FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Heart Failure in Adults
Digoxin is indicated for the treatment of mild to moderate heart failure in adults. Digoxin increases left ventricular ejection fraction and improves heart failure symptoms, as evidenced by improved exercise capacity and decreased heart failure-related hospitalizations and emergency care, while having no effect on mortality. Where possible, digoxin should be used in combination with a diuretic and an angiotensin-converting enzyme (ACE) inhibitor.
2 DOSAGE AND ADMINISTRATION
2.1 Important Dosing and Administration Information
In selecting a digoxin dosing regimen, it is important to consider factors that affect digoxin blood levels (e.g., body weight, age, renal function, concomitant drugs) since toxic levels of digoxin are only slightly higher than therapeutic levels. Dosing can be either initiated with a loading dose followed by maintenance dosing if rapid titration is desired or initiated with maintenance dosing without a loading dose.
Parenteral administration of digoxin should be used only when the need for rapid digitalization is urgent or when the drug cannot be taken orally. Intramuscular injection can lead to severe pain at the injection site, thus intravenous administration is preferred. If the drug must be administered by the intramuscular route, it should be injected deep into the muscle followed by massage. For adults, no more than 500 mcg of Digoxin Injection should be injected into a single site. For pediatric patients, see the full prescribing information for pediatric digoxin injection (not available from West-Ward) for specific recommendations.
Administer the dose over a period of 5 minutes or longer and avoid bolus administration to prevent systemic and coronary vasoconstriction. Mixing of Digoxin Injection with other drugs in the same container or simultaneous administration in the same intravenous line is not recommended.
Digoxin Injection can be administered undiluted or diluted with a 4-fold or greater volume of Sterile Water for Injection, 0.9% Sodium Chloride Injection, or 5% Dextrose Injection. The use of less than a 4-fold volume of diluent could lead to precipitation of the digoxin. Immediate use of the diluted product is recommended.
If tuberculin syringes are used to measure very small doses do not flush with the parenteral solution after its contents are expelled into an indwelling vascular catheter to avoid overadministration of digoxin.
Consider interruption or reduction in digoxin dose prior to electrical cardioversion [see Warnings and Precautions (5.4)].
2.2 Loading Dosing Regimen in Adults and Pediatric Patients Over 10 Years Old
| mcg = microgram | |
| Age | Total IV Loading Dose (mcg/kg) Administer half the total loading dose initially, then ¼ the loading dose every 6-8 hours twice |
| Adults and pediatric patients over 10 years old | 8-12 |
2.3 Maintenance Dosing in Adults and Pediatric Patients Over 10 Years Old
The maintenance dose is based on lean body weight, renal function, age, and concomitant products [see Clinical Pharmacology (12.3)].
The recommended starting maintenance dose in adults and pediatric patients over 10 years old with normal renal function is given in Table 2. Doses may be increased every 2 weeks according to clinical response, serum drug levels, and toxicity.
| mcg = microgram | |
| Age | Total Intravenous Maintenance Dose, mcg/kg/day (given once daily) |
| Adults and pediatric patients over 10 years old | 2.4-3.6 |
Table 3 provides the recommended (once daily) maintenance dose for adults and pediatric patients over 10 years old according to lean body weight and renal function. The doses are based on studies in adult patients with heart failure. Alternatively, the maintenance dose may be estimated by the following formula (peak body stores lost each day through elimination):
Total Maintenance Dose = Loading Dose (i.e., Peak Body Stores) x % Daily Loss/100
(% Daily Loss = 14 + Creatinine clearance/5)
Reduce the dose of digoxin in patients whose lean weight is an abnormally small fraction of their total body mass because of obesity or edema.
|
a For adults, creatinine clearance was corrected to 70-kg body weight or 1.73 m2 body surface area. If only serum creatinine concentrations (Scr) are available, a corrected Ccr may be estimated in men as (140 – Age)/Scr. For women, this result should be multiplied by 0.85. For pediatric patients, the modified Schwartz equation may be used. The formula is based on height in cm and Scr in mg/dL where k is a constant. Ccr is corrected to 1.73 m2 body surface area. During the first year of life, the value of k is 0.33 for pre-term babies and 0.45 for term infants. The k is 0.55 for pediatric patients and adolescent girls and 0.7 for adolescent boys. GFR (mL/min/1.73 m2) = (k x Height)/Scr b If no loading dose administered c The doses listed assume average body composition. |
|||||||||
| Corrected Creatinine Clearancea | Lean Body Weightc | Number of Days Before Steady State Achievedb |
|||||||
| kg | 40 | 50 | 60 | 70 | 80 | 90 | 100 | ||
| 10 mL/min | 64 | 80 | 96 | 112 | 128 | 144 | 160 | 19 | |
| 20 mL/min | 72 | 90 | 108 | 126 | 144 | 162 | 180 | 16 | |
| 30 mL/min | 80 | 100 | 120 | 140 | 160 | 180 | 200 | 14 | |
| 40 mL/min | 88 | 110 | 132 | 154 | 176 | 198 | 220 | 13 | |
| 50 mL/min | 96 | 120 | 144 | 168 | 192 | 216 | 240 | 12 | |
| 60 mL/min | 104 | 130 | 156 | 182 | 208 | 234 | 260 | 11 | |
| 70 mL/min | 112 | 140 | 168 | 196 | 224 | 252 | 280 | 10 | |
| 80 mL/min | 120 | 150 | 180 | 210 | 240 | 270 | 300 | 9 | |
| 90 mL/min | 128 | 160 | 192 | 224 | 256 | 288 | 320 | 8 | |
| 100 mL/min | 136 | 170 | 204 | 238 | 272 | 306 | 340 | 7 | |
2.4 Monitoring to Assess Safety, Efficacy, and Therapeutic Blood Levels
Monitor for signs and symptoms of digoxin toxicity and clinical response. Adjust dose based on toxicity, efficacy, and blood levels.
