METFORMIN HYDROCHLORIDE- metformin hydrochloride tablet, film coated
REMEDYREPACK INC.
----------
BOXED WARNING
Lactic Acidosis
The reported incidence of lactic acidosis in patients receiving metformin hydrochloride is very low (approximately 0.03 cases/1000 patient-years, with approximately 0.015 fatal cases/1000 patient-years). In more than 20,000 patient-years exposure to metformin in clinical trials, there were no reports of lactic acidosis. Reported cases have occurred primarily in diabetic patients with significant renal insufficiency, including both intrinsic renal disease and renal hypoperfusion, often in the setting of multiple concomitant medical/surgical problems and multiple concomitant medications. Patients with congestive heart failure requiring pharmacologic management, in particular those with unstable or acute congestive heart failure who are at risk of hypoperfusion and hypoxemia, are at increased risk of lactic acidosis. The risk of lactic acidosis increases with the degree of renal dysfunction and the patient's age. The risk of lactic acidosis may, therefore, be significantly decreased by regular monitoring of renal function in patients taking metformin and by use of the minimum effective dose of metformin. In particular, treatment of the elderly should be accompanied by careful monitoring of renal function. Metformin treatment should not be initiated in patientsyears of age unless measurement of creatinine clearance demonstrates that renal function is not reduced, as these patients are more susceptible to developing lactic acidosis. In addition, metformin should be promptly withheld in the presence of any condition associated with hypoxemia, dehydration, or sepsis. Because impaired hepatic function may significantly limit the ability to clear lactate, metformin should generally be avoided in patients with clinical or laboratory evidence of hepatic disease. Patients should be cautioned against excessive alcohol intake, either acute or chronic, when taking metformin hydrochloride tablets, since alcohol potentiates the effects of metformin hydrochloride on lactate metabolism. In addition, metformin should be temporarily discontinued prior to any intravascular radiocontrast study and for any surgical procedure (see alsoPRECAUTIONS
).
The onset of lactic acidosis often is subtle, and accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, increasing somnolence, and nonspecific abdominal distress. There may be associated hypothermia, hypotension, and resistant bradyarrhythmias with more marked acidosis. The patient and the patient's physician must be aware of the possible importance of such symptoms and the patient should be instructed to notify the physician immediately if they occur (see also
PRECAUTIONS
). Metformin hydrochloride tablets should be withdrawn until the situation is clarified. Serum electrolytes, ketones, blood glucose, and if indicated, blood pH, lactate levels, and even blood metformin levels may be useful. Once a patient is stabilized on any dose level of metformin, gastrointestinal symptoms, which are common during initiation of therapy, are unlikely to be drug related. Later occurrence of
Levels of fasting venous plasma lactate above the upper limit of normal but less than 5 mmol/L in patients taking metformin do not necessarily indicate impending lactic acidosis and may be explainable by other mechanisms, such as poorly controlled diabetes or obesity, vigorous physical activity, or technical problems in sample handling. (See also
PRECAUTIONS
.)
Lactic acidosis should be suspected in any diabetic patient with metabolic acidosis lacking evidence of ketoacidosis (ketonuria and ketonemia).
Lactic acidosis is a medical emergency that must be treated in a hospital setting. In a patient with lactic acidosis who is taking metformin, the drug should be discontinued immediately and general supportive measures promptly instituted. Because metformin hydrochloride is dialyzable (with a clearance of up to 170 mL/min under good hemodynamic conditions), prompt hemodialysis is recommended to correct the acidosis and remove the accumulated metformin. Such management often results in prompt reversal of symptoms and recovery. (See also
CONTRAINDICATIONS
and
PRECAUTIONS
.)
