ZUPLENZ
-
ondansetron film, soluble
Par Pharmaceutical, Inc.
----------
|
|||||||||||||||||||||
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Prevention of Nausea and Vomiting Associated With Highly Emetogenic Cancer Chemotherapy
ZUPLENZ (ondansetron) oral soluble film is indicated for the prevention of nausea and vomiting associated with highly emetogenic cancer chemotherapy, including cisplatin ≥50 mg/m 2[see Clinical Studies (14.1)]
1.2 Prevention of Nausea and Vomiting Associated With Moderately Emetogenic Cancer Chemotherapy
ZUPLENZ is indicated for the prevention of nausea and vomiting associated with initial and repeat courses of moderately emetogenic cancer chemotherapy [see Clinical Studies (14.1)].
1.3 Prevention of Nausea and Vomiting Associated With Radiotherapy
ZUPLENZ is indicated for the prevention of nausea and vomiting associated with radiotherapy in patients receiving either total body irradiation, single high-dose fraction to the abdomen, or daily fractions to the abdomen [see Clinical Studies (14.2)].
1.4 Prevention of Postoperative Nausea and/or Vomiting
ZUPLENZ is indicated for the prevention of postoperative nausea and/or vomiting. As with other antiemetics, routine prophylaxis is not recommended for patients in whom there is little expectation that nausea and/or vomiting will occur postoperatively. In patients where nausea and/or vomiting must be avoided postoperatively, ZUPLENZ is recommended even where the incidence of postoperative nausea and/or vomiting is low [see Clinical Studies (14.3)].
2 DOSAGE AND ADMINISTRATION
2.1 Prevention of Nausea and Vomiting Associated With Highly Emetogenic Cancer Chemotherapy
The recommended adult oral dosage of ZUPLENZ (ondansetron) oral soluble film is 24 mg given successively as three 8 mg films administered 30 minutes before the start of single-day highly emetogenic chemotherapy, including cisplatin ≥50 mg/m 2. Each ZUPLENZ oral soluble film should be allowed to dissolve completely before administering the next film. [see Dosage and Administration (2.6)]. Multiday, single-dose administration of a 24 mg dosage has not been studied.
Safety and effectiveness of ZUPLENZ in pediatric patients have not been established for this indication.
2.2 Prevention of Nausea and Vomiting Associated With Moderately Emetogenic Cancer Chemotherapy
The recommended adult oral dosage is one 8 mg ZUPLENZ oral soluble film given twice a day. The first dose should be administered 30 minutes before the start of emetogenic chemotherapy, with a subsequent dose 8 hours after the first dose. One 8 mg ZUPLENZ oral soluble film should be administered twice a day (every 12 hours) for 1 to 2 days after completion of chemotherapy [see Dosage and Administration (2.6)].
For pediatric patients 12 years of age and older, the dosage is the same as for adults. For pediatric patients 4 through 11 years of age, the dosage is one 4 mg ZUPLENZ oral soluble film given three times a day. The first dose should be administered 30 minutes before the start of emetogenic chemotherapy, with subsequent doses 4 and 8 hours after the first dose. One 4 mg ZUPLENZ oral soluble film should be administered three times a day (every 8 hours) for 1 to 2 days after completion of chemotherapy [see Dosage and Administration (2.6)].
2.3 Prevention of Nausea and Vomiting Associated With Radiotherapy
The recommended adult oral dosage of ZUPLENZ oral soluble film is one 8 mg film given three times a day [see Dosage and Administration (2.6)].
For total body irradiation, one 8 mg ZUPLENZ oral soluble film should be administered 1 to 2 hours before each fraction of radiotherapy administered each day.
For single high-dose fraction radiotherapy to the abdomen, one 8 mg ZUPLENZ oral soluble film should be administered 1 to 2 hours before radiotherapy, with subsequent doses every 8 hours after the first dose for 1 to 2 days after completion of radiotherapy.
For daily fractionated radiotherapy to the abdomen, one 8 mg ZUPLENZ oral soluble film should be administered 1 to 2 hours before radiotherapy, with subsequent doses every 8 hours after the first dose for each day radiotherapy is given.
Safety and effectiveness of ZUPLENZ in pediatric patients have not been established for this indication.
2.4 Prevention of Postoperative Nausea and/or Vomiting
The recommended adult oral dosage of ZUPLENZ oral soluble film is 16 mg given successively as two 8 mg films 1 hour before induction of anesthesia. Each ZUPLENZ oral soluble film should be allowed to dissolve completely before administering the next film [see Dosage and Administration (2.6)].
Safety and effectiveness of ZUPLENZ in pediatric patients have not been established for this indication.