Serum digoxin levels less than 0.5 ng/mL have been associated with diminished efficacy, while levels above 2 ng/mL have been associated with increased toxicity without increased benefit.
Interpret the serum digoxin concentration in the overall clinical context, and do not use an isolated measurement of serum digoxin concentration as the basis for increasing or decreasing the digoxin dose. Serum digoxin concentrations may be falsely elevated by endogenous digoxin-like substances [see Drug Interactions (7.4)]. If the assay is sensitive to these substances, consider obtaining a baseline digoxin level before starting digoxin and correct post-treatment values by the reported baseline level.
Obtain serum digoxin concentrations just before the next scheduled digoxin dose or at least 6 hours after the last dose. The digoxin concentration is likely to be 10-25% lower when sampled right before the next dose (24 hours after dosing) compared to sampling 8 hours after dosing (using once-daily dosing). However, there will be only minor differences in digoxin concentrations using twice daily dosing whether sampling is done at 8 or 12 hours after a dose.
2.5 Switching from Intravenous Digoxin to Oral Digoxin
When switching from intravenous to oral digoxin formulations, make allowances for differences in bioavailability when calculating maintenance dosages (see Table 4).
| Absolute Bioavailability | Equivalent Doses (mcg) | ||||
| Digoxin Tablets | 60-80% | 62.5 | 125 | 250 | 500 |
| Digoxin Intravenous Injection | 100% | 50 | 100 | 200 | 400 |
3 DOSAGE FORMS AND STRENGTHS
Digoxin Injection: Ampuls of 500 mcg (0.5 mg) in 2 mL (250 mcg [0.25 mg] per 1 mL).
4 CONTRAINDICATIONS
Digoxin is contraindicated in patients with:
- Ventricular fibrillation [see Warnings and Precautions (5.1)]
- Known hypersensitivity to digoxin (reactions seen include unexplained rash, swelling of the mouth, lips or throat or a difficulty in breathing). A hypersensitivity reaction to other digitalis preparations usually constitutes a contraindication to digoxin.
5 WARNINGS AND PRECAUTIONS
5.1 Ventricular Fibrillation in Patients With Accessory AV Pathway (Wolff-Parkinson-White Syndrome)
Patients with Wolff-Parkinson-White syndrome who develop atrial fibrillation are at high risk of ventricular fibrillation. Treatment of these patients with digoxin leads to greater slowing of conduction in the atrioventricular node than in accessory pathways, and the risks of rapid ventricular response leading to ventricular fibrillation are thereby increased.
5.2 Sinus Bradycardia and Sino-atrial Block
Digoxin may cause severe sinus bradycardia or sino-atrial block particularly in patients with pre-existing sinus node disease and may cause advanced or complete heart block in patients with pre-existing incomplete AV block. Consider insertion of a pacemaker before treatment with digoxin.
5.3 Digoxin Toxicity
Signs and symptoms of digoxin toxicity include anorexia, nausea, vomiting, visual changes and cardiac arrhythmias [first-degree, second-degree (Wenckebach), or third-degree heart block (including asystole); atrial tachycardia with block; AV dissociation; accelerated junctional (nodal) rhythm; unifocal or multiform ventricular premature contractions (especially bigeminy or trigeminy); ventricular tachycardia; and ventricular fibrillation]. Toxicity is usually associated with digoxin levels greater than 2 ng/mL although symptoms may also occur at lower levels. Low body weight, advanced age or impaired renal function, hypokalemia, hypercalcemia, or hypomagnesemia may predispose to digoxin toxicity. Obtain serum digoxin levels in patients with signs or symptoms of digoxin therapy and interrupt or adjust dose if necessary [see Adverse Reactions (6) and Overdosage (10)]. Assess serum electrolytes and renal function periodically.
The earliest and most frequent manifestation of digoxin toxicity in infants and children is the appearance of cardiac arrhythmias, including sinus bradycardia. In children, the use of digoxin may produce any arrhythmia. The most common are conduction disturbances or supraventricular tachyarrhythmias, such as atrial tachycardia (with or without block) and junctional (nodal) tachycardia. Ventricular arrhythmias are less common. Sinus bradycardia may be a sign of impending digoxin intoxication, especially in infants, even in the absence of first-degree heart block. Any arrhythmias or alteration in cardiac conduction that develops in a child taking digoxin should initially be assumed to be a consequence of digoxin intoxication.
Given that adult patients with heart failure have some symptoms in common with digoxin toxicity, it may be difficult to distinguish digoxin toxicity from heart failure. Misidentification of their etiology might lead the clinician to continue or increase digoxin dosing, when dosing should actually be suspended. When the etiology of these signs and symptoms is not clear, measure serum digoxin levels.
