ARANESP - darbepoetin alfa injection, solution
Physicians Total Care, Inc.
----------
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use Aranesp safely and effectively. See full prescribing information for Aranesp.
Aranesp® (darbepoetin alfa) injection, for intravenous or subcutaneous use Initial U.S. Approval: 2001 WARNING: ESAs INCREASE THE RISK OF DEATH, MYOCARDIAL INFARCTION, STROKE, VENOUS THROMBOEMBOLISM, THROMBOSIS OF VASCULAR ACCESS AND TUMOR PROGRESSION OR RECURRENCESee full prescribing information for complete boxed warning.
RECENT MAJOR CHANGESDosage and Administration: INDICATIONS AND USAGEAranesp is an erythropoiesis-stimulating agent (ESA) indicated for the treatment of anemia due to:
Limitations of Use Aranesp has not been shown to improve quality of life, fatigue, or patient well-being (1.3).
DOSAGE AND ADMINISTRATION
DOSAGE FORMS AND STRENGTHSCONTRAINDICATIONSWARNINGS AND PRECAUTIONS
ADVERSE REACTIONS
To report SUSPECTED ADVERSE REACTIONS, contact Amgen Medical Information at 1-800-77-AMGEN (1-800-772-6436) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide. Revised: 2/2014 |
FULL PRESCRIBING INFORMATION
WARNING: ESAs INCREASE THE RISK OF DEATH, MYOCARDIAL INFARCTION, STROKE, VENOUS THROMBOEMBOLISM, THROMBOSIS OF VASCULAR ACCESS AND TUMOR PROGRESSION OR RECURRENCE
Chronic Kidney Disease:
- In controlled trials, patients experienced greater risks for death, serious adverse cardiovascular reactions, and stroke when administered erythropoiesis-stimulating agents (ESAs) to target a hemoglobin level of greater than 11 g/dL.
- No trial has identified a hemoglobin target level, Aranesp dose, or dosing strategy that does not increase these risks.
- Use the lowest Aranesp dose sufficient to reduce the need for red blood cell (RBC) transfusions [see Warnings and Precautions (5.1)].
Cancer:
- ESAs shortened overall survival and/or increased the risk of tumor progression or recurrence in clinical studies of patients with breast, non-small cell lung, head and neck, lymphoid, and cervical cancers [see Table 3, Warnings and Precautions (5.3)].
- Because of these risks, prescribers and hospitals must enroll in and comply with the ESA APPRISE Oncology Program to prescribe and/or dispense Aranesp to patients with cancer. To enroll in the ESA APPRISE Oncology Program, visit www.esa-apprise.com or call 1-866-284-8089 for further assistance [see Warnings and Precautions (5.2)].
- To decrease these risks, as well as the risk of serious cardiovascular and thromboembolic reactions, use the lowest dose needed to avoid RBC transfusions [see Dosage and Administration (2.3)].
- Use ESAs only for anemia from myelosuppressive chemotherapy [see Indications and Usage (1.2)].
- ESAs are not indicated for patients receiving myelosuppressive chemotherapy when the anticipated outcome is cure [see Indications and Usage (1.3)].
- Discontinue following the completion of a chemotherapy course [see Dosage and Administration (2.3)].
1 INDICATIONS AND USAGE
1.1 Anemia Due to Chronic Kidney Disease
Aranesp is indicated for the treatment of anemia due to chronic kidney disease (CKD), including patients on dialysis and patients not on dialysis.
1.2 Anemia Due to Chemotherapy in Patients With Cancer
Aranesp is indicated for the treatment of anemia in patients with non-myeloid malignancies where anemia is due to the effect of concomitant myelosuppressive chemotherapy, and upon initiation, there is a minimum of two additional months of planned chemotherapy.
1.3 Limitations of Use
Aranesp has not been shown to improve quality of life, fatigue, or patient well-being.
Aranesp is not indicated for use:
- In patients with cancer receiving hormonal agents, biologic products, or radiotherapy, unless also receiving concomitant myelosuppressive chemotherapy.
- In patients with cancer receiving myelosuppressive chemotherapy when the anticipated outcome is cure.
- As a substitute for RBC transfusions in patients who require immediate correction of anemia [see Clinical Pharmacology (12.2)].
2 DOSAGE AND ADMINISTRATION
2.1 Evaluation of Iron Stores and Nutritional Factors
Evaluate the iron status in all patients before and during treatment and maintain iron repletion. Correct or exclude other causes of anemia (e.g., vitamin deficiency, metabolic or chronic inflammatory conditions, bleeding, etc.) before initiating Aranesp [see Warnings and Precautions (5.10)].
2.2 Patients with Chronic Kidney Disease
In controlled trials, patients experienced greater risks for death, serious adverse cardiovascular reactions, and stroke when administered erythropoiesis-stimulating agents (ESAs) to target a hemoglobin level of greater than 11 g/dL. No trial has identified a hemoglobin target level, Aranesp dose, or dosing strategy that does not increase these risks. Individualize dosing and use the lowest dose of Aranesp sufficient to reduce the need for RBC transfusions [see Warnings and Precautions (5.1)]. Physicians and patients should weigh the possible benefits of decreasing transfusions against the increased risks of death and other serious cardiovascular adverse events [see Boxed Warning and Clinical Studies (14)].
For all patients with CKD
When initiating or adjusting therapy, monitor hemoglobin levels at least weekly until stable, then monitor at least monthly. When adjusting therapy consider hemoglobin rate of rise, rate of decline, ESA responsiveness and hemoglobin variability. A single hemoglobin excursion may not require a dosing change.
- Do not increase the dose more frequently than once every 4 weeks. Decreases in dose can occur more frequently. Avoid frequent dose adjustments.
- If the hemoglobin rises rapidly (e.g., more than 1 g/dL in any 2-week period), reduce the dose of Aranesp by 25% or more as needed to reduce rapid responses.
- For patients who do not respond adequately, if the hemoglobin has not increased by more than 1 g/dL after 4 weeks of therapy, increase the dose by 25%.
- For patients who do not respond adequately over a 12-week escalation period, increasing the Aranesp dose further is unlikely to improve response and may increase risks. Use the lowest dose that will maintain a hemoglobin level sufficient to reduce the need for RBC transfusions. Evaluate other causes of anemia. Discontinue Aranesp if responsiveness does not improve.
For patients with CKD on dialysis:
- Initiate Aranesp treatment when the hemoglobin level is less than 10 g/dL.
- If the hemoglobin level approaches or exceeds 11 g/dL, reduce or interrupt the dose of Aranesp.
- The recommended starting dose is 0.45 mcg/kg intravenously or subcutaneously as a weekly injection or 0.75 mcg/kg once every 2 weeks as appropriate. The intravenous route is recommended for patients on hemodialysis.
For patients with CKD not on dialysis:
- Consider initiating Aranesp treatment only when the hemoglobin level is less than 10 g/dL and the following considerations apply:
- The rate of hemoglobin decline indicates the likelihood of requiring a RBC transfusion and,
- Reducing the risk of alloimmunization and/or other RBC transfusion-related risks is a goal.
- If the hemoglobin level exceeds 10 g/dL, reduce or interrupt the dose of Aranesp, and use the lowest dose of Aranesp sufficient to reduce the need for RBC transfusions.
- The recommended starting dose is 0.45 mcg/kg body weight intravenously or subcutaneously given once at four week intervals as appropriate.
When treating patients who have chronic kidney disease and cancer, physicians should refer to Warnings and Precautions (5.1 and 5.3).
Refer patients who self-administer Aranesp to the Instructions for Use [see Patient Counseling Information (17)].
Conversion from Epoetin alfa to Aranesp in patients with CKD on dialysis
Aranesp is administered less frequently than epoetin alfa.
- Administer Aranesp once weekly in patients who were receiving epoetin alfa 2 to 3 times weekly.
- Administer Aranesp once every 2 weeks in patients who were receiving epoetin alfa once weekly.
Estimate the starting weekly dose of Aranesp for adults and pediatric patients on the basis of the weekly epoetin alfa dose at the time of substitution (see Table 1). Maintain the route of administration (intravenous or subcutaneous injection).
| Previous Weekly Epoetin alfa Dose (Units/week) | Aranesp Dose (mcg/week) | |
| Adult | Pediatric | |
| < 1,500 | 6.25 | |
| 1,500 to 2,499 | 6.25 | 6.25 |
| 2,500 to 4,999 | 12.5 | 10 |
| 5,000 to 10,999 | 25 | 20 |
| 11,000 to 17,999 | 40 | 40 |
| 18,000 to 33,999 | 60 | 60 |
| 34,000 to 89,999 | 100 | 100 |
| ≥ 90,000 | 200 | 200 |
Conversion from Epoetin alfa to Aranesp in patients with CKD not on dialysis
The dose conversion depicted in Table 1 does not accurately estimate the once monthly dose of Aranesp.
2.3 Patients on Cancer Chemotherapy
Initiate Aranesp in patients on cancer chemotherapy only if the hemoglobin is less than 10 g/dL, and if there is a minimum of two additional months of planned chemotherapy.
Use the lowest dose of Aranesp necessary to avoid RBC transfusions.
Recommended Starting Dose
The recommended starting dose and schedules are:
- 2.25 mcg/kg every week subcutaneously until completion of a chemotherapy course
- 500 mcg every 3 weeks subcutaneously until completion of a chemotherapy course
| Dose Adjustment | Weekly Schedule | Every 3 Week Schedule |
| Reduce dose by 40% | Reduce dose by 40% |
| If hemoglobin exceeds a level needed to avoid RBC transfusion |
|
|
| If hemoglobin increases by less than 1 g/dL and remains below 10 g/dL after 6 weeks of therapy | Increase dose to 4.5 mcg/kg/week | No dose adjustment |
| Discontinue Aranesp | Discontinue Aranesp |
2.4 Preparation and Administration
- The needle cover of the prefilled syringe contains dry natural rubber (a derivative of latex), which may cause allergic reactions.
- Do not shake. Do not use Aranesp that has been shaken or frozen.
- Protect vials and prefilled syringes from light.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. Do not use any vials or prefilled syringes exhibiting particulate matter or discoloration.
- Discard unused portion of Aranesp in vials or prefilled syringes. Do not re-enter vial.
- Do not dilute Aranesp and do not administer in conjunction with other drug solutions.
3 DOSAGE FORMS AND STRENGTHS
Aranesp is available as a polysorbate-containing solution.
- Single-dose vials: 25, 40, 60, 100, 200, 300, and 500 mcg Aranesp/1 mL, and 150 mcg Aranesp/0.75 mL
- Single-dose prefilled syringes: 25 mcg Aranesp/0.42 mL, 40 mcg Aranesp/0.4 mL, 60 mcg Aranesp/0.3 mL, 100 mcg Aranesp/0.5 mL, and 150 mcg Aranesp/0.3 mL, 200 mcg Aranesp/0.4 mL, 300 mcg Aranesp/0.6 mL, and 500 mcg Aranesp/1 mL
5 WARNINGS AND PRECAUTIONS
5.1 Increased Mortality, Myocardial Infarction, Stroke, and Thromboembolism
- In controlled clinical trials of patients with CKD comparing higher hemoglobin targets (13 - 14 g/dL) to lower targets (9 - 11.3 g/dL), Aranesp and other ESAs increased the risk of death, myocardial infarction, stroke, congestive heart failure, thrombosis of hemodialysis vascular access, and other thromboembolic events in the higher target groups.
- Using Aranesp to target a hemoglobin level of greater than 11 g/dL increases the risk of serious adverse cardiovascular reactions and has not been shown to provide additional benefit [see Clinical Studies (14.1)]. Use caution in patients with coexistent cardiovascular disease and stroke [see Dosage and Administration (2.2)]. Patients with CKD and an insufficient hemoglobin response to ESA therapy may be at even greater risk for cardiovascular reactions and mortality than other patients. A rate of hemoglobin rise of greater than 1 g/dL over 2 weeks may contribute to these risks.
