METHYLDOPATE HYDROCHLORIDE- methyldopate hydrochloride injection, solution
American Regent, Inc.
----------
Methyldopate
HCl Injection, USP
DESCRIPTION
Methyldopate HCl Injection, USP, is an antihypertensive agent for intravenous use. Sterile, nonpyrogenic.
Methyldopate hydrochloride [levo-3-(3,4-dihydroxyphenyl)-2-methylalanine, ethyl ester hydrochloride] is the ethyl ester of methyldopa, supplied as the hydrochloride salt with a molecular weight of 275.73. Methyldopate hydrochloride is more soluble and stable in solution than methyldopa and is the preferred form for intravenous use.
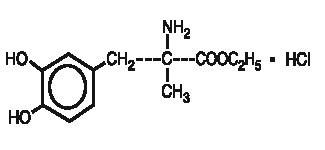
The molecular formula for Methyldopate hydrochloride is C12H17NO4·HCl and the structural formula is:
Each mL contains:
Methyldopate Hydrochloride ......... 50 mg
Citric Acid (Anhydrous) ................. 5 mg
Edetate Disodium ......................... 0.5 mg
Monothioglycerol ........................... 2 mg
Water for Injection ................q.s. to 1 mL
Methylparaben 1.5 mg and Propylparaben 0.2 mg added as preservatives, Sodium Bisulfite 3.2 mg added as an antioxidant. pH adjusted with Sodium Hydroxide and/or Hydrochloric Acid.
CLINICAL PHARMACOLOGY
Methyldopate, an antihypertensive agent, is an aromatic-amino-acid decarboxylase inhibitor in animals and in man. Although the mechanism of action has yet to be conclusively demonstrated, the antihypertensive effect of methyldopa probably is due to its metabolism to alpha-methyl-norepinephrine, which then lowers arterial pressure by stimulation of central inhibitory alpha-adrenergic receptors, false neurotransmission, and/or reduction of plasma renin activity. Methyldopa has been shown to cause a net reduction in the tissue concentration of serotonin, dopamine, norepinephrine, and epinephrine.
Only methyldopa, the L-isomer of alpha-methyldopa, has the ability to inhibit dopa decarboxylase and to deplete animal tissues of norepinephrine. In man, the antihypertensive activity appears to be due solely to the L-isomer. About twice the dose of the racemate (DL-alpha-methyldopa) is required for equal antihypertensive effect.
Methyldopa has no direct effect on cardiac function and usually does not reduce glomerular filtration rate, renal blood flow, or filtration fraction. Cardiac output usually is maintained without cardiac acceleration. In some patients the heart rate is slowed.
Normal or elevated plasma renin activity may decrease in the course of methyldopa therapy.
Methyldopa reduces both supine and standing blood pressure. It usually produces highly effective lowering of the supine pressure with infrequent symptomatic postural hypotension. Exercise hypotension and diurnal blood pressure variations rarely occur.
Pharmacokinetics and Metabolism
Methyldopate hydrochloride is the ethyl ester of methyldopa hydrochloride and possesses the same pharmacologic attributes.
Methyldopa is extensively metabolized. The known urinary metabolites are ∝-methyldopa mono-0-sulfate; 3-0-methyl-∝-methyldopa; 3,4-dihydroxyphenylacetone; ∝-methyldopamine; 3-0-methyl-∝-methyldopamine and their conjugates.
Following intravenous administration of methyldopate hydrochloride a decrease in blood pressure may occur in four to six hours and last 10 to 16 hours.
Approximately 49 percent of the dose of methyldopate hydrochloride is excreted in the urine as methyldopa and its mono-0-sulfate. The renal clearance of methyldopa following methyldopate hydrochloride is about 156 mL/min in normal subjects and is diminished in renal insufficiency. Following methyldopate hydrochloride injection the plasma half-life of methyldopa is 90-127 minutes. Approximately 17 percent of a dose of methyldopate hydrochloride given to normal subjects appears in plasma as free methyldopa.
Methyldopa crosses the placental barrier, appears in cord blood, and appears in breast milk.
INDICATIONS AND USAGE
Hypertension, when parenteral medication is indicated. The treatment of hypertensive crises may be initiated with Methyldopate HCl Injection.
CONTRAINDICATIONS
Methyldopate hydrochloride is contraindicated in patients:
- with active hepatic disease, such as acute hepatitis and active cirrhosis.
