Label: CLOPIDOGREL tablet, film coated
-
Contains inactivated NDC Code(s)
NDC Code(s): 55648-314-00, 55648-314-01, 55648-314-02, 55648-314-03, view more55648-314-04, 55648-315-00, 55648-315-01, 55648-315-02, 55648-315-04 - Packager: Wockhardt Limited
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated November 13, 2012
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use clopidogrel safely and effectively. See full prescribing information for clopidogrel.
Clopidogrel Tablets, USP
Initial U.S. Approval: 1997WARNING: DIMINISHED EFFECTIVENESS IN POOR
METABOLIZERS
See full prescribing information for complete boxed warning.
- Effectiveness of clopidogrel depends on activation to an active metabolite by the cytochrome P450 (CYP) system, principally CYP2C19. (5.1)
- Poor metabolizers treated with clopidogrel at recommended doses exhibit higher cardiovascular event rates following acute coronary syndrome (ACS) or percutaneous coronary intervention (PCI) than patients with normal CYP2C19 function. (12.5)
- Tests are available to identify a patient's CYP2C19 genotype and can be used as an aid in determining therapeutic strategy. (12.5)
- Consider alternative treatment or treatment strategies in patients identified as CYP2C19 poor metabolizers. (2.3, 5.1)
INDICATIONS AND USAGE
Clopidogrel is a P2Y12 platelet inhibitor indicated for:
● Acute coronary syndrome
- For patients with non-ST-segment elevation ACS [unstable angina (UA)/non-ST-elevation myocardial infarction (NSTEMI)] including patients who are to be managed medically and those who are to be managed with coronary revascularization, clopidogrel tablets has been shown to decrease the rate of a combined endpoint of cardiovascular death, myocardial infarction (MI), or stroke as well as the rate of a combined endpoint of cardiovascular death, MI, stroke, or refractory ischemia. (1.1)
- For patients with ST-elevation myocardial infarction (STEMI), clopidogrel tablets has been shown to reduce the rate of death from any cause and the rate of a combined endpoint of death, re-infarction, or stroke. The benefit for patients who undergo primary PCI is unknown. (1.1)
● Recent myocardial infarction (MI), recent stroke, or established peripheral arterial disease. Clopidogrel tablets has been shown to reduce the combined endpoint of new ischemic stroke (fatal or not), new MI (fatal or not), and other vascular death. (1.2)
DOSAGE AND ADMINISTRATION
● Acute coronary syndrome (2.1)
- Non-ST-segment elevation ACS (UA/NSTEMI): 300 mg loading dose followed by 75 mg once daily, in combination with aspirin (75-325 mg once daily)
- STEMI: 75 mg once daily, in combination with aspirin (75-325 mg once daily), with or without a loading dose and with or without thrombolytics
● Recent MI, recent stroke, or established peripheral arterial disease: 75 mg once daily (2.2)
DOSAGE FORMS AND STRENGTHS
Tablets: 75 mg, 300 mg (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Reduced effectiveness in impaired CYP2C19 function: Avoid concomitant use with omeprazole or esomeprazole. (5.1)
- Bleeding: Clopidogrel increases risk of bleeding. Discontinue 5 days prior to elective surgery. (5.2)
- Discontinuation of clopidogrel: Premature discontinuation increases risk of cardiovascular events. (5.3)
- Recent transient ischemic attack or stroke: Combination use of clopidogrel and aspirin in these patients was not shown to be more effective than clopidogrel alone, but was shown to increase major bleeding. (5.4)
- Thrombotic thrombocytopenic purpura (TTP): TTP has been reported with clopidogrel, including fatal cases. (5.5)
ADVERSE REACTIONS
Bleeding, including life-threatening and fatal bleeding, is the most commonly reported adverse reaction. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Wockhardt USA LLC. at 1-800-346-6854 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
USE IN SPECIFIC POPULATIONS
Nursing mothers: Discontinue drug or nursing, taking into consideration importance of drug to mother. (8.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2012
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: DIMINISHED EFFECTIVENESS IN POOR METABOLIZERS
1. INDICATIONS AND USAGE
1.1 Acute Coronary Syndrome (ACS)
1.2 Recent MI, Recent Stroke, or Established Peripheral Arterial Disease
2. DOSAGE AND ADMINISTRATION
2.1 Acute Coronary Syndrome
2.2 Recent MI, Recent Stroke, or Established Peripheral Arterial Disease
2.3 CYP2C19 Poor Metabolizers
2.4 Use with Proton Pump Inhibitors (PPI)
3. DOSAGE FORMS AND STRENGTHS
4. CONTRAINDICATIONS
4.1 Active Bleeding
4.2 Hypersensitivity
5. WARNINGS AND PRECAUTIONS
5.1 Diminished Antiplatelet Activity Due to Impaired CYP2C19 Function
5.2 General Risk of Bleeding
5.3 Discontinuation of Clopidogrel
5.4 Patients with Recent Transient Ischemic Attack (TIA) or Stroke
5.5 Thrombotic Thrombocytopenic Purpura (TTP)
6. ADVERSE REACTIONS
6.1 Clinical Studies Experience
6.2 Postmarketing Experience
7. DRUG INTERACTIONS
7.1 CYP2C19 Inhibitors
7.2 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
7.3 Warfarin (CYP2C9 Substrates)
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
10. OVERDOSAGE
11. DESCRIPTION
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 12.4
12.5 Pharmacogenomics
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
14. CLINICAL STUDIES
14.1 Acute Coronary Syndrome
14.2 Recent Myocardial Infarction, Recent Stroke, or Established Peripheral Arterial Disease
14.3 Lack of Established Benefit of Clopidogrel plus Aspirin in Patients with Multiple Risk Factors or Established Vascular Disease
16. HOW SUPPLIED/STORAGE AND HANDLING
17. PATIENT COUNSELING INFORMATION
17.1 Benefits and Risks
17.2 Bleeding
17.3 Other Signs and Symptoms Requiring Medical Attention
17.4 Invasive Procedures
17.5 Concomitant Medications
17.6 Medication Guide
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: DIMINISHED EFFECTIVENESS IN POOR METABOLIZERS
The effectiveness of clopidogrel is dependent on its activation to an active metabolite by the cytochrome P450 (CYP) system, principally CYP2C19 [see Warnings and Precautions (5.1)]. Clopidogrel at recommended doses forms less of that metabolite and has a smaller effect on platelet function in patients who are CYP2C19 poor metabolizers. Poor metabolizers with acute coronary syndrome or undergoing percutaneous coronary intervention treated with clopidogrel at recommended doses exhibit higher cardiovascular event rates than do patients with normal CYP2C19 function. Tests are available to identify a patient's CYP2C19 genotype; these tests can be used as an aid in determining therapeutic strategy [see Clinical Pharmacology (12.5)]. Consider alternative treatment or treatment strategies in patients identified as CYP2C19 poor metabolizers [see Dosage and Administration (2.3)].
-
1. INDICATIONS AND USAGE
1.1 Acute Coronary Syndrome (ACS)
- For patients with non-ST-segment elevation ACS [unstable angina (UA)/non-ST-elevation myocardial infarction (NSTEMI)], including patients who are to be managed medically and those who are to be managed with coronary revascularization, clopidogrel tablet has been shown to decrease the rate of a combined endpoint of cardiovascular death, myocardial infarction (MI), or stroke as well as the rate of a combined endpoint of cardiovascular death, MI, stroke, or refractory ischemia.
- For patients with ST-elevation myocardial infarction (STEMI), clopidogrel tablet has been shown to reduce the rate of death from any cause and the rate of a combined endpoint of death, re-infarction, or stroke. The benefit for patients who undergo primary percutaneous coronary intervention is unknown.
The optimal duration of clopidogrel tablets therapy in ACS is unknown.
1.2 Recent MI, Recent Stroke, or Established Peripheral Arterial Disease
For patients with a history of recent myocardial infarction (MI), recent stroke, or established peripheral arterial disease, clopidogrel tablet has been shown to reduce the rate of a combined endpoint of new ischemic stroke (fatal or not), new MI (fatal or not), and other vascular death.
-
2. DOSAGE AND ADMINISTRATION
2.1 Acute Coronary Syndrome
Clopidogrel tablets can be administered with or without food [see Clinical Pharmacology (12.3)]
- For patients with non-ST-elevation ACS (UA/NSTEMI), initiate clopidogrel tablets with a single 300 mg oral loading dose and then continue at 75 mg once daily. Initiate aspirin (75-325 mg once daily) and continue in combination with clopidogrel tablets [see Clinical Studies (14.1)].
