TARCEVA- erlotinib hydrochloride tablet
Avera McKennan Hospital
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use TARCEVA safely and effectively. See full prescribing information for TARCEVA.
TARCEVA ® (erlotinib) tablets, for oral use Initial U.S. Approval: 2004 INDICATIONS AND USAGETARCEVA is a kinase inhibitor indicated for:
Limitations of Use:
DOSAGE AND ADMINISTRATIONDOSAGE FORMS AND STRENGTHS
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact OSI Pharmaceuticals, LLC, at 1-800-572-1932 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. DRUG INTERACTIONSUSE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION. Revised: 11/2015 |
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Non-Small Cell Lung Cancer (NSCLC)
TARCEVA is indicated for:
- The first-line treatment of patients with metastatic non-small cell lung cancer (NSCLC) whose tumors have epidermal growth factor receptor (EGFR) exon 19 deletions or exon 21 (L858R) substitution mutations as detected by an FDA-approved test [see Clinical Studies ( 14.1)] .
- The maintenance treatment of patients with locally advanced or metastatic non-small cell lung cancer whose disease has not progressed after four cycles of platinum-based first-line chemotherapy [see Clinical Studies ( 14.2)] .
- The treatment of patients with locally advanced or metastatic non-small cell lung cancer after failure of at least one prior chemotherapy regimen [see Clinical Studies ( 14.3)] .
Limitations of use:
- TARCEVA is not recommended for use in combination with platinum-based chemotherapy [see Clinical Studies ( 14.4)] .
- Safety and efficacy of TARCEVA have not been evaluated as first-line treatment in patients with metastatic NSCLC whose tumors have EGFR mutations other than exon 19 deletions or exon 21 (L858R) substitution [see Clinical Studies ( 14.1)] .
1.2 Pancreatic Cancer
TARCEVA in combination with gemcitabine is indicated for the first-line treatment of patients with locally advanced, unresectable or metastatic pancreatic cancer [see Clinical Studies ( 14.5)] .
2 DOSAGE AND ADMINISTRATION
2.1 Patient Selection
Select patients for the first-line treatment of metastatic NSCLC with TARCEVA based on the presence of EGFR exon 19 deletions or exon 21 (L858R) substitution mutations in tumor specimens [See Clinical Studies ( 14.1)] . Information on FDA-approved tests for the detection of EGFR mutations in NSCLC is available at: http://www.fda.gov/CompanionDiagnostics
2.2 Recommended Dose – NSCLC
The recommended daily dose of TARCEVA for NSCLC is 150 mg taken on an empty stomach, i.e., at least one hour before or two hours after the ingestion of food. Treatment should continue until disease progression or unacceptable toxicity occurs.
2.3 Recommended Dose – Pancreatic Cancer
The recommended daily dose of TARCEVA for pancreatic cancer is 100 mg taken once daily in combination with gemcitabine. Take TARCEVA on an empty stomach, i.e., at least one hour before or two hours after the ingestion of food. Treatment should continue until disease progression or unacceptable toxicity occurs [see Clinical Studies ( 14.5)].
2.4 Dose Modifications
Discontinue TARCEVA for:
- Interstitial Lung Disease (ILD) [see Warnings and Precautions ( 5.1)].
- Severe hepatic toxicity that does not improve significantly or resolve within three weeks [see Warnings and Precautions ( 5.3)].
- Gastrointestinal perforation [see Warnings and Precautions ( 5.4)].
- Severe bullous, blistering or exfoliating skin conditions [see Warnings and Precautions ( 5.5)].
- Corneal perforation or severe ulceration [see Warnings and Precautions ( 5.9)].
Withhold TARCEVA:
- During diagnostic evaluation for possible ILD.
- For severe (CTCAE grade 3 to 4) renal toxicity, and consider discontinuation of TARCEVA [see Warnings and Precautions ( 5.2)].
- In patients without pre-existing hepatic impairment for total bilirubin levels greater than 3 times the upper limit of normal or transaminases greater than 5 times the upper limit of normal, and consider discontinuation of TARCEVA [see Warnings and Precautions ( 5.3)].
- In patients with pre-existing hepatic impairment or biliary obstruction for doubling of bilirubin or tripling of transaminases values over baseline and consider discontinuation of TARCEVA [see Warnings and Precautions ( 5.3)].
- For persistent severe diarrhea not responsive to medical management (e.g., loperamide).
- For severe rash not responsive to medical management.
- For keratitis of (NCI-CTC version 4.0) grade 3-4 or for grade 2 lasting more than 2 weeks [see Warnings and Precautions ( 5.9)] .
- For acute/worsening ocular disorders such as eye pain, and consider discontinuation of TARCEVA [see Warnings and Precautions ( 5.9)].
Reduce TARCEVA by 50 mg decrements:
- If severe reactions occur with concomitant use of strong CYP3A4 inhibitors [such as atazanavir, clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, troleandomycin (TAO), voriconazole, or grapefruit or grapefruit juice] or when using concomitantly with an inhibitor of both CYP3A4 and CYP1A2 (e.g., ciprofloxacin). Avoid concomitant use if possible [see Drug Interactions ( 7)].
- When restarting therapy following withholding treatment for a dose-limiting toxicity that has resolved to baseline or grade ≤ 1.
Increase TARCEVA by 50 mg increments as tolerated for:
- Concomitant use with CYP3A4 inducers, such as rifampin, rifabutin, rifapentine, phenytoin, carbamazepine, phenobarbital, or St. John’s Wort. Increase doses by 50 mg increments at 2 week intervals to a maximum of 450 mg. Avoid concomitant use, if possible [see Drug Interactions ( 7)].
- Concurrent cigarette smoking. Increase by 50 mg increments at 2 week intervals to a maximum of 300 mg. Immediately reduce the dose of TARCEVA to the recommended dose (150 mg or 100 mg daily) upon cessation of smoking [see Drug Interactions ( 7) and Clinical Pharmacology ( 12.3)] .
Drugs Affecting Gastric pH
- Avoid concomitant use of TARCEVA with proton pump inhibitors if possible. Separation of doses may not eliminate the interaction since proton pump inhibitors affect the pH of the upper GI tract for an extended period.
- If treatment with an H 2-receptor antagonist such as ranitidine is required, TARCEVA must be taken 10 hours after the H 2-receptor antagonist dosing and at least 2 hours before the next dose of the H 2-receptor antagonist.
- Although the effect of antacids on erlotinib pharmacokinetics has not been evaluated, the antacid dose and the TARCEVA dose should be separated by several hours, if an antacid is necessary.
3 DOSAGE FORMS AND STRENGTHS
25 mg tablets
White film-coated tablets for daily oral administration. Round, biconvex face and straight sides, white film-coated, printed in orange with a “T” and “25” on one side and plain on the other side.
100 mg tablets
White film-coated tablets for daily oral administration. Round, biconvex face and straight sides, white film-coated, printed in gray with “T” and “100” on one side and plain on the other side.
150 mg tablets
White film-coated tablets for daily oral administration. Round, biconvex face and straight sides, white film-coated, printed in maroon with “T” and “150” on one side and plain on the other side.
5 WARNINGS AND PRECAUTIONS
5.1 Interstitial Lung Disease (ILD)
Cases of serious ILD, including fatal cases, can occur with TARCEVA treatment. The overall incidence of ILD in approximately 32,000 TARCEVA-treated patients in uncontrolled studies and studies with concurrent chemotherapy was approximately 1.1%. In patients with ILD, the onset of symptoms was between 5 days to more than 9 months (median 39 days) after initiating TARCEVA therapy.
Withhold TARCEVA for acute onset of new or progressive unexplained pulmonary symptoms such as dyspnea, cough, and fever pending diagnostic evaluation. If ILD is confirmed, permanently discontinue TARCEVA [see Dosage and Administration ( 2.4)] .
5.2 Renal Failure
Hepatorenal syndrome, severe acute renal failure including fatal cases, and renal insufficiency can occur with TARCEVA treatment. Renal failure may arise from exacerbation of underlying baseline hepatic impairment or severe dehydration. The pooled incidence of severe renal impairment in the 3 monotherapy lung cancer studies was 0.5% in the TARCEVA arms and 0.8% in the control arms. The incidence of renal impairment in the pancreatic cancer study was 1.4% in the TARCEVA plus gemcitabine arm and 0.4% in the control arm. Withhold TARCEVA in patients developing severe renal impairment until renal toxicity is resolved. Perform periodic monitoring of renal function and serum electrolytes during TARCEVA treatment [see Adverse Reactions ( 6.1) and Dosage and Administration ( 2.4)] .
