ABILIFY- aripiprazole tablet
REMEDYREPACK INC.
----------
These highlights do not include all the information needed to use ABILIFY safely and effectively. See full prescribing information for ABILIFY.ABILIFY® (aripiprazole) TabletsABILIFY DISCMELT® (aripiprazole) Orally Disintegrating TabletsABILIFY® (aripiprazole) Oral SolutionABILIFY® (aripiprazole) Injection FOR INTRAMUSCULAR USE ONLY Initial U.S. Approval: 2002
BOXED WARNING
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. ABILIFY (aripiprazole) is not approved for the treatment of patients with dementia-related psychosis [see WARNINGS AND PRECAUTIONS (5.1)] .
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of adjunctive ABILIFY or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. ABILIFY is not approved for use in pediatric patients with depression [see WARNINGS AND PRECAUTIONS (5.2)] .
INDICATIONS & USAGE
ABILIFY is an atypical antipsychotic indicated
as oral formulations for the:
Treatment of schizophrenia (1.1)
- Adults: Efficacy was established in four 4-6 week trials and one maintenance trial in patients with schizophrenia (14.1)
- Adolescents (ages 13-17): Efficacy was established in one 6-week trial in patients with schizophrenia (14.1)
Acute treatment of manic or mixed episodes associated with bipolar I disorder as monotherapy and as an adjunct to lithium or valproate (1.2)
- Adults: Efficacy was established in four 3-week monotherapy trials and one 6-week adjunctive trial in patients with manic or mixed episodes (14.2)
- Pediatric Patients (ages 10-17): Efficacy was established in one 4-week monotherapy trial in patients with manic or mixed episodes (14.2)
Maintenance treatment of bipolar I disorder, both as monotherapy and as an adjunct to lithium or valproate (1.2)
- Adults: Efficacy was established in one maintenance monotherapy trial and in one maintenance adjunctive trial (14.2)
Adjunctive treatment of major depressive disorder (MDD) (1.3)
- Adults: Efficacy was established in two 6-week trials in patients with MDD who had an inadequate response to antidepressant therapy during the current episode (14.3)
Treatment of irritability associated with autistic disorder (1.4)
- Pediatric Patients (ages 6-17 years): Efficacy was established in two 8-week trials in patients with autistic disorder (14.4)
as an injection for the:
Acute treatment of agitation associated with schizophrenia or bipolar I disorder (1.5)
- Adults: Efficacy was established in three 24-hour trials in agitated patients with schizophrenia or manic/mixed episodes of bipolar I disorder (14.5)
ABILIFY is indicated for the treatment of schizophrenia. The efficacy of ABILIFY was established in four 4-6 week trials in adults and one 6-week trial in adolescents (13 to 17 years). Maintenance efficacy was demonstrated in one trial in adults and can be extrapolated to adolescents [see CLINICAL STUDIES (14.1)] .
Acute Treatment of Manic and Mixed Episodes
ABILIFY is indicated for the acute treatment of manic and mixed episodes associated with bipolar I disorder, both as monotherapy and as an adjunct to lithium or valproate. Efficacy as monotherapy was established in four 3-week monotherapy trials in adults and one 4-week monotherapy trial in pediatric patients (10 to 17 years). Efficacy as adjunctive therapy was established in one 6-week adjunctive trial in adults [see CLINICAL STUDIES (14.2)] .
Maintenance Treatment of Bipolar I Disorder
ABILIFY is indicated for the maintenance treatment of bipolar I disorder, both as monotherapy and as an adjunct to either lithium or valproate. Maintenance efficacy was demonstrated in one monotherapy maintenance trial and in one adjunctive maintenance trial in adults [see CLINICAL STUDIES (14.2)] .
ABILIFY is indicated for use as an adjunctive therapy to antidepressants for the treatment of major depressive disorder (MDD). Efficacy was established in two 6-week trials in adults with MDD who had an inadequate response to antidepressant therapy during the current episode [see CLINICAL STUDIES (14.3)] .
ABILIFY is indicated for the treatment of irritability associated with autistic disorder. Efficacy was established in two 8-week trials in pediatric patients (aged 6 to 17 years) with irritability associated with autistic disorder (including symptoms of aggression towards others, deliberate self-injuriousness, temper tantrums, and quickly changing moods) [see CLINICAL STUDIES (14.4)] .
ABILIFY Injection is indicated for the acute treatment of agitation associated with schizophrenia or bipolar disorder, manic or mixed. “Psychomotor agitation” is defined in DSM-IV as “excessive motor activity associated with a feeling of inner tension.” Patients experiencing agitation often manifest behaviors that interfere with their diagnosis and care (eg, threatening behaviors, escalating or urgently distressing behavior, or self-exhausting behavior), leading clinicians to the use of intramuscular antipsychotic medications to achieve immediate control of the agitation. Efficacy was established in three short-term (24-hour) trials in adults [see CLINICAL STUDIES (14.5)] .
Psychiatric disorders in children and adolescents are often serious mental disorders with variable symptom profiles that are not always congruent with adult diagnostic criteria. It is recommended that psychotropic medication therapy for pediatric patients only be initiated after a thorough diagnostic evaluation has been conducted and careful consideration given to the risks associated with medication treatment. Medication treatment for pediatric patients with schizophrenia, bipolar I disorder, and irritability associated with autistic disorder is indicated as part of a total treatment program that often includes psychological, educational, and social interventions.
DOSAGE & ADMINISTRATION
| Initial
Dose | Recommended
Dose | Maximum
Dose |
|
| Schizophrenia – adults (2.1) | 10-15 mg/day | 10-15 mg/day | 30 mg/day |
| Schizophrenia – adolescents (2.1) | 2 mg/day | 10 mg/day | 30 mg/day |
| Bipolar mania – adults: monotherapy (2.2) | 15 mg/day | 15 mg/day | 30 mg/day |
| Bipolar mania – adults: adjunct to lithium or valproate (2.2) | 10-15 mg/day | 15 mg/day | 30 mg/day |
| Bipolar mania – pediatric patients: monotherapy or as an adjunct to lithium or valproate (2.2) | 2 mg/day | 10 mg/day | 30 mg/day |
| As an adjunct to antidepressants for the treatment of major depressive disorder – adults (2.3) | 2-5 mg/day | 5-10 mg/day | 15 mg/day |
| Irritability associated with autistic disorder – pediatric patients (2.4) | 2 mg/day | 5-10 mg/day | 15 mg/day |
| Agitation associated with schizophrenia or bipolar mania – adults (2.5) | 9.75 mg/1.3 mL
injected IM | 30 mg/day
injected IM |
- Oral formulations: Administer once daily without regard to meals (2)
- IM injection: Wait at least 2 hours between doses. Maximum daily dose 30 mg (2.5)
Adults
Dose Selection: The recommended starting and target dose for ABILIFY is 10 mg/day or 15 mg/day administered on a once-a-day schedule without regard to meals. ABILIFY has been systematically evaluated and shown to be effective in a dose range of 10 mg/day to 30 mg/day, when administered as the tablet formulation; however, doses higher than 10 mg/day or 15 mg/day were not more effective than 10 mg/day or 15 mg/day. Dosage increases should generally not be made before 2 weeks, the time needed to achieve steady-state [see CLINICAL STUDIES (14.1)] .
Maintenance Treatment: Maintenance of efficacy in schizophrenia was demonstrated in a trial involving patients with schizophrenia who had been symptomatically stable on other antipsychotic medications for periods of 3 months or longer. These patients were discontinued from those medications and randomized to either ABILIFY 15 mg/day or placebo, and observed for relapse [see CLINICAL STUDIES (14.1)] . Patients should be periodically reassessed to determine the continued need for maintenance treatment.
Adolescents
Dose Selection: The recommended target dose of ABILIFY is 10 mg/day. Aripiprazole was studied in adolescent patients 13 to 17 years of age with schizophrenia at daily doses of 10 mg and 30 mg. The starting daily dose of the tablet formulation in these patients was 2 mg, which was titrated to 5 mg after 2 days and to the target dose of 10 mg after 2 additional days. Subsequent dose increases should be administered in 5 mg increments. The 30 mg/day dose was not shown to be more efficacious than the 10 mg/day dose. ABILIFY can be administered without regard to meals [see CLINICAL STUDIES (14.1)] .
Maintenance Treatment: The efficacy of ABILIFY for the maintenance treatment of schizophrenia in the adolescent population has not been evaluated. While there is no body of evidence available to answer the question of how long the adolescent patient treated with ABILIFY should be maintained on the drug, maintenance efficacy can be extrapolated from adult data along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients. Thus, it is generally recommended that responding patients be continued beyond the acute response, but at the lowest dose needed to maintain remission. Patients should be periodically reassessed to determine the need for maintenance treatment.
Switching from Other Antipsychotics
There are no systematically collected data to specifically address switching patients with schizophrenia from other antipsychotics to ABILIFY or concerning concomitant administration with other antipsychotics. While immediate discontinuation of the previous antipsychotic treatment may be acceptable for some patients with schizophrenia, more gradual discontinuation may be most appropriate for others. In all cases, the period of overlapping antipsychotic administration should be minimized.
Acute Treatment of Manic and Mixed Episodes
Adults: The recommended starting dose in adults is 15 mg given once daily as monotherapy and 10 mg to 15 mg given once daily as adjunctive therapy with lithium or valproate. ABILIFY can be given without regard to meals. The recommended target dose of ABILIFY is 15 mg/day, as monotherapy or as adjunctive therapy with lithium or valproate. The dose may be increased to 30 mg/day based on clinical response. The safety of doses above 30 mg/day has not been evaluated in clinical trials.
Pediatrics: The recommended starting dose in pediatric patients (10 to 17 years) as monotherapy is 2 mg/day, with titration to 5 mg/day after 2 days, and a target dose of 10 mg/day after 2 additional days. Recommended dosing as adjunctive therapy to lithium or valproate is the same. Subsequent dose increases, if needed, should be administered in 5 mg/day increments. ABILIFY can be given without regard to meals [see CLINICAL STUDIES (14.2)] .
Maintenance Treatment
The recommended dose for maintenance treatment, whether as monotherapy or as adjunctive therapy, is the same dose needed to stabilize patients during acute treatment, both for adult and pediatric patients. Patients should be periodically reassessed to determine the continued need for maintenance treatment [see CLINICAL STUDIES (14.2)].
Adults
Dose Selection: The recommended starting dose for ABILIFY as adjunctive treatment for patients already taking an antidepressant is 2 mg/day to 5 mg/day. The efficacy of ABILIFY as an adjunctive therapy for major depressive disorder was established within a dose range of 2 mg/day to 15 mg/day. Dose adjustments of up to 5 mg/day should occur gradually, at intervals of no less than 1 week [see CLINICAL STUDIES (14.3)] .
Maintenance Treatment: The efficacy of ABILIFY for the adjunctive maintenance treatment of major depressive disorder has not been evaluated. While there is no body of evidence available to answer the question of how long the patient treated with ABILIFY should be maintained, patients should be periodically reassessed to determine the continued need for maintenance treatment.
Pediatric Patients
Dose Selection: The efficacy of aripiprazole has been established in the treatment of pediatric patients 6 to 17 years of age with irritability associated with autistic disorder at doses of 5 mg/day to 15 mg/day. The dosage of ABILIFY should be individualized according to tolerability and response.
Dosing should be initiated at 2 mg/day. The dose should be increased to 5 mg/day, with subsequent increases to 10 mg/day or 15 mg/day if needed. Dose adjustments of up to 5 mg/day should occur gradually, at intervals of no less than 1 week [see CLINICAL STUDIES (14.4)] .
Maintenance Treatment: The efficacy of ABILIFY for the maintenance treatment of irritability associated with autistic disorder has not been evaluated. While there is no body of evidence available to answer the question of how long the patient treated with ABILIFY should be maintained, patients should be periodically reassessed to determine the continued need for maintenance treatment.
Adults
Dose Selection: The recommended dose in these patients is 9.75 mg. The effectiveness of aripiprazole injection in controlling agitation in schizophrenia and bipolar mania was demonstrated over a dose range of 5.25 mg to 15 mg. No additional benefit was demonstrated for 15 mg compared to 9.75 mg. A lower dose of 5.25 mg may be considered when clinical factors warrant. If agitation warranting a second dose persists following the initial dose, cumulative doses up to a total of 30 mg/day may be given. However, the efficacy of repeated doses of aripiprazole injection in agitated patients has not been systematically evaluated in controlled clinical trials. The safety of total daily doses greater than 30 mg or injections given more frequently than every 2 hours have not been adequately evaluated in clinical trials [see CLINICAL STUDIES (14.5)] .
If ongoing aripiprazole therapy is clinically indicated, oral aripiprazole in a range of 10 mg/day to 30 mg/day should replace aripiprazole injection as soon as possible [see DOSAGE AND ADMINISTRATION (2.1 and 2.2)] .
Administration of ABILIFY Injection
To administer ABILIFY Injection, draw up the required volume of solution into the syringe as shown in Table 1. Discard any unused portion.
| Single-Dose | Required Volume of Solution |
|---|---|
| 5.25 mg | 0.7 mL |
| 9.75 mg | 1.3 mL |
| 15 mg | 2 mL |
ABILIFY Injection is intended for intramuscular use only. Do not administer intravenously or subcutaneously. Inject slowly, deep into the muscle mass.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Dosage adjustments in adults are not routinely indicated on the basis of age, gender, race, or renal or hepatic impairment status [see USE IN SPECIFIC POPULATIONS (8.4- 8.10)] .
Dosage adjustment for patients taking aripiprazole concomitantly with strong CYP3A4 inhibitors:
When concomitant administration of aripiprazole with strong CYP3A4 inhibitors such as ketoconazole or clarithromycin is indicated, the aripiprazole dose should be reduced to one-half of the usual dose. When the CYP3A4 inhibitor is withdrawn from the combination therapy, the aripiprazole dose should then be increased
[see DRUG INTERACTIONS (7.1)]
.
Dosage adjustment for patients taking aripiprazole concomitantly with potential CYP2D6 inhibitors:
When concomitant administration of potential CYP2D6 inhibitors such as quinidine, fluoxetine, or paroxetine with aripiprazole occurs, aripiprazole dose should be reduced at least to one-half of its normal dose. When the CYP2D6 inhibitor is withdrawn from the combination therapy, the aripiprazole dose should then be increased
[see DRUG INTERACTIONS (7.1)]
. When adjunctive ABILIFY is administered to patients with major depressive disorder, ABILIFY should be administered without dosage adjustment as specified in
DOSAGE AND ADMINISTRATION (2.3)
.
Dosing recommendation in patients taking aripiprazole concomitantly with strong CYP3A4 and CYP2D6 inhibitors:
When concomitant administration of aripiprazole with strong inhibitors of CYP3A4 (such as ketoconazole or clarithromycin) and CYP2D6 (such as quinidine, fluoxetine, or paroxetine) is indicated, the aripiprazole dose should be reduced to one-quarter (25%) of the usual dose. When the CYP3A4 and/or CYP2D6 inhibitor is withdrawn from the combination therapy, the aripiprazole dose should be increased
[see DRUG INTERACTIONS
(7.1)].
Dosing recommendation in patients taking aripiprazole concomitantly with strong, moderate, or weak inhibitors of CYP3A4 and CYP2D6:
Patients who may be receiving a combination of strong, moderate, and weak inhibitors of CYP3A4 and CYP2D6 (eg, a potent CYP3A4 inhibitor and a moderate CYP2D6 inhibitor or a moderate CYP3A4 inhibitor with a moderate CYP2D6 inhibitor), the dosing may be reduced to one-quarter (25%) of the usual dose initially and then adjusted to achieve a favorable clinical response.
Dosing recommendation in patients who are classified as CYP2D6 poor metabolizers (PM):
The aripiprazole dose in PM patients should initially be reduced to one-half (50%) of the usual dose and then adjusted to achieve a favorable clinical response. The dose of aripiprazole for PM patients who are administered a strong CYP3A4 inhibitor should be reduced to one-quarter (25%) of the usual dose
[see CLINICAL PHARMACOLOGY (12.3)]
.
Dosage adjustment for patients taking potential CYP3A4 inducers:
When a potential CYP3A4 inducer such as carbamazepine is added to aripiprazole therapy, the aripiprazole dose should be doubled. Additional dose increases should be based on clinical evaluation. When the CYP3A4 inducer is withdrawn from the combination therapy, the aripiprazole dose should be reduced to 10 mg to 15 mg
[see DRUG INTERACTIONS (7.1)]
.
The oral solution can be substituted for tablets on a mg-per-mg basis up to the 25 mg dose level. Patients receiving 30 mg tablets should receive 25 mg of the solution [see CLINICAL PHARMACOLOGY (12.3)] .
The dosing for ABILIFY Orally Disintegrating Tablets is the same as for the oral tablets [see DOSAGE AND ADMINISTRATION (2.1, 2.2, 2.3, and 2.4)] .
DOSAGE FORMS & STRENGTHS
ABILIFY ® (aripiprazole) Tablets are available as described in Table 2.
| Tablet
Strength | Tablet
Color/Shape | Tablet
Markings |
| 2 mg | green
modified rectangle | “A-006”
and “2” |
| 5 mg | blue
modified rectangle | “A-007”
and “5” |
| 10 mg | pink
modified rectangle | “A-008”
and “10” |
| 15 mg | yellow
round | “A-009”
and “15” |
| 20 mg | white
round | “A-010”
and “20” |
| 30 mg | pink
round | “A-011”
and “30” |
ABILIFY DISCMELT ® (aripiprazole) Orally Disintegrating Tablets are available as described in Table 3.
| Tablet
Strength | Tablet
Color/Shape | Tablet
Markings |
| 10 mg | pink (with scattered specks)
round | “A” and “640”
“10” |
| 15 mg | yellow (with scattered specks)
round | “A” and “641”
“15” |
ABILIFY ® (aripiprazole) Oral Solution (1 mg/mL) is a clear, colorless to light-yellow solution, supplied in child-resistant bottles along with a calibrated oral dosing cup.
ABILIFY ® (aripiprazole) Injection for Intramuscular Use is a clear, colorless solution available as a ready-to-use, 9.75 mg/1.3 mL (7.5 mg/mL) solution in clear, Type 1 glass vials.
CONTRAINDICATIONS
Known hypersensitivity reaction to ABILIFY. Reactions have ranged from pruritus/urticaria to anaphylaxis [see ADVERSE REACTIONS (6.3)] .
WARNINGS AND PRECAUTIONS
- Elderly Patients with Dementia-Related Psychosis: Increased incidence of cerebrovascular adverse events (eg, stroke, transient ischemic attack, including fatalities) (5.1)
- Suicidality and Antidepressants: Increased risk of suicidality in children, adolescents, and young adults with major depressive disorder (5.2)
- Neuroleptic Malignant Syndrome: Manage with immediate discontinuation and close monitoring (5.3)
- Tardive Dyskinesia: Discontinue if clinically appropriate (5.4)
-
Metabolic Changes: Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and body weight gain
(5.5)
- Hyperglycemia/Diabetes Mellitus: Monitor glucose regularly in patients with and at risk for diabetes (5.5)
- Dyslipidemia: Undesirable alterations in lipid levels have been observed in patients treated with atypical antipsychotics (5.5)
- Weight Gain: Weight gain has been observed with atypical antipsychotic use. Monitor weight (5.5)
- Orthostatic Hypotension: Use with caution in patients with known cardiovascular or cerebrovascular disease (5.6)
- Leukopenia, Neutropenia, and Agranulocytosis: have been reported with antipsychotics including ABILIFY. Patients with a history of a clinically significant low white blood cell count (WBC) or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of ABILIFY should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors (5.7)
- Seizures/Convulsions: Use cautiously in patients with a history of seizures or with conditions that lower the seizure threshold (5.8)
- Potential for Cognitive and Motor Impairment: Use caution when operating machinery (5.9)
- Suicide: The possibility of a suicide attempt is inherent in schizophrenia and bipolar disorder. Closely supervise high-risk patients (5.11)
Increased Mortality
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. ABILIFY (aripiprazole) is not approved for the treatment of patients with dementia-related psychosis [see BOXED WARNING] .