- with liver disorders previously associated with methyldopa therapy (see WARNINGS).
- with hypersensitivity to any component of this product, including sulfites (see WARNINGS).
- on therapy with monoamine oxidase (MAO) inhibitors.
WARNINGS
It is important to recognize that a positive Coombs test, hemolytic anemia, and liver disorders may occur with methyldopa therapy. The rare occurrences of hemolytic anemia or liver disorders could lead to potentially fatal complications unless properly recognized and managed. Read this section carefully to understand these reactions.
With prolonged methyldopa therapy, 10 to 20 percent of patients develop a positive direct Coombs test which usually occurs between 6 and 12 months of methyldopa therapy. Lowest incidence is at daily dosage of 1 gram or less. This on rare occasions may be associated with hemolytic anemia, which could lead to potentially fatal complications. One cannot predict which patients with a positive direct Coombs test may develop hemolytic anemia.
Prior existence or development of a positive direct Coombs test is not in itself a contraindication to use of methyldopa. If a positive Coombs test develops during methyldopa therapy, the physician should determine whether hemolytic anemia exists and whether the positive Coombs test may be a problem. For example, in addition to a positive direct Coombs test there is less often a positive indirect Coombs test which may interfere with cross matching of blood.
Before treatment is started, it is desirable to do a blood count (hematocrit, hemoglobin, or red cell count) for a baseline or to establish whether there is anemia. Periodic blood counts should be done during therapy to detect hemolytic anemia. It may be useful to do a direct Coombs test before therapy and at 6 and 12 months after the start of therapy.
If Coombs-positive hemolytic anemia occurs, the cause may be methyldopa and the drug should be discontinued. Usually the anemia remits promptly. If not, corticosteroids may be given and other causes of anemia should be considered. If the hemolytic anemia is related to methyldopa, the drug should not be reinstituted.
When methyldopa causes Coombs positivity alone or with hemolytic anemia, the red cell is usually coated with gamma globulin of the lgG (gamma G) class only. The positive Coombs test may not revert to normal until weeks to months after methyldopa is stopped.
Should the need for transfusion arise in a patient receiving methyldopa, both a direct and indirect Coombs test should be performed. In the absence of hemolytic anemia, usually only the direct Coombs test will be positive. A positive direct Coombs test alone will not interfere with typing or cross matching. If the indirect Coombs test is also positive, problems may arise in the major cross match and the assistance of a hematologist or transfusion expert will be needed.
Occasionally, fever has occurred within the first three weeks of methyldopa therapy, associated in some cases with eosinophilia or abnormalities in one or more liver function tests, such as serum alkaline phosphatase, serum transaminases (SGOT, SGPT), bilirubin and prothrombin time. Jaundice, with or without fever, may occur with onset usually within the first two to three months of therapy. In some patients the findings are consistent with those of cholestasis. In others the findings are consistent with hepatitis and hepatocellular injury.
Rarely fatal hepatic necrosis has been reported after use of methyldopa. These hepatic changes may represent hypersensitivity reactions. Periodic determination of hepatic function should be done particularly during the first 6 to 12 weeks of therapy or whenever an unexplained fever occurs. If fever, abnormalities in liver function tests, or jaundice appear, stop therapy with methyldopa. If caused by methyldopa, the temperature and abnormalities in liver function characteristically have reverted to normal when the drug was discontinued. Methyldopa should not be reinstituted in such patients.
Rarely, a reversible reduction of the white blood cell count with a primary effect on the granulocytes has been seen. The granulocyte count returned promptly to normal on discontinuance of the drug. Rare cases of granulocytopenia have been reported. In each instance, upon stopping the drug, the white cell count returned to normal. Reversible thrombocytopenia has occurred rarely.
Contains sodium bisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
PRECAUTIONS
General
Methyldopa should be used with caution in patients with a history of previous liver disease or dysfunction (see “WARNINGS”).
Some patients taking methyldopa experience clinical edema or weight gain which may be controlled by use of a diuretic. Methyldopa should not be continued if edema progresses or signs of heart failure appear.
A paradoxical pressor response has been reported with intravenous administration of Methyldopate HCl Injection.
Hypertension has recurred occasionally after dialysis in patients given methyldopa because the drug is removed by this procedure.
Rarely involuntary choreoathetotic movements have been observed during therapy with methyldopa in patients with severe bilateral cerebrovascular disease. Should these movements occur, stop therapy.