5.3 Hepatotoxicity with or without Hepatic Impairment
Hepatic failure and hepatorenal syndrome, including fatal cases, can occur with TARCEVA treatment in patients with normal hepatic function; the risk of hepatic toxicity is increased in patients with baseline hepatic impairment. In clinical studies where patients with moderate to severe hepatic impairment were excluded, the pooled incidence of hepatic failure in the 3 monotherapy lung cancer studies was 0.4% in the TARCEVA arms and 0% in the control arms. The incidence of hepatic failure in the pancreatic cancer study was 0.4% in the TARCEVA plus gemcitabine arm and 0.4% in the control arm. In a pharmacokinetic study in 15 patients with moderate hepatic impairment (Child-Pugh B) associated with significant liver tumor burden, 10 of these 15 patients died within 30 days of the last TARCEVA dose. One patient died from hepatorenal syndrome, 1 patient died from rapidly progressing liver failure and the remaining 8 patients died from progressive disease. Six out of the 10 patients who died had baseline total bilirubin > 3 x ULN.
Perform periodic liver testing (transaminases, bilirubin, and alkaline phosphatase) during treatment with TARCEVA. Increased frequency of monitoring of liver function is required for patients with pre-existing hepatic impairment or biliary obstruction. Withhold TARCEVA in patients without pre-existing hepatic impairment for total bilirubin levels greater than 3 times the upper limit of normal or transaminases greater than 5 times the upper limit of normal. Withhold TARCEVA in patients with pre-existing hepatic impairment or biliary obstruction for doubling of bilirubin or tripling of transaminases values over baseline. Discontinue TARCEVA in patients whose abnormal liver tests meeting the above criteria do not improve significantly or resolve within three weeks [see Dosage and Administration ( 2.4) and Clinical Pharmacology ( 12.3)].
5.4 Gastrointestinal Perforation
Gastrointestinal perforation, including fatal cases, can occur with TARCEVA treatment. Patients receiving concomitant anti-angiogenic agents, corticosteroids, NSAIDs, or taxane-based chemotherapy, or who have prior history of peptic ulceration or diverticular disease may be at increased risk of perforation [see Adverse Reactions ( 6.1, 6.2)] . The pooled incidence of gastrointestinal perforation in the 3 monotherapy lung cancer studies was 0.2% in the TARCEVA arms and 0.1% in the control arms. The incidence of gastrointestinal perforation in the pancreatic cancer study was 0.4% in the TARCEVA plus gemcitabine arm and 0% in the control arm. Permanently discontinue TARCEVA in patients who develop gastrointestinal perforation [see Dosage and Administration ( 2.4)] .
5.5 Bullous and Exfoliative Skin Disorders
Bullous, blistering and exfoliative skin conditions, including cases suggestive of Stevens-Johnson syndrome/Toxic epidermal necrolysis, which in some cases were fatal, can occur with TARCEVA treatment [see Adverse Reactions ( 6.1, 6.2)] . The pooled incidence of bullous and exfoliative skin disorders in the 3 monotherapy lung cancer studies was 1.2% in the TARCEVA arms and 0% in the control arms. The incidence of bullous and exfoliative skin disorders in the pancreatic cancer study was 0.4% in the TARCEVA plus gemcitabine arm and 0% in the control arm. Discontinue TARCEVA treatment if the patient develops severe bullous, blistering or exfoliating conditions [see Dosage and Administration ( 2.4)] .
5.6 Myocardial Infarction/Ischemia
In the pancreatic carcinoma trial, six patients (incidence of 2.1%) in the TARCEVA/gemcitabine group developed myocardial infarction/ischemia. One of these patients died due to myocardial infarction. In comparison, 3 patients in the placebo/gemcitabine group developed myocardial infarction (incidence 1.1%), and one died due to myocardial infarction. The pooled incidence of myocardial infarction/ischemia in the 3 monotherapy lung cancer studies was 0.2% in the TARCEVA arms and 0.4% in the control arms.
5.7 Cerebrovascular Accident
In the pancreatic carcinoma trial, seven patients in the TARCEVA/gemcitabine group developed cerebrovascular accidents (incidence: 2.5%). One of these was hemorrhagic and was the only fatal event. In comparison, in the placebo/gemcitabine group there were no cerebrovascular accidents. The pooled incidence of cerebrovascular accident in the 3 monotherapy lung cancer studies was 0.6% in the TARCEVA arms and 0.9% in the control arms.
5.8 Microangiopathic Hemolytic Anemia with Thrombocytopenia
The pooled incidence of microangiopathic hemolytic anemia with thrombocytopenia in the 3 monotherapy lung cancer studies was 0% in the TARCEVA arms and 0.1% in the control arms. The incidence of microangiopathic hemolytic anemia with thrombocytopenia in the pancreatic cancer study was 1.4% in the TARCEVA plus gemcitabine arm and 0% in the control arm.
5.9 Ocular Disorders
Decreased tear production, abnormal eyelash growth, keratoconjunctivitis sicca or keratitis can occur with TARCEVA treatment and can lead to corneal perforation or ulceration [see Adverse Reactions ( 6.1) and ( 6.2)] . The pooled incidence of ocular disorders in the 3 monotherapy lung cancer studies was 17.8% in the TARCEVA arms and 4% in the control arms. The incidence of ocular disorders in the pancreatic cancer study was 12.8% in the TARCEVA plus gemcitabine arm and 11.4% in the control arm. Interrupt or discontinue TARCEVA therapy if patients present with acute or worsening ocular disorders such as eye pain [see Dosage and Administration ( 2.4)] .
5.10 Hemorrhage in Patients Taking Warfarin
Severe and fatal hemorrhage associated with International Normalized Ratio (INR) elevations can occur when TARCEVA and warfarin are administered concurrently. Regularly monitor prothrombin time and INR during TARCEVA treatment in patients taking warfarin or other coumarin-derivative anticoagulants [see Adverse Reactions ( 6.1) and Drug Interactions ( 7)] .
5.11 Embryo-Fetal Toxicity
Based on its mechanism of action, TARCEVA can cause fetal harm when administered to a pregnant woman. When given during organogenesis, erlotinib administration resulted in embryo-fetal lethality and abortion in rabbits at doses approximately 3 times the recommended human daily dose of 150 mg. If TARCEVA is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus [see Use in Specific Populations ( 8.1)] .
Advise females of reproductive potential to use highly effective contraception during therapy, and for at least 2 weeks after the last dose of TARCEVA. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking TARCEVA [see Use in Specific Populations ( 8.1) and ( 8.6)] .
6 ADVERSE REACTIONS
The following serious adverse reactions, which may include fatalities, are discussed in greater detail in other sections of the labeling:
- Interstitial Lung Disease (ILD) [see Warnings and Precautions ( 5.1)]
- Renal Failure [see Warnings and Precautions ( 5.2)]
- Hepatotoxicity with or without Hepatic Impairment [see Warnings and Precautions ( 5.3)]
- Gastrointestinal Perforation [see Warnings and Precautions ( 5.4)]
- Bullous and Exfoliative Skin Disorders [see Warnings and Precautions ( 5.5)]
- Myocardial Infarction/Ischemia [see Warnings and Precautions ( 5.6)]
- Cerebrovascular Accident [see Warnings and Precautions ( 5.7)]
- Microangiopathic Hemolytic Anemia with Thrombocytopenia [see Warnings and Precautions ( 5.8)]
- Ocular Disorders [see Warnings and Precautions ( 5.9)]
- Hemorrhage in Patients Taking Warfarin [see Warnings and Precautions ( 5.10)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Safety evaluation of TARCEVA is based on more than 1200 cancer patients who received TARCEVA as monotherapy, more than 300 patients who received TARCEVA 100 or 150 mg plus gemcitabine, and 1228 patients who received TARCEVA concurrently with other chemotherapies. The most common adverse reactions with TARCEVA are rash and diarrhea usually with onset during the first month of treatment. The incidences of rash and diarrhea from clinical studies of TARCEVA for the treatment of NSCLC and pancreatic cancer were 70% for rash and 42% for diarrhea.