Cerebrovascular Adverse Events, Including Stroke
In placebo-controlled clinical studies (two flexible dose and one fixed dose study) of dementia-related psychosis, there was an increased incidence of cerebrovascular adverse events (eg, stroke, transient ischemic attack), including fatalities, in aripiprazole-treated patients (mean age: 84 years; range: 78-88 years). In the fixed-dose study, there was a statistically significant dose response relationship for cerebrovascular adverse events in patients treated with aripiprazole. Aripiprazole is not approved for the treatment of patients with dementia-related psychosis [see also BOXED WARNING] .
Safety Experience in Elderly Patients with Psychosis Associated with Alzheimer’s Disease
In three, 10-week, placebo-controlled studies of aripiprazole in elderly patients with psychosis associated with Alzheimer’s disease (n=938; mean age: 82.4 years; range: 56-99 years), the treatment-emergent adverse events that were reported at an incidence of ≥3% and aripiprazole incidence at least twice that for placebo were lethargy [placebo 2%, aripiprazole 5%], somnolence (including sedation) [placebo 3%, aripiprazole 8%], and incontinence (primarily, urinary incontinence) [placebo 1%, aripiprazole 5%], excessive salivation [placebo 0%, aripiprazole 4%], and lightheadedness [placebo 1%, aripiprazole 4%].
The safety and efficacy of ABILIFY in the treatment of patients with psychosis associated with dementia have not been established. If the prescriber elects to treat such patients with ABILIFY, vigilance should be exercised, particularly for the emergence of difficulty swallowing or excessive somnolence, which could predispose to accidental injury or aspiration [see also BOXED WARNING] .
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term, placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with MDD and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, Obsessive Compulsive Disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 4.
| Age Range | Drug-Placebo Difference in Number of
Cases of Suicidality per 1000 Patients Treated |
| Increases Compared to Placebo | |
| <18 | 14 additional cases |
| 18-24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25-64 | 1 fewer case |
| ≥65 | 6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, ie, beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for MDD as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient’s presenting symptoms.
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to healthcare providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for ABILIFY should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder: A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression.
It should be noted that ABILIFY is not approved for use in treating depression in the pediatric population.
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) may occur with administration of antipsychotic drugs, including aripiprazole. Rare cases of NMS occurred during aripiprazole treatment in the worldwide clinical database. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to exclude cases where the clinical presentation includes both serious medical illness (eg, pneumonia, systemic infection) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system pathology.
The management of NMS should include: 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy; 2) intensive symptomatic treatment and medical monitoring; and 3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing tardive dyskinesia and the likelihood that it will become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase. However, the syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses.
There is no known treatment for established cases of tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment, itself, however, may suppress (or partially suppress) the signs and symptoms of the syndrome and, thereby, may possibly mask the underlying process. The effect that symptomatic suppression has upon the long-term course of the syndrome is unknown.
Given these considerations, ABILIFY should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that (1) is known to respond to antipsychotic drugs and (2) for whom alternative, equally effective, but potentially less harmful treatments are not available or appropriate. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on ABILIFY, drug discontinuation should be considered. However, some patients may require treatment with ABILIFY despite the presence of the syndrome.
Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and body weight gain. While all drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
Hyperglycemia/Diabetes Mellitus
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics. There have been reports of hyperglycemia in patients treated with ABILIFY [see ADVERSE REACTIONS (6.2, 6.3)] . Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of treatment-emergent hyperglycemia-related adverse events in patients treated with the atypical antipsychotics. Because ABILIFY was not marketed at the time these studies were performed, it is not known if ABILIFY is associated with this increased risk. Precise risk estimates for hyperglycemia-related adverse events in patients treated with atypical antipsychotics are not available.
Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (eg, obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the suspect drug.
Adults
In an analysis of 13 placebo-controlled monotherapy trials in adults, primarily with schizophrenia or bipolar disorder, the mean change in fasting glucose in aripiprazole-treated patients (+4.4 mg/dL; median exposure 25 days; N=1057) was not significantly different than in placebo-treated patients (+2.5 mg/dL; median exposure 22 days; N=799). Table 5 shows the proportion of aripiprazole-treated patients with normal and borderline fasting glucose at baseline (medium exposure 25 days) that had treatment-emergent high fasting glucose measurements compared to placebo-treated patients (median exposure 22 days).
| Category Change (at least once) from Baseline | Treatment Arm | n/N | % | |
|---|---|---|---|---|
| Fasting Glucose | Normal to High
(<100 mg/dL to ≥126 mg/dL) | Aripiprazole | 31/822 | 3.8 |
| Placebo | 22/605 | 3.6 | ||
| Borderline to High
(≥100 mg/dL and <126 mg/dL to ≥126 mg/dL) | Aripiprazole | 31/176 | 17.6 | |
| Placebo | 13/142 | 9.2 |
At 24 weeks, the mean change in fasting glucose in aripiprazole-treated patients was not significantly different than in placebo-treated patients [+2.2 mg/dL (n=42) and +9.6 mg/dL (n=28), respectively].
The mean change in fasting glucose in adjunctive aripiprazole-treated patients with major depressive disorder (+0.7 mg/dL; median exposure 42 days; N=241) was not significantly different than in placebo-treated patients (+0.8 mg/dL; median exposure 42 days; N=246). Table 6 shows the proportion of adult patients with changes in fasting glucose levels from two placebo-controlled, adjunctive trials (median exposure 42 days) in patients with major depressive disorder.
| Category Change (at least once) from Baseline | Treatment Arm | n/N | % | |
|---|---|---|---|---|
| Fasting Glucose | Normal to High
(<100 mg/dL to ≥126 mg/dL) | Aripiprazole | 2/201 | 1.0 |
| Placebo | 2/204 | 1.0 | ||
| Borderline to High
(≥100 mg/dL and <126 mg/dL to ≥126 mg/dL) | Aripiprazole | 4/34 | 11.8 | |
| Placebo | 3/37 | 8.1 |
Pediatric Patients and Adolescents
In an analysis of two placebo-controlled trials in adolescents with schizophrenia (13 to 17 years) and pediatric patients with bipolar disorder (10 to 17 years), the mean change in fasting glucose in aripiprazole-treated patients (+4.8 mg/dL; with a median exposure of 43 days; N=259) was not significantly different than in placebo-treated patients (+1.7 mg/dL; with a median exposure of 42 days; N=123).
In an analysis of two placebo-controlled trials in pediatric and adolescent patients with irritability associated with autistic disorder (6 to 17 years) with median exposure of 56 days, the mean change in fasting glucose in aripiprazole-treated patients (–0.2 mg/dL; N=83) was not significantly different than in placebo-treated patients (–0.6 mg/dL; N=33). Table 7 shows the proportion of patients with changes in fasting glucose levels from the pooled adolescent schizophrenia and pediatric bipolar patients (median exposure of 42-43 days) as well as from two placebo-controlled trials in pediatric patients (6 to 17 years) with irritability associated with autistic disorder (median exposure of 56 days).
| Category Change (at least once) from Baseline | Indication | Treatment Arm | n/N | % |
|---|---|---|---|---|
| Fasting Glucose
Normal to High (<100 mg/dL to ≥126 mg/dL) |
||||
| Pooled Schizophrenia and Bipolar Disorder | Aripiprazole | 2/236 | 0.8 | |
| Placebo | 2/110 | 1.8 | ||
| Irritability Associated with Autistic Disorder | Aripiprazole | 0/73 | 0 | |
| Placebo | 0/32 | 0 | ||
| Fasting Glucose
Borderline to High (≥100 mg/dL and <126 mg/dL to ≥126 mg/dL) |
||||
| Pooled Schizophrenia and Bipolar Disorder | Aripiprazole | 1/22 | 4.5 | |
| Placebo | 0/12 | 0 | ||
| Irritabiity Associated with Autistic Disorder | Aripiprazole | 0/9 | 0 | |
| Placebo | 0/1 | 0 |
At 12 weeks in the pooled adolescent schizophrenia and pediatric bipolar disorder trials, the mean change in fasting glucose in aripiprazole-treated patients was not significantly different than in placebo-treated patients [+2.4 mg/dL (n=81) and +0.1 mg/dL (n=15), respectively].
Dyslipidemia
Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics.
There were no significant differences between aripiprazole- and placebo-treated patients in the proportion with changes from normal to clinically significant levels for fasting/nonfasting total cholesterol, fasting triglycerides, fasting LDLs, and fasting/nonfasting HDLs. Analyses of patients with at least 12 or 24 weeks of exposure were limited by small numbers of patients.
Adults
Table 8 shows the proportion of adult patients, primarily from pooled schizophrenia and bipolar disorder monotherapy placebo-controlled trials, with changes in total cholesterol (pooled from 17 trials; median exposure 21 to 25 days), fasting triglycerides (pooled from eight trials; median exposure 42 days), fasting LDL cholesterol (pooled from eight trials; median exposure 39 to 45 days, except for placebo-treated patients with baseline normal fasting LDL measurements, who had median treatment exposure of 24 days) and HDL cholesterol (pooled from nine trials; median exposure 40 to 42 days).
| Treatment Arm | n/N | % | |
|---|---|---|---|
| Total Cholesterol
Normal to High (<200 mg/dL to ≥240 mg/dL) |
|||
| Aripiprazole | 34/1357 | 2.5 | |
| Placebo | 27/973 | 2.8 | |
| Fasting Triglycerides
Normal to High (<150 mg/dL to ≥200 mg/dL) |
|||
| Aripiprazole | 40/539 | 7.4 | |
| Placebo | 30/431 | 7.0 | |
| Fasting LDL Cholesterol
Normal to High (<100 mg/dL to ≥160 mg/dL) |
|||
| Aripiprazole | 2/332 | 0.6 | |
| Placebo | 2/268 | 0.7 | |
| HDL Cholesterol
Normal to Low (≥40 mg/dL to <40 mg/dL) |
|||
| Aripiprazole | 121/1066 | 11.4 | |
| Placebo | 99/794 | 12.5 |
In monotherapy trials in adults, the proportion of patients at 12 weeks and 24 weeks with changes from Normal to High in total cholesterol (fasting/nonfasting), fasting triglycerides, and fasting LDL cholesterol were similar between aripiprazole- and placebo-treated patients: at 12 weeks, Total Cholesterol (fasting/nonfasting), 1/71 (1.4%) vs. 3/74 (4.1%); Fasting Triglycerides, 8/62 (12.9%) vs. 5/37 (13.5%); Fasting LDL Cholesterol, 0/34 (0%) vs. 1/25 (4.0%), respectively; and at 24 weeks, Total Cholesterol (fasting/nonfasting), 1/42 (2.4%) vs. 3/37 (8.1%); Fasting Triglycerides, 5/34 (14.7%) vs. 5/20 (25%); Fasting LDL Cholesterol, 0/22 (0%) vs. 1/18 (5.6%), respectively.
Table 9 shows the proportion of patients with changes in total cholesterol (fasting/nonfasting), fasting triglycerides, fasting LDL cholesterol, and HDL cholesterol from two placebo-controlled adjunctive trials in adult patients with major depressive disorder (median exposure 42 days).
| Treatment Arm | n/N | % | |
|---|---|---|---|
| Total Cholesterol
Normal to High (<200 mg/dL to ≥240 mg/dL) |
|||
| Aripiprazole | 3/139 | 2.2 | |
| Placebo | 7/135 | 5.2 | |
| Fasting Triglycerides
Normal to High (<150 mg/dL to ≥200 mg/dL) |
|||
| Aripiprazole | 14/145 | 9.7 | |
| Placebo | 6/147 | 4.1 | |
| Fasting LDL Cholesterol
Normal to High (<100 mg/dL to ≥160 mg/dL) |
|||
| Aripiprazole | 0/54 | 0 | |
| Placebo | 0/73 | 0 | |
| HDL Cholesterol
Normal to Low (≥40 mg/dL to <40 mg/dL) |
|||
| Aripiprazole | 17/318 | 5.3 | |
| Placebo | 10/286 | 3.5 |
Pediatric Patients and Adolescents
Table 10 shows the proportion of adolescents with schizophrenia (13 to 17 years) and pediatric patients with bipolar disorder (10 to 17 years) with changes in total cholesterol and HDL cholesterol (pooled from two placebo-controlled trials; median exposure 42 to 43 days) and fasting triglycerides (pooled from two placebo-controlled trials; median exposure 42 to 44 days).
| Treatment Arm | n/N | % | |
|---|---|---|---|
| Total Cholesterol
Normal to High (<170 mg/dL to ≥200 mg/dL) |
|||
| Aripiprazole | 3/220 | 1.4 | |
| Placebo | 0/116 | 0 | |
| Fasting Triglycerides
Normal to High (<150 mg/dL to ≥200 mg/dL) |
|||
| Aripiprazole | 7/187 | 3.7 | |
| Placebo | 4/85 | 4.7 | |
| HDL Cholesterol
Normal to Low (≥40 mg/dL to <40 mg/dL) |
|||
| Aripiprazole | 27/236 | 11.4 | |
| Placebo | 22/109 | 20.2 |
In monotherapy trials of adolescents with schizophrenia and pediatric patients with bipolar disorder, the proportion of patients at 12 weeks and 24 weeks with changes from Normal to High in total cholesterol (fasting/nonfasting), fasting triglycerides, and fasting LDL cholesterol were similar between aripiprazole- and placebo-treated patients: at 12 weeks, Total Cholesterol (fasting/nonfasting), 0/57 (0%) vs. 0/15 (0%); Fasting Triglycerides, 2/72 (2.8%) vs. 1/14 (7.1%), respectively; and at 24 weeks, Total Cholesterol (fasting/nonfasting), 0/36 (0%) vs. 0/12 (0%); Fasting Triglycerides, 1/47 (2.1%) vs. 1/10 (10.0%), respectively.
Table 11 shows the proportion of patients with changes in total cholesterol (fasting/nonfasting) and fasting triglycerides (median exposure 56 days) and HDL cholesterol (median exposure 55 to 56 days) from two placebo-controlled trials in pediatric patients (6 to 17 years) with irritability associated with autistic disorder.
| Treatment Arm | n/N | % | |
|---|---|---|---|
| Total Cholesterol
Normal to High (<170 mg/dL to ≥200 mg/dL) |
|||
| Aripiprazole | 1/95 | 1.1 | |
| Placebo | 0/34 | 0 | |
| Fasting Triglycerides
Normal to High (<150 mg/dL to ≥200 mg/dL) |
|||
| Aripiprazole | 0/75 | 0 | |
| Placebo | 0/30 | 0 | |
| HDL Cholesterol
Normal to Low (≥40 mg/dL to <40 mg/dL) |
|||
| Aripiprazole | 9/107 | 8.4 | |
| Placebo | 5/49 | 10.2 |
Weight Gain
Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
Adults
In an analysis of 13 placebo-controlled monotherapy trials, primarily from pooled schizophrenia and bipolar disorder, with a median exposure of 21 to 25 days, the mean change in body weight in aripiprazole-treated patients was +0.3 kg (N=1673) compared to –0.1 kg (N=1100) in placebo-controlled patients. At 24 weeks, the mean change from baseline in body weight in aripiprazole-treated patients was –1.5 kg (n=73) compared to –0.2 kg (n=46) in placebo-treated patients.
In the trials adding aripiprazole to antidepressants, patients first received 8 weeks of antidepressant treatment followed by 6 weeks of adjunctive aripiprazole or placebo in addition to their ongoing antidepressant treatment. The mean change in body weight in patients receiving adjunctive aripiprazole was +1.7 kg (N=347) compared to +0.4 kg (N=330) in patients receiving adjunctive placebo.
Table 12 shows the percentage of adult patients with weight gain ≥7% of body weight by indication.
| Indication | Treatment
Arm | N | Patients
n (%) |
|
|---|---|---|---|---|
| Weight gain ≥7% of body weight | ||||
| Schizophrenia a | Aripiprazole | 852 | 69 (8.1) | |
| Placebo | 379 | 12 (3.2) | ||
| Bipolar Mania b | Aripiprazole | 719 | 16 (2.2) | |
| Placebo | 598 | 16 (2.7) | ||
| Major Depressive Disorder (Adjunctive Therapy) c | Aripiprazole | 347 | 18 (5.2) | |
| Placebo | 330 | 2 (0.6) |
Pediatric Patients and Adolescents
In an analysis of two placebo-controlled trials in adolescents with schizophrenia (13 to 17 years) and pediatric patients with bipolar disorder (10 to 17 years) with median exposure of 42 to 43 days, the mean change in body weight in aripiprazole-treated patients was +1.6 kg (N=381) compared to +0.3 kg (N=187) in placebo-treated patients. At 24 weeks, the mean change from baseline in body weight in aripiprazole-treated patients was +5.8 kg (n=62) compared to +1.4 kg (n=13) in placebo-treated patients.
In two short-term, placebo-controlled trials in patients (6 to 17 years) with irritability associated with autistic disorder with median exposure of 56 days, the mean change in body weight in aripiprazole-treated patients was +1.6 kg (n=209) compared to +0.4 kg (n=98) in placebo-treated patients.
Table 13 shows the percentage of pediatric and adolescent patients with weight gain ≥7% of body weight by indication.
| Indication | Treatment
Arm | N | Patients
n (%) |
|
|---|---|---|---|---|
| Weight gain ≥7%
of body weight |
||||
| Pooled Schizophrenia
and Bipolar Mania a | Aripiprazole | 381 | 20 (5.2) | |
| Placebo | 187 | 3 (1.6) | ||
| Irritability Associated
with Autistic Disorder b | Aripiprazole | 209 | 55 (26.3) | |
| Placebo | 98 | 7 (7.1) |
In an open-label trial that enrolled patients from the two placebo-controlled trials of adolescents with schizophrenia (13 to 17 years) and pediatric patients with bipolar disorder (10 to 17 years), 73.2% of patients (238/325) completed 26 weeks of therapy with ABILIFY. After 26 weeks, 32.8% of patients gained ≥7% of their body weight, not adjusted for normal growth. To adjust for normal growth, z-scores were derived (measured in standard deviations [SD]), which normalize for the natural growth of pediatric patients and adolescents by comparisons to age- and gender-matched population standards. A z-score change <0.5 SD is considered not clinically significant. After 26 weeks, the mean change in z-score was 0.09 SD.
In an open-label trial that enrolled patients from two short-term, placebo-controlled trials, patients (6 to 17 years) with irritability associated with autistic disorder, as well as de novo patients, 60.3% (199/330) completed one year of therapy with ABILIFY. The mean change in weight z-score was 0.26 SDs for patients receiving >9 months of treatment.
