lopinavir is essentially completely metabolized by CYP3A. Ritonavir inhibits the metabolism of lopinavir, thereby increasing the plasma levels of lopinavir. Across studies, administration of KALETRA 400/100 mg twice daily yields mean steady-state lopinavir plasma concentrations 15- to 20-fold higher than those of ritonavir in HIV-1 infected patients. The plasma levels of ritonavir are less than 7% of those obtained after the ritonavir dose of 600 mg twice daily. The in vitro antiviral EC50 of lopinavir is approximately 10-fold lower than that of ritonavir. Therefore, the antiviral activity of KALETRA is due to lopinavir.
Figure 1 displays the mean steady-state plasma concentrations of lopinavir and ritonavir after KALETRA 400/100 mg twice daily with food for 3 weeks from a pharmacokinetic study in HIV-1 infected adult subjects (n = 19).
Figure 1. Mean Steady-State Plasma Concentrations with 95% Confidence Intervals (CI) for HIV-1 Infected Adult Subjects (N = 19)
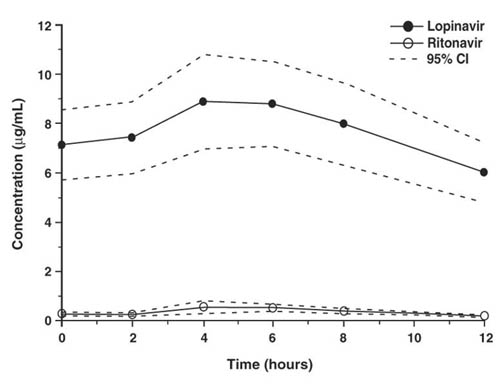
In a pharmacokinetic study in HIV-1 positive subjects (n = 19), multiple dosing with 400/100 mg KALETRA twice daily with food for 3 weeks produced a mean ± SD lopinavir peak plasma concentration (Cmax) of 9.8 ± 3.7 µg per mL, occurring approximately 4 hours after administration. The mean steady-state trough concentration prior to the morning dose was 7.1 ± 2.9 µg per mL and minimum concentration within a dosing interval was 5.5 ± 2.7 µg per mL. Lopinavir AUC over a 12 hour dosing interval averaged 92.6 ± 36.7 µg•h per mL. The absolute bioavailability of lopinavir co-formulated with ritonavir in humans has not been established. Under nonfasting conditions (500 kcal, 25% from fat), lopinavir concentrations were similar following administration of KALETRA co-formulated capsules and oral solution. When administered under fasting conditions, both the mean AUC and Cmax of lopinavir were 22% lower for the KALETRA oral solution relative to the capsule formulation.
Effects of Food on Oral Absorption
Administration of a single 400/100 mg dose of KALETRA capsules with a moderate fat meal (500-682 kcal, 23 to 25% calories from fat) was associated with a mean increase of 48 and 23% in lopinavir AUC and Cmax, respectively, relative to fasting. Relative to fasting, administration of KALETRA capsules with a high fat meal (872 kcal, 56% from fat) increased lopinavir AUC and Cmax by 97 and 43%, respectively. To enhance bioavailability and minimize pharmacokinetic variability KALETRA capsules should be taken with food.
At steady state, lopinavir is approximately 98-99% bound to plasma proteins. Lopinavir binds to both alpha-1-acid glycoprotein (AAG) and albumin; however, it has a higher affinity for AAG. At steady state, lopinavir protein binding remains constant over the range of observed concentrations after 400/100 mg KALETRA twice daily, and is similar between healthy volunteers and HIV-1 positive patients.
In vitro experiments with human hepatic microsomes indicate that lopinavir primarily undergoes oxidative metabolism. Lopinavir is extensively metabolized by the hepatic cytochrome P450 system, almost exclusively by the CYP3A isozyme. Ritonavir is a potent CYP3A inhibitor which inhibits the metabolism of lopinavir, and therefore increases plasma levels of lopinavir. A 14C-lopinavir study in humans showed that 89% of the plasma radioactivity after a single 400/100 mg KALETRA dose was due to parent drug. At least 13 lopinavir oxidative metabolites have been identified in man. Ritonavir has been shown to induce metabolic enzymes, resulting in the induction of its own metabolism. Pre-dose lopinavir concentrations decline with time during multiple dosing, stabilizing after approximately 10 to 16 days.
Following a 400/100 mg 14C-lopinavir/ritonavir dose, approximately 10.4 ± 2.3% and 82.6 ± 2.5% of an administered dose of 14C-lopinavir can be accounted for in urine and feces, respectively, after 8 days. Unchanged lopinavir accounted for approximately 2.2 and 19.8% of the administered dose in urine and feces, respectively. After multiple dosing, less than 3% of the lopinavir dose is excreted unchanged in the urine. The apparent oral clearance (CL/F) of lopinavir is 5.98 ± 5.75 L per hr (mean ± SD, n = 19).
The pharmacokinetics of once daily KALETRA have been evaluated in HIV-1 infected subjects naïve to antiretroviral treatment. KALETRA 800/200 mg was administered in combination with emtricitabine 200 mg and tenofovir DF 300 mg as part of a once daily regimen. Multiple dosing of 800/200 mg KALETRA once daily for 4 weeks with food (n = 24) produced a mean ± SD lopinavir peak plasma concentration (Cmax) of 11.8 ± 3.7 µg per mL, occurring approximately 6 hours after administration. The mean steady-state lopinavir trough concentration prior to the morning dose was 3.2 ± 2.1 µg per mL and minimum concentration within a dosing interval was 1.7 ± 1.6 µg per mL. Lopinavir AUC over a 24 hour dosing interval averaged 154.1 ± 61.4 µg•h per mL.
The pharmacokinetics of once daily KALETRA has also been evaluated in treatment experienced HIV-1 infected subjects. Lopinavir exposure (Cmax, AUC[0-24h], Ctrough) with once daily KALETRA administration in treatment experienced subjects is comparable to the once daily lopinavir exposure in treatment naïve subjects.
No gender related pharmacokinetic differences have been observed in adult patients. No clinically important pharmacokinetic differences due to race have been identified. Lopinavir pharmacokinetics have not been studied in elderly patients.
The pharmacokinetics of KALETRA soft gelatin capsule and oral solution (Group 1: 400/100 mg per m2 twice daily plus 2 NRTIs; Group 2: 480/120 mg per m2 twice daily plus at least 1 NRTI plus 1 NNRTI) have been evaluated in children and adolescents at least 2 years to less than 18 years of age who had failed prior therapy (n=26) in Study 1038. KALETRA doses of 400/100 and 480/120 mg per m2 resulted in high lopinavir exposure, as almost all subjects had lopinavir AUC12 above 100 µg•h per mL. Both groups of subjects also achieved relatively high average minimum lopinavir concentrations.
In an open-label pharmacokinetic study, 12 HIV-infected pregnant women received KALETRA 400 mg/100 mg (two 200/50 mg tablets) twice daily as part of an antiretroviral regimen. Plasma concentrations of lopinavir were measured over 12-hour periods during the second trimester (20-24 weeks gestation), the third trimester (30 weeks gestation) and at 8 weeks post-partum. The C12h values of lopinavir were lower during the second and third trimester by approximately 40% as compared to post-partum, but this decrease is not considered clinically relevant in patients with no documented KALETRA-associated resistance substitutions receiving 400 mg/100 mg twice daily.
