Label: CEFTRIAXONE injection, powder, for solution
-
Contains inactivated NDC Code(s)
NDC Code(s): 68330-001-01, 68330-001-10, 68330-002-01, 68330-002-10, view more68330-003-01, 68330-003-10, 68330-004-01, 68330-004-10, 68330-005-01, 68330-005-10, 68330-006-01, 68330-006-10 - Packager: Cephazone Pharma LLC
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated September 7, 2012
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
- SPL UNCLASSIFIED SECTION
-
DESCRIPTION
Ceftriaxone is a sterile, semisynthetic, broad-spectrum cephalosporin antibiotic for intravenous or intramuscular administration. Ceftriaxone sodium is (6R, 7R)-7-[2-(2-Amino-4-thiazolyl)glyoxylamido]-8-oxo-3-[[(l,2,5,6-tetrahydro-2-methyl-5,6-dioxo-as-triazin-3-yl)thio]methyl]-5-thia-l-azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, 72-(Z)-(O-methyloxime), disodium salt, sesquaterhydrate.
The chemical formula of ceftriaxone sodium is C18H16NaNa207S3∙3.5H20. It has a calculated molecular weight of 661.60 and the following structural formula:
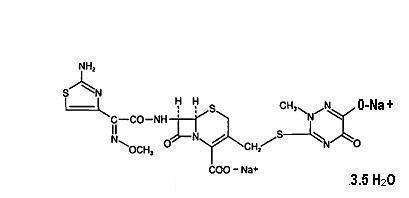
Ceftriaxone is a white to yellowish-orange crystalline powder which is readily soluble in water, sparingly soluble in methanol and very slightly soluble in ethanol. The pH of a 1 % aqueous solution is approximately 6.7. The color of ceftriaxone solutions ranges from light yellow to amber, depending on the length of storage, concentration and diluent used.
Each vial contains ceftriaxone sodium equivalent to 250 mg, 500 mg, 1 gram, or 2 grams of ceftriaxone. Each piggyback bottle contains ceftriaxone sodium equivalent to 1 gram or 2 grams of ceftriaxone. Ceftriaxone contains approximately 83 mg (3.6 mEq) of sodium per gram of ceftriaxone activity.
-
CLINICAL PHARMACOLOGY
Average plasma concentrations of ceftriaxone following a single 30-minute intravenous (IV) infusion of a 0.5,1 or 2 g dose and intramuscular (IM) administration of a single 0.5 (250 mg/mL or 350 mg/mL concentrations) or 1 g dose in healthy subjects are presented in Table 1
TABLE 1. Ceftriaxone Plasma Concentrations After Single Dose Administration. IV doses were infused at a constant rate over 30 minutes. ND=Not determined.
Average Plasma Concentrations (mcg/mL)
Dose/Route
0.5 hr.
1 hr.
2hr.
4hr.
6 hr.
8 hr.
12hr.
16 hr.
24 hr.
0.5 g IV*
82
59
48
37
29
23
15
10
5
0.5 g IM 250 mg/mL
22
33
38
35
30
26
16
ND
5
0.5 g IM 350 mg/mL
20
32
38
34
31
24
16
ND
5
1 g IV*
151
111
88
67
53
43
28
18
9
1 g IM
40
68
76
68
56
44
29
ND
ND
2 g IV*
257
192
154
117
89
74
46
31
15
Ceftriaxone was completely absorbed following IM administration with mean maximum plasma concentrations occurring between 2 and 3 hours post-dose. Multiple IV or IM doses ranging from 0.5 to 2 g at 12 to 24 hour intervals resulted in 15% to 36% accumulation of ceftriaxone above single dose values.
Ceftriaxone concentrations in urine are shown in Table 2.
TABLE 2. Urinary Concentrations of Ceftriaxone After Single Dose Administration ND = Not determined
Dose/Route
Average Urinary Concentrations (mcg/mL)
0 to 2 hr.
2 to 4 hr.
4 to 8 hr.
8 to 12 hr.
12 to 24 hr.
24 to 48 hr.
0.5 g IV
526
366
142
87
70
15
0.5 g IM
115
425
308
127
96
28
1 g IV
995
855
293
147
132
32
1 g IM
504
628
418
237
ND
ND
2 g IV
2692
1976
757
274
198
40
Thirty-three percent to 67% of a ceftriaxone dose was excreted in the urine as unchanged drug and the remainder was secreted in the bile and ultimately found in the feces as microbiologically inactive compounds. After a 1 g IV dose, average concentrations of ceftriaxone, determined from 1 to 3 hours after dosing, were 581 mcg/mL in the gallbladder bile, 788 mcg/mL in the common duct bile, 898 mcg/mL in the cystic duct bile, 78.2 mcg/g in the gallbladder wall and 62.1 mcg/mL in the concurrent plasma.
Over a 0.15 to 3 g dose range in healthy adult subjects, the values of elimination half life ranged from 5.8 to 8.7 hours; apparent volume of distribution from 5.78 to 13.5 L; plasma clearance from 0.58 to 1.45 L/hour and renal clearance from 0.32 to 0.73 L/hour. Ceftriaxone is reversibly bound to human plasma proteins, and the binding decreased from a value of 95% bound at plasma concentration of <25 mcg/mL to a value of 85% bound at 300 mcg/mL Ceftriaxone crosses the blood placenta barrier.
The average values of maximum plasma concentration, elimination half-life, plasma clearance and volume of distribution after a 50 mg/kg IV dose and after a 75 mg/kg IV dose in pediatric patients suffering from bacterial meningitis are shown in Table 3. Ceftriaxone penetrated the inflamed meninges of infants and pediatric patients; CSF concentrations after a 50 mg/kg IV dose and after a 75 mg/kg IV dose are also shown in Table 3.
TABLE 3. Average Pharmacokinetic Parameters of Ceftriaxone in Pediatric Patients with Meningitis.
50 mg/kg IV
75 mg/kg IV
Maximum Plasma Concentration (mcg/mL)
216
275
Elimination Half-life (hr)
4.6
4.3
Plasma Clearance (mL/hr/kg)
49
60
Volume of Distribution (mL/kg)
338
373
CSF Concentration-inflamed meninges (mcg/mL)
5.6
6.4
Range (mcg/mL)
1.3 to 18.5
1.3 to 44
Time after dose (hr)
3.7 (±1.6)
3.3 (±1.4)
Compared to that in healthy adult subjects, the pharmacokinetics of ceftriaxone were only minimally altered in elderly subjects and in patients with renal impairment or hepatic dysfunction (Table 4); therefore, dosage adjustments are not necessary for these patients with ceftriaxone dosages up to 2 g per day. Ceftriaxone was not removed to any significant extent from the plasma by hemodialysis. In six of 26 dialysis patients, the elimination rate of ceftriaxone was markedly reduced.