5.4 Risk of Ventricular Arrhythmias During Electrical Cardioversion
It may be desirable to reduce the dose of or discontinue digoxin for 1-2 days prior to electrical cardioversion of atrial fibrillation to avoid the induction of ventricular arrhythmias, but physicians must consider the consequences of increasing the ventricular response if digoxin is decreased or withdrawn. If digitalis toxicity is suspected, elective cardioversion should be delayed. If it is not prudent to delay cardioversion, the lowest possible energy level should be selected to avoid provoking ventricular arrhythmias.
5.5 Risk of Ischemia in Patients With Acute Myocardial Infarction
Digoxin is not recommended in patients with acute myocardial infarction because digoxin may increase myocardial oxygen demand and lead to ischemia.
5.6 Vasoconstriction in Patients With Myocarditis
Digoxin can precipitate vasoconstriction and may promote production of pro-inflammatory cytokines; therefore, avoid use in patients with myocarditis.
5.7 Decreased Cardiac Output in Patients With Preserved Left Ventricular Systolic Function
Patients with heart failure associated with preserved left ventricular ejection fraction may experience decreased cardiac output with use of digoxin. Such disorders include restrictive cardiomyopathy, constrictive pericarditis, amyloid heart disease, and acute cor pulmonale. Patients with idiopathic hypertrophic subaortic stenosis may have worsening of the outflow obstruction due to the inotropic effects of digoxin. Patients with amyloid heart disease may be more susceptible to digoxin toxicity at therapeutic levels because of an increased binding of digoxin to extracellular amyloid fibrils.
Digoxin should generally be avoided in these patients, although it has been used for ventricular rate control in the subgroup of patients with atrial fibrillation.
5.8 Reduced Efficacy in Patients With Hypocalcemia
Hypocalcemia can nullify the effects of digoxin in humans; thus, digoxin may be ineffective until serum calcium is restored to normal. These interactions are related to the fact that digoxin affects contractility and excitability of the heart in a manner similar to that of calcium.
5.9 Altered Response in Thyroid Disorders and Hypermetabolic States
Hypothyroidism may reduce the requirements for digoxin.
Heart failure and/or atrial arrhythmias resulting from hypermetabolic or hyperdynamic states (e.g., hyperthyroidism, hypoxia, or arteriovenous shunt) are best treated by addressing the underlying condition. Atrial arrhythmias associated with hypermetabolic states are particularly resistant to digoxin treatment. Patients with beri beri heart disease may fail to respond adequately to digoxin if the underlying thiamine deficiency is not treated concomitantly.
6 ADVERSE REACTIONS
The following adverse reactions are included in more detail in the Warnings and Precautions section of the label:
- Cardiac arrhythmias [see Warnings and Precautions (5.1, 5.2)]
- Digoxin Toxicity [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In general, the adverse reactions of digoxin are dose-dependent and occur at doses higher than those needed to achieve a therapeutic effect. Hence, adverse reactions are less common when digoxin is used within the recommended dose range, is maintained within the therapeutic serum concentration range, and when there is careful attention to concurrent medications and conditions.
In the DIG trial (a trial investigating the effect of digoxin on mortality and morbidity in patients with heart failure), the incidence of hospitalization for suspected digoxin toxicity was 2% in patients taking digoxin compared to 0.9% in patients taking placebo [see Clinical Studies (14.1)].
The overall incidence of adverse reactions with digoxin has been reported as 5-20%, with 15-20% of adverse events considered serious. Cardiac toxicity accounts for about one-half, gastrointestinal disturbances for about one-fourth, and CNS and other toxicity for about one-fourth of these adverse events.
Gastrointestinal: In addition to nausea and vomiting, the use of digoxin has been associated with abdominal pain, intestinal ischemia, and hemorrhagic necrosis of the intestines.
CNS: Digoxin can cause headache, weakness, dizziness, apathy, confusion, and mental disturbances (such as anxiety, depression, delirium, and hallucination).
Other: Gynecomastia has been occasionally observed following the prolonged use of digoxin. Thrombocytopenia and maculopapular rash and other skin reactions have been rarely observed.
7 DRUG INTERACTIONS
Digoxin has a narrow therapeutic index, increased monitoring of serum digoxin concentrations and for potential signs and symptoms of clinical toxicity is necessary when initiating, adjusting, or discontinuing drugs that may interact with digoxin. Prescribers should consult the prescribing information of any drug which is co-prescribed with digoxin for potential drug interaction information.
7.1 P-Glycoprotein (PGP) Inducers/Inhibitors
Digoxin is a substrate of P-glycoprotein, at the level of intestinal absorption, renal tubular section and biliary-intestinal secretion. Therefore, drugs that induce/inhibit P-glycoprotein have the potential to alter digoxin pharmacokinetics.