When treating pediatric patients for any indication, weight gain should be monitored and assessed against that expected for normal growth.
Aripiprazole may cause orthostatic hypotension, perhaps due to its α 1-adrenergic receptor antagonism. The incidence of orthostatic hypotension-associated events from short-term, placebo-controlled trials of adult patients on oral ABILIFY (n=2467) included (aripiprazole incidence, placebo incidence) orthostatic hypotension (1%, 0.3%), postural dizziness (0.5%, 0.3%), and syncope (0.5%, 0.4%); of pediatric patients 6 to 17 years of age (n=611) on oral ABILIFY included orthostatic hypotension (0.5%, 0%), postural dizziness (0.3%, 0%), and syncope (0.2%, 0%); and of patients on ABILIFY Injection (n=501) included orthostatic hypotension (0.6%, 0%), postural dizziness (0.2%, 0.5%), and syncope (0.4%, 0%).
The incidence of a significant orthostatic change in blood pressure (defined as a decrease in systolic blood pressure ≥20 mmHg accompanied by an increase in heart rate ≥25 when comparing standing to supine values) for aripiprazole was not meaningfully different from placebo (aripiprazole incidence, placebo incidence): in adult oral aripiprazole-treated patients (4%, 2%), in pediatric oral aripiprazole-treated patients aged 6 to 17 years (0.2%, 1%), or in aripiprazole injection-treated patients (3%, 2%).
Aripiprazole should be used with caution in patients with known cardiovascular disease (history of myocardial infarction or ischemic heart disease, heart failure, or conduction abnormalities), cerebrovascular disease, or conditions which would predispose patients to hypotension (dehydration, hypovolemia, and treatment with antihypertensive medications).
If parenteral benzodiazepine therapy is deemed necessary in addition to aripiprazole injection treatment, patients should be monitored for excessive sedation and for orthostatic hypotension [see DRUG INTERACTIONS (7.3)] .
Class Effect: In clinical trial and/or postmarketing experience, events of leukopenia/neutropenia have been reported temporally related to antipsychotic agents, including ABILIFY. Agranulocytosis has also been reported.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of ABILIFY should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count <1000/mm 3) should discontinue ABILIFY and have their WBC followed until recovery.
In short-term, placebo-controlled trials, seizures/convulsions occurred in 0.1% (3/2467) of adult patients treated with oral aripiprazole, in 0.2% (1/611) of pediatric patients (6 to 17 years), and in 0.2% (1/501) of adult aripiprazole injection-treated patients.
As with other antipsychotic drugs, aripiprazole should be used cautiously in patients with a history of seizures or with conditions that lower the seizure threshold, eg, Alzheimer’s dementia. Conditions that lower the seizure threshold may be more prevalent in a population of 65 years or older.
ABILIFY, like other antipsychotics, may have the potential to impair judgment, thinking, or motor skills. For example, in short-term, placebo-controlled trials, somnolence (including sedation) was reported as follows (aripiprazole incidence, placebo incidence): in adult patients (n=2467) treated with oral ABILIFY (11%, 6%), in pediatric patients ages 6 to 17 (n=611) (24%, 6%), and in adult patients (n=501) on ABILIFY Injection (9%, 6%). Somnolence (including sedation) led to discontinuation in 0.3% (8/2467) of adult patients and 3% (15/611) of pediatric patients (6 to 17 years) on oral ABILIFY in short-term, placebo-controlled trials, but did not lead to discontinuation of any adult patients on ABILIFY Injection.
Despite the relatively modest increased incidence of these events compared to placebo, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that therapy with ABILIFY does not affect them adversely.
Disruption of the body’s ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing aripiprazole for patients who will be experiencing conditions which may contribute to an elevation in core body temperature, (eg, exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration) [see ADVERSE REACTIONS (6.3)] .
The possibility of a suicide attempt is inherent in psychotic illnesses, bipolar disorder, and major depressive disorder, and close supervision of high-risk patients should accompany drug therapy. Prescriptions for ABILIFY should be written for the smallest quantity consistent with good patient management in order to reduce the risk of overdose [see ADVERSE REACTIONS (6.2, 6.3)] .
In two 6-week, placebo-controlled studies of aripiprazole as adjunctive treatment of major depressive disorder, the incidences of suicidal ideation and suicide attempts were 0% (0/371) for aripiprazole and 0.5% (2/366) for placebo.
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use, including ABILIFY. Aspiration pneumonia is a common cause of morbidity and mortality in elderly patients, in particular those with advanced Alzheimer’s dementia. Aripiprazole and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia [see WARNINGS AND PRECAUTIONS (5.1) and ADVERSE REACTIONS (6.3)] .
Clinical experience with ABILIFY in patients with certain concomitant systemic illnesses is limited [see USE IN SPECIFIC POPULATIONS (8.6, 8.7)] .
ABILIFY has not been evaluated or used to any appreciable extent in patients with a recent history of myocardial infarction or unstable heart disease. Patients with these diagnoses were excluded from premarketing clinical studies [see WARNINGS AND PRECAUTIONS (5.1, 5.6)] .
ADVERSE REACTIONS
Commonly observed adverse reactions (incidence ≥5% and at least twice that for placebo) were (6.2):
- Adult patients with schizophrenia: akathisia
- Pediatric patients (13 to 17 years) with schizophrenia: extrapyramidal disorder, somnolence, and tremor
- Adult patients (monotherapy) with bipolar mania: akathisia, sedation, restlessness, tremor, and extrapyramidal disorder
- Adult patients (adjunctive therapy with lithium or valproate) with bipolar mania: akathisia, insomnia, and extrapyramidal disorder
- Pediatric patients (10 to 17 years) with bipolar mania: somnolence, extrapyramidal disorder, fatigue, nausea, akathisia, blurred vision, salivary hypersecretion, and dizziness
- Adult patients with major depressive disorder (adjunctive treatment to antidepressant therapy): akathisia, restlessness, insomnia, constipation, fatigue, and blurred vision
- Pediatric patients (6 to 17 years) with autistic disorder: sedation, fatigue, vomiting, somnolence, tremor, pyrexia, drooling, decreased appetite, salivary hypersecretion, extrapyramidal disorder, and lethargy
- Adult patients with agitation associated with schizophrenia or bipolar mania: nausea
To report SUSPECTED ADVERSE REACTIONS, contact Bristol-Myers Squibb at 1-800-721-5072 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
The following are discussed in more detail in other sections of the labeling:
- Use in Elderly Patients with Dementia-Related Psychosis [see BOXED WARNING and WARNINGS AND PRECAUTIONS (5.1)]
- Clinical Worsening of Depression and Suicide Risk [see BOXED WARNING and WARNINGS AND PRECAUTIONS (5.2)]
- Neuroleptic Malignant Syndrome (NMS) [see WARNINGS AND PRECAUTIONS (5.3)]
- Tardive Dyskinesia [see WARNINGS AND PRECAUTIONS (5.4)]
- Metabolic Changes [see WARNINGS AND PRECAUTIONS (5.5)]
- Orthostatic Hypotension [see WARNINGS AND PRECAUTIONS (5.6)]
- Leukopenia, Neutropenia, and Agranulocytosis [see WARNINGS AND PRECAUTIONS (5.7)]
- Seizures/Convulsions [see WARNINGS AND PRECAUTIONS (5.8)]
- Potential for Cognitive and Motor Impairment [see WARNINGS AND PRECAUTIONS (5.9)]
- Body Temperature Regulation [see WARNINGS AND PRECAUTIONS (5.10)]
- Suicide [see WARNINGS AND PRECAUTIONS (5.11)]
- Dysphagia [see WARNINGS AND PRECAUTIONS (5.12)]
- Use in Patients with Concomitant Illness [see WARNINGS AND PRECAUTIONS (5.13)]
The most common adverse reactions in adult patients in clinical trials (≥10%) were nausea, vomiting, constipation, headache, dizziness, akathisia, anxiety, insomnia, and restlessness.
The most common adverse reactions in the pediatric clinical trials (≥10%) were somnolence, headache, vomiting, extrapyramidal disorder, fatigue, increased appetite, insomnia, nausea, nasopharyngitis, and weight increased.
Aripiprazole has been evaluated for safety in 13,543 adult patients who participated in multiple-dose, clinical trials in schizophrenia, bipolar disorder, major depressive disorder, Dementia of the Alzheimer’s type, Parkinson’s disease, and alcoholism, and who had approximately 7619 patient-years of exposure to oral aripiprazole and 749 patients with exposure to aripiprazole injection. A total of 3390 patients were treated with oral aripiprazole for at least 180 days and 1933 patients treated with oral aripiprazole had at least 1 year of exposure.
Aripiprazole has been evaluated for safety in 920 patients (6 to 17 years) who participated in multiple-dose, clinical trials in schizophrenia, bipolar mania, or autistic disorder and who had approximately 517 patient-years of exposure to oral aripiprazole. A total of 465 pediatric patients were treated with oral aripiprazole for at least 180 days and 117 pediatric patients treated with oral aripiprazole had at least 1 year of exposure.
The conditions and duration of treatment with aripiprazole (monotherapy and adjunctive therapy with antidepressants or mood stabilizers) included (in overlapping categories) double-blind, comparative and noncomparative open-label studies, inpatient and outpatient studies, fixed- and flexible-dose studies, and short- and longer-term exposure.
Adverse events during exposure were obtained by collecting volunteered adverse events, as well as results of physical examinations, vital signs, weights, laboratory analyses, and ECG. Adverse experiences were recorded by clinical investigators using terminology of their own choosing. In the tables and tabulations that follow, MedDRA dictionary terminology has been used to classify reported adverse events into a smaller number of standardized event categories, in order to provide a meaningful estimate of the proportion of individuals experiencing adverse events.
The stated frequencies of adverse reactions represent the proportion of individuals who experienced at least once, a treatment-emergent adverse event of the type listed. An event was considered treatment emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation. There was no attempt to use investigator causality assessments; ie, all events meeting the defined criteria, regardless of investigator causality, are included.
Throughout this section, adverse reactions are reported. These are adverse events that were considered to be reasonably associated with the use of ABILIFY (adverse drug reactions) based on the comprehensive assessment of the available adverse event information. A causal association for ABILIFY often cannot be reliably established in individual cases.
The figures in the tables and tabulations cannot be used to predict the incidence of side effects in the course of usual medical practice where patient characteristics and other factors differ from those that prevailed in the clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigations involving different treatment, uses, and investigators. The cited figures, however, do provide the prescriber with some basis for estimating the relative contribution of drug and nondrug factors to the adverse reaction incidence in the population studied.
Adult Patients with Schizophrenia
The following findings are based on a pool of five placebo-controlled trials (four 4-week and one 6-week) in which oral aripiprazole was administered in doses ranging from 2 mg/day to 30 mg/day.
Adverse Reactions Associated with Discontinuation of Treatment
Overall, there was little difference in the incidence of discontinuation due to adverse reactions between aripiprazole-treated (7%) and placebo-treated (9%) patients. The types of adverse reactions that led to discontinuation were similar for the aripiprazole-treated and placebo-treated patients.
Commonly Observed Adverse Reactions
The only commonly observed adverse reaction associated with the use of aripiprazole in patients with schizophrenia (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) was akathisia (aripiprazole 8%; placebo 4%).
Adult Patients with Bipolar Mania
Monotherapy
The following findings are based on a pool of 3-week, placebo-controlled, bipolar mania trials in which oral aripiprazole was administered at doses of 15 mg/day or 30 mg/day.
Adverse Reactions Associated with Discontinuation of Treatment
Overall, in patients with bipolar mania, there was little difference in the incidence of discontinuation due to adverse reactions between aripiprazole-treated (11%) and placebo-treated (10%) patients. The types of adverse reactions that led to discontinuation were similar between the aripiprazole-treated and placebo-treated patients.
Commonly Observed Adverse Reactions
Commonly observed adverse reactions associated with the use of aripiprazole in patients with bipolar mania (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) are shown in Table 14.
| Percentage of Patients Reporting Reaction | ||
|---|---|---|
|
Preferred Term | Aripiprazole
(n=917) | Placebo
(n=753) |
| Akathisia | 13 | 4 |
| Sedation | 8 | 3 |
| Restlessness | 6 | 3 |
| Tremor | 6 | 3 |
| Extrapyramidal Disorder | 5 | 2 |
Less Common Adverse Reactions in Adults
Table 15 enumerates the pooled incidence, rounded to the nearest percent, of adverse reactions that occurred during acute therapy (up to 6 weeks in schizophrenia and up to 3 weeks in bipolar mania), including only those reactions that occurred in 2% or more of patients treated with aripiprazole (doses ≥2 mg/day) and for which the incidence in patients treated with aripiprazole was greater than the incidence in patients treated with placebo in the combined dataset.
| Percentage of Patients Reporting Reaction a | ||
|---|---|---|
| System Organ Class
Preferred Term | Aripiprazole
(n=1843) | Placebo
(n=1166) |
| Eye Disorders | ||
| Blurred Vision | 3 | 1 |
| Gastrointestinal Disorders | ||
| Nausea | 15 | 11 |
| Constipation | 11 | 7 |
| Vomiting | 11 | 6 |
| Dyspepsia | 9 | 7 |
| Dry Mouth | 5 | 4 |
| Toothache | 4 | 3 |
| Abdominal Discomfort | 3 | 2 |
| Stomach Discomfort | 3 | 2 |
| General Disorders and Administration Site Conditions | ||
| Fatigue | 6 | 4 |
| Pain | 3 | 2 |
| Musculoskeletal and Connective Tissue Disorders | ||
| Musculoskeletal Stiffness | 4 | 3 |
| Pain in Extremity | 4 | 2 |
| Myalgia | 2 | 1 |
| Muscle Spasms | 2 | 1 |
| Nervous System Disorders | ||
| Headache | 27 | 23 |
| Dizziness | 10 | 7 |
| Akathisia | 10 | 4 |
| Sedation | 7 | 4 |
| Extrapyramidal Disorder | 5 | 3 |
| Tremor | 5 | 3 |
| Somnolence | 5 | 3 |
| Psychiatric Disorders | ||
| Agitation | 19 | 17 |
| Insomnia | 18 | 13 |
| Anxiety | 17 | 13 |
| Restlessness | 5 | 3 |
| Respiratory, Thoracic, and Mediastinal Disorders | ||
| Pharyngolaryngeal Pain | 3 | 2 |
| Cough | 3 | 2 |
An examination of population subgroups did not reveal any clear evidence of differential adverse reaction incidence on the basis of age, gender, or race.
Adult Patients with Adjunctive Therapy with Bipolar Mania
The following findings are based on a placebo-controlled trial of adult patients with bipolar disorder in which aripiprazole was administered at doses of 15 mg/day or 30 mg/day as adjunctive therapy with lithium or valproate.
Adverse Reactions Associated with Discontinuation of Treatment
In a study of patients who were already tolerating either lithium or valproate as monotherapy, discontinuation rates due to adverse reactions were 12% for patients treated with adjunctive aripiprazole compared to 6% for patients treated with adjunctive placebo. The most common adverse drug reactions associated with discontinuation in the adjunctive aripiprazole-treated compared to placebo-treated patients were akathisia (5% and 1%, respectively) and tremor (2% and 1%, respectively).
Commonly Observed Adverse Reactions
The commonly observed adverse reactions associated with adjunctive aripiprazole and lithium or valproate in patients with bipolar mania (incidence of 5% or greater and incidence at least twice that for adjunctive placebo) were: akathisia, insomnia, and extrapyramidal disorder.
Less Common Adverse Reactions in Adult Patients with Adjunctive Therapy in Bipolar Mania
Table 16 enumerates the incidence, rounded to the nearest percent, of adverse reactions that occurred during acute treatment (up to 6 weeks), including only those reactions that occurred in 2% or more of patients treated with adjunctive aripiprazole (doses of 15 mg/day or 30 mg/day) and lithium or valproate and for which the incidence in patients treated with this combination was greater than the incidence in patients treated with placebo plus lithium or valproate.
| Percentage of Patients Reporting Reaction a | ||
|---|---|---|
| System Organ Class
Preferred Term | Aripiprazole +
Li or Val* (n=253) | Placebo +
Li or Val* (n=130) |
| Gastrointestinal Disorders | ||
| Nausea | 8 | 5 |
| Vomiting | 4 | 0 |
| Salivary Hypersecretion | 4 | 2 |
| Dry Mouth | 2 | 1 |
| Infections and Infestations | ||
| Nasopharyngitis | 3 | 2 |
| Investigations | ||
| Weight Increased | 2 | 1 |
| Nervous System Disorders | ||
| Akathisia | 19 | 5 |
| Tremor | 9 | 6 |
| Extrapyramidal Disorder | 5 | 1 |
| Dizziness | 4 | 1 |
| Sedation | 4 | 2 |
| Psychiatric Disorders | ||
| Insomnia | 8 | 4 |
| Anxiety | 4 | 1 |
| Restlessness | 2 | 1 |
Pediatric Patients (13 to 17 years) with Schizophrenia
The following findings are based on one 6-week, placebo-controlled trial in which oral aripiprazole was administered in doses ranging from 2 mg/day to 30 mg/day.
Adverse Reactions Associated with Discontinuation of Treatment
The incidence of discontinuation due to adverse reactions between aripiprazole-treated and placebo-treated pediatric patients (13 to 17 years) was 5% and 2%, respectively.
Commonly Observed Adverse Reactions
Commonly observed adverse reactions associated with the use of aripiprazole in adolescent patients with schizophrenia (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) were extrapyramidal disorder, somnolence, and tremor.
Pediatric Patients (10 to 17 years) with Bipolar Mania
The following findings are based on one 4-week, placebo-controlled trial in which oral aripiprazole was administered in doses of 10 mg/day or 30 mg/day.
Adverse Reactions Associated with Discontinuation of Treatment
The incidence of discontinuation due to adverse reactions between aripiprazole-treated and placebo-treated pediatric patients (10 to 17 years) was 7% and 2%, respectively.
Commonly Observed Adverse Reactions
Commonly observed adverse reactions associated with the use of aripiprazole in pediatric patients with bipolar mania (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) are shown in Table 17.
| Percentage of Patients Reporting Reaction | ||
|---|---|---|
|
Preferred Term | Aripiprazole
(n=197) | Placebo
(n=97) |
| Somnolence | 23 | 3 |
| Extrapyramidal Disorder | 20 | 3 |
| Fatigue | 11 | 4 |
| Nausea | 11 | 4 |
| Akathisia | 10 | 2 |
| Blurred Vision | 8 | 0 |
| Salivary Hypersecretion | 6 | 0 |
| Dizziness | 5 | 1 |
Pediatric Patients (6 to 17 years) with Autistic Disorder
The following findings are based on two 8-week, placebo-controlled trials in which oral aripiprazole was administered in doses of 2 mg/day to 15 mg/day.
Adverse Reactions Associated with Discontinuation of Treatment
The incidence of discontinuation due to adverse reactions between aripiprazole-treated and placebo-treated pediatric patients (6 to 17 years) was 10% and 8%, respectively.