TABLE 4. Average Pharmacokinetic Parameters of Ceftriaxone in Humans - *
- creatinine clearance
Subject Group
Elimination
Half-Life
(hr)
Plasma
Clearance
(L/hr)
Volume of
Distribution (L)
Healthy Subjects
5.8 to 8.7
0.58 to 1.45
5.8 to 13.5
Elderly Subjects (mean age, 70.5 yr)
8.9
0.83
10.7
Patients With Renal Impairment
Hemodialysis Patients(0 to 5 mL/min)*
14.7
0.65
13.7
Severe (5 to 15 mL/min)
15.7
0.56
12.5
Moderate (16 to 30 mL/min)
11.4
0.72
11.8
Mild (31 to 60 mL/min)
12.4
0.70
13.3
Patients With Liver Disease
8.8
1.1
13.6
The elimination of ceftriaxone is not altered when ceftriaxone is co-administered with probenecid.
Pharmacokinetics in the Middle Ear Fluid: In one study, total ceftriaxone concentrations (bound and unbound) were measured in middle ear fluid obtained during the insertion of tympanostomy tubes in 42 pediatric patients with otitis media. Sampling times were from 1 to 50 hours after a single intramuscular injection of 50 mg/kg of ceftriaxone. Mean (± SD) ceftriaxone levels in the middle ear reached a peak of 35 (± 12) mcg/mL at 24 hours, and remained at 19 (± 7) mcg/mL at 48 hours. Based on middle ear fluid ceftriaxone concentrations in the 23 to 25 hour and the 46 to 50 hour sampling time intervals, a half-life of 25 hours was calculated. Ceftriaxone is highly bound to plasma proteins. The extent of binding to proteins in the middle ear fluid is unknown.
Interaction with Calcium: Two in vitro studies, one using adult plasma and the other neonatal plasma from umbilical cord blood have been carried out to assess interaction of ceftriaxone and calcium. Ceftriaxone concentrations up to 1 mM (in excess of concentrations achieved in vivo following administration of 2 grams ceftriaxone infused over 30 minutes) were used in combination with calcium concentrations up to 12 mM (48 mg/dL). Recovery of ceftriaxone from plasma was reduced with calcium concentrations of 6 mM (24 mg/dL) or higher in adult plasma or 4 mM (16 mg/dL) or higher in neonatal plasma. This may be reflective of ceftriaxone-calcium precipitation.
Microbiology: The bactericidal activity of ceftriaxone results from inhibition of cell wall synthesis. Ceftriaxone has a high degree of stability in the presence of beta-lactamases, both penicillinases and cephalosporinases, of gram-negative and gram-positive bacteria.
In an in vitro study antagonistic effects have been observed with the combination of chloramphenicol and ceftriaxone.
Ceftriaxone has been shown to be active against most strains of the following microorganism, both in vitro and in clinical infections described in the INDICATIONS AND USAGE section.
Aerobic gram-negative microorganisms:
Acinetobacter calcoaceticus
Enterobacter aerogenes
Enterobacter cloacae
Escherichia coli
Haemophilus influenzae (including ampicillin-resistant and beta-lactamase producing strains)
Haemophilus parainfluenzae
Klebsiella oxytoca
Klebsiella pneumoniae
Moraxella catarrhalis (including beta-lactamase producing strains)
Morganella morganii
Neisseria gonorrhoeae (including penicillinase- and nonpenicillinase-producing strains)
Neisseria meningitidis
Proteus mirabilis
Proteus vulgaris
Serratia marcescens
Ceftriaxone is also active against many strains of Pseudomonas aeruginosa
NOTE: Many strains of the above organisms that are resistant to multiple antibiotics, e.g., penicillins, cephalosporins, and aminoglycosides, are susceptible to ceftriaxone.
Aerobic gram-positive microorganisms:
Staphylococcus aureus (including penicillinase-producing strains)
Staphylococcus epidermidis
Streptococcus pneumoniae
Streptococcus pyogenes
Viridans group streptococci
NOTE: Methicillin-resistant staphylococci are resistant to cephalosporins, including ceftriaxone. Most strains of Group D streptococci and enterococci, e.g., Enterococcus (Streptococcus) faecalis, are resistant.
Anaerobic microorganisms:
Bacteroides fragilis
Clostridium species
Peptostreptococcus species
NOTE Most strains of Clostridium difficile are resistant.
The following in vitro data are available, but their clinical significance is unknown. Ceftriaxone exhibits in vitro minimal inhibitory concentrations (MICs) of ≤ 1 mcg/mL or less against most strains of the following microorganisms, however, the safety and effectiveness of ceftriaxone in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobic gram-negative microorganisms:
Citrobacter diversus
Citrobacter freundii
Providencia species (including Providencia rettgeri)
Salmonella species (including Salmonella typhi)
Shigella species
Aerobic gram-positive microorganisms:
Streptococcus agalactiae
Anaerobic microorganisms:
Prevotella (Bacteroides) bivius
Porphyromonas (Bacteroides) melaninogenicus
Susceptibility Tests:
Dilution Techniques: Quantitative methods are used to determine antimicrobial minimal inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure1 Standardized procedures are based on a dilution method (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of ceftriaxone powder. For details of susceptibility test methodologies, the most recent documents of the Clinical and Laboratory Standards Institute (CLSI) for antimicrobial susceptibility testing1-3 should be consulted.
The MIC values for aerobic organisms should be interpreted according to the following criteria:
For Enterobacteriaceae:
MIC (mcg/mL)
Interpretation
≤1
(S) Susceptible
2
(I) Intermediate
≥4
(R) Resistant
The following interpretive criteria should be used when testing Haemophilus species using Haemophilus Test Media (HTM)
MIC (mcg/mL)
Interpretation
≤2
(S) Susceptible
The absence of resistant strains precludes defining any categories other than "Susceptible". Strains yielding results suggestive of a "Nonsusceptible" category should be submitted to a reference laboratory for further testing.
The following interpretive criteria4 should be used when testing Neisseria gonorrhoeae when using GC agar base and 1 % defined growth supplement.
MIC (mcg/mL)
Interpretation
≤0.25
(S) Susceptible
The following Interpretive criteria4 should be used when testing Neisseria meningitidis on Mueller-Hinton agar with 5% defribinated sheep blood.
MIC (mcg/mL)
Interpretation
≤0.12
(S) Susceptible
The absence of resistant neisserial strains precludes defining any categories other than "Susceptible". Strains yielding results suggestive of a "Nonsusceptible" category should be submitted to a reference laboratory for further testing.
When testing Staphylococcus aureus (methicillin-susceptible, MSSA) the following interpretive criteria should be applied:
MIC (mcg/mL)
Interpretation
≤4
(S) Susceptible
8
(I) Intermediate
≥16
(R) Resistant
For staphylococcal Infections, a daily dose of 2 to 4 grams should be administered to achieve >90% target attainment (see DOSAGE AND ADMINISTRATION).
The following interpretive criteria should be used when testing Streptococcus pneumoniae using Mueller-Hinton broth with 2 to 5% lysed horse blood.