- For patients with STEMI, the recommended dose of clopidogrel tablet is 75 mg once daily orally, administered in combination with aspirin (75-325 mg once daily), with or without thrombolytics. Clopidogrel tablets may be initiated with or without a loading dose [see Clinical Studies (14.1)].
2.2 Recent MI, Recent Stroke, or Established Peripheral Arterial Disease
The recommended daily dose of clopidogrel tablet is 75 mg once daily orally, with or without food [see Clinical Pharmacology (12.3)].
2.3 CYP2C19 Poor Metabolizers
CYP2C19 poor metabolizer status is associated with diminished antiplatelet response to clopidogrel. Although a higher dose regimen in poor metabolizers increases antiplatelet response [see Clinical Pharmacology (12.5)], an appropriate dose regimen for this patient population has not been established.
2.4 Use with Proton Pump Inhibitors (PPI)
Avoid using omeprazole or esomeprazole with clopidogrel. Omeprazole and esomeprazole significantly reduce the antiplatelet activity of clopidogrel. When concomitant administration of a PPI is required, consider using another acid-reducing agent with minimal or no CYP2C19 inhibitory effect on the formation of clopidogrel active metabolite [see Warnings and Precautions (5.1), Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
- 3. DOSAGE FORMS AND STRENGTHS
-
4. CONTRAINDICATIONS
4.1 Active Bleeding
Clopidogrel is contraindicated in patients with active pathological bleeding such as peptic ulcer or intracranial hemorrhage.
4.2 Hypersensitivity
Clopidogrel is contraindicated in patients with hypersensitivity (e.g., anaphylaxis) to clopidogrel or any component of the product [see Adverse Reactions (6.2)].
-
5. WARNINGS AND PRECAUTIONS
5.1 Diminished Antiplatelet Activity Due to Impaired CYP2C19 Function
Clopidogrel is a prodrug. Inhibition of platelet aggregation by clopidogrel is achieved through an active metabolite. The metabolism of clopidogrel to its active metabolite can be impaired by genetic variations in CYP2C19 [see Boxed Warning] and by concomitant medications that interfere with CYP2C19.
Proton Pump Inhibitors
Avoid concomitant use of clopidogrel with omeprazole or esomeprazole because both significantly reduce the antiplatelet activity of clopidogrel [see Drug Interactions (7.1) and Dosage and Administration (2.4)].
5.2 General Risk of Bleeding
Thienopyridines, including clopidogrel, increase the risk of bleeding. If a patient is to undergo surgery and an antiplatelet effect is not desired, discontinue clopidogrel five days prior to surgery. In patients who stopped therapy more than five days prior to CABG the rates of major bleeding were similar (event rate 4.4% clopidogrel + aspirin; 5.3% placebo + aspirin). In patients who remained on therapy within five days of CABG, the major bleeding rate was 9.6% for clopidogrel + aspirin, and 6.3% for placebo + aspirin.
Thienopyridines inhibit platelet aggregation for the lifetime of the platelet (7-10 days), so withholding a dose will not be useful in managing a bleeding event or the risk of bleeding associated with an invasive procedure. Because the half-life of clopidogrel’s active metabolite is short, it may be possible to restore hemostasis by administering exogenous platelets; however, platelet transfusions within 4 hours of the loading dose or 2 hours of the maintenance dose may be less effective.
5.3 Discontinuation of Clopidogrel
Avoid lapses in therapy, and if clopidogrel must be temporarily discontinued, restart as soon as possible. Premature discontinuation of clopidogrel may increase the risk of cardiovascular events.
5.4 Patients with Recent Transient Ischemic Attack (TIA) or Stroke
In patients with recent TIA or stroke who are at high risk for recurrent ischemic events, the combination of aspirin and clopidogrel has not been shown to be more effective than clopidogrel alone, but the combination has been shown to increase major bleeding.
5.5 Thrombotic Thrombocytopenic Purpura (TTP)
TTP, sometimes fatal, has been reported following use of clopidogrel, sometimes after a short exposure (<2 weeks). TTP is a serious condition that requires urgent treatment including plasmapheresis (plasma exchange). It is characterized by thrombocytopenia, microangiopathic hemolytic anemia (schistocytes [fragmented RBCs] seen on peripheral smear), neurological findings, renal dysfunction, and fever [see Adverse Reactions (6.2)].
-
6. ADVERSE REACTIONS
6.1 Clinical Studies Experience
Because clinical trials are conducted under widely varying conditions and durations of follow up, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clopidogrel has been evaluated for safety in more than 54,000 patients, including over 21,000 patients treated for 1 year or more. The clinically important adverse reactions observed in trials comparing clopidogrel plus aspirin to placebo plus aspirin and trials comparing clopidogrel alone to aspirin alone are discussed below.
Bleeding
CURE
In CURE, clopidogrel use with aspirin was associated with an increase in major bleeding (primarily gastrointestinal and at puncture sites) compared to placebo with aspirin (see Table 1). The incidence of intracranial hemorrhage (0.1%) and fatal bleeding (0.2%) were the same in both groups. Other bleeding events that were reported more frequently in the clopidogrel group were epistaxis, hematuria, and bruise.
The overall incidence of bleeding is described in Table 1.
Table 1: CURE Incidence of Bleeding Complications (% patients) * Other standard therapies were used as appropriate.
† Life-threatening and other major bleeding.
‡ Major bleeding event rate for clopidogrel + aspirin was dose-dependent on aspirin: <100 mg = 2.6%; 100-200 mg = 3.5%; >200 mg = 4.9% Major bleeding event rates for clopidogrel + aspirin by age were: <65 years = 2.5%, ≥65 to <75 years = 4.1%, ≥75 years = 5.9%
§ Major bleeding event rate for placebo + aspirin was dose-dependent on aspirin: <100 mg = 2.0%; 100-200 mg = 2.3%; >200 mg = 4.0% Major bleeding event rates for placebo + aspirin by age were: <65 years = 2.1%, ≥65 to <75 years = 3.1%, ≥75 years = 3.6%
¶ Led to interruption of study medication.
Event
Clopidogrel (+aspirin)*
(n=6259)
Placebo
(+aspirin)*
(n=6303)
Major bleeding †
3.7‡
2.7§
Life-threatening bleeding
2.2
1.8
Fatal
0.2
0.2
5 g/dL hemoglobin drop
0.9
0.9
Requiring surgical intervention
0.7
0.7
Hemorrhagic strokes
0.1
0.1
Requiring inotropes
0.5
0.5
Requiring transfusion (≥ 4 units)
1.2
1.0
Other major bleeding
1.6
1.0
Significantly disabling
0.4
0.3
Intraocular bleeding with significant loss of vision
0.05
0.03
Requiring 2-3 units of blood
1.3
0.9
Minor bleeding ¶
5.1
2.4
Ninety-two percent (92%) of the patients in the CURE study received heparin or low molecular weight heparin (LMWH), and the rate of bleeding in these patients was similar to the overall results.
COMMIT
In COMMIT, similar rates of major bleeding were observed in the clopidogrel and placebo groups, both of which also received aspirin (see Table 2).
Table 2: Incidence of Bleeding Events in COMMIT (% patients) * Major bleeds were cerebral bleeds or non-cerebral bleeds thought to have caused death or that required transfusion.
** The relative rate of major noncerebral or cerebral bleeding was independent of age. Event rates for clopidogrel + aspirin by age were: <60 years = 0.3%, ≥60 to <70 years = 0.7%, ≥70 years = 0.8%. Event rates for placebo + aspirin by age were: <60 years = 0.4%, ≥60 to <70 years = 0.6%, ≥70 years = 0.7%.
Type of bleeding
Clopidogrel
(+ aspirin)
(n=22961)
Placebo
(+ aspirin)
(n=22891)
p-value
Major* noncerebral or cerebral bleeding**
0.6
0.5
0.59
Major noncerebral
0.4
0.3
0.48
Fatal
0.2
0.2
0.90
Hemorrhagic stroke
0.2
0.2
0.91
Fatal
0.2
0.2
0.81
Other noncerebral bleeding (non-major)
3.6
3.1
0.005
Any noncerebral bleeding
3.9
3.4
0.004
CAPRIE (Clopidogrel vs. Aspirin)
In CAPRIE, gastrointestinal hemorrhage occurred at a rate of 2.0% in those taking clopidogrel vs. 2.7% in those taking aspirin; bleeding requiring hospitalization occurred in 0.7% and 1.1%, respectively. The incidence of intracranial hemorrhage was 0.4% for clopidogrel compared to 0.5% for aspirin.