7.2 Pharmacokinetic Drug Interactions
Pharmacokinetic interactions have been observed and reported primarily when digoxin is co-administered by oral route. There are very few studies that have evaluated the drug interaction when digoxin is administered via IV route. The magnitude of digoxin exposure change through IV route is generally lower than that through oral route. Table below provides available interaction data using digoxin IV formulation (NA means not available).
| Digoxin concentrations increased greater than 50% | |||
| Digoxin Serum Concentration Increase | Digoxin AUC Increase | Recommendations | |
| Quinidine | NA | 54-83% | Measure serum digoxin concentrations before initiating concomitant drugs. Reduce digoxin concentrations by decreasing dose by approximately 30-50% or by modifying the dosing frequency and continue monitoring. |
| Ritonavir | NA | 86% | |
| Digoxin concentrations increased less than 50% | |||
| Amiodarone | 17% | 40% | Measure serum digoxin concentrations before initiating concomitant drugs. Reduce digoxin concentrations by decreasing the dose by approximately 15-30% or by modifying the dosing frequency and continue monitoring. |
| Propafenone | 28% | 29% | |
| Quinine | NA | 34-38% | |
| Spironolactone | NA | 44% | |
| Verapamil | NA | 24% | |
7.3 Potentially Significant Pharmacodynamic Drug Interactions
Because of considerable variability of pharmacodynamic interactions, the dosage of digoxin should be individualized when patients receive these medications concurrently.
| Drugs that Affect Renal Function | A decline in GFR or tubular secretion, as from ACE inhibitors, angiotensin receptor blockers, nonsteroidal anti-inflammatory drugs [NSAIDs], COX-2 inhibitors may impair the excretion of digoxin. |
|
| Antiarrthymics | Dofetilide | Concomitant administration with digoxin was associated with a higher rate of torsades de pointes. |
| Sotalol | Proarrhythmic events were more common in patients receiving sotalol and digoxin than on either alone; it is not clear whether this represents an interaction or is related to the presence of CHF, a known risk factor for proarrhythmia, in patients receiving digoxin. | |
| Dronedarone | Sudden death was more common in patients receiving digoxin with dronedarone than on either alone; it is not clear whether this represents an interaction or is related to the presence of advanced heart disease, a known risk factor for sudden death in patients receiving digoxin. | |
| Parathyroid Hormone Analog | Teriparatide | Sporadic case reports have suggested that hypercalcemia may predispose patients to digitalis toxicity. Teriparatide transiently increases serum calcium. |
| Thyroid supplement | Thyroid | Treatment of hypothyroidism in patients taking digoxin may increase the dose requirements of digoxin. |
| Sympathomimetics | Epinephrine Norepinephrine Dopamine | Can increase the risk of cardiac arrhythmias. |
| Neuromuscular Blocking Agents | Succinylcholine | May cause sudden extrusion of potassium from muscle cells, causing arrhythmias in patients taking digoxin. |
| Supplements | Calcium | If administered rapidly by intravenous route, can produce serious arrhythmias in digitalized patients. |
| Beta-adrenergic blockers and calcium channel blockers | Additive effects on AV node conduction can result in bradycardia and advanced or complete heart block. | |
| Ivabradine | Can increase the risk of bradycardia. | |
7.4 Drug/Laboratory Test Interactions
Endogenous substances of unknown composition (digoxin-like immunoreactive substances [DLIS]) can interfere with standard radioimmunoassays for digoxin. The interference most often causes results to be falsely positive or falsely elevated, but sometimes it causes results to be falsely reduced. Some assays are more subject to these failings than others. Several LC/MS/MS methods are available that may provide less susceptibility to DLIS interference. DLIS are present in up to half of all neonates and in varying percentages of pregnant women, patients with hypertrophic cardiomyopathy, patients with renal or hepatic dysfunction, and other patients who are volume-expanded for any reason. The measured levels of DLIS (as digoxin equivalents) are usually low (0.2-0.4 ng/mL), but sometimes they reach levels that would be considered therapeutic or even toxic.
In some assays, spironolactone, canrenone, and potassium canrenoate may be falsely detected as digoxin, at levels up to 0.5 ng/mL. Some traditional Chinese and Ayurvedic medicine substances like Chan Su, Siberian Ginseng, Asian Ginseng, Ashwagandha, or Dashen can cause similar interference.
Spironolactone and DLIS are much more extensively protein-bound than digoxin. As a result, assays of free digoxin levels in protein-free ultrafiltrate (which tend to be about 25% less than total levels, consistent with the usual extent of protein binding) are less affected by spironolactone or DLIS. It should be noted that ultrafiltration does not solve all interference problems with alternative medicines. The use of an LC/MS/MS method may be the better option according to the good results it provides, especially in terms of specificity and limit of quantization.
8 USE IN SPECIFIC POPULATIONS
8.2 Labor and Delivery
There are not enough data from clinical trials to determine the safety and efficacy of digoxin during labor and delivery.
8.3 Nursing Mothers
Studies have shown that digoxin distributes into breast milk and that the milk-to-serum concentration ratio is approximately 0.6-0.9. However, the estimated exposure of a nursing infant to digoxin via breastfeeding is far below the usual infant maintenance dose. Therefore, this amount should have no pharmacologic effect upon the infant.
8.4 Pediatric Use
The safety and effectiveness of digoxin in the control of ventricular rate in children with atrial fibrillation have not been established.
The safety and effectiveness of digoxin in the treatment of heart failure in children have not been established in adequate and well-controlled studies. However, in published literature of children with heart failure of various etiologies (e.g., ventricular septal defects, anthracycline toxicity, patent ductus arteriosus), treatment with digoxin has been associated with improvements in hemodynamic parameters and in clinical signs and symptoms.
Newborn infants display considerable variability in their tolerance to digoxin. Premature and immature infants are particularly sensitive to the effects of digoxin, and the dosage of the drug must not only be reduced but must be individualized according to their degree of maturity.
