Label: TESTOSTERONE solution
- NDC Code(s): 68180-943-11
- Packager: Lupin Pharmaceuticals, Inc.
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: CIII
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated April 23, 2020
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Medication Guide: HTML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use TESTOSTERONE TOPICAL SOLUTION USP safely and effectively. See full prescribing information for TESTOSTERONE TOPICAL SOLUTION USP.
TESTOSTERONE topical solution USP, for topical use, CIII
Initial U.S. Approval: 1953WARNING: SECONDARY EXPOSURE TO TESTOSTERONE
See full prescribing information for complete boxed warning.
- Virilization has been reported in children who were secondarily exposed to topical testosterone products (5.2)
- Children should avoid contact with unwashed or unclothed application sites in men using testosterone topical solution (2.2, 5.2)
- Healthcare providers should advise patients to strictly adhere to recommended instructions for use (2.2,5.2, 17)
INDICATIONS AND USAGE
DOSAGE AND ADMINISTRATION
Prior to initiating testosterone topical solution USP, confirm the diagnosis of hypogonadism by ensuring that serum testosterone has been measured in the morning on at least two separate days and that these concentrations are below the normal range (2).
- Starting testosterone topical solution USP dose is 60 mg of testosterone (1 pump actuation of 30 mg of testosterone to each axilla), applied once daily, at the same time each morning. (2.1)
- Apply to clean, dry intact skin of the axilla, not to any other parts of the body including the abdomen or genitals (2.2)
- Dose adjustment: The dose of testosterone may be decreased from 60 mg (2 pump actuations) to 30 mg (1 pump actuation) or increased from 60 mg to 90 mg (3 pump actuations) or from 90 mg to 120 mg (4 pump actuations) based on the serum testosterone concentration from a single blood draw 2 to 8 hours after applying testosterone topical solution USP and at least 14 days after starting treatment or following dose adjustment. (2.2)
- Patients should wash hands immediately with soap and water after applying testosterone topical solution USP and cover the application site with clothing after the solution has dried. Wash the application site thoroughly with soap and water prior to any situation where skin-to-skin contact of the application site with another person is anticipated. (2.2)
- The application site and dose of testosterone topical solution USP are not interchangeable with other topical testosterone products. (2.1)
DOSAGE FORMS AND STRENGTHS
Testosterone topical solution is available as follows:
- a metered-dose pump that delivers 30 mg of testosterone per pump.
Each metered-dose pump is supplied with an applicator. (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- Monitor patients with benign prostatic hyperplasia (BPH) for worsening of signs and symptoms of BPH (5.1)
- Avoid unintentional exposure of women or children to testosterone topical solution. Secondary exposure to testosterone can produce signs of virilization. Testosterone topical solution should be discontinued until the cause of the virilization is identified (2.2, 5.2)
- Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE) have been reported in patients using testosterone products. Evaluate patients with signs or symptoms consistent with DVT or PE. (5.4)
- Some postmarketing studies have shown an increased risk of myocardial infarction and stroke associated with use of testosterone replacement therapy. (5.5)
- Exogenous administration of testosterone may lead to azoospermia (5.8)
- Edema with or without congestive heart failure, may be a complication in patients with preexisting cardiac, renal, or hepatic disease (5.10).
- Sleep apnea may occur in those with risk factors (5.12)
- Monitor serum testosterone, prostate specific antigen (PSA), liver function, lipid concentrations, hematocrit and hemoglobin periodically (5.1,5.3, 5.9, 5.13)
- Testosterone topical solution is flammable until dry (5.16)
ADVERSE REACTIONS
Most common adverse reactions (incidence >4%) are skin application site reactions, increased hematocrit, headache, diarrhea, vomiting, and increased serum PSA (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Lupin Pharmaceuticals, Inc. at 1-800-399-2561 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- Androgens may decrease blood glucose and insulin requirement in diabetic patients (7.1).
- Changes in anticoagulant activity may be seen with androgens. More frequent monitoring of International Normalized Ratio (INR) and prothrombin time is recommended (7.2).
- Use of testosterone with Adrenocorticotropic Hormone (ACTH) or corticosteroids may result in increased fluid retention. Use with caution, particularly in patients with cardiac, renal, or hepatic disease (7.3).
USE IN SPECIFIC POPULATIONS
- There are insufficient long-term safety data in geriatric patients using testosterone topical solution to assess the potential risks of cardiovascular disease and prostate cancer (8.5).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 4/2020
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
WARNING: SECONDARY EXPOSURE TO TESTOSTERONE
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Dosing and Dose Adjustment
2.2 Administration Instructions
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Worsening of Benign Prostatic Hyperplasia and Potential Risk of Prostate Cancer
5.2 Potential for Secondary Exposure to Testosterone
5.3 Polycythemia
5.4 Venous Thromboembolism
5.5 Cardiovascular Risk
5.6 Abuse of Testosterone and Monitoring of Serum Testosterone Concentrations
5.7 Use in Women
5.8 Potential for Adverse Effects on Spermatogenesis
5.9 Hepatic Adverse Effects
5.10 Edema
5.11 Gynecomastia
5.12 Sleep Apnea
5.13 Lipids
5.14 Hypercalcemia
5.15 Decreased Thyroxine-binding Globulin
5.16 Flammability
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Insulin
7.2 Oral anticoagulants
7.3 Corticosteroids
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.3 Nursing Mothers
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Renal Impairment
8.7 Hepatic Impairment
8.8 Use in Men with Body Mass Index (BMI) >35 kg/m2
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
9.2 Abuse
9.3 Dependence
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Clinical Studies in Hypogonadal Men
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
16.2 Storage and Handling
17 PATIENT COUNSELING INFORMATION
17.1 Use in Men with Known or Suspected Prostate or Breast Cancer
17.2 Potential for Secondary Exposure to Testosterone and Steps to Prevent Secondary Exposure
17.3 Potential Adverse Reactions with Androgens
17.4 Patients should be advised of these Application Instructions
- *
- Sections or subsections omitted from the full prescribing information are not listed.
-
BOXED WARNING
(What is this?)
WARNING: SECONDARY EXPOSURE TO TESTOSTERONE
- Virilization has been reported in children who were secondarily exposed to topical testosterone products [see WARNINGS AND PRECAUTIONS (5.2)] .
- Children should avoid contact with unwashed or unclothed application sites in men using testosterone topical solution [see DOSAGE AND ADMINISTRATION (2.2) and WARNINGS AND PRECAUTIONS (5.2)] .
- Healthcare providers should advise patients to strictly adhere to recommended instructions for use [see DOSAGE AND ADMINISTRATION (2.2), WARNINGS AND PRECAUTIONS (5.2) and PATIENT COUNSELING INFORMATION (17)] .
-
1 INDICATIONS AND USAGE
Testosterone topical solution USP is indicated for replacement therapy in males for conditions associated with a deficiency or absence of endogenous testosterone:
- Primary hypogonadism (congenital or acquired): testicular failure due to conditions such as cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchiectomy, Klinefelter's syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. These men usually have low serum testosterone concentrations and gonadotropins (FSH, LH) above the normal range.
- Hypogonadotropic hypogonadism (congenital or acquired): gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. These men have low testosterone serum concentrations but have gonadotropins in the normal or low range.
- Safety and efficacy of testosterone topical solution USP in men with "age-related hypogonadism" (also referred to as "late-onset hypogonadism") have not been established.
- Safety and efficacy of testosterone topical solution USP in males <18 years old have not been established [see USE IN SPECIFIC POPULATIONS (8.4)] .
-
2 DOSAGE AND ADMINISTRATION
Prior to initiating testosterone topical solution USP, confirm the diagnosis of hypogonadism by ensuring that serum testosterone concentrations have been measured in the morning on at least two separate days and that these serum testosterone concentrations are below the normal range.
2.1 Dosing and Dose Adjustment
The recommended starting dose of testosterone topical solution USP is 60 mg of testosterone (2 pump actuations) applied once daily.
To ensure proper dosing, serum testosterone concentrations should be measured after initiation of therapy to ensure that the desired concentrations (300 ng/dL to 1050 ng/dL) are achieved. The testosterone topical solution USP dose can be adjusted based on the serum testosterone concentration from a single blood draw 2 to 8 hours after applying testosterone topical solution USP and at least 14 days after starting treatment or following dose adjustment.
If the measured serum testosterone concentration is below 300 ng/dL, the daily testosterone dose may be increased from 60 mg (2 pump actuations) to 90 mg (3 pump actuations) or from 90 mg to 120 mg (4 pump actuations). If the serum testosterone concentration exceeds 1050 ng/dL, the daily testosterone dose should be decreased from 60 mg (2 pump actuations) to 30 mg (1 pump actuation) as instructed by a physician. If the serum testosterone concentration consistently exceeds 1050 ng/dL at the lowest daily dose of 30 mg (1 pump actuation), testosterone topical solution USP therapy should be discontinued.