DESCRIPTION
Metformin hydrochloride tablets are oral antihyperglycemic drugs used in the management of type 2 diabetes. Metformin hydrochloride (N,N-dimethylimidodicarbonimidic diamide hydrochloride) is not chemically or pharmacologically related to any other classes of oral antihyperglycemic agents. The structural formula is as shown:
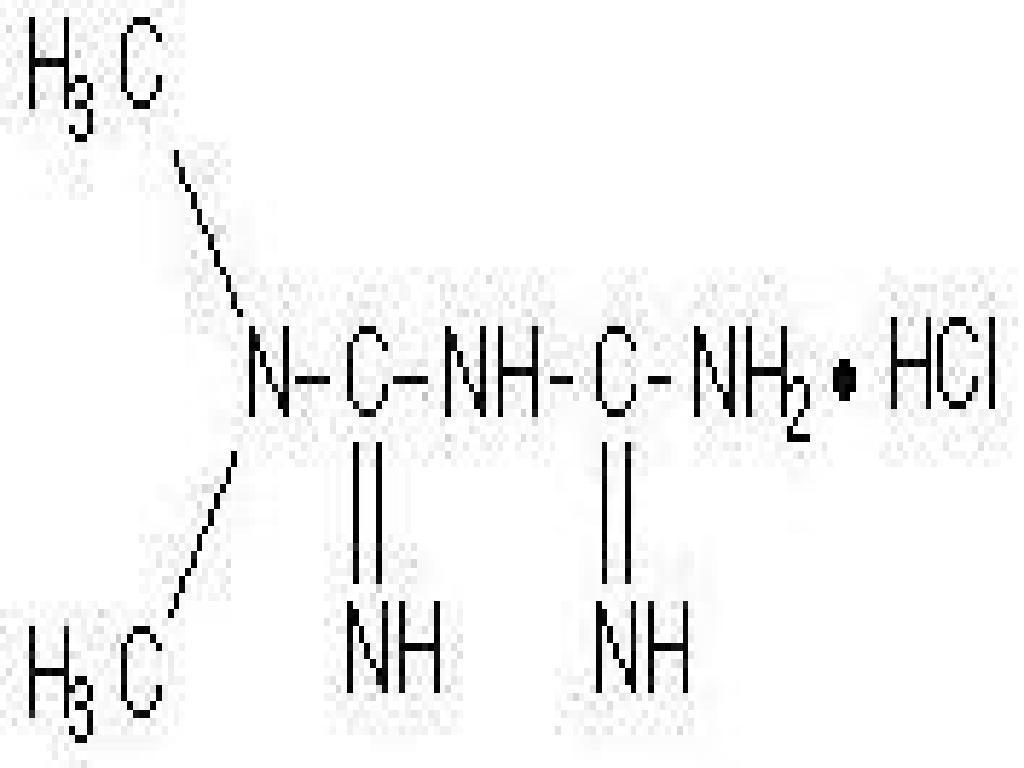
Metformin hydrochloride is a white to off-white crystalline compound with a molecular formula of C4H11N5HCl and a molecular weight of 165.63. Metformin hydrochloride is freely soluble in water and is practically insoluble in acetone, ether, and chloroform. The pKa of metformin is 12.4. The pH of a 1% aqueous solution of metformin hydrochloride is 6.68.
Metformin hydrochloride tablets, for oral administration, contains 500 mg, 850 mg, or 1000 mg of metformin hydrochloride. Each tablet contains the inactive ingredients povidone and magnesium stearate. In addition, the coating for the 500 mg, 850 mg, and 1000 mg contains hypromellose and polyethylene glycol.
INDICATIONS & USAGE
Metformin hydrochloride tablets are indicated as an adjunct to diet and exercise to improve glycemic control in adults and children with type 2 diabetes mellitus.
CONTRAINDICATIONS
Metformin hydrochloride tablets are contraindicated in patients with:
1. Renal disease or renal dysfunction (e.g., as suggested by serum creatinine levels1.5 mg/dL [males],1.4 mg/dL [females] or abnormal creatinine clearance) which may also result from conditions such as cardiovascular collapse (shock), acute myocardial infarction, and septicemia (see
WARNINGS
and
PRECAUTIONS
.)