8.5 Geriatric Use
The majority of clinical experience gained with digoxin has been in the elderly population. This experience has not identified differences in response or adverse effects between the elderly and younger patients. However, this drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, which should be based on renal function, and it may be useful to monitor renal function [see Dosage and Administration (2.1)].
8.6 Renal Impairment
The clearance of digoxin can be primarily correlated with the renal function as indicated by creatinine clearance. Table 3 provides the usual daily maintenance dose requirements for digoxin based on creatinine clearance [see Dosage and Administration (2.3)].
Digoxin is primarily excreted by the kidneys; therefore, patients with impaired renal function require smaller than usual maintenance doses of digoxin [see Dosage and Administration (2.3)]. Because of the prolonged elimination half-life, a longer period of time is required to achieve an initial or new steady-state serum concentration in patients with renal impairment than in patients with normal renal function. If appropriate care is not taken to reduce the dose of digoxin, such patients are at high risk for toxicity, and toxic effects will last longer in such patients than in patients with normal renal function.
10 OVERDOSAGE
10.1 Signs and Symptoms in Adults
The signs and symptoms of toxicity are generally similar to those previously described [see Adverse Reactions (6.1)] but may be more frequent and can be more severe. Signs and symptoms of digoxin toxicity become more frequent with levels above 2 ng/mL. However, in deciding whether a patient’s symptoms are due to digoxin, the clinical state together with serum electrolyte levels and thyroid function are important factors [see Dosage and Administration (2)].
Adults: The most common signs and symptoms of digoxin toxicity are nausea, vomiting, anorexia, and fatigue that occur in 30-70% of patients who are overdosed. Extremely high serum concentrations produce hyperkalemia especially in patients with impaired renal function. Almost every type of cardiac arrhythmia has been associated with digoxin overdose and multiple rhythm disturbances in the same patient are common. Peak cardiac effects occur 3-6 hours following ingestion and may persist for 24 hours or longer. Arrhythmias that are considered more characteristic of digoxin toxicity are new-onset Mobitz type 1 A-V block, accelerated junctional rhythms, non-paroxysmal atrial tachycardia with A-V block, and bi-directional ventricular tachycardia. Cardiac arrest from asystole or ventricular fibrillation is usually fatal.
Digoxin toxicity is related to serum concentration. As digoxin serum levels increase above 1.2 ng/mL, there is a potential for increase in adverse reactions. Furthermore, lower potassium levels increases the risk for adverse reactions. In adults with heart disease, clinical observations suggest that an overdose of digoxin of 10-15 mg results in death of half of patients. A dose above 25 mg ingested by an adult without heart disease appeared to be uniformly fatal if no Digoxin Immune Fab (DIGIBIND®, DIGIFAB®) was administered.
Among the extra-cardiac manifestations, gastrointestinal symptoms (e.g., nausea, vomiting, anorexia) are very common (up to 80% incidence) and precede cardiac manifestations in approximately half of the patients in most literature reports. Neurologic manifestations (e.g., dizziness, various CNS disturbances), fatigue, and malaise are very common. Visual manifestations may also occur with aberration in color vision (predominance of yellow green) the most frequent. Neurological and visual symptoms may persist after other signs of toxicity have resolved. In chronic toxicity, nonspecific extra-cardiac symptoms, such as malaise and weakness, may predominate.
10.2 Treatment
Chronic Overdose
If there is suspicion of toxicity, discontinue digoxin and place the patient on a cardiac monitor. Correct factors such as electrolyte abnormalities, thyroid dysfunction, and concomitant medications [see Dosage and Administration (2.4]. Correct hypokalemia by administering potassium so that serum potassium is maintained between 4.0 and 5.5 mmol/L. Potassium is usually administered orally, but when correction of the arrhythmia is urgent and serum potassium concentration is low, potassium may be administered by the intravenous route. Monitor electrocardiogram for any evidence of potassium toxicity (e.g., peaking of T waves) and to observe the effect on the arrhythmia. Avoid potassium salts in patients with bradycardia or heart block. Symptomatic arrhythmias may be treated with Digoxin Immune Fab.
Acute Overdose
Patients who have intentionally or accidently ingested massive doses of digoxin should receive activated charcoal orally or by nasogastric tube regardless of the time since ingestion since digoxin recirculates to the intestine by enterohepatic circulation. In addition to cardiac monitoring, temporarily discontinue digoxin until the adverse reaction resolves. Correct factors that may be contributing to the adverse reactions [see Warnings and Precautions (5)]. In particular, correct hypokalemia and hypomagnesemia. Digoxin is not effectively removed from the body by dialysis because of its large extravascular volume of distribution. Life threatening arrhythmias (ventricular tachycardia, ventricular fibrillation, high degree A-V block, bradyarrhythma, sinus arrest) or hyperkalemia requires administration of Digoxin Immune Fab. Digoxin Immune Fab has been shown to be 80-90% effective in reversing signs and symptoms of digoxin toxicity. Bradycardia and heart block caused by digoxin are parasympathetically mediated and respond to atropine. A temporary cardiac pacemaker may also be used. Ventricular arrhythmias may respond to lidocaine or phenytoin. When a large amount of digoxin has been ingested, especially in patients with impaired renal function, hyperkalemia may be present due to release of potassium from skeletal muscle. In this case, treatment with Digoxin Immune Fab is indicated; an initial treatment with glucose and insulin may be needed if the hyperkalemia is life-threatening. Once the adverse reaction has resolved, therapy with digoxin may be reinstituted following a careful reassessment of dose.