- In controlled clinical trials of patients with cancer, Aranesp and other ESAs increased the risks for death and serious adverse cardiovascular reactions. These adverse reactions included myocardial infarction and stroke.
- In controlled clinical trials, ESAs increased the risk of death in patients undergoing coronary artery bypass graft surgery (CABG) and the risk of deep venous thrombosis (DVT) in patients undergoing orthopedic procedures.
The design and overall results of the 3 large trials comparing higher and lower hemoglobin targets are shown in Table 2.
| Normal Hematocrit Study (NHS) (N = 1265) | CHOIR (N = 1432) | TREAT (N = 4038) |
|
| Time Period of Trial | 1993 to 1996 | 2003 to 2006 | 2004 to 2009 |
| Population | CKD patients on hemodialysis with coexisting CHF or CAD, hematocrit 30 ± 3% on epoetin alfa | CKD patients not on dialysis with hemoglobin < 11 g/dL not previously administered epoetin alfa | CKD patients not on dialysis with type II diabetes, hemoglobin ≤ 11 g/dL |
| Hemoglobin Target; Higher vs. Lower (g/dL) | 14.0 vs. 10.0 | 13.5 vs. 11.3 | 13.0 vs. ≥ 9.0 |
| Median (Q1, Q3) Achieved Hemoglobin level (g/dL) | 12.6 (11.6, 13.3) vs. 10.3 (10.0, 10.7) | 13.0 (12.2, 13.4) vs. 11.4 (11.1, 11.6) | 12.5 (12.0, 12.8) vs. 10.6 (9.9, 11.3) |
| Primary Endpoint | All-cause mortality or non-fatal MI | All-cause mortality, MI, hospitalization for CHF, or stroke | All-cause mortality, MI, myocardial ischemia, heart failure, and stroke |
| Hazard Ratio or Relative Risk (95% CI) | 1.28 (1.06 - 1.56) | 1.34 (1.03 - 1.74) | 1.05 (0.94 - 1.17) |
| Adverse Outcome for Higher Target Group | All-cause mortality | All-cause mortality | Stroke |
| Hazard Ratio or Relative Risk (95% CI) | 1.27 (1.04 - 1.54) | 1.48 (0.97 - 2.27) | 1.92 (1.38 - 2.68) |
Patients with Chronic Kidney Disease
Normal Hematocrit Study (NHS): A prospective, randomized, open-label study of 1265 patients with chronic kidney disease on dialysis with documented evidence of congestive heart failure or ischemic heart disease was designed to test the hypothesis that a higher target hematocrit (Hct) would result in improved outcomes compared with a lower target Hct. In this study, patients were randomized to epoetin alfa treatment targeted to a maintenance hemoglobin of either 14 ± 1 g/dL or 10 ± 1 g/dL. The trial was terminated early with adverse safety findings of higher mortality in the high hematocrit target group. Higher mortality (35% vs. 29%) was observed for the patients randomized to a target hemoglobin of 14 g/dL than for the patients randomized to a target hemoglobin of 10 g/dL. For all-cause mortality, the HR = 1.27; 95% CI (1.04, 1.54); p=0.018. The incidence of nonfatal myocardial infarction, vascular access thrombosis, and other thrombotic events was also higher in the group randomized to a target hemoglobin of 14 g/dL.
CHOIR: A randomized, prospective trial, 1432 patients with anemia due to CKD who were not undergoing dialysis and who had not previously received epoetin alfa therapy were randomized to epoetin alfa treatment targeting a maintenance hemoglobin concentration of either 13.5 g/dL or 11.3 g/dL. The trial was terminated early with adverse safety findings. A major cardiovascular event (death, myocardial infarction, stroke, or hospitalization for congestive heart failure) occurred in 125 of the 715 patients (18%) in the higher hemoglobin group compared to 97 of the 717 patients (14%) in the lower hemoglobin group [hazard ratio (HR) 1.34, 95% CI: 1.03, 1.74; p = 0.03].
TREAT: A randomized, double-blind, placebo-controlled, prospective trial of 4038 patients with CKD not on dialysis (eGFR of 20 – 60 mL/min), anemia (hemoglobin levels ≤ 11 g/dL), and type 2 diabetes mellitus, patients were randomized to receive either Aranesp treatment or a matching placebo. Placebo group patients also received Aranesp when their hemoglobin levels were below 9 g/dL. The trial objectives were to demonstrate the benefit of Aranesp treatment of the anemia to a target hemoglobin level of 13 g/dL, when compared to a "placebo" group, by reducing the occurrence of either of two primary endpoints: (1) a composite cardiovascular endpoint of all-cause mortality or a specified cardiovascular event (myocardial ischemia, CHF, MI, and CVA) or (2) a composite renal endpoint of all-cause mortality or progression to end stage renal disease. The overall risks for each of the two primary endpoints (the cardiovascular composite and the renal composite) were not reduced with Aranesp treatment (see Table 2), but the risk of stroke was increased nearly two-fold in the Aranesp-treated group versus the placebo group: annualized stroke rate 2.1% vs. 1.1%, respectively, HR 1.92; 95% CI: 1.38, 2.68; p < 0.001. The relative risk of stroke was particularly high in patients with a prior stroke: annualized stroke rate 5.2% in the Aranesp treated group and 1.9% in the placebo group, HR 3.07; 95% CI: 1.44, 6.54. Also, among Aranesp-treated subjects with a past history of cancer, there were more deaths due to all causes and more deaths adjudicated as due to cancer, in comparison with the control group.
Patients with Cancer
An increased incidence of thromboembolic reactions, some serious and life-threatening, occurred in patients with cancer treated with ESAs.
In a randomized, placebo-controlled study (Study 1 in Table 3 [see Warnings and Precautions (5.3)]) of 939 women with metastatic breast cancer receiving chemotherapy, patients received either weekly epoetin alfa or placebo for up to a year. This study was designed to show that survival was superior when epoetin alfa was administered to prevent anemia (maintain hemoglobin levels between 12 and 14 g/dL or hematocrit between 36% and 42%). This study was terminated prematurely when interim results demonstrated a higher mortality at 4 months (8.7% vs. 3.4%) and a higher rate of fatal thrombotic reactions (1.1% vs. 0.2%) in the first 4 months of the study among patients treated with epoetin alfa. Based on Kaplan-Meier estimates, at the time of study termination, the 12-month survival was lower in the epoetin alfa group than in the placebo group (70% vs. 76%; HR 1.37, 95% CI: 1.07, 1.75; p = 0.012).
Patients Having Surgery
Aranesp is not approved for reduction of RBC transfusions in patients scheduled for surgical procedures.
An increased incidence of DVT in patients receiving epoetin alfa undergoing surgical orthopedic procedures was demonstrated. In a randomized, controlled study, 680 adult patients, not receiving prophylactic anticoagulation and undergoing spinal surgery, received epoetin alfa and standard of care (SOC) treatment (n = 340) or SOC treatment alone (n = 340). A higher incidence of DVTs, determined by either color flow duplex imaging or by clinical symptoms, was observed in the epoetin alfa group (16 [4.7%] patients) compared with the SOC group (7 [2.1%] patients). In addition to the 23 patients with DVTs included in the primary analysis, 19 [2.8%] patients experienced 1 other thrombovascular event (TVE) each (12 [3.5%] in the epoetin alfa group and 7 [2.1%] in the SOC group).
Increased mortality was observed in a randomized, placebo-controlled study of epoetin alfa in adult patients who were undergoing CABG surgery (7 deaths in 126 patients randomized to epoetin alfa versus no deaths among 56 patients receiving placebo). Four of these deaths occurred during the period of study drug administration and all 4 deaths were associated with thrombotic events.
5.2 Prescribing and Distribution Program for Aranesp in Patients With Cancer
In order to prescribe and/or dispense Aranesp to patients with cancer and anemia due to myelosuppressive chemotherapy, prescribers and hospitals must enroll in and comply with the ESA APPRISE Oncology Program requirements. To enroll, visit www.esa-apprise.com or call 1-866-284-8089 for further assistance. Additionally, prior to each new course of Aranesp in patients with cancer, prescribers and patients must provide written acknowledgment of a discussion of the risks of Aranesp.
5.3 Increased Mortality and/or Increased Risk of Tumor Progression or Recurrence in Patients With Cancer
ESAs resulted in decreased locoregional control/progression-free survival and/or overall survival (see Table 3). These findings were observed in studies of patients with advanced head and neck cancer receiving radiation therapy (Studies 5 and 6), in patients receiving chemotherapy for metastatic breast cancer (Study 1) or lymphoid malignancy (Study 2), and in patients with non-small cell lung cancer or various malignancies who were not receiving chemotherapy or radiotherapy (Studies 7 and 8).
| Study/Tumor/(n) | Hemoglobin Target | Hemoglobin(Median; Q1, Q3) | Primary Efficacy Outcome | Adverse Outcome for ESA- containing Arm |
| Chemotherapy | ||||
| Study 1 Metastatic breast cancer (n = 939) | 12-14 g/dL | 12.9 g/dL;12.2, 13.3 g/dL | 12-month overall survival | Decreased 12-month survival |
| Study 2 Lymphoid malignancy (n = 344) |
13-15 g/dL (M) 13-14 g/dL (F) | 11 g/dL;9.8, 12.1 g/dL | Proportion of patients achieving a hemoglobin response | Decreased overall survival |
| Study 3 Early breast cancer (n = 733) | 12.5-13 g/dL |
13.1 g/dL; 12.5, 13.7 g/dL | Relapse-free and overall survival |
Decreased 3-year relapse-free and overall survival |
| Study 4 Cervical cancer (n = 114) | 12-14 g/dL | 12.7 g/dL; 12.1, 13.3 g/dL | Progression-free and overall survival and locoregional control | Decreased 3-year progression-free and overall survival and locoregional control |
| Radiotherapy Alone | ||||
| Study 5 Head and neck cancer (n = 351) |
≥15 g/dL (M) ≥14 g/dL (F) | Not available | Locoregional progression-free survival | Decreased 5-year locoregional progression-free and overall survival |
| Study 6 Head and neck cancer (n = 522) | 14-15.5 g/dL | Not available | Locoregional disease control | Decreased locoregional disease control |
| No Chemotherapy or Radiotherapy | ||||
| Study 7 Non-small cell lung cancer (n = 70) | 12-14 g/dL | Not available | Quality of life | Decreased overall survival |
| Study 8 Non-myeloid malignancy (n = 989) | 12-13 g/dL |
10.6 g/dL; 9.4, 11.8 g/dL | RBC transfusions | Decreased overall survival |
Decreased Overall Survival
Study 1 was described in the previous section [see Warnings and Precautions (5.1)]. Mortality at 4 months (8.7% vs. 3.4%) was significantly higher in the epoetin alfa arm. The most common investigator-attributed cause of death within the first 4 months was disease progression; 28 of 41 deaths in the epoetin alfa arm and 13 of 16 deaths in the placebo arm were attributed to disease progression. Investigator-assessed time to tumor progression was not different between the 2 groups. Survival at 12 months was significantly lower in the epoetin alfa arm (70% vs. 76%; HR 1.37, 95% CI: 1.07, 1.75; p = 0.012).
Study 2 was a randomized, double-blind study (darbepoetin alfa vs. placebo) conducted in 344 anemic patients with lymphoid malignancy receiving chemotherapy. With a median follow-up of 29 months, overall mortality rates were significantly higher among patients randomized to darbepoetin alfa as compared to placebo (HR 1.36, 95% CI: 1.02, 1.82).
Study 7 was a multicenter, randomized, double-blind study (epoetin alfa vs. placebo) in which patients with advanced non-small cell lung cancer receiving only palliative radiotherapy or no active therapy were treated with epoetin alfa to achieve and maintain hemoglobin levels between 12 and 14 g/dL. Following an interim analysis of 70 patients (planned accrual 300 patients), a significant difference in survival in favor of the patients in the placebo arm of the study was observed (median survival 63 vs. 129 days; HR 1.84; p = 0.04).