2.5 Dosage Adjustment for Patients with Impaired Hepatic Function
In patients with severe hepatic impairment (Child-Pugh score of 10 or greater) 2, clearance is reduced and apparent volume of distribution is increased with a resultant increase in plasma half-life [see Clinical Pharmacology (12.3)]. In such patients, a total daily dose of 8 mg should not be exceeded.
2.6 Important Administration Instructions
With dry hands, fold the pouch along the dotted line to expose the tear notch. While still folded, tear the pouch carefully along the edge and remove the ZUPLENZ oral soluble film from the pouch. Immediately place the film on top of the tongue where it dissolves in 4 to 20 seconds. Once the ZUPLENZ oral soluble film is dissolved, swallow with or without liquid [see Clinical Pharmacology (12.3)]. Wash hands after taking ZUPLENZ.
3 DOSAGE FORMS AND STRENGTHS
ZUPLENZ (ondansetron) oral soluble film is available in 4 mg and 8mg strengths. The thin white opaque films are rectangularly shaped strips with a printed identifier in black ink of “4 mg” for ZUPLENZ 4 mg or “8 mg” for ZUPLENZ 8mg.
4 CONTRAINDICATIONS
The concomitant use of apomorphine with ondansetron is contraindicated based on reports of profound hypotension and loss of consciousness when apomorphine was administered with ondansetron.
ZUPLENZ (ondansetron) oral soluble film is contraindicated for patients known to have hypersensitivity to the drug. Anaphylactic reactions have been reported in patients taking ondansetron.
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity
Hypersensitivity reactions, including anaphylaxis and bronchospasm, have been reported in patients who have exhibited hypersensitivity to other selective 5-HT 3 receptor antagonists.
5.2 Electrocardiographic Changes
Rarely and predominantly with intravenous ondansetron, transient electrocardiographic changes, including QT interval prolongation, have been reported.
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The following adverse events have been reported in clinical trials of patients treated with ondansetron, the active ingredient of ZUPLENZ. A causal relationship to therapy with ondansetron was unclear in many cases.
Chemotherapy-Induced Nausea and Vomiting
| Adverse Event | Ondansetron 24 mg once daily N=300 | Ondansetron 8 mg twice a day N=124 | Ondansetron 32 mg once daily N=117 |
| Headache | 33 (11%) | 16 (13%) | 17 (15%) |
| Diarrhea | 13 (4%) | 9 (7%) | 3 (3%) |
| Adverse Event | Ondansetron 8 mg twice daily N=242 | Ondansetron 8 mg three times day. N=415 | Placebo N=262 |
| Headache | 58 (24%) | 113 (27%) | 34 (13%) |
| Malaise/fatigue | 32 (13%) | 37 (9%) | 6 (2%) |
| Constipation | 22 (9%) | 26 (6%) | 1 (<1%) |
| Diarrhea | 15 (6%) | 16 (4%) | 10 (4%) |
Central Nervous System: There have been rare reports consistent with, but not diagnostic of, extrapyramidal reactions in patients receiving ondansetron.
Hepatic: In 723 patients receiving cyclophosphamide-based chemotherapy in US clinical trials, AST and/or ALT values have been reported to exceed twice the upper limit of normal in approximately 1% to 2% of patients receiving ondansetron HCl tablets. The increases were transient and did not appear to be related to dose or duration of therapy. On repeat exposure, similar transient elevations in transaminase values occurred in some courses, but symptomatic hepatic disease did not occur. The role of cancer chemotherapy in these biochemical changes cannot be clearly determined. There have been reports of liver failure and death in patients with cancer receiving concurrent medications including potentially hepatotoxic cytotoxic chemotherapy and antibiotics. The etiology of the liver failure is unclear.
Integumentary: Rash has occurred in approximately 1% of patients receiving ondansetron.
Other: Rare cases of anaphylaxis, bronchospasm, tachycardia, angina (chest pain), hypokalemia, electrocardiographic alterations, vascular occlusive events, and grand mal seizures have been reported. Except for bronchospasm and anaphylaxis, the relationship to ondansetron was unclear.
Radiation-Induced Nausea and Vomiting
The adverse events reported in patients receiving ondansetron HCl tablets and concurrent radiotherapy were similar to those reported in patients receiving ondansetron HCl tablets and concurrent chemotherapy. The most frequently reported adverse events were headache, constipation, and diarrhea.
Postoperative Nausea and Vomiting
6.2 Postmarketing Experience
The following events have been identified during post-approval use of ondansetron. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The events have been chosen for inclusion due to a combination of their seriousness, frequency of reporting, or potential causal connection to ondansetron.
Cardiovascular: Rarely and predominantly with intravenous ondansetron, transient ECG changes including QT interval prolongation have been reported.
