LAMISIL- terbinafine hydrochloride granule
Novartis Pharmaceuticals Corporation
----------
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use LAMISIL® Oral Granules safely and effectively. See full prescribing information for LAMISIL Oral Granules.
LAMISIL® (terbinafine hydrochloride) oral granules, for oral use Initial U.S. Approval: 1992 INDICATIONS AND USAGELAMISIL Oral Granules are an allylamine antifungal indicated for the treatment of tinea capitis in patients 4 years of age and older. (1) DOSAGE AND ADMINISTRATIONPrior to administering, evaluate patients for evidence of chronic or active liver disease. (2.1) Take once a day with food for 6 weeks (dose based on body weight). The entire contents of each packet of granules should be sprinkled on a spoonful of non-acidic food (for example, pudding or mashed potatoes) and swallowed in its entirety. (2.2)
DOSAGE FORMS AND STRENGTHSOral Granules, 125 mg or 187.5 mg (terbinafine base equivalent) per packet. (3) CONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONSCommon (greater than 3% in patients treated with LAMISIL Oral Granules) reported adverse events include: nasopharyngitis, headache, pyrexia, cough, vomiting, upper respiratory tract infection, nausea, upper abdominal pain, and diarrhea. (6.1)
DRUG INTERACTIONSTerbinafine is an inhibitor of CYP450 2D6 isozyme and has an effect on metabolism of desipramine. Drug interactions have also been noted with cimetidine, fluconazole, cyclosporine, rifampin, and caffeine. (7.1) See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 3/2019 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
LAMISIL (terbinafine hydrochloride) Oral Granules are indicated for the treatment of tinea capitis in patients 4 years of age and older.
2 DOSAGE AND ADMINISTRATION
2.1 Assessment Prior to Initiation
Before administering LAMISIL Oral Granules, evaluate patients for evidence of chronic or active liver disease [see Contraindications (4) and Warnings and Precautions (5.1)].
2.2 Dosage
Take LAMISIL (terbinafine hydrochloride) Oral Granules once a day for 6 weeks based upon body weight (see Table 1). Sprinkle the contents of each packet on a spoonful of pudding or other soft, nonacidic food such as mashed potatoes and swallow the entire spoonful (without chewing); do not use applesauce or fruit-based foods. Take with food. If 2 packets (250 mg) are required with each dose, either the content of both packets may be sprinkled on 1 spoonful, or the contents of both packets may be sprinkled on 2 spoonfuls of nonacidic food as directed above.
| < 25 kg | 125 mg/day |
| 25-35 kg | 187.5 mg/day |
| > 35 kg | 250 mg/day |
3 DOSAGE FORMS AND STRENGTHS
Oral Granules, 125 mg or 187.5 mg (terbinafine base equivalent) per packet. The film-coated granules are off-white to yellowish, round, biconvex, each having a diameter of approximately 2.1 mm.
4 CONTRAINDICATIONS
LAMISIL (terbinafine hydrochloride) Oral Granules are contraindicated in patients with:
- Chronic or active liver disease [see Warnings and Precautions (5.1)]
- History of allergic reaction to oral terbinafine because of the risk of anaphylaxis [see Adverse Reactions (6.2)]
5 WARNINGS AND PRECAUTIONS
5.1 Hepatotoxicity
LAMISIL Oral Granules are contraindicated for patients with chronic or active liver disease. Before prescribing LAMISIL Oral Granules, perform liver function tests because hepatotoxicity may occur in patients with and without preexisting liver disease. Cases of liver failure, some leading to liver transplant or death, have occurred with the use of oral terbinafine during postmarketing experience in individuals with and without preexisting liver disease. In the majority of liver cases reported in association with oral terbinafine use, the patients had serious underlying systemic conditions. The severity of hepatic events and/or their outcome may be worse in patients with active or chronic liver disease. Periodic monitoring of liver function tests is recommended. Discontinue LAMISIL Oral Granules if biochemical or clinical evidence of liver injury develops.
Warn patients prescribed LAMISIL Oral Granules and/or their caregivers to report immediately to their healthcare providers any symptoms or signs of persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain or jaundice, dark urine, or pale stools. Advise patients with these symptoms to discontinue LAMISIL Oral Granules, and immediately evaluate the patient’s liver function.