Study 8 was a randomized, double-blind study (darbepoetin alfa vs. placebo) in 989 anemic patients with active malignant disease, neither receiving nor planning to receive chemotherapy or radiation therapy. There was no evidence of a statistically significant reduction in proportion of patients receiving RBC transfusions. The median survival was shorter in the darbepoetin alfa treatment group than in the placebo group (8 months vs. 10.8 months; HR 1.30, 95% CI: 1.07, 1.57).
Decreased Progression-free Survival and Overall Survival
Study 3 was a randomized, open-label, controlled, factorial design study in which darbepoetin alfa was administered to prevent anemia in 733 women receiving neo-adjuvant breast cancer treatment. A final analysis was performed after a median follow-up of approximately 3 years. The 3-year survival rate was lower (86% vs. 90%; HR 1.42, 95% CI: 0.93, 2.18) and the 3-year relapse-free survival rate was lower (72% vs. 78%; HR 1.33, 95% CI: 0.99, 1.79) in the darbepoetin alfa-treated arm compared to the control arm.
Study 4 was a randomized, open-label, controlled study that enrolled 114 of a planned 460 cervical cancer patients receiving chemotherapy and radiotherapy. Patients were randomized to receive epoetin alfa to maintain hemoglobin between 12 and 14 g/dL or to RBC transfusion support as needed. The study was terminated prematurely due to an increase in thromboembolic adverse reactions in epoetin alfa-treated patients compared to control (19% vs. 9%). Both local recurrence (21% vs. 20%) and distant recurrence (12% vs. 7%) were more frequent in epoetin alfa-treated patients compared to control. Progression-free survival at 3 years was lower in the epoetin alfa-treated group compared to control (59% vs. 62%; HR 1.06, 95% CI: 0.58, 1.91). Overall survival at 3 years was lower in the epoetin alfa-treated group compared to control (61% vs. 71%; HR 1.28, 95% CI: 0.68, 2.42).
Study 5 was a randomized, placebo-controlled study in 351 head and neck cancer patients where epoetin beta or placebo was administered to achieve target hemoglobins ≥ 14 and ≥ 15 g/dL for women and men, respectively. Locoregional progression-free survival was significantly shorter in patients receiving epoetin beta (HR 1.62, 95% CI: 1.22, 2.14; p = 0.0008) with medians of 406 days and 745 days in the epoetin beta and placebo arms respectively. Overall survival was significantly shorter in patients receiving epoetin beta (HR 1.39, 95% CI: 1.05, 1.84; p = 0.02).
Decreased Locoregional Control
Study 6 was a randomized, open-label, controlled study conducted in 522 patients with primary squamous cell carcinoma of the head and neck receiving radiation therapy alone (no chemotherapy) who were randomized to receive darbepoetin alfa to maintain hemoglobin levels of 14 to15.5 g/dL or no darbepoetin alfa. An interim analysis performed on 484 patients demonstrated that locoregional control at 5 years was significantly shorter in patients receiving darbepoetin alfa (RR 1.44, 95% CI: 1.06, 1.96; p = 0.02). Overall survival was shorter in patients receiving darbepoetin alfa (RR 1.28, 95% CI: 0.98, 1.68; p = 0.08).
5.4 Hypertension
Aranesp is contraindicated in patients with uncontrolled hypertension. In Aranesp clinical studies, approximately 40% of patients with CKD required initiation or intensification of antihypertensive therapy during the early phase of treatment. Hypertensive encephalopathy and seizures have been reported in patients with CKD receiving Aranesp.
Appropriately control hypertension prior to initiation of and during treatment with Aranesp. Reduce or withhold Aranesp if blood pressure becomes difficult to control. Advise patients of the importance of compliance with antihypertensive therapy and dietary restrictions [see Patient Counseling Information (17)].
5.5 Seizures
Aranesp increases the risk of seizures in patients with CKD. During the first several months following initiation of Aranesp, monitor patients closely for premonitory neurologic symptoms. Advise patients to contact their healthcare practitioner for new-onset seizures, premonitory symptoms, or change in seizure frequency.
5.6 Lack or Loss of Hemoglobin Response to Aranesp
For lack or loss of hemoglobin response to Aranesp, initiate a search for causative factors (e.g., iron deficiency, infection, inflammation, bleeding). If typical causes of lack or loss of hemoglobin response are excluded, evaluate for PRCA [see Warnings and Precautions (5.7)]. In the absence of PRCA, follow dosing recommendations for management of patients with an insufficient hemoglobin response to Aranesp therapy [see Dosage and Administration (2.2)].
5.7 Pure Red Cell Aplasia
Cases of PRCA and of severe anemia, with or without other cytopenias that arise following the development of neutralizing antibodies to erythropoietin have been reported in patients treated with Aranesp. This has been reported predominantly in patients with CKD receiving ESAs by subcutaneous administration. PRCA has also been reported in patients receiving ESAs for anemia related to hepatitis C treatment (an indication for which Aranesp is not approved).
If severe anemia and low reticulocyte count develop during treatment with Aranesp, withhold Aranesp and evaluate patients for neutralizing antibodies to erythropoietin. Contact Amgen (1-800-77-AMGEN) to perform assays for binding and neutralizing antibodies. Permanently discontinue Aranesp in patients who develop PRCA following treatment with Aranesp or other erythropoietin protein drugs. Do not switch patients to other ESAs.
5.8 Serious Allergic Reactions
Serious allergic reactions, including anaphylactic reactions, angioedema, bronchospasm, skin rash, and urticaria may occur with Aranesp. Immediately and permanently discontinue Aranesp and administer appropriate therapy if a serious allergic or anaphylactic reaction occurs.
5.9 Dialysis Management
Patients may require adjustments in their dialysis prescriptions after initiation of Aranesp. Patients receiving Aranesp may require increased anticoagulation with heparin to prevent clotting of the extracorporeal circuit during hemodialysis.
5.10 Laboratory Monitoring
Evaluate transferrin saturation and serum ferritin prior to and during Aranesp treatment. Administer supplemental iron therapy when serum ferritin is less than 100 mcg/L or when serum transferrin saturation is less than 20% [see Dosage and Administration (2.1)]. The majority of patients with CKD will require supplemental iron during the course of ESA therapy. Following initiation of therapy and after each dose adjustment, monitor hemoglobin weekly until the hemoglobin is stable and sufficient to minimize the need for RBC transfusion. Thereafter, hemoglobin may be monitored less frequently provided hemoglobin levels remain stable.
6 ADVERSE REACTIONS
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Increased Mortality, Myocardial Infarction, Stroke, and Thromboembolism [see Warnings and Precautions (5.1)]
- Increased mortality and/or increased risk of tumor progression or recurrence in Patients With Cancer [see Warnings and Precautions (5.3)]
- Hypertension [see Warnings and Precautions (5.4)]
- Seizures [see Warnings and Precautions (5.5)]
- PRCA [see Warnings and Precautions (5.7)]
- Serious allergic reactions [see Warnings and Precautions (5.8)]
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of other drugs and may not reflect the rates observed in practice.
Patients with Chronic Kidney Disease
Adult Patients
Adverse reactions were determined based on pooled data from 5 randomized, active-controlled studies of Aranesp with a total of 1357 patients (Aranesp 766, epoetin alfa 591). The median duration of exposure for patients receiving Aranesp was 340 days, with 580 patients exposed for greater than 6 months and 360 patients exposed for greater than 1 year. The median (25th, 75th percentiles) weight-adjusted dose of Aranesp was 0.50 mcg/kg (0.32, 0.81). The median (range) age for patients administered Aranesp was 62 years (18 to 88). In the Aranesp group, 55% were male, 72% were white, 83% were receiving dialysis, and 17% were not receiving dialysis.
Table 4 lists adverse reactions occurring in ≥ 5% of patients treated with Aranesp.
| Adverse Reaction | Patients Treated With Aranesp (n = 766) |
| Hypertension | 31% |
| Dyspnea | 17% |
| Peripheral edema | 17% |
| Cough | 12% |
| Procedural hypotension | 10% |
| Angina pectoris | 8% |
| Vascular access complications | 8% |
| Fluid overload | 7% |
| Rash/Erythema | 5% |
| Arteriovenous graft thrombosis | 5% |
Rates of adverse reactions with Aranesp therapy were similar to those observed with other recombinant erythropoietins in these studies.
Pediatric Patients
Aranesp was administered to 81 pediatric patients with CKD who had stable hemoglobin concentrations while previously receiving epoetin alfa [see Clinical Studies (14.1)]. In this study, the most frequently reported serious adverse reactions with Aranesp were hypertension and convulsions. The most commonly reported adverse reactions were hypertension, injection site pain, rash, and convulsions. Aranesp administration was discontinued because of injection site pain in 2 patients and moderate hypertension in a third patient.
Studies have not evaluated the effects of Aranesp when administered to pediatric patients as the initial treatment for the anemia associated with CKD.
Cancer Patients Receiving Chemotherapy
Adverse reactions were based on data from a randomized, double-blind, placebo-controlled study of Aranesp in 597 patients (Aranesp 301, placebo 296) with extensive stage small cell lung cancer (SCLC) receiving platinum-based chemotherapy. All patients were white, 64% were male, and the median age was 61 years (range: 28 to 82 years); 25% of the study population were from North America, Western Europe, and Australia. Patients received Aranesp at a dose of 300 mcg or placebo weekly for 4 weeks then every 3 weeks for a total of 24 weeks, and the median duration of exposure was 19 weeks (range: 1 to 26 weeks).
Adverse reactions were also based on data from 7 randomized, double-blind, placebo-controlled studies, including the SCLC study described above, that enrolled 2112 patients (Aranesp 1203, placebo 909) with non-myeloid malignancies. Most patients were white (95%), male (52%), and the median age was 63 years (range: 18 to 91 years); 73% of the study population were from North America, Western Europe, and Australia. Dosing and schedules varied by study from once weekly to once every 4 weeks, and the median duration of exposure was 12 weeks (range: 1 to 27 weeks).
| Adverse Reaction | SCLC Study | All Placebo-controlled Studies | ||||
|
Aranesp (n = 301) |
Placebo (n = 296) |
Aranesp (n = 1203) |
Placebo (n = 909) |
|||
| Thromboembolic Adverse Reactions, n (%) | 24 (8.0%) | 13 (4.4%) | 73 (6.1%) | 37 (4.1%) | ||
| Arterial | 10 (3.3%) | 3 (1.0%) | 15 (1.2%) | 5 (0.6%) | ||
| Myocardial infarction | 5 (1.7%) | 0 | 7 (0.6%) | 2 (0.2%) | ||
| Venous | 14 (4.7%) | 10 (3.4%) | 60 (5.0%) | 32 (3.5%) | ||
| Pulmonary embolism | 5 (1.7%) | 3 (1.0%) | 16 (1.3%) | 6 (0.7%) | ||
| Cerebrovascular disorders | 14 (4.7%) | 9 (3.0%) | 20 (1.7%) | 17 (1.9%) | ||
In addition to the thrombovascular adverse reactions, abdominal pain and edema occurred at a higher incidence in patients taking Aranesp compared to patients on placebo. Among all placebo-controlled studies, abdominal pain (13.2% vs. 9.4%) and edema (12.8% vs. 9.7%) were reported more frequently in patients receiving Aranesp compared to the placebo group. In the SCLC study the incidence of abdominal pain (10.3% vs. 3.4%) and edema (5.6% vs. 5.1%) in the Aranesp-treated patients compared to those receiving placebo.
6.2 Postmarketing Experience
Because postmarketing reporting of adverse reactions is voluntary and from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been identified during postmarketing use of Aranesp:
6.3 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. Neutralizing antibodies to darbepoetin alfa that cross-react with endogenous erythropoietin and other ESAs can result in PRCA or severe anemia (with or without other cytopenias) [see Warnings and Precautions (5.7)].