General: Flushing. Rare cases of hypersensitivity reactions, sometimes severe (e.g., anaphylaxis reactions, angioedema, bronchospasm, shortness of breath, hypotension, laryngeal edema, stridor) have also been reported. Laryngospasm, shock, and cardiopulmonary arrest have occurred during allergic reactions in patients receiving injectable ondansetron.
Hepatobiliary: Liver enzyme abnormalities
Neurology: Oculogyric crisis, appearing alone, as well as with other dystonic reactions
Eye Disorders: Cases of transient blindness, predominantly during intravenous administration, have been reported. These cases of transient blindness were reported to resolve within a few minutes up to 48 hours.
7 DRUG INTERACTIONS
Ondansetron does not itself appear to induce or inhibit the cytochrome P-450 drug-metabolizing enzyme system of the liver [see Clinical Pharmacology (12.3)]. Because ondansetron is metabolized by hepatic cytochrome P-450 drug-metabolizing enzymes (CYP3A4, CYP2D6, CYP1A2), inducers or inhibitors of these enzymes may change the clearance and, hence, the half-life of ondansetron. On the basis of available data, no dosage adjustment is recommended for patients on these drugs.
7.1 Apomorphine
Based on reports of profound hypotension and loss of consciousness when apomorphine was administered with ondansetron, the concomitant use of apomorphine with ondansetron is contraindicated [see Contraindications (4)].
7.2 Phenytoin, Carbamazepine, Rifampicin
In patients treated with potent inducers of CYP3A4 (i.e., phenytoin, carbamazepine, and rifampicin), the clearance of ondansetron was significantly increased and ondansetron blood concentrations were decreased. In a pharmacokinetic study of 16 epileptic patients maintained chronically on CYP3A4 inducers, carbamazepine, or phenytoin, reduction in AUC, Cmax, and T½ of ondansetron was observed. 1 However, on the basis of available data, no dosage adjustment for ondansetron is recommended for patients on these drugs. 1,3
7.3 Tramadol
Although there are no data on pharmacokinetic drug interactions between ondansetron and tramadol, data from two small studies indicate that concomitant use of ondansetron may result in reduced analgesic activity of tramadol. Patients in the studies self administered tramadol more frequently, leading to an increased cumulative dose in patient controlled administration (PCA) of tramadol. 4,5
7.4 Chemotherapy
In humans, carmustine, etoposide, and cisplatin do not affect the pharmacokinetics of ondansetron.
In a crossover study in 76 pediatric patients, intravenous ondansetron did not increase blood levels of high-dose methotrexate.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category B. Reproduction studies have been performed in pregnant rats and rabbits at daily oral doses up to 15 and 30 mg/kg/day, respectively, (approximately 8 and 30 times the human dose of 16mg/day, based on body surface area), and have revealed no evidence of impaired fertility or harm to the fetus due to ondansetron. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, ZUPLENZ (ondansetron) oral soluble film should be used during pregnancy only if clearly needed.
8.3 Nursing Mothers
Ondansetron is excreted in the milk of rats. It is not known whether ondansetron is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when ZUPLENZ oral soluble film is administered to a nursing woman.
8.4 Pediatric Use
Little information is available about dosage in pediatric patients less than 4 years of age. For dosage recommendations in the prevention of nausea and vomiting associated with moderately emetogenic cancer chemotherapy for patients 4 years of age and older [see Dosage and Administration (2.2)]. The safety and effectiveness in pediatric patients have not been established for the following indications: prevention of nausea and vomiting associated with highly emetogenic cancer chemotherapy, prevention of nausea and vomiting associated with radiotherapy, and prevention of postoperative nausea and/or vomiting.
8.5 Geriatric Use
Of the total number of subjects enrolled in cancer chemotherapy-induced and postoperative nausea and vomiting in US- and foreign-controlled clinical trials, for which there were subgroup analyses, 938 were 65 years of age and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Dosage adjustment is not needed in patients over the age of 65 [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
The dosage recommendation is the same as for the general population. There is no experience beyond first-day administration of ondansetron.
8.7 Hepatic Impairment
In patients with severe hepatic impairment (Child-Pugh score of 10 or greater) 2, clearance is reduced and apparent volume of distribution is increased with a resultant increase in plasma half-life [see Clinical Pharmacology (12.3)]. In such patients, a total daily dose of 8 mg should not be exceeded.
9 DRUG ABUSE AND DEPENDENCE
Animal studies have shown that ondansetron is not discriminated as a benzodiazepine nor does it substitute for benzodiazepines in direct addiction studies.
10 OVERDOSAGE
There is no specific antidote for ondansetron overdose. Patients should be managed with appropriate supportive therapy. Individual intravenous doses as large as 150 mg and total daily intravenous doses as large as 252 mg have been inadvertently administered without significant adverse events. These doses are more than 10 times the recommended daily dose.