2. Known hypersensitivity to metformin hydrochloride.
3. Acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma. Diabetic ketoacidosis should be treated with insulin.
Metformin should be temporarily discontinued in patients undergoing radiologic studies involving intravascular administration of iodinated contrast materials, because use of such products may result in acute alteration of renal function. (See also
PRECAUTIONS
.)
WARNINGS
Lactic Acidosis
The reported incidence of lactic acidosis in patients receiving metformin hydrochloride is very low (approximately 0.03 cases/1000 patient-years, with approximately 0.015 fatal cases/1000 patient-years). In more than 20,000 patient-years exposure to metformin in clinical trials, there were no reports of lactic acidosis. Reported cases have occurred primarily in diabetic patients with significant renal insufficiency, including both intrinsic renal disease and renal hypoperfusion, often in the setting of multiple concomitant medical/surgical problems and multiple concomitant medications. Patients with congestive heart failure requiring pharmacologic management, in particular those with unstable or acute congestive heart failure who are at risk of hypoperfusion and hypoxemia, are at increased risk of lactic acidosis. The risk of lactic acidosis increases with the degree of renal dysfunction and the patient's age. The risk of lactic acidosis may, therefore, be significantly decreased by regular monitoring of renal function in patients taking metformin and by use of the minimum effective dose of metformin. In particular, treatment of the elderly should be accompanied by careful monitoring of renal function. Metformin treatment should not be initiated in patientsyears of age unless measurement of creatinine clearance demonstrates that renal function is not reduced, as these patients are more susceptible to developing lactic acidosis. In addition, metformin should be promptly withheld in the presence of any condition associated with hypoxemia, dehydration, or sepsis. Because impaired hepatic function may significantly limit the ability to clear lactate, metformin should generally be avoided in patients with clinical or laboratory evidence of hepatic disease. Patients should be cautioned against excessive alcohol intake, either acute or chronic, when taking metformin hydrochloride tablets, since alcohol potentiates the effects of metformin hydrochloride on lactate metabolism. In addition, metformin should be temporarily discontinued prior to any intravascular radiocontrast study and for any surgical procedure (see also
PRECAUTIONS
).
The onset of lactic acidosis often is subtle, and accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, increasing somnolence, and nonspecific abdominal distress. There may be associated hypothermia, hypotension, and resistant bradyarrhythmias with more marked acidosis. The patient and the patient's physician must be aware of the possible importance of such symptoms and the patient should be instructed to notify the physician immediately if they occur (see also
PRECAUTIONS
). Metformin hydrochloride tablets should be withdrawn until the situation is clarified. Serum electrolytes, ketones, blood glucose, and if indicated, blood pH, lactate levels, and even blood metformin levels may be useful. Once a patient is stabilized on any dose level of metformin, gastrointestinal symptoms, which are common during initiation of therapy, are unlikely to be drug related. Later occurrence of gastrointestinal symptoms could be due to lactic acidosis or other serious disease.
Levels of fasting venous plasma lactate above the upper limit of normal but less than 5 mmol/L in patients taking metformin do not necessarily indicate impending lactic acidosis and may be explainable by other mechanisms, such as poorly controlled diabetes or obesity, vigorous physical activity, or technical problems in sample handling. (See also
PRECAUTIONS
.)
Lactic acidosis should be suspected in any diabetic patient with metabolic acidosis lacking evidence of ketoacidosis (ketonuria and ketonemia).
Lactic acidosis is a medical emergency that must be treated in a hospital setting. In a patient with lactic acidosis who is taking metformin, the drug should be discontinued immediately and general supportive measures promptly instituted. Because metformin hydrochloride is dialyzable (with a clearance of up to 170 mL/min under good hemodynamic conditions), prompt hemodialysis is recommended to correct the acidosis and remove the accumulated metformin. Such management often results in prompt reversal of symptoms and recovery. (See also
CONTRAINDICATIONS
and
PRECAUTIONS
.)
