MENACTRA- neisseria meningitidis group a capsular polysaccharide diphtheria toxoid conjugate antigen, neisseria meningitidis group y capsular polysaccharide diphtheria toxoid conjugate antigen, neisseria meningitidis group c capsular polysaccharide diphtheria toxoid conjugate antigen and neisseria meningitidis group w-135 capsular polysaccharide diphtheria toxoid conjugate antigen injection, solution
REMEDYREPACK INC.
----------
These highlights do not include all the information needed to use Menactra® safely and effectively. See full prescribing information for Menactra vaccine. Menactra®, Meningococcal (Groups A, C, Y and W-135) Polysaccharide Diphtheria Toxoid Conjugate Vaccine Solution for Intramuscular Injection Initial U.S. Approval: 2005
INDICATIONS & USAGE
Menactra ®, Meningococcal (Groups A, C, Y and W-135) Polysaccharide Diphtheria Toxoid Conjugate Vaccine, is indicated for active immunization to prevent invasive meningococcal disease caused by N meningitidis serogroups A, C, Y and W-135. Menactra vaccine is approved for use in individuals 9 months through 55 years of age. Menactra vaccine does not prevent N meningitidis serogroup B disease.
DOSAGE & ADMINISTRATION
A 0.5 mL dose for intramuscular injection. ( 2)
Primary Vaccination:
- Children 9 through 23 months of age: Two doses, three months apart.
- Individuals 2 through 55 years of age: A single dose.
Booster Vaccination:
- A single booster dose may be given to individuals 15 through 55 years of age at continued risk for meningococcal disease, if at least 4 years have elapsed since the prior dose.
Menactra vaccine is a clear to slightly turbid solution. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. If any of these conditions exist, the vaccine should not be administered.
Withdraw the 0.5 mL dose of vaccine from the single-dose vial using a sterile needle and syringe.
Menactra vaccine is administered as a 0.5 mL dose by intramuscular injection. Do not administer this product intravenously or subcutaneously.
Primary Vaccination:
- In children 9 through 23 months of age, Menactra vaccine is given as a 2-dose series three months apart.
- Individuals 2 through 55 years of age, Menactra vaccine is given as a single dose.
Booster Vaccination:
- A single booster dose may be given to individuals 15 through 55 years of age at continued risk for meningococcal disease, if at least 4 years have elapsed since the prior dose.
DOSAGE FORMS & STRENGTHS
Menactra vaccine is a solution supplied in 0.5 mL single-dose vials. [See Description (11) for a complete listing of ingredients.]
CONTRAINDICATIONS
Severe allergic reaction (eg, anaphylaxis) after a previous dose of a meningococcal capsular polysaccharide-, diphtheria toxoid- or CRM 197-containing vaccine, or to any component of Menactra vaccine [see Description (11)].
WARNINGS AND PRECAUTIONS
- Persons previously diagnosed with Guillain-Barré syndrome (GBS) may be at increased risk of GBS following receipt of Menactra vaccine. The decision to give Menactra vaccine should take into account the potential benefits and risks. ( 5.1)
Persons previously diagnosed with Guillain-Barré syndrome (GBS) may be at increased risk of GBS following receipt of Menactra vaccine. The decision to give Menactra vaccine should take into account the potential benefits and risks.
GBS has been reported in temporal relationship following administration of Menactra vaccine. (1) (2) The risk of GBS following Menactra vaccination was evaluated in a post-marketing retrospective cohort study [ Post-Marketing Experience (6.2)].
Prior to administration, the healthcare provider should review the immunization history for possible vaccine sensitivity and previous vaccination-related adverse reactions to allow an assessment of benefits and risks. Epinephrine and other appropriate agents used for the control of immediate allergic reactions must be immediately available should an acute anaphylactic reaction occur.
Immunocompromised persons, including individuals receiving immunosuppressant therapy, may have a diminished immune response to Menactra vaccine.
Menactra vaccine may not protect all recipients.
Syncope (fainting) has been reported following vaccination with Menactra vaccine. Procedures should be in place to prevent falling injury and manage syncopal reactions.
ADVERSE REACTIONS
- Common (≥10%) solicited adverse events in infants and toddlers 9 and 12 months of age were injection site tenderness, erythema, and swelling; irritability, abnormal crying, drowsiness, appetite loss, vomiting, and fever. ( 6)
- Common (≥10%) solicited adverse events in individuals 2 through 55 years of age who received a single dose were injection site pain, redness, induration, and swelling; anorexia and diarrhea. Other common solicited adverse events were irritability and drowsiness (2-10 years of age), headache, fatigue, malaise, and arthralgia (11-55 years of age). ( 6)
To report SUSPECTED ADVERSE REACTIONS, contact Sanofi Pasteur Inc. at 1-800-822-2463 (1-800-VACCINE) or VAERS at 1-800-822-7967 or http://vaers.hhs.gov.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice.
Children 9 Through 12 Months of Age
The safety of Menactra vaccine was evaluated in four clinical studies that enrolled 3721 participants who received Menactra vaccine at 9 and 12 months of age. At 12 months of age these children also received one or more other recommended vaccines [Measles, Mumps, Rubella and Varicella Virus Vaccine Live (MMRV) or Measles, Mumps, and Rubella Virus Vaccine (MMR) and Varicella Virus Vaccine Live (V) each manufactured by Merck & Co., Inc., Pneumococcal 7-valent Conjugate Vaccine (Diphtheria CRM 197 Protein) manufactured by Wyeth Pharmaceuticals Inc. (PCV7), Hepatitis A Vaccine manufactured by Merck & Co., Inc. (HepA). A control group of 997 children was enrolled at 12 months of age and received two or more childhood vaccines [MMRV (or MMR+V), PCV7, HepA] at 12 months of age [see Concomitant Vaccine Administration (14.3)]. Three percent of individuals received MMR and V, instead of MMRV, at 12 months of age.
The primary safety study was a controlled trial that enrolled 1256 children who received Menactra vaccine at 9 and 12 months of age. At 12 months of age these children received MMRV (or MMR+V), PCV7 and HepA. A control group of 522 children received MMRV, PCV7 and HepA. Of the 1778 children, 78% of participants (Menactra vaccine, N=1056; control group, N=322) were enrolled at United States (US) sites and 22% at a Chilean site. (Menactra vaccine, N=200; control group, N=200).
