ONCASPAR- pegaspargase injection, solution
Sigma-Tau Pharmaceuticals, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use Oncaspar® safely and effectively. See full prescribing information for Oncaspar®.
Oncaspar®(pegaspargase) injection, for intramuscular or intravenous use Initial U.S. Approval: 1994 INDICATIONS AND USAGEDOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSMost common adverse reactions (≥ 2%) are allergic reactions (including anaphylaxis), central nervous system (CNS) thrombosis, coagulopathy, elevated transaminases, hyperbilirubinemia, hyperglycemia, and pancreatitis. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Sigma-Tau Pharmaceuticals, Inc. at 1-888-393-4584 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION. Revised: 5/2015 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Recommended Dose
- The recommended dose of Oncaspar® is 2,500 International Units/m2 intramuscularly or intravenously. Oncaspar® should be administered no more frequently than every 14 days.
2.2 Instructions for Administration
- When Oncaspar® is administered intramuscularly, the volume at a single injection site should be limited to 2 mL. If the volume to be administered is greater than 2 mL, multiple injection sites should be used. Oncaspar® does not contain a preservative. Use only one dose per vial; discard unused product.
- When administered intravenously, Oncaspar® should be given over a period of 1 to 2 hours in 100 mL of sodium chloride or dextrose injection 5%, through an infusion that is already running. After the solution is diluted for intravenous use, the solution should be used immediately. If immediate use is not possible, the diluted solution should be stored refrigerated at 2°C to 8°C (36°F to 46°F). Storage after dilution should not exceed 48 hours from the time of preparation to completion of administration. Protect infusion bags from direct sunlight.
2.3 Preparation and Handling Precautions
- Do not administer Oncaspar® if drug has been:
- •
- frozen
- •
- stored at room temperature 15° to 25°C (59° to 77°F) for more than 48 hours
- •
- shaken or vigorously agitated [see How Supplied/Storage and Handling (16)]
- Parenteral drug products should be inspected visually for particulate matter, cloudiness, or discoloration prior to administration, whenever solution and container permit. If any of these are present, discard the vial.
4 CONTRAINDICATIONS
- •
- History of serious allergic reactions to Oncaspar®.
- •
- History of serious thrombosis with prior L-asparaginase therapy.
- •
- History of pancreatitis with prior L-asparaginase therapy.
- •
- History of serious hemorrhagic events with prior L-asparaginase therapy.
5 WARNINGS AND PRECAUTIONS
5.1 Anaphylaxis and Serious Allergic Reactions
- Anaphylaxis and serious allergic reactions can occur in patients receiving Oncaspar®. The risk of serious allergic reactions is higher in patients with known hypersensitivity to other forms of L-asparaginase. Observe patients for 1 hour after administration of Oncaspar® in a setting with resuscitation equipment and other agents necessary to treat anaphylaxis (for example, epinephrine, oxygen, intravenous steroids, antihistamines). Discontinue Oncaspar® in patients with serious allergic reactions.
5.2 Thrombosis
- Serious thrombotic events, including sagittal sinus thrombosis can occur in patients receiving Oncaspar®. Discontinue Oncaspar® in patients with serious thrombotic events.
5.3 Pancreatitis
- Pancreatitis can occur in patients receiving Oncaspar®. Evaluate patients with abdominal pain for evidence of pancreatitis. Discontinue Oncaspar® in patients with pancreatitis.
5.4 Glucose Intolerance
- Glucose intolerance can occur in patients receiving Oncaspar®. In some cases, glucose intolerance is irreversible. Monitor serum glucose.
5.5 Coagulopathy
- Increased prothrombin time, increased partial thromboplastin time, and hypofibrinogenemia can occur in patients receiving Oncaspar®. Monitor coagulation parameters at baseline and periodically during and after treatment. Initiate treatment with fresh-frozen plasma to replace coagulation factors in patients with severe or symptomatic coagulopathy.
