Label: GABAPENTIN tablet, film coated
-
Contains inactivated NDC Code(s)
NDC Code(s): 61919-104-30, 61919-104-60, 61919-104-90 - Packager: DIRECT RX
- This is a repackaged label.
- Source NDC Code(s): 68382-205
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated November 4, 2015
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
DESCRIPTION SECTION
Gabapentin is described as 1-(aminomethyl)cyclohexaneacetic acid with a molecular formula of C9H17NO2 and a molecular weight of 171.24. The structural formula of gabapentin is:
Gabapentin, USP is a white to off-white powder with a pKa1 of 3.7 and a pKa2 of 10.7. It is freely soluble in water, 0.1 N hydrochloric acid, 0.1 N sodium hydroxide and glacial acetic acid; slightly soluble in methanol, very slightly soluble in ethanol, 2-propanol; insoluble in toluene. The log of the partition coefficient (n-octanol/0.05M phosphate buffer) at pH 7.4 is –1.25.
Each gabapentin tablet, USP intended for oral administration contains 600 mg and 800 mg of gabapentin. In addition each tablet contains following inactive ingredients: copovidone, low substituted hydroxypropyl cellulose, magnesium stearate, mannitol, poloxamer, povidone and talc.
-
CLINICAL PHARMACOLOGY SECTION
Mechanism of Action
The mechanism by which gabapentin exerts its analgesic action is unknown, but in animal models of analgesia, gabapentin prevents allodynia (pain-related behavior in response to a normally innocuous stimulus) and hyperalgesia (exaggerated response to painful stimuli). In particular, gabapentin prevents pain-related responses in several models of neuropathic pain in rats or mice (e.g., spinal nerve ligation models, streptozocin-induced diabetes model, spinal cord injury model, acute herpes zoster infection model). Gabapentin also decreases pain-related responses after peripheral inflammation (carrageenan footpad test, late phase of formalin test). Gabapentin did not alter immediate pain-related behaviors (rat tail flick test, formalin footpad acute phase, acetic acid abdominal constriction test, footpad heat irradiation test). The relevance of these models to human pain is not known.
The mechanism by which gabapentin exerts its anticonvulsant action is unknown, but in animal test systems designed to detect anticonvulsant activity, gabapentin prevents seizures as do other marketed anticonvulsants. Gabapentin exhibits antiseizure activity in mice and rats in both the maximal electroshock and pentylenetetrazole seizure models and other preclinical models (e.g., strains with genetic epilepsy, etc.). The relevance of these models to human epilepsy is not known.
Gabapentin is structurally related to the neurotransmitter GABA (gamma-aminobutyric acid) but it does not modify GABAA or GABAB radioligand binding, it is not converted metabolically into GABA or a GABA agonist, and it is not an inhibitor of GABA uptake or degradation. Gabapentin was tested in radioligand binding assays at concentrations up to 100 µM and did not exhibit affinity for a number of other common receptor sites, including benzodiazepine, glutamate, N-methyl-D-aspartate (NMDA), quisqualate, kainate, strychnine-insensitive or strychnine-sensitive glycine, alpha 1, alpha 2, or beta adrenergic, adenosine A1 or A2, cholinergic muscarinic or nicotinic, dopamine D1 or D2, histamine H1, serotonin S1 or S2, opiate mu, delta or kappa, cannabinoid 1, voltage-sensitive calcium channel sites labeled with nitrendipine or diltiazem, or at voltage-sensitive sodium channel sites labeled with batrachotoxinin A 20-alpha-benzoate. Furthermore, gabapentin did not alter the cellular uptake of dopamine, noradrenaline, or serotonin.
In vitro studies with radiolabeled gabapentin have revealed a gabapentin binding site in areas of rat brain including neocortex and hippocampus. A high-affinity binding protein in animal brain tissue has been identified as an auxiliary subunit of voltage-activated calcium channels. However, functional correlates of gabapentin binding, if any, remain to be elucidated.
Pharmacokinetics and Drug Metabolism
All pharmacological actions following gabapentin administration are due to the activity of the parent compound; gabapentin is not appreciably metabolized in humans.
