DILANTIN- phenytoin sodium capsule, extended release
Parke-Davis Div of Pfizer Inc
----------
DESCRIPTION
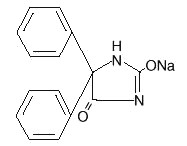
Phenytoin sodium is an antiepileptic drug. Phenytoin sodium is related to the barbiturates in chemical structure, but has a five-membered ring. The chemical name is sodium 5,5-diphenyl-2, 4-imidazolidinedione, having the following structural formula:
Each Dilantin— 100 mg (extended phenytoin sodium capsule, USP)—contains 100 mg phenytoin sodium. Also contains lactose monohydrate, NF; confectioner's sugar, NF; talc, USP; and magnesium stearate, NF. The capsule body contains titanium dioxide, USP and gelatin, NF. The capsule cap contains FD&C red No. 28; FD&C yellow No. 6; and gelatin NF. Product in vivo performance is characterized by a slow and extended rate of absorption with peak blood concentrations expected in 4 to 12 hours as contrasted to Prompt Phenytoin Sodium Capsules, USP with a rapid rate of absorption with peak blood concentration expected in 1½ to 3 hours.
CLINICAL PHARMACOLOGY
Phenytoin is an antiepileptic drug which can be used in the treatment of epilepsy. The primary site of action appears to be the motor cortex where spread of seizure activity is inhibited. Possibly by promoting sodium efflux from neurons, phenytoin tends to stabilize the threshold against hyperexcitability caused by excessive stimulation or environmental changes capable of reducing membrane sodium gradient. This includes the reduction of posttetanic potentiation at synapses. Loss of posttetanic potentiation prevents cortical seizure foci from detonating adjacent cortical areas. Phenytoin reduces the maximal activity of brain stem centers responsible for the tonic phase of tonic-clonic (grand mal) seizures.
The plasma half-life in man after oral administration of phenytoin averages 22 hours, with a range of 7 to 42 hours. Steady-state therapeutic levels are achieved at least 7 to 10 days (5–7 half-lives) after initiation of therapy with recommended doses of 300 mg/day.
When serum level determinations are necessary, they should be obtained at least 5–7 half-lives after treatment initiation, dosage change, or addition or subtraction of another drug to the regimen so that equilibrium or steady-state will have been achieved. Trough levels provide information about clinically effective serum level range and confirm patient compliance and are obtained just prior to the patient's next scheduled dose. Peak levels indicate an individual's threshold for emergence of dose-related side effects and are obtained at the time of expected peak concentration. For Dilantin capsules, peak serum levels occur 4 to 12 hours after administration.
Optimum control without clinical signs of toxicity occurs more often with serum levels between 10 and 20 mcg/mL, although some mild cases of tonic-clonic (grand mal) epilepsy may be controlled with lower serum levels of phenytoin.
In most patients maintained at a steady dosage, stable phenytoin serum levels are achieved. There may be wide interpatient variability in phenytoin serum levels with equivalent dosages. Patients with unusually low levels may be noncompliant or hypermetabolizers of phenytoin. Unusually high levels result from liver disease, congenital enzyme deficiency, or drug interactions which result in metabolic interference. The patient with large variations in phenytoin plasma levels, despite standard doses, presents a difficult clinical problem. Serum level determinations in such patients may be particularly helpful. As phenytoin is highly protein bound, free phenytoin levels may be altered in patients whose protein binding characteristics differ from normal.
Most of the drug is excreted in the bile as inactive metabolites which are then reabsorbed from the intestinal tract and excreted in the urine. Urinary excretion of phenytoin and its metabolites occurs partly with glomerular filtration but more importantly by tubular secretion. Because phenytoin is hydroxylated in the liver by an enzyme system which is saturable at high plasma levels, small incremental doses may increase the half-life and produce very substantial increases in serum levels, when these are in the upper range. The steady-state level may be disproportionately increased, with resultant intoxication, from an increase in dosage of 10% or more.
INDICATIONS AND USAGE
Dilantin is indicated for the control of generalized tonic-clonic (grand mal) and complex partial (psychomotor, temporal lobe) seizures and prevention and treatment of seizures occurring during or following neurosurgery.
