VERAMYST- fluticasone furoate spray, metered
GlaxoSmithKline LLC
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use VERAMYST safely and effectively. See full prescribing information for VERAMYST.
VERAMYST (fluticasone furoate) Nasal Spray Initial U.S. Approval: 2007 INDICATIONS AND USAGEVERAMYST Nasal Spray is a corticosteroid indicated for treatment of symptoms of seasonal and perennial allergic rhinitis in adults and children ≥2 years. (1.1) DOSAGE AND ADMINISTRATIONFor intranasal use only. Usual starting dosages:
DOSAGE FORMS AND STRENGTHSCONTRAINDICATIONSHypersensitivity to ingredients. (4) WARNINGS AND PRECAUTIONS
ADVERSE REACTIONSThe most common adverse reactions (>1% incidence) included headache, epistaxis, pharyngolaryngeal pain, nasal ulceration, back pain, pyrexia, and cough. (6.1) To report SUSPECTED ADVERSE REACTIONS, contact GlaxoSmithKline at 1-888-825-5249 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSUSE IN SPECIFIC POPULATIONSHepatic impairment may increase exposure to fluticasone furoate. Use with caution in patients with moderate or severe hepatic impairment. (8.6) See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 7/2016 |
FULL PRESCRIBING INFORMATION
2 DOSAGE AND ADMINISTRATION
Administer VERAMYST Nasal Spray by the intranasal route only. Prime VERAMYST Nasal Spray before using for the first time by shaking the contents well and releasing 6 sprays into the air away from the face. When VERAMYST Nasal Spray has not been used for more than 30 days or if the cap has been left off the bottle for 5 days or longer, prime the pump again until a fine mist appears. Shake VERAMYST Nasal Spray well before each use.
Titrate an individual patient to the minimum effective dosage to reduce the possibility of side effects.
2.1 Adults and Adolescents Aged 12 Years and Older
The recommended starting dosage is 110 mcg once daily administered as 2 sprays (27.5 mcg/spray) in each nostril. When the maximum benefit has been achieved and symptoms have been controlled, reducing the dosage to 55 mcg (1 spray in each nostril) once daily may be effective in maintaining control of allergic rhinitis symptoms.
2.2 Children Aged 2 to 11 Years
The recommended starting dosage in children is 55 mcg once daily administered as 1 spray (27.5 mcg/spray) in each nostril. Children not adequately responding to 55 mcg may use 110 mcg (2 sprays in each nostril) once daily. Once symptoms have been controlled, dosage reduction to 55 mcg once daily is recommended.
3 DOSAGE FORMS AND STRENGTHS
VERAMYST Nasal Spray is a nasal spray suspension. Each spray (50 microliters) delivers 27.5 mcg of fluticasone furoate.
4 CONTRAINDICATIONS
VERAMYST Nasal Spray is contraindicated in patients with hypersensitivity to any of its ingredients [see Warnings and Precautions (5.3)].
5 WARNINGS AND PRECAUTIONS
5.1 Local Nasal Effects
Epistaxis and Nasal Ulceration
In clinical trials of 2 to 52 weeks’ duration, epistaxis and nasal ulcerations were observed more frequently and some epistaxis events were more severe in patients treated with VERAMYST Nasal Spray than those who received placebo [see Adverse Reactions (6.1)].
Candida Infection
Evidence of localized infections of the nose with Candida albicans was seen on nasal exams in 7 of 2,745 patients treated with VERAMYST Nasal Spray during clinical trials and was reported as an adverse event in 3 patients. When such an infection develops, it may require treatment with appropriate local therapy and discontinuation of VERAMYST Nasal Spray. Therefore, patients using VERAMYST Nasal Spray over several months or longer should be examined periodically for evidence of Candida infection or other signs of adverse effects on the nasal mucosa.
Nasal Septal Perforation
Postmarketing cases of nasal septal perforation have been reported in patients following the intranasal application of VERAMYST Nasal Spray [see Adverse Reactions (6.2)].
Impaired Wound Healing
Because of the inhibitory effect of corticosteroids on wound healing, patients who have experienced recent nasal ulcers, nasal surgery, or nasal trauma should not use VERAMYST Nasal Spray until healing has occurred.
5.2 Glaucoma and Cataracts
Nasal and inhaled corticosteroids may result in the development of glaucoma and/or cataracts. Therefore, close monitoring is warranted in patients with a change in vision or with a history of increased intraocular pressure (IOP), glaucoma, and/or cataracts.
Glaucoma and cataract formation was evaluated with intraocular pressure measurements and slit lamp examinations in 1 controlled 12-month trial in 806 adolescent and adult patients aged 12 years and older and in 1 controlled 12-week trial in 558 children aged 2 to 11 years. The patients had perennial allergic rhinitis and were treated with either VERAMYST Nasal Spray (110 mcg once daily in adult and adolescent patients and 55 or 110 mcg once daily in pediatric patients) or placebo. Intraocular pressure remained within the normal range (less than 21 mmHg) in greater than or equal to 98% of the patients in any treatment group in both trials. However, in the 12-month trial in adolescents and adults, 12 patients, all treated with VERAMYST Nasal Spray 110 mcg once daily, had intraocular pressure measurements that increased above normal levels (greater than or equal to 21 mmHg). In the same trial, 7 patients (6 treated with VERAMYST Nasal Spray 110 mcg once daily and 1 patient treated with placebo) had cataracts identified during the trial that were not present at baseline.
5.3 Hypersensitivity Reactions, Including Anaphylaxis
Hypersensitivity reactions, including anaphylaxis, angioedema, rash, and urticaria, may occur after administration of VERAMYST Nasal Spray. Discontinue VERAMYST Nasal Spray if such reactions occur [see Contraindications (4)].
5.4 Immunosuppression
Persons who are using drugs that suppress the immune system are more susceptible to infections than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in susceptible children or adults using corticosteroids. In children or adults who have not had these diseases or have not been properly immunized, particular care should be taken to avoid exposure. How the dose, route, and duration of corticosteroid administration affect the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If a patient is exposed to chickenpox, prophylaxis with varicella zoster immune globulin (VZIG) may be indicated. If a patient is exposed to measles, prophylaxis with pooled intramuscular immunoglobulin (IG) may be indicated. (See the respective package inserts for complete VZIG and IG prescribing information.) If chickenpox or measles develops, treatment with antiviral agents may be considered.
Corticosteroids should be used with caution, if at all, in patients with active or quiescent tuberculous infections of the respiratory tract, untreated local or systemic fungal or bacterial infections, systemic viral or parasitic infections, or ocular herpes simplex because of the potential for worsening of these infections.
5.5 Hypothalamic-Pituitary-Adrenal Axis Effects
Hypercorticism and Adrenal Suppression
When intranasal steroids are used at higher-than-recommended dosages or in susceptible individuals at recommended dosages, systemic corticosteroid effects such as hypercorticism and adrenal suppression may appear. If such changes occur, the dosage of VERAMYST Nasal Spray should be discontinued slowly, consistent with accepted procedures for discontinuing oral corticosteroid therapy.
The replacement of a systemic corticosteroid with a topical corticosteroid can be accompanied by signs of adrenal insufficiency. In addition, some patients may experience symptoms of corticosteroid withdrawal, e.g., joint and/or muscular pain, lassitude, depression. Patients previously treated for prolonged periods with systemic corticosteroids and transferred to topical corticosteroids should be carefully monitored for acute adrenal insufficiency in response to stress. In those patients who have asthma or other clinical conditions requiring long-term systemic corticosteroid treatment, rapid decreases in systemic corticosteroid dosages may cause a severe exacerbation of their symptoms.
5.6 Use of Cytochrome P450 3A4 Inhibitors
Coadministration with ritonavir is not recommended because of the risk of systemic effects secondary to increased exposure to fluticasone furoate. Use caution with the coadministration of VERAMYST Nasal Spray and other potent cytochrome P450 3A4(CYP3A4) inhibitors, such as ketoconazole [see Drug Interactions (7)].