Individuals 2 Through 55 Years of Age
The safety of Menactra vaccine was evaluated in eight clinical studies that enrolled 10,057 participants aged 2-55 years who received Menactra vaccine and 5,266 participants who received Menomune ® – A/C/Y/W-135, Meningococcal Polysaccharide Vaccine, Groups A, C, Y and W-135 Combined. There were no substantive differences in demographic characteristics between the vaccine groups. Among Menactra vaccine recipients 2-55 years of age 24.0%, 16.2%, 40.4% and 19.4% were in the 2-10, 11-14, 15-25 and 26-55-year age groups, respectively. Among Menomune – A/C/Y/W-135 vaccine recipients 2-55 years of age 42.3%, 9.3%, 30.0% and 18.5% were in the 2-10, 11-14, 15-25 and 26-55-year age groups, respectively. The three primary safety studies were randomized, active-controlled trials that enrolled participants 2-10 years of age (Menactra vaccine, N=1713; Menomune – A/C/Y/W-135 vaccine, N=1519), 11-18 years of age (Menactra vaccine, N=2270; Menomune – A/C/Y/W-135 vaccine, N=972) and 18-55 years of age (Menactra vaccine, N=1384; Menomune – A/C/Y/W-135 vaccine, N=1170), respectively. Of the 3232 children 2-10 years of age, 68% of participants (Menactra vaccine, N=1164; Menomune – A/C/Y/W-135 vaccine, N=1031) were enrolled at US sites and 32% (Menactra vaccine, N=549; Menomune – A/C/Y/W-135 vaccine, N=488) of participants at a Chilean site. The median ages in the Chilean and US subpopulations were 5 and 6 years, respectively. All adolescents and adults were enrolled at US sites. As the route of administration differed for the two vaccines (Menactra vaccine given intramuscularly, Menomune – A/C/Y/W-135 vaccine given subcutaneously), study personnel collecting the safety data differed from personnel administering the vaccine.
Booster Vaccination Study
In an open-label trial conducted in the US, 834 individuals were enrolled to receive a single dose of Menactra vaccine 4-6 years after a prior dose. The median age of participants was 17.1 years at the time of the booster dose.
Safety Evaluation
Participants were monitored after each vaccination for 20 or 30 minutes for immediate reactions, depending on the study. Solicited injection site and systemic reactions were recorded in a diary card for 7 consecutive days after each vaccination. Participants were monitored for 28 days (30 days for infants and toddlers) for unsolicited adverse events and for 6 months post-vaccination for visits to an emergency room, unexpected visits to an office physician, and serious adverse events. Unsolicited adverse event information was obtained either by telephone interview or at an interim clinic visit. Information regarding adverse events that occurred in the 6-month post-vaccination time period was obtained via a scripted telephone interview.
Serious Adverse Events in All Safety Studies
Serious adverse events (SAEs) were reported during a 6-month time period following vaccinations in individuals 9 months through 55 years of age. In children who received Menactra vaccine at 9 months and at 12 months of age, SAEs occurred at a rate of 2.0% - 2.5%. In participants who received one or more childhood vaccine(s) (without co-administration of Menactra vaccine) at 12 months of age, SAEs occurred at a rate of 1.6% - 3.6%, depending on the number and type of vaccines received. In children 2-10 years of age, SAEs occurred at a rate of 0.6% following Menactra vaccine and at a rate of 0.7% following Menomune – A/C/Y/W-135 vaccine. In adolescents 11 through 18 years of age and adults 18 years through 55 years of age, SAEs occurred at a rate of 1.0% following Menactra vaccine and at a rate of 1.3% following Menomune – A/C/Y/W-135 vaccine. In adolescents and adults, SAEs occurred at a rate of 1.3% following booster vaccination with Menactra vaccine.
Solicited Adverse Events in the Primary Safety Studies
The most frequently reported solicited injection site and systemic adverse reactions within 7 days following vaccination in children 9 months and 12 months of age (Table 1) were injection site tenderness and irritability.
The most frequently reported solicited injection site and systemic adverse reactions in US children aged 2-10 years of age (Table 2) were injection site pain and irritability. Diarrhea, drowsiness, and anorexia were also common.
The most commonly reported solicited injection site and systemic adverse reactions in adolescents, ages 11-18 years (Table 3), and adults, ages 18-55 years (Table 4), after a single dose were injection site pain, headache and fatigue. Except for redness in adults, injection site reactions were more frequently reported after Menactra vaccination than after Menomune – A/C/Y/W-135 vaccination.
| Menactra vaccine at 9 months of age | Menactra + PCV7 *+ MMRV † + HepA ‡ vaccines at 12 months of age | PCV7 1+ MMRV 2+ HepA 3 vaccines at 12 months of age | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N §=998 - 1002 | N 4=898 - 908 | N 4=302 - 307 | |||||||
| Reaction | Any | Grade 2 | Grade 3 | Any | Grade 2 | Grade 3 | Any | Grade 2 | Grade 3 |
| Local/Injection Site | |||||||||
| Tenderness ¶ | |||||||||
| Menactra Site | 37.4 | 4.3 | 0.6 | 48.5 | 7.5 | 1.3 | - | - | - |
| PCV7 Site | - | - | - | 45.6 | 9.4 | 1.6 | 45.7 | 8.3 | 0.3 |
| MMRV Site | - | - | - | 38.9 | 7.1 | 1.0 | 43.0 | 5.2 | 0.0 |
| HepA Site | - | - | - | 43.4 | 8.7 | 1.4 | 40.9 | 4.6 | 0.3 |
| Erythema # | |||||||||
| Menactra Site | 30.2 | 2.5 | 0.3 | 30.1 | 1.3 | 0.1 | - | - | - |
| PCV7 Site | - | - | - | 29.4 | 2.6 | 0.2 | 32.6 | 3.0 | 0.7 |
| MMRV Site | - | - | - | 22.5 | 0.9 | 0.3 | 33.2 | 5.9 | 0.0 |
| HepA Site | - | - | - | 25.1 | 1.1 | 0.0 | 26.6 | 0.7 | 0.0 |
| Swelling 6 | |||||||||