Oral Bioavailability
Gabapentin bioavailability is not dose proportional; i.e., as dose is increased, bioavailability decreases. Bioavailability of gabapentin is approximately 60%, 47%, 34%, 33%, and 27% following 900, 1200, 2400, 3600, and 4800 mg/day given in 3 divided doses, respectively. Food has only a slight effect on the rate and extent of absorption of gabapentin (14% increase in AUC and Cmax).
Distribution
Less than 3% of gabapentin circulates bound to plasma protein. The apparent volume of distribution of gabapentin after 150 mg intravenous administration is 58±6 L (Mean ±SD). In patients with epilepsy, steady-state predose (Cmin) concentrations of gabapentin in cerebrospinal fluid were approximately 20% of the corresponding plasma concentrations.
Elimination
Gabapentin is eliminated from the systemic circulation by renal excretion as unchanged drug. Gabapentin is not appreciably metabolized in humans.
Gabapentin elimination half-life is 5 to 7 hours and is unaltered by dose or following multiple dosing. Gabapentin elimination rate constant, plasma clearance, and renal clearance are directly proportional to creatinine clearance (see CLINICAL PHARMACOLOGY, Special Populations: Adult Patients With Renal Insufficiency, below). In elderly patients, and in patients with impaired renal function, gabapentin plasma clearance is reduced. Gabapentin can be removed from plasma by hemodialysis.
Dosage adjustment in patients with compromised renal function or undergoing hemodialysis is recommended (see DOSAGE AND ADMINISTRATION, Table 6).
Special PopulationsAdult Patients With Renal Insufficiency
Subjects (N=60) with renal insufficiency (mean creatinine clearance ranging from 13-114 mL/min) were administered single 400 mg oral doses of gabapentin. The mean gabapentin half- life ranged from about 6.5 hours (patients with creatinine clearance >60 mL/min) to 52 hours (creatinine clearance <30 mL/min) and gabapentin renal clearance from about 90 mL/min (>60 mL/min group) to about 10 mL/min (<30 mL/min). Mean plasma clearance (CL/F) decreased from approximately 190 mL/min to 20 mL/min.
Dosage adjustment in adult patients with compromised renal function is necessary (see DOSAGE AND ADMINISTRATION). Pediatric patients with renal insufficiency have not been studied.
Hemodialysis
In a study in anuric adult subjects (N=11), the apparent elimination half-life of gabapentin on nondialysis days was about 132 hours; during dialysis the apparent half-life of gabapentin was reduced to 3.8 hours. Hemodialysis thus has a significant effect on gabapentin elimination in anuric subjects.
Dosage adjustment in patients undergoing hemodialysis is necessary (see DOSAGE AND ADMINISTRATION).
Hepatic Disease
Because gabapentin is not metabolized, no study was performed in patients with hepatic impairment.
Age
The effect of age was studied in subjects 20-80 years of age. Apparent oral clearance (CL/F) of gabapentin decreased as age increased, from about 225 mL/min in those under 30 years of age to about 125 mL/min in those over 70 years of age. Renal clearance (CLr) and CLr adjusted for body surface area also declined with age; however, the decline in the renal clearance of gabapentin with age can largely be explained by the decline in renal function. Reduction of gabapentin dose may be required in patients who have age related compromised renal function. (see PRECAUTIONS, Geriatric Use and DOSAGE AND ADMINISTRATION).
Pediatric
Gabapentin pharmacokinetics were determined in 48 pediatric subjects between the ages of 1 month and 12 years following a dose of approximately 10 mg/kg. Peak plasma concentrations were similar across the entire age group and occurred 2 to 3 hours postdose. In general, pediatric subjects between 1 month and <5 years of age achieved approximately 30% lower exposure (AUC) than that observed in those 5 years of age and older. Accordingly, oral clearance normalized per body weight was higher in the younger children. Apparent oral clearance of gabapentin was directly proportional to creatinine clearance. Gabapentin elimination half-life averaged 4.7 hours and was similar across the age groups studied.
A population pharmacokinetic analysis was performed in 253 pediatric subjects between 1 month and 13 years of age. Patients received 10 to 65 mg/kg/day given TID. Apparent oral clearance (CL/F) was directly proportional to creatinine clearance and this relationship was similar following a single dose and at steady state. Higher oral clearance values were observed in children <5 years of age compared to those observed in children 5 years of age and older, when normalized per body weight. The clearance was highly variable in infants <1 year of age. The normalized CL/F values observed in pediatric patients 5 years of age and older were consistent with values observed in adults after a single dose. The oral volume of distribution normalized per body weight was constant across the age range.