5.7 Effect on Growth
Corticosteroids may cause a reduction in growth velocity when administered to pediatric patients. Monitor the growth routinely of pediatric patients receiving VERAMYST Nasal Spray. To minimize the systemic effects of intranasal corticosteroids, including VERAMYST Nasal Spray, titrate each patient’s dose to the lowest dosage that effectively controls his/her symptoms [see Use in Specific Populations (8.4)].
6 ADVERSE REACTIONS
Systemic and local corticosteroid use may result in the following:
- •
- Epistaxis, ulcerations, Candida albicans infection, impaired wound healing, and nasal septal perforation [see Warnings and Precautions (5.1)]
- •
- Cataracts and glaucoma [see Warnings and Precautions (5.2)]
- •
- Immunosuppression [see Warnings and Precautions (5.4)]
- •
- Hypothalamic-pituitary-adrenal (HPA) axis effects, including growth reduction [see Warnings and Precautions (5.5), Use in Specific Populations (8.4)]
6.1 Clinical Trials Experience
The safety data described below reflect exposure to VERAMYST Nasal Spray in 1,563 patients with seasonal or perennial allergic rhinitis in 9 controlled clinical trials of 2 to 12 weeks’ duration. The data from adults and adolescents are based upon 6 clinical trials in which 768 patients with seasonal or perennial allergic rhinitis (473 females and 295 males aged 12 years and older) were treated with VERAMYST Nasal Spray 110 mcg once daily for 2 to 6 weeks. The racial distribution of adult and adolescent patients receiving VERAMYST Nasal Spray was 82% white, 5% black, and 13% other. The data from pediatric patients are based upon 3 clinical trials in which 795 children with seasonal or perennial rhinitis (352 females and 443 males aged 2 to 11 years) were treated with VERAMYST Nasal Spray 55 or 110 mcg once daily for 2 to 12 weeks. The racial distribution of pediatric patients receiving VERAMYST Nasal Spray was 75% white, 11% black, and 14% other.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adults and Adolescents Aged 12 Years and Older
Overall adverse reactions were reported with approximately the same frequency by patients treated with VERAMYST Nasal Spray and those receiving placebo. Less than 3% of patients in clinical trials discontinued treatment because of adverse reactions. The rate of withdrawal among patients receiving VERAMYST Nasal Spray was similar to or lower than the rate among patients receiving placebo.
Table 1 displays the common adverse reactions (greater than 1% in any patient group receiving VERAMYST Nasal Spray) that occurred more frequently in patients aged 12 years and older treated with VERAMYST Nasal Spray compared with placebo-treated patients.
|
Adverse Event |
Adult and Adolescent Patients Aged 12 Years and Older |
|
|
Vehicle Placebo (n = 774) |
VERAMYST Nasal Spray 110 mcg Once Daily (n = 768) |
|
|
Headache |
54 (7%) |
72 (9%) |
|
Epistaxis |
32 (4%) |
45 (6%) |
|
Pharyngolaryngeal pain |
8 (1%) |
15 (2%) |
|
Nasal ulceration |
3 (<1%) |
11 (1%) |
|
Back pain |
7 (<1%) |
9 (1%) |
There were no differences in the incidence of adverse reactions based on gender or race. Clinical trials did not include sufficient numbers of patients aged 65 years and older to determine whether they respond differently from younger subjects.
Pediatric Patients Aged 2 to 11 Years
In the 3 clinical trials in pediatric patients aged 2 to younger than 12 years, overall adverse reactions were reported with approximately the same frequency by patients treated with VERAMYST Nasal Spray and those receiving placebo. Table 2 displays the common adverse reactions (greater than 3% in any patient group receiving VERAMYST Nasal Spray) that occurred more frequently in patients aged 2 to 11 years treated with VERAMYST Nasal Spray compared with placebo-treated patients.
|
Adverse Event |
Pediatric Patients Aged 2 to Younger than 12 Years |
||
|
Vehicle Placebo (n = 429) |
VERAMYST Nasal Spray 55 mcg Once Daily (n = 369) |
VERAMYST Nasal Spray 110 mcg Once Daily (n = 426) |
|
|
Headache |
31 (7%) |
28 (8%) |
33 (8%) |
|
Nasopharyngitis |
21 (5%) |
20 (5%) |
21 (5%) |
|
Epistaxis |
19 (4%) |
17 (5%) |
17 (4%) |
|
Pyrexia |
7 (2%) |
17 (5%) |
19 (4%) |
|
Pharyngolaryngeal pain |
14 (3%) |
16 (4%) |
12 (3%) |
|
Cough |
12 (3%) |
12 (3%) |
16 (4%) |
There were no differences in the incidence of adverse reactions based on gender or race. Pyrexia occurred more frequently in children aged 2 to younger than 6 years compared with children aged 6 to younger than 12 years.
Long-term (52-Week) Safety Trial
In a 52-week, placebo-controlled, long-term safety trial, 605 patients (307 females and 298 males aged 12 years and older) with perennial allergic rhinitis were treated with VERAMYST Nasal Spray 110 mcg once daily for 12 months and 201 were treated with placebo nasal spray. While most adverse reactions were similar in type and rate between the treatment groups, epistaxis occurred more frequently in patients who received VERAMYST Nasal Spray (123/605, 20%) than in patients who received placebo (17/201, 8%). Epistaxis tended to be more severe in patients treated with VERAMYST Nasal Spray. All 17 reports of epistaxis that occurred in patients who received placebo were of mild intensity, while 83, 39, and 1 of the total 123 epistaxis events in patients treated with VERAMYST Nasal Spray were of mild, moderate, and severe intensity, respectively. No patient experienced a nasal septal perforation during this trial.
6.2 Postmarketing Experience
In addition to adverse reactions reported from clinical trials, the following adverse reactions have been identified during postmarketing use of VERAMYST Nasal Spray. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These events have been chosen for inclusion due to either their seriousness, frequency of reporting, or causal connection to fluticasone furoate or a combination of these factors.
Immune System Disorders
Hypersensitivity reactions, including anaphylaxis, angioedema, rash, and urticaria.
Respiratory, Thoracic, and Mediastinal Disorders
Rhinalgia, nasal discomfort (including nasal burning, nasal irritation, and nasal soreness), nasal dryness, and nasal septal perforation.
7 DRUG INTERACTIONS
Fluticasone furoate is cleared by extensive first-pass metabolism mediated by CYP3A4. In a drug interaction trial of intranasal fluticasone furoate and the CYP3A4 inhibitor ketoconazole given as a 200-mg once-daily dose for 7 days, 6 of 20 subjects receiving fluticasone furoate and ketoconazole had measurable but low levels of fluticasone furoate compared with 1 of 20 receiving fluticasone furoate and placebo. Based on this trial and the low systemic exposure, there was a 5% reduction in 24-hour serum cortisol levels with ketoconazole compared with placebo. The data from this trial should be carefully interpreted because the trial was conducted with ketoconazole 200 mg once daily rather than 400 mg, which is the maximum recommended dosage. Therefore, caution is required with the coadministration of VERAMYST Nasal Spray and ketoconazole or other potent CYP3A4 inhibitors.
Based on data with another glucocorticoid, fluticasone propionate, metabolized by CYP3A4, coadministration of VERAMYST Nasal Spray with the potent CYP3A4 inhibitor ritonavir is not recommended because of the risk of systemic effects secondary to increased exposure to fluticasone furoate. High exposure to corticosteroids increases the potential for systemic side effects, such as cortisol suppression.
Enzyme induction and inhibition data suggest that fluticasone furoate is unlikely to significantly alter the cytochrome P450-mediated metabolism of other compounds at clinically relevant intranasal dosages.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Teratogenic Effects
Pregnancy Category C. Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels.