Meningitis:
MIC (mcg/mL)
Interpretation
≤0.5
(S) Susceptible
1
(I) Intermediate
≥2
(R) Resistant
Non-meningitis infections:
MIC (mcg/mL)
Interpretation
≤1
(S) Susceptible
2
(I) Intermediate
≥4
(R) Resistant
For β-hemolytic streptococci the following interpretive criteria should be used when testing on cation-adjusted Mueller-Hinton broth with 2 to 5% lysed horse blood:
MIC (mcg/mL)
Interpretation
≤0.5
(S) Susceptible
For the Viridians Group streptococci the following interpretive criteria should be applied:
MIC (mcg/mL)
Interpretation
≤1
(S) Susceptible
2
(I) Intermediate
≥4
(R) Resistant
A report of "Susceptible" indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of "Intermediate" indicates that the results should be considered equivocal, and if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of the drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of the laboratory procedures. Standardized ceftriaxone powder should provide the following MIC values:
Microorganism
ATCC
MIC(mcg/mL)
Escherichia coli
25922
0.03 to 0.12
Staphylococcus aureus
29213
1 to 8
Pseudomonas aeruginosa
27853
8 to 64
Haemophilus influenzae
49247
0.06 to 0.25
Neisseria gonorrhoeae
49226
0.004 to 0.015
Streptococcus pneumoniae
49619
0.03 to 0.12
Diffusion Techniques: Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure3 requires the use of standardized inoculum concentrations. This procedure uses paper disc impregnated with 30 mcg of ceftriaxone to test the susceptibility of microorganisms to Ceftriaxone.
Reports from the laboratory providing results of the standard single disc susceptibility test with a 30 mcg ceftriaxone disc should be interpreted according to the following criteria for aerobic organisms:
For Enterobacteriaceae:
Zone Diameter (mm)
Interpretation
≥23
(S) Susceptible
20 to 22
(I) Intermediate
≤19
(R) Resistant
When testing Haemophilus influenzae on Haemophilus Test media (HTM), the following interpretive criteria should be used:
Zone Diameter (mm)
Interpretation
≥26
(S) Susceptible
The absence of resistant strains precludes defining any categories other than "Susceptible". Strains yielding results suggestive of a "Nonsusceptible" category should be submitted to a reference laboratory for further testing.
The following Interpretive criteria should be used when testing Neisseria gonorrhoeae when using GC agar base and 1 % defined growth supplement
Zone Diameter (mm)
Interpretation
≥35
(S) Susceptible
For Neisseria meningitidis, the following disc diffusion criteria apply:5
Zone Diameter (mm)
Interpretation
≥34
(S) Susceptible
For Staphylococcus aureus (methicillin-susceptible, MSSA), the following interpretive criteria apply:
Zone Diameter (mm)
Interpretation
≥21
(S) Susceptible
14 to 20
(I) Intermediate
≤13
(R) Resistant
The following interpretive criteria should be used when testing β-hemolytic streptococci using Mueller-Hinton agar supplemented with 5% sheep blood incubated in 5% C02
Zone Diameter (mm)
Interpretation
≥24
(S) Susceptible
For the Viridians Group streptococci the following criteria apply:
Zone Diameter (mm)
Interpretation
≥27
(S) Susceptible
25 to 26
(I)Intermediate
≤24
(R) Resistant
Interpretation should be as stated above for results using dilution techniques. Interpretation involves correlation of the diameter obtained in the disc test with the MIC for ceftriaxone.
Disc diffusion interpretative criteria for ceftriaxone discs against Streptococcus pneumoniae are not available; however, isolates of pneumococci with oxacillin zone diameters of >20 mm are susceptible (MIC ≤ 0.06 mcg/mL) to penicillin and can be considered susceptible to ceftriaxone.
Streptococcus pneumoniae isolates should not be reported as penicillin (ceftriaxone) resistant or intermediate based solely on an oxacillin zone diameter of ≤ 19 mm. The ceftriaxone MIC should be determined for those isolates with oxacillin zone diameters ≤ 19 mm.
As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms that are used to control the technical aspects of the laboratory procedures. For the diffusion technique, the 30 mcg ceftriaxone disc should provide the following zone diameters in these laboratory test quality control strains3.
Microorganism
ATCC
Zone Diameter Ranges (mm)
Escherichia coli
25922
29 to 35
Staphylococcus aureus
29213
22 to 28
Pseudomonas aeruginosa
27853
17 to 23
Haemophilus influenzae
49247
31 to 39
Neisseria gonorrhoeae
49226
39 to 51
Streptococcus pneumoniae
49619
30 to 35
Anaerobic Susceptibility Testing by Agar Dilution: For anaerobic bacteria, the susceptibility to ceftriaxone as MICs can be determined by standardized test methods6. The MIC values obtained should be interpreted according to the following criteria
MIC (mcg/mL)
Interpretation
≤16
(S) Susceptible
32
(I) Intermediate
≥64
(R) Resistant
As with other susceptibility techniques, the use of laboratory control microorganisms is required to control the technical aspects of the laboratory standardized procedures. Standardized ceftriaxone powder should provide the following MIC values for the indicated standardized anaerobic dilution6 testing method:
Method
Microorganism
ATCC® #
MIC (mcg/mL)
Agar
Bacteroides fragilis
25285
32 to 128
Bacteroides thetaiotaomicron
29741
64 to 256
-
INDICATIONS AND USAGE
Before instituting treatment with ceftriaxone, appropriate specimens should be obtained for isolation of the causative organism and for determination of its susceptibility to the drug. Therapy may be instituted prior to obtaining results of susceptibility testing.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of ceftriaxone and other antibacterial drugs, ceftriaxone should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria.
When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Ceftriaxone for injection, USP is indicated for the treatment of the following infections when caused by susceptible organisms:
LOWER RESPIRATORY TRACT INFECTIONS caused by Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella pneumoniae, Escherichia coli, Enterobacter aerogenes, Proteus mirabilis or Serratia marcescens.
ACUTE BACTERIAL OTTTIS MEDIA caused by Streptococcus pneumoniae, Haemophilus influenzae (including beta-lactamase producing strains) or Moraxella catarrhalis (including beta-lactamase producing strains)
NOTE: In one study lower clinical cure rates were observed with single dose of ceftriaxone compared to 10 days of oral therapy. In a second study comparable cure rates were observed between single dose ceftriaxone and the comparator. The potentially lower clinical cure rate of ceftriaxone should be balanced against the potential advantages of parenteral therapy (see CLINICAL STUDIES).
SKIN AND SKIN STRUCTURE INFECTIONS caused by Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus pyogenes, Viridans group streptococci, Escherichia coli, Enterobacter cloacae, Klebsiella oxytoca, Klebsiella pneumoniae, Proteus mirabilis, Morganella morganii*, Pseudomonas aeruginosa, Serratia marcescens, Acinetobacter calcoaceticus, Bacteroides fragilis* or Peptostreptococcus species.
URINARY TRACT INFECTIONS (complicated and uncomplicated) caused by Escherichia coli, Proteus mirabilis, Proteus vulgaris, Morganella morganii or Klebsiella pneumoniae.