Non-Small Cell Lung Cancer
First-Line Treatment of Patients with EGFR Mutations
The most frequent (≥ 30%) adverse reactions in TARCEVA-treated patients were diarrhea, asthenia, rash, cough, dyspnea and decreased appetite. In TARCEVA-treated patients the median time to onset of rash was 15 days and the median time to onset of diarrhea was 32 days.
The most frequent Grade 3-4 adverse reactions in TARCEVA-treated patients were rash and diarrhea.
Dose interruptions or reductions due to adverse reactions occurred in 37% of TARCEVA-treated patients, and 14.3% of TARCEVA-treated patients discontinued therapy due to adverse reactions. In TARCEVA-treated patients, the most frequently reported adverse reactions leading to dose modification were rash (13%), diarrhea (10%), and asthenia (3.6%).
Selected, common adverse reactions in Study 4, occurring in at least 10% of patients who received TARCEVA or chemotherapy and an increase in ≥ 5% in the TARCEVA treated group, are summarized by NCI-CTC (version 3.0) Grade in Table 1. The median duration of TARCEVA treatment was 9.6 months in Study 4.
|
||||
|
TARCEVA
|
Chemotherapy* N = 83 |
|||
|
MedDRA Preferred Term |
All Grades % |
Grades 3-4 % |
All Grades % |
Grades 3-4 % |
|
Rash † |
85 |
14 |
5 |
0 |
|
Diarrhea |
62 |
5 |
21 |
1 |
|
Cough |
48 |
1 |
40 |
0 |
|
Dyspnea |
45 |
8 |
30 |
4 |
|
Dry skin |
21 |
1 |
2 |
0 |
|
Back pain |
19 |
2 |
5 |
0 |
|
Chest pain |
18 |
1 |
12 |
0 |
|
Conjunctivitis |
18 |
0 |
0 |
0 |
|
Mucosal inflammation |
18 |
1 |
6 |
0 |
|
Pruritus |
16 |
0 |
1 |
0 |
|
Paronychia |
14 |
0 |
0 |
0 |
|
Arthralgia |
13 |
1 |
6 |
1 |
|
Musculoskeletal pain |
11 |
1 |
1 |
0 |
Hepatic Toxicity: One TARCEVA-treated patient experienced fatal hepatic failure and four additional patients experienced grade 3-4 liver test abnormalities in Study 4 [see Warnings and Precautions ( 5.3)] .
Maintenance Treatment
Adverse reactions, regardless of causality, that occurred in at least 3% of patients treated with single-agent TARCEVA at 150 mg and at least 3% more often than in the placebo group in the randomized maintenance trial (Study 3) are summarized by NCI-CTC (version 3.0) Grade in Table 2.
The most common adverse reactions in patients receiving single-agent TARCEVA 150 mg were rash and diarrhea. Grade 3-4 rash and diarrhea occurred in 9% and 2%, respectively, in TARCEVA-treated patients. Rash and diarrhea resulted in study discontinuation in 1% and 0.5% of TARCEVA-treated patients, respectively. Dose reduction or interruption for rash and diarrhea was needed in 5% and 3% of patients, respectively. In TARCEVA-treated patients the median time to onset of rash was 10 days, and the median time to onset of diarrhea was 15 days.
|
||||||
|
TARCEVA N = 433 |
PLACEBO N = 445 |
|||||
|
NCI-CTC Grade |
Any Grade |
Grade 3 |
Grade 4 |
Any Grade |
Grade 3 |
Grade 4 |
|
MedDRA Preferred Term |
% |
% |
% |
% |
% |
% |
|
Rash * |
60 |
9 |
0 |
9 |
0 |
0 |
|
Diarrhea |
20 |
2 |
0 |
4 |
0 |
0 |
Liver test abnormalities including ALT elevations were observed at Grade 2 or greater severity in 3% of TARCEVA-treated patients and 1% of placebo-treated patients. Grade 2 and above bilirubin elevations were observed in 5% of TARCEVA-treated patients and in < 1% in the placebo group [see Dosage and Administration ( 2.4) and Warnings and Precaution ( 5.3)] .
Second/Third Line Treatment
Adverse reactions, regardless of causality, that occurred in at least 10% of patients treated with single-agent TARCEVA at 150 mg and at least 5% more often than in the placebo group in the randomized trial of patients with NSCLC are summarized by NCI-CTC (version 2.0) Grade in Table 3.
The most common adverse reactions in this patient population were rash and diarrhea. Grade 3-4 rash and diarrhea occurred in 9% and 6%, respectively, in TARCEVA-treated patients. Rash and diarrhea each resulted in study discontinuation in 1% of TARCEVA-treated patients. Six percent and 1% of patients needed dose reduction for rash and diarrhea, respectively. The median time to onset of rash was 8 days, and the median time to onset of diarrhea was 12 days.
|
||||||
|
TARCEVA 150 mg N=485 |
Placebo N=242 |
|||||
|
NCI-CTC Grade |
Any Grade |
Grade 3 |
Grade 4 |
Any Grade |
Grade 3 |
Grade 4 |
|
MedDRA Preferred Term |
% |
% |
% |
% |
% |
% |
|
Rash * |
75 |
8 |
<1 |
17 |
0 |
0 |
|
Diarrhea |
54 |
6 |
<1 |
18 |
<1 |
0 |
|
Anorexia |
52 |
8 |
1 |
38 |
5 |
<1 |
|
Fatigue |
52 |
14 |
4 |
45 |
16 |
4 |
|
Dyspnea |
41 |
17 |
11 |
35 |
15 |
11 |
|
Nausea |
33 |
3 |
0 |
24 |
2 |
0 |
|
Infection |
24 |
4 |
0 |
15 |
2 |
0 |
|
Stomatitis |
17 |
<1 |
0 |
3 |
0 |
0 |
|
Pruritus |
13 |
<1 |
0 |
5 |
0 |
0 |
|
Dry skin |
12 |
0 |
0 |
4 |
0 |
0 |
|
Conjunctivitis |
12 |
<1 |
0 |
2 |
<1 |
0 |
|
Keratoconjunctivitis sicca |
12 |
0 |
0 |
3 |
0 |
0 |
Liver function test abnormalities (including elevated alanine aminotransferase (ALT), aspartate aminotransferase (AST) and bilirubin) were observed in patients receiving single-agent TARCEVA 150 mg. These elevations were mainly transient or associated with liver metastases. Grade 2 (> 2.5 – 5.0 x ULN) ALT elevations occurred in 4% and < 1% of TARCEVA and placebo treated patients, respectively. Grade 3 (> 5.0 – 20.0 x ULN) elevations were not observed in TARCEVA-treated patients. TARCEVA dosing should be interrupted or discontinued if changes in liver function are severe [see Dosage and Administration ( 2.4)] .
Pancreatic Cancer - TARCEVA Administered Concurrently with Gemcitabine
This was a randomized, double blind placebo-controlled study of TARCEVA (150 mg or 100 mg daily) or placebo plus gemcitabine (1000 mg/m 2 IV) in patients with locally advanced, unresectable or metastatic pancreatic cancer (Study 2). The safety population comprised 282 patients in the erlotinib group (259 in the 100 mg cohort and 23 in the 150 mg cohort) and 280 patients in the placebo group (256 in the 100 mg cohort and 24 in the 150 mg cohort).
Adverse reactions that occurred in at least 10% of patients treated with TARCEVA 100 mg plus gemcitabine in the randomized trial of patients with pancreatic cancer (Study 2) are summarized by NCI-CTC (version 2.0) Grade in Table 4.
The most common adverse reactions in pancreatic cancer patients receiving TARCEVA 100 mg plus gemcitabine were fatigue, rash, nausea, anorexia and diarrhea. In the TARCEVA plus gemcitabine arm, Grade 3-4 rash and diarrhea were each reported in 5% of patients. The median time to onset of rash and diarrhea was 10 days and 15 days, respectively. Rash and diarrhea each resulted in dose reductions in 2% of patients, and resulted in study discontinuation in up to 1% of patients receiving TARCEVA plus gemcitabine. Severe adverse reactions (≥ Grade 3 NCI-CTC) in the TARCEVA plus gemcitabine group with incidences < 5% included syncope, arrhythmias, ileus, pancreatitis, hemolytic anemia including microangiopathic hemolytic anemia with thrombocytopenia, myocardial infarction/ischemia, cerebrovascular accidents including cerebral hemorrhage, and renal insufficiency [see Warnings and Precautions ( 5)] .