These pharmacokinetic data indicate that the effective daily dose in pediatric patients with epilepsy ages 3 and 4 years should be 40 mg/kg/day to achieve average plasma concentrations similar to those achieved in patients 5 years of age and older receiving gabapentin at 30 mg/kg/day (see DOSAGE AND ADMINISTRATION).
Gender
Although no formal study has been conducted to compare the pharmacokinetics of gabapentin in men and women, it appears that the pharmacokinetic parameters for males and females are similar and there are no significant gender differences.
Race
Pharmacokinetic differences due to race have not been studied. Because gabapentin is primarily renally excreted and there are no important racial differences in creatinine clearance, pharmacokinetic differences due to race are not expected.
Clinical StudiesPostherpetic Neuralgia
Gabapentin tablets were evaluated for the management of postherpetic neuralgia (PHN) in 2 randomized, double-blind, placebo-controlled, multicenter studies; N=563 patients in the intent-to-treat (ITT) population (Table 1). Patients were enrolled if they continued to have pain for more than 3 months after healing of the herpes zoster skin rash.
Table 1 Controlled PHN Studies: Duration, Dosages, and Number of Patients Study Study Duration Gabapentin (mg/day)a
Target DosePatients Receiving
GabapentinPatients Receiving
PlaceboaGiven in 3 divided doses (TID)
1 8 weeks 3600 113 116 2 7 weeks 1800, 2400 223 111 Total 336 227 Each study included a 1-week baseline during which patients were screened for eligibility and a 7- or 8-week double-blind phase (3 or 4 weeks of titration and 4 weeks of fixed dose). Patients initiated treatment with titration to a maximum of 900 mg/day gabapentin over 3 days. Dosages were then to be titrated in 600 to 1200 mg/day increments at 3- to 7-day intervals to target dose over 3 to 4 weeks. In Study 1, patients were continued on lower doses if not able to achieve the target dose. During baseline and treatment, patients recorded their pain in a daily diary using an 11-point numeric pain rating scale ranging from 0 (no pain) to 10 (worst possible pain). A mean pain score during baseline of at least 4 was required for randomization (baseline mean pain score for Studies 1 and 2 combined was 6.4). Analyses were conducted using the ITT population (all randomized patients who received at least one dose of study medication).
Both studies showed significant differences from placebo at all doses tested.
A significant reduction in weekly mean pain scores was seen by Week 1 in both studies, and significant differences were maintained to the end of treatment. Comparable treatment effects were observed in all active treatment arms. Pharmacokinetic/pharmacodynamic modeling provided confirmatory evidence of efficacy across all doses. Figures 1 and 2 show these changes for Studies 1 and 2.
Figure 1
Weekly Mean Pain Scores (Observed Cases in ITT Population): Study 1
Figure 2
Weekly Mean Pain Scores (Observed Cases in ITT Population): Study 2
The proportion of responders (those patients reporting at least 50% improvement in endpoint pain score compared with baseline) was calculated for each study (Figure 3).
Figure 3
Proportion of Responders (patients with ≥50% reduction in pain score) at Endpoint:
Controlled PHN Studies
Epilepsy
The effectiveness of gabapentin tablets as adjunctive therapy (added to other antiepileptic drugs) was established in multicenter placebo-controlled, double-blind, parallel-group clinical trials in adult and pediatric patients (3 years and older) with refractory partial seizures.
Evidence of effectiveness was obtained in three trials conducted in 705 patients (age 12 years and above) and one trial conducted in 247 pediatric patients (3 to 12 years of age). The patients enrolled had a history of at least 4 partial seizures per month in spite of receiving one or more antiepileptic drugs at therapeutic levels and were observed on their established antiepileptic drug regimen during a 12-week baseline period (6 weeks in the study of pediatric patients). In patients continuing to have at least 2 (or 4 in some studies) seizures per month, gabapentin tablet or placebo was then added on to the existing therapy during a 12-week treatment period. Effectiveness was assessed primarily on the basis of the percent of patients with a 50% or greater reduction in seizure frequency from baseline to treatment (the "responder rate") and a derived measure called response ratio, a measure of change defined as (T - B)/(T + B), in which B is the patient's baseline seizure frequency and T is the patient's seizure frequency during treatment. Response ratio is distributed within the range -1 to +1. A zero value indicates no change while complete elimination of seizures would give a value of -1; increased seizure rates would give positive values. A response ratio of -0.33 corresponds to a 50% reduction in seizure frequency. The results given below are for all partial seizures in the intent-to-treat (all patients who received any doses of treatment) population in each study, unless otherwise indicated.