There were no teratogenic effects in rats and rabbits at inhaled fluticasone furoate dosages of up to 91 and 8 mcg/kg/day, respectively (approximately 7 and 1 times, respectively, the maximum recommended daily intranasal dose in adults on a mcg/m2 basis). There was also no effect on pre- or post-natal development in rats treated with up to 27 mcg/kg/day by inhalation during gestation and lactation (approximately 2 times the maximum recommended daily intranasal dose in adults on a mcg/m2 basis).
There are no adequate and well-controlled studies in pregnant women. VERAMYST Nasal Spray should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nonteratogenic Effects
Hypoadrenalism may occur in infants born of mothers receiving corticosteroids during pregnancy. Such infants should be carefully monitored.
8.3 Nursing Mothers
It is not known whether fluticasone furoate is excreted in human breast milk. However, other corticosteroids have been detected in human milk. Since there are no data from controlled trials on the use of intranasal fluticasone furoate by nursing mothers, caution should be exercised when VERAMYST Nasal Spray is administered to a nursing woman.
8.4 Pediatric Use
Controlled clinical trials with VERAMYST Nasal Spray included 1,224 patients aged 2 to 11 years and 344 adolescent patients aged 12 to 17 years [see Clinical Studies (14.1)]. The safety and effectiveness of VERAMYST Nasal Spray in children younger than 2 years have not been established.
Controlled clinical trials have shown that intranasal corticosteroids may cause a reduction in growth velocity in pediatric patients. This effect has been observed in the absence of laboratory evidence of HPA axis suppression, suggesting that growth velocity is a more sensitive indicator of systemic corticosteroid exposure in pediatric patients than some commonly used tests of HPA axis function. The long-term effects of reduction in growth velocity associated with intranasal corticosteroids, including the impact on final adult height, are unknown. The potential for “catch-up” growth following discontinuation of treatment with intranasal corticosteroids has not been adequately studied. The growth of pediatric patients receiving intranasal corticosteroids, including VERAMYST Nasal Spray, should be monitored routinely (e.g., via stadiometry). The potential growth effects of prolonged treatment should be weighed against the clinical benefits obtained and the risks/benefits of treatment alternatives. To minimize the systemic effects of intranasal corticosteroids, including VERAMYST Nasal Spray, each patient’s dose should be titrated to the lowest dosage that effectively controls his/her symptoms.
A randomized, double-blind, parallel-group, multicenter, 1-year placebo-controlled clinical growth trial evaluated the effect of 110 mcg of VERAMYST Nasal Spray once daily on growth velocity in 474 prepubescent children (girls aged 5 to 7.5 years and boys aged 5 to 8.5 years) with stadiometry. Mean growth velocity over the 52-week treatment period was lower in the patients receiving VERAMYST Nasal Spray (5.19 cm/year compared with placebo (5.46 cm/year). The mean treatment difference was -0.27 cm/year (95% CI: -0.48 to -0.06) [see Warnings and Precautions (5.7)].
8.5 Geriatric Use
Clinical studies of VERAMYST Nasal Spray did not include sufficient numbers of subjects aged 65 years and older to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
10 OVERDOSAGE
Chronic overdosage may result in signs/symptoms of hypercorticism [see Warnings and Precautions (5.5)]. There are no data on the effects of acute or chronic overdosage with VERAMYST Nasal Spray. Because of low systemic bioavailability and an absence of acute drug-related systemic findings in clinical trials (with dosages of up to 440 mcg/day for 2 weeks [4 times the maximum recommended daily dose]), overdose is unlikely to require any therapy other than observation.
Intranasal administration of up to 2,640 mcg/day (24 times the recommended adult dose) of fluticasone furoate was administered to healthy human volunteers for 3 days. Single- and repeat-dose trials with orally inhaled fluticasone furoate doses of 50 to 4,000 mcg have shown decreased mean serum cortisol at doses of 500 mcg or higher. The oral median lethal dose in mice and rats was greater than 2,000 mg/kg (approximately 74,000 and 147,000 times, respectively, the maximum recommended daily intranasal dose in adults and 52,000 and 105,000 times, respectively, the maximum recommended daily intranasal dose in children, on a mcg/m2 basis).
Acute overdosage with the intranasal dosage form is unlikely since 1 bottle of VERAMYST Nasal Spray contains approximately 3 mg of fluticasone furoate, and the bioavailability of fluticasone furoate is less than 1% for 2.64 mg/day given intranasally and 1% for 2 mg/day given as an oral solution.
11 DESCRIPTION
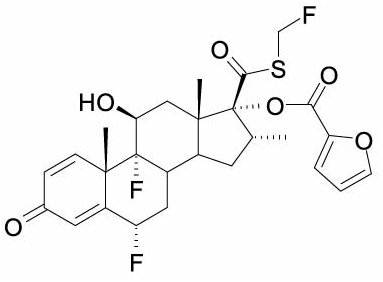
Fluticasone furoate, the active component of VERAMYST Nasal Spray, is a synthetic fluorinated corticosteroid having the chemical name (6α,11β,16α,17α)-6,9-difluoro-17-{[(fluoro-methyl)thio]carbonyl}-11-hydroxy-16-methyl-3-oxoandrosta-1,4-dien-17-yl 2-furancarboxylate and the following chemical structure:
Fluticasone furoate is a white powder with a molecular weight of 538.6, and the empirical formula is C27H29F3O6S. It is practically insoluble in water.
VERAMYST Nasal Spray is an aqueous suspension of micronized fluticasone furoate for topical administration to the nasal mucosa by means of a metering (50 microliters), atomizing spray pump. After initial priming [see Dosage and Administration (2)], each actuation delivers 27.5 mcg of fluticasone furoate in a volume of 50 microliters of nasal spray suspension. VERAMYST Nasal Spray also contains 0.015% w/w benzalkonium chloride, dextrose anhydrous, edetate disodium, microcrystalline cellulose and carboxymethylcellulose sodium, polysorbate 80, and purified water. It has a pH of approximately 6.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Fluticasone furoate is a synthetic trifluorinated corticosteroid with potent anti-inflammatory activity. The precise mechanism through which fluticasone furoate affects rhinitis symptoms is not known. Corticosteroids have been shown to have a wide range of actions on multiple cell types (e.g., mast cells, eosinophils, neutrophils, macrophages, lymphocytes) and mediators (e.g., histamine, eicosanoids, leukotrienes, cytokines) involved in inflammation. Specific effects of fluticasone furoate demonstrated in in vitro and in vivo models included activation of the glucocorticoid response element, inhibition of pro-inflammatory transcription factors such as NFkB, and inhibition of antigen-induced lung eosinophilia in sensitized rats.
Fluticasone furoate has been shown in vitro to exhibit a binding affinity for the human glucocorticoid receptor that is approximately 29.9 times that of dexamethasone and 1.7 times that of fluticasone propionate. The clinical relevance of these findings is unknown.
12.2 Pharmacodynamics
Adrenal Function
The effects of VERAMYST Nasal Spray on adrenal function have been evaluated in 4 controlled clinical trials in patients with perennial allergic rhinitis. Two 6-week clinical trials were designed specifically to assess the effect of VERAMYST Nasal Spray on the HPA axis with assessments of both 24-hour urinary cortisol excretion and serum cortisol levels in domiciled patients. In addition, one 52-week safety trial and one 12-week safety and efficacy trial included assessments of 24-hour urinary cortisol excretion. Details of the trials and results are described below. In all 4 trials, since serum fluticasone determinations were generally below the limit of quantification, compliance was assured by efficacy assessments.