LABORATORY TESTS
Response to all diabetic therapies should be monitored by periodic measurements of fasting blood glucose and glycosylated hemoglobin levels, with a goal of decreasing these levels toward the normal range. During initial dose titration, fasting glucose can be used to determine the therapeutic response. Thereafter, both glucose and glycosylated hemoglobin should be monitored. Measurements of glycosylated hemoglobin may be especially useful for evaluating long-term control (see also
DOSAGE AND ADMINISTRATION
).
Initial and periodic monitoring of hematologic parameters (e.g., hemoglobin/hematocrit and red blood cell indices) and renal function (serum creatinine) should be performed, at least on an annual basis. While megaloblastic anemia has rarely been seen with metformin hydrochloride tablets therapy, if this is suspected, vitamin B12 deficiency should be excluded.
DRUG INTERACTIONS
GlyburideIn a single-dose interaction study in type 2 diabetes patients, coadministration of metformin and glyburide did not result in any changes in either metformin pharmacokinetics or pharmacodynamics. Decreases in glyburide AUC and Cmax were observed, but were highly variable. The single-dose nature of this study and the lack of correlation between glyburide blood levels and pharmacodynamic effects, makes the clinical significance of this interaction uncertain (see
DOSAGE AND ADMINISTRATION: Concomitant Metformin and Oral Sulfonylurea Therapy in Adult Patients
).
FurosemideA single-dose, metformin-furosemide drug interaction study in healthy subjects demonstrated that pharmacokinetic parameters of both compounds were affected by coadministration. Furosemide increased the metformin plasma and blood Cmax by 22% and blood AUC by 15%, without any significant change in metformin renal clearance. When administered with metformin, the Cmax and AUC of furosemide were 31% and 12% smaller, respectively, than when administered alone, and the terminal half-life was decreased by 32%, without any significant change in furosemide renal clearance. No information is available about the interaction of metformin and furosemide when coadministered chronically.
NifedipineA single-dose, metformin-nifedipine drug interaction study in normal healthy volunteers demonstrated that coadministration of nifedipine increased plasma metformin Cmax and AUC by 20% and 9%, respectively, and increased the amount excreted in the urine. Tmax and half-life were unaffected. Nifedipine appears to enhance the absorption of metformin. Metformin had minimal effects on nifedipine.
Cationic drugsCationic drugs (e.g., amiloride, digoxin, morphine, procainamide, quinidine, quinine, ranitidine, triamterene, trimethoprim, or vancomycin) that are eliminated by renal tubular secretion theoretically have the potential for interaction with metformin by competing for common renal tubular transport systems. Such interaction between metformin and oral cimetidine has been observed in normal healthy volunteers in both single- and multiple-dose, metformin-cimetidine drug interaction studies, with a 60% increase in peak metformin plasma and whole blood concentrations and a 40% increase in plasma and whole blood metformin AUC. There was no change in elimination half-life in the single-dose study. Metformin had no effect on cimetidine pharmacokinetics. Although such interactions remain theoretical (except for cimetidine), careful patient monitoring and dose adjustment of metformin and/or the interfering drug is recommended in patients who are taking cationic medications that are excreted via the proximal renal tubular secretory system.
OtherCertain drugs tend to produce hyperglycemia and may lead to loss of glycemic control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, calcium channel blocking drugs, and isoniazid. When such drugs are administered to a patient receiving metformin, the patient should be closely observed for loss of blood glucose control. When such drugs are withdrawn from a patient receiving metformin, the patient should be observed closely for hypoglycemia.
In healthy volunteers, the pharmacokinetics of metformin and propranolol, and metformin and ibuprofen were not affected when coadministered in single-dose interaction studies.
Metformin is negligibly bound to plasma proteins and is, therefore, less likely to interact with highly protein-bound drugs such as salicylates, sulfonamides, chloramphenicol, and probenecid, as compared to the sulfonylureas, which are extensively bound to serum proteins.