The 150 mg cohort was associated with a higher rate of certain class-specific adverse reactions including rash and required more frequent dose reduction or interruption.
|
* Includes all MedDRA preferred terms in the Infections and Infestations System Organ Class
† Rash as a composite term includes: rash, palmar-plantar erythrodysaesthesia syndrome, pigmentation disorder, dermatitis acneiform, folliculitis, photosensitivity reaction, Stevens-Johnson syndrome, urticaria, erythematous rash, skin disorder, skin ulcer. |
|||||||||||||||||||||||||
|
TARCEVA + Gemcitabine 1000 mg/m 2 IV N=259 |
Placebo + Gemcitabine 1000 mg/m 2 IV N=256 |
||||||||||||||||||||||||
|
NCI-CTC Grade |
Any Grade |
Grade 3 |
Grade 4 |
Any Grade |
Grade 3 |
Grade 4 |
|||||||||||||||||||
|
MedDRA Preferred Term |
% |
% |
% |
% |
% |
% |
|||||||||||||||||||
|
Rash † |
70 |
5 |
0 |
30 |
1 |
0 |
|||||||||||||||||||
|
Diarrhea |
48 |
5 |
<1 |
36 |
2 |
0 |
|||||||||||||||||||
|
Weight decreased |
39 |
2 |
0 |
29 |
<1 |
0 |
|||||||||||||||||||
|
Infection* |
39 |
13 |
3 |
30 |
9 |
2 |
|||||||||||||||||||
|
Pyrexia |
36 |
3 |
0 |
30 |
4 |
0 |
|||||||||||||||||||
|
Stomatitis |
22 |
<1 |
0 |
12 |
0 |
0 |
|||||||||||||||||||
|
Depression |
19 |
2 |
0 |
14 |
<1 |
0 |
|||||||||||||||||||
|
Cough |
16 |
0 |
0 |
11 |
0 |
0 |
|||||||||||||||||||
|
Headache |
15 |
<1 |
0 |
10 |
0 |
0 |
|||||||||||||||||||
Ten patients (4%) in the TARCEVA/gemcitabine group and three patients (1%) in the placebo/gemcitabine group developed deep venous thrombosis. The overall incidence of grade 3 or 4 thrombotic events, including deep venous thrombosis was 11% for TARCEVA plus gemcitabine and 9% for placebo plus gemcitabine.
The incidences of liver test abnormalities (≥ Grade 2) in Study 2 are provided in Table 5[see Dosage and Administration ( 2.4) and Warnings and Precautions ( 5.3)] .
|
TARCEVA + Gemcitabine 1000 mg/m 2 IV N=259 |
Placebo + Gemcitabine 1000 mg/m 2 IV N=256 |
|||||
|
NCI-CTC Grade |
Grade 2 |
Grade 3 |
Grade 4 |
Grade 2 |
Grade 3 |
Grade 4 |
|
Bilirubin |
17% |
10% |
<1% |
11% |
10% |
3% |
|
ALT |
31% |
13% |
<1% |
22% |
9% |
0% |
|
AST |
24% |
10% |
<1% |
19% |
9% |
0% |
NSCLC and Pancreatic Indications: Selected Low Frequency Adverse Reactions
Gastrointestinal Disorders
Cases of gastrointestinal bleeding (including fatalities) have been reported, some associated with concomitant warfarin or NSAID administration
[see
Warnings and Precautions (
5.10) and
Drug Interactions (
7)]
. These adverse reactions were reported as peptic ulcer bleeding (gastritis, gastroduodenal ulcers), hematemesis, hematochezia, melena and hemorrhage from possible colitis.
6.2 Post-Marketing Experience
The following adverse reactions have been identified during post approval use of TARCEVA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Musculoskeletal and Connective Tissue Disorders: myopathy, including rhabdomyolysis, in combination with statin therapy
Eye Disorders: ocular inflammation including uveitis
7 DRUG INTERACTIONS
CYP3A4 Inhibitors
Erlotinib is metabolized predominantly by CYP3A4. Co-treatment with the potent CYP3A4 inhibitor ketoconazole increased erlotinib AUC by 67%. When TARCEVA was co-administered with ciprofloxacin, an inhibitor of both CYP3A4 and CYP1A2, the erlotinib exposure [AUC] and maximum concentration [C
max] increased by 39% and 17%, respectively. Dose modifications are recommended
[see
Dosage and Administration (
2.4)]
.
CYP3A4 Inducers
Pre-treatment with the CYP3A4 inducer rifampicin for 7-11 days prior to TARCEVA decreased erlotinib AUC by 58% to 80%. Dose modifications are recommended
[see
Dosage and Administration (
2.4)]
.
Drugs Affecting Gastric pH
Co-administration of TARCEVA with omeprazole decreased erlotinib AUC by 46% and co-administration of TARCEVA with ranitidine 300 mg decreased erlotinib AUC by 33%. When TARCEVA was administered with ranitidine 150 mg twice daily (at least 10 h after the previous ranitidine evening dose and 2 h before the ranitidine morning dose), erlotinib AUC decreased by 15%. Increasing the dose of TARCEVA when co-administered with such agents is not likely to compensate for the loss of exposure. Scheduling modifications are recommended
[see
Dosage and Administration (
2.4) and
Clinical Pharmacology (
12.3)]
.
Cigarette Smoking
Cigarette smoking results in reductions in erlotinib AUC. Dose modifications are recommended
[see
Dosage and Administration (
2.4) and
Clinical Pharmacology (
12.3)]
.
Anticoagulants
Interaction with coumarin-derived anticoagulants, including warfarin, leading to increased International Normalized Ratio (INR) and bleeding adverse reactions, which in some cases were fatal, have been reported in patients receiving TARCEVA. Regularly monitor prothrombin time or INR in patients taking coumarin-derived anticoagulants. Dose modifications of TARCEVA are not recommended
[see
Warnings and Precautions (
5.10) and
Adverse Reactions (
6.1)]
.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category D
Risk Summary
Based on its mechanism of action, TARCEVA can cause fetal harm when administered to a pregnant woman. When given during organogenesis, erlotinib administration resulted in embryo-fetal lethality and abortion in rabbits at doses approximately 3 times the recommended human daily dose of 150 mg. If TARCEVA is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus
[see
Warnings and Precautions (
5.11)]
.
Animal Data
Erlotinib has been shown to cause maternal toxicity resulting in embryo-fetal lethality and abortion in rabbits when given during the period of organogenesis at doses that result in plasma drug concentrations approximately 3 times those achieved at the recommended dose in humans (AUCs at 150 mg daily dose). During the same period, there was no increase in the incidence of embryo-fetal lethality or abortion in rabbits or rats at doses resulting in exposures approximately equal to those in humans at the recommended daily dose. In an independent fertility study female rats treated with 30 mg/m
2/day or 60 mg/m
2/day (0.3 or 0.7 times the recommended daily dose, on a mg/m
2 basis) of erlotinib had an increase in early resorptions that resulted in a decrease in the number of live fetuses.
No teratogenic effects were observed in rabbits or rats dosed with erlotinib during organogenesis at doses up to 600 mg/m 2/day in the rabbit (3 times the plasma drug concentration seen in humans at 150 mg/day) and up to 60 mg/m 2/day in the rat (0.7 times the recommended dose of 150 mg/day on a mg/m 2 basis).
8.3 Nursing Mothers
It is not known whether erlotinib is present in human milk. Because many drugs are present in human milk and because of the potential for serious adverse reactions in nursing infants from TARCEVA, a decision should be made whether to discontinue nursing or discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of TARCEVA in pediatric patients have not been established.