Lopinavir pharmacokinetics have not been studied in patients with renal impairment; however, since the renal clearance of lopinavir is negligible, a decrease in total body clearance is not expected in patients with renal impairment.
Lopinavir is principally metabolized and eliminated by the liver. Multiple dosing of KALETRA 400/100 mg twice daily to HIV-1 and HCV co-infected patients with mild to moderate hepatic impairment (n = 12) resulted in a 30% increase in lopinavir AUC and 20% increase in Cmax compared to HIV-1 infected subjects with normal hepatic function (n = 12). Additionally, the plasma protein binding of lopinavir was statistically significantly lower in both mild and moderate hepatic impairment compared to controls (99.09 vs. 99.31%, respectively). Caution should be exercised when administering KALETRA to subjects with hepatic impairment. KALETRA has not been studied in patients with severe hepatic impairment [see Warnings and Precautions (5.3) and Use in Specific Populations (8.6)].
KALETRA is an inhibitor of the P450 isoform CYP3A in vitro. Co-administration of KALETRA and drugs primarily metabolized by CYP3A may result in increased plasma concentrations of the other drug, which could increase or prolong its therapeutic and adverse effects [see Contraindications (4), Warnings and Precautions (5) and Drug Interactions (7)].
KALETRA does not inhibit CYP2D6, CYP2C9, CYP2C19, CYP2E1, CYP2B6 or CYP1A2 at clinically relevant concentrations.
KALETRA has been shown in vivo to induce its own metabolism and to increase the biotransformation of some drugs metabolized by cytochrome P450 enzymes and by glucuronidation.
KALETRA is metabolized by CYP3A. Drugs that induce CYP3A activity would be expected to increase the clearance of lopinavir, resulting in lowered plasma concentrations of lopinavir. Although not noted with concurrent ketoconazole, co-administration of KALETRA and other drugs that inhibit CYP3A may increase lopinavir plasma concentrations.
Drug interaction studies were performed with KALETRA and other drugs likely to be co-administered and some drugs commonly used as probes for pharmacokinetic interactions. The effects of co-administration of KALETRA on the AUC, Cmax and Cmin are summarized in Table 6 (effect of other drugs on lopinavir) and Table 7 (effect of KALETRA on other drugs). The effects of other drugs on ritonavir are not shown since they generally correlate with those observed with lopinavir (if lopinavir concentrations are decreased, ritonavir concentrations are decreased) unless otherwise indicated in the table footnotes. For information regarding clinical recommendations, see Table 5 in Drug Interactions (7).
| Co- administered Drug | Dose of Co- administered Drug (mg) | Dose of KALETRA (mg) | n | Ratio (in combination with co- administered drug/alone) of Lopinavir Pharmacokinetic Parameters (90% CI); No Effect = 1.00 |
||
| Cmax | AUC | Cmin | ||||
| Boceprevir | 800 q8h, 6 d | 400/100 tablet twice daily, 22 d | 13 | 0.70 (0.65, 0.77) | 0.6612
(0.60, 0.72) | 0.57 (0.49, 0.65) |
| Efavirenz1,2 | 600 at bedtime, 9 d | 400/100 capsule twice daily, 9 d | 11, 7* | 0.97 (0.78, 1.22) | 0.81 (0.64, 1.03) | 0.61 (0.38, 0.97) |
| 600 at bedtime, 9 d | 500/125 tablet twice daily, 10 d | 19 | 1.12 (1.02, 1.23) | 1.06 (0.96, 1.17) | 0.90 (0.78, 1.04) |
|
| 600 at bedtime, 9 d | 600/150 tablet twice daily, 10 d | 23 | 1.36 (1.28, 1.44) | 1.36 (1.28, 1.44) | 1.32 (1.21, 1.44) |
|
| Elbasvir/ grazoprevir14 | 50 once daily, 7 d | 400/100 twice daily, 21d | 9 | 1.02 (0.92, 1.13) | 1.02 (0.93, 1.13) | 1.07 (0.97, 1.18) |
| 200 once daily, 7 d | 13 | 0.97 (0.88, 1.08) | 1.03 (0.96, 1.16) | 0.97 (0.81, 1.15) |
||
| Etravirine | 200 twice daily | 400/100 twice day (tablets) | 16 | 0.89 (0.82-0.96) | 0.87 (0.83-0.92) | 0.80 (0.73-0.88) |
| Fosamprenavir3 | 700 twice daily plus ritonavir 100 twice daily, 14 d | 400/100 capsule twice daily, 14 d | 18 | 1.30 (0.85, 1.47) | 1.37 (0.80, 1.55) | 1.52 (0.72, 1.82) |
| Ketoconazole | 200 single dose | 400/100 capsule twice daily, 16 d | 12 | 0.89 (0.80, 0.99) | 0.87 (0.75, 1.00) | 0.75 (0.55, 1.00) |
| Nelfinavir | 1000 twice daily, 10 d | 400/100 capsule twice daily, 21 d | 13 | 0.79 (0.70, 0.89) | 0.73 (0.63, 0.85) | 0.62 (0.49, 0.78) |
| Nevirapine | 200 twice daily, steady- state (> 1 yr)4# | 400/100 capsule twice daily, steady- state | 22, 19* | 0.81 (0.62, 1.05) | 0.73 (0.53, 0.98) | 0.49 (0.28, 0.74) |
| 7 mg/kg or 4 mg/kg once daily, 2 wk; twice daily 1 wk5 | (> 1 yr) 300/75 mg/m2 oral solution twice daily, 3 wk | 12, 15* | 0.86 (0.64, 1.16) | 0.78 (0.56, 1.09) | 0.45 (0.25, 0.81) |
|
| Ombitasvir/ paritaprevir/ ritonavir+ dasabuvir | 25/150/100 + dasabuvir 400, 28 d | 400/100 tablet twice daily, 14 d | 6 | 0.87 (0.76, 0.99) | 0.94 (0.81, 1.10) | 1.15 (0.93, 1.42) |
| Omeprazole | 40 once daily, 5 d | 400/100 tablet twice daily, 10 d | 12 | 1.08 (0.99, 1.17) | 1.07 (0.99, 1.15) | 1.03 (0.90, 1.18) |
| 40 once daily, 5 d | 800/200 tablet once daily, 10 d | 12 | 0.94 (0.88, 1.00) | 0.92 (0.86, 0.99) | 0.71 (0.57, 0.89) |
|
| Pitavastatin6 | 4 once daily, 5 d | 400/100 tablet twice daily, 16 d | 23 | 0.93 (0.88, 0.98) | 0.91 (0.86, 0.97) | N/A |
| Pravastatin | 20 once daily, 4 d | 400/100 capsule twice daily, 14 d | 12 | 0.98 (0.89, 1.08) | 0.95 (0.85, 1.05) | 0.88 (0.77, 1.02) |
| Rifabutin | 150 once daily, 10 d | 400/100 capsule twice daily, 20 d | 14 | 1.08 (0.97, 1.19) | 1.17 (1.04, 1.31) | 1.20 (0.96, 1.65) |
| Ranitidine | 150 single dose | 400/100 tablet twice daily, 10 d | 12 | 0.99 (0.95, 1.03) | 0.97 (0.93, 1.01) | 0.90 (0.85, 0.95) |
| 150 single dose | 800/200 tablet once daily, 10 d | 10 | 0.97 (0.95, 1.00) | 0.95 (0.91, 0.99) | 0.82 (0.74, 0.91) |
|
| Rifampin | 600 once daily, 10 d | 400/100 capsule twice daily, 20 d | 22 | 0.45 (0.40, 0.51) | 0.25 (0.21, 0.29) | 0.01 (0.01, 0.02) |
