Label: COSYNTROPIN injection, powder, lyophilized, for solution
- NDC Code(s): 0781-3440-71, 0781-3440-95
- Packager: Sandoz Inc
- Category: HUMAN PRESCRIPTION DRUG LABEL
- DEA Schedule: None
- Marketing Status: Abbreviated New Drug Application
Drug Label Information
Updated January 10, 2024
If you are a consumer or patient please visit this version.
- Download DRUG LABEL INFO: PDF XML
- Official Label (Printer Friendly)
-
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use COSYNTROPIN FOR INJECTION safely and effectively. See full prescribing information for COSYNTROPIN FOR INJECTION.
COSYNTROPIN for injection, for intravenous or intramuscular use
Initial U.S. Approval: 2008INDICATIONS AND USAGE
Cosyntropin for injection is an adrenocorticotropin hormone indicated, in combination with other diagnostic tests, for use as a diagnostic agent in the screening of adrenocortical insufficiency in adults and pediatric patients. (1)
DOSAGE AND ADMINISTRATION
- •
- In general, stop glucocorticoids and spironolactone on the day of cosyntropin for injection testing. For long-acting glucocorticoids, stop for a longer period before cosyntropin for injection testing. (2.1)
- •
- For adults, the recommended dose is 0.25 mg to be administered by intravenous or intramuscular injection. (2.2)
- •
- For pediatric patients, the recommended dose to be administered by intravenous or intramuscular injection is (2.3):
- o
- 0.125 mg for patients birth to less than 2 years of age
- o
- 0.25 mg for patients 2 to 17 years of age
- •
- Obtain blood samples for serum cortisol level at baseline and exactly 30 and 60 minutes after cosyntropin for injection administration. (2.5)
- •
- See Full Prescribing Information for reconstitution and interpretation of cortisol levels information. (2.4, 2.6)
DOSAGE FORMS AND STRENGTHS
- •
- For injection: 0.25 mg of cosyntropin as a lyophilized powder in single-dose vial for reconstitution (3)
CONTRAINDICATIONS
WARNINGS AND PRECAUTIONS
- •
- Hypersensitivity: reactions including anaphylaxis have been reported. Monitor patients for hypersensitivity reactions and treat as needed. (5.1)
- •
- Diagnostic Inaccuracies: Cortisol levels and subsequent diagnosis of adrenocortical insufficiency following cosyntropin for injection administration may be inaccurate if patients are on certain medications because of their effect on cortisol or cortisol binding globulin levels. Any condition that elevates or lowers cortisol binding globulin levels may increase or decrease plasma total cortisol levels, respectively. (2.1, 5.2, 7)
ADVERSE REACTIONS
Most common adverse reactions are: anaphylactic reaction, bradycardia, tachycardia, hypertension, peripheral edema, and rash (6)
To report SUSPECTED ADVERSE REACTIONS, contact Sandoz Inc. at 1-800-525-8747 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
- •
- Drug effects on plasma cortisol levels:
- o
- Accuracy of the test results can be affected by concomitant medications.
- o
- Glucocorticoids and spironolactone: May falsely elevate plasma cortisol levels. Stop these drugs on day of cosyntropin for injection testing. Long-acting glucocorticoids may need to be stopped for a longer period before cosyntropin for injection testing. (7)
- o
- Estrogen: May elevate plasma total cortisol levels. Stop estrogen containing drugs 4 to 6 weeks before cosyntropin for injection testing. (7)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 1/2024
-
Table of Contents
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Important Information Before Conducting Cosyntropin for Injection Testing
2.2 Recommended Dose for Adults
2.3 Recommended Dose for Pediatric Patients
2.4 Reconstitution Instructions
2.5 Administration Information
2.6 Interpretation of Plasma Cortisol Levels after Cosyntropin for Injection
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity to Cosyntropin for Injection
5.2 Diagnostic Inaccuracies
6 ADVERSE REACTIONS
7 DRUG INTERACTIONS
7.1 Drug Effects on Plasma Cortisol Levels
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
- *
- Sections or subsections omitted from the full prescribing information are not listed.
- 1 INDICATIONS AND USAGE
-
2 DOSAGE AND ADMINISTRATION
2.1 Important Information Before Conducting Cosyntropin for Injection Testing
- •
- In general, stop glucocorticoids and spironolactone on the day of cosyntropin for injection testing. However, long-acting glucocorticoids may need to be stopped for a longer period before cosyntropin for injection testing [seeWarnings and Precautions (5.2), Drug Interactions (7)].
- •
- Stop estrogen-containing drugs four to six weeks before cosyntropin for injection testing [see Warnings andPrecautions (5.2), Drug Interactions (7)].
2.2 Recommended Dose for Adults
- •
- The recommended dose of cosyntropin for injection in adults is 0.25 mg to be administered by intravenous or intramuscular injection.
2.3 Recommended Dose for Pediatric Patients
- •
- The recommended dose of cosyntropin for injection in pediatric patients, aged birth to 17 years, to be administered by intravenous or intramuscular injection is presented in Table 1.
Table 1. Recommended Cosyntropin for Injection Dose for Pediatric Patients
Age
Recommended Dose
Volume of Reconstituted Solution
Birth to less than 2 years
0.125 mg
0.5 mL
2 to 17 years
0.25 mg
1 mL
2.4 Reconstitution Instructions
- •
- Aseptically reconstitute the lyophilized powder in the vial using 1 mL of 0.9% Sodium Chloride Injection, USP and gently swirl.
- •
- After reconstitution, the final concentration of cosyntropin for injection reconstituted solution is 0.25 mg/mL.
- •
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. The reconstituted cosyntropin for injection solution should be clear and colorless, and free of particulates. If cosyntropin for injection solution is cloudy or contains particulates, do not administer.
- •
- If the cosyntropin for injection reconstituted solution is not used immediately, discard the unused cosyntropin for injection reconstituted solution.
2.5 Administration Information
- •
- Cosyntropin for injection may be administered by intramuscular or intravenous injection.
- •
- Obtain blood sample for baseline serum cortisol. Obtain blood samples again for assessment of cortisol levels exactly 30 minutes and 60 minutes after administration of cosyntropin for injection.
2.6 Interpretation of Plasma Cortisol Levels after Cosyntropin for Injection
- •
- Stimulated plasma cortisol levels of less than 18 mcg/dL at 30- or 60-minutes post cosyntropin for injection are suggestive of adrenocortical insufficiency. Cutoff values for exclusion of adrenocortical insufficiency may vary according to the assay used. Test results can be affected by concomitant medications and certain medical conditions [see Warnings and Precautions (5.2)].
- 3 DOSAGE FORMS AND STRENGTHS
-
4 CONTRAINDICATIONS
Cosyntropin for injection is contraindicated in patients with a history of hypersensitivity to cosyntropin or to any excipients of cosyntropin for injection. Reactions have included anaphylaxis [see Warnings and Precautions (5.1)].
-
5 WARNINGS AND PRECAUTIONS
5.1 Hypersensitivity to Cosyntropin for Injection
Cosyntropin for injection hypersensitivity reactions including anaphylaxis have been reported. Monitor patients for hypersensitivity reactions and treat as needed.
5.2 Diagnostic Inaccuracies
Cortisol levels and subsequent diagnosis of adrenocortical insufficiency following cosyntropin for injection administration may be inaccurate if patients are on certain medications because of their effect on cortisol or cortisol binding globulin levels.
Glucocorticoids and spironolactone may result in falsely elevated cortisol levels. Stop these drugs on the day of cosyntropin for injection testing. Long-acting glucocorticoids may need to be stopped for a longer period before cosyntropin for injection testing [see Dosage and Administration (2.1) and Drug Interactions (7)].
Estrogen-containing drugs increase cortisol binding globulin levels which can increase plasma total cortisol levels. To obtain accurate plasma total cortisol levels, stop estrogen containing drugs four to six weeks before cosyntropin for injection testing to allow cortisol binding globulin levels to return to levels within the reference range [see Dosage and Administration(2.1)and Drug Interactions (7)]. Alternatively, concomitant measurement of cortisol binding globulin at the time of testing can be done; if cortisol binding globulin levels are elevated, plasma total cortisol levels are considered inaccurate.
Any condition that elevates or lowers cortisol binding globulin levels may increase or decrease plasma total cortisol levels, respectively. Cortisol binding globulin levels can be low in cirrhosis or nephrotic syndrome. Measure cortisol binding globulin levels as necessary to ensure accuracy of interpretation of plasma total cortisol levels.
-
6 ADVERSE REACTIONS
Because adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The following adverse reactions have been identified during post approval use of cosyntropin for injection:
- •
- anaphylactic reaction
- •
- bradycardia
- •
- tachycardia
- •
- hypertension
- •
- peripheral edema
- •
- rash
-
7 DRUG INTERACTIONS
7.1 Drug Effects on Plasma Cortisol Levels
- •
- Accuracy of the test results can be affected by concomitant medications. Plasma cortisol levels and subsequent diagnosis of adrenocortical insufficiency following cosyntropin for injection administration may be inaccurate if patients are on certain medications because of their effect on cortisol or cortisol binding globulin levels [see Dosage and Administration (2.1) and Warnings and Precautions (5.2)].
- •
- Glucocorticoids and spironolactone: May falsely elevate plasma cortisol levels. Stop these drugs on the day of cosyntropin for injection testing. Long-acting glucocorticoids may need to be stopped for a longer period before cosyntropin for injection testing.
- •
- Estrogen: May elevate plasma total cortisol levels. Stop estrogen containing drugs 4 to 6 weeks before cosyntropin for injection testing to allow cortisol binding globulin levels to return to levels within the reference range. Alternatively, concomitant measurement of cortisol binding globulin at the time of testing can be done; if cortisol binding globulin levels are elevated, plasma total cortisol levels are considered inaccurate.
-
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
Available data from case reports over decades of use with cosyntropin during pregnancy have not identified an increasedrisk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Unidentified adrenal insufficiency can resultin adverse maternal or fetal outcomes (see Clinical Considerations).
The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk for major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
Unidentified adrenal insufficiency during pregnancy can result in maternal and/or fetal death; therefore, the diagnosis of suspected adrenal insufficiency during pregnancy should not be delayed.
8.2 Lactation
Risk Summary
There are no data on the presence of cosyntropin in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for cosyntropin for injection and any potential adverse effects on the breastfed infant from cosyntropin for injection or from the underlying maternal condition.
8.4 Pediatric Use
Cosyntropin for injection is approved for use in pediatric patients [see Dosage and Administration (2.3)].
-
11 DESCRIPTION
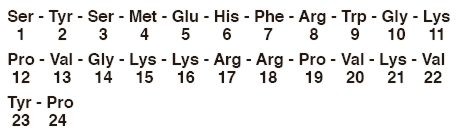
Cosyntropin is an adrenocorticotropic hormone (ACTH). Cosyntropin is synthetic beta 1 - 24 corticotropin, a synthetic subunit of ACTH. It is an open chain polypeptide containing, the first 24 of the 39 amino acids of natural ACTH in sequence from N terminal. The sequence of amino acids in the 1 - 24 compound is as follows:
Molecular Formula: C136H210N40O31S
Molecular Weight: 2933 g/mol.
Cosyntropin for injection is a sterile lyophilized powder in single-dose vials containing 0.25 mg of cosyntropin and 10 mg of mannitol.
-
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
Cosyntropin exhibits the full corticosteroidogenic activity of natural ACTH. Various studies have shown that the biologic activity of ACTH resides in the N-terminal portion of the molecule and that the 1-20 amino acid residue is the minimal sequence retaining full activity. Partial or complete loss of activity is noted with progressive shortening of the chain beyond 20 amino acid residues. For example, the decrement from 20 to 19 results in a 70% loss of potency.
The pharmacologic profile of cosyntropin is similar to that of purified natural ACTH. It has been established that 0.25 mg of cosyntropin will stimulate the adrenal cortex maximally and to the same extent as 25 units of natural ACTH. This dose of cosyntropin will produce maximal secretion of 17-OH corticosteroids, 17-ketosteroids and/or 17-ketogenic steroids.
12.2 Pharmacodynamics
Animal, human and synthetic ACTH (1-39) which all contain 39 amino acids exhibit similar immunologic activity. This activity resides in the C-terminal portion of the molecule and the 22-39 amino acid residues exhibit the greatest degree of antigenicity. In contrast, synthetic polypeptides containing 1-19 or fewer amino acids have no detectable immunologic activity. Those containing 1-26, 1-24 or 1-23 amino acids have very little immunologic although full biologic activity. This property of cosyntropin assumes added importance in view of the known antigenicity of natural ACTH.
- 13 NONCLINICAL TOXICOLOGY
-
16 HOW SUPPLIED/STORAGE AND HANDLING
How Supplied
Cosyntropin for injection 0.25 mg, in a single-dose vial for reconstitution.
Box contains 10 single-dose vials NDC 0781-3440-95
Storage and Handling
Store at 20º to 25ºC (68º to 77ºF); excursions permitted between 15° to 30°C (59° to 86°F) [see USP Controlled Room
Temperature].
Cosyntropin for injection is intended as a single-dose injection and contains no antimicrobial preservative. Any unused
portion should be discarded.
-
17 PATIENT COUNSELING INFORMATION
Advise the patient and/or caregiver to read the FDA-approved patient labeling (Patient Information).
Hypersensitivity Reactions, Including Anaphylaxis
Inform patients and/or caregivers of the early signs of hypersensitivity reactions including rash, hives, itching, facialswelling, tightness of the chest, and wheezing [see Contraindications (4), Warnings and Precautions (5.1)].
Drug Interference with Cosyntropin for Injection Testing
Advise patients and/or caregivers to stop taking glucocorticoids and spironolactone on the day of cosyntropin for injection testing. However, for patients taking long-acting glucocorticoids, advise them to stop for longer periods before cosyntropin for injection testing. Advise patients to stop taking estrogen-containing drugs four to six weeks before cosyntropin for injection testing [seeDosage and Administration (2.1), Warnings and Precautions (5.2), and Drug Interactions (7)].
Manufactured by Oakwood Labs, for
Sandoz Inc., Princeton, NJ 08540
- PACKAGE/LABEL PRINCIPAL DISPLAY PANEL
-
INGREDIENTS AND APPEARANCE
COSYNTROPIN
cosyntropin injection, powder, lyophilized, for solutionProduct Information Product Type HUMAN PRESCRIPTION DRUG Item Code (Source) NDC:0781-3440 Route of Administration INTRAVENOUS Active Ingredient/Active Moiety Ingredient Name Basis of Strength Strength COSYNTROPIN (UNII: 72YY86EA29) (COSYNTROPIN - UNII:72YY86EA29) COSYNTROPIN 0.25 mg in 1 mL Inactive Ingredients Ingredient Name Strength MANNITOL (UNII: 3OWL53L36A) 10 mg in 1 mL Packaging # Item Code Package Description Marketing Start Date Marketing End Date 1 NDC:0781-3440-95 10 in 1 CARTON 06/29/2012 1 NDC:0781-3440-71 1 mL in 1 VIAL; Type 0: Not a Combination Product Marketing Information Marketing Category Application Number or Monograph Citation Marketing Start Date Marketing End Date ANDA ANDA202147 06/29/2012 Labeler - Sandoz Inc (005387188)