UNCOMPLICATED GONORRHEA (cervical/urethral and rectal) caused by Neisseria gonorrhoeae, including both penicillinase- and nonpenicillinase-producing strains, and pharyngeal gonorrhea caused by nonpenicillinase-producing strains of Neisseria gonorrhoeae.
PELVIC INFLAMMATORY DISEASE caused by Neisseria gonorrhoeae. Ceftriaxone, like other cephalosporins, has no activity against Chlamydia trachomatis. Therefore, when cephalosporins are used in the treatment of patients with pelvic inflammatory disease and Chlamydia trachomatis is one of the suspected pathogens, appropriate antichlamydial coverage should be added.
BACTERIAL SEPTICEMIA caused by Staphylococcus aureus, Streptococcus pneumoniae, Escherichia coli, Haemophilus influenzae or Klebsiella pneumoniae.
BONE AND JOINT INFECTIONS caused by Staphylococcus aureus, Streptococcus pneumoniae, Escherichia coli, Proteus mirabilis, Klebsiella pneumoniae or Enterobacter species.
INTRA-ABDOMINAL INFECTIONS caused by Escherichia coli, Klebsiella pneumoniae, Bacteroides fragilis, Clostridium species (Note: most strains of Clostridium difficile are resistant) or Peptostreptococcus species.
MENINGITIS caused by Haemophilus influenzae, Neisseria meningitidis or Streptococcus pneumoniae. Ceftriaxone has also been used successfully in limited number of cases of meningitis and shunt infection caused by Staphylococcus epidermidis* and Escherichia coli.*
*Efficacy for this organism in this organ system was studied in fewer than ten infections.
SURGICAL PROPHYLAXIS: The preoperative administration of a single 1 g dose of ceftriaxone may reduce the incidence of postoperative infections in patients undergoing surgical procedures classified as contaminated or potentially contaminated (e.g. vaginal or abdominal hysterectomy or cholecystectomy for chronic calculous cholecystitis in high-risk patients, such as those over 70 years of age, with acute cholecystitis not requiring therapeutic antimicrobials, obstructive jaundice or common duct bile stones) and in surgical patients for whom infection at the operative site would present serious risk (e.g., during coronary artery bypass surgery).
Although ceftriaxone has been shown to have been as effective as cefazolin in the prevention of infection following coronary artery bypass surgery, no placebo-controlled trials have been conducted to evaluate any cephalosporin antibiotic in the prevention of infection following coronary artery bypass surgery.
When administered prior to surgical procedures for which it is indicated, a single 1 g dose of ceftriaxone provides protection from most infections due to susceptible organisms throughout the course of the procedure.
-
CONTRAINDICATIONS
Ceftriaxone is contraindicated in patients with known allergy to the cephalosporin class of antibiotics.
Neonates (≤28 days)
Hyperbilirubinemic neonates, especially prematures, should not be treated with ceftriaxone for injection. In vitro studies have shown that ceftriaxone can displace bilirubin from its binding to serum albumin, leading to a possible risk of bilirubin encephalopathy in these patients.
Ceftriaxone is contraindicated in neonates if they require (or are expected to require) treatment with calcium-containing IV solutions, including continuous calcium-containing infusions such as parenteral nutrition because of the risk of precipitation of ceftriaxone-calcium (see CLINICAL PHARMACOLOGY, WARNINGS and DOSAGE AND ADMINISTRATION).
A small number of cases of fatal outcomes in which a crystalline material was observed in the lungs and kidneys at autopsy have been reported in neonates receiving Ceftriaxone and calcium-containing fluids. In some of these cases, the same intravenous infusion line was used for both Ceftriaxone and calcium containing fluids and in some a precipitate was observed in the intravenous infusion line. At least one fatality has been reported in a neonate in whom Ceftriaxone and calcium-containing fluids were administered at different time points via different intravenous lines; no crystalline material was observed at autopsy in this neonate. There have been no similar reports in patients other than neonates.
-
WARNINGS
Hypersensitivity
BEFORE THERAPY WTTH CEFTRIAXONE IS INSTITUTED, CAREFUL INQUIRY SHOULD BE MADE TO DETERMINE WHETHER THE PATIENT HAS HAD PREVIOUS HYPERSENSITIVITY REACTIONS TO CEPHALOSPORINS, PENICILLINS OR OTHER DRUGS. THIS PRODUCT SHOULD BE GIVEN CAUTIOUSLY TO PENICILLIN-SENSITIVE PATIENTS. ANTIBIOTICS SHOULD BE ADMINISTERED WTTH CAUTION TO ANY PATIENT WHO HAS DEMONSTRATED SOME FORM OF ALLERGY PARTICULARLY TO DRUGS. SERIOUS ACUTE HYPERSENSITIVITY REACTIONS MAY REQUIRE THE USE OF SUBCUTANEOUS EPINEPHRINE AND OTHER EMERGENCY MEASURES.
As with other cephalosporins anaphylactic reactions with fatal outcome have been reported, even if a patient is not known to be allergic or previously exposed.
Interaction with Calcium-Containing Products
Do not use diluents containing calcium, such as Ringer’s solution or Hartmann’s solution, to reconstitute ceftriaxone vials or to further dilute a reconstituted vial for IV administration because a precipitate can form. Precipitation of ceftriaxone-calcium can also occur when ceftriaxone is mixed with calcium-containing solutions in the same IV administration line. Ceftriaxone must not be administered simultaneously with calcium-containing IV solutions, including continuous calcium-containing infusions such as parenteral nutrition via a Y-site. However, in patients other than neonates, ceftriaxone and calcium-containing solutions may be administered sequentially of one another if the infusion lines are thoroughly flushed between infusions with a compatible fluid. In vitro studies using adult and neonatal plasma from umbilical cord blood demonstrated that neonates have an increased risk of precipitation of ceftriaxone-calcium (see CLINICAL PHARMACOLOGY, CONTRAINDICATIONS AND DOSAGE AND ADMINISTRATION).
Clostridium difficile
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including ceftriaxone and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Hemolytic Anemia
An immune mediated hemolytic anemia has been observed in patients receiving cephalosporin class antibacterials including ceftriaxone. Severe cases of hemolytic anemia, including fatalities, have been reported during treatment in both adults and children. If a patient develops anemia while on ceftriaxone, the diagnosis of a cephalosporin associated anemia should be considered and ceftriaxone stopped until the etiology is determined.
-
PRECAUTIONS
General:
Prescribing ceftriaxone in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Although transient elevations of BUN and serum creatinine have been observed, at the recommended dosages, the nephrotoxic potential of ceftriaxone is similar to that of other cephalosporins.
Ceftriaxone is excreted via both biliary and renal excretion (see CLINICAL PHARMACOLOGY). Therefore, patients with renal failure normally require no adjustment in dosage when usual doses of ceftriaxone are administered.
Dosage adjustments should not be necessary in patients with hepatic dysfunction; however, in patients with both hepatic dysfunction and significant renal disease, caution should be exercised and the ceftriaxone dosage should not exceed 2 g daily.