| 600 once daily, 14 d | 800/200 capsule twice daily, 9 d7 | 10 | 1.02 (0.85, 1.23) | 0.84 (0.64, 1.10) | 0.43 (0.19, 0.96) |
|
| 600 once daily, 14 d | 400/400 capsule twice daily, 9 d8 | 9 | 0.93 (0.81, 1.07) | 0.98 (0.81, 1.17) | 1.03 (0.68, 1.56) |
|
| Rilpivirine | 150 once daily13 | 400/100 twice daily (capsules) | 15 | 0.96 (0.88-1.05) | 0.99 (0.89-1.10) | 0.89 (0.73-1.08) |
| Ritonavir4 | 100 twice daily, 3-4 wk# | 400/100 capsule twice daily, 3-4 wk | 8, 21* | 1.28 (0.94, 1.76) | 1.46 (1.04, 2.06) | 2.16 (1.29, 3.62) |
| Tenofovir disoproxil fumarate9 | 300 once daily, 14 d | 400/100 capsule twice daily, 14 d | 24 | NC† | NC† | NC† |
| Tipranavir/ ritonavir4 | 500/200 twice daily (28 doses) # | 400/100 capsule twice daily (27 doses) | 21, 69 | 0.53 (0.40, 0.69)10 | 0.45 (0.32, 0.63)10 | 0.30 (0.17, 0.51)10 0.48 (0.40, 0.58)11 |
| All interaction studies conducted in healthy, HIV-1 negative subjects unless otherwise indicated. 1 The pharmacokinetics of ritonavir are unaffected by concurrent efavirenz. 2 Reference for comparison is lopinavir/ritonavir 400/100 mg twice daily without efavirenz. 3 Data extracted from the fosamprenavir package insert. 4 Study conducted in HIV-1 positive adult subjects. 5 Study conducted in HIV-1 positive pediatric subjects ranging in age from 6 months to 12 years. 6 Data extracted from the pitavastatin package insert and results presented at the 2011 International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention (Morgan, et al, poster #MOPE170). 7 Titrated to 800/200 twice daily as 533/133 twice daily x 1 d, 667/167 twice daily x 1 d, then 800/200 twice daily x 7 d, compared to 400/100 twice daily x 10 days alone. 8 Titrated to 400/400 twice daily as 400/200 twice daily x 1 d, 400/300 twice daily x 1 d, then 400/400 twice daily x 7 d, compared to 400/100 twice daily x 10 days alone. 9 Data extracted from the tenofovir package insert. 10 Intensive PK analysis. 11 Drug levels obtained at 8-16 hrs post-dose. 12 AUC parameter is AUC(0-last) 13 This interaction study has been performed with a dose higher than the recommended dose for rilpivirine (25 mg once daily) assessing the maximal effect on the co-administered drug. 14 Data extracted from the elbasvir/grazoprevir package insert. * Parallel group design; n for KALETRA + co-administered drug, n for KALETRA alone. N/A = Not available. † NC = No change. # For the nevirapine 200 mg twice daily study, ritonavir, and tipranavir/ritonavir studies, KALETRA was administered with or without food. For all other studies, KALETRA was administered with food. |
||||||
| Co- administered Drug | Dose of Co- administered Drug (mg) | Dose of KALETRA (mg) | n | Ratio (in combination with KALETRA/alone) of Co-administered Drug Pharmacokinetic Parameters (90% CI); No Effect = 1.00 |
||
| Cmax | AUC | Cmin | ||||
| Bedaquiline1 | 400 single dose | 400/100 twice daily, 24 d | N/A | N/A | 1.22 (1.11, 1.34) | N/A |
| Boceprevir | 800 q8h, 6 d | 400/100 tablet twice daily, 22 d | 139 | 0.50 (0.45, 0.55) | 0.55 (0.49, 0.61) | 0.43 (0.36, 0.53) |
| Desipramine2 | 100 single dose | 400/100 capsule twice daily, 10 d | 15 | 0.91 (0.84, 0.97) | 1.05 (0.96, 1.16) | N/A |
| Efavirenz | 600 at bedtime, 9 d | 400/100 capsule twice daily, 9 d | 11, 12* | 0.91 (0.72, 1.15) | 0.84 (0.62, 1.15) | 0.84 (0.58, 1.20) |
| Elbasvir/ grazoprevir11 | 50 once daily, 7 d | 400/100 twice daily, 21d | 10 | 2.87 (2.29, 3.58) | 3.71 (3.05, 4.53) | 4.58 (3.72, 5.64) |
| 200 once daily, 7 d | 13 | 7.31 (5.65, 9.45) | 12.86 (10.25, 16.13) | 21.70 (12.99, 36.25) |
||
| Ethinyl Estradiol | 35 µg once daily, 21 d (Ortho Novum®) | 400/100 capsule twice daily, 14 d | 12 | 0.59 (0.52, 0.66) | 0.58 (0.54, 0.62) | 0.42 (0.36, 0.49) |
| Etravirine | 200 twice daily | 400/100 twice day (tablets) | 16 | 0.70 (0.64-0.78) | 0.65 (0.59-0.71) | 0.55 (0.49-0.62) |
| Fosamprenavir3 | 700 twice daily plus ritonavir 100 twice daily, 14 d | 400/100 capsule twice daily, 14 d | 18 | 0.42 (0.30, 0.58) | 0.37 (0.28, 0.49) | 0.35 (0.27, 0.46) |
| Indinavir4 | 600 twice daily, 10 d combo nonfasting vs. 800 three times daily, 5 d alone fasting | 400/100 capsule twice daily, 15 d | 13 | 0.71 (0.63, 0.81) | 0.91 (0.75, 1.10) | 3.47 (2.60, 4.64) |
| Ketoconazole | 200 single dose | 400/100 capsule twice daily, 16 d | 12 | 1.13 (0.91, 1.40) | 3.04 (2.44, 3.79) | N/A |
| Maraviroc13 | 300 twice daily | 400/100 twice daily | 11 | 1.97 (1.66, 2.34) | 3.95 (3.43, 4.56) | 9.24 (7.98, 10.7) |
| Methadone | 5 single dose | 400/100 capsule twice daily, 10 d | 11 | 0.55 (0.48, 0.64) | 0.47 (0.42, 0.53) | N/A |
| Nelfinavir4 | 1000 twice daily, 10 d combo vs. 1250 twice daily 14 d alone | 400/100 capsule twice daily, 21 d | 13 | 0.93 (0.82, 1.05) | 1.07 (0.95, 1.19) | 1.86 (1.57, 2.22) |
| M8 metabolite | 2.36 (1.91, 2.91) | 3.46 (2.78, 4.31) | 7.49 (5.85, 9.58) |
|||
| Nevirapine | 200 once daily, 14 d; twice daily, 6 d | 400/100 capsule twice daily, 20 d | 5, 6* | 1.05 (0.72, 1.52) | 1.08 (0.72, 1.64) | 1.15 (0.71, 1.86) |
| Norethindrone | 1 once daily, 21 d (Ortho Novum®) | 400/100 capsule twice daily, 14 d | 12 | 0.84 (0.75, 0.94) | 0.83 (0.73, 0.94) | 0.68 (0.54, 0.85) |
| Ombitasvir/ paritaprevir/ ritonavir+ dasabuvir | 25/150/100 + dasabuvir 400, 28 d | 400/100 tablet twice daily, 14 d | 6 | 1.14 (1.01, 1.28) | 1.17 (1.07, 1.28) | 1.24 (1.14, 1.34) |
| 2.04 (1.30, 3.20) | 2.17 (1.63, 2.89) | 2.36 (1.00, 5.55) |
||||
| 1.55 (1.16, 2.09) | 2.05 (1.49, 2.81) | 5.25 (3.33, 8.28) |
||||
| 0.99 (0.75, 1.31) | 0.93 (0.75, 1.15) | 0.68 (0.57, 0.80) |
||||
| Pitavastatin5 | 4 once daily, 5 d | 400/100 tablet twice daily, 16 d | 23 | 0.96 (0.84, 1.10) | 0.80 (0.73, 0.87) | N/A |
| Pravastatin | 20 once daily, 4 d | 400/100 capsule twice daily, 14 d | 12 | 1.26 (0.87, 1.83) | 1.33 (0.91, 1.94) | N/A |
