EFAVIRENZ, LAMIVUDINE AND TENOFOVIR DISOPROXIL FUMARATE- efavirenz, lamivudine and tenofovir disoproxil fumarate tablet
Macleods Pharmaceuticals Limited
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use EFAVIRENZ, LAMIVUDINE and TENOFOVIR DISOPROXIL FUMARATE tablets safely and effectively. See full prescribing information for EFAVIRENZ, LAMIVUDINE and TENOFOVIR DISOPROXIL FUMARATE tablets.
EFAVIRENZ, LAMIVUDINE and TENOFOVIR DISOPROXIL FUMARATE tablets, for oral use Initial U.S. Approval: 2019 WARNING: POST TREATMENT ACUTE EXACERBATONS OF HEPATITIS BSee full prescribing information for complete boxed warning.Severe acute exacerbations of hepatitis B virus (HBV) have been reported in HBV-infected patients who have discontinued anti-HBV therapy, including lamivudine or tenofovir disoproxil fumarate, two components of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Monitor hepatic function closely in HBV-infected patients who discountinue efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. If appropriate, initiation of anti-HBV therapy may be warranted. ( 5.1) INDICATIONS AND USAGEEfavirenz, lamivudine and tenofovir disoproxil fumarate tablets is three-drug combination of efavirenz (EFV), a non-nucleoside reverse transcriptase inhibitor, and lamivudine and tenofovir disoproxil fumarate, both nucleo(t)side reverse transcriptase inhibitors and is indicated as a complete regimen for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in adults and pediatric patients weighing at least 35 kg. ( 1) DOSAGE AND ADMINISTRATION• Testing: Prior to or when initiating efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, test for HBV infection. Prior to initiation and during use of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, on a clinically appropriate schedule, assess serum creatinine, estimated creatinine clearance, urine glucose, and urine protein in all patients. In patients with chronic kidney disease, also assess serum phosphorous. (
2.1)
DOSAGE FORMS AND STRENGTHSTablets: 400 mg efavirenz, 300 mg lamivudine and 300 mg tenofovir disoproxil fumarate. ( 3) CONTRAINDICATIONSWARNINGS AND PRECAUTIONS• Risk of adverse reactions or loss of virologic response due to drug interactions: Consult full prescribing information prior to and during treatment for important potential drug interactions. Consider alternatives toefavirenz, lamivudine and tenofovir disoproxil fumarate tabletsin patients taking other medications with a known risk of Torsade de Pointes or in patients at higher risk of Torsade de Pointes. (
5.2)
ADVERSE REACTIONS• Most common adverse reactions (> 5% with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets) are rash and dizziness. (
6)
DRUG INTERACTIONS• Efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsshould not be administered with other antiretroviral medications for the treatment of HIV-1 infection. (
7.1)
USE IN SPECIFIC POPULATIONS• Pregnancy:Women should avoid pregnancy during EFV therapy, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, and for 12 weeks after discontinuation. (
5.6)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling. Revised: 3/2019 |
FULL PRESCRIBING INFORMATION
WARNING: POST TREATMENT ACUTE EXACERBATIONS OF HEPATITIS B
Severe acute exacerbations of hepatitis B virus (HBV) have been reported in HBV-infected patients who have discontinued anti-HBV therapy, including lamivudine and tenofovir disoproxil fumarate, two components of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in HBV-infected patients who discontinue efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. If appropriate, initiation of anti-hepatitis B therapy may be warranted [see Warnings and Precautions ( 5.1)].
1 INDICATIONS & USAGE
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is indicated as a complete regimen for the treatment of human immunodeficiency virus type 1 (HIV-1) infection in adults and pediatric patients weighing at least 35 kg.
2 DOSAGE & ADMINISTRATION
2.1 Testing Prior to Initiation and During Treatment with Efavirenz, Lamivudine and Tenofovir Disoproxil Fumarate Tablets
Prior to or when initiating efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, test patients for hepatitis B virus (HBV) infection [see Warnings and Precautions ( 5.1)].
Prior to initiation and during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, assess serum creatinine, estimated creatinine clearance, urine glucose, and urine protein in all patients. In patients with chronic kidney disease, also assess serum phosphorus. [see Warnings and Precautions ( 5.3)].
2.2 Recommended Dosage
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is a fixed-dose combination product containing 400 mg of efavirenz (EFV), 300 mg of lamivudine (3TC), and 300 mg of tenofovir disoproxil fumarate (TDF). The recommended dosage regimen of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets in adults and pediatric patients weighing at least 35 kg (77 lb) is one tablet once daily orally. Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets should be taken on an empty stomach, preferably at bedtime.Dosing at bedtime may improve the tolerability of nervous system symptoms [see Warnings and Precautions ( 5.5) and Adverse Reactions ( 6.1)].
2.3 Not Recommended in Renal Impairment
Because efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is a fixed-dose combination product and cannot be dose adjusted, it is not recommended for patients requiring dosage adjustment, patients with creatinine clearance less than 50 mL per min, or patients with end-stage renal disease (ESRD) requiring hemodialysis [see Use in Specific Populations ( 8.6)].
3 DOSAGE FORMS & STRENGTHS
Efavirenz, lamivudine and tenofovir disoproxil fumarate film-coated tablets are pink colored, capsule shaped, biconvex, film coated tablets debossed with “F 31” on one side and plain on the other side containing 400 mg of efavirenz, 300 mg of lamivudine and 300 mg of tenofovir disoproxil fumarate.
4 CONTRAINDICATIONS
4.1 Hypersensitivity
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is contraindicated in patients:
•with prior hypersensitivity reaction (e.g., Stevens-Johnson syndrome, erythema multiforme, or toxic skin eruptions)to efavirenz
[see Warnings and Precautions (
5.7)]
, lamivudine, or tenofovir disoproxil fumarate.
•when coadministered with elbasvir and grazoprevir
[see Warnings and Precautions (
5.2) and Drug Interactions (
7.5)].
5 WARNINGS AND PRECAUTIONS
5.1 Severe Acute Exacerbation of Hepatitis B in Patients with HBV Infection
All patients should be tested for the presence of chronic hepatitis B virus (HBV) before or when initiating efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets.
Discontinuation of anti-HBV therapy, including 3TC and TDF, two components of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, may be associated with severe acute exacerbations of hepatitis B. Patients infected with HBV who discontinue efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets should be closely monitored with both clinical and laboratory follow-up for at least several months after stopping treatment. If appropriate, resumption of anti-hepatitis B therapy may be warranted.
5.2 Risk of Adverse Reactions or Loss of Virologic Response Due to Drug Interactions
The concomitant use of efavirenz, lamivudine, and tenofovir disoproxil fumarate tabletsand other drugs may result in known or potentially significant drug interactions, some of which may lead to [see Contraindications ( 4) and Drug Interactions ( 7.5)]:
• Loss of therapeutic effect of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets and possible development of resistance.
• Possible clinically significant adverse reactions from greater exposures of concomitant drugs.
QTc prolongation has been observed with the use of EFV [see Drug Interactions ( 7.2, 7.5) and Clinical Pharmacology ( 12.2)], a component of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets. Consider alternatives to efavirenz, lamivudine, and tenofovir disoproxil fumarate tabletswhen coadministered with a drug with a known risk of Torsade de Pointes or when administered to patients at higher risk of Torsade de Pointes.
See Table 5 for steps to prevent or manage these possible and known significant drug interactions, including dosing recommendations. Consider the potential for drug interactions prior to and during therapy with efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets; review concomitant medications during therapy with efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets therapy; and monitor for the adverse reactions associated with the concomitant drugs.
5.3 New Onset or Worsening Renal Impairment
TDF, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, is principally eliminated by the kidney. Renal impairment, including cases of acute renal failure and Fanconi syndrome (renal tubular injury with severe hypophosphatemia), has been reported with the use of TDF [see Adverse Reactions ( 6.2)].
Prior to initiation and during use of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, on a clinically appropriate schedule, assess serum creatine, estimated creatine clearance, urine glucose, and urine protein in all patients. In patients with chronic kidney disease, also assess serum phosphorus.
Avoid efavirenz, lamivudine and tenofovir disoproxil fumarate tablets with concurrent or recent use of a nephrotoxic agent (e.g., high-dose or multiple non-steroidal anti-inflammatory drugs (NSAIDs)) [see Drug Interactions ( 7.7)]. Cases of acute renal failure after initiation of high dose or multiple NSAIDs have been reported in HIV-infected patients with risk factors for renal dysfunction who appeared stable on TDF. Some patients required hospitalization and renal replacement therapy. Alternatives to NSAIDs should be considered, if needed, in patients at risk for renal dysfunction.
Persistent or worsening bone pain, pain in extremities, fractures and/or muscular pain or weakness may be manifestations of proximal renal tubulopathy and should prompt an evaluation of renal function in at-risk patients.
5.4 Psychiatric Symptoms
Serious psychiatric adverse experiences have been reported in patients treated with EFV, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. In controlled trials of 1008 patients treated with regimens containing EFV for a mean of 2.1 years and 635 patients treated with control regimens for a mean of 1.5 years, the frequency (regardless of causality) of specific serious psychiatric events among patients who received EFV or control regimens, respectively, were severe depression (2.4%, 0.9%), suicidal ideation (0.7%, 0.3%), nonfatal suicide attempts (0.5%, 0), aggressive behavior (0.4%, 0.5%), paranoid reactions (0.4%, 0.3%), and manic reactions (0.2%, 0.3%). When psychiatric symptoms similar to those noted above were combined and evaluated as a group in a multifactorial analysis of data from a study using EFV 600 mg, treatment with EFV was associated with an increase in the occurrence of these selected psychiatric symptoms. Other factors associated with an increase in the occurrence of these psychiatric symptoms were history of injection drug use, psychiatric history, and receipt of psychiatric medication at study entry; similar associations were observed in both the EFV and control treatment groups. In a study using EFV 600 mg, onset of new serious psychiatric symptoms occurred throughout the study for both efavirenz-treated and control-treated patients. One percent of EFV-treated patients discontinued or interrupted treatment because of one or more of these selected psychiatric symptoms.
In the ENCORE1 (Evaluation of Novel Concepts in Optimization of antiRetroviral Efficacy) Trial, at Week 48 the frequency (regardless of causality) of the most common (occurring in > 1% patients) psychiatric events among patients who received EFV 400 mg (N = 321) or EFV 600 mg (N = 309) regimens, respectively, were: abnormal dreams (8.7%, 11.3%), insomnia (6.2%, 6.5%), somnolence (3.1%, 3.9%), depression (3.1%, 1.6%), nightmare (1.9%, 2.6%), sleep disorder (2.2%, 1.3%), and anxiety (1.2%, 1.3%).
There have also been occasional postmarketing reports of death by suicide, delusions, and psychosis-like behavior, although a causal relationship to the use of EFV cannot be determined from these reports [see Adverse Reactions ( 6.2)]. Postmarketing cases of catatonia have also been reported and may be associated with increased efavirenz exposure. Patients with serious psychiatric adverse experiences should seek immediate medical evaluation to assess the possibility that the symptoms may be related to the use of EFV, and if so, to determine whether the risks of continued therapy outweigh the benefits.
5.5 Nervous System Symptoms
Fifty-three percent (531/1008) of patients receiving EFV, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, in controlled trials reported central nervous system symptoms (any grade, regardless of causality) compared to 25% (156/635) of patients receiving control regimens. These symptoms included, but were not limited to, dizziness (28.1% of the 1008 patients), insomnia (16.3%), impaired concentration (8.3%), somnolence (7.0%), abnormal dreams (6.2%), and hallucinations (1.2%). These symptoms were severe in 2.0% of patients and 2.1% of patients discontinued therapy as a result. These symptoms usually begin during the first or second day of therapy and generally resolve after the first 2 to 4 weeks of therapy. After 4 weeks of therapy, the prevalence of nervous system symptoms of at least moderate severity ranged from 5% to 9% in patients treated with regimens containing EFV and from 3% to 5% in patients treated with a control regimen. Inform patients that these common symptoms were likely to improve with continued therapy and were not predictive of subsequent onset of the less frequent psychiatric symptoms [see Warnings and Precautions ( 5.4)]. Dosing at bedtime may improve the tolerability of these nervous system symptoms [see Dosage and Administration ( 2.2)].
In the ENCORE1 Trial, at Week 48, 40% of EFV 400 mg recipients and 48% of EFV 600 mg recipients reported central nervous system disorders. The most common symptoms (> 10%) were dizziness (27% vs. 35%) and headache (11% vs. 11%).
5.6 Embryo-Fetal Toxicity
EFV, a component of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, may cause fetal harm when administered during the first trimester to a pregnant woman. Advise females of reproductive potential who are receiving EFV to avoid pregnancy [seeUse in Specific Populations ( 8.1, 8.3)]
5.7 Skin and Systemic Hypersensitivity Reaction
In controlled clinical trials, 26% (266/1008) of patients treated with EFV 600 mg experienced new-onset skin rash compared with 17% (111/635) of patients treated in control groups. Rash associated with blistering, moist desquamation, or ulceration occurred in 0.9% (9/1008) of patients treated with EFV. The incidence of Grade 4 rash (e.g., erythema multiforme, Stevens-Johnson syndrome) in patients treated with EFV in all studies and expanded access was 0.1%. Rashes are usually mild-to-moderate maculopapular skin eruptions that occur within the first 2 weeks of initiating therapy with EFV (median time to onset of rash in adults was 11 days) and, in most patients continuing therapy with EFV, rash resolves within 1 month (median duration, 16 days). The discontinuation rate for rash in clinical trials was 1.7% (17/1008).
EFV can generally be reinitiated in patients interrupting therapy because of rash. EFV should be discontinued in patients developing severe rash associated with blistering, desquamation, mucosal involvement, or fever. Appropriate antihistamines and/or corticosteroids may improve the tolerability and hasten the resolution of rash. For patients who have had a life-threatening cutaneous reaction (e.g., Stephens-Johnson syndrome), alternate therapy should be considered [see Contraindications ( 4)].
In the ENCORE1 Trial at Week 48, different types of rash (such as rash, rash papular, rash maculopapular and rash pruritic) occurred in 32% of EFV 600 mg recipients and 26% of EFV 400 mg recipients. Grade 3-4 rash was reported in 3% of EFV 600 mg recipients and 1% of EFV 400 mg recipients. The discontinuation rate for rash in the ENCORE1 Trail was 3% of EFV 600 mg recipients and 1% of EFV 400 mg recipients.
5.8 Hepatotoxicity
Postmarketing cases of hepatitis, including fulminant hepatitis progressing to liver failure requiring transplantation or resulting in death, have been reported in patients treated with EFV. Reports have included patients with underlying hepatic disease, including coinfection with hepatitis B or C, and patients without pre-existing hepatic disease or other identifiable risk factors.
EFV, a component of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, is not recommended for patients with moderate or severe hepatic impairment. Careful monitoring is recommended for patients with mild hepatic impairment receiving EFV [see Adverse Reactions ( 6.1) and Use in Specific Populations ( 8.7)].
Monitoring of liver enzymes before and during treatment is recommended for all patients [see Dosage and Administration ( 2.4)]. Consider discontinuing efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets in patients with persistent elevations of serum transaminases to greater than five times the upper limit of the normal range.
Discontinue efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets if elevation of serum transaminases is accompanied by clinical signs or symptoms of hepatitis or hepatic decompensation.