Commonly Observed Adverse Reactions
Commonly observed adverse reactions associated with the use of aripiprazole in pediatric patients with autistic disorder (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) are shown in Table 18.
| Percentage of Patients Reporting Reaction | ||
|---|---|---|
|
Preferred Term | Aripiprazole
(n=212) | Placebo
(n=101) |
| Sedation | 21 | 4 |
| Fatigue | 17 | 2 |
| Vomiting | 14 | 7 |
| Somnolence | 10 | 4 |
| Tremor | 10 | 0 |
| Pyrexia | 9 | 1 |
| Drooling | 9 | 0 |
| Decreased Appetite | 7 | 2 |
| Salivary Hypersecretion | 6 | 1 |
| Extrapyramidal Disorder | 6 | 0 |
| Lethargy | 5 | 0 |
Less Common Adverse Reactions in Pediatric Patients (6 to 17 years) with Schizophrenia, Bipolar Mania, or Autistic Disorder
Table 19 enumerates the pooled incidence, rounded to the nearest percent, of adverse reactions that occurred during acute therapy (up to 6 weeks in schizophrenia, up to 4 weeks in bipolar mania, and up to 8 weeks in autistic disorder), including only those reactions that occurred in 1% or more of pediatric patients treated with aripiprazole (doses ≥2 mg/day) and for which the incidence in patients treated with aripiprazole was greater than the incidence in patients treated with placebo.
| Percentage of Patients Reporting Reaction a | ||
|---|---|---|
| System Organ Class
Preferred Term | Aripiprazole
(n=611) | Placebo
(n=298) |
| Eye Disorders | ||
| Blurred Vision | 3 | 0 |
| Gastrointestinal Disorders | ||
| Vomiting | 9 | 7 |
| Nausea | 8 | 4 |
| Diarrhea | 5 | 3 |
| Salivary Hypersecretion | 4 | 1 |
| Abdominal Pain Upper | 3 | 2 |
| Constipation | 3 | 2 |
| Dry Mouth | 1 | 0 |
| General Disorders and Administration Site Conditions | ||
| Fatigue | 10 | 2 |
| Pyrexia | 5 | 1 |
| Irritability | 1 | 0 |
| Thirst | 1 | 0 |
| Infections and Infestations | ||
| Nasopharyngitis | 6 | 3 |
| Investigations | ||
| Weight Increased | 2 | 1 |
| Metabolism and Nutrition Disorders | ||
| Increased Appetite | 7 | 3 |
| Decreased Appetite | 4 | 2 |
| Musculoskeletal and Connective Tissue Disorders | ||
| Arthralgia | 1 | 0 |
| Musculoskeletal Stiffness | 1 | 0 |
| Nervous System Disorders | ||
| Somnolence | 16 | 4 |
| Extrapyramidal Disorder | 14 | 2 |
| Headache | 13 | 12 |
| Sedation | 8 | 1 |
| Akathisia | 6 | 1 |
| Tremor | 6 | 1 |
| Drooling | 4 | 0 |
| Dizziness | 3 | 1 |
| Lethargy | 2 | 0 |
| Dystonia | 1 | 0 |
| Dyskinesia | 1 | 0 |
| Hypersomnia | 1 | 0 |
| Reproductive System and Breast Disorders | ||
| Dysmenorrhoea* | 2 | 1 |
| Respiratory, Thoracic, and Mediastinal Disorders | ||
| Rhinorrhoea | 2 | 1 |
| Skin and Subcutaneous Tissue Disorders | ||
| Rash | 2 | 1 |
Adult Patients Receiving ABILIFY as Adjunctive Treatment of Major Depressive Disorder
The following findings are based on a pool of two placebo-controlled trials of patients with major depressive disorder in which aripiprazole was administered at doses of 2 mg to 20 mg as adjunctive treatment to continued antidepressant therapy.
Adverse Reactions Associated with Discontinuation of Treatment
The incidence of discontinuation due to adverse reactions was 6% for adjunctive aripiprazole-treated patients and 2% for adjunctive placebo-treated patients.
Commonly Observed Adverse Reactions
The commonly observed adverse reactions associated with the use of adjunctive aripiprazole in patients with major depressive disorder (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo) were: akathisia, restlessness, insomnia, constipation, fatigue, and blurred vision.
Less Common Adverse Reactions in Adult Patients with Major Depressive Disorder
Table 20 enumerates the pooled incidence, rounded to the nearest percent, of adverse reactions that occurred during acute therapy (up to 6 weeks), including only those adverse reactions that occurred in 2% or more of patients treated with adjunctive aripiprazole (doses ≥2 mg/day) and for which the incidence in patients treated with adjunctive aripiprazole was greater than the incidence in patients treated with adjunctive placebo in the combined dataset.
| Percentage of Patients Reporting Reaction a | ||
|---|---|---|
| System Organ Class
Preferred Term | Aripiprazole+ADT*
(n=371) | Placebo+ADT*
(n=366) |
| Eye Disorders | ||
| Blurred Vision | 6 | 1 |
| Gastrointestinal Disorders | ||
| Constipation | 5 | 2 |
| General Disorders and Administration Site Conditions | ||
| Fatigue | 8 | 4 |
| Feeling Jittery | 3 | 1 |
| Infections and Infestations | ||
| Upper Respiratory Tract Infection | 6 | 4 |
| Investigations | ||
| Weight Increased | 3 | 2 |
| Metabolism and Nutrition Disorders | ||
| Increased Appetite | 3 | 2 |
| Musculoskeletal and Connective Tissue Disorders | ||
| Arthralgia | 4 | 3 |
| Myalgia | 3 | 1 |
| Nervous System Disorders | ||
| Akathisia | 25 | 4 |
| Somnolence | 6 | 4 |
| Tremor | 5 | 4 |
| Sedation | 4 | 2 |
| Dizziness | 4 | 2 |
| Disturbance in Attention | 3 | 1 |
| Extrapyramidal Disorder | 2 | 0 |
| Psychiatric Disorders | ||
| Restlessness | 12 | 2 |
| Insomnia | 8 | 2 |
Patients with Agitation Associated with Schizophrenia or Bipolar Mania (Intramuscular Injection)
The following findings are based on a pool of three placebo-controlled trials of patients with agitation associated with schizophrenia or bipolar mania in which aripiprazole injection was administered at doses of 5.25 mg to 15 mg.
Adverse Reactions Associated with Discontinuation of Treatment
Overall, in patients with agitation associated with schizophrenia or bipolar mania, there was little difference in the incidence of discontinuation due to adverse reactions between aripiprazole-treated (0.8%) and placebo-treated (0.5%) patients.
Commonly Observed Adverse Reactions
There was one commonly observed adverse reaction (nausea) associated with the use of aripiprazole injection in patients with agitation associated with schizophrenia and bipolar mania (incidence of 5% or greater and aripiprazole incidence at least twice that for placebo).
Less Common Adverse Reactions in Patients with Agitation Associated with Schizophrenia or Bipolar Mania
Table 21 enumerates the pooled incidence, rounded to the nearest percent, of adverse reactions that occurred during acute therapy (24-hour), including only those adverse reactions that occurred in 2% or more of patients treated with aripiprazole injection (doses ≥5.25 mg/day) and for which the incidence in patients treated with aripiprazole injection was greater than the incidence in patients treated with placebo in the combined dataset.
| Percentage of Patients Reporting Reaction a | ||
|---|---|---|
| System Organ Class
Preferred Term | Aripiprazole
(n=501) | Placebo
(n=220) |
| Cardiac Disorders | ||
| Tachycardia | 2 | <1 |
| Gastrointestinal Disorders | ||
| Nausea | 9 | 3 |
| Vomiting | 3 | 1 |
| General Disorders and Administration Site Conditions | ||
| Fatigue | 2 | 1 |
| Nervous System Disorders | ||
| Headache | 12 | 7 |
| Dizziness | 8 | 5 |
| Somnolence | 7 | 4 |
| Sedation | 3 | 2 |
| Akathisia | 2 | 0 |
Dose-Related Adverse Reactions
Schizophrenia
Dose response relationships for the incidence of treatment-emergent adverse events were evaluated from four trials in adult patients with schizophrenia comparing various fixed doses (2 mg/day, 5 mg/day, 10 mg/day, 15 mg/day, 20 mg/day, and 30 mg/day) of oral aripiprazole to placebo. This analysis, stratified by study, indicated that the only adverse reaction to have a possible dose response relationship, and then most prominent only with 30 mg, was somnolence [including sedation]; (incidences were placebo, 7.1%; 10 mg, 8.5%; 15 mg, 8.7%; 20 mg, 7.5%; 30 mg, 12.6%).
In the study of pediatric patients (13 to 17 years of age) with schizophrenia, three common adverse reactions appeared to have a possible dose response relationship: extrapyramidal disorder (incidences were placebo, 5.0%; 10 mg, 13.0%; 30 mg, 21.6%); somnolence (incidences were placebo, 6.0%; 10 mg, 11.0%; 30 mg, 21.6%); and tremor (incidences were placebo, 2.0%; 10 mg, 2.0%; 30 mg, 11.8%).
Bipolar Mania
In the study of pediatric patients (10 to 17 years of age) with bipolar mania, four common adverse reactions had a possible dose response relationship at 4 weeks; extrapyramidal disorder (incidences were placebo, 3.1%; 10 mg, 12.2%; 30 mg, 27.3%); somnolence (incidences were placebo, 3.1%; 10 mg, 19.4%; 30 mg, 26.3%); akathisia (incidences were placebo, 2.1%; 10 mg, 8.2%; 30 mg, 11.1%); and salivary hypersecretion (incidences were placebo, 0%; 10 mg, 3.1%; 30 mg, 8.1%).
Autistic Disorder
In a study of pediatric patients (6 to 17 years of age) with autistic disorder, one common adverse reaction had a possible dose response relationship: fatigue (incidences were placebo, 0%; 5 mg, 3.8%; 10 mg, 22.0%; 15 mg, 18.5%).
Extrapyramidal Symptoms
Schizophrenia
In short-term, placebo-controlled trials in schizophrenia in adults, the incidence of reported EPS-related events, excluding events related to akathisia, for aripiprazole-treated patients was 13% vs. 12% for placebo; and the incidence of akathisia-related events for aripiprazole-treated patients was 8% vs. 4% for placebo. In the short-term, placebo-controlled trial of schizophrenia in pediatric patients (13 to 17 years), the incidence of reported EPS-related events, excluding events related to akathisia, for aripiprazole-treated patients was 25% vs. 7% for placebo; and the incidence of akathisia-related events for aripiprazole-treated patients was 9% vs. 6% for placebo.
Objectively collected data from those trials was collected on the Simpson Angus Rating Scale (for EPS), the Barnes Akathisia Scale (for akathisia), and the Assessments of Involuntary Movement Scales (for dyskinesias). In the adult schizophrenia trials, the objectively collected data did not show a difference between aripiprazole and placebo, with the exception of the Barnes Akathisia Scale (aripiprazole, 0.08; placebo, −0.05). In the pediatric (13 to 17 years) schizophrenia trial, the objectively collected data did not show a difference between aripiprazole and placebo, with the exception of the Simpson Angus Rating Scale (aripiprazole, 0.24; placebo, −0.29).
Similarly, in a long-term (26-week), placebo-controlled trial of schizophrenia in adults, objectively collected data on the Simpson Angus Rating Scale (for EPS), the Barnes Akathisia Scale (for akathisia), and the Assessments of Involuntary Movement Scales (for dyskinesias) did not show a difference between aripiprazole and placebo.
Bipolar Mania
In the short-term, placebo-controlled trials in bipolar mania in adults, the incidence of reported EPS-related events, excluding events related to akathisia, for monotherapy aripiprazole-treated patients was 16% vs. 8% for placebo and the incidence of akathisia-related events for monotherapy aripiprazole-treated patients was 13% vs. 4% for placebo. In the 6-week, placebo-controlled trial in bipolar mania for adjunctive therapy with lithium or valproate, the incidence of reported EPS-related events, excluding events related to akathisia for adjunctive aripiprazole-treated patients was 15% vs. 8% for adjunctive placebo and the incidence of akathisia-related events for adjunctive aripiprazole-treated patients was 19% vs. 5% for adjunctive placebo. In the short-term, placebo-controlled trial in bipolar mania in pediatric (10 to 17 years) patients, the incidence of reported EPS-related events, excluding events related to akathisia, for aripiprazole-treated patients was 26% vs. 5% for placebo and the incidence of akathisia-related events for aripiprazole-treated patients was 10% vs. 2% for placebo.
In the adult bipolar mania trials with monotherapy aripiprazole, the Simpson Angus Rating Scale and the Barnes Akathisia Scale showed a significant difference between aripiprazole and placebo (aripiprazole, 0.50; placebo, −0.01 and aripiprazole, 0.21; placebo, −0.05). Changes in the Assessments of Involuntary Movement Scales were similar for the aripiprazole and placebo groups. In the bipolar mania trials with aripiprazole as adjunctive therapy with either lithium or valproate, the Simpson Angus Rating Scale and the Barnes Akathisia Scale showed a significant difference between adjunctive aripiprazole and adjunctive placebo (aripiprazole, 0.73; placebo, 0.07 and aripiprazole, 0.30; placebo, 0.11). Changes in the Assessments of Involuntary Movement Scales were similar for adjunctive aripiprazole and adjunctive placebo. In the pediatric (10 to 17 years), short-term, bipolar mania trial, the Simpson Angus Rating Scale showed a significant difference between aripiprazole and placebo (aripiprazole, 0.90; placebo, –0.05). Changes in the Barnes Akathisia Scale and the Assessments of Involuntary Movement Scales were similar for the aripiprazole and placebo groups.
Major Depressive Disorder
In the short-term, placebo-controlled trials in major depressive disorder, the incidence of reported EPS-related events, excluding events related to akathisia, for adjunctive aripiprazole-treated patients was 8% vs. 5% for adjunctive placebo-treated patients; and the incidence of akathisia-related events for adjunctive aripiprazole-treated patients was 25% vs. 4% for adjunctive placebo-treated patients.
In the major depressive disorder trials, the Simpson Angus Rating Scale and the Barnes Akathisia Scale showed a significant difference between adjunctive aripiprazole and adjunctive placebo (aripiprazole, 0.31; placebo, 0.03 and aripiprazole, 0.22; placebo, 0.02). Changes in the Assessments of Involuntary Movement Scales were similar for the adjunctive aripiprazole and adjunctive placebo groups.
Autistic Disorder
In the short-term, placebo-controlled trials in autistic disorder in pediatric patients (6 to 17 years), the incidence of reported EPS-related events, excluding events related to akathisia, for aripiprazole-treated patients was 18% vs. 2% for placebo and the incidence of akathisia-related events for aripiprazole-treated patients was 3% vs. 9% for placebo.
In the pediatric (6 to 17 years) short-term autistic disorder trials, the Simpson Angus Rating Scale showed a significant difference between aripiprazole and placebo (aripiprazole, 0.1; placebo, −0.4). Changes in the Barnes Akathisia Scale and the Assessments of Involuntary Movement Scales were similar for the aripiprazole and placebo groups.
Agitation Associated with Schizophrenia or Bipolar Mania
In the placebo-controlled trials in patients with agitation associated with schizophrenia or bipolar mania, the incidence of reported EPS-related events excluding events related to akathisia for aripiprazole-treated patients was 2% vs. 2% for placebo and the incidence of akathisia-related events for aripiprazole-treated patients was 2% vs. 0% for placebo. Objectively collected data on the Simpson Angus Rating Scale (for EPS) and the Barnes Akathisia Scale (for akathisia) for all treatment groups did not show a difference between aripiprazole and placebo.
Dystonia
Class Effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
Laboratory Test Abnormalities
A between group comparison for 3-week to 6-week, placebo-controlled trials in adults or 4-week to 8-week, placebo-controlled trials in pediatric patients (6 to 17 years) revealed no medically important differences between the aripiprazole and placebo groups in the proportions of patients experiencing potentially clinically significant changes in routine serum chemistry, hematology, or urinalysis parameters. Similarly, there were no aripiprazole/placebo differences in the incidence of discontinuations for changes in serum chemistry, hematology, or urinalysis in adult or pediatric patients.
ECG Changes
Between group comparisons for a pooled analysis of placebo-controlled trials in patients with schizophrenia, bipolar mania, or major depressive disorder revealed no significant differences between oral aripiprazole and placebo in the proportion of patients experiencing potentially important changes in ECG parameters. Aripiprazole was associated with a median increase in heart rate of 2 beats per minute compared to no increase among placebo patients.
In the pooled, placebo-controlled trials in patients with agitation associated with schizophrenia or bipolar mania, there were no significant differences between aripiprazole injection and placebo in the proportion of patients experiencing potentially important changes in ECG parameters, as measured by standard 12-lead ECGs.
Additional Findings Observed in Clinical Trials
Adverse Reactions in Long-Term, Double-Blind, Placebo-Controlled Trials
The adverse reactions reported in a 26-week, double-blind trial comparing oral ABILIFY and placebo in patients with schizophrenia were generally consistent with those reported in the short-term, placebo-controlled trials, except for a higher incidence of tremor [8% (12/153) for ABILIFY vs. 2% (3/153) for placebo]. In this study, the majority of the cases of tremor were of mild intensity (8/12 mild and 4/12 moderate), occurred early in therapy (9/12 ≤49 days), and were of limited duration (7/12 ≤10 days). Tremor infrequently led to discontinuation (<1%) of ABILIFY. In addition, in a long-term (52-week), active-controlled study, the incidence of tremor was 5% (40/859) for ABILIFY. A similar profile was observed in a long-term monotherapy study and a long-term adjunctive study with lithium and valproate in bipolar disorder.
Other Adverse Reactions Observed During the Premarketing Evaluation of Aripiprazole
Following is a list of MedDRA terms that reflect adverse reactions as defined in ADVERSE REACTIONS (6.1) reported by patients treated with oral aripiprazole at multiple doses ≥2 mg/day during any phase of a trial within the database of 13,543 adult patients. All events assessed as possible adverse drug reactions have been included with the exception of more commonly occurring events. In addition, medically/clinically meaningful adverse reactions, particularly those that are likely to be useful to the prescriber or that have pharmacologic plausibility, have been included. Events already listed in other parts of ADVERSE REACTIONS (6), or those considered in WARNINGS AND PRECAUTIONS (5) or OVERDOSAGE (10) have been excluded. Although the reactions reported occurred during treatment with aripiprazole, they were not necessarily caused by it.
Events are further categorized by MedDRA system organ class and listed in order of decreasing frequency according to the following definitions: those occurring in at least 1/100 patients (only those not already listed in the tabulated results from placebo-controlled trials appear in this listing); those occurring in 1/100 to 1/1000 patients; and those occurring in fewer than 1/1000 patients.
