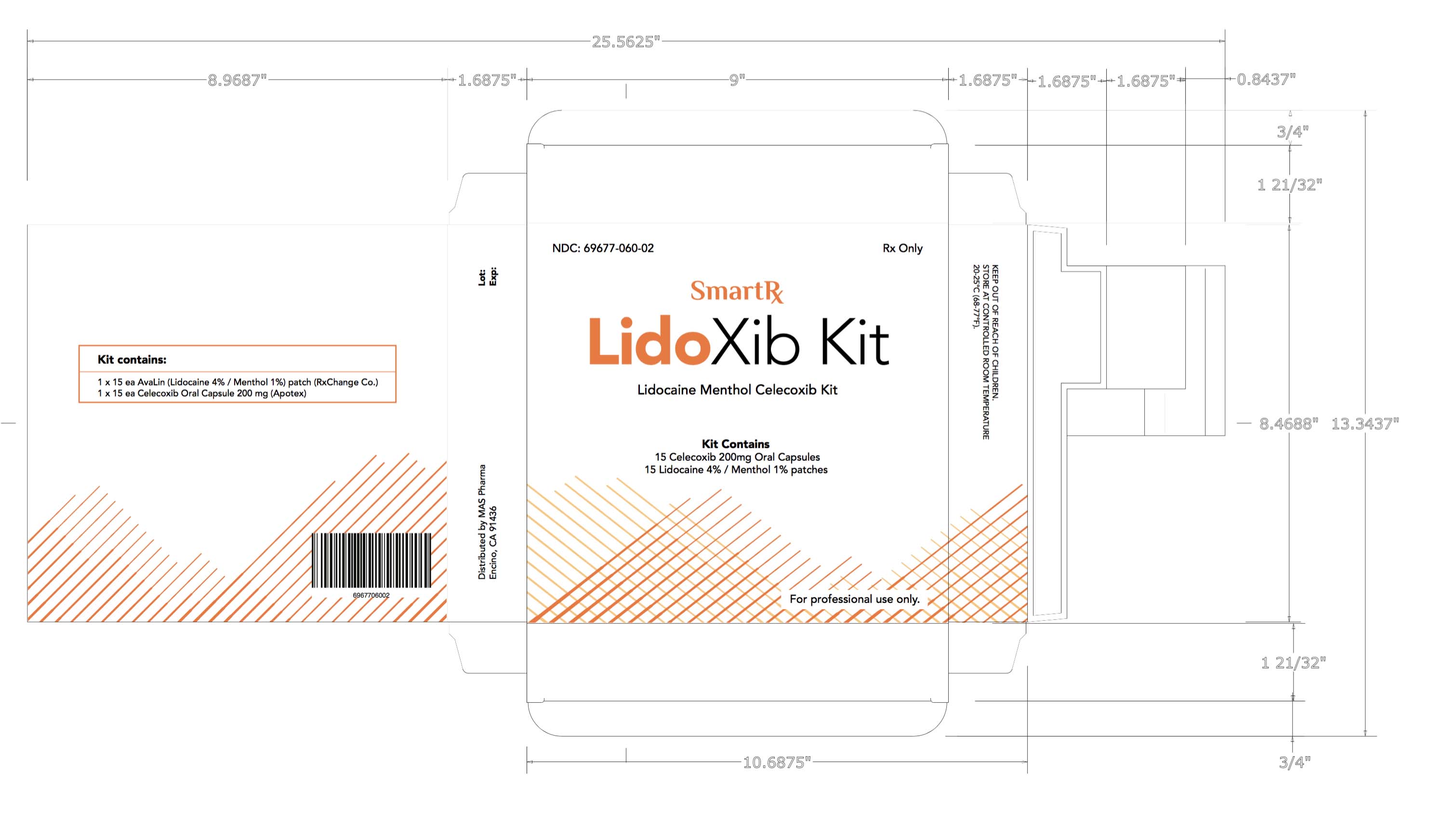
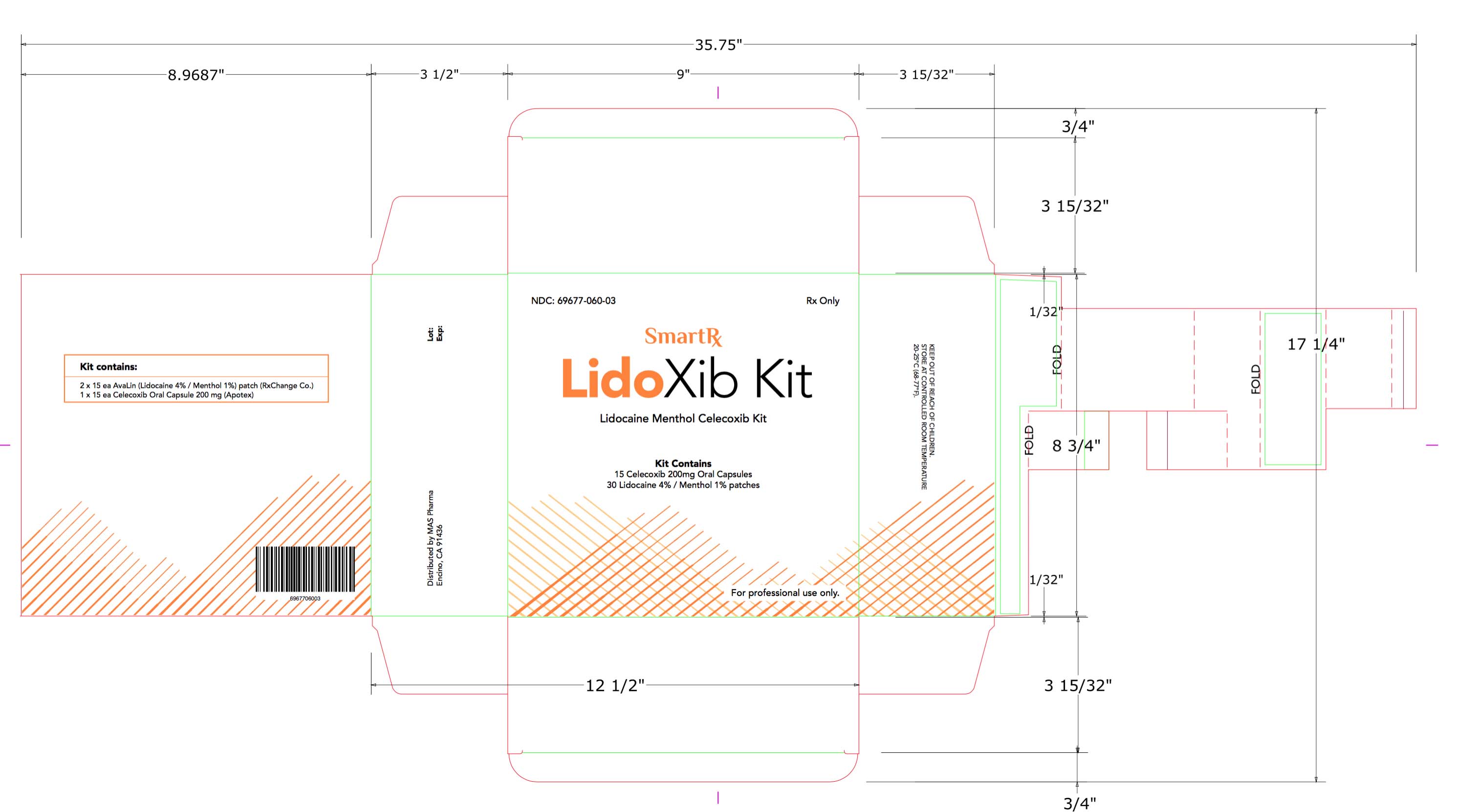
LIDOXIB- celecoxib, lidocaine, menthol
MAS Management Group
Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here.
----------
INDICATIONS AND USAGE
Carefully consider the potential benefits and risks of celecoxib and other treatment options before deciding to use celecoxib capsules. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals
DOSAGE AND ADMINISTRATION
Use lowest effective dose for the shortest duration consistent with treatment goals for the individual patient.
These doses can be given without regard to timing of meals.
Osteoarthritis
For relief of the signs and symptoms of OA the recommended oral dose is 200 mg per day administered as a single dose or as 100 mg twice daily.
Rheumatoid Arthritis
For relief of the signs and symptoms of RA the recommended oral dose is 100 to 200 mg twice daily.
Juvenile Rheumatoid Arthritis
For the relief of the signs and symptoms of JRA the recommended oral dose for pediatric patients (age 2 years and older) is based on weight. For patients ≥10 kg to ≤25 kg the recommended dose is 50 mg twice daily. For patients >25 kg the recommended dose is 100 mg twice daily.
For patients who have difficulty swallowing capsules, the contents of a celecoxib capsule can be added to applesauce. The entire capsule contents are carefully emptied onto a level teaspoon of cool or room temperature applesauce and ingested immediately with water. The sprinkled capsule contents on applesauce are stable for up to 6 hours under refrigerated conditions (2 to 8° C/ 35 to 45° F).
Ankylosing Spondylitis
For the management of the signs and symptoms of AS, the recommended dose of celecoxib capsules is 200 mg daily in single (once per day) or divided (twice per day) doses. If no effect is observed after 6 weeks, a trial of 400 mg daily may be worthwhile. If no effect is observed after 6 weeks on 400 mg daily, a response is not likely and consideration should be given to alternate treatment options.
CONTRAINDICATIONS
Celecoxib capsules are contraindicated:
- In patients with known hypersensitivity to celecoxib, aspirin, or other NSAIDs.
- In patients who have demonstrated allergic-type reactions to sulfonamides.
- In patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe anaphylactoid reactions to NSAIDs, some of them fatal, have been reported in such patients.
- For the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery.
WARNINGS AND PRECAUTIONS
WARNING: CARDIOVASCULAR AND GASTROINTESTINAL RISKS
Cardiovascular Thrombotic Events
- · Nonsteroidal anti-inflammatory drugs (NSAIDS) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.
- · Celecoxib is contraindicated in the setting of coronary artery bypass graft (CABG) surgery.
Gastrointestinal Risk
- · NSAIDs, including celecoxib, cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events.
Cardiovascular Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDS of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, including myocardial infarction (MI) and stroke, which can be fatal. Based on available data, it is unclear that the risk for CV thrombotic events is similar for all NSAIDs. The relative increase in serious CV thrombotic events over baseline conferred by NSAID use appears to be similar in those with and without known CV disease or risk factors for CV disease. However, patients with known CV disease or risk factors had a higher absolute incidence of excess serious CV thrombotic events, due to their increased baseline rate. Some observational studies found that this increased risk of serious CV thrombotic events began as early as the first weeks of treatment. The increase in CV thrombotic risk has been observed most consistently at higher doses.
To minimize the potential risk for an adverse CV event in NSAID-treated patients, use the lowest effective dose for the shortest duration possible. Physicians and patients should remain alert for the development of such events, throughout the entire treatment course, even in the absence of previous CV symptoms. Patients should be informed about the symptoms of serious CV events and the steps to take if they occur. There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID, such as celecoxib increases the risk of serious gastrointestinal (GI) events.
Status Post Coronary Artery Bypass Graft (CABG) Surgery
Two large, controlled, clinical trials of a different COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery found an increased incidence of myocardial infarction and stroke.
Post-MI Patients
Observational studies conducted in the Danish National Registry have demonstrated that patients treated with NSAIDs in the post-MI period were at increased risk of reinfarction, CV-related death, and all-cause mortality beginning in the first week of treatment. In this same cohort, the incidence of death in the first year post MI was 20 per 100 person years in NSAID-treated patients compared to 12 per 100 person years in non-NSAID exposed patients. Although the absolute rate of death declined somewhat after the first year post-MI, the increased relative risk of death in NSAID users persisted over at least the next four years of follow-up.
Avoid the use of celecoxib in patients with a recent MI unless the benefits are expected to outweigh the risk of recurrent CV thrombotic events. If celecoxib is used in patients with a recent MI, monitor patients for signs of cardiac ischemia.
Hypertension
As with all NSAIDs, celecoxib can lead to the onset of new hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including celecoxib, should be used with caution in patients with hypertension. Blood pressure should be monitored closely during the initiation of therapy with celecoxib and throughout the course of therapy. The rates of hypertension from the CLASS trial in the celecoxib, ibuprofen and diclofenac-treated patients were 2.4%, 4.2% and 2.5%, respectively.
Gastrointestinal (GI) Effects
Risk of GI Ulceration, Bleeding, and Perforation
NSAIDs, including celecoxib, can cause serious gastrointestinal events including bleeding, ulceration, and perforation of the stomach, small intestine or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients who develop a serious upper GI adverse event on NSAID therapy is symptomatic. Complicated and symptomatic ulcer rates were 0.78% at nine months for all patients in the CLASS trial, and 2.19% for the subgroup on low-dose ASA. Patients 65 years of age and older had an incidence of 1.40% at nine months, 3.06% when also taking ASA. With longer duration of use of NSAIDs, there is a trend for increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
NSAIDs should be prescribed with extreme caution in patients with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10-fold increased risk for developing a GI bleed compared to patients with neither of these risk factors. Other factors that increase the risk of GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore special care should be taken in treating this population.
To minimize the potential risk for an adverse GI event, the lowest effective dose should be used for the shortest duration consistent with individual patient treatment goals. Physicians and patients should remain alert for signs and symptoms of GI ulceration and bleeding during celecoxib therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. For high-risk patients, alternate therapies that do not involve NSAIDs should be considered.
Hepatic Effects
Borderline elevations of one or more liver-associated enzymes may occur in up to 15% of patients taking NSAIDs, and notable elevations of ALT or AST (approximately 3 or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Rare cases of severe hepatic reactions, including jaundice and fatal fulminant hepatitis, liver necrosis and hepatic failure (some with fatal outcome) have been reported with NSAIDs, including celecoxib. In controlled clinical trials of celecoxib, the incidence of borderline elevations (greater than or equal to 1.2 times and less than 3 times the upper limit of normal) of liver associated enzymes was 6% for celecoxib and 5% for placebo, and approximately 0.2% of patients taking celecoxib and 0.3% of patients taking placebo had notable elevations of ALT and AST.
A patient with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred, should be monitored carefully for evidence of the development of a more severe hepatic reaction while on therapy with celecoxib. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), celecoxib should be discontinued.
Renal Effects
Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of an NSAID may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics, ACE-inhibitors, angiotensin II receptor antagonists, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state. Clinical trials with celecoxib have shown renal effects similar to those observed with comparator NSAIDs.
No information is available from controlled clinical studies regarding the use of celecoxib in patients with advanced renal disease. Therefore, treatment with celecoxib is not recommended in these patients with advanced renal disease. If celecoxib therapy must be initiated, close monitoring of the patient's renal function is advisable.
Anaphylactoid Reactions
As with NSAIDs in general, anaphylactoid reactions have occurred in patients without known prior exposure to celecoxib. In post-marketing experience, rare cases of anaphylactic reactions and angioedema have been reported in patients receiving celecoxib. Celecoxib should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs. Emergency help should be sought in cases where an anaphylactoid reaction occurs.
Skin Reactions
Celecoxib is a sulfonamide and can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events can occur without warning and in patients without prior known sulfa allergy. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
Pregnancy
In late pregnancy, starting at 30 weeks gestation, celecoxib should be avoided because it may cause premature closure of the ductus arteriosus.
Corticosteroid Treatment
Celecoxib cannot be expected to substitute for corticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to exacerbation of corticosteroid-responsive illness. Patients on prolonged corticosteroid therapy should have their therapy tapered slowly if a decision is made to discontinue corticosteroids.
Hematological Effects
Anemia is sometimes seen in patients receiving celecoxib. In controlled clinical trials the incidence of anemia was 0.6% with celecoxib and 0.4% with placebo. Patients on long-term treatment with celecoxib should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia or blood loss. Celecoxib does not generally affect platelet counts, prothrombin time (PT), or partial thromboplastin time (PTT), and does not inhibit platelet aggregation at indicated dosages.
Disseminated Intravascular Coagulation (DIC)
Celecoxib should be used only with caution in pediatric patients with systemic onset JRA due to the risk of disseminated intravascular coagulation.
Preexisting Asthma
Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm, which can be fatal. Since cross reactivity, including bronchospasm, between aspirin and other nonsteroidal anti-inflammatory drugs has been reported in such aspirin-sensitive patients, celecoxib should not be administered to patients with this form of aspirin sensitivity and should be used with caution in patients with preexisting asthma.
Laboratory Tests
Because serious GI tract ulcerations and bleeding can occur without warning symptoms, physicians should monitor for signs or symptoms of GI bleeding. Patients on long-term treatment with NSAIDs should have a CBC and a chemistry profile checked periodically. If abnormal liver tests or renal tests persist or worsen, celecoxib should be discontinued.
In controlled clinical trials, elevated BUN occurred more frequently in patients receiving celecoxib compared with patients on placebo. This laboratory abnormality was also seen in patients who received comparator NSAIDs in these studies. The clinical significance of this abnormality has not been established.
ADVERSE REACTIONS
Of the celecoxib-treated patients in the pre-marketing controlled clinical trials, approximately 4,250 were patients with OA, approximately 2,100 were patients with RA, and approximately 1,050 were patients with post-surgical pain. More than 8,500 patients received a total daily dose of celecoxib of 200 mg (100 mg twice daily or 200 mg once daily) or more, including more than 400 treated at 800 mg (400 mg twice daily). Approximately 3,900 patients received celecoxib at these doses for 6 months or more; approximately 2,300 of these have received it for 1 year or more and 124 of these have received it for 2 years or more.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse reaction information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates.
DRUG INTERACTIONS
- Concomitant use of celecoxib and warfarin may result in increased risk of bleeding complications.
- Concomitant use of celecoxib increases lithium plasma levels.
- Concomitant use of celecoxib may reduce the antihypertensive effect of ACE Inhibitors and angiotensin II antagonists.
- Use caution with drugs known to inhibit P450 2C9 or metabolized by 2D6 due to the potential for increased plasma levels.
General: Celecoxib metabolism is predominantly mediated via cytochrome P450 (CYP) 2C9 in the liver. Co-administration of celecoxib with drugs that are known to inhibit CYP2C9 should be done with caution. Significant interactions may occur when celecoxib is administered together with drugs that inhibit CYP2C9.
In vitro studies indicate that celecoxib, although not a substrate, is an inhibitor of CYP2D6. Therefore, there is a potential for an in vivo drug interaction with drugs that are metabolized by CYP2D6.
Warfarin
Anticoagulant activity should be monitored, particularly in the first few days, after initiating or changing celecoxib therapy in patients receiving warfarin or similar agents, since these patients are at an increased risk of bleeding complications. The effect of celecoxib on the anticoagulant effect of warfarin was studied in a group of healthy subjects receiving daily 2 to 5 mg doses of warfarin. In these subjects, celecoxib did not alter the anticoagulant effect of warfarin as determined by prothrombin time. However, in post-marketing experience, serious bleeding events, some of which were fatal, have been reported, predominantly in the elderly, in association with increases in prothrombin time in patients receiving celecoxib concurrently with warfarin.
Lithium
In a study conducted in healthy subjects, mean steady-state lithium plasma levels increased approximately 17% in subjects receiving lithium 450 mg twice daily with celecoxib 200 mg twice daily as compared to subjects receiving lithium alone. Patients on lithium treatment should be closely monitored when celecoxib is introduced or withdrawn.
Aspirin
Celecoxib can be used with low-dose aspirin. However, concomitant administration of aspirin with celecoxib increases the rate of GI ulceration or other complications, compared to use of celecoxib alone and. Because of its lack of platelet effects, celecoxib is not a substitute for aspirin for cardiovascular prophylaxis [see CLINICAL PHARMACOLOGY].
ACE-Inhibitors and Angiotensin II Antagonists
Reports suggest that NSAIDs may diminish the antihypertensive effect of Angiotensin Converting Enzyme (ACE) inhibitors and angiotensin II antagonists. This interaction should be given consideration in patients taking celecoxib capsules concomitantly with ACE-inhibitors and angiotensin II antagonists [see CLINICAL PHARMACOLOGY].
Fluconazole
Concomitant administration of fluconazole at 200 mg once daily resulted in a two-fold increase in celecoxib plasma concentration. This increase is due to the inhibition of celecoxib metabolism via P450 2C9 by fluconazole. Celecoxib should be introduced at the lowest recommended dose in patients receiving fluconazole.
Furosemide
Clinical studies, as well as post-marketing observations, have shown that NSAIDs can reduce the natriuretic effect of furosemide and thiazides in some patients. This response has been attributed to inhibition of renal prostaglandin synthesis.
USE IN SPECIFIC POPULATIONS
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 11/2015
Labor and Delivery
Celecoxib produced no evidence of delayed labor or parturition at oral doses up to 100 mg/kg in rats (approximately 7-fold human exposure as measured by the AUC0–24 at 200 mg BID). The effects of celecoxib on labor and delivery in pregnant women are unknown.
Nursing Mothers
Limited data from 3 published reports that included a total of 12 breastfeeding women showed low levels of celecoxib in breast milk. The calculated average daily infant dose was 10 to 40 mcg/kg/day, less than 1% of the weight-based therapeutic dose for a two-year old-child. A report of two breastfed infants 17 and 22 months of age did not show any adverse events. Caution should be exercised when celecoxib is administered to a nursing woman.
Pediatric Use
Celecoxib is approved for relief of the signs and symptoms of Juvenile Rheumatoid Arthritis in patients 2 years and older. Safety and efficacy have not been studied beyond six months in children. The long-term cardiovascular toxicity in children exposed to celecoxib has not been evaluated and it is unknown if long-term risks may be similar to that seen in adults exposed to celecoxib or other COX-2 selective and non-selective NSAIDs.
The use of celecoxib in patients 2 years to 17 years of age with pauciarticular, polyarticular course JRA or in patients with systemic onset JRA was studied in a 12-week, double-blind, active controlled, pharmacokinetic, safety and efficacy study, with a 12-week open-label extension. Celecoxib has not been studied in patients under the age of 2 years, in patients with body weight less than 10 kg (22 lbs), and in patients with active systemic features. Patients with systemic onset JRA (without active systemic features) appear to be at risk for the development of abnormal coagulation laboratory tests. In some patients with systemic onset JRA, both celecoxib and naproxen were associated with mild prolongation of activated partial thromboplastin time (APTT) but not prothrombin time (PT). NSAIDs including celecoxib should be used only with caution in patients with systemic onset JRA, due to the risk of disseminated intravascular coagulation. Patients with systemic onset JRA should be monitored for the development of abnormal coagulation tests.
Alternative therapies for treatment of JRA should be considered in pediatric patients identified to be CYP2C9 poor metabolizers.
Geriatric Use
Of the total number of patients who received celecoxib in pre-approval clinical trials, more than 3,300 were 65 to 74 years of age, while approximately 1,300 additional patients were 75 years and over. No substantial differences in effectiveness were observed between these subjects and younger subjects. In clinical studies comparing renal function as measured by the GFR, BUN and creatinine, and platelet function as measured by bleeding time and platelet aggregation, the results were not different between elderly and young volunteers. However, as with other NSAIDs, including those that selectively inhibit COX-2, there have been more spontaneous post-marketing reports of fatal GI events and acute renal failure in the elderly than in younger patients.
Hepatic Insufficiency
The daily recommended dose of celecoxib capsules in patients with moderate hepatic impairment (Child-Pugh Class B) should be reduced by 50%. The use of celecoxib capsules in patients with severe hepatic impairment is not recommended.
Poor Metabolizers of CYP2C9 Substrates
Patients who are known or suspected to be poor CYP2C9 metabolizers based on genotype or previous history/experience with other CYP2C9 substrates (such as warfarin, phenytoin) should be administered celecoxib with caution. Consider starting treatment at half the lowest recommended dose in poor metabolizers (i.e., CYP2C9*3/*3). Alternative management should be considered in JRA patients identified to be CYP2C9 poor metabolizers.
OVERDOSAGE
No overdoses of celecoxib were reported during clinical trials. Doses up to 2400 mg/day for up to 10 days in 12 patients did not result in serious toxicity. Symptoms following acute NSAID overdoses are usually limited to lethargy, drowsiness, nausea, vomiting, and epigastric pain, which are generally reversible with supportive care. Gastrointestinal bleeding can occur. Hypertension, acute renal failure, respiratory depression and coma may occur, but are rare. Anaphylactoid reactions have been reported with therapeutic ingestion of NSAIDs, and may occur following an overdose.
Patients should be managed by symptomatic and supportive care following an NSAID overdose. There are no specific antidotes. No information is available regarding the removal of celecoxib by hemodialysis, but based on its high degree of plasma protein binding (>97%) dialysis is unlikely to be useful in overdose. Emesis and/or activated charcoal (60 to 100 g in adults, 1 to 2 g/kg in children) and/or osmotic cathartic may be indicated in patients seen within 4 hours of ingestion with symptoms or following a large overdose. Forced diuresis, alkalinization of urine, hemodialysis, or hemoperfusion may not be useful due to high protein binding.
DESCRIPTION
Celecoxib is chemically designated as 4-[5-(4-methylphenyl)- 3-(trifluoromethyl)-1H-pyrazol-1-yl] benzenesulfonamide and is a diaryl-substituted pyrazole. The empirical formula is C17H14F3N3O2S, and the molecular weight is 381.38; the chemical structure is as follows:
Celecoxib capsules for oral administration contain either 50 mg, 100 mg, or 200 mg of celecoxib, together with inactive ingredients including: crospovidone, sodium lauryl sulphate, povidone, magnesium stearate. The capsule shell contains gelatin and titanium dioxide. The capsule imprinting ink for the 50 mg strength contains shellac, ethyl alcohol, isopropyl alcohol, butyl alcohol, propylene glycol, sodium hydroxide, titanium dioxide, povidone and FD&C Red #40 Aluminum Lake. The capsule imprinting ink for the 100 mg strength contains shellac, ethyl alcohol, isopropyl alcohol, butyl alcohol, propylene glycol, strong ammonia solution, and FD&C Blue #2 Aluminum Lake. The capsule imprinting ink for the 200 mg strength contains shellac, ethyl alcohol, isopropyl alcohol, butyl alcohol, propylene glycol, strong ammonia solution, iron oxide yellow, and dimethicone.
CLINICAL PHARMACOLOGY
Mechanism of Action
Celecoxib is a nonsteroidal anti-inflammatory drug that exhibits anti-inflammatory, analgesic, and antipyretic activities in animal models. The mechanism of action of celecoxib is believed to be due to inhibition of prostaglandin synthesis, primarily via inhibition of cyclooxygenase-2 (COX-2), and at therapeutic concentrations in humans, celecoxib does not inhibit the cyclooxygenase-1 (COX-1) isoenzyme. In animal colon tumor models, celecoxib reduced the incidence and multiplicity of tumors.
Pharmacogenomics
CYP2C9 activity is reduced in individuals with genetic polymorphisms that lead to reduced enzyme activity, such as those homozygous for the CYP2C9*2 and CYP2C9*3 polymorphisms. Limited data from 4 published reports that included a total of 8 subjects with the homozygous CYP2C9*3/*3 genotype showed celecoxib systemic levels that were 3- to 7-fold higher in these subjects compared to subjects with CYP2C9*1/*1 or *I/*3 genotypes. The pharmacokinetics of celecoxib have not been evaluated in subjects with other CYP2C9 polymorphisms, such as *2, *5, *6, *9 and *11. It is estimated that the frequency of the homozygous *3/*3 genotype is 0.3% to 1.0% in various ethnic groups.
NONCLINICAL TOXICOLOGY
Carcinogenesis, Mutagenesis, Impairment of Fertility
Celecoxib was not carcinogenic in rats given oral doses up to 200 mg/kg for males and 10 mg/kg for females (approximately 2-to 4-fold the human exposure as measured by the AUC0–24 at 200 mg twice daily) or in mice given oral doses up to 25 mg/kg for males and 50 mg/kg for females (approximately equal to human exposure as measured by the AUC0–24 at 200 mg twice daily) for two years.
Celecoxib was not mutagenic in an Ames test and a mutation assay in Chinese hamster ovary (CHO) cells, nor clastogenic in a chromosome aberration assay in CHO cells and an in vivo micronucleus test in rat bone marrow.
Celecoxib did not impair male and female fertility in rats at oral doses up to 600 mg/kg/day (approximately 11-fold human exposure at 200 mg twice daily based on the AUC0–24).
Animal Toxicology
An increase in the incidence of background findings of spermatocele with or without secondary changes such as epididymal hypospermia as well as minimal to slight dilation of the seminiferous tubules was seen in the juvenile rat. These reproductive findings while apparently treatment-related did not increase in incidence or severity with dose and may indicate an exacerbation of a spontaneous condition. Similar reproductive findings were not observed in studies of juvenile or adult dogs or in adult rats treated with celecoxib. The clinical significance of this observation is unknown.
CLINICAL STUDIES
Osteoarthritis
Celecoxib has demonstrated significant reduction in joint pain compared to placebo. Celecoxib was evaluated for treatment of the signs and the symptoms of OA of the knee and hip in placebo- and active-controlled clinical trials of up to 12 weeks duration. In patients with OA, treatment with celecoxib 100 mg twice daily or 200 mg once daily resulted in improvement in WOMAC (Western Ontario and McMaster Universities) osteoarthritis index, a composite of pain, stiffness, and functional measures in OA. In three 12-week studies of pain accompanying OA flare, celecoxib doses of 100 mg twice daily and 200 mg twice daily provided significant reduction of pain within 24 to 48 hours of initiation of dosing. At doses of 100 mg twice daily or 200 mg twice daily the effectiveness of celecoxib was shown to be similar to that of naproxen 500 mg twice daily. Doses of 200 mg twice daily provided no additional benefit above that seen with 100 mg twice daily. A total daily dose of 200 mg has been shown to be equally effective whether administered as 100 mg twice daily or 200 mg once daily.
Rheumatoid Arthritis
Celecoxib has demonstrated significant reduction in joint tenderness/pain and joint swelling compared to placebo. Celecoxib was evaluated for treatment of the signs and symptoms of RA in placebo- and active-controlled clinical trials of up to 24 weeks in duration. Celecoxib was shown to be superior to placebo in these studies, using the ACR20 Responder Index, a composite of clinical, laboratory, and functional measures in RA. Celecoxib doses of 100 mg twice daily and 200 mg twice daily were similar in effectiveness and both were comparable to naproxen 500 mg twice daily.
Although celecoxib 100 mg twice daily and 200 mg twice daily provided similar overall effectiveness, some patients derived additional benefit from the 200 mg twice daily dose. Doses of 400 mg twice daily provided no additional benefit above that seen with 100 to 200 mg twice daily.
Juvenile Rheumatoid Arthritis
In a 12-week, randomized, double-blind active-controlled, parallel-group, multicenter, non-inferiority study, patients from 2 years to 17 years of age with pauciarticular, polyarticular course JRA or systemic onset JRA (with currently inactive systemic features), received one of the following treatments: celecoxib 3 mg/kg (to a maximum of 150 mg) twice daily; celecoxib 6 mg/kg (to a maximum of 300 mg) twice daily; or naproxen 7.5 mg/kg (to a maximum of 500 mg) twice daily. The response rates were based upon the JRA Definition of Improvement greater than or equal to 30% (JRA DOI 30) criterion, which is a composite of clinical, laboratory, and functional measures of JRA. The JRA DOI 30 response rates at week 12 were 69%, 80% and 67% in the celecoxib 3 mg/kg BID, celecoxib 6 mg/kg BID, and naproxen 7.5 mg/kg BID treatment groups, respectively.
The efficacy and safety of celecoxib for JRA have not been studied beyond six months. The long-term cardiovascular toxicity in children exposed to celecoxib has not been evaluated and it is unknown if the long-term risk may be similar to that seen in adults exposed to celecoxib or other COX-2 selective and non-selective NSAIDs.
Ankylosing Spondylitis
Celecoxib was evaluated in AS patients in two placebo- and active-controlled clinical trials of 6 and 12 weeks duration. Celecoxib at doses of 100 mg twice daily, 200 mg once daily and 400 mg once daily was shown to be statistically superior to placebo in these studies for all three co-primary efficacy measures assessing global pain intensity (Visual Analogue Scale), global disease activity (Visual Analogue Scale) and functional impairment (Bath Ankylosing Spondylitis Functional Index). In the 12-week study, there was no difference in the extent of improvement between the 200 mg and 400 mg celecoxib doses in a comparison of mean change from baseline, but there was a greater percentage of patients who responded to celecoxib 400 mg, 53%, than to celecoxib 200 mg, 44%, using the Assessment in Ankylosing Spondylitis response criteria (ASAS 20). The ASAS 20 defines a responder as improvement from baseline of at least 20% and an absolute improvement of at least 10 mm, on a 0 to 100 mm scale, in at least three of the four following domains: patient global pain, Bath Ankylosing Spondylitis Functional Index, and inflammation. The responder analysis also demonstrated no change in the responder rates beyond 6 weeks.
HOW SUPPLIED/STORAGE AND HANDLING
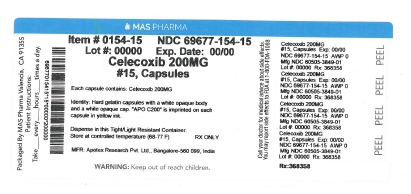
Celecoxib capsules 200 mg are available for oral administration as hard gelatin capsules with a white opaque body and a white opaque cap. “APO C200” is imprinted on each capsule in yellow ink. They are supplied as follows:
Bottles of 30s NDC 60505-3849-3
Bottles of 100s NDC 60505-3849-1
Bottles of 500s NDC 60505-3849-5
Bottles of 1000 NDC 60505-3849-8
Unit Dose Blisters of 100 NDC 60505-3849-0
PATIENT COUNSELING INFORMATION
Patients should be informed of the following information before initiating therapy with celecoxib capsules and periodically during the course of ongoing therapy.
Medication Guide
Patients should be informed of the availability of a Medication Guide for NSAIDs that accompanies each prescription dispensed, and should be instructed to read the Medication Guide prior to using celecoxib capsules.
Cardiovascular Effects
Advise patients to be alert for the symptoms of cardiovascular thrombotic events, including chest pain, shortness of breath, weakness, or slurring of speech, and to report any of these symptoms to their health care provider immediately [see WARNINGS AND PRECAUTIONS].
Patients should be informed that celecoxib can lead to the onset of new hypertension or worsening of preexisting hypertension, and that celecoxib may impair the response of some antihypertensive agents. Patients should be instructed on the proper follow up for monitoring of blood pressure. [see WARNINGS AND PRECAUTIONS] and DRUG INTERACTIONS].
Gastrointestinal Effects
Patients should be informed that celecoxib capsules can cause gastrointestinal discomfort and more serious side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Patients should be informed of the signs and symptoms of ulcerations and bleeding, and to seek immediate medical advice if they observe any signs or symptoms that are indicative of these disorders, including epigastric pain, dyspepsia, melena, and hematemesis [see WARNINGS AND PRECAUTIONS].
Hepatic Effects
Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). Patients should be instructed that they should stop therapy and seek immediate medical therapy if these signs and symptoms occur [see WARNINGS AND PRECAUTIONS, USE IN SPECIFIC POPULATIONS].
Adverse Skin Reactions
Patients should be informed that celecoxib is a sulfonamide and can cause serious skin side effects such as exfoliative dermatitis, SJS, and TEN, which may result in hospitalizations and even death. Although serious skin reactions may occur without warning, patients should be informed of the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and seek immediate medical advice when observing any indicative signs or symptoms.
Patients should be advised to stop celecoxib capsules immediately if they develop any type of rash and contact their physician as soon as possible.
Patients with prior history of sulfa allergy should not take celecoxib capsules [see WARNINGS AND PRECAUTIONS].
Weight Gain and Edema
Long-term administration of NSAIDs including celecoxib has resulted in renal injury. Patients at greatest risk are those taking diuretics, ACE-inhibitors, angiotensin II antagonists, or with renal or liver dysfunction, heart failure, and the elderly [see WARNINGS AND PRECAUTIONS, USE IN SPECIFIC POPULATIONS].
Advise patients to be alert for the symptoms of congestive heart failure including shortness of breath, unexplained weight gain, or edema and to contact their healthcare provider if such symptoms occur [see WARNINGS AND PRECAUTIONS].
Anaphylactoid Reactions
Patients should be informed of the signs and symptoms of an anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). Patients should be instructed to seek immediate emergency assistance if they develop any of these signs and symptoms [see WARNINGS AND PRECAUTIONS].
Effects During Pregnancy
Patients should be informed that in late pregnancy celecoxib capsules should be avoided because it may cause premature closure of the ductus arteriosus [see WARNINGS AND PRECAUTIONS, USE IN SPECIFIC POPULATIONS].
Preexisting Asthma
Patients should be instructed to tell their physicians if they have a history of asthma or aspirin-sensitive asthma because the use of NSAIDs in patients with aspirin-sensitive asthma has been associated with severe bronchospasm, which can be fatal. Patients with this form of aspirin sensitivity should be instructed not to take celecoxib capsules. Patients with preexisting asthma should be instructed to seek immediate medical attention if their asthma worsens after taking celecoxib capsules [see WARNINGS AND PRECAUTION].
MEDICATION GUIDE
Medication Guide for
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
What is the most important information I should know about medicines called Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)?
NSAIDs can cause serious side effects, including:
Increased risk of a heart attack or stroke that can lead to death. This risk may happen early in treatment and may increase:
- with increasing doses of NSAIDs
- with longer use of NSAIDs
Do not take NSAIDs right before or after a heart surgery called a “coronary artery bypass graft (CABG)."
Avoid taking NSAIDs after a recent heart attack, unless your healthcare provider tells you to. You may have an increased risk of another heart attack if you take NSAIDs after a recent heart attack.
Increased risk of bleeding, ulcers, and tears (perforation) of the esophagus (tube leading from the mouth to the stomach), stomach and intestines:
- anytime during use
- without warning symptoms
- that may cause death
The risk of getting an ulcer or bleeding increases with:
- past history of stomach ulcers, or stomach or intestinal bleeding with use of NSAIDs
- taking medicines called “corticosteroids”, “anticoagulants”, “SSRIs”, or “SNRIs”
- increasing doses of NSAIDs
- longer use of NSAIDs
- smoking
- drinking alcohol
- older age
- poor health
- advanced liver disease
- bleeding problems
NSAIDs should only be used: :
- exactly as prescribed
- at the lowest dose possible for your treatment
- for the shortest time needed
What are NSAIDs?
NSAIDs are used to treat pain and redness, swelling, and heat (inflammation) from medical conditions such as different types of arthritis, menstrual cramps, and other types of short-term pain.
Who should not take NSAIDs?
Do not take NSAIDs:
- if you have had an asthma attack, hives, or other allergic reaction with aspirin or any other NSAIDs.
- right before or after heart bypass surgery.
Before taking NSAIDs, tell your healthcare provider about all of your medical conditions, including if you:
- have liver or kidney problems
- have high blood pressure
- have asthma
- are pregnant or plan to become pregnant. Talk to your healthcare provider if you are considering taking NSAIDs during pregnancy. You should not take NSAIDs after 29 weeks of pregnancy.
- are breastfeeding or plan to breast feed.
Tell your healthcare provider about all of the medicines you take, including prescription or over-the-counter medicines, vitamins or herbal supplements. NSAIDs and some other medicines can interact with each other and cause serious side effects. Do not start taking any new medicine without talking to your healthcare provider first.
What are the possible side effects of NSAIDs?
NSAIDs can cause serious side effects, including:
See “What is the most important information I should know about medicines called Nonsteroidal Anti-inflammatory Drugs (NSAIDs)?
- new or worse high blood pressure
- heart failure
- liver problems including liver failure
- kidney problems including kidney failure
- low red blood cells (anemia)
- life-threatening skin reactions
- life-threatening allergic reactions
Other side effects of NSAIDs include: stomach pain, constipation, diarrhea, gas, heartburn, nausea, vomiting, and dizziness.
Get emergency help right away if you get any of the following symptoms:
- shortness of breath or trouble breathing
- chest pain
- weakness in one part or side of your body
- slurred speech
- swelling of the face or throat
Stop taking your NSAID and call your healthcare provider right away if you get any of the following symptoms:
- nausea
- more tired or weaker than usual
- diarrhea
- itching
- your skin or eyes look yellow
- indigestion or stomach pain
- flu-like symptoms
- vomit blood
- there is blood in your bowel movement or it is black and sticky like tar
- unusual weight gain
- skin rash or blisters with fever
- swelling of the arms, legs, hands and feet
If you take too much of your NSAID, call your healthcare provider or get medical help right away.
These are not all the possible side effects of NSAIDs. For more information, ask your healthcare provider or pharmacist about NSAIDs.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Other information about NSAIDs
- Aspirin is an NSAID but it does not increase the chance of a heart attack. Aspirin can cause bleeding in the brain, stomach, and intestines. Aspirin can also cause ulcers in the stomach and intestines.
- Some NSAIDs are sold in lower doses without a prescription (over-the-counter). Talk to your healthcare provider before using over-the-counter NSAIDs for more than 10 days.
General information about the safe and effective use of NSAIDs
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use NSAIDs for a condition for which it was not prescribed. Do not give NSAIDs to other people, even if they have the same symptoms that you have. It may harm them.
If you would like more information about NSAIDs, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about NSAIDs that is written for health professionals.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Manufactured by
Apotex Inc
Toronto, Ontario
Canada M9L 1T9
Manufactured by
Apotex Research Pvt. Ltd.
Bangalore - 560 099
Manufactured for
Apotex Corp.
Weston, Florida
USA 33326
Revised: November 2016
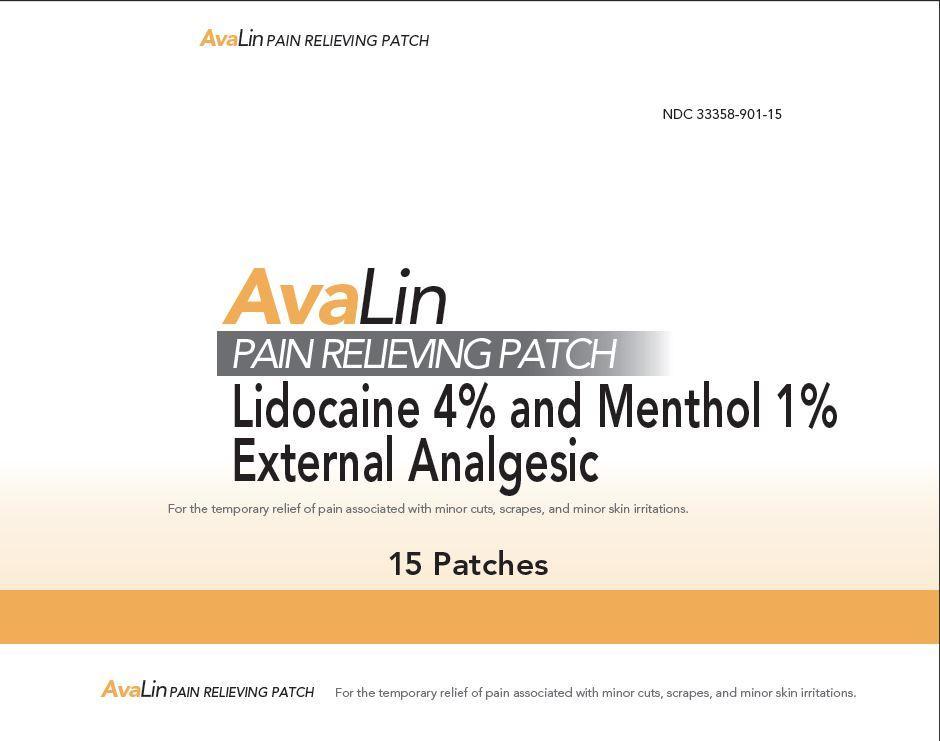
DIRECTIONS
- Adults and children 2 years of age and older: Apply to the affected area not more than 3 to 4 times daily.
- Children under 2 years of age: Consult a doctor.
- Clean and dry affected area.
- Remove patch from backing and apply to affected area.
- Use one patch at a time.
- Leave patch on affected area for up to 8-hours at a time
INACTIVE INGREDIENTS
acrylic acid, aluminum hydroxide, carmellose sodium, 2-ethylhexyl acrylate, glycerin, isopropyl myristate, methyl acrylate, nonoxynol-30, polyacrylate, polyacrylic acid, polysorbate 80, sorbitan sesquioleate, starch, talc, tartaric acid, titanium dioxide, water
| LIDOXIB
celecoxib, lidocaine, menthol kit |
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
| Labeler - MAS Management Group (079363782) |