Other bleeding events that were reported more frequently in the clopidogrel group were epistaxis and hematoma.
Other Adverse Events
In CURE and CHARISMA, which compared clopidogrel plus aspirin to aspirin alone, there was no difference in the rate of adverse events (other than bleeding) between clopidogrel and placebo.
In CAPRIE, which compared clopidogrel to aspirin, pruritus was more frequently reported in those taking clopidogrel. No other difference in the rate of adverse events (other than bleeding) was reported.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of clopidogrel. Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Blood and lymphatic system disorders: Agranulocytosis, aplastic anemia/pancytopenia, thrombotic thrombocytopenic purpura (TTP)
- Eye disorders: Eye (conjunctival, ocular, retinal) bleeding
- Gastrointestinal disorders: Gastrointestinal and retroperitoneal hemorrhage with fatal outcome, colitis (including ulcerative or lymphocytic colitis), pancreatitis, stomatitis, gastric/duodenal ulcer, diarrhea
- General disorders and administration site condition: Fever, hemorrhage of operative wound
- Hepato-biliary disorders: Acute liver failure, hepatitis (non-infectious), abnormal liver function test
- Immune system disorders: Hypersensitivity reactions, anaphylactoid reactions, serum sickness
- Musculoskeletal, connective tissue and bone disorders: Musculoskeletal bleeding, myalgia, arthralgia, arthritis
- Nervous system disorders: Taste disorders, fatal intracranial bleeding, headache
- Psychiatric disorders: Confusion, hallucinations
- Respiratory, thoracic and mediastinal disorders: Bronchospasm, interstitial pneumonitis, respiratory tract bleeding
- Renal and urinary disorders: Increased creatinine levels
- Skin and subcutaneous tissue disorders: Maculopapular or erythematous rash, urticaria, bullous dermatitis, eczema, toxic epidermal necrolysis, Stevens-Johnson syndrome, angioedema, erythema multiforme, skin bleeding, lichen planus, generalized pruritus
- Vascular disorders: Vasculitis, hypotension
-
7. DRUG INTERACTIONS
7.1 CYP2C19 Inhibitors
Clopidogrel is metabolized to its active metabolite in part by CYP2C19. Concomitant use of certain drugs that inhibit the activity of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition [see Warnings and Precautions (5.1) and Dosage and Administration (2.4)].
Proton Pump Inhibitors (PPI)
Avoid concomitant use of clopidogrel with omeprazole or esomeprazole. In clinical studies, omeprazole was shown to reduce the antiplatelet activity of clopidogrel when given concomitantly or 12 hours apart. A higher dose regimen of clopidogrel concomitantly administered with omeprazole increases antiplatelet response; an appropriate dose regimen has not been established. A similar reduction in antiplatelet activity was observed with esomeprazole when given concomitantly with clopidogrel. Consider using another acid-reducing agent with minimal or no CYP2C19 inhibitory effect on the formation of clopidogrel active metabolite. Dexlansoprazole, lansoprazole and pantoprazole had less effect on the antiplatelet activity of clopidogrel than did omeprazole or esomeprazole [see Dosage and Administration (2.4), Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
7.2 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Coadministration of clopidogrel and NSAIDs increases the risk of gastrointestinal bleeding.
7.3 Warfarin (CYP2C9 Substrates)
Although the administration of clopidogrel 75 mg per day did not modify the pharmacokinetics of S-warfarin (a CYP2C9 substrate) or INR in patients receiving long-term warfarin therapy, coadministration of clopidogrel with warfarin increases the risk of bleeding because of independent effects on hemostasis.
However, at high concentrations in vitro, clopidogrel inhibits CYP2C9.
-
8. USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Reproduction studies performed in rats and rabbits at doses up to 500 and 300 mg/kg/day, respectively (65 and 78 times the recommended daily human dose, respectively, on a mg/m2 basis), revealed no evidence of impaired fertility or fetotoxicity due to clopidogrel. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of a human response, clopidogrel should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
Studies in rats have shown that clopidogrel and/or its metabolites are excreted in the milk. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from clopidogrel, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
Safety and effectiveness in the pediatric population have not been established.
Additional information describing a clinical study in which efficacy was not demonstrated in neonates and infants is approved in the package insert for Bristol-Myers Squibb’s clopidogrel tablets. However, due to Bristol-Myers Squibb’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
8.5 Geriatric Use
Of the total number of subjects in the CAPRIE and CURE controlled clinical studies, approximately 50% of patients treated with clopidogrel were 65 years of age and older, and 15% were 75 years and older. In COMMIT, approximately 58% of the patients treated with clopidogrel were 60 years and older, 26% of whom were 70 years and older.
The observed risk of bleeding events with clopidogrel plus aspirin versus placebo plus aspirin by age category is provided in Table 1 and Table 2 for the CURE and COMMIT trials, respectively [see Adverse Reactions (6.1)]. No dosage adjustment is necessary in elderly patients.
8.6 Renal Impairment
Experience is limited in patients with severe and moderate renal impairment [see Clinical Pharmacology (12.2)].
8.7 Hepatic Impairment
No dosage adjustment is necessary in patients with hepatic impairment [see Clinical Pharmacology (12.2)].
-
10. OVERDOSAGE
Platelet inhibition by clopidogrel is irreversible and will last for the life of the platelet. Overdose following clopidogrel administration may result in bleeding complications. A single oral dose of clopidogrel at 1500 or 2000 mg/kg was lethal to mice and to rats and at 3000 mg/kg to baboons. Symptoms of acute toxicity were vomiting, prostration, difficult breathing, and gastrointestinal hemorrhage in animals.
Based on biological plausibility, platelet transfusion may restore clotting ability.
-
11. DESCRIPTION
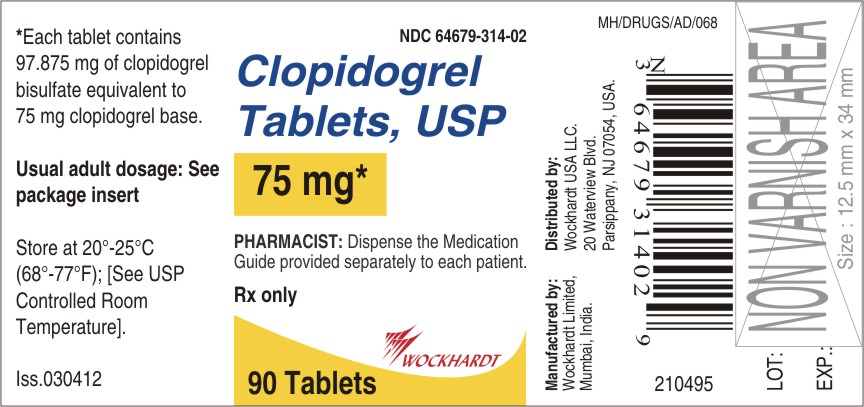
Clopidogrel bisulfate is a thienopyridine class inhibitor of P2Y12 ADP platelet receptors. Chemically it is methyl (+)-(S)-α-(2-chlorophenyl)-6,7-dihydrothieno[3,2-c]pyridine-5(4H) acetate sulfate (1:1). The empirical formula of clopidogrel bisulfate is C16H16ClNO2S•H2SO4 and its molecular weight is 419.9.
The structural formula is as follows:
Clopidogrel bisulfate is white to off white powder. It is practically insoluble in water at neutral pH but freely soluble at pH 1. It also dissolves freely in methanol, dissolves sparingly in methylene chloride, and is practically insoluble in ethyl ether. It has a specific optical rotation of about +56°.
Clopidogrel tablet, USP for oral administration is provided as either pink, round, biconvex, debossed, film-coated tablets containing 97.875 mg of clopidogrel bisulfate which is the molar equivalent of 75 mg of clopidogrel base or pink, modified capsule shaped, debossed film-coated tablets containing 391.5 mg of clopidogrel bisulfate which is the molar equivalent of 300 mg of clopidogrel base.
Each tablet contains glyceryl behenate, hydrogenated castor oil, hydroxypropylcellulose, mannitol, microcrystalline cellulose and polyethylene glycol 6000 as inactive ingredients. The pink film coating contains iron oxide red, hypromellose 2910, lactose monohydrate, titanium dioxide and triacetin.