CARCINOGENESIS & MUTAGENESIS & IMPAIRMENT OF FERTILITY
Long-term carcinogenicity studies have been performed in rats (dosing duration of 104 weeks) and mice (dosing duration of 91 weeks) at doses up to and including 900 mg/kg/day and 1500 mg/kg/day, respectively.
These doses are both approximately four times the maximum recommended human daily dose of 2000 mg based on body surface area comparisons. No evidence of carcinogenicity with metformin was found in either male or female mice. Similarly, there was no tumorigenic potential observed with metformin in male rats. There was, however, an increased incidence of benign stromal uterine polyps in female rats treated with 900 mg/kg/day.
There was no evidence of a mutagenic potential of metformin in the following in vitro tests: Ames test (S. typhimurium), gene mutation test (mouse lymphoma cells), or chromosomal aberrations test (human lymphocytes). Results in the in vivo mouse micronucleus test were also negative.
Fertility of male or female rats was unaffected by metformin when administered at doses as high as 600 mg/kg/day, which is approximately three times the maximum recommended human daily dose based on body surface area comparisons.
PREGNANCY
Teratogenic effects
Pregnancy Category B
Recent information strongly suggests that abnormal blood glucose levels during pregnancy are associated with a higher incidence of congenital abnormalities. Most experts recommend that insulin be used during pregnancy to maintain blood glucose levels as close to normal as possible. Because animal reproduction studies are not always predictive of human response, metformin should not be used during pregnancy unless clearly needed.
There are no adequate and well-controlled studies in pregnant women with metformin. Metformin was not teratogenic in rats and rabbits at doses up to 600 mg/kg/day. This represents an exposure of about two and six times the maximum recommended human daily dose of 2000 mg based on body surface area comparisons for rats and rabbits, respectively. Determination of fetal concentrations demonstrated a partial placental barrier to metformin.
NURSING MOTHERS
Studies in lactating rats show that metformin is excreted into milk and reaches levels comparable to those in plasma. Similar studies have not been conducted in nursing mothers. Because the potential for hypoglycemia in nursing infants may exist, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. If metformin is discontinued, and if diet alone is inadequate for controlling blood glucose, insulin therapy should be considered.
PEDIATRIC USE
The safety and effectiveness of metformin hydrochloride tablets for the treatment of type 2 diabetes have been established in pediatric patients ages 10 to 16 years (studies have not been conducted in pediatric patients below the age of 10 years). Use of metformin hydrochloride tablets in this age group is supported by evidence from adequate and well-controlled studies of metformin hydrochloride tablets in adults with additional data from a controlled clinical study in pediatric patients ages 10 to 16 years with type 2 diabetes, which demonstrated a similar response in glycemic control to that seen in adults. (See
CLINICAL PHARMACOLOGY: Pediatric Clinical Studies
.) In this study, adverse effects were similar to those described in adults. (See
ADVERSE REACTIONS: Pediatric Patients
.) A maximum daily dose of 2000 mg is recommended. (see
DOSAGE AND ADMINISTRATION: Recommended Dosing Schedule: Pediatrics
.)
GERIATRIC USE
Controlled clinical studies of metformin did not include sufficient numbers of elderly patients to determine whether they respond differently from younger patients, although other reported clinical experience has not identified differences in responses between the elderly and younger patients. Metformin is known to be substantially excreted by the kidney and because the risk of serious adverse reactions to the drug is greater in patients with impaired renal function, metformin should only be used in patients with normal renal function (see
CONTRAINDICATIONS
,
WARNINGS
, and
CLINICAL PHARMACOLOGY: Pharmacokinetics
). Because aging is associated with reduced renal function, metformin should be used with caution as age increases. Care should be taken in dose selection and should be based on careful and regular monitoring of renal function. Generally, elderly patients should not be titrated to the maximum dose of metformin (see also
WARNINGS
and
DOSAGE AND ADMINISTRATION
).