Laboratory Tests
Blood count, Coombs test, and liver function tests are recommended before initiating therapy and at periodic intervals (see “WARNINGS”).
Drug Interactions
When methyldopa is used with other antihypertensive drugs, potentiation of antihypertensive effect may occur. Patients should be followed carefully to detect side reactions or unusual manifestations of drug idiosyncrasy.
Patients may require reduced doses of anesthetics when on methyldopa. If hypotension does occur during anesthesia, it usually can be controlled by vasopressors. The adrenergic receptors remain sensitive during treatment with methyldopa.
When methyldopa and lithium are given concomitantly the patient should be carefully monitored for symptoms of lithium toxicity. Read the circular for lithium preparations.
Monoamine oxidase (MAO) inhibitors: See CONTRAINDICATIONS.
Drug/Laboratory Test Interactions
Methyldopa may interfere with measurement of: urinary uric acid by the phosphotungstate method, serum creatinine by the alkaline picrate method, and SGOT by colorimetric methods. Interference with spectrophotometric methods for SGOT analysis has not been reported.
Since methyldopa causes fluorescence in urine samples at the same wavelengths as catecholamines, falsely high levels of urinary catecholamines may be reported. This will interfere with the diagnosis of pheochromocytoma. It is important to recognize this phenomenon before a patient with a possible pheochromocytoma is subjected to surgery. Methyldopa does not interfere with measurement of VMA (vanillylmandelic acid), a test for pheochromocytoma, by those methods which convert VMA to vanillin. Methyldopa is not recommended for the treatment of patients with pheochromocytoma. Rarely, when urine is exposed to air after voiding, it may darken because of breakdown of methyldopa or its metabolites.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No evidence of a tumorigenic effect was seen when methyldopa was given for two years to mice at doses up to 1800 mg/kg/day or to rats at doses up to 240 mg/kg/day (30 and 4 times the maximum recommended human dose in mice and rats, respectively, when compared on the basis of body weight; 2.5 and 0.6 times the maximum recommended human dose in mice and rats, respectively, when compared on the basis of body surface area; calculations assume a patient weight of 50 kg).
Methyldopa was not mutagenic in the Ames Test and did not increase chromosomal aberration or sister chromatic exchanges in Chinese hamster ovary cells. These in vitro studies were carried out both with and without exogenous metabolic activation.
Fertility was unaffected when methyldopa was given to male and female rats at 100 mg/kg/day (1.7 times the maximum daily human dose when compared on the basis of body weight; 0.2 times the maximum daily human dose when compared on the basis of body surface area). Methyldopa decreased sperm count, sperm motility, the number of late spermatids and the male fertility index when given to male rats at 200 and 400 mg/kg/day (3.3 and 6.7 times the maximum daily human dose when compared on the basis of body weight; 0.5 and 1 times the maximum daily human dose when compared on the basis of body surface area).
Long-term studies in animals have not been performed to evaluate the carcinogenic potential of methyldopate hydrochloride; nor have evaluations of this ester's mutagenic potential or potential to affect fertility been carried out.
Pregnancy
Pregnancy Category C. Animal reproduction studies have not been conducted with Methyldopate HCl. It is also not known whether Methyldopate HCl can affect reproduction capacity or can cause fetal harm when given to a pregnant woman. Methyldopate HCl should be given to a pregnant woman only if clearly needed.
Nursing Mothers
Methyldopa appears in breast milk. Therefore, caution should be exercised when methyldopa is given to a nursing woman.
Pediatric Use
There are no well-controlled clinical trials in pediatric patients. Information on dosing in pediatric patients is supported by evidence from published literature regarding the treatment of hypertension in pediatric patients. (See DOSAGE AND ADMINISTRATION.)
ADVERSE REACTIONS
Sedation, usually transient, may occur during the initial period of therapy or whenever the dose is increased. Headache, asthenia, or weakness may be noted as early and transient symptoms. However, significant adverse effects due to methyldopa have been infrequent and this agent usually is well tolerated.
The following adverse reactions have been reported and, within each category, are listed in order of decreasing severity.
Cardiovascular: Aggravation of angina pectoris, congestive heart failure, prolonged carotid sinus hypersensitivity, paradoxical pressor response with intravenous use, orthostatic hypotension (decrease daily dosage), edema and weight gain, bradycardia.