6 ADVERSE REACTIONS
- The following serious adverse reactions are described in greater detail in other sections of the label:
- •
- Anaphylaxis and serious allergic reactions [see Warnings and Precautions (5.1)]
- •
- Serious thrombosis [see Warnings and Precautions (5.2)]
- •
- Pancreatitis [see Warnings and Precautions (5.3)]
- •
- Glucose intolerance [see Warnings and Precautions (5.4)]
- •
- Coagulopathy [see Warnings and Precautions (5.5)]
- •
- Hepatotoxicity and abnormal liver function [see Warnings and Precautions (5.6)]
- The most common adverse reactions with Oncaspar® are allergic reactions (including anaphylaxis), hyperglycemia, pancreatitis, central nervous system (CNS) thrombosis, coagulopathy, hyperbilirubinemia, and elevated transaminases.
Hyperlipidemia (hypercholesterolemia and hypertriglyceridemia) has been reported in patients exposed to Oncaspar®.
6.1 Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in clinical practice.
First-Line ALL
- The data presented below are derived from 2 studies in patients with standard-risk ALL who received Oncaspar® as a component of first-line multi-agent chemotherapy. Study 1 was a randomized (1:1), active-controlled study that enrolled 118 patients, with a median age of 4.7 years (1.1-9.9 years), of whom 54% were males and 65% White, 14% Hispanic, 8% Black, 8% Asian, and 6% other. Of the 59 patients in Study 1 who were randomized to Oncaspar®, 48 patients (81%) received all 3 planned doses of Oncaspar®, 6 (10%) received 2 doses, 4 (7%) received 1 dose, and 1 patient (2%) did not receive the assigned treatment. Study 2 is an ongoing, multi-factorial design study in which all patients received Oncaspar® as a component of various multi-agent chemotherapy regimens; interim safety data are available for 2,770 patients. Study participants had a median age of 4 years (1-10 years), and were 55% male, 68% White, 18% Hispanic, 4% Black, 3% Asian, and 7% other. Per protocol, the schedule of Oncaspar® varied by treatment arm, with intermittent doses of Oncaspar® for up to 10 months.
- In Study 1, detailed safety information was collected for pre-specified adverse reactions identified as asparaginase-induced adverse reactions and for grade 3 and 4 non-hematologic adverse reactions according to the Children’s Cancer Group (CCG) Toxicity and Complication Criteria. The per-patient incidence, by treatment arm, for these selected adverse reactions occurring at a severity of grade 3 or 4 are presented in Table 1 below:
|
Oncaspar®
|
Native
|
|
|
Abnormal Liver Tests |
3 (5%) |
5 (8%) |
|
Elevated Transaminases* |
2 (3%) |
4 (7%) |
|
Hyperbilirubinemia |
1 (2%) |
1 (2%) |
|
Hyperglycemia |
3 (5%) |
2 (3%) |
|
Central Nervous System |
2 (3%) |
2 (3%) |
|
Coagulopathy† |
1 (2%) |
3 (5%) |
|
Pancreatitis |
1 (2%) |
1 (2%) |
|
Clinical Allergic Reactions to |
1 (2%) |
0 |
Previously Treated ALL
- Adverse reaction information was obtained from 5 clinical trials that enrolled a total of 174 patients with relapsed ALL who received Oncaspar® as a single agent or in combination with multi-agent chemotherapy. The toxicity profile of Oncaspar® in patients with previously treated relapsed ALL is similar to that reported above with the exception of clinical allergic reactions (see Table 2). The most common adverse reactions of Oncaspar® were clinical allergic reactions, elevated transaminases, hyperbilirubinemia, and coagulopathies. The most common serious adverse events due to Oncaspar® treatment were thrombosis (4%), hyperglycemia requiring insulin therapy (3%), and pancreatitis (1%).
6.2 Allergic Reactions
- Allergic reactions include the following: bronchospasm, hypotension, laryngeal edema, local erythema or swelling, systemic rash, and urticaria.
First-Line ALL
- Among 58 Oncaspar®-treated patients enrolled in Study 1, clinical allergic reactions were reported in 2 patients (3%). One patient experienced a grade 1 allergic reaction and the other grade 3 hives; both occurred during the first delayed intensification phase of the study (see Table 2).
Previously Treated ALL
- Among 62 patients with relapsed ALL and prior hypersensitivity reactions to asparaginase, 35 patients (56%) had a history of clinical allergic reactions to native Escherichia (E.) coli L-asparaginase, and 27 patients (44%) had history of clinical allergic reactions to both native E. coli and native Erwinia L-asparaginase. Twenty (32%) of these 62 patients experienced clinical allergic reactions to Oncaspar® (see Table 2).