One study compared gabapentin tablets 1200 mg/day divided TID with placebo. Responder rate was 23% (14/61) in the gabapentin tablets group and 9% (6/66) in the placebo group; the difference between groups was statistically significant. Response ratio was also better in the gabapentin tablets group (-0.199) than in the placebo group (-0.044), a difference that also achieved statistical significance.
A second study compared primarily 1200 mg/day divided TID gabapentin tablets (N=101) with placebo (N=98). Additional smaller gabapentin tablets dosage groups (600 mg/day, N=53; 1800 mg/day, N=54) were also studied for information regarding dose response. Responder rate was higher in the gabapentin tablets 1200 mg/day group (16%) than in the placebo group (8%), but the difference was not statistically significant. The responder rate at 600 mg (17%) was also not significantly higher than in the placebo, but the responder rate in the 1800 mg group (26%) was statistically significantly superior to the placebo rate. Response ratio was better in the gabapentin tablets 1200 mg/day group (-0.103) than in the placebo group (-0.022); but this difference was also not statistically significant (p = 0.224). A better response was seen in the gabapentin tablets 600 mg/day group (-0.105) and 1800 mg/day group (-0.222) than in the 1200 mg/day group, with the 1800 mg/day group achieving statistical significance compared to the placebo group.
A third study compared gabapentin tablets 900 mg/day divided TID (N=111) and placebo (N=109). An additional gabapentin tablets 1200 mg/day dosage group (N=52) provided dose-response data. A statistically significant difference in responder rate was seen in the gabapentin tablets 900 mg/day group (22%) compared to that in the placebo group (10%). Response ratio was also statistically significantly superior in the gabapentin tablets 900 mg/day group (-0.119) compared to that in the placebo group (-0.027), as was response ratio in 1200 mg/day gabapentin tablets (-0.184) compared to placebo.
Analyses were also performed in each study to examine the effect of gabapentin tablets on preventing secondarily generalized tonic-clonic seizures. Patients who experienced a secondarily generalized tonic-clonic seizure in either the baseline or in the treatment period in all three placebo-controlled studies were included in these analyses. There were several response ratio comparisons that showed a statistically significant advantage for gabapentin tablets compared to placebo and favorable trends for almost all comparisons.
Analysis of responder rate using combined data from all three studies and all doses (N=162, gabapentin tablets; N=89, placebo) also showed a significant advantage for gabapentin tablets over placebo in reducing the frequency of secondarily generalized tonic-clonic seizures.
In two of the three controlled studies, more than one dose of gabapentin tablets was used. Within each study, the results did not show a consistently increased response to dose. However, looking across studies, a trend toward increasing efficacy with increasing dose is evident (see Figure 4).
Figure 4
Responder Rate in Patients Receiving Gabapentin Tablets Expressed as a Difference from Placebo by Dose and Study: Adjunctive Therapy Studies in Patients ≥12 Years of Age with Partial Seizures
In the figure, treatment effect magnitude, measured on the Y axis in terms of the difference in the proportion of gabapentin and placebo-assigned patients attaining a 50% or greater reduction in seizure frequency from baseline, is plotted against the daily dose of gabapentin administered (X axis).
Although no formal analysis by gender has been performed, estimates of response (Response Ratio) derived from clinical trials (398 men, 307 women) indicate no important gender differences exist. There was no consistent pattern indicating that age had any effect on the response to gabapentin. There were insufficient numbers of patients of races other than Caucasian to permit a comparison of efficacy among racial groups.