The application site and dose of testosterone topical solution USP are not interchangeable with other topical testosterone products.
2.2 Administration Instructions
Testosterone topical solution USP is applied to the axilla, preferably at the same time each morning, to clean, dry, intact skin. Do not apply testosterone topical solution USP to other parts of the body including to the scrotum, penis, abdomen, shoulders or upper arms. After applying the solution, the application site should be allowed to dry completely prior to dressing. Avoid fire, flames or smoking until the solution has dried since alcohol based products, including testosterone topical solution USP, are flammable.
When deodorants or antiperspirants are used as part of a regular program for personal hygiene, they should not interfere with the efficacy of testosterone topical solution USP in treating hypogonadism. If patients use an antiperspirant or deodorant (stick or roll-on) then it should be applied at least 2 minutes prior to the application of testosterone topical solution USP to avoid contamination of the stick or roll-on product.
Patients should be advised to avoid swimming or washing the application site until two hours following application of testosterone topical solution USP [see CLINICAL PHARMACOLOGY (12.3)].
To reduce the likelihood of interpersonal transfer of testosterone, the application site should always be washed prior to any skin-to-skin contact regardless of the length of time since application. [see WARNINGS AND PRECAUTIONS (5.2)].
Testosterone topical solution USP is available as pump actuated metered-dose pump.
Pump Actuated Metered-Dose Pump
Testosterone topical solution USP is applied to the axilla using an applicator. When using testosterone topical solution USP for the first time, patients should be instructed to prime the pump by depressing the pump three times, discard any product dispensed directly into a basin, sink, or toilet and then wash the liquid away thoroughly. This priming should be done only prior to the first use of each pump. After priming, patients should completely depress the pump one time (1 pump actuation) to dispense 30 mg of testosterone. Ensure that the liquid is directed into the cup. The cup should be filled with no more than 30 mg (1 pump actuation) of testosterone. Dosing that requires greater than one pump actuation must be applied in increments of 30 mg as is shown in Table 1.
Keeping the applicator upright, patients should place it up into the axilla and wipe steadily down and up into the axilla. If the solution drips or runs, it can be wiped back up with the applicator cup. The solution should not be rubbed into the skin with fingers or hand. The process is then repeated with application of 30 mg of testosterone (1 pump actuation) to the other axilla to achieve a total of 60 mg of testosterone applied. For patients prescribed the 90 mg dose of testosterone, the procedure is the same, but three applications are required. To dose 120 mg of testosterone, four applications are required alternating left and right for each application as shown in Table 1. When repeat application to the same axilla is required, the axilla should be allowed to dry completely before more testosterone topical solution USP is applied.
After use, the applicator should be rinsed under room temperature, running water and then patted dry with a tissue. The applicator and cap are then replaced on the bottle for storage.
Table 1: Application Technique Daily Prescribed Dose of Testosterone
Number of Pump Actuations
Application
30 mg (once daily)
1
Apply once to one axilla only (left OR right)
60 mg (once daily)
2
Apply once to the left axilla and then apply once to the right axilla.
90 mg (once daily)
3
Apply once to the left and once to the right axilla, wait for the product to dry, and then apply once again to the left OR right axilla.
120 mg (once daily)
4
Apply once to the left and once to the right axilla, wait for the product to dry, and then apply once again to the left AND once to the right axilla.
Hands should be washed thoroughly with soap and water after testosterone topical solution USP has been applied [see WARNINGS AND PRECAUTIONS (5.2)].
Strict adherence to the following precautions is advised in order to minimize the potential for secondary exposure to testosterone from testosterone topical solution USP treated skin:
- Children and women should avoid contact with the unclothed or unwashed application sites on the skin of men using testosterone topical solution USP.
- Patients should wash their hands immediately with soap and water after application of testosterone topical solution USP.
- Patients should cover the application site(s) with clothing (e.g., a T-shirt) after the solution has dried.
- Prior to any situation in which direct skin-to-skin contact is anticipated, patients should wash the application site thoroughly with soap and water to remove any testosterone residue.
- In the event that unwashed or unclothed skin to which testosterone topical solution USP has been applied comes in direct contact with the skin of another person, the general area of contact on the other person should be washed with soap and water as soon as possible.
While interpersonal testosterone transfer can occur with a T-shirt on, it has been shown that transfer can be substantially reduced by wearing a T-shirt and the majority of residual testosterone is removed from the skin surface by washing with soap and water.
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
- Testosterone topical solution is contraindicated in men with carcinoma of the breast or known or suspected carcinoma of the prostate [see WARNINGS AND PRECAUTION (5.1)] .
- Testosterone topical solution is contraindicated in women who are, or who may become pregnant, or who are breastfeeding. Testosterone topical solution may cause fetal harm when administered to a pregnant woman. Testosterone topical solution may cause serious adverse reactions in nursing infants. If a pregnant woman is exposed to testosterone topical solution, she should be apprised of the potential hazard to the fetus. [see USE IN SPECIFIC POPULATIONS (8.1,8.3)] .
-
5 WARNINGS AND PRECAUTIONS
5.1 Worsening of Benign Prostatic Hyperplasia and Potential Risk of Prostate Cancer
- Monitor patients with benign prostatic hyperplasia (BPH) for worsening of signs and symptoms of BPH.
- Patients treated with Androgens may be at increased risk for prostate cancer. Evaluate patients for prostate cancer prior to initiating treatment. It would be appropriate to reevaluate patients 3 to 6 months after initiation of treatment, and then in accordance with prostate cancer screening practices. [see CONTRAINDICATIONS (4)] .
5.2 Potential for Secondary Exposure to Testosterone
Cases of secondary exposure to testosterone in children and women have been reported with topical testosterone products applied to the abdomen or upper arms, including cases of secondary exposure resulting in virilization of children. Signs and symptoms have included enlargement of the penis or clitoris, development of pubic hair, increased erections and libido, aggressive behavior, and advanced bone age. In most cases, these signs and symptoms regressed with removal of the exposure to testosterone. In a few cases, however, enlarged genitalia did not fully return to age-appropriate normal size, and bone age remained modestly greater than chronological age. The risk of transfer was increased in some of these cases by not adhering to precautions for the appropriate use of the topical testosterone product. Children and women should avoid contact with unwashed or unclothed application sites in men using testosterone topical solution [see DOSAGE AND ADMINISTRATION (2.2), USE IN SPECIFIC POPULATIONS (8.1) and CLINICAL PHARMACOLOGY (12.3)].
Inappropriate changes in genital size or development of pubic hair or libido in children, or changes in body hair distribution, significant increase in acne, or other signs of virilization in adult women should be brought to the attention of a physician and the possibility of secondary exposure to testosterone should also be brought to the attention of a physician. Testosterone therapy should be promptly discontinued at least until the cause of virilization has been identified. [see DOSAGE AND ADMINISTRATION (2.2)].
5.3 Polycythemia
Increases in hematocrit, reflective of increases in red blood cell mass, may require lowering or discontinuation of testosterone. Check hematocrit prior to initiating testosterone treatment. It would be appropriate to re-evaluate the hematocrit 3 to 6 months after starting testosterone treatment, and then annually. If hematocrit becomes elevated, stop therapy until hematocrit decreases to an acceptable level. An increase in red blood cell mass may increase the risk of thromboembolic events.
5.4 Venous Thromboembolism
There have been postmarketing reports of venous thromboembolic events, including deep vein thrombosis (DVT) and pulmonary embolism (PE), in patients using testosterone products, such as testosterone topical solution. Evaluate patients who report symptoms of pain, edema, warmth and erythema in the lower extremity for DVT and those who present with acute shortness of breath for PE. If a venous thromboembolic event is suspected, discontinue treatment with testosterone topical solution and initiate appropriate workup and management [see ADVERSE REACTIONS (6.2)].
5.5 Cardiovascular Risk
Long term clinical safety trials have not been conducted to assess the cardiovascular outcomes of testosterone replacement therapy in men. To date, epidemiologic studies and randomized controlled trials have been inconclusive for determining the risk of major adverse cardiovascular events (MACE), such as non-fatal myocardial infarction, non-fatal stroke, and cardiovascular death, with the use of testosterone compared to non-use. Some studies, but not all, have reported an increased risk of MACE in association with use of testosterone replacement therapy in men. Patients should be informed of this possible risk when deciding whether to use or to continue to use testosterone topical solution.
5.6 Abuse of Testosterone and Monitoring of Serum Testosterone Concentrations
Testosterone has been subject to abuse, typically at doses higher than recommended for the approved indication and in combination with other anabolic androgenic steroids. Anabolic androgenic steroid abuse can lead to serious cardiovascular and psychiatric adverse reactions [see DRUG ABUSE AND DEPENDENCE (9)].