5.9 Risk of Hepatic Decompensation When Usedwith Interferon- and Ribavirin-Based Regimens
In vitro studies have shown ribavirin can reduce the phosphorylation of pyrimidine nucleoside analogues such as 3TC, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Although no evidence of a pharmacokinetic or pharmacodynamic interaction (e.g., loss of HIV-1/HCV virologic suppression) was seen when ribavirin was coadministered with 3TC in HIV-1/HCV co-infected patients [see Clinical Pharmacology ( 12.3)], hepatic decompensation (some fatal) has occurred in HIV-1/HCV co-infected patients receiving combination antiretroviral therapy for HIV-1 and interferon alfa with or without ribavirin. Patients receiving interferon alfa with or without ribavirin and 3TC should be closely monitored for treatment-associated toxicities, especially hepatic decompensation. Discontinuation of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets should be considered as medically appropriate. Dose reduction or discontinuation of interferon alfa, ribavirin, or both should also be considered if worsening clinical toxicities are observed, including hepatic decompensation (e.g., Child-Pugh >6). See the complete prescribing information for interferon and ribavirin.
5.10 Pancreatitis
In pediatric patients with a history of prior antiretroviral nucleoside exposure, a history of pancreatitis, or other significant risk factors for the development of pancreatitis, 3TC, a component ofefavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, should be used with caution. Treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets should be stopped immediately if clinical signs, symptoms, or laboratory abnormalities suggestive of pancreatitis occur [see Adverse Reactions ( 6.1)].
5.11 Convulsions
Convulsions have been observed in patients receiving EFV, a component of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, generally in the presence of known medical history of seizures [see Nonclinical Toxicology ( 13.2)]. Caution must be taken in any patient with a history of seizures. Patients who are receiving concomitant anticonvulsant medications primarily metabolized by the liver, such as phenytoin and phenobarbital, may require periodic monitoring of plasma levels [see Drug Interactions ( 7.5)].
5.12 Lipid Elevations
Treatment with EFV, a component of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets,has resulted in increases in the concentration of total cholesterol and triglycerides. Cholesterol and triglyceride testing should be performed before initiating therapy with efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets and at periodic intervals during therapy.
5.13 Bone Loss and Mineralization Defects
Bone Mineral Density
In clinical trials in HIV-1 infected adults, TDF, a component of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, was associated with slightly greater decreases in bone mineral density (BMD) and increases in biochemical markers of bone metabolism, suggesting increased bone turnover relative to comparators. Serum parathyroid hormone levels and 1,25 Vitamin D levels were also higher in subjects receiving TDF.
Clinical trials evaluating TDF in pediatric subjects were conducted. Under normal circumstances, BMD increases rapidly in pediatric patients. In HIV-1 infected subjects 2 years to less than 18 years of age, bone effects were similar to those observed in adult subjects and suggest increased bone turnover. Total body BMD gain was less in the TDF-treated HIV-1 infected pediatric subjects as compared to the control groups. Similar trends were observed in HBV-infected subjects 12 years to less than 18 years of age. In all pediatric trials, skeletal growth (height) appeared to be unaffected for the duration of the clinical trials.
The effects of TDF-associated changes in BMD and biochemical markers on long-term bone health and future fracture risk in adults and pediatric subjects 2 years and older are unknown. The long-term effect of lower spine and total body BMD on skeletal growth in pediatric patients, and in particular, the effects of long-duration exposure in younger children is unknown.
Although the effect of supplementation with calcium and vitamin D was not studied, such supplementation may be beneficial for all patients. If bone abnormalities are suspected, then appropriate consultation should be obtained. Assessment of BMD should be considered for adult and pediatric patients who have a history of pathologic bone fracture or other risk factors for osteoporosis or bone loss. If bone abnormalities are suspected, appropriate consultation should be obtained.
Mineralization Defects:
Cases of osteomalacia associated with proximal renal tubulopathy, manifested as bone pain or pain in extremities and which may contribute to fractures, have been reported in association with the use of TD
[see Adverse Reactions (
6.2)].
Arthralgias and muscle pain or weakness have also been reported in cases of proximal renal tubulopathy. Hypophosphatemia and osteomalacia secondary to proximal renal tubulopathy should be considered in patients at risk of renal dysfunction who present with persistent or worsening bone or muscle symptoms while receiving products containing TDF
[see Warnings and Precautions (
5.3)].
5.14 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including the components of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jirovecii pneumonia [PCP], or tuberculosis), which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves’ disease, polymyositis, and Guillain-Barre syndrome) have also been reported to occur in the setting of immune reconstitution, however, the time to onset is more variable, and can occur many months after initiation of treatment.
5.15 Lactic Acidosis and Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues, including 3TC and TDF, two componentsof efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets,alone or in combination with other antiretrovirals. Treatment with efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets should be suspended in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
6 ADVERSE REACTIONS
The following adverse reactions are discussed in other sections of the labeling:
- Exacerbations of Hepatitis B [see Boxed Warning, Warnings and Precautions ( 5.2)].
- New Onset or Worsening Renal Impairment [see Warnings and Precautions ( 5.3)].
- Psychiatric Symptoms [see Warnings and Precautions ( 5.4)].
- Nervous System Symptoms [see Warnings and Precautions ( 5.5)].
- Skin and Systemic Hypersensitivity Reaction [see Warnings and Precautions ( 5.7)].
- Hepatotoxicity [see Warnings and Precautions ( 5.8)]
- Hepatic Decompensation in Patients Co-infected with HIV-1 and Hepatitis C [see Warnings and Precautions ( 5.9)].
- Pancreatitis [see Warnings and Precautions ( 5.10)]
- Bone Loss and Mineralization Defects
[see Warnings and Precautions (
5.13)].
- Immune Reconstitution Syndrome
[see Warnings and Precautions (
5.14)].
- Lactic Acidosis and Severe Hepatomegaly with Steatosis
[see Warnings and Precautions (
5.15)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Efavirenz, Lamivudine and Tenofovir Disoproxil Fumarate
Clinical Trials in Treatment-Naïve HIV-1 Infected Adult Subjects
In Trial 903, 600 antiretrovial-naïve subjects received TDF (N=299) or stavudine (d4T) (N=301) administered in combination with 3TC and EFV for 144 weeks. The most common adverse reactions were mild to moderate gastrointestinal events and dizziness.
Mild adverse reactions (Grade 1) were common with a similar incidence in both arms and included dizziness, diarrhea, and nausea. Table 1 provides the treatment-emergent adverse reactions (Grades 2-4) occurring in greater than or equal to 5% of subjects treated in any treatment group.
Table 1 Selected Adverse Reactionsa (Grades 2-4) Reported in 5% in Any Treatment Group in Trial 903 (0–144 Weeks)
|
| TDF+3TC+EFV
| d4T+3TC+EFV
|
|
| N=299
| N=301
|
| Rash event
b
| 18%
| 12%
|
| Headache
| 14%
| 17%
|
| Pain
| 13%
| 12%
|
| Diarrhea
| 11%
| 13%
|
| Depression
| 11%
| 10%
|
| Back pain
| 9%
| 8%
|
| Nausea
| 8%
| 9%
|
| Fever
| 8%
| 7%
|
| Abdominal pain
| 7%
| 12%
|
| Asthenia
| 6%
| 7%
|
| Anxiety
| 6%
| 6%
|
| Vomiting
| 5%
| 9%
|
| Insomnia
| 5%
| 8%
|
| Arthralgia
| 5%
| 7%
|
| Pneumonia
| 5%
| 5%
|
| Dyspepsia
| 4%
| 5%
|
| Dizziness
| 3%
| 6%
|
| Myalgia
| 3%
| 5%
|
| Lipodystrophy
c
| 1%
| 8%
|
| Peripheral neuropathy
d
| 1%
| 5%
|
a. Frequencies of adverse reactions are based on all treatment-emergent adverse events, regardless of relationship to study drug.
b. Rash event includes rash, pruritus, maculopapular rash, urticaria, vesiculobullous rash, and pustular rash.
c. Lipodystrophy represents a variety of investigator-described adverse events not a protocol-defined syndrome.
d. Peripheral neuropathy includes peripheral neuritis and neuropathy.
ENCORE1 Trial -Adverse Reactions: The most common adverse reactions seen in a double-blind comparative controlled trial in which 630 treatment-naïve subjects received EFV 400 mg (N = 321) or EFV 600 mg (N = 309) in combination with fixed-dose emtricitabine (FTC)/TDF for 48 weeks were mild to moderate gastrointestinal events, dizziness, abnormal dreams, and rash. Table 2 provides selected clinical adverse reactions of moderate or severe intensity occurring in greater than or equal to 2% of treatment-naive subjects receiving combination therapy including EFV 400 mg or EFV 600 mg.
Table 2 Selected Adverse Reactionsa(Grades 2-4) Reported in ≥ 2% in Either Treatment Group in the ENCORE1 Trial through Week 48
|
| EFV 400 mg + FTC/TDF
| EFV 600 mg + FTC/TDF
|
| N = 321
| N = 309
|
|
| Rash event
b
| 9%
| 13%
|
| Dizziness
| 6%
| 9%
|
| Insomnia
| 3%
| 4%
|
| Abnormal dreams
| 2%
| 2%
|
| Headache
| 1%
| 3%
|
| Diarrhea
| 2%
| 3%
|
| Vomiting
| 1%
| 2%
|
| Pyrexia
| 2%
| 1%
|
| Upper respiratory tract infection
| 3%
| 1%
|
| Nasopharyngitis
| 3%
| 2%
|
| Herpes zoster
| 3%
| 1%
|
| Gastroenteritis
| 2%
| 2%
|
a Frequencies of adverse reactions are based on all treatment-emergent adverse events, regardless of relationship to study drug.
b Rash events include dermatitis allergic, drug hypersensitivity, pruritus generalized, eosinophilic pustular folliculitis, rash, rash erythematous, rash generalized, rash macular, rash maculopapular, rash morbilliform, rash papular, rash pruritic, rash vesicular, and urticaria.
Laboratory Abnormalities:Table 3 provides a list of laboratory abnormalities (Grades 3−4) observed in Trial 903. With the exception of fasting cholesterol and fasting triglyceride elevations that were more common in the d4T group (40% and 9%) compared with the TDF group (19% and 1%) respectively, laboratory abnormalities observed in this trial occurred with similar frequency in the TDF and d4T treatment arms.
Table 3 Grades 3-4 Laboratory Abnormalities Reported in 1% of Patients Randomized to Efavirenz, Lamivudine and Tenofovir disoproxil fumarate in Trial 903 (0-144 Weeks)
|
| TDF + 3TC + EFV
| d4T + 3TC + EFV
|
|
| N=299
| N=301
|
| Any ≥ Grade 3 Laboratory Abnormality
| 36%
| 42%
|
| Fasting Cholesterol (>240 mg/dL)
| 19%
| 40%
|
| Creatine Kinase (M: >990 U/L; F: >845 U/L)
| 12%
| 12%
|
| Serum Amylase (>175 U/L)
| 9%
| 8%
|
| AST (M: >180 U/L; F: >170 U/L)
| 5%
| 7%
|
| ALT (M: >215 U/L; F: >170 U/L)
| 4%
| 5%
|
| Hematuria (>100 RBC/HPF)
| 7%
| 7%
|
| Neutrophils (<750/mm
3)
| 3%
| 1%
|
| Fasting Triglycerides (>750 mg/dL)
| 1%
| 9%
|
In ENCORE1 Trial, a summary of Grade 3 and 4 laboratory abnormalities is provided in Table 4.
Table 4 Grades 3-4 Laboratory Abnormalities in ≥ 2% in Either Treatment Group Through Week 48
| Laboratory Parameter
| EFV 400 mg + FTC + TDF
| EFV 600 mg + FTC + TDF
|
| N = 321
| N = 309
|
|
| ALT
| 5%
| 3%
|
| AST
| 2%
| 2%
|
| Total bilirubin
| 0.3%
| 3%
|
| Cholesterol
| 2%
| 5%
|
| Neutrophils
| 2%
| 3%
|
| Phosphorus
| 2%
| 3%
|
Pancreatitis: Pancreatitis, which has been fatal in some cases, has been observed in antiretroviral nucleoside-experienced pediatric subjects receiving 3TC alone or in combination with other antiretroviral agents [see Warnings and Precautions ( 5.10)].
Changes in Bone Mineral Density:
In HIV-1 infected adult subjects in Trial 903, there was a significantly greater mean percentage decrease from baseline in BMD at the lumbar spine in subjects receiving TDF + 3TC + EFV (-2.2% ± 3.9) compared with subjects receiving d4T + 3TC + EFV (-1.0% ± 4.6) through 144 weeks. Changes in BMD at the hip were similar between the two treatment groups (-2.8% ± 3.5 in the TDF group vs. -2.4% ± 4.5 in the d4T group). In both groups, the majority of the reduction in BMD occurred in the first 24–48 weeks of the trial and this reduction was sustained through Week 144. Twenty-eight percent of TDF-treated subjects vs. 21% of the d4T-treated subjects lost at least 5% of BMD at the spine or 7% of BMD at the hip. Clinically relevant fractures (excluding fingers and toes) were reported in 4 subjects in the TDF group and 6 subjects in the d4T group. In addition, there were significant increases in biochemical markers of bone metabolism (serum bone-specific alkaline phosphatase, serum osteocalcin, serum C telopeptide, and urinary N telopeptide) and higher serum parathyroid hormone levels and 1,25 Vitamin Dlevels in the TDF group relative to the d4T group; however, except for bone-specific alkaline phosphatase, these changes resulted in values that remained within the normal range
[see Warnings and Precautions (
5.13)].
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of EFV, 3TC, or TDF. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
EFV
Body as a Whole: allergic reactions, asthenia, redistribution/accumulation of body fat
Central and Peripheral Nervous System: abnormal coordination, ataxia, cerebellar coordination and balance disturbances, convulsions, hypoesthesia, paresthesia, neuropathy, tremor, vertigo
Endocrine: gynecomastia
Gastrointestinal: constipation, malabsorption
Cardiovascular: flushing, palpitations
Liver and Biliary System: hepatic enzyme increase, hepatic failure, hepatitis.
Metabolic and Nutritional: hypercholesterolemia, hypertriglyceridemia
Musculoskeletal: arthralgia, myalgia, myopathy
Psychiatric: aggressive reactions, agitation, delusions, emotionallability, mania, neurosis, paranoia, psychosis, suicide, catatonia
Respiratory: dyspnea
Skin and Appendages: erythema multiforme, photoallergic dermatitis, Stevens-Johnson syndrome
Special Senses: abnormal vision, tinnitus
3TC
Body as a Whole: redistribution/accumulation of body fat
Endocrine and Metabolic: hyperglycemia.
General: weakness.
Hemic and Lymphatic: anemia (including pure red cell aplasia and severe anemias progressing on therapy).
Hepatic and Pancreatic: lactic acidosis and hepatic steatosis [see Warnings and Precautions (5.15)], posttreatment exacerbation of hepatitis B [see Warnings and Precautions (5.1)].
Hypersensitivity: anaphylaxis, urticaria.
Musculoskeletal: muscle weakness, CPK elevation, rhabdomyolysis.
Skin: alopecia, pruritus.