5.2 Taste Disturbance Including Loss of Taste
Taste disturbance, including taste loss, has been reported with the use of oral terbinafine. It can be severe enough to result in decreased food intake, weight loss, anxiety, and depressive symptoms. Taste disturbance may resolve within several weeks after discontinuation of treatment, but may be prolonged (greater than 1 year), or may be permanent. If symptoms of a taste disturbance occur, LAMISIL Oral Granules should be discontinued.
5.3 Smell Disturbance Including Loss of Smell
Smell disturbance, including loss of smell, has been reported with the use of oral terbinafine. Smell disturbance may resolve after discontinuation of treatment, but may be prolonged (greater than one year), or may be permanent. If symptoms of a smell disturbance occur, LAMISIL Oral Granules should be discontinued.
5.4 Depressive Symptoms
Depressive symptoms have occurred during postmarketing use of oral terbinafine. Prescribers should be alert to the development of depressive symptoms, and patients should be instructed to report depressive symptoms to their physician.
5.5 Hematologic Effects
Transient decreases in absolute lymphocyte counts (ALCs) have been observed in controlled clinical trials. In placebo-controlled trials, 8/465 subjects receiving LAMISIL Tablets (1.7%) and 3/137 subjects receiving placebo (2.2%) had decreases in ALC to below 1000/mm3 on 2 or more occasions. In patients with known or suspected immunodeficiency, physicians should consider monitoring complete blood counts (CBCs) if treatment continues for more than 6 weeks. Cases of severe neutropenia have been reported. These were reversible upon discontinuation of oral terbinafine, with or without supportive therapy. If clinical signs and symptoms suggestive of secondary infection occur, a CBC should be obtained. If the neutrophil count is less than or equal to 1000 cells/mm3, LAMISIL Oral Granules should be discontinued and supportive management started.
5.6 Serious Skin/Hypersensitivity Reactions
There have been postmarketing reports of serious skin/hypersensitivity reactions [e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, exfoliative dermatitis, bullous dermatitis, and drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome] with oral terbinafine. Manifestations of DRESS syndrome may include cutaneous reaction (such as rash or exfoliative dermatitis), eosinophilia, and one or more organ complications such as hepatitis, pneumonitis, nephritis, myocarditis, and pericarditis. If progressive skin rash or signs/symptoms of the above drug reactions occur, treatment with LAMISIL Oral Granules should be discontinued.
5.7 Lupus Erythematosus
During postmarketing experience, precipitation and exacerbation of cutaneous and systemic lupus erythematosus have been reported in patients taking oral terbinafine. Therapy should be discontinued in patients with clinical signs and symptoms suggestive of lupus erythematosus.
5.8 Thrombotic Microangiopathy
Cases of thrombotic microangiopathy (TMA), including thrombotic thrombocytopenic purpura and hemolytic uremic syndrome, some fatal, have been reported with terbinafine. Discontinue terbinafine if clinical symptoms and laboratory findings consistent with TMA occur. The findings of unexplained thrombocytopenia and anemia should prompt further evaluation and consideration of diagnosis of TMA.
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
LAMISIL (terbinafine hydrochloride) Oral Granules
The data described below reflect exposure to terbinafine including 1042 subjects exposed for a median of 42 days. LAMISIL Oral Granules was studied in 2 active-controlled trials (n = 1042). The population was children aged 4 to 12 years old, 64% male and 36% female, 21% Caucasian, 47% Black, and 32% Other. Baseline disease (dermatophyte) characteristics of subjects included 49% having T. tonsurans, 15% T. violaceum, 15% M. canis, 2% M. audouinii, and 1% others. Subjects received once daily, for 6 weeks, oral doses of LAMISIL Oral Granules based on body weight: less than 25 kg 125 mg/day, 25-35 kg 187.5 mg/day, and greater than 35 kg 250 mg/day.
Adverse events reported in the 2 trials are listed in the table below.
| LAMISIL Oral Granules (%) N = 1042 | Griseofulvin Oral Suspension (%) N = 507 |
|
| Nasopharyngitis | 10 | 11 |
| Headache | 7 | 8 |
| Pyrexia | 7 | 6 |
| Cough | 6 | 5 |
| Vomiting | 5 | 5 |
| Upper respiratory tract infection | 5 | 5 |
| Upper abdominal pain | 4 | 4 |
| Diarrhea | 3 | 4 |
| Influenza | 2 | 1 |
| Abdominal pain | 2 | 1 |
| Pharyngolaryngeal pain | 2 | 2 |
| Nausea | 2 | 2 |
| Rash | 2 | 2 |
| Rhinorrhea | 2 | 0 |
| Nasal congestion | 2 | 1 |
| Pruritus | 1 | 1 |
| Toothache | 1 | 1 |
In the pooled pivotal trials, 2% (17/1042) of subjects in the terbinafine group and 2% (6/507) in the griseofulvin group experienced discontinuation of study drug due to adverse events. The most common categories of adverse events causing discontinuation in those exposed to terbinafine included gastrointestinal disorders, skin and subcutaneous disorders, and infections and infestations.