| Rifabutin | 150 once daily, 10 d; combo vs. 300 once daily, 10 d; alone | 400/100 capsule twice daily, 10 d | 12 | 2.12 (1.89, 2.38) | 3.03 (2.79, 3.30) | 4.90 (3.18, 5.76) |
| 25-O-desacetyl rifabutin | 23.6 (13.7, 25.3) | 47.5 (29.3, 51.8) | 94.9 (74.0, 122) |
|||
| Rifabutin + 25-O-desacetyl rifabutin6 | 3.46 (3.07, 3.91) | 5.73 (5.08, 6.46) | 9.53 (7.56, 12.01) |
|||
| Rilpivirine | 150 once daily10 | 400/100 twice daily (capsules) | 15 | 1.29 (1.18-1.40) | 1.52 (1.36-1.70) | 1.74 (1.46-2.08) |
| Rosuvastatin7 | 20 once daily, 7 d | 400/100 tablet twice daily, 7 d | 15 | 4.66 (3.4, 6.4) | 2.08 (1.66, 2.6) | 1.04 (0.9, 1.2) |
| Tenofovir alafenamide12 | 10 once daily | 800/200 tablet once daily | 10 | 2.19 (1.72, 2.79) | 1.47 (1.17, 1.85) | N/A |
| Tenofovir disoproxil fumarate8 | 300 once daily, 14 d | 400/100 capsule twice daily, 14 d | 24 | NC† | 1.32 (1.26, 1.38) | 1.51 (1.32, 1.66) |
| All interaction studies conducted in healthy, HIV-1 negative subjects unless otherwise indicated. 1 Data extracted from the bedaquiline package insert. 2 Desipramine is a probe substrate for assessing effects on CYP2D6-mediated metabolism. 3 Data extracted from the fosamprenavir package insert. 4 Ratio of parameters for indinavir, and nelfinavir are not normalized for dose. 5 Data extracted from the pitavastatin package insert and results presented at the 2011 International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention (Morgan, et al, poster #MOPE170). 6 Effect on the dose-normalized sum of rifabutin parent and 25-O-desacetyl rifabutin active metabolite. 7 Kiser, et al. J Acquir Immune Defic Syndr. 2008 Apr 15;47(5):570-8. 8 Data extracted from the tenofovir package insert. 9 N=12 for Cmin (test arm) 10 This interaction study has been performed with a dose higher than the recommended dose for rilpivirine (25 mg once daily) assessing the maximal effect on the co-administered drug. 11 Data extracted from the elbasvir/grazoprevir package insert 12 Data extracted from the tenofovir alafenamide/emtricitabine package insert 13 Data extracted from the maraviroc package insert * Parallel group design; n for KALETRA + co-administered drug, n for co-administered drug alone. N/A = Not available. † NC = No change. |
||||||
12.4 Microbiology
Lopinavir, an inhibitor of the HIV-1 protease, prevents cleavage of the Gag-Pol polyprotein, resulting in the production of immature, non-infectious viral particles.
The antiviral activity of lopinavir against laboratory HIV strains and clinical HIV-1 isolates was evaluated in acutely infected lymphoblastic cell lines and peripheral blood lymphocytes, respectively. In the absence of human serum, the mean 50% effective concentration (EC50) values of lopinavir against five different HIV-1 subtype B laboratory strains ranged from 10-27 nM (0.006-0.017 µg per mL, 1 µg per mL = 1.6 µM) and ranged from 4-11 nM (0.003-0.007 µg per mL) against several HIV-1 subtype B clinical isolates (n = 6). In the presence of 50% human serum, the mean EC50 values of lopinavir against these five HIV-1 laboratory strains ranged from 65-289 nM (0.04-0.18 µg per mL), representing a 7 to 11-fold attenuation. Combination antiviral drug activity studies with lopinavir in cell cultures demonstrated additive to antagonistic activity with nelfinavir and additive to synergistic activity with amprenavir, atazanavir, indinavir, saquinavir and tipranavir. The EC50 values of lopinavir against three different HIV-2 strains ranged from 12-180 nM (0.008-113 μg per mL).
HIV-1 isolates with reduced susceptibility to lopinavir have been selected in cell culture. The presence of ritonavir does not appear to influence the selection of lopinavir-resistant viruses in cell culture.
The selection of resistance to KALETRA in antiretroviral treatment naïve patients has not yet been characterized. In a study of 653 antiretroviral treatment naïve patients (Study 863), plasma viral isolates from each patient on treatment with plasma HIV-1 RNA greater than 400 copies per mL at Week 24, 32, 40 and/or 48 were analyzed. No evidence of resistance to KALETRA was observed in 37 evaluable KALETRA-treated patients (0%). Evidence of genotypic resistance to nelfinavir, defined as the presence of the D30N and/or L90M substitution in HIV-1 protease, was observed in 25/76 (33%) of evaluable nelfinavir-treated patients. The selection of resistance to KALETRA in antiretroviral treatment naïve pediatric patients (Study 940) appears to be consistent with that seen in adult patients (Study 863).
Resistance to KALETRA has been noted to emerge in patients treated with other protease inhibitors prior to KALETRA therapy. In studies of 227 antiretroviral treatment naïve (100) and protease inhibitor experienced (127) patients, isolates from 4 of 23 patients with quantifiable (greater than 400 copies per mL) viral RNA following treatment with KALETRA for 12 to 100 weeks displayed significantly reduced susceptibility to lopinavir compared to the corresponding baseline viral isolates. Three of these patients had previously received treatment with a single protease inhibitor (indinavir, nelfinavir, or saquinavir) and one patient had received treatment with multiple protease inhibitors (indinavir, ritonavir, and saquinavir). All four of these patients had at least 4 substitutions associated with protease inhibitor resistance immediately prior to KALETRA therapy. Following viral rebound, isolates from these patients all contained additional substitutions, some of which are recognized to be associated with protease inhibitor resistance. However, there are insufficient data at this time to identify patterns of lopinavir resistance-associated substitutions in isolates from patients on KALETRA therapy. The assessment of these patterns is under study.