| Menactra Site | 16.8 | 0.9 | 0.2 | 16.2 | 0.9 | 0.1 | - | - | - |
| PCV7 Site | - | - | - | 19.5 | 1.3 | 0.4 | 16.6 | 1.3 | 0.7 |
| MMRV Site | - | - | - | 12.1 | 0.4 | 0.1 | 14.1 | 0.3 | 0.0 |
| HepA Site | - | - | - | 16.4 | 0.7 | 0.2 | 13.5 | 0.0 | 0.3 |
| Systemic | |||||||||
| Irritability Þ | 56.8 | 23.1 | 2.9 | 62.1 | 25.7 | 3.7 | 64.8 | 28.7 | 4.2 |
| Abnormal crying ß | 33.3 | 8.3 | 2.0 | 40.0 | 11.5 | 2.4 | 39.4 | 10.1 | 0.7 |
| Drowsiness à | 30.2 | 3.5 | 0.7 | 39.8 | 5.3 | 1.1 | 39.1 | 5.2 | 0.7 |
| Appetite loss è | 30.2 | 7.1 | 1.2 | 35.7 | 7.6 | 2.6 | 31.9 | 6.5 | 0.7 |
| Vomiting ð | 14.1 | 4.6 | 0.3 | 11.0 | 4.4 | 0.2 | 9.8 | 2.0 | 0.0 |
| Fever ø | 12.2 | 4.5 | 1.1 | 24.5 | 11.9 | 2.2 | 21.8 | 7.3 | 2.6 |
| Menactra vaccine | Menomune – A/C/Y/W-135 vaccine | |||||
|---|---|---|---|---|---|---|
| N *=1156 - 1157 | N 13=1027 | |||||
| Reaction | Any | Grade 2 | Grade 3 | Any | Grade 2 | Grade 3 |
| Local/Injection Site | ||||||
| Pain † | 45.0 | 4.9 | 0.3 | 26.1 | 2.5 | 0.0 |
| Redness ‡ | 21.8 | 4.6 | 3.9 | 7.9 | 0.5 | 0.0 |
| Induration 15 | 18.9 | 3.4 | 1.4 | 4.2 | 0.6 | 0.0 |
| Swelling 15 | 17.4 | 3.9 | 1.9 | 2.8 | 0.3 | 0.0 |
| Systemic | ||||||
| Irritability § | 12.4 | 3.0 | 0.3 | 12.2 | 2.6 | 0.6 |
| Diarrhea ¶ | 11.1 | 2.1 | 0.2 | 11.8 | 2.5 | 0.3 |
| Drowsiness # | 10.8 | 2.7 | 0.3 | 11.2 | 2.5 | 0.5 |
| Anorexia Þ | 8.2 | 1.7 | 0.4 | 8.7 | 1.3 | 0.8 |
| Arthralgia ß | 6.8 | 0.5 | 0.2 | 5.3 | 0.7 | 0.0 |
| Fever à | 5.2 | 1.7 | 0.3 | 5.2 | 1.7 | 0.2 |
| Rash è | 3.4 | - | - | 3.0 | - | - |
| Vomiting ð | 3.0 | 0.7 | 0.3 | 2.7 | 0.7 | 0.6 |
| Seizure 22 | 0.0 | - | - | 0.0 | - | - |
| Menactra vaccine | Menomune – A/C/Y/W-135 vaccine | |||||
|---|---|---|---|---|---|---|
| N *=2264 - 2265 | N 24=970 | |||||
| Reaction | Any | Grade 2 | Grade 3 | Any | Grade 2 | Grade 3 |
| Local/Injection Site | ||||||
| Pain † | 59.2 ‡ | 12.8 26 | 0.3 | 28.7 | 2.6 | 0.0 |
| Induration § | 15.7 26 | 2.5 26 | 0.3 | 5.2 | 0.5 | 0.0 |
| Redness 27 | 10.9 26 | 1.6 26 | 0.6 26 | 5.7 | 0.4 | 0.0 |
| Swelling 27 | 10.8 26 | 1.9 26 | 0.5 26 | 3.6 | 0.3 | 0.0 |
| Systemic | ||||||
| Headache ¶ | 35.6 26 | 9.6 26 | 1.1 | 29.3 | 6.5 | 0.4 |
| Fatigue 28 | 30.0 26 | 7.5 | 1.1 26 | 25.1 | 6.2 | 0.2 |
| Malaise 28 | 21.9 26 | 5.8 26 | 1.1 | 16.8 | 3.4 | 0.4 |
| Arthralgia 28 | 17.4 26 | 3.6 26 | 0.4 | 10.2 | 2.1 | 0.1 |
| Diarrhea # | 12.0 | 1.6 | 0.3 | 10.2 | 1.3 | 0.0 |
| Anorexia Þ | 10.7 26 | 2.0 | 0.3 | 7.7 | 1.1 | 0.2 |
| Chills 28 | 7.0 26 | 1.7 26 | 0.2 | 3.5 | 0.4 | 0.1 |
| Fever ß | 5.1 26 | 0.6 | 0.0 | 3.0 | 0.3 | 0.1 |
| Vomiting à | 1.9 | 0.4 | 0.3 | 1.4 | 0.5 | 0.3 |
| Rash è | 1.6 | - | - | 1.4 | - | - |
| Seizure 33 | 0.0 | - | - | 0.0 | - | - |
| Menactra vaccine | Menomune – A/C/Y/W-135 vaccine | |||||
|---|---|---|---|---|---|---|
| N *=1371 | N 34=1159 | |||||
| Reaction | Any | Grade 2 | Grade 3 | Any | Grade 2 | Grade 3 |
| Local/Injection Site | ||||||
| Pain † | 53.9 ‡ | 11.3 36 | 0.2 | 48.1 | 3.3 | 0.1 |
| Induration § | 17.1 36 | 3.4 36 | 0.7 36 | 11.0 | 1.0 | 0.0 |
| Redness 37 | 14.4 | 2.9 | 1.1 36 | 16.0 | 1.9 | 0.1 |
| Swelling 37 | 12.6 36 | 2.3 36 | 0.9 36 | 7.6 | 0.7 | 0.0 |
| Systemic | ||||||
| Headache ¶ | 41.4 | 10.1 | 1.2 | 41.8 | 8.9 | 0.9 |
| Fatigue 38 | 34.7 | 8.3 | 0.9 | 32.3 | 6.6 | 0.4 |
| Malaise 38 | 23.6 | 6.6 36 | 1.1 | 22.3 | 4.7 | 0.9 |
| Arthralgia 38 | 19.8 36 | 4.7 36 | 0.3 | 16.0 | 2.6 | 0.1 |
| Diarrhea # | 16.0 | 2.6 | 0.4 | 14.0 | 2.9 | 0.3 |
| Anorexia Þ | 11.8 | 2.3 | 0.4 | 9.9 | 1.6 | 0.4 |
| Chills 38 | 9.7 36 | 2.1 36 | 0.6 36 | 5.6 | 1.0 | 0.0 |
| Vomiting ß | 2.3 | 0.4 | 0.2 | 1.5 | 0.2 | 0.4 |
| Fever à | 1.5 36 | 0.3 | 0.0 | 0.5 | 0.1 | 0.0 |
| Rash è | 1.4 | - | - | 0.8 | - | - |
| Seizure 43 | 0.0 | - | - | 0.0 | - | - |
Solicited Adverse Events in a Booster Vaccination Study
[For a description of the study design and number of participants, see Clinical Trials Experience, Booster Vaccination Study (6.1)] The most common solicited injection site and systemic reactions within 7 days of vaccination were pain (60.2%) and myalgia (42.8%), respectively. Overall rates of solicited injection site reactions and solicited systemic reactions were similar to those observed in adolescents and adults after a single Menactra dose. The majority of solicited reactions were Grade 1 or 2 and resolved within 3 days.
Adverse Events in Concomitant Vaccine Studies
Solicited Injection Site and Systemic Reactions when Given with Routine Pediatric Vaccines
For a description of the study design and number of participants [see Clinical Trials Experience (6.1), Concomitant Vaccine Administration (14.3)]. In the primary safety study, 1378 US children were enrolled to receive Menactra vaccine alone at 9 months of age and Menactra vaccine plus one or more other routinely administered vaccines (MMRV, PCV7 and HepA) at 12 months of age (N=961). Another group of children received two or more routinely administered vaccines (MMRV, PCV7 and HepA) (control group, n=321) at 12 months of age. The frequency of occurrence of solicited adverse events is presented in Table 1. Participants who received Menactra vaccine and the concomitant vaccines at 12 months of age described above reported similar frequencies of tenderness, redness and swelling at the Menactra vaccine injection site and at the concomitant vaccine injection sites. Tenderness was the most frequent injection site reaction (48%, 39%, 46% and 43% at the Menactra vaccine, MMRV, PCV7 and HepA sites, respectively). Irritability was the most frequent systemic reaction, reported in 62% of recipients of Menactra vaccine plus concomitant vaccines, and 65% of the control group. [See Concomitant Vaccine Administration (14.3)].