Phenytoin serum level determinations may be necessary for optimal dosage adjustments (see DOSAGE AND ADMINISTRATION and CLINICAL PHARMACOLOGY sections).
CONTRAINDICATIONS
Phenytoin is contraindicated in those patients who are hypersensitive to phenytoin or its inactive ingredients or other hydantoins.
WARNINGS
Effects of Abrupt Withdrawal
Abrupt withdrawal of phenytoin in epileptic patients may precipitate status epilepticus. When, in the judgment of the clinician, the need for dosage reduction, discontinuation, or substitution of alternative antiepileptic medication arises, this should be done gradually. However, in the event of an allergic or hypersensitivity reaction, rapid substitution of alternative therapy may be necessary. In this case, alternative therapy should be an antiepileptic drug not belonging to the hydantoin chemical class.
Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including Dilantin, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5–100 years) in the clinical trials analyzed.
Table 1 shows absolute and relative risk by indication for all evaluated AEDs.
| Indication | Placebo Patients with Events Per 1000 Patients | Drug Patients with Events Per 1000 Patients | Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients | Risk Difference: Additional Drug Patients with Events Per 1000 Patients |
|---|---|---|---|---|
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing Dilantin or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Lymphadenopathy
There have been a number of reports suggesting a relationship between phenytoin and the development of lymphadenopathy (local or generalized) including benign lymph node hyperplasia, pseudolymphoma, lymphoma, and Hodgkin's disease. Although a cause and effect relationship has not been established, the occurrence of lymphadenopathy indicates the need to differentiate such a condition from other types of lymph node pathology. Lymph node involvement may occur with or without symptoms and signs resembling serum sickness, e.g., fever, rash, and liver involvement.
In all cases of lymphadenopathy, follow-up observation for an extended period is indicated and every effort should be made to achieve seizure control using alternative antiepileptic drugs.
Effects of Alcohol Use on Phenytoin Serum Levels
Acute alcoholic intake may increase phenytoin serum levels, while chronic alcohol use may decrease serum levels.
Exacerbation of Porphyria
In view of isolated reports associating phenytoin with exacerbation of porphyria, caution should be exercised in using this medication in patients suffering from this disease.
Usage In Pregnancy
Clinical
- A.
-
Risks to Mother. An increase in seizure frequency may occur during pregnancy because of altered phenytoin pharmacokinetics. Periodic measurement of plasma phenytoin concentrations may be valuable in the management of pregnant women as a guide to appropriate adjustment of dosage (see PRECAUTIONS, Laboratory Tests). However, postpartum restoration of the original dosage will probably be indicated.
- B.
-
Risks to the Fetus. If this drug is used during pregnancy, or if the patient becomes pregnant while taking the drug, the patient should be apprised of the potential harm to the fetus.
Prenatal exposure to phenytoin may increase the risks for congenital malformations and other adverse developmental outcomes. Increased frequencies of major malformations (such as orofacial clefts and cardiac defects), minor anomalies (dysmorphic facial features, nail and digit hypoplasia), growth abnormalities (including microcephaly), and mental deficiency have been reported among children born to epileptic women who took phenytoin alone or in combination with other antiepileptic drugs during pregnancy. There have also been several reported cases of malignancies, including neuroblastoma, in children whose mothers received phenytoin during pregnancy. The overall incidence of malformations for children of epileptic women treated with antiepileptic drugs (phenytoin and/or others) during pregnancy is about 10%, or two- to three-fold that in the general population. However, the relative contributions of antiepileptic drugs and other factors associated with epilepsy to this increased risk are uncertain and in most cases it has not been possible to attribute specific developmental abnormalities to particular antiepileptic drugs.
Patients should consult with their physicians to weigh the risks and benefits of phenytoin during pregnancy.
- C.
- Postpartum Period. A potentially life-threatening bleeding disorder related to decreased levels of vitamin K-dependent clotting factors may occur in newborns exposed to phenytoin in utero. This drug-induced condition can be prevented with vitamin K administration to the mother before delivery and to the neonate after birth.