-
12. CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Clopidogrel is an inhibitor of platelet activation and aggregation through the irreversible binding of its active metabolite to the P2Y12 class of ADP receptors on platelets.
12.2 Pharmacodynamics
Clopidogrel must be metabolized by CYP450 enzymes to produce the active metabolite that inhibits platelet aggregation. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP-mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible. Consequently, platelets exposed to clopidogrel’s active metabolite are affected for the remainder of their lifespan (about 7 to 10 days). Platelet aggregation induced by agonists other than ADP is also inhibited by blocking the amplification of platelet activation by released ADP.
Dose-dependent inhibition of platelet aggregation can be seen 2 hours after single oral doses of clopidogrel tablets. Repeated doses of 75 mg clopidogrel tablets per day inhibit ADP-induced platelet aggregation on the first day, and inhibition reaches steady state between Day 3 and Day 7. At steady state, the average inhibition level observed with a dose of 75 mg clopidogrel tablets per day was between 40% and 60%. Platelet aggregation and bleeding time gradually return to baseline values after treatment is discontinued, generally in about 5 days.
Geriatric Patients
Elderly (≥75 years) and young healthy subjects had similar effects on platelet aggregation.
Renally-Impaired Patients
After repeated doses of 75 mg clopidogrel tablets per day, patients with severe renal impairment (creatinine clearance from 5 to 15 mL/min) and moderate renal impairment (creatinine clearance from 30 to 60 mL/min) showed low (25%) inhibition of ADP-induced platelet aggregation.
Hepatically-Impaired Patients
After repeated doses of 75 mg clopidogrel tablets per day for 10 days in patients with severe hepatic impairment, inhibition of ADP-induced platelet aggregation was similar to that observed in healthy subjects.
Gender
In a small study comparing men and women, less inhibition of ADP-induced platelet aggregation was observed in women.
12.3 Pharmacokinetics
Clopidogrel is a prodrug and is metabolized to a pharmacologically active metabolite and inactive metabolites.
Absorption
After single and repeated oral doses of 75 mg per day, clopidogrel is rapidly absorbed. Absorption is at least 50%, based on urinary excretion of clopidogrel metabolites.
Effect of Food
Clopidogrel can be administered with or without food. In a study in healthy male subjects when clopidogrel tablets 75 mg per day was given with a standard breakfast, mean inhibition of ADP-induced platelet aggregation was reduced by less than 9%. The active metabolite AUC0-24 was unchanged in the presence of food, while there was a 57% decrease in active metabolite Cmax. Similar results were observed when a clopidogrel tablets 300 mg loading dose was administered with a high-fat breakfast.
Metabolism
Clopidogrel is extensively metabolized by two main metabolic pathways: one mediated by esterases and leading to hydrolysis into an inactive carboxylic acid derivative (85% of circulating metabolites) and one mediated by multiple cytochrome P450 enzymes. Cytochromes first oxidize clopidogrel to a 2-oxo-clopidogrel intermediate metabolite. Subsequent metabolism of the 2-oxo-clopidogrel intermediate metabolite results in formation of the active metabolite, a thiol derivative of clopidogrel. This metabolic pathway is mediated by CYP2C19, CYP3A, CYP2B6 and CYP1A2. The active thiol metabolite binds rapidly and irreversibly to platelet receptors, thus inhibiting platelet aggregation for the lifespan of the platelet.
The Cmax of the active metabolite is twice as high following a single 300 mg clopidogrel loading dose as it is after four days of 75 mg maintenance dose. Cmax occurs approximately 30 to 60 minutes after dosing. In the 75 to 300 mg dose range, the pharmacokinetics of the active metabolite deviates from dose proportionality: increasing the dose by a factor of four results in 2.0- and 2.7-fold increases in Cmax and AUC, respectively.
Elimination
Following an oral dose of 14C-labeled clopidogrel in humans, approximately 50% of total radioactivity was excreted in urine and approximately 46% in feces over the 5 days post-dosing. After a single, oral dose of 75 mg, clopidogrel has a half-life of approximately 6 hours. The half-life of the active metabolite is about 30 minutes.
Drug Interactions
Clopidogrel is metabolized to its active metabolite in part by CYP2C19. Concomitant use of certain inhibitors of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition.
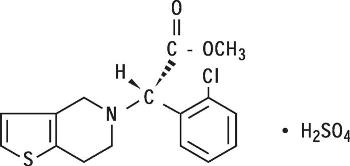
Proton Pump Inhibitors (PPI)
The effect of proton pump inhibitors (PPI) on the systemic exposure to the clopidogrel active metabolite following multiple doses of clopidogrel tablets 75 mg evaluated in dedicated drug interaction studies is presented in Figure 1.
Figure 1: Exposure to Clopidogrel Active Metabolite Following Multiple Doses of Clopidogrel Tablets 75 mg Alone or with Proton Pump Inhibitors (PPIs)
Pharmacodynamic and pharmacokinetic parameters measured in these studies showed that the interaction was highest with omeprazole and least with dexlansoprazole.
12.5 Pharmacogenomics
CYP2C19 is involved in the formation of both the active metabolite and the 2-oxo-clopidogrel intermediate metabolite. Clopidogrel active metabolite pharmacokinetics and antiplatelet effects, as measured by ex vivo platelet aggregation assays, differ according to CYP2C19 genotype. Genetic variants of other CYP450 enzymes may also affect the formation of clopidogrel’s active metabolite.
The CYP2C19*1 allele corresponds to fully functional metabolism while the CYP2C19*2 and *3 alleles are nonfunctional. CYP2C19*2 and *3 account for the majority of reduced function alleles in white (85%) and Asian (99%) poor metabolizers. Other alleles associated with absent or reduced metabolism are less frequent, and include, but are not limited to, CYP2C19*4, *5, *6, *7, and *8. A patient with poor metabolizer status will possess two loss-of-function alleles as defined above. Published frequencies for poor CYP2C19 metabolizer genotypes are approximately 2% for whites, 4% for blacks and 14% for Chinese. Tests are available to determine a patient’s CYP2C19 genotype.
A crossover study in 40 healthy subjects, 10 each in the four CYP2C19 metabolizer groups, evaluated pharmacokinetic and antiplatelet responses using 300 mg followed by 75 mg per day and 600 mg followed by 150 mg per day, each for a total of 5 days. Decreased active metabolite exposure and diminished inhibition of platelet aggregation were observed in the poor metabolizers as compared to the other groups. When poor metabolizers received the 600 mg/150 mg regimen, active metabolite exposure and antiplatelet response were greater than with the 300 mg/75 mg regimen (see Table 3). An appropriate dose regimen for this patient population has not been established in clinical outcome trials.
Table 3: Active Metabolite Pharmacokinetics and Antiplatelet Responses by CYP2C19 Metabolizer Status
Dose
Ultrarapid
(n=10)
Extensive
(n=10)
Intermediate
(n=10)
Poor
(n=10)
Cmax (ng/mL)
300 mg (24 h)
24 (10)
32 (21)
23 (11)
11 (4)
600 mg (24 h)
36 (13)
44 (27)
39 (23)
17 (6)
75 mg (Day 5)
12 (6)
13 (7)
12 (5)
4 (1)
150 mg (Day 5)
16 (9)
19 (5)
18 (7)
7 (2)
IPA (%)*
300 mg (24 h)
40 (21)
39 (28)
37 (21)
24 (26)
600 mg (24 h)
51 (28)
49 (23)
56 (22)
32 (25)
75 mg (Day 5)
56 (13)
58 (19)
60 (18)
37 (23)
150 mg (Day5)
68 (18)
73 (9)
74 (14)
61 (14)
VASP-PRI(%)†
300 mg (24 h)
73 (12)
68 (16)
78 (12)
91 (12)
600 mg (24 h)
51 (20)
48 (20)
56 (26)
85 (14)
75 mg (Day 5)
40 (9)
39 (14)
50 (16)
83 (13)
150 mg (Day 5)
20 (10)
24 (10)
29 (11)
61 (18)
Values are mean (SD)
* Inhibition of platelet aggregation with 5 mcM ADP; larger value indicates greater platelet inhibition
† Vasodilator-stimulated phosphoprotein - platelet reactivity index; smaller value indicates greater platelet inhibition
Some published studies suggest that intermediate metabolizers have decreased active metabolite exposure and diminished antiplatelet effects.