Solicited Injection site and Systemic Reactions when Given with Tetanus and Diphtheria Toxoid Adsorbed Vaccine
In a clinical study, rates of local and systemic reactions after Menactra vaccine and Tetanus and Diphtheria Toxoid Adsorbed (Td) vaccine manufactured by Sanofi Pasteur Inc. were compared [see Drug Interactions (7), and Concomitant Vaccine Administration (14.3) for study description]. Injection site pain was reported more frequently after Td vaccination than after Menactra vaccination (71% versus 53%). The overall rate of systemic adverse events was higher when Menactra and Td vaccines were given concomitantly than when Menactra vaccine was administered 28 days after Td (59% versus 36%). In both groups, the most common reactions were headache (Menactra vaccine + Td, 36%; Td + Placebo, 34%; Menactra vaccine alone, 22%) and fatigue (Menactra vaccine + Td, 32%; Td + Placebo, 29%; Menactra vaccine alone, 17%). Fever ≥40.0ºC occurred at ≤0.5% in all groups.
Solicited Injection site and Systemic Reactions when Given with Typhoid Vi Polysaccharide Vaccine
In a clinical study, rates of local and systemic reactions after Menactra vaccine and Typhoid Vi Polysaccharide Vaccine, produced by Sanofi Pasteur SA were compared [see Drug Interactions (7) and Concomitant Vaccine Administration (14.3)] for a description of the concomitantly administered vaccine, study design and number of participants. More participants experienced pain after Typhoid vaccination than after Menactra vaccination (Typhoid + Placebo, 76% versus Menactra vaccine + Typhoid, 47%). The majority (70%-77%) of injection site solicited reactions for both groups at either injection site were reported as Grade 1 and resolved within 3 days post-vaccination. In both groups, the most common systemic reaction was headache (Menactra vaccine + Typhoid, 41%; Typhoid + Placebo, 42%; Menactra vaccine alone, 33%) and fatigue (Menactra vaccine + Typhoid, 38%; Typhoid + Placebo, 35%; Menactra vaccine alone, 27%). Fever ≥40.0ºC and seizures were not reported in either group.
In addition to reports in clinical trials, worldwide voluntary adverse events reports received since market introduction of Menactra vaccine are listed below. This list includes serious events and/or events which were included based on severity, frequency of reporting or a plausible causal connection to Menactra vaccine. Because these events were reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to vaccination.
-
Immune System Disorders
Hypersensitivity reactions such as anaphylaxis/anaphylactic reaction, wheezing, difficulty breathing, upper airway swelling, urticaria, erythema, pruritus, hypotension -
Nervous System Disorders
Guillain-Barré syndrome, paraesthesia, vasovagal syncope, dizziness, convulsion, facial palsy, acute disseminated encephalomyelitis, transverse myelitis -
Musculoskeletal and Connective Tissue Disorders
Myalgia
Post-marketing Safety Study
The risk of GBS following receipt of Menactra vaccine was evaluated in a US retrospective cohort study using healthcare claims data from 9,578,688 individuals 11 through 18 years of age, of whom 1,431,906 (15%) received Menactra vaccine. Of 72 medical chart-confirmed GBS cases, none had received Menactra vaccine within 42 days prior to symptom onset. An additional 129 potential cases of GBS could not be confirmed or excluded due to absent or insufficient medical chart information. In an analysis that took into account the missing data, estimates of the attributable risk of GBS ranged from 0 to 5 additional cases of GBS per 1,000,000 vaccinees within the 6-week period following vaccination.
- 1
- PCV7 (Prevnar
- 2
- MMRV (ProQuad
- 3
- HepA (VAQTA
- 4
- N = The number of subjects with available data.
- 5
- Grade 2: cries and protests when injection site is touched, Grade 3: cries when injected limb is moved, or the movement of the injected limb is reduced.
- 6
- Grade 2: ≥1.0 inches to <2.0 inches, Grade 3: ≥2.0 inches.
- 7
- Grade 2: requires increased attention, Grade 3: inconsolable.
- 8
- Grade 2: 1 to 3 hours, Grade 3: >3 hours.
- 9
- Grade 2: not interested in surroundings or did not wake up for a feed/meal, Grade 3: sleeping most of the time or difficult to wake up.
- 10
- Grade 2: missed 1 or 2 feeds/meals completely, Grade 3: refuses ≥3 feeds/meals or refuses most feeds/meals.
- 11
- Grade 2: 2 to 5 episodes per 24 hours, Grade 3: ≥6 episodes per 24 hours or requiring parenteral hydration.
- 12
- Grade 2: >38.5°C to ≤39.5°C, Grade 3: >39.5°C.
- 13
- N = The total number of subjects reporting at least one solicited reaction. The median age of participants was 6 years in both vaccine groups.
- 14
- Grade 2: interferes with normal activities, Grade 3: disabling, unwilling to move arm.
- 15
- Grade 2: 1.0-2.0 inches, Grade 3: >2.0 inches.
- 16
- Grade 2: 1-3 hours duration, Grade 3: >3 hours duration.
- 17
- Grade 2: 3-4 episodes, Grade 3: ≥5 episodes.
- 18
- Grade 2: interferes with normal activities, Grade 3: disabling, unwilling to engage in play or interact with others.
- 19
- Grade 2: skipped 2 meals, Grade 3: skipped ≥3 meals.
- 20
- Grade 2: decreased range of motion due to pain or discomfort, Grade 3: unable to move major joints due to pain.
- 21
- Oral equivalent temperature; Grade 2: 38.4°C to 39.4ºC, Grade 3: ≥39.5ºC.
- 22
- These solicited adverse events were reported as present or absent only.
- 23
- Grade 2: 2 episodes, Grade 3: ≥3 episodes.
- 24
- N = The number of subjects with available data.
- 25
- Grade 2: interferes with or limits usual arm movement, Grade 3: disabling, unable to move arm.
- 26
- Denotes
- 27
- Grade 2: 1.0-2.0 inches, Grade 3: >2.0 inches.
- 28
- Grade 2: interferes with normal activities, Grade 3: requiring bed rest.
- 29
- Grade 2: 3-4 episodes, Grade 3: ≥5 episodes.
- 30
- Grade 2: skipped 2 meals, Grade 3: skipped ≥3 meals.
- 31
- Oral equivalent temperature; Grade 2: 38.5°C to 39.4ºC, Grade 3: ≥39.5ºC.
- 32
- Grade 2: 2 episodes, Grade 3: ≥3 episodes.