In addition to the adverse events listed above, the following events have been described in the setting of ondansetron overdose: “Sudden blindness” (amaurosis) of 2 to 3 minutes’ duration plus severe constipation occurred in 1 patient that was administered 72 mg of ondansetron intravenously as a single dose. Hypotension (and faintness) occurred in a patient that took 48 mg of ondansetron HCl tablets. Following infusion of 32 mg over only a 4-minute period, a vasovagal episode with transient second-degree heart block was observed. In all instances, the events resolved completely.
11 DESCRIPTION
ZUPLENZ (ondansetron) oral soluble film is a white opaque orally dissolving film designed to be applied on top of the tongue where it will dissolve in 4 to 20 seconds and then is swallowed with saliva.
ZUPLENZ does not require water to aid dissolution or swallowing.
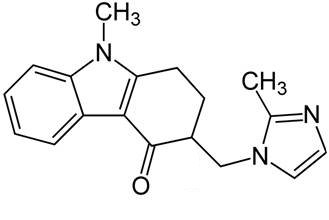
The active ingredient in ZUPLENZ is ondansetron base, the racemic form of ondansetron, and a selective blocking agent of the serotonin 5-HT 3 receptor type. Chemically it is (±) 1, 2, 3, 9-tetrahydro-9-methyl-3-[(2-methyl-1H-imidazol-1-yl)methyl]-4H-carbazol-4-one.
The empirical formula is C 18H19N3O representing a molecular weight of 293.3. Each 4 mg ZUPLENZ oral soluble film for oral administration contains 4 mg ondansetron base. Each 8 mg ZUPLENZ oral soluble film for oral administration contains 8 mg ondansetron base. Each ZUPLENZ oral soluble film also contains the inactive ingredients butylated hydroxyltoluene, calcium carbonate, colloidal silicon dioxide, erythritol, hydroxypropyl methylcellulose, monoammonium glycyrrhizinate, peppermint flavor, polyethylene oxide, sodium bicarbonate, sucralose, titanium dioxide and xanthan gum.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action Section
Ondansetron is a selective 5-HT 3 receptor antagonist. While its mechanism of action has not been fully characterized, ondansetron is not a dopamine-receptor antagonist. Serotonin receptors of the 5-HT3 type are present both peripherally on vagal nerve terminals and centrally in the chemoreceptor trigger zone of the area postrema. It is not certain whether ondansetron’s antiemetic action is mediated centrally, peripherally, or in both sites. However, cytotoxic chemotherapy appears to be associated with release of serotonin from the enterochromaffin cells of the small intestine. In humans, urinary 5-HIAA (5-hydroxyindoleacetic acid) excretion increases after cisplatin administration in parallel with the onset of emesis. The released serotonin may stimulate the vagal afferents through the 5-HT3 receptors and initiate the vomiting reflex.
12.2 Pharmacodynamics
In normal volunteers, single intravenous doses of 0.15 mg/kg of ondansetron had no effect on esophageal motility, gastric motility, lower esophageal sphincter pressure, or small intestinal transit time. Multiday administration of ondansetron has been shown to slow colonic transit in normal volunteers. Ondansetron has no effect on plasma prolactin concentrations.
12.3 Pharmacokinetics
Ondansetron is well absorbed from the gastrointestinal tract and undergoes some first-pass metabolism. After a single dose of ZUPLENZ (ondansetron) oral soluble film 8 mg under fasting conditions (n=46), the peak plasma concentrations were achieved in 1.3 hours and the mean elimination half-life was 4.6 hours in healthy subjects. The mean (±S.D.) C max and AUC were 37.28 (±14.9) ng/mL and 225 (±88.1) ng•h/mL, respectively. In the same study, mean ondansetron Cmax and AUC following administration of 8 mg ZUPLENZ oral soluble film were comparable to those after 8 mg ondansetron ODT (orally disintegrating tablet). The systemic exposure after administration of ZUPLENZ oral soluble film 8 mg with or without water was found to be comparable.
In a study using ondansetron tablets, ondansetron systemic exposure did not increase proportionately to dose. AUC from a 16 mg tablet was 24% greater than predicted from an 8 mg tablet dose. This may reflect some reduction of first-pass metabolism at higher oral doses.
When ZUPLENZ 8 mg was administered with a high fat meal, the mean time to peak plasma concentration (T max) was delayed by approximately 1 hour while AUC was similar to that under fasting conditions. Under the same fed conditions, both Cmax and AUC were comparable between ZUPLENZ 8 mg and ondansetron ODT 8 mg.
Plasma protein binding of ondansetron as measured in vitro was 70% to 76% over the concentration range of 10 to 500 ng/mL. Circulating drug also distributes into erythrocytes.