If testosterone abuse is suspected, check serum testosterone concentrations to ensure they are within therapeutic range. However, testosterone levels may be in the normal or subnormal range in men abusing synthetic testosterone derivatives. Counsel patients concerning the serious adverse reactions associated with abuse of testosterone and anabolic androgenic steroids. Conversely, consider the possibility of testosterone and anabolic androgenic steroid abuse in suspected patients who present with serious cardiovascular or psychiatric adverse events.
5.7 Use in Women
Due to lack of controlled studies in women and potential virilizing effects, testosterone topical solution is not indicated for use in women [see CONTRAINDICATIONS (4) and USE IN SPECIFIC POPULATIONS (8.1, 8.3)].
5.8 Potential for Adverse Effects on Spermatogenesis
At large doses of exogenous androgens, including testosterone topical solution, spermatogenesis may be suppressed through feedback inhibition of pituitary follicle-stimulating hormone (FSH) which could possibly lead to adverse effects on semen parameters including sperm count.
5.9 Hepatic Adverse Effects
Prolonged use of high doses of orally active 17-alpha-alkyl androgens (methyltestosterone) has been associated with serious hepatic adverse effects (peliosis hepatitis, hepatic neoplasms, cholestatic hepatitis, and jaundice). Peliosis hepatitis can be a life-threatening or fatal complication. Long-term therapy with intramuscular testosterone enanthate has produced multiple hepatic adenomas. Testosterone topical solution is not known to cause these adverse effects.
5.10 Edema
Androgens, including testosterone topical solution, may promote retention of sodium and water. Edema, with or without congestive heart failure, may be a serious complication in patients with pre-existing cardiac, renal, or hepatic disease [see ADVERSE REACTIONS (6)].
5.11 Gynecomastia
Gynecomastia may develop and may persist in patients being treated with androgens, including testosterone topical solution, for hypogonadism.
5.12 Sleep Apnea
The treatment of hypogonadal men with testosterone may potentiate sleep apnea in some patients, especially those with risk factors such as obesity and chronic lung disease.
5.13 Lipids
Changes in serum lipid profile may require dose adjustment or discontinuation of testosterone therapy.
5.14 Hypercalcemia
Androgens, including testosterone topical solution, should be used with caution in cancer patients at risk of hypercalcemia (and associated hypercalciuria). Regular monitoring of serum calcium concentrations is recommended in these patients.
5.15 Decreased Thyroxine-binding Globulin
Androgens, including testosterone topical solution, may decrease concentrations of thyroxin-binding globulins, resulting in decreased total T4 serum concentration and increased resin uptake of T3 and T4. Free thyroid hormone concentration remain unchanged, however there is no clinical evidence of thyroid dysfunction.
-
6 ADVERSE REACTIONS
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trials in Hypogonadal Men
Table 2 shows the treatment emergent adverse reactions that were reported by either >4% of 155 patients in a 120 day, Phase 3 study or by >4% of 71 patients who continued to use testosterone topical solution for up to 180 days. These data reflect the experience primarily with a testosterone dose of 60 mg, which was taken by all patients at the start of the study, and was the maintenance dose for 97 patients. However, the doses used varied from 30 mg to 120 mg.
Event
120 Days
(155 Patients)
180 Days
(71 Patients)
Application Site Irritation
11 (7%)
6 (8%)
Application Site Erythema
8 (5%)
5 (7%)
Headache
8 (5%)
4 (6%)
Hematocrit Increased
6 (4%)
5 (7%)
Diarrhea
4 (3%)
3 (4%)
Vomiting
4 (3%)
3 (4%)
PSA Increased
2 (1%)
3 (4%)
Other less common adverse reactions reported by at least 2 patients in the 120 day trial included: application site edema, application site warmth, increased hemoglobin, hypertension, erythema (general), increased blood glucose, acne, nasopharyngitis, anger and anxiety. Other less common adverse reactions reported in fewer than 1% of patients in the 120 day trial included: asthenia, affect lability, folliculitis, increased lacrimation, breast tenderness, increased blood pressure, increased blood testosterone, neoplasm prostate and elevated red blood cell count.
During the 120 day trial one patient discontinued treatment because of affect lability/anger which was considered possibly related to testosterone topical solution administration.
During the 120 day clinical trial there was an increase in mean PSA values of 0.13 ± 0.68 ng/mL from baseline. At the end of the 180 day extension clinical trial, there was an overall increase in mean PSA values of 0.1 ± 0.54 ng/mL.
Following the 120 day study, seventy-one (71) patients entered a two-month extension study with testosterone topical solution. Two patients (3%) had adverse reactions that led to discontinuation of treatment during the period from Day 120 to Day 180. These reactions were: one patient with application site irritation (considered possibly related to testosterone topical solution application) and one patient with dry skin and erythema, but not at the application site (considered not related to testosterone topical solution administration) and application site erythema (considered possibly related to testosterone topical solution administration).
No serious adverse reactions to testosterone topical solution were reported during either the 120 day trial, or the extension to 180 days.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of testosterone topical solution. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiovascular Disorders
myocardial infarction, stroke [see WARNINGS AND PRECAUTIONS (5.5)].
Vascular Disorders
Venous thromboembolism [see WARNINGS AND PRECAUTIONS (5.4)].
-
7 DRUG INTERACTIONS
7.1 Insulin
Changes in insulin sensitivity or glycemic control may occur in patients treated with androgens. In diabetic patients, the metabolic effects of androgens may decrease blood glucose and, therefore, insulin requirement.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category X [see CONTRAINDICATIONS (4)]
Testosterone topical solution is contraindicated during pregnancy or in women who may become pregnant. Testosterone is teratogenic and may cause fetal harm. Exposure of a female fetus to androgens may result in varying degrees of virilization. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
8.3 Nursing Mothers
Although it is not known how much testosterone transfers into human milk, testosterone topical solution is contraindicated in nursing women because of the potential for serious adverse reactions in nursing infants. Testosterone and other androgens may adversely affect lactation. [see CONTRAINDICATIONS (4)].
8.4 Pediatric Use
Safety and efficacy of testosterone topical solution has not been established in males <18 years of age. Improper use may result in acceleration of bone age and premature closure of epiphyses.
8.5 Geriatric Use
There have not been sufficient numbers of geriatric patients involved in controlled clinical studies utilizing testosterone topical solution to determine whether efficacy in those over 65 years of age differs from younger patients. Of the 155 patients enrolled in the pivotal clinical study utilizing testosterone topical solution, 21 were over 65 years of age. Additionally, there were insufficient long-term safety data in these patients utilizing testosterone topical solution to assess a potential incremental risk of cardiovascular disease and prostate cancer.
-
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
Testosterone topical solution contains testosterone, a Schedule III controlled substance in the Controlled Substances Act.
9.2 Abuse
Drug abuse is intentional non-therapeutic use of a drug, even once, for its rewarding psychological and physiological effects. Abuse and misuse of testosterone are seen in male and female adults and adolescents. Testosterone, often in combination with other anabolic androgenic steroids (AAS), and not obtained by prescription through a pharmacy, may be abused by athletes and bodybuilders. There have been reports of misuse by men taking higher doses of legally obtained testosterone than prescribed and continuing testosterone despite adverse events or against medical advice.
Abuse-Related Adverse Reactions
Serious adverse reactions have been reported in individuals who abuse anabolic androgenic steroids and include cardiac arrest, myocardial infarction, hypertrophic cardiomyopathy, congestive heart failure, cerebrovascular accident, hepatotoxicity, and serious psychiatric manifestations, including major depression, mania, paranoia, psychosis, delusions, hallucinations, hostility and aggression.
The following adverse reactions have also been reported in men: transient ischemic attacks, convulsions, hypomania, irritability, dyslipidemias, testicular atrophy, subfertility, and infertility.
The following additional adverse reactions have been reported in women: hirsutism, virilization, deepening of voice, clitoral enlargement, breast atrophy, male-pattern baldness, and menstrual irregularities.
The following adverse reactions have been reported in male and female adolescents: premature closure of bony epiphyses with termination of growth, and precocious puberty.
Because these reactions are reported voluntarily from a population of uncertain size and may include abuse of other agents, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
9.3 Dependence
Behaviors Associated with Addiction
Continued abuse of testosterone and other anabolic steroids, leading to addiction is characterized by the following behaviors:
- Taking greater dosages than prescribed
- Continued drug use despite medical and social problems due to drug use
- Spending significant time to obtain the drug when supplies of the drug are interrupted
- Giving a higher priority to drug use than other obligations
- Having difficulty in discontinuing the drug despite desires and attempts to do so
- Experiencing withdrawal symptoms upon abrupt discontinuation of use
Physical dependence is characterized by withdrawal symptoms after abrupt drug discontinuation or a significant dose reduction of a drug. Individuals taking supratherapeutic doses of testosterone may experience withdrawal symptoms lasting for weeks or months which include depressed mood, major depression, fatigue, craving, restlessness, irritability, anorexia, insomnia, decreased libido and hypogonadotropic hypogonadism.