- 33
- These solicited adverse events were reported as present or absent only.
- 34
- N = The number of subjects with available data.
- 35
- Grade 2: interferes with or limits usual arm movement, Grade 3: disabling, unable to move arm.
- 36
- Denotes
- 37
- Grade 2: 1.0-2.0 inches, Grade 3: >2.0 inches.
- 38
- Grade 2: interferes with normal activities, Grade 3: requiring bed rest.
- 39
- Grade 2: 3-4 episodes, Grade 3: ≥5 episodes.
- 40
- Grade 2: skipped 2 meals, Grade 3: skipped ≥3 meals.
- 41
- Grade 2: 2 episodes, Grade 3: ≥3 episodes.
- 42
- Oral equivalent temperature; Grade 2: 39.0°C to 39.9ºC, Grade 3: ≥40.0ºC.
- 43
- These solicited adverse events were reported as present or absent only.
DRUG INTERACTIONS
- Pneumococcal antibody responses to some serotypes in Prevnar (PCV7) were decreased following co-administration of Menactra vaccine and PCV7. ( 7.1)
Menactra vaccine was concomitantly administered with Typhim Vi ® [Typhoid Vi Polysaccharide Vaccine] (Typhoid) and Tetanus and Diphtheria Toxoids Adsorbed, For Adult Use (Td), in individuals 18 through 55 and 11 through 17 years of age, respectively. In children younger than 2 years of age, Menactra was co-administered with one or more of the following vaccines: PCV7, MMR, V, MMRV, or HepA [see Clinical Studies (14) and Adverse Reactions (6)].
Data are not available to assess the safety and immunogenicity of Menactra and DTaP-containing vaccines when administered concomitantly at 15 months of age.
Pneumococcal antibody responses to some serotypes in PCV7 were decreased following co-administration of Menactra vaccine and PCV7 [see Concomitant Vaccine Administration (14.3)].
Do not mix Menactra vaccine with other vaccines in the same syringe. When Menactra vaccine is administered concomitantly with other injectable vaccines, the vaccines should be administered with different syringes and given at separate injection sites.
Immunosuppressive therapies, including irradiation, antimetabolites, alkylating agents, cytotoxic drugs, and corticosteroids (used in greater than physiologic doses) may reduce the immune response to vaccines.
USE IN SPECIFIC POPULATIONS
- Safety and effectiveness of Menactra vaccine have not been established in children younger than 9 months of age, pregnant women, nursing mothers, and adults older than 55 years of age. ( 8.1, 8.3, 8.4, 8.5)
- A pregnancy registry is available. Contact Sanofi Pasteur Inc. at 1-800-822-2463. ( 8.1)
Pregnancy Category C
Animal reproduction studies have not been conducted with Menactra vaccine. It is also not known whether Menactra vaccine can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. There are no adequate and well controlled studies in pregnant women. Menactra vaccine should only be given to a pregnant woman if clearly needed. Assessment of the effects on animal reproduction has not been fully conducted with Menactra vaccine as effects on male fertility in animals has not been evaluated. The effect of Menactra vaccine on embryo-fetal and pre-weaning development was evaluated in one developmental toxicity study in mice. Animals were administered Menactra vaccine on Day 14 prior to gestation and during the period of organogenesis (gestation Day 6) . The total dose given per time point was 0.1 mL/mouse via intramuscular injection (900 times the human dose, adjusted by body weight). There were no adverse effects on pregnancy, parturition, lactation or pre-weaning development noted in this study. Skeletal examinations revealed one fetus (1 of 234 examined) in the vaccine group with a cleft palate. None were observed in the concurrent control group (0 of 174 examined). There are no data that suggest that this isolated finding is vaccine-related, and there were no vaccine-related fetal malformations or other evidence of teratogenesis observed in this study.
Healthcare providers are encouraged to register women who receive Menactra vaccine during pregnancy in Sanofi Pasteur Inc.'s vaccination pregnancy registry by calling 1-800-822-2463.
It is not known whether Menactra vaccine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Menactra vaccine is administered to a nursing woman.
Menactra vaccine is not approved for use in infants under 9 months of age. Available data show that infants administered three doses of Menactra vaccine (at 2, 4, and 6 months of age) had diminished responses to each meningococcal vaccine serogroup compared to older children given two doses at 9 and 12 months of age.
Safety and effectiveness of Menactra vaccine in adults older than 55 years of age have not been established.
DESCRIPTION
Menactra ®, Meningococcal (Groups A, C, Y and W-135) Polysaccharide Diphtheria Toxoid Conjugate Vaccine, is a sterile, intramuscularly administered vaccine that contains Neisseria meningitidis serogroup A, C, Y and W-135 capsular polysaccharide antigens individually conjugated to diphtheria toxoid protein. N meningitidis A, C, Y and W-135 strains are cultured on Mueller Hinton agar (3) and grown in Watson Scherp (4) media containing casamino acid. The polysaccharides are extracted from the N meningitidis cells and purified by centrifugation, detergent precipitation, alcohol precipitation, solvent extraction and diafiltration. To prepare the polysaccharides for conjugation, they are depolymerized, derivatized, and purified by diafiltration. Diphtheria toxin is derived from Corynebacterium diphtheriae grown in modified culture medium containing hydrolyzed casein (5) and is detoxified using formaldehyde. The diphtheria toxoid protein is purified by ammonium sulfate fractionation and diafiltration. The derivatized polysaccharides are covalently linked to diphtheria toxoid and purified by serial diafiltration. The four meningococcal components, present as individual serogroup-specific glycoconjugates, compose the final formulated vaccine. No preservative or adjuvant is added during manufacture. Each 0.5 mL dose may contain residual amounts of formaldehyde of less than 2.66 mcg (0.000532%), by calculation. Potency of Menactra vaccine is determined by quantifying the amount of each polysaccharide antigen that is conjugated to diphtheria toxoid protein and the amount of unconjugated polysaccharide present.
Menactra vaccine is manufactured as a sterile, clear to slightly turbid liquid. Each 0.5 mL dose of vaccine is formulated in sodium phosphate buffered isotonic sodium chloride solution to contain 4 mcg each of meningococcal A, C, Y and W-135 polysaccharides conjugated to approximately 48 mcg of diphtheria toxoid protein carrier.
The vial stopper is not made with natural rubber latex.
CLINICAL PHARMACOLOGY
The presence of bactericidal anti-capsular meningococcal antibodies has been associated with protection from invasive meningococcal disease (6) (7). Menactra vaccine induces the production of bactericidal antibodies specific to the capsular polysaccharides of serogroups A, C, Y and W-135.
NONCLINICAL TOXICOLOGY
Menactra vaccine has not been evaluated for carcinogenic or mutagenic potential, or for impairment of fertility.