In clinical studies, the percentage of patients with antibodies to Aranesp was examined using the Biacore® assay. Sera from 1501 patients with CKD and 1159 cancer patients were tested. At baseline, prior to Aranesp treatment, binding antibodies were detected in 59 patients (4%) with CKD and 36 cancer patients (3%). During Aranesp therapy (range: 22 to 177 weeks), a follow-up sample was taken. One additional patient with CKD and 8 additional cancer patients developed antibodies capable of binding Aranesp. None of the patients had antibodies capable of neutralizing the activity of Aranesp or endogenous erythropoietin at baseline or at end of study. No clinical sequelae consistent with PRCA were associated with the presence of these antibodies.
The incidence of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Aranesp with the incidence of antibodies to other products may be misleading.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
There are no adequate and well-controlled studies of Aranesp use in pregnant women. In animal reproduction and developmental toxicity studies, Aranesp increased early post-implantation loss. Use Aranesp during pregnancy only if the potential benefit justifies the potential risk to the fetus.
When Aranesp was administered intravenously to healthy pregnant rats and rabbits, there was no evidence of embryofetal toxicity or other adverse outcomes at the intravenous doses tested, up to 20 mcg/kg/day. This animal dose level of 20 mcg/kg/day is approximately 20-fold higher than the clinical recommended starting dose, depending on the patient’s treatment indication. Slightly reduced fetal weights were observed when healthy rat and rabbit mothers received doses of 1 mcg/kg or more. This dose of 1 mcg/kg is near the clinical recommended starting dose. While no adverse effects on uterine implantation occurred in animals, there was an increase in early post-implantation loss in animal fertility studies. It is not clear whether the increased post-implantation loss reflects a drug effect on the uterine environment or on the conceptus. No significant placental transfer of Aranesp was detected.
In a peri/postnatal development study, pregnant female rats received Aranesp intravenously every other day from implantation throughout pregnancy and lactation. The lowest dose tested, 0.5 mcg/kg, did not cause fetal toxicity; this dose is approximately equivalent to the clinical recommended starting dose. At maternal doses of 2.5 mcg/kg and higher, pups had decreased fetal body weights, which correlated with a slight increase in the incidence of fetal deaths, as well as delayed eye opening and delayed preputial separation [see Nonclinical Toxicology (13.3)].
Women who become pregnant during Aranesp treatment are encouraged to enroll in Amgen’s Pregnancy Surveillance Program. Patients or their physicians should call 1-800-772-6436 (1-800-77-AMGEN) to enroll.
8.3 Nursing Mothers
It is not known whether Aranesp is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Aranesp is administered to a nursing woman.
8.4 Pediatric Use
Pediatric Patients with CKD
Aranesp safety and efficacy were similar between adults and pediatric patients with CKD who were over 1 year of age when patients were transitioned from treatment with epoetin alfa to Aranesp [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14.1)]. Aranesp safety and efficacy have not been established in the initial treatment of anemic pediatric patients with CKD or in the transition from another erythropoietin to Aranesp in pediatric CKD patients less than 1 year of age.
Pediatric Cancer Patients
The safety and efficacy of Aranesp in pediatric cancer patients have not been established.
8.5 Geriatric Use
Of the 1801 patients with CKD in clinical studies of Aranesp, 44% were age 65 and over, while 17% were age 75 and over. Of the 873 patients in clinical studies receiving Aranesp and concomitant cancer chemotherapy, 45% were age 65 and over, while 14% were age 75 and over. No differences in safety or efficacy were observed between older and younger patients.
10 OVERDOSAGE
Aranesp overdosage can cause hemoglobin levels above the desired level, which should be managed with discontinuation or reduction of Aranesp dosage and/or with phlebotomy, as clinically indicated [see Pharmacodynamics (12.2)]. Cases of severe hypertension have been observed following overdose with ESAs [see Warnings and Precautions (5.4)].
11 DESCRIPTION
Aranesp (darbepoetin alfa) is an erythropoiesis-stimulating protein that is produced in Chinese hamster ovary (CHO) cells by recombinant DNA technology. Aranesp is a 165-amino acid protein that differs from recombinant human erythropoietin in containing 5 N-linked oligosaccharide chains, whereas recombinant human erythropoietin contains 3 chains. The 2 additional N-glycosylation sites result from amino acid substitutions in the erythropoietin peptide backbone. The approximate molecular weight of darbepoetin alfa is 37,000 daltons.
Aranesp is formulated as a sterile, colorless, preservative-free solution containing polysorbate for intravenous or subcutaneous administration. Each 1 mL contains polysorbate 80 (0.05 mg), sodium chloride (8.18 mg), sodium phosphate dibasic anhydrous (0.66 mg), and sodium phosphate monobasic monohydrate (2.12 mg) in Water for Injection, USP (pH 6.2 ± 0.2).
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Aranesp stimulates erythropoiesis by the same mechanism as endogenous erythropoietin.
12.2 Pharmacodynamics
Increased hemoglobin levels are not generally observed until 2 to 6 weeks after initiating treatment with Aranesp.
12.3 Pharmacokinetics
Adult Patients with CKD
The pharmacokinetics of Aranesp were studied in patients with CKD receiving or not receiving dialysis and cancer patients receiving chemotherapy.
Following intravenous administration of Aranesp to patients with CKD receiving dialysis, Aranesp serum concentration-time profiles were biphasic, with a distribution half-life of approximately 1.4 hours and a mean terminal half-life (t1/2) of 21 hours. The t1/2 of Aranesp was approximately 3-fold longer than that of epoetin alfa when administered intravenously.
Following subcutaneous administration of Aranesp to patients with CKD (receiving or not receiving dialysis), absorption was slow and Cmax occurred at 48 hours (range: 12 to 72 hours). In patients with CKD receiving dialysis, the average t1/2 was 46 hours (range: 12 to 89 hours), and in patients with CKD not receiving dialysis, the average t1/2 was 70 hours (range: 35 to 139 hours). Aranesp apparent clearance was approximately 1.4 times faster on average in patients receiving dialysis compared to patients not receiving dialysis. The bioavailability of Aranesp in patients with CKD receiving dialysis after subcutaneous administration was 37% (range: 30% to 50%).
Pediatric Patients with CKD
Aranesp pharmacokinetics was studied in 12 pediatric patients (age 3 to 16 years) with CKD receiving or not receiving dialysis. Following a single intravenous or subcutaneous Aranesp dose, Cmax and t1/2 were similar to those obtained in adult patients with CKD on dialysis. Following a single subcutaneous dose, the average bioavailability was 54% (range: 32% to 70%), which was higher than that obtained in adult patients with CKD on dialysis.
Adult Cancer Patients
Following the first subcutaneous dose of 6.75 mcg/kg (equivalent to 500 mcg for a 74-kg patient) in patients with cancer, the mean t1/2 was 74 hours (range: 24 to 144 hours) and Cmax was observed at 71 hours (range: 28 to 120 hours). When administered on a once every 3 week schedule, 48-hour postdose Aranesp levels after the fourth dose were similar to those after the first dose.
Over the dose range of 0.45 to 4.5 mcg/kg Aranesp administered intravenously or subcutaneously on a once weekly schedule and 4.5 to 15 mcg/kg administered subcutaneously on a once every 3 week schedule, systemic exposure was approximately proportional to dose. No evidence of accumulation was observed beyond an expected less than 2-fold increase in blood levels when compared to the initial dose.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity
The carcinogenic potential of Aranesp has not been evaluated in long-term animal studies. In toxicity studies of approximately 6 months duration in rats and dogs, no tumorigenic or unexpected mitogenic responses were observed in any tissue type.
Mutagenicity
Aranesp was not mutagenic or clastogenic under the conditions tested. Aranesp was negative in the in vitro bacterial reverse mutation assay, the in vitro mammalian cell gene mutation assay (using CHO cells), and in the in vivo mouse erythrocyte micronucleus assay.
Impairment of Fertility
Aranesp increased the incidence of post-implantation losses in rats. Male and female rats received intravenous doses prior to and during mating; then females were treated 3 times weekly during the first trimester of gestation (gestation days 1, 3, 5, and 7). No effect on reproductive performance, fertility, or sperm assessment parameters were detected at any of the doses evaluated (up to 10 mcg/kg, administered 3 times weekly). The dose of 10 mcg/kg is more than 10-fold higher than the clinical recommended starting dose. An increase in post-implantation fetal loss was seen at doses equal to or greater than 0.5 mcg/kg, administered 3 times weekly. The dose of 0.5 mcg/kg is approximately equivalent to the clinical recommended starting dose. Signs of exaggerated pharmacology were not observed in the mother receiving 0.5 mcg/kg or less, but were observed at 2.5 mcg/kg and higher.
13.3 Reproductive and Developmental Toxicology
When Aranesp was administered intravenously during organogenesis to pregnant rats (gestational days 6 to 15) and rabbits (gestational days 6 to 18), no evidence of direct embryotoxic, fetotoxic, or teratogenic outcomes were observed at the doses tested, up to 20 mcg/kg/day. This animal dose level of 20 mcg/kg/day is approximately 20-fold higher than the clinical recommended starting dose, depending on the patient’s treatment indication. The only adverse effect observed was a slight reduction in fetal weight, which occurred only at doses causing exaggerated pharmacological effects in both the rat and rabbit dams (1 mcg/kg/day and higher). No deleterious effects on uterine implantation were seen in either species.
No significant placental transfer of Aranesp was observed in rats; placental transfer was not evaluated in rabbits.
In a peri/postnatal development study, pregnant female rats were treated intravenously with Aranesp day 6 of gestation through day 23 of lactation at 2.5 mcg/kg and higher every other day. Pups of treated mothers had decreased fetal body weights, which correlated with slight increases in the incidences of fetal death, as well as delayed eye opening and delayed preputial separation. The offspring (F1 generation) of the treated rats were observed postnatally; rats from the F1 generation reached maturity and were mated; no Aranesp-related effects were apparent for their offspring (F2 generation fetuses).
14 CLINICAL STUDIES
Clinical studies in the nephrology and chemotherapy-induced anemia clinical programs are designated with the prefixes “N” and “C”, respectively.
14.1 Patients With Chronic Kidney Disease
Patients with chronic kidney disease on dialysis: ESA effects on rates of transfusion
In early clinical studies conducted in CKD patients on dialysis, ESAs have been shown to reduce the use of RBC transfusions. These studies enrolled patients with mean baseline hemoglobin levels of approximately 7.5 g/dL and ESAs were generally titrated to achieve a hemoglobin level of approximately 12 g/dL. Fewer transfusions were given during the ESA treatment period when compared to a pre-treatment interval.
In the Normal Hematocrit Study, the yearly transfusion rate was 51.5% in the lower hemoglobin group (10 g/dL) and 32.4% in the higher hemoglobin group (14 g/dL).
Patients with chronic kidney disease not on dialysis: ESA effects on rates of transfusion
In TREAT, a randomized, double-blind trial of 4038 patients with CKD and type 2 diabetes not on dialysis, a post-hoc analysis showed that the proportion of patients receiving RBC transfusions was lower in patients administered Aranesp to target a hemoglobin of 13 g/dL compared to the control arm in which Aranesp was administered intermittently if hemoglobin concentration decreased to less than 9 g/dL (15% versus 25%, respectively). In CHOIR, a randomized open-label study of 1432 patients with CKD not on dialysis, use of an ESA to target a higher (13.5 g/dL) versus lower (11.3 g/dL) hemoglobin goal did not reduce the use of RBC transfusions. In each trial, no benefits occurred for the cardiovascular or end-stage renal disease outcomes. In each trial, the potential benefit of ESA therapy was offset by worse cardiovascular safety outcomes resulting in an unfavorable benefit-risk profile [see Warnings and Precautions (5.1)].
ESA Effects on quality of life
Aranesp use has not been demonstrated in controlled clinical trials to improve quality of life, fatigue, or patient well-being.