Alterations in prothrombin times have occurred rarely in patients treated with ceftriaxone. Patients with impaired vitamin K synthesis or low vitamin K stores e.g., (chronic hepatic disease and malnutrition) may require monitoring of prothrombin time during ceftriaxone treatment. Vitamin K administration (10 mg weekly) may be necessary if the prothrombin time is prolonged before or during therapy.
Prolonged use of ceftriaxone may result in overgrowth of nonsusceptible organisms. Careful observation of the patient is essential.If superinfection occurs during therapy, appropriate measures should be taken.
Ceftriaxone should be prescribed with caution in individuals with history of gastrointestinal disease, especially colitis
There have been reports of sonographic abnormalities in the gallbladder of patients treated with ceftriaxone; some of these patients also had symptoms of gallbladder disease. These abnormalities appear on sonography as an echo without acoustical shadowing suggesting sludge or as an echo with acoustical shadowing which may be misinterpreted as gallstones. The chemical nature of the sonographically detected material has been determined to be predominantly a ceftriaxone-calcium salt. The condition appears to be transient and reversible upon discontinuation of ceftriaxone and institution of conservative management. Therefore, ceftriaxone should be discontinued in patients who develop signs and symptoms suggestive of gallbladder disease and/or the sonographic findings described above.
Cases of pancreatitis, possibly secondary to biliary obstruction, have been reported rarely in patients treated with ceftriaxone. Most patients presented with risk factors for biliary stasis and biliary sludge (preceding major therapy, severe illness, total parenteral nutrition). A cofactor role of ceftriaxone-related biliary precipitation cannot be ruled out.
Information for Patients:
Patients should be counseled that antibacterial drugs including ceftriaxone should only be used to treat bacterial infections. They do not treat viral infections (e.g. common cold).
When ceftriaxone is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by ceftriaxone or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
Carcinogenesis: Considering the maximum duration of treatment and the class of the compound, carcinogenicity studies with ceftriaxone in animals have not been performed. The maximum duration of animal toxicity studies was 6 months.
Mutagenesis: Genetic toxicology tests included the Ames test, a micronucleus test and a test for chromosomal aberrations in human lymphocytes cultured in vitro with ceftriaxone. Ceftriaxone showed no potential for mutagenic activity in these studies.
Impairment of Fertility: Ceftriaxone produced no impairment of fertility when given intravenously to rats at daily doses up to 586 mg/kg/day, approximately 20 times the recommended clinical dose of 2 g/day.
Pregnancy:
Teratogenic Effects: Pregnancy Category B. Reproductive studies have been performed in mice and rats at doses up to 20 times the usual human dose and have no evidence of embryotoxicity, fetotoxicity or teratogenicity. In primates, no embryotoxicity or teratogenicity was demonstrated at a dose approximately 3 times the human dose.
There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproductive studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Nonterafogenic Effects: In rats, in the Segment I (fertility and general reproduction) and Segment III (perinatal and postnatal) studies with intravenously administered ceftriaxone, no adverse effects were noted on various reproductive parameters during gestation and lactation, including postnatal growth, functional behavior and reproductive ability of the offspring, at doses of 586 mg/kg/day or less.
Nursing Mothers:
Low concentrations of ceftriaxone are excreted in human milk. Caution should be exercised when ceftriaxone is administered to a nursing woman.
Pediatric Use:
Safety and effectiveness of ceftriaxone in neonates, infants and pediatric patients have been established for the dosages described in the DOSAGE AND ADMINISTRATION section. In vitro studies have shown that ceftriaxone, like some other cephalosporins, can displace bilirubin from serum albumin. Ceftriaxone should not be administered to hyperbilirubinemic neonates, especially prematures (see CONTRAINDICATIONS).
Geriatric Use:
Of the total number of subjects in clinical studies of ceftriaxone, 32% were 60 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
The pharmacokinetics of ceftriaxone were only minimally altered in geriatric patients compared to healthy adult subjects and dosage adjustments are not necessary for geriatric patients with ceftriaxone dosages up to a 2 grams per day (see CLINICAL PHARMACOLOGY).
-
ADVERSE REACTIONS
Ceftriaxone is generally well tolerated. In clinical trials, the following adverse reactions, which were considered to be related to ceftriaxone therapy or of uncertain etiology, were observed.
LOCAL REACTIONS- pain, induration and tenderness was 1% overall. Phlebitis was reported in < 1% after IV administration. The incidence of warmth, tightness or induration was 17% (3/17) after IM administration of 350 mg/mL and 5% (1/20) after IM administration of 250 mg/mL.
HYPERSENSITIVITY- rash (1.7%). Less frequently reported (<1 %) were pruritis, fever or chills.
HEMATOLOGIC – eosinophilia (6%), thrombocytosis (5.1%) and leukopenia (2.1%). Less frequently reported (<1%) were anemia, hemolytic anemia, neutropenia, lymphopenia, thrombocytopenia and prolongation of the prothrombin time.
GASTROINTESTINAL - diarrhea (2.7%). Less frequently reported (<1 %) were nausea or vomiting, and dysgeusia. The onset of pseudomembranous colitis symptoms may occur during or after antibacterial treatment (see WARNINGS).
HEPATIC- elevations of SGOT (3.1%) or SGPT (3.3%). Less frequently reported (<1%) were elevations of alkaline phosphatase and bilirubin.
RENAL - elevations of the BUN (1.2%). Less frequently reported (<1 %) were elevations of creatinine and the presence of casts in the urine.
CENTRAL NERVOUS SYSTEM - headache or dizziness were reported occasionally (<1 %).
GENITOURINARY- moniliasis or vaginitis were reported occasionally (<1 %).
MISCELLANEOUS- diaphoresis and flushing were reported occasionally (<1 %)
Other rarely observed adverse reactions (<0.1%) include abdominal pain, agranulocytosis, allergic pneumonitis, anaphylaxis, basophilia, biliary lithiasis, bronchospasm, colitis, dyspepsia, epistaxis, flatulence, gallbladder sludge, glycosuria, hematuria, jaundice, leukocytosis, lymphocytosis, monocytosis, nephrolithiasis, palpitations, a decrease in the prothrombin time, renal precipitations, seizures, and serum sickness.
Postmarketing Experience: In addition to the adverse reactions reported during clinical trials, the following adverse experiences have been reported during clinical practice in patients treated with ceftriaxone. Data are generally insufficient to allow an estimate of incidence or to establish causation.
A small number of cases of fatal outcomes in which a crystalline material was observed in the lungs and kidneys at autopsy have been reported in neonates receiving ceftriaxone and calcium-containing fluids. In some of these cases, the same intravenous infusion line was used for both ceftriaxone and calcium-containing fluids and in some a precipitate was observed in the intravenous infusion line. At least one fatality has been reported in a neonate in whom ceftriaxone and calcium-containing fluids were administered at different time points via different intravenous lines; no crystalline material was observed at autopsy in this neonate. There have been no similar reports in patients other than neonates.
GASTROINTESTINAL – stomatitis and glossitis.