A fourth study in pediatric patients age 3 to 12 years compared 25 - 35 mg/kg/day gabapentin tablets (N=118) with placebo (N=127). For all partial seizures in the intent-to-treat population, the response ratio was statistically significantly better for the gabapentin tablets group (-0.146) than for the placebo group (-0.079). For the same population, the responder rate for gabapentin tablets (21%) was not significantly different from placebo (18%).
A study in pediatric patients age 1 month to 3 years compared 40 mg/kg/day gabapentin tablets (N=38) with placebo (N=38) in patients who were receiving at least one marketed antiepileptic drug and had at least one partial seizure during the screening period (within 2 weeks prior to baseline). Patients had up to 48 hours of baseline and up to 72 hours of double-blind video EEG monitoring to record and count the occurrence of seizures. There were no statistically significant differences between treatments in either the response ratio or responder rate.
-
DRUG ABUSE AND DEPENDENCE SECTION
Controlled Substance
Gabapentin is not a scheduled drug.
Abuse
Gabapentin does not exhibit affinity for benzodiazepine, opiate (mu, delta or kappa), or cannabinoid 1 receptor sites. A small number of postmarketing cases report gabapentin misuse and abuse. These individuals were taking higher than recommended doses of gabapentin for unapproved uses. Most of the individuals described in these reports had a history of poly-substance abuse or used gabapentin to relieve symptoms of withdrawal from other substances. When prescribing gabapentin carefully evaluate patients for a history of drug abuse and observe them for signs and symptoms of gabapentin misuse or abuse (e.g. development of tolerance, self-dose escalation, and drug-seeking behavior).
Dependence
There are rare postmarketing reports of individuals experiencing withdrawal symptoms shortly after discontinuing higher than recommended doses of gabapentin used to treat illnesses for which the drug is not approved. Such symptoms included agitation, disorientation and confusion after suddenly discontinuing gabapentin that resolved after restarting gabapentin. Most of these individuals had a history of poly-substance abuse or used gabapentin to relieve symptoms of withdrawal from other substances. The dependence and abuse potential of gabapentin has not been evaluated in human studies.
-
OVERDOSAGE SECTION
A lethal dose of gabapentin was not identified in mice and rats receiving single oral doses as high as 8000 mg/kg. Signs of acute toxicity in animals included ataxia, labored breathing, ptosis, sedation, hypoactivity, or excitation.
Acute oral overdoses of gabapentin tablets up to 49 grams have been reported. In these cases, double vision, slurred speech, drowsiness, lethargy and diarrhea, were observed. All patients recovered with supportive care.
Gabapentin can be removed by hemodialysis. Although hemodialysis has not been performed in the few overdose cases reported, it may be indicated by the patient's clinical state or in patients with significant renal impairment.
-
DOSAGE & ADMINISTRATION SECTION
Gabapentin tablets are given orally with or without food. Patients should be informed that, should they break the scored 600 or 800 mg tablet in order to administer a half-tablet, they should take the unused half-tablet as the next dose. Half-tablets not used within several days of breaking the scored tablet should be discarded.
If gabapentin tablets dose is reduced, discontinued, or substituted with an alternative medication, this should be done gradually over a minimum of 1 week (a longer period may be needed at the discretion of the prescriber).
Postherpetic Neuralgia
In adults with postherpetic neuralgia, gabapentin therapy may be initiated as a single 300-mg dose on Day 1, 600 mg/day on Day 2 (divided BID), and 900 mg/day on Day 3 (divided TID). The dose can subsequently be titrated up as needed for pain relief to a daily dose of 1800 mg (divided TID). In clinical studies, efficacy was demonstrated over a range of doses from 1800 mg/day to 3600 mg/day with comparable effects across the dose range. Additional benefit of using doses greater than 1800 mg/day was not demonstrated.
Epilepsy
Gabapentin tablets are recommended for add-on therapy in patients 3 years of age and older. Effectiveness in pediatric patients below the age of 3 years has not been established.
Patients >12 years of age
The effective dose of gabapentin is 900 to 1800 mg/day and given in divided doses (three times a day) using 300 or 400 mg capsules, or 600 or 800 mg tablets. The starting dose is 300 mg three times a day. If necessary, the dose may be increased using 300 or 400 mg capsules, or 600 or 800 mg tablets three times a day up to 1800 mg/day. Dosages up to 2400 mg/day have been well tolerated in long-term clinical studies. Doses of 3600 mg/day have also been administered to a small number of patients for a relatively short duration, and have been well tolerated. The maximum time between doses in the TID schedule should not exceed 12 hours.