Digestive: Pancreatitis, colitis, vomiting, diarrhea, sialadenitis, sore or ``black′′ tongue, nausea, constipation, distension, flatus, dryness of mouth.
Endocrine: Hyperprolactinemia.
Hematologic: Bone marrow depression, leukopenia, granulocytopenia, thrombocytopenia, hemolytic anemia; positive tests for antinuclear antibody, LE cells, and rheumatoid factor, positive Coombs tests.
Hepatic: Liver disorders including hepatitis, jaundice, abnormal liver function test (see “WARNINGS”).
Hypersensitivity: Myocarditis, pericarditis, vasculitis, lupus-like syndrome, drug-related fever, eosinophilia.
Nervous System/Psychiatric: Parkinsonism, Bell's palsy, decreased mental acuity, choreoathetotic movements, symptoms of cerebrovascular insufficiency, psychic disturbances including nightmares and reversible mild psychoses or depression, headache, sedation, asthenia or weakness, dizziness, lightheadedness, paresthesias.
Metabolic: Rise in BUN.
Musculoskeletal: Arthralgia, with or without joint swelling; myalgia.
Respiratory: Nasal stuffiness.
Skin: Toxic epidermal necrolysis, rash.
Urogenital: Amenorrhea, breast enlargement, gynecomastia, lactation, impotence, decreased libido.
OVERDOSAGE
Acute overdosage may produce acute hypotension with other responses attributable to brain and gastrointestinal malfunction (excessive sedation, weakness, bradycardia, dizziness, lightheadedness, constipation, distention, flatus, diarrhea, nausea, vomiting).
In the event of overdosage, symptomatic and supportive measures should be employed. Management includes special attention to cardiac rate and output, blood volume, electrolyte balance, paralytic ileus, urinary function and cerebral activity.
Sympathomimetic drugs [e.g., levarterenol, epinephrine, ARAMINE* (Metaraminol Bitartrate, MSD)] may be indicated.
The acute intravenous LD50 of Methyldopate HCl in the mouse is 321 mg/kg.
DOSAGE AND ADMINISTRATION
Methyldopate HCl Injection when given intravenously in effective doses, causes a decline in blood pressure that may begin in four to six hours and last 10 to 16 hours after injection.
Add the desired dose of Methyldopate HCl Injection to 100 mL of Dextrose Injection 5%, USP. Alternatively the desired dose may be given in 5% dextrose in water in a concentration of 100 mg/10 mL. Give this intravenous infusion slowly over a period of 30 to 60 minutes.
Adults: The usual adult dosage intravenously is 250 mg to 500 mg at six hour intervals as required. The maximum recommended intravenous dose is 1 gram every six hours.
When control has been obtained, oral therapy with tablets may be substituted for intravenous therapy, starting with the same dosage schedule used for the parenteral route. The effectiveness and anticipated responses are described in the circular for tablets.
Since methyldopate has a relatively short duration of action, withdrawal is followed by return of hypertension usually within 48 hours. This is not complicated by an overshoot of blood pressure.
Occasionally tolerance may occur, usually between the second and third month of therapy. Adding a diuretic or increasing the dosage of methyldopa frequently will restore effective control of blood pressure. A thiazide may be added at any time during methyldopa therapy and is recommended if therapy has not been started with a thiazide or if effective control of blood pressure cannot be maintained on 2 grams of methyldopa daily.
Methyldopa is largely excreted by the kidney and patients with impaired renal function may respond to smaller doses. Syncope in older patients may be related to an increased sensitivity and advanced arteriosclerotic vascular disease. This may be avoided by lower doses.
Pediatric Patients: The recommended daily dosage is 20 to 40 mg/kg of body weight in divided doses every six hours. The maximum dosage is 65 mg/kg or 3 grams daily, whichever is less. When the blood pressure is under control, continue with oral therapy using tablets in the same dosage as for the parenteral route. (see PRECAUTIONS, Pediatric Use.)
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
HOW SUPPLIED
Methyldopate HCl Injection, USP 250 mg/5 mL (50 mg/mL).
NDC 0517-8905-10 5 mL Single Dose Vial Boxes of 10
Store at 20°-25°C (68°-77°F); excursions permitted to 15°-30°C (59°-86°F) (See USP Controlled Room Temperature).
Rx Only
IN8905
Rev. 11/05
MG #7604
AMERICAN
REGENT, INC.