ESA Effects on rates of death and other serious cardiac adverse events
Three randomized outcome trials (Normal Hematocrit Study [NHS], Correction of Anemia with Epoetin Alfa in Chronic Kidney Disease [CHOIR], and Trial of Darbepoetin Alfa in Type 2 Diabetes and CKD [TREAT]) have been conducted in patients with CKD using Epogen/PROCRIT/Aranesp to target higher vs. lower hemoglobin levels. Though these trials were designed to establish a cardiovascular or renal benefit of targeting higher hemoglobin levels, in all 3 studies, patients randomized to the higher hemoglobin target experienced worse cardiovascular outcomes and showed no reduction in progression to ESRD. In each trial, the potential benefit of ESA therapy was offset by worse cardiovascular safety outcomes resulting in an unfavorable benefit-risk profile [see Warnings and Precautions (5.1)].
Other ESA trials
Two studies evaluated the safety and efficacy of the de novo use of Aranesp for the correction of anemia in adult patients with CKD, and 3 studies (2 in adults and 1 in pediatric patients) assessed the ability of Aranesp to maintain hemoglobin concentrations in patients with CKD who had been receiving other recombinant erythropoietins.
De Novo Use of Aranesp
Once Weekly Aranesp Starting Dose
In 2 randomized, open-label studies, Aranesp or epoetin alfa was administered for the correction of anemia in patients with CKD who had not been receiving prior treatment with exogenous erythropoietin. Study N1 evaluated CKD patients receiving dialysis; Study N2 evaluated patients not requiring dialysis. In both studies, the starting dose of Aranesp was 0.45 mcg/kg administered once weekly. The starting dose of epoetin alfa was 50 Units/kg 3 times weekly in Study N1 and 50 Units/kg twice weekly in Study N2. When necessary, dosage adjustments were instituted to maintain hemoglobin in the study target range of 11 to 13 g/dL. (Note: The recommended hemoglobin target range is lower than the target range of these studies [see Dosage and Administration (2.2)].) The primary efficacy endpoint was the proportion of patients who experienced at least a 1 g/dL increase in hemoglobin concentration to a level of at least 11 g/dL by 20 weeks (Study N1) or 24 weeks (Study N2). The studies were designed to assess the safety and effectiveness of Aranesp but not to support conclusions regarding comparisons between the 2 products.
In Study N1, the primary efficacy endpoint was achieved by 72% (95% CI: 62%, 81%) of the 90 patients treated with Aranesp and 84% (95% CI: 66%, 95%) of the 31 patients treated with epoetin alfa. The mean increase in hemoglobin over the initial 4 weeks of Aranesp treatment was 1.1 g/dL (95% CI: 0.82 g/dL, 1.37 g/dL).
In Study N2, the primary efficacy endpoint was achieved by 93% (95% CI: 87%, 97%) of the 129 patients treated with Aranesp and 92% (95% CI: 78%, 98%) of the 37 patients treated with epoetin alfa. The mean increase in hemoglobin from baseline through the initial 4 weeks of Aranesp treatment was 1.38 g/dL (95% CI: 1.21 g/dL, 1.55 g/dL).
Once Every 2 Week Aranesp Starting Dose
In 2 single-arm studies (N3 and N4), Aranesp was administered for the correction of anemia in CKD patients not receiving dialysis. In both studies, the starting dose of Aranesp was 0.75 mcg/kg administered once every 2 weeks.
In Study N3 (study duration of 18 weeks), the hemoglobin goal (hemoglobin concentration ≥ 11 g/dL) was achieved by 92% (95% CI: 86%, 96%) of the 128 patients treated with Aranesp.
In Study N4 (study duration of 24 weeks), the hemoglobin goal (hemoglobin concentration of 11 to 13 g/dL) was achieved by 85% (95% CI: 77%, 93%) of the 75 patients treated with Aranesp.
Conversion from Other Recombinant Erythropoietins
Two studies of adults (N5 and N6) and 1 study in pediatric patients (N7) were conducted in patients who had been receiving other recombinant erythropoietins for treatment of the anemia due to CKD. The studies compared the abilities of Aranesp and other erythropoietins to maintain hemoglobin concentrations within a study target range of 9 to 13 g/dL in adults and 10 to 12.5 g/dL in pediatric patients. (Note: The recommended hemoglobin target is lower than the target range of these studies [see Dosage and Administration (2.2)].) Patients who had been receiving stable doses of other recombinant erythropoietins were randomized to Aranesp or continued with their prior erythropoietin at the previous dose and schedule. For patients randomized to Aranesp, the initial weekly dose was determined on the basis of the previous total weekly dose of recombinant erythropoietin.
Adult Patients
Study N5 was a double-blind study in which 169 hemodialysis patients were randomized to treatment with Aranesp and 338 patients continued on epoetin alfa. Study N6 was an open-label study in which 347 patients were randomized to treatment with Aranesp and 175 patients were randomized to continue on epoetin alfa or epoetin beta. Of the patients randomized to Aranesp, 92% were receiving hemodialysis and 8% were receiving peritoneal dialysis.
In Study N5, a median weekly dose of 0.53 mcg/kg Aranesp (25th, 75th percentiles: 0.30, 0.93 mcg/kg) was required to maintain hemoglobin in the study target range. In Study N6, a median weekly dose of 0.41 mcg/kg Aranesp (25th, 75th percentiles: 0.26, 0.65 mcg/kg) was required to maintain hemoglobin in the study target range.
Pediatric Patients
Study N7 was an open-label, randomized study conducted in the United States in pediatric patients from 1 to 18 years of age with CKD receiving or not receiving dialysis. Eighty-one patients with hemoglobin concentrations that were stable on epoetin alfa received darbepoetin alfa (subcutaneously or intravenously), and 42 patients continued to receive epoetin alfa at the current dose, schedule, and route of administration. Patients received darbepoetin alfa once weekly if previously receiving epoetin alfa 2 or 3 times weekly or once every other week if previously receiving epoetin alfa weekly. A median weekly dose of 0.41 mcg/kg darbepoetin alfa (25th, 75th percentiles: 0.25, 0.82 mcg/kg) was required to maintain hemoglobin in the study target range.
14.2 Cancer Patients Receiving Chemotherapy
The safety and efficacy of Aranesp was assessed in two multicenter, randomized studies in patients with anemia due to the effect of concomitantly administered cancer chemotherapy. Study C1 was a randomized (1:1), placebo-controlled, double-blind, multinational study conducted in 314 patients where Aranesp was administered weekly. Study C2 was a randomized (1:1), double-blind, double-dummy, active-controlled, multinational study conducted in 705 patients where Aranesp was administered either every week or every 3 weeks. Efficacy was demonstrated by a statistically significant reduction in the proportion of patients receiving RBC transfusions among patients who were on study therapy for more than 28 days.
Study C1
Study C1 was conducted in anemic patients (hemoglobin ≤ 11 g/dL) with non-small cell lung cancer or small cell lung cancer who were scheduled to receive at least 12 weeks of a platinum-containing chemotherapy regimen. Randomization was stratified by tumor type and region (Australia vs. Canada vs. Europe). Patients received Aranesp 2.25 mcg/kg or placebo as a weekly subcutaneous injection commencing on the first day of the chemotherapy cycle. Efficacy was determined by a reduction in the proportion of patients who received RBC transfusions between week 5 (day 29) and end of treatment period (12 weeks) in the subset of 297 randomized patients (148 Aranesp and 149 placebo) who were on-study at the beginning of study week 5. All 297 patients were white, 72% were male, 71% had non-small cell histology, and the median age was 62 years (range: 36 to 80). A significantly lower proportion of patients in the Aranesp arm received RBC transfusions during week 5 to the end of treatment compared to patients in the placebo arm (crude percentages: 26% vs. 50%; p < 0.001, based on a comparison of the difference in Kaplan-Meier proportions using the Cochran-Mantel-Haenszel strata-adjusted Chi-square test).
Study C2
Study C2 was conducted in anemic patients (hemoglobin < 11 g/dL) with non-myeloid malignancies receiving chemotherapy. Randomization was stratified by region (Western vs. Central/Eastern Europe), tumor type (lung and gynecological vs. others), and baseline hemoglobin (< 10 vs. ≥ 10 g/dL); all patients received double-dummy placebo and either Aranesp 500 mcg every 3 weeks or Aranesp 2.25 mcg/kg weekly subcutaneous injections for 15 weeks. Only 1 patient was non-white, 55% were female, and the median age was 60 years (range: 20 to 86). One hundred seven patients (16%) had lung or gynecological cancer while 565 (84%) had other tumor types. In both treatment schedules, the dose was reduced by 40% of the previous dose if hemoglobin level increased by more than 1 g/dL in a 14-day period.
Efficacy was determined by a comparison of the proportion of patients who received at least 1 RBC transfusion between week 5 (day 29) and the end of treatment. Three hundred thirty-five patients in the every 3 week dosing arm and 337 patients in the weekly dosing arm remained on study through or beyond day 29 and were evaluable for efficacy. Two hundred thirty-eight patients (71%) in the every 3 week arm and 261 patients (77%) patients in the weekly arm required dose reductions. Twenty-three percent (95% CI: 18%, 28%) of patients in the every 3 week treatment schedule and 28% (95% CI: 24%, 34%) in the weekly schedule received at least 1 RBC transfusion. The observed difference in the RBC transfusion rates (every 3 week minus weekly) was -5.8% (95% CI: -12.4%, 0.8%).
Study C3
Lack of Efficacy in Improving Survival
Study C3 was conducted in patients required to have a hemoglobin concentration ≥ 9 g/dL and ≤ 13 g/dL with previously untreated extensive-stage small cell lung cancer (SCLC) receiving platinum and etoposide chemotherapy. Randomization was stratified by region (Western Europe, Australia/North America, and rest of world), Eastern Cooperative Oncology Group (ECOG) performance status (0 or 1 vs. 2), and lactate dehydrogenase (below vs. above the upper limit of normal). Patients were randomized to receive Aranesp (n = 298) at a dose of 300 mcg once weekly for the first 4 weeks, followed by 300 mcg once every 3 weeks for the remainder of the treatment period or placebo (n = 298).
This study was designed to detect a prolongation in overall survival (from a median of 9 months to a median of 12 months). For the final analysis, there was no evidence of improved survival (p=0.43, log-rank test).
16 HOW SUPPLIED/STORAGE AND HANDLING
Store at 36°F to 46°F (2°C to 8°C). Do not freeze.
Do not shake. Protect from light; store Aranesp in the carton until use.
Do not use Aranesp that has been shaken or frozen.
Aranesp is available in the following packages:
Single-dose Vial
| 1 Vial/Pack, 4 Packs/Case | 4 Vials/Pack, 10 Packs/Case |
Single-dose Prefilled Syringe (SingleJect®) with a 27-gauge, ½-inch needle with an UltraSafe® Needle Guard that is manually activated to cover the needle during disposal
| 1 Syringe/Pack, 4 Packs/Case | 4 Syringes/Pack, 10 Packs/Case |
| 200 mcg/0.4 mL (NDC 54868-5428-0) 300 mcg/0.6 mL 500 mcg/1 mL | 25 mcg/0.42 mL 40 mcg/0.4 mL 60 mcg/0.3 mL 100 mcg/0.5 mL |
17 PATIENT COUNSELING INFORMATION
See Medication Guide.
Prior to treatment, inform patients of the risks and benefits of Aranesp.
Inform patients with cancer that they must sign the patient-healthcare provider acknowledgment form before the start of each treatment course with Aranesp and that healthcare providers must enroll and comply with the ESA APPRISE Oncology Program in order to prescribe Aranesp.
Inform patients:
- To read the Medication Guide.
- Of the increased risks of mortality, serious cardiovascular reactions, thromboembolic reactions, stroke, and tumor progression [see Warnings and Precautions (5.1, 5.3)]
- To undergo regular blood pressure monitoring, adhere to prescribed anti-hypertensive regimen and follow recommended dietary restrictions.