Adults - Oral Administration
Blood and Lymphatic System Disorders:
≥1/1000 patients and <1/100 patients
- leukopenia, neutropenia, thrombocytopenia
Cardiac Disorders:
≥1/1000 patients and <1/100 patients
- bradycardia, palpitations, cardiopulmonary failure, myocardial infarction, cardio-respiratory arrest, atrioventricular block, extrasystoles, sinus tachycardia, atrial fibrillation, angina pectoris, myocardial ischemia;
<1/1000 patients
- atrial flutter, supraventricular tachycardia, ventricular tachycardia
Eye Disorders:
≥1/1000 patients and <1/100 patients
- photophobia, diplopia, eyelid edema, photopsia
Gastrointestinal Disorders:
≥1/1000 patients and <1/100 patients
- gastroesophageal reflux disease, swollen tongue, esophagitis;
<1/1000 patients
- pancreatitis
General Disorders and Administration Site Conditions:
≥1/100 patients
- asthenia, peripheral edema, chest pain;
≥1/1000 patients and <1/100 patients
- face edema, angioedema;
<1/1000 patients
- hypothermia
Hepatobiliary Disorders:
<1/1000 patients
- hepatitis, jaundice
Immune System Disorders:
≥1/1000 patients and <1/100 patients
- hypersensitivity
Injury, Poisoning, and Procedural Complications:
≥1/100 patients
- fall;
≥1/1000 patients and <1/100 patients
- self mutilation;
<1/1000 patients
- heat stroke
Investigations:
≥1/100 patients
- weight decreased, creatine phosphokinase increased;
≥1/1000 patients and <1/100 patients
- hepatic enzyme increased, blood glucose increased, blood prolactin increased, blood urea increased, electrocardiogram QT prolonged, blood creatinine increased, blood bilirubin increased;
<1/1000 patients
- blood lactate dehydrogenase increased, glycosylated hemoglobin increased, gamma-glutamyl transferase increased
Metabolism and Nutrition Disorders:
≥1/1000 patients and <1/100 patients
- hyperlipidemia, anorexia, diabetes mellitus (including blood insulin increased, carbohydrate tolerance decreased, diabetes mellitus non-insulin-dependent, glucose tolerance impaired, glycosuria, glucose urine, glucose urine present), hyperglycemia, hypokalemia, hyponatremia, hypoglycemia, polydipsia;
<1/1000 patients
- diabetic ketoacidosis
Musculoskeletal and Connective Tissue Disorders:
≥1/1000 patients and <1/100 patients
- muscle rigidity, muscular weakness, muscle tightness, mobility decreased;
<1/1000 patients
- rhabdomyolysis
Nervous System Disorders:
≥1/100 patients
- coordination abnormal;
≥1/1000 patients and <1/100 patients
- speech disorder, parkinsonism, memory impairment, cogwheel rigidity, cerebrovascular accident, hypokinesia, tardive dyskinesia, hypotonia, myoclonus, hypertonia, akinesia, bradykinesia;
<1/1000 patients
- Grand Mal convulsion, choreoathetosis
Psychiatric Disorders:
≥1/100 patients
- suicidal ideation;
≥1/1000 patients and <1/100 patients
- aggression, loss of libido, suicide attempt, hostility, libido increased, anger, anorgasmia, delirium, intentional self injury, completed suicide, tic, homicidal ideation;
<1/1000 patients
- catatonia, sleep walking
Renal and Urinary Disorders:
≥1/1000 patients and <1/100 patients
- urinary retention, polyuria, nocturia
Reproductive System and Breast Disorders:
≥1/1000 patients and <1/100 patients
- menstruation irregular, erectile dysfunction, amenorrhea, breast pain;
<1/1000 patients
- gynaecomastia, priapism
Respiratory, Thoracic, and Mediastinal Disorders:
≥1/100 patients
- nasal congestion, dyspnea, pneumonia aspiration
Skin and Subcutaneous Tissue Disorders:
≥1/100 patients
- rash (including erythematous, exfoliative, generalized, macular, maculopapular, papular rash; acneiform, allergic, contact, exfoliative, seborrheic dermatitis, neurodermatitis, and drug eruption), hyperhydrosis;
≥1/1000 patients and <1/100 patients
- pruritus, photosensitivity reaction, alopecia, urticaria
Vascular Disorders:
≥1/100 patients
- hypertension;
≥1/1000 patients and <1/100 patients
- hypotension
Pediatric Patients - Oral Administration
Most adverse events observed in the pooled database of 920 pediatric patients, aged 6 to 17 years, were also observed in the adult population. Additional adverse reactions observed in the pediatric population are listed below.
Gastrointestinal Disorders:
≥1/1000 patients and <1/100 patients
- tongue dry, tongue spasm
Investigations:
≥1/100 patients
- blood insulin increased
Nervous System Disorders:
≥1/1000 patients and <1/100 patients
- sleep talking
Skin and Subcutaneous Tissue Disorders:
≥1/1000 patients and <1/100 patients
- hirsutism
Adults - Intramuscular Injection
Most adverse reactions observed in the pooled database of 749 adult patients treated with aripiprazole injection, were also observed in the adult population treated with oral aripiprazole. Additional adverse reactions observed in the aripiprazole injection population are listed below.
General Disorders and Administration Site Conditions:
≥1/100 patients
- injection site reaction;
≥1/1000 patients and <1/100 patients
- venipuncture site bruise
The following adverse reactions have been identified during postapproval use of ABILIFY. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to establish a causal relationship to drug exposure: rare occurrences of allergic reaction (anaphylactic reaction, angioedema, laryngospasm, pruritus/urticaria, or oropharyngeal spasm), and blood glucose fluctuation.
DRUG INTERACTIONS
Given the primary CNS effects of aripiprazole, caution should be used when ABILIFY is taken in combination with other centrally-acting drugs or alcohol.
Due to its alpha adrenergic antagonism, aripiprazole has the potential to enhance the effect of certain antihypertensive agents.
Aripiprazole is not a substrate of CYP1A1, CYP1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, or CYP2E1 enzymes. Aripiprazole also does not undergo direct glucuronidation. This suggests that an interaction of aripiprazole with inhibitors or inducers of these enzymes, or other factors, like smoking, is unlikely.
Both CYP3A4 and CYP2D6 are responsible for aripiprazole metabolism. Agents that induce CYP3A4 (eg, carbamazepine) could cause an increase in aripiprazole clearance and lower blood levels. Inhibitors of CYP3A4 (eg, ketoconazole) or CYP2D6 (eg, quinidine, fluoxetine, or paroxetine) can inhibit aripiprazole elimination and cause increased blood levels.
Ketoconazole and Other CYP3A4 Inhibitors
Coadministration of ketoconazole (200 mg/day for 14 days) with a 15 mg single dose of aripiprazole increased the AUC of aripiprazole and its active metabolite by 63% and 77%, respectively. The effect of a higher ketoconazole dose (400 mg/day) has not been studied. When ketoconazole is given concomitantly with aripiprazole, the aripiprazole dose should be reduced to one-half of its normal dose. Other strong inhibitors of CYP3A4 (itraconazole) would be expected to have similar effects and need similar dose reductions; moderate inhibitors (erythromycin, grapefruit juice) have not been studied. When the CYP3A4 inhibitor is withdrawn from the combination therapy, the aripiprazole dose should be increased.
Quinidine and Other CYP2D6 Inhibitors
Coadministration of a 10 mg single dose of aripiprazole with quinidine (166 mg/day for 13 days), a potent inhibitor of CYP2D6, increased the AUC of aripiprazole by 112% but decreased the AUC of its active metabolite, dehydro-aripiprazole, by 35%. Aripiprazole dose should be reduced to one-half of its normal dose when quinidine is given concomitantly with aripiprazole. Other significant inhibitors of CYP2D6, such as fluoxetine or paroxetine, would be expected to have similar effects and should lead to similar dose reductions. When the CYP2D6 inhibitor is withdrawn from the combination therapy, the aripiprazole dose should be increased. When adjunctive ABILIFY is administered to patients with major depressive disorder, ABILIFY should be administered without dosage adjustment as specified in DOSAGE AND ADMINISTRATION (2.3).
Carbamazepine and Other CYP3A4 Inducers
Coadministration of carbamazepine (200 mg twice daily), a potent CYP3A4 inducer, with aripiprazole (30 mg/day) resulted in an approximate 70% decrease in Cmax and AUC values of both aripiprazole and its active metabolite, dehydro-aripiprazole. When carbamazepine is added to aripiprazole therapy, aripiprazole dose should be doubled. Additional dose increases should be based on clinical evaluation. When carbamazepine is withdrawn from the combination therapy, the aripiprazole dose should be reduced.
Aripiprazole is unlikely to cause clinically important pharmacokinetic interactions with drugs metabolized by cytochrome P450 enzymes. In in vivo studies, 10 mg/day to 30 mg/day doses of aripiprazole had no significant effect on metabolism by CYP2D6 (dextromethorphan), CYP2C9 (warfarin), CYP2C19 (omeprazole, warfarin), and CYP3A4 (dextromethorphan) substrates. Additionally, aripiprazole and dehydro-aripiprazole did not show potential for altering CYP1A2-mediated metabolism in vitro.
No effect of aripiprazole was seen on the pharmacokinetics of lithium or valproate.
Alcohol
There was no significant difference between aripiprazole coadministered with ethanol and placebo coadministered with ethanol on performance of gross motor skills or stimulus response in healthy subjects. As with most psychoactive medications, patients should be advised to avoid alcohol while taking ABILIFY.
Famotidine
Coadministration of aripiprazole (given in a single dose of 15 mg) with a 40 mg single dose of the H 2 antagonist famotidine, a potent gastric acid blocker, decreased the solubility of aripiprazole and, hence, its rate of absorption, reducing by 37% and 21% the Cmax of aripiprazole and dehydro-aripiprazole, respectively, and by 13% and 15%, respectively, the extent of absorption (AUC). No dosage adjustment of aripiprazole is required when administered concomitantly with famotidine.
Valproate
When valproate (500 mg/day-1500 mg/day) and aripiprazole (30 mg/day) were coadministered, at steady-state the Cmax and AUC of aripiprazole were decreased by 25%. No dosage adjustment of aripiprazole is required when administered concomitantly with valproate.
When aripiprazole (30 mg/day) and valproate (1000 mg/day) were coadministered, at steady-state there were no clinically significant changes in the Cmax or AUC of valproate. No dosage adjustment of valproate is required when administered concomitantly with aripiprazole.
Lithium
A pharmacokinetic interaction of aripiprazole with lithium is unlikely because lithium is not bound to plasma proteins, is not metabolized, and is almost entirely excreted unchanged in urine. Coadministration of therapeutic doses of lithium (1200 mg/day-1800 mg/day) for 21 days with aripiprazole (30 mg/day) did not result in clinically significant changes in the pharmacokinetics of aripiprazole or its active metabolite, dehydro-aripiprazole (Cmax and AUC increased by less than 20%). No dosage adjustment of aripiprazole is required when administered concomitantly with lithium.
Coadministration of aripiprazole (30 mg/day) with lithium (900 mg/day) did not result in clinically significant changes in the pharmacokinetics of lithium. No dosage adjustment of lithium is required when administered concomitantly with aripiprazole.
Lamotrigine
Coadministration of 10 mg/day to 30 mg/day oral doses of aripiprazole for 14 days to patients with bipolar I disorder had no effect on the steady-state pharmacokinetics of 100 mg/day to 400 mg/day lamotrigine, a UDP-glucuronosyltransferase 1A4 substrate. No dosage adjustment of lamotrigine is required when aripiprazole is added to lamotrigine.
Dextromethorphan
Aripiprazole at doses of 10 mg/day to 30 mg/day for 14 days had no effect on dextromethorphan’s O-dealkylation to its major metabolite, dextrorphan, a pathway dependent on CYP2D6 activity. Aripiprazole also had no effect on dextromethorphan’s N-demethylation to its metabolite 3-methoxymorphinan, a pathway dependent on CYP3A4 activity. No dosage adjustment of dextromethorphan is required when administered concomitantly with aripiprazole.
Warfarin
Aripiprazole 10 mg/day for 14 days had no effect on the pharmacokinetics of R-warfarin and S-warfarin or on the pharmacodynamic end point of International Normalized Ratio, indicating the lack of a clinically relevant effect of aripiprazole on CYP2C9 and CYP2C19 metabolism or the binding of highly protein-bound warfarin. No dosage adjustment of warfarin is required when administered concomitantly with aripiprazole.
Omeprazole
Aripiprazole 10 mg/day for 15 days had no effect on the pharmacokinetics of a single 20 mg dose of omeprazole, a CYP2C19 substrate, in healthy subjects. No dosage adjustment of omeprazole is required when administered concomitantly with aripiprazole.
Lorazepam
Coadministration of lorazepam injection (2 mg) and aripiprazole injection (15 mg) to healthy subjects (n=40: 35 males and 5 females; ages 19-45 years old) did not result in clinically important changes in the pharmacokinetics of either drug. No dosage adjustment of aripiprazole is required when administered concomitantly with lorazepam. However, the intensity of sedation was greater with the combination as compared to that observed with aripiprazole alone and the orthostatic hypotension observed was greater with the combination as compared to that observed with lorazepam alone [see WARNINGS AND PRECAUTIONS (5.6)] .
Escitalopram
Coadministration of 10 mg/day oral doses of aripiprazole for 14 days to healthy subjects had no effect on the steady-state pharmacokinetics of 10 mg/day escitalopram, a substrate of CYP2C19 and CYP3A4. No dosage adjustment of escitalopram is required when aripiprazole is added to escitalopram.
Venlafaxine
Coadministration of 10 mg/day to 20 mg/day oral doses of aripiprazole for 14 days to healthy subjects had no effect on the steady-state pharmacokinetics of venlafaxine and O-desmethylvenlafaxine following 75 mg/day venlafaxine XR, a CYP2D6 substrate. No dosage adjustment of venlafaxine is required when aripiprazole is added to venlafaxine.
Fluoxetine, Paroxetine, and Sertraline
A population pharmacokinetic analysis in patients with major depressive disorder showed no substantial change in plasma concentrations of fluoxetine (20 mg/day or 40 mg/day), paroxetine CR (37.5 mg/day or 50 mg/day), or sertraline (100 mg/day or 150 mg/day) dosed to steady-state. The steady-state plasma concentrations of fluoxetine and norfluoxetine increased by about 18% and 36%, respectively, and concentrations of paroxetine decreased by about 27%. The steady-state plasma concentrations of sertraline and desmethylsertraline were not substantially changed when these antidepressant therapies were coadministered with aripiprazole. Aripiprazole dosing was 2 mg/day to 15 mg/day (when given with fluoxetine or paroxetine) or 2 mg/day to 20 mg/day (when given with sertraline).
USE IN SPECIFIC POPULATIONS
In general, no dosage adjustment for ABILIFY is required on the basis of a patient’s age, gender, race, smoking status, hepatic function, or renal function [see DOSAGE AND ADMINISTRATION (2.5)] .
Teratogenic Effects
Pregnancy Category C: In animal studies, aripiprazole demonstrated developmental toxicity, including possible teratogenic effects in rats and rabbits.
Pregnant rats were treated with oral doses of 3 mg/kg/day, 10 mg/kg/day, and 30 mg/kg/day (1 times, 3 times, and 10 times the maximum recommended human dose [MRHD] on a mg/m 2 basis) of aripiprazole during the period of organogenesis. Gestation was slightly prolonged at 30 mg/kg. Treatment caused a slight delay in fetal development, as evidenced by decreased fetal weight (30 mg/kg), undescended testes (30 mg/kg), and delayed skeletal ossification (10 mg/kg and 30 mg/kg). There were no adverse effects on embryofetal or pup survival. Delivered offspring had decreased body weights (10 mg/kg and 30 mg/kg), and increased incidences of hepatodiaphragmatic nodules and diaphragmatic hernia at 30 mg/kg (the other dose groups were not examined for these findings). A low incidence of diaphragmatic hernia was also seen in the fetuses exposed to 30 mg/kg. Postnatally, delayed vaginal opening was seen at 10 mg/kg and 30 mg/kg and impaired reproductive performance (decreased fertility rate, corpora lutea, implants, live fetuses, and increased post-implantation loss, likely mediated through effects on female offspring) was seen at 30 mg/kg. Some maternal toxicity was seen at 30 mg/kg; however, there was no evidence to suggest that these developmental effects were secondary to maternal toxicity.
In pregnant rats receiving aripiprazole injection intravenously (3 mg/kg/day, 9 mg/kg/day, and 27 mg/kg/day) during the period of organogenesis, decreased fetal weight and delayed skeletal ossification were seen at the highest dose, which also caused some maternal toxicity.
Pregnant rabbits were treated with oral doses of 10 mg/kg/day, 30 mg/kg/day, and 100 mg/kg/day (2 times, 3 times, and 11 times human exposure at MRHD based on AUC and 6 times, 19 times, and 65 times the MRHD based on mg/m 2) of aripiprazole during the period of organogenesis. Decreased maternal food consumption and increased abortions were seen at 100 mg/kg. Treatment caused increased fetal mortality (100 mg/kg), decreased fetal weight (30 mg/kg and 100 mg/kg), increased incidence of a skeletal abnormality (fused sternebrae at 30 mg/kg and 100 mg/kg), and minor skeletal variations (100 mg/kg).
In pregnant rabbits receiving aripiprazole injection intravenously (3 mg/kg/day, 10 mg/kg/day, and 30 mg/kg/day) during the period of organogenesis, the highest dose, which caused pronounced maternal toxicity, resulted in decreased fetal weight, increased fetal abnormalities (primarily skeletal), and decreased fetal skeletal ossification. The fetal no-effect dose was 10 mg/kg, which produced 5 times the human exposure at the MRHD based on AUC and is 6 times the MRHD based on mg/m 2.
In a study in which rats were treated with oral doses of 3 mg/kg/day, 10 mg/kg/day, and 30 mg/kg/day (1 times, 3 times, and 10 times the MRHD on a mg/m 2 basis) of aripiprazole perinatally and postnatally (from day 17 of gestation through day 21 postpartum), slight maternal toxicity and slightly prolonged gestation were seen at 30 mg/kg. An increase in stillbirths and decreases in pup weight (persisting into adulthood) and survival were seen at this dose.
In rats receiving aripiprazole injection intravenously (3 mg/kg/day, 8 mg/kg/day, and 20 mg/kg/day) from day 6 of gestation through day 20 postpartum, an increase in stillbirths was seen at 8 mg/kg and 20 mg/kg, and decreases in early postnatal pup weights and survival were seen at 20 mg/kg. These doses produced some maternal toxicity. There were no effects on postnatal behavioral and reproductive development.
Non-teratogenic Effects
There are no adequate and well-controlled studies in pregnant women. It is not known whether aripiprazole can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity. Neonates exposed to antipsychotic drugs during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery. There have been reports of agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder in these neonates. These complications have varied in severity; while in some cases symptoms have been self-limited, in other cases neonates have required intensive care unit support and prolonged hospitalization.
Aripiprazole should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
The effect of aripiprazole on labor and delivery in humans is unknown.
Aripiprazole has been demonstrated to be excreted in milk of rats during lactation. In humans, data on excretion in breast milk is limited. It is recommended that women receiving aripiprazole should not breast-feed.
Safety and effectiveness in pediatric patients with major depressive disorder or agitation associated with schizophrenia or bipolar mania have not been established.
Safety and effectiveness in pediatric patients with schizophrenia were established in a 6-week, placebo-controlled clinical trial in 202 pediatric patients aged 13 to 17 years [see INDICATIONS AND USAGE (1.1), DOSAGE AND ADMINISTRATION (2.1), ADVERSE REACTIONS (6.2), and CLINICAL STUDIES (14.1)] . Although maintenance efficacy in pediatric patients has not been systematically evaluated, maintenance efficacy can be extrapolated from adult data along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients.
Safety and effectiveness in pediatric patients with bipolar mania were established in a 4-week, placebo-controlled clinical trial in 197 pediatric patients aged 10 to 17 years [see INDICATIONS AND USAGE (1.2), DOSAGE AND ADMINISTRATION (2.2), ADVERSE REACTIONS (6.2), and CLINICAL STUDIES (14.2)] . Although maintenance efficacy in pediatric patients has not been systematically evaluated, maintenance efficacy can be extrapolated from adult data along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients.