Drug dependence in individuals using approved doses of testosterone for approved indications has not been documented.
-
10 OVERDOSAGE
No cases of overdose with testosterone topical solution have been reported in clinical trials. There is one report of acute overdosage by injection of testosterone enanthate: testosterone concentrations of up to 11,400 ng/dL were implicated in a cerebrovascular accident. Treatment of overdosage would consist of discontinuation of testosterone topical solution together with appropriate symptomatic and supportive care.
-
11 DESCRIPTION
Testosterone topical solution USP is a clear, colorless, homogeneous solution containing 30 mg of testosterone USP in 1.5 mL of testosterone topical solution USP for topical administration through the axilla. The active pharmacologic ingredient in testosterone topical solution USP is testosterone USP. Testosterone USP is a white to practically white powder or crystals chemically described as 17-beta hydroxyandrost-4-en-3-one. The structural formula is:
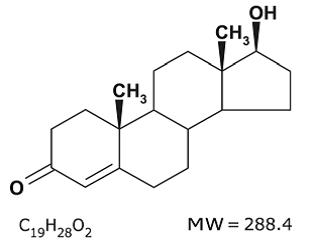
The inactive ingredients are ethanol, isopropyl alcohol, octisalate and povidone.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Endogenous androgens, including testosterone and dihydrotestosterone (DHT), are responsible for the normal growth and development of the male sex organs and for maintenance of secondary sex characteristics. These effects include the growth and maturation of prostate, seminal vesicles, penis and scrotum; the development of male hair distribution, such as facial, pubic, chest and axillary hair; laryngeal enlargement, vocal cord thickening, alterations in body musculature and fat distribution. Testosterone and DHT are necessary for the normal development of secondary sex characteristics.
Male hypogonadism, a clinical syndrome resulting from insufficient secretion of testosterone, has two main etiologies. Primary hypogonadism is caused by defects of the gonads, such as Klinefelter's Syndrome or Leydig cell aplasia, whereas secondary hypogonadism is the failure of the hypothalamus (or pituitary) to produce sufficient gonadotropins (FSH, LH).
12.2 Pharmacodynamics
No specific pharmacodynamic studies were conducted using testosterone topical solution.
12.3 Pharmacokinetics
Testosterone topical solution delivers physiologic circulating testosterone that approximate normal concentration range (i.e., 300 to 1050 ng/dL) seen in healthy men following application to the axilla.
On the skin, the ethanol and isopropyl alcohol evaporate leaving testosterone and octisalate. The skin acts as a reservoir from which testosterone is released into the systemic circulation over time (see Figure 1). In general, steady-state serum concentrations are achieved by approximately 14 days of daily dosing.
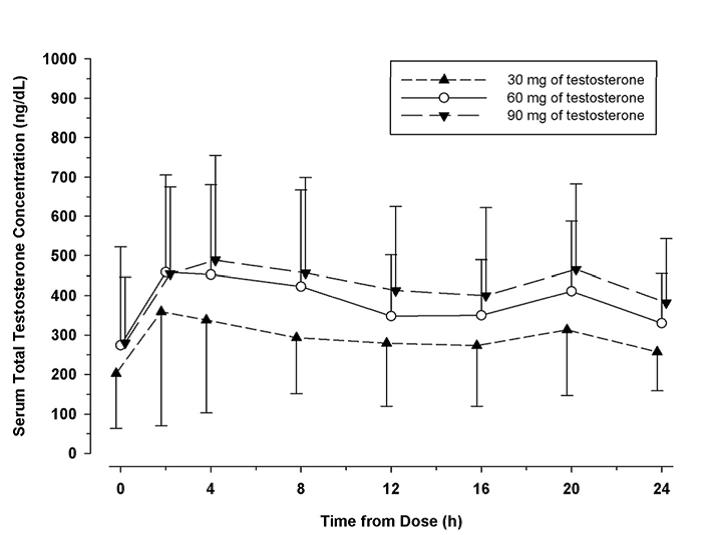
Figure 1: Mean (±SD) Serum Testosterone Concentrations on Day 7 in Patients Following Testosterone Topical Solution Once-Daily Application of 30 mg, 60 mg, or 90 mg of Testosterone
When testosterone topical solution treatment is discontinued after achieving steady-state, serum testosterone concentrations returned to their pretreatment concentrations by 7 to 10 days after the last application.
Distribution
Circulating testosterone is primarily bound in the serum to sex hormone-binding globulin (SHBG) and albumin. Approximately 40% of testosterone in plasma is bound to SHBG, 2% remains unbound (free) and the rest is bound to albumin and other proteins.
Metabolism
Testosterone is metabolized to various 17-keto steroids through two different pathways. The major active metabolites of testosterone are estradiol and dihydrotestosterone (DHT).
DHT concentration increased in parallel with testosterone concentration during testosterone topical solution treatment. The mean steady-state DHT/T ratio remained within normal limits and ranged from 0.17 to 0.26 across all doses on Days 15, 60, and 120.
Excretion
There is considerable variation in the half-life of testosterone as reported in the literature, ranging from 10 to 100 minutes. About 90% of a dose of testosterone given intramuscularly is excreted in the urine as glucuronic and sulfuric acid conjugates of testosterone and its metabolites; about 6% of a dose is excreted in the feces, mostly in the unconjugated form. Inactivation of testosterone occurs primarily in the liver.
Potential for Testosterone Transfer:
The potential for testosterone transfer from males dosed with testosterone topical solution to healthy females was evaluated in a clinical study conducted with a 2% testosterone formulation. 10 males were treated with 60 mg of testosterone in each axilla (the maximum testosterone dose of 120 mg). At 2 hours after the application of testosterone topical solution to the males, the females rubbed their outer forearms for 15 minutes on the axilla of the males. The males had covered the application area with a T-shirt. Serum concentrations of testosterone were monitored in the female subjects for 72 hours after the transfer procedure. Study results show a 13% and 17% increase in testosterone exposure (AUC[0 to 24]) and maximum testosterone concentration (Cmax), respectively, compared to baseline in these females. In a prior clinical study conducted with a 1% testosterone formulation under similar study conditions, direct skin-to-skin transfer showed a 131% and 297% increase in testosterone exposure (AUC[0 to 72]) and maximum testosterone concentration (Cmax), respectively, compared to when men had covered the application area with a T-shirt.
In a clinical study conducted with a 2% testosterone formulation to evaluate the effect of washing on the residual amount of testosterone at the axilla, 10 healthy male subjects received 60 mg of testosterone to each axilla (the maximum testosterone dose of 120 mg). Following 5 minutes of drying time, the left axilla was wiped with alcohol towelettes which were assayed for testosterone content. Subjects were required to shower with soap and water 30 minutes after application. The right axilla was then wiped with alcohol towelettes which were assayed for testosterone content. A mean (SD) of 3.1 (2.8) mg of residual testosterone (i.e., 92.6% reduction compared to when axilla was not washed) was recovered after washing this area with soap and water. [see DOSAGE AND ADMINISTRATION (2.2) and WARNINGS AND PRECAUTIONS (5.2)].
Use of Deodorants and Anti-perspirants:
In a parallel designed clinical study evaluating the effect of deodorants and antiperspirants in healthy premenopausal females dosed with testosterone topical solution, each subject applied either a combined deodorant/antiperspirant spray (6 subjects) or stick (6 subjects) or a deodorant spray (6 subjects) to a single axilla 2 minutes before the application of 30 mg of testosterone to the same axilla. A control group of 6 subjects only applied 30 mg of testosterone to a single axilla. Blood samples were collected for 72 hours from all subjects following testosterone topical solution administration. Although a decrease of up to 33% of testosterone exposure (AUC[0 to 72]) was observed when antiperspirants or deodorants are used 2 minutes prior to testosterone topical solution application, underarm deodorant or antiperspirant spray or stick products may be used 2 minutes prior to testosterone topical solution application as part of normal, consistent, and daily routine. [see DOSAGE AND ADMINISTRATION (2.2), and PATIENT COUNSELING INFORMATION (17.4)].
Effect of Showering/Washing:
In a parallel designed clinical study to evaluate the effect of washing on the testosterone systemic exposure, two groups of 6 healthy premenopausal female subjects were each dosed with 30 mg of testosterone to a single axilla. The application sites of each group were washed with soap and water 2 hours or 6 hours after the application of testosterone topical solution. A control group of 6 female subjects applied 30 mg of testosterone to a single axilla and did not wash the application site. Blood samples were collected for 72 hours from all subjects following dosing with testosterone topical solution. A decrease of up to 35% of testosterone exposure (AUC[0 to 72]) was observed when applications sites were washed 2 hours and 6 hours after testosterone topical solution application. Patients should be advised to avoid swimming or washing the application site until 2 hours following application of testosterone topical solution. [see DOSAGE AND ADMINISTRATION (2.2) and PATIENT COUNSELING INFORMATION (17.4)].