- To contact their healthcare provider for new-onset neurologic symptoms or change in seizure frequency.
- Of the need to have regular laboratory tests for hemoglobin.
Instruct patients who self-administer Aranesp of the:
- Importance of following the Instructions for Use.
- Dangers of reusing needles, syringes, or unused portions of single-dose vials.
- Proper disposal of used syringes, needles, and unused vials, and of the full container.

Aranesp® (darbepoetin alfa)
Manufactured by:
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, CA 91320-1799 U.S.A.
Patent: http://pat.amgen.com/aranesp/
©2001-2013 Amgen Inc. All rights reserved.
* UltraSafe® is a registered trademark of Safety Syringes, Inc.
1xxxxxx- v28
PMV 28
MEDICATION GUIDE
-
Aranesp® (Air-uh-nesp)
(darbepoetin alfa)
Read this Medication Guide:
- before you start Aranesp.
- if you are told by your healthcare provider that there is new information about Aranesp.
- if you are told by your healthcare provider that you may inject Aranesp at home, read this Medication Guide each time you receive a new supply of medicine.
This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment. Talk with your healthcare provider regularly about the use of Aranesp and ask if there is new information about Aranesp.
What is the most important information I should know about Aranesp?
Aranesp may cause serious side effects that can lead to death, including:
For people with cancer:
- Your tumor may grow faster and you may die sooner if you choose to take Aranesp. Your healthcare provider has received special training in order to prescribe Aranesp and will talk with you in detail about these risks.
For all people who take Aranesp, including people with cancer or chronic kidney disease:
- Serious heart problems, such as heart attack or heart failure, and stroke. You may die sooner if you are treated with Aranesp to increase red blood cells (RBCs) to near the same level found in healthy people.
- Blood clots. Blood clots may happen at any time while taking Aranesp. If you are receiving Aranesp for any reason and you are going to have surgery, talk to your healthcare provider about whether or not you need to take a blood thinner to lessen the chance of blood clots during or following surgery. Clots can form in blood vessels (veins), especially in your leg (deep venous thrombosis or DVT). Pieces of a blood clot may travel to the lungs and block the blood circulation in the lungs (pulmonary embolus).
- Call your healthcare provider or get medical help right away if you have any of these symptoms:
- Chest pain
- Trouble breathing or shortness of breath
- Pain in your legs, with or without swelling
- A cool or pale arm or leg
- Sudden confusion, trouble speaking, or trouble understanding others’ speech
- Sudden numbness or weakness in your face, arm, or leg, especially on one side of your body
- Sudden trouble seeing
- Sudden trouble walking, dizziness, loss of balance or coordination
- Loss of consciousness (fainting)
- Hemodialysis vascular access stops working
See “What are the possible side effects of Aranesp?” below for more information.
If you decide to take Aranesp, your healthcare provider should prescribe the smallest dose of Aranesp that is necessary to reduce your chance of needing red blood cell transfusions.
What is Aranesp?
Aranesp is a prescription medicine used to treat anemia. People with anemia have a lower-than-normal number of RBCs. Aranesp works like the human protein called erythropoietin to help your body make more RBCs. Aranesp is used to reduce or avoid the need for RBC transfusions.
Aranesp may be used to treat anemia if it is caused by:
- Chronic kidney disease (you may or may not be on dialysis).
- Chemotherapy that will be used for at least two months after starting Aranesp.
If your hemoglobin level stays too high or if your hemoglobin goes up too quickly, this may lead to serious health problems which may result in death. These serious health problems may happen if you take Aranesp, even if you do not have an increase in your hemoglobin level.
Aranesp should not be used for the treatment of anemia:
- If you have cancer and you will not be receiving chemotherapy that may cause anemia.
- If you have a cancer that has a high chance of being cured. Talk with your healthcare provider about the kind of cancer you have.
- In place of emergency treatment for anemia (RBC transfusions).
Aranesp has not been proven to improve the quality of life, fatigue, or well-being.
Who should not take Aranesp?
Do not take Aranesp if you:
- Have cancer and have not been counseled by your healthcare provider about treatment with Aranesp.
- Have high blood pressure that is not controlled (uncontrolled hypertension).
- Have been told by your healthcare provider that you have or have ever had a type of anemia called Pure Red Cell Aplasia (PRCA) that starts after treatment with Aranesp or other erythropoietin protein medicines.
- Have had a serious allergic reaction to Aranesp.
What should I tell my healthcare provider before taking Aranesp?
Aranesp may not be right for you. Tell your healthcare provider about all your health conditions, including if you:
- Have heart disease.
- Have high blood pressure.
- Have had a seizure (convulsion) or stroke.
- Are allergic to latex.
- Have any other medical conditions.
- Are pregnant or planning to become pregnant. It is not known if Aranesp may harm your unborn baby. Talk to your healthcare provider about possible pregnancy and birth control choices that are right for you. If you are pregnant, discuss with your healthcare provider about enrolling in Amgen's Pregnancy Surveillance Program or call 1-800-772-6436 (l-800-77-AMGEN).
- Are breastfeeding or planning to breastfeed. It is not known if Aranesp passes into breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and nonprescription medicines, vitamins, and herbal supplements.
Know the medicines you take. Keep a list of your medicines with you and show it to your healthcare provider when you get a new medicine.
How should I take Aranesp?
- If you or your caregiver has been trained to give Aranesp shots (injections) at home:
- Be sure that you read, understand, and follow the “Instructions for Use” that come with Aranesp.
- Take Aranesp exactly as your healthcare provider tells you to. Do not change the dose of Aranesp unless told to do so by your healthcare provider.
- Your healthcare provider will show you how much Aranesp to use, how to inject it, how often it should be injected, and how to safely throw away the used vials, syringes, and needles.
- If you miss a dose of Aranesp, call your healthcare provider right away and ask what to do.
- If you take more than the prescribed amount of Aranesp, call your healthcare provider right away.
- During treatment with Aranesp, continue to follow your healthcare provider’s instructions for diet and medicines.
- Have your blood pressure checked as instructed by your healthcare provider.
What are the possible side effects of Aranesp?
Aranesp may cause serious side effects.
- See “What is the most important information I should know about Aranesp?”
- High blood pressure. High blood pressure is a common side effect of Aranesp in patients with chronic kidney disease. Your blood pressure may go up or be difficult to control with blood pressure medicine while taking Aranesp. This can happen even if you have never had high blood pressure before. Your healthcare provider should check your blood pressure often. If your blood pressure does go up, your healthcare provider may prescribe new or more blood pressure medicine.
- Seizures. If you have any seizures while taking Aranesp, get medical help right away and tell your healthcare provider.
- Antibodies to Aranesp. Your body may make antibodies to Aranesp. These antibodies can block or lessen your body’s ability to make RBCs and cause you to have severe anemia. Call your healthcare provider if you have unusual tiredness, lack of energy, dizziness, or fainting. You may need to stop taking Aranesp.
- Serious allergic reactions. Serious allergic reactions can cause a rash over your whole body, shortness of breath, wheezing, dizziness and fainting because of a drop in blood pressure, swelling around your mouth or eyes, fast pulse, or sweating. If you have a serious allergic reaction, stop using Aranesp and call your healthcare provider or get medical help right away.
The needle cover on the prefilled syringe contains latex. If you know you are allergic to latex, talk to your healthcare provider before using Aranesp.
Common side effects of Aranesp include:
- shortness of breath
- cough
- low blood pressure during dialysis
- abdominal pain
- edema (swelling) of the arms or legs
These are not all of the possible side effects of Aranesp. Your healthcare provider can give you a more complete list. Tell your healthcare provider about any side effects that bother you or that do not go away.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store Aranesp?
- Do not shake Aranesp.
- Protect Aranesp from light.
- Store Aranesp in the refrigerator between 36°F to 46°F (2°C to 8°C).
- Do not freeze Aranesp. Do not use Aranesp that has been frozen.
- Throw away the Aranesp vial or prefilled syringe after one use. Do not re-use even if there is medicine left.
Keep Aranesp and all medicines out of the reach of children.
General information about Aranesp
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Use Aranesp only for the condition for which it has been prescribed. Do not give Aranesp to other patients even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about Aranesp. If you would like more information about Aranesp, talk with your healthcare provider. You can ask your healthcare provider or pharmacist for information about Aranesp that is written for healthcare professionals. For more information, go to the following website: www.aranesp.com or call 1-800-77-AMGEN.
What are the ingredients in Aranesp?
Active Ingredient: darbepoetin alfa
Inactive Ingredients: polysorbate 80, sodium phosphate monobasic monohydrate, sodium phosphate dibasic anhydrous, and sodium chloride in Water for Injection, USP.
This Medication Guide has been approved by the U.S. Food and Drug Administration.

Manufactured by:
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, CA 91320-1799 U.S.A.
Revised: 12/2013
© 2001-2013 Amgen Inc. All rights reserved.
1xxxxxx – v5
PMV 5
Instructions for Use
Aranesp® (Air-uh-nesp)
(darbepoetin alfa)
Single-Dose Vial
Use these Instructions for Use if you or your caregiver has been trained to give Aranesp injections at home. Do not give yourself the injection unless you have received training from your healthcare provider. If you are not sure about giving the injection or if you have questions, ask your healthcare provider for help.
Before reading these Instructions for Use, read the Medication Guide that comes with Aranesp for the most important information you need to know.
When you receive your Aranesp vial and syringes make sure that:
- The name Aranesp appears on the carton and vial label.
- The expiration date on the vial label has not passed. Do not use a vial of Aranesp after the expiration date on the label.
- The dose strength of the Aranesp vial (number of micrograms [mcg] in the colored square on the package and on the vial label) is the same as your healthcare provider prescribed.
- The Aranesp liquid in the vial is clear and colorless. Do not use Aranesp if the liquid in the vial looks discolored or cloudy, or if the liquid has lumps, flakes, or particles.
- The Aranesp vial has a color cap on the top of the vial. Do not use a vial of Aranesp if the color cap on the top of the vial has been removed or is missing.
- Use only the type of disposable syringe and needle that your healthcare provider has prescribed.
- Do not shake Aranesp. Shaking could cause Aranesp not to work. If you shake Aranesp, the solution in the vial may look foamy and should not be used.
- Do not freeze Aranesp. Do not use a vial of Aranesp that has been frozen.
- Store Aranesp in the refrigerator between 36°F to 46°F (2°C to 8°C).
- Keep Aranesp away from light.
- Single-dose vials of Aranesp should be used only one time. Throw the vial away after use even if there is medicine left in the vial.
How should I prepare for an injection of Aranesp?
- Always keep an extra syringe and needle on hand.
- Follow your healthcare provider’s instructions on how to measure your dose of Aranesp. This dose will be measured in milliliter (mL) or cc (1 mL is the same as 1 cc). Use a syringe that is marked in tenths of mL (for example, 0.2 mL or 0.2 cc). Using the wrong syringe can lead to a mistake in your dose and you could inject too much or too little Aranesp.
Only use disposable syringes and needles. Use the syringes and needles only one time and then throw them away as instructed by your healthcare provider.
Important: Follow these instructions exactly to help avoid infections.
Preparing the dose:
- Remove the vial of Aranesp from the refrigerator. During this time, protect the solution from light. Keep the vial in its carton until you are ready to prepare the dose. Do not leave the vial in light.
- Do not use a single-dose vial of Aranesp more than one time.
- Do not shake Aranesp.
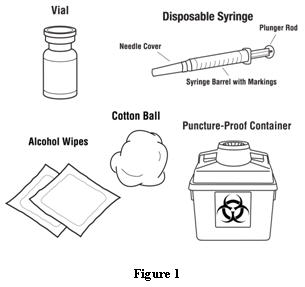
- Gather the other supplies you will need for your injection (vial, syringe, alcohol wipes, cotton ball, and a puncture-proof container for throwing away the syringe and needle). See Figure 1.