The efficacy of adjunctive ABILIFY with concomitant lithium or valproate in the treatment of manic or mixed episodes in pediatric patients has not been systematically evaluated. However, such efficacy and lack of pharmacokinetic interaction between aripiprazole and lithium or valproate can be extrapolated from adult data, along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients.
Safety and effectiveness in pediatric patients demonstrating irritability associated with autistic disorder were established in two 8-week, placebo-controlled clinical trials in 212 pediatric patients aged 6 to 17 years [see INDICATIONS AND USAGE (1.4), DOSAGE AND ADMINISTRATION (2.4), ADVERSE REACTIONS (6.2), and CLINICAL STUDIES (14.4)] . Maintenance efficacy in pediatric patients has not been systematically evaluated.
The pharmacokinetics of aripiprazole and dehydro-aripiprazole in pediatric patients, 10 to 17 years of age, were similar to those in adults after correcting for the differences in body weight.
In formal single-dose pharmacokinetic studies (with aripiprazole given in a single dose of 15 mg), aripiprazole clearance was 20% lower in elderly (≥65 years) subjects compared to younger adult subjects (18 to 64 years). There was no detectable age effect, however, in the population pharmacokinetic analysis in schizophrenia patients. Also, the pharmacokinetics of aripiprazole after multiple doses in elderly patients appeared similar to that observed in young, healthy subjects. No dosage adjustment is recommended for elderly patients [see also BOXED WARNING and WARNINGS AND PRECAUTIONS (5.1)] .
Of the 13,543 patients treated with oral aripiprazole in clinical trials, 1073 (8%) were ≥65 years old and 799 (6%) were ≥75 years old. The majority (81%) of the 1073 patients were diagnosed with Dementia of the Alzheimer’s type.
Placebo-controlled studies of oral aripiprazole in schizophrenia, bipolar mania, or major depressive disorder did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Of the 749 patients treated with aripiprazole injection in clinical trials, 99 (13%) were ≥65 years old and 78 (10%) were ≥75 years old. Placebo-controlled studies of aripiprazole injection in patients with agitation associated with schizophrenia or bipolar mania did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Studies of elderly patients with psychosis associated with Alzheimer’s disease have suggested that there may be a different tolerability profile in this population compared to younger patients with schizophrenia [see also BOXED WARNING and WARNINGS AND PRECAUTIONS (5.1)] . The safety and efficacy of ABILIFY in the treatment of patients with psychosis associated with Alzheimer’s disease has not been established. If the prescriber elects to treat such patients with ABILIFY, vigilance should be exercised.
In patients with severe renal impairment (creatinine clearance <30 mL/min), Cmax of aripiprazole (given in a single dose of 15 mg) and dehydro-aripiprazole increased by 36% and 53%, respectively, but AUC was 15% lower for aripiprazole and 7% higher for dehydro-aripiprazole. Renal excretion of both unchanged aripiprazole and dehydro-aripiprazole is less than 1% of the dose. No dosage adjustment is required in subjects with renal impairment.
In a single-dose study (15 mg of aripiprazole) in subjects with varying degrees of liver cirrhosis (Child-Pugh Classes A, B, and C), the AUC of aripiprazole, compared to healthy subjects, increased 31% in mild HI, increased 8% in moderate HI, and decreased 20% in severe HI. None of these differences would require dose adjustment.
Cmax and AUC of aripiprazole and its active metabolite, dehydro-aripiprazole, are 30% to 40% higher in women than in men, and correspondingly, the apparent oral clearance of aripiprazole is lower in women. These differences, however, are largely explained by differences in body weight (25%) between men and women. No dosage adjustment is recommended based on gender.
Although no specific pharmacokinetic study was conducted to investigate the effects of race on the disposition of aripiprazole, population pharmacokinetic evaluation revealed no evidence of clinically significant race-related differences in the pharmacokinetics of aripiprazole. No dosage adjustment is recommended based on race.
Based on studies utilizing human liver enzymes in vitro, aripiprazole is not a substrate for CYP1A2 and also does not undergo direct glucuronidation. Smoking should, therefore, not have an effect on the pharmacokinetics of aripiprazole. Consistent with these in vitro results, population pharmacokinetic evaluation did not reveal any significant pharmacokinetic differences between smokers and nonsmokers. No dosage adjustment is recommended based on smoking status.
DRUG ABUSE AND DEPENDENCE
ABILIFY is not a controlled substance.
Aripiprazole has not been systematically studied in humans for its potential for abuse, tolerance, or physical dependence. In physical dependence studies in monkeys, withdrawal symptoms were observed upon abrupt cessation of dosing. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of ABILIFY misuse or abuse (eg, development of tolerance, increases in dose, drug-seeking behavior).
OVERDOSAGE
MedDRA terminology has been used to classify the adverse reactions.
In clinical trials and in postmarketing experience, adverse reactions of deliberate or accidental overdosage with oral aripiprazole have been reported worldwide. These include overdoses with oral aripiprazole alone and in combination with other substances. No fatality was reported with aripiprazole alone. The largest known dose with a known outcome involved acute ingestion of 1260 mg of oral aripiprazole (42 times the maximum recommended daily dose) by a patient who fully recovered. Deliberate or accidental overdosage was also reported in children (age 12 and younger) involving oral aripiprazole ingestions up to 195 mg with no fatalities.
Common adverse reactions (reported in at least 5% of all overdose cases) reported with oral aripiprazole overdosage (alone or in combination with other substances) include vomiting, somnolence, and tremor. Other clinically important signs and symptoms observed in one or more patients with aripiprazole overdoses (alone or with other substances) include acidosis, aggression, aspartate aminotransferase increased, atrial fibrillation, bradycardia, coma, confusional state, convulsion, blood creatine phosphokinase increased, depressed level of consciousness, hypertension, hypokalemia, hypotension, lethargy, loss of consciousness, QRS complex prolonged, QT prolonged, pneumonia aspiration, respiratory arrest, status epilepticus, and tachycardia.
No specific information is available on the treatment of overdose with aripiprazole. An electrocardiogram should be obtained in case of overdosage and if QT interval prolongation is present, cardiac monitoring should be instituted. Otherwise, management of overdose should concentrate on supportive therapy, maintaining an adequate airway, oxygenation and ventilation, and management of symptoms. Close medical supervision and monitoring should continue until the patient recovers.
Charcoal: In the event of an overdose of ABILIFY, an early charcoal administration may be useful in partially preventing the absorption of aripiprazole. Administration of 50 g of activated charcoal, one hour after a single 15 mg oral dose of aripiprazole, decreased the mean AUC and Cmax of aripiprazole by 50%.
Hemodialysis: Although there is no information on the effect of hemodialysis in treating an overdose with aripiprazole, hemodialysis is unlikely to be useful in overdose management since aripiprazole is highly bound to plasma proteins.
DESCRIPTION
Aripiprazole is a psychotropic drug that is available as ABILIFY ® (aripiprazole) Tablets, ABILIFY DISCMELT ® (aripiprazole) Orally Disintegrating Tablets, ABILIFY ® (aripiprazole) Oral Solution, and ABILIFY ® (aripiprazole) Injection, a solution for intramuscular injection. Aripiprazole is 7-[4-[4-(2,3-dichlorophenyl)-1-piperazinyl]butoxy]-3,4-dihydrocarbostyril. The empirical formula is C 23H 27Cl 2N 3O 2 and its molecular weight is 448.38. The chemical structure is:
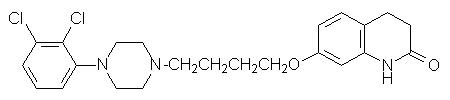
ABILIFY Tablets are available in 2 mg, 5 mg, 10 mg, 15 mg, 20 mg, and 30 mg strengths. Inactive ingredients include cornstarch, hydroxypropyl cellulose, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. Colorants include ferric oxide (yellow or red) and FD&C Blue No. 2 Aluminum Lake.
ABILIFY DISCMELT Orally Disintegrating Tablets are available in 10 mg and 15 mg strengths. Inactive ingredients include acesulfame potassium, aspartame, calcium silicate, croscarmellose sodium, crospovidone, crème de vanilla (natural and artificial flavors), magnesium stearate, microcrystalline cellulose, silicon dioxide, tartaric acid, and xylitol. Colorants include ferric oxide (yellow or red) and FD&C Blue No. 2 Aluminum Lake.
ABILIFY Oral Solution is a clear, colorless to light-yellow solution available in a concentration of 1 mg/mL. The inactive ingredients for this solution include disodium edetate, fructose, glycerin, dl-lactic acid, methylparaben, propylene glycol, propylparaben, sodium hydroxide, sucrose, and purified water. The oral solution is flavored with natural orange cream and other natural flavors.
ABILIFY Injection is available in single-dose vials as a ready-to-use, 9.75 mg/1.3 mL (7.5 mg/mL) clear, colorless, sterile, aqueous solution for intramuscular use only. Inactive ingredients for this solution include 150 mg/mL of sulfobutylether β-cyclodextrin (SBECD), tartaric acid, sodium hydroxide, and water for injection.
CLINICAL PHARMACOLOGY
The mechanism of action of aripiprazole, as with other drugs having efficacy in schizophrenia, bipolar disorder, major depressive disorder, irritability associated with autistic disorder, and agitation associated with schizophrenia or bipolar disorder, is unknown. However, it has been proposed that the efficacy of aripiprazole is mediated through a combination of partial agonist activity at D 2 and 5-HT 1A receptors and antagonist activity at 5-HT 2A receptors. Actions at receptors other than D 2, 5-HT 1A, and 5-HT 2A may explain some of the other clinical effects of aripiprazole (eg, the orthostatic hypotension observed with aripiprazole may be explained by its antagonist activity at adrenergic alpha 1 receptors).
Aripiprazole exhibits high affinity for dopamine D 2 and D 3, serotonin 5-HT 1A and 5-HT 2A receptors (K i values of 0.34 nM, 0.8 nM, 1.7 nM, and 3.4 nM, respectively), moderate affinity for dopamine D 4, serotonin 5-HT 2C and 5-HT 7, alpha 1-adrenergic and histamine H 1 receptors (K i values of 44 nM, 15 nM, 39 nM, 57 nM, and 61 nM, respectively), and moderate affinity for the serotonin reuptake site (K i=98 nM). Aripiprazole has no appreciable affinity for cholinergic muscarinic receptors (IC 50>1000 nM). Aripiprazole functions as a partial agonist at the dopamine D 2 and the serotonin 5-HT 1A receptors, and as an antagonist at serotonin 5-HT 2A receptor.
ABILIFY activity is presumably primarily due to the parent drug, aripiprazole, and to a lesser extent, to its major metabolite, dehydro-aripiprazole, which has been shown to have affinities for D 2 receptors similar to the parent drug and represents 40% of the parent drug exposure in plasma. The mean elimination half-lives are about 75 hours and 94 hours for aripiprazole and dehydro-aripiprazole, respectively. Steady-state concentrations are attained within 14 days of dosing for both active moieties. Aripiprazole accumulation is predictable from single-dose pharmacokinetics. At steady-state, the pharmacokinetics of aripiprazole are dose-proportional. Elimination of aripiprazole is mainly through hepatic metabolism involving two P450 isozymes, CYP2D6 and CYP3A4.
Pharmacokinetic studies showed that ABILIFY DISCMELT Orally Disintegrating Tablets are bioequivalent to ABILIFY Tablets.
ORAL ADMINISTRATION
Absorption
Tablet: Aripiprazole is well absorbed after administration of the tablet, with peak plasma concentrations occurring within 3 hours to 5 hours; the absolute oral bioavailability of the tablet formulation is 87%. ABILIFY can be administered with or without food. Administration of a 15 mg ABILIFY Tablet with a standard high-fat meal did not significantly affect the Cmax or AUC of aripiprazole or its active metabolite, dehydro-aripiprazole, but delayed Tmax by 3 hours for aripiprazole and 12 hours for dehydro-aripiprazole.
Oral Solution: Aripiprazole is well absorbed when administered orally as the solution. At equivalent doses, the plasma concentrations of aripiprazole from the solution were higher than that from the tablet formulation. In a relative bioavailability study comparing the pharmacokinetics of 30 mg aripiprazole as the oral solution to 30 mg aripiprazole tablets in healthy subjects, the solution to tablet ratios of geometric mean Cmax and AUC values were 122% and 114%, respectively [see DOSAGE AND ADMINISTRATION (2.6)] . The single-dose pharmacokinetics of aripiprazole were linear and dose-proportional between the doses of 5 mg to 30 mg.
Distribution
The steady-state volume of distribution of aripiprazole following intravenous administration is high (404 L or 4.9 L/kg), indicating extensive extravascular distribution. At therapeutic concentrations, aripiprazole and its major metabolite are greater than 99% bound to serum proteins, primarily to albumin. In healthy human volunteers administered 0.5 mg/day to 30 mg/day aripiprazole for 14 days, there was dose-dependent D 2 receptor occupancy indicating brain penetration of aripiprazole in humans.
Metabolism and Elimination
Aripiprazole is metabolized primarily by three biotransformation pathways: dehydrogenation, hydroxylation, and N-dealkylation. Based on in vitro studies, CYP3A4 and CYP2D6 enzymes are responsible for dehydrogenation and hydroxylation of aripiprazole, and N-dealkylation is catalyzed by CYP3A4. Aripiprazole is the predominant drug moiety in the systemic circulation. At steady-state, dehydro-aripiprazole, the active metabolite, represents about 40% of aripiprazole AUC in plasma.
Approximately 8% of Caucasians and 3–8% of Black/African Americans lack the capacity to metabolize CYP2D6 substrates and are classified as poor metabolizers (PM), whereas the rest are extensive metabolizers (EM). PMs have about an 80% increase in aripiprazole exposure and about a 30% decrease in exposure to the active metabolite compared to EMs, resulting in about a 60% higher exposure to the total active moieties from a given dose of aripiprazole compared to EMs. Coadministration of ABILIFY with known inhibitors of CYP2D6, such as quinidine or fluoxetine in EMs, approximately doubles aripiprazole plasma exposure, and dose adjustment is needed [see DRUG INTERACTIONS (7.1)] . Similarly, PMs have higher exposure to aripiprazole compared to EMs; hence, PMs should have their initial dose reduced by one-half. Laboratory tests are available to identify CYP2D6 PMs. The mean elimination half-lives are about 75 hours and 146 hours for aripiprazole in EMs and PMs, respectively. Aripiprazole does not inhibit or induce the CYP2D6 pathway.
Following a single oral dose of [ 14C]-labeled aripiprazole, approximately 25% and 55% of the administered radioactivity was recovered in the urine and feces, respectively. Less than 1% of unchanged aripiprazole was excreted in the urine and approximately 18% of the oral dose was recovered unchanged in the feces.
INTRAMUSCULAR ADMINISTRATION
In two pharmacokinetic studies of aripiprazole injection administered intramuscularly to healthy subjects, the median times to the peak plasma concentrations were at 1 hour and 3 hours. A 5 mg intramuscular injection of aripiprazole had an absolute bioavailability of 100%. The geometric mean maximum concentration achieved after an intramuscular dose was on average 19% higher than the Cmax of the oral tablet. While the systemic exposure over 24 hours was generally similar between aripiprazole injection given intramuscularly and after oral tablet administration, the aripiprazole AUC in the first 2 hours after an intramuscular injection was 90% greater than the AUC after the same dose as a tablet. In stable patients with schizophrenia or schizoaffective disorder, the pharmacokinetics of aripiprazole after intramuscular administration were linear over a dose range of 1 mg to 45 mg. Although the metabolism of aripiprazole injection was not systematically evaluated, the intramuscular route of administration would not be expected to alter the metabolic pathways.
NONCLINICAL TOXICOLOGY
Carcinogenesis
Lifetime carcinogenicity studies were conducted in ICR mice and in Sprague-Dawley (SD) and F344 rats. Aripiprazole was administered for 2 years in the diet at doses of 1 mg/kg/day, 3 mg/kg/day, 10 mg/kg/day, and 30 mg/kg/day to ICR mice and 1 mg/kg/day, 3 mg/kg/day, and 10 mg/kg/day to F344 rats (0.2 times to 5 times and 0.3 times to 3 times the maximum recommended human dose [MRHD] based on mg/m 2, respectively). In addition, SD rats were dosed orally for 2 years at 10 mg/kg/day, 20 mg/kg/day, 40 mg/kg/day, and 60 mg/kg/day (3 times to 19 times the MRHD based on mg/m 2). Aripiprazole did not induce tumors in male mice or rats. In female mice, the incidences of pituitary gland adenomas and mammary gland adenocarcinomas and adenoacanthomas were increased at dietary doses of 3 mg/kg/day to 30 mg/kg/day (0.1 times to 0.9 times human exposure at MRHD based on AUC and 0.5 times to 5 times the MRHD based on mg/m 2). In female rats, the incidence of mammary gland fibroadenomas was increased at a dietary dose of 10 mg/kg/day (0.1 times human exposure at MRHD based on AUC and 3 times the MRHD based on mg/m 2); and the incidences of adrenocortical carcinomas and combined adrenocortical adenomas/carcinomas were increased at an oral dose of 60 mg/kg/day (14 times human exposure at MRHD based on AUC and 19 times the MRHD based on mg/m 2).
Proliferative changes in the pituitary and mammary gland of rodents have been observed following chronic administration of other antipsychotic agents and are considered prolactin-mediated. Serum prolactin was not measured in the aripiprazole carcinogenicity studies. However, increases in serum prolactin levels were observed in female mice in a 13-week dietary study at the doses associated with mammary gland and pituitary tumors. Serum prolactin was not increased in female rats in 4-week and 13-week dietary studies at the dose associated with mammary gland tumors. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unknown.
Mutagenesis
The mutagenic potential of aripiprazole was tested in the in vitro bacterial reverse-mutation assay, the in vitro bacterial DNA repair assay, the in vitro forward gene mutation assay in mouse lymphoma cells, the in vitro chromosomal aberration assay in Chinese hamster lung (CHL) cells, the in vivo micronucleus assay in mice, and the unscheduled DNA synthesis assay in rats. Aripiprazole and a metabolite (2,3-DCPP) were clastogenic in the in vitro chromosomal aberration assay in CHL cells with and without metabolic activation. The metabolite, 2,3-DCPP, produced increases in numerical aberrations in the in vitro assay in CHL cells in the absence of metabolic activation. A positive response was obtained in the in vivo micronucleus assay in mice; however, the response was due to a mechanism not considered relevant to humans.
Impairment of Fertility
Female rats were treated with oral doses of 2 mg/kg/day, 6 mg/kg/day, and 20 mg/kg/day (0.6 times, 2 times, and 6 times the maximum recommended human dose [MRHD] on a mg/m 2 basis) of aripiprazole from 2 weeks prior to mating through day 7 of gestation. Estrus cycle irregularities and increased corpora lutea were seen at all doses, but no impairment of fertility was seen. Increased pre-implantation loss was seen at 6 mg/kg and 20 mg/kg and decreased fetal weight was seen at 20 mg/kg.
Male rats were treated with oral doses of 20 mg/kg/day, 40 mg/kg/day, and 60 mg/kg/day (6 times, 13 times, and 19 times the MRHD on a mg/m 2 basis) of aripiprazole from 9 weeks prior to mating through mating. Disturbances in spermatogenesis were seen at 60 mg/kg and prostate atrophy was seen at 40 mg/kg and 60 mg/kg, but no impairment of fertility was seen.