-
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Testosterone has been tested by subcutaneous injection and implantation in mice and rats. In mice, the implant induced cervical-uterine tumors, which metastasized in some cases. There is suggestive evidence that injection of testosterone into some strains of female mice increases their susceptibility to hepatoma. Testosterone is also known to increase the number of tumors and decrease the degree of differentiation of chemically induced carcinomas of the liver in rats. Testosterone was negative in the in vitro Ames and in the in vivo mouse micronucleus assays. The administration of exogenous testosterone has been reported to suppress spermatogenesis in the rat, dog and non-human primates, which was reversible on cessation of the treatment.
-
14 CLINICAL STUDIES
14.1 Clinical Studies in Hypogonadal Men
Testosterone topical solution was evaluated in a multicenter, open label, 120-day trial that enrolled 155 hypogonadal men at 26 clinical research centers. The median age of subjects was 53 years with a range of 19 to 78 years. Of the 144 subjects whose race was recorded, 122 (84.7%) were Caucasian, 13 (9.0%) were Hispanic, 6 (4.2%) were African Americans, 1 (0.7%) was Asian and 2 (1.4%) had race recorded as "Other".
Patients were instructed to apply testosterone topical solution to unclothed, clean, dry, and unbroken skin. The solution was applied to the axillary area. Patients were not instructed to alter their normal grooming routine, e.g., shave under the arm.
During the initial testosterone topical solution treatment period (Days 1 to 15) 143 patients were treated with 60 mg of testosterone daily. On Day 45 of the trial, patients were maintained at the same dose, or were titrated up or down, based on their 24 hour average serum testosterone concentration measured on Day 15. On Day 90 of the trial, patients were maintained at the same dose, or were titrated up or down, based on their 24 hour average serum testosterone concentration measured on Day 60.
On day 120, 75% of responding patients finished the study on the starting dose of 60 mg of testosterone, while 2% had been titrated to 30 mg, 17% had been titrated to 90 mg and 6% had been titrated to the 120 mg dose.
On day 60, 84.8% of subjects had total testosterone concentrations in the normal range. Of those who had sufficient data for analysis on day 120, 84.1%, had their average serum testosterone concentration in the normal range of 300 to 1050 ng/dL.
Table 3 summarizes the proportion of subjects having average testosterone concentrations within the normal range on Days 60 and 120.
Table 3: Proportion of subjects who had an average Serum Total Testosterone in the range 300 to 1050 ng/dL and completed 120 days of treatment (N=138*) - *
- Three patients who withdrew from the study due to adverse reactions are included as treatment failures.
- †
- Normal represents the percentage of patients with average testosterone concentration in the range of 300 to 1050 ng/dL.
- ‡
- On Day 15, 72.2% of the 90 subjects in the US study population had an average serum testosterone in the range of 300 ng/dL to 1050 ng/dL.
Evaluation Time
Statistics
Value
Baseline Testosterone
Mean (SD)
194.6 ng/dL (92.9 ng/dL)
Day 15
Normal†
76.1%‡
95% CI
(69.0%, 83.2%)
Day 60
Normal†
84.8%
95% CI
(78.8%, 90.8%)
Day 120
Normal†
84.1%
95% CI
(77.9%, 90.2%)
Of the 135 patients who completed the 120 day treatment, 123 patients did so with no deviation from the protocol. By day 120, average serum testosterone concentration was within normal range for 67% of those who titrated down on the 30 mg dose, 89% of those on the 60 mg dose, 86% of those who titrated up to 90 mg and 70% of those who titrated up to the 120 mg dose. Table 4 below summarizes the testosterone concentration data in the patients who completed 120 days.
Table 4: Baseline-unadjusted Arithmetic Mean (±SD) Steady-State Serum Testosterone Concentrations on Days 15, 60 and 120 in Patients Who Completed 120 Days of Treatment
Dose of Testosterone Topical Solution
30 mg
60 mg
90 mg
120 mg
Overall
Day 15
[N=0]
[N=135]
[N=0]
[N=0]
[N=135]
Cavg (ng/dL)
--
456 (±226)
---
--
456 (±226)
Cmax (ng/dL)
--
744 (±502)
--
--
744 (±502)
Day 60
[N=1]
[N=105]
[N=29]
[N=0]
[N=135]
Cavg (ng/dL)
343 (--)
523 (±207)
368 (±138)
--
488 (±204)
Cmax (ng/dL)
491 (--)
898 (±664)
646 (±382)
--
840 (±620)
Day 120
[N=3]
[N=97]
[N=25]
[N=10]
[N=135]
Cavg (ng/dL)
493 (±239)
506 (±175)
415 (±165)
390 (±160)
480 (±177)
Cmax (ng/dL)
779 (±416)
839 (±436)
664 (±336)
658 (±353)
792 (±417)
Figure 2 summarizes the pharmacokinetic profiles of total testosterone in patients completing 120 days of testosterone topical solution treatment administered as 60 mg of testosterone for the initial 15 days followed by possible titration according to follow-up testosterone measurements.
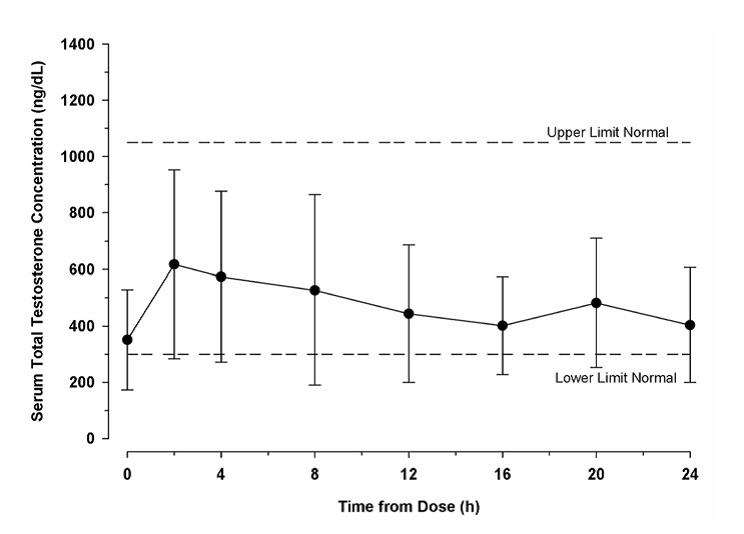
Figure 2: Mean (± SD) Steady-State Serum Testosterone Concentrations on Day 120 (30, 60, 90 or 120 mg testosterone) in Patients Who Completed 120 Days (N=135) of Testosterone Topical Solution Once-Daily Treatment
-
16 HOW SUPPLIED/STORAGE AND HANDLING
16.1 How Supplied
Testosterone topical solution USP is available as a metered-dose pump containing 110 mL of solution. The pump is capable of dispensing 90 mL of solution in 60 metered pump actuations. One actuation delivers 30 mg of testosterone in 1.5 mL of solution. Each metered-dose pump is supplied with an applicator. The bottle and the applicator cup are not made with natural rubber latex.
NDC
Pump Type
68180-943-11
Pump Actuated
16.2 Storage and Handling
Keep testosterone topical solution out of reach of children.
Store upright at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Used testosterone topical solution bottles and applicators should be discarded in household trash in a manner that prevents accidental exposure of children or pets.
-
17 PATIENT COUNSELING INFORMATION
See FDA-Approved Medication Guide.
Patients should be informed of the following information:
17.1 Use in Men with Known or Suspected Prostate or Breast Cancer
Men with known or suspected prostate or breast cancer should not use testosterone topical solution [see CONTRAINDICATIONS (4) and WARNINGS AND PRECAUTION (5.1)].
17.2 Potential for Secondary Exposure to Testosterone and Steps to Prevent Secondary Exposure
Cases of secondary exposure to testosterone in children and women have been reported with topical testosterone products applied to the abdomen, shoulders or upper arms, including cases of secondary exposure resulting in virilization of children, with signs and symptoms including enlargement of the penis or clitoris, premature development of pubic hair, increased erections, aggressive behavior and advanced bone age. Inappropriate changes in genital size or premature development of pubic hair or libido in children, or changes in hair distribution, increase in acne, or other signs of testosterone effects in adult women should be brought to the attention of a physician and the possibility of secondary exposure to testosterone topical solution also should be brought to the attention of a physician. Testosterone topical solution should be promptly discontinued at least until the cause of virilization is identified.
Strict adherence to the following precautions is advised in order to minimize the potential for secondary exposure to testosterone from testosterone topical solution treated skin:
- Testosterone topical solution should only be applied to the axilla, not to any other part of the body.