No ophthalmologic safety signal was identified in the pooled pivotal trials. Ophthalmologic assessments included dilated fundoscopy to assess for refractile bodies in the retina, visual acuity assessment, and color vision testing. Of the 940 subjects in the terbinafine group and 471 subjects in the griseofulvin group who completed dilated fundoscopy at posttreatment visits, none of the subjects were found to have refractile bodies of the retina at baseline or end of treatment. For visual acuity, 1% (11/837) of subjects treated with terbinafine and 2% (7/426) of subjects treated with griseofulvin showed a doubling of visual angle after 6 weeks of treatment, while 2% (15/837) treated with terbinafine and 3% (12/426) treated with griseofulvin showed a halving of the visual angle after 6 weeks of treatment. Of subjects who completed yellow-blue color vision assessment for acquired defects, 5% (13/262) of subjects treated with terbinafine and 6% (8/129) of subjects treated with griseofulvin had color confusion on more than 1 symbol at Week 6 than at baseline, while 13% (33/262) of subjects treated with terbinafine and 13% (17/129) of subjects treated with griseofulvin identified more symbols correctly at Week 6 than at baseline.
LAMISIL (terbinafine hydrochloride) Tablets
Adverse events reported in 3 US/Canadian placebo-controlled trials included diarrhea (6%), rashes (6%), dyspepsia (4%), nausea (3%), liver abnormalities (3%), pruritus (3%), taste disturbances (3%), abdominal pain (2%), and urticaria (1%).
Changes in the ocular lens and retina have been reported following the use of LAMISIL Tablets in clinical trials in adult subjects with onychomycosis. The clinical significance of these changes is unknown.
6.2 Postmarketing Experience
The following adverse events have been identified during post-approval use of oral terbinafine. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders: Pancytopenia, agranulocytosis, severe neutropenia, thrombocytopenia, anemia, thrombotic microangiopathy (TMA), including thrombotic thrombocytopenic purpura and hemolytic uremic syndrome [see Warnings and Precautions (5.5, 5.8)]
Immune system disorders: Serious hypersensitivity reactions e.g., angioedema and allergic reactions (including anaphylaxis), precipitation and exacerbation of cutaneous and systemic lupus erythematosus [see Warnings and Precautions (5.7)], serum sickness-like reaction
Psychiatric disorders: Anxiety and depressive symptoms independent of taste disturbance have been reported with oral terbinafine use. In some cases, depressive symptoms have been reported to subside with discontinuance of therapy and to recur with reinstitution of therapy [see Warnings and Precautions (5.4)].
Nervous system disorders: Cases of taste disturbance, including taste loss, have been reported with the use of oral terbinafine. It can be severe enough to result in decreased food intake, weight loss, anxiety, and depressive symptoms. Cases of smell disturbance, including smell loss, have been reported with the use of oral terbinafine [see Warnings and Precautions (5.2, 5.3)]. Cases of paresthesia and hypoesthesia have been reported with the use of oral terbinafine.
Eye disorders: Visual field defects, reduced visual acuity
Ear and labyrinth disorders: Hearing impairment, vertigo, tinnitus
Vascular disorders: Vasculitis
Gastrointestinal disorders: Pancreatitis, vomiting
Hepatobiliary disorders: Cases of liver failure some leading to liver transplant or death [see Warnings and Precautions (5.1)], idiosyncratic and symptomatic hepatic injury. Cases of hepatitis, cholestasis, and increased hepatic enzymes [see Warnings and Precautions (5.1)] have been seen with the use of oral terbinafine.