TDF
Immune System Disorders: allergic reaction, including angioedema
Metabolism and Nutrition Disorders: lactic acidosis, hypokalemia, hypophosphatemia
Respiratory, Thoracic, and Mediastinal Disorders: dyspnea
Gastrointestinal Disorders: pancreatitis, increased amylase, abdominal pain
Renal and Urinary Disorders: acute renal failure, renal failure, acute tubular necrosis, Fanconi syndrome, proximal renal tubulopathy, interstitial nephritis (including acute cases), nephrogenic diabetes insipidus, renal insufficiency, increased creatinine, proteinuria, polyuria
Hepatobiliary Disorders: hepatic steatosis, hepatitis, increased liver enzymes (most commonly AST, ALT gamma GT)
Skin and Subcutaneous Tissue Disorders: rash
Musculoskeletal and Connective Tissue Disorders: rhabdomyolysis, osteomalacia (manifested as bone pain and which may contribute to fractures), muscular weakness, myopathy
General Disorders and Administration Site Conditions: asthenia
The following adverse reactions, listed under the body system headings above, may occur as a consequence of proximal renal tubulopathy: rhabdomyolysis, osteomalacia, hypokalemia, muscular weakness, myopathy, hypophosphatemia.
7 DRUG INTERACTIONS
7.1 Not Recommended with Other Antiretroviral Medications
Efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets is a complete regimen for the treatment of HIV-1 infection; therefore, it should not be administered with other antiretroviral medications for treatment of HIV-1 infection.
7.2 QT Prolonging Drugs
There is limited information available on the potential for a pharmacodynamic interaction between EFV and drugs that prolong the QTc interval. QTc prolongation has been observed with the use of EFV [see Clinical Pharmacology ( 12.2)]. Consider alternatives to EFVwhen coadministered with a drug with a known risk of Torsade de Pointes.
7.3 Drugs Affecting Renal Function
Tenofovir is primarily eliminated by the kidneys [see Clinical Pharmacology ( 12.3)]. Coadministration of efavirenz, lamivudine and tenofovir disoproxil fumaratetabletswith drugs that are eliminated by active tubular secretion may increase serum concentrations of tenofovir and/or coadministered drug. Some examples include, but are not limited to,acyclovir, cidofovir, ganciclovir, valacyclovir, valganciclovir, aminoglycosides (e.g., gentamicin), and high-dose or multiple NSAIDs [see Warnings and Precautions ( 5.3)]. Drugs that decrease renal function may increase concentrations of tenofovir.
Do not administer efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets with HEPSERA (adefovir dipivoxil).
7.4 Cannabinoid Test Interaction
EFV does not bind to cannabinoid receptors. False-positive urine cannabinoid test results have been reported with some screening assays in uninfected and HIV-infected subjects receiving EFV. Confirmation of positive screening tests for cannabinoids by a more specific method is recommended.
7.5 Established and Other Potentially Significant Drug Interactions
EFV has been shown in vivo to induce CYP3A and CYP2B6. Other compounds that are substrates of CYP3A or CYP2B6 may have decreased plasma concentrations when coadministered with EFV.
Drugs that induce CYP3A activity (e.g., phenobarbital, rifampin, rifabutin) would be expected to increase the clearance of EFV resulting in lowered plasma concentrations.
No drug interaction studies have been conducted using efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets. However, drug interaction studies have been conducted with the individual components of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets (EFV, 3TC, and TDF) [see Clinical Pharmacology ( 12.3)].
Drug interactions with EFV are summarized in Table 5. For pharmacokinetics data, [see Clinical Pharmacology ( 12.3)] Tables 7 and 8. This table includes potentially significant interactions, but is not all inclusive.
Table 5 Established and Other Potentially Significant Drug Interactions with EFV: Alteration in Dose or Regimen May Be Recommended Based on Drug Interaction Studies or Predicted Interaction
| Concomitant Drug
Class: Drug Name | Effect
| Clinical Comment
|
| Anticoagulant:
Warfarin | ↑ or ↓ warfarin
| Monitor INR and adjust warfarin dosage if necessary.
|
| Anticonvulsants:
Carbamazepine | ↓ carbamazepine
*
↓ EFV * | There are insufficient data to make a dose recommendation for EFV. Alternative anticonvulsant treatment should be used.
|
| Phenytoin
Phenobarbital | ↓ anticonvulsant
↓ EFV | Monitor anticonvulsant plasma levels periodically because of potential for reduction in anticonvulsant and/or EFV plasma levels.
|
| Antidepressants:
Bupropion Sertraline |
↓ bupropion * ↓ sertraline * |
Increases in bupropion dosage should be guided by clinical response. Bupropion dose should not exceed the maximum recommended dose. Increases in sertraline dosage should be guided by clinical response. |
| Antifungals:
Itraconazole Ketoconazole Posaconazole |
↓ itraconazole* ↓ hydroxyitraconazole * ↓ ketoconazole ↓ posaconazole * |
Consider alternative antifungal treatment because no dose recommendation for itraconazole or ketoconazole can be made. Avoid concomitant use unless the benefit outweighs the risks. |
| Anti-infective:
Clarithromycin |
↓ clarithromycin * ↑ 14-OH metabolite * |
Consider alternatives to macrolide antibiotics because of the risk of QT interval prolongation. |
| Antimycobacterial:
Rifabutin Rifampin |
↓ rifabutin * ↓ EFV* | Increase daily dose of rifabutin by 50%. Consider doubling the rifabutin dose in regimens where rifabutin is given 2 or 3 times a week.
Increase EFV total daily dose to 800 mg once daily when coadministered with rifampin to patients weighing 50 kg or more. |
| Antimalarials:
Artemether/lumefantrine Atovaquone/ proguanil | ↓ artemether
*
↓ dihydroartemisinin * ↓ lumefantrine * ↓ atovaquone ↓ proguanil | Consider alternatives to artemether/lumefantrine because of the risk of QT interval prolongation
[see Warnings and Precautions (5.2)].
Concomitant administration is not recommended. |
| Calcium channel blockers:
Diltiazem Others (e.g., felodipine, nicardipine, nifedipine, verapamil) | ↓ diltiazem
*
↓ desacetyl diltiazem * ↓ N-monodesmethyldiltiazem * ↓ calcium channel blocker | Diltiazem dose adjustments should be guided by clinical response (refer to the full prescribing information for diltiazem).
When coadministered with EFV, dosage adjustment of calcium channels blocker may be needed and should be guided by clinical response (refer to the full prescribing information for the calcium channel blocker). |
| HMG-CoA reductase
inhibitors: Atorvastatin Pravastatin Simvastatin |
↓ atorvastatin * ↓ pravastatin * ↓ simvastatin * |
Plasma concentrations of atorvastatin, pravastatin, and simvastatin decreased. Consult the full prescribing information for the HMG-CoA reductase inhibitor for guidance on individualizing the dose. |
| Hepatitis C antiviral agents:
Boceprevir Elbasvir/Grazoprevir Pibrentasvir/Glecaprevir Simeprevir Velpatasvir/Sofosbuvir Velpatasvir/Sofosbuvir/ Voxilaprevir Ledipasvir/Sofosbuvir |
↓ boceprevir * ↓ elbasvir ↓ grazoprevir ↓ pibrentasvir ↓ glecaprevir ↓ simeprevir * ↔ EFV ↓ velpatasvir ↓ velpatasvir ↓ voxilaprevir ↑TDF |
Concomitant administration of boceprevir is not recommended. Coadministration of EFV with elbasvir/grazoprevir is contraindicated [see Contraindications (4)] because it may lead to loss of virologic response to elbasvir/grazoprevir. Coadministration of EFV is not recommended because it may lead to reduced therapeutic effect of pibrentasvir/glecaprevir. Concomitant administration of simeprevir is not recommended. Coadministration of EFV and sofosbuvir/velpatasvir is not recommended because it may result in loss of therapeutic effect of sofosbuvir/velpatasvir. Coadministration of EFV and sofosbuvir/velpatasvir/voxilaprevir is not recommended because it may result in loss of therapeutic effect of sofosbuvir/velpatasvir/voxilaprevir. Monitor for adverse reactions associated with TDF. |
| Hepatitis B antiviral agents
Adefovir dipivoxil |
|
Concomitant administration of adefovir dipivoxil is not recommended. |
| Hormonal contraceptives:
Oral Ethinyl estradiol/ Norgestimate Implant Etonogestrel |
↓ active metabolites of norgestimate * ↓ etonogestrel |
A reliable method of barrier contraception should be used in addition to hormonal contraceptives. A reliable method of barrier contraception should be used in addition to hormonal contraceptives. Decreased exposure of etonogestrel may be expected. There have been postmarketing reports of contraceptive failure with etonogestrel in EFV-exposed patients. |
| Immunosuppressants: Cyclosporine, tacrolimus,
sirolimus, and others metabolized by CYP3A |
↓ immunosuppressant |
Dose adjustments of the immunosuppressant may be required. Close monitoring of immunosuppressant concentrations for at least 2 weeks (until stable concentrations are reached) is recommended when starting or stopping treatment with EFV. |
| Narcotic analgesic:
Methadone |
↓ methadone* |
Monitor for signs of methadone withdrawal and increase methadone dose if required to alleviate withdrawal symptoms. |
* The interaction between EFV and the drug was evaluated in a clinical study. All other drug interactions shown are predicted.
This table is not all-inclusive.
7.6 Drugs without Clinically Significant Interactions
No dosage adjustment is recommended when efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is administered with the following: aluminum/magnesium hydroxide antacids, azithromycin, cetirizine, famotidine, fluconazole, and lorazepam.
7.7 Drugs Inhibiting Organic Cation Transporters
3TC, a component of efavirenz, lamivudine and tenofovir disoproxil fumaratetablets, is predominantly eliminated in the urine by active organic cationic secretion. The possibility of interactions with other drugs administered concurrently should be considered, particularly when their main route of elimination is active renal secretion via the organic cationic transport system (e.g., trimethoprim) [see Clinical Pharmacology ( 12.3)]. No data are available regarding interactions with other drugs that have renal clearance mechanisms similar to that of 3TC.
7.8 Sorbitol
Coadministration of single doses of 3TC and sorbitol resulted in a sorbitol dose-dependent reduction in 3TC. When possible, avoid use of sorbitol-containing medicines with 3TC
[see Clinical Pharmacology (
12.3)].
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsduring pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
There are retrospective case reports of neural tube defects in infants whose mothers were exposed to EFV-containing regimens in the first trimester of pregnancy.
Although a causal relationship has not been established between exposure to EFV in the first trimester and neural tube defects, similar malformations have been observed in studies conducted in monkeys at doses similar to the human dose. In addition, fetal and embryonic toxicities occurred in rats, at a dose ten times less than the human exposure at recommended clinical dose. Because of the potential risk of neural tube defects, EFV should not be used in the first trimester of pregnancy. Advise pregnant women of the potential risk to a fetus.
Prospective pregnancy data from the APR are not sufficient to adequately assess this risk of birth defects or miscarriage. EFV and 3TC have been evaluated in a limited number of women as reported to the APR. Available data from the APR show no difference in the risk of major birth defects for EFV and 3TC compared to the background rate for major birth defects of 2.7% in the U.S. reference population of the Metropolitan Atlanta Congenital Defects Program (MACDP) (see Data).
Oral administration of 3TC to pregnant rabbits during organogenesis resulted in embryolethality at systemic exposure (AUC) similar to the recommended clinical dose; however, no adverse development effects were observed with oral administration of 3TC to pregnant rats during organogenesis at plasma concentrations (C max) 35 times the recommended clinical dose (see Data). No adverse developmental effects were observed when TDF was administered at doses/exposures ≥14 (TDF) and 2.7 (tenofovir) times those of the recommended daily dose of TDF (see Data).
The rate of miscarriage is not reported in the APR. The background risk for major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background rate for major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Human Data: EFV: There are retrospective postmarketing reports of findings consistent with neural tube defects, including meningomyelocele, all in infants of mothers exposed to EFV-containing regimens in the first trimester.
Based on prospective reports from the APR of approximately 1000 live births following exposure to EFV-containing regimens (including over 800 live births exposed in the first trimester), there was no difference between EFV and overall birth defects compared with the background birth defect rate of 2.7% in the U.S. reference population of the MACDP. As of the interim APR report issued December 2014, the prevalence of birth defects following first-trimester exposure was 2.3% (95% CI: 1.4%-3.6%). One of these prospectively reported defects with first-trimester exposure was aneural tube defect. A single case of anophthalmia with first-trimester exposure to EFV has also been prospectively reported. This case also included severe oblique facial clefts and amniotic banding, which have a known association with anophthalmia.
3TC: Based on prospective reports from the APR of over 11,000 exposures to 3TC during pregnancy resulting in live births (including over 4,500 exposed in the first trimester), there was no difference between 3TC and overall risk of birth defects for 3TC compared with the background birth defect rate of 2.7% in the U.S. reference population of the MACDP. The prevalence of defects in live births was 3.1% (95% CI: 2.6% to 3.6%) following first trimester exposure to 3TC-containing regimens and 2.8% (95% CI: 2.5%, 3.3%) following second/third trimester exposure to 3TC-containing regimens.
3TC pharmacokinetics were studied in pregnant women during 2 clinical studies conducted in South Africa. The trials assessed pharmacokinetics in 16 women at 36 weeks gestation using 150 mg 3TC twice daily with zidovudine, 10 women at 38 weeks gestation using 150 mg 3TC twice daily with zidovudine, and 10 women at 38 weeks gestation using 3TC 300 mg twice daily without other antiretrovirals. These trials were not designed or powered to provide efficacy information. 3TC concentrations were generally similar in maternal, neonatal, and umbilical cord serum samples. In a subset of subjects, amniotic fluid specimens were collected following natural rupture of membranes and confirmed that 3TC crosses the placenta in humans. Based on limited data at delivery, median (range) amniotic fluid concentrations of 3TC were 3.9 (1.2 to 12.8)–fold greater compared with paired maternal serum concentration (n = 8).
TDF: Based on prospective reports from the APR exposures to TDF-containing regimens during pregnancy resulting in live births (including 3,342 exposed in the first trimester and 1,475 exposed in the second/third trimester), there was no increase in overall major birth defects with TDF compared with the background birth defect rate of 2.7% in a U.S. reference population of the MACDP. The prevalence of major birth defects in live births was 2.3% (95% CI: 1.8% to 2.8%) with first trimester exposure to TDF-containing regimens, and 2.1% (95% CI: 1.4% to 3.0%) with the second/third trimester exposure to TDF-containing regimens.
Prospective reports from the APR of overall major birth defects in pregnancies exposed to TDF are compared with a U.S. background major birth defect rate. Methodological limitations of the APR include the use of MACDP as the external comparator group. Limitations of using an external comparator include differences in methodology and populations, as well as confounding due to the underlying disease.
Animal Data: EFV: Effects of EFV on embryo-fetal development have been studied in three nonclinical species (cynomolgus monkeys, rats, and rabbits). In monkeys, EFV 60 mg/kg/day was administered to pregnant females throughout pregnancy (gestation days 20 through 150). The maternal systemic drug exposures (AUC) were 1.3 times the exposure in humans at the recommended clinical dose (600 mg/day), with fetal umbilical venous drug concentrations approximately 0.7 times the maternal values. Three of 20 fetuses/infants had one or more malformations; there were no malformed fetuses or infants from placebo-treated mothers. The malformations that occurred in these three monkey fetuses included anencephaly and unilateral anophthalmia in one fetus, microphthalmia in a second, and cleft palate in the third. There was no NOAEL (no observable adverse effect level) established for this study because only one dosage was evaluated. In rats, EFV was administered either during organogenesis (gestation days 7 to 18) or from gestation day 7 through lactation day 21 at 50, 100, or 200 mg/kg/day. Administration of 200 mg/kg/day in rats was associated with increase in the incidence of early resorptions; and doses 100 mg/kg/day and greater were associated with early neonatal mortality. The AUC at the NOAEL (50 mg/kg/day) in this rat study was 0.1 times that in humans at the recommended clinical dose. Drug concentrations in the milk on lactation day 10 were approximately 8 times higher than those in maternal plasma. In pregnant rabbits, EFV was neither embryo lethal nor teratogenic when administered at doses of 25, 50, and 75 mg/kg/day over the period of organogenesis (gestation days 6 through 18). The AUC at the NOAEL (75 mg/kg/day) in rabbits was 0.4 times that in humans at the recommended clinical dose.