ADVERSE REACTIONS
In a U.S. double-blind clinical study of metformin hydrochloride tablets in patients with type 2 diabetes, a total of 141 patients received metformin hydrochloride tablets therapy (up to 2550 mg per day) and 145 patients received placebo. Adverse reactions reported in greater than 5% of the metformin hydrochloride tablets patients, and that were more common in metformin hydrochloride tablets- than placebo-treated patients, are listed in Table 7.
Table 7: Most Common Adverse Reactions (>5 Percent) in a Placebo-Controlled Clinical Study of Metformin Hydrochloride Tablets Monotherapy*
Adverse ReactionMetformin HydrochlorideTabletsPlaceboMonotherapy(n=145)(n=141)% Patients
Diarrhea53.211.7Nausea/Vomiting25.58.3Flatulence12.15.5Asthenia9.25.5Indigestion7.14.1Abdominal Discomfort6.44.8Headache5.74.8* Reactions that were more common in metformin hydrochloride tablets- than placebo-treated patients.
Diarrhea led to discontinuation of study medication in 6% of patients treated with metformin hydrochloride tablets. Additionally, the following adverse reactions were reported in1 to5% of metformin hydrochloride tablets patients and were more commonly reported with metformin hydrochloride tablets than placebo: abnormal stools, hypoglycemia, myalgia, lightheaded, dyspnea, nail disorder, rash, sweating increased, taste disorder, chest discomfort, chills, flu syndrome, flushing, palpitation.
Pediatric Patients
In clinical trials with metformin hydrochloride tablets in pediatric patients with type 2 diabetes, the profile of adverse reactions was similar to that observed in adults
OVERDOSAGE
Overdose of metformin hydrochloride has occurred, including ingestion of amounts greater than 50 grams. Hypoglycemia was reported in approximately 10% of cases, but no causal association with metformin hydrochloride has been established. Lactic acidosis has been reported in approximately 32% of metformin overdose cases (see
WARNINGS
). Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Therefore, hemodialysis may be useful for removal of accumulated drug from patients in whom metformin overdosage is suspected.
HOW SUPPLIED
Metformin hydrochloride tablets, USP are supplied as:
500 mg Tablets: White, biconvex, circular shaped film coated tablets withA'debossed on one side and12'debossed on the other side.
Bottles of 50 NDC 65862-008-50
Bottles of 60 NDC 65862-008-60
Bottles of 90 NDC 65862-008-90
Bottles of 100 NDC 65862-008-01
Bottles of 300 NDC 65862-008-33
Bottles of 500 NDC 65862-008-05
Bottles of 1000 NDC 65862-008-99
Bottles of 4500 NDC 65862-008-45
850 mg Tablets: White, biconvex, circular shaped film coated tablets withA'debossed on one side and13'debossed on the other side.
Bottles of 50 NDC 65862-009-50
Bottles of 60 NDC 65862-009-60
Bottles of 90 NDC 65862-009-90
Bottles of 100 NDC 65862-009-01
Bottles of 300 NDC 65862-009-33
Bottles of 500 NDC 65862-009-05
Bottles of 1000 NDC 65862-009-99
Bottles of 2500 NDC 65862-009-44
1000 mg Tablets: White, biconvex, oval shaped film coated tablets with a score line in between1'and4'on one side andA'debossed on the other side.
Bottles of 50 NDC 65862-010-50
Bottles of 60 NDC 65862-010-60
Bottles of 90 NDC 65862-010-90
Bottles of 100 NDC 65862-010-01
Bottles of 300 NDC 65862-010-33
Bottles of 500 NDC 65862-010-05
Bottles of 1000 NDC 65862-010-99
Bottles of 2000 NDC 65862-010-46
STORAGE AND HANDLING
Store at 20to 25(68to 77to 30(59to 86[see USP Controlled Room Temperature].
Dispense in light-resistant containers.
| METFORMIN HYDROCHLORIDE
metformin hydrochloride tablet, film coated |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - REMEDYREPACK INC. (829572556) |