The relationship between CYP2C19 genotype and clopidogrel treatment outcome was evaluated in retrospective analyses of clopidogrel-treated subjects in CHARISMA (n=2428) and TRITON-TIMI 38 (n=1477), and in several published cohort studies. In TRITON-TIMI 38 and the majority of the cohort studies, the combined group of patients with either intermediate or poor metabolizer status had a higher rate of cardiovascular events (death, myocardial infarction, and stroke) or stent thrombosis compared to extensive metabolizers. In CHARISMA and one cohort study, the increased event rate was observed only in poor metabolizers.
-
13. NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment Of Fertility
There was no evidence of tumorigenicity when clopidogrel was administered for 78 weeks to mice and 104 weeks to rats at dosages up to 77 mg/kg per day, which afforded plasma exposures >25 times that in humans at the recommended daily dose of 75 mg.
Clopidogrel was not genotoxic in four in vitro tests (Ames test, DNA-repair test in rat hepatocytes, gene mutation assay in Chinese hamster fibroblasts, and metaphase chromosome analysis of human lymphocytes) and in one in vivo test (micronucleus test by oral route in mice). Clopidogrel was found to have no effect on fertility of male and female rats at oral doses up to 400 mg/kg per day (52 times the recommended human dose on a mg/m2 basis).
-
14. CLINICAL STUDIES
14.1 Acute Coronary Syndrome
The CURE study included 12,562 patients with ACS without ST-elevation (UA or NSTEMI) and presenting within 24 hours of onset of the most recent episode of chest pain or symptoms consistent with ischemia. Patients were required to have either ECG changes compatible with new ischemia (without ST-elevation) or elevated cardiac enzymes or troponin I or T to at least twice the upper limit of normal. The patient population was largely Caucasian (82%) and included 38% women, and 52% patients ≥65 years of age.
Patients were randomized to receive clopidogrel tablets (300-mg loading dose followed by 75 mg once daily) or placebo, and were treated for up to one year. Patients also received aspirin (75-325 mg once daily) and other standard therapies such as heparin. The use of GPIIb/IIIa inhibitors was not permitted for three days prior to randomization.
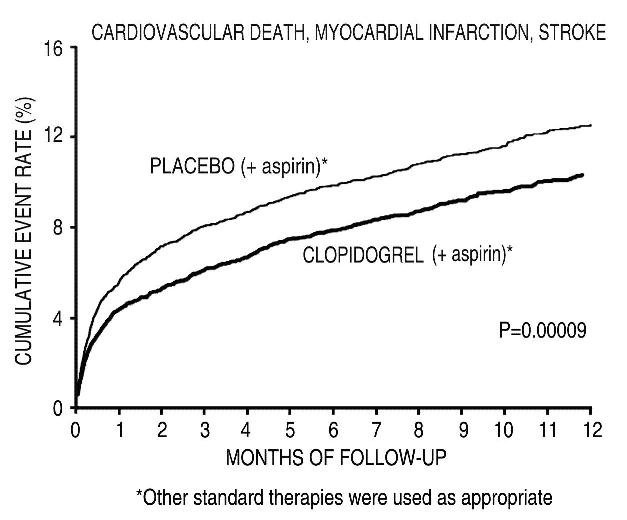
The number of patients experiencing the primary outcome (CV death, MI, or stroke) was 582 (9.3%) in the clopidogrel-treated group and 719 (11.4%) in the placebo-treated group, a 20% relative risk reduction (95% CI of 10%-28%; p < 0.001) for the clopidogrel-treated group (see Table 4).
Table 4: Outcome Events in the CURE Primary Analysis * Other standard therapies were used as appropriate.
† The individual components do not represent a breakdown of the primary and co-primary outcomes, but rather the total number of subjects experiencing an event during the course of the study.
Outcome
Clopidogrel
(+ aspirin)*
Placebo
(+ aspirin)*
Relative Risk Reduction (%)
(95% CI)
(n=6259)
(n=6303)
Primary outcome
582 (9.3%)
719 (11.4%)
20%
(Cardiovascular death, MI, stroke)
(10.3, 27.9)
p < 0.001
All Individual Outcome Events:†
CV death
318 (5.1%)
345 (5.5%)
7%
(-7.7, 20.6)
MI
324 (5.2%)
419 (6.6%)
23%
(11.0, 33.4)
Stroke
75 (1.2%)
87 (1.4%)
14%
(-17.7, 36.6)
Most of the benefit of clopidogrel occurred in the first two months, but the difference from placebo was maintained throughout the course of the trial (up to 12 months) (see Figure 2).
Figure 2: Cardiovascular Death, Myocardial Infarction, and Stroke in the CURE Study
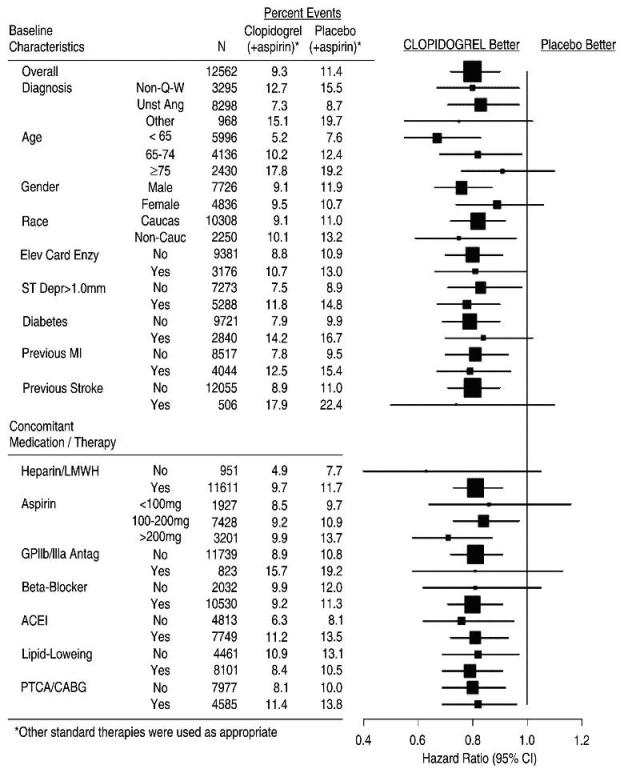
In CURE, the use of clopidogrel was associated with a lower incidence of CV death, MI or stroke in patient populations with different characteristics, as shown in Figure 3. The benefits associated with clopidogrel were independent of the use of other acute and long-term cardiovascular therapies, including heparin/LMWH, intravenous glycoprotein IIb/IIIa (GPIIb/IIIa) inhibitors, lipid-lowering drugs, beta-blockers, and ACE-inhibitors. The efficacy of clopidogrel was observed independently of the dose of aspirin (75-325 mg once daily). The use of oral anticoagulants, non-study anti-platelet drugs, and chronic NSAIDs was not allowed in CURE.
Figure 3: Hazard Ratio for Patient Baseline Characteristics and On-Study Concomitant Medications/Interventions for the CURE Study
The use of clopidogrel in CURE was associated with a decrease in the use of thrombolytic therapy (71 patients [1.1%] in the clopidogrel group, 126 patients [2.0%] in the placebo group; relative risk reduction of 43%), and GPIIb/IIIa inhibitors (369 patients [5.9%] in the clopidogrel group, 454 patients [7.2%] in the placebo group, relative risk reduction of 18%). The use of clopidogrel in CURE did not affect the number of patients treated with CABG or PCI (with or without stenting), (2253 patients [36.0%] in the clopidogrel group, 2324 patients [36.9%] in the placebo group; relative risk reduction of 4.0%).
COMMIT
In patients with STEMI, the safety and efficacy of clopidogrel were evaluated in the randomized, placebo-controlled, double-blind study, COMMIT. COMMIT included 45,852 patients presenting within 24 hours of the onset of the symptoms of myocardial infarction with supporting ECG abnormalities (i.e., ST-elevation, ST-depression or left bundle-branch block). Patients were randomized to receive clopidogrel tablets (75 mg once daily) or placebo, in combination with aspirin (162 mg per day), for 28 days or until hospital discharge, whichever came first.
The primary endpoints were death from any cause and the first occurrence of re-infarction, stroke or death.
The patient population included 28% women, 58% age ≥ 60 years (26% age ≥ 70 years), 55% patients who received thrombolytics, 68% who received ACE-inhibitors, and only 3% who underwent PCI.