Skin and subcutaneous tissue disorders: Serious skin reactions (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, exfoliative dermatitis, bullous dermatitis, and DRESS syndrome) [see Warnings and Precautions (5.6)], acute generalized exanthematous pustulosis, psoriasiform eruptions or exacerbation of psoriasis, photosensitivity reactions, hair loss
Musculoskeletal and connective tissue disorders: Rhabdomyolysis, arthralgia, myalgia
General disorders and administration site conditions: Malaise, fatigue, influenza-like illness, pyrexia
Investigations: Altered prothrombin time (prolongation and reduction) in patients concomitantly treated with warfarin and increased blood creatine phosphokinase have been reported
7 DRUG INTERACTIONS
7.1 Drug-Drug Interactions
In vivo studies have shown that terbinafine is an inhibitor of the CYP450 2D6 isozyme. Drugs predominantly metabolized by the CYP450 2D6 isozyme include the following drug classes: tricyclic antidepressants, selective serotonin reuptake inhibitors, beta-blockers, antiarrhythmics class 1C (e.g., flecainide and propafenone) and monoamine oxidase inhibitors Type B. Coadministration of LAMISIL (terbinafine hydrochloride) Oral Granules should be done with careful monitoring and may require a reduction in dose of the 2D6-metabolized drug. In a study to assess the effects of terbinafine on desipramine in healthy volunteers characterized as normal metabolizers, the administration of terbinafine resulted in a 2-fold increase in Cmax and a 5-fold increase in area under the curve (AUC). In this study, these effects were shown to persist at the last observation at 4 weeks after discontinuation of LAMISIL. In studies in healthy subjects characterized as extensive metabolizers of dextromethorphan (antitussive drug and CYP2D6 probe substrate), terbinafine increases the dextromethorphan/dextrorphan metabolite ratio in urine by 16- to 97-fold, on average. Thus, terbinafine may convert extensive CYP2D6 metabolizers to poor metabolizer status.
In vitro studies with human liver microsomes showed that terbinafine does not inhibit the metabolism of tolbutamide, ethinylestradiol, ethoxycoumarin, cyclosporine, cisapride and fluvastatin. In vivo drug-drug interaction studies conducted in healthy volunteer subjects showed that terbinafine does not affect the clearance of antipyrine or digoxin. Terbinafine decreases the clearance of caffeine by 19%. Terbinafine increases the clearance of cyclosporine by 15%.
The influence of terbinafine on the pharmacokinetics of fluconazole, cotrimoxazole (trimethoprim and sulfamethoxazole), zidovudine or theophylline was not considered to be clinically significant.
Coadministration of a single dose of fluconazole (100 mg) with a single dose of terbinafine resulted in a 52% and 69% increase in terbinafine Cmax and AUC, respectively. Fluconazole is an inhibitor of CYP2C9 and CYP3A enzymes. Based on this finding, it is likely that other inhibitors of both CYP2C9 and CYP3A4 (e.g., ketoconazole, amiodarone) may also lead to a substantial increase in the systemic exposure (Cmax and AUC) of terbinafine when concomitantly administered.
There have been spontaneous reports of increase or decrease in prothrombin times in patients concomitantly taking oral terbinafine and warfarin, however, a causal relationship between terbinafine and these changes has not been established.
Terbinafine clearance is increased 100% by rifampin, a CYP450 enzyme inducer, and decreased 33% by cimetidine, a CYP450 enzyme inhibitor. Terbinafine clearance is unaffected by cyclosporine. There is no information available from adequate drug-drug interaction studies with the following classes of drugs: oral contraceptives, hormone replacement therapies, hypoglycemics, phenytoins, thiazide diuretics, and calcium channel blockers.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from postmarketing cases on the use of oral terbinafine in pregnant women are insufficient to evaluate a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
In animal reproduction studies, terbinafine did not cause malformations or any harm to the fetus when administered to pregnant rabbits and rats during the period of organogenesis at oral doses up to 12 and 23 times the Maximum Recommended Human Dose (MRHD), respectively (see Data).
All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. The background risk of major birth defects and miscarriage for the indicated population is unknown; however, in the U.S. general population, the estimated background risk of major birth defects is 2%-4% and of miscarriage is 15%-20% of clinically recognized pregnancies.
Data
Animal Data
In embryo-fetal development studies in rats and rabbits, pregnant animals received orally (by gavage) doses of terbinafine up to 300 mg/kg/day, during the period of organogenesis. There were no maternal or embryo-fetal effects in either species up to the maximum dose tested. The 300 mg/kg/day dose level in rats and rabbits corresponds to 23 and 12 times the MRHD [based on body surface area (BSA) comparisons], respectively.