SHIRLEY, NY 11967
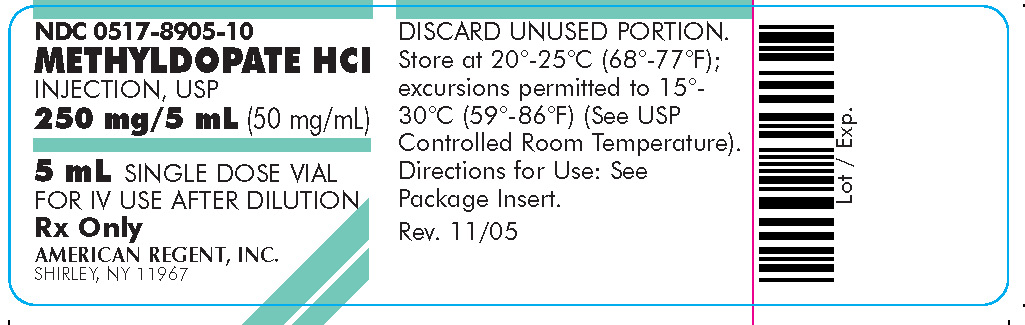
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - Container
NDC 0517-8905-10
METHYLDOPATE HCl
INJECTION, USP
250 mg/5 mL (50 mg/mL)
5 mL SINGLE DOSE VIAL
FOR IV USE AFTER DILUTION
Rx Only
AMERICAN REGENT, INC.
SHIRLEY, NY 11967
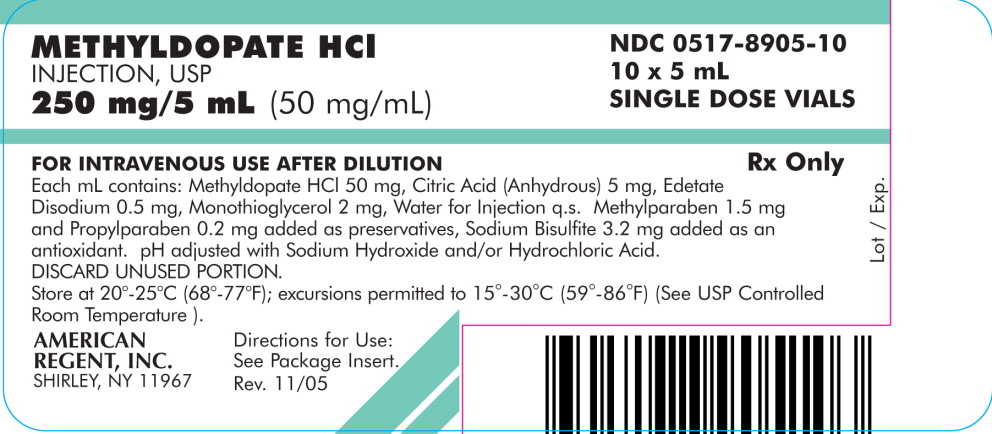
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL - Carton
PRINCIPAL DISPLAY PANEL – Carton
METHYLDOPATE HCl
INJECTION, USP
250 mg/5 mL (50 mg/mL)
NDC 0517-8905-10
10 x 5 mL
SINGLE DOSE VIALS
FOR INTRAVENOUS USE AFTER DILUTION
Rx Only
Each mL contains: Methyldopate HCl 50 mg, Citric Acid (Anhydrous) 5 mg, Edetate Disodium 0.5 mg, Monothioglycerol 2 mg, Water for Injection q.s. Methylparaben 1.5 mg and Propylparaben 0.2 mg added as preservatives, Sodium Bisulfite 3.2 mg added as an antioxidant. pH adjusted with Sodium Hydroxide and/or Hydrochloric Acid.
DISCARD UNUSED PORTION.
Store at 20°-25°C (68°-77°F); excursions permitted to 15°-30°C (59°-86°F) (See USP Controlled Room Temperature).
Directions for Use: See Package Insert.
AMERICAN
REGENT, INC.
SHIRLEY, NY 11967
Rev. 11/05
| METHYLDOPATE HYDROCHLORIDE
methyldopate hydrochloride injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - American Regent, Inc. (622781813) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Luitpold Pharmaceuticals, Inc. | 002033710 | ANALYSIS(0517-8905, 0517-8905) , MANUFACTURE(0517-8905, 0517-8905) , STERILIZE(0517-8905, 0517-8905) | |