As shown in Table 5 and Figures 4 and 5 below, clopidogrel significantly reduced the relative risk of death from any cause by 7% (p=0.029), and the relative risk of the combination of re-infarction, stroke or death by 9% (p=0.002).
Table 5: Outcome Events in the COMMIT Analysis * The difference between the composite endpoint and the sum of death+non-fatal MI+non-fatal stroke indicates that 9 patients (2 clopidogrel and 7 placebo) suffered both a non-fatal stroke and a non-fatal MI.
** Non-fatal MI and non-fatal stroke exclude patients who died (of any cause).
Event
Clopidogrel
(+ aspirin)
(N=22961)
Placebo
(+ aspirin)
(N=22891)
Odds ratio
(95% CI)
p-value
Composite endpoint: Death,
MI, or Stroke*
2121 (9.2%)
2310 (10.1%)
0.91 (0.86, 0.97)
0.002
Death
Non-fatal MI**
Non-fatal Stroke**
1726 (7.5%)
270 (1.2%)
127 (0.6%)
1845 (8.1%)
330 (1.4%)
142 (0.6%)
0.93 (0.87, 0.99)
0.81 (0.69, 0.95)
0.89 (0.70, 1.13)
0.029
0.011
0.33
Figure 4: Cumulative Event Rates for Death in the COMMIT Study*
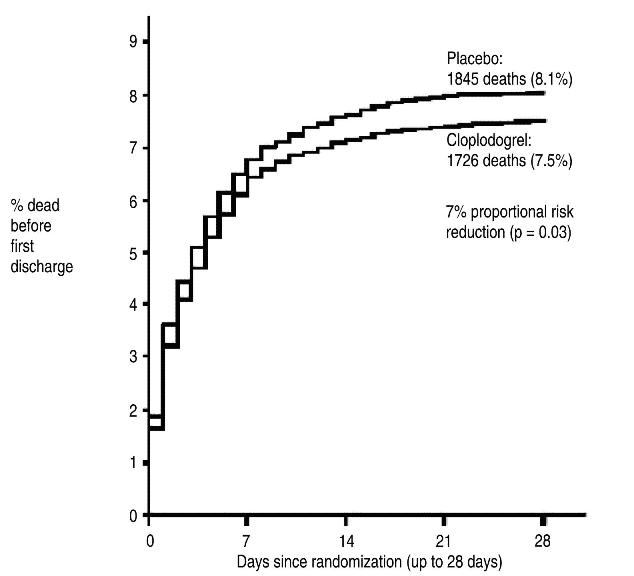
*All treated patients received aspirin.
Figure 5: Cumulative Event Rates for the Combined Endpoint Re-Infarction, Stroke or Death in the COMMIT Study*
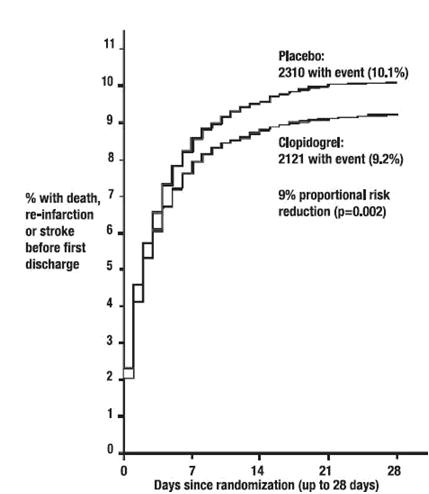
*All treated patients received aspirin.
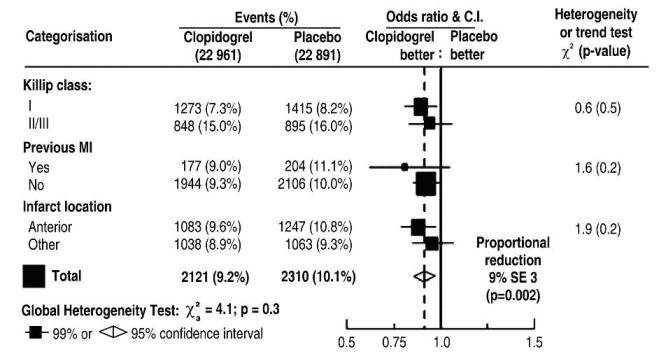
The effect of clopidogrel did not differ significantly in various pre-specified subgroups as shown in Figure 6. The effect was also similar in non-prespecified subgroups including those based on infarct location, Killip class or prior MI history (see Figure 7). Such subgroup analyses should be interpreted cautiously.
Figure 6: Effects of Adding Clopidogrel to Aspirin on the Combined Primary Endpoint across Baseline and Concomitant Medication Subgroups for the COMMIT Study
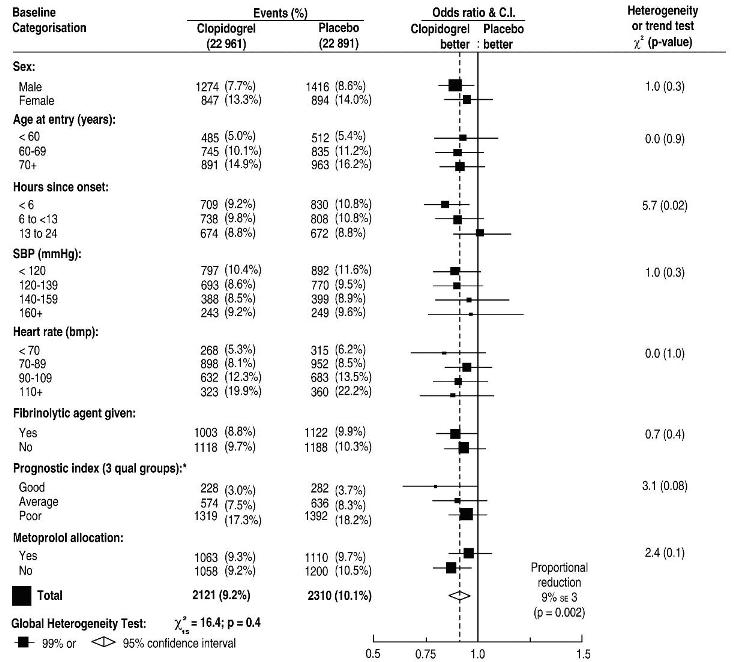
* Three similar-sized prognostic index groups were based on absolute risk of primary composite outcome for each patient calculated from baseline prognostic variables (excluding allocated treatments) with a Cox regression model.
Figure 7: Effects of Adding Clopidogrel to Aspirin in the Non-Prespecified Subgroups in the COMMIT Study
14.2 Recent Myocardial Infarction, Recent Stroke, or Established Peripheral Arterial Disease
The CAPRIE trial was a 19,185-patient, 304-center, international, randomized, double-blind, parallel-group study comparing clopidogrel tablets (75 mg daily) to aspirin (325 mg daily). The patients randomized had: 1) recent histories of myocardial infarction (within 35 days); 2) recent histories of ischemic stroke (within 6 months) with at least a week of residual neurological signs; or 3) established peripheral arterial disease. Patients received randomized treatment for an average of 1.6 years (maximum of 3 years).
The trial's primary outcome was the time to first occurrence of new ischemic stroke (fatal or not), new myocardial infarction (fatal or not), or other vascular death. Deaths not easily attributable to nonvascular causes were all classified as vascular.
Table 6: Outcome Events in the CAPRIE Primary Analysis
Clopidogrel
aspirin
Patients
n=9599
n=9586
Ischemic stroke (fatal or not)
438 (4.6%)
461 (4.8%)
MI (fatal or not)
275 (2.9%)
333 (3.5%)
Other vascular death
226 (2.4%)
226 (2.4%)
Total
939 (9.8%)
1020 (10.6%)
As shown in the table 6, clopidogrel was associated with a lower incidence of outcome events, primarily MI. The overall relative risk reduction (9.8% vs. 10.6%) was 8.7%, p=0.045. Similar results were obtained when all-cause mortality and all-cause strokes were counted instead of vascular mortality and ischemic strokes (risk reduction 6.9%). In patients who survived an on-study stroke or myocardial infarction, the incidence of subsequent events was lower in the clopidogrel group.
The curves showing the overall event rate are shown in Figure 8. The event curves separated early and continued to diverge over the 3-year follow-up period.