CLINICAL STUDIES
The serum bactericidal assay (SBA) used to test sera contained an exogenous complement source that was either human (SBA-H) or baby rabbit (SBA-BR). (8)
The response to vaccination following two doses of vaccine administered to children 9 and 12 months of age and following one dose of vaccine administered to children 2 through 10 years of age was evaluated by the proportion of subjects having an SBA-H antibody titer of 1:8 or greater, for each serogroup. In individuals 11 through 55 years of age, the response to vaccination with a single dose of vaccine was evaluated by the proportion of subjects with a 4-fold or greater increase in bactericidal antibody to each serogroup as measured by SBA-BR. For individuals 2 through 55 years of age, vaccine efficacy after a single dose was inferred from the demonstration of immunologic equivalence to a US-licensed meningococcal polysaccharide vaccine, Menomune – A/C/Y/W-135 vaccine as assessed by SBA.
Children 9 through 12 Months of Age
In a randomized, US, multi-center trial, children received Menactra vaccine at 9 months and 12 months of age. The first Menactra dose was administered alone, followed by a second Menactra vaccine dose given alone (N=404), or with MMRV (N=302), or with PCV7 (N=422). For all participants, sera were obtained approximately 30 days after last vaccination. There were no substantive differences in demographic characteristics between the vaccine groups. The median age range for administration of the first dose of Menactra was 278-279 days of age.
| Vaccinations administered at 12 months of age following a dose of Menactra at 9 months of age | |||||||
|---|---|---|---|---|---|---|---|
| Menactra vaccine | Menactra + MMRV vaccines | Menactra + PCV7 vaccines | |||||
| (N=272-277) † | (N=177-180) 45 | (N=264-267) 45 | |||||
| Serogroup | (95% CI) ‡ | (95% CI) 46 | (95% CI) 46 | ||||
| A | % ≥1:8 § | 95.6 | (92.4; 97.7) | 92.7 | (87.8; 96.0) | 90.5 | (86.3; 93.8) |
| GMT | 54.9 | (46.8; 64.5) | 52.0 | (41.8; 64.7) | 41.0 | (34.6; 48.5) | |
| C | % ≥1:8 47 | 100.0 | (98.7; 100.0) | 98.9 | (96.0; 99.9) | 97.8 | (95.2; 99.2) |
| GMT | 141.8 | (123.5; 162.9) | 161.9 | (136.3; 192.3) | 109.5 | (94.1; 127.5) | |
| Y | %≥1:8 47 | 96.4 | (93.4; 98.2) | 96.6 | (92.8; 98.8) | 95.1 | (91.8; 97.4) |
| GMT | 52.4 | (45.4; 60.6) | 60.2 | (50.4; 71.7) | 39.9 | (34.4; 46.2) | |
| W-135 | %≥1:8 47 | 86.4 | (81.8; 90.3) | 88.2 | (82.5; 92.5) | 81.2 | (76.0; 85.7) |
| GMT | 24.3 | (20.8; 28.3) | 27.9 | (22.7; 34.3) | 17.9 | (15.2; 21.0) | |
Administration of Menactra to children at 12 months and 15 months of age was evaluated in a US study. Prior to the first dose, 33.3% [n=16/48] of participants had an SBA-H titer ≥1:8 to Serogroup A, and 0-2% [n=0-1 of 50-51] to Serogroups C, Y and W-135. After the second dose, percentages of participants with an SBA-H titer ≥1:8 were: 85.2%, Serogroup A [n=46/54]; 100.0%, Serogroup C [n=54/54]; 96.3%, Serogroup Y [n=52/54]; 96.2%, Serogroup W-135 [n=50/52].
Individuals 2 through 55 Years of Age
Immunogenicity was evaluated in three comparative, randomized, US, multi-center, active controlled clinical trials that enrolled children (2 through 10 years of age), adolescents (11 through 18 years of age), and adults (18 through 55 years of age). Participants received a single dose of Menactra vaccine (N=2526) or Menomune – A/C/Y/W-135 vaccine (N=2317). For all age groups studied, sera were obtained before and approximately 28 days after vaccination. [Blinding procedures for safety assessments are described in Adverse Reactions (6).]
In each of the trials, there were no substantive differences in demographic characteristics between the vaccine groups, between immunogenicity subsets or the overall study population. In the study of children 2 through 10 years of age, the median age of participants was 3 years; 95% completed the study. In the adolescent trial, the median age for both groups was 14 years; 99% completed the study. In the adult trial, the median age for both groups was 24 years; 94% completed the study.
Immunogenicity in Children 2 through 10 Years of Age
Of 1408 enrolled children 2 through 10 years of age, immune responses evaluated in a subset of Menactra vaccine participants (2 through 3 years of age, n=52; 4-10 years of age, n=84) and Menomune – A/C/Y/W-135 vaccine participants (2 through 3 years of age, n=53; 4-10 years of age, n=84) were comparable for all four serogroups (Table 6).
| Ages 2 through 3 Years | Ages 4 through 10 Years | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Menactra vaccine | Menomune – A/C/Y/W-135 vaccine | Menactra vaccine | Menomune – A/C/Y/W-135 vaccine | ||||||
| N †=48-52 | N 49=50-53 | N 49=84 | N 49=84 | ||||||
| Serogroup | (95% CI) ‡ | (95% CI) 50 | (95% CI) 50 | (95% CI) 50 | |||||
| A | % ≥1:8 § | 73 | (59,84) | 64 | (50,77) | 81 | (71,89) | 55 | (44,66) |
| GMT | 10 | (8,13) | 10 | (7,12) | 19 | (14,26) | 7 | (6,9) | |
| C | % ≥1:8 51 | 63 | (48,76) | 38 | (25,53) | 79 | (68,87) | 48 | (37,59) |
| GMT | 27 | (14,52) | 11 | (5,21) | 28 | (19,41) | 12 | (7,18) | |
| Y | % ≥1:8 51 | 88 | (75,95) | 73 | (59,84) | 99 | (94,100) | 92 | (84,97) |
| GMT | 51 | (31,84) | 18 | (11,27) | 99 | (75,132) | 46 | (33,66) | |
| W-135 | % ≥1:8 51 | 63 | (47,76) | 33 | (20,47) | 85 | (75,92) | 79 | (68,87) |
| GMT | 15 | (9,25) | 5 | (3,6) | 24 | (18,33) | 20 | (14,27) | |
In the subset of participants 2 through 3 years of age with undetectable pre-vaccination titers (ie, SBA-H titers <1:4 at Day 0), seroconversion rates (defined as the proportions of participants with SBA-H titers ≥1:8 by Day 28) were similar between the Menactra vaccine and Menomune – A/C/Y/W-135 vaccine recipients. Menactra vaccine participants achieved seroconversion rates of: 57%, Serogroup A (n=12/21); 62%, Serogroup C (n=29/47); 84%, Serogroup Y (n=26/31); 53%, Serogroup W-135 (n=20/38). The seroconversion rates for Menomune – A/C/Y/W-135 vaccine recipients were: 55%, Serogroup A (n=16/29); 30%, Serogroup C (n=13/43); 57%, Serogroup Y (n=17/30); 26%, Serogroup W-135 (n=11/43).