Clinical Trials Specifically Designed to Assess Hypothalamic-Pituitary-Adrenal Axis Effect: In a 6-week randomized, double-blind, parallel-group trial in adult and adolescent patients aged 12 years and older with perennial allergic rhinitis, VERAMYST Nasal Spray 110 mcg was compared with both placebo nasal spray and prednisone as a positive-control group that received prednisone 10 mg orally once daily for the final 7 days of the treatment period. Adrenal function was assessed by 24-hour urinary cortisol excretion before and after 6 weeks of treatment and by serial serum cortisol levels. Patients were domiciled for collection of 24-hour urinary cortisol. After 6 weeks of treatment, there was a change from baseline in the mean 24-hour urinary cortisol excretion in the group treated with VERAMYST Nasal Spray (n = 43) of -1.16 mcg/day compared with -3.48 mcg/day in the placebo group (n = 42). The difference from placebo in the group treated with VERAMYST Nasal Spray was 2.32 mcg/day (95% CI: -6.76, 11.39). Urinary cortisol data were not available for the positive-control (prednisone) treatment group. For serum cortisol levels, after 6 weeks of treatment there was a change from baseline in the mean (0 to 24 hours) of -0.38 and 0.08 mcg/dL for the group treated with VERAMYST Nasal Spray (n = 43) and the placebo group (n = 44), respectively, with a difference between the group treated with VERAMYST Nasal Spray and the placebo group of -0.47 mcg/dL (95% CI: -1.31, 0.37). For comparison, in the positive-control (prednisone, n = 12) treatment group, there was a change in mean serum cortisol (0 to 24 hours) from baseline of -4.49 mcg/dL with a difference between the prednisone and placebo group of -4.57 mcg/dL (95% CI: -5.83, -3.31).
The second 6-week trial conducted in children aged 2 to 11 years was of similar design to the adult trial, including adrenal function assessments, but did not include a prednisone positive-control arm. Patients were treated once daily with VERAMYST Nasal Spray 110 mcg or placebo nasal spray. After 6 weeks of treatment, there was a change in the mean 24-hour urinary cortisol excretion in the group treated with VERAMYST Nasal Spray (n = 43) of 0.49 mcg/day compared with 1.92 mcg/day in the placebo group (n = 41), with a difference between the group treated with VERAMYST Nasal Spray and the placebo group of -1.43 mcg/day (95% CI: -5.21, 2.35). For serum cortisol levels, after 6 weeks, there was a change from baseline in mean (0 to 24 hours) of -0.34 and -0.23 mcg/dL for the group treated with VERAMYST Nasal Spray (n = 48) and for the placebo group (n = 47), respectively, with a difference between the group treated with VERAMYST Nasal Spray and the placebo group of -0.11 mcg/dL (95% CI: -0.88, 0.66).
Additional Hypothalamic-Pituitary-Adrenal Axis Assessments
In the 52-week safety trial in adolescents and adults aged 12 years and older with perennial allergic rhinitis, VERAMYST Nasal Spray 110 mcg (n = 605) was compared with placebo nasal spray (n = 201). Adrenal function was assessed by 24-hour urinary cortisol excretion in a subset of patients who received VERAMYST Nasal Spray (n = 370) or placebo (n = 120) before and after 52 weeks of treatment. After 52 weeks of treatment, the mean change from baseline 24-hour urinary cortisol excretion was 5.84 mcg/day in the group treated with VERAMYST Nasal Spray and 3.34 mcg/day in the placebo group. The difference from placebo in mean change from baseline 24-hour urinary cortisol excretion was 2.50 mcg/day (95% CI: -5.49, 10.49).
In the 12-week safety and efficacy trial in children aged 2 to 11 years with perennial allergic rhinitis, VERAMYST Nasal Spray 55 mcg (n = 185) and VERAMYST Nasal Spray 110 mcg (n = 185) were compared with placebo nasal spray (n = 188). Adrenal function was assessed by measurement of 24-hour urinary free cortisol in a subset of patients who were aged 6 to 11 years (103 to 109 patients per group) before and after 12 weeks of treatment. After 12 weeks of treatment, there was a decrease in mean 24-hour urinary cortisol excretion from baseline in the group treated with VERAMYST Nasal Spray 55 mcg (n = 109) of -2.93 mcg/day and in the group treated with VERAMYST Nasal Spray 110 mcg (n = 103) of -2.07 mcg/day compared with an increase in the placebo group (n = 107) of 0.08 mcg/day. The difference from placebo in mean change from baseline in 24-hour urinary cortisol excretion for the group treated with VERAMYST Nasal Spray 55 mcg was -3.01 mcg/day (95% CI: -6.16, 0.13) and -2.14 mcg/day (95% CI: -5.33, 1.04) for the group treated with VERAMYST Nasal Spray 110 mcg.
When the results of the HPA axis assessments described above are taken as a whole, an effect of intranasal fluticasone furoate on adrenal function cannot be ruled out, especially in pediatric patients.
Cardiac Effects
A QT/QTc trial did not demonstrate an effect of fluticasone furoate administration on the QTc interval. The effect of a single dose of 4,000 mcg of orally inhaled fluticasone furoate on the QTc interval was evaluated over 24 hours in 40 healthy male and female subjects in a placebo-and positive-controlled (a single dose of 400 mg oral moxifloxacin) cross-over trial. The QTcF maximal mean change from baseline following fluticasone furoate was similar to that observed with placebo with a treatment difference of 0.788 msec (90% CI: -1.802, 3.378). In contrast, moxifloxacin given as a 400-mg tablet resulted in prolongation of the QTcF maximal mean change from baseline compared with placebo with a treatment difference of 9.929 msec (90% CI: 7.339, 12.520). While a single dose of fluticasone furoate had no effect on the QTc interval, the effects of fluticasone furoate may not be at steady state following single dose. The effect of fluticasone furoate on the QTc interval following multiple-dose administration is unknown.
12.3 Pharmacokinetics
Absorption
Following intranasal administration of fluticasone furoate, most of the dose is eventually swallowed and undergoes incomplete absorption and extensive first-pass metabolism in the liver and gut, resulting in negligible systemic exposure. At the highest recommended intranasal dosage of 110 mcg once daily for up to 12 months in adults and up to 12 weeks in children, plasma concentrations of fluticasone furoate are typically not quantifiable despite the use of a sensitive HPLC-MS/MS assay with a lower limit of quantification (LOQ) of 10 pg/mL. However, in a few isolated cases (less than 0.3%) fluticasone furoate was detected in high concentrations above 500 pg/mL, and in a single case the concentration was as high as 1,430 pg/mL in the 52-week trial. There was no relationship between these concentrations and cortisol levels in these subjects. The reasons for these high concentrations are unknown.
Absolute bioavailability was evaluated in 16 male and female subjects following supratherapeutic dosages of fluticasone furoate (880 mcg given intranasally at 8-hour intervals for 10 doses, or 2,640 mcg/day). The average absolute bioavailability was 0.50% (90% CI: 0.34%, 0.74%).
Due to the low bioavailability by the intranasal route, the majority of the pharmacokinetic data was obtained via other routes of administration. Trials using oral solution and intravenous dosing of radiolabeled drug have demonstrated that at least 30% of fluticasone furoate is absorbed and then rapidly cleared from plasma. Oral bioavailability is on average 1.26%, and the majority of the circulating radioactivity is due to inactive metabolites.
Distribution
Following intravenous administration, the mean volume of distribution at steady state is 608 L.
Binding of fluticasone furoate to human plasma proteins is greater than 99%.
Metabolism
In vivo studies have revealed no evidence of cleavage of the furoate moiety to form fluticasone. Fluticasone furoate is cleared (total plasma clearance of 58.7 L/h) from systemic circulation principally by hepatic metabolism via CYP3A4. The principal route of metabolism is hydrolysis of the S-fluoromethyl carbothioate function to form the inactive 17β-carboxylic acid metabolite.
Elimination
Fluticasone furoate and its metabolites are eliminated primarily in the feces, accounting for approximately 101% and 90% of the orally and intravenously administered dose, respectively. Urinary excretion accounted for approximately 1% and 2% of the orally and intravenously administered dose, respectively. The elimination phase half-life averaged 15.1 hours following intravenous administration.