3TC: 3TC was administered orally to pregnant rats (at 90, 600, and 4,000 mg per kg per day) and rabbits (at 90, 300, and 1,000 mg per kg per day and at 15, 40, and 90 mg per kg per day) during organogenesis (on gestation Days 7 through 16 [rat] and 8 through 20 [rabbit]). No evidence of fetal malformations due to 3TC was observed in rats and rabbits at doses producing plasma concentrations (C max) approximately 35 times higher than human exposure at the recommended daily dose. Evidence of early embryolethality was seen in the rabbit at system exposures (AUC) similar to those observed in humans, but there was no indication of this effect in the rat at plasma concentrations (C max) 35 times higher than human exposure at the recommended daily dose. Studies in pregnant rats showed that 3TC is transferred to the fetus through the placenta. In the fertility/pre-and postnatal development study in rats, 3TC was administered orally at doses of 180, 900, and 4,000 mg per kg per day (from prior to mating through postnatal Day 20). In the study, development of the offspring, including fertility and reproductive performance, was not affected by maternal administration of 3TC.
TDF: TDF was administered orally to pregnant rats (at 0, 50, 150, or 450 mg/kg/day) and rabbits (at 0, 30, 100, or 300 mg/kg/day) through organogenesis (on gestation days 7 through 17, and 6 through 18, respectively). No significant toxicological effects were observed in embryo-fetal toxicity studies performed with TDF in rats at doses up to 14 times the human dose based on body surface area comparisons and in rabbits at doses up to 19 times the human dose based on body surface area comparisons. In a pre/postnatal development study in rats, TDF was administered orally through lactation at doses up to 600 mg/kg/day; no adverse effects were observed in the offspring at tenofovir exposures of approximately 2.7 times higher than human exposures at the recommended daily dose of TDF.
8.2 Lactation
Risk Summary
The Centers for Disease Control and Prevention recommends that HIV-1-infected mothers not breastfeed their infants to avoid risking postnatal transmission of HIV-1 infection.
EFV, 3TC and TDF have been shown to be present in human breast milk. It is not known if 3TC or TDF affect milk production or have effects on the breastfed infant.
Because of the potential for (1) HIV 1 transmission (in HIV-negative infants), (2) developing viral resistance (in HIV-positive infants), and (3) adverse reactions in a breastfed infant similar to those seen in adults, instruct mothers not to breastfeed if they are receiving efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
Data
Human Data: TDF: In a study of 50 breastfeeding women on a tenofovir-containing regimen between 1 and 24 weeks postpartum (median 13 weeks), after 7 days of treatment, tenofovir was undetectable in the plasma of most infants. There were no serious adverse events.
8.3 Females and Males of Reproductive Potential
Because of potential teratogenic effects, pregnancy should be avoided in women receiving efavirenz, lamivudine and tenofovir disoproxil fumarate tablets [seeWarnings and Precautions ( 5.6),Use in Specific Populations ( 8.1).]
Pregnancy Testing: Females of reproductive potential should undergo pregnancy testing before initiation of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
Contraception: Females of reproductive potential should use effective contraception during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsand for 12 weeks after discontinuing efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsdue to the long half-life of EFV. Barrier contraception shouldalways be used in combination with other methods of contraception. Hormonal methods that contain progesterone may have decreased effectiveness [see Drug Interactions ( 7.5)].
8.4 Pediatric Use
The safety and effectiveness of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets as a fixed dose formulation in pediatric patients infected with HIV-1 and weighing at least 35 kg have been established based on clinical studies using the individual components (EFV, 3TC, TDF).
8.5 Geriatric Use
Clinical studies of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for the elderly patient should be exercised in the administration of 3TC in elderly patients reflectingthe greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Renal Impairment
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is not recommended for patients with creatinine clearance less than 50 mL per min or patients with end-stage renal disease (ESRD) requiring hemodialysis because efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsit is a fixed-dose combination and the dosage of the individual components cannot be adjusted. If a dose reduction of 3TC or TDF, two components of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, is required for patients with creatinine clearance less than 50 mL per min, then the individual components should be used [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)].
8.7 Hepatic Impairment
Efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsis not recommended for patients with moderate or severe hepatic impairment because there are insufficient data to determine whether dose adjustment is necessary. Patients with mild hepatic impairment may be treated with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets without any adjustment in dose [see Dosage and Administration ( 2.4), Warnings and Precautions ( 5.8) and Clinical Pharmacology ( 12.3)].
10 OVERDOSAGE
If overdose occurs the patient must be monitored for evidence of toxicity, and standard supportive treatment applied as necessary.
EFV: Some patients accidentally taking 600 mg twice daily have reported increased nervous system symptoms. One patient experienced involuntary muscle contractions.
Treatment of overdose with EFV should consist of general supportive measures, including monitoring of vital signs and observation of the patient’s clinical status. Administration of activated charcoal may be used to aid removal of unabsorbed drug. There is no specific antidote for overdose with EFV. Since EFV is highly protein bound, dialysis is unlikely to significantly remove the drug from blood.
3TC: Because a negligible amount of 3TC was removed via (4-hour) hemodialysis, continuous ambulatory peritoneal dialysis, and automated peritoneal dialysis, it is not known if continuous hemodialysis would provide clinical benefit in a 3TC overdose event.
TDF: Tenofovir is efficiently removed by hemodialysis with an extraction coefficient of approximately 54%. Following a single 300 mg dose of TDF, a four-hour hemodialysis session removed approximately 10% of the administered tenofovir dose.
11 DESCRIPTION
Efavirenz, lamivudine and tenofovir fumarate tablets is a fixed-dose combination containing EFV, 3TC, and TDF with inhibitory activity against HIV-1. EFV is a non-nucleoside reverse transcriptase inhibitor (NNRTI), 3TC is a synthetic nucleoside analog. TDF which is converted in vivo to tenofovir, is an acyclic a nucleoside phosphonate (nucleotide) analog of adenosine 5'-monophosphate.
Efavirenz, lamivudine and tenofovir fumarate tabletsare for oral administration. Each tablet contains 400 mg of FV, 300 mg of 3TC and 300 mg of TDF(equivalent to 245 mg of tenofovir disoproxil) as active ingredients. The tablets include the following inactive ingredients: croscarmellose sodium, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, pregelatinized starch, poloxamer,and sodium lauryl sulphate.The tablets are coated with ferric oxide red, hydroxypropyl methylcellulose, lactose monohydrate, titanium dioxide, and triacetin. In this insert, all dosages are expressed in terms of tenofovir disoproxil fumarate except where otherwise noted.
EFV: EFV is chemically described as (S)-6-chloro-4-(cyclopropylethynyl)-1,4-dihydro-4-(trifluoromethyl)-2H-3,1-benzoxazin-2-one. Its molecular formula is C
14H
9ClF
3NO
2 and its structural formula is:
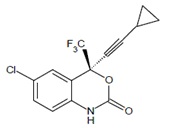
EFV is a white to off white powder with a molecular mass of 315.68. It is practically insoluble in water (<10 microgram/mL).
3TC: The chemical name of 3TC is (2R,cis)-4-amino-1-(2-hydroxymethyl-1,3-oxathiolan-5-yl)-(1H)-pyrimidin-2-one. 3TC is the (-)enantiomer of a dideoxy analogue of cytidine. 3TC has also been referred to as (-)2',3'-dideoxy, 3'thiacytidine. It has a molecular formula of C
8H
11N
3O
3S and a molecular weight of 229.3 g per mol. It has the following structural formula:
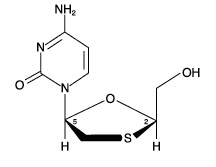
3TC is a white to off-white solid with a solubility of approximately 70 mg per mL in water at 20°C.
Tenofovir: TDF (a prodrug of tenofovir) is a fumaric acid salt of bis-isopropoxycarbonyloxymethyl ester derivative of tenofovir..
The chemical name of TDF is 9-[(R)-2[[bis[[(isopropoxycarbonyl)oxy]methoxy]phosphinyl]methoxy]propyl]adenine fumarate (1:1). It has a molecular formula of C
19H
30N
5O
10P•C
4H
4O
4 and a molecular weight of 635.52. It has the following structural formula:
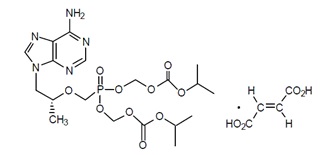
TDF is a white to off-white crystalline powder with a solubility of 13.4 mg/mL in distilled water at 25 oC. It has an octanol/phosphate buffer (pH 6.5) partition coefficient (log p) of 1.25 at 25 oC.
12 CLINICAL PHARMACOLOGY
12.2 Pharmacodynamics
Cardiac Electrophysiology: The effect of EFV on the QTc interval was evaluated in an open-label, positive and placebo-controlled, fixed single sequence 3-period, 3-treatment crossover QT study in 58 healthy subjects enriched for CYP2B6 polymorphisms. The mean C max of EFV in subjects with CYP2B6 *6/*6 genotype following the administration of 600 mg daily dose for 14 days was 2.25-fold the mean C max observed in subjects with CYP2B6 *1/*1 genotype. A positive relationship between EFV concentration and QTc prolongation was observed. Based on the concentration-QTc relationship, the mean QTc prolongation and its upper bound 90% confidence interval are 8.7 ms and 11.3 ms in subjects with CYP2B6*6/*6 genotype following the administration of 600 mg daily dose for 14 days [see Warnings and Precautions ( 5.2)].
12.3 Pharmacokinetics
The effect of food on efavirenz, lamivudine and tenofovir disoproxil fumarate tablets has not been evaluated.
EFV:
In HIV-1 infected subjects time-to-peak plasma concentrations were approximately 3 to 5 hours and steady-state plasma concentrations were reached in 6 to 10 days. EFV is highly bound (approximately 99.5 to 99.75%) to human plasma proteins, predominantly albumin. Following administration of 14C-labeled EFV, 14 to 34% of the dose was recovered in the urine (mostly as metabolites) and 16 to 61% was recovered in feces (mostly as parent drug). In vitro studies suggest CYP3A and CYP2B6 are the major isozymes responsible for EFV metabolism. EFV has been shown to induce CYP enzymes, resulting in induction of its own metabolism. EFV has a terminal half-life of 52 to 76 hours after single doses and 40 to 55 hours after multiple doses.
3TC:
Following oral administration, 3TC is rapidly absorbed and extensively distributed. After multiple dose oral administration of 3TC 300 mg once daily for 7 days to 60 healthy subjects, steady-state Cmax (Cmax,ss) was 2.04 ± 0.54 mcg per mL (mean ± SD) and the 24 hour steady state AUC (AUC 24,ss) was 8.87 ± 1.83 mcg•hour per mL. Binding to plasma protein is low. Approximately 70% of an intravenous dose of 3TC is recovered as unchanged drug in the urine. Metabolism of 3TC is a minor route of elimination. In humans, the only known metabolite is the trans sulfoxide metabolite (approximately 5% of an oral dose after 12 hours). In most single-dose trials in HIV-1-infected subjects, HBV-infected subjects, or healthy subjects with serum sampling for 24 hours after dosing, the observed mean elimination half-life (t ½) ranged from 5 to 7 hours. In HIV-1-infected subjects, total clearance was 398.5 ± 69.1 mL per min (mean ± SD).
TDF:
The pharmacokinetic properties of TDF are summarized in Table 6. Following oral administration of TDF, maximum tenofovir serum concentrations are achieved in 1.0 ± 0.4 hour. Less than 0.7% of tenofovir binds to human plasma proteins in vitro and the binding is independent of concentration over the range of 0.01 to 25 μg/mL. Approximately 70 to 80% of the intravenous dose of tenofovir is recovered as unchanged drug in the urine. Tenofovir is eliminated by a combination of glomerular filtration and active tubular secretion. Following a single oral dose of TDF, the terminal elimination half-life of tenofovir is approximately 17 hours.
Table 6 Single Dose Pharmacokinetic Parameters for Tenofovir in Adults a
|
| Tenofovir
|
| Fasted Oral Bioavailability
b (%)
| 25 (NC to 45.0)
|
| Plasma Terminal Elimination Half-Life
b (hr)
| 17 (12.0 to 25.7)
|
| Cmax
c (mcg/mL)
| 0.30±0.09
|
| AUC
c (mcg·hr/mL)
| 2.29±0.69
|
| CL/F
c (mL/min)
| 1043±115
|
| CLrenal
c (mL/min)
| 243±33
|
a. NC=Not calculated
b. Median (range)
c. Mean (± SD)
Special Populations
Race
EFV and 3TC: There are no significant or clinically relevant racial differences in EFV and 3TC pharmacokinetics.
Tenofovir Disoproxil Fumarate: There were insufficient numbers from racial and ethnic groups other than Caucasian to adequately determine potential pharmacokinetic differences among these populations.
Gender:
There are no significant or clinically relevant gender differences in the pharmacokinetics of EFV, 3TC, and TDF.
Geriatric Patients:
The pharmacokinetics of 3TC and TDF have not been studied in patients over 65 years of age.
Pediatric Patients:
Efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsshould not be administered to pediatric patients weighing less than 35 kg (77 lb).
Renal Impairment :[see Use in Specific Populations ( 8.6)].
The pharmacokinetics of TDF, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, are altered in subjects with renal impairment [see Warnings and Precautions ( 5.3)] . In subjects with creatinine clearance below 50 mL per min or with end stage renal disease (ESRD) requiring dialysis, Cmax, and AUC 0-∞ of tenofovir were increased. Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is not recommended for patients with creatinine clearance less than 50 mL per min or patients with ESRD requiring hemodialysis because it is a fixed-dose combination formulation that cannot be adjusted.
Hepatic Impairment
EFV: A multiple-dose study showed no significant effect on EFV pharmacokinetics in patients with mild hepatic impairment (Child-Pugh Class A) compared with controls. There were insufficient data to determine whether moderate or severe hepatic impairment (Child-Pugh Class B or C) affects EFV pharmacokinetics.
3TC: The pharmacokinetic properties of 3TC have been determined in adults with impaired hepatic function. Pharmacokinetic parameters were not altered by diminishing hepatic function. Safety and efficacy of 3TC have not been established in the presence of decompensate liver disease.
TDF: The pharmacokinetics of tenofovir following a 300 mg single dose of TDF have been studied in non-HIV infected subjects with moderate to severe hepatic impairment. There were no substantial alterations in tenofovir pharmacokinetics in subjects with hepatic impairment compared with unimpaired subjects. No change in TDF dosing is required in patients with hepatic impairment.
Drug Interactions Studies:[see Drug Interactions ( 7).]