In a rat peri- and postnatal development study, terbinafine doses of up to 300 mg/kg/day given by oral gavage during late pregnancy and lactation (Day 15 of gestation to Day 20 post-partum) had no adverse effects on parturition and lactation.
8.2 Lactation
Risk Summary
After oral administration, terbinafine is present in human milk. However, there are no data on the effects on the breastfed child or on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for LAMISIL Oral Granules and any potential adverse effects on the breastfed child from LAMISIL Oral Granules or from the underlying maternal condition.
8.4 Pediatric Use
LAMISIL Oral Granules was studied in 2 randomized, active-controlled trials in which 1021 subjects, 4 to 12 years old, having a clinical diagnosis of tinea capitis confirmed by potassium hydroxide (KOH) microscopy were treated with LAMISIL Oral Granules at the labeled dose for up to 6 weeks. The most common adverse events were nasopharyngitis, headache, pyrexia, cough, vomiting, and upper respiratory tract infection [see Adverse Reactions (6.1)].
8.6 Renal Impairment
In patients with renal impairment (creatinine clearance less than or equal to 50 mL/min) the use of LAMISIL Oral Granules has not been adequately studied.
8.7 Hepatic Impairment
LAMISIL Oral Granules are contraindicated for patients with chronic or active liver disease [see Contraindications (4) and Warnings and Precautions (5.1)]. Cases of liver failure, some leading to liver transplant or death, have occurred with the use of oral terbinafine during postmarketing experience in individuals with and without preexisting liver disease. The severity of hepatic events and/or their outcome may be worse in patients with active or chronic liver disease.
10 OVERDOSAGE
Clinical experience regarding overdose with oral terbinafine is limited. Doses up to 5 g in adults (20 times the therapeutic daily adult dose) have been reported without inducing serious adverse reactions. The symptoms of overdose included nausea, vomiting, abdominal pain, dizziness, rash, frequent urination, and headache.
11 DESCRIPTION
LAMISIL (terbinafine hydrochloride) Oral Granules 125 mg and 187.5 mg contain the synthetic allylamine antifungal compound, terbinafine hydrochloride.
Chemically, terbinafine hydrochloride is (E)-N-(6,6-dimethyl-2-hepten-4-ynyl)-N-methyl-1-naphthalenemethanamine hydrochloride. It has the empirical formula C21H26ClN with a molecular weight of 327.90, and the following structural formula:
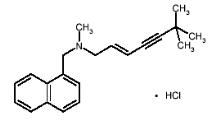
Terbinafine hydrochloride is a white to off-white fine crystalline powder. It is freely soluble in methanol and methylene chloride, soluble in ethanol, and slightly soluble in water.
Each packet of LAMISIL Oral Granules contains:
Active Ingredients: terbinafine hydrochloride (equivalent to 125 mg or 187.5 mg terbinafine base)
Inactive Ingredients: basic butylated methacrylate copolymer, colloidal silicon dioxide NF, dibutyl sebacate NF, hypromellose USP, magnesium stearate NF, microcrystalline cellulose NF, nitrogen NF (filling gas), polyethylene glycol NF, sodium lauryl sulfate NF, and sodium starch glycolate NF.
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
The pharmacodynamics of LAMISIL (terbinafine hydrochloride) Oral Granules is unknown.
12.3 Pharmacokinetics
The pharmacokinetics in children 4 to 8 years of age with tinea capitis was investigated in a pharmacokinetic study after single and repeated (for 42 days) oral administration of LAMISIL Oral Granules (N = 16), once daily, using the body weight groups and doses described in Section 2. The systemic exposure (Cmax and AUC0-24) of terbinafine in children had a relatively high interindividual variability (ranging from 36% to 64%). At steady state the AUC0-24 increased by a mean factor of 1.9 to 2.1 across doses. The mean (SD) effective half-life obtained from the observed accumulation was 26.7 (13.8) hours and 30.5 (9.3) hours for the 125 mg and 187.5 mg doses, respectively.