In an open-label, multi-center trial, 25 pediatric patients (median age 14 years, range 3-20 years) with recurrent or refractory ependymoma were randomized (1:1) to TARCEVA or etoposide. Thirteen patients received TARCEVA at a dose of 85 mg/m 2/day orally until disease progression, death, patient request or investigator decision to discontinue study drug or intolerable toxicity. Four patients randomized to etoposide also received TARCEVA following disease progression. The trial was terminated prematurely for lack of efficacy; there were no objective responses observed in these 17 TARCEVA-treated patients.
No new adverse events were identified in the pediatric population.
Based on the population pharmacokinetics analysis conducted in 105 pediatric patients (2 to 21 years old) with cancer, the geometric mean estimates of CL/F/BSA (apparent clearance normalized to body surface area) were comparable across the three age groups: 2-6 years (n=29), 7-16 years (n=59), and 17-21 years (n=17).
8.5 Geriatric Use
Of the 1297 subjects in clinical studies of TARCEVA for the treatment of NSCLC and pancreatic cancer 40% were 65 and older while 10% were 75 and older. No overall differences in safety or efficacy were observed between subjects 65 years and older and those younger than 65.
8.6 Females and Males of Reproductive Potential
Contraception
Females
Counsel patients on pregnancy planning and prevention. Advise female patients of reproductive potential to use highly effective contraception during treatment with TARCEVA, and for at least 2 weeks after the last dose of TARCEVA. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking TARCEVA
[see
Use in Specific Populations (
8.1)].
8.7 Patients with Hepatic Impairment
Patients with hepatic impairment (total bilirubin > upper limit of normal (ULN) or Child-Pugh A, B and C) should be closely monitored during therapy with TARCEVA. Treatment with TARCEVA should be used with extra caution in patients with total bilirubin > 3 x ULN [see Warnings and Precautions ( 5.3), Adverse Reactions ( 6.1, 6.2), and Dosage and Administration ( 2.4)] .
In vitro and in vivo evidence suggest that erlotinib is cleared primarily by the liver. However, erlotinib exposure was similar in patients with moderately impaired hepatic function (Child-Pugh B) compared with patients with adequate hepatic function including patients with primary liver cancer or hepatic metastases [see Dosage and Administration ( 2.4) and Clinical Pharmacology ( 12.3)] .
10 OVERDOSAGE
Single oral doses of TARCEVA up to 1,000 mg in healthy subjects and weekly doses up to 1,600 mg in cancer patients have been tolerated. Repeated twice-daily doses of 200 mg single-agent TARCEVA in healthy subjects were poorly tolerated after only a few days of dosing. Based on the data from these studies, an unacceptable incidence of severe adverse reactions, such as diarrhea, rash, and liver transaminase elevation, may occur above the recommended dose [see Dosage and Administration ( 2)]. In case of suspected overdose, TARCEVA should be withheld and symptomatic treatment instituted.
11 DESCRIPTION
TARCEVA (erlotinib), a kinase inhibitor, is a quinazolinamine with the chemical name N-(3-ethynylphenyl)-6,7-bis(2-methoxyethoxy)-4-quinazolinamine. TARCEVA contains erlotinib as the hydrochloride salt that has the following structural formula:
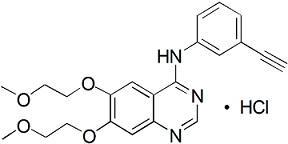
Erlotinib hydrochloride has the molecular formula C 22H 23N 3O 4.HCl and a molecular weight of 429.90. The molecule has a pK a of 5.42 at 25 oC. Erlotinib hydrochloride is very slightly soluble in water, slightly soluble in methanol and practically insoluble in acetonitrile, acetone, ethyl acetate and hexane.
Aqueous solubility of erlotinib hydrochloride is dependent on pH with increased solubility at a pH of less than 5 due to protonation of the secondary amine. Over the pH range of 1.4 to 9.6, maximal solubility of approximately 0.4 mg/mL occurs at a pH of approximately 2.
TARCEVA tablets for oral administration are available in three dosage strengths containing erlotinib hydrochloride (27.3 mg, 109.3 mg and 163.9 mg) equivalent to 25 mg, 100 mg and 150 mg erlotinib and the following inactive ingredients: lactose monohydrate, hypromellose, hydroxypropyl cellulose, magnesium stearate, microcrystalline cellulose, sodium starch glycolate, sodium lauryl sulfate and titanium dioxide. The tablets also contain trace amounts of color additives, including FD&C Yellow #6 (25 mg only) for product identification.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Epidermal growth factor receptor (EGFR) is expressed on the cell surface of both normal and cancer cells. In some tumor cells signaling through this receptor plays a role in tumor cell survival and proliferation irrespective of EGFR mutation status. Erlotinib reversibly inhibits the kinase activity of EGFR, preventing autophosphorylation of tyrosine residues associated with the receptor and thereby inhibiting further downstream signaling. Erlotinib binding affinity for EGFR exon 19 deletion or exon 21 (L858R) mutations is higher than its affinity for the wild type receptor. Erlotinib inhibition of other tyrosine kinase receptors has not been fully characterized.
12.3 Pharmacokinetics
Absorption and Distribution:
Erlotinib is about 60% absorbed after oral administration and its bioavailability is substantially increased by food to almost 100%. Peak plasma levels occur 4 hours after dosing. The solubility of erlotinib is pH dependent. Erlotinib solubility decreases as pH increases. Co-administration of TARCEVA with omeprazole, a proton pump inhibitor, decreased the erlotinib exposure [AUC] and maximum concentration [C max] by 46% and 61%, respectively. When TARCEVA was administered 2 hours following a 300 mg dose of ranitidine, an H 2 receptor antagonist, the erlotinib AUC was reduced by 33% and C max by 54%. When TARCEVA was administered with ranitidine 150 mg twice daily (at least 10 h after the previous ranitidine evening dose and 2 h before the ranitidine morning dose), the erlotinib AUC and C max decreased by 15% and 17%, respectively [see Drug Interactions ( 7) ].
Following absorption, erlotinib is approximately 93% protein bound to plasma albumin and alpha-1 acid glycoprotein (AAG). Erlotinib has an apparent volume of distribution of 232 liters.
Metabolism and Excretion:
A population pharmacokinetic analysis in 591 patients receiving the single-agent TARCEVA 2 nd/3 rd line regimen showed a median half-life of 36.2 hours. Time to reach steady state plasma concentration would therefore be 7 - 8 days. No significant relationships of clearance to covariates of patient age, body weight or gender were observed. Smokers had a 24% higher rate of erlotinib clearance.
An additional population pharmacokinetic analysis was conducted in 291 NSCLC patients administered single-agent erlotinib as maintenance treatment. This analysis demonstrated that covariates affecting erlotinib clearance in this patient population were similar to those seen in the prior single-agent pharmacokinetic analysis. No new covariate effects were identified.
A third population pharmacokinetic analysis was conducted that incorporated erlotinib data from 204 pancreatic cancer patients who received erlotinib plus gemcitabine. Similar results were observed to those seen in the prior single-agent pharmacokinetic analysis. No new covariate effects were identified. Co-administration of gemcitabine had no effect on erlotinib plasma clearance.
In vitro assays of cytochrome P450 metabolism showed that erlotinib is metabolized primarily by CYP3A4 and to a lesser extent by CYP1A2, and the extrahepatic isoform CYP1A1. Following a 100 mg oral dose, 91% of the dose was recovered: 83% in feces (1% of the dose as intact parent) and 8% in urine (0.3% of the dose as intact parent).
Cigarette smoking reduces erlotinib exposure. In the Phase 3 NSCLC trial, current smokers achieved erlotinib steady-state trough plasma concentrations which were approximately 2-fold less than the former smokers or patients who had never smoked. This effect was accompanied by a 24% increase in apparent erlotinib plasma clearance. In a separate study which evaluated the single-dose pharmacokinetics of erlotinib in healthy volunteers, current smokers cleared the drug faster than former smokers or volunteers who had never smoked. The AUC
0-infinity in smokers was about 1/3 to 1/2 of that in never/former smokers. In another study which was conducted in NSCLC patients (N=35) who were current smokers, pharmacokinetic analyses at steady-state indicated a dose-proportional increase in erlotinib exposure when the TARCEVA dose was increased from 150 mg to 300 mg. However, the exact dose to be recommended for patients who currently smoke is unknown
[see
Drug Interactions (
7) and
Patient Counseling Information (
17)
].