Pediatric Patients Age 3 to 12 years
The starting dose should range from 10-15 mg/kg/day in 3 divided doses, and the effective dose reached by upward titration over a period of approximately 3 days. The effective dose of gabapentin tablets in patients 5 years of age and older is 25–35 mg/kg/day and given in divided doses (three times a day). The effective dose in pediatric patients ages 3 and 4 years is 40 mg/kg/day and given in divided doses (three times a day) (see CLINICAL PHARMACOLOGY, Pediatrics). Dosages up to 50 mg/kg/day have been well tolerated in a long-term clinical study. The maximum time interval between doses should not exceed 12 hours.
It is not necessary to monitor gabapentin plasma concentrations to optimize gabapentin therapy. Further, because there are no significant pharmacokinetic interactions among gabapentin and other commonly used antiepileptic drugs, the addition of gabapentin does not alter the plasma levels of these drugs appreciably.
If gabapentin tablets are discontinued and/or an alternate anticonvulsant medication is added to the therapy, this should be done gradually over a minimum of 1 week.
Dosage in Renal Impairment
Creatinine clearance is difficult to measure in outpatients. In patients with stable renal function, creatinine clearance (CCr) can be reasonably well estimated using the equation of Cockcroft and Gault:
for females CCr=(0.85)(140-age)(weight)/[(72)(SCr)]
for males CCr=(140-age)(weight)/[(72)(SCr)]
in which age is in years, weight is in kilograms and SCr is serum creatinine in mg/dL.
Dosage adjustment in patients ≥12 years of age with compromised renal function or undergoing hemodialysis is recommended as follows (see dosing recommendations above for effective doses in each indication).
Table 6 Gabapentin Tablets Dosage Based on Renal Function Renal Function
Creatinine Clearance
(mL/min)Total Daily
Dose Range
(mg/day)Dose Regimen (mg) a For patients with creatinine clearance <15 mL/min, reduce daily dose in proportion to creatinine clearance (e.g., patients with a creatinine clearance of 7.5 mL/min should receive one-half the daily dose that patients with a creatinine clearance of 15 mL/min receive).
b Patients on hemodialysis should receive maintenance doses based on estimates of creatinine clearance as indicated in the upper portion of the table and a supplemental post-hemodialysis dose administered after each 4 hours of hemodialysis as indicated in the lower portion of the table.
≥60 900-3600 300 TID 400 TID 600 TID 800 TID 1200 TID >30-59 400-1400 200 BID 300 BID 400 BID 500 BID 700 BID >15-29 200-700 200 QD 300 QD 400 QD 500 QD 700 QD 15a 100-300 100 QD 125 QD 150 QD 200 QD 300 QD Post-Hemodialysis Supplemental Dose (mg)b Hemodialysis 125b 150b 200b 250b 350b The use of gabapentin tablets in patients <12 years of age with compromised renal function has not been studied.
Dosage in Elderly
Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and dose should be adjusted based on creatinine clearance values in these patients.
-
HOW SUPPLIED SECTION
Gabapentin Tablets, USP 600 mg are white to off-white having mottled spots, oval-shaped, biconvex, film-coated tablets debossed with 'ZE72' with bisect on one side and plain with bisect on other side and are supplied as follows:
NDC 68382-204-01 in bottle of 100 tablets
NDC 68382-204-05 in bottle of 500 tablets
NDC 68382-204-10 in bottle of 1000 tablets
Gabapentin Tablets, USP 800 mg are white to off-white having mottled spots, oval-shaped, bevelled-edge, biconvex, film-coated tablets debossed with 'ZE71' with bisect on one side and plain with bisect on other side and are supplied as follows:
NDC 68382-205-01 in bottle of 100 tablets
NDC 68382-205-05 in bottle of 500 tablets
NDC 68382-205-10 in bottle of 1000 tablets
NDC 68382-205-30 in unit-dose blister cartons of 100 (10 x 10) unit dose tablets
-
STORAGE AND HANDLING SECTION
Store at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight container.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Manufactured by:
Cadila Healthcare Ltd.