- Check the date on the Aranesp vial to be sure that the drug has not expired.
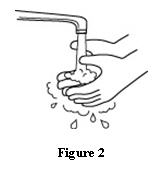
- Wash your hands well with soap and water before preparing the medicine. See Figure 2.
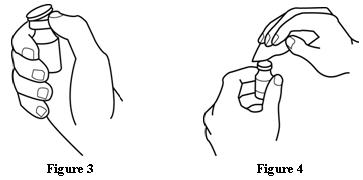
- Flip off the protective color cap on the top of the vial. Do not remove the grey rubber stopper. Wipe the top of the grey rubber stopper with an alcohol wipe. See Figures 3 and 4.
- Check the package containing the syringe. If the package has been opened or damaged, do not use that syringe. Throw away the syringe in the puncture-proof disposable container. If the syringe package is undamaged, open the package and remove the syringe.
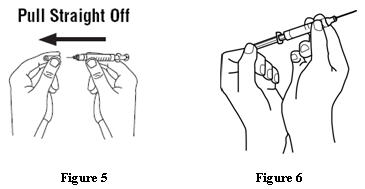
- Using a syringe and needle that has been recommended by your healthcare provider, carefully remove the needle cover. See Figure 5. Then draw air into the syringe by pulling back on the plunger. The amount of air drawn into the syringe should be equal to the amount (mL or cc) of the Aranesp dose prescribed by your healthcare provider. See Figure 6.
- With the vial on a flat work surface, insert the needle straight down through the grey rubber stopper of the Aranesp vial. See Figure 7.
- Push the plunger of the syringe down to inject the air from the syringe into the vial of Aranesp. The air injected into the vial will allow Aranesp to be easily withdrawn into the syringe. See Figure 7.
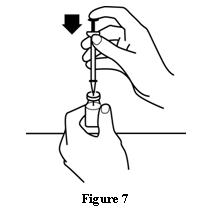
- Keep the needle inside the vial. Turn the vial and syringe upside down. Be sure the tip of the needle is in the Aranesp liquid. Keep the vial upside down. Slowly pull back on the plunger to fill the syringe with Aranesp liquid to the number (mL or cc) that matches the dose your healthcare provider prescribed. See Figure 8.
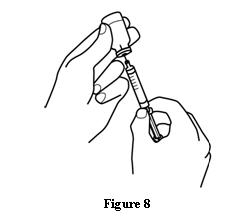
- Keep the needle in the vial. Check for air bubbles in the syringe. A small amount of air is harmless. Too large an air bubble will give you the wrong Aranesp dose. To remove air bubbles, gently tap the syringe with your fingers until the air bubbles rise to the top of the syringe. Slowly push the plunger up to force the air bubbles out of the syringe. Keep the tip of the needle in the Aranesp liquid. Pull the plunger back to the number on the syringe that matches your dose. Check again for air bubbles. If there are still air bubbles, repeat the steps above to remove them. See Figures 9 and 10.
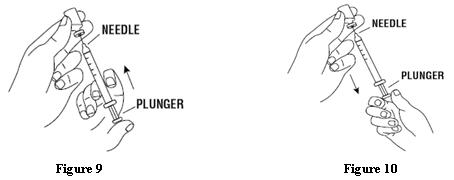
- Double-check that you have the correct dose in the syringe. Lay the vial down on its side with the needle still in it until after you have selected and prepared a site for injection.
Selecting and preparing the injection site:
Aranesp can be injected into your body using two different ways (routes) as described below. Follow your healthcare provider’s instructions about how you should inject Aranesp. In patients on hemodialysis, the intravenous (IV) route is recommended.
1. Subcutaneous Route:
- Aranesp can be injected directly into a layer of fat under your skin. This is called a subcutaneous injection. When giving subcutaneous injections, follow your healthcare provider’s instructions about changing the site for each injection. You may wish to write down the site where you have injected.
- Do not inject Aranesp into an area that is tender, red, bruised, hard, or has scars or stretch marks. Recommended sites for injection are shown in Figure 11 below, including:
- The outer area of the upper arms
- The abdomen (except for the 2-inch area around the navel)
- The front of the middle thighs
- The upper outer area of the buttocks
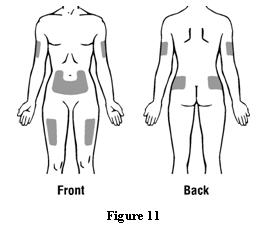
- Clean the skin with an alcohol wipe where the injection is to be made. Be careful not to touch the skin that has been wiped clean. See Figure 12.
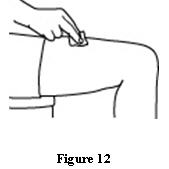
- Double-check that the correct amount of Aranesp is in the syringe.
- Remove the prepared syringe and needle from the vial of Aranesp and hold it in the hand that you will use to inject the medicine.
- Use the other hand to pinch a fold of skin at the cleaned injection site. Do not touch the cleaned area of skin. See Figure 13.
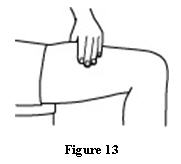
- Hold the syringe like you would hold a pencil. Use a quick “dart-like” motion to insert the needle either straight up and down (90-degree angle) or at a slight angle (45 degrees) into the skin. Inject the prescribed dose subcutaneously as directed by your doctor, nurse, or pharmacist. See Figure 14.
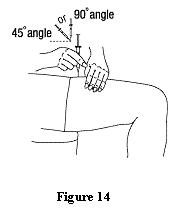
- Pull the needle out of the skin and press a cotton ball or gauze over the injection site and hold it there for several seconds. Do not recap the needle.
- Dispose of the used syringe and needle as described below. Do not reuse syringes and needles.
2. Intravenous Route:
- Aranesp can be injected in your vein through a special access port placed by your healthcare provider. This type of Aranesp injection is called an intravenous (IV) injection. This route is usually for hemodialysis patients.
- If you have a dialysis vascular access, make sure it is working by checking it as your healthcare provider has shown you. Be sure to let your healthcare provider know right away if you are having any problems, or if you have any questions.
- Wipe off the venous port of the hemodialysis tubing with an alcohol wipe. See Figure 15.
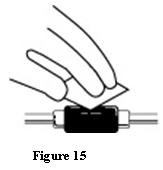
- Insert the needle of the syringe into the cleaned venous port and push the plunger all the way down to inject all the Aranesp. See Figure 16.
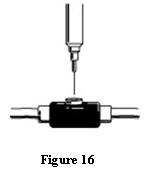
- Remove the syringe from the venous port. Do not recap the needle.
- Dispose of the used syringe and needle as described below.
How should I dispose of the vials, syringes, and needles?
Do not reuse the single-dose vials, syringes, or needles. Throw away the vials, syringes, and needles as instructed by your healthcare provider or by following these steps:
- Do not throw the vials, syringes, or needles in the household trash or recycle.
- Do not put the needle cover back on the needle.
- Place all used needles and syringes in a puncture-proof disposable container with a lid. Do not use glass or clear plastic containers, or any container that will be recycled or returned to a store.
- Keep the puncture-proof disposable container out of the reach of children.
- When the puncture-proof disposable container is full, tape around the cap or lid to make sure the cap or lid does not come off. Throw away the puncture-proof disposable container as instructed by your healthcare provider. There may be special state and local laws for disposing of used needles and syringes. Do not throw the puncture-proof disposable container in the household trash. Do not recycle.
Keep Aranesp and all medicines out of reach of children.
These Instructions for Use have been approved by the U.S. Food and Drug Administration.

Manufactured by:
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, CA 91320-1799 U.S.A.
Revised: 05/2012
©2001-2012 Amgen Inc. All rights reserved.
1xxxxxx - v3
PMV 3
Instructions for Use
Aranesp® (Air-uh-nesp)
(darbepoetin alfa)
Single-Dose Prefilled Syringe (SingleJect®)
Use these Instructions for Use if you or your caregiver has been trained to give Aranesp injections at home. Do not give yourself the injection unless you have received training from your healthcare provider. If you are not sure about giving the injection or if you have questions, ask your healthcare provider for help.
Before reading these Instructions for Use, read the Medication Guide that comes with Aranesp for the most important information you need to know.
When you receive your Aranesp prefilled syringe make sure that:
- The name Aranesp appears on the carton and prefilled syringe label.
- The expiration date on the prefilled syringe label has not passed. Do not use a prefilled syringe of Aranesp after the expiration date on the label.
- The dose strength of the Aranesp prefilled syringe (number of micrograms [mcg] in the colored square on the package and on the prefilled syringe label) is the same as your healthcare provider prescribed.
- The Aranesp liquid in the prefilled syringe is clear and colorless. Do not use Aranesp if the liquid in the prefilled syringe looks discolored or cloudy, or if the liquid has lumps, flakes, or particles.
- Do not use Aranesp in a prefilled syringe if the grey cover on the needle is off, or the needle guard (clear yellow plastic sleeve on the syringe) has been pulled to extend over the needle (activated).
- Do not shake Aranesp. Shaking could cause Aranesp not to work. If you shake Aranesp the solution may look foamy and it should not be used.
- Do not freeze Aranesp. Do not use an Aranesp prefilled syringe that has been frozen.
- Store Aranesp in the refrigerator between 36°F to 46°F (2°C to 8°C).
- Keep Aranesp away from light.
How should I prepare for an injection of Aranesp?
Follow your healthcare provider’s instructions on how to measure your dose of Aranesp. This dose will be measured in milliliter (mL) or cc (1 mL is the same as 1 cc).
Use the prefilled syringe only one time and throw it away as instructed by your healthcare provider.
Important: Follow these instructions exactly to help avoid infections.
Preparing the dose:
- Remove one prefilled syringe from the refrigerator. During this time, protect the prefilled syringe from light. Keep the prefilled syringe in its wrapper until you are ready to prepare your dose. Do not leave the prefilled syringe in light.
- Use each Aranesp prefilled syringe only one time.
- Do not shake Aranesp.
- Gather the other supplies you will need for your injection (prefilled syringe with a clear yellow plastic needle guard attached, alcohol wipes, cotton ball, and a puncture-proof container for throwing away the prefilled syringe). See Figure 1.
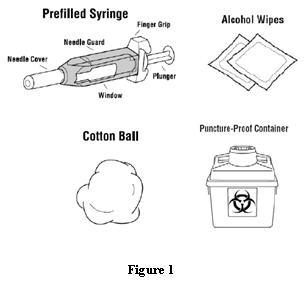
- Check the date on the label on your Aranesp prefilled syringe to be sure that the drug has not expired.
- Wash your hands well with soap and water before preparing the medicine. See Figure 2.
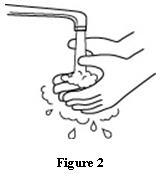
- Open the package and remove the syringe from the tray. Check to see that the needle cover is on and the yellow needle guard is covering the barrel of the syringe. If the needle guard is covering the needle, then it has already been activated. Do not use that syringe. Throw away the syringe in the puncture-proof disposable container. Use a new syringe. Do not slide the needle guard over the needle cover before injection. This will “activate” or lock the needle guard.
- Hold the syringe with the needle pointing up to prevent the Aranesp from leaking out of the needle. Carefully pull the needle cover straight off. See Figure 3.
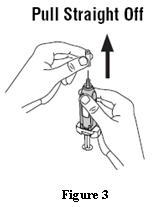
- Check the syringe for air bubbles. If there are air bubbles, gently tap the syringe with your fingers until the air bubbles rise to the top of the syringe. Slowly push the plunger up to force the air bubbles out of the syringe. See Figure 4.
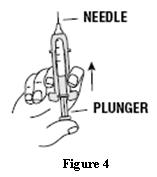
- Keep holding the syringe up. Slowly push the plunger to the line on the syringe that matches the dose your healthcare provider has prescribed.
- Check again to make sure that you have the correct dose in the syringe.