Special Populations:
Patients with Hepatic Impairment
Hepatic failure and hepatorenal syndrome, including fatal cases, can occur with TARCEVA treatment in patients with normal hepatic function; the risk of hepatic toxicity is increased in patients with baseline hepatic impairment. [see Warnings and Precautions ( 5.3), Adverse Reactions ( 6.1, 6.2), and Dosage and Administration ( 2.4)] .
In vitro and in vivo evidence suggest that erlotinib is cleared primarily by the liver. However, erlotinib exposure was similar in patients with moderately impaired hepatic function (Child-Pugh B) compared with patients with adequate hepatic function including patients with primary liver cancer or hepatic metastases.
Patients with Renal Impairment
Less than 9% of a single dose is excreted in the urine. No clinical studies have been conducted in patients with compromised renal function.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year carcinogenicity studies were conducted in mice and rats with erlotinib at oral doses of up to 60 mg/kg/day in mice, 5 mg/kg/day in female rats, and 10 mg/kg/day in male rats. The studies were negative for carcinogenic findings. Exposure in mice at the highest dose tested was approximately 10 times the exposure in humans at the erlotinib dose of 150 mg/day. The highest dose evaluated in male rats resulted in exposures that were twice those in humans and exposures at the highest tested dose in female rats were slightly lower than those in humans.
Erlotinib did not cause genetic damage in a series of in vitro assays (bacterial mutation, human lymphocyte chromosome aberration and mammalian cell mutation) and in the in vivo mouse bone marrow micronucleus test.
Erlotinib did not impair fertility in either male or female rats.
14 CLINICAL STUDIES
14.1 Non-Small Cell Lung Cancer (NSCLC) – First-Line Treatment of Patients with EGFR Mutations
The safety and efficacy of TARCEVA as monotherapy for the first-line treatment of patients with metastatic NSCLC containing EGFR exon 19 deletions or exon 21 (L858R) substitution mutations was demonstrated in a randomized, open-label, clinical trial conducted in Europe (Study 4). One hundred seventy-four (174) White patients were randomized 1:1 to receive erlotinib 150 mg once daily until disease progression (n=86) or four cycles of a standard platinum-based doublet chemotherapy (n=88); standard chemotherapy regimens were cisplatin plus gemcitabine, cisplatin plus docetaxel, carboplatin plus gemcitabine, and carboplatin plus docetaxel. The main efficacy outcome measure was progression-free survival (PFS) as assessed by the investigator. Randomization was stratified by EGFR mutation (exon 19 deletion or exon 21 (L858R) substitution) and ECOG PS (0 vs. 1 vs. 2). EGFR mutation status for screening and enrollment of patients was determined by a clinical trials assay (CTA). Tumor samples from 134 patients (69 patients from the erlotinib arm and 65 patients from the chemotherapy arm) were tested retrospectively by the FDA-approved companion diagnostic, the cobas® EGFR Mutation Test.
The baseline demographics of the overall study population were as follows: female (72%), white (99%), age ≥ 65 years (51%), ECOG PS 1 (53%), with ECOG PS 0 (33%), and ECOG PS 2 (14%), current smoker (11%), past-smoker (20%), and never smoker (69%). The disease characteristics were 93% stage IV and 7% Stage IIIb with pleural effusion as classified by the American Joint Commission on Cancer (AJCC, 6 th edition), 93% adenocarcinoma histology, 66% exon 19 mutation deletions and 34% exon 21 (L858R) point mutation by a CTA.
A statistically significant improvement in investigator-determined PFS was demonstrated for patients randomized to erlotinib compared to those randomized chemotherapy (see Table 6 and Figure 1). Similar results for PFS were observed for the subgroup evaluated by an independent-review committee (approximately 75% of patients in Study 4 evaluated) and in the subgroup of 134 patients (77% of the Study 4 population) with EGFR mutations confirmed by the cobas® EGFR Mutation Test.
A protocol-specified analysis of overall survival conducted at the time of the final analysis of PFS showed no statistically significant difference between the TARCEVA and chemotherapy arms. At the time of the data cut-off, 84% of patients in the chemotherapy arm had received at least one subsequent treatment, of whom 97% received an EGFR tyrosine kinase inhibitor. In the TARCEVA arm, 66% of patients had received at least one subsequent treatment.
|
||
|
Erlotinib (N = 86) |
Chemotherapy (N = 88) |
|
|
Progression-free Survival |
||
| Number of Progressions or Deaths |
71 (83%) |
63 (72%) |
| Median PFS in Months (95% CI) |
10.4 (8.7, 12.9) |
5.2 (4.6, 6.0) |
| Hazard Ratio (95% CI) * |
0.34 (0.23, 0.49) |
|
| P-value (unstratified log-rank test) |
<0.001 |
|
|
Overall Survival |
||
| Number of Deaths (%) |
55 (64%) |
54 (61%) |
| Median OS in Months (95% CI) |
22.9 (17.0, 26.8) |
19.5 (17.3, 28.4) |
| Hazard Ratio (95% CI) * |
0.93 (0.64, 1.35) |
|
|
Objective Response |
||
| Objective Response Rate (95% CI) |
65% (54.1%, 75.1%) |
16% (9.0%, 25.3%) |
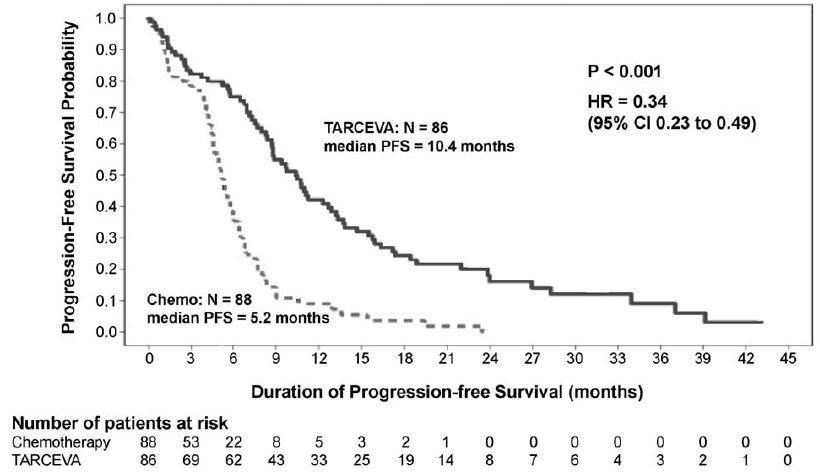 Figure 1: Kaplan-Meier Plot of Investigator-Assessed PFS in Study 4
Figure 1: Kaplan-Meier Plot of Investigator-Assessed PFS in Study 4
Figure 1: Kaplan-Meier Plot of Investigator-Assessed PFS in Study 4
In exploratory subgroup analyses based on EGFR mutation subtype, the hazard ratio (HR) for PFS was 0.27 (95% CI 0.17 to 0.43) in patients with exon 19 deletions and 0.52 (95% CI 0.29 to 0.95) in patients with exon 21 (L858R) substitution. The HR for OS was 0.94 (95% CI 0.57 to 1.54) in the exon 19 deletion subgroup and 0.99 (95% CI 0.56 to 1.76) in the exon 21 (L858R) substitution subgroup.
14.2 NSCLC - Maintenance Treatment
The efficacy and safety of TARCEVA as maintenance treatment of NSCLC were demonstrated in a randomized, double-blind, placebo-controlled trial conducted in 26 countries, in 889 patients with locally advanced or metastatic NSCLC whose disease did not progress during first-line platinum-based chemotherapy (Study 3). Patients were randomized 1:1 to receive TARCEVA 150 mg or placebo orally once daily (438 TARCEVA, 451 placebo) until disease progression or unacceptable toxicity. The primary objective of the study was to determine if the administration of TARCEVA after standard platinum-based chemotherapy in the treatment of NSCLC resulted in improved progression free survival (PFS) when compared with placebo, in all patients or in patients with EGFR immunohistochemistry (IHC) positive tumors.
Demographic characteristics were balanced between the two treatment groups.