Ahmedabad, India
Distributed by:
Zydus Pharmaceuticals USA Inc.
Pennington, NJ 08534
Rev.: 04/14
Revision Date: 2014/04/05
-
SPL MEDGUIDE SECTION
Gabapentin Tablets, USP
Read the Medication Guide before you start taking gabapentin tablets and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about Gabapentin Tablets? Do not stop taking gabapentin tablets without first talking to your healthcare provider.
Stopping gabapentin tablets suddenly can cause serious problems.
Gabapentin tablets can cause serious side effects including:
- Like other antiepileptic drugs, gabapentin tablets may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
Do not stop taking gabapentin tablets without first talking to a healthcare provider.
- Stopping gabapentin tablets suddenly can cause serious problems. Stopping a seizure medicine suddenly in a patient who has epilepsy can cause seizures that will not stop (status epilepticus).
Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
2. Changes in behavior and thinking -Using gabapentin tablets in children 3 to 12 years of age can cause emotional changes, aggressive behavior, problems with concentration, restlessness, changes in school performance, and hyperactivity.
3. Gabapentin may cause a serious or life-threatening allergic reaction that may affect your skin or other parts of your body such as your liver or blood cells. You may or may not have rash when you get this type of reaction. It may cause you to be hospitalized or to stop gabapentin. Call a healthcare provider right away if you have any of the following symptoms:
- skin rash
- hives
- fever
- swollen glands that do not go away
- swelling of your lip and tongue
- yellowing of your skin or of the whites of the eyes
- unusual bruising or bleeding
- severe fatigue or weakness
- unexpected muscle pain
- frequent infections
These symptoms may be the first signs of a serious reaction. A healthcare provider should examine you to decide if you should continue taking gabapentin.
What is Gabapentin Tablets?
Gabapentin tablets is a prescription medicine used to treat:
- Pain from damaged nerves (postherpetic pain) that follows healing of shingles (a painful rash that comes after a herpes zoster infection) in adults.
- Partial seizures when taken together with other medicines in adults and children 3 years of age and older.
Who should not take Gabapentin Tablets?
Do not take gabapentin tablets if you are allergic to gabapentin or any of the other ingredients in gabapentin tablets. See the end of this Medication Guide for a complete list of ingredients in gabapentin tablets.
What should I tell my healthcare provider before taking Gabapentin Tablets?
Before taking gabapentin tablets, tell your healthcare provider if you:
- have or have had kidney problems or are on hemodialysis
- have or have had depression, mood problems, or suicidal thoughts or behavior
- are pregnant or plan to become pregnant. It is not known if gabapentin tablets can harm your unborn baby. Tell your healthcare provider right away if you become pregnant while taking gabapentin tablets. You and your healthcare provider will decide if you should take gabapentin tablets while you are pregnant.
- If you become pregnant while taking gabapentin tablets, talk to your healthcare provider about registering with the North American Antiepileptic Drug (NAAED) Pregnancy Registry. The purpose of this registry is to collect information about the safety of antiepileptic drugs during pregnancy. You can enroll in this registry by calling 1-888-233-2334.
- are breastfeeding or plan to breastfeed. Gabapentin tablets can pass into breast milk. You and your healthcare provider should decide how you will feed your baby while you take gabapentin tablets.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Taking gabapentin tablets with certain other medicines can cause side effects or affect how well they work. Do not start or stop other medicines without talking to your healthcare provider.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine.
How should I take Gabapentin Tablets?
- Take gabapentin tablets exactly as prescribed. Your healthcare provider will tell you how much gabapentin tablets to take.
- Do not change your dose of gabapentin tablets without talking to your healthcare provider. If you break a tablet in half, the unused half of the tablet should be taken at your next scheduled dose. Half tablets not used within several days of breaking should be thrown away.
- Gabapentin tablets can be taken with or without food. If you take an antacid containing aluminum and magnesium, such as Maalox®*, Mylanta®*, Gelusil®*, Gaviscon®*, or Di-Gel®*, you should wait at least 2 hours before taking your next dose of gabapentin tablets.
- If you take too much gabapentin tablets, call your healthcare provider or your local Poison Control Center right away.
What should I avoid while taking Gabapentin Tablets?