Skin reactions
Dilantin can cause rare, serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson Syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. Although serious skin reactions may occur without warning, patients should be alert for the signs and symptoms of skin rash and blisters, fever, or other signs hypersensitivity such as itching, and should seek medical advice from their physician immediately when observing any indicative signs or symptoms. The physician should advise the patient to discontinue treatment if the rash appears (see WARNINGS section regarding drug discontinuation). If the rash is of a milder type (measles-like or scarlatiniform), therapy may be resumed after the rash has completely disappeared. If the rash recurs upon reinstitution of therapy, further Dilantin medication is contraindicated. Published literature has suggested that there may be an increased, although still rare, risk of hypersensitivity reactions, including skin rash, SJS, TEN, hepatotoxicity, and Anticonvulsant Hypersensitivity Syndrome in black patients.
Studies in patients of Chinese ancestry have found a strong association between the risk of developing SJS/TEN and the presence of HLA-B*1502, an inherited allelic variant of the HLA B gene, in patients using another anticonvulsive drug. Limited evidence suggests that HLA-B*1502 may be a risk factor for the development of SJS/TEN in patients of Asian ancestry taking drugs associated with SJS/TEN, including phenytoin. Consideration should be given to avoiding use of drugs associated with SJS/TEN, including Dilantin, in HLA-B*1502 positive patients when alternative therapies are otherwise equally available.
Anticonvulsant Hypersensitivity Syndrome
Anticonvulsant Hypersensitivity Syndrome (AHS) is a rare drug induced, multiorgan syndrome which is potentially fatal and occurs in some patients taking anticonvulsant medication. It is characterized by fever, rash, lymphadenopathy, and other multiorgan pathologies, often hepatic. The mechanism is unknown. The interval between first drug exposure and symptoms is usually 2–4 weeks but has been reported in individuals receiving anticonvulsants for 3 or more months. Although up to 1 in 5 patients on Dilantin may develop cutaneous eruptions, only a small proportion will progress to AHS.
Patients at higher risk for developing AHS include black patients, patients who have a family history of or who have experienced this syndrome in the past, and immuno-suppressed patients. The syndrome is more severe in previously sensitized individuals. If a patient is diagnosed with AHS, discontinue the Dilantin and provide appropriate supportive measures.
PRECAUTIONS
General
The liver is the chief site of biotransformation of phenytoin; patients with impaired liver function, elderly patients, or those who are gravely ill may show early signs of toxicity.
A small percentage of individuals who have been treated with phenytoin have been shown to metabolize the drug slowly. Slow metabolism may be due to limited enzyme availability and lack of induction; it appears to be genetically determined.
Published literature has suggested that there may be an increased, although still rare, risk of hypersensitivity reactions, including skin rash, SJS, TEN, hepatotoxicity, and Anticonvulsant Hypersensitivity Syndrome in black patients. (See WARNINGS section).
Phenytoin should be discontinued if a skin rash appears (see WARNINGS section regarding drug discontinuation). If the rash is exfoliative, purpuric, or bullous or if lupus erythematosus, Stevens-Johnson syndrome, or toxic epidermal necrolysis is suspected, use of this drug should not be resumed and alternative therapy should be considered. (See ADVERSE REACTIONS section.) If the rash is of a milder type (measles-like or scarlatiniform), therapy may be resumed after the rash has completely disappeared. If the rash recurs upon reinstitution of therapy, further phenytoin medication is contraindicated.
Phenytoin and other hydantoins are contraindicated in patients who have experienced phenytoin hypersensitivity (see CONTRAINDICATIONS). Additionally, caution should be exercised if using structurally similar compounds (e.g., barbiturates, succinimides, oxazolidinediones, and other related compounds) in these same patients.
Hyperglycemia, resulting from the drug's inhibitory effects on insulin release, has been reported. Phenytoin may also raise the serum glucose level in diabetic patients.
Phenytoin and other anticonvulsants that have been shown to induce the CYP450 enzyme are thought to affect bone mineral metabolism indirectly by increasing the metabolism of Vitamin D3. This may lead to Vitamin D deficiency and heightened risk of osteomalacia, bone fractures, osteoporosis, hypocalcemia, and hypophosphatemia in chronically treated epileptic patients.