11 DESCRIPTION
Digoxin is one of the cardiac (or digitalis) glycosides, a closely related group of drugs having in common specific effects on the myocardium. These drugs are found in a number of plants. Digoxin is extracted from the leaves of Digitalis lanata. The term “digitalis” is used to designate the whole group of glycosides. The glycosides are composed of two portions: a sugar and a cardenolide (hence “glycosides”).
Digoxin has the chemical name: 3β-[(O-2,6-dideoxy-β-D-ribo-hexopyranosyl-(1→4)-O-2,6-dideoxy-β-D-ribo-hexopyranosyl-(1→4)-2,6-dideoxy-β-D-ribo-hexopyranosyl)oxy]-12β,14-dihydroxy-5β-card-20(22)-enolide, and the following structural formula:
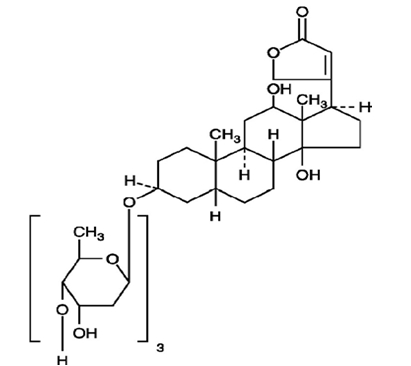
C41H64O14 MW 780.94
Digoxin exists as odorless white crystals that melt with decomposition above 230°C. The drug is practically insoluble in water and in ether; slightly soluble in diluted (50%) alcohol and in chloroform; and freely soluble in pyridine.
Digoxin Injection is a sterile solution for slow intravenous or deep intramuscular injection. Each mL contains digoxin 250 mcg (0.25 mg), alcohol 0.1 mL, propylene glycol 0.4 mL, dibasic sodium phosphate, anhydrous 3 mg and citric acid, anhydrous 0.8 mg in Water for Injection. pH 6.7-7.3; citric acid and/or sodium phosphate added, if necessary, for pH adjustment. Dilution is not required.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
All of digoxin’s actions are mediated through its effects on Na-K ATPase. This enzyme, the “sodium pump,” is responsible for maintaining the intracellular milieu throughout the body by moving sodium ions out of and potassium ions into cells. By inhibiting Na-K ATPase, digoxin
- causes increased availability of intracellular calcium in the myocardium and conduction system, with consequent increased inotropy, increased automaticity, and reduced conduction velocity
- indirectly causes parasympathetic stimulation of the autonomic nervous system, with consequent effects on the sino-atrial (SA) and atrioventricular (AV) nodes
- reduces catecholamine reuptake at nerve terminals, rendering blood vessels more sensitive to endogenous or exogenous catecholamines
- increases baroreceptor sensitization, with consequent increased carotid sinus nerve activity and enhanced sympathetic withdrawal for any given increment in mean arterial pressure
- increases (at higher concentrations) sympathetic outflow from the central nervous system (CNS) to both cardiac and peripheral sympathetic nerves
- allows (at higher concentrations) progressive efflux of intracellular potassium, with consequent increase in serum potassium levels.
The cardiologic consequences of these direct and indirect effects are an increase in the force and velocity of myocardial systolic contraction (positive inotropic action), a slowing of the heart rate (negative chronotropic effect), decreased conduction velocity through the AV node, and a decrease in the degree of activation of the sympathetic nervous system and renin-angiotensin system (neurohormonal deactivating effect).
12.2 Pharmacodynamics
The times to onset of pharmacologic effect and to peak effect of preparations of digoxin are shown in Table 5.
| a Documented for ventricular response rate in atrial fibrillation, inotropic effects and electrocardiographic changes. b Depending upon rate of infusion. |
||
| Product | Time to Onset of Effecta | Time to Peak Effecta |
| Digoxin Tablets | 0.5-2 hours | 2-6 hours |
| Digoxin Injection/IV | 5-30 minutesb | 1-4 hours |
Hemodynamic Effects: Short- and long-term therapy with the drug increases cardiac output and lowers pulmonary artery pressure, pulmonary capillary wedge pressure, and systemic vascular resistance in patients with heart failure. These hemodynamic effects are accompanied by an increase in the left ventricular ejection fraction and a decrease in end-systolic and end-diastolic dimensions.
ECG Changes: The use of therapeutic doses of digoxin may cause prolongation of the PR interval and depression of the ST segment on the electrocardiogram. Digoxin may produce false positive ST-T changes on the electrocardiogram during exercise testing. These electrophysiologic effects are not indicative of toxicity. Digoxin does not significantly reduce heart rate during exercise.
12.3 Pharmacokinetics
Note: The following data are from studies performed in adults, unless otherwise stated.
Comparisons of the systemic availability and equivalent doses for oral preparations of digoxin are shown in Table 4 [see Dosage and Administration (2.5)].
Distribution: Following drug administration, a 6-8 hour tissue distribution phase is observed. This is followed by a much more gradual decline in the serum concentration of the drug, which is dependent on the elimination of digoxin from the body. The peak height and slope of the early portion (absorption/distribution phases) of the serum concentration-time curve are dependent upon the route of administration and the absorption characteristics of the formulation. Clinical evidence indicates that the early high serum concentrations do not reflect the concentration of digoxin at its site of action, but that with chronic use, the steady-state post-distribution serum concentrations are in equilibrium with tissue concentrations and correlate with pharmacologic effects. In individual patients, these post-distribution serum concentrations may be useful in evaluating therapeutic and toxic effects [see Dosage and Administration (2.1)].