GENITOURINARY – oliguria.
DERMATOLOGIC – exanthema, allergic dermatitis, urticaria, edema. As with many medications, isolated cases of severe cutaneous adverse reactions (erythema multiforme, Stevens-Johnson syndrome or Lyell’s syndrome/toxic epidermal necrolysis) have been reported.
Cephalosporin Class Adverse Reactions
In addition to the adverse reactions listed above which have been observed in patients treated with ceftriaxone, the following adverse reactions and altered laboratory test results have been reported for cephalosporin class antibiotics:
Adverse Reactions: Allergic reactions, drug fever, serum sickness-like reaction, renal dysfunction, toxic nephropathy, reversible hyperactivity, hypertonia, hepatic dysfunction including cholestasis, aplastic anemia, hemorrhage, and superinfection.
Altered Laboratory Tests: Positive direct Coombs' test, false-positive test for urinary glucose, and elevated LDH.
Several cephalosporins have been implicated in triggering seizures, particularly in patients with renal impairment when the dosage was not reduced (see DOSAGE AND ADMINISTRATION). If seizures associated with drug therapy occur, the drug should be discontinued. Anticonvulsant therapy can be given if clinically indicated.
- OVERDOSAGE
-
DOSAGE AND ADMINISTRATION
Ceftriaxone may be administered intravenously or intramuscularly.
Do not use diluents containing calcium, such as Ringer’s solution or Hartmann’s solution, to reconstitute ceftriaxone vials or to further dilute a reconstituted vial for IV administration because a precipitate can form. Precipitation of ceftriaxone-calcium can also occur when ceftriaxone is mixed with calcium-containing solutions in the same IV administration line.
Ceftriaxone must not be administered simultaneously with calcium-containing IV solutions, including continuous calcium-containing infusions such as parenteral nutrition via a Y-site. However, in patients other than neonates, ceftriaxone and calcium-containing solutions may be administered sequentially of one another if the infusion lines are thoroughly flushed between infusions with a compatible fluid (see WARNINGS).
There have been no reports of an interaction between ceftriaxone and oral calcium containing products or interaction between intramuscular ceftriaxone and calcium containing products (IV or oral).
NEONATES
Hyperbilirubinemic neonates, especially prematures, should not be treated with ceftriaxone (see CONTRAINDICATIONS).
Ceftriaxone is contraindicated in neonates if they require (or are expected to require) treatment with calcium-containing IV solutions, including continuous calcium-containing infusions such as parenteral nutrition because of the risk of precipitation of ceftriaxone-calcium (see CONTRAINDICATIONS)
PEDIATRIC PATIENTS: For the treatment of skin and skin structure infections, the recommended total daily dose is 50 to 75 mg/kg given once a day (or in equally divided doses twice a day). The total daily dose should not exceed 2 grams.
For the treatment of acute bacterial otitis media, a single intramuscular dose of 50 mg/kg (not to exceed 1 gram) is recommended (see INDICATIONS AND USAGE).
For the treatment of serious miscellaneous infections, other than meningitis, the recommended total daily dose is 50 to 75 mg/kg, given in divided doses every 12 hours. The total daily dose should not exceed 2 grams.
In the treatment of meningitis, it is recommended that the initial therapeutic dose be 100 mg/kg (not to exceed 4 grams). Thereafter, a total daily dose of 100 mg/kg/day (not to exceed 4 grams daily) is recommended. The daily dose may be administered once a day (or in equally divided doses every 12 hours). The usual duration of therapy is 7 to 14 days.
ADULTS: The usual daily dose is 1 to 2 grams given once a day (or in equally divided doses twice a day) depending on the type and severity of infection. For infections caused by Staphylococcus aureus (MSSA), the recommended daily dose is 2 to 4 grams, in order to achieve >90% target attainment. The total daily dose should not exceed 4 grams.
If Chlamydia trachomatis is a suspected pathogen, appropriate antichlamydial coverage should be added, because ceftriaxone sodium has no activity against this organism.
For the treatment of uncomplicated gonococcal infections, a single intramuscular dose of 250 mg is recommended.
For preoperative use (surgical prophylaxis), a single dose of 1 gram administered intravenously 1/2 to 2 hours before surgery is recommended.
Generally, ceftriaxone therapy should be continued for at least 2 days after the signs and symptoms of infection have disappeared. The usual duration of therapy is 4 to 14 days; in complicated infections, longer therapy may be required.
When treating infections caused by Streptococcus pyogenes, therapy should be continued for at least 10 days.
No dosage adjustment is necessary for patients with impairment of renal or hepatic function.
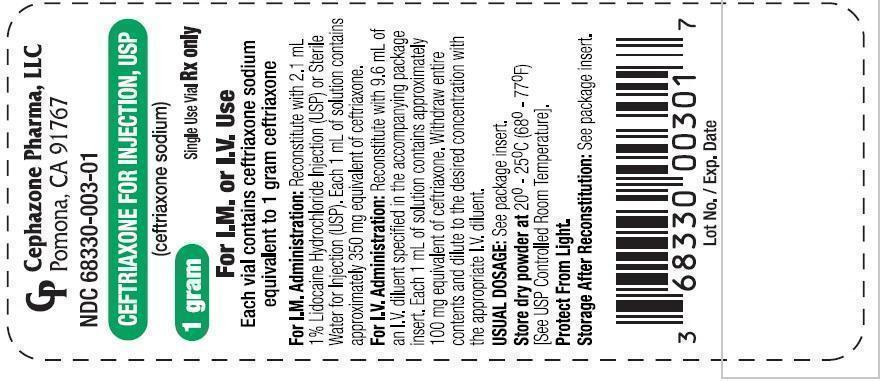
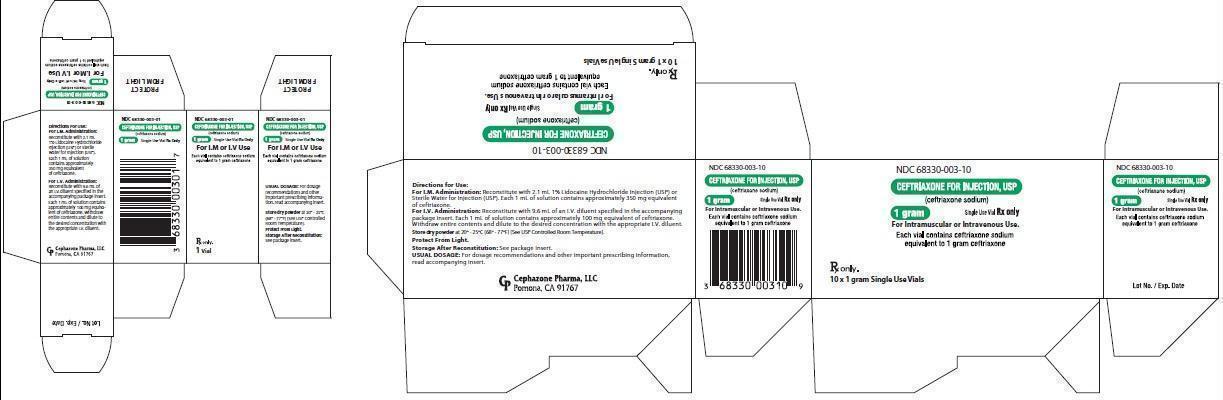
DIRECTIONS FOR USE:
Intramuscular Administration: Reconstitute ceftriaxone powder with the appropriate diluent (see COMPATIBILITY AND STABILITY).