Baseline demographics of the overall study population were as follows: male (74%), age < 65 years (66%), ECOG PS 1 (69%), ECOG PS 0 (31%), white (84%), Asian (15%), current smoker (55%), past-smoker (27%), and never smoker (17%). Disease characteristics were as follows: Stage IV (75%), Stage IIIb with effusion (25%) as classified by AJCC (6 th edition) with histologic subtypes of adenocarcinoma including bronchioalveolar (45%), squamous (40%) and large cell (5%); and EGFR IHC positive (70%), negative (14%), indeterminate (4%), and missing (12%).
|
Median in Months (95% CI) |
Hazard Ratio* (95% CI) |
p-value† |
||
|
TARCEVA 150 mg N = 438 |
Placebo N = 451 |
|||
|
Progression-Free Survival based on investigator's assessment |
2.8 (2.8, 3.1) |
2.6 (1.9, 2.7) |
0.71 (0.62, 0.82) |
p < 0.0001 |
|
Overall Survival |
12.0 (10.6, 13.9) |
11.0 (9.9, 12.1) |
0.81 (0.70, 0.95) |
0.0088 |
Figure 2 depicts the Kaplan-Meier Curves for Overall Survival (ITT Population).
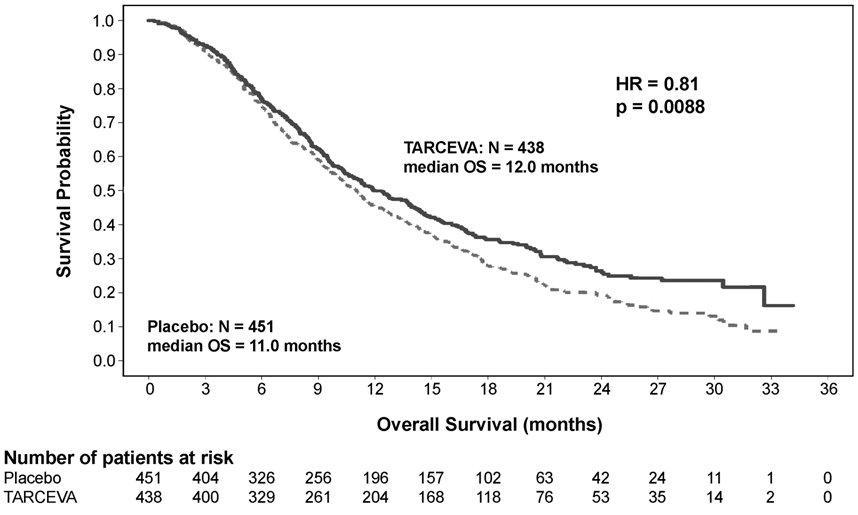
Figure 2: Kaplan - Meier Curve for Overall Survival of Patients by Treatment Group in Study 3
Figure 2: Kaplan - Meier Curve for Overall Survival of Patients by Treatment Group in Study 3
Note: HR is from a univariate Cox regression model.
The PFS and OS Hazard Ratios, respectively, in patients with EGFR IHC-positive tumors were 0.69 (95% CI: 0.58, 0.82) and 0.77 (95% CI: 0.64, 0.93). The PFS and OS Hazard Ratios in patients with IHC-negative tumors were 0.77 (95% CI: 0.51, 1.14) and 0.91 (95% CI: 0.59, 1.38), respectively.
Patients with adenocarcinoma had an OS Hazard Ratio of 0.77 (95% CI: 0.61, 0.97) and patients with squamous histology had an OS Hazard Ratio of 0.86 (95% CI: 0.68, 1.10).
14.3 NSCLC –Second/Third Line Treatment
The efficacy and safety of single-agent TARCEVA was assessed in a randomized, double blind, placebo-controlled trial in 731 patients with locally advanced or metastatic NSCLC after failure of at least one chemotherapy regimen (Study 1). Patients were randomized 2:1 to receive TARCEVA 150 mg or placebo (488 TARCEVA, 243 placebo) orally once daily until disease progression or unacceptable toxicity. Study endpoints included overall survival, response rate, and progression-free survival (PFS). Duration of response was also examined. The primary endpoint was survival. The study was conducted in 17 countries.
Baseline demographics of the overall study population were as follows: male (65%), white (78%), Asian (12%), black (4%), age < 65 years (62%), ECOG PS 1 (53%), ECOG PS 0 (13%), ECOG PS 2 (25%), ECOG PS 3 (9%), current or ex-smoker (75%), never smoker (20%), and exposure to prior platinum therapy (93%). Tumor characteristics were as follows: adenocarcinoma (50%), squamous (30%), undifferentiated large cell (9%), and mixed non-small cell (2%).
The results of the study are shown in Table 8.
|
|||||
|
TARCEVA |
Placebo |
Hazard Ratio* |
95% CI |
p-value |
|
|
Survival |
Median 6.7 mo |
Median 4.7 mo |
0.73 |
0.61 - 0.86 |
<0.001 † |
|
1-year Survival |
31.2% |
21.5% | |||
|
Progression-Free Survival |
Median 9.9 wk |
Median 7.9 wk |
0.59 |
0.50 - 0.70 |
<0.001 † |
|
Tumor Response (CR+PR) |
8.9% |
0.9% |
<0.001 ‡ |
||
|
Response Duration |
Median 34.3 wk |
Median 15.9 wk | |||
Survival was evaluated in the intent-to-treat population. Figure 3 depicts the Kaplan-Meier curves for overall survival. The primary survival and PFS analyses were two-sided Log-Rank tests stratified by ECOG performance status, number of prior regimens, prior platinum, best response to prior chemotherapy.
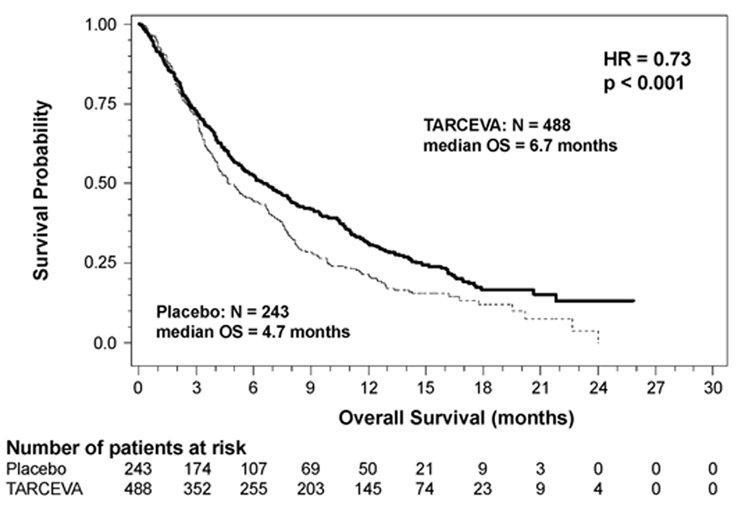 Figure 3: Kaplan - Meier Curve for Overall Survival of Patients by Treatment Group in Study 1
Figure 3: Kaplan - Meier Curve for Overall Survival of Patients by Treatment Group in Study 1
Figure 3: Kaplan - Meier Curve for Overall Survival of Patients by Treatment Group in Study 1
Note: HR is from Cox regression model with the following covariates: ECOG performance status, number of prior regimens, prior platinum, best response to prior chemotherapy. P-value is from two-sided Log-Rank test stratified by ECOG performance status, number of prior regimens, prior platinum, best response to prior chemotherapy.
14.4 NSCLC – Lack of Efficacy of TARCEVA Administered Concurrently with Chemotherapy
Results from two, multicenter, placebo-controlled, randomized, trials in over 1000 patients conducted in first-line patients with locally advanced or metastatic NSCLC showed no clinical benefit with the concurrent administration of TARCEVA with platinum-based chemotherapy [carboplatin and paclitaxel (TARCEVA, N = 526) or gemcitabine and cisplatin (TARCEVA, N = 580)].