Ondansetron is extensively metabolized in humans, with approximately 5% of a radiolabeled dose recovered as the parent compound from the urine. The primary metabolic pathway is hydroxylation on the indole ring followed by subsequent glucuronide or sulfate conjugation. Although some nonconjugated metabolites have pharmacologic activity, these are not found in plasma at concentrations likely to significantly contribute to the biological activity of ondansetron. The metabolites are observed in the urine.
In vitro metabolism studies have shown that ondansetron is a substrate for human hepatic cytochrome P-450 enzymes, including CYP1A2, CYP2D6, and CYP3A4. In terms of overall ondansetron turnover, CYP3A4 played the predominant role. Because of the multiplicity of metabolic enzymes capable of metabolizing ondansetron, it is likely that inhibition or loss of one enzyme (e.g., CYP2D6 genetic deficiency) will be compensated by others and may result in little change in overall rates of ondansetron elimination. Ondansetron elimination may be affected by cytochrome P-450 inducers.
Gender differences were shown in the disposition of ondansetron given as a single dose. The extent and rate of ondansetron's absorption is greater in women than men. It is not known whether these gender-related differences were clinically important.
| Gender | Mean Weight (kg) | n | Cmax (ng/mL) | Tmax (h) | T 1/2 (h) | AUC (h•ng/mL) |
| M F | 62 56.7 | 39 7 | 35.2 49.1 | 1.67 1.7 | 4.54 5.39 | 207 323 |
A reduction in clearance and increase in elimination half-life are seen in patients over 75 years of age. In clinical trials with cancer patients, safety and efficacy was similar in patients over 65 years of age and those under 65 years of age; there was an insufficient number of patients over 75 years of age to permit conclusions in that age-group. No dosage adjustment is recommended in the elderly.
In patients with mild-to-moderate hepatic impairment, clearance is reduced 2-fold and mean half-life is increased to 11.6 hours compared to 5.7 hours in healthy subjects. In patients with severe hepatic impairment (Child-Pugh score of 10 or greater) 2, clearance is reduced 2-fold to 3-fold and apparent volume of distribution is increased with a resultant increase in half-life to 20 hours. In patients with severe hepatic impairment, a total daily dose of 8 mg should not be exceeded.
Due to the very small contribution (5%) of renal clearance to the overall clearance, renal impairment was not expected to significantly influence the total clearance of ondansetron. However, ondansetron oral mean plasma clearance was reduced by about 50% in patients with severe renal impairment (creatinine clearance <30 mL/min). This reduction in clearance is variable and was not consistent with an increase in half-life. No reduction in dose or dosing frequency in these patients is warranted.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenic effects were not seen in 2-year studies in rats and mice with oral ondansetron doses up to 10 mg/kg/day and 30 mg/kg/day, respectively (approximately 5 and 8 times the human dose of 16 mg/day, based on body surface area). Ondansetron was not mutagenic in standard tests for mutagenicity. Oral administration of ondansetron up to 15 mg/kg/day (approximately 8 times the human dose of 16 mg/day, based on body surface area) did not affect fertility or general reproductive performance of male and female rats.
14 CLINICAL STUDIES
The clinical efficacy of ondansetron, the active ingredient of ZUPLENZ, was assessed in clinical trials as described below.
14.1 Chemotherapy-Induced Nausea and Vomiting
Highly Emetogenic Chemotherapy
In 2 randomized, double-blind, monotherapy trials, a single 24 mg ondansetron HCl tablet was superior to a relevant historical placebo control in the prevention of nausea and vomiting associated with highly emetogenic cancer chemotherapy, including cisplatin ≥50 mg/m 2. Steroid administration was excluded from these clinical trials. More than 90% of patients receiving a cisplatin dose ≥50 mg/m2 in the historical placebo comparator experienced vomiting in the absence of antiemetic therapy.
The first trial compared oral doses of ondansetron 24 mg once a day, 8 mg twice a day, and 32 mg once a day in 357 adult cancer patients receiving chemotherapy regimens containing cisplatin ≥50 mg/m 2. A total of 66% of patients in the ondansetron 24 mg once-a-day group, 55% in the ondansetron 8 mg twice-a-day group, and 55% in the ondansetron 32 mg once-a-day group completed the 24-hour study period with no emetic episodes and no rescue antiemetic medications, the primary endpoint of efficacy. Each of the 3 treatment groups was shown to be statistically significantly superior to a historical placebo control.
In the same trial, 56% of patients receiving oral ondansetron 24 mg once a day experienced no nausea during the 24-hour study period, compared with 36% of patients in the oral ondansetron 8-mg twice-a-day group (p = 0.001) and 50% in the oral ondansetron 32-mg once-a-day group.