Phenytoin is not indicated for seizures due to hypoglycemic or other metabolic causes. Appropriate diagnostic procedures should be performed as indicated.
Phenytoin is not effective for absence (petit mal) seizures. If tonic-clonic (grand mal) and absence (petit mal) seizures are present, combined drug therapy is needed.
Serum levels of phenytoin sustained above the optimal range may produce confusional states referred to as "delirium," "psychosis," or "encephalopathy," or rarely irreversible cerebellar dysfunction. Accordingly, at the first sign of acute toxicity, plasma levels are recommended. Dose reduction of phenytoin therapy is indicated if plasma levels are excessive; if symptoms persist, termination is recommended. (See WARNINGS section.)
Information for Patients
Inform patients of the availability of a Medication Guide, and instruct them to read the Medication Guide prior to taking Dilantin. Instruct patients to take Dilantin only as prescribed.
Patients taking phenytoin should be advised of the importance of adhering strictly to the prescribed dosage regimen, and of informing the physician of any clinical condition in which it is not possible to take the drug orally as prescribed, e.g., surgery, etc.
Patients should also be cautioned on the use of other drugs or alcoholic beverages without first seeking the physician's advice.
Patients should be instructed to call their physician if skin rash develops.
The importance of good dental hygiene should be stressed in order to minimize the development of gingival hyperplasia and its complications.
Patients, their caregivers, and families should be counseled that AEDs, including Dilantin, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Patients should be encouraged to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This Registry is collecting information about the safety of antiepileptics drugs during pregnancy. To enroll, patients can call the toll free number 1-888-233-2334 (see PRECAUTIONS: Pregnancy section).
Do not use capsules which are discolored.
Laboratory Tests
Phenytoin serum level determinations may be necessary to achieve optimal dosage adjustments.
Drug Interactions
There are many drugs which may increase or decrease phenytoin levels or which phenytoin may affect. Serum level determinations for phenytoin are especially helpful when possible drug interactions are suspected. The most commonly occurring drug interactions are:
- Drugs which may increase phenytoin serum levels include: acute alcohol intake, amiodarone, chloramphenicol, chlordiazepoxide, cimetidine, diazepam, dicumarol, disulfiram, estrogens, ethosuximide, fluoxetine, fluorouracil, fluvoxamine, H2-antagonists, halothane, isoniazid, methylphenidate, omeprazole, phenothiazines, phenylbutazone, salicylates, sertraline, succinimides, sulfonamides, ticlopidine, tolbutamide, trazodone.
- Drugs which may decrease phenytoin levels include: carbamazepine, chronic alcohol abuse, reserpine, and sucralfate. Moban® brand of molindone hydrochloride contains calcium ions which interfere with the absorption of phenytoin. Ingestion times of phenytoin and antacid preparations containing calcium should be staggered in patients with low serum phenytoin levels to prevent absorption problems.
- Drugs which may either increase or decrease phenytoin serum levels include: phenobarbital, sodium valproate, and valproic acid. Similarly, the effect of phenytoin on phenobarbital, teniposide, valproic acid, and sodium valproate serum levels is unpredictable.
- Although not a true drug interaction, tricyclic antidepressants may precipitate seizures in susceptible patients and phenytoin dosage may need to be adjusted.
- Drugs whose efficacy is impaired by phenytoin include: azoles, corticosteroids, coumarin anticoagulants, digitoxin, doxycycline, estrogens, furosemide, oral contraceptives, paroxetine, quinidine, rifampin, sertraline, teniposide, theophylline, vitamin D.
Drug Enteral Feeding/Nutritional Preparations Interaction
Literature reports suggest that patients who have received enteral feeding preparations and/or related nutritional supplements have lower than expected phenytoin plasma levels. It is therefore suggested that phenytoin not be administered concomitantly with an enteral feeding preparation. More frequent serum phenytoin level monitoring may be necessary in these patients.