Population Pharmacokinetics
Fluticasone furoate is typically not quantifiable in plasma following intranasal dosing of 110 mcg once daily with the exception of isolated cases of very high plasma levels (see Absorption). Overall, quantifiable levels (greater than 10 pg/mL) were observed in less than 31% of patients aged 12 years and older and in less than 16% of children (aged 2 to 11 years) following intranasal dosing of 110 mcg once daily and in less than 7% of children following intranasal dosing of 55 mcg once daily. There was no evidence to suggest that the presence or absence of detectable levels of fluticasone furoate was related to gender, age, or race.
Hepatic Impairment
The pharmacokinetics of fluticasone furoate following intranasal administration in subjects with hepatic impairment have not been evaluated. Data available with orally inhaled fluticasone furoate/vilanterol are applicable to intranasal dosing of fluticasone furoate. Following repeat dosing of orally inhaled fluticasone furoate/vilanterol 200 mcg/25 mcg (100 mcg/12.5 mcg in the severe impairment group) for 7 days, fluticasone furoate systemic exposure (AUC) increased 34%, 83%, and 75% in subjects with mild, moderate, and severe hepatic impairment, respectively, compared with healthy subjects.
In subjects with moderate hepatic impairment receiving fluticasone furoate/vilanterol 200 mcg/25 mcg, mean serum cortisol (0 to 24 hours) was reduced by 34% (90% CI: 11%, 51%) compared with healthy subjects. In subjects with severe hepatic impairment receiving fluticasone furoate/vilanterol 100 mcg/12.5 mcg, mean serum cortisol (0 to 24 hours) was increased by 14% (90% CI: -16%, 55%) compared with healthy subjects [see Use in Specific Populations (8.6)].
Renal Impairment
Fluticasone furoate is not detectable in urine from healthy subjects following intranasal dosing. Less than 1% of dose-related material is excreted in urine [see Use in Specific Populations (8.7)].
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Fluticasone furoate produced no treatment-related increases in the incidence of tumors in 2-year inhalation studies in rats and mice at doses of up to 9 and 19 mcg/kg/day, respectively (less than the maximum recommended daily intranasal dose in adults and children on a mcg/m2 basis).
Fluticasone furoate did not induce gene mutation in bacteria or chromosomal damage in a mammalian cell mutation test in mouse lymphoma L5178Y cells in vitro. There was also no evidence of genotoxicity in the in vivo micronucleus test in rats.
No evidence of impairment of fertility was observed in reproductive studies conducted in male and female rats at inhaled fluticasone furoate doses of up to 24 and 91 mcg/kg/day, respectively (approximately 2 and 7 times, respectively, the maximum recommended daily intranasal dose in adults on a mcg/m2 basis).
14 CLINICAL STUDIES
14.1 Seasonal and Perennial Allergic Rhinitis
Adult and Adolescent Patients Aged 12 Years and Older
The efficacy and safety of VERAMYST Nasal Spray was evaluated in 5 randomized, double-blind, parallel-group, multicenter, placebo-controlled clinical trials of 2 to 4 weeks’ duration in adult and adolescent patients aged 12 years and older with symptoms of seasonal or perennial allergic rhinitis. The 5 clinical trials included one 2-week dose-ranging trial in patients with seasonal allergic rhinitis, three 2-week confirmatory efficacy trials in patients with seasonal allergic rhinitis, and one 4-week efficacy trial in patients with perennial allergic rhinitis. These trials included 1,829 patients (697 males and 1,132 females). About 75% of patients were Caucasian, and the mean age was 36 years. Of these patients, 722 received VERAMYST Nasal Spray 110 mcg once daily administered as 2 sprays in each nostril.
Assessment of efficacy was based on total nasal symptom score (TNSS). TNSS is calculated as the sum of the patients’ scoring of the 4 individual nasal symptoms (rhinorrhea, nasal congestion, sneezing, and nasal itching) on a 0 to 3 categorical severity scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe) as reflective(rTNSS) or instantaneous (iTNSS). rTNSS required the patients to record symptom severity over the previous 12 hours; iTNSS required patients to record symptom severity at the time immediately prior to the next dose. Morning and evening rTNSS scores were averaged over the treatment period and the difference from placebo in the change from baseline rTNSS was the primary efficacy endpoint. The morning iTNSS (AM iTNSS) reflects the TNSS at the end of the 24-hour dosing interval and is an indication of whether the effect was maintained over the 24-hour dosing interval.
Additional secondary efficacy variables were assessed, including the total ocular symptom score (TOSS) and the Rhinoconjunctivitis Quality of Life Questionnaire (RQLQ). TOSS is calculated as the sum of the patients’ scoring of the 3 individual ocular symptoms (itching/burning, tearing/watering, and redness) on a 0 to 3 categorical severity scale (0 = absent, 1 = mild, 2 = moderate, 3 = severe) as reflective (rTOSS) or instantaneous scores (iTOSS). To assess efficacy, rTOSS and AM iTOSS were evaluated as described above for the TNSS. Patients’ perceptions of disease-specific quality of life were evaluated through use of the RQLQ, which assesses the impact of allergic rhinitis treatment through 28 items in 7 domains (activities, sleep, non-nose/eye symptoms, practical problems, nasal symptoms, eye symptoms, and emotional) on a 7-point scale where 0 = no impairment and 6 = maximum impairment. An overall RQLQ score is calculated from the mean of all items in the instrument. An absolute difference of greater than or equal to 0.5 in mean change from baseline over placebo is considered the minimally important difference (MID) for the RQLQ.
Dose-ranging Trial: The dose-ranging trial was a 2-week trial that evaluated the efficacy of 4 doses of fluticasone furoate nasal spray (440, 220, 110, and 55 mcg) in patients with seasonal allergic rhinitis. In this trial, each of the 4 doses of fluticasone furoate nasal spray demonstrated greater decreases in the rTNSS than placebo, and the difference was statistically significant (Table 3).
|
Treatment |
n |
Baseline (AM + PM) |
Change from Baseline |
Difference from Placebo |
||
|
LS Mean |
95% CI |
P Value |
||||
|
Fluticasone furoate 440 mcg |
130 |
9.6 |
-4.02 |
-2.19 |
-2.75, -1.62 |
<0.001 |
|
Fluticasone furoate 220 mcg |
129 |
9.5 |
-3.19 |
-1.36 |
-1.93, -0.79 |
<0.001 |
|
Fluticasone furoate 110 mcg |
127 |
9.5 |
-3.84 |
-2.01 |
-2.58, -1.44 |
<0.001 |
|
Fluticasone furoate 55 mcg |
125 |
9.6 |
-3.50 |
-1.68 |
-2.25, -1.10 |
<0.001 |
|
Placebo |
128 |
9.6 |
-1.83 | |||
Each of the 4 doses of fluticasone furoate nasal spray also demonstrated greater decreases in the AM iTNSS than placebo, and the difference between each of the 4 fluticasone furoate treatment groups and placebo was statistically significant, indicating that the effect was maintained over the 24-hour dosing interval.
Seasonal Allergic Rhinitis Trials: Three clinical trials were designed to evaluate the efficacy of VERAMYST Nasal Spray 110 mcg once daily compared with placebo in patients with seasonal allergic rhinitis over a 2-week treatment period. In all 3 trials, VERAMYST Nasal Spray 110 mcg demonstrated a greater decrease from baseline in the rTNSS and AM iTNSS than placebo, and the difference from placebo was statistically significant. In terms of ocular symptoms, in all 3 seasonal allergic rhinitis trials, VERAMYST Nasal Spray 110 mcg demonstrated a greater decrease from baseline in the rTOSS than placebo and the difference from placebo was statistically significant. For the RQLQ in all 3 seasonal allergic rhinitis trials, VERAMYST Nasal Spray 110 mcg demonstrated greater decrease from baseline in the overall RQLQ than placebo, and the difference from placebo was statistically significant. The difference in the overall RQLQ score mean change from baseline between the groups treated with VERAMYST Nasal Spray and placebo ranged from -0.60 to -0.70 in the 3 trials, meeting the minimally important difference criterion. Table 4 displays the efficacy results from a representative trial in patients with seasonal allergic rhinitis.