Systemic exposure to terbinafine in the children did not exceed the highest values of the systemic exposure in adults receiving repeated once daily doses of 250 mg LAMISIL (terbinafine hydrochloride) Tablets. A population pharmacokinetic evaluation of oral terbinafine that included children 4-12 years of age and adults 18-45 years of age (N = 113) found that clearance (CL/F) of terbinafine is dependent on body weight in a nonlinear manner. For a typical child of 25 kg CL/F was predicted to be 19 L/h and for a typical adult of 70 kg body weight it was predicted to be 27 L/h. Over the weight range for pediatric patients included in the analysis (14.1 kg-68 kg), the predicted CL/F ranged between 15.6-26.7 L/hr. In plasma, terbinafine is greater than 99% bound to plasma proteins. Prior to excretion, terbinafine is rapidly and extensively metabolized by at least 7 CYP isoenzymes with major contributions from CYP2C9, CYP1A2, CYP3A4, CYP2C8, and CYP2C19. No metabolites have been identified that have antifungal activity similar to terbinafine. Approximately 70% of the administered dose is eliminated in the urine. In adult patients with renal impairment (creatinine clearance less than or equal to 50 mL/min) or hepatic cirrhosis, the clearance of terbinafine is decreased by approximately 50% compared to normal volunteers.
12.4 Microbiology
Terbinafine, an allylamine antifungal, inhibits biosynthesis of ergosterol, an essential component of fungal cell membrane, via inhibition of squalene epoxidase enzyme. This results in fungal cell death primarily due to the increased membrane permeability mediated by the accumulation of high concentrations of squalene but not due to ergosterol deficiency. Depending on the concentration of the drug and the fungal species tested in vitro, terbinafine may be fungicidal. However, the clinical significance of in vitro data is unknown.
LAMISIL Oral Granules has been studied in tinea capitis [see Clinical Studies (14)].
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 28-month oral carcinogenicity study in rats, an increase in the incidence of liver tumors was observed in males at the highest dose tested, 69 mg/kg/day (2 times the MRHD based on AUC comparisons of the parent terbinafine); however, even though dose-limiting toxicity was not achieved at the highest tested dose, higher doses were not tested.
The results of a variety of in vitro (mutations in E. coli and S. typhimurium, DNA repair in rat hepatocytes, mutagenicity in Chinese hamster fibroblasts, chromosome aberration and sister chromatid exchanges in Chinese hamster lung cells), and in vivo (chromosome aberration in Chinese hamsters, micronucleus test in mice) genotoxicity tests gave no evidence of a mutagenic or clastogenic potential.
Oral reproduction studies in rats at doses up to 300 mg/kg/day (12 times the MRHD based on BSA comparisons) did not reveal any specific effects on fertility or other reproductive parameters. Intravaginal application of terbinafine hydrochloride at 150 mg/day in pregnant rabbits did not increase the incidence of abortions or premature deliveries nor affect fetal parameters.
13.2 Animal Toxicology and/or Pharmacology
A wide range of in vivo studies in mice, rats, dogs, and monkeys, and in vitro studies using rat, monkey, and human hepatocytes suggest that peroxisome proliferation in the liver is a rat-specific finding. However, other effects, including increased liver weights and activated partial thromboplastin time (APTT), occurred in dogs and monkeys at doses giving Css trough levels of the parent terbinafine 2-3 times those seen in humans at the MRHD.
In a 52-week oral toxicology study conducted in juvenile maturing dogs, increased heart and liver weights were noted in males and signs of central nervous system (CNS) disturbance including 3 cases of single episodes of seizures were noted in females at the highest dose tested, 100 mg/kg/day [19 times (males) and 10 times (females) the MRHD based on AUC comparisons of the parent terbinafine]. No treatment related findings were noted at 30 mg/kg/day [1.6 times (males) and 1.9 times (females) the MRHD based on AUC comparisons of the parent terbinafine] in this study.
14 CLINICAL STUDIES
Two randomized, multinational trials were conducted to investigate the safety and efficacy of LAMISIL (terbinafine hydrochloride) Oral Granules in the treatment of subjects 4 to 12 years old with tinea capitis. LAMISIL Oral Granules was dosed based on body weight. Griseofulvin dosed at 10–20 mg/kg was used as a comparator. Subjects were dosed for 6 weeks and followed for an additional 4 weeks.
The 2 trials enrolled 50% of subjects from the U.S. Additionally, among those with positive cultures, 65% and 54% of infections were due to T. tonsurans, and 19% and 17% due to M. canis in Studies 1 and 2, respectively.