Drug/Laboratory Test Interactions
Phenytoin may decrease serum concentrations of T4. It may also produce lower than normal values for dexamethasone or metyrapone tests. Phenytoin may cause increased serum levels of glucose, alkaline phosphatase, and gamma glutamyl transpeptidase (GGT).
Care should be taken when using immunoanalytical methods to measure plasma phenytoin concentrations.
Pregnancy
Pregnancy Category D
See WARNINGS section.
To provide information regarding the effects of in utero exposure to Dilantin, physicians are advised to recommend that pregnant patients taking Dilantin enroll in the NAAED Pregnancy Registry. This can be done by calling the toll free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
ADVERSE REACTIONS
Central Nervous System
The most common manifestations encountered with phenytoin therapy are referable to this system and are usually dose-related. These include nystagmus, ataxia, slurred speech, decreased coordination, and mental confusion. Dizziness, insomnia, transient nervousness, motor twitchings, paresthesias, somnolence and headaches have also been observed. There have also been rare reports of phenytoin-induced dyskinesias, including chorea, dystonia, tremor, and asterixis, similar to those induced by phenothiazine and other neuroleptic drugs.
A predominantly sensory peripheral polyneuropathy has been observed in patients receiving long-term phenytoin therapy.
Integumentary System
Dermatological manifestations sometimes accompanied by fever have included scarlatiniform or morbilliform rashes. A morbilliform rash (measles-like) is the most common; other types of dermatitis are seen more rarely. Other more serious forms which may be fatal have included bullous, exfoliative or purpuric dermatitis, lupus erythematosus, Stevens-Johnson syndrome, and toxic epidermal necrolysis (see PRECAUTIONS and WARNINGS section).
Hemopoietic System
Hemopoietic complications, some fatal, have occasionally been reported in association with administration of phenytoin. These have included thrombocytopenia, leukopenia, granulocytopenia, agranulocytosis, and pancytopenia with or without bone marrow suppression. While macrocytosis and megaloblastic anemia have occurred, these conditions usually respond to folic acid therapy. Lymphadenopathy including benign lymph node hyperplasia, pseudolymphoma, lymphoma, and Hodgkin's disease have been reported (see WARNINGS section).
Connective Tissue System
Coarsening of the facial features, enlargement of the lips, gingival hyperplasia, hypertrichosis, and Peyronie's disease.
Immunologic
Anticonvulsant Hypersensitivity Syndrome(AHS) (which may include, but is not limited to, symptoms such as arthralgias, eosinophilia, fever, liver dysfunction, lymphadenopathy, or rash), systemic lupus erythematosus, periarteritis nodosa and immunoglobulin abnormalities.
Musculoskeletal System
Bone fractures and osteomalacia have been associated with long-term (> 10 years) use of phenytoin by patients with chronic epilepsy. Osteoporosis and other disorders of bone metabolism such as hypocalcemia, hypophosphatemia and decreased levels of Vitamin D metabolites have also been reported.
OVERDOSAGE
The lethal dose in pediatric patients is not known. The lethal dose in adults is estimated to be 2 to 5 grams. The initial symptoms are nystagmus, ataxia, and dysarthria. Other signs are tremor, hyperreflexia, lethargy, slurred speech, nausea, vomiting. The patient may become comatose and hypotensive. Death is due to respiratory and circulatory depression.
There are marked variations among individuals with respect to phenytoin plasma levels where toxicity may occur. Nystagmus, on lateral gaze, usually appears at 20 mcg/mL, ataxia at 30 mcg/mL; dysarthria and lethargy appear when the plasma concentration is over 40 mcg/mL, but as high a concentration as 50 mcg/mL has been reported without evidence of toxicity. As much as 25 times the therapeutic dose has been taken to result in a serum concentration over 100 mcg/mL with complete recovery.
Treatment
Treatment is nonspecific since there is no known antidote.
The adequacy of the respiratory and circulatory systems should be carefully observed and appropriate supportive measures employed. Hemodialysis can be considered since phenytoin is not completely bound to plasma proteins. Total exchange transfusion has been used in the treatment of severe intoxication in pediatric patients.