Perennial Allergic Rhinitis Trials: One clinical trial was designed to evaluate the efficacy of VERAMYST Nasal Spray 110 mcg once daily compared with placebo in patients with perennial allergic rhinitis over a 4-week treatment period. VERAMYST Nasal Spray 110 mcg demonstrated a greater decrease from baseline in the rTNSS and AM iTNSS than placebo, and the difference from placebo was statistically significant. Similar to patients with seasonal allergic rhinitis, the improvement of nasal symptoms with VERAMYST Nasal Spray in patients with perennial allergic rhinitis persisted for a full 24 hours, as evaluated by AM iTNSS immediately prior to the next dose. However, unlike the trials in patients with seasonal allergic rhinitis, patients with perennial allergic rhinitis who were treated with VERAMYST Nasal Spray 110 mcg did not demonstrate statistically significant improvement from baseline in rTOSS or in disease-specific quality of life as measured by the RQLQ compared with placebo. In addition, the overall RQLQ score mean change from baseline difference between the group treated with VERAMYST Nasal Spray and the placebo group was -0.23, which did not meet the minimally important difference of greater than or equal to 0.5. Table 4 displays the efficacy results from the clinical trial in patients with perennial allergic rhinitis.
|
Treatment |
n |
Baseline |
Change from Baseline – LS Mean |
Difference from Placebo |
|||
|
LS Mean |
95% CI |
P Value |
|||||
|
Reflective Total Nasal Symptom Scores |
|||||||
|
Seasonal allergic rhinitis trial | |||||||
|
151 |
9.6 |
-3.55 |
-1.47 |
-2.01, -0.94 |
<0.001 |
|
|
147 |
9.9 |
-2.07 | ||||
|
Perennial allergic rhinitis trial | |||||||
|
149 |
8.6 |
-2.78 |
-0.71 |
-1.20, -0.21 |
0.005 |
|
|
153 |
8.7 |
-2.08 | ||||
|
Instantaneous Total Nasal Symptom Scores |
|||||||
|
Seasonal allergic rhinitis trial | |||||||
|
151 |
9.4 |
-2.90 |
-1.38 |
-1.90, -0.85 |
<0.001 |
|
|
147 |
9.3 |
-1.53 | ||||
|
Perennial allergic rhinitis trial | |||||||
|
149 |
8.2 |
-2.45 |
-0.71 |
-1.20, -0.21 |
0.006 |
|
|
153 |
8.3 |
-1.75 | ||||
|
Reflective Total Ocular Symptom Scores |
|||||||
|
Seasonal allergic rhinitis trial | |||||||
|
151 |
6.6 |
-2.23 |
-0.60 |
-1.01, -0.19 |
0.004 |
|
|
147 |
6.5 |
-1.63 | ||||
|
Perennial allergic rhinitis trial | |||||||
|
149 |
4.8 |
-1.39 |
-0.15 |
-0.52, 0.22 |
0.428 |
|
|
153 |
5.0 |
-1.24 | ||||
|
Rhinoconjunctivitis Quality of Life Questionnaire |
|||||||
|
Seasonal allergic rhinitis trial | |||||||
|
144 |
3.9 |
-1.77 |
-0.60 |
-0.93, -0.28 |
<0.001 |
|
|
144 |
3.9 |
-1.16 | ||||
|
Perennial allergic rhinitis trial | |||||||
|
143 |
3.5 |
-1.41 |
-0.23 |
-0.59, 0.13 |
0.214 |
|
|
151 |
3.4 |
-1.18 | ||||
Onset of action was evaluated by frequent instantaneous TNSS assessments after the first dose in the clinical trials in patients with seasonal allergic rhinitis and perennial allergic rhinitis. Onset of action was generally observed within 24 hours in patients with seasonal allergic rhinitis. In patients with perennial rhinitis, onset of action was observed after 4 days of treatment. Continued improvement in symptoms was observed over approximately 1 and 3 weeks in patients with seasonal or perennial allergic rhinitis, respectively.
Pediatric Patients Aged 2 to 11 Years
The efficacy and safety of VERAMYST Nasal Spray were evaluated in 1,112 children (633 boys and 479 girls), mean age of 8 years with seasonal or perennial allergic rhinitis in 2 controlled clinical trials. The pediatric patients were treated with VERAMYST Nasal Spray 55 or 110 mcg once daily for 2 to 12 weeks (n = 369 for each dose). The trials were similar in design to the trials conducted in adolescents and adults; however, the efficacy determination was made from patient- or parent/guardian-reported TNSS for children aged 6 to younger than 12 years. Children treated with VERAMYST Nasal Spray generally exhibited greater decreases in nasal symptoms than placebo-treated patients. In seasonal allergic rhinitis, the difference in rTNSS was statistically significant only for the 110-mcg dose. In perennial allergic rhinitis, the difference in rTNSS was statistically significant only for the 55-mcg dose. Changes in rTOSS in the seasonal allergic rhinitis trial were not statistically significant compared with placebo for either dose. rTOSS was not assessed in the perennial allergic rhinitis trial. Table 5 displays the efficacy results from the clinical trials in patients with perennial allergic rhinitis and seasonal allergic rhinitis in children aged 6 to younger than 12 years. Efficacy in children aged 2 to younger than 6 years was supported by a numerical decrease in the rTNSS.
|
Treatment |
n |
Baseline |
Change from Baseline – LS Mean |
Difference from Placebo |
||
|
LS Mean |
95% CI |
P Value |
||||
|
Reflective Total Nasal Symptom Scores |
||||||
|
Seasonal allergic rhinitis trial | ||||||
|
151 |
8.6 |
-2.71 |
-0.16 |
-0.69, 0.37 |
0.553 |
|
146 |
8.5 |
-3.16 |
-0.62 |
-1.15, -0.08 |
0.025 |
|
149 |
8.4 |
-2.54 | |||
|
Perennial allergic rhinitis trial | ||||||
|
144 |
8.5 |
-4.16 |
-0.75 |
-1.24, -0.27 |
0.003 |
|
140 |
8.6 |
-3.86 |
-0.45 |
-0.95, 0.04 |
0.073 |
|
147 |
8.5 |
-3.41 | |||
|
Instantaneous Total Nasal Symptom Scores |
||||||
|
Seasonal allergic rhinitis trial | ||||||
|
151 |
8.4 |
-2.37 |
-0.23 |
-0.77, 0.30 |
0.389 |
|
146 |
8.3 |
-2.80 |
-0.67 |
-1.21, -0.13 |
0.015 |
|
149 |
8.4 |
-2.13 | |||
|
Perennial allergic rhinitis trial | ||||||
|
144 |
8.3 |
-3.62 |
-0.75 |
-1.24, -0.27 |
0.002 |
|
140 |
8.3 |
-3.52 |
-0.65 |
-1.14, -0.16 |
0.009 |
|
147 |
8.3 |
-2.87 | |||
|
Reflective Total Ocular Symptom Scores |
||||||
|
Seasonal allergic rhinitis trial | ||||||
|
151 |
4.4 |
-1.26 |
0.04 |
-0.33, 0.41 |
0.826 |
|
146 |
4.1 |
-1.45 |
-0.15 |
-0.52, 0.22 |
0.426 |
|
149 |
3.8 |
-1.30 | |||
16 HOW SUPPLIED/STORAGE AND HANDLING
VERAMYST Nasal Spray, 27.5 mcg per spray, is supplied in a brown glass bottle enclosed in a nasal device with a nozzle and a mist-release button to actuate the spray in a box of 1 (NDC 0173-0753-00) with FDA-Approved Patient Labeling (see Patient Instructions for Use for proper actuation of the device). Each bottle contains a net fill weight of 10 g of white, liquid suspension and will provide 120 metered sprays. After priming [see Dosage and Administration (2)], each spray delivers a fine mist containing 27.5 mcg of fluticasone furoate in 50 microliters of formulation through the nozzle. The contents of the bottle can be viewed through an indicator window. Shake the contents well before each use. The correct amount of medication in each spray cannot be assured before the initial priming and after 120 sprays have been used, even though the bottle is not completely empty. The nasal device should be discarded after 120 sprays have been used.