Digoxin is concentrated in tissues and therefore has a large apparent volume of distribution (approximately 475-500 L). Digoxin crosses both the blood-brain barrier and the placenta. At delivery, the serum digoxin concentration in the newborn is similar to the serum concentration in the mother. Approximately 25% of digoxin in the plasma is bound to protein. Serum digoxin concentrations are not significantly altered by large changes in fat tissue weight, so that its distribution space correlates best with lean (i.e., ideal) body weight, not total body weight.
Metabolism: Only a small percentage (13%) of a dose of digoxin is metabolized in healthy volunteers. The urinary metabolites, which include dihydrodigoxin, digoxigenin bisdigitoxoside, and their glucuronide and sulfate conjugates are polar in nature and are postulated to be formed via hydrolysis, oxidation, and conjugation. The metabolism of digoxin is not dependent upon the cytochrome P-450 system, and digoxin is not known to induce or inhibit the cytochrome P-450 system.
Excretion: Elimination of digoxin follows first-order kinetics (that is, the quantity of digoxin eliminated at any time is proportional to the total body content). Following intravenous administration to healthy volunteers, 50-70% of a digoxin dose is excreted unchanged in the urine. Renal excretion of digoxin is proportional to creatinine clearance and is largely independent of urine flow. In healthy volunteers with normal renal function, digoxin has a half-life of 1.5-2 days. The half-life in anuric patients is prolonged to 3.5-5 days. Digoxin is not effectively removed from the body by dialysis, exchange transfusion, or during cardiopulmonary bypass because most of the drug is bound to extravascular tissues.
Special Populations: Geriatrics: Because of age-related declines in renal function, elderly patients would be expected to eliminate digoxin more slowly than younger subjects. Elderly patients may also exhibit a lower volume of distribution of digoxin due to age-related loss of lean muscle mass. Thus, the dosage of digoxin should be carefully selected and monitored in elderly patients [see Use in Specific Populations (8.5)].
Gender: In a study of 184 patients, the clearance of digoxin was 12% lower in female than in male patients. This difference is not likely to be clinically important.
Hepatic Impairment: Because only a small percentage (approximately 13%) of a dose of digoxin undergoes metabolism, hepatic impairment would not be expected to significantly alter the pharmacokinetics of digoxin. In a small study, plasma digoxin concentration profiles in patients with acute hepatitis generally fell within the range of profiles in a group of healthy subjects. No dosage adjustments are recommended for patients with hepatic impairment; however, serum digoxin concentrations should be used, as appropriate, to help guide dosing in these patients.
Renal Impairment: Since the clearance of digoxin correlates with creatinine clearance, patients with renal impairment generally demonstrate prolonged digoxin elimination half-lives and greater exposures to digoxin. Therefore, titrate carefully in these patients based on clinical response and based on monitoring of serum digoxin concentrations, as appropriate.
Race: The impact of race differences on digoxin pharmacokinetics has not been formally studied. Because digoxin is primarily eliminated as unchanged drug via the kidney and because there are no important differences in creatinine clearance among races, pharmacokinetic differences due to race are not expected.
14 CLINICAL STUDIES
14.1 Chronic Heart Failure
Two 12-week, double-blind, placebo-controlled studies enrolled 178 (RADIANCE trial) and 88 (PROVED trial) adult patients with NYHA Class II or III heart failure previously treated with oral digoxin, a diuretic, and an ACE inhibitor (RADIANCE only) and randomized them to placebo or treatment with Digoxin Tablets. Both trials demonstrated better preservation of exercise capacity in patients randomized to digoxin. Continued treatment with digoxin reduced the risk of developing worsening heart failure, as evidenced by heart failure-related hospitalizations and emergency care and the need for concomitant heart failure therapy.
DIG Trial of Digoxin in Patients with Heart Failure
The Digitalis Investigation Group (DIG) main trial was a 37-week, multicenter, randomized, double-blind mortality study comparing digoxin to placebo in 6800 adult patients with heart failure and left ventricular ejection fraction less than or equal to 0.45. At randomization, 67% were NYHA class I or II, 71% had heart failure of ischemic etiology, 44% had been receiving digoxin, and most were receiving a concomitant ACE inhibitor (94%) and diuretics (82%). As in the smaller trials described above, patients who had been receiving open-label digoxin were withdrawn from this treatment before randomization. Randomization to digoxin was again associated with a significant reduction in the incidence of hospitalization, whether scored as number of hospitalizations for heart failure (relative risk 75%), risk of having at least one such hospitalization during the trial (RR 72%), or number of hospitalizations for any cause (RR 94%). On the other hand, randomization to digoxin had no apparent effect on mortality (RR 99%, with confidence limits of 91-107%).
14.2 Chronic Atrial Fibrillation
Digoxin has also been studied as a means of controlling the ventricular response to chronic atrial fibrillation in adults. Digoxin reduced the resting heart rate, but not the heart rate during exercise.
In 3 different randomized, double-blind trials that included a total of 315 adult patients, digoxin was compared to placebo for the conversion of recent-onset atrial fibrillation to sinus rhythm. Conversion was equally likely, and equally rapid, in the digoxin and placebo groups. In a randomized 120-patient trial comparing digoxin, sotalol, and amiodarone, patients randomized to digoxin had the lowest incidence of conversion to sinus rhythm, and the least satisfactory rate control when conversion did not occur.