Inject diluent into vial, shake vial thoroughly to form solution. Withdraw entire contents of vial into syringe to equal total labeled dose.
After reconstitution, each 1 mL of solution contains approximately 250 mg or 350 mg equivalent of ceftriaxone according to the amount of diluent indicated below. If required, more dilute solutions could be utilized. A 350 mg/mL concentration is not recommended for the 250 mg vial since it may not be possible to withdraw the entire contents.
As with all intramuscular preparations, ceftriaxone should be injected well within the body of a relatively large muscle; aspiration helps to avoid unintentional injection into a blood vessel.
Vial Dosage Size
Amount of Diluent to be added
250 mg/mL
350 mg/mL
250 mg
0.9 mL
--------
500 mg
1.8 mL
1.0 mL
1 g
3.6 mL
2.1 mL
2 g
7.2 mL
4.2 mL
Intravenous Administration: Ceftriaxone should be administered intravenously by infusion over a period of 30 minutes. Concentrations between 10 mg/mL and 40 mg/mL are recommended; however, lower concentrations may be used if desired, reconstitute vials or "piggyback" bottles with an appropriate IV diluent (See COMPATIBILITY AND STABILITY).
Vial Dosage Size
Amount of Diluent to be added
250 mg
2.4 mL
500 mg
4.8 mL
1 g
9.6 mL
2 g
19.2 mL
After reconstitution, each 1 mL of solution contains approximately 100 mg equivalent of ceftriaxone. Withdraw entire contents and dilute to the desired concentration with the appropriate IV diluent.
Piggyback Bottle Dosage Size
Amount of Diluent to be added
1 g
10 mL
2 g
20 mL
After reconstitution, further dilute to 50 mL or 100 mL volumes with the appropriate IV diluent.
COMPATIBILITY AND STABILITY: Ceftriaxone has been shown to be compatible with Flagyl® IV (metronidazole hydrochloride). The concentration should not exceed 5 to 7.5 mg/mL metronidazole hydrochloride with ceftriaxone 10 mg/mL as an admixture.
The admixture is stable for 24 hours at room temperature only in 0.9% sodium chloride injection or 5% dextrose in water (D5W). No compatibility studies have been conducted with the Flagyl® IV RTU® (metronidazole) formulation or using other diluents. Metronidazole at concentrations greater than 8 mg/mL will precipitate. Do not refrigerate the admixture as precipitation will occur.
Vancomycin, amsacrine, aminoglycosides, and fluconazole are physically incompatible with ceftriaxone in admixtures. When any of these drugs are to be administered concomitantly with ceftriaxone by intermittent intravenous infusion, it is recommended that they be given sequentially, with thorough flushing of the intravenous lines (with one of the compatible fluids) between the administrations.
Do not use diluents containing calcium, such as Ringer's solution or Hartmann's solution, to reconstitute ceftriaxone vials or to further dilute a reconstituted vial for IV administration. Particulate formation can result.
Ceftriaxone for injection solutions should not be physically mixed with or piggybacked into solutions containing other antimicrobial drugs or into diluent solutions other than those listed above, due to possible incompatibility (see WARNINGS).
Ceftriaxone for injection should be stored at 20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature] and protected from light. After reconstitution, protection from normal light is not necessary. The color of solution ranges from light yellow to amber, depending on the lenght of storage, concentration and diluent used.
Ceftriaxone intramuscular solution remain stable (loss of potency less than 10%) for the following time periods:
Diluent
Concentration
Storage
mg/mL
Room Temp. (25°C)
Refrigerated (4°C)
Sterile Water for Injection
100,
2 days
10 days
250,350
24 hours
3 days
0.9% Sodium Chloride
Solution
100,
2 days
10 days
250,350
24 hours
3 days
5% Dextrose Solution
100,
2 days
10 days
250,350
24 hours
3 days
Bacteriostatic Water + 0.9%
Benzyl Alcohol
100,
24 hours
10 days
250,350
24 hours
3 days
1 % Lidocaine Solution
(without epinephrine)
100,
24 hours
10 days
250,350
24 hours
3 days
Ceftriaxone intravenous solutions, at concentrations of 10, 20 and 40 mg/mL, remain stable (loss potency less than 10%) for the following time periods stored in glass or PVC containers.
- *
- Data available for 10 to 40 mg/mL concentrations in this diluent in PVC containers only.
Diluent
Storage
Room Temp. (25°C)
Refrigerated (4°C)
Sterile Water
2 days
10 days
0.9% Sodium Chloride Solution
2 days
10 days
5% Dextrose Solution
2 days
10 days
10% Dextrose Solution
2 days
10 days
5% Dextrose+0.9% Sodium Chloride Solution*
2 days
Incompatible
5% Dextrose + 0.45% Sodium Chloride Solution
2 days
Incompatible
The following intravenous ceftriaxone solutions are stable at room temperature (25°C) for 24 hours, at concentrations between 10 mg/mL and 40 mg/mL: Sodium Lactate (PVC Container), 10% Invert Sugar (glass container), 5% Sodium Bicarbonate (glass container), Freamine III (glass container), Normosol-M in 5% Dextrose (glass and PVC containers), Ionosol-B in 5% Dextrose (glass container), 5% Mannitol (glass container), 10% Mannitol (glass container).
After the indicated stability time periods, unused portions of solutions should be discarded.
NOTE: Parenteral drug products should be inspected visually for particulate matter before administration.
Ceftriaxone reconstituted with 5% Dextrose or 0.9% Sodium Chloride solution at concentrations between 10 mg/mL and 40 mg/mL, and then stored in frozen state (-20°C) in PVC or polyolefin containers, remains stable for 26 weeks.
Frozen solutions of ceftriaxone for injection should be thawed at room temperature before use. After thawing, unused portions should be discarded. DO NOT REFREEZE.
-
ANIMAL PHARMACOLOGY:
Concretions consisting of the precipitated calcium salt of ceftriaxone have been found in the gallbladder bile of dogs and baboons treated with ceftriaxone.
These appeared as a gritty sediment in dogs that received 100 mg/kg/day for 4 weeks. A similar phenomenon has been observed in baboons but only after a protracted dosing period (6 months) at higher dose levels (335 mg/kg/day or more). The likelihood of this occurrence in humans is considered to be low, since ceftriaxone has a greater plasma half life in humans, the calcium salt of ceftriaxone is more soluble in human gallbladder bile and the calcium content of human gallbladder bile is relatively low.