- Children and women should avoid contact with the unwashed skin of the axilla or unclothed application sites of men where testosterone topical solution has been applied.
- Patients should wash their hands immediately with soap and water after application of testosterone topical solution.
- Patients should cover the axilla application site(s) with clothing (e.g., a shirt) after waiting 3 minutes for the solution to dry.
- Prior to any situation in which direct skin-to-skin contact of the axilla is anticipated, patients should wash the axilla to which testosterone topical solution has been applied thoroughly with soap and water to remove any testosterone residue.
- In the event that unwashed or unclothed skin to which testosterone topical solution has been applied comes in direct contact with the skin of another person, the general area of contact on the other person should be washed with soap and water as soon as possible [see DOSAGE AND ADMINISTRATION (2.2), WARNINGS AND PRECAUTIONS (5.2) and CLINICAL PHARMACOLOGY (12.3)] .
17.3 Potential Adverse Reactions with Androgens
Patients should be informed that treatment with Androgens may lead to adverse reactions which include:
- Changes in urinary habits such as increased urination at night, trouble starting your urine stream, passing urine many times during the day, having an urge that you have to go to the bathroom right away, having urine accident, being unable to pass urine and having a weak urine flow.
- Breathing disturbances, including those associated with sleep, or excessive daytime sleepiness.
- Too frequent or persistent erections of the penis.
- Nausea, vomiting, changes in skin color, or ankle swelling.
17.4 Patients should be advised of these Application Instructions
- Ensure that the patient understands how to administer the correct dose.
- The pump should be primed by depressing it 3 times prior to its first use. No priming is needed with subsequent uses of that pump.
- Testosterone topical solution should NOT be applied to the scrotum, penis, abdomen, shoulders or upper arms.
- With testosterone doses greater than 60 mg, which require two applications of testosterone topical solution to the same axilla, the product should be allowed to dry after the first application before the second is applied.
- Testosterone topical solution should be applied once daily at approximately the same time each day. Testosterone topical solution should be applied to clean, dry skin.
- Patients may use an antiperspirant or deodorant spray before applying testosterone topical solution. If patients use a stick or roll-on antiperspirant or deodorant, then it should be applied at least 2 minutes prior to application of testosterone topical solution to avoid contamination of the stick or roll-on product.
- Avoid swimming or washing the application site until two hours following application of testosterone topical solution [see DOSAGE AND ADMINISTRATION (2) and CLINICAL PHARMACOLOGY (12.3)] .
- Avoid splashing in the eyes. In case of contact with eyes, flush thoroughly with water. If irritation persists, seek medical advice.
- Do not drink testosterone topical solution.
Lupin Pharmaceuticals, Inc.
Baltimore, Maryland 21202
United States
Manufactured by:
Lupin Limited
Pithampur (M.P.) – 454 775
India
April 2020 ID#:262878
-
MEDICATION GUIDE
Testosterone (tes TOS ter one) Topical Solution USP, for topical use CIII
What is the most important information I should know about testosterone topical solution?
1. Testosterone topical solution can transfer from your body to others including, children and women. Children and women should avoid contact with the unwashed or not covered (unclothed) areas where testosterone topical solution has been applied to your skin. Early signs and symptoms of puberty have occurred in young children who have come in direct contact with testosterone by touching areas where men have used testosterone topical solution.
Children
Signs and symptoms of early puberty in a child when they come in direct contact with testosterone topical solution may include:
Abnormal sexual changes:
- enlarged penis or clitoris.
- early growth of hair near the vagina or around the penis (pubic hair).
- erections or acting out sexual urges (sex drive).
- acting aggressively, behaving in an angry or violent way.
Signs and symptoms in women when they come in direct contact with testosterone topical solution may include:
- changes in body hair.
- an abnormal increase in pimples (acne).
Stop using testosterone topical solution and call your healthcare provider right away if you see any signs and symptoms in a child or a woman that may have happened through accidental touching of the area where you have applied testosterone topical solution:
2. To lower the risk of transfer of testosterone topical solution from your body to others, follow these important instructions:
- Apply testosterone topical solution only to your armpits.
- Wash your hands right away with soap and water after applying testosterone topical solution.
- After the solution has dried, cover the application area with clothing. Keep the area covered until you have washed the application area well or have showered.
- If you expect to have skin-to-skin contact with another person, first wash the application area well with soap and water.
- If a child or woman touches the area where you have applied testosterone topical solution, that area on the child or woman should be washed well with soap and water right away.
What is testosterone topical solution?
- Testosterone topical solution is a prescription medicine that contains testosterone. Testosterone topical solution is used to treat adult males who have low or no testosterone due to certain medical conditions.
- Your healthcare provider will test your blood before you start and while you are using testosterone topical solution.
- It is not known if testosterone topical solution is safe or effective to treat men who have low testosterone due to aging.
- It is not known if testosterone topical solution is safe and effective in children younger than 18 years old. Improper use of testosterone topical solution may affect bone growth in children.
- Testosterone topical solution is a controlled substance (CIII) because it contains testosterone that can be a target for people who abuse prescription medicines. Keep your testosterone topical solution in a safe place to protect it. Never give testosterone topical solution to anyone else, even if they have the same symptoms you have. Selling or giving away this medicine may harm others and it is against the law.
- Testosterone topical solution is not meant for use in women.
Do not use testosterone topical solution if you:
- have breast cancer.
- have or might have prostate cancer.
- are pregnant or may become pregnant or are breastfeeding. Testosterone topical solution may harm your unborn or breastfeeding baby.
Women who are pregnant or who may become pregnant should avoid contact with the area of the skin where testosterone topical solution has been applied.
Before using testosterone topical solution, tell your healthcare provider about all of your medical conditions, including if you:
- have breast cancer.
- have or might have prostate cancer.
- have urinary problems due to an enlarged prostate.
- have heart problems.
- have kidney or liver problems.
- have problems breathing while you sleep (sleep apnea).
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Using testosterone topical solution with other medicines can affect each other.
Especially tell your healthcare provider if you take:
- insulin
- medicines that decrease blood clotting (blood thinners)
- corticosteroids
How should I use testosterone topical solution?
- See the detailed Instructions for Use for information about how to use testosterone topical solution at the end of this Medication Guide.
- Testosterone topical solution comes in a metered-dose pump or twist actuated dispenser. Make sure you have the right pump or dispenser that is prescribed for you.
- It is important that you apply testosterone topical solution exactly as your healthcare provider tells you to.
- Your healthcare provider may change your testosterone topical solution dose. Do not change your testosterone topical solution dose without talking to your healthcare provider.
- Apply testosterone topical solution at about the same time each morning. Testosterone topical solution should be applied after showering or bathing.
What are the possible side effects of testosterone topical solution?
Testosterone topical solution can cause serious side effects including:
See also "What is the most important information I should know about testosterone topical solution?"
-
If you already have an enlarged prostate, your symptoms can get worse while using testosterone topical solution. This can include:
- increased urination at night.
- trouble starting your urine stream.
- having to pass urine many times during the day.
- having an urge to go to the bathroom right away.
- having a urine accident.
- being unable to pass urine or weak urine flow.
- Possible increased risk of prostate cancer. Your healthcare provider should check you for prostate cancer or any other prostate problems before you start and while you use testosterone topical solution.
- Blood clots in the legs or lungs. Signs and symptoms of a blood clot in your leg can include leg pain, swelling or redness. Signs and symptoms of a blood clot in your lungs can include difficulty breathing or chest pain.
- Possible increased risk of heart attack or stroke.
- In large doses testosterone topical solution may lower your sperm count.
- Swelling of your ankles, feet, or body, with or without heart failure.
- Enlarged or painful breasts.
- Have problems breathing while you sleep (sleep apnea).
Call your healthcare provider right away if you have any of the serious side effects listed above.
The most common side effects of testosterone topical solution include:
- skin redness or irritation where testosterone topical solution is applied
- increased red blood cell count
- headache
- diarrhea
- vomiting
- increase in blood level of Prostate Specific Antigen (a test used to screen for prostate cancer)
Other side effects include more erections than are normal for you or erections that last a long time.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of testosterone topical solution. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of testosterone topical solution.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use testosterone topical solution for a condition for which it was not prescribed. Do not give testosterone topical solution to other people, even if they have the same symptoms you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about testosterone topical solution that is written for health professionals.
What are the ingredients in testosterone topical solution?
Active ingredient: testosterone USP.
Inactive ingredients: ethanol, isopropyl alcohol, octisalate, and povidone.
The bottle and the applicator cup are not made with natural rubber latex.
For more information, go to www.lupinpharmaceuticals.com or call 1-800-399-2561.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Testosterone (tes TOS ter one) Topical Solution USP, for topical use, CIII
Read this Instructions for Use for testosterone topical solution before you start using it and each time you get a refill. There may be new information. This leaflet does not take the place of talking to your healthcare provider about your medical condition or treatment.
Applying Testosterone Topical Solution:
- Testosterone topical solution is to be applied to the armpits only. Do not apply mtestosterone topical solution to any other parts of your body such as your stomach area (abdomen), penis, scrotum, shoulders or upper arms.
- Do not apply testosterone topical solution with your fingers or hands.
- Apply testosterone topical solution at about the same time each morning. Testosterone topical solution should be applied after showering or bathing.
- Avoid swimming or bathing for at least 2 hours after you apply testosterone topical solution.
- You can use an antiperspirant or deodorant before applying testosterone topical solution. If you use antiperspirant or deodorant, then it should be applied at least 2 minutes before you apply testosterone topical solution.
- Testosterone topical solution is flammable until dry. Let testosterone topical solution dry before smoking or going near an open flame.
- Avoid splashing in the eyes. In case of contact with eyes, flush thoroughly with water. If irritation persists, seek medical advice.
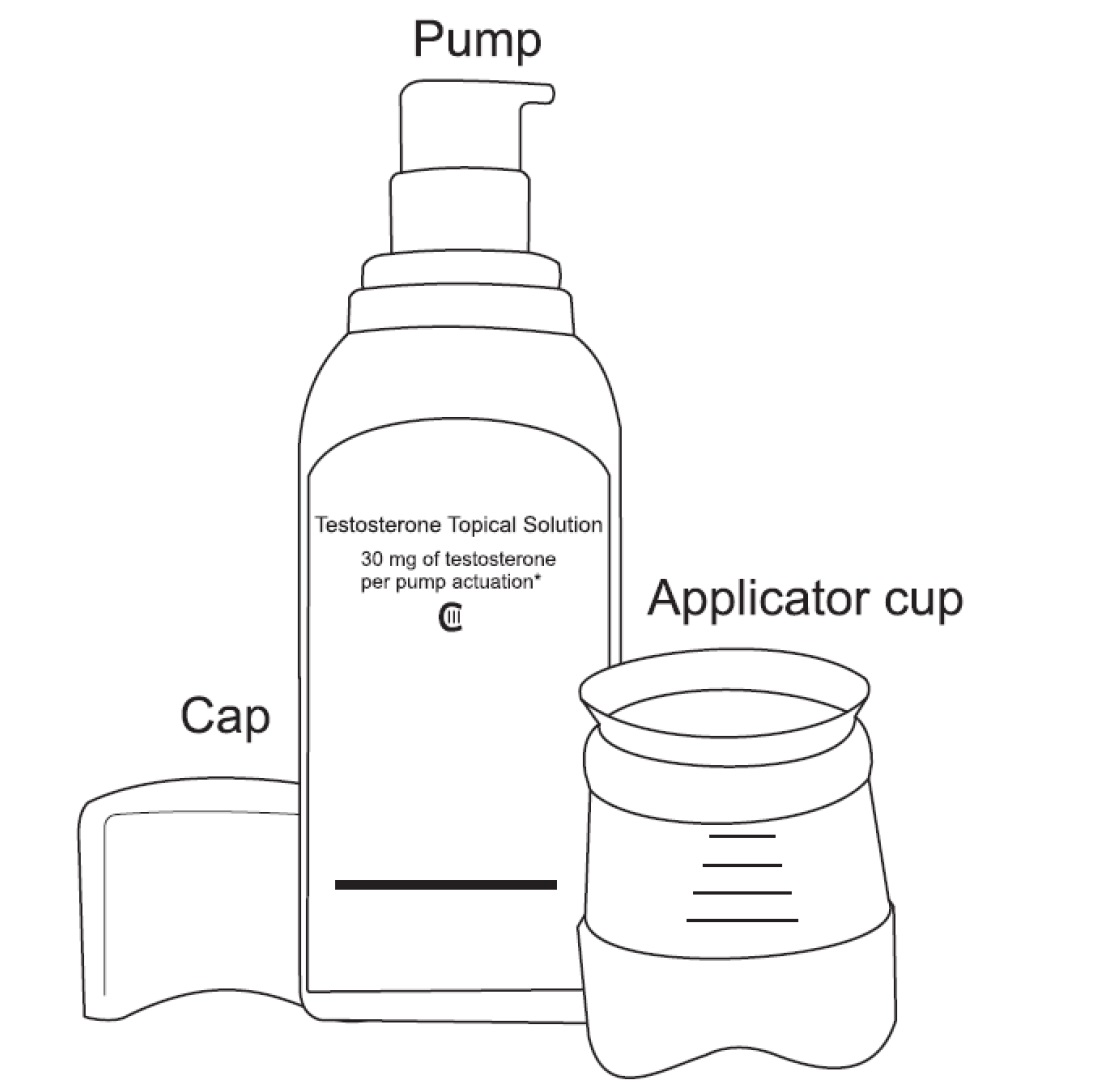
Testosterone Topical Solution Figure 1
- Before using a new bottle of testosterone topical solution for the first time, you will need to prime the pump. To prime the testosterone topical solution pump gently push down on the pump 3 times. Do not use any testosterone topical solution that came out while priming. Wash it down the sink to avoid accidental exposure to others. Your testosterone topical solution pump is now ready to use.
- Use testosterone topical solution exactly as your healthcare provider tells you to use it. Your healthcare provider will tell you the dose of testosterone topical solution that is right for you. Apply your dose correctly by following the application instructions in the table below.
Find Your Dose as Prescribed by Your Healthcare Provider
Each application equals 1 press (depression) of the pump.
30 mg
Apply 1 application one time to one armpit only (left or right).
60 mg
Apply 2 applications: one to the left armpit and then one to the right armpit.
90 mg
Apply 3 applications: one to the left and one to the right armpit, wait for the product to dry, and then apply again one to the left or right armpit.
120 mg
Apply 4 applications: one to the left and one to the right armpit, wait for the product to dry, and then apply again one to the left and one to the right armpit.
- Before applying testosterone topical solution, make sure that your armpit is clean, dry and that there is no broken skin.
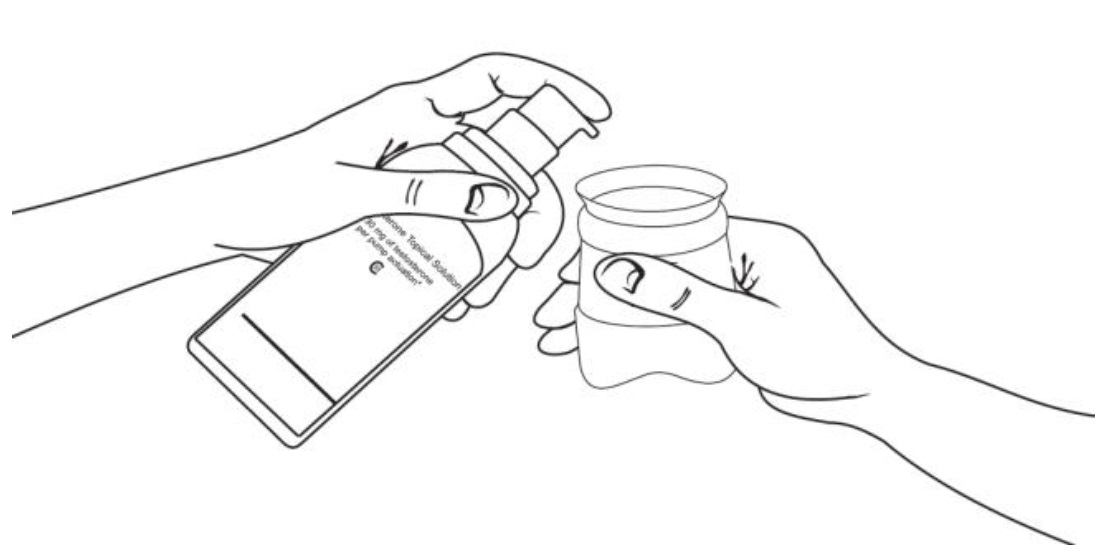
- Remove the cap and the applicator cup from the pump. Then, position the nozzle over the applicator cup and gently press down on (depress) the pump (see Figure 2 ).

- To apply the testosterone topical solution, keep the applicator upright, place it up into the armpit application site and wipe steadily down and up (see Figure 3 ).
- If testosterone topical solution drips or runs, wipe it back up with the applicator cup. Do not rub in the solution with your fingers or hand after it has been applied.
- Let the application site dry completely for 3 minutes before putting on a shirt.
- After you have finished applying testosterone topical solution, rinse the applicator cup with room temperature running water, and then pat it dry with a tissue. Carefully replace the applicator cup and cap back onto the bottle and make sure you store the bottle safely.
- Clean up any spilled solution from surfaces such as the sink or floor to make sure others do not come into contact with it.
- Wash your hands with soap and water right away.
How should I store testosterone topical solution?
- Store testosterone topical solution upright at room temperature between 68°F to 77°F (20°C to 25°C).
- When it is time to throw away the bottle, safely throw away all parts of the testosterone topical solution dispenser including the bottle applicator cup and cap into the household trash.
- Be careful to prevent accidental exposure of children or pets.
- Keep testosterone topical solution away from fire.
Keep testosterone topical solution and all medicines out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration.
Manufactured for:
Lupin Pharmaceuticals, Inc.
Baltimore, Maryland 21202
United States
Manufactured by:
Lupin Limited
Pithampur (M.P.) – 454 775
India
April 2020 ID#: 262879
-
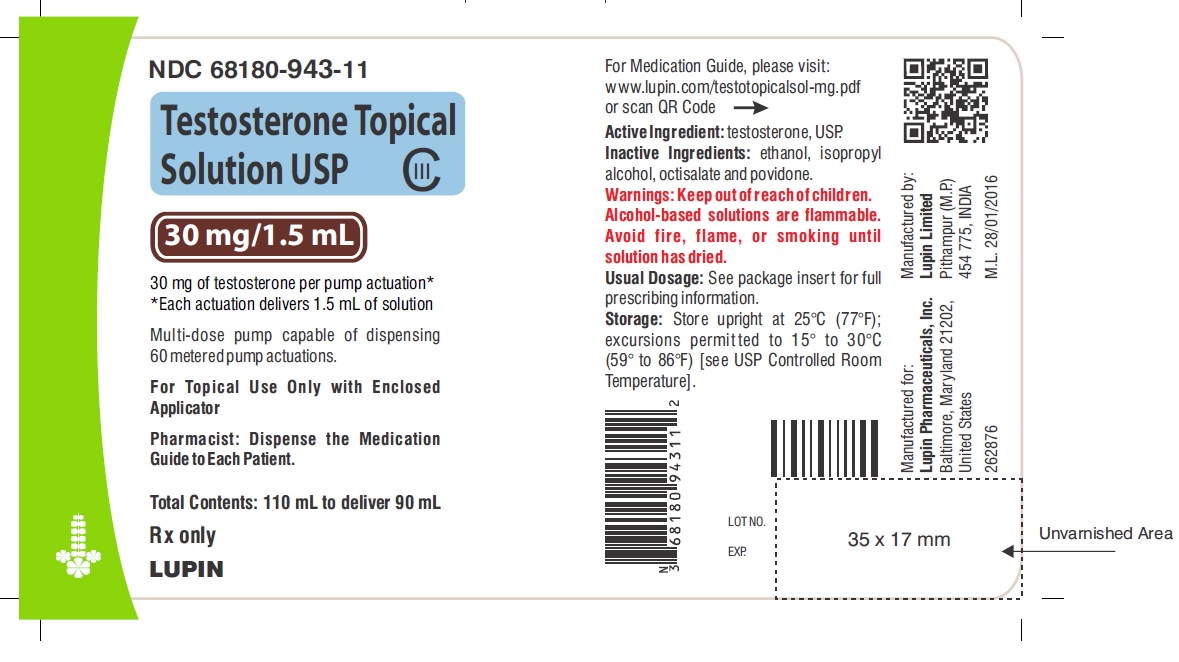
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL
30 mg of testosterone per pump actuation CIII
Each actuation delivers 1.5 mL of solution
Multi-dose pump capable of dispensing 60 metered pump actuations.
For topical use only with enclosed applicator
Dispense the enclosed Medication Guide to each patient
Rx Only
NDC 68180-943-11
Carton Label
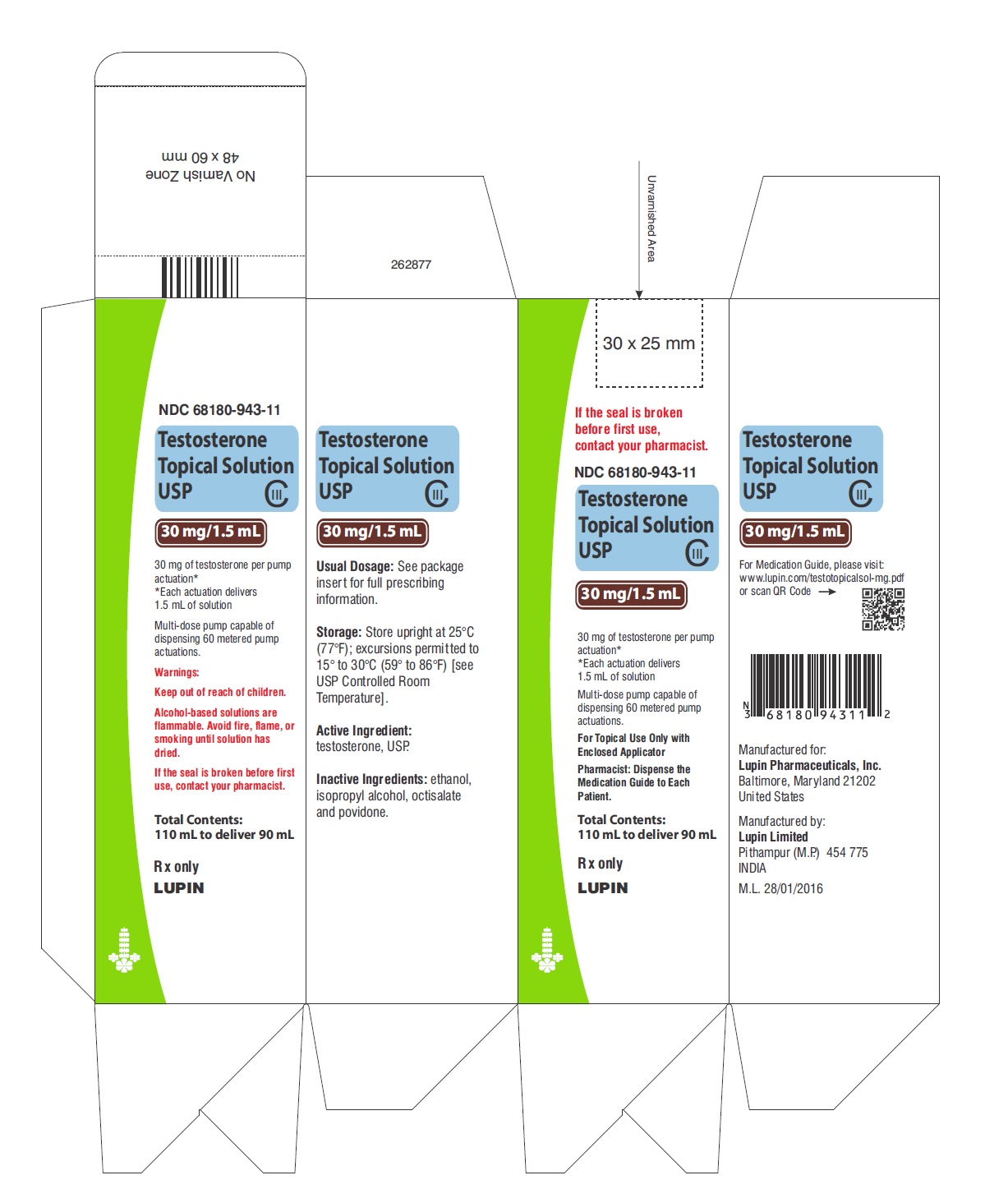
30 mg of testosterone per pump actuation CIII
Each actuation delivers 1.5 mL of solution
Multi-dose pump capable of dispensing 60 metered pump actuations.
For topical use only with enclosed applicator
Dispense the enclosed Medication Guide to each patient
Rx Only
NDC 68180-943-11
Container Label
-
INGREDIENTS AND APPEARANCE
TESTOSTERONE
testosterone solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:68180-943 Route of Administration TOPICAL DEA Schedule CIII Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength TESTOSTERONE (UNII: 3XMK78S47O) (TESTOSTERONE - UNII:3XMK78S47O) TESTOSTERONE 30 mg in 1.5 mL Inactive Ingredients Ingredient Name Strength ALCOHOL (UNII: 3K9958V90M) ISOPROPYL ALCOHOL (UNII: ND2M416302) OCTISALATE (UNII: 4X49Y0596W) POVIDONE (UNII: FZ989GH94E) Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:68180-943-11 1 in 1 CARTON 02/23/2018 1 90 mL in 1 BOTTLE, WITH APPLICATOR; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA208061 02/23/2018 Labeler - Lupin Pharmaceuticals, Inc. (089153071) Registrant - LUPIN LIMITED (675923163) Establishment Name Address ID/FEI Business Operations LUPIN LIMITED 650595213 MANUFACTURE(68180-943) , PACK(68180-943)