- When you put the syringe down on your work surface, be careful not to let the needle touch anything.
Selecting and preparing the injection site:
Aranesp can be injected into your body using two different ways (routes) as described below. Follow your healthcare provider's instructions about how you should inject Aranesp. For patients on hemodialysis, the intravenous (IV) route is recommended.
1. Subcutaneous Route:
- Aranesp can be injected directly into a layer of fat under your skin. This is called a subcutaneous injection. When giving subcutaneous injections, follow your healthcare provider’s instructions about changing the site for each injection. You may wish to write down the site where you have injected.
- Do not inject Aranesp into an area that is tender, red, bruised, hard, or has scars or stretch marks. Recommended sites for injection are shown in Figure 5 below, including:
- The outer area of the upper arms
- The abdomen (except for the 2-inch area around the navel)
- The front of the middle thighs
- The upper outer area of your buttocks
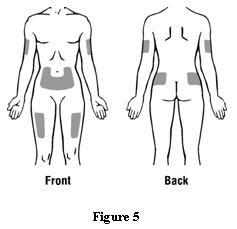
- Clean the skin with an alcohol wipe where the injection is to be made. Be careful not to touch the skin that has been wiped clean. See Figure 6.
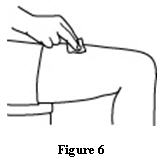
- Hold the prefilled syringe in the hand that you will use to inject the medicine.
- Use the other hand to pinch a fold of skin at the cleaned injection site. Do not touch the cleaned area of skin. See Figure 7. Note: Hold the syringe barrel through the two needle guard windows when giving the injection.
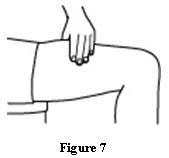
- Hold the syringe like you would hold a pencil. Use a quick “dart-like” motion to insert the needle either straight up and down (90-degree angle) or at a slight angle (45 degrees) into the skin. Inject the prescribed dose subcutaneously as directed by your doctor, nurse, or pharmacist. See Figure 8.
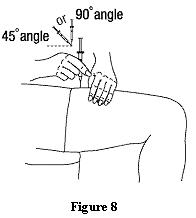
- Pull the needle out of the skin and press a cotton ball or gauze over the injection site and hold it there for several seconds. Do not recap the needle.
- Dispose of the used prefilled syringe as described below. Do not reuse the prefilled syringe.
2. Intravenous Route:
- Aranesp can be injected in your vein through a special access port placed by your healthcare provider. This type of Aranesp injection is called an intravenous (IV) injection. This route is usually for hemodialysis patients.
- If you have a dialysis vascular access, make sure it is working by checking it as your healthcare provider has shown you. Be sure to let your healthcare provider know right away if you are having any problems, or if you have any questions.
- Wipe off the venous port of the hemodialysis tubing with an alcohol wipe. See Figure 9.
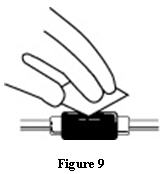
- Insert the needle of the prefilled syringe into the cleaned venous port and push the plunger all the way down to inject all the Aranesp. See Figure 10.

- Remove the prefilled syringe from the venous port. Do not recap the needle.
- Dispose of the used prefilled syringe as described below. Do not reuse the prefilled syringe.
Activation of the needle guard on used prefilled syringes
After injecting Aranesp from the prefilled syringe, do not recap the needle. Keep your hands behind the needle at all times. To activate the needle guard, hold the finger grip of the syringe with one hand and grasp the needle guard with your free hand. Slide the needle guard completely over the needle until the needle guard clicks into place. See Figures 11 and 12. NOTE: If you do not hear a click, the needle guard may not be completely activated.
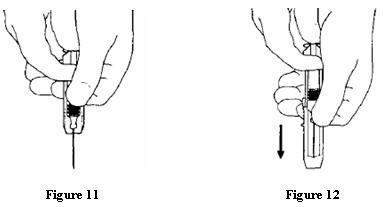
How should I dispose of the prefilled syringe?
Do not reuse the prefilled syringe. Throw away the prefilled syringe with the activated needle guard as directed by your healthcare provider or by following these steps:
- Do not throw the prefilled syringes in the household trash or recycle.
- Do not put the needle cover back on the needle.
- Place the used prefilled syringe in a puncture-proof disposable container with a lid. Do not use glass or clear plastic containers, or any container that will be recycled or returned to a store.
- Keep the puncture-proof disposable container out of the reach of children.
- When the puncture-proof disposable container is full, tape around the cap or lid to make sure the cap or lid does not come off. Throw away the puncture-proof disposable container as instructed by your healthcare provider. There may be special state and local laws for disposing of used prefilled syringes. Do not throw the puncture-proof disposable container in the household trash. Do not recycle.
Keep Aranesp and all medicines out of reach of children.
These Instructions for Use have been approved by the U.S Food and Drug Administration.

Manufactured by:
Amgen Inc.
One Amgen Center Drive
Thousand Oaks, CA 91320-1799 U.S.A.
Revised: 05/2012
©2001-2012 Amgen Inc. All rights reserved.
1xxxxxx - v3
PMV 3
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - PREFILLED SYRINGE, 200 mcg
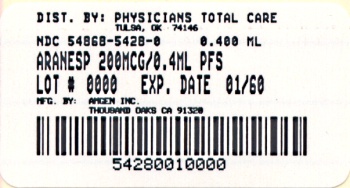
Single Use Prefilled Syringe with 27 Gauge Needle
1 x 200 mcg/0.4 mL Prefilled Syringe
AMGEN ®
Aranesp ® SingleJect ®
(darbepoetin alfa)
recombinant
Albumin Free
200 mcg
200 mcg/0.4 mL
ATTENTION: Enclosed medication guide is required for each patient. For more copies see aranesp.com or call 1-800-77AMGEN.
Store at 2° to 8°C (36° to 46°F).
Do Not Freeze or Shake. Protect from Light.
This Product Contains Dry Natural Rubber.
Rx Only
Manufactured by Amgen Inc. Thousand Oaks, CA 91320-1799 U.S.A.
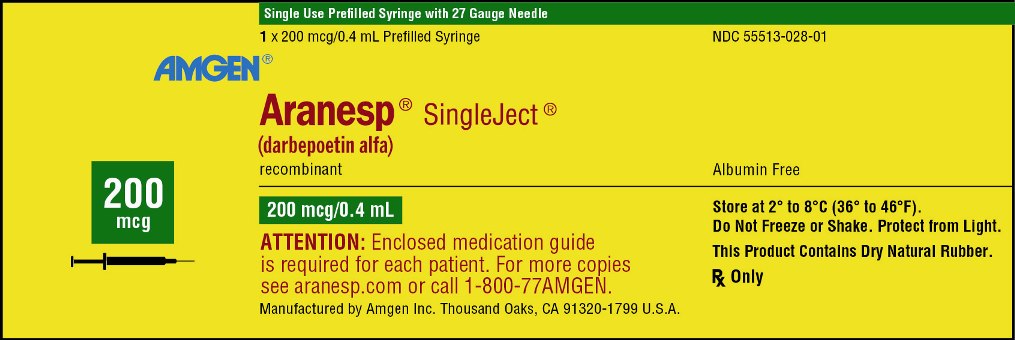
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - PREFILLED SYRINGE, 300 mcg
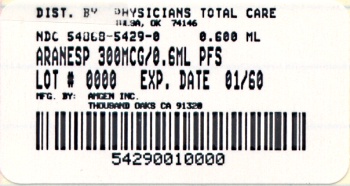
Single Use Prefilled Syringe with 27 Gauge Needle
1 x 300 mcg/0.6 mL Prefilled Syringe
AMGEN ®
Aranesp ® SingleJect ®
(darbepoetin alfa)
recombinant
Albumin Free
300 mcg
300 mcg/0.6 mL
ATTENTION: Enclosed medication guide is required for each patient. For more copies see aranesp.com or call 1-800-77AMGEN.
Store at 2° to 8°C (36° to 46°F).
Do Not Freeze or Shake. Protect from Light.
This Product Contains Dry Natural Rubber.
Rx Only
Manufactured by Amgen Inc. Thousand Oaks, CA 91320-1799 U.S.A.
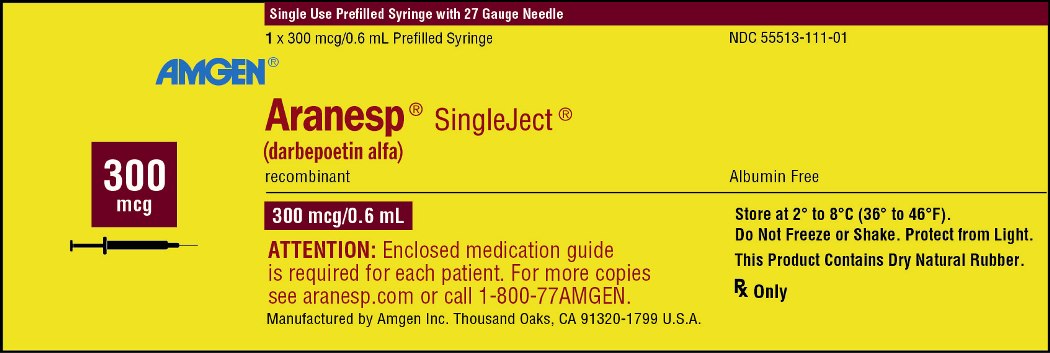
PACKAGE LABEL - PRINCIPAL DISPLAY PANEL - PREFILLED SYRINGE, 500 mcg
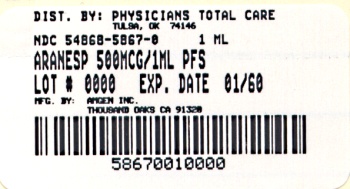
Single Use Prefilled Syringe with 27 Gauge Needle
1 x 500 mcg/1 mL Prefilled Syringe
AMGEN ®
Aranesp ® SingleJect ®
(darbepoetin alfa)
recombinant
Albumin Free
500 mcg
500 mcg/1 mL
ATTENTION: Enclosed medication guide is required for each patient. For more copies see aranesp.com or call 1-800-77AMGEN.
Store at 2° to 8°C (36° to 46°F).
Do Not Freeze or Shake. Protect from Light.
This Product Contains Dry Natural Rubber.
Rx Only
Manufactured by Amgen Inc. Thousand Oaks, CA 91320-1799 U.S.A.
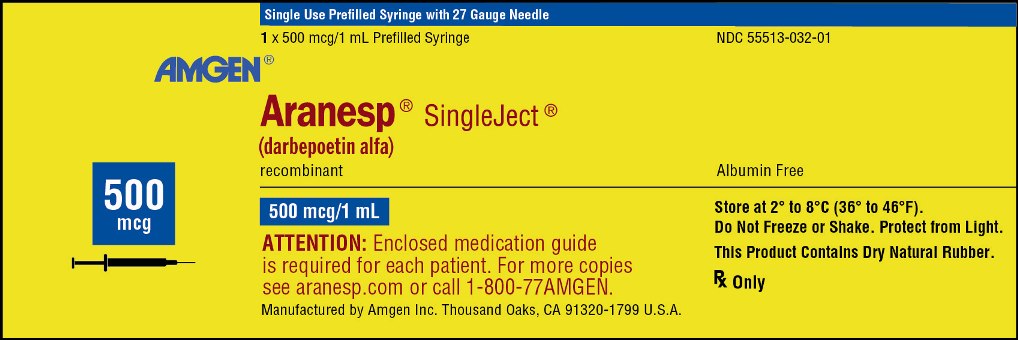
| ARANESP
darbepoetin alfa injection, solution |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| ARANESP
darbepoetin alfa injection, solution |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| ARANESP
darbepoetin alfa injection, solution |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Labeler - Physicians Total Care, Inc. (194123980) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Physicians Total Care, Inc. | 194123980 | relabel(54868-5428, 54868-5429, 54868-5867) | |