In a second trial, efficacy of the oral ondansetron 24-mg once-a-day regimen in the prevention of nausea and vomiting associated with highly emetogenic cancer chemotherapy, including cisplatin ≥50 mg/m 2, was confirmed.
Moderately Emetogenic Chemotherapy
In 1 double-blind US study in 67 patients, ondansetron HCl tablets 8 mg administered twice a day were significantly more effective than placebo in preventing vomiting induced by cyclophosphamide-based chemotherapy containing doxorubicin. Treatment response is based on the total number of emetic episodes over the 3-day study period. The results of this study are summarized in Table 5.
In 1 double-blind US study in 336 patients, ondansetron HCl tablets 8 mg administered twice a day were as effective as ondansetron HCl tablets 8 mg administered 3 times a day in preventing nausea and vomiting induced by cyclophosphamide-based chemotherapy containing either methotrexate or doxorubicin.
Treatment response is based on the total number of emetic episodes over the 3-day study period. The results of this study are summarized in Table 6.
In uncontrolled trials, 148 patients receiving cyclophosphamide-based chemotherapy were re-treated with ondansetron HCl tablets 8 mg three times daily during subsequent chemotherapy for a total of 396 re-treatment courses. No emetic episodes occurred in 314 (79%) of the re-treatment courses, and only 1 to 2 emetic episodes occurred in 43 (11%) of the re-treatment courses.
Three open-label, uncontrolled, foreign trials have been performed with 182 pediatric patients 4 to 18 years old with cancer who were given a variety of cisplatin or non-cisplatin regimens. In these foreign trials, the initial dose of ondansetron HCl injection ranged from 0.04 to 0.87 mg/kg for a total dose of 2.16mg to 12 mg. This was followed by the administration of ondansetron HCl tablets ranging from 4mg to 24 mg daily for 3 days. In these studies, 58% of the 170 evaluable patients had a complete response (no emetic episodes) on day 1. Two studies showed the response rates for patients less than 12 years of age who received ondansetron HCl tablets 4 mg three times a daily to be similar to those in patients 12 to 18 years of age who received ondansetron HCl tablets 8 mg three times daily. Thus, prevention of emesis in these pediatric patients was essentially the same as for patients older than 18 years of age. Overall, ondansetron HCl tablets were well tolerated in these pediatric patients.
14.2 Radiation-Induced Nausea and Vomiting
In a randomized, double-blind study in 20 patients, ondansetron HCl tablets (8 mg given 1.5 hours before each fraction of radiotherapy for 4 days) were significantly more effective than placebo in preventing vomiting induced by total body irradiation. Total body irradiation consisted of 11 fractions (120 cGy per fraction) over 4 days for a total of 1,320 cGy. Patients received 3 fractions for 3 days, then 2 fractions on day 4.
Single High-Dose Fraction Radiotherapy
Ondansetron was significantly more effective than metoclopramide with respect to complete control of emesis (0 emetic episodes) in a double-blind trial in 105 patients receiving single high-dose radiotherapy (800 to 1,000 cGy) over an anterior or posterior field size of >80 cm2 to the abdomen. Patients received the first dose of ondansetron HCl tablets (8 mg) or metoclopramide (10 mg) 1 to 2 hours before radiotherapy. If radiotherapy was given in the morning, 2 additional doses of study treatment were given (1 tablet late afternoon and 1 tablet before bedtime). If radiotherapy was given in the afternoon, patients took only 1 further tablet that day before bedtime. Patients continued the oral medication on a three times daily basis for 3 days.
Daily Fractionated Radiotherapy
Ondansetron was significantly more effective than prochlorperazine with respect to complete control of emesis (0 emetic episodes) in a double-blind trial in 135 patients receiving a 1- to 4-week course of fractionated radiotherapy (180 cGy doses) over a field size of >100 cm 2 to the abdomen. Patients received the first dose of ondansetron HCl tablets (8 mg) or prochlorperazine (10 mg) 1 to 2 hours before the patient received the first daily radiotherapy fraction, with 2 subsequent doses on a three times a day basis. Patients continued the oral medication on a three times daily basis on each day of radiotherapy.
14.3 Postoperative Nausea and Vomiting
Surgical patients who received ondansetron 1 hour before the induction of general balanced anesthesia (barbiturate: thiopental, methohexital, or thiamylal; opioid: alfentanil, sufentanil, morphine, or fentanyl; nitrous oxide; neuromuscular blockade: succinylcholine/curare or gallamine and/or vecuronium, pancuronium, or atracurium; and supplemental isoflurane or enflurane) were evaluated in 2 double-blind studies (1 US study, 1 foreign) involving 865 patients. Ondansetron HCl tablets (16 mg) were significantly more effective than placebo in preventing postoperative nausea and vomiting.