In the subset of participants 4 through 10 years of age with undetectable pre-vaccination titers (ie, SBA-H titers <1:4 at Day 0), seroconversion rates (defined as the proportions of participants with SBA-H titers ≥1:8 by Day 28) were similar between the Menactra vaccine and Menomune – A/C/Y/W-135 vaccine recipients. Menactra vaccine participants achieved seroconversion rates of: 69%, Serogroup A (n=11/16); 81%, Serogroup C (n=50/62); 98%, Serogroup Y (n=45/46); 69%, Serogroup W-135 (n=27/39). The seroconversion rates for Menomune – A/C/Y/W-135 vaccine recipients were: 48%, Serogroup A (n=10/21); 38%, Serogroup C (n=19/50); 84%, Serogroup Y (n=38/45); 68%, Serogroup W-135 (n=26/38).
Immunogenicity in Adolescents 11 through 18 Years of Age
Results from the comparative clinical trial conducted in 881 adolescents aged 11 through 18 years showed that the immune responses to Menactra vaccine and Menomune – A/C/Y/W-135 vaccine were similar for all four serogroups (Table 7).
In participants with undetectable pre-vaccination titers (ie, SBA-BR titers <1:8 at Day 0), seroconversion rates (defined as the proportions of participants achieving a ≥4-fold rise in SBA-BR titers by Day 28) were similar between the Menactra vaccine and Menomune – A/C/Y/W-135 vaccine recipients. Menactra vaccine participants achieved seroconversion rates of: 100%, Serogroup A (n=81/81); 99%, Serogroup C (n=153/155); 98%, Serogroup Y (n=60/61); 99%, Serogroup W-135 (n=161/164). The seroconversion rates for Menomune – A/C/Y/W-135 vaccine recipients were: 100%, Serogroup A (n=93/93); 99%, Serogroup C (n=151/152); 100%, Serogroup Y (n=47/47); 99%, Serogroup W-135 (n=138/139).
Immunogenicity in Adults 18 through 55 Years of Age
Results from the comparative clinical trial conducted in 2554 adults aged 18 through 55 years showed that the immune responses to Menactra vaccine and Menomune – A/C/Y/W-135 vaccine were similar for all four serogroups (Table 7).
| Ages 11 through 18 Years | Ages 18 through 55 Years | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Menactra vaccine | Menomune – A/C/Y/W-135 vaccine | Menactra vaccine | Menomune – A/C/Y/W-135 vaccine | ||||||
| N †=423 | N 53=423 | N 53=1280 | N 53=1098 | ||||||
| Serogroup | (95% CI) ‡ | (95% CI) 54 | (95% CI) 54 | (95% CI) 54 | |||||
| A | % ≥4-fold rise § | 92.7 | (89.8, 95.0) | 92.4 | (89.5, 94.8) | 80.5 | (78.2, 82.6) | 84.6 | (82.3, 86.7) |
| GMT | 5483 | (4920, 6111) | 3246 | (2910, 3620) | 3897 | (3647, 4164) | 4114 | (3832, 4417) | |
| C | % ≥4-fold rise 55 | 91.7 | (88.7, 94.2) | 88.7 | (85.2, 91.5) | 88.5 | (86.6, 90.2) | 89.7 | (87.8, 91.4) |
| GMT | 1924 | (1662, 2228) | 1639 | (1406, 1911) | 3231 | (2955, 3533) | 3469 | (3148, 3823) | |
| Y | % ≥4-fold rise 55 | 81.8 | (77.8, 85.4) | 80.1 | (76.0, 83.8) | 73.5 | (71.0, 75.9) | 79.4 | (76.9, 81.8) |
| GMT | 1322 | (1162, 1505) | 1228 | (1088, 1386) | 1750 | (1597, 1918) | 2449 | (2237, 2680) | |
| W-135 | % ≥4-fold rise 55 | 96.7 | (94.5, 98.2) | 95.3 | (92.8, 97.1) | 89.4 | (87.6, 91.0) | 94.4 | (92.8, 95.6) |
| GMT | 1407 | (1232, 1607) | 1545 | (1384, 1725) | 1271 | (1172, 1378) | 1871 | (1723, 2032) | |
In participants with undetectable pre-vaccination titers (ie, SBA-BR titers <1:8 at Day 0), seroconversion rates (defined as the proportions of participants achieving a ≥4-fold rise in SBA-BR titers by Day 28) were similar between the Menactra vaccine and Menomune – A/C/Y/W-135 vaccine recipients. Menactra vaccine participants achieved seroconversion rates of: 100%, Serogroup A (n=156/156); 99%, Serogroup C (n=343/345); 91%, Serogroup Y (n=253/279); 97%, Serogroup W-135 (n=360/373). The seroconversion rates for Menomune – A/C/Y/W-135 vaccine recipients were: 99%, Serogroup A (n=143/144); 98%, Serogroup C (n=297/304); 97%, Serogroup Y (n=221/228); 99%, Serogroup W-135 (n=325/328).
Immunogenicity in Adolescents and Adults Following Booster Vaccination
[For a description of the study design and number of participants, see Clinical Trials Experience, Booster Vaccination Study (6.1).] Prior to revaccination, the percentage of subjects (n=781) with an SBA-H titer ≥1:8 were 64.5%, 44.2%, 38.7%, and 68.5% for Serogroups A, C, Y, and W-135, respectively. Among the subset of trial participants (n=112) for whom SBA-H responses at Day 6 were assessed, 86.6%, 91.1%, 94.6%, and 92.0% achieved a ≥4-fold rise in SBA-H titer for Serogroups A, C, Y, and W-135, respectively. The proportions of participants (n=781) who achieved a ≥4-fold rise in SBA-H titer by Day 28 were 95.0%, 95.3%, 97.1%, and 96% for Serogroups A, C, Y, and W-135, respectively. The proportions of participants who achieved an SBA-H titer ≥1:8 by Day 28 were >99% for each serogroup.
MMRV (or MMR+V) or PCV7
In a US, active-controlled trial, 1179 children received Menactra vaccine at 9 months and 12 months of age. At 12 months of age these children received Menactra concomitantly with MMRV (N=616), or MMR+V (N=48), or PCV7 (N=250). Another group of 12-month old children received MMRV+PCV7 (N=485). Sera were obtained approximately 30 days after the last vaccinations. Measles, mumps, rubella and varicella antibody responses among children who received Menactra vaccine and MMRV (or MMR and V) were comparable to corresponding antibody responses among children who received MMRV and PCV7.
When Menactra was given concomitantly with PCV7, the non-inferiority criteria for comparisons of pneumococcal IgG GMCs (upper limit of the two-sided 95% CI of the GMC ratio ≤2) were not met for 3 of 7 serotypes (4, 6B, 18C). In a subset of subjects with available sera, pneumococcal opsonophagocytic assay GMT data were consistent with IgG GMC data.