Cross-resistance - Preclinical Studies
Varying degrees of cross-resistance have been observed among HIV-1 protease inhibitors. Little information is available on the cross-resistance of viruses that developed decreased susceptibility to lopinavir during KALETRA therapy.
The antiviral activity in cell culture of lopinavir against clinical isolates from patients previously treated with a single protease inhibitor was determined. Isolates that displayed greater than 4-fold reduced susceptibility to nelfinavir (n = 13) and saquinavir (n = 4), displayed less than 4-fold reduced susceptibility to lopinavir. Isolates with greater than 4-fold reduced susceptibility to indinavir (n = 16) and ritonavir (n = 3) displayed a mean of 5.7- and 8.3-fold reduced susceptibility to lopinavir, respectively. Isolates from patients previously treated with two or more protease inhibitors showed greater reductions in susceptibility to lopinavir, as described in the following paragraph.
Clinical Studies - Antiviral Activity of KALETRA in Patients with Previous Protease Inhibitor Therapies
The clinical relevance of reduced susceptibility in cell culture to lopinavir has been examined by assessing the virologic response to KALETRA therapy in treatment-experienced patients, with respect to baseline viral genotype in three studies and baseline viral phenotype in one study.
Virologic response to KALETRA has been shown to be affected by the presence of three or more of the following amino acid substitutions in protease at baseline: L10F/I/R/V, K20M/N/R, L24I, L33F, M36I, I47V, G48V, I54L/T/V, V82A/C/F/S/T, and I84V. Table 8 shows the 48-week virologic response (HIV-1 RNA less than 400 copies per mL) according to the number of the above protease inhibitor resistance-associated substitutions at baseline in studies 888 and 765 [see Clinical Studies (14.2) and (14.3)] and study 957 (see below). Once daily administration of KALETRA for adult patients with three or more of the above substitutions is not recommended.
Virologic response to KALETRA therapy with respect to phenotypic susceptibility to lopinavir at baseline was examined in Study 957. In this study 56 NNRTI-naïve patients with HIV-1 RNA greater than 1,000 copies per mL despite previous therapy with at least two protease inhibitors selected from indinavir, nelfinavir, ritonavir, and saquinavir were randomized to receive one of two doses of KALETRA in combination with efavirenz and nucleoside reverse transcriptase inhibitors (NRTIs). The EC50 values of lopinavir against the 56 baseline viral isolates ranged from 0.5- to 96-fold the wild-type EC50 value. Fifty-five percent (31/56) of these baseline isolates displayed greater than 4-fold reduced susceptibility to lopinavir. These 31 isolates had a median reduction in lopinavir susceptibility of 18-fold. Response to therapy by baseline lopinavir susceptibility is shown in Table 9.
| Lopinavir susceptibility2 at baseline | HIV-1 RNA <400 copies/mL (%) | HIV-1 RNA <50 copies/mL (%) |
| < 10 fold | 25/27 (93%) | 22/27 (81%) |
| > 10 and < 40 fold | 11/15 (73%) | 9/15 (60%) |
| ≥ 40 fold | 2/8 (25%) | 2/8 (25%) |
| 1 Lopinavir susceptibility was determined by recombinant phenotypic technology performed by Virologic. 2 Fold change in susceptibility from wild type. |
||
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Lopinavir/ritonavir combination was evaluated for carcinogenic potential by oral gavage administration to mice and rats for up to 104 weeks. Results showed an increase in the incidence of benign hepatocellular adenomas and an increase in the combined incidence of hepatocellular adenomas plus carcinoma in both males and females in mice and males in rats at doses that produced approximately 1.6-2.2 times (mice) and 0.5 times (rats) the human exposure (based on AUC0-24hr measurement) at the recommended dose of 400/100 mg KALETRA twice daily. Administration of lopinavir/ritonavir did not cause a statistically significant increase in the incidence of any other benign or malignant neoplasm in mice or rats.
Carcinogenicity studies in mice and rats have been carried out on ritonavir. In male mice, there was a dose dependent increase in the incidence of both adenomas and combined adenomas and carcinomas in the liver. Based on AUC measurements, the exposure at the high dose was approximately 4-fold for males that of the exposure in humans with the recommended therapeutic dose (400/100 mg KALETRA twice daily). There were no carcinogenic effects seen in females at the dosages tested. The exposure at the high dose was approximately 9-fold for the females that of the exposure in humans. There were no carcinogenic effects in rats. In this study, the exposure at the high dose was approximately 0.7-fold that of the exposure in humans with the 400/100 mg KALETRA twice daily regimen. Based on the exposures achieved in the animal studies, the significance of the observed effects is not known.
Neither lopinavir nor ritonavir was found to be mutagenic or clastogenic in a battery of in vitro and in vivo assays including the Ames bacterial reverse mutation assay using S. typhimurium and E. coli, the mouse lymphoma assay, the mouse micronucleus test and chromosomal aberration assays in human lymphocytes.
Lopinavir in combination with ritonavir at a 2:1 ratio produced no effects on fertility in male and female rats at levels of 10/5, 30/15 or 100/50 mg per kg per day. Based on AUC measurements, the exposures in rats at the high doses were approximately 0.7-fold for lopinavir and 1.8-fold for ritonavir of the exposures in humans at the recommended therapeutic dose (400/100 mg twice daily).
14 CLINICAL STUDIES
14.1 Adult Patients without Prior Antiretroviral Therapy
Study 863: KALETRA Capsules twice daily plus stavudine plus lamivudine compared to nelfinavir three times daily plus stavudine plus lamivudine
Study 863 was a randomized, double-blind, multicenter trial comparing treatment with KALETRA capsules (400/100 mg twice daily) plus stavudine and lamivudine versus nelfinavir (750 mg three times daily) plus stavudine and lamivudine in 653 antiretroviral treatment naïve patients. Patients had a mean age of 38 years (range: 19 to 84), 57% were Caucasian, and 80% were male. Mean baseline CD4+ cell count was 259 cells/mm3 (range: 2 to 949 cells/mm3) and mean baseline plasma HIV-1 RNA was 4.9 log10 copies/mL (range: 2.6 to 6.8 log10 copies/mL).