In acute overdosage, the possibility of other CNS depressants, including alcohol, should be borne in mind.
DOSAGE AND ADMINISTRATION
Serum concentrations should be monitored in changing from Dilantin (extended phenytoin sodium capsules, USP to Prompt Phenytoin Sodium Capsules, USP, and from the sodium salt to the free acid form.
Dilantin (extended phenytoin sodium capsules, USP) are formulated with the sodium salt of phenytoin. The free acid form of phenytoin is used in Dilantin-125 Suspension and Dilantin Infatabs. Because there is approximately an 8% increase in drug content with the free acid form over that of the sodium salt, dosage adjustments and serum level monitoring may be necessary when switching from a product formulated with the free acid to a product formulated with the sodium salt and vice versa.
General
Dosage should be individualized to provide maximum benefit. In some cases, serum blood level determinations may be necessary for optimal dosage adjustments—the clinically effective serum level is usually 10–20 mcg/mL. With recommended dosage, a period of seven to ten days may be required to achieve steady-state blood levels with phenytoin and changes in dosage (increase or decrease) should not be carried out at intervals shorter than seven to ten days.
Adult Dosage
Divided daily dosage
Patients who have received no previous treatment may be started on one 100-mg Dilantin (extended phenytoin sodium capsules, USP) three times daily and the dosage then adjusted to suit individual requirements. For most adults, the satisfactory maintenance dosage will be one capsule three to four times a day. An increase up to two capsules three times a day may be made, if necessary.
Once-a-day dosage
In adults, if seizure control is established with divided doses of three 100-mg Dilantin (extended phenytoin sodium capsules, USP) daily, once-a-day dosage with 300 mg of Dilantin (extended phenytoin sodium capsules, USP) may be considered. Studies comparing divided doses of 300 mg with a single daily dose of this quantity indicated absorption, peak plasma levels, biologic half-life, difference between peak and minimum values, and urinary recovery were equivalent. Once-a-day dosage offers a convenience to the individual patient or to nursing personnel for institutionalized patients and is intended to be used only for patients requiring this amount of drug daily. A major problem in motivating noncompliant patients may also be lessened when the patient can take this drug once a day. However, patients should be cautioned not to miss a dose, inadvertently.
Only Dilantin (extended phenytoin sodium capsules, USP) are recommended for once-a-day dosing. Inherent differences in dissolution characteristics and resultant absorption rates of phenytoin due to different manufacturing procedures and/or dosage forms preclude such recommendation for other phenytoin products. When a change in the dosage form or brand is prescribed, careful monitoring of phenytoin serum levels should be carried out.
Loading dose
Some authorities have advocated use of an oral loading dose of phenytoin in adults who require rapid steady-state serum levels and where intravenous administration is not desirable. This dosing regimen should be reserved for patients in a clinic or hospital setting where phenytoin serum levels can be closely monitored. Patients with a history of renal or liver disease should not receive the oral loading regimen.
Initially, one gram of Dilantin (extended phenytoin sodium capsules, USP) is divided into three doses (400 mg, 300 mg, 300 mg) and administered at two-hour intervals. Normal maintenance dosage is then instituted 24 hours after the loading dose, with frequent serum level determinations.
Pediatric Dosage
Initially, 5 mg/kg/day in two or three equally divided doses, with subsequent dosage individualized to a maximum of 300 mg daily. A recommended daily maintenance dosage is usually 4 to 8 mg/kg. Children over 6 years old and adolescents may require the minimum adult dose (300 mg/day).
HOW SUPPLIED
Hard, filled No. 3 capsules containing a white powder. The medium orange cap having "PD" printed in black ink and the white, opaque body having "DILANTIN" over "100 mg" printed in black ink.
100's (NDC 0071-0369-24)
1,000's (NDC 0071-0369-32)
Unit Dose 100's (NDC 0071-0369-40)
MEDICATION GUIDE
DILANTIN (Dī lan' tĭn)
(Phenytoin and Phenytoin sodium)
Oral Suspension, Tablets, Extended Oral Capsules
Read this Medication Guide before you start taking DILANTIN and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. If you have any questions about DILANTIN, ask your healthcare provider or pharmacist.