Td
In a double-blind, randomized, controlled trial, 1021 participants aged 11 through 17 years received Td and Menactra vaccines concomitantly (N=509), or Td followed one month later by Menactra vaccine (N=512). Sera were obtained approximately 28 days after each respective vaccination. The proportions of participants with a 4-fold or greater increase in SBA-BR titer to meningococcal Serogroups C, Y and W-135 were higher when Menactra vaccine was given concomitantly with Td (86-96%) than when Menactra vaccine was given one month following Td (65-91%). Anti-tetanus and anti-diphtheria antibody responses were similar in both study groups.
Typhim Vi
In a double-blind, randomized, controlled trial, 945 participants aged 18 through 55 years received Typhim Vi and Menactra vaccines concomitantly (N=469), or Typhim Vi vaccine followed one month later by Menactra vaccine (N=476). Sera were obtained approximately 28 days after each respective vaccination. The antibody responses to Menactra vaccine and to Typhim Vi vaccine components were similar in both study groups.
- 44
- Serum bactericidal assay with an exogenous human complement (SBA-H) source.
- 45
- N=Number of participants with at least one valid serology result from a blood sample obtained between Days 30 to 44 post vaccination.
- 46
- 95% CIs for the proportions are calculated based on the Clopper-Pearson Exact method and normal approximation for that of the GMTs.
- 47
- The proportion of participants achieving an SBA-H titer of at least 1:8 thirty days after the second dose of Menactra vaccine.
- 48
- Serum bactericidal assay with an exogenous human complement (SBA-H) source.
- 49
- N=Number of subset participants with at least one valid serology result at Day 0 and Day 28.
- 50
- The 95% CI for the Geometric Mean Titer (GMT) was calculated based on an approximation to the normal distribution.
- 51
- The proportion of participants achieving an SBA-H titer of at least 1:8 was assessed using a 10% non-inferiority margin and a one-sided Type 1 error rate of 0.025.
- 52
- Serum bactericidal assay with baby rabbit complement (SBA-BR).
- 53
- N=Number of subset participants with at least one valid serology result at Day 0 and Day 28.
- 54
- The 95% CI for the Geometric Mean Titer (GMT) was calculated based on an approximation to the normal distribution.
- 55
- Menactra vaccine was non-inferior to Menomune – A/C/Y/W-135 vaccine. Non-inferiority was assessed by the proportion of participants with a 4-fold or greater rise in SBA-BR titer for
REFERENCES
1CDC. Guillain-Barré syndrome among recipients of Menactra® meningococcal conjugate vaccine-United States, June 2005-September 2006. MMWR Morb Mortal Wkly Rep 2006;55:1120-1124. Erratum in: MMWR Morb Mortal Wkly Rep 2006;55(43):1177.2Harvard Medical School/Harvard Pilgrim Health Care Institute. Risk of Guillain-Barré Syndrome Following Meningococcal Conjugate (MCV4) Vaccination. Final Study Report, Revised March 11, 2010.3Mueller JH, et al. A protein-free medium for primary isolation of the gonococcus and meningococcus. Proc Soc Exp Biol Med 1941;48:330-333.4Watson RG, et al. The specific hapten of group C (group IIa) meningococcus. I. Preparation and immunological behavior. J Immunol 1958;81:331-336.5Mueller JH, et al. Production of diphtheria toxin of high potency (100 Lf) on a reproducible medium. J Immunol 1941;40:21-32.6Mäkelä PH, et al. Evolution of conjugate vaccines. Expert Rev Vaccines 2002;1:399-410.7Goldschneider I, et al. Human immunity to the meningococcus. I. The role of humoral antibodies. J Exp Med 1969;129:1307-1326.8Maslanka SE, et al. Standardization and a multilaboratory comparison of Neisseria meningitidis serogroup A and C serum bactericidal assays. Clin and Diag Lab Immunol 1997;4:156-167.
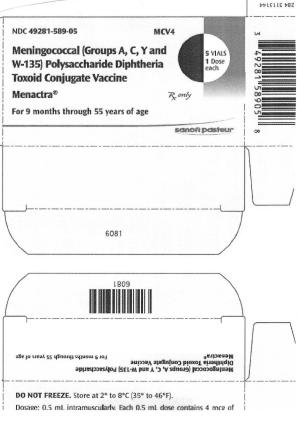
HOW SUPPLIED
- Single-dose vial, 0.5 mL (NDC 49281-589-58). Supplied as a package of 5 vials (NDC 49281-589-05).
Store at 2° to 8°C (35° to 46°F). DO NOT FREEZE. Frozen/previously frozen product should not be used. Do not use after the expiration date.
INFORMATION FOR PATIENTS
Vaccine Information Statements are required by the National Childhood Vaccine Injury Act of 1986 to be given prior to immunization to the patient, parent, or guardian. These materials are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines.)
Inform the patients, parents or guardians about:
- Potential benefits and risks of immunization with Menactra vaccine.
- Potential for adverse reactions that have been temporally associated with administration of Menactra vaccine or other vaccines containing similar components.
- Reporting any adverse reactions to their healthcare provider.
- The Sanofi Pasteur Inc. Pregnancy Registry, as appropriate.
SPL UNCLASSIFIED
Menactra vaccine is a registered trademark of Sanofi Pasteur Inc.
Manufactured by:
Sanofi Pasteur Inc.
Swiftwater PA 18370 USA
6463
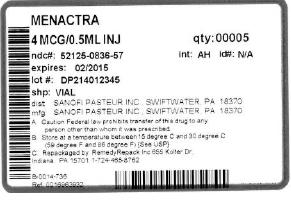
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
DRUG: Menactra
GENERIC: NEISSERIA MENINGITIDIS GROUP A CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN, NEISSERIA MENINGITIDIS GROUP C CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN, NEISSERIA MENINGITIDIS GROUP Y CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN, and NEISSERIA MENINGITIDIS GROUP W-135 CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN
DOSAGE: INJECTION, SOLUTION
ADMINSTRATION: INTRAMUSCULAR
NDC: 52125-836-57
ACTIVE INGREDIENT(S):
- NEISSERIA MENINGITIDIS GROUP A CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN 4ug in 0.5mL
- NEISSERIA MENINGITIDIS GROUP Y CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN 4ug in 0.5mL
- NEISSERIA MENINGITIDIS GROUP C CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN 4ug in 0.5mL
- NEISSERIA MENINGITIDIS GROUP W-135 CAPSULAR POLYSACCHARIDE DIPHTHERIA TOXOID CONJUGATE ANTIGEN 4ug in 0.5mL
INACTIVE INGREDIENT(S):
- formaldehyde
PACKAGING: 0.5 mL in 1 VIAL, SINGLE-DOSE
| MENACTRA
neisseria meningitidis group a capsular polysaccharide diphtheria toxoid conjugate antigen, neisseria meningitidis group c capsular polysaccharide diphtheria toxoid conjugate antigen, neisseria meningitidis group y capsular polysaccharide diphtheria toxoid conjugate antigen, and neisseria meningitidis group w-135 capsular polysaccharide diphtheria toxoid conjugate antigen injection, solution |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - REMEDYREPACK INC. (829572556) |