The primary efficacy endpoint was the proportion of subjects with complete cure (negative KOH, negative culture, and absence of clinical signs of infection) at Week 10. Table 3 below lists the efficacy results for Studies 1 and 2 overall and according to the dermatophyte species (T. tonsurans, M. canis, or Other).
| Study 1 | Study 2 | ||||
| Terbinafine | Griseofulvin | Terbinafine | Griseofulvin | ||
| All Dermatophytes | (N = 411) | (N = 197) | (N = 441) | (N = 237) | |
| Complete Cure | 190 (46.2%) | 67 (34.0%) | 194 (44.0%) | 103 (43.5%) | |
| T. tonsurans | (N = 264) | (N = 131) | (N = 243) | (N = 126) | |
| Complete Cure | 148 (56.1%) | 45 (34.4%) | 116 (47.7%) | 46 (36.5%) | |
| M. canis | (N = 80) | (N = 37) | (N = 72) | (N = 45) | |
| Complete Cure | 19 (23.8%) | 13 (35.1%) | 22 (30.6%) | 23 (51.1%) | |
| Other* | (N = 67) | (N = 29) | (N = 126) | (N = 66) | |
| Complete Cure | 23 (34.2%) | 9 (31.0%) | 56 (44.4%) | 34 (51.5%) | |
| *T. violaceum, M. audouinii, T. mentagrophytes, T. rubrum, M. gypseum, and M. vanbreuseghemii. | |||||
16 HOW SUPPLIED/STORAGE AND HANDLING
LAMISIL (terbinafine hydrochloride) Oral Granules 125 mg and 187.5 mg
LAMISIL Oral Granules is supplied in cartons containing 14 laminated aluminum packets. Each packet contains approximately either 30 or 45 off-white to yellowish, round, biconvex, film-coated granules, corresponding to a single total dose of 125 mg or 187.5 mg (terbinafine base equivalent) per packet.
125 mg per packet
Carton of 14 packets………..………………………….………..NDC 0078-0499-58
Pack of 3 cartons each containing 14 packets (42 packets).........NDC 0078-0499-59
187.5 mg per packet
Carton of 14 packets………….………………………………....NDC 0078-0500-58
Pack of 3 cartons each containing 14 packets (42 packets)..........NDC 0078-0500-59
Storage conditions of LAMISIL Oral Granules 125 mg and 187.5 mg: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-Approved Medication Guide and Instructions for Use.
Patients taking LAMISIL (terbinafine hydrochloride) Oral Granules should receive the following information and instructions:
- Advise patients and/or their guardian to immediately report to their physician or get emergency help if they experience any of the following symptoms: hives, mouth sores, blistering and peeling of skin, swelling of face, lips, tongue, or throat, difficulty swallowing or breathing. LAMISIL Oral Granules treatment should be discontinued.
- Advise patients prescribed LAMISIL Oral Granules and/or their guardian to report immediately to their physician any symptoms of persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain, jaundice, dark urine, or pale stools. LAMISIL Oral Granules treatment should be discontinued.
- Advise patients and/or their guardian to report to their physician any signs of taste disturbance, smell disturbance, and/or depressive symptoms, fever, skin eruption, lymph node enlargement, erythema, scaling, loss of pigment, and unusual photosensitivity that can result in a rash. LAMISIL Oral Granules treatment should be discontinued.
- Advise patients and/or their guardian to minimize exposure to natural and artificial sunlight (tanning beds or UVA/B treatment) while using LAMISIL Oral Granules.
- Advise patients and/or their guardian to call their physician if they take too many LAMISIL Oral Granules.
- Advise patients to call their physician if they become pregnant during treatment with LAMISIL Oral Granules.
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
© Novartis
T2019-47
| This Medication Guide has been approved by the U.S. Food and Drug Administration | Revised: March 2019 | |
| MEDICATION GUIDE
LAMISIL® (lam-i-sil) (terbinafine hydrochloride) Oral Granules |
||
| What is the most important information I should know about LAMISIL Oral Granules?
LAMISIL Oral Granules may cause serious side effects, including: |
||
|
||
|
| |
| Your doctor should do a blood test to check you for liver problems before you start treatment with LAMISIL Oral Granules. Your doctor may also check you for liver problems during treatment, and tell you to stop taking LAMISIL Oral Granules if you develop liver problems. | ||
| What is LAMISIL Oral Granules?
LAMISIL Oral Granules is a prescription medicine used to treat a fungal infection of the scalp (tinea capitis) in people 4 years of age and older. It is not known if LAMISIL Oral Granules are safe and effective in children under 4 years of age for the treatment of tinea capitis. |
||
| Who should not take LAMISIL Oral Granules? Do not take LAMISIL Oral Granules if you:
|
||
| What should I tell my doctor before taking LAMISIL Oral Granules? Before taking LAMISIL Oral Granules, tell your doctor about all of your medical conditions, including if you:
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. |
||
How should I take LAMISIL Oral Granules?
|
||
|
|
|
| What should I avoid while taking LAMISIL Oral Granules?