Treatment response and outcomes of randomized treatment are presented in Table 10.
| Outcome | ||
| Responder1 | 75% | 62% |
| Virologic failure2
Rebound Never suppressed through Week 48 | 9% 7% 2% | 25% 15% 9% |
| Death | 2% | 1% |
| Discontinued due to adverse events | 4% | 4% |
| Discontinued for other reasons3 | 10% | 8% |
| 1 Patients achieved and maintained confirmed HIV-1 RNA < 400 copies/mL through Week 48. 2 Includes confirmed viral rebound and failure to achieve confirmed < 400 copies/mL through Week 48. 3 Includes lost to follow-up, patient's withdrawal, non-compliance, protocol violation and other reasons. Overall discontinuation through Week 48, including patients who discontinued subsequent to virologic failure, was 17% in the KALETRA arm and 24% in the nelfinavir arm. |
||
Through 48 weeks of therapy, there was a statistically significantly higher proportion of patients in the KALETRA arm compared to the nelfinavir arm with HIV-1 RNA < 400 copies/mL (75% vs. 62%, respectively) and HIV-1 RNA less than 50 copies/mL (67% vs. 52%, respectively). Treatment response by baseline HIV-1 RNA level subgroups is presented in Table 11.
| Baseline Viral Load (HIV-1 RNA copies/mL) | KALETRA +d4T+3TC | Nelfinavir +d4T+3TC | ||||
| <400 copies/mL1 | <50 copies/mL2 | n | <400 copies/mL1 | <50 copies/mL2 | n | |
| < 30,000 | 74% | 71% | 82 | 79% | 72% | 87 |
| ≥ 30,000 to < 100,000 | 81% | 73% | 79 | 67% | 54% | 79 |
| ≥ 100,000 to < 250,000 | 75% | 64% | 83 | 60% | 47% | 72 |
| ≥ 250,000 | 72% | 60% | 82 | 44% | 33% | 89 |
| 1 Patients achieved and maintained confirmed HIV-1 RNA < 400 copies/mL through Week 48. 2 Patients achieved HIV-1 RNA < 50 copies/mL at Week 48. |
||||||
Through 48 weeks of therapy, the mean increase from baseline in CD4+ cell count was 207 cells/mm3 for the KALETRA arm and 195 cells/mm3 for the nelfinavir arm.
Study 418: KALETRA Capsules once-daily plus tenofovir DF plus emtricitabine compared to KALETRA Capsules twice-daily plus tenofovir DF plus emtricitabine
Study 418 is an ongoing, randomized, open-label, multicenter trial comparing treatment with KALETRA 800/200 mg once-daily plus tenofovir DF and emtricitabine versus KALETRA 400/100 mg twice-daily plus tenofovir DF and emtricitabine in 190 antiretroviral treatment-naïve patients. Patients had a mean age of 39 years (range: 19 to 75), 54% were Caucasian, and 78% were male. Mean baseline CD4 cell count was 260 cells/mm3 (range: 3 to 1006 cells/mm3) and mean baseline plasma HIV-1 RNA was 4.8 log10 copies/mL (range: 2.6 to 6.4 log10 copies/mL).
Treatment response and outcomes of randomized treatment are presented in Table 12.
| Outcome | ||
| Responder1 | 71% | 65% |
| Virologic failure2
Rebound Never suppressed through Week 48 | 10% 6% 3% | 9% 5% 4% |
| Death | 0% | 1% |
| Discontinued due to an adverse event | 12% | 7% |
| Discontinued for other reasons3 | 7% | 17% |
| 1 Patients achieved and maintained confirmed HIV-1 RNA < 50 copies/mL through Week 48. 2 Includes confirmed viral rebound and failure to achieve confirmed < 50 copies/mL through Week 48. 3 Includes lost to follow-up, patient’s withdrawal, non-compliance, protocol violation and other reasons. |
||
Through 48 weeks of therapy, 71% in the KALETRA once-daily arm and 65% in the KALETRA twice-daily arm achieved and maintained HIV-1 RNA less than 50 copies/mL (95% confidence interval for the difference, -7.6% to 19.5%). Mean CD4 cell count increases at Week 48 were 185 cells/mm3 for the KALETRA once-daily arm and 196 cells/mm3 for the KALETRA twice-daily arm.
Study 730: KALETRA Tablets once daily plus tenofovir DF plus emtricitabine compared to KALETRA Tablets twice daily plus tenofovir DF plus emtricitabine
Study 730 was a randomized, open-label, multicenter trial comparing treatment with KALETRA 800/200 mg once daily plus tenofovir DF and emtricitabine versus KALETRA 400/100 mg twice daily plus tenofovir DF and emtricitabine in 664 antiretroviral treatment-naïve patients. Patients were randomized in a 1:1 ratio to receive either KALETRA 800/200 mg once daily (n = 333) or KALETRA 400/100 mg twice daily (n = 331). Further stratification within each group was 1:1 (tablet vs. capsule). Patients administered the capsule were switched to the tablet formulation at Week 8 and maintained on their randomized dosing schedule. Patients were administered emtricitabine 200 mg once daily and tenofovir DF 300 mg once daily. Mean age of patients enrolled was 39 years (range: 19 to 71); 75% were Caucasian, and 78% were male. Mean baseline CD4+ cell count was 216 cells/mm3 (range: 20 to 775 cells/mm3) and mean baseline plasma HIV-1 RNA was 5.0 log10 copies/mL (range: 1.7 to 7.0 log10 copies/mL).
Treatment response and outcomes of randomized treatment through Week 48 are presented in Table 13.
| Outcome | ||
| Responder1 | 78% | 77% |
| Virologic failure2
Rebound Never suppressed through Week 48 | 10% 5% 5% | 8% 5% 3% |
| Death | 1% | <1% |
| Discontinued due to adverse events | 4% | 3% |
| Discontinued for other reasons3 | 8% | 11% |
| 1 Patients achieved and maintained confirmed HIV-1 RNA < 50 copies/mL through Week 48. 2 Includes confirmed viral rebound and failure to achieve confirmed < 50 copies/mL through Week 48. 3 Includes lost to follow-up, patient's withdrawal, non-compliance, protocol violation and other reasons. |
||
Through 48 weeks of therapy, 78% in the KALETRA once daily arm and 77% in the KALETRA twice daily arm achieved and maintained HIV-1 RNA less than 50 copies/mL (95% confidence interval for the difference, -5.9% to 6.8%). Mean CD4+ cell count increases at Week 48 were 186 cells/mm3 for the KALETRA once daily arm and 198 cells/mm3 for the KALETRA twice daily arm.
14.2 Adult Patients with Prior Antiretroviral Therapy
Study 888: KALETRA Capsules twice daily plus nevirapine plus NRTIs compared to investigator-selected protease inhibitor(s) plus nevirapine plus NRTIs
Study 888 was a randomized, open-label, multicenter trial comparing treatment with KALETRA capsules (400/100 mg twice daily) plus nevirapine and nucleoside reverse transcriptase inhibitors versus investigator-selected protease inhibitor(s) plus nevirapine and nucleoside reverse transcriptase inhibitors in 288 single protease inhibitor-experienced, non-nucleoside reverse transcriptase inhibitor (NNRTI)-naïve patients. Patients had a mean age of 40 years (range: 18 to 74), 68% were Caucasian, and 86% were male. Mean baseline CD4+ cell count was 322 cells/mm3 (range: 10 to 1059 cells/mm3) and mean baseline plasma HIV-1 RNA was 4.1 log10 copies/mL (range: 2.6 to 6.0 log10 copies/mL).
Treatment response and outcomes of randomized treatment through Week 48 are presented in Table 14.
Through 48 weeks of therapy, there was a statistically significantly higher proportion of patients in the KALETRA arm compared to the investigator-selected protease inhibitor(s) arm with HIV-1 RNA less than 400 copies/mL (57% vs. 33%, respectively).
Through 48 weeks of therapy, the mean increase from baseline in CD4+ cell count was 111 cells/mm3 for the KALETRA arm and 112 cells/mm3 for the investigator-selected protease inhibitor(s) arm.