Aripiprazole produced retinal degeneration in albino rats in a 26-week chronic toxicity study at a dose of 60 mg/kg and in a 2-year carcinogenicity study at doses of 40 mg/kg and 60 mg/kg. The 40 mg/kg and 60 mg/kg doses are 13 times and 19 times the maximum recommended human dose (MRHD) based on mg/m 2 and 7 times to 14 times human exposure at MRHD based on AUC. Evaluation of the retinas of albino mice and of monkeys did not reveal evidence of retinal degeneration. Additional studies to further evaluate the mechanism have not been performed. The relevance of this finding to human risk is unknown.
CLINICAL STUDIES
Adults
The efficacy of ABILIFY in the treatment of schizophrenia was evaluated in five short-term (4-week and 6-week), placebo-controlled trials of acutely relapsed inpatients who predominantly met DSM-III/IV criteria for schizophrenia. Four of the five trials were able to distinguish aripiprazole from placebo, but one study, the smallest, did not. Three of these studies also included an active control group consisting of either risperidone (one trial) or haloperidol (two trials), but they were not designed to allow for a comparison of ABILIFY and the active comparators.
In the four positive trials for ABILIFY, four primary measures were used for assessing psychiatric signs and symptoms. The Positive and Negative Syndrome Scale (PANSS) is a multi-item inventory of general psychopathology used to evaluate the effects of drug treatment in schizophrenia. The PANSS positive subscale is a subset of items in the PANSS that rates seven positive symptoms of schizophrenia (delusions, conceptual disorganization, hallucinatory behavior, excitement, grandiosity, suspiciousness/persecution, and hostility). The PANSS negative subscale is a subset of items in the PANSS that rates seven negative symptoms of schizophrenia (blunted affect, emotional withdrawal, poor rapport, passive apathetic withdrawal, difficulty in abstract thinking, lack of spontaneity/flow of conversation, stereotyped thinking). The Clinical Global Impression (CGI) assessment reflects the impression of a skilled observer, fully familiar with the manifestations of schizophrenia, about the overall clinical state of the patient.
In a 4-week trial (n=414) comparing two fixed doses of ABILIFY (15 mg/day or 30 mg/day) to placebo, both doses of ABILIFY were superior to placebo in the PANSS total score, PANSS positive subscale, and CGI-severity score. In addition, the 15 mg dose was superior to placebo in the PANSS negative subscale.
In a 4-week trial (n=404) comparing two fixed doses of ABILIFY (20 mg/day or 30 mg/day) to placebo, both doses of ABILIFY were superior to placebo in the PANSS total score, PANSS positive subscale, PANSS negative subscale, and CGI-severity score.
In a 6-week trial (n=420) comparing three fixed doses of ABILIFY (10 mg/day, 15 mg/day, or 20 mg/day) to placebo, all three doses of ABILIFY were superior to placebo in the PANSS total score, PANSS positive subscale, and the PANSS negative subscale.
In a 6-week trial (n=367) comparing three fixed doses of ABILIFY (2 mg/day, 5 mg/day, or 10 mg/day) to placebo, the 10 mg dose of ABILIFY was superior to placebo in the PANSS total score, the primary outcome measure of the study. The 2 mg and 5 mg doses did not demonstrate superiority to placebo on the primary outcome measure.
In a fifth study, a 4-week trial (n=103) comparing ABILIFY in a range of 5 mg/day to 30 mg/day to placebo, ABILIFY was only significantly different compared to placebo in a responder analysis based on the CGI-severity score, a primary outcome for that trial.
Thus, the efficacy of 10 mg, 15 mg, 20 mg, and 30 mg daily doses was established in two studies for each dose. Among these doses, there was no evidence that the higher dose groups offered any advantage over the lowest dose group of these studies.
An examination of population subgroups did not reveal any clear evidence of differential responsiveness on the basis of age, gender, or race.
A longer-term trial enrolled 310 inpatients or outpatients meeting DSM-IV criteria for schizophrenia who were, by history, symptomatically stable on other antipsychotic medications for periods of 3 months or longer. These patients were discontinued from their antipsychotic medications and randomized to ABILIFY 15 mg/day or placebo for up to 26 weeks of observation for relapse. Relapse during the double-blind phase was defined as CGI-Improvement score of ≥5 (minimally worse), scores ≥5 (moderately severe) on the hostility or uncooperativeness items of the PANSS, or ≥20% increase in the PANSS total score. Patients receiving ABILIFY 15 mg/day experienced a significantly longer time to relapse over the subsequent 26 weeks compared to those receiving placebo.
Pediatric Patients
The efficacy of ABILIFY (aripiprazole) in the treatment of schizophrenia in pediatric patients (13 to 17 years of age) was evaluated in one 6-week, placebo-controlled trial of outpatients who met DSM-IV criteria for schizophrenia and had a PANSS score ≥70 at baseline. In this trial (n=302) comparing two fixed doses of ABILIFY (10 mg/day or 30 mg/day) to placebo, ABILIFY was titrated starting from 2 mg/day to the target dose in 5 days in the 10 mg/day treatment arm and in 11 days in the 30 mg/day treatment arm. Both doses of ABILIFY were superior to placebo in the PANSS total score, the primary outcome measure of the study. The 30 mg/day dosage was not shown to be more efficacious than the 10 mg/day dose. Although maintenance efficacy in pediatric patients has not been systematically evaluated, maintenance efficacy can be extrapolated from adult data along with comparisons of aripiprazole pharmacokinetic parameters in adult and pediatric patients.
Acute Treatment of Manic and Mixed Episodes
Adults
Monotherapy
The efficacy of ABILIFY as monotherapy in the acute treatment of manic episodes was established in four 3-week, placebo-controlled trials in hospitalized patients who met the DSM-IV criteria for bipolar I disorder with manic or mixed episodes. These studies included patients with or without psychotic features and two of the studies also included patients with or without a rapid-cycling course.
The primary instrument used for assessing manic symptoms was the Young Mania Rating Scale (Y-MRS), an 11-item clinician-rated scale traditionally used to assess the degree of manic symptomatology (irritability, disruptive/aggressive behavior, sleep, elevated mood, speech, increased activity, sexual interest, language/thought disorder, thought content, appearance, and insight) in a range from 0 (no manic features) to 60 (maximum score). A key secondary instrument included the Clinical Global Impression-Bipolar (CGI-BP) Scale.
In the four positive, 3-week, placebo-controlled trials (n=268; n=248; n=480; n=485) which evaluated ABILIFY in a range of 15 mg to 30 mg, once daily (with a starting dose of 15 mg/day in two studies and 30 mg/day in two studies), ABILIFY was superior to placebo in the reduction of Y-MRS total score and CGI-BP Severity of Illness score (mania). In the two studies with a starting dose of 15 mg/day, 48% and 44% of patients were on 15 mg/day at endpoint. In the two studies with a starting dose of 30 mg/day, 86% and 85% of patients were on 30 mg/day at endpoint.
Adjunctive Therapy
The efficacy of adjunctive ABILIFY with concomitant lithium or valproate in the treatment of manic or mixed episodes was established in a 6-week, placebo-controlled study (n=384) with a 2-week lead-in mood stabilizer monotherapy phase in adult patients who met DSM-IV criteria for bipolar I disorder. This study included patients with manic or mixed episodes and with or without psychotic features.
Patients were initiated on open-label lithium (0.6 mEq/L to 1.0 mEq/L) or valproate (50 μg/mL to 125 μg/mL) at therapeutic serum levels, and remained on stable doses for 2 weeks. At the end of 2 weeks, patients demonstrating inadequate response (Y-MRS total score ≥16 and ≤25% improvement on the Y-MRS total score) to lithium or valproate were randomized to receive either aripiprazole (15 mg/day or an increase to 30 mg/day as early as day 7) or placebo as adjunctive therapy with open-label lithium or valproate. In the 6-week, placebo-controlled phase, adjunctive ABILIFY starting at 15 mg/day with concomitant lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.0 mEq/L or 50 μg/mL to 125 μg/mL, respectively) was superior to lithium or valproate with adjunctive placebo in the reduction of the Y-MRS total score and CGI-BP Severity of Illness score (mania). Seventy-one percent of the patients coadministered valproate and 62% of the patients coadministered lithium were on 15 mg/day at 6-week endpoint.
Pediatric Patients
The efficacy of ABILIFY in the treatment of bipolar I disorder in pediatric patients (10 to 17 years of age) was evaluated in one 4-week, placebo-controlled trial (n=296) of outpatients who met DSM-IV criteria for bipolar I disorder manic or mixed episodes with or without psychotic features and had a Y-MRS score ≥20 at baseline. This double-blind, placebo-controlled trial compared two fixed doses of ABILIFY (10 mg/day or 30 mg/day) to placebo. The ABILIFY dose was started at 2 mg/day, which was titrated to 5 mg/day after 2 days, and to the target dose in 5 days in the 10 mg/day treatment arm, and in 13 days in the 30 mg/day treatment arm. Both doses of ABILIFY were superior to placebo in change from baseline to week 4 on the Y-MRS total score.
Maintenance Treatment of Bipolar I Disorder
Monotherapy Maintenance Therapy
A maintenance trial was conducted in adult patients meeting DSM-IV criteria for bipolar I disorder with a recent manic or mixed episode who had been stabilized on open-label ABILIFY and who had maintained a clinical response for at least 6 weeks. The first phase of this trial was an open-label stabilization period in which inpatients and outpatients were clinically stabilized and then maintained on open-label ABILIFY (15 mg/day or 30 mg/day, with a starting dose of 30 mg/day) for at least 6 consecutive weeks. One hundred sixty-one outpatients were then randomized in a double-blind fashion, to either the same dose of ABILIFY they were on at the end of the stabilization and maintenance period or placebo and were then monitored for manic or depressive relapse. During the randomization phase, ABILIFY was superior to placebo on time to the number of combined affective relapses (manic plus depressive), the primary outcome measure for this study. A total of 55 mood events were observed during the double-blind treatment phase. Nineteen were from the ABILIFY group and 36 were from the placebo group. The number of observed manic episodes in the ABILIFY group (6) were fewer than that in the placebo group (19), while the number of depressive episodes in the ABILIFY group (9) was similar to that in the placebo group (11).
An examination of population subgroups did not reveal any clear evidence of differential responsiveness on the basis of age and gender; however, there were insufficient numbers of patients in each of the ethnic groups to adequately assess inter-group differences.
Adjunctive Maintenance Therapy
An adjunctive maintenance trial was conducted in adult patients meeting DSM-IV criteria for bipolar I disorder with a recent manic or mixed episode. Patients were initiated on open-label lithium (0.6 mEq/L to 1.0 mEq/L) or valproate (50 μg/mL to 125 μg/mL) at therapeutic serum levels, and remained on stable doses for 2 weeks. At the end of 2 weeks, patients demonstrating inadequate response (Y-MRS total score ≥16 and ≤35% improvement on the Y-MRS total score) to lithium or valproate received aripiprazole with a starting dose of 15 mg/day with the option to increase to 30 mg or reduce to 10 mg as early as day 4, as adjunctive therapy with open-label lithium or valproate. Prior to randomization, patients on the combination of single-blind aripiprazole and lithium or valproate were required to maintain stability (Y-MRS and MADRS total scores ≤12) for 12 consecutive weeks. Three hundred thirty-seven patients were then randomized in a double-blind fashion, to either the same dose of ABILIFY they were on at the end of the stabilization period or placebo plus lithium or valproate and were then monitored for manic, mixed, or depressive relapse for a maximum of 52 weeks. ABILIFY was superior to placebo on the primary endpoint, time from randomization to relapse to any mood event. A mood event was defined as hospitalization for a manic, mixed, or depressive episode, study discontinuation due to lack of efficacy accompanied by Y-MRS score >16 and/or a MADRS >16, or an SAE of worsening disease accompanied by Y-MRS score >16 and/or a MADRS >16. A total of 68 mood events were observed during the double-blind treatment phase. Twenty-five were from the ABILIFY group and 43 were from the placebo group. The number of observed manic episodes in the ABILIFY group (7) were fewer than that in the placebo group (19), while the number of depressive episodes in the ABILIFY group (14) was similar to that in the placebo group (18). The Kaplan-Meier curves of the time from randomization to relapse to any mood event during the 52-week, double-blind treatment phase for ABILIFY and placebo groups are shown in Figure 1.
Figure 1: Kaplan-Meier Estimation of Proportion of Relapses to Any Mood Event for ABILIFY and Placebo Groups
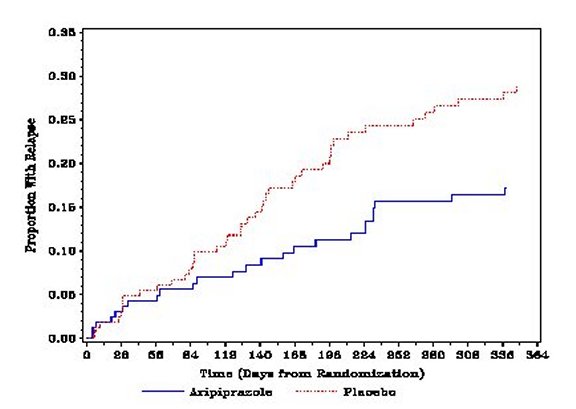
An examination of population subgroups did not reveal any clear evidence of differential responsiveness on the basis of age and gender; however, there were insufficient numbers of patients in each of the ethnic groups to adequately assess inter-group differences.
Adults
The efficacy of ABILIFY (aripiprazole) in the adjunctive treatment of major depressive disorder (MDD) was demonstrated in two short-term (6-week), placebo-controlled trials of adult patients meeting DSM-IV criteria for MDD who had had an inadequate response to prior antidepressant therapy (1 to 3 courses) in the current episode and who had also demonstrated an inadequate response to 8 weeks of prospective antidepressant therapy (paroxetine controlled-release, venlafaxine extended-release, fluoxetine, escitalopram, or sertraline). Inadequate response for prospective treatment was defined as less than 50% improvement on the 17-item version of the Hamilton Depression Rating Scale (HAMD17), minimal HAMD17 score of 14, and a Clinical Global Impressions Improvement rating of no better than minimal improvement. Inadequate response to prior treatment was defined as less than 50% improvement as perceived by the patient after a minimum of 6 weeks of antidepressant therapy at or above the minimal effective dose.
The primary instrument used for assessing depressive symptoms was the Montgomery-Asberg Depression Rating Scale (MADRS), a 10-item clinician-rated scale used to assess the degree of depressive symptomatology (apparent sadness, reported sadness, inner tension, reduced sleep, reduced appetite, concentration difficulties, lassitude, inability to feel, pessimistic thoughts, and suicidal thoughts). The key secondary instrument was the Sheehan Disability Scale (SDS), a 3-item self-rated instrument used to assess the impact of depression on three domains of functioning (work/school, social life, and family life) with each item scored from 0 (not at all) to 10 (extreme).
In the two trials (n=381, n=362), ABILIFY was superior to placebo in reducing mean MADRS total scores. In one study, ABILIFY was also superior to placebo in reducing the mean SDS score.
In both trials, patients received ABILIFY adjunctive to antidepressants at a dose of 5 mg/day. Based on tolerability and efficacy, doses could be adjusted by 5 mg increments, one week apart. Allowable doses were: 2 mg/day, 5 mg/day, 10 mg/day, 15 mg/day, and for patients who were not on potent CYP2D6 inhibitors fluoxetine and paroxetine, 20 mg/day. The mean final dose at the end point for the two trials was 10.7 mg/day and 11.4 mg/day.
An examination of population subgroups did not reveal evidence of differential response based on age, choice of prospective antidepressant, or race. With regard to gender, a smaller mean reduction on the MADRS total score was seen in males than in females.
Pediatric Patients
The efficacy of ABILIFY (aripiprazole) in the treatment of irritability associated with autistic disorder was established in two 8-week, placebo-controlled trials in pediatric patients (6 to 17 years of age) who met the DSM-IV criteria for autistic disorder and demonstrated behaviors such as tantrums, aggression, self-injurious behavior, or a combination of these problems. Over 75% of these subjects were under 13 years of age.
Efficacy was evaluated using two assessment scales: the Aberrant Behavior Checklist (ABC) and the Clinical Global Impression-Improvement (CGI-I) scale. The primary outcome measure in both trials was the change from baseline to endpoint in the Irritability subscale of the ABC (ABC-I). The ABC-I subscale measured the emotional and behavioral symptoms of irritability in autistic disorder, including aggression towards others, deliberate self-injuriousness, temper tantrums, and quickly changing moods.
The results of these trials are as follows:
In one of the 8-week, placebo-controlled trials, children and adolescents with autistic disorder (n=98), aged 6 to 17 years, received daily doses of placebo or ABILIFY 2 mg/day to 15 mg/day. ABILIFY, starting at 2 mg/day with increases allowed up to 15 mg/day based on clinical response, significantly improved scores on the ABC-I subscale and on the CGI-I scale compared with placebo. The mean daily dose of ABILIFY at the end of 8-week treatment was 8.6 mg/day.
In the other 8-week, placebo-controlled trial in children and adolescents with autistic disorder (n=218), aged 6 to 17 years, three fixed doses of ABILIFY (5 mg/day, 10 mg/day, or 15 mg/day) were compared to placebo. ABILIFY dosing started at 2 mg/day and was increased to 5 mg/day after one week. After a second week, it was increased to 10 mg/day for patients in the 10 mg and 15 mg dose arms, and after a third week, it was increased to 15 mg/day in the 15 mg/day treatment arm. All three doses of ABILIFY significantly improved scores on the ABC-I subscale compared with placebo.
The efficacy of intramuscular aripiprazole for injection for the treatment of agitation was established in three short-term (24-hour), placebo-controlled trials in agitated inpatients from two diagnostic groups: schizophrenia and bipolar I disorder (manic or mixed episodes, with or without psychotic features). Each of the trials included a single active comparator treatment arm of either haloperidol injection (schizophrenia studies) or lorazepam injection (bipolar mania study). Patients could receive up to three injections during the 24-hour treatment periods; however, patients could not receive the second injection until after the initial 2-hour period when the primary efficacy measure was assessed. Patients enrolled in the trials needed to be: (1) judged by the clinical investigators as clinically agitated and clinically appropriate candidates for treatment with intramuscular medication, and (2) exhibiting a level of agitation that met or exceeded a threshold score of ≥15 on the five items comprising the Positive and Negative Syndrome Scale (PANSS) Excited Component (ie, poor impulse control, tension, hostility, uncooperativeness, and excitement items) with at least two individual item scores ≥4 using a 1-7 scoring system (1 = absent, 4 = moderate, 7 = extreme). In the studies, the mean baseline PANSS Excited Component score was 19, with scores ranging from 15 to 34 (out of a maximum score of 35), thus suggesting predominantly moderate levels of agitation with some patients experiencing mild or severe levels of agitation. The primary efficacy measure used for assessing agitation signs and symptoms in these trials was the change from baseline in the PANSS Excited Component at 2 hours post-injection. A key secondary measure was the Clinical Global Impression of Improvement (CGI-I) Scale. The results of the trials follow:
In a placebo-controlled trial in agitated inpatients predominantly meeting DSM-IV criteria for schizophrenia (n=350), four fixed aripiprazole injection doses of 1 mg, 5.25 mg, 9.75 mg, and 15 mg were evaluated. At 2 hours post-injection, the 5.25 mg, 9.75 mg, and 15 mg doses were statistically superior to placebo in the PANSS Excited Component and on the CGI-I Scale.