Avoid sunlight. LAMISIL Oral Granules can make your skin sensitive to the sun and the light from sunlamps and tanning beds. You can get a severe sunburn. Use sunscreen and wear a hat and clothes that cover your skin if you have to be in sunlight. Talk to your doctor if you get sunburn. |
||
| What are the possible side effects of LAMISIL Oral Granules?
LAMISIL Oral Granules may cause serious side effects, including:
|
||
|
| |
|
||
|
||
|
| |
|
||
Also tell your doctor about any new symptoms, such as cough, chest pain, fast heartbeat, or blood in your urine.
|
||
|
| |
| These are not all of the possible side effects of LAMISIL Oral Granules. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||
How should I store LAMISIL Oral Granules?
Keep LAMISIL Oral Granules and all medicines out of the reach of children. |
||
| General information about the safe and effective use of LAMISIL Oral Granules
Medicines are sometimes prescribed for purposes other than those listed in Medication Guide. Do not use LAMISIL Oral Granules for a condition for which it was not prescribed. Do not give LAMISIL Oral Granules to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or doctor for information about LAMISIL Oral Granules that is written for health professionals. |
||
| What are the ingredients in LAMISIL Oral Granules?
Active ingredient: terbinafine hydrochloride Inactive ingredients: basic butylated methacrylate copolymer, colloidal silicon dioxide NF, dibutyl sebacate NF, hypromellose USP, magnesium stearate NF, microcrystalline cellulose NF, nitrogen NF (filling gas), polyethylene glycol NF, sodium lauryl sulfate NF, and sodium starch glycolate NF Distributed by: Novartis Pharmaceuticals Corporation East Hanover, New Jersey 07936 © Novartis T2019-48 |
||
INSTRUCTIONS FOR USE
LAMISIL® (Lam-i-sil)
(terbinafine hydrochloride) Oral Granules
- Before taking or giving a dose of LAMISIL Oral Granules, read this Instructions for Use to be sure you prepare, and take or give the Oral Granules correctly.
- Follow your doctor’s instructions for the dose of LAMISIL Oral Granules to take or give. The dose is based on your or your child’s body weight. The prescribed dose may be either 1 packet or 2 packets of LAMISIL Oral Granules.
- Ask your doctor or pharmacist if you are not sure how to prepare, take or give the prescribed dose of LAMISIL Oral Granules.
Preparing and giving a dose of LAMISIL Oral Granules for children and adults.
- Remove the prescribed number of packets (either 1 or 2) of LAMISIL Oral Granules from the carton.
- Hold the packet with the cut line on top.
- Tear the packet open along cut line, or use scissors to cut across line.
- Prepare a small amount of soft food, such as pudding or other soft, non-acidic food such as mashed potatoes. Do not use applesauce or fruit-based foods.
- Carefully pour the entire contents of the prescribed number of packets of LAMISIL Oral Granules onto the soft food.
- If your dose is 1 packet of LAMISIL Oral Granules, use 1 spoonful of soft food for your dose.
- If your dose is 2 packets of LAMISIL Oral Granules, you can either sprinkle the contents of both packets onto 1 spoonful of soft food, or you can sprinkle each packet onto a separate spoonful of soft food.
- Carefully pour the entire contents of the prescribed number of packets of LAMISIL Oral Granules onto the soft food.
- Make sure that no LAMISIL Oral Granules remain in the packet.
- Take or give all of the soft food and LAMISIL Oral Granules combination.
- Swallow combination of food and Oral Granules without chewing.
- Take with food.
- Swallow combination of food and Oral Granules without chewing.
How should I store LAMISIL Oral Granules?
- Store LAMISIL Oral Granules at room temperature between 68°F to 77°F (20°C to 25°C).
Keep LAMISIL Oral Granules and all medicines out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration. Issued: August 2016
Distributed by:
Novartis Pharmaceuticals Corporation
East Hanover, New Jersey 07936
© Novartis
T2016-71
August 2016
| LAMISIL
terbinafine hydrochloride granule |
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
| LAMISIL
terbinafine hydrochloride granule |
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||
| Labeler - Novartis Pharmaceuticals Corporation (002147023) |