Study 802: KALETRA Tablets 800/200 mg Once Daily Versus 400/100 mg Twice Daily when Co-administered with Nucleoside/Nucleotide Reverse Transcriptase Inhibitors in Antiretroviral-Experienced, HIV-1 Infected Subjects
M06-802 was a randomized open-label study comparing the safety, tolerability, and antiviral activity of once daily and twice daily dosing of KALETRA tablets in 599 subjects with detectable viral loads while receiving their current antiviral therapy. Of the enrolled subjects, 55% on both treatment arms had not been previously treated with a protease inhibitor and 81 – 88% had received prior NNRTIs as part of their anti-HIV treatment regimen. Patients were randomized in a 1:1 ratio to receive either KALETRA 800/200 mg once daily (n = 300) or KALETRA 400/100 mg twice daily (n = 299). Patients were administered at least two nucleoside/nucleotide reverse transcriptase inhibitors selected by the investigator. Mean age of patients enrolled was 41 years (range: 21 to 73); 51% were Caucasian, and 66% were male. Mean baseline CD4+ cell count was 254 cells/mm3 (range: 4 to 952 cells/mm3) and mean baseline plasma HIV-1 RNA was 4.3 log10 copies/mL (range: 1.7 to 6.6 log10 copies/mL).
Treatment response and outcomes of randomized treatment through Week 48 are presented in Table 15.
| Outcome | KALETRA Once Daily + NRTIs (n = 300) | KALETRA Twice Daily + NRTIs (n = 299) |
| Virologic Success (HIV-1 RNA <50 copies/mL) | 57% | 54% |
| Virologic failure1 | 22% | 24% |
| No virologic data in Week 48 window | ||
| Discontinued study due to adverse event or death2 | 5% | 7% |
| Discontinued study for other reasons3 | 13% | 12% |
| Missing data during window but on study | 3% | 3% |
| 1 Includes patients who discontinued prior to Week 48 for lack or loss of efficacy and patients with HIV-1 RNA ≥ 50 copies/mL at Week 48. 2 Includes patients who discontinued due to adverse events or death at any time from Day 1 through Week 48 if this resulted in no virologic data on treatment at Week 48. 3 Includes withdrawal of consent, loss to follow-up, non-compliance, protocol violation and other reasons. |
||
Through 48 weeks of treatment, the mean change from baseline for CD4+ cell count was 135 cells/mm3 for the once daily group and 122 cells/mm3 for the twice daily group.
14.3 Other Studies Supporting Approval in Adult Patients
Study 720: KALETRA twice daily plus stavudine plus lamivudine
Study 765: KALETRA twice daily plus nevirapine plus NRTIs
Study 720 (patients without prior antiretroviral therapy) and study 765 (patients with prior protease inhibitor therapy) were randomized, blinded, multi-center trials evaluating treatment with KALETRA at up to three dose levels (200/100 mg twice daily [720 only], 400/100 mg twice daily, and 400/200 mg twice daily). In Study 720, all patients switched to 400/100 mg twice daily between Weeks 48-72. Patients in study 720 had a mean age of 35 years, 70% were Caucasian, and 96% were male, while patients in study 765 had a mean age of 40 years, 73% were Caucasian, and 90% were male. Mean (range) baseline CD4+ cell counts for patients in study 720 and study 765 were 338 (3-918) and 372 (72-807) cells/mm3, respectively. Mean (range) baseline plasma HIV-1 RNA levels for patients in study 720 and study 765 were 4.9 (3.3 to 6.3) and 4.0 (2.9 to 5.8) log10 copies/mL, respectively.
Through 360 weeks of treatment in study 720, the proportion of patients with HIV-1 RNA less than 400 (less than 50) copies/mL was 61% (59%) [n = 100]. Among patients completing 360 weeks of treatment with CD4+ cell count measurements [n=60], the mean (median) increase in CD4+ cell count was 501 (457) cells/mm3. Thirty-nine patients (39%) discontinued the study, including 13 (13%) discontinuations due to adverse reactions and 1 (1%) death.
Through 144 weeks of treatment in study 765, the proportion of patients with HIV-1 RNA less than 400 (less than 50) copies/mL was 54% (50%) [n = 70], and the corresponding mean increase in CD4+ cell count was 212 cells/mm3. Twenty-seven patients (39%) discontinued the study, including 5 (7%) discontinuations secondary to adverse reactions and 2 (3%) deaths.
14.4 Pediatric Studies
See Clinical Pharmacology (12.3) for pharmacokinetic results.
Study 940 was an open-label, multicenter trial evaluating the pharmacokinetic profile, tolerability, safety and efficacy of KALETRA oral solution containing lopinavir 80 mg/mL and ritonavir 20 mg/mL in 100 antiretroviral naïve (44%) and experienced (56%) pediatric patients. All patients were non-nucleoside reverse transcriptase inhibitor naïve. Patients were randomized to either 230 mg lopinavir/57.5 mg ritonavir/m2 or 300 mg lopinavir/75 mg ritonavir/m2. Naïve patients also received lamivudine and stavudine. Experienced patients received nevirapine plus up to two nucleoside reverse transcriptase inhibitors.
Safety, efficacy and pharmacokinetic profiles of the two dose regimens were assessed after three weeks of therapy in each patient. After analysis of these data, all patients were continued on the 300 mg lopinavir/75 mg ritonavir/m2 dose. Patients had a mean age of 5 years (range 6 months to 12 years) with 14% less than 2 years. Mean baseline CD4+ cell count was 838 cells/mm3 and mean baseline plasma HIV-1 RNA was 4.7 log10 copies/mL.
Through 48 weeks of therapy, the proportion of patients who achieved and sustained an HIV-1 RNA < 400 copies/mL was 80% for antiretroviral naïve patients and 71% for antiretroviral experienced patients. The mean increase from baseline in CD4+ cell count was 404 cells/mm3 for antiretroviral naïve and 284 cells/mm3 for antiretroviral experienced patients treated through 48 weeks. At 48 weeks, two patients (2%) had prematurely discontinued the study. One antiretroviral naïve patient prematurely discontinued secondary to an adverse reaction, while one antiretroviral experienced patient prematurely discontinued secondary to an HIV-1 related event.
Dose selection in pediatric patients was based on the following:
- Among patients 6 months to 12 years of age, the 230/57.5 mg/m2 oral solution twice daily regimen without nevirapine and the 300/75 mg/m2 oral solution twice daily regimen with nevirapine provided lopinavir plasma concentrations similar to those obtained in adult patients receiving the 400/100 mg twice daily regimen (without nevirapine). These doses resulted in treatment benefit (proportion of patients with HIV-1 RNA less than 400 copies/mL) similar to that seen in the adult clinical trials.
- Among patients 12 to 18 years of age receiving 400/100 mg/m2 or 480/120 mg/m2 (with efavirenz) twice daily, plasma concentrations were 60-100% higher than among 6 to 12 year old patients receiving 230/57.5 mg/m2. Mean apparent clearance was similar to that observed in adult patients receiving standard dose and in patients 6 to 12 years of age. Although changes in HIV-1 RNA in patients with prior treatment failure were less than anticipated, the pharmacokinetic data supports use of similar dosing as in patients 6 to 12 years of age, not to exceed the recommended adult dose.
- For all age groups, the body surface area dosing was converted to body weight dosing using the patient’s prescribed lopinavir dose.