Store the device in the upright position with the cap in place between 15° and 30°C (59° and 86°F). Do not freeze or refrigerate.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
Local Nasal Effects
Inform patients that treatment with VERAMYST Nasal Spray may lead to adverse reactions, which include epistaxis and nasal ulceration. Candida infection may also occur with treatment with VERAMYST Nasal Spray. In addition, nasal corticosteroids are associated with nasal septal perforation and impaired wound healing. Advise patients who have experienced recent nasal ulcers, nasal surgery, or nasal trauma to not use VERAMYST Nasal Spray until healing has occurred [see Warnings and Precautions (5.1)].
Cataracts and Glaucoma
Inform patients that glaucoma and cataracts are associated with nasal and inhaled corticosteroid use. Instruct patients to inform their healthcare providers if a change in vision is noted while using VERAMYST Nasal Spray [see Warnings and Precautions (5.2)].
Hypersensitivity Reactions, including Anaphylaxis
Inform patients that hypersensitivity reactions, including anaphylaxis, angioedema, rash, and urticaria, may occur after administration of VERAMYST Nasal Spray. Instruct patients to discontinue use of VERAMYST Nasal Spray if such reactions occur [see Warnings and Precautions (5.3)].
Immunosuppression
Warn patients who are on immunosuppressant doses of corticosteroids to avoid exposure to chickenpox or measles and, if exposed, to consult their healthcare providers without delay. Inform patients of potential worsening of existing tuberculosis; fungal, bacterial, viral, or parasitic infections; or ocular herpes simplex [see Warnings and Precautions (5.4)].
Effect on Growth
Advise parents that VERAMYST Nasal Spray may slow growth in children. A child taking VERAMYST Nasal Spray should have his/her growth checked regularly [see Warnings and Precautions (5.7), Use in Specific Populations (8.4)].
Use Daily for Best Effect
Instruct patients to use VERAMYST Nasal Spray on a regular once-daily basis for optimal effect. VERAMYST Nasal Spray, like other corticosteroids, does not have an immediate effect on rhinitis symptoms. Although significant improvement is usually achieved within 24 hours in patients with seasonal allergic rhinitis and 4 days in patients with perennial allergic rhinitis, maximum benefit may not be reached for several days. Instruct the patient to not increase the prescribed dosage but contact the healthcare provider if symptoms do not improve or if the condition worsens.
Keep Spray Out of Eyes
Inform patients to avoid spraying VERAMYST Nasal Spray in their eyes.
Potential Drug Interactions
Advise patients that coadministration of VERAMYST Nasal Spray and ritonavir is not recommended and to be cautious if coadministering with ketoconazole.
VERAMYST is a registered trademark of the GSK group of companies.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2016 the GSK group of companies. All rights reserved.
VRM:12PI
Patient Information
VERAMYST® [VAIR-uh-mist]
(fluticasone furoate)
Nasal Spray
For Intranasal Use Only
Read the Patient Information that comes with VERAMYST Nasal Spray carefully before you start using it and each time you get a refill. There may be new information. Keep the leaflet for reference because it gives you a summary of important information about VERAMYST Nasal Spray. This leaflet does not take the place of talking to your healthcare provider about your medical condition or your treatment.
What is VERAMYST Nasal Spray?
VERAMYST Nasal Spray is a medicine that treats seasonal and year-round allergy symptoms in adults and children 2 years old and older.
VERAMYST Nasal Spray contains fluticasone furoate, which is a man-made (synthetic) corticosteroid. When you spray VERAMYST Nasal Spray into your nose, it helps reduce the nasal symptoms of allergic rhinitis (inflammation of the lining of the nose), such as stuffy nose, runny nose, nasal itching, and sneezing. VERAMYST Nasal Spray may also help red, itchy, and watery eyes in adults and teenagers with seasonal allergic rhinitis.
Your healthcare provider has prescribed VERAMYST Nasal Spray to treat your symptoms of allergic rhinitis.
It is not known if VERAMYST Nasal Spray is safe and effective in children under 2 years of age.
Who should not use VERAMYST Nasal Spray?
Do not use VERAMYST Nasal Spray if you are allergic to fluticasone furoate or any of the ingredients in VERAMYST Nasal Spray. See the end of this Patient Information leaflet for a complete list of ingredients in VERAMYST Nasal Spray.
What should I tell my healthcare provider before taking VERAMYST Nasal Spray?
Tell your healthcare provider about all of your medical conditions, including if you:
- •
- have had recent nasal sores, nasal surgery, or nasal injury.
- •
- have liver problems.
- •
- have eye or vision problems, such as cataracts or glaucoma (increased pressure in your eye).
- •
- have tuberculosis or any untreated fungal, bacterial, viral infections, or eye infections caused by herpes.
- •
- are exposed to chickenpox or measles.
- •
- are feeling unwell or have any symptoms that you do not understand.
- •
- are pregnant or plan to become pregnant. It is not known if VERAMYST Nasal Spray will harm your unborn baby. Talk to your healthcare provider if you are pregnant or plan to become pregnant.
- •
- are breastfeeding or plan to breastfeed. It is not known if VERAMYST Nasal Spray can pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take VERAMYST Nasal Spray.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal products. VERAMYST Nasal Spray and other medicines may affect each other, causing side effects. Be certain to tell your healthcare provider if you are taking a medicine that contains ritonavir (commonly used to treat HIV infection or AIDS).
How should I use VERAMYST Nasal Spray?
- •
- This medicine is for use in the nose only. Do not spray it in your eyes or mouth.
- •
- An adult should help a young child use this medicine.
- •
- This medicine has been prescribed for you by your healthcare provider. Do not give this medicine to anyone else.
- •
- Use VERAMYST Nasal Spray exactly as your healthcare provider tells you to. Do not take more of your medicine or take it more often than your healthcare provider tells you. The prescription label will usually tell you how many sprays to take and how often. If it does not or if you are not sure, ask your healthcare provider or pharmacist.
- •
- For people aged 12 years and older, the usual starting dosage is 2 sprays in each nostril, 1 time a day. After you begin to feel better, your healthcare provider may tell you that 1 spray in each nostril 1 time a day may be enough for you.
- •
- For children aged 2 to 11 years, the usual starting dosage is 1 spray in each nostril, 1 time a day. Your healthcare provider may tell you to take 2 sprays in each nostril 1 time a day. After you begin to feel better, your healthcare provider may change the dosage to 1 spray in each nostril 1 time a day. An adult should help a young child use this medicine.
- •
- Do not use VERAMYST Nasal Spray after 120 sprays (plus the initial priming sprays) have been used or after the expiration date, whichever comes first. The bottle may not be completely empty. The expiration date is printed as “EXP” on the product label and box. Before you throw away VERAMYST Nasal Spray, talk to your healthcare provider to see if you need a refill of your prescription. If your healthcare provider tells you to continue using VERAMYST Nasal Spray, throw away the empty or expired bottle and use a new bottle of VERAMYST Nasal Spray. Follow the Instructions for Use below.
- •
- Do not take extra doses or stop taking VERAMYST Nasal Spray without telling your healthcare provider.
- •
- VERAMYST Nasal Spray may begin to work within 24 hours after you take your first dose. It may take several days before it has its greatest effect. If your symptoms do not improve or get worse, call your healthcare provider.
- •
- You will get the best results if you keep using VERAMYST Nasal Spray regularly each day without missing a dose. If you miss a dose by several hours, just take your next dose at the usual time. Do not take an extra dose.
What are the possible side effects of VERAMYST Nasal Spray?