- Among 112 patients with relapsed ALL with no prior hypersensitivity reactions to asparaginase, 11 patients (10%) experienced clinical allergic reactions to Oncaspar® (see Table 2).
|
Toxicity Grade, n (%) | |||||
|
Patient Status |
1 |
2 |
3 |
4 |
Total |
|
Previously |
7 (11) |
8 (13) |
4 (6) |
1 (2) |
20 (32) |
|
Non- |
5 (4) |
4 (4) |
1 (1) |
1 (1) |
11 (10) |
|
First Line (n=58) |
1 (2) |
0 |
1 (2) |
0 |
2 (3) |
6.3 Immunogenicity
- As with all therapeutic proteins, there is a potential for immunogenicity, defined as development of binding and/or neutralizing antibodies to the product.
- In Study 1, Oncaspar®-treated patients were assessed for evidence of binding antibodies using an enzyme-linked immunosorbent assay (ELISA) method. The incidence of protocol-specified “high-titer” antibody formation was 2% in Induction (n=48), 10% in Delayed Intensification 1 (n=50), and 11% in Delayed Intensification 2 (n=44). There is insufficient information to determine whether the development of antibodies is associated with an increased risk of clinical allergic reactions, altered pharmacokinetics, or loss of anti-leukemic efficacy.
- The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay, and the observed incidence of antibody positivity in an assay may be influenced by several factors including sample handling, concomitant medications, and underlying disease. Therefore, comparison of the incidence of antibodies to Oncaspar® with the incidence of antibodies to other products may be misleading.
7 DRUG INTERACTIONS
- No formal drug interaction studies, between Oncaspar® and other drugs, have been performed.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
- Pregnancy Category C. Animal reproduction studies have not been conducted with Oncaspar®. It is also not known whether Oncaspar® can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Oncaspar® should be given to a pregnant woman only if clearly needed.
8.3 Nursing Mothers
- It is not known whether Oncaspar® is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Oncaspar®, a decision should be made to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
10 OVERDOSAGE
- Three patients received 10,000 International Units/m2 of Oncaspar® as an intravenous infusion. One patient experienced a slight increase in liver enzymes. A second patient developed a rash 10 minutes after the start of the infusion, which was controlled with the administration of an antihistamine and by slowing down the infusion rate. A third patient did not experience any adverse reactions.
11 DESCRIPTION
- Oncaspar® (pegaspargase) is L-asparaginase (L-asparagine amidohydrolase) that is covalently conjugated to monomethoxypolyethylene glycol (mPEG). L-asparaginase is a tetrameric enzyme that is produced endogenously by E. coli and consists of identical 34.5 kDa subunits. Approximately 69 to 82 molecules of mPEG are linked to L-asparaginase; the molecular weight of each mPEG molecule is about 5 kDa. Oncaspar® activity is expressed in International Units. One International Unit of L-asparaginase is defined as the amount of enzyme required to generate 1 micromole of ammonia per minute at pH 7.3 and 37°C.
- Oncaspar® is supplied as a clear, colorless, preservative-free, isotonic sterile solution in phosphate-buffered saline, pH 7.3. Each milliliter contains 750 ± 150 International Units of pegaspargase, dibasic sodium phosphate, USP (5.58 mg), monobasic sodium phosphate, USP, (1.20 mg) and sodium chloride, USP (8.50 mg) in water for injection, USP.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
- The mechanism of action of Oncaspar® is thought to be based on selective killing of leukemic cells due to depletion of plasma asparagine. Some leukemic cells are unable to synthesize asparagine due to a lack of asparagine synthetase and are dependent on an exogenous source of asparagine for survival. Depletion of asparagine, which results from treatment with the enzyme L-asparaginase, kills the leukemic cells. Normal cells, however, are less affected by the depletion due to their ability to synthesize asparagine.
12.2 Pharmacodynamics
- In Study 1, pharmacodynamics were assessed in 57 newly diagnosed pediatric patients with standard-risk ALL who received three intramuscular doses of Oncaspar® (2,500 International Units/m2), one each during induction and two delayed intensification treatment phases. Pharmacodynamic activity was assessed through serial measurements of asparagine in sera (n=57) and cerebrospinal fluid (CSF) (n=50). The data for asparagine depletion are presented in CLINICAL STUDIES [see Clinical Studies (14)].