EFV: EFV has been shown in vivo to cause hepatic enzyme induction, thus increasing the biotransformation of some drugs metabolized by CYP3A and CYP2B6. In vitro studies have shown that efavirenz inhibited CYP isozymes 2C9, 2C19, and 3A4 with K i values (8.5 to 17 µM) in the range of observed efavirenz plasma concentrations. In in vitro studies, EFV did not inhibit CYP2E1 and inhibited CYP2D6 and CYP1A2 (Ki values 82 to 160 µM) only at concentrations well above those achieved clinically. Coadministration of EFV with drugs primarily metabolized by CYP2C9, CPY2C19, CYP3A, or CYP2B6 isozymes may result in altered plasma concentrations of the coadministered drug. Drugs which induce CYP3A and CYP2B6 activity would be expected to increase the clearance of EFV resulting in lowered plasma concentrations.
Drug interaction studies were performed with EFV and other drugs likely to be coadministered or drugs commonly used as probes for pharmacokinetic interaction. The effects of coadministration of EFV on the C
max, AUC, and C
min are summarized in Table 7(effect of EFV on other drugs) and Table 8(effect of other drugs on EFV). For information regarding clinical recommendations see
Drug Interactions (7.5).
|
Table 7 Effect of EFV on Coadministered Drug Plasma C max, AUC, and C min |
||||||
|---|---|---|---|---|---|---|
|
|
Number of Subjects |
Coadministered Drug (mean % change) |
||||
|
Coadministered Drug |
Dose |
EFV Dose |
C max (90% CI) |
AUC (90% CI) |
C min (90% CI) |
|
|
Boceprevir |
800 mg tid x 6 days |
600 mg qd x 16 days |
NA |
↓ 8% (↓ 22-↑ 8%) |
↓ 19% (11-25%) |
↓ 44% (26-58%) |
|
Simeprevir |
150 mg qd x 14 days |
600 mg qd x 14 days |
23 |
↓ 51% (↓ 46-↓ 56%) |
↓ 71% (↓ 67-↓ 74%) |
↓ 91% (↓ 88-↓ 92%) |
|
Ledipasvir/ Sofosbuvir d |
90/400 mg qd x 14 days |
600 mg qd x 14 days |
15 |
↓34 (↓ 25-↓ 41) |
↓ 34 (↓ 25-↓ 41) |
↓ 34 (¯ 24-↓ 43) |
|
Ledipasvir |
|
|
|
↔ |
↔ |
NA |
|
Sofosbuvir GS-331007 e |
|
|
|
↔ |
↔ |
↔ |
|
Sofosbuvir f |
400 mg qd single dose |
600 mg qd x 14 days |
16 |
↓ 19 (↓ 40- ↑10) |
↔ |
NA |
|
GS-331007 e |
|
|
|
↓ 23 (↓16-↓ 30) |
↓ 16 (↓24-↓ 8) |
NA |
|
Sofosbuvir/ Velpatasvir g |
400/100 mg qd x 14 days |
600 mg qd x 14 days |
14 |
|
|
|
|
Sofosbuvir |
|
|
|
↑38 ( ↑14- ↑ 67) |
↔ |
NA |
|
GS-331007 e |
|
|
|
↓14 (↓ 20-↓7) |
↔ |
↔ |
|
Velpatasvir |
|
|
|
↓ 47 (↓ 57-¯↓36) |
↓ 53 (↓ 61-↓43) |
↓ 57 (↓ 64-↓ 48) |
|
Azithromycin |
600 mg single dose |
400 mg qd x 7 days |
14 |
↑ 22% (4-42%) |
↔ |
NA |
|
Clarithromycin |
500 mg q12h x 7 days |
400 mg qd x 7 days |
11 |
↓ 26% (15-35%) |
↓ 39% (30-46%) |
↓ 53% (42-63%) |
|
14-OH metabolite |
|
|
|
↑ 49% (32-69%) |
↑ 34% (18-53%) |
↑ 26% (9-45%) |
|
Fluconazole |
200 mg x 7 days |
400 mg qd x 7 days |
10 |
↔ |
↔ |
↔ |
|
Itraconazole |
200 mg q12h x 28 days |
600 mg qd x 14 days |
18 |
↓ 37% (20-51%) |
↓ 39% (21-53%) |
↓ 44% (27-58%) |
|
Hydroxy-itraconazole |
|
|
|
↓ 35% (12-52%) |
↓ 37% (14-55%) |
↓ 43% (18-60%) |
|
Posaconazole |
400 mg (oral suspension) bid x 10 and 20 days |
400 mg qd x 10 and 20 days |
11 |
↓ 45% (34-53%) |
↓ 50% (40-57%) |
NA |
|
Rifabutin |
300 mg qd x 14 days |
600 mg qd x 14 days |
9 |
↓ 32% (15-46%) |
↓ 38% (28-47%) |
↓ 45% (31-56%) |
|
Voriconazole |
400 mg po q12h x 1 day, then 200 mg po q12h x 8 days |
400 mg qd x 9 days |
NA |
↓ 61% a |
↓ 77% a |
NA |
|
|
300 mg po q12h days 2‑7 |
300 mg qd x 7 days |
NA |
↓ 36% b (21-49%) |
↓ 55% b (45-62%) |
NA |
|
|
400 mg po q12h days 2‑7 |
300 mg qd x 7 days |
NA |
↑ 23% b (↓ 1-↑ 53%) |
↓ 7% b (↓ 23-↑ 13%) |
NA |
|
Artemether/ lumefantrine |
Artemether 20 mg/ lumefantrine 120 mg tablets (6 4-tablet doses over 3 days) |
600 mg qd x 26 days |
12 |
|
|
|
|
Artemether |
|
↓ 21% |
↓ 51% |
NA |
||
|
dihydroartemisinin |
|
↓ 38% |
↓ 46% |
NA |
||
|
lumefantrine |
|
↔ |
↓ 21% |
NA |
||
|
Atorvastatin |
10 mg qd x 4 days |
600 mg qd x 15 days |
14 |
↓ 14% (1-26%) |
↓ 43% (34-50%) |
↓ 69% (49-81%) |
|
Total active (including metabolites) |
|
|
|
↓ 15% (2-26%) |
↓ 32% (21-41%) |
↓ 48% (23-64%) |
|
Pravastatin |
40 mg qd x 4 days |
600 mg qd x 15 days |
13 |
↓ 32% (↓ 59-↑ 12%) |
↓ 44% (26-57%) |
↓ 19% (0-35%) |
|
Simvastatin |
40 mg qd x 4 days |
600 mg qd x 15 days |
14 |
↓ 72% (63-79%) |
↓ 68% (62-73%) |
↓ 45% (20-62%) |
|
Total active (including metabolites) |
|
|
|
↓ 68% (55-78%) |
↓ 60% (52-68%) |
NA c |
|
Carbamazepine |
200 mg qd x 3 days, 200 mg bid x 3 days, then 400 mg qd x 29 days |
600 mg qd x 14 days |
12 |
↓ 20% (15-24%) |
↓ 27% (20-33%) |
↓ 35% (24-44%) |
|
Epoxide metabolite |
|
|
|
↔ |
↔ |
↓ 13% (↓ 30-↑ 7%) |
|
Cetirizine |
10 mg single dose |
600 mg qd x 10 days |
11 |
↓ 24% (18-30%) |
↔ |
NA |
|
Diltiazem |
240 mg x 21 days |
600 mg qd x 14 days |
13 |
↓ 60% (50-68%) |
↓ 69% (55-79%) |
↓ 63% (44-75%) |
|
Desacetyl diltiazem |
|
|
|
↓ 64% (57-69%) |
↓ 75% (59-84%) |
↓ 62% (44-75%) |
|
N-monodes-methyl diltiazem |
|
|
|
↓ 28% (7-44%) |
↓ 37% (17-52%) |
↓ 37% (17-52%) |
|
Ethinyl estradiol/ Norgestimate |
0.035 mg/0.25 mg x 14 days |
600 mg qd x 14 days |
|
|
|
|
|
Ethinyl estradiol |
|
|
21 |
↔ |
↔ |
↔ |
|
Norelgestromine |
|
|
21 |
↓ 46% (39-52%) |
↓ 64% (62-67%) |
↓ 82% (79-85%) |
|
Levonorgestrel |
|
|
6 |
↓ 80% (77-83%) |
↓ 83% (79-87%) |
↓ 86% (80-90%) |
|
Lorazepam |
2 mg single dose |
600 mg qd x 10 days |
12 |
↑ 16% (2-32%) |
↔ |
NA |
|
Methadone |
Stable maintenance 35‑100 mg daily |
600 mg qd x 14‑21 days |
11 |
↓ 45% (25-59%) |
↓ 52% (33-66%) |
NA |
|
Bupropion |
150 mg single dose (sustained-release) |
600 mg qd x 14 days |
13 |
↓ 34% (21-47%) |
↓ 55% (48-62%) |
NA |
|
Hydroxy-bupropion |
|
|
|
↑ 50% (20-80%) |
↔ |
NA |
|
Paroxetine |
20 mg qd x 14 days |
600 mg qd x 14 days |
16 |
↔ |
↔ |
↔ |
|
Sertraline |
50 mg qd x 14 days |
600 mg qd x 14 days |
13 |
↓ 29% (15-40%) |
↓ 39% (27-50%) |
↓ 46% (31-58%) |
|
↑ Indicates increase ↓ Indicates decrease ↔ Indicates no change or a mean increase or decrease of < 10%. a 90% CI not available. b Relative to steady-state administration of voriconazole (400 mg for 1 day, then 200 mg po q12h for 2 days). c Not available because of insufficient data. d Study conducted with ATRIPLA ®coadministered with HARVONI ®. e Thepredominantcirculatingnucleosidemetabolite of sofosbuvir. f Study conducted with ATRIPLA coadministered with SOVALDI ® (sofosbuvir). g Study conducted with ATRIPLA coadministered with EPCLUSA ®. NA = not available. |
||||||
| Table 8 Effect of Coadministered Drug on EFV Plasma Cmax, AUC, and Cmin
|
||||||
|---|---|---|---|---|---|---|
|
| Number of Subjects
| EFV
(mean % change) |
||||
| Coadministered Drug
| Dose
| EFV Dose
| Cmax
(90% CI) | AUC
(90% CI) | Cmin
(90% CI) |
|
| Boceprevir
| 800 mg tid x 6 days
| 600 mg qd x 16 days
| NA
| ↑ 11%
(2-20%) | ↑ 20%
(15-26%) | NA
|
| Simeprevir
| 150 mg qd x 14 days
| 600 mg qd x 14 days
| 23
| ↔
| ↓ 10%
(5-15%) | ↓ 13%
(7-19%) |
| Azithromycin
| 600 mg single dose
| 400 mg qd x 7 days
| 14
| ↔
| ↔
| ↔
|
| Clarithromycin
| 500 mg q12h x 7 days
| 400 mg qd x 7 days
| 12
| ↑ 11%
(3-19%) | ↔
| ↔
|
| Fluconazole
| 200 mg x 7 days
| 400 mg qd x 7 days
| 10
| ↔
| ↑ 16%
(6-26%) | ↑ 22%
(5-41%) |
| Itraconazole
| 200 mg q12h x 14 days
| 600 mg qd x 28 days
| 16
| ↔
| ↔
| ↔
|
| Rifabutin
| 300 mg qd x 14 days
| 600 mg qd x 14 days
| 11
| ↔
| ↔
| ↓ 12%
(↓ 24-↑ 1%) |
| Rifampin
| 600 mg x 7 days
| 600 mg qd x 7 days
| 12
| ↓ 20%
(11-28%) | ↓ 26%
(15-36%) | ↓ 32%
(15-46%) |
| Voriconazole
| 400 mg po q12h x 1 day, then 200 mg po q12h x 8 days
| 400 mg qd x 9 days
| NA
| ↑ 38%a
| ↑ 44%
a
| NA
|
| 300 mg po q12h days 2-7
| 300 mg qd x 7 days
| NA
| ↓ 14%
b
(7-21%) | ↔
b
| NA
|
|
| 400 mg po q12h days 2-7
| 300 mg qd x 7 days
| NA
| ↔b
| ↑ 17%b
(6-29%) | NA
|
|
| Artemether/
Lumefantrine | Artemether 20 mg/ lumefantrine 120 mg tablets (6 4-tablet doses over 3 days)
| 600 mg qd x 26 days
| 12
| ↔
| ↓ 17%
| NA
|
| Atorvastatin
| 10 mg qd x 4 days
| 600 mg qd x 15 days
| 14
| ↔
| ↔
| ↔
|
| Pravastatin
| 40 mg qd x 4 days
| 600 mg qd x 15 days
| 11
| ↔
| ↔
| ↔
|
| Simvastatin
| 40 mg qd x 4 days
| 600 mg qd x 15 days
| 14
| ↓ 12%
(↓ 28-↑ 8%) | ↔
| ↓ 12%
(↓ 25-↑ 3%) |
| Aluminum hydroxide 400 mg, magnesium hydroxide 400 mg, plus simethicone 40 mg
| 30 mL single dose
| 400 mg single dose
| 17
| ↔
| ↔
| NA
|
| Carbamazepine
| 200 mg qd x 3 days, 200 mg bid x 3 days, then 400 mg qd x 15 days
| 600 mg qd x 35 days
| 14
| ↓ 21%
(15-26%) | ↓ 36%
(32-40%) | ↓ 47%
(41-53%) |
| Cetirizine
| 10 mg single dose
| 600 mg qd x 10 days
| 11
| ↔
| ↔
| ↔
|
| Diltiazem
| 240 mg x 14 days
| 600 mg qd x 28 days
| 12
| ↑ 16%
(6-26%) | ↑ 11%
(5-18%) | ↑ 13%
(1-26%) |
| Famotidine
| 40 mg single dose
| 400 mg single dose
| 17
| ↔
| ↔
| NA
|
| Paroxetine
| 20 mg qd x 14 days
| 600 mg qd x 14 days
| 12
| ↔
| ↔
| ↔
|
| Sertraline
| 50 mg qd x 14 days
| 600 mg qd x 14 days
| 13
| ↑ 11%
(6-16%) | ↔
| ↔
|
| ↑ Indicates increase ↓ Indicates decrease ↔ Indicates no change or a mean increase or decrease of < 10%.
a 90% CI not available. b Relative to steady-state administration of efavirenz (600 mg once daily for 9 days). NA = not available. |
||||||
3TC
Effect of 3TC on the Pharmacokinetics of Other Agents: Based on in vitro study results, 3TC at therapeutic drug exposures is not expected to affect the pharmacokinetics of drugs that are substrates of the following transporters: organic anion transporter polypeptide 1B1/3 (OATP1B1/3), breast cancer resistance protein (BCRP), P-glycoprotein (P-gp), multidrug and toxin extrusion protein 1 (MATE1), MATE2-K, organic cation transporter 1 (OCT1), OCT2, or OCT3.
Effect of Other Agents on the Pharmacokinetics of 3TC: 3TC is a substrate of MATE1, MATE2-K, and OCT2 in vitro. Trimethoprim (an inhibitor of these drug transporters) has been shown to increase 3TC plasma concentrations. This interaction is not considered clinically significant as no dose adjustment of 3TC is needed.
3TC is a substrate of P-gp and BCRP; however, considering its absolute bioavailability (87%), it is unlikely that these transporters play a significant role in the absorption of 3TC. Therefore, coadministration of drugs that are inhibitors of these efflux transporters is unlikely to affect the disposition and elimination of 3TC.