VERAMYST Nasal Spray may cause serious side effects, including:
- •
- thrush (candidiasis), a fungal infection in your mouth and throat. Tell your healthcare provider if you have any redness or white colored patches in your mouth or throat.
- •
-
hole in the cartilage in the nose (nasal septal perforation). Symptoms of nasal septal perforation may include:
- •
- crusting in the nose
- •
- nosebleeds
- •
- runny nose
- •
- whistling sound when you breathe
- •
- slow wound healing. You should not use VERAMYST Nasal Spray until your nose has healed if you have a sore in your nose, have had surgery on your nose, or if your nose has been injured.
- •
- eye problems such as glaucoma and cataracts. If you have a history of glaucoma or cataracts or have a family history of these eye problems, you should have regular eye exams while you use VERAMYST Nasal Spray.
- •
-
serious allergic reactions. Serious allergic reactions can happen with VERAMYST Nasal Spray. Stop using VERAMYST Nasal Spray and call your healthcare provider right away if you have any of the following signs of a serious allergic reaction:
- •
- shortness of breath or trouble breathing
- •
- skin rash, redness, or swelling
- •
- severe itching
- •
- swelling of the lips, tongue, or face
- •
-
immune system problems that may increase your risk of infections. You are more likely to get infections if you take medicines that may weaken your body’s ability to fight infections. Avoid contact with people who have contagious diseases such as chicken pox or measles while you use VERAMYST Nasal Spray. Symptoms of an infection may include:
- •
- fever
- •
- pain
- •
- aches
- •
- chills
- •
- feeling tired
- •
- nausea
- •
- vomiting
- •
-
adrenal insufficiency. Adrenal insufficiency is a condition in which the adrenal glands do not make enough steroid hormones. Symptoms of adrenal insufficiency may include:
- •
- tiredness
- •
- weakness
- •
- dizziness
- •
- nausea
- •
- vomiting
- •
- slowed or delayed growth in children. A child’s growth should be checked regularly while using VERAMYST Nasal Spray.
The most common side effects of VERAMYST Nasal Spray include:
- •
-
adults and adolescents 12 years of age and older
- •
- headaches
- •
- nose bleeds
- •
- sore throat
- •
- nose sores
- •
- back pain
- •
-
children 2 to 12 years of age
- •
- headaches
- •
- sore throat
- •
- nose bleeds
- •
- fever
- •
- cough
Tell your healthcare provider if you have any side effect that bothers you or does not go away.
These are not all of the possible side effects of VERAMYST Nasal Spray. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What should I know about allergic rhinitis?
“Rhinitis” means inflammation of the lining of the nose. It is sometimes called “hay fever.” Allergic rhinitis can be caused by allergies to pollen, animal dander, house dust mite, and mold spores. If you have allergic rhinitis, your nose becomes stuffy, runny, and itchy. You may also sneeze a lot. You may also have red, itchy, watery eyes; itchy throat; or blocked, itchy ears.
What are the ingredients in VERAMYST Nasal Spray?
Active ingredient: fluticasone furoate
Inactive ingredients: 0.015% w/w benzalkonium chloride, dextrose anhydrous, edetate disodium, microcrystalline cellulose, carboxymethylcellulose sodium, polysorbate 80, and purified water
Instructions for Use
Read this leaflet carefully before you start to use VERAMYST Nasal Spray. If you have any questions, ask your healthcare provider or pharmacist.
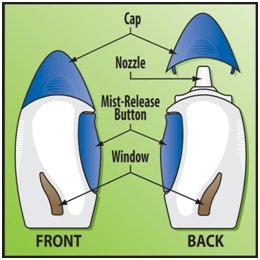
The parts of the VERAMYST Nasal Spray
VERAMYST Nasal Spray comes in a brown glass bottle inside a nasal device. It contains 120 sprays plus the first priming sprays. Be careful not to drop it. If you accidentally drop the device, check it for damage. If the device is damaged, return it to your pharmacist.
The Cap has a tab that keeps the Mist-Release Button from being pressed accidentally. It also helps keep the nozzle clean. Do not throw the cap away. Always keep the cap on the device when you are not using it.
The Nozzle is small and short, so it will fit inside your nose. The medicine comes out of the nozzle.
Pressing the Mist-Release Button sprays a measured amount of medicine from the nozzle as a gentle, fine mist. Because the button is on the side of the device, you can keep the nozzle in the right place in your nose while you press the button.
The Window lets you see if there is medicine left in the bottle when you hold it in front of a bright light. (You may not be able to see the medicine in a full bottle because the liquid level is above the window.)
How to prime your VERAMYST Nasal Spray
Priming helps to make sure you always get the same full dose of medicine. You need to prime VERAMYST Nasal Spray:
- •
- before you use a new bottle for the first time.
- •
- if you have not used your VERAMYST Nasal Spray for 30 days or longer.
- •
- if the cap has been left off the bottle for 5 days or longer.
- •
- if the device does not seem to be working right.
To prime VERAMYST Nasal Spray:
- 1.
- With the cap on, shake the device well (Figure 1). This is important to make the medicine a liquid that will spray.
- 2.
- Take the cap off by squeezing the finger grips and pulling it straight off (Figure 2).
- 3.
- Hold the device with the nozzle pointing up and away from you. Place your thumb or fingers on the button. Press the button all the way in 6 times or until a fine mist sprays from the nozzle (Figure 3). Your VERAMYST Nasal Spray is now ready to use.
How to use your VERAMYST Nasal Spray
Follow the instructions below. If you have any questions, ask your healthcare provider or pharmacist.
Before taking a dose of VERAMYST Nasal Spray, gently blow your nose to clear your nostrils. Shake the bottle well. Then do these 3 simple steps: Place, Press, Repeat.
1. PLACE
Tilt your head forward a little bit. Hold the device upright. PLACE the nozzle in one of your nostrils (Figure 4).
Point the end of the nozzle toward the side of your nose, away from the center of your nose (septum). This helps get the medicine to the right part of your nose.
2. PRESS
PRESS the button all the way in 1 time to spray the medicine in your nose while you are breathing in (Figure 5).
Do not get any spray in your eyes. If you do, rinse your eyes well with water.
Take the nozzle out of your nose. Breathe out through your mouth (Figure 6).
3. REPEAT
To deliver the medicine to the other nostril, REPEAT Steps 1 and 2 in the other nostril (Figure 7).
If your healthcare provider has told you to take 2 sprays in each nostril, do Steps 1-3 again.
Put the cap back on the device after you have finished taking your dose.
How to clean your VERAMYST Nasal Spray
After each use: wipe the nozzle with a clean, dry tissue (Figure 8). Never try to clean the nozzle with a pin or anything sharp because this will damage the nozzle. Do not use water to clean the nozzle.
Once a week: clean the inside of the cap with a clean, dry tissue (Figure 9). This will help keep the nozzle from getting blocked.
How to store your VERAMYST Nasal Spray
- •
- Keep your VERAMYST Nasal Spray and all medicines out of the reach of children.
- •
- Store between 59°F and 86°F (15°C and 30°C). Do not refrigerate or freeze.
- •
- Store with the cap on.
- •
- Store in an upright position.
This Patient Information has been approved by the U.S. Food and Drug Administration.
VERAMYST is a registered trademark of the GSK group of companies.
GlaxoSmithKline
Research Triangle Park, NC 27709
©2016 the GSK group of companies. All rights reserved.
July 2016
VRM:12PIL
PRINCIPAL DISPLAY PANEL
NDC 0173-0753-00
Veramyst®
(fluticasone furoate)
Nasal Spray
27.5 mcg per spray
For Intranasal Use Only.
ATTENTION PHARMACIST: Dispense with enclosed Patient Information leaflet.
Important: Read accompanying directions carefully.
Rx only
120 Metered Sprays
10 g net fill weight
Made in Singapore
©2015, GSK group of companies
Rev. 3/15
10000000132551
| VERAMYST
fluticasone furoate spray, metered |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - GlaxoSmithKline LLC (167380711) |