-
HOW SUPPLIED
Ceftriaxone for Injection, USP is available as a sterile crystalline powder in glass vials and piggyback bottles. The following packages are available:
Vials containing 250 mg equivalent of ceftriaxone. Box of 1 (NDC No. 68330-001 -01) and box of 10 (NDC No. 68330-001-10)
Vials containing 500 mg equivalent of ceftriaxone. Box of 1 (NDC No. 68330-002-01) and box of 10 (NDC No. 68330-002-10)
Vials containing 1 g equivalent of ceftriaxone. Box of 1 (NDC No.68330-003-01) and box of 10 (NDC No. 68330-003-10)
Vials containing 2 g equivalent of ceftriaxone. Box of 1 (NDC No.68330-004-01) and box of 10 (NDC No. 68330-004-10)
Piggyback bottles containing 1 g equivalent of ceftriaxone. Box of 1 (NDC No.68330-005-01) and box of 10(NDC NO. 68330-005-10)
Piggyback bottles containing 2 g equivalent of ceftriaxone. Box of 1 (NDC No. 68330-006-01) and box of 10(NDC No. 68330-006-10)
NOTE: Ceftriaxone for injection, USP should be stored at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature] and protected from light.
-
CLINICAL STUDIES
Clinical Trials in Pediatric Patients With Acute Bacterial Otitis Media: In two adequate and well-controlled U.S. clinical trials, a single IM dose of ceftriaxone was compared with a 10 day course of oral antibiotic in pediatric patients between the ages of 3 months and 6 years. The clinical cure rates and statistical outcome appear in the table below:
Clinical Efficacy in Evaluable Population
Study Day
Ceftriaxone
Single Dose
Comparator – 10 days
of Oral Therapy
95% Confidence
Interval
Statistical Outcome
Study 1 –U.S.
14
28
74% (220/296)
58% (167/288)
Amoxicillin/Clavulanate
82% (274/302)
67% (200/297)
(-14.4%, -0.5%)
(-17.5%, -1.2%)
Ceftriaxone is lower than control
at study day 14 and 28
Study 2 – U.S.7
14
28
54%(113/210)
35% (73/206)
TMP-SMZ
60% (124/206)
45%(93/205)
(-16.4%, 3.6%)
(-19.9%, 0.0%)
Ceftriaxone is equivalent to
control at study day 14 and 28
An open-label bacteriologic study of ceftriaxone without a comparator enrolled 108 pediatric patients, 79 of whom had positive baseline cultures for one or more of the common pathogens. The results of this study are tabulated as follows:
Week 2 and 4 Bacteriologic Eradication Rates in the Per Protocol Analysis in the Roche Bacteriologic Study by pathogen:
Study Day
13-15
Study Day
30+2
Organism
No. Analyzed
No. Erad (%)
No. Analyzed
No. Erad (%)
Streptococcus pneumoniae
38
32 (84)
35
25 (71)
Haemophilus influenzae
33
28 (85)
31
22 (71)
Moraxella catarrhalis
15
12 (80)
15
9 (60)
-
REFERENCES
- Clinical and Laboratory Standards Institute (CLSI). Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard - Eighth Edition. CLSI document M07-A8. CLSI, 940 West Valley Road, Suite 1400, Wayne, PA 19087, 2009.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing; Twentieth Informational Supplement. CLSI document M100-S20. CLSI, 940 West Valley Road, Suite 1400, Wayne, PA 19087, 2010.
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard - Tenth Edition. CLSI document M02-A10. CLSI, 940 West Valley Road, Suite 1400, Wayne, PA 19087, 2009.
- Burgess DS, Frei CR, Lewis II JS, et al. The contribution of pharmokinetic-pharmacodynamic modeling with Monte Carlo simulation to the development of susceptibility breakpoints for Neisseria meningitidis. Clin Microbiol Infect. 2007; 13:33-39.
- Jorgenson JH, Crawford SA, Fulcher LC, et al. Multilaboratory evaluation of disk diffusion antimicrobial susceptibility testing of Neisseria meningitides isolates. J Clin Microbiol. 2006;44(5):1744-1754.
- Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Susceptibility Testing of Anaerobic Bacteria; Approved Standard - Seventh Edition. CLSI document M11-A7. CLSI, 940 West Valley Road, Suite 1400, Wayne, PA 19087, 2007.
- Barnett ED, Teele DW, Klein JO, et al. Comparison of Ceftriaxone and Trimethoprim-Sulfamethoxazole for Acute Otitis Media. Pediatrics. Vol. 99, No.1, January 1997.
- SPL UNCLASSIFIED SECTION
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
CEFTRIAXONE
ceftriaxone injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68330-001 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFTRIAXONE SODIUM (UNII: 023Z5BR09K) (CEFTRIAXONE - UNII:75J73V1629) CEFTRIAXONE 250 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68330-001-10 10 in 1 CARTON 1 NDC:68330-001-01 1 in 1 BOX 1 1 in 1 VIAL, GLASS Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065294 07/15/2008 CEFTRIAXONE
ceftriaxone injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68330-002 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFTRIAXONE SODIUM (UNII: 023Z5BR09K) (CEFTRIAXONE - UNII:75J73V1629) CEFTRIAXONE 500 mg Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68330-002-10 10 in 1 CARTON 1 NDC:68330-002-01 1 in 1 BOX 1 1 in 1 VIAL, GLASS Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065294 07/15/2008 CEFTRIAXONE
ceftriaxone injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68330-003 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFTRIAXONE SODIUM (UNII: 023Z5BR09K) (CEFTRIAXONE - UNII:75J73V1629) CEFTRIAXONE 1 g Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68330-003-10 10 in 1 CARTON 1 NDC:68330-003-01 1 in 1 BOX 1 1 in 1 VIAL, GLASS Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065294 07/15/2008 CEFTRIAXONE
ceftriaxone injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68330-004 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFTRIAXONE SODIUM (UNII: 023Z5BR09K) (CEFTRIAXONE - UNII:75J73V1629) CEFTRIAXONE 2 g Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68330-004-10 10 in 1 CARTON 1 NDC:68330-004-01 1 in 1 BOX 1 1 in 1 VIAL, GLASS Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065294 07/15/2008 CEFTRIAXONE
ceftriaxone injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68330-005 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFTRIAXONE SODIUM (UNII: 023Z5BR09K) (CEFTRIAXONE - UNII:75J73V1629) CEFTRIAXONE 1 g Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68330-005-10 10 in 1 CARTON 1 NDC:68330-005-01 1 in 1 BOX 1 1 in 1 VIAL, PIGGYBACK Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065294 07/15/2008 CEFTRIAXONE
ceftriaxone injection, powder, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68330-006 Route of Administration INTRAMUSCULAR, INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CEFTRIAXONE SODIUM (UNII: 023Z5BR09K) (CEFTRIAXONE - UNII:75J73V1629) CEFTRIAXONE 2 g Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68330-006-10 10 in 1 CARTON 1 NDC:68330-006-01 1 in 1 BOX 1 1 in 1 VIAL, PIGGYBACK Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA065294 07/15/2008 Labeler - Cephazone Pharma LLC (138954909)