Interferon Alfa: There was no significant pharmacokinetic interaction between 3TC and interferon alfa in a trial of 19 healthy male subjects [see Warnings and Precautions ( 5.9)].
Ribavirin: In vitro data indicate ribavirin reduces phosphorylation of 3TC, stavudine, and zidovudine. However, no pharmacokinetic (e.g., plasma concentrations or intracellular triphosphorylated active metabolite concentrations) or pharmacodynamic (e.g., loss of HIV-1/HCV virologic suppression) interaction was observed when ribavirin and 3TC (n = 18), stavudine (n = 10), or zidovudine (n = 6) were coadministered as part of a multi-drug regimen to HIV-1/HCV co-infected subjects [see Warnings and Precautions (5.9)].
Sorbitol (Excipient): 3TC and sorbitol solutions were coadministered to 16 healthy adult subjects in an open-label, randomized-sequence, 4-period, crossover trial. Each subject received a single 300-mg dose of 3TC oral solution alone or coadministered with a single dose of 3.2 grams, 10.2 grams, or 13.4 grams of sorbitol in solution. Coadministration of 3TC with sorbitol resulted in dose-dependent decreases of 20%, 39%, and 44% in the AUC (0-24), 14%, 32%, and 36% in the AUC (∞), and 28%, 52%, and 55% in the C max of 3TC, respectively.
Trimethoprim/Sulfamethoxazole: 3TC and TMP/SMX were coadministered to 14 HIV-1-positive subjects in a single-center, open-label, randomized, crossover trial. Each subject received treatment with a single 300 mg dose of lamivudine and TMP 160 mg/SMX 800 mg once a day for 5 days with concomitant administration of 3TC 300 mg with the fifth dose in a crossover design. Coadministration of TMP/SMX with 3TC resulted in an increase of 43% ± 23% (mean ± SD) in lamivudine AUC∞, a decrease of 29% ± 13% in lamivudine oral clearance, and a decrease of 30% ± 36% in 3TC renal clearance. The pharmacokinetic properties of TMP and SMX were not altered by coadministration with lamivudine. There is no information regarding the effect on 3TC pharmacokinetics of higher doses of TMP/SMX such as those used in treat PCP.
TDF
At concentrations substantially higher (~300-fold) than those observed in vivo, tenofovir did not inhibit in vitro drug metabolism mediated by any of the following human CYP isoforms: CYP3A4, CYP2D6, CYP2C9, or CYP2E1. However, a small (6%) but statistically significant reduction in metabolism of CYP1A substrate was observed. Based on the results of in vitro experiments and the known elimination pathway of tenofovir, the potential for CYP mediated interactions involving TDF with other medicinal products is low.
Table 9 summarizes pharmacokinetic effects of coadministered drug on tenofovir pharmacokinetics. No clinically significant drug interactions have been observed between TDF and ribavirinor sofosbuvir.
Table 9 Drug Interactions: Changes in Pharmacokinetic Parameters for Tenofovir a in the Presence of the Coadministered Drug
| Coadministered Drug
| Dose of Coadministered Drug (mg)
| N
| % Change of Tenofovir Pharmacokinetic Parameters
b(90% CI)
|
||
|---|---|---|---|---|---|
| C
max
| AUC
| C
min
|
|||
| Ledipasvir/ Sofosbuvir
e,f
| 90/400oncedaily × 10days
| 24
| ↑ 47
(↑ 37 to↑58) | ↑ 35
(↑ 29 to↑ 42) | ↑ 47
(↑ 38 to↑57) |
| Ledipasvir/ Sofosbuvir
e,g
| 23
| ↑ 64
(↑ 54 to↑74) | ↑ 50
(↑ 42 to↑59) | ↑ 59
(↑ 49 to↑70) |
|
| Ledipasvir/ Sofosbuvir
h
| 90/400oncedaily × 14 days
| 15
| ↑ 79
(↑ 56 to↑104) | ↑ 98
(↑ 77 to↑123) | ↑ 163
(↑ 132to↑ 197) |
| Sofosbuvir
i
| 400singledose
| 16
| ↑ 25
(↑8 to ↑ 45) | ⇔
| ⇔
|
| Sofosbuvir/ Velpatasvir
j
| 400/100 once daily
| 24
| ↑ 44
(↑33to↑55) | ↑ 40
(↑34to↑ 46) | ↑ 84
(↑76to↑92) |
| Sofosbuvir/ Velpatasvir
k
| 400/100 once daily
| 30
| ↑ 46
(↑39to↑54) | ↑ 40
(↑34to↑45) | ↑ 70
(↑61to↑79) |
| Sofosbuvir/ Velpatasvir/
Voxilaprevir l | 400/100/100 +
Voxilaprevir m 100 once daily | 29
| ↑48
(↑36 to ↑61) | ↑39
(↑32 to ↑46) | ↑47
(↑38 to ↑56) |
| Tacrolimus
| 0.05 mg/kg twice daily × 7 days
| 21
| ↑ 13
(↑1 to↑ 27) | ⇔
| ⇔
|
a Subjects received VIREAD 300 mg once daily.
b Increase = ↑; Decrease = ↓; No Effect = ⇔; NC = Not Calculated
e Data generated from simultaneous dosing with HARVONI (ledipasvir/sofosbuvir). Staggered administration (12 hours apart) provided similar results.
f Comparison based on exposures when administered as atazanavir/ritonavir + FTC/TDF.
g Comparison based on exposures when administered as darunavir/ritonavir + FTC/TDF.
h Study conducted with ATRIPLA(EFV/FTC/TDF) coadministered with HARVONI; coadministration with HARVONI also results in comparable increases in tenofovir exposure when TDF is administered as COMPLERA(FTC/rilpivirine/TDF), or TRUVADA + dolutegravir.
i Study conducted with ATRIPLA coadministered with SOVALDI (sofosbuvir).
j Study conducted with COMPLERAcoadministered with EPCLUSA; coadministration with EPCLUSA also results in comparable increases in tenofovir exposures when TDF is administered as ATRIPLA, STRIBILD (elvitegravir/cobicistat/FTC/TDF), TRUVADA + atazanavir/ritonavir, or TRUVADA + darunavir/ritonavir.
k Administered as raltegravir + FTC/TDF.
l Comparison based on exposures when administered as darunavir/ritonavir + FTC/TDF.
m Study conducted with additional voxilaprevir 100 mg to achieve voxilaprevir exposures expected in HCV-infected patients
12.4 Microbiology
Mechanism of Action
EFV: EFV is an NNRTI of HIV-1. EFV activity is mediated predominantly by noncompetitive inhibition of HIV-1 reverse transcriptase (RT). HIV-2 RT and human cellular DNA polymerases α, β, γ, and δ are not inhibited by EFV.
3TC: 3TC is a synthetic nucleoside analogue. Intracellularly, 3TC is phosphorylated to its active 5′-triphosphate metabolite, lamivudine triphosphate (3TC-TP). The principal mode of action of 3TC-TP is inhibition of HIV-1 reverse transcriptase (RT) via DNA chain termination after incorporation of the nucleotide analogue.
TDF: TDF is an acyclic nucleoside phosphonate diester analog of adenosine monophosphate. TDF requires initial diester hydrolysis for conversion to tenofovir and subsequent phosphorylations by cellular enzymes to form tenofovir diphosphate, an obligate chain terminator. Tenofovir diphosphate inhibits the activity of HIV-1 reverse transcriptase by competing with the natural substrate deoxyadenosine 5’-triphosphate and, after incorporation into DNA, by DNA chain termination. Tenofovir diphosphate is a weak inhibitor of mammalian DNA polymerases α, β, and mitochondrial DNA polymerase γ.
Antiviral Activity in Cell Culture
EFV: The concentration of EFV inhibiting replication of wild-type laboratory adapted strains and clinical isolates in cell culture by 90 to 95% (EC 90 to 95) ranged from 1.7 to 25 nM in lymphoblastoid cell lines, peripheral blood mononuclear cells (PBMCs), and macrophage/monocyte cultures. EFV demonstrated antiviral activity against clade B and most non-clade B isolates (subtypes A, AE, AG, C, D, F, G, J, N), but had reduced antiviral activity against group O viruses.
3TC:The antiviral activity of 3TC against HIV-1 was assessed in a number of cell lines including monocytes and PBMCs using standard susceptibility assays. EC50 values were in the range of 0.003 to 15 microM (1 microM = 0.23 mcg per mL). The median EC50 values of lamivudine were 60 nM (range: 20 to 70 nM), 35 nM (range: 30 to 40 nM), 30 nM (range: 20 to 90 nM), 20 nM (range: 3 to 40 nM), 30 nM (range: 1 to 60 nM), 30 nM (range: 20 to 70 nM), 30 nM (range: 3 to 70 nM), and 30 nM (range: 20 to 90 nM) against HIV-1 clades A-G and group O viruses (n = 3 except n = 2 for clade B) respectively. The EC50 values against HIV-2 isolates (n = 4) ranged from 0.003 to 0.120 microM in PBMCs. 3TC was not antagonistic to all tested anti-HIV agents. Ribavirin (50 microM) used in the treatment of chronic HCV infection decreased the anti-HIV-1 activity of lamivudine by 3.5-fold in MT-4 cells.
TDF: The antiviral activity of tenofovir against laboratory and clinical isolates of HIV-1 was assessed in lymphoblastoid cell lines, primary monocyte/macrophage cells and peripheral blood lymphocytes. The EC 50 (50% effective concentration) values for tenofovir were in the range of 0.04 microM to 8.5 microM. Tenofovir displayed antiviral activity in cell culture against HIV-1 clades A, B, C, D, E, F, G, and O (EC 50 values ranged from 0.5 μM to 2.2 μM) and strain-specific activity against HIV-2 (EC 50 values ranged from 1.6 μM to 5.5 μM). Please see the full prescribing information for TDF for information regarding the inhibitory activity of TDF against HBV.
Resistance in Cell Culture
EFV: In cell culture, HIV-1 isolates with reduced susceptibility to EFV (>380-fold increase in EC 90 value) emerged rapidly in the presence of drug. Genotypic characterization of these viruses identified single amino acid substitutions L100I or V179D, double substitutions L100I/V108I, and triple substitutions L100I/V179D/Y181C in RT.
Clinical isolates with reduced susceptibility in cell culture to EFV have been obtained. One or more RT substitutions at amino acid positions A98, L100, K101, K103, V106, V108, Y188, G190, P225, F227 and M230 were observed in patients failing treatment with EFV in combination with indinavir, or with 3TC plus zidovudine. The K103N substitution was the most frequently observed.
3TC:
3TC-resistant variants of HIV-1 have been selected in cell culture. Genotypic analysis showed that the resistance was predominantly due to a methionine to valine or isoleucine (M184V/I).
TDF: HIV-1 isolates with reduced susceptibility to tenofovir have been selected in cell culture. These viruses expressed a K65R substitution in reverse transcriptase and showed a 2- to 4-fold reduction in susceptibility to tenofovir.In addition, a K70E substitution in HIV-1 reverse transcriptase has been selected by tenofovir and results in low-level reduced susceptibility to tenofovir. K65R substitutions developed in some subjects failing a TDF regimen.
Cross-Resistance
EFV: Cross-resistance among NNRTIs has been observed. Clinical isolates previously characterized as EFV-resistant were also phenotypically resistant in cell culture to delavirdine (DLV) and nevirapine (NVP) compared to baseline. DLV- and/or NVP-resistant clinical viral isolates with NNRTI resistance-associated substitutions (A98G, L100I, K101E/P, K103N/S, V106A, Y181X, Y188X, G190X, P225H, F227L, or M230L) showed reduced susceptibility to EFV in cell culture. Greater than 90% of NRTI-resistant clinical isolates tested in cell culture retained susceptibility to EFV.
3TC: Cross-resistance among certain NRTIs has been observed. 3TC-resistant HIV-1 isolates were cross-resistant in cell culture to didanosine (ddI). Cross-resistance is also expected with abacavir and emtricitabine as these select M184V substitutions.
TDF: Cross-resistance among certain NRTIs has been recognized. The K65R and K70E substitution selected by tenofovir are also selected in some HIV-1 infected subjects treated with abacavir, didanosine, or zalcitabine. HIV-1 isolates with the K65R substitution also showed reduced susceptibility to emtricitabine and 3TC. HIV-1 isolates from subjects (N=20) whose HIV-1 expressed a mean of 3 zidovudine-associated RT amino acid substitutions (M41L, D67N, K70R, L210W, T215Y/F, or K219Q/E/N) showed a 3.1-fold decrease in the susceptibility to tenofovir. Subjects whose virus expressed an L74V substitution without zidovudine resistance-associated substitutions (N=8) had reduced response to TDF. Limited data are available for patients whose virus expressed a Y115F substitution (N=3), Q151M substitution (N=2), or T69 insertion (N=4), all of whom had a reduced response.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis & Mutagenesis & Impairment Of Fertility
EFV: Long-term carcinogenicity studies in mice and rats were carried out with EFV. Mice were dosed with 0, 25, 75, 150, or 300 mg/kg/day for 2 years. Incidences of hepatocellular adenomas and carcinomas and pulmonary alveolar/bronchiolar adenomas were increased above background in females. No increases in tumor incidence above background were seen in males. There was no NOAEL in female established for this study because tumor findings occurred at all doses. AUC at the NOAEL (150 mg/kg) in the males was approximately 0.9 times that in humans at the recommended clinical dose. In the rat study, no increases in tumor incidence were observed at doses up to 100 mg/kg/day, for which AUCs were 0.1 (males) or 0.2 (females) times those in humans at the recommended clinical dose.
EFV tested negative in a battery of in vitro and in vivo genotoxicity assays. These included bacterial mutation assays in S. typhimurium and E. coli, mammalian mutation assays in Chinese hamster ovary cells, chromosome aberration assays in human peripheral blood lymphocytes or Chinese hamster ovary cells, and an in vivo mouse bone marrow micronucleus assay.
EFV did not impair mating or fertility of male or female rats, and did not affect sperm of treated male rats. The reproductive performance of offspring born to female rats given EFV was not affected. The AUCs at the NOAEL values in male (200 mg/kg) and female (100 mg/kg) rats were approximately ≤0.15 times that in humans at the recommended clinical dose
3TC: Long-term carcinogenicity studies with 3TC in mice and rats showed no evidence of carcinogenic potential at exposures up to 10 times (mice) and 58 times (rats) the human exposures at the recommended dose of 300 mg.
3TC was mutagenic in an L5178Y mouse lymphoma assay and clastogenic in a cytogenetic assay using cultured human lymphocytes. 3TC was not mutagenic in a microbial mutagenicity assay, in an in vitro cell transformation assay, in a rat micronucleus test, in a rat bone marrow cytogenetic assay, and in an assay for unscheduled DNA synthesis in rat liver. 3TC showed no evidence of in vivo genotoxic activity in the rat at oral doses of up to 2,000 mg per kg, producing plasma levels of 35 to 45 times those in humans at the recommended dose for HIV-1 infection.
TDF: Long-term oral carcinogenicity studies of TDF in mice and rats were carried out at exposures up to approximately 16 times (mice) and 5 times (rats) those observed in humans at the therapeutic dose for HIV-1 infection. At the high dose in female mice, liver adenomas were increased at exposures 16 times that in humans. In rats, the study was negative for carcinogenic findings at exposures up to 5 times that observed in humans at the therapeutic dose.