The study populations in all trials thus far consisted of women undergoing inpatient surgical procedures. No studies have been performed in males. No controlled clinical study comparing ondansetron HCl tablets to ondansetron injection has been performed.
15 REFERENCES
- Britto MR, Hussey EK, Mydlow P, et al. Effect of enzyme inducers on ondansetron (OND) metabolism in humans. Clin Pharmacol Ther. 1997;61:228.
- Pugh RNH, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Brit J Surg. 1973;60:646-649.
- Villikka K, Kivisto KT, Neuvonen PJ. The effect of rifampin on the pharmacokinetics of oral and intravenous ondansetron. Clin Pharmacol Ther. 1999;65:377-381.
- De Witte JL, Schoenmaekers B, Sessler DI, et al. Anesth Analg. 2001;92:1319-1321.
- Arcioni R, della Rocca M, Romanò R, et al. Anesth Analg. 2002;94:1553-1557.
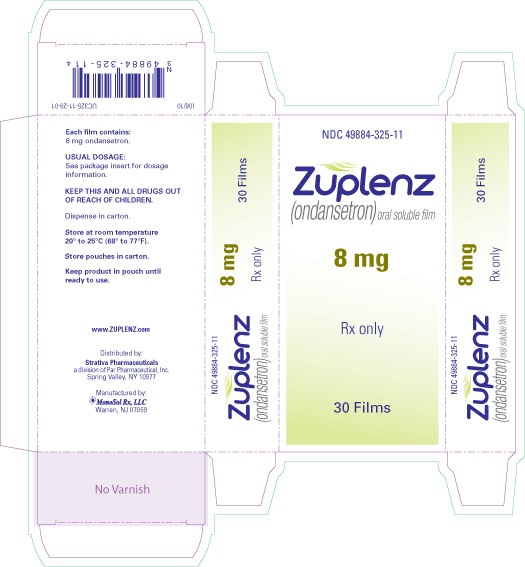
16 HOW SUPPLIED / STORAGE AND HANDLING
ZUPLENZ (ondansetron) oral soluble film 4 mg and ZUPLENZ (ondansetron) oral soluble film 8 mg, are supplied as thin rectangular white opaque films in individual foil-foil sealed child resistant pouches. Individual films are identified by “4 mg” or “8 mg”, according to the respective strengths, which is printed using pharmaceutical grade edible ink.
Individual pouches of ZUPLENZ 4 mg oral soluble film (NDC 49884-324-52) are packaged in boxes of 10 (NDC 49884-324-62).
Individual pouches of ZUPLENZ 8 mg oral soluble film (NDC 49884-325-52) are packaged in boxes of 10 (NDC 49884-325-62).
Store at controlled room temperature 20° to 25°C (68° to 77°F). Store pouches in cartons. Keep product in pouch until ready to use.
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Patient Labeling
17.1 Instructions for use
Advise patients to carefully read the “Patient Information” and “Instructions for Use” accompanying each package of ZUPLENZ (ondansetron) oral soluble film.
Inform patients that ZUPLENZ film may cause headache, malaise/fatigue, constipation, and diarrhea. The patient should report the use of all medications, especially apomorphine, to their health care provider. Concomitant use of apomorphine and ondansetron may cause a significant drop in blood pressure and loss of consciousness.
Inform patients that ZUPLENZ may cause hypersensitivity reactions, some as severe as anaphylaxis and bronchospasm. The patient should report any hypersensitivity reactions to this and other 5-HT 3 receptor antagonists to their health care provider.
Instruct patients on how to use ZUPLENZ films:
The patient should keep the film in the pouch until ready to use and not chew or swallow the film. With dry hands, the patient should fold the pouch along the dotted line to expose the tear notch. While still folded, the patient should tear the pouch carefully along the edge and remove the ZUPLENZ oral soluble film from the pouch. The patient should immediately place the film on top of the tongue where it dissolves in 4 to 20 seconds, and then swallow with saliva. Once the film dissolves, the patient may swallow liquid but it is not required. The patient should wash his hands after taking ZUPLENZ.
PATIENT INFORMATION
Read the Patient Information that comes with ZUPLENZ before you start taking it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your doctor about your medical condition or treatment.
ZUPLENZ is a prescription medicine that is used in adults to prevent nausea and vomiting:
- Caused by certain cancer chemotherapy medicines, radiation therapy to your stomach-area (abdomen), or radiation therapy to your entire body.
- that may happen after surgery
In children aged 4 years and older, ZUPLENZ is only used to prevent nausea and vomiting due to certain cancer chemotherapy medicines.
It is not known if ZUPLENZ is safe and works in children to prevent nausea and vomiting with radiation therapy, or nausea and vomiting that may happen after surgery in children.
Do not take ZUPLENZ if you take apomorphine hydrochloride (Apokyn).