Figure 8: Fatal or Non-Fatal Vascular Events in the CAPRIE Study
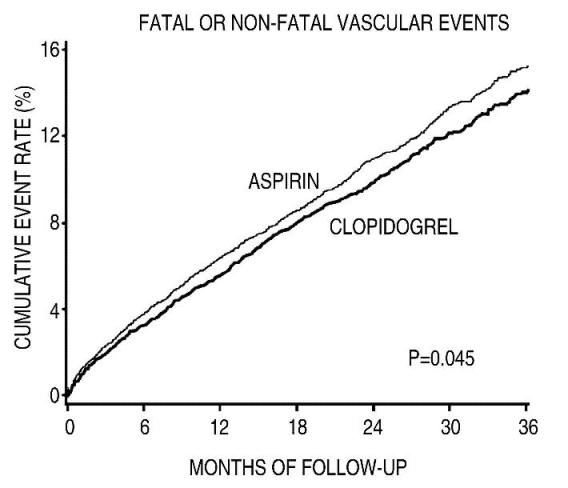
The statistical significance favoring clopidogrel over aspirin was marginal (p=0.045). However, because aspirin is itself effective in reducing cardiovascular events in patients with recent myocardial infarction or stroke, the effect of clopidogrel are substantial.
The CAPRIE trial included a population that was randomized on the basis of 3 entry criteria. The efficacy of clopidogrel relative to aspirin was heterogeneous across these randomized subgroups (p=0.043). It is not clear whether this difference is real or a chance occurrence. Although the CAPRIE trial was not designed to evaluate the relative benefit of clopidogrel over aspirin in the individual patient subgroups, the benefit appeared to be strongest in patients who were enrolled because of peripheral vascular disease (especially those who also had a history of myocardial infarction) and weaker in stroke patients. In patients who were enrolled in the trial on the sole basis of a recent myocardial infarction, clopidogrel was not numerically superior to aspirin.
14.3 Lack of Established Benefit of Clopidogrel plus Aspirin in Patients with Multiple Risk Factors or Established Vascular Disease
The CHARISMA trial was a 15,603 subject, randomized, double-blind, parallel group study comparing clopidogrel tablets (75 mg daily) to placebo for prevention of ischemic events in patients with vascular disease or multiple risk factors for atherosclerosis. All subjects were treated with aspirin 75-162 mg daily. The mean duration of treatment was 23 months. The study failed to demonstrate a reduction in the occurrence of the primary endpoint, a composite of CV death, MI, or stroke. A total of 534 (6.9%) patients in the clopidogrel group versus 573 (7.4%) patients in the placebo group experienced a primary outcome event (p=0.22). Bleeding of all severities was more common in the subjects randomized to clopidogrel.
-
16. HOW SUPPLIED/STORAGE AND HANDLING
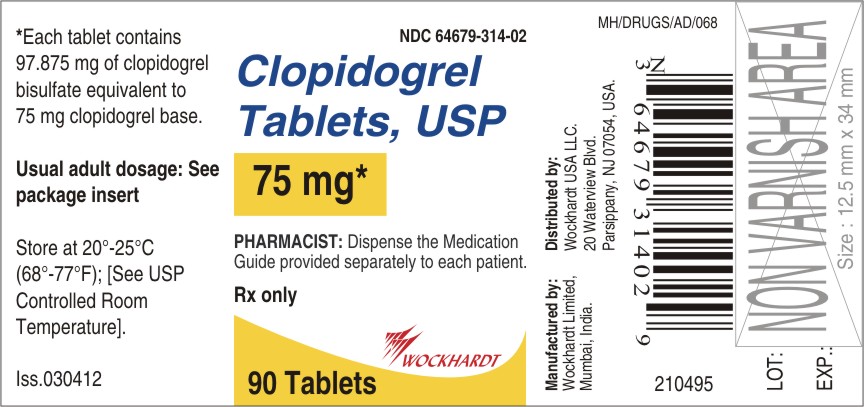
Clopidogrel tablets USP,75 mg are available as pink, round, biconvex, film-coated tablets debossed with "W 314" on one side and plain on other. Tablets are provided as follows:
NDC 64679-314-01, bottle of 30 tablets
NDC 64679-314-02, bottle of 90 tablets
NDC 64679-314-03, bottle of 500 tablets
NDC 64679-314-04, unit dose packages of 100 tablets
Clopidogrel tablets USP, 300 mg are available as pink, modified capsule shaped, biconvex, film-coated tablets debossed with "W 315" on one side and plain on other. Tablets are provided as follows:
NDC 64679-315-01, bottle of 30 tablets
NDC 64679-315-02, bottle of 90 tablets
NDC 64679-315-04, unit dose packages of 100 tablets
Store at 20°-25°C (68°-77°F); [See USP Controlled Room Temperature].
-
17. PATIENT COUNSELING INFORMATION
17.1 Benefits and Risks
- Summarize the effectiveness features and potential side effects of clopidogrel tablets, USP.
- Tell patients to take clopidogrel tablets, USP exactly as prescribed.
- Remind patients not to discontinue clopidogrel tablets, USP without first discussing it with the physician who prescribed clopidogrel tablets, USP.
17.2 Bleeding
- Will bruise and bleed more easily.
- Will take longer than usual to stop bleeding.
- Should report any unanticipated, prolonged, or excessive bleeding, or blood in their stool or urine.
17.3 Other Signs and Symptoms Requiring Medical Attention
- Inform patients that TTP is a rare but serious condition that has been reported with clopidogrel and other drugs in this class of drugs.
- Instruct patients to get prompt medical attention if they experience any of the following symptoms that cannot otherwise be explained: fever, weakness, extreme skin paleness, purple skin patches, yellowing of the skin or eyes, or neurological changes.
17.4 Invasive Procedures
- inform physicians and dentists that they are taking clopidogrel tablets, USP before any invasive procedure is scheduled.
- tell the doctor performing the invasive procedure to talk to the prescribing health care professional before stopping clopidogrel tablets, USP.
17.5 Concomitant Medications
Ask patients to list all prescription medications, over-the-counter medications, or dietary supplements they are taking or plan to take, including prescription or over-the-counter proton pump inhibitors (e.g., omeprazole), warfarin, or NSAIDs [see Warnings and Precautions (5)].
17.6 Medication Guide
Clopidogrel Tablets, USP
Read this Medication Guide before you start taking clopidogrel tablets and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking with your doctor about your medical condition or your treatment.
What is the most important information I should know about clopidogrel tablets, USP?
1. Clopidogrel tablets, USP may not work as well in people who:
-
MEDICATION GUIDE
- have certain genetic factors that affect how the body breaks down clopidogrel tablets. Your doctor may do genetic tests to make sure clopidogrel tablet is right for you.
- take certain medicines, especially omeprazole (Prilosec®) or Esomeprazole (Nexium®). Your doctor may change the medicine you take for stomach acid problems while you take clopidogrel tablets.
2. Clopidogrel tablets can cause bleeding which can be serious and can sometimes lead to death. Clopidogrel tablet is a blood thinner medicine that lowers the chance of blood clots forming in your body. While you take clopidogrel tablets:
- you may bruise and bleed more easily
- you are more likely to have nose bleeds
- it will take longer for any bleeding to stop
Call your doctor right away if you have any of these signs or symptoms of bleeding:
- unexpected bleeding or bleeding that lasts a long time
- blood in your urine (pink, red or brown urine)
- red or black stools (looks like tar)
- bruises that happen without a known cause or get larger
- cough up blood or blood clots
- vomit blood or your vomit looks like coffee grounds
Do not stop taking clopidogrel tablets, USP without talking to the doctor who prescribes it for you. People who are treated with a stent, and stop taking clopidogrel tablets too soon, have a higher risk of getting a blood clot on the stent, having a heart attack, or dying. If you must stop clopidogrel tablets because of bleeding, your risk of a heart attack may be higher.
What is Clopidogrel?
Clopidogrel is a prescription medicine used to treat people who have any of the following:
- chest pain due to heart problems
- poor circulation in their legs (peripheral arterial disease)
- a heart attack
- a stroke
Clopidogrel tablet is used alone or with aspirin to lower your chance of having another serious problem with your heart or blood vessels such as heart attack, stroke, or blood clot that can lead to death.
Platelets are blood cells that help your blood clot normally. Clopidogrel tablets helps to prevent platelets from sticking together and forming a clot that can block an artery.
It is not known if clopidogrel tablet is safe and effective in children.
Who should not take clopidogrel tablets, USP?
Do not take clopidogrel tablets if you:
- currently have a condition that causes bleeding, such as a stomach ulcer
- are allergic to clopidogrel or other ingredients in clopidogrel tablets, USP. See the end of this leaflet for a complete list of ingredients in clopidogrel tablets, USP.
What should I tell my doctor before taking clopidogrel tablets, USP?
Before you take clopidogrel tablets, USP, tell your doctor if you:
- have a history of bowel (gastrointestinal) or stomach ulcers
- have a history of bleeding problems
- plan to have surgery or a dental procedure. See "How should I take clopidogrel tablets, USP?"
- are pregnant or plan to become pregnant. It is not known if clopidogrel tablets, USP will harm your unborn baby
- are breastfeeding or plan to breastfeed. It is not known if clopidogrel tablets, USP passes into your breast milk. You and your doctor should decide if you will take clopidogrel tablets or breastfeed. You should not do both without talking to your doctor.
Tell all of your doctors and your dentist that you are taking clopidogrel tablets, USP. They should talk to the doctor who prescribed clopidogrel tablets, USP for you before you have any surgery or invasive procedure.
Tell your doctor about all the medicines you take, including prescription, non-prescription medicines, vitamins and herbal supplements.
Clopidogrel tablets, USP may affect the way other medicines work, and other medicines may affect how clopidogrel tablets, USP works. See "What is the most important information I should know about clopidogrel tablets, USP?"
Taking clopidogrel tablets, USP with certain other medicines may increase your risk of bleeding. Especially tell your doctor if you take:
- aspirin, especially if you have had a stroke. Always talk to your doctor about whether you should take aspirin along with clopidogrel tablets, USP to treat your condition.
- Non-steroidal anti-inflammatory drugs (NSAIDs). Ask your doctor or pharmacist for a list of NSAID medicines if you are not sure.
- warfarin (Coumadin®, Jantoven®)
Know the medicines you take. Keep a list of them to show your doctor or pharmacist when you get a new medicine.
How should I take clopidogrel tablets, USP?
- Take clopidogrel tablets, USP exactly as your doctor tells you.
- Do not change your dose or stop taking clopidogrel tablets without talking to your doctor first. Stopping clopidogrel tablets may increase your risk of heart attack or stroke.
- Take clopidogrel tablets with aspirin as instructed by your doctor.
- You can take clopidogrel tablets with or without food.
- If you miss a dose, take clopidogrel tablets as soon as you remember. If it is almost time for your next dose, skip the missed dose. Take the next dose at your regular time. Do not take 2 doses of clopidogrel tablets at the same time unless your doctor tells you to.
- If you take too much clopidogrel tablets, call your doctor or go to the nearest emergency room right away.
- Talk with your doctor about stopping your clopidogrel tablets before you have surgery. Your doctor may tell you to stop taking clopidogrel tablets at least 5 days before you have surgery to avoid excessive bleeding during surgery.
What are the possible side effects of clopidogrel tablets, USP?
Clopidogrel tablets, USP can cause serious side effects including:
● See "What is the most important information I should know about clopidogrel tablets?"
● A blood clotting problem called Thrombotic Thrombocytopenic Purpura (TTP). TTP can happen with clopidogrel tablets, USP, sometimes after a short time (less than 2 weeks). TTP is a blood clotting problem where blood clots form in blood vessels; and can happen anywhere in the body. TTP needs to be treated in a hospital right away, because it may cause death. Get medical help right away if you have any of these symptoms and they can not be explained by another medical condition:
- purplish spots (called purpura) on the skin or in the mouth (mucous membranes) due to bleeding under the skin
- your skin or the whites of your eyes are yellow (jaundice)
- you feel tired or weak
- your skin looks very pale
- fever
- fast heart rate or feeling short of breath
- headache
- speech changes
- confusion
- coma
- stroke
- seizure
- low amount of urine, or urine that is pink or has blood in it
- stomach area (abdominal) pain
- nausea, vomiting, or diarrhea
- vision changes
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of clopidogrel tablets. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store clopidogrel tablets, USP?
● Store clopidogrel tablets at 20°-25°C (68°-77°F)
Keep clopidogrel tablets, USP and all medicines out of the reach of children.
General information about clopidogrel tablets, USP
Medicines are sometimes used for purposes other than those listed in a Medication Guide. Do not take clopidogrel tablets for a condition for which it was not prescribed. Do not give clopidogrel tablets to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about clopidogrel tablets, USP. If you would like more information, talk to your doctor. Ask your doctor or pharmacist for information about clopidogrel tablets that was written for healthcare professionals.
For more information call 1-800-346-6854.
What are the ingredients in clopidogrel tablets, USP?
Active ingredient: clopidogrel bisulfate
Inactive ingredients:
Tablet: glyceryl behenate, hydrogenated castor oil, hydroxypropylcellulose, mannitol, microcrystalline cellulose and polyethylene glycol 6000 as inactive ingredients.
Film coating: iron oxide red, hypromellose 2910, lactose monohydrate, titanium dioxide and triacetin.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Coumadin® is a registered trademark of Bristol-Myers Squibb Pharma Company.
Prilosec® is a registered trademark of AstraZeneca.
Jantoven® is a registered trademark of USL Pharma.
- PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
CLOPIDOGREL
clopidogrel tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55648-314 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOPIDOGREL BISULFATE (UNII: 08I79HTP27) (CLOPIDOGREL - UNII:A74586SNO7) CLOPIDOGREL 75 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) FERRIC OXIDE RED (UNII: 1K09F3G675) GLYCERYL DIBEHENATE (UNII: R8WTH25YS2) HYDROGENATED CASTOR OIL (UNII: ZF94AP8MEY) HYDROXYPROPYL CELLULOSE (UNII: RFW2ET671P) HYPROMELLOSE 2910 (15 MPA.S) (UNII: 36SFW2JZ0W) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MANNITOL (UNII: 3OWL53L36A) POLYETHYLENE GLYCOL 6000 (UNII: 30IQX730WE) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIACETIN (UNII: XHX3C3X673) Product Characteristics Color PINK Score no score Shape ROUND (biconvex) Size 9mm Flavor Imprint Code W314 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55648-314-01 30 in 1 BOTTLE 2 NDC:55648-314-02 90 in 1 BOTTLE 3 NDC:55648-314-03 500 in 1 BOTTLE 4 NDC:55648-314-04 10 in 1 CARTON 4 10 in 1 BLISTER PACK 5 NDC:55648-314-00 5000 in 1 POUCH Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA202266 05/22/2012 CLOPIDOGREL
clopidogrel tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:55648-315 Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength CLOPIDOGREL BISULFATE (UNII: 08I79HTP27) (CLOPIDOGREL - UNII:A74586SNO7) CLOPIDOGREL 300 mg Inactive Ingredients Ingredient Name Strength CELLULOSE, MICROCRYSTALLINE (UNII: OP1R32D61U) FERRIC OXIDE RED (UNII: 1K09F3G675) GLYCERYL DIBEHENATE (UNII: R8WTH25YS2) HYDROGENATED CASTOR OIL (UNII: ZF94AP8MEY) HYDROXYPROPYL CELLULOSE (UNII: RFW2ET671P) HYPROMELLOSE 2910 (15 MPA.S) (UNII: 36SFW2JZ0W) LACTOSE MONOHYDRATE (UNII: EWQ57Q8I5X) MANNITOL (UNII: 3OWL53L36A) POLYETHYLENE GLYCOL 6000 (UNII: 30IQX730WE) TITANIUM DIOXIDE (UNII: 15FIX9V2JP) TRIACETIN (UNII: XHX3C3X673) Product Characteristics Color PINK Score no score Shape CAPSULE (modified capsule biconvex) Size 18mm Flavor Imprint Code W315 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:55648-315-01 30 in 1 BOTTLE 2 NDC:55648-315-02 90 in 1 BOTTLE 3 NDC:55648-315-04 10 in 1 CARTON 3 10 in 1 BLISTER PACK 4 NDC:55648-315-00 1500 in 1 POUCH Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA202266 11/13/2012 Labeler - Wockhardt Limited (650069115) Registrant - Wockhardt Limited (650069115) Establishment Name Address ID/FEI Business Operations Wockhardt Limited 676257570 ANALYSIS(55648-314, 55648-315) , MANUFACTURE(55648-314, 55648-315) , PACK(55648-314, 55648-315) , LABEL(55648-314, 55648-315)