TDF was mutagenic in the in vitro mouse lymphoma assay and negative in an in vitro bacterial mutagenicity test (Ames test). In an in vivo mouse micronucleus assay, TDF was negative when administered to male mice.
There were no effects on fertility, mating performance or early embryonic development when TDF was administered to male rats at a dose equivalent to 10 times the human dose based on body surface area comparisons for 28 days prior to mating and to female rats for 15 days prior to mating through day seven of gestation. There was, however, an alteration of the estrous cycle in female rats.
13.2 Animal Pharmacology & OR Toxicology
EFV: Nonsustained convulsions were observed in 6 of 20 monkeys receiving EFV at doses yielding plasma AUC values 4- to 13-fold greater than those in humans given the recommended dose [see Warnings and Precautions ( 5.11)].
TDF: Tenofovir and TDF administered in toxicology studies to rats, dogs, and monkeys at exposures (based on AUCs) greater than or equal to 6 fold those observed in humans caused bone toxicity. In monkeys the bone toxicity was diagnosed as osteomalacia. Osteomalacia observed in monkeys appeared to be reversible upon dose reduction or discontinuation of tenofovir. In rats and dogs, the bone toxicity manifested as reduced bone mineral density. The mechanism(s) underlying bone toxicity is unknown.
Evidence of renal toxicity was noted in 4 animal species. Increases in serum creatinine, BUN, glycosuria, proteinuria, phosphaturia, and/or calciuria and decreases in serum phosphate were observed to varying degrees in these animals. These toxicities were noted at exposures (based on AUCs) 2 to 20 times higher than those observed in humans. The relationship of the renal abnormalities, particularly the phosphaturia, to the bone toxicity is not known.
14 CLINICAL STUDIES
14.1 Clinical Efficacy in Patients with HIV-1 Infection
Treatment-Naïve Adult Patients
The efficacy of EFV 400 mg, 3TC 300 mg, and TDF 300 mg in the treatment of HIV-1 infection in adults with no antiretroviral treatment history was established in trials of:
· Trial 903 which evaluated the efficacy of a three-drug regimen including EFV 600 mg, 3TC 300 mg and TDF 300 mg
· ENCORE1, which evaluated the comparability of 400 mg of EFV in a triple drug regimen to a 600 mg dose of EFV in a triple drug regimen.
Trial 903: Data through 144 weeks are reported for Trial 903, a double-blind, active-controlled multicenter trial comparing TDF (300 mg once daily) administered in combination with 3TC and EFV versus stavudine (d4T), 3TC, and EFV in 600 antiretroviral-naïve subjects. Subjects had a mean age of 36 years (range 18 to 64), 74% were male, 64% were Caucasian and 20% were Black. The mean baseline CD4 +cell count was 279 cells/mm 3(range 3 to 956) and median baseline plasma HIV-1 RNA was 77,600 copies/mL (range 417 to 5,130,000). Subjects were stratified by baseline HIV-1 RNA and CD4 +cell count. Forty-three percent of subjects had baseline viral loads >100,000 copies/mL and 39% had CD4 +cell counts <200 cells/mm 3. Table 10 provides treatment outcomes through 48 and 144 weeks.
Table 10 Outcomes of Randomized Treatment at Week 48 and 144 (Trial 903)
|
| At Week 48
| At Week 144
|
||
| Outcomes
| TDF+3TC
+EFV (N=299) | d4T+3TC
+EFV (N=301) | TDF+3TC+EFV (N=299)
| d4T+3TC+EFV
(N=301) |
| Responder
a
| 79%
| 82%
| 68%
| 62%
|
| Virologic failure
b
| 6%
| 4%
| 10%
| 8%
|
| Rebound
| 5%
| 3%
| 8%
| 7%
|
| Never suppressed
| 0%
| 1%
| 0%
| 0%
|
| Added an antiretroviral agent
| 1%
| 1%
| 2%
| 1%
|
| Death
| <1%
| 1%
| <1%
| 2%
|
| Discontinued due to adverse event
| 6%
| 6%
| 8%
| 13%
|
| Discontinued for other reasons
c
| 8%
| 7%
| 14%
| 15%
|
a. Subjects achieved and maintained confirmed HIV-1 RNA <400 copies/mL through Week 48 and 144.
b. Includes confirmed viral rebound and failure to achieve confirmed <400 copies/mL through Week 48 and 144.
c. Includes lost to follow-up, subject’s withdrawal, noncompliance, protocol violation and other reasons.
Achievement of plasma HIV-1 RNA concentrations of less than 400 copies/mL at Week 144 was similar between the two treatment groups for the population stratified at baseline on the basis of HIV-1 RNA concentration (> or ≤100,000 copies/mL) and CD4 + cell count (< or ≥200 cells/mm 3). Through 144 weeks of therapy, 62% and 58% of subjects in the TDF and d4T arms, respectively achieved and maintained confirmed HIV-1 RNA <50 copies/mL. The mean increase from baseline in CD4 +cell count was 263 cells/mm 3 for the TDF arm and 283 cells/mm 3for the d4T arm. Through 144 weeks, 11 subjects in the TDF group and 9 subjects in the d4T group experienced a new CDC Class C event.
The ENCORE1 Trial was a randomized, multinational clinical study comparing EFV 400 mg vs. EFV 600 mg in 630 antiretroviral-naïve adult subjects. Subjects were randomized 1:1 to receive EFV 400 mg in combination with TDF 300 mg plus FTC 200 mg all given once daily or EFV 600 mg in combination with TDF 300 mg/FTC 200 mg given once daily. The randomization was stratified by the clinical sites and the screening visit plasma HIV RNA level, either < 100,000 copies/mL or ≥ 100,000 copies/mL.
Subjects had a mean age of 36 years (range 18 to 69), 68% were male, 37% were of African heritage, 33% were of Asian ethnicity, 17% were Hispanic and 13% were Caucasian.
The mean baseline CD4+ cell count was 273 cells/mm 3 (range 38 to 679). Median baseline viral load was 56,469 copies/mL (range 162 to 10,000,000). Thirty-four percent of subjects had baseline viral load of ≥ 100,000 copies/mL.
Table 11 provides treatment outcomes through Week 48.
Table 11 Virologic Outcomes of Randomized Treatment in Trial ENCORE 1 in Treatment-Naïve Subjects at Week 48
|
| At Week 48
|
|
| Outcomes (< 50 copies/mL)
| EFV400 mg +FTC+ TDF
(N = 321) | EFV600 mg +FTC + TDF
(N = 309) |
| Responder
a
HIV-1 RNA < 50 copies/mL | 86%
| 84%
|
| Virologic failure
b
HIV-1 RNA ≥ 50 copies/mL | 11%
| 11%
|
| Rebound
| 9%
| 8%
|
| Never suppresse
d
| 2%
| 3%
|
| Death
| 1%
| 1%
|
| Discontinued for other reasons
c
| 2%
| 4%
|
a Subjects achieved confirmed HIV-1 RNA < 50 copies/mL at Week 48.
b Includes confirmed viral rebound and failure to achieve confirmed < 50 copies/mL through Week 48
c Includes discontinued due to Adverse Event, lost to follow-up, subject’s withdrawal, noncompliance, protocol violation and other reasons.
Achievement of plasma HIV-1 RNA concentrations of less than 50 copies/mL at Week 48 was similar between the two treatment groups for the population stratified at baseline on the basis of HIV-1 RNA concentration (< or ≥100,000 copies/mL). The mean increase at Week 48 from baseline in CD4 +cell count was 183 cells/mm 3 for the EFV 400 mg arm and 158 cells/mm 3for the EFV 600 mg arm. Through 48 weeks, 11 subjects in the EFV 400 mg group and 5 subjects in the EFV 600 mg group experienced a new CDC Class C event.
16 HOW SUPPLIED/STORAGE AND HANDLING
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets 400mg/300mg/300mgarepink colored, capsule shaped, biconvex, film coated tablets debossed with “F 31” on one side and plain on the other side.
Bottle of 30 tablets with silica gel desiccant, induction seal, and child-resistant cap - NDC 33342-362-07
Bottle of 90 tablets with silica gel desiccant, induction seal,and child-resistant cap - NDC 33342-362-10
Bottle of 180 tablets with silica gel desiccant and induction seal - NDC 33342-362-57
Store below 30ºC (86°F)
Store and dispense in original bottle, protect from moisture, and keep bottle tightly closed. Do not remove desiccant. Keep out of reach of children.
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Drug Interactions:Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets may interact with many drugs; therefore, advise patients to report to their healthcare provider the use of any other prescription, nonprescription medication, or herbal products, particularly St. John’s wort [see Contraindications ( 4) and Drug Interactions ( 7)] .
Patients with Hepatitis B or C Co-infection: Inform patients that severe acute exacerbations of hepatitis B have been reported in patients infected with hepatitis B virus (HBV) who have discontinued TDF and 3TC, two components of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Advise patients not to discontinue efavirenz, lamivudine and tenofovir disoproxil fumarate tablets without first informing their healthcare provider. All patients should be tested for HBV infection before or when starting efavirenz, lamivudine and tenofovir disoproxil fumarate tablets and those who are infected with HBV need close medical follow-up for several months after stopping efavirenz, lamivudine and tenofovir disoproxil fumarate tablets to monitor for exacerbations of hepatitis [see Warnings and Precautions ( 5.1)] .
Inform patients with HIV-1/HCV co-infection that hepatic decompensation (some fatal) has occurred in HIV-1/HCV co-infected patients receiving combination antiretroviral therapy for HIV-1 and interferon alfa with or without ribavirin [see Warnings and Precautions ( 5.9)] .
New Onset or Worsening Renal Impairment:Inform patients that renal impairment, including cases of acute renal failure and Fanconi syndrome, has been reported. Advise patients with creatinine clearance less than 50 mL per min or patients with end-stage renal disease (ESRD) requiring hemodialysis to avoid efavirenz, lamivudine and tenofovir disoproxil fumarate tablets with concurrent or recent use of a nephrotoxic agent (e.g., high-dose or multiple NSAIDs) [see Dosageand Administration ( 2.3), Warnings and Precautions ( 5.3)] .
Psychiatric Symptoms: Inform patients that serious psychiatric symptoms including severe depression, suicide attempts, aggressive behavior, delusions, paranoia, psychosis-like symptoms and catatonia have been reported in patients receiving EFV [s eeWarnings and Precauti ons ( 5.4)] . Advise patients to seek immediate medical evaluation if they experience severe psychiatric adverse experiences. Advise patients to inform their physician of any history of mental illness or substance abuse.
Nervous System Symptoms: Inform patients that central nervous system symptoms (NSS) including dizziness, insomnia, impaired concentration, drowsiness, and abnormal dreams are commonly reported during the first weeks of therapy with EFV, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets [seeWarnings and Precautions ( 5.5)] . Dosing at bedtime may improve the tolerability of these symptoms, which are likely to improve with continued therapy. Alert patients to the potential for additive effects when efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsis used concomitantly with alcohol or psychoactive drugs. Instruct patients that if they experience NSS to avoid potentially hazardous tasks such as driving or operating machinery [see Dosage and Administration ( 2.2)] .
Embryo-Fetal Toxicity:Apprise patients of the potential harm to the fetus if efavirenz, lamivudine and tenofovir disoproxil fumarate tabletsis used during the first trimester of pregnancy, or if the patient becomes pregnant while taking this drug. Instruct adults and adolescents of childbearing potential receving efavirenz, lamivudine and tenofovir disoproxil fumarate tablets to avoid pregnancy and to notify their healthcare provider if they become pregnant or plan to become pregnant with taking efavirenz, lamivudine and tenofovir disoproxil fumarate tablets [see Warnings and Precautions ( 5.6)]. A reliable form of barrier contraception must always be used in combination with other methods of contraception, including oral or other hormonal contraception. Because of the long half-life of EFV, recommend use of adequate contraceptive measures for 12 weeks after discontinuation of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets [see Use in Specific Populations ( 8.1, 8.3)] .
Rash: Inform patients that rash is a common side effect of EFV, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets [seeWarnings and Precautions ( 5.7)] . Rashes usually go away without any change in treatment. However, since rash may be serious, patients should be advised to contact their physician promptly if rash occurs.
Hepatotoxicity: Inform patients to watch for early warning signs of liver inflammation or failure, such as fatigue, weakness, lack of appetite, nausea and vomiting, as well as later signs such as jaundice, confusion, abdominal swelling, and discolored feces and to consult their healthcare provider promptly if such symptoms occur [see Warnings and Precautions ( 5.8)].
Risk of Pancreatitis: Advise parents or guardians to monitor pediatric patients for signs and symptoms of pancreatitis [see Warnings and Precautions ( 5.10)] .
Convulsions:Inform patients that convulsions have been reported with the use of EFV, a component of a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Patients who receiving concomitant anticonvulsant medications primarily metabolizedby the liver may require monitoring of plasma levels [see Warnings and Precautions ( 5.11)].
Lipid Elevations: Advise patients treatment with EFV, a component of a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, has resulted in increases in the concentration of total cholesterol and triglycerides [see Warnings and Precautions ( 5.12)].
Bone Loss and Mineralization Defects: Inform patients that decreases in bone mineral density have been observed with the use of TDF, a component of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Advise patients that bone mineral density monitoring may be performed in patietnswho have a history of pathologic bone fracture or other risk factors for osteoporosis or bone loss [see Warnings and Precautions ( 5.13)] .
Immune Reconstitution Syndrome: Advise patients to inform their healthcare provider immediately of any signs and symptoms of infection as inflammation from previous infection may occur soon after combination antiretroviral therapy, including when efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets is started [see Warnings and Precautions ( 5.14)].
Lactic Acidosis/Hepatomegaly: Inform patients that lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported. Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets should be suspended in any patients who develop clinical symptoms suggestive of lactic acidosis or pronounced hepatotoxicity (including nausea, vomiting, unusual or unexpected stomach discomfort, and weakness) [see Warnings and Precautions ( 5.15)] .
Pregnancy Exposure Registry: Advise patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to efavirenz, lamivudine, and tenofovir disoproxil fumarate tabletsduring pregnancy [see Use in Specific Populations (8.1)].
Lactation:Instruct mothers with HIV-1 infection not to breastfeed because HIV-1 can be passed to the baby in the breast milk [see Use in Specific Populations ( 8.2)] .
Missed Dose:Instruct patients that if they miss a dose of efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets, to take it as soon as they remember. Advise patients not to double their next dose or take more than the prescribed dose.
Storage: Instruct patients to store efavirenz, lamivudine, and tenofovir disoproxil fumarate tablets in the original bottle, protect from moisture, and keep the bottle tightly closed. Do not remove desiccant.
Other brands listed are the registered trademarks of their respective owners and are not trademarks of Macleods Pharmaceuticals Limited.
Rx only
Manufactured for:
Macleods Pharma USA, Inc.
Plainsboro, NJ08536
Manufactured by:
Macleods Pharmaceuticals Ltd.
Daman, (U.T.), INDIA
Patient Information
Efavirenz, Lamivudine and Tenofovir Disoproxil Fumarate Tablets, 400 mg/300 mg/300 mg (EF-a-VIR-enz, la-MIV-ue-deen and ten-OF-oh-vir DYE-soe-PROX-il FUE-ma-rate)
What is the most important information I should know about efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets can cause serious side effects, including:
• Worsening of hepatitis B virus (HBV) infection. Your healthcare provider will test you for HBV before starting efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. If you have HBV infection and take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, your HBV may get worse (flare-up) if you stop taking efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. A “flare-up” is when your HBV infection suddenly returns in a worse way than before.
o Do not run out of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Refill your prescription or talk to your healthcare provider before your efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is all gone.
o
Do not stop taking efavirenz, lamivudine and tenofovir disoproxil fumarate tablets without first talking with your healthcare provider. If you stop taking efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, your healthcare provider will need to check your health often and do blood tests regularly for several months to check your liver.