14.5 Pancreatic Cancer - TARCEVA Administered Concurrently with Gemcitabine
The efficacy and safety of TARCEVA in combination with gemcitabine as a first-line treatment was assessed in a randomized, double blind, placebo-controlled trial in 569 patients with locally advanced, unresectable or metastatic pancreatic cancer (Study 2). Patients were randomized 1:1 to receive TARCEVA (100 mg or 150 mg) or placebo once daily on a continuous schedule plus gemcitabine IV (1000 mg/m 2, Cycle 1 - Days 1, 8, 15, 22, 29, 36 and 43 of an 8 week cycle; Cycle 2 and subsequent cycles - Days 1, 8 and 15 of a 4-week cycle [the approved dose and schedule for pancreatic cancer, see the gemcitabine package insert]). TARCEVA or placebo was taken orally once daily until disease progression or unacceptable toxicity. The primary endpoint was survival. Secondary endpoints included response rate, and progression-free survival (PFS). Duration of response was also examined. The study was conducted in 18 countries. A total of 285 patients were randomized to receive gemcitabine plus TARCEVA (261 patients in the 100 mg cohort and 24 patients in the 150 mg cohort) and 284 patients were randomized to receive gemcitabine plus placebo (260 patients in the 100 mg cohort and 24 patients in the 150 mg cohort). Too few patients were treated in the 150 mg cohort to draw conclusions.
In the 100 mg cohort, baseline demographics of the overall study population were as follows: male (52%), white (88%), Asian (7%), black (2%), age < 65 years (53%), ECOG PS 1 (51%), ECOG PS 0 (32%), and ECOG PS 2 (17%). There was a slightly larger proportion of females in the TARCEVA arm (51%) compared with the placebo arm (44%). The median time from initial diagnosis to randomization was approximately 1.0 month. The majority of the patients (76%) had distant metastases at baseline and 24% had locally advanced disease.
The results of the study are shown in Table 9.
|
TARCEVA +
|
Placebo +
|
Hazard Ratio * |
95% CI |
p-value |
|
|
Survival |
Median 6.4 mo 250 deaths |
Median 6.0 mo 254 deaths |
0.81 |
0.68 - 0.97 |
0.028 † |
|
1-year Survival |
23.8% |
19.4% | |||
|
Progression-Free Survival |
Median 3.8 mo 225 events |
Median 3.5 mo 232 events |
0.76 |
0.64 - 0.92 |
0.006 † |
|
Tumor Response (CR+PR) |
8.6% |
7.9% |
0.87 ‡ |
||
|
Response Duration |
Median 23.9 wk |
Median 23.3 wk | |||
Survival was evaluated in the intent-to-treat population. Figure 4 depicts the Kaplan-Meier curves for overall survival in the 100 mg cohort. The primary survival and PFS analyses were two-sided Log-Rank tests stratified by ECOG performance status and extent of disease.
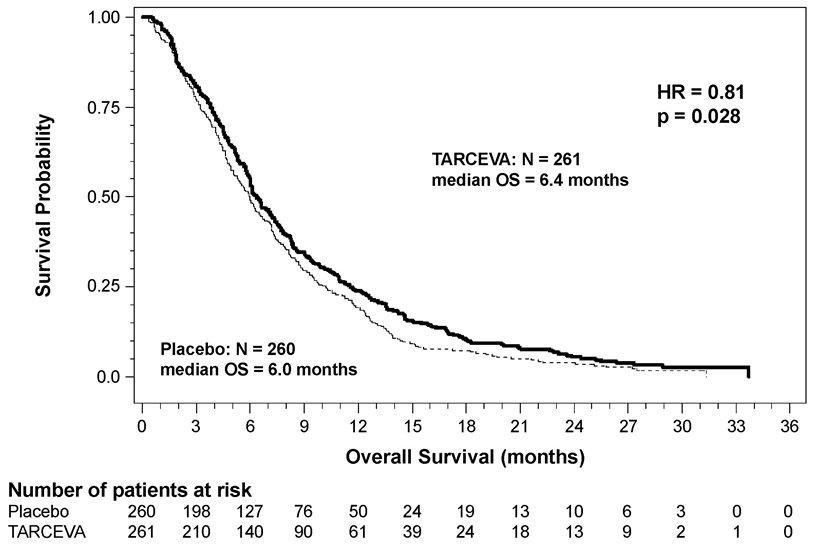 Figure 4: Kaplan - Meier Curve for Overall Survival: 100 mg Cohort in Study 2
Figure 4: Kaplan - Meier Curve for Overall Survival: 100 mg Cohort in Study 2
Figure 4: Kaplan - Meier Curve for Overall Survival: 100 mg Cohort in Study 2
Note: HR is from Cox regression model with the following covariates: ECOG performance status and extent of disease. The p-value is from two-sided Log-Rank test stratified by ECOG performance status and extent of disease.
16 HOW SUPPLIED/STORAGE AND HANDLING
100 mg Tablets
Round, biconvex face and straight sides, white film-coated, printed in gray with “T” and “100” on one side and plain on the other side; supplied in:
Bottles of 30: NDC 50242-063-01
NDC 69189-0063-1 single dose pack with one tablet as repackaged by Avera McKennan Hospital
Store at 25°C (77°F); excursions permitted to 15°C - 30°C (59°F - 86°F). See USP Controlled Room Temperature.
17 PATIENT COUNSELING INFORMATION
Advise patients to contact their health care provider for:
•Severe or persistent diarrhea, nausea, anorexia, or vomiting [see Adverse Reactions ( 6.1)] •Onset or worsening of unexplained shortness of breath or cough [see Warnings and Precautions ( 5.1)] •Eye irritation [see Warnings and Precautions ( 5.9)] •Onset or worsening of skin rash or development of bullous lesions or desquamation [see Warnings and Precautions ( 5.5)] •Any changes in smoking status [see Clinical Pharmacology ( 12.3)]
Advise patients on the presentation of skin, hair and nail disorders.
•In patients who develop skin rash, the appearance of the rash is typically erythematous and maculopapular and it may resemble acne with follicular pustules, but is histopathologically different. This skin reaction commonly occurs on the face, upper chest and back, but may be more generalized or severe (NCI-CTC Grade 3 or 4) with desquamation. Skin reactions may occur or worsen in sun exposed areas. Symptoms associated with rash may include itching, tenderness and/or burning.•Hyperpigmentation or dry skin, with or without digital skin fissures, have been reported and in the majority of cases were associated with rash.•Hair and nail disorders, including hirsutism and brittle and loose nails, have been reported.
Instruct patients on initial management of rash or diarrhea.
•Given that skin reactions are anticipated when taking TARCEVA, proactive intervention may include alcohol-free emollient cream and use of sunscreen or avoidance of sun exposure [see Adverse Reactions ( 6.1)] .•Management of rash may include topical corticosteroids or antibiotics with anti-inflammatory properties. These approaches were used in the NSCLC and pancreatic pivotal clinical trials. Acne preparations with drying properties may aggravate the dry skin and erythema. Treatment of rash has not been formally studied and should be based on rash severity.•Diarrhea can usually be managed with loperamide.
Counsel patients on pregnancy planning and prevention.
•Advise females of reproductive potential to use highly effective contraception during treatment with TARCEVA, and for at least 2 weeks after the last dose of TARCEVA.•Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, during treatment with TARCEVA [see Use in Specific Populations ( 8.1), ( 8.6)]. •Advise breast-feeding mothers to discontinue nursing while receiving TARCEVA [see Use in Specific Populations ( 8.3)] .
Advise patients to stop smoking. Advise patients that the dose of TARCEVA may need to be adjusted if they smoke. [see Clinical Pharmacology ( 12.3)] .
Manufactured for:
OSI Pharmaceuticals, LLC, Northbrook, IL 60062
an affiliate of Astellas Pharma US, Inc.
Product of Japan or Italy – See bottle label for origin
Manufactured by:
Kremers Urban Pharmaceuticals, Inc., Seymour, IN 47274
Distributed by:
Genentech USA, Inc., A Member of the Roche Group, 1 DNA Way, South San Francisco, CA 94080-4990
For further information please call 1-877-TARCEVA (1-877-827-2382).
TARCEVA is a trademark of OSI Pharmaceuticals, LLC, Northbrook, IL, 60062, USA, an affiliate of Astellas Pharma US, Inc.
©2015 Astellas Pharma US, Inc., and Genentech, Inc. All rights reserved.
14A002-TAR-SPL
| TARCEVA
erlotinib hydrochloride tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Avera McKennan Hospital (068647668) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Avera McKennan Hospital | 068647668 | relabel(69189-0063) , repack(69189-0063) | |