What is the most important information I should know about DILANTIN?
Do not stop taking DILANTIN without first talking to your healthcare provider.
Stopping DILANTIN suddenly can cause serious problems.
DILANTIN can cause serious side effects including:
- 1.
-
Like other antiepileptic drugs, DILANTIN may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase activity and talking (mania)
- other unusual changes in behavior or mood
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
Do not stop taking DILANTIN without first talking to a healthcare provider.
-
Stopping DILANTIN suddenly can cause serious problems. Stopping a seizure medicine suddenly in a patient who has epilepsy can cause seizures that will not stop (status epilepticus).
Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
- 2.
-
Dilantin may harm your unborn baby.
- If you take DILANTIN during pregnancy, your baby is at risk for serious birth defects.
- Birth defects may occur even in children born to women who are not taking any medicines and do not have other risk factors
- If you take DILANTIN during pregnancy, your baby is also at risk for bleeding problems right after birth. Your healthcare provider may give you and your baby medicine to prevent this.
- All women of child-bearing age should talk to their healthcare provider about using other possible treatments instead of DILANTIN. If the decision is made to use DILANTIN, you should use effective birth control (contraception) unless you are planning to become pregnant.
- Tell your healthcare provider right away if you become pregnant while taking DILANTIN. You and your healthcare provider should decide if you will take DILANTIN while you are pregnant.
- Pregnancy Registry: If you become pregnant while taking DILANTIN, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334. The purpose of this registry is to collect information about the safety of antiepileptic drugs during pregnancy.
- 3.
- Swollen glands (lymph nodes)
- 4.
-
Allergic reactions or serious problems which may affect organs and other parts of your body like the liver or blood cells. You may or may not have a rash with these types of reactions. Symptoms include:
- swelling of your face, eyes, lips, or tongue
- trouble swallowing or breathing
- a skin rash
- hives
- fever, swollen glands, or sore throat that do not go away or come and go
- painful sores in the mouth or around your eyes
- yellowing of your skin or eyes
- unusual bruising or bleeding
- severe fatigue or weakness
- severe muscle pain
- frequent infections or an infection that does not go away
Call your healthcare provider right away if you have any of the symptoms listed above.
What is DILANTIN?
DILANTIN is a prescription medicine used to treat tonic-clonic (grand mal), complex partial (psychomotor or temporal lobe) seizures, and to prevent and treat seizures that happen during or after brain surgery.
Who should not take DILANTIN?
Do not take DILANTIN if you:
- are allergic to phenytoin or any of the ingredients in DILANTIN. See the end of this leaflet for a complete list of ingredients in DILANTIN.
- have had an allergic reaction to CEREBYX (fosphenytoin), PEGANONE (ethotoin), or MESANTOIN (mephenytoin).
What should I tell my healthcare provider before taking DILANTIN?
Before you take DILANTIN, tell your healthcare provider if you:
- Have or had liver disease
- Have or had porphyria
- Have or had diabetes
- Have or have had depression, mood problems, or suicidal thoughts or behavior
- Are pregnant or plan to become pregnant.
- If you become pregnant while taking DILANTIN, the level of DILANTIN in your blood may decrease, causing your seizures to become worse. Your healthcare provider may change your dose of DILANTIN.
- Are breast feeding or plan to breastfeed. DILANTIN can pass into breast milk. You and your healthcare provider should decide if you will take DILANTIN or breastfeed. You should not do both.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Taking DILANTIN with certain other medicines can cause side effects or affect how well they work. Do not start or stop other medicines without talking to your healthcare provider.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take DILANTIN?
- Take DILANTIN exactly as prescribed. Your healthcare provider will tell you how much DILANTIN to take.
- Your healthcare provider may change your dose. Do not change your dose of DILANTIN without talking to your healthcare provider.
- DILANTIN can cause overgrowth of your gums. Brushing and flossing your teeth and seeing a dentist regularly while taking DILANTIN can help prevent this.
- If you take too much DILANTIN, call your healthcare provider or local Poison Control Center right away.