•
Changes in the electrical activity of your heart called QT prolongation. QT prolongation can cause irregular heartbeats that can be life-threatening. Tell your healthcare provider if you feel faint, lightheaded, dizzy, or feel your heart beating irregularly or fast during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
•
New or worse kidney problems, including kidney failure. Your healthcare provider will do blood and urine tests to check your kidneys before and during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Tell your healthcare provider if you get signs and symptoms of kidney problems, including bone pain that does not go away or worsening bone pain, pain in your arms, hands, legs or feet, broken (fractured) bones, muscle pain or weakness.
•
Serious mental health problems. Get medical help right away if you get any of the following symptoms:
|
|
|
|
|
|
|
For more information about side effects, see the section
, “What are the possible side effects of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?”
What is efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets is a prescription medicine that is used without other antiviral medicines to treat human immunodeficiency virus-1 (HIV-1) in adults and children who weigh at least 77 pounds (35 kg).
HIV-1 is the virus that causes AIDS (Acquired Immune Deficiency Syndrome).
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets contains the prescription medicines efavirenz, lamivudine and tenofovir disoproxil fumarate.
Do not take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets if you:
•
are allergic to efavirenz, lamivudine, tenofovir disoproxil fumarate, or any of the ingredients in efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. See the end of this Patient Information leaflet for a complete list of ingredients in efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
• are currently taking elbasvir and grazoprevir.
Before you take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, tell your healthcare provider about all of your medical conditions, including if you:
• have liver problems, including hepatitis B or C infection
• have kidney problems, including end-stage renal disease (ESRD) that requires dialysis
• have a history of mental health problems
• have a history of drug or alcohol abuse
• have a heart problem, including QT prolongation
• have bone problems, including a history of bone fractures
• have a history of seizures
• are pregnant or plan to become pregnant. Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets may harm your unborn baby.
o You should not become pregnant during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
o Females who are able to become pregnant should use effective birth control (contraception) during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets and for 12 weeks after stopping treatment. A barrier form of birth control should always be used along with another type of birth control.
o Your healthcare provider should do a pregnancy test before you start efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
Pregnancy Registry. There is a pregnancy registry for women who take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets during pregnancy. The purpose of this registry is to collect information about the health of you and your baby. Talk to your healthcare provider about how you can take part in this registry.
• are breastfeeding or plan to breastfeed. Do not breastfeed if you take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
o You should not breastfeed if you have HIV-1 because of the risk of passing HIV-1 to your baby.
o Talk to your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements.
Some medicines interact with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets may affect the way other medicines work, and other medicines may affect how efavirenz, lamivudine and tenofovir disoproxil fumarate tablets works. Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.
• You can ask your healthcare provider or pharmacist for a list of medicines that interact with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
• Do not start taking a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets with other medicines.
How should I take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?
• Take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets exactly as your healthcare provider tells you to take it.
• Take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets 1 time each day, preferably at bedtime. Taking efavirenz, lamivudine and tenofovir disoproxil fumarate tablets at bedtime might help to make some of the side effects less bothersome.
• Take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets on an empty stomach.
•
Do not miss a dose of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. If you miss a dose, take the missed dose as soon as you remember. Do not double your dose or take more tablets than prescribed by your healthcare provider.
• Stay under the care of your healthcare provider during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
• Do not run out of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. The virus in your blood may increase and the virus may become harder to treat. When your supply starts to run low, get more from your healthcare provider or pharmacy.
• If you take too much efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, go to the nearest hospital emergency room right away
What should I avoid while taking efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?
You should avoid taking medicines that contain sorbitol during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
What are the possible side effects of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?
Efavirenz, lamivudine and tenofovir disoproxil fumarate tablets may cause serious side effects, including:
- See “What is the most important information I should know about efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?”
-
Nervous system problems are common in people who take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, but can be severe. These symptoms usually begin during the first or second day of treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets and usually go away after 2 to 4 weeks of treatment. These symptoms may become worse if you drink alcohol or take a medicine for mental health problems. Symptoms may include:
- dizziness
- trouble concentrating
- trouble sleeping
- drowsiness
- unusual dreams
- headache
- seeing or hearing things that are not real (hallucinations)
If you get symptoms of nervous system problems during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets, you should avoid driving, operating machinery, or doing anything that needs you to be alert.
• Skin reactions and allergic reactions. Skin reactions or rash can happen and can sometimes be severe. Skin rash usually goes away without any change in treatment. If you develop a rash or a rash with any of the following symptoms, call your healthcare provider right away:
|
|
- Severe liver problems. In some cases, severe liver problems can lead to death. Your liver may become large (hepatomegaly) and you may develop fat in your liver (steatosis). Inflammation of your liver (hepatitis) that can lead to liver failure requiring a liver transplant has been reported in some people treated with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Your healthcare provider may do blood tests to check your liver before and during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
Call your healthcare provider right away if you get any of the following signs or symptoms of liver problems:
|
|
|
|
|
|
- Use with interferon and ribavirin-based regimens. Worsening of liver disease that has caused death has happened in people infected with HIV-1 and hepatitis C virus who were taking antiretroviral medicines for HIV-1 and were also being treated for hepatitis C with interferon alfa with or without ribavirin. If you are taking efavirenz, lamivudine and tenofovir disoproxil fumarate tablets and interferon alfa with or without ribavirin, tell your healthcare provider if you have any new symptoms.
-
Risk of inflammation of the pancreas (pancreatitis). Children may be at risk for developing pancreatitis during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets if they:
- have taken nucleoside analogue medicines in the past
- have a history of pancreatitis
- have other risk factors for pancreatitis
Call your healthcare provider right away if your child develops signs and symptoms of pancreatitis including severe upper stomach-area pain, with or without nausea and vomiting. Your healthcare provider may tell you to stop giving efavirenz, lamivudine and tenofovir disoproxil fumarate tablets to your child if their symptoms and blood test results show that your child may have pancreatitis.
- Seizures. Seizures are more likely to happen if you have had seizures in the past.
- Increases in blood fat levels (cholesterol and triglycerides). Your healthcare provider will check your blood fat levels before and during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
- Bone problems can happen in some people who take efavirenz, lamivudine and tenofovir disoproxil fumarate tablets. Bone problems include bone pain, softening or thinning (which may lead to fractures). Your healthcare provider may need to do tests to check your bones. Tell your healthcare provider if you have any bone pain, pain in your hands or feet, or muscle pain or weakness during treatment with efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
- Changes in your immune system (Immune Reconstitution Syndrome) can happen when you start taking HIV-1 medicines. Your immune system may get stronger and begin to fight infections that have been hidden in your body for a long time. Tell your healthcare provider if you start having new symptoms after starting your HIV-1 medicine.
- Too much lactic acid in your blood (lactic acidosis). Lactic acidosis is a serious medical emergency that can lead to death.
Tell your healthcare provider right away if you get any of the following symptoms that could be signs of lactic acidosis:
|
|
|
|
|
|
|
|
The most common side effects of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets are rash and dizziness.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?
- Store efavirenz, lamivudine and tenofovir disoproxil fumarate tablets tablets below 86°F (30°C).
- Keep efavirenz, lamivudine and tenofovir disoproxil fumarate tablets tablets in the original container.
- Keep the bottle tightly closed. The bottle contains a desiccant that helps to keep the tablets dry. Do not remove desiccant.
Keep efavirenz, lamivudine and tenofovir disoproxil fumarate tablets and all medicines out of the reach of children.
General information about the safe and effective use of efavirenz, lamivudine and tenofovir disoproxil fumarate tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use efavirenz, lamivudine and tenofovir disoproxil fumarate tablets for a condition for which it was not prescribed. Do not give efavirenz, lamivudine and tenofovir disoproxil fumarate tablets to other people, even if they have the same symptoms that you have. It may harm them. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about efavirenz, lamivudine and tenofovir disoproxil fumarate tablets that is written for health professionals.
What are the ingredients in efavirenz, lamivudine and tenofovir disoproxil fumarate tablets?
Active ingredient: efavirenz, lamivudine, and tenofovir disoproxil fumarate
Inactive ingredients: croscarmellose sodium, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate, microcrystalline cellulose, pregelatinized starch, poloxamer, and sodium lauryl sulphate. The tablets are coated with ferric oxide red, hydroxypropyl methylcellulose, lactose monohydrate, titanium dioxide, and triacetin.
Manufactured for:
Macleods Pharma USA, Inc., Plainsboro, NJ 08536
Manufactured by:
Macleods Pharmaceuticals Ltd., Daman, (U.T.), INDIA
For more information, call Macleods Pharma USA, Inc. at 1-888-943-3210.
This Patient Information has been approved by the U.S. Food and Drug Administration.
Issued: 03/2019
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
Efavirenz, Lamivudine and Tenofovir disoproxil fumarate Tablets 400 mg/300 mg/300 mg
30's count
NDC-33342-362-07
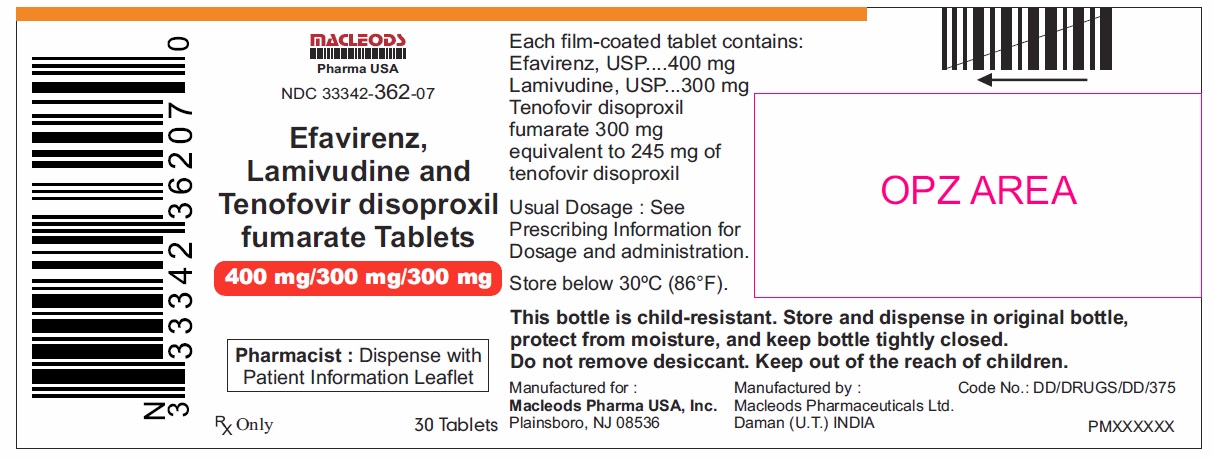
Efavirenz, Lamivudine and Tenofovir disoproxil fumarate Tablets 400 mg/300 mg/300 mg
90's count
NDC-33342-362-10
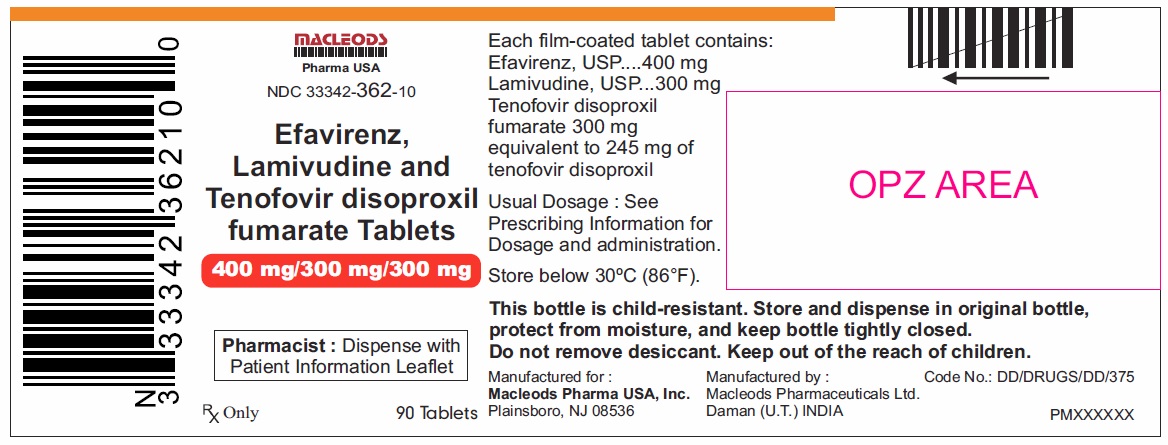
Efavirenz, Lamivudine and Tenofovir disoproxil fumarate Tablets 400 mg/300 mg/300 mg
180's count
NDC-33342-362-57
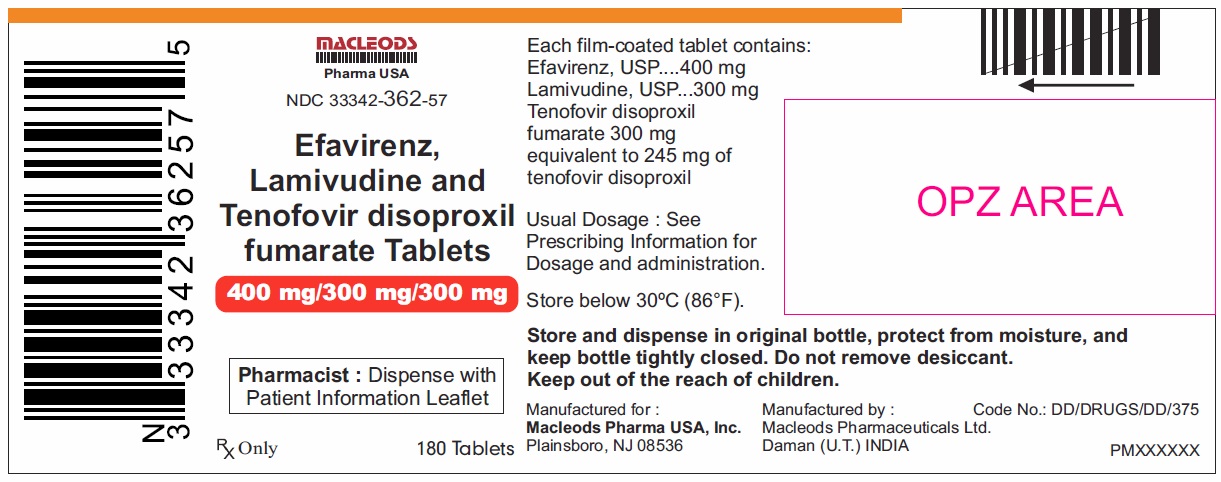
| EFAVIRENZ, LAMIVUDINE AND TENOFOVIR DISOPROXIL FUMARATE
efavirenz, lamivudine and tenofovir disoproxil fumarate tablet |
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||
| Labeler - Macleods Pharmaceuticals Limited (862128535) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Macleods Pharmaceuticals Limited | 918608365 | analysis(33342-362) , label(33342-362) , manufacture(33342-362) , pack(33342-362) | |