In a second placebo-controlled trial in agitated inpatients predominantly meeting DSM-IV criteria for schizophrenia (n=445), one fixed aripiprazole injection dose of 9.75 mg was evaluated. At 2 hours post-injection, aripiprazole for injection was statistically superior to placebo in the PANSS Excited Component and on the CGI-I Scale.
In a placebo-controlled trial in agitated inpatients meeting DSM-IV criteria for bipolar I disorder (manic or mixed) (n=291), two fixed aripiprazole injection doses of 9.75 mg and 15 mg were evaluated. At 2 hours post-injection, both doses were statistically superior to placebo in the PANSS Excited Component.
Examination of population subsets (age, race, and gender) did not reveal any differential responsiveness on the basis of these subgroupings.
HOW SUPPLIED
ABILIFY ® (aripiprazole) Tablets have markings on one side and are available in the strengths and packages listed in Table 22.
| Tablet
Strength | Tablet
Color/Shape | Tablet
Markings | Pack
Size | NDC
Code |
|---|---|---|---|---|
| 2 mg | green
modified rectangle | “A-006”
and “2” | Bottle of 30
| 59148-006-13
|
| 5 mg | blue
modified rectangle | “A-007”
and “5” | Bottle of 30
Blister of 100 | 59148-007-13
59148-007-35 |
| 10 mg | pink
modified rectangle | “A-008”
and “10” | Bottle of 30
Blister of 100 | 59148-008-13
59148-008-35 |
| 15 mg | yellow
round | “A-009”
and “15” | Bottle of 30
Blister of 100 | 59148-009-13
59148-009-35 |
| 20 mg | white
round | “A-010”
and “20” | Bottle of 30
Blister of 100 | 59148-010-13
59148-010-35 |
| 30 mg | pink
round | “A-011”
and “30” | Bottle of 30
Blister of 100 | 59148-011-13
59148-011-35 |
ABILIFY DISCMELT ® (aripiprazole) Orally Disintegrating Tablets are round tablets with markings on either side. ABILIFY DISCMELT is available in the strengths and packages listed in Table 23.
| Tablet
Strength | Tablet
Color | Tablet
Markings | Pack
Size | NDC
Code |
|---|---|---|---|---|
| 10 mg | pink (with
scattered specks) | “A” and “640”
“10” | Blister of 30 | 59148-640-23 |
| 15 mg | yellow (with
scattered specks) | “A” and “641”
“15” | Blister of 30 | 59148-641-23 |
ABILIFY ® (aripiprazole) Oral Solution (1 mg/mL) is supplied in child-resistant bottles along with a calibrated oral dosing cup. ABILIFY Oral Solution is available as follows:
150 mL bottle NDC 59148-013-15
ABILIFY ® (aripiprazole) Injection for intramuscular use is available as a ready-to-use, 9.75 mg/1.3 mL (7.5 mg/mL) solution in clear, Type 1 glass vials as follows:
9.75 mg/1.3 mL single-dose vial NDC 59148-016-65
Tablets
Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
Oral Solution
Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature]. Opened bottles of ABILIFY Oral Solution can be used for up to 6 months after opening, but not beyond the expiration date on the bottle. The bottle and its contents should be discarded after the expiration date.
Injection
Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature]. Protect from light by storing in the original container. Retain in carton until time of use.
INFORMATION FOR PATIENTS
See Medication Guide
Physicians are advised to discuss the following issues with patients for whom they prescribe ABILIFY:
Increased Mortality in Elderly Patients with Dementia-Related Psychosis
Patients and caregivers should be advised that elderly patients with dementia-related psychoses treated with antipsychotic drugs are at increased risk of death. ABILIFY is not approved for elderly patients with dementia-related psychosis [see WARNINGS AND PRECAUTIONS (5.1)] .
Clinical Worsening of Depression and Suicide Risk
Patients, their families, and their caregivers should be encouraged to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Families and caregivers of patients should be advised to look for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient’s prescriber or health professional, especially if they are severe, abrupt in onset, or were not part of the patient’s presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication [see WARNINGS AND PRECAUTIONS (5.2)] .
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with ABILIFY and should counsel them in its appropriate use. A patient Medication Guide including information about “Antidepressant Medicines, Depression and other Serious Mental Illness, and Suicidal Thoughts or Actions” is available for ABILIFY. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. It should be noted that ABILIFY is not approved as a single agent for treatment of depression and has not been evaluated in pediatric major depressive disorder.
Use of Orally Disintegrating Tablet
Do not open the blister until ready to administer. For single tablet removal, open the package and peel back the foil on the blister to expose the tablet. Do not push the tablet through the foil because this could damage the tablet. Immediately upon opening the blister, using dry hands, remove the tablet and place the entire ABILIFY DISCMELT Orally Disintegrating Tablet on the tongue. Tablet disintegration occurs rapidly in saliva. It is recommended that ABILIFY DISCMELT be taken without liquid. However, if needed, it can be taken with liquid. Do not attempt to split the tablet.
Interference with Cognitive and Motor Performance
Because aripiprazole may have the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that aripiprazole therapy does not affect them adversely [see WARNINGS AND PRECAUTIONS (5.9)] .
Pregnancy
Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during therapy with ABILIFY [see USE IN SPECIFIC POPULATIONS (8.1)] .
Nursing
Patients should be advised not to breast-feed an infant if they are taking ABILIFY [see USE IN SPECIFIC POPULATIONS (8.3)] .
Concomitant Medication
Patients should be advised to inform their physicians if they are taking, or plan to take, any prescription or over-the-counter drugs, since there is a potential for interactions [see DRUG INTERACTIONS (7)] .
Alcohol
Patients should be advised to avoid alcohol while taking ABILIFY [see DRUG INTERACTIONS (7.2)] .
Heat Exposure and Dehydration
Patients should be advised regarding appropriate care in avoiding overheating and dehydration [see WARNINGS AND PRECAUTIONS (5.10)] .
Sugar Content
Patients should be advised that each mL of ABILIFY Oral Solution contains 400 mg of sucrose and 200 mg of fructose.
Phenylketonurics
Phenylalanine is a component of aspartame. Each ABILIFY DISCMELT Orally Disintegrating Tablet contains the following amounts: 10 mg - 1.12 mg phenylalanine and 15 mg - 1.68 mg phenylalanine.
Tablets manufactured by Otsuka Pharmaceutical Co, Ltd, Tokyo, 101-8535 Japan or Bristol-Myers Squibb Company, Princeton, NJ 08543 USA
Orally Disintegrating Tablets, Oral Solution, and Injection manufactured by
Bristol-Myers Squibb Company, Princeton, NJ 08543 USA
Distributed and marketed by Otsuka America Pharmaceutical, Inc, Rockville, MD 20850 USA
Marketed by Bristol-Myers Squibb Company, Princeton, NJ 08543 USA
ABILIFY is a trademark of Otsuka Pharmaceutical Company.
1239550B2 03US12L-0104 Rev February 2012
© 2012, Otsuka Pharmaceutical Co, Ltd, Tokyo, 101-8535 Japan
SPL MEDGUIDE
MEDICATION GUIDE
ABILIFY® (a BIL ĭ fī)
Generic name: aripiprazole
Read this Medication Guide before you start taking ABILIFY and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about ABILIFY?
(For other side effects, also see “ What are the possible side effects of ABILIFY?”)
Serious side effects may happen when you take ABILIFY, including:
- Increased risk of death in elderly patients with dementia-related psychosis: Medicines like ABILIFY can raise the risk of death in elderly people who have lost touch with reality (psychosis) due to confusion and memory loss (dementia). ABILIFY is not approved for the treatment of patients with dementia-related psychosis.
Risk of suicidal thoughts or actions: Antidepressant medicines, depression and other serious mental illnesses, and suicidal thoughts or actions:
- Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment.
- Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions. These include people who have (or have a family history of) bipolar illness (also called manic-depressive illness) or suicidal thoughts or actions.
-
How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
- Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed.
- Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings.
- Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling very agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
What else do I need to know about antidepressant medicines?
- Never stop an antidepressant medicine without first talking to a healthcare provider. Stopping an antidepressant medicine suddenly can cause other symptoms.
- Antidepressants are medicines used to treat depression and other illnesses. It is important to discuss all the risks of treating depression and also the risks of not treating it. Patients and their families or other caregivers should discuss all treatment choices with the healthcare provider, not just the use of antidepressants.
- Antidepressant medicines have other side effects. Talk to the healthcare provider about the side effects of the medicine prescribed for you or your family member.
- Antidepressant medicines can interact with other medicines. Know all of the medicines that you or your family member takes. Keep a list of all medicines to show the healthcare provider. Do not start new medicines without first checking with your healthcare provider.
- Not all antidepressant medicines prescribed for children are FDA approved for use in children. Talk to your child’s healthcare provider for more information.
What is ABILIFY?
ABILIFY is a prescription medicine used to treat:
- schizophrenia in people age 13 years and older
- bipolar I disorder in people age 10 years and older, including:
- manic or mixed episodes that happen with bipolar I disorder
- manic or mixed episodes that happen with bipolar I disorder, when used with the medicine lithium or valproate
- long-term treatment of bipolar I disorder
- major depressive disorder in adults, as an add-on treatment to an antidepressant medicine when you do not get better with an antidepressant alone
- irritability associated with autistic disorder in children and adolescents ages 6 to 17 years old
- agitation associated with schizophrenia or bipolar disorder
The symptoms of schizophrenia include:
- losing touch with reality (psychosis)
- seeing things or hearing voices that are not there (hallucinations)
- believing things that are not true (delusions)
- being suspicious (paranoia)
- disorganized speech and thinking
- bizarre behavior
The symptoms of bipolar I disorder include:
- extreme mood swings that include feeling depressed and high or irritable mood
- talking too fast and too much
- impulsive behavior
- having more energy and restlessness than usual
- needing less sleep than usual
The symptoms of major depressive disorder (MDD) include:
- feeling of sadness and emptiness
- loss of interest in activities that you once enjoyed and loss of energy
- problems focusing and making decisions
- feeling of worthlessness or guilt
- changes in sleep or eating patterns
- thoughts of death or suicide
The symptoms of irritability associated with autistic disorder include:
- aggressive behavior towards others
- intentionally trying to harm oneself
- temper tantrums
- quickly changing moods
The symptoms of agitation associated with schizophrenia or bipolar disorder include:
- hostility or aggressive behavior
- agitation and inner tension
- self-exhausting behavior
What should I tell my healthcare provider before taking ABILIFY?
Before taking ABILIFY, tell your healthcare provider if you have or had:
- diabetes or high blood sugar in you or your family; your healthcare provider should check your blood sugar before you start ABILIFY and also during therapy.
- seizures (convulsions).
- low or high blood pressure.
- heart problems or stroke.
- pregnancy or plans to become pregnant. It is not known if ABILIFY will harm your unborn baby.
- breast-feeding or plans to breast-feed. It is not known if ABILIFY will pass into your breast milk. You and your healthcare provider should decide if you will take ABILIFY or breast-feed. You should not do both.
- low white blood cell count.
- phenylketonuria. ABILIFY DISCMELT Orally Disintegrating Tablets contain phenylalanine.
- any other medical conditions.
Tell your healthcare provider about all the medicines that you take or recently have taken, including prescription medicines, non-prescription medicines, herbal supplements, and vitamins.
ABILIFY and other medicines may affect each other causing possible serious side effects. ABILIFY may affect the way other medicines work, and other medicines may affect how ABILIFY works.
Your healthcare provider can tell you if it is safe to take ABILIFY with your other medicines. Do not start or stop any medicines while taking ABILIFY without talking to your healthcare provider first. Know the medicines you take. Keep a list of your medicines to show your healthcare provider and pharmacist when you get a new medicine.
How should I take ABILIFY?
- Take ABILIFY exactly as your healthcare provider tells you to take it. Do not change the dose or stop taking ABILIFY yourself.
- ABILIFY can be taken with or without food.
- ABILIFY tablets should be swallowed whole.
- If you miss a dose of ABILIFY, take the missed dose as soon as you remember. If it is almost time for the next dose, just skip the missed dose and take your next dose at the regular time. Do not take two doses of ABILIFY at the same time.
- If you have been prescribed ABILIFY DISCMELT, take it as follows:
- Do not open the blister until ready to take the DISCMELT tablet.
- To remove one DISCMELT tablet, open the package and peel back the foil on the blister to expose the tablet.
- Do not push the tablet through the foil because this could damage the tablet.
- Immediately upon opening the blister, using dry hands, remove the tablet and place the entire ABILIFY DISCMELT Orally Disintegrating Tablet on the tongue.
- Tablet disintegration occurs rapidly in saliva. It is recommended that ABILIFY DISCMELT be taken without liquid. However, if needed, it can be taken with liquid.
- Do not attempt to split the DISCMELT tablet.
If you take too much ABILIFY, call your healthcare provider or poison control center at 1-800-222-1222 right away, or go to the nearest hospital emergency room.
What should I avoid while taking ABILIFY?
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how ABILIFY affects you. ABILIFY may make you drowsy.
- Do not drink alcohol while taking ABILIFY.
- Avoid getting over-heated or dehydrated.
- Do not over-exercise.
- In hot weather, stay inside in a cool place if possible.
- Stay out of the sun. Do not wear too much or heavy clothing.
- Drink plenty of water.
What are the possible side effects of ABILIFY?
Serious side effects have been reported with ABILIFY including:
Also see “What is the most important information I should know about ABILIFY?” at the beginning of this Medication Guide.
- Neuroleptic malignant syndrome (NMS): Tell your healthcare provider right away if you have some or all of the following symptoms: high fever, stiff muscles, confusion, sweating, changes in pulse, heart rate, and blood pressure. These may be symptoms of a rare and serious condition that can lead to death. Call your healthcare provider right away if you have any of these symptoms.
-
High blood sugar (hyperglycemia): Increases in blood sugar can happen in some people who take ABILIFY. Extremely high blood sugar can lead to coma or death. If you have diabetes or risk factors for diabetes (such as being overweight or a family history of diabetes), your healthcare provider should check your blood sugar before you start ABILIFY and during therapy.
Call your healthcare provider if you have any of these symptoms of high blood sugar while taking ABILIFY:- feel very thirsty
- need to urinate more than usual
- feel very hungry
- feel weak or tired
- feel sick to your stomach
- feel confused, or your breath smells fruity
- Increase in weight: Weight gain has been reported in patients taking medicines like ABILIFY, so you and your healthcare provider should check your weight regularly. For children and adolescent patients (6 to 17 years of age) weight gain should be compared against that expected with normal growth.
- Difficulty swallowing: may lead to aspiration and choking.
- Tardive dyskinesia: Call your healthcare provider about any movements you cannot control in your face, tongue, or other body parts. These may be signs of a serious condition. Tardive dyskinesia may not go away, even if you stop taking ABILIFY. Tardive dyskinesia may also start after you stop taking ABILIFY.
- Orthostatic hypotension (decreased blood pressure): lightheadedness or fainting when rising too quickly from a sitting or lying position.
- Low white blood cell count
- Seizures (convulsions)
Common side effects with ABILIFY in adults include:
| • nausea | • inner sense of restlessness/need to move (akathisia) |
| • vomiting | • anxiety |
| • constipation | • insomnia |
| • headache | • restlessness |
| • dizziness |
Common side effects with ABILIFY in children include:
| • feeling sleepy | • insomnia |
| • headache | • nausea |
| • vomiting | • stuffy nose |
| • fatigue | • weight gain |
| • increased appetite | • uncontrolled movement such as restlessness, tremor, muscle stiffness |
These are not all the possible side effects of ABILIFY. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ABILIFY?
- Store ABILIFY at room temperature, between 59°F to 86°F (15°C to 30°C).
- Opened bottles of ABILIFY Oral Solution can be used for up to 6 months after opening, but not beyond the expiration date on the bottle.
Keep ABILIFY and all medicines out of the reach of children.
General information about ABILIFY
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ABILIFY for a condition for which it was not prescribed. Do not give ABILIFY to other people, even if they have the same condition. It may harm them.
This Medication Guide summarizes the most important information about ABILIFY. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about ABILIFY that was written for healthcare professionals. For more information about ABILIFY visit www.abilify.com.
What are the ingredients in ABILIFY?
Active ingredient: aripiprazole
Inactive ingredients:
Tablets: cornstarch, hydroxypropyl, cellulose, lactose monohydrate, magnesium stearate, and microcrystalline cellulose. Colorants include ferric oxide (yellow or red) and FD&C Blue No. 2 Aluminum Lake.
ABILIFY DISCMELT Orally Disintegrating Tablets: acesulfame potassium, aspartame (which contains phenylalanine), calcium silicate, croscarmellose sodium, crospovidone, crème de vanilla (natural and artificial flavors), magnesium stearate, microcrystalline cellulose, silicon dioxide, tartaric acid, and xylitol. Colorants include ferric oxide (yellow or red) and FD&C Blue No. 2 Aluminum Lake.
ABILIFY Oral Solution: disodium edetate, fructose (200 mg per mL), glycerin, dl-lactic acid, methylparaben, propylene glycol, propylparaben, sodium hydroxide, sucrose (400 mg per mL), and purified water. The oral solution is flavored with natural orange cream and other natural flavors.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
ABILIFY is a trademark of Otsuka Pharmaceutical Company.
1239550B2 03US12L-0104C Rev February 2012
© 2012, Otsuka Pharmaceutical Co, Ltd, Tokyo, 101-8535 Japan
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
DRUG: ABILIFY
GENERIC: ARIPIPRAZOLE
DOSAGE: TABLET
ADMINSTRATION: ORAL
NDC: 24236-837-35
ACTIVE INGREDIENT(S):
- ARIPIPRAZOLE 5mg in 1
INACTIVE INGREDIENT(S):
- ALUMINUM OXIDE
- FERRIC OXIDE YELLOW
- FD&C BLUE NO. 2
- FERRIC OXIDE RED
- CELLULOSE, MICROCRYSTALLINE
- HYDROXYPROPYL CELLULOSE
- LACTOSE MONOHYDRATE
- MAGNESIUM STEARATE
- STARCH, CORN
COLOR: blue
SHAPE: RECTANGLE
SCORE: No score
SIZE: 8 mm
IMPRINT: A;007;5
PACKAGING: 30 in 1 CANISTER
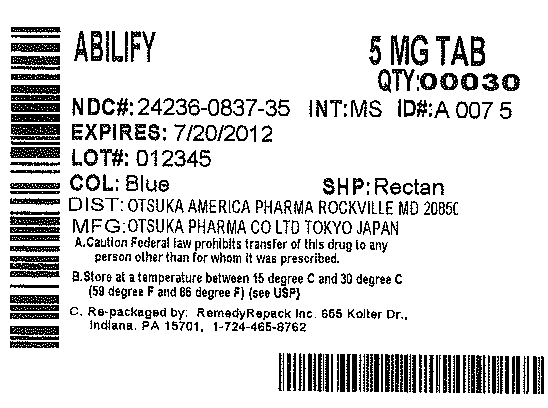

| ABILIFY
aripiprazole tablet |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| Labeler - REMEDYREPACK INC. (829572556) |