- Do not stop taking DILANTIN without first talking to your healthcare provider. Stopping DILANTIN suddenly can cause serious problems.
What should I avoid while taking DILANTIN?
Do not drink alcohol while you take DILANTIN without first talking to your healthcare provider. Drinking alcohol while taking DILANTIN may change your blood levels of DILANTIN which can cause serious problems.
Do not drive, operate heavy machinery, or do other dangerous activities until you know how DILANTIN affects you. DILANTIN can slow your thinking and motor skills.
What are the possible side effects of DILANTIN?
See "What is the most important information I should know about DILANTIN?"
DILANTIN may cause other serious side effects including:
- Softening of your bones (osteomalacia). This can cause broken bones.
Call your healthcare provider right away, if you have any of the symptoms listed above.
The most common side effects of DILANTIN include:
- problems with walking and coordination
- slurred speech
- confusion
- dizziness
- trouble sleeping
- nervousness
- tremor
- headache
- nausea
- vomiting
- constipation
- rash
These are not all the possible side effects of DILANTIN. For more information, ask your healthcare provider or pharmacist.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store DILANTIN?
- Store DILANTIN-125 Suspension at room temperature between 68°F to 77°F (20°C to 25°C). Protect from light. Do not freeze.
- Store DILANTIN INFATABS at room temperature between 68°F to 77°F (20°C to 25°C). Protect from moisture.
- Store DILANTIN Capsules at room temperature between 68°F to 77°F (20°C to 25°C) in tight, light-resistant containers. Protect from moisture.
Keep DILANTIN and all medicines out of the reach of children.
General information about DILANTIN
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use DILANTIN for a condition for which it was not prescribed. Do not give DILANTIN to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about DILANTIN. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about DILANTIN that was written for healthcare professionals.
For more information about DILANTIN, visit http://www.pfizer.com or call 1-800-438-1985.
What are the ingredients in DILANTIN?
Oral Suspension
Active ingredient: phenytoin
Inactive ingredients: USP; alcohol, USP (maximum content not greater than 0.6 percent); banana flavor; carboxymethylcellulose sodium, USP; citric acid, anhydrous, USP; glycerin, USP; magnesium aluminum silicate, NF; orange oil concentrate; polysorbate 40, NF; purified water, USP; sodium benzoate, NF; sucrose, NF; vanillin, NF; and FD&C yellow No. 6.
Tablet
Each tablet is a yellow triangular scored chewable tablet.
Active ingredient: 50 mg phenytoin
Inactive ingredients: D & C yellow No. 10, A1 lake, FD&C yellow No. 6, flavor, saccharin sodium, sucrose, talc, and other ingredients.
Extended Oral Capsule
Dilantin 100mg: Each capsule contains a white powder. The medium orange cap has "PD" imprinted in black ink and the white, opaque body has "DILANTIN" over "100 mg" printed in black ink.
Active ingredient: 100 mg phenytoin sodium
Inactive ingredients: lactose monohydrate, confectioner's sugar, talc, and magnesium stearate. The capsule body contains titanium dioxide and gelatin. The capsule cap contains FD&C red No. 28, FD&C yellow No. 6, and gelatin.
Dilantin 30mg: Each capsule contains a white powder. The small pale pink opaque cap has "PD" imprinted in black ink and the white, opaque body has "Dilantin 30 mg" printed in black ink.
Active ingredient: 30 mg phenytoin sodium
Inactive ingredients: lactose monohydrate, confectioner's sugar, talc, and magnesium stearate. The capsule shell cap and body contain Titanium Dioxide (cap and body); gelatin (cap and body); D&C yellow No. 10 (cap); FD&C red No. 3 (cap).
This Medication Guide has been approved by the U.S. Food and Drug Administration.
LAB-0398-2.0
July 2011
| DILANTIN
phenytoin sodium capsule, extended release |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Parke-Davis Div of Pfizer Inc (829076962) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
| Pharmacia and Upjohn Company | 829076566 | MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
| Pfizer Pharmaceuticals LLC | 829084552 | MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
| Warner Chilcott Company, LLC | 152356536 | MANUFACTURE | |