16 HOW SUPPLIED/STORAGE AND HANDLING
KALETRA® (lopinavir/ritonavir) capsules are available in the following strengths and package sizes:
| Kaletra Capsules, 133.3 mg lopinavir and 33.3 mg ritonavir |
|
| Presentation | Orange soft gelatin capsules imprinted with the “a” logo and the code PK. |
| Bottle Size and NDC Number | Bottles of 180 capsules (NDC 0074-3959-77) |
| Recommended Storage | Store KALETRA soft gelatin capsules at 36 - 46°F (2 - 8°C) until dispensed. Avoid exposure to excessive heat. For patient use, refrigerated KALETRA capsules remain stable until the expiration date printed on the label. If stored at room temperature up to 77°F (25°C), capsules should be used within 2 months. |
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide)
General Administration Information [see Dosage and Administration (2)]:
- Advise patients to pay special attention to accurate administration of their dose to minimize the risk of accidental overdose or underdose of KALETRA.
- Advise caregivers to inform their healthcare provider if their child’s weight changes in order to make sure that the child’s KALETRA dose is adjusted as needed.
- Inform patients and caregivers that KALETRA capsules should be taken with food to enhance absorption.
- Advise patients to remain under the care of a healthcare provider while using KALETRA and to take KALETRA in combination with other antiretroviral drugs as prescribed.
- Advise patients not to alter the dose or discontinue therapy without consulting with their healthcare provider. If a dose of KALETRA is missed patients should take the dose as soon as possible and then return to their normal schedule. However, if a dose is skipped the patient should not double the next dose.
- Inform patients that it is important to take KALETRA on a regular dosing schedule as directed and to avoid missing doses as that can result in development of resistance.
- Inform patients that Kaletra is not a cure for HIV-1 infection and that they may continue to experience illnesses associated with HIV-1 infection, including opportunistic infections.
Inform patients that KALETRA may interact with some drugs; therefore, patients should be advised to report to their healthcare provider the use of any other prescription, non-prescription medication or herbal products, such as St. John's Wort [see Contraindications (4), Warnings and Precautions (5.1) and Drug Interactions (7)].
Advise patients that pancreatitis has been observed in patients receiving KALETRA and to alert their healthcare provider if they experience symptoms such as nausea, vomiting or abdominal pain [see Warnings and Precautions (5.2)].
Inform patients that skin rash ranging in severity from mild to toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome, erythema multiforme, urticaria, and angioedema have been reported in patients receiving KALETRA or its components lopinavir and/or ritonavir. Advise patients to contact their healthcare provider if they develop a rash while taking KALETRA [see Adverse Reactions (6.1)].
Pre-existing liver disease including Hepatitis B or C can worsen with use of KALETRA. This can be seen as worsening of transaminase elevations or hepatic decompensation. Advise patients that their liver function tests will need to be monitored closely especially during the first several months of KALETRA treatment and that they should notify their healthcare provider if they develop the signs and symptoms of worsening liver disease including loss of appetite, abdominal pain, jaundice, and itchy skin [see Warnings and Precautions (5.3)].
QT and PR Interval Prolongation
Advise patients that KALETRA may produce changes in the electrocardiogram (e.g., PR and/or QT prolongation) and to consult their healthcare provider if they experience symptoms such as dizziness, lightheadedness, abnormal heart rhythm or loss of consciousness [see Warnings and Precautions (5.4, 5.5)].
Diabetes Mellitus/Hyperglycemia
Advise patients that new onset of diabetes or exacerbation of pre-existing diabetes mellitus, and hyperglycemia have been reported during KALETRA use. Advise patients to notify their healthcare provider if they develop the signs and symptoms of diabetes mellitus including frequent urination, excessive thirst, extreme hunger or unusual weight loss and/or an increased blood sugar while on KALETRA as they may require a change in their diabetes treatment or new treatment [see Warnings and Precautions (5.6)].
Immune Reconstitution Syndrome
Advise patients that immune reconstitution syndrome has been reported in HIV-infected patients treated with combination antiretroviral therapy, including KALETRA [see Warnings and Precautions (5.7)].
Advise patients that treatment with KALETRA therapy can result in substantial increases in the concentration of total cholesterol and triglycerides [see Warnings and Precautions (5.8)].
Advise patients that redistribution or accumulation of body fat may occur in patients receiving antiretroviral therapy and that the cause and long term health effects of these conditions are not known at this time [see Warnings and Precautions (5.9)].
Advise patients with hemophilia that they may experience increased bleeding when treated with protease inhibitors such as KALETRA [see Warnings and Precautions (5.10)].
Inform patients that there is an antiretroviral pregnancy registry that monitors fetal outcomes of pregnant women exposed to KALETRA [see Use in Specific Populations (8.1)].
Instruct women with HIV-1 infection not to breastfeed because HIV-1 can be passed to the baby in breast milk [see Use in Specific Populations (8.2)].
AbbVie Inc.
North Chicago, IL 60064 USA
The brands listed are trademarks of their respective owners and are not trademarks of AbbVie Inc. The makers of these brands are not affiliated with and do not endorse AbbVie Inc. or its products.
| MEDICATION GUIDE
KALETRA® (kuh-LEE-tra) (lopinavir and ritonavir) capsules |
|
| What is the most important information I should know about KALETRA?
KALETRA may cause serious side effects, including: |
|
|
|
|
|
|
|
|
|
|
|
| See “What are the possible side effects of KALETRA?” for more information about serious side effects. | |
| What is KALETRA?
KALETRA is a prescription medicine that is used with other antiretroviral medicines to treat Human Immunodeficiency Virus-1 (HIV-1) infection in adults and children 14 days of age and older. HIV is the virus that causes AIDS (Acquired Immune Deficiency Syndrome). It is not known if KALETRA is safe and effective in children under 14 days old. |
|
| Who should not take KALETRA?
Do not take KALETRA if you:
|
|
Before taking KALETRA, tell your healthcare provider about all of your medical conditions, including if you:
Keep a list of your medicines to show your healthcare provider and pharmacist. You can ask your healthcare provider or pharmacist for a list of medicines that interact with KALETRA. Do not start taking a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take KALETRA with other medicines. Your healthcare provider may need to change the dose of other medicines during treatment with KALETRA. |
|
|
|
| What are the possible side effects of KALETRA?
KALETRA can cause serious side effects, including:
|
|
|
|
|
|
|
|
|
|
| These are not all of the possible side effects of KALETRA. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|
How should I store KALETRA?
|
|
| General information about the safe and effective use of KALETRA.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use KALETRA for a condition for which it was not prescribed. Do not give KALETRA to other people, even if they have the same condition you have. It may harm them. You can ask your pharmacist or healthcare provider for information about KALETRA that is written for health professionals. |
|
| What are the ingredients in KALETRA?
Active ingredients: lopinavir and ritonavir Inactive ingredients: FD&C Yellow No. 6, gelatin, glycerin, oleic acid, polyoxyl 35 castor oil, propylene glycol, sorbitol special, titanium dioxide, and water. For more information about KALETRA call 1-800-633-9110 or go to www.KALETRA.com AbbVie Inc., North Chicago, IL 60064 USA The brands listed are trademarks of their respective owners and are not trademarks of AbbVie Inc. The makers of these brands are not affiliated with and do not endorse AbbVie Inc. or its products. © 2020 AbbVie Inc. All rights reserved. |
|
This Medication Guide has been approved by the U.S. Food and Drug Administration.
| KALETRA
lopinavir and ritonavir capsule, liquid filled |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| Labeler - AbbVie Inc. (078458370) |