Do not take ZUPLENZ if youhave had an allergic reaction to ZUPLENZ orare allergic to any of its ingredients. See the end of this leaflet for a complete list of ingredients in ZUPLENZ.
Ask your doctor if you are not sure.
What should I tell my doctor before taking ZUPLENZ?
- have liver problems
- have any other medical conditions
- are pregnant or plan to become pregnant. It is not known if ZUPLENZ will harm your unborn baby.
- are breastfeeding or plan to breastfeed. It is not known if ZUPLENZ passes into your breast milk.
Before you take ZUPLENZ oral soluble film, tell you doctor if you:
Tell your doctor about all the medicines you take, including prescription and non-prescription, vitamins, and herbal supplements. Some medicines may affect how ZUPLENZ works, and ZUPLENZ may affect how other medicines work. Using ZUPLENZ with certain other medicines may cause serious side effects. Especially tell your doctor if you take:
- apomorphine hydrochloride (Apokyn)
- tramadol hydrochloride (Ultram, Ultram ER, Ryzolt)
- another medicine for nausea and vomiting
Ask your doctor or pharmacist if you are not sure if your medicine is listed above.
Know the medicines you take. Keep a list of them to show to your doctor or pharmacist each time you start a new medicine.
Take ZUPLENZ exactly as your doctor tells you to take it.
- An adult should help a young child use this medicine.
- See the “Instructions for Use” at the end of this leaflet.
What are the possible side effects of ZUPLENZ ?
ZUPLENZ may cause serious side effects, including:
- severe allergic reactions. Stop taking ZUPLENZ and tell your doctor right away if you have any of these signs or symptoms of an allergic reaction with ZUPLENZ:
- rash
- hives
- itching
- trouble breathing
- chest tightness or chest pain
- swelling of your mouth, face, lips, or tongue
The most common side effects of ZUPLENZ are:
- headache
- tiredness and body discomfort
- constipation
- diarrhea
These are not all the possible side effects of ZUPLENZ. For more information, ask your doctor or your pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
- Store ZUPLENZ at room temperature, 68°F to 77°F (20°C to 25°C).
- Keep the film in the foil pouch until ready to use. Keep foil pouches in the carton.
- Use the film strip right away, after you take it from the pouch.
Keep ZUPLENZ and all medicines out of the reach of children.
General information about ZUPLENZ
Medicines are sometimes used for purposes other than those listed in Patient Information leaflets. Do not use ZUPLENZ for a condition for which it was not prescribed. Do not give ZUPLENZ to other people, even if they have the same condition that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about ZUPLENZ. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about ZUPLENZ that is written for healthcare professionals. You can also visit www.ZUPLENZ.com or call 1-800-828-9393.
What are the ingredients in ZUPLENZ ?
Active ingredient: ondansetron
Inactive ingredients: butylated hydroxytoluene, calcium carbonate, colloidal silicon dioxide, erythritol, hydroxypropyl methylcellulose, monoammonium glycyrrhizinate, peppermint flavor, polyethylene oxide, sodium bicarbonate, sucralose, titanium oxide and xanthan gum.
Strativa Pharmaceuticals, a division of Par Pharmaceutical, Inc.
©2010 Par Pharmaceutical, Inc.
1. Keep the film in the foil pouch until ready to use. Use the film right away, after you take it from the pouch.
2. Make sure your hands are dry.
3. Fold the pouch along the dotted line to expose the tear notch. See Figure A.
4. While still folded, tear the pouch carefully along the edge. See Figure B.
5. Take the ZUPLENZ film strip from the pouch. See Figure C.
6. Put the ZUPLENZ film on top of your tongue, where it will dissolve in 4 to 20 seconds. See Figure D.
7. Do not chew or swallow the film whole.
8. Swallow after the film dissolves. You may swallow the dissolved film with or without liquid.
9. Wash your hands after taking ZUPLENZ.
Strativa Pharmaceuticals, a division of Par Pharmaceutical, Inc.
| ZUPLENZ
ondansetron film, soluble |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA022524 | 07/05/2010 | 07/31/2012 |
| ZUPLENZ
ondansetron film, soluble |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Marketing Information | |||
| Marketing Category | Application Number or Monograph Citation | Marketing Start Date | Marketing End Date |
| NDA | NDA022524 | 07/05/2010 | 11/30/2012 |
| Labeler - Par Pharmaceutical, Inc. (092733690) |
| Registrant - Par Pharmaceutical, Inc (092733690) |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| MonoSol Rx | 785935235 | manufacture | |
| Establishment | |||
| Name | Address | ID/FEI | Operations |
| Lancaster Laboratories | 069777290 | analysis | |
Revised: 12/2012 Par Pharmaceutical, Inc.