- Do not drink alcohol or take other medicines that make you sleepy or dizzy while taking gabapentin tablets without first talking with your healthcare provider. Taking gabapentin tablets with alcohol or drugs that cause sleepiness or dizziness may make your sleepiness or dizziness worse.
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how gabapentin tablet affects you. Gabapentin tablets can slow your thinking and motor skills.
What are the possible side effects of Gabapentin Tablets?
- See "What is the most important information I should know about Gabapentin Tablets?"
- The most common side effects of gabapentin tablets include:
- dizziness
- difficulty with speaking
- lack of coordination
- temporary loss of memory (amnesia)
- viral infection
- tremor
- feeling drowsy
- difficulty with coordination
- feeling tired
- double vision
- fever
- unusual eye movement
- jerky movements
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of gabapentin tablets. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Gabapentin Tablets?
Store gabapentin tablets at 20° to 25°C (68° to 77°F) [See USP Controlled Room Temperature].
Dispense in a tight container.
Keep Gabapentin Tablets and all medicines out of the reach of children.
General information about the safe and effective use of Gabapentin Tablets
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use gabapentin tablets for a condition for which it was not prescribed. Do not give gabapentin tablets to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about gabapentin tablets. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about gabapentin tablets that was written for healthcare professionals. Please address medical inquiries to, (MedicalAffairs@zydususa.com) Tel.:1-877-993-8779.
What are the ingredients in Gabapentin Tablets?
Active ingredient: gabapentin, USP
Inactive ingredients: copovidone, low substituted hydroxypropyl cellulose, magnesium stearate, mannitol, poloxamer, povidone and talc
*All trademarks are the property of their respective owners.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
This product's label may have been updated. For current full prescribing information, please visit www.zydususa.com.
Manufactured by:
Cadila Healthcare Ltd.
Ahmedabad, India
Distributed by:
Zydus Pharmaceuticals USA Inc.
Pennington, NJ 08534
Rev.: 07/13
Revision Date: 2013/07/05
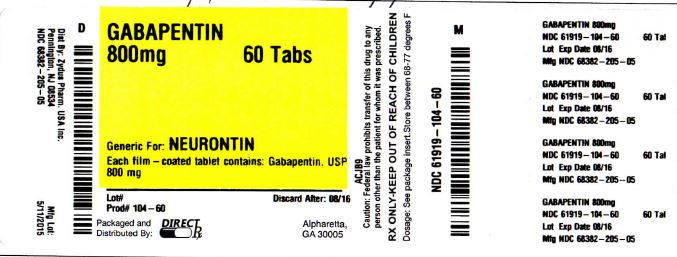
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
NDC 68382-204-01 in bottle of 100 tablets
Gabapentin Tablets USP, 600 mg
Rx only
100 tablets
ZYDUS
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
GABAPENTIN
gabapentin tablet, film coatedProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:61919-104(NDC:68382-205) Route of Administration ORAL Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength GABAPENTIN (UNII: 6CW7F3G59X) (GABAPENTIN - UNII:6CW7F3G59X) GABAPENTIN 800 mg Inactive Ingredients Ingredient Name Strength COPOVIDONE (UNII: D9C330MD8B) HYDROXYPROPYL CELLULOSE, LOW SUBSTITUTED (UNII: 2165RE0K14) MAGNESIUM STEARATE (UNII: 70097M6I30) MANNITOL (UNII: 3OWL53L36A) POLOXAMER 407 (UNII: TUF2IVW3M2) POVIDONE (UNII: FZ989GH94E) TALC (UNII: 7SEV7J4R1U) Product Characteristics Color white Score 2 pieces Shape OVAL Size 20mm Flavor Imprint Code ZE71 Contains Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:61919-104-90 90 in 1 BOTTLE; Type 0: Not a Combination Product 01/01/2014 2 NDC:61919-104-60 60 in 1 BOTTLE; Type 0: Not a Combination Product 01/01/2014 3 NDC:61919-104-30 30 in 1 BOTTLE; Type 0: Not a Combination Product 01/01/2014 Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA078926 01/01/2014 Labeler - DIRECT RX (079254320) Establishment Name Address ID/FEI Business Operations DIRECT RX 079254320 relabel(61919-104) , repack(61919-104)