12.3 Pharmacokinetics
- Pharmacokinetic assessments were based on an enzymatic assay measuring asparaginase activity. Serum pharmacokinetics were assessed in 34 newly diagnosed pediatric patients with standard-risk ALL in Study 1 following intramuscular administration of 2,500 International Units/m2. The elimination half-life of Oncaspar® was approximately 5.8 days during the induction phase. Similar elimination half-lives were observed during Delayed Intensification 1 and Delayed Intensification 2. Concentrations greater than 0.1 International Units/mL were observed in over 90% of the samples from patients treated with Oncaspar® during induction, Delayed Intensification 1, and Delayed Intensification 2 for approximately 20 days.
- In 3 pharmacokinetic studies, 37 patients with relapsed ALL received Oncaspar® at 2,500 International Units/m2 intramuscularly every 2 weeks. The plasma half-life of Oncaspar® was 3.2 ± 1.8 days in 9 patients who were previously hypersensitive to native E. coli L-asparaginase and 5.7 ± 3.2 days in 28 non-hypersensitive patients. The area under the plasma concentration-time curve (AUC) was 9.5 ± 4.0 International Units/mL/day in the previously hypersensitive patients and 9.8 ± 6.0 International Units/mL/day in the non-hypersensitive patients.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
- •
- No long-term carcinogenicity studies in animals have been performed with Oncaspar®.
- •
- No relevant studies addressing mutagenic potential have been conducted. Oncaspar® did not exhibit a mutagenic effect when tested against Salmonella typhimurium strains in the Ames assay.
- •
- No studies have been performed on impairment of fertility.
14 CLINICAL STUDIES
14.1 First-Line ALL
- The safety and effectiveness of Oncaspar® was evaluated in an open-label, multicenter, randomized, active-controlled study (Study 1). In this study, 118 pediatric patients aged 1 to 9 years with previously untreated standard-risk ALL were randomized 1:1 to Oncaspar® or native E. coli L-asparaginase as part of combination therapy. Oncaspar® was administered intramuscularly at a dose of 2,500 International Units/m2 on Day 3 of the 4-week induction phase and on Day 3 of each of two 8-week delayed intensification phases. Native E. coli L-asparaginase was administered intramuscularly at a dose of 6,000 International Units/m2 three times weekly for 9 doses during induction and for 6 doses during each delayed intensification phase.
- The primary determination of effectiveness was based on demonstration of similar asparagine depletion (magnitude and duration) in the Oncaspar® and native E. coli L-asparaginase arms. The protocol-specified goal was achievement of asparagine depletion to a serum concentration of ≤1 μM. The proportion of patients with this level of depletion was similar between the 2 study arms during all 3 phases of treatment at the protocol-specified time points.
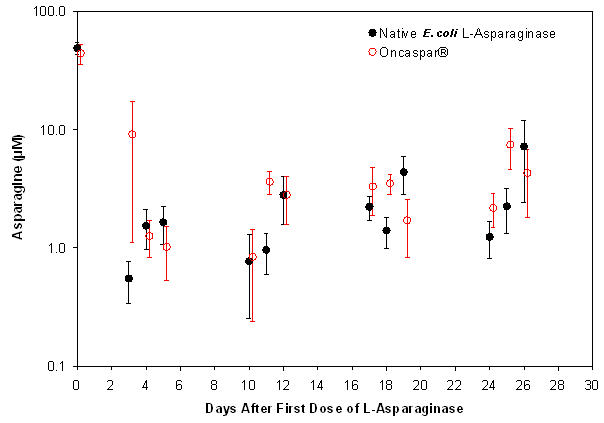
- In all phases of treatment, serum asparagine concentrations decreased within 4 days of the first dose of asparaginase in the treatment phase and remained low for approximately 3 weeks for both Oncaspar® and native E. coli L-asparaginase arms. Serum asparagine concentrations during the induction phase are shown in Figure 1. The patterns of serum asparagine depletion in the 2 delayed intensification phases are similar to the pattern of serum asparagine depletion in the induction phase.
FIGURE 1 MEAN (± STANDARD ERROR) SERUM ASPARAGINE CONCENTRATIONS DURING STUDY 1 INDUCTION PHASE
FIGURE 1 MEAN (± STANDARD ERROR) SERUM ASPARAGINE CONCENTRATIONS DURING STUDY 1 INDUCTION PHASE
Note: Oncaspar® (2,500 International Units/m2 intramuscular) was administered on Day 3 of the 4-week induction phase. Native E. coli L-asparaginase (6,000 International Units/m2 intramuscular) was administered 3 times weekly for 9 doses during induction.
- CSF asparagine concentrations were determined in 50 patients during the induction phase. CSF asparagine decreased from a mean pretreatment concentration of 3.1 µM to 1.7 µM on Day 4 ± 1 and 1.5 µM 25 ± 1 days after administration of Oncaspar®. These findings were similar to those observed in the native E. coli L-asparaginase treatment arm.
- While the 3-year Event-Free Survival (EFS) for the Oncaspar® and native E. coli L-asparaginase study arms were similar and in the range of 80%, Study 1 was not designed to evaluate for differences in EFS rates.
14.2 ALL Patients Hypersensitive to Asparaginase
- The safety and effectiveness of Oncaspar® was evaluated in 4 open-label studies enrolling a total of 42 patients with multiply-relapsed, acute leukemia [39 (93%) with ALL] with a history of prior clinical allergic reaction to asparaginase. Hypersensitivity to asparaginase was defined by a history of systemic rash, urticaria, bronchospasm, laryngeal edema, hypotension, or local erythema, urticaria, or swelling, greater than 2 centimeters, for at least 10 minutes following administration of any form of native E. coli L-asparaginase. All patients received Oncaspar® at a dose of 2,000 or 2,500 International Units/m2 administered intramuscularly or intravenously every 14 days. Patients received Oncaspar® as a single agent or in combination with multi-agent chemotherapy. The re-induction response rate was 50% (95% confidence interval: 35%, 65%), based upon 36% complete remissions and 14% partial remissions. These results were similar to the overall response rates reported for patients with ALL receiving second-line, native E. coli L-asparaginase-containing re-induction chemotherapy. Anti-tumor activity was also observed with single-agent Oncaspar®. Three responses (1 complete remission and 2 partial remissions) were observed in 9 adult and pediatric patients with relapsed ALL and hypersensitivity to native E. coli L-asparaginase.
16 HOW SUPPLIED/STORAGE AND HANDLING
Oncaspar® (pegaspargase) is supplied as a sterile solution in Type I single-use vials containing 3,750 International Units of L-asparaginase per 5 mL solution (NDC 54482-301-01).
Store Oncaspar® under refrigeration at 2°C to 8ºC (36°F to 46°F). Do not shake or freeze product. Protect from light. Do not use Oncaspar® after the expiration date on the vial.
17 PATIENT COUNSELING INFORMATION
17.1 Serious Allergic Reactions
- Inform patients of the possibility of serious allergic reactions, including anaphylaxis, and to seek immediate medical care for any swellings or difficulty breathing.
PRINCIPAL DISPLAY PANEL - CARTON LABEL
Carton Label
NDC 54482-301-01
PEGASPARGASE
ONCASPAR®
Injection
3750 International
Units Per 5 mL
(750 International
Units Per mL)
For intravenous or intramuscular
use. Single-use vial. Discard
unused portion.
Rx ONLY
DOSAGE: See package insert for
complete prescribing
information.
Store at 2-8°C (36-46°F). Do
not freeze or shake.
Store in carton to protect from
light.
Sigma-Tau
Pharmaceuticals, Inc.,
9841 Washingtonian Blvd.
Gaithersburg, MD 20878
U.S. License No. 1850
ACTIVE INGREDIENTS:
Contains 6.5 mg of L-asparaginase protein
(conjugated to multiple 5kDa mPEGs) per mL.
E.coli is used in the manufacture of the
product.
INACTIVE INGREDIENTS:
Dibasic Sodium Phosphate.............5.58 mg
Monobasic Sodium Phosphate.........1.2 mg
Sodium Chloride.................................8.5 mg
Water for Injection.....................qs to 1.0 mL
No U.S. Standard of Potency
Contains no preservative.
| ONCASPAR
pegaspargase injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Sigma-Tau Pharmaceuticals, Inc. (068301431) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sigma-Tau PharmaSource, Inc. | 961822389 | MANUFACTURE(54482-301) | |