In at least one study, digoxin was studied as a means of delaying reversion to atrial fibrillation in adult patients with frequent recurrence of this arrhythmia. This was a randomized, double-blind, 43-patient crossover study. Digoxin increased the mean time between symptomatic recurrent episodes by 54%, but had no effect on the frequency of fibrillatory episodes seen during continuous electrocardiographic monitoring.
16 HOW SUPPLIED/STORAGE AND HANDLING
Digoxin Injection, USP is available as:
500 mcg/2 mL (250 mcg/mL) ampuls packaged in 25s (NDC 0641-1410-35)
Store at 20˚ to 25˚C (68˚ to 77˚F), excursions permitted to 15˚ to 30˚C (59˚ to 86˚F) [see USP Controlled Room Temperature]. Protect from light.
17 PATIENT COUNSELING INFORMATION
- Advise patients that digoxin is used to treat heart failure and heart arrhythmias.
- Instruct patients to take this medication as directed.
- Advise patients that many drugs can interact with digoxin. Instruct patients to inform their doctor and pharmacist if they are taking any over the counter medications, including herbal medication, or are started on a new prescription.
- Advise patient that blood tests will be necessary to ensure that their digoxin dose is appropriate for them.
- Advise patients to contact their doctor or a health care professional if they experience nausea, vomiting, persistent diarrhea, confusion, weakness, or visual disturbances (including blurred vision, green-yellow color disturbances, halo effect) as these could be signs that the dose of digoxin may be too high.
- Advise parents or caregivers that the symptoms of having too high digoxin doses may be difficult to recognize in infants and pediatric patients. Symptoms such as weight loss, failure to thrive in infants, abdominal pain, and behavioral disturbances may be indications of digoxin toxicity.
- Instruct the patient to monitor and record their heart rate and blood pressure daily.
- Instruct women of childbearing potential who become or are planning to become pregnant to consult a physician prior to initiation or continuing therapy with digoxin.
Manufactured by:
HIKMA FARMACÊUTICA (PORTUGAL), S.A.
Estrada do Rio da Mό, 8, 8A e 8B – Fervença – 2705-906 Terrugem SNT, PORTUGAL
Distributed by:
Hikma Pharmaceuticals USA Inc.
Berkeley Heights, NJ 07922
Revised July 2020
462-636-05
PIN299-WES/6
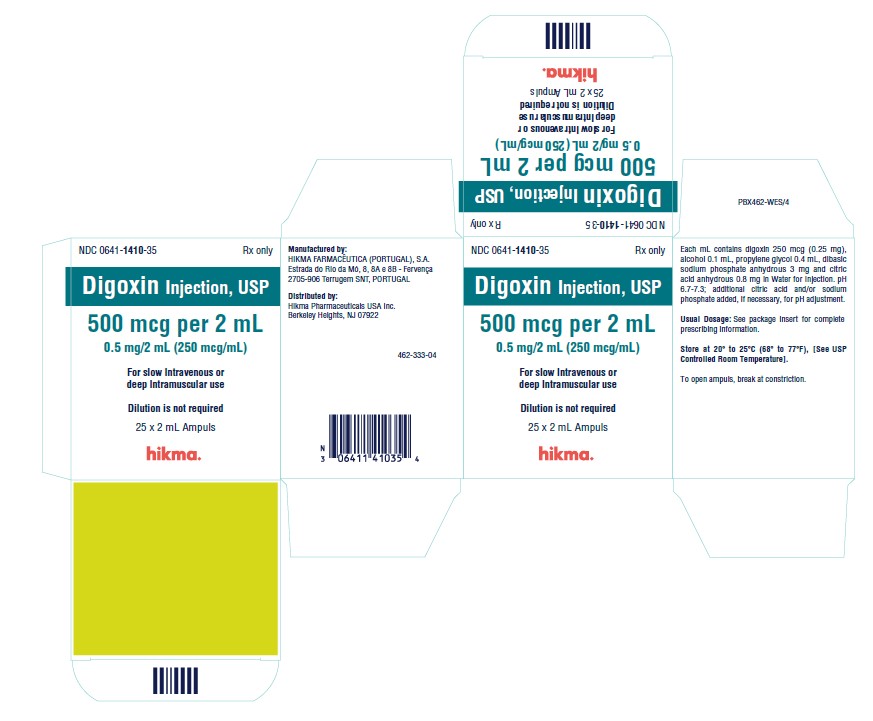
PRINCIPAL DISPLAY PANEL
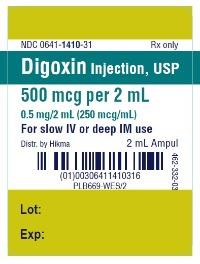
NDC 0641-1410-31 Rx only
Digoxin Injection, USP
500 mcg per 2 mL
0.5 mg/2 mL (250 mcg/mL)
For slow IV or deep IM use
2 mL Ampul
NDC 0641-1410-35 Rx only
Digoxin Injection, USP
500 mcg per 2 mL
0.5 mg/2 mL (250 mcg/mL)
For slow Intravenous or
deep Intramuscular use
Dilution